Young's Modulus in Bioelectronics: Engineering Soft Materials for Seamless Tissue Integration and Advanced Therapies
This article provides a comprehensive analysis of Young's modulus as a critical design parameter in bioelectronic materials.
Young's Modulus in Bioelectronics: Engineering Soft Materials for Seamless Tissue Integration and Advanced Therapies
Abstract
This article provides a comprehensive analysis of Young's modulus as a critical design parameter in bioelectronic materials. Tailored for researchers, scientists, and drug development professionals, it explores the fundamental challenge of mechanical mismatch with biological tissues, surveys innovative material strategies like hydrogels and soft composites, and details optimization techniques for enhanced device stability and signal fidelity. The content further covers rigorous validation methodologies and comparative analyses of material performance, offering a holistic guide for developing next-generation bioelectronic implants and therapies that seamlessly integrate with the body.
The Mechanical Mismatch Problem: Why Young's Modulus is Critical for Biointegration
Defining Young's Modulus and Its Significance in Bioelectronic Interfaces
Young's modulus, a fundamental mechanical property quantifying material stiffness, has emerged as a critical parameter in the development of advanced bioelectronic interfaces. This technical guide examines the definition and calculation of Young's modulus, explores its pivotal role in ensuring mechanical compatibility between electronic devices and biological tissues, and details experimental methodologies for its characterization. The convergence of materials science and biomedical engineering has positioned Young's modulus as a central design criterion for next-generation bioelectronic systems that maintain long-term stability and functionality within biological environments. By establishing clear relationships between material stiffness and biointerface performance, this review provides researchers with foundational knowledge and practical frameworks for developing mechanically-compliant bioelectronic devices.
Young's modulus (E), also referred to as the elastic modulus, is a fundamental mechanical property that quantifies the stiffness of a solid material. It is defined as the ratio of stress (force per unit area) to strain (proportional deformation) in a material within the linear elasticity regime of a uniaxial deformation [1] [2]. This property serves as a direct measure of a material's resistance to elastic deformation under applied load, with higher values indicating greater stiffness.
The mathematical expression of Young's modulus is derived from Hooke's Law for elastic materials:
E = σ/ε
Where:
- E is Young's modulus (Pa or GPa)
- σ is the tensile stress (force per unit area, F/A)
- ε is the axial strain (change in length per original length, ΔL/L₀) [1]
This relationship can be expanded to the practical calculation form:
E = (F × L₀) / (A × ΔL)
Where F is the applied force, A is the cross-sectional area, L₀ is the original length, and ΔL is the change in length [1]. In essence, materials with a high Young's modulus (such as metals and ceramics) deform minimally under applied stress, while those with a low Young's modulus (such as rubbers and gels) exhibit significant deformation under the same conditions [2].
The conceptual understanding of Young's modulus can be traced to 18th-century experiments by Giordano Riccati, though it bears the name of the 19th-century British scientist Thomas Young [1]. Its significance extends across engineering disciplines, particularly in bioelectronics, where it determines how seamlessly synthetic materials can integrate with biological systems.
The Critical Role of Young's Modulus in Bioelectronic Interfaces
The Mechanical Mismatch Challenge
Bioelectronic interfaces bridge the divide between electronic devices and biological tissues, enabling advanced monitoring, regulation, and interaction with living organisms [3]. A fundamental challenge in this field stems from the significant discrepancy between the mechanical properties of conventional electronic materials and those of biological tissues:
- Conventional electronics typically utilize rigid materials like silicon and metals with Young's moduli in the gigapascal (GPa) range (e.g., silicon ~130-180 GPa, gold ~79 GPa) [4] [5]
- Biological tissues are soft, dynamic structures with moduli in the kilopascal (kPa) range (e.g., brain tissue ~1-4 kPa, skin ~0.5-2 MPa) [6] [7]
This mechanical mismatch of several orders of magnitude creates substantial challenges at the biointerface. Traditional rigid devices interact with tissues as de facto foreign bodies, leading to:
- Inflammation and fibrotic encapsulation through the foreign body response [8]
- Tissue damage and chronic inflammation during natural tissue movement [5]
- Unstable electrical interfaces and signal degradation over time [5]
- Device failure due to shear stresses and micromotion at the tissue-device interface [4]
Consequences of Mechanical Mismatch
The biological response to mechanically mismatched implants significantly compromises device functionality. Following implantation, the body recognizes stiff materials as foreign, triggering a cascade of events including protein adsorption, inflammatory cell recruitment, and fibroblast activation. This ultimately results in the formation of a fibrous capsule that isolates the device from the target tissue [8].
For neural interfaces, this fibrotic response is particularly detrimental. The encapsulation layer:
- Increases electrode impedance, reducing signal-to-noise ratio in recording applications [5]
- Elevates stimulation thresholds, requiring higher currents for effective neuromodulation [8]
- Physically displaces electrodes from their target neurons, diminishing spatial resolution [5]
Studies have demonstrated that rigid microelectrodes experience significant signal degradation over weeks to months as this foreign body response progresses [5]. Furthermore, the mechanical strain concentration at the interface between moving tissue and stiff implants can lead to both tissue damage and device failure through fatigue or delamination [6].
Quantitative Analysis of Young's Modulus in Biological and Synthetic Materials
Young's Modulus of Biological Tissues
Table 1: Young's Modulus Ranges of Biological Tissues and Conventional Electronics
| Material Category | Specific Material/Tissue | Young's Modulus Range | Citation |
|---|---|---|---|
| Neural Tissue | Brain Tissue | 1 - 4 kPa | [7] |
| Peripheral Tissues | Skin | 0.5 - 2 MPa | [6] |
| Cardiac Tissue | Heart | 100 - 500 kPa | [6] |
| Conventional Electronics | Silicon | 130 - 180 GPa | [5] |
| Conventional Electronics | Metals (Gold, Platinum) | 70 - 170 GPa | [4] |
| Conventional Electronics | Traditional Elastomers | 1 - 10 MPa | [6] |
Young's Modulus of Advanced Bioelectronic Materials
Table 2: Young's Modulus of Advanced Bioelectronic Materials
| Material Category | Specific Material | Young's Modulus | Tissue Compatibility | Citation |
|---|---|---|---|---|
| Conductive Polymers | PEDOT:PSS (annealed) | 1.1 MPa - 1.5 GPa | Moderate | [7] |
| Conductive Polymers | PEDOT:PSS (hydrogel) | 31 kPa | High for brain | [7] |
| Hydrogels | PVA/PAAm | 1 - 100 kPa | High for soft tissues | [6] |
| Elastomers | PDMS | 0.5 - 4 MPa | Moderate | [6] |
| Nanocomposites | PEDOT:PSS-PVA Hydrogel | 191 kPa | High for brain | [7] |
| Nanocomposites | Conductive Hydrogels | 2 - 31 kPa | High for soft tissues | [7] |
The data reveals that advanced bioelectronic materials can be engineered to closely match the mechanical properties of target tissues. Hydrogels and certain conductive polymer formulations achieve the kPa range required for neural interfaces, while moderately stiff elastomers in the MPa range may be suitable for peripheral applications.
Theoretical Frameworks for Conformability and Mechanical Integration
The ability of a bioelectronic device to conform to biological surfaces is governed by theoretical models that balance bending energy, adhesion energy, and tissue deformation. For rough surfaces like skin, theoretical models represent the surface as a sinusoidal profile and calculate the total energy of the conformal system as [3]:
Ūconformal = Ūbending + Ūskin + Ūadhesion
Where conformal attachment requires Ūconformal < 0. This model derives the conformability criterion for bioelectronics [3]:
πh²/γλ < 16/Eskin + λ³/π³EI
Where h represents wrinkle amplitude, λ represents wavelength, γ represents the skin-electronics interfacial energy coefficient, E_skin represents Young's modulus of the skin, and EI represents the effective bending stiffness of the bioelectronics.
For non-developable surfaces (with non-zero Gaussian curvature) like spherical organ surfaces, the conformability challenge increases. A model for mounting a circular thin film on a rigid sphere establishes the stability criterion for full conformability [3]:
Rf⁴/128Rs⁴ + h²/12(1-ν)Rs² ≤ λ/Eh
Where Rf and Rs are the radii of the film and sphere, h is film thickness, E is Young's modulus, ν is Poisson's ratio, and λ is the interfacial energy coefficient. This model indicates that optimal conformal attachment to spherical surfaces requires small size ratios, minimal thickness, and soft materials with low modulus [3].
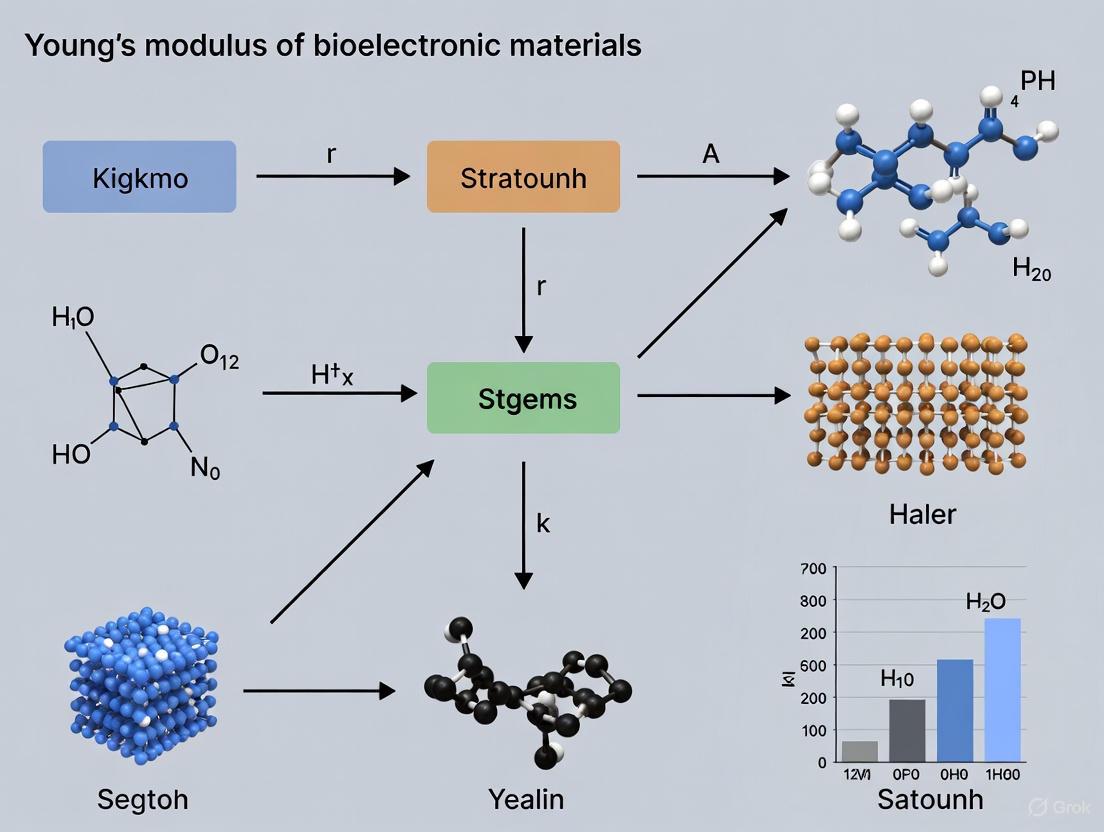
Diagram 1: Theoretical framework for bioelectronic conformability on biological surfaces, illustrating how material properties, surface geometry, and interfacial interactions determine interface stability.
Experimental Methodologies for Young's Modulus Characterization
Tensile Testing of Bulk Materials
The standard method for determining Young's modulus of bioelectronic materials involves uniaxial tensile testing, which provides direct stress-strain data for modulus calculation:
Protocol:
- Sample Preparation: Prepare dog-bone shaped specimens of standardized dimensions (e.g., ASTM D638) using solution casting, 3D printing, or microfabrication techniques
- Mounting: Secure the specimen in the tensile testing grips with careful alignment to avoid torsional stresses
- Testing Parameters: Apply uniaxial tension at a constant strain rate (typically 1-10 mm/min for soft materials) while measuring force and displacement
- Data Collection: Record stress (force/original cross-sectional area) and strain (change in length/original length) simultaneously
- Modulus Calculation: Determine Young's modulus as the slope of the initial linear portion of the stress-strain curve (typically 0-10% strain for elastic materials) [1] [2]
For highly compliant materials like hydrogels, specialized equipment with low-force load cells (0.1-10N range) is essential for accurate measurements. Environmental control may be necessary to maintain hydration during testing.
Nanoindentation for Thin Films and Biological Tissues
Nanoindentation provides localized mechanical characterization crucial for thin-film bioelectronic materials and biological tissues:
Protocol:
- Sample Preparation: Mount thin films on rigid substrates or prepare tissue sections with minimal alteration to native mechanical properties
- Tip Selection: Choose appropriate indenter geometry (spherical tips for soft materials, Berkovich for stiffer materials)
- Testing Parameters:
- Apply controlled force or displacement sequences with precise spatial positioning
- Implement appropriate hold periods to account for viscoelastic relaxation
- Conduct multiple tests across different sample regions for statistical significance
- Data Analysis: Extract reduced modulus from force-displacement curves using Oliver-Pharr method, then calculate Young's modulus considering Poisson's ratio [6]
This technique is particularly valuable for characterizing the mechanical properties of conductive polymer coatings and hydrogel-based electrodes at biologically relevant length scales.
Electrical-Mechanical Correlation Measurements
Advanced characterization couples mechanical testing with electrical measurements to simulate operational conditions:
Protocol:
- Integrated Setup: Combine tensile testing apparatus with impedance analyzers or source-measure units
- Simultaneous Monitoring: Measure electrical properties (conductivity, impedance) while applying mechanical strain
- Cyclic Testing: Subject materials to repeated loading-unloading cycles to assess electromechanical durability
- Environmental Control: Conduct tests in physiologically relevant environments (aqueous solutions, 37°C) [7]
This approach provides critical insights into how the electrical functionality of bioelectronic materials withstands the mechanical deformations encountered in biological environments.
Diagram 2: Comprehensive workflow for Young's modulus characterization of bioelectronic materials, highlighting method selection based on material properties and application requirements.
The Scientist's Toolkit: Essential Materials for Mechanically-Matched Bioelectronics
Table 3: Essential Research Reagents and Materials for Bioelectronic Interfaces
| Material Category | Specific Examples | Key Functions | Young's Modulus Range | Citation |
|---|---|---|---|---|
| Conductive Polymers | PEDOT:PSS, PANI, PPy | Electrode material, Conductive traces | 1 kPa - 1 GPa (tunable) | [7] |
| Hydrogel Matrices | PVA, PAAm, Gelatin, Alginate | Tissue-integration, Drug delivery | 1 - 100 kPa | [6] |
| Elastomers | PDMS, Ecoflex, SEBS | Substrate material, Encapsulation | 0.1 - 4 MPa | [6] |
| Conductive Nanofillers | Gold nanowires, Carbon nanotubes, Graphene | Enhancing conductivity, Mechanical reinforcement | Varies by composition | [6] |
| Dynamic Polymers | Polyelectrolytes, Stimuli-responsive polymers | Electrically tunable mechanical properties | Modulable via electric fields | [9] |
| Bioresorbable Materials | PLGA, PLA, Silk fibroin | Temporary implants, Reduced extraction surgery | 0.5 - 5 GPa | [4] |
Emerging Trends and Future Perspectives
Electrically Tunable Mechanical Properties
Recent research has revealed that certain polyelectrolyte materials exhibit electric field-dependent mechanical properties, opening possibilities for dynamically adjustable biointerfaces. Molecular dynamics simulations demonstrate that applied electric fields induce orientation changes in polyelectrolyte chains, enhancing attractive interactions between charged monomers and resulting in increased ultimate tensile stress and Young's modulus [9]. This electromechanical coupling enables materials that can dynamically adjust their stiffness in response to electrical stimuli, potentially allowing implants to optimize their mechanical properties for different physiological states.
Multifunctional Nanocomposites
The development of intrinsically stretchable conductive nanocomposites represents a paradigm shift in bioelectronic materials. By integrating conductive nanofillers (metal nanowires, carbon nanotubes, graphene) within soft polymeric matrices (elastomers, hydrogels), researchers have created materials that simultaneously achieve:
- Tissue-matching mechanical properties (Young's modulus: 1 kPa - 1 MPa)
- High electrical conductivity (>100 S/cm)
- Stretchability (>100% strain) [6]
These nanocomposites establish low-impedance conformal interfaces with tissues that are essential for high-fidelity biosignal recording and precise electroceutical interventions.
Closed-Loop Bioelectronic Systems
The integration of mechanically compliant interfaces with wireless technologies and artificial intelligence is enabling next-generation closed-loop therapeutic systems. These systems leverage conformable bioelectronics for continuous physiological monitoring, AI-driven analytics for signal interpretation and prediction, and responsive stimulation for precise therapeutic intervention [6]. The mechanical compatibility of the interface ensures long-term stability of the recording and stimulation capabilities essential for these autonomous systems.
Young's modulus has evolved from a fundamental material property to a critical design parameter in bioelectronic interfaces. The precise matching of mechanical properties between synthetic devices and biological tissues enables stable, long-term integration that is essential for advancing bioelectronic medicine. Through continued innovation in material synthesis, theoretical modeling, and characterization techniques, researchers are developing increasingly sophisticated bioelectronic systems that seamlessly merge with biological environments. The ongoing convergence of materials science, electrical engineering, and biology promises a future where bioelectronic interfaces become indistinguishable from the tissues they monitor and modulate, enabling unprecedented capabilities in healthcare and human enhancement.
A fundamental challenge in bioelectronic medicine is the profound mechanical mismatch between conventional electronic materials and the soft, dynamic tissues of the human body. This stiffness disparity, quantified by Young's modulus (a measure of material stiffness), poses significant barriers to long-term device functionality and biological integration [4]. Traditional electronic materials like silicon and metals possess Young's moduli in the gigapascal (GPa) range, creating orders of magnitude difference with biological tissues that typically exhibit moduli in the kilopascal (kPa) to megapascal (MPa) range [4] [10]. This mechanical mismatch triggers inflammatory responses, fibrotic encapsulation, and device failure through mechanisms including micromotion-induced damage and compromised signal fidelity [4] [8].
The field is consequently undergoing a paradigm shift from rigid to soft, flexible bioelectronic systems. As research advances, precise quantification of this "stiffness gap" becomes imperative for designing next-generation bioelectronic interfaces that seamlessly integrate with target tissues [10]. This whitepaper provides a comprehensive technical analysis of Young's modulus values across biological tissues and electronic materials, details experimental methodologies for modulus characterization, and outlines material strategies to bridge this mechanical divide for enhanced therapeutic outcomes.
Quantitative Analysis of the Stiffness Gap
The mechanical properties of biological tissues and conventional electronics span several orders of magnitude. The following tables provide a comparative analysis of their Young's modulus values, highlighting the fundamental challenge in biointegration.
Table 1: Young's Modulus of Biological Tissues and Synthetic Mimics
| Material Category | Specific Material/Tissue | Young's Modulus | Measurement Context/Notes |
|---|---|---|---|
| Biological Tissues | Soft Tissues (general) | 1 kPa - 100 MPa [10] | Broad range encompassing various organs |
| Agar Gel (Tissue Mimic) | Adjustable based on concentration [11] | Used for its tunable, tissue-like mechanical properties | |
| Electronic Materials | Silicon | ~170 GPa [4] | Conventional semiconductor substrate |
| Metals (e.g., Copper, Gold) | >100 GPa [4] | Conventional wiring and electrodes | |
| Soft Electronic Materials | Polymers & Elastomers | 1 kPa - 1 MPa [4] | Typical range for soft bioelectronics |
| Gallium | 79.37 - 83.84 GPa [12] | Measured between -70°C and 20°C |
Table 2: Young's Modulus of Conventional vs. Soft Bioelectronic Materials
| Property | Rigid Bioelectronics | Soft & Flexible Bioelectronics |
|---|---|---|
| Typical Material Types | Silicon, metals, ceramics [4] | Polymers, elastomers, hydrogels, thin-film materials [4] |
| Young's Modulus | > 1 GPa [4] | 1 kPa – 1 MPa (typically) [4] |
| Bending Stiffness | > 10-6 Nm [4] | < 10-9 Nm [4] |
| Tissue Integration | Stiffness mismatch causes inflammation and fibrotic encapsulation [4] | Soft, conformal materials match tissue mechanics and reduce immune response [4] |
Experimental Protocols for Measuring Young's Modulus
Accurate characterization of mechanical properties is essential for developing compatible bioelectronic interfaces. The following section details standardized and emerging methodologies.
Atomic Force Microscopy (AFM) for Soft Tissues and Organoids
AFM is exceptionally valuable for measuring mechanical properties at the micro- and nanoscale, particularly for soft biological samples like organoids [13].
Protocol Summary: [13]
- Sample Preparation: Embed organoids in Optimal Cutting Temperature (OCT) compound and slice into sections using a cryostat to expose the surface for measurement.
- AFM Setup: Mount the sample and select an appropriate AFM probe (e.g., a spherical tip). Pre-calibrate the probe's spring constant.
- Force Mapping: Program the AFM to perform an array of force-distance curves across the sample surface. The probe approaches, indents, and retracts from the surface at each point.
- Data Analysis: Fit the retraction portion of the force-distance curve using a contact mechanics model (e.g., Hertz, Sneddon) to calculate the local Young's modulus based on the relationship between force and indentation depth.
Indentation Testing and Acoustic Impedance Correlation
For larger, hydrogel-based tissue mimics, a combination of macro-indentation and Scanning Acoustic Microscopy (SAM) provides an effective empirical approach.
Protocol Summary: [11]
- Sample Preparation: Prepare agar gels at various concentrations (e.g., 5% to 20%) to create a range of stiffnesses mimicking biological tissues.
- Acoustic Impedance Measurement: Use SAM to measure the local acoustic impedance (Z) across the sample surface. The acoustic impedance is derived from the reflection coefficient of high-frequency ultrasound.
- Mechanical Indentation Test: Perform indentation tests on the same samples using a mechanical tester to determine the apparent Young's modulus (E) from the force-displacement data.
- Empirical Correlation: Establish a power-law relationship between the measured acoustic impedance and Young's modulus (e.g., ( E = k \cdot Z^m )), which can then be used to estimate modulus from SAM data alone.
Non-Destructive Methods for Engineered Materials
Dynamic methods like the Impulse Excitation Technique (IET) and Ultrasonic (US) testing are crucial for characterizing fabricated materials without destruction.
Protocol Summary: [14]
- Impulse Excitation Technique (IET): A sample is lightly tapped to induce vibration. The fundamental resonant frequency ((ff)) is measured, and Young's modulus ((E)) is calculated using the formula: (E = 0.9465 \cdot (m ff^2 / b) \cdot (L^3 / t^3) \cdot T), where (m), (b), (L), and (t) are mass, width, length, and thickness, and (T) is a correction factor.
- Ultrasonic (US) Method: The speed ((VL)) of an ultrasonic wave traveling through a material is measured. Young's modulus is calculated using (E = VL^2 \cdot \rho \cdot (1+\nu)(1-2\nu)/(1-\nu)), where (\rho) is density and (\nu) is Poisson's ratio.
The Scientist's Toolkit: Essential Reagents and Materials
Developing bioelectronic devices with matched mechanical properties requires a specific set of functional materials.
Table 3: Research Reagent Solutions for Bioelectronics
| Category/Item | Function in Research | Specific Examples & Properties |
|---|---|---|
| Soft Substrates & Insulators | Provide flexible support and electrical insulation; dictate overall device modulus. | Parylene-C: Biocompatible, ultrathin films (<5 μm) for flexible OECTs [10]. PET: Polyethylene terephthalate, used for flexible multifunctional sensing platforms [10]. |
| Soft Conductors | Form stretchable interconnects and electrodes for signal transmission. | PEDOT:PSS: Conductive polymer, active layer in OECTs, compatible with flexible platforms [10]. Silver Nanowires: Used for creating transparent, flexible electrodes [10]. |
| Tissue Mimics & Phantoms | Serve as in vitro models for method development and testing. | Agar Gels: Tunable stiffness by concentration; used to simulate soft tissue mechanics [11]. |
| Stimuli-Responsive Materials | Enable shape-morphing and minimally invasive deployment of devices. | Hydrogels: Injectable, swellable, or moldable for deep tissue access and drug release [4] [10]. Dielectric Elastomers: Used in soft actuators for dynamic device positioning [15]. |
The quantification of the stiffness gap between biological tissues and conventional electronics provides a critical foundation for the future of bioelectronic medicine. The data and methodologies presented herein illuminate a clear path forward: the adoption of soft, flexible, and mechanically compliant materials is not merely an optimization but a necessity for stable long-term integration with the body [4] [10]. Emerging material strategies, including ultraflexible electronics, injectable meshes, and stimuli-responsive composites, are actively bridging this mechanical divide [15]. By prioritizing mechanical compatibility alongside electrical performance, researchers can overcome persistent biological challenges like the foreign body response [8] and unlock a new generation of high-fidelity, chronically stable bioelectronic therapies for a wide spectrum of diseases.
The seamless integration of bioelectronic devices with biological tissues is paramount for the advancement of personalized medicine, neural interfaces, and chronic health monitoring. The mechanical properties of these devices, particularly their stiffness (Young's modulus), play a defining role in their long-term performance and biocompatibility. Biological tissues, such as the brain, skin, and nerves, are intrinsically soft and dynamic, with Young's moduli typically ranging from 0.1 kPa to 100 kPa [4] [16]. In stark contrast, conventional electronic materials like silicon and metals possess moduli in the gigapascal range, creating a significant mechanical mismatch at the tissue-device interface [4] [17].
This mechanical mismatch is not a passive phenomenon; it initiates a cascade of adverse biological and technical consequences. When a rigid device is implanted or attached to soft tissue, the disparity in mechanical compliance leads to chronic inflammation, signal degradation, and ultimately, device failure. This whitepaper delves into the mechanisms underlying these failures, guided by the central thesis that matching the Young's modulus of bioelectronic materials to that of target tissues is a critical pathway toward achieving stable, long-lasting bioelectronic interfaces. The following sections will explore the consequences of mechanical mismatch, detail experimental methodologies for its investigation, and outline emerging material strategies that promise to bridge the mechanical divide.
The Triad of Failure: Consequences of Mechanical Mismatch
Chronic Inflammation and the Foreign Body Response
The body's reaction to a mechanically mismatched device is a primary obstacle to long-term bioelectronic stability. The innate immune system perceives the stiff, foreign object as a threat, triggering a Foreign Body Response (FBR). This response begins with an acute inflammatory phase, where immune cells like macrophages and microglia are activated and release inflammatory cytokines [18]. If the mechanical mismatch persists, this transitions into a chronic phase characterized by the formation of a glial scar in the central nervous system or a fibrotic capsule around peripheral implants [18] [19].
The core issue is that a rigid device constantly exerts stress on the surrounding compliant tissue, especially with the body's natural micromovements—from pulsations, breathing, or general motion. This chronic mechanical irritation sustains the inflammatory state. The resulting glial or fibrotic capsule acts as an insulating barrier, physically isolating the electrode from its target neurons and dramatically increasing the electrical impedance at the interface [18] [19]. This encapsulation is a direct biological consequence of the unresolved mechanical mismatch and is a major contributor to the decline in recording and stimulation efficacy over time.
Signal Degradation and Performance Loss
The biological encapsulation driven by mechanical mismatch directly undermines the primary function of a bioelectronic device: high-fidelity signal transmission. The consequences for signal quality are severe:
- Increased Electrical Impedance: The layer of scar tissue, which has poor electrical conductivity, increases the distance between the electrode and the target cells. This leads to a significant rise in interface impedance, which attenuates the small electrical signals from neurons before they can reach the recording electrode [18] [20].
- Reduced Signal-to-Noise Ratio (SNR): Higher impedance correlates with increased thermal noise. This, combined with the signal attenuation from the fibrous capsule, makes it exceedingly difficult to distinguish faint, physiologically relevant signals from the electrical background noise, leading to a poor SNR [18].
- Stimulation Inefficiency: For stimulating electrodes, a higher impedance requires more voltage to deliver the necessary therapeutic current. This not only increases power consumption but also elevates the risk of inducing unwanted electrochemical reactions that can damage both the electrode and the surrounding tissue [18].
Over time, these factors can lead to a complete loss of usable signal, rendering the device ineffective for both diagnostic and therapeutic applications.
Mechanical and Material Failure Modes
Beyond the biological response, the mechanical mismatch itself can induce direct physical failure of the device. The constant strain and micromotion at the interface between a rigid device and soft tissue can lead to several failure modes [20] [19]:
- Material Fatigue: Repetitive stress cycles can cause cracking of brittle semiconductor substrates like silicon or delamination of thin-film metal traces.
- Insulation Failure: The polymer coatings used to insulate lead wires (e.g., polyimide, parylene) can degrade or crack under chronic mechanical strain, leading to electrical shorts or exposure of conductive surfaces.
- Strain Concentration at Interfaces: Finite Element Modeling (FEM) has shown that mechanical strain is often concentrated at the borders between different materials within a device, such as where a metal trace meets a silicon substrate. These areas become points of failure, with small protrusions being particularly vulnerable [20].
These abiotic failure mechanisms are a direct result of the device's inability to flex and move harmoniously with the tissue it interfaces with, ultimately leading to a loss of structural integrity and electronic function.
Table 1: Quantitative Impact of Mechanical Mismatch on Bioelectronic Performance
| Failure Mode | Primary Cause | Measurable Outcome | Typical Timeline |
|---|---|---|---|
| Foreign Body Response | Chronic irritation from stiff device | Glial scar formation; >50% increase in impedance [18] | Weeks to months |
| Signal Attenuation | Insulating fibrotic capsule | Signal-to-Noise Ratio (SNR) degradation [18] | Months to years |
| Mechanical Fatigue | Cyclic strain & micromotion | Cracking of silicon shanks; delamination of traces [20] | Months to years |
| Stimulation Inefficiency | High interface impedance | Increased voltage requirement; risk of tissue damage [18] | Anytime post-encapsulation |
Investigating Mechanical Mismatch: Experimental Protocols and Characterization
A multi-faceted experimental approach is essential to understand and quantify the effects of mechanical mismatch. The following protocols represent key methodologies used in the field.
Protocol 1: Nanoscale Mechanical Characterization via Atomic Force Microscomy (AFM)
Objective: To measure the nanoscale Young's modulus and surface morphology of thin-film bioelectronic materials deposited on flexible substrates [21].
- Sample Preparation: Deposit the material of interest (e.g., Au, PEDOT:PSS) at varying thicknesses (e.g., 5 nm to 100 nm) onto a flexible substrate such as polyethylene terephthalate (PET) [21].
- AFM Setup: Utilize an atomic force microscope equipped with a calibrated cantilever probe. The force-distance curve mode is used to quantify the tip-sample interaction.
- Data Acquisition: Map the surface topography and acquire force-distance curves at multiple points across the sample surface. The slope of the retraction curve in the contact region is proportional to the Young's modulus.
- Data Analysis: Apply appropriate contact models (e.g., Hertzian, DMT) to the force-distance data to calculate the local Young's modulus. Compile data to create spatial maps of mechanical properties and correlate with film thickness.
Protocol 2: In Vivo Assessment of the Foreign Body Response
Objective: To evaluate the chronic inflammatory tissue response and recording performance of an implanted neural electrode.
- Device Implantation: Sterilize and surgically implant the neural probe (e.g., planar silicon electrode) into the target region of an animal model (e.g., mouse cortex) [20].
- Chronic Electrophysiology: Over a period of several months, regularly record neural signals (single-unit and multi-unit activity) and perform Electrochemical Impedance Spectroscopy (EIS) to monitor changes in signal quality and interface impedance [20].
- Histological Analysis: At endpoint, perfuse and fix the brain. Section the tissue containing the implant track and stain for inflammatory markers (e.g., Iba1 for microglia, GFAP for astrocytes) and neuronal nuclei (NeuN).
- Correlative Analysis: Correlate the electrophysiological data (signal quality, impedance) with the histological evidence of glial scarring and neuronal loss around the implant site to establish a direct link between the FBR and performance degradation [20].
Theoretical Modeling of Conformability
Theoretical models provide a framework for designing devices that minimize mechanical mismatch. For instance, the conformability of a thin-film device on a rough surface (like skin) can be modeled by considering the total energy of the system: ( {\bar{U}}{\text{conformal}}={\bar{U}}{\text{bending}}+{\bar{U}}{\text{skin}}+{\bar{U}}{\text{adhesion}} ), where the terms represent the bending energy of the device, the elastic energy of the skin, and the interfacial adhesion energy, respectively. A conformal attachment is achieved when ( {\bar{U}}_{\text{conformal}} < 0 ) [3]. For non-developable surfaces (with non-zero Gaussian curvature like a sphere), models show that to achieve stable conformal attachment, a device should have a small size, minimal thickness, and a low Young's modulus [3].
Diagram 1: Experimental workflow for analyzing mechanical mismatch. The approach combines nanoscale material characterization, in vivo biological response assessment, and theoretical modeling to form a comprehensive understanding.
Material Strategies for Mechanical Harmony
To mitigate the consequences of mechanical mismatch, the field is shifting from rigid to soft and compliant materials. The goal is to develop devices with a bending stiffness below 10⁻⁹ Nm, contrasting sharply with the >10⁻⁶ Nm of conventional rigid electronics [4]. Key material strategies include:
Conducting Polymer Hydrogels
Materials like PEDOT:PSS hydrogels represent a promising frontier. They can be engineered to achieve a full spectrum of moduli (0.28 kPa to 15 kPa) that match various soft tissues, while maintaining high electrical conductivity (1.99 S/m to 5.25 S/m) [16]. Their mixed ionic-electronic conductivity facilitates efficient charge transfer with biological tissue. When used as electrodes, these hydrogels provide a stable interface for recording electromyogram (EMG), electrocardiogram (ECG), and electroencephalogram (EEG) signals with SNRs as high as 20.0 dB, outperforming traditional rigid electrodes [16].
Ultrathin and Flexible Metallic Films
Even conventional metals like gold can be made more compliant through geometric design. Research shows that Au films thinner than 10 nm fail to form a continuous conductive layer, while films thicker than 25 nm on PET substrates maintain reliable conductivity and mechanical stability under bending conditions [21]. The use of ultrathin substrates (e.g., 1.4 μm PET films) drastically reduces bending stiffness, allowing devices to achieve conformal contact with curved surfaces through van der Waals forces alone, without aggressive adhesives [10].
Textile and Nanostructured Composites
Integrating conductive nanomaterials like carbon nanotubes (CNTs) and graphene into electrospun nanofibers creates pressure-sensitive, breathable, and highly flexible sensing networks [10]. These composite structures can achieve conformal contact over large areas (e.g., 9 × 9 cm²), enabling applications like full-body motion sensing and health monitoring [10].
Table 2: Material Solutions for Mitigating Mechanical Mismatch
| Material Class | Example Materials | Young's Modulus Range | Key Advantages | Validated Performance |
|---|---|---|---|---|
| Conducting Polymer Hydrogels | PEDOT:PSS with modifiers [16] [22] | 0.28 kPa – 15 kPa [16] | Tissue-matched softness, mixed ionic-electronic conduction | SNR up to 20.0 dB for EEG/ECG/EMG [16] |
| Ultrathin Metallic Films | Au on PET [21] | N/A (Bending stiffness reduced) | High conductivity, established fabrication | Stable conductivity on PET when >25nm thick [21] |
| Nanostructured Composites | CNT/Graphene-PET nanofibers [10] | N/A (Geometric flexibility) | Breathability, large-area conformity | >90% transmittance, bending-insensitive pressure sensing [10] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Bioelectronic Interface Studies
| Reagent/Material | Function in Research | Specific Example & Rationale |
|---|---|---|
| Flexible Substrates | Provides a soft, bendable base for device fabrication. | Polyethylene Terephthalate (PET): Excellent optical and thermal properties; allows creation of ultrathin (<1.4 μm) devices for conformal contact [21] [10]. |
| Conductive Polymers | Forms soft, electroactive layers for recording and stimulation. | PEDOT:PSS: Offers high conductivity and biocompatibility; can be modified into hydrogels for tissue-matched modulus [16] [22]. |
| Nanostructured Coatings | Increases electroactive surface area to lower impedance. | Iridium Oxide (SIROF) & Platinum Nanograss: Coating electrodes with these materials drastically increases surface area, reducing impedance and improving charge injection capacity [18]. |
| Anti-inflammatory Coatings | Modulates the biological interface to suppress the FBR. | Dexamethasone-eluting coatings: Locally releases anti-inflammatory drugs to suppress acute immune response post-implantation [18]. |
| Hydrogel Matrices | Mimics the extracellular matrix, improving biocompatibility. | Zwitterionic Hydrogels: Provide a hydrating, neutrally charged interface that resists non-specific protein adsorption, reducing inflammation and enabling long-term (≥4 weeks) stable implantation [22]. |
The evidence is conclusive: a significant mechanical mismatch between bioelectronic devices and biological tissues leads to a detrimental triad of chronic inflammation, signal degradation, and device failure. The rigid nature of conventional electronics incites a foreign body response, resulting in an insulating glial or fibrotic capsule that isolates the device and increases electrical impedance. Concurrently, mechanical strain and micromotion induce material fatigue and structural failure in the device itself.
The path forward, central to modern bioelectronic materials research, is the development of devices that achieve mechanical and electrical harmony with biology. This involves the adoption of soft, compliant materials such as conducting polymer hydrogels, ultrathin geometric designs, and nanostructured composites. These strategies aim to reduce bending stiffness to levels compatible with soft, dynamic tissues. Future research must continue to refine these material systems, focusing on their long-term stability, reliable fabrication, and seamless integration with wireless power and data transmission systems. By prioritizing the matching of Young's modulus, the field of bioelectronics can move beyond simply avoiding failure and toward creating truly stable, high-fidelity interfaces that unlock their full therapeutic and diagnostic potential.
The evolution of bioelectronic medicine hinges on the development of devices that can seamlessly integrate with biological tissues for long-term diagnostic monitoring and therapeutic intervention. A critical determinant of this integration is the mechanical compatibility between the implantable device and the host tissue, primarily governed by the material property known as Young's modulus, a measure of stiffness or elastic resistance to deformation [23]. The pervasive challenge in biointerface design is the significant mechanical mismatch between conventional electronic materials, which are often rigid, and soft, dynamic biological tissues [10] [4] [5]. This mismatch induces chronic inflammation, fibrotic encapsulation, and device failure, ultimately compromising the long-term stability and functionality of the interface [24] [23].
This whitepaper synthesizes current research to define the target Young's modulus values for stable interfaces with neural, cardiac, and skin tissues. Framed within the broader context of materials science for bioelectronics, it provides a foundational guide for researchers and engineers aiming to design next-generation bioelectronic devices with enhanced biocompatibility and chronic stability.
Fundamental Principles of Mechanical Matching at Biointerfaces
The human body is composed of soft, dynamic tissues that undergo continuous movement and deformation. The Young's modulus of common bioelectronic materials and target tissues spans several orders of magnitude, creating a fundamental design challenge.
Foreign Body Response (FBR) and Fibrosis: When a rigid implant is introduced into soft tissue, the mechanical mismatch creates sustained stress at the interface. This perceived injury activates immune cells, leading to a cascade of events: activation of microglia and astrocytes in the brain, proliferation of fibroblasts in peripheral tissues, and the eventual deposition of collagen and other extracellular matrix components to form a dense, fibrotic capsule around the device [24] [23] [25]. This capsule acts as an insulating layer, increasing impedance for recording electrodes and reducing the efficiency of stimulating electrodes, thereby degrading signal fidelity over time [24] [23].
The "Mechanical Invisibility" Paradigm: The optimal strategy to mitigate FBR is to design devices that are mechanically "invisible" to the host immune system [24]. This involves engineering devices whose bending stiffness (a product of Young's modulus and the geometric moment of inertia) and effective modulus closely match those of the surrounding tissue. For implants, this minimizes relative micromotion and chronic stress, while for wearables, it ensures conformal contact and comfort, reducing motion artifacts [24] [10].
Quantifying Bending Stiffness: The bending stiffness of an electrode shaft is a critical parameter for penetrating implants. For a simple rod electrode with a circular cross-section, it is given by: ( EI = E \frac{\pi r^4}{4} ) where (E) is Young's modulus and (r) is the radius [24]. This formula highlights that reducing the device's cross-sectional area (miniaturization) is as crucial as selecting a low-modulus material for achieving tissue-like flexibility.
The diagram below illustrates the critical relationship between material properties, device design, and the ultimate biological and functional outcomes at the biointerface.
Target Tissues and Ideal Material Properties
The mechanical properties of target tissues vary significantly, necessitating tailored approaches for interface design. The table below summarizes the target Young's modulus ranges for key application areas.
Table 1: Target Young's Modulus Values for Bioelectronic Interfaces
| Target Tissue/Interface | Tissue Young's Modulus | Target Device Modulus | Key Design Considerations |
|---|---|---|---|
| Neural Tissue (Brain) | 1–10 kPa [24] [23] [5] | ~1–100 kPa [23] [25] [5] | Minimize bending stiffness for penetrating electrodes; use ultra-flexible, sub-μm thick substrates for cortical surface electrodes. |
| Cardiac Tissue | Information not explicitly stated in search results | Information not explicitly stated in search results | Requires elastic, flexible, and conductive materials to withstand continuous cyclic strain from heartbeats [26]. |
| Skin Interface | Information not explicitly stated in search results | < 1 MPa (for conformal contact) [10] | Ultralow bending stiffness (< 10⁻⁹ N·m) for conformal adhesion via van der Waals forces; stretchability to accommodate joint movement [10]. |
| Conventional Rigid Electronics | — | Silicon: ~10² GPaPlatinum: ~10² MPa [23] | Significant mechanical mismatch with all soft tissues, leading to chronic inflammation and device failure. |
Neural Interfaces
The brain is exceptionally soft, with a Young's modulus of approximately 1–10 kPa [24] [23] [5]. Conventional rigid electrodes, such as those made from silicon (≈10² GPa) or platinum (≈10² MPa), are orders of magnitude stiffer, causing significant mechanical mismatch [23].
Deep Brain Flexible Electrodes: The ideal strategy involves using flexible materials with a low Young's modulus, combined with geometric miniaturization, to reduce bending stiffness. This allows the electrode to mimic the softness of brain tissue, reducing chronic inflammation and the formation of glial scars [24]. For example, filamentary electrodes with widths as small as 7 μm and thicknesses of 1.5 μm have been developed to achieve a cross-sectional area at the subcellular level, minimizing acute injury during implantation and chronic micromotion thereafter [24].
Flexible and Injectable Platforms: Beyond penetrating probes, there is a push toward flexible patch-type electrodes for cortical surface mapping and injectable mesh electronics. These devices leverage ultra-thin polymer substrates (e.g., parylene-C, polyimide) with thicknesses often below 10 μm, resulting in a bending stiffness so low that they can conform to the cortical surface without causing significant irritation [10] [5]. The goal is to achieve an effective modulus that falls within the ~1–100 kPa range to ensure mechanical compatibility with the brain [25] [5].
Cardiac Interfaces
While the search results do not provide a specific Young's modulus value for cardiac tissue, they emphasize that the heart is a dynamic, contractile organ. Therefore, materials for cardiac interfaces must be not only flexible but also elastic and stretchable to withstand continuous cyclic strain [26].
- Conductive Biomaterials: Cardiac tissue engineering often employs conductive biomaterials that mimic the native extracellular matrix. These materials need to support electrical signal propagation between cardiomyocytes while matching the mechanical properties of the myocardium. Typical strategies use biodegradable elastomeric polymers, often in composite form with conductive nanomaterials like carbon nanotubes or gold nanowires, to create scaffolds that are both electrically conductive and mechanically compliant [26].
Skin Interfaces
The skin is the primary interface for wearable bioelectronics. Its modulus varies by location, but the key to a stable, high-fidelity interface is achieving conformal contact over large, curvilinear areas, often under dynamic motion [10].
Ultralow Bending Stiffness: The primary design parameter is bending stiffness rather than Young's modulus alone. By using ultrathin (< 1–10 μm) device geometries, even materials with a moderately high modulus (like polyimide or PET) can achieve bending stiffness low enough for conformal, van der Waals-driven adhesion to the epidermis without external adhesives [10]. This minimizes motion artifacts and improves signal quality for long-term electrophysiological monitoring (ECG, EMG, EEG) [27] [10].
Mechanically Adaptive Materials: Innovative strategies include modulus-adjustable materials. For instance, dry microneedle electrodes (MNEs) made from shape memory polymers (SMPs) can be stiff at room temperature for skin penetration and then soften at body temperature to match the mechanics of the surrounding skin tissue, thereby minimizing invasiveness and improving comfort during long-term use [27].
Experimental Protocols for Characterizing Biointerfaces
Protocol: Nanoscale Mechanical Characterization of Flexible Electrodes
This protocol outlines the procedure for measuring the Young's modulus of thin-film conductive layers used in flexible electronics, as demonstrated in studies on gold films [21].
- Sample Preparation: Deposit the material of interest (e.g., Gold) onto a flexible substrate (e.g., Polyethylene Terephthalate, PET) using standard deposition techniques like sputtering or evaporation. Prepare samples with a range of thicknesses (e.g., 5 nm to 100 nm) [21].
- Atomic Force Microscopy (AFM) Indentation:
- Use an AFM system equipped with a calibrated cantilever and a sharp tip.
- Engage the tip with the sample surface and obtain force-distance curves at multiple locations across the sample.
- The slope of the force-distance curve in the contact region is related to the sample's Young's modulus.
- Data Analysis: Fit the retraction curve of the force-distance data to an appropriate contact mechanics model (e.g., Hertzian, DMT, or JKR models) to extract the local Young's modulus value. Compile results from multiple measurements to report an average and standard deviation [21].
- Correlative Electrical Measurement: Simultaneously or subsequently, measure the electrical resistance of the film under flat and bent conditions to correlate mechanical flexibility with electrical performance [21].
Protocol: In Vivo Assessment of Foreign Body Response
This protocol describes a standard method for evaluating the biocompatibility and chronic stability of a neural implant.
- Device Implantation: Sterilize the neural interface device. Under approved animal care protocols, anesthetize the animal and stereotactically implant the device into the target brain region (e.g., motor cortex, hippocampus) [24] [23].
- Chronic Electrophysiological Recording: Over a period of weeks to months, periodically record neural signals (e.g., single-unit activity, local field potentials) from the implant. Key metrics include signal-to-noise ratio (SNR), spike amplitude, and recording stability [24] [5].
- Impedance Spectroscopy: Regularly measure the electrode-electrolyte impedance, typically at 1 kHz. A gradual increase in impedance often correlates with the formation of a fibrotic, insulating scar tissue around the electrode [24] [23].
- Histological Analysis (Endpoint): At the end of the study, perfuse the animal and extract the brain.
- Tissue Sectioning: Cryosection the brain tissue containing the implant track into thin slices.
- Staining: Perform immunohistochemical staining for specific cell markers:
- Imaging and Quantification: Use fluorescence or confocal microscopy to image the stained tissue. Quantify the intensity and thickness of the glial scar and the density of neurons within a defined radius (e.g., 100 μm) from the implant interface [23].
The workflow for the comprehensive in vivo assessment of a bioelectronic interface is summarized below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Developing bioelectronic interfaces with tailored Young's modulus requires a specific set of materials and reagents. The following table details key components used in the field.
Table 2: Research Reagent Solutions for Biointerface Development
| Material/Reagent | Function | Example Use Case |
|---|---|---|
| PEDOT:PSS | Conductive polymer; provides high electrical conductivity and ionic/electronic coupling while maintaining mechanical softness [27] [25]. | Coating for microneedle electrodes and cortical surface arrays to achieve low impedance and high-fidelity recording [27]. |
| Shape Memory Polymers (SMPs) | Substrate material with modulus-adjustable properties; stiff for implantation, soft at body temperature to minimize mismatch [27]. | Core material for mechanically adaptive dry microneedle electrodes (MDMEs) for skin and brain interfaces [27]. |
| Carbon Nanotubes (CNTs) & Graphene | Carbon-based nanomaterials; used as conductive fillers in composites to impart electrical conductivity and strength to soft polymers [26] [25]. | Creating conductive, flexible cardiac patches and fiber-based neural interfaces [26] [25]. |
| Polyimide (PI) & Parylene-C | Flexible, biocompatible polymer substrates; provide electrical insulation and structural support with low bending stiffness [24] [10]. | Substrate for ultraflexible, conformal epidermal electronic devices and implantable neural probes [24] [10]. |
| Liquid Metals (e.g., EGaIn) | Highly conductive and stretchable conductor; maintains conductivity under extreme deformation [25]. | Stretchable interconnects in wearable and implantable devices that require large strain tolerance [25]. |
| Gold (Au) Thin Films | Conductive metal layer; offers excellent conductivity and stability, with flexibility achievable at sub-micron thicknesses [21]. | Electrode material on flexible PET substrates for skin-worn electrodes; optimal conductivity is achieved with films >25 nm thick [21]. |
Achieving a stable, long-term bioelectronic interface is fundamentally an exercise in mechanical engineering at the soft-soft material boundary. The ideal target for Young's modulus in bioelectronic devices is unequivocally in the kPa to low MPa range, closely mirroring the mechanical properties of the host tissue. For the brain, this means striving for devices with moduli of 1–100 kPa, while for skin interfaces, achieving an ultralow bending stiffness through geometric thinning is paramount.
Future advancements will likely focus on several key areas:
- Multimodal and 3D Interfaces: The integration of electrical, optical, and chemical functionalities into a single, mechanically compliant device will provide a more comprehensive toolkit for neuroscience and cardiac research [5].
- Advanced Materials: The exploration of novel composites, liquid metals, and fully biodegradable conductive polymers will further close the mechanical and functional gap between electronics and biology [25].
- Intelligent Interfaces: The development of "living" bioelectronics that can adapt, self-heal, and even promote neural regeneration represents the next frontier, promising interfaces that are not only mechanically invisible but also biologically integrated [5].
By adhering to the principle of mechanical matching, researchers can overcome a significant barrier to chronic device reliability, accelerating the translation of bioelectronic technologies from the laboratory to the clinic.
Material Innovations and Fabrication Techniques for Modulus-Matched Bioelectronics
The development of bioelectronic devices for seamless integration with biological tissues represents a frontier in medical science. A central challenge in this field is the profound mechanical mismatch between conventional electronic materials and soft biological structures. Traditional electronic materials, such as silicon and metals, possess elastic moduli in the range of 10-200 GPa [28]. In stark contrast, biological tissues, including skin, neural tissue, and organs, are soft and elastic, typically exhibiting Young's modulus values of 1-100 kPa [28]. This discrepancy of approximately six orders of magnitude leads to significant strain concentration at the biotic-abiotic interface, causing mechanical damage, impaired signal transduction, chronic inflammation, and eventual device failure [28]. Consequently, there is a critical need for materials that simultaneously achieve tissue-like softness and electronic functionality.
Conductive hydrogels have emerged as a promising class of materials to address this challenge. These materials combine the tuneable mechanical properties of hydrogels with the electrical conductivity necessary for bioelectronic applications [29] [30]. By precisely engineering their composition and structure, researchers can create hydrogel-based materials with Young's modulus values that closely match those of target tissues while maintaining sufficient conductivity for applications such as biosensing, electrical stimulation, and drug delivery [28] [31]. This whitepaper provides a comprehensive technical overview of the material strategies, properties, and characterization methods for developing hydrogel-based materials with tissue-like softness and conductivity, framed within the context of Young's modulus considerations for bioelectronic integration.
Material Systems and Conduction Mechanisms
Conductive hydrogels achieve their electrical properties through various mechanisms and material compositions. The three primary approaches include the incorporation of conductive fillers, use of intrinsically conductive polymers, and exploitation of ionic conductivity.
Conductive Filler-Based Systems
These systems incorporate conductive nanomaterials within hydrogel matrices to create percolating conductive networks:
- Carbon-Based Materials: Graphene and carbon nanotubes offer high conductivity but often require high loading levels that compromise mechanical properties. A novel approach using pristine graphene at oil-water interfaces creates self-assembled percolating networks within hydrogels, achieving conductivities up to 15 mS/m with minimal filler content [32].
- Metal-Based Nanomaterials: Silver and gold nanowires provide excellent conductivity but may present cytotoxicity concerns and higher costs [29].
- Liquid Metals: Materials like gallium-based alloys offer unique combinations of conductivity and fluidity, enabling stretchable conductive pathways [29].
Intrinsically Conductive Polymer Hydrogels
These systems utilize conductive polymers as the primary hydrogel matrix or as integrated components:
- PEDOT-Based Systems: Poly(3,4-ethylenedioxythiophene) variants are widely used, including PEDOT:PSS, PEDOT:CHC, and novel alternatives like PEDOT:DBSA, which offers improved biocompatibility with Young's modulus values matching soft tissues (0.5-5 kPa) [33] [34] [31].
- Other Conductive Polymers: Polyaniline (PANI) and polypyrrole (PPy) provide alternative conductive platforms with different mechanical and electrochemical properties [30].
Ionic Conductive Hydrogels
These systems rely on ion transport through hydrated networks, typically offering lower conductivity but superior transparency and mechanical matching with extremely soft tissues [30].
Table 1: Conduction Mechanisms in Hydrogel-Based Materials
| Conduction Type | Mechanism | Advantages | Conductivity Range | Young's Modulus Range |
|---|---|---|---|---|
| Electronic (Filler-Based) | Electron transport through percolating networks | High conductivity, Stability | 0.1-15 mS/m [32] | 1-100 kPa [32] |
| Electronic (Polymer-Based) | Electron transport along conjugated polymer chains | Homogeneous structure, Tunability | 1-1000 S/m [31] | 0.5-5 kPa [31] |
| Ionic | Ion migration through hydrated pores | High transparency, Excellent softness | 0.01-1 S/m [30] | 0.1-10 kPa [30] |
Quantitative Properties of Hydrogel Material Systems
The mechanical and electrical properties of conductive hydrogels vary significantly based on their composition and structural design. The following table summarizes key parameters for prominent material systems reported in recent literature.
Table 2: Mechanical and Electrical Properties of Conductive Hydrogel Systems
| Material System | Young's Modulus | Conductivity | Tensile Strain | Key Features | Ref. |
|---|---|---|---|---|---|
| PEDOT:DBSA Hydrogel | Matches soft tissues | Sufficient for cell stimulation; Low impedance at 1 Hz | High flexibility | Pure conductive hydrogel, excellent biocompatibility | [31] |
| PEDOT:CHC/Silk (1:1) | Optimal mechanical properties | Electrically programmable | Exceptional resilience | >90% drug loading, hierarchical architecture | [33] [34] |
| Graphene/PHMA Foam | Tunable via composition | Up to 15 mS/m | Flexible foam structure | Self-assembled percolating network, minimal filler | [32] |
| Fe³⁺-Gelatin/P(AAc-co-AAm) | Tunable via Fe³⁺ concentration | Tunable conductivity | 569% elongation | Dynamic cross-linking, self-healing capability | [28] |
| GL-PVA-Gelatin | 3.18× increase with 50% GL | Not specified | Balanced elasticity | Dual-network, hydrogen bonding enhancement | [28] |
Fabrication and Experimental Methodologies
Granular Hydrogel Fabrication for Injectable Bioelectronics
Granular hydrogels represent an emerging approach for creating injectable or printable conductive materials. The following workflow illustrates the fabrication process for PEDOT:PSS microparticles and their assembly into functional bioelectronic components:
Diagram 1: Granular hydrogel fabrication workflow (3 steps)
Detailed Protocol:
- Emulsion Preparation: Create a water-in-oil emulsion by adding aqueous PEDOT:PSS solution to an oil phase with vigorous stirring. The two-phase system resembles an "oil-and-vinegar salad dressing" [35].
- Crosslinking: Heat the emulsion to crosslink the polymer, forming stable spherical hydrogel microparticles. Temperature and duration control particle size and mechanical properties.
- Assembly: Pack microparticles tightly to create a granular hydrogel material. The particles maintain micropores between them while flowing like liquids when force is applied [35].
- Application: Extrude through needles or 3D printing nozzles to create customized electrode structures that can conform to topographically diverse biological surfaces [35].
Hierarchical Conductive Polymer Hydrogel Synthesis
For more structured hydrogel systems with enhanced drug loading capacity, hierarchical architectures can be created:
PEDOT:CHC/Silk Hydrogel Fabrication [33] [34]:
- CHC Synthesis: Carboxymethyl-hexanoyl chitosan (CHC) is synthesized through chemical modification of chitosan to create an amphiphilic polymer with self-assembly capabilities.
- PEDOT:CHC Formation: Dissolve 0.2 mg CHC in 50 mL distilled water at 50°C until completely dissolved. Add 1.7 mL EDOT monomer and stir for 30 minutes. Add 5 mL FeCl₃·6H₂O oxidant solution to initiate polymerization. React for 24 hours, then purify the resulting PEDOT:CHC.
- Hierarchical Structure Formation: PEDOT:CHC self-assembles into hollow microgel structures driven by thermodynamic forces to minimize surface energy.
- Silk Integration: Blend PEDOT:CHC with silk fibroin solution at varying ratios (optimally 1:1) to form interpenetrating networks that provide mechanical reinforcement while maintaining electroactivity.
The Scientist's Toolkit: Essential Research Reagents
Successful development of conductive hydrogels requires specific materials and characterization approaches. The following table outlines key reagents and their functions in creating and optimizing these materials.
Table 3: Essential Research Reagents for Conductive Hydrogel Development
| Reagent/Material | Function | Example Application | Key Properties |
|---|---|---|---|
| PEDOT:PSS | Conductive polymer | Granular hydrogels, Composite electrodes | Biocompatibility, Mixed ionic-electronic conduction [35] |
| PEDOT:DBSA | Conductive polymer | Pure conductive hydrogels | Tunable mechanical properties, Low impedance [31] |
| Silk Fibroin | Structural biopolymer | Hierarchical hydrogels, Mechanical reinforcement | Biocompatibility, Mechanical strength, Crystalline structure [33] |
| CHC (Carboxymethyl-Hexanoyl Chitosan) | Amphiphilic dopant | Drug-eluting hydrogels | Self-assembly, High drug encapsulation (>90%) [33] [34] |
| Pristine Graphene | Conductive filler | Porous hydrogel foams | High conductivity, Self-assembling percolation networks [32] |
| Fe³⁺ Ions | Dynamic crosslinker | Mechanically tunable hydrogels | Ionic coordination, Redox activity, Self-healing [28] |
| Glycerol (GL) | Binary solvent component | Dual-network hydrogels | Hydrogen bonding, Mechanical enhancement [28] |
Advanced Applications in Bioelectronics
Programmable Drug Delivery for Diabetic Wound Healing
Conductive hydrogels enable electrically-triggered drug release systems for advanced wound care. The following diagram illustrates the operational mechanism of a hierarchical PEDOT:CHC/silk hydrogel for diabetic wound treatment:
Diagram 2: Electrically-triggered drug release mechanism (5 steps)
System Optimization Parameters [33] [34]:
- Electrical Stimulation Parameters: Voltage (0.5-3V), frequency (0.1-100 Hz), waveform (DC, pulsed), and duration can be systematically optimized to achieve precise spatiotemporal control of drug release.
- Electrode Geometry: Interdigitated electrode arrays improve field distribution and release control compared to simple planar electrodes.
- Material Composition: The PEDOT:CHC to silk ratio (optimally 1:1) balances mechanical resilience (>90% drug encapsulation efficiency) with electrochemical responsiveness.
Tissue-Integrated Sensors and Stimulators
Granular conductive hydrogels enable novel biointegration approaches:
- Conformal Contact: Injectable granular hydrogels can spread over tissues or encapsulate cells, enabling continuous monitoring of biological activity [35].
- In Vivo Validation: Researchers have successfully measured local field potentials corresponding to odor sensing in locust antennae using PEDOT:PSS granular hydrogels [35].
- Customizable Electrodes: 3D printing capability allows creation of patient-specific electrode geometries that match individual anatomical features [35].
Hydrogel-based materials with tissue-like softness and conductivity represent a transformative approach to bioelectronic integration. By precisely engineering material composition, structure, and conduction mechanisms, researchers can create systems with Young's modulus values that closely match biological tissues (1-100 kPa) while maintaining sufficient electrical functionality for sensing, stimulation, and drug delivery applications. Continued advancement in this field requires multidisciplinary approaches that combine materials science, electrical engineering, and biological expertise to address remaining challenges in long-term stability, manufacturing scalability, and clinical translation. The development of standardized characterization protocols specifically tailored for soft, hydrated conductive materials will further accelerate progress in this rapidly evolving field.
The field of bioelectronics has been fundamentally reshaped by the development of conductive polymers (CPs) and their nanocomposites, which uniquely blend the electronic functions of semiconductors with the mechanical properties of plastics. The discovery of conductive polyacetylene in 1977, recognized by the 2000 Nobel Prize in Chemistry, marked the birth of this material class and opened avenues for organic electronic materials with biomedical potential [36] [37]. Unlike traditional metals and inorganic semiconductors, conductive polymers offer electronic-ionic hybrid conductivity, mechanical softness, and versatile chemical modification capabilities, making them ideally suited for bio-interfacing applications [38]. Their relevance to Young's modulus research in bioelectronics is paramount: these materials can be engineered to match the mechanical properties of biological tissues, thereby minimizing mechanical mismatch at the tissue-implant interface—a critical factor in reducing chronic inflammation and improving long-term device performance [38] [39] [37].
The fundamental structure enabling conductivity in these polymers is a conjugated molecular backbone consisting of chains of alternating single and double bonds, which facilitates electron delocalization through overlapping p-orbitals [38]. Their conductivity can be significantly enhanced through doping, which generates charge carriers (polarons and bipolarons) within the polymer structure [40]. This unique combination of properties has positioned conductive polymers as transformative materials for a new generation of flexible, stretchable, and implantable bioelectronic devices.
Material Properties and Characterization
Key Conductive Polymers and Their Properties
Table 1: Fundamental Properties of Major Conductive Polymers
| Polymer | Electrical Conductivity Range | Key Properties | Primary Applications in Bioelectronics |
|---|---|---|---|
| PEDOT:PSS | 1–104 S·cm⁻¹ (standard); up to ~8800 S·cm⁻¹ with advanced processing [39] | High conductivity, transparency, flexibility, intrinsic stretchability, air stability [41] | Neural electrodes, wearable sensors, organic electrochemical transistors [39] [37] |
| Polyaniline (PANI) | 10−2–100 S·cm⁻¹ (emeraldine salt) [41] | Tunable conductivity, environmental stability, ease of synthesis, pH-dependent properties [36] [41] | Biosensors, corrosion protection, energy storage devices [36] [40] |
| Polypyrrole (PPy) | Variable with doping; can achieve high conductivity [41] | Good environmental stability, high conductivity, redox properties, biocompatibility [36] [41] | Neural interfaces, drug delivery systems, biosensors [36] [38] |
| Polyacetylene (PA) | 104–105 S·cm⁻¹ when doped [41] | High conductivity when doped, photoconductivity, gas permeability [41] | Limited due to instability; historical significance [41] |
Mechanical Properties and Young's Modulus Considerations
The Young's modulus of conductive polymers is a critical parameter in bioelectronics, as mechanical mismatch with soft biological tissues can lead to fibrotic encapsulation and device failure [38]. Traditional metallic electrodes like platinum and gold have modulus values in the GPa to TPa range, while neural tissue has a modulus of approximately 0.1-1 kPa [38]. Conductive polymers help bridge this gap:
- PEDOT:PSS can be processed to achieve tissue-mimetic softness while maintaining high conductivity [39]. Recent advances in vertically phase-separated PEDOT:PSS films demonstrate simultaneous achievement of high conductivity (>8500 S·cm⁻¹) and enhanced biointerface interactions [39].
- Conductive elastomers developed by embedding PEDOT nanowires in polyurethane matrices create fully polymeric electrode materials with tunable mechanical properties, though increasing nanowire content typically increases Young's modulus while decreasing strain at failure [42].
- Conductive hydrogels (CHs) and conductive polymeric hydrogels (CPHs) provide exceptional flexibility, tensile strength, and biocompatibility, making them ideal for electrical devices interfacing with biological systems [36].
Table 2: Mechanical and Electrical Properties of Conductive Materials for Bioelectronics
| Material Type | Young's Modulus Range | Electrical Conductivity Range | Advantages for Biointerfacing | |
|---|---|---|---|---|
| Metals (Pt, Au) | GPa to TPa range [38] | ~105 S·cm⁻¹ [37] | Excellent conductivity, long-term stability | High stiffness causes mechanical mismatch |
| Conductive Polymers (PEDOT:PSS) | kPa to MPa range (tunable) [38] [39] | 1–8800 S·cm⁻¹ [39] | Soft, flexible, tissue-matching modulus | Stability challenges under physiological conditions |
| Conductive Elastomers | kPa to MPa range (tunable with filler loading) [42] | Variable with composition | Fully polymeric, compliant mechanics | Conductivity typically lower than pure metals |
| Biological Tissues | 0.1–1 kPa (neural tissue) [38] | Ionic conduction | Native environment | - |
Fabrication and Processing Methodologies
Synthesis Techniques for Conductive Polymers
The synthesis of conductive polymers can be achieved through various methods, each offering distinct advantages for bioelectronic applications:
Chemical Polymerization: This scalable, economical approach uses oxidizing agents such as ammonium persulfate or enzymatic catalysts to initiate polymerization [40]. The mechanism involves oxidation of monomer units to form radical cations, which combine to form dimers and eventually polymer chains [40]. Enzymatic polymerization using peroxidase or laccase offers milder, more environmentally friendly conditions for synthesizing polyaniline and polypyrrole [40].
Electrochemical Polymerization: This method allows direct deposition of conductive polymer films onto electrode surfaces, enabling precise control over film thickness and morphology [36] [40]. The process involves applying a potential to oxidize monomers in solution, forming polymer films on the working electrode [40]. This technique is particularly valuable for creating neural interfaces and biosensors.
Interfacial Polymerization: This approach creates polymers at liquid-liquid or liquid-solid interfaces, resulting in materials with high porosity and specific surface area [40]. For example, PEDOT produced through interfacial polymerization can achieve a porosity of 70.61% and specific surface area >58 m²/g, making it ideal for supercapacitors and sensing applications [40].
Advanced Processing and Patterning Techniques
For integration into bioelectronic devices, conductive polymers require precise patterning and deposition:
Solution-Based Processing: Techniques including spin coating, drop coating, shear coating, and dip coating enable simple deposition of conductive polymer thin films [41]. These methods benefit from the processability of many conductive polymers and their composites.
Printing Technologies: Inkjet printing, screen printing, and 3D printing allow patterned deposition of conductive polymers for flexible electronics [41]. These additive manufacturing approaches enable complex geometries and customized device architectures.
Laser Processing: Recent advances demonstrate high-fidelity patterning of PEDOT:PSS films using laser systems, creating customized sensor arrays for wearable and implantable applications [39].
Experimental Protocol: In Situ Polymerization of PEDOT:PSS Nanocomposites
Objective: To create a highly conductive PEDOT:PSS film with vertical phase separation for bioelectronic applications.
Materials:
- Commercial PEDOT:PSS ink
- Ethylene glycol (EG)
- Metastable liquid-liquid contact (MLLC) doping dispersion
- Polyurethane substrate
- Blade coater
- Annealing oven
Procedure:
- Substrate Preparation: Clean and treat polyurethane substrate with oxygen plasma to ensure uniform wettability.
- Prismatic Film Formation: Blade coat commercial PEDOT:PSS ink onto substrate at controlled thickness (typically 1-5 µm) and drying conditions.
- Solid-Liquid Interface Doping: Shear MLLC-doping dispersion onto the pristine film surface. The MLLC dispersion is an EG-diluted PEDOT:PSS formulation with reduced PSS/PEDOT molar ratio (~1.73).
- Phase Separation Induction: During annealing at 60-80°C, solvent evaporation prompts hydrophilic PSS chains to accumulate at the surface while PEDOT-rich domains form high crystallization at the bottom.
- Characterization: Verify vertical phase separation through XPS depth profiling, with PSS/PEDOT ratio decreasing from 11.5 at the surface to 0.74 at the bottom [39].
Key Parameters: Coating speed, doping solvent composition, and annealing conditions critically influence the resulting vertical phase separation and conductivity.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Conductive Polymer Research
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| PEDOT:PSS | Primary conductive polymer for flexible electronics | Aqueous dispersion, tunable conductivity, transparency, commercial availability [41] [39] |
| Polyaniline (PANI) | Versatile conductive polymer for sensors and energy storage | Three oxidation states, pH-dependent conductivity, environmental stability [36] [41] |
| Polypyrrole (PPy) | Biocompatible polymer for neural interfaces and biosensors | Good environmental stability, redox properties, ease of polymerization [36] [41] |
| Ethylene Glycol (EG) | Secondary dopant for PEDOT:PSS | Enhances conductivity by inducing phase separation and improving PEDOT crystallinity [39] |
| Dimethyl Sulfoxide (DMSO) | Common secondary dopant for conductive polymers | Improves charge transport properties by modifying polymer chain arrangement [39] |
| Carbon Nanotubes | Conductive fillers for nanocomposites | High aspect ratio, exceptional conductivity, mechanical reinforcement [36] [37] |
| Graphene and Derivatives | Two-dimensional conductive fillers | High surface area, excellent electrical and thermal properties [36] [37] |
| Biodegradable Polymer Matrices | Substrates for bioresorbable electronics | PLA, PCL, gelatin; provide temporary support then degrade [43] [37] |
Bioelectronic Applications and Experimental Outcomes
Neural Interfaces and Recording Systems
Conductive polymers have revolutionized neural interface technology by providing softer, more compliant electrode materials. Standard parameters for neural electrodes include low impedance, high charge storage capacity, and appropriate charge injection limits [38]. CP-based electrodes significantly improve these parameters:
- Neural Recording: PEDOT-based coatings on traditional electrodes reduce impedance by 1-2 orders of magnitude, improving signal-to-noise ratio for capturing neural signals [38].
- Neural Stimulation: CP electrodes exhibit higher charge injection limits compared to bare metal electrodes, enabling more effective neural stimulation with reduced risk of tissue damage [38].
- Chronic Stability: The mechanical compliance of CPs minimizes the foreign body response, reducing glial scarring and maintaining signal quality over extended implantation periods [38].
Wearable and Implantable Sensors
The flexible nature of conductive polymer nanocomposites makes them ideal for sensors that conform to biological tissues:
- Electrophysiological Monitoring: Vertically phase-separated PEDOT:PSS films with laser-patterned arrays enable high-fidelity acquisition of electrocardiogram (ECG), electromyogram (EMG), and electroencephalogram (EEG) signals [39].
- Strain Sensors: Conductive elastomers with embedded PEDOT nanowires can detect mechanical deformations associated with joint movement, respiration, and pulse waves [42].
- Chemical Sensors: Functionalized conductive polymers can detect biomarkers, electrolytes, and neurotransmitters through changes in their electrical properties [41] [38].
Tissue Engineering and Regenerative Medicine
Conductive polymers serve as active scaffolds in tissue engineering, providing electrical cues that direct cell behavior:
- Neural Tissue Regeneration: PPy and PEDOT scaffolds enhance neurite outgrowth and direct cell migration when subjected to electrical stimulation [38].
- Bone Tissue Engineering: PANI-based composites support osteogenic differentiation when combined with electrical stimulation [38].
- Cardiac Tissue Engineering: Conductive patches improve the maturation and synchronous beating of cardiomyocytes [37].
Current Challenges and Future Perspectives
Despite significant progress, conductive polymers face several challenges in bioelectronic applications:
Long-Term Stability: The electroactive stability of conducting polymers can be poor, with potential degradation under physiological conditions [44]. Environmental factors like moisture and oxygen can contribute to this degradation, potentially leading to loss of conductivity [44].
Biocompatibility and Cytotoxicity: While generally more biocompatible than rigid materials, some conductive polymers and their degradation products may induce inflammatory responses or cytotoxicity [37]. Ongoing research focuses on surface modification and composite strategies to enhance biocompatibility.
Manufacturing Scalability: Transitioning from laboratory-scale production to industrial manufacturing remains challenging [45] [44]. Standardization of material properties and development of robust quality control measures are needed for clinical translation.
Future research directions include the development of bioresorbable conductive polymers that safely degrade after fulfilling their function, AI-guided material design to optimize properties for specific applications, and multifunctional systems that combine sensing, stimulation, and drug delivery capabilities [37]. As the field advances, conductive polymers and nanocomposites are poised to play an increasingly central role in bridging the gap between electronic and biological systems, ultimately enabling more effective and seamless biointegration.
Conductive polymers and nanocomposites represent a transformative material class that successfully blends flexibility with electronic function. Their tunable mechanical properties, particularly Young's modulus, make them uniquely suited for bioelectronic applications where matching tissue mechanics is essential for long-term performance. Continued research addressing stability challenges, enhancing biocompatibility, and developing scalable manufacturing processes will accelerate the clinical translation of these remarkable materials. As interdisciplinary collaborations between materials scientists, engineers, and biologists deepen, conductive polymers are positioned to enable a new generation of soft, compliant bioelectronic devices that seamlessly integrate with the human body.
The evolution of bioelectronic medicine is characterized by a fundamental paradigm shift from rigid to soft, mechanically compliant systems. For implantable and wearable devices to function reliably within the dynamic, humid environment of the human body, they must overcome persistent challenges associated with the mechanical mismatch between conventional electronic materials and biological tissues [10]. This mechanical mismatch induces chronic inflammation, fibrotic encapsulation, and eventual device failure, significantly limiting the long-term stability and therapeutic efficacy of bioelectronic technologies [4]. The field has therefore increasingly turned to geometric engineering—the strategic design of physical structures—as a core strategy to circumvent the intrinsic material limitations of high-performance semiconductors and conductors.
Geometric engineering operates on the principle that a structure's mechanical performance is not solely determined by its constituent materials' properties but also by its physical architecture. By incorporating specific design motifs such as serpentine interconnects, open-mesh networks, and ultrathin substrates, engineers can create devices that exhibit macroscopic compliance while utilizing microscale components of inherently stiff materials [46] [47]. This approach is critically framed within the context of Young's modulus research, which quantifies material stiffness. The goal is not always to discover new soft materials but to intelligently design structures that behave as though they are soft, achieving effective moduli that match those of target tissues (typically in the kPa to low MPa range), even when built from materials with GPa-scale moduli [4]. This technical guide details the core geometric strategies, their experimental validation, and their implementation in advanced bioelectronic devices.
Core Geometric Strategies and Their Mechanics
Ultrathin and Freestanding Substrates
The foundation of compliant bioelectronics is the reduction of bending stiffness, which is proportional to the cube of thickness. By fabricating devices on ultrathin polymer substrates (e.g., polyimide or parylene-C with thicknesses ≤ 10 µm), the structure becomes highly flexible and achieves conformal contact with curvilinear biological surfaces through van der Waals forces alone, often without need for aggressive adhesives [10].
- Key Mechanical Principle: Reducing thickness moves the neutral mechanical plane—the plane within a bent structure that experiences zero strain—closer to the active electronic components. This configuration minimizes strain in critical semiconductor layers when the device is flexed [46].
- Experimental Realization: State-of-the-art organic electrochemical transistors (OECTs) have been demonstrated on parylene-C substrates as thin as 1–5 µm, enabling high-fidelity recording of electrocardiogram (ECG), electrooculogram (EOG), and electromyogram (EMG) signals directly from the skin with minimal motion artifact [10]. These devices can achieve transconductance values exceeding 400 mS, proving that miniaturization and softness do not necessitate a sacrifice in electronic performance.
Serpentine Interconnects and Structural Ribbons
Serpentine patterns are a cornerstone geometric feature for enabling stretchability in systems composed of non-stretchable materials. These meandering, ribbon-like structures accommodate applied tensile strain through out-of-plane buckling and twisting, rather than through intrinsic material stretching [46] [47].
- Key Mechanical Principle: When integrated with an elastomeric substrate like poly(dimethylsiloxane) (PDMS), pre-strained then relaxed, serpentine ribbons pop into out-of-plane arcs. Subsequent stretching of the system primarily flattens these arcs, accommodating large macroscopic strains (over 100%) while inducing minimal strain (often <1%) in the material itself [46].
- Design Optimization: The stretchability and compliance of a serpentine ribbon are governed by its geometric parameters. Table 1 summarizes the impact of these parameters, derived from theoretical, numerical, and experimental studies [47].
Table 1: Effect of Serpentine Geometric Parameters on Mechanical Performance
| Geometric Parameter | Effect on Stretchability | Effect on Compliance (Reduced Stiffness) |
|---|---|---|
| Larger Arc Radius | Increases | Increases |
| Larger Arc Angle | Increases | Increases |
| Longer Arm Length | Increases (by several orders if infinite) | Increases |
| Narrower Ribbon Width | Increases | Increases |
Open-Mesh Designs and Strategic Porosity
Transforming a continuous film into an open, porous mesh is a highly effective method to enhance both stretchability and biocompatibility. This design strategy reduces the effective structural stiffness and allows for biological tissue integration, which is crucial for chronic implants [48] [46].
- Key Mechanical Principle: Mesh designs localize deformation to the flexible interconnects between rigid, functional islands. This confines strain to specific, designed regions, protecting active components. Furthermore, the porosity enables fluid transport and tissue ingrowth, promoting stable bio-integration and reducing foreign body response [48].
- Anisotropy and Design Control: As demonstrated in hernia repair meshes, mechanical properties like stiffness and maximum force can vary dramatically (e.g., stiffness from 0.3 N/mm to 4.6 N/mm) based on the mesh's geometric parameters and the direction of applied load [49]. This anisotropy can be strategically leveraged by orienting the mesh during implantation to align with the highest stress directions in the tissue [49].
- Geometric Influence on Strength: In 3D-printed titanium (Ti6Al4V) mesh scaffolds for spinal fusion cages, the height of the connection point between mesh arms significantly impacts mechanical performance. A small change in this parameter (to 0.24 mm) resulted in measurably higher stiffness and failure force, demonstrating how subtle geometric modifications can tailor mechanical properties for specific load-bearing applications [48].
Experimental Protocols for Validation
Validating the performance of geometrically engineered devices requires a suite of mechanical and electrical tests. Below are detailed methodologies for key experiments.
Uni-axial Tensile Testing for Mesh Materials
This protocol characterizes the fundamental mechanical properties of mesh structures and is adapted from standards used for hernia meshes [49].
- Objective: To determine the maximum force, breaking strain, and stiffness of a mesh sample in both longitudinal and transverse directions.
- Materials and Equipment:
- Universal tensile testing machine with a calibrated load cell.
- Custom or standardized grips designed to prevent sample slippage.
- Sample specimens cut to a standardized width (e.g., 1 cm) and length.
- Non-contact strain measurement system (e.g., video extensometer) is recommended for thin, compliant samples.
- Procedure:
- Mount the sample in the grips, ensuring it is aligned without pre-tension.
- For non-contact strain measurement, apply markers or use a natural pattern on the sample for the tracking system to follow.
- Apply a uni-axial tensile load at a constant strain rate (e.g., 10 mm/min) until sample failure.
- Simultaneously record the applied force and the displacement (or direct strain).
- Repeat for a statistically significant number of samples (n ≥ 5) in both material directions.
- Data Analysis:
- Maximum Force (N/cm): The peak force recorded before failure, normalized by the sample width.
- Breaking Strain (%): The strain at the point of sample failure.
- Stiffness (N/mm): The slope of the linear (elastic) region of the force-displacement curve.
Electrical Performance Under Strain
This protocol assesses the stability of electronic functionality during mechanical deformation, a critical metric for stretchable bioelectronics [46].
- Objective: To monitor the electrical properties of integrated circuits (e.g., transistors, ring oscillators) while subjecting the device to controlled levels of strain.
- Materials and Equipment:
- Custom-built or commercial strain stage capable of precise, cyclic elongation.
- Source measure units (SMUs) or a parameter analyzer for electrical characterization.
- Probe station with micromanipulators for contacting device pads.
- Device under test (DUT) on an elastomeric substrate (e.g., PDMS).
- Procedure:
- Mount the DUT on the strain stage and connect electrical probes.
- Measure baseline electrical performance (e.g., current-voltage (I-V) curves for transistors, oscillation frequency for ring oscillators).
- Apply a predefined strain (e.g., 10%, 20%, ... up to 100%) and hold the position.
- Repeat the electrical measurements at each strain level.
- Return the stage to 0% strain and re-measure to assess recovery and hysteresis.
- Optionally, perform cyclic straining (e.g., 1000 cycles at 20% strain) with periodic electrical checks to evaluate fatigue.
- Data Analysis:
- Plot key electrical parameters (mobility, on/off ratio, frequency) as a function of applied strain.
- A stable device will show minimal change in these parameters across the tested strain range.
Visual Image Tracing (VIT) for Thin Films
This non-contact method is ideal for accurately measuring the mechanical properties of thin films and micro-scale structures [50].
- Objective: To simultaneously measure Young’s modulus and Poisson’s ratio of a freestanding thin film.
- Materials and Equipment:
- Micro-tensile testing unit with a piezoelectric actuator and a high-resolution load cell.
- Two CCD cameras coupled with optical microscopes for orthogonal views.
- Freestanding thin film specimen with patterned markers or a inherent surface pattern.
- Data acquisition system running pattern-tracking software (e.g., built with LabVIEW).
- Procedure:
- Fabricate a freestanding thin film specimen (e.g., 500 µm wide, 1–5 µm thick Au) using lithography and etching processes on a silicon carrier wafer, which is later released [50].
- Mount the specimen on the micro-tensile tester.
- Apply a tensile load. The VIT system acquires images at a high frame rate (10 frames/s) and tracks the displacement between markers with high resolution (50 nm).
- One camera tracks axial strain, while the orthogonal camera tracks transverse strain.
- Data Analysis:
- Young’s Modulus (E): Calculated from the slope of the stress-strain curve in the elastic region. For example, thin Au films measured with this method show E ≈ 59–62 GPa [50].
- Poisson’s Ratio (ν): Calculated as the negative ratio of transverse strain to axial strain during elastic deformation.
Data Presentation and Performance Comparison
The following tables consolidate quantitative data from the literature to illustrate the performance achievable through geometric engineering.
Table 2: Mechanical Properties of Various Mesh and Geometric Designs
| Material / Design | Young's Modulus / Stiffness | Failure Force / Strength | Maximum Strain |
|---|---|---|---|
| Hernia Meshes (Various PP) [49] | 0.3 ± 0.1 to 4.6 ± 0.5 N/mm (stiffness) | 11.1 ± 6.4 to 100.9 ± 9.4 N/cm | 150 ± 6% to 340 ± 20% |
| SSWM/GF Hybrid (Mesh 120) [51] | - | 539.19 MPa (tensile) | - |
| Thin Au Films (1-5 µm) [50] | 59 – 62 GPa | Yield strength: 479 – 892 MPa (thickness-dependent) | - |
| Noncoplanar Mesh CMOS [46] | Effective stiffness drastically reduced | - | Up to ≈140% (system-level) |
Table 3: The Scientist's Toolkit: Essential Materials for Fabrication
| Research Reagent / Material | Function in Experiment / Device |
|---|---|
| Poly(dimethylsiloxane) (PDMS) | An elastomeric substrate that provides stretchability and biocompatibility. |
| Polyimide (PI) | A high-temperature polymer used for ultrathin, flexible substrates and encapsulation. |
| Parylene-C | A biocompatible polymer used as an ultrathin (<5 µm) substrate and conformal coating. |
| Single-Crystalline Silicon Ribbons | The high-performance semiconductor material for active devices in stretchable systems. |
| Ti/Au (5 nm/150 nm) | A common metallization stack for interconnects in flexible and stretchable electronics. |
| Poly(methylmethacrylate) (PMMA) | A sacrificial layer used to release fabricated devices from a rigid carrier wafer. |
| PEDOT:PSS | A conductive polymer used as an active layer in flexible organic electrochemical transistors (OECTs). |
Visualization of Concepts and Workflows
The following diagrams illustrate the core relationships and experimental workflows described in this guide.
Geometric Engineering Principles
Serpentine Interconnect Fabrication
Geometric engineering provides a powerful and versatile toolkit for overcoming the most significant mechanical challenges in bioelectronics. The strategic implementation of ultrathin substrates, serpentine interconnects, and open-mesh designs enables the creation of devices that maintain the high electrical performance of inorganic semiconductors while achieving the mechanical compliance of biological tissues. This synergy is essential for the next generation of chronic implants and high-fidelity wearables that require stable, long-term integration with the body.
Future research will likely focus on the multi-objective optimization of these geometries, balancing not only stretchability and compliance but also factors like fatigue resistance over millions of cycles, volumetric efficiency for miniaturization, and the facilitation of specific biological responses such as directed tissue ingrowth. Furthermore, the integration of these passive geometric strategies with active, functional materials like liquid metal conductors and self-healing polymers presents a promising frontier. As the field progresses, the principles of geometric engineering will remain foundational to the development of bioelectronic medicines that are truly seamless, stable, and effective.
In the evolving landscape of bioelectronic materials research, the mechanical properties of interfacing materials, particularly their Young's modulus, are paramount for ensuring seamless and stable integration with biological tissues. The inherent mechanical mismatch between conventional rigid electronics and soft, dynamic biological systems often leads to issues such as poor contact, signal interference, and inflammatory responses, ultimately compromising device performance and biocompatibility [52]. Hydrogels, three-dimensional networks of hydrophilic polymers, have emerged as a leading candidate to bridge this mechanical divide. Their high water content, tunable mechanical properties, and biocompatibility allow them to mimic the native extracellular matrix, making them ideal for creating compliant bioelectronic interfaces [53] [54].
The advent of 3D printing technology has further amplified the potential of hydrogels by enabling the fabrication of complex, customized structures that were previously unattainable. Among the most significant advancements are the development of modulus-tunable and multifunctional hydrogel inks. These inks can be engineered to possess a wide range of mechanical stiffnesses, from ultrasoft to stiff (0.1–500 kPa), matching the elastic modulus of various biological tissues from the brain to skin [55] [56]. Moreover, by incorporating functional nanofillers such as conductive polymers or carbon nanotubes, these hydrogels can be endowed with high electrical conductivity, self-healing capabilities, and viscoelasticity, transforming them into sophisticated platforms for soft bioelectronics [57] [55]. This technical guide delves into the design principles, fabrication methodologies, and characterization techniques for these advanced hydrogel inks, providing a roadmap for their application in next-generation bioelectronic devices.
Material Design and Composition
The creation of high-performance, 3D-printable hydrogel inks hinges on a sophisticated multi-material approach. This strategy involves selecting a base polymer for scaffold formation, incorporating functional fillers for electronic properties, and employing crosslinking mechanisms to fine-tune mechanical behavior.
Base Polymers and Network Design
The foundation of any hydrogel ink is its polymer network, which can be derived from natural, synthetic, or hybrid sources. The choice of polymer dictates the ink's basic biocompatibility, gelation kinetics, and structural integrity.
- Natural Polymers: Materials like alginate, chitosan, gelatin, and hyaluronic acid are prized for their inherent bioactivity and biocompatibility. They often contain cell-adhesion motifs and are susceptible to enzymatic degradation, facilitating cell-mediated remodeling [53] [58]. However, they can suffer from batch-to-batch variability and limited independent tunability of mechanical properties [53]. To enhance their printability and mechanical strength, natural polymers are often chemically modified. A prominent example is gelatin methacryloyl (GelMA), where methacrylate groups are grafted onto gelatin, allowing it to form stable, UV-cross-linkable hydrogels [53].
- Synthetic Polymers: Polymers such as polyethylene glycol (PEG), polyacrylamide (PAAm), and Pluronic F-127 offer a "blank slate" with high reproducibility and precise control over mechanical properties [53] [59]. Their properties can be tuned independently of biological cues, making them ideal for fundamental mechanobiology studies. Triblock copolymers like Pluronic F-127 are particularly useful for 3D printing, as they provide high viscosity for fine-resolution printing through thermal gelation [59].
- Interpenetrating Networks (IPNs): To overcome the limitations of single-network hydrogels, IPNs are frequently employed. An IPN consists of two or more independent polymer networks interlaced on a molecular scale [58]. A common design involves a first network providing structural integrity and a second, conductive network enabling functionality. For instance, a loose physical gel of PEDOT:PSS can be interpenetrated with a robust secondary polymer network (e.g., PEG-diacrylate), resulting in a hydrogel that is both mechanically sturdy and highly conductive [55].
Functional Nanofillers
To transition from passive scaffolds to active bioelectronic components, hydrogel inks are infused with functional nanofillers.
- Conductive Polymers: Poly(3,4-ethylenedioxythiophene):poly(styrene sulfonate) (PEDOT:PSS) is a frontrunner due to its commercial availability, water solubility, biocompatibility, and intrinsic conductivity [55]. It is typically used in the form of colloidal particles dispersed in the aqueous ink.
- Carbon-Based Materials: Functionalized Carbon Nanotubes (fCNTs) are incorporated to significantly enhance electrical conductivity and mechanical toughness [57]. Their high aspect ratio and conductivity create efficient percolation networks within the hydrogel. Graphene oxide (GO) is another versatile filler, which can impart photothermal properties, allowing for light-triggered modulation of the hydrogel's modulus [59].
Cross-Linking Strategies for Modulus Tunability
The elastic modulus of a hydrogel is primarily governed by its cross-link density. Advanced inks employ a combination of cross-linking mechanisms to achieve a wide and reversible range of stiffness.
- Covalent Cross-Linking: This involves forming permanent chemical bonds between polymer chains using reactions such as free radical polymerization (initiated by UV light or heat), Schiff base formation, or click chemistry. This provides mechanical stability but is typically irreversible [56] [58].
- Physical Cross-Linking: This relies on dynamic, non-covalent interactions, including:
- Ionic Interactions: Divalent cations (e.g., Ca²⁺) can cross-link anionic polymers like alginate. The use of calcium propionate, which carries hydrophobic groups, can create cross-links that strengthen with temperature, leading to thermal stiffening [59].
- Hydrophobic Interactions: The aggregation of hydrophobic domains in polymers like Pluronic F-127 or modified polymers can form physical cross-links that are temperature-sensitive [59].
- Interfacial Jamming: In liquid-in-liquid printing, the self-assembly of PEDOT:PSS particles and PDMS-based surfactants at the water-oil interface forms an elastic film that kinetically traps the ink in a 3D shape before permanent gelation [55].
The synergy of these mechanisms allows for the creation of hydrogels with tunable mechanics (Young's modulus of 10–300 kPa), high stretchability (up to ~1000% strain), and self-healing properties [57].
Table 1: Key Components of Multifunctional Hydrogel Inks
| Component Category | Example Materials | Primary Function | Key Characteristic |
|---|---|---|---|
| Base Polymer | GelMA, Alginate, Chitosan, PEG, Pluronic F-127, PAAm | Provides the 3D scaffold, hydrates the network, determines baseline biocompatibility. | GelMA: Photocross-linkable, bioactive. Pluronic: Thermoresponsive, good for printability. |
| Conductive Filler | PEDOT:PSS, fCNTs | Imparts electrical conductivity to the hydrogel. | PEDOT:PSS: High conductivity, biocompatible. fCNTs: High conductivity, improves toughness. |
| Mechanical Modulator | Ca²⁺ ions, PDMS-NH₂, covalent cross-linkers (e.g., MBAm) | Tunes the elastic modulus and viscoelastic properties through cross-link density. | Ca²⁺ ions: Enable ionic cross-linking, can be temperature-sensitive. |
| Functional Additive | Graphene Oxide (GO) | Adds advanced properties like photothermal response. | GO: Enables light-controlled modulus changes. |
3D Printing Techniques for Hydrogels
Not all 3D printing techniques are suitable for processing soft, water-rich hydrogel inks. The most commonly used methods are material extrusion, vat photopolymerization, and material jetting, each with distinct advantages and limitations for biofabrication [56].
Material Extrusion (MEX)
In material extrusion, the hydrogel ink is selectively dispensed through a nozzle or orifice onto a build platform [56]. It is one of the most widely used techniques due to its accessibility and ability to handle high-viscosity materials and cell-laden inks.
- Process: A pneumatic or mechanical (piston/screw) system applies pressure to extrude a continuous filament of ink in a layer-by-layer fashion.
- Ink Requirements: Inks must exhibit shear-thinning behavior (viscosity decreases under shear stress during extrusion) and rapid recovery to maintain the shape of the deposited filament. Thermoresponsive polymers like Pluronic F-127 are ideal, as they are liquid at low temperatures and gel upon warming on the build plate [59].
- Advantages: Compatible with a wide range of materials and bioprinting; relatively low cost.
- Limitations: Limited resolution (typically >100 μm); potential for high shear stresses that can damage encapsulated cells.
Vat Photopolymerization (VP)
This technique uses a light source to selectively cure a liquid photopolymer resin in a vat layer by layer. Stereolithography (SLA) and Digital Light Processing (DLP) are common VP technologies [56].
- Process: In SLA, a laser scans the surface of the vat, curing the resin at specific points. In DLP, an entire layer is projected and cured at once, significantly speeding up the process.
- Ink Requirements: Inks must be photo-curable, typically containing photointiators and light-sensitive polymers like GelMA or PEG-diacrylate.
- Advantages: High resolution and accuracy (can achieve features <50 μm); fast printing speed (especially DLP); smooth surface finish.
- Limitations: Limited to photopolymerizable materials; potential cytotoxicity of photoinitiators and UV light; difficulty in creating multi-material structures.
Liquid-in-Liquid 3D Printing
This is an emerging freeform technique that enables the fabrication of complex 3D structures without the need for layered deposition.
- Process: An aqueous hydrogel ink is extruded into an immiscible oil bath. The key innovation is the use of interfacial jamming, where components like PEDOT:PSS and PDMS-NH₂ surfactants spontaneously assemble at the liquid-liquid interface to form an elastic film [55]. This film arrests Rayleigh-Plateau instabilities and kinetically traps the ink in the designed 3D non-equilibrium shape, which is then stabilized via chemical or physical gelation.
- Ink Requirements: The ink and oil phases must be formulated to promote rapid interfacial assembly. Controlling the pH is often critical to optimize electrostatic interactions between components [55].
- Advantages: Enables overhanging structures and complex geometries without support materials; decouples printing rheology from final mechanical properties.
- Limitations: A relatively new and complex process requiring precise control over interfacial chemistry.
Diagram 1: Workflow for 3D Printing Hydrogel Inks. This chart outlines the decision points and parallel processes for different advanced printing techniques.
Experimental Protocols and Characterization
Rigorous characterization is essential to link the composition and processing of hydrogel inks to their final properties and performance.
Measuring Mechanical Properties
Accurately determining the Young's modulus (E) of soft hydrogels is critical for mechanobiology and ensuring mechanical compatibility with tissues.
- Atomic Force Microscopy (AFM): Considered the gold standard for measuring the local elastic modulus of hydrogels at the micro-scale. A cantilever with a sharp tip indents the sample, and the force-displacement curve is used to calculate E [60].
- Macroindentation: A simple, low-cost, and high-throughput alternative. A sphere of known weight and radius is placed on the hydrogel, and the indentation depth (δ) is measured optically. The Young's modulus is calculated using a modified Hertzian model that accounts for the finite geometry of the sample [60]: E_NH-fdh = (9F / 16R^(1/2)δ^(3/2)) * (f(R/h, ω) / g(δ/h, Rh/D²)) where F is the force, R is the sphere radius, h is the gel height, and D is the gel diameter. The factors f and g are correction factors [60].
- Rheometry: Used to characterize the viscoelastic properties of hydrogels, typically reported as the storage modulus (G', elastic response) and loss modulus (G", viscous response). This is crucial for understanding the ink's behavior during printing and its performance under dynamic mechanical stress.
Table 2: Quantitative Performance of Multifunctional Hydrogel Inks
| Material System | Young's Modulus (Elasticity) | Electrical Conductivity | Key Functional Properties | Reference |
|---|---|---|---|---|
| PEDOT:PSS-based IPN | Tunable within physiological range | Up to 301 S/m (with 9 mg/mL PEDOT:PSS) | High conductivity for a low filler content; suitable for implantable chips. | [55] |
| fCNT-Nanocomposite | 10 - 300 kPa | ~20 S/m | Stretchability (~1000% strain), self-healing (within 5 min), toughness (400-731 kJ/m³). | [57] |
| Pluronic F-127 / Ionic | Thermally tunable (reversible) | N/A (Focus on mechanics) | Thermal stiffening effect triggered by temperature or light (with GO additive). | [59] |
| Standard PAAm Hydrogels | <0.7 kPa to 40 kPa | N/A (Model system) | Used as a well-characterized model for validating mechanobiology measurement techniques. | [60] |
Protocol: Fabrication of a 3D-Printed Conductive Hydrogel via Liquid-in-Liquid Printing
This protocol outlines the key steps for creating a high-conductivity, 3D-PEDOT:PSS hydrogel structure [55].
Ink Preparation:
- Prepare the aqueous hydrogel precursor ink. This typically contains:
- PEDOT:PSS dispersion (e.g., 0.1–20 mg/mL).
- A secondary polymer precursor (e.g., PEG-diacrylate) for forming an interpenetrating network.
- A photoinitiator (e.g., Irgacure 2959) for UV cross-linking.
- Adjust the pH of the ink to ~2.07 using an acid like HCl to optimize the co-assembly kinetics with the surfactant.
- Prepare the aqueous hydrogel precursor ink. This typically contains:
Oil Bath Preparation:
- Prepare an immiscible oil phase (e.g., toluene or silicone oil).
- Dissolve a PDMS-based surfactant terminated with primary amines (PDMS-NH₂, e.g., Mn 4000 g/mol) into the oil phase at a concentration of 10 vol%.
Printing and Interfacial Jamming:
- Load the aqueous ink into a syringe equipped with a dispensing nozzle.
- Extrude the ink into the prepared oil bath. The extrusion rate must be optimized (e.g., 0.07 mL/min) to prevent jet breakup.
- As the ink is extruded, PEDOT:PSS particles and PDMS-NH₂ surfactants rapidly co-assemble at the water-oil interface via electrostatic interactions, forming a jammed elastic film (PPSs). This film stabilizes the extruded filament in its programmed 3D shape.
Gelation and Post-Processing:
- Once the 3D structure is fully printed, expose the entire construct to UV light (e.g., 365 nm wavelength) for a specified duration to photopolymerize the secondary polymer network (e.g., PEG-diacrylate), locking the structure permanently.
- Carefully retrieve the cured hydrogel structure from the oil bath.
- Wash the structure thoroughly with a solvent like ethanol and then water to remove residual oil and surfactants.
Applications in Bioelectronics and Mechanobiology
The unique properties of 3D-printed modulus-tunable hydrogels open up transformative applications at the interface of biology and electronics.
- Implantable Bioelectronic Devices: These hydrogels can be fabricated into soft, conformable electrodes for neural interfaces, mitigating the foreign body response and improving signal fidelity. Their biocompatibility and matched modulus allow for seamless integration with brain or nerve tissue for applications in treating neurological disorders [55] [52]. Furthermore, they can be customized into implantable biochips for near-field communication (NFC), enabling wireless monitoring and therapy [55].
- Wearable Biosensors: The combination of stretchability, conductivity, and self-healing makes these hydrogels ideal for wearable strain sensors. They can be 3D-printed into ring-shaped sensors that monitor physiological signals like pulse or joint movement, providing comfortable and long-term tracking due to their mechanical tissue compatibility [57].
- Disease Modeling and Drug Screening: Hydrogels with tunable stiffness provide in vitro platforms to study disease mechanisms. For instance, pancreatic tumouroids and kidney organoids cultured in 3D hydrogels that mimic the stiffness of fibrotic microenvironments have been shown to exhibit disease-specific behaviors, providing a powerful model for drug screening and toxicity testing [53] [56].
- Regenerative Medicine and Tissue Engineering: By mimicking the mechanical properties of specific tissues, these hydrogels guide stem cell differentiation and tissue regeneration. Human mesenchymal stem cells (hMSCs) differentiate towards osteogenic lineages on stiffer substrates and adipogenic lineages on softer ones [53]. 3D-printed hydrogel scaffolds can thus be designed to promote the regeneration of bone, cartilage, or muscle.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Modulus-Tunable Conductive Hydrogels
| Reagent / Material | Function in the Experiment | Typical Example / Specification |
|---|---|---|
| PEDOT:PSS Dispersion | Provides the primary conductive component in the hydrogel ink. | Heraeus Clevios PH1000; typically used at 0.1-20 mg/mL [55]. |
| PDMS-NH₂ Surfactant | Co-assembles with PEDOT:PSS at the liquid-liquid interface to enable 3D structuring. | Bis(3-aminopropyl)-terminated polydimethylsiloxane (Mn ~4000 g/mol) [55]. |
| Pluronic F-127 | A thermoresponsive triblock copolymer that enhances printability and contributes to thermal stiffening. | Sigma-Aldrich; used as a base polymer for extrusion-based printing [59]. |
| Functionalized CNTs (fCNTs) | Significantly enhances electrical conductivity and mechanical toughness of the composite hydrogel. | Carboxylated or aminated single-walled/multi-walled carbon nanotubes [57]. |
| GelMA (Gelatin Methacryloyl) | A photopolymerizable, bioactive base polymer derived from natural gelatin. | Often synthesized in-house or sourced from companies like Advanced BioMatrix [53] [54]. |
| Calcium Propionate | A source of Ca²⁺ ions that enables ionic and hydrophobic cross-linking, leading to thermal stiffening. | Used in Pluronic-based systems to create additional physical crosslinks at high temperatures [59]. |
| Photoinitiator | Initiates polymerization upon exposure to light, crucial for vat photopolymerization and post-print curing. | Irgacure 2959 (for UV light, ~365 nm) [55]. |
The development of 3D-printable, modulus-tunable, and multifunctional hydrogel inks represents a significant leap forward in bioelectronic materials research. By leveraging sophisticated material designs that combine polymers and nanofillers through multiple cross-linking mechanisms, researchers can now engineer hydrogels that precisely mimic the mechanical and functional properties of biological tissues. Coupled with advanced fabrication techniques like liquid-in-liquid printing, these inks enable the creation of complex, customized 3D structures that seamlessly integrate with the human body. As the field progresses, the convergence of these smart materials with artificial intelligence for design optimization and decentralized manufacturing models will further accelerate the development of next-generation bioelectronic devices for personalized medicine, advanced diagnostics, and regenerative therapies.
Solving Real-World Challenges: Durability, Stability, and Long-Term Performance
Strategies for Enhancing Mechanical Robustness and Fracture Resistance
The advancement of bioelectronic interfaces, particularly for neural applications, is fundamentally constrained by the mechanical mismatch between conventional rigid electronic materials and soft, dynamic biological tissues. This disparity in Young's modulus—a critical measure of a material's stiffness or resistance to elastic deformation under stress—can induce significant inflammatory responses, fibrotic encapsulation, and device failure, thereby compromising long-term functionality and biocompatibility [7]. For brain tissue, which exhibits a Young's modulus in the range of 1–4 kilopascals (kPa), traditional inorganic materials like metals and silicon are millions of times stiffer, creating a profound mechanical mismatch [7]. Therefore, developing strategies to engineer materials with tissue-like mechanical properties, particularly a compliant Young's modulus, while maintaining electrical performance and fracture resistance, is a paramount objective in modern bioelectronics research. This whitepaper details advanced material and engineering strategies to enhance the mechanical robustness and fracture resistance of bioelectronic materials, with a specific focus on their implications for Young's modulus.
Material-Based Enhancement Strategies
The core of enhancing mechanical compatibility lies in developing materials that intrinsically possess a low Young's modulus and high fracture toughness.
Conductive Polymer Composites
Poly(3,4-ethylenedioxythiophene):polystyrenesulfonate (PEDOT:PSS) has emerged as a leading conductive polymer for biointerfaces due to its combination of high electrical conductivity, excellent biocompatibility, and mechanically compliant nature. Its Young's modulus can be engineered to fall within a range of 0.1 to 10 Megapascals (MPa), dramatically closer to that of neural tissue (1-4 kPa) than rigid alternatives [7].
Strategies to tailor the properties of PEDOT:PSS include:
- Chemical Additives and Cross-linking: The incorporation of additives like ethylene glycol (EG) or dodecylbenzenesulfonic acid (DBSA), followed by thermal annealing, can significantly enhance electrical conductivity, achieving values up to 652 S/cm [7]. Simultaneously, formulating PEDOT:PSS into hydrogels with cross-linkers such as poly(vinyl alcohol) (PVA) can yield materials with a stretchability of up to 72% strain and a Young's modulus of 191 kPa, further closing the mechanical gap with soft tissue [7].
- Composite Formations: Creating composites with carbon nanotubes (CNTs) or other polymers allows for the optimization of the mechanical and electrical property matrix. For instance, a PEDOT:PSS and PHEMA-based composite has been used to create microelectrode arrays (MEAs) with a Young's modulus of 322 kPa and a high charge injection capacity [7].
Atomic Layer Deposition (ALD) for Interface Engineering
While ALD is typically used to deposit thin, stiff ceramic coatings, a novel approach leverages the residual stresses within these films to enhance fracture resistance in underlying substrates. Research on micro-architected ceramics has demonstrated that ALD coatings like Al₂O₃ can induce beneficial compressive stresses in the substrate, thereby increasing the apparent fracture toughness by up to 165% in systems such as fused silica micro-pillars [61]. This stress engineering strategy is particularly powerful for architected meta-materials with high surface-to-volume ratios, where the interface properties dominate the macroscopic mechanical behavior [61].
Hydrogels and Soft Composites
Hydrogels represent the state of the art in matching the native mechanical environment of cells and tissues. Their networks of hydrophilic polymers can be tuned to exhibit a wide range of Young's moduli, from fractions of a kPa to several hundred kPa. Conductive hydrogels, formed by blending conductive polymers like PEDOT:PSS with hydrogel matrices, are ideal for bioelectronics. As shown in Table 1, a PEDOT:PSS-based hydrogel processed via direct ink writing (DIW) can achieve a Young's modulus as low as 31 kPa in its hydrogel state, which is exceptionally compliant [7].
The following tables summarize key quantitative data from the literature, providing a direct comparison of the mechanical and electrical properties achievable through different material strategies.
Table 1: Mechanical and Electrical Properties of PEDOT:PSS-Based Formulations
| Active Components | Material Format | Young's Modulus | Conductivity / Electrode Impedance | Key Mechanical Feature | Ref. |
|---|---|---|---|---|---|
| PEDOT:PSS, DMSO | Hydrogel (Annealed) | 1.1 MPa | 28 S/cm | Stiffness suitable for microfabrication | [7] |
| PEDOT:PSS, CNT, PHEMA | Spherical Electrode | 10 kPa | ~1 kΩ at 1 kHz | Matches brain tissue softness | [7] |
| PEDOT:PSS, PVA | Hydrogel | 191 kPa | 1.14 kΩ at 1 kHz | 72% strain stretchability | [7] |
| PEDOT:PSS, DBSA | Hydrogel (DIW) | 31 kPa (Hydrogel) | 35 S/cm (Hydrogel) | Compliant, printable ink | [7] |
| PEDOT:PSS, H₂SO₄ | Spin-coated Film | Not Specified | 652 S/cm; 90 kΩ at 1 kHz | High conductivity for thin films | [7] |
Table 2: Fracture Toughness Enhancement via ALD Coating
| Substrate Material | Coating Material | Change in Fracture Toughness | Key Mechanism | Ref. |
|---|---|---|---|---|
| Fused Silica | Al₂O₃ | +165% | Tensile stress in coating induces substrate compression | [61] |
| Glassy Carbon | Al₂O₃ | Reduction (Specific % not stated) | Differing crack morphology leading to adverse failure | [61] |
Experimental Protocols for Key Measurements
Reproducible and accurate characterization of mechanical and electrical properties is fundamental to research in this field. Below are detailed protocols for two critical techniques.
Nanoindentation for Young's Modulus Measurement
Nanoindentation is a standard method for determining the Young's modulus of thin films and small material volumes.
Detailed Protocol:
- Instrument and Tip: Use a commercial nanoindenter (e.g., MTS NanoIndenter XP) equipped with a Berkovich diamond indenter tip [62].
- Sample Preparation: Mount the sample (e.g., a DNA film or polymer coating) firmly on the sample stage to prevent movement. Ensure the surface is clean and level.
- Calibration: Calibrate the instrument and the area function of the indenter tip using a standard reference sample with a known modulus (e.g., fused silica).
- Testing Parameters:
- Set the indentation depth range for analysis. For soft films, a range of 100 to 200 nm is often representative, avoiding influences from the underlying substrate or excessive surface effects [62].
- Utilize the Continuous Stiffness Measurement (CSM) module to measure stiffness continuously as a function of depth.
- Data Analysis: Apply the Oliver-Pharr method to the load-displacement data to determine the reduced modulus (Eᵣ) and hardness [62]. The representative Young's modulus (Eₛ) of the sample is then calculated using the following relationship, assuming a Poisson's ratio (νₛ) for the material (e.g., 0.3 for a DNA film [62]):
- 1/Eᵣ = (1 - νₛ²)/Eₛ + (1 - νᵢ²)/Eᵢ
- Where Eᵢ and νᵢ are the Young's modulus and Poisson's ratio of the indenter tip (for diamond, Eᵢ = 1140 GPa, νᵢ = 0.07).
- Replication: Repeat the test across multiple locations on the sample (e.g., nine trials) to obtain a statistically significant average value [62].
Piezoelectric Ultrasonic Composite Oscillator Technique
This technique is highly effective for simultaneously characterizing the Young's modulus and internal friction (damping) of materials, especially low-melting-point metals like gallium, which are difficult to machine.
Detailed Protocol:
- System Setup: Construct a composite oscillator system where the sample is acoustically bonded between a drive piezoelectric transducer and a receiver piezoelectric transducer [12].
- Resonance Measurement: Sweep the frequency of the applied AC signal to the drive transducer to find the system's resonance and anti-resonance frequencies.
- Data Collection: Record these frequencies at varying temperatures of interest (e.g., from -70 °C to 20 °C for gallium) [12].
- Calculation:
- Young's Modulus: Use explicit theoretical formulas that relate the resonant frequency shifts to the elastic modulus of the sample material. The modulus is calculated from the measured data, revealing its temperature dependence (e.g., a linear decrease from 83.84 GPa at -70 °C to 79.37 GPa at 20 °C for gallium) [12].
- Internal Friction: Determine the internal friction (or damping capacity) from the width of the resonance peak or the difference between resonance and anti-resonance frequencies. This can reveal material relaxation processes, such as the longitudinal internal friction peak observed in gallium at approximately -12 °C [12].
Visualization of Strategy Development and Workflow
The following diagrams illustrate the logical relationship between the different enhancement strategies and a standard experimental workflow for developing and characterizing a compliant bioelectronic material.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table catalogs key materials and reagents used in the featured research for developing robust bioelectronic interfaces.
Table 3: Essential Research Reagents and Materials
| Item Name | Function / Application | Key Characteristics / Rationale |
|---|---|---|
| PEDOT:PSS | Primary conductive polymer for electrodes and coatings. | High conductivity, mechanical flexibility, biocompatibility, and solution processability [7]. |
| Ethylene Glycol (EG) / DMSO | Secondary dopant for PEDOT:PSS. | Enhances electrical conductivity by several orders of magnitude through molecular rearrangement [7]. |
| Dodecylbenzenesulfonic Acid (DBSA) | Surfactant and conductivity enhancer for PEDOT:PSS. | Improves film formation and electrical performance [7]. |
| (3-Glycidyloxypropyl)trimethoxysilane (GOPS) | Cross-linker for PEDOT:PSS. | Increases water stability and mechanical integrity of films [7]. |
| Poly(vinyl alcohol) (PVA) / PHEMA | Hydrogel matrix polymer. | Provides a soft, hydrating network to match tissue mechanics and enable stretchability [7]. |
| Carbon Nanotubes (CNTs) | Conductive filler in composites. | Enhances electrical conductivity and mechanical toughness of polymer composites [7]. |
| ALD Al₂O₃ / ZnO | Thin-film coating for interface engineering. | Imparts residual stress to modify fracture behavior and enhance toughness of micro-structures [61]. |
| Berkovich Diamond Indenter | Nanoindentation tip. | Standard geometry for measuring Young's modulus and hardness of small volumes and thin films [62]. |
| Piezoelectric Ultrasonic Composite Oscillator | Measurement setup for elastic properties. | Enables simultaneous measurement of Young's modulus and internal friction, especially for challenging materials like gallium [12]. |
The convergence of material science and mechanical engineering is driving a paradigm shift in bioelectronics towards devices that are not only electrically sophisticated but also mechanically harmonious with biological systems. The strategies outlined—centered on engineering a compliant Young's modulus through conductive polymers, hydrogels, and sophisticated interface control—provide a robust roadmap for developing the next generation of neural interfaces. By systematically applying these strategies and employing rigorous characterization protocols, researchers can create devices that minimize immune response, ensure long-term stability, and ultimately unlock the full therapeutic and diagnostic potential of bioelectronic medicine.
Combating Swelling and Maintaining Electrical Performance in Humid Environments
In the field of bioelectronic materials research, the interplay between environmental humidity, material swelling, and electrical performance presents a critical challenge. Bioelectronic devices, designed for intimate integration with biological tissues, frequently operate in hydrated environments nearing 100% relative humidity (RH). This exposure can lead to water uptake, volumetric swelling, and plasticization of polymer matrices, ultimately degrading their mechanical integrity and electrical functionality. The Young's modulus, a fundamental descriptor of material stiffness, is highly sensitive to water content, with implications for both device reliability and biocompatibility. A mechanical mismatch at the biotic-abiotic interface can induce shear stresses, provoke foreign-body responses, and lead to device failure. This whitepaper synthesizes current research to provide a technical guide on the mechanisms of humidity-induced degradation and the strategies to mitigate it, ensuring the stable performance of bioelectronic materials in humid environments.
Core Mechanisms: How Humidity Affects Material Properties
Humidity impacts bioelectronic materials through two primary pathways: the alteration of mechanical properties and the disruption of electrical conduction. Understanding these mechanisms is foundational to developing effective countermeasures.
Swelling and Plasticization
The infiltration of water molecules into a polymer matrix can significantly alter its mechanical properties. For polyelectrolyte multilayers (PEMs) and related polymers, exposure to humid environments leads to substantial swelling and a decrease in Young's modulus, a phenomenon known as plasticization [63]. The extent of this effect is governed by the material's chemical composition and molecular architecture. For instance, PEM systems rich in hydrogen-bonding sites can exhibit unique behaviors, including an abrupt swelling transition at intermediate humidity or even anti-plasticization in some cases [63]. The water absorption process in many polymers follows a recognizable pattern: a stage of rapid uptake (0–12 hours), followed by a plateau (12–60 hours), and sometimes a late rebound (60–100 hours) [64].
Non-Monotonic Electrical Response
The effect of humidity on electrical conductivity is particularly complex in conjugated polyelectrolytes (CPEs), which are mixed ionic-electronic conductors (MIECs). Studies on materials like the poly[3-(potassium-n-alkanoate) thiophene-2,5-diyl] (P3KnT) series reveal a non-monotonic relationship between electronic conductivity (( \sigmae )) and relative humidity [65]. Initially, hydration facilitates a self-doping mechanism, where water molecules liberate free cations, allowing bound anions to stabilize charge carriers (polarons) on the polymer backbone. This process increases ( \sigmae ) up to a critical RH point. Beyond this point, however, electronic conductivity decreases. This decline is attributed to two factors:
- Disruption of Ordered Domains: Water infiltration swells the material, disrupting the locally ordered, π-stacked domains that are crucial for efficient electronic transport [65].
- Swelling of Amorphous Domains: The swelling of amorphous domains impedes the electronic transport pathways that connect the ordered domains [65].
In contrast, ionic conductivity (( \sigma_i )) in these systems demonstrates a consistent, monotonic increase with rising RH, as the presence of more water facilitates ion mobility [65].
Quantitative Data on Material Performance in Humid Environments
The following tables summarize experimental data on the response of various polymers and composites to humidity, providing a basis for material selection.
Table 1: Water Absorption and Tensile Properties of FFF Polymers at Different Humidity Levels [64].
| Polymer | Total Water Uptake Ranking | Young's Modulus Trend with Increasing RH | Ultimate Tensile Strength Trend with Increasing RH |
|---|---|---|---|
| Nylon | Highest | Significant Decrease | Decrease |
| PETG | High | Decrease | Decrease |
| PLA | Medium | Decrease | Decrease |
| ABS | Medium | Decrease | Decrease |
| TPU | Low | Decrease | Decrease |
| PEEK | Low | Slight Decrease | Slight Decrease |
Table 2: Humidity-Dependent Mixed Conductivity in P3KnT Conjugated Polyelectrolytes [65].
| Polymer | Side-chain Length (n) | Ionic Conductivity, ( \sigma_i ) (S/cm) | Electronic Conductivity, ( \sigma_e ) (S/cm) | Peak ( \sigma_e ) Humidity |
|---|---|---|---|---|
| P3K4T | 4 | Monotonic increase to ~10⁻² at 95% RH | Non-monotonic; peaks then decreases | ~65% RH |
| P3K5T | 5 | Monotonic increase to ~10⁻² at 95% RH | Non-monotonic; peaks then decreases | ~75% RH |
| P3K6T | 6 | Monotonic increase to ~10⁻¹ at 95% RH | Non-monotonic; peaks then decreases | ~80% RH |
| P3K7T | 7 | ~10⁻¹ at 95% RH | ~1.7×10⁻² at 85% RH; ~8.0×10⁻³ at 95% RH | ~85% RH |
Experimental Protocols for Characterizing Humidity Effects
To evaluate and screen materials for humid environment applications, researchers can employ the following standardized experimental protocols.
Humidity-Dependent Tensile Testing
Objective: To characterize the mechanical properties (Young's modulus, ultimate tensile strength, strain at break) of polymer specimens as a function of relative humidity. Materials: Universal testing machine, environmental chamber with humidity control, dog-bone tensile specimens (e.g., according to ASTM D638), data acquisition system. Methodology:
- Specimen Acclimatization: Condition tensile specimens in controlled environments at target RH levels (e.g., 15%, 45%, 95%) for a predetermined duration (e.g., 100 hours) to ensure equilibrium moisture uptake [64].
- Mechanical Testing: Perform uniaxial tensile tests on acclimatized specimens inside the environmental chamber to maintain constant RH conditions during testing.
- Data Analysis: Calculate Young's modulus from the initial linear slope of the stress-strain curve. Determine ultimate tensile strength and elongation at break from the peak of the curve and strain at failure, respectively.
In Situ Humidity-Dependent GIWAXS
Objective: To correlate the non-monotonic electronic conductivity changes with nanoscale structural evolution under humidity. Materials: Grazing incidence wide-angle X-ray scattering (GIWAXS) setup, humidity-controlled sample cell, thin-film specimens of conductive polymers. Methodology:
- Humidity Control: Mount the thin-film sample in a cell where the RH can be precisely controlled and varied.
- Scattering Measurement: Collect 2D GIWAXS patterns at incremental RH levels, particularly through the range where electronic conductivity is known to peak and decline [65].
- Structural Analysis: Analyze the scattering patterns to determine the evolution of π-stacking peak positions, intensities, and full width at half maximum (FWHM). A loss of intensity and peak broadening at high RH indicates the disruption of ordered domains, directly linking structure to the drop in ( \sigma_e ) [65].
Electrochemical Impedance Spectroscopy
Objective: To deconvolute and measure the ionic (( \sigmai )) and electronic (( \sigmae )) conductivity of mixed conductors under humidity. Materials: Potentiostat with impedance capability, two-point or four-point probe cell, environmental chamber. Methodology:
- Sample Preparation: Fabricate thin-film devices with appropriate electrodes for in-plane conductivity measurements.
- Impedance Measurement: Perform EIS measurements across a frequency range (e.g., 1 Hz to 1 MHz) at various RH levels.
- Data Fitting: Fit the resulting impedance spectra to an equivalent circuit model. The low-frequency response is often dominated by ionic transport, while the high-frequency response relates to electronic transport. This allows for the extraction of separate ( \sigmai ) and ( \sigmae ) values [65].
Protection Strategies and Material Design Solutions
Combating swelling and performance degradation requires a multi-faceted approach, from material-level innovation to device-level protection.
Material Selection and Chemical Tuning
- Side-Chain Engineering: As demonstrated by the P3KnT series, increasing the length of hydrophobic alkyl side chains (e.g., from P3K4T to P3K7T) enhances resiliency to swelling. Longer side chains better shield the conductive backbone, allowing materials to maintain higher electronic conductivity at elevated RH [65].
- Utilization of Organogels: Unlike water-swollen hydrogels, organogels (polymer networks swollen with organic solvents) exhibit superior resistance to dehydration and swelling in aqueous environments, making them attractive for robust bioelectronic applications [28].
- Development of Hybrid Systems: Organohydrogels, which integrate both hydrophilic and hydrophobic domains into a unified network, offer a promising path forward. These materials can exhibit resilience to freezing, self-healing capabilities, and stable performance under extreme environmental conditions [28].
Device-Level Protection Strategies
- Conformal Coatings: Applying a thin, protective polymeric layer (e.g., acrylic, urethane, or silicone) directly onto a printed circuit board (PCB) creates a barrier against moisture ingress. This is a primary defense against short circuits and corrosion [66].
- Enclosure Design: Employing enclosures with a high Ingress Protection (IP) rating (e.g., IP67 or IP68) is crucial for devices exposed to liquids or high humidity. The IP rating defines the level of protection against solids and liquids, with higher numbers indicating better protection [66].
- Strategic Use of Desiccants: For packaged systems or during storage, incorporating desiccants like silica gel can control internal humidity by adsorbing ambient moisture, thereby protecting sensitive components [66].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Humidity Effects Research.
| Item | Function/Description | Example Use-Case |
|---|---|---|
| Tetra-PEG Gel | A model polymer gel system with a uniform network structure and low degree of defects. | Serves as an ideal system for rigorously testing theories of gel elasticity and swellability without the complicating effects of structural inhomogeneities [67]. |
| P3KnT Conjugated Polyelectrolytes | A series of polythiophene-based CPEs with varying alkyl side-chain lengths (n=4-7). | Used to study the structure-property relationship between side-chain chemistry, humidity-induced swelling, and mixed ionic-electronic conductivity [65]. |
| Polyelectrolyte Multilayer (PEM) Films | Ultrathin films fabricated via layer-by-layer deposition of oppositely charged polyelectrolytes. | Model systems for investigating the effect of RH on the Young's modulus of polyelectrolyte-based materials and the role of molecular architecture [63]. |
| Environmental Chamber | A test enclosure capable of precisely controlling temperature and relative humidity. | Essential for acclimatizing specimens and performing mechanical or electrical characterization under constant, known RH conditions [64]. |
| Dynamic Vapor Sorption (DVS) Instrument | Measures the equilibrium water uptake and swelling kinetics of a material as a function of RH. | Quantifies the extent of water absorption and dimensional changes in polymer films under humid conditions [65]. |
| Grazing Incidence Wide-Angle X-Ray Scattering (GIWAXS) | A technique for characterizing the nanoscale structure and morphology of thin films. | Used for in situ monitoring of humidity-induced structural changes, such as the disruption of π-stacked domains in conjugated polymers [65]. |
The challenge of maintaining electrical performance in the face of humidity-driven swelling is a central concern in advancing bioelectronic materials. The phenomenon is complex, involving a trade-off between the hydration necessary for ionic conduction and biocompatibility, and the structural integrity required for electronic performance and mechanical stability. Research has shown that the Young's modulus of many polymeric materials is highly sensitive to moisture, and that electrical conductivity often follows a non-monotonic path with increasing humidity. Addressing this requires a holistic strategy, combining intelligent material design—such as side-chain engineering and the development of hybrid gel systems—with robust device-level protection, including conformal coatings and sealed enclosures. The experimental protocols and materials outlined in this whitepaper provide a roadmap for researchers to characterize these effects systematically and develop next-generation bioelectronic devices capable of reliable operation in humid physiological environments.
Self-healing materials (SHMs) represent a transformative advancement in materials science, offering the capability to automatically repair damage and restore functional integrity without external intervention. Within bioelectronic devices—which form critical interfaces between electronic components and biological tissues—the integration of self-healing properties addresses fundamental challenges in device longevity, mechanical compliance, and functional reliability. The mechanical properties of these materials, particularly Young's modulus (the ratio of tensile stress to tensile strain), must be carefully engineered to match the moduli of biological tissues (typically 0.1 kPa to 1 GPa) to minimize interfacial stress and maintain signal fidelity at the biotic-abiotic interface.
These materials employ either intrinsic mechanisms (utilizing inherent reversible bonds within the material) or extrinsic mechanisms (incorporating encapsulated healing agents that release upon damage) to achieve autonomous repair. The development of SHMs for bioelectronics represents an interdisciplinary frontier spanning materials science, chemistry, electronics, and bioengineering, with the potential to significantly enhance the durability and operational lifespan of medical implants, wearable sensors, and other biointegrated devices.
Fundamental Mechanisms of Self-Healing
Self-healing mechanisms are broadly categorized as extrinsic or intrinsic, each with distinct operational principles and material requirements crucial for bioelectronic integration.
Extrinsic Self-Healing Systems
Extrinsic systems incorporate pre-embedded healing agents that release upon damage:
- Microcapsule-Based Systems: Polymer shells (e.g., urea-formaldehyde, silica) containing healing agents (monomers, catalysts, or solvents) rupture when damage occurs, releasing their contents into crack planes. Subsequent polymerization restores mechanical integrity [68]. Key parameters include microcapsule size distribution, shell thickness, and core content, which directly influence healing efficiency and kinetics.
- Vascular Systems: interconnected microchannel networks (inspired by biological circulatory systems) store and transport healing agents. These systems enable multiple healing cycles at the same site, unlike single-use microcapsules. Vascular networks can be constructed as 1D, 2D, or 3D structures within the polymer matrix [68].
Table 1: Comparison of Extrinsic Self-Healing Mechanisms
| Feature | Microcapsule-Based | Vascular Network |
|---|---|---|
| Healing Cycles | Single use per location | Multiple cycles possible |
| Healing Agent Volume | Limited by capsule size/density | Larger reservoir capacity |
| Manufacturing Complexity | Moderate (capsule synthesis + integration) | High (channel formation + sealing) |
| Impact on Mechanical Properties | Potential stress concentrators | May affect structural integrity |
| Bioelectronic Suitability | Thin films, coatings | Larger implants, structural components |
Intrinsic Self-Healing Systems
Intrinsic systems utilize reversible chemical bonds within the polymer matrix that can spontaneously reform after damage:
- Dynamic Covalent Bonds: Include Diels-Alder cycloadditions, disulfide exchanges, imine formations, and boronate ester complexes. These bonds undergo reversible cleavage and reformation under specific stimuli (heat, light, pH changes) [68].
- Supramolecular Interactions: Non-covalent interactions such as hydrogen bonding, metal-ligand coordination, π-π stacking, and host-guest interactions. These systems typically exhibit faster healing kinetics at moderate temperatures but generally provide lower mechanical strength than covalent networks [69].
The healing process in intrinsic systems relies on molecular diffusion across damaged interfaces, followed by bond reformation. This mechanism is particularly suitable for bioelectronic applications where repeated damage-repair cycles are anticipated, and external healing agents are undesirable.
Figure 1: Classification of Self-Healing Mechanisms in Bioelectronic Materials
Material Systems and Their Properties for Bioelectronics
Self-Healing Polymers and Elastomers
Polymer-based systems dominate bioelectronic applications due to their tunable mechanical properties and compatibility with biological tissues:
- Conductive Self-Healing Elastomers: Incorporate conductive fillers (carbon nanotubes, graphene, metal nanoparticles) within self-healing polymer matrices. These materials maintain electrical conductivity while achieving autonomous healing through dynamic covalent bonds or supramolecular interactions [69]. Successful systems have demonstrated both high conductivity (>1 S/cm) and healing efficiencies (>90%) after complete fracture.
- Self-Healing Hydrogels: Water-swollen polymer networks with reversible crosslinks ideal for tissue-interfacing applications. These materials naturally exhibit tissue-like compliance (Young's modulus: 0.1-100 kPa) and can be engineered with ionic or electronic conductivity. Multistrength hydrogen bonding systems have achieved exceptional mechanical properties including notch-insensitive high stretchability, high toughness, and autonomous self-healing even in artificial sweat [69].
Advanced Composites and Ceramics
- Fiber-Reinforced Composites: Incorporate hollow glass fibers or vascular networks containing healing agents. These systems are particularly valuable for structural components of bioelectronic devices where mechanical integrity is paramount.
- Self-Healing Ceramics: While less common in bioelectronics, these materials offer exceptional scratch resistance and durability for protective coatings on implantable devices.
Table 2: Self-Healing Material Properties Relevant to Bioelectronics
| Material Class | Typical Young's Modulus | Healing Mechanism | Healing Efficiency | Conductivity | Bioelectronic Applications |
|---|---|---|---|---|---|
| Supramolecular Elastomers | 0.1-10 MPa | Hydrogen bonding, Metal-ligand | 80-99% | 10⁻⁶-10 S/cm | Stretchable sensors, Electronic skin |
| Dynamic Covalent Polymers | 1 MPa-1 GPa | Diels-Alder, Disulfide | 70-95% | 10⁻⁸-10⁻² S/cm | Implantable electrode coatings |
| Self-Healing Hydrogels | 0.1-100 kPa | Ionic, Host-guest | 85-98% | 0.1-10 S/cm (ionic) | Tissue interfaces, Drug delivery |
| Conductive Composites | 10 MPa-5 GPa | Microcapsule, Vascular | 60-90% | 10²-10⁵ S/cm | Interconnects, Circuit repair |
Experimental Characterization and Methodologies
Mechanical Property Assessment
Standardized methodologies for evaluating self-healing performance in bioelectronic materials:
- Fracture-Healing Tests: Utilize notched specimens in tensile, tear, or bending configurations to quantify healing efficiency. Pre-cracked samples are subjected to controlled damage, allowed to heal under specified conditions, then mechanically tested to measure property recovery [70].
- Healing Efficiency Calculation: η = (Xhealed / Xvirgin) × 100%, where X represents mechanical properties such as fracture toughness, tensile strength, or elongation at break.
- Cyclic Damage-Healing Tests: Assess the material's ability to undergo multiple healing cycles at the same location, critical for applications requiring long-term durability.
For bioelectronic materials, these mechanical tests are coupled with electrical characterization to ensure functional recovery of both structural and conductive properties.
Electrical Performance Monitoring
- Resistance Recovery Measurements: Track changes in electrical resistance during damage and healing cycles. Full functional recovery typically requires restoration of both mechanical integrity and electrical conductivity.
- Impedance Spectroscopy: Particularly important for bioelectronic interfaces, where the electrode-tissue impedance directly impacts signal quality and stimulation efficiency.
Figure 2: Experimental Workflow for Characterizing Self-Healing Materials
Research Reagent Solutions for Self-Healing Bioelectronics
Table 3: Essential Research Reagents for Self-Healing Bioelectronic Materials
| Reagent/Material | Function | Application Examples | Key Considerations |
|---|---|---|---|
| Dicyclopentadiene (DCPD) | Monomer for ring-opening metathesis polymerization | Microcapsule-based self-healing systems | Requires Grubbs' catalyst for polymerization [71] |
| Grubbs' Catalyst | Ruthenium-based catalyst for ROMP | Polymerization of DCPD in microcapsule systems | Sensitivity to air and moisture [71] |
| Dynamic Covalent Monomers | Furan, maleimide, disulfide compounds | Intrinsic self-healing polymers | Specific stimulus requirements (heat, light, pH) [68] |
| Conductive Fillers | Carbon nanotubes, graphene, metal nanoparticles | Electrically conductive self-healing composites | Concentration-dependent percolation threshold [69] |
| Supramolecular Crosslinkers | Ureidopyrimidinone, terpyridine ligands | Reversible polymer networks | Bond strength and kinetics of reformation [69] |
| Hydrogel Precursors | Polyvinyl alcohol, alginate, hyaluronic acid | Tissue-like conductive hydrogels | Biocompatibility, swelling behavior [69] |
Implementation in Bioelectronic Devices
Current Applications and Performance
Self-healing materials are being integrated across diverse bioelectronic platforms:
- Wearable Health Monitoring: Self-healing elastomers in stretchable sensors maintain signal integrity during repeated deformation. These systems can autonomously repair cuts or scratches that would otherwise compromise device function [72]. Recent advances include materials that self-heal even in wet environments, crucial for wearable perspiration management.
- Implantable Bioelectronics: Neural interfaces and cardiac patches benefit from self-healing properties that maintain electrode functionality under mechanical stress. Materials with tissue-matched modulus minimize inflammatory responses while providing reliable long-term operation [69].
- Electronic Skin and Soft Robotics: Multifunctional self-healing systems integrate sensing, actuation, and communication capabilities. These platforms can recover from damage similar to biological skin, significantly extending operational lifetime in prosthetics and human-machine interfaces [69].
Manufacturing and Integration Considerations
- Microfabrication Compatibility: Self-healing materials must withstand processing conditions (lithography, etching, deposition) without compromising healing functionality.
- Encapsulation Strategies: Bioelectronic devices require protection from biological environments while maintaining self-healing capabilities at critical interfaces.
- Scalability and Reproducibility: Transition from laboratory demonstrations to clinically viable devices necessitates consistent material properties and reliable performance across manufacturing batches.
Future Perspectives and Research Directions
The field of self-healing materials for bioelectronics continues to evolve with several emerging frontiers:
- Multifunctional Systems: Next-generation materials that simultaneously self-heal mechanical damage, restore electrical conductivity, and maintain other functionalities (optical transparency, permeability, biodegradability).
- Stimuli-Responsive Healing: Development of materials that activate healing processes in response to specific biological cues or environmental changes relevant to clinical applications.
- AI-Enhanced Materials Systems: Integration of sensing, healing, and machine learning to create "smart-healing" systems that predict failure points and initiate preventive repairs [69].
- Advanced Manufacturing: Utilization of 3D/4D printing and other additive manufacturing techniques to create complex vascular networks for healing agent distribution in bioelectronic devices.
The ongoing convergence of materials science with bioelectronics will continue to yield increasingly sophisticated self-healing systems, ultimately enabling biointegrated devices with unprecedented durability, reliability, and functional longevity.
Ensuring Conformal Contact and Strong Bioadhesion on Dynamic Tissue Surfaces
The advancement of bioelectronic interfaces for diagnostics, monitoring, and therapy hinges on the creation of devices that can form stable, intimate, and functional interfaces with biological tissues. Achieving such stable integration is profoundly challenging due to the inherent properties of living tissues: they are soft, wet, dynamically moving, and topologically complex. Traditional rigid electronic devices, with Young's moduli many orders of magnitude higher than biological tissues, create a significant mechanical mismatch. This mismatch leads to tissue damage, inflammatory responses, unstable signal acquisition, and ultimately, device failure [73] [10].
This technical guide delves into the core principles and methodologies for ensuring conformal contact and robust bioadhesion on dynamic tissue surfaces. Framed within the critical context of Young's modulus matching, we explore the material strategies, theoretical models, and experimental protocols that enable the development of next-generation bioelectronics capable of seamless integration with the biological world. The goal is to move from bulky, rigid implants to tissue-like, mechanically adaptive systems that can withstand the demanding environment of the human body [73] [74].
Core Principles: Mechanical Matching and Conformal Contact
The Critical Role of Young's Modulus
The Young's modulus (E), a measure of a material's stiffness, is a foundational parameter in biointerface design. A significant mechanical mismatch between a device and tissue induces strain at the interface, provoking a foreign body response that leads to fibrotic encapsulation, reduced signal-to-noise ratio, and device drift.
Table 1: Young's Modulus of Biological Tissues and Common Electronics Materials
| Material or Tissue Type | Young's Modulus | Characteristics and Relevance |
|---|---|---|
| Neural Tissues | 100 Pa - 10 kPa [73] | Extremely soft and delicate; highly susceptible to damage from rigid devices. |
| Skin | Varies with layer and location [10] | A dynamic, curvilinear surface that requires stretchable and flexible interfaces. |
| Conventional Metals (e.g., Au, Pt) | GPa range (e.g., ~79 GPa for Au) [73] | Several orders of magnitude stiffer than tissues; cause significant mechanical mismatch. |
| Silicon | ~130-180 GPa [73] | High stiffness and brittleness make it unsuitable for direct tissue interfacing without design strategies. |
| Polydimethylsiloxane (PDMS) | ~360 kPa - ~2 MPa [73] | A soft elastomer, but can still be 10-1000x stiffer than very soft tissues like brain. |
| Hydrogels (e.g., Alginate) | 10 Pa - 100 kPa [73] | Can be engineered to match the modulus of a wide range of tissues, ideal for mechanical matching. |
Theoretical Models of Conformability
Achieving conformal contact is a complex process governed by the interplay of bending stiffness, interfacial adhesion, and the geometry of both the device and the target tissue. Theoretical models provide a framework for designing devices that can overcome geometric mismatches.
- Conformability on Rough Surfaces: The skin and organ surfaces are not smooth but feature micro-roughness. A model treating the skin as a sinusoidal profile ((y=(1+cos(2\pi x/\lambda))h/2)) defines the total energy of a conformal system as ( {\bar{U}}{\text{conformal}}={\bar{U}}{\text{bending}}+{\bar{U}}{\text{skin}}+{\bar{U}}{\text{adhesion}} ). For conformal contact to occur (( {\bar{U}}_{\text{conformal}} < 0 )), the device must have low bending stiffness (low Young's modulus and small thickness) and high interfacial adhesion energy [3].
- Global Conformability on Non-Developable Surfaces: Biological surfaces often have non-zero Gaussian curvature (e.g., spheres, saddles). A model for mounting a circular thin film on a rigid sphere shows that full conformability is favored by a small device-to-surface size ratio, minimal thickness, and a soft material with a low Young's modulus [3]. The strain developed during this process can be calculated, informing the required stretchability of the device materials [3].
Material Strategies for Conformal and Adhesive Bioelectronics
Soft and Conductive Materials
The core challenge is to create materials that are both mechanically tissue-like and electronically functional.
- Conductive Hydrogels: Hydrogels are prime candidates due to their high water content, biocompatibility, and tunable mechanical properties that can closely match those of tissues [73]. To overcome their typically poor conductivity, they can be enhanced with conductive polymers (e.g., PEDOT:PSS) or nanomaterial fillers (e.g., graphene flakes, carbon nanotubes) [73]. For example, an ionically conductive alginate hydrogel matrix blended with graphene and carbon nanotubes was used to create a viscoelastic electrode that conformed to the cortical surface of a rat brain and nerves in a bovine heart without causing damage [73].
- Ultrathin Geometries: Reducing the feature size of rigid inorganic materials is another powerful strategy. An ultrathin silicon membrane (~2 μm) supported by a PDMS substrate was demonstrated to wrap around a sciatic nerve seamlessly, enabling light-induced stimulation [73]. Similarly, creating ultrathin (<5 μm) and flexible devices on substrates like parylene-C minimizes bending stiffness, allowing for van der Waals-force-driven conformal contact with tissues like skin without the need for sutures or strong adhesives [10].
Structurally Adaptive and Self-Adhesive Systems
Beyond intrinsic softness, advanced material architectures can provide active conformability and robust adhesion.
- Supercontractile Polymers: A recent innovation involves mechanically adaptive supercontractile polymer films that yield large and rapid contractions. This allows a device to actively shrink-wrap around soft, wet, and irregular tissues, providing a standardized interface without traditional suturing [74].
- Dual-Layer Adhesive Patches: A sophisticated approach involves patches with distinct functional layers. A prime example is a silk fibroin (SF)-based patch featuring a thin bioadhesive layer for interfacial bonding and a highly tough hydrogel matrix layer for mechanical cohesion [75]. The bioadhesive layer, often incorporating catechol groups from compounds like tannic acid (TA), mimics marine mussel adhesion, providing robust, water-resistant bonding to various soft tissues. The tough hydrogel matrix, often based on interpenetrating polymer networks (e.g., methacrylate-modified SF/acrylamide covalently cross-linked with an ionically cross-linked alginate network), dissipates energy under deformation, preventing mechanical failure [75].
Experimental Protocols and Methodologies
Fabrication of a Dual-Layer Silk Fibroin Adhesive Patch
This protocol outlines the creation of a highly tough and conformal SF-based adhesive patch for sutureless sealing and repair, as demonstrated in recent research [75].
1. Synthesis of Methacrylate-Modified Silk Fibroin (SFGMA):
- Purpose: To create a photocross-linkable SF derivative for forming a covalently cross-linked hydrogel network.
- Procedure: Dissolve degummed SF fibers in a 9.3 M LiBr solution. Dialyze against deionized water for 3 days. Modify the SF solution by reacting with glycidyl methacrylate (GMA) at 60°C for 4-6 hours. Finally, dialyze the product against water to remove unreacted GMA and lyophilize to obtain SFGMA.
2. Fabrication of the Tough Hydrogel Matrix Layer:
- Purpose: To create the primary structural layer with high toughness to withstand dynamic tissue movements.
- Procedure: Prepare a precursor solution by dissolving SFGMA and acrylamide (AM) in deionized water. Add a photoinitiator (e.g., Irgacure 2959) and sodium alginate to the solution. Pour the solution into a mold and expose to UV light (e.g., 365 nm wavelength) to initiate free-radical polymerization, creating a covalently cross-linked poly(SFGMA-AM) network. Subsequently, immerse the hydrogel in a calcium chloride solution to ionically cross-link the alginate, forming a dual-crosslinked interpenetrating network.
3. Application of the Bioadhesive Layer:
- Purpose: To provide strong, mussel-inspired adhesion to wet tissue surfaces.
- Procedure: Prepare a bioadhesive precursor from a mixture of SF, TA, and polyethylene glycol (PEG). Coat this precursor solution onto the porous surface of the pre-formed tough hydrogel matrix layer. Allow it to cure and air-dry to form a tightly integrated, dual-layer SF patch.
4. Ex Vivo and In Vivo Adhesion Testing:
- Purpose: To quantitatively evaluate the performance of the adhesive patch.
- Procedure:
- Lap-Shear Test: Use porcine skin or other soft tissues. Apply the SF patch to an overlapping area of two tissue sections. Mount the assembly on a mechanical tester and measure the shear strength required for detachment at a constant pull rate.
- Burst Pressure Test: For sealing applications, create a defect in an ex vivo porcine stomach or intestine. Seal the defect with the SF patch. Connect the organ to a pressure-controlled fluid line and gradually increase the pressure until leakage occurs, recording the burst pressure.
- In Vivo Therapeutic Efficacy: In a rat model of gastric perforation or sciatic nerve injury, apply the SF patch for sutureless repair. Monitor over time for post-operative leakage, infection, functional recovery (e.g., limb movement for nerve repair), and finally, conduct histological analysis to assess tissue integration and inflammatory response.
Conformability Analysis for Ultrathin Bioelectronics
This methodology describes how to model and validate the conformal attachment of a thin-film device to a target biosurface [3].
1. Device Fabrication via Ultraviolet Lithography:
- Purpose: To create an ultrathin, flexible electronic device.
- Procedure: Spin-coat a sacrificial layer (e.g., polyacrylic acid) onto a silicon wafer. Then, spin-coat a polyimide (PI) precursor as the substrate. Pattern metal (e.g., Cr/Au) interconnects and electrodes via photolithography, evaporation, and lift-off. Subsequently, spin-coat another layer of PI to encapsulate the metal, creating a polyimide/metal/polyimide sandwich structure. Finally, release the device from the handle wafer by dissolving the sacrificial layer.
2. Theoretical Conformability Assessment:
- Purpose: To predict if the device will achieve conformal contact on a specific tissue surface.
- Procedure: For a target spherical surface (e.g., the eye or a specific organ), use the model for a circular thin film on a rigid sphere [3]. Input parameters including the device's radius ((Rf)), thickness ((h)), Young's modulus ((E)), Poisson's ratio ((\nu)), and the interfacial adhesion energy ((\gamma)). Calculate the stable criterion for full conformability: ( \frac{{R}{\text{f}}^{4}}{128{R}{\text{s}}^{4}}+\frac{{h}^{2}}{12\left(1-\nu \right){R}{\text{s}}^{2}}\le \frac{\lambda }{{Eh}} ). A positive result indicates the device design is suitable.
3. Experimental Validation:
- Purpose: To visually and functionally confirm conformal contact.
- Procedure: Mount the released thin-film device onto the target tissue surface (e.g., the skin or brain cortex of an animal model). Use optical coherence tomography (OCT) or scanning electron microscopy (SEM) of the cross-section to visualize the interface and check for gaps. Electrically, measure the contact impedance or the quality of electrophysiological signals (e.g., EEG, ECG) over time; a stable, low impedance and high-fidelity signal are indicators of good, stable conformal contact.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Bioadhesion and Conformal Contact Research
| Item | Function and Application |
|---|---|
| Silk Fibroin (SF) | A natural biomacromolecule serving as a tough, biocompatible, and biodegradable base material for hydrogels and adhesive layers [75]. |
| Tannic Acid (TA) | A polyphenolic compound that provides catechol groups for mussel-inspired, robust underwater adhesion on tissue surfaces [75]. |
| Glycidyl Methacrylate (GMA) | A modifying agent used to introduce photocross-linkable methacrylate groups onto polymers like SF, enabling UV-cured hydrogel formation [75]. |
| Poly(ethylene glycol) (PEG) | A hydrophilic polymer used to modify mechanical properties and improve biocompatibility in hydrogel matrices [75]. |
| Sodium Alginate | A natural polymer that forms ionically cross-linked networks with divalent cations (e.g., Ca²⁺), used to toughen hydrogels [75]. |
| PEDOT:PSS | A conductive polymer hydrogel used to create soft, flexible electrodes for recording and stimulation of electrophysiological signals [73] [10]. |
| Carbon Nanotubes (CNTs) / Graphene | Conductive nanomaterial fillers blended into hydrogel matrices to enhance electronic conductivity while maintaining softness [73] [10]. |
| Parylene-C | A biocompatible polymer used as an ultrathin, flexible substrate and encapsulation layer for implantable bioelectronic devices [10]. |
Visualizing Strategies and Workflows
Strategy Integration for Stable Biointerfaces
Dual-Layer Adhesive Patch Fabrication
The path to reliable bioelectronic integration is paved with the principles of mechanical compatibility and robust interfacial adhesion. Success requires a multi-faceted approach: engineering materials and devices with a Young's modulus that mirrors the target tissue, leveraging geometric designs that minimize bending stiffness, and employing novel chemical strategies for strong, water-resistant bonding. The emergence of advanced material systems—such as dual-layer adhesive patches that decouple the demands of mechanical toughness and surface adhesion, and supercontractile polymers that actively achieve conformal contact—signifies a major leap forward. As these technologies mature, they will unlock new possibilities in chronic implants, high-fidelity biosensing, and precise therapeutic modulation, ultimately enabling a future where electronics seamlessly integrate with the human body.
Benchmarking Performance: In Vitro, In Vivo, and Comparative Material Analysis
Standardized Testing Protocols for Mechanical and Electrical Characterization
In the field of bioelectronic materials research, the integration of electronic components with biological systems necessitates a deep understanding of their mechanical and electrical properties. The mechanical compliance of these materials, often quantified by Young's Modulus, is critical for ensuring seamless integration with soft, dynamic biological tissues without causing inflammation or device failure [4]. Simultaneously, rigorous electrical characterization ensures device safety and reliability in humid, saline biological environments [76] [77]. This guide details the standardized testing protocols essential for the comprehensive characterization of bioelectronic materials, providing researchers and product development professionals with a structured framework for evaluation.
Mechanical Characterization of Bioelectronic Materials
Mechanical testing determines how materials behave under various forces, providing key insights into properties like strength, hardness, and elasticity. For bioelectronics, whose successful operation hinges on mechanical compatibility with soft tissues, these tests are indispensable [78] [79].
Fundamental Mechanical Tests and Standards
The following tests are fundamental to evaluating the properties of materials used in bioelectronic devices.
Table 1: Core Mechanical Testing Methods for Material Properties
| Test Method | Key Properties Measured | Applicable Standards | Relevance to Bioelectronics |
|---|---|---|---|
| Tensile Testing | Ultimate tensile strength, Yield strength, Young's Modulus (Elastic Modulus), Ductility (Elongation to failure) [78] [79] | ASTM E8 (Metals), ASTM D638 (Plastics) [80] | Determines baseline mechanical behavior under tension; critical for ensuring materials can withstand stretching forces without failure [78]. |
| Hardness Testing | Material resistance to localized plastic deformation (e.g., indentation) [78] | ASTM E18 (Rockwell for Metals), ASTM D2240 (Durometer for Rubbers) [80] | A fast, inexpensive method to check material consistency and effects of heat treatment [79]. |
| Impact Testing | Toughness (Energy absorbed during fracture) [78] [79] | ASTM E23 (Notched Bar Impact) [80] | Evaluates behavior under sudden shock loads, important for wearable devices that may be dropped [78]. |
| Fatigue Testing | Fatigue strength, Fatigue life (S-N curve) [78] [79] | ASTM E139 | Assesses durability under repeated loading/unloading cycles, simulating bodily movements like heartbeats or walking [78]. |
| Creep Testing | Creep strain, Creep rupture strength [78] [79] | ASTM D2990 (Plastics) [80] | Determines long-term deformation under constant load, crucial for chronically implanted devices under constant stress [78]. |
Experimental Protocol: Tensile Testing for Young's Modulus
1. Objective: To determine the stress-strain relationship of a material and calculate its Young's Modulus (Elastic Modulus). 2. Scope: Applicable to metallic wires, polymer films, and thin substrates used in bioelectronics. 3. Apparatus: Universal testing machine, extensometer or strain gauge, specimen grips. 4. Specimen Preparation:
- Prepare specimens according to the relevant standard (e.g., ASTM E8 or D638) with a defined gauge length and cross-section [80].
- Ensure specimens are free of surface imperfections. 5. Procedure: a. Measure the cross-sectional dimensions of the specimen's gauge length. b. Mount the specimen securely in the testing machine, ensuring it is aligned axially to avoid bending. c. Attach the extensometer to the gauge length for accurate strain measurement. d. Apply a tensile load to the specimen at a constant, controlled strain rate as specified by the standard. e. Continuously record the applied load (force) and the corresponding elongation (strain) until the specimen fractures. f. Remove the extensometer before fracture to prevent damage. 6. Data Analysis:
- Calculate Engineering Stress: ( \sigma = F / A0 ), where ( F ) is the force and ( A0 ) is the original cross-sectional area.
- Calculate Engineering Strain: ( \epsilon = \Delta L / L0 ), where ( \Delta L ) is the elongation and ( L0 ) is the original gauge length.
- Plot the stress-strain curve. Young's Modulus (E) is the slope of the initial linear-elastic portion of the curve: ( E = \Delta \sigma / \Delta \epsilon ) [78] [79].
Electrical Characterization and Safety Protocols
Electrical safety testing is paramount for any device interfacing with the human body. These tests verify that devices remain safe under both normal and single-fault conditions, preventing electric shock to patients or users [76] [77].
Key Electrical Safety Tests
International standards, such as IEC 60601-1 for medical electrical equipment, define a series of tests to ensure basic safety. The newer IEC 62353 standard is often used for recurrent testing in field environments like hospitals [77].
Table 2: Essential Electrical Safety Tests and Limits
| Test | Purpose | Test Conditions | Standard & Typical Limits |
|---|---|---|---|
| Protective Earth Resistance | To verify the integrity and low resistance of the earth conductor in Class I equipment [76]. | 10A-25A AC for 5 sec (type test) or 1A or less (field test) [76]. | IEC 60601-1 / IEC 62353: Resistance ≤ 0.2 Ω [76]. |
| Insulation Resistance | To measure the effectiveness of insulation between live parts and accessible parts [76]. | 500V DC applied between live/neutral (linked) and earth (Class I) [76]. | HEI 95 / DB9801: Resistance ≥ 50 MΩ (Can be as low as 1MΩ for certain heaters) [76]. |
| Earth Leakage Current | To measure the current flowing from the mains parts through insulation to the protective earth conductor [76]. | Normal Condition (NC) and Single Fault Condition (SFC - e.g., neutral open) [76]. | IEC 60601-1 (2005): NC: 5 mA; SFC: 10 mA [76]. |
| Touch/Enclosure Leakage Current | To measure the current that could flow through a person touching the equipment enclosure [76]. | NC and SFC (e.g., protective earth open) [76]. | IEC 60601-1: NC: 0.1 mA; SFC: 0.5 mA [76]. |
| Patient Leakage Current | To measure the current that could flow through a patient connected to an applied part (e.g., a lead or electrode) [76]. | Measured from applied parts to earth. Stricter limits for cardiac applications (Type CF) [76]. | IEC 60601-1: Varies by applied part type (B, BF, CF); most stringent for CF [76]. |
Experimental Protocol: Leakage Current Measurements
1. Objective: To verify that leakage currents from the equipment enclosure and patient-applied parts remain within safe limits under normal and single-fault conditions. 2. Scope: Applicable to all Class I and Class II bioelectronic equipment with accessible conductive surfaces or patient connections. 3. Apparatus: Electrical Safety Analyzer (ESA) compliant with IEC 61010-1, capable of simulating Normal and Single Fault Conditions [77]. 4. Setup:
- Ensure the Equipment Under Test (EUT) is switched on.
- Connect the ESA to the mains supply and the EUT as per the manufacturer's instructions. For patient leakage tests, connect to the applied parts [76].
- Place the EUT on an insulating surface. 5. Procedure for Earth Leakage Current: a. Set the ESA to measure Earth Leakage Current. b. Perform the measurement in Normal Condition (NC) with mains polarity normal and reversed. Record the highest reading. c. Introduce a Single Fault Condition (SFC), typically an open neutral conductor. Repeat the measurement. d. Compare the results against the limits specified in the relevant standard (e.g., 5mA for NC in IEC 60601-1:2005) [76]. 6. Procedure for Touch/Enclosure Leakage Current: a. Set the ESA to measure Touch/Enclosure Leakage Current. b. For Class I equipment, perform the measurement under the SFC of an open protective earth conductor. For Class II equipment, measure in NC [76]. c. Use a test probe to contact all accessible conductive parts (e.g., fascia, handles) with mains polarity normal and reversed to find the "worst-case" reading [76]. d. Ensure the reading does not exceed 0.1mA (NC) or 0.5mA (SFC) [76].
The Scientist's Toolkit: Research Reagent Solutions
Successful characterization relies on specialized materials and equipment. The following table details essential items for the standardized testing of bioelectronic materials.
Table 3: Essential Research Tools for Bioelectronic Material Characterization
| Item / Solution | Function | Application Example |
|---|---|---|
| Universal Testing Machine | Applies controlled tensile, compressive, or flexural loads to a specimen while measuring its response. | Performing tensile tests to determine the Young's Modulus of a conductive polymer film [78] [79]. |
| Electrical Safety Analyzer (ESA) | A specialized instrument that performs electrical safety tests by generating precise voltages and measuring leakage currents and resistances [77]. | Conducting protective earth resistance and patient leakage current tests on a prototype wearable ECG monitor [76] [77]. |
| Leakage Current Measuring Device (MD) | A standardized circuit defined by IEC 60601-1 to accurately simulate the impedance of the human body for leakage current measurements [76]. | Used internally by an ESA or built as a standalone unit for validating patient leakage currents according to the standard. |
| Hardness Tester (e.g., Vickers, Rockwell) | Indents a material with a specific shape and load to quantify its resistance to permanent surface deformation. | Quality control check on the hardness of a polymer substrate before and after a sterilization process [78] [80]. |
| Conductive Hydrogels | Soft, ionic conductors that interface between rigid electronics and biological tissue, improving signal quality and comfort. | Used as a biocompatible electrode interface on epidermal electronic patches for recording electrophysiological signals [10]. |
The pathway to reliable and safe bioelectronic devices is built upon a foundation of rigorous and standardized mechanical and electrical characterization. Accurately determining the Young's Modulus and other mechanical properties ensures devices are soft, flexible, and compatible with biological tissues, thereby mitigating immune responses and enhancing long-term performance [4]. Concurrently, adherence to international electrical safety standards like IEC 60601-1 and IEC 62353 is non-negotiable for preventing patient harm and ensuring device reliability in clinical environments [76] [77]. As the field advances towards increasingly sophisticated closed-loop systems for personalized diagnostics and therapeutics, the consistent application of these detailed testing protocols will remain a critical enabler of innovation and clinical translation.
In the field of bioelectronic materials research, the parameter of Young's modulus—a fundamental measure of a material's stiffness—is a critical determinant of device performance. While in vitro characterization provides initial data, in vivo validation remains an indispensable step for translating laboratory innovations into clinical applications. This process evaluates how bioelectronic interfaces, designed with tissue-like mechanical properties, interact with the complex biological environment of a living system. The primary challenge stems from the significant mechanical mismatch between conventional electronic materials and biological tissues; metals and inorganic semiconductors used in electrodes have Young's moduli many orders of magnitude greater than the ~100 Pa to 10 kPa typical of neural tissues [73]. This mismatch can provoke chronic inflammatory responses, fibrosis, and device failure, ultimately compromising the functional efficacy of the implant [81] [73].
Consequently, in vivo studies are mandated by regulatory bodies to assess biocompatibility and functional efficacy before human trials. The goal of modern research is to develop "tissue-like" bioelectronics that minimize these mismatches, creating devices that are both mechanically and biologically compatible with their target organs [73]. This guide details the protocols, metrics, and regulatory considerations for conducting robust in vivo validation of bioelectronic materials, with a specific focus on how a material's Young's modulus influences its integration and performance within a living organism.
Core Principles: Biocompatibility, Efficacy, and Mechanical Matching
Defining Biocompatibility and Functional Efficacy
For a bioelectronic device to be deemed successful, it must demonstrate both biocompatibility and functional efficacy throughout its intended operational lifespan.
Biocompatibility: According to the internationally accepted definition, biocompatibility is "the ability of a material to perform with an appropriate host response in a specific situation" [81]. This extends beyond mere inertness; the device must not provoke adverse immune responses, cause systemic toxicity, or induce complications such as restenosis in cardiovascular applications [81]. Evaluation encompasses a range of responses, including cytotoxicity, sensitization, and irritation, often referred to as the "Big Three" in biocompatibility testing [82].
Functional Efficacy: This measures the device's ability to perform its intended function reliably within the biological environment. For a bioelectronic implant, this could involve stable recording of electrophysiological signals (e.g., neural spikes, ECG) or consistent delivery of therapeutic stimulation over the chronic implantation period [10] [73]. Efficacy is directly threatened by the body's response to mechanical mismatch, which can lead to signal degradation due to scarring or device displacement [73].
The Critical Role of Young's Modulus
Young's modulus is a key property in predicting the host response and long-term stability of a bioelectronic device. The following table summarizes the stiffness of common bioelectronic materials compared to biological tissues.
Table 1: Young's Modulus of Bioelectronic Materials and Biological Tissues
| Material or Tissue | Young's Modulus | Contextual Notes |
|---|---|---|
| Neural Tissues | 100 Pa – 10 kPa | Highly soft and viscoelastic [73] |
| Cardiac Muscle | ~10 kPa (Lamb cortex, rat heart) | Similar viscoelastic property to neural tissues [73] |
| Alginate Hydrogel | 10 Pa – 100 kPa | Tunable to match tissue mechanics [73] |
| Parylene-C Substrate | ~3 GPa | Considered "flexible" in electronics but much stiffer than tissue [10] |
| Gold (Au) Films | Varies with thickness | Nanoscale modulus characterized by AFM; thinner films are more flexible but less conductive [21] |
| Gallium | 79.37 - 83.84 GPa | Low-melting-point metal, modulus decreases with temperature [12] |
| Conventional Metals (Au, Pt) | 10s to 100s of GPa | Inherently rigid, causing significant mechanical mismatch [73] |
Strategies to overcome this mechanical mismatch focus on creating devices with low bending stiffness, which is a function of both the material's intrinsic Young's modulus and the device's geometry. Key approaches include:
- Using Hydrogels and Soft Polymers: Materials like alginate hydrogels, with moduli comparable to tissue, can be enhanced with conductive polymers or nanomaterial fillers to achieve both compliance and conductivity [73].
- Ultra-thin Geometries: Reducing the critical dimensions of rigid inorganic materials (e.g., creating ~2 μm thick silicon membranes) dramatically improves their flexibility and conformability [73].
- Stretchable Composites: Incorporating metals into stretchable architectures, such as porous silicone or elastic microstructured interconnects, allows them to withstand deformation without failure [73].
Regulatory Framework and the "Big Three" Biocompatibility Tests
Regulatory approval for medical devices, including bioelectronic implants, requires rigorous biocompatibility testing following internationally recognized standards. The ISO 10993 series is the cornerstone of this framework, providing guidance on the biological evaluation of medical devices [82] [81]. A core principle in modern regulation is the 3R+DQ principle (Replacement, Reduction, Refinement, plus Design and Quality), which emphasizes the ethical and scientific justification for animal studies [83]. Animal testing is only warranted when non-animal alternatives cannot provide the necessary safety data [82].
The "Big Three" biocompatibility assessments—cytotoxicity, sensitization, and irritation—are required for almost all medical devices [82]. The following workflow outlines the decision-making process for in vivo validation within this regulatory context.
Decision Flow for In Vivo Validation
Detailed Experimental Protocols for the "Big Three"
1. Cytotoxicity Testing (ISO 10993-5)
- Objective: To determine if the device or its leachables cause harmful effects to living cells.
- Method: Extracts of the device material are prepared using appropriate solvents (e.g., culture medium with serum, saline, or vegetable oil) as per ISO 10993-12 [82]. Cultured mammalian cells (e.g., L929 fibroblasts) are exposed to these extracts for approximately 24 hours [82].
- Endpoint Analysis:
2. Sensitization Assessment
- Objective: To evaluate the potential for the device to cause an allergic contact dermatitis response.
- In Vivo Method (e.g., Guinea Pig Maximization Test, Murine Local Lymph Node Assay): The material extract is repeatedly exposed to the skin of the animal. The response is graded based on the presence of redness, swelling, or other signs of an allergic reaction upon re-challenge.
3. Irritation Testing
- Objective: To determine if the device causes localized, reversible inflammatory responses at the site of contact.
- In Vivo Method (e.g., Intracutaneous Reactivity Test): The extract of the device is injected intracutaneously into rabbits. The injection sites are scored against a control for signs of erythema (redness) and oedema (swelling) at 24, 48, and 72 hours post-injection.
Advanced In Vivo Models for Functional Efficacy Assessment
Beyond the "Big Three," assessing how a device performs its intended function in a living system is crucial. This requires sophisticated animal models tailored to the device's application.
Cardiovascular Stent Models
Bioresorbable metallic stents (BRS) represent a major advancement in cardiovascular bioelectronics. Their functional efficacy depends on mechanical support, degradation rate, and biocompatibility [81]. Animal models, typically porcine or murine, are used to evaluate these parameters.
Table 2: Key Metrics for In Vivo Evaluation of Bioresorbable Stents
| Evaluation Category | Key Quantitative Metrics | Measurement Techniques |
|---|---|---|
| Biocompatibility & Host Response | - Thickness of neointimal hyperplasia- Degree of inflammation score- Presence of fibrin deposition | - Histopathology (H&E staining)- Immunohistochemistry |
| Functional Efficacy | - Patency rate (blood flow)- Percentage of in-stent restenosis- Occurrence of thrombosis | - Angiography- Ultrasound imaging (IVUS) |
| Degradation & Mechanical Integrity | - Degradation rate (mm/year)- Residual tensile strength (MPa)- Elastic recoil | - Micro-CT scanning- Explant mechanical testing |
| Systemic Toxicity | - Ion concentration in blood (e.g., Mg²⁺, Zn²⁺)- Organ pathology (e.g., liver, kidney) | - ICP-MS (Inductively Coupled Plasma Mass Spectrometry)- Histological analysis |
Neural Interface Models
For neural bioelectronics, functional efficacy is measured by the quality of signal recording and the precision of stimulation. The following diagram illustrates the integrated workflow for validating a neural implant, from material properties to in vivo outcomes.
Neural Implant Validation Logic
Functional Readouts in Rodent Models:
- Motor Control: A "tissue-like" electrode applied to the brainstem of mice can deliver localized electrical stimulation to precisely control tongue, whisker, and neck muscle movements, demonstrating high-resolution functional efficacy [73].
- Sensory Restoration: In auditory brainstem implants, soft and conformable devices with elastic microstructured interconnects show strong responses in electrically evoked auditory brainstem responses (eABRs), confirming functional restoration [73].
- Chronic Signal Stability: The consistent recording of neural spike amplitudes over weeks or months, without degradation due to inflammation or encapsulation, is a key metric of success for recording electrodes [73].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for In Vivo Validation
| Reagent / Material | Function in Validation | Specific Examples & Notes |
|---|---|---|
| L929 Fibroblast Cells | In vitro cytotoxicity testing per ISO 10993-5 [82]. | Standardized cell line for initial biocompatibility screening. |
| Extraction Solvents | Preparation of device extracts for in vitro and in vivo tests [82]. | Physiological saline, vegetable oil, culture medium. Conditions specified in ISO 10993-12. |
| MTT/XTT Assay Kits | Quantitative measurement of cell viability and metabolic activity [82]. | Colorimetric assays; results indicate cytotoxic potential. |
| Histological Stains (H&E) | Microscopic evaluation of tissue response post-explant [81]. | Assesses inflammation, fibrosis, and tissue integration. |
| Alginate Hydrogels | Base material for soft, conductive neural interfaces [73]. | Modulus tunable from 10 Pa to 100 kPa; can be blended with CNTs/graphene for conductivity. |
| Parylene-C | A flexible polymer used as a substrate for ultrathin electronics [10]. | Biocompatible, used in sub-5μm thick devices for conformal contact. |
| Polyrotaxane (PR) | A supramolecular structure for creating highly stretchable conductors [73]. | Enables conductivity under 100% strain for dynamic organ interfaces. |
In vivo validation remains a critical, irreplaceable bridge between the development of bioelectronic materials with optimized Young's modulus and their safe application in humans. The process, guided by ethical principles and rigorous regulatory standards, ensures that devices are not only mechanically compatible but also biologically safe and functionally effective. The future of this field lies in the continued development of advanced "tissue-like" materials such as supramolecular hydrogels and ultra-thin composites that further minimize mechanical mismatch [73]. Furthermore, the integration of artificial intelligence and 3D printing holds promise for optimizing device design and fabrication, potentially reducing the reliance on animal models through better predictive in silico models [73]. As these technologies converge, the path to clinical translation for bioelectronic implants will become more efficient, yielding devices that seamlessly integrate with the human body for chronic diagnostic and therapeutic applications.
In the rapidly advancing field of bioelectronics, the mechanical compatibility of materials with biological tissues is as crucial as their electrical performance. The Young's modulus, a fundamental measure of a material's stiffness, has emerged as a pivotal parameter in the design of next-generation bioelectronic interfaces. This review provides a comparative analysis of three principal material classes—hydrogels, conductive polymers, and elastomeric composites—framed within the context of their mechanical properties, specifically their Young's modulus, and their applicability in bioelectronic devices. The inherent mismatch between traditional rigid electronic components and soft, dynamic biological tissues (which typically exhibit moduli in the kPa to low MPa range) can lead to poor contact, signal interference, inflammatory responses, and device failure [52]. This analysis delves into how each material system addresses this challenge, balancing electrical functionality with mechanical compliance to enable stable, long-term, and high-fidelity integration with biological systems.
Material Classes and Their Fundamental Properties
Hydrogels
Hydrogels are three-dimensional, hydrophilic polymer networks capable of retaining large amounts of water, which confers tissue-like softness, high biocompatibility, and often, ionic conductivity [84] [85]. Their mechanical properties, including Young's modulus, are highly tunable through parameters such as polymer concentration, cross-linking density, and network architecture.
A significant advancement has been the development of double-network (DN) hydrogels, which dramatically improve toughness and mechanical strength. As pioneered by Gong et al., DN hydrogels consist of two interpenetrating networks: a rigid, brittle first network that dissipates energy through sacrificial bonds, and a soft, ductile second network that provides stretchability [85]. For instance, a fully physically cross-linked Agar/hydrophobic associated polyacrylamide (HPAAm) hydrogel demonstrated a tensile strength of 0.267 MPa [85]. Furthermore, the incorporation of nanofillers like cellulose can significantly enhance mechanical properties. Studies on cellulose-composited ionic-covalent entanglement (ICE) hydrogels based on gelatin methacrylate/alginate (G/A) showed that microfibrillated cellulose (MFC) and nanofibrillated cellulose (NFC) could increase the Young's modulus to 363.43 kPa and 325.75 kPa, respectively, attributed to synergistic hydrogen bonding between the cellulose fiber network and the ICE matrix [86].
Conductive hydrogels are created by incorporating conductive fillers (e.g., carbon-based materials, metal nanoparticles) or polymers (e.g., PEDOT:PSS) into the hydrogel matrix, or by using ionic conductivity [84] [87]. A notable example is a polyvinyl alcohol (PVA)-based conductive hydrogel containing PEDOT:PSS and Laponite (LAP), which achieved an electrical conductivity of 17.9 S/m while maintaining a high tensile strength of 884 kPa and a Young's modulus of 3.42 MPa [88].
Conductive Polymers
Conductive polymers (CPs), such as poly(3,4-ethylenedioxythiophene):poly(styrenesulfonate) (PEDOT:PSS), polyaniline (PANI), and polypyrrole (PPy), are characterized by their conjugated molecular backbones that enable electronic charge transport [84] [87]. While they offer excellent electrical properties and are often processable, their mechanical properties in pure form can be a limitation. They are often brittle and exhibit a high Young's modulus. To overcome this, they are frequently blended with soft, insulating matrix polymers to form compliant conductive composites.
The mechanical and electrical properties of such composites are well-described by percolation theory. A foundational study on gold-polydimethylsiloxane (PDMS) nanocomposites created by metal-ion implantation revealed that electrical conductivity and Young's modulus follow different percolation behaviors within the same sample [89]. This means that a composite can be designed to conduct electricity (by exceeding the electrical percolation threshold where conductive particles form a connected network) while minimizing the increase in stiffness, thus decoupling these two properties [89]. This principle is key to developing CP-based materials that are both conductive and soft.
Elastomeric Composites
Elastomers, such as PDMS, polyurethane (PU), and Ecoflex, are inherently stretchable, resilient, and durable polymers, making them ideal for applications requiring repeated mechanical loading [87]. Their native Young's modulus is typically low, matching that of many soft tissues. However, they are electrical insulators. To impart conductivity, conductive fillers—including metal nanoparticles, carbon nanotubes (CNTs), graphene, MXenes, or liquid metals—are incorporated to form elastomeric composites [90] [87].
A critical concept in this field is the "multiple network elastomer" or "molecular composite." Inspired by tough hydrogels, this approach involves embedding a stiff, cross-linked polymer network (the "filler network") within a soft, stretchable elastomeric matrix (the "matrix network") [91]. The synthesis involves creating a highly cross-linked first network, swelling it in a second monomer, and polymerizing it. The volume fraction of the stiff filler network (φFN) determines the composite's overall modulus, following the relationship λ₀³ = 1/φFN, where λ₀ is the isotropic prestretch of the filler network [91]. This method successfully combines high fracture toughness with fully reversible elasticity, even for moduli above 1 MPa [91]. The resulting materials exhibit a strain-dependent stiffening mechanism where the filler network breaks in a controlled manner to dissipate energy and resist crack propagation.
Table 1: Comparative Summary of Key Material Properties.
| Material Class | Typical Young's Modulus Range | Typical Conductivity Range | Key Mechanical Characteristics | Primary Conduction Mechanism |
|---|---|---|---|---|
| Hydrogels | kPa to low MPa [86] [88] [85] | S/m to tens of S/m [88] | Tunable softness, high toughness (DN), viscoelasticity | Ionic / Electronic (with fillers) |
| Conductive Polymers | High (pristine), tunable via blending | Up to thousands of S/cm [90] | Often brittle, requires composite design | Electronic (via conjugated backbone) |
| Elastomeric Composites | kPa to MPa [91] | Up to ~10 S/cm in blends [90] | High stretchability, toughness, resilience | Electronic (via percolating filler network) |
Table 2: Representative Experimental Data from Literature.
| Material System | Young's Modulus | Tensile Strength | Conductivity | Key Feature | Ref. |
|---|---|---|---|---|---|
| PVA-LAP-PEDOT:PSS Hydrogel | 3.42 MPa | 884 kPa | 17.9 S/m | EF-responsive drug release | [88] |
| Cellulose/GelMA-Alginate ICE | 363.43 kPa (MFC) | - | - | Enhanced compression resistance | [86] |
| Agar/HPAAm DN Hydrogel | - | 0.267 MPa | - | Fully physical, self-healing | [85] |
| PAMPS/P(NiPAAm-co-AAM) DN | - | 25 MPa (Compressive) | - | Fully chemical cross-linking | [85] |
| Au-PDMS Nanocomposite | Modeled via percolation theory | - | Modeled via percolation theory | Decoupled electrical/mechanical percolation | [89] |
| Molecular Composite EA(3.42) | ~2 MPa (from Fig. 2B) | - | - | 2.88 wt% filler, high toughness | [91] |
Experimental Protocols for Key Studies
Protocol 1: Fabrication of a Conductive Hydrogel e-Patch
This protocol details the creation of a multifunctional, electro-responsive hydrogel patch for wound healing, as described in [88].
Materials:
- Polyvinyl Alcohol (PVA): Biocompatible polymer matrix, FDA-approved.
- PEDOT:PSS: Conductive polymer filler to impart electronic conductivity.
- Laponite (LAP): Synthetic nanoclay that provides electrically sensitive rheological behavior and enhances drug release control.
- Tannic Acid (TA): Used as a cross-linking agent during the freeze-thaw process.
- Natural Rubber Latex (NRL): Forms the flexible and elastic support layer.
- Diclofenac Sodium (DF): Model anti-inflammatory drug for controlled release studies.
Methodology:
- Preparation of Conductive Ink: A solution is prepared by dissolving PVA in deionized water, followed by the addition of 1.25% wt PEDOT:PSS and 0.5% wt LAP. The mixture is stirred thoroughly to achieve homogeneity.
- Fabrication of Support Layer: A separate solution of 15% PVA in NRL is cast and allowed to set, forming the flexible backing layer.
- Patterned Freeze-Thaw Cross-linking: The conductive PVA/LAP/PEDOT:PSS ink is printed onto the NRL support layer. The construct is then subjected to a cyclic freeze-thaw process in the presence of tannic acid. This physical cross-linking method creates a stable 3D network via hydrogen bonding without toxic chemical cross-linkers.
- Drug Loading: The hydrogel patch is immersed in a solution of Diclofenac sodium, allowing the drug to diffuse into the swollen network.
- Characterization: Mechanical properties are tested via tensile tests. Electrical conductivity is measured via a four-point probe method. Drug release is quantified under applied electric fields using UV-Vis spectroscopy.
Protocol 2: Synthesis of Elastomeric Molecular Composites
This protocol outlines the creation of tough, multiple-network elastomers as presented in [91].
Materials:
- Ethyl Acrylate (EA): Primary monomer for both filler and matrix networks.
- Cross-linker: A chemical cross-linker (e.g., di-functional acrylate) for the first network.
- Initiator: A thermal initiator for polymerization (e.g., azobisisobutyronitrile, AIBN).
Methodology:
- Synthesis of Filler Network (EA(1)): The first network is polymerized with a high cross-linking density, resulting in a stiff and brittle elastomer.
- Swelling and Prestretching: The filler network is swollen in a second batch of ethyl acrylate monomer containing an initiator. The degree of swelling determines the isotropic prestretch (λ₀) of the filler network strands. The volume fraction of the filler network (φ_FN) is calculated as 1/λ₀³.
- Polymerization of Matrix Network: The swollen network is subjected to a second polymerization step, creating a double-network (DN) elastomer. This process can be repeated to create triple (TN) or multiple networks with progressively lower filler network content.
- Mechanical Testing: Samples are cut into dumbbell shapes and subjected to uniaxial tensile tests at a constant stretch rate (e.g., 0.02 s⁻¹) to fracture. Stress-strain curves are analyzed to determine Young's modulus (E), and the strain hardening behavior is fitted with constitutive models like the Gent model.
Protocol 3: Determining Percolation in Nanocomposites
This protocol is based on the study of metal-ion implanted PDMS, which provides a quantitative basis for separating electrical and mechanical percolation [89].
Materials:
- Polydimethylsiloxane (PDMS): Elastomeric substrate.
- Metal Sources: Gold and Titanium for implantation.
Methodology:
- Sample Fabrication (Implantation): PDMS samples are implanted with gold or titanium ions using a Filtered Cathode Vacuum Arc (FCVA) plasma source. The process is performed under high vacuum with ion energies ranging from 2.5 to 10 keV and doses from 10¹⁵ to 5×10¹⁶ ions cm⁻².
- Microstructural Analysis (TEM): Cross-sectional transmission electron microscopy (TEM) is performed on the implanted layers. This critical step allows for the accurate determination of the metal volume fraction in the composite and the analysis of nanoparticle size and distribution.
- Electrical Characterization: The electrical conductivity (σ) of the nanocomposite layer is measured.
- Mechanical Characterization: The Young's modulus (Y) of the same nanocomposite samples is measured.
- Percolation Analysis: Both conductivity and Young's modulus are plotted against the independently measured metal volume fraction. The data is fitted with percolation theory equations, allowing the determination of distinct percolation thresholds and critical exponents for electrical and mechanical properties.
Visualization of Material Design and Property Relationships
The following diagram illustrates the structural concepts and property relationships of the three material classes discussed.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Bioelectronic Material Research.
| Reagent/Material | Function in Research | Example Application |
|---|---|---|
| Polyvinyl Alcohol (PVA) | Synthetic polymer matrix for hydrogels; provides biocompatibility and tunable mechanical properties via freeze-thaw cycling. | Hydrogel-based bio-electronic patches [88]. |
| PEDOT:PSS | Intrinsically conductive polymer; imparts electronic conductivity to hydrogels and elastomers. | Conductive filler in PVA hydrogels [88]; component in conductive inks [87]. |
| Alginate, Gelatin Methacrylate | Natural polymers forming hydrogel networks; offer biocompatibility and cell interaction sites. | Base for cellulose-composited ICE hydrogels [86]. |
| PDMS (Polydimethylsiloxane) | Silicone-based elastomer; provides excellent stretchability, transparency, and biocompatibility. | Matrix for metal-ion implanted nanocomposites [89]; base for molecular composites [91]. |
| Micro/Nanofibrillated Cellulose | Natural nanofiller; reinforces hydrogel mechanical strength and toughness via hydrogen bonding. | Mechanical reinforcement in gelatin methacrylate/alginate hydrogels [86]. |
| Laponite (LAP) | Synthetic nanoclay; enhances mechanical properties and enables electro-responsive behavior (e.g., drug release). | Component for electric field-triggered drug release in hydrogels [88]. |
| Metal Nanoparticles (Au, Ag) | Conductive filler; forms percolating networks for electron transport in composites. | Creation of conductive layers via ion implantation [89]; filler in elastomeric composites [87]. |
| Tannic Acid | Natural cross-linker; enables physical, non-toxic cross-linking of polymer chains (e.g., via hydrogen bonds). | Cross-linking agent in patterned freeze-thaw synthesis [88]. |
The choice between hydrogels, conductive polymers, and elastomeric composites for bioelectronic applications is dictated by the specific mechanical and electrical requirements of the target biological interface. Hydrogels excel in environments demanding extreme softness, high water content, and ionic conduction or drug delivery. Conductive polymers offer high electrical performance but require sophisticated composite design to achieve mechanical compliance. Elastomeric composites provide unparalleled toughness and stretchability, making them ideal for dynamic, load-bearing implants and wearables. The overarching theme in modern bioelectronic materials research is the deliberate decoupling of electrical and mechanical properties, guided by principles such as sacrificial bonding in double-network hydrogels and percolation theory in composites. This nuanced understanding of Young's modulus and its relationship with other material properties is fundamental to developing the next generation of biointegrated electronic devices.
The clinical translation of bioelectronic devices represents a frontier in modern medicine, offering novel therapeutic solutions for a range of conditions from neurological disorders to cardiovascular diseases. Within the broader context of Young's modulus research on bioelectronic materials, a critical challenge emerges: the mechanical mismatch between conventional electronic materials and soft biological tissues. This discrepancy in mechanical properties, particularly Young's modulus—the measure of a material's stiffness—directly impacts device reliability, long-term stability, and ultimately, clinical viability [10] [4].
Biological tissues, including brain, nerve, and muscle, are soft, dynamic, and viscoelastic, with Young's modulus values typically ranging from 0.1 kPa to 1 MPa [10] [92]. In stark contrast, traditional electronic materials like silicon and metals possess moduli in the gigapascal range (GPa), creating a stiffness mismatch of several orders of magnitude [4]. This mechanical mismatch causes micromotion-induced inflammation, fibrotic encapsulation, reduced signal fidelity, and eventual device failure [10] [4]. Consequently, understanding and engineering the Young's modulus of bioelectronic materials has become a central focus for achieving reliable, stable devices worthy of clinical translation.
This technical guide explores the pathway to clinical translation through the lens of materials mechanics, addressing three fundamental pillars: (1) material strategies for reliability through mechanical compatibility, (2) methodologies for stability assessment, and (3) navigation of the complex regulatory landscape for mechanically-advanced bioelectronics.
Material Strategies: Engineering Young's Modulus for Reliability
The Soft Bioelectronics Paradigm
The field is undergoing a paradigm shift from rigid to soft, compliant bioelectronics that mirror the mechanical properties of biological tissues [4]. This transition requires innovative material solutions with tailored Young's modulus values. The following table summarizes key material classes and their mechanical properties relevant to bioelectronics:
Table 1: Mechanical Properties of Bioelectronic Materials and Biological Tissues
| Material/Tissue | Young's Modulus Range | Key Characteristics | Bioelectronic Applications |
|---|---|---|---|
| Neural Tissue | 0.1 - 3 kPa [10] | Extremely soft, viscoelastic | Target for brain interfaces, peripheral nerve stimulators |
| Muscle & Skin | 1 - 100 kPa [10] | Soft, elastic, dynamic | Target for wearable sensors, muscle stimulators |
| Conductive Polymers (PEDOT:PSS) | 1 - 3 GPa [93] | Moderate stiffness, conductive for ions and electrons | Electrodes, transistors, neural recording |
| Elastomers (PDMS, Ecoflex) | 0.1 - 3 MPa [10] | Stretchable, biocompatible | Substrates, encapsulants for wearable devices |
| Hydrogels | 1 kPa - 1 MPa [10] | Hydrated, tissue-like modulus | Injectable electronics, tissue integration layers |
| Metals (Au, Pt) | 50 - 200 GPa [10] | High stiffness, ductile, conductive | Traditional electrodes (require ultrathin geometries) |
| Silicon | 130 - 190 GPa [4] | High stiffness, semiconducting | Conventional electronics (require strategic placement) |
Material Solutions for Mechanical Compatibility
Several material engineering strategies have emerged to address the mechanical mismatch problem:
Conductive Polymers and Processing Advances: Poly(3,4-ethylenedioxythiophene)-poly(styrenesulfonate) (PEDOT:PSS) is a cornerstone material that conducts both ionic and electronic charges, bridging communication between biology and electronics [93]. Recent research has discovered that thermal processing above conventional thresholds can stabilize PEDOT:PSS in water without chemical crosslinkers, producing a material with three times higher electrical conductivity and excellent batch-to-batch consistency [93]. This heat-treated PEDOT:PSS maintains electrical performance when stretched and has demonstrated stability in chronic in vivo experiments for over 20 days post-implantation [93].
Structural Engineering for Effective Softness: Beyond intrinsic material properties, structural design can dramatically reduce effective modulus. Fabricating devices in ultrathin geometries (e.g., < 5 μm thickness) on substrates like parylene-C significantly reduces bending stiffness, enabling conformal contact driven by van der Waals forces without external adhesives [10]. Placing stiff components along the neutral mechanical plane or using mesh, kirigami, or origami designs further enhances mechanical compatibility while preserving electronic performance [10] [4].
Biodegradable Metals: Zinc-based biodegradable materials offer an intermediate corrosion behavior and favorable mechanical properties for temporary implants. Alloying and surface modifications can tailor their degradation rates and mechanical performance to match the healing timeline of surrounding tissues, providing support until the tissue regenerates before safely dissolving [94].
Stability Assessment: Methodologies and Protocols
Experimental Framework for Stability Evaluation
Assessing the long-term stability of bioelectronic devices requires a multi-faceted experimental approach that evaluates performance under biologically-relevant conditions.
Mechanical Testing Protocols:
- Nanoindentation via Atomic Force Microscopy (AFM): AFM nanoindentation quantifies Young's modulus of materials and tissues by pressing a sharp tip into the sample and monitoring cantilever deformation [92]. Force-distance (F–z) curves are converted to force-indentation (F−h) curves, and mechanical properties are extracted using contact mechanics models, most commonly Hertzian mechanics [92]. For a conical indenter, the relationship is F = (2E tan(θ)/(π(1-v²))) h², where E is Young's modulus, θ is the cone's half-angle, and v is the Poisson's ratio.
- Accelerated Aging in Simulated Biological Environments: Devices are subjected to phosphate-buffered saline (PBS) or simulated body fluid (SBF) at 37°C to mimic physiological conditions. Electrochemical impedance spectroscopy tracks changes in electrode interface properties over time, identifying corrosion or delamination [94].
- Cyclic Mechanical Strain Testing: Using commercial strain systems, devices undergo repeated stretching or bending (thousands to millions of cycles) at strains mimicking body movements (e.g., 10-30% for skin). Electrical conductivity and functionality are monitored throughout to assess mechanical fatigue resistance [10].
Electrical Performance Monitoring:
- Chronic In Vivo Electrophysiology: For implanted devices, signal-to-noise ratio (SNR) and electrode impedance are tracked longitudinally in animal models. A stable interface maintains consistent SNR, while increasing impedance often indicates fibrosis or material degradation [4] [93].
- Stretchable Interconnect Assessment: The resistance of stretchable conductive traces (e.g., made from liquid metals or wrinkled thin films) is measured under static and dynamic strain to ensure reliable connectivity during body movement [10].
Biological Response Evaluation:
- Histological Analysis: Post-explantation, tissue is sectioned and stained for markers of inflammation (e.g., CD68 for macrophages), fibrosis (e.g., collagen deposition), and neuronal health (e.g., NeuN for neurons). Devices with better mechanical matching show reduced glial scarring and neuronal loss [4].
- Immunohistochemistry: Specific cell types and immune responses are quantified around the implant interface. A stable, biocompatible interface integrates with minimal chronic inflammatory response [94].
Stability Challenges and Failure Modes
Key failure modes for bioelectronic devices include:
- Water Permeation: Moisture ingress is a primary failure mechanism, causing corrosion, delamination, and electrical short circuits. Effective encapsulation with materials like ultrathin parylene or silicon nitride is critical, but must balance barrier properties with flexibility [4].
- Fatigue Fracture: Repeated mechanical stress can crack conductive traces or semiconductor components, leading to electrical failure. Strategic placement of rigid islands on the neutral mechanical plane and using strain-relief structures can mitigate this risk [10].
- Biofouling and Fibrosis: The foreign body response leads to protein adsorption and collagenous capsule formation, isolating the device and degrading signal quality. Surface modifications with soft hydrogels or anti-inflammatory drug elution can reduce this response [4] [94].
The Regulatory Pathway to Clinical Translation
Navigating Global Regulatory Frameworks
The path from laboratory research to clinical application requires rigorous adherence to regulatory standards that ensure safety and efficacy. The following diagram outlines the core logical relationship between material properties, device function, and the resulting regulatory evidence required for approval.
Regulatory bodies, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), require comprehensive evidence that addresses the unique challenges of soft bioelectronics [94] [95]. Key regulations include:
- ISO 10993 Series (Biological Evaluation of Medical Devices): This standard mandates rigorous biocompatibility testing based on the nature and duration of body contact. It requires evaluation of cytotoxicity, sensitization, and systemic toxicity, which can be influenced by material degradation products or leachables from novel polymers [94].
- FDA 510(k) or Premarket Approval (PMA): In the U.S., most bioelectronic devices require a 510(k) submission demonstrating substantial equivalence to a predicate device, or a more rigorous PMA for novel, high-risk devices. The submission must include detailed mechanical performance data, reliability testing, and sterilization validation [94].
- EU Medical Device Regulation (MDR): The MDR requires a comprehensive technical dossier, including detailed material characterization, clinical evaluation, and post-market surveillance plans. Instructions for use and labelling must be translated into the official language(s) of each member state where the device is marketed [95].
The Researcher's Toolkit: Essential Reagents and Materials
Successful development and regulatory approval depend on carefully selected materials and standardized testing protocols.
Table 2: Essential Research Reagents and Materials for Bioelectronic Translation
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| PEDOT:PSS | Conductive polymer for electrodes and transistors | Bridging ionic/electronic conduction; requires stability optimization (e.g., thermal processing) [93]. |
| Parylene-C | Biostable, conformal encapsulation layer | Provides moisture barrier while maintaining flexibility; deposited via chemical vapor deposition [10]. |
| Biodegradable Zn Alloys | Material for temporary implants | Degrades in body; mechanical properties and degradation rate must match tissue regeneration timeline [94]. |
| Simulated Body Fluid (SBF) | In vitro accelerated aging | Mimics ionic composition of blood plasma for corrosion and stability testing [94]. |
| Cell Culture Media | Cytotoxicity testing (ISO 10993-5) | Assesses biocompatibility of extracts or direct contact with materials [94]. |
| AFM Cantilevers | Nanomechanical characterization | Measures Young's modulus of materials and tissues; requires calibration of spring constant [92]. |
The clinical translation of bioelectronic devices is intrinsically linked to the successful engineering of their mechanical properties, with Young's modulus serving as a critical design parameter. By developing materials and devices that mimic the soft, dynamic nature of biological tissues, researchers can significantly enhance reliability and long-term stability. This path requires a multidisciplinary approach, integrating materials science with rigorous mechanical and biological testing, all while navigating an increasingly complex global regulatory landscape. The future of bioelectronic medicine lies in closing the mechanical mismatch gap, creating devices that seamlessly integrate with the human body for chronic, high-performance operation.
Conclusion
Mastering Young's modulus is no longer a secondary consideration but a foundational principle for the next generation of bioelectronic medicine. The convergence of material science and device engineering has yielded a versatile toolkit—from modulus-tunable hydrogels to geometrically soft electronics—that effectively bridges the mechanical divide with biological tissues. This progress directly addresses chronic challenges of inflammation and signal instability, paving the way for robust, long-lasting neural interfaces, organ-mounted sensors, and closed-loop therapeutic systems. Future advancements will be driven by the integration of artificial intelligence for predictive material design, the development of novel bioresorbable and battery-free devices, and a deeper focus on creating personalized bioelectronics that adapt to individual anatomical and physiological needs, ultimately solidifying the role of bioelectronics as a pillar of 21st-century therapeutics.
References
- 1. Young's modulus [https://en.wikipedia.org/wiki/Young%27s_modulus]
- 2. What is Young's Modulus? Understanding the Basics of ... [https://polyspectra.com/what-is-youngs-modulus/]
- 3. Conforming strategies for bioelectronics on arbitrary surfaces [https://www.nature.com/articles/s44328-025-00064-9]
- 4. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 5. Advances in bioelectronics for neural interfacing [https://link.springer.com/article/10.1557/s43579-025-00822-w]
- 6. Integrated implantable bioelectronic system based on ... [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00012-6]
- 7. PEDOT:PSS-based bioelectronics for brain monitoring and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075682/]
- 8. Clinical challenges and opportunities related to the ... [https://www.sciencedirect.com/science/article/pii/S1742706124007566]
- 9. Electric Field-Induced Modulation of Mechanical Behavior ... [https://www.sciencedirect.com/science/article/abs/pii/S1751616125002954]
- 10. Materials strategy and device fabrication for stable closed ... [https://www.nature.com/articles/s44328-025-00045-y]
- 11. Empirical estimation of Young's modulus for biological tissue ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0320705]
- 12. Experimental study of Young's modulus and internal friction ... [https://www.sciencedirect.com/science/article/pii/S2095034925000042]
- 13. Protocol for measuring the Young's modulus of organoids ... [https://www.sciencedirect.com/science/article/pii/S266616672500231X]
- 14. A Comparative Analysis of Selected Methods for ... [https://www.mdpi.com/1996-1944/15/1/149]
- 15. Recent Advances in Stimuli‐Responsive Materials and Soft ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243729/]
- 16. Synergistic mastery: Advancing mechanical and electrical ... [https://www.sciencedirect.com/science/article/pii/S2452199X25002439]
- 17. Implantable bioelectronics toward long-term stability and ... [https://www.sciencedirect.com/science/article/pii/S2590238521000564]
- 18. Ithy - Bridging Brain and Machine: Unlocking the Secrets of the... [https://ithy.com/article/neuron-electrode-interface-impedance-solutions-9snk6nr6]
- 19. Overcoming failure: improving acceptance and success of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00168-7]
- 20. modes of chronically implanted planar... Mechanical failure [https://pubmed.ncbi.nlm.nih.gov/25453935/]
- 21. Nanoscale Young's modulus and resistivity of flexible Au ... [https://www.sciencedirect.com/science/article/abs/pii/S016943322500635X]
- 22. Chemically revised conducting polymers with inflammation ... [https://www.sciencedirect.com/science/article/pii/S2452199X23000488]
- 23. Revolutionizing brain‒computer interfaces - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243264/]
- 24. Long-term stability strategies of deep brain flexible neural ... [https://www.nature.com/articles/s41528-025-00410-x]
- 25. Emerging fiber-based neural interfaces with conductive ... [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d4mh01854k]
- 26. Advances in Conductive Biomaterials for Cardiac Tissue ... [https://www.mdpi.com/2073-4360/17/5/620]
- 27. Modulus-adjustable and mechanically adaptive dry ... [https://www.nature.com/articles/s41528-025-00458-9]
- 28. Emerging roles of hydrogels, organogels, and their hybrids ... [https://www.nature.com/articles/s44328-025-00055-w]
- 29. Recent advances in conductive hydrogels for soft ... [https://www.sciencedirect.com/science/article/pii/S2950235724000222]
- 30. Single- and Multi-Network Hydrogels for Soft Electronics— ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294428/]
- 31. Novel conductive PEDOT:DBSA hydrogels with tuneable ... [https://pubs.rsc.org/en/content/articlelanding/2025/ma/d4ma00987h]
- 32. Electrically conducting porous hydrogels by a self-assembled ... [https://pubs.rsc.org/en/content/articlehtml/2025/sm/d4sm01311e]
- 33. Hierarchically structured conductive hydrogels for ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925003803]
- 34. Hierarchically structured conductive hydrogels for ... [https://pubmed.ncbi.nlm.nih.gov/40268199]
- 35. Engineers create hydrogels to monitor activity in the body [https://source.washu.edu/2025/10/engineers-create-hydrogels-to-monitor-activity-in-the-body/]
- 36. Advances in Conductive Polymer-Based Flexible ... [https://www.mdpi.com/2504-477X/9/1/42]
- 37. Electrically Conductive Materials: Opportunities and ... [https://www.sciencedirect.com/science/article/abs/pii/S2352492825023347]
- 38. Electrically conducting polymers for bio-interfacing ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566320306102]
- 39. Highly conductive polymer with vertical phase separation ... [https://www.nature.com/articles/s41528-025-00441-4]
- 40. Conductive Polymers and Their Nanocomposites [https://www.mdpi.com/2073-4360/15/18/3783]
- 41. Recent Developments and Implementations of Conductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9504310/]
- 42. Flexible Nanowire Conductive Elastomers for Applications ... [https://pubmed.ncbi.nlm.nih.gov/34892455/]
- 43. Review of sustainable, eco-friendly, and conductive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10876511/]
- 44. Conducting Polymers Market, Industry Size Forecast [Latest] [https://www.marketsandmarkets.com/Market-Reports/conducting-polymer-market-145936286.html]
- 45. Conductive Polymers Market | Global Market Analysis Report [https://www.futuremarketinsights.com/reports/conductive-polymers-market]
- 46. Materials and noncoplanar mesh designs for integrated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2584145/]
- 47. Stretchability and compliance of freestanding serpentine- ... [https://www.sciencedirect.com/science/article/pii/S0020768314003011]
- 48. Mechanical properties and osteointegration of the mesh ... [https://www.sciencedirect.com/science/article/abs/pii/S1751616123001157]
- 49. Mechanical Properties of Mesh Materials Used for Hernia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3470559/]
- 50. Measurement of Young's modulus and Poisson's ratio for ... [https://www.sciencedirect.com/science/article/pii/S1567173908001958]
- 51. Effect of mesh sizes on the mechanical properties ... [https://www.nature.com/articles/s41598-025-20038-1]
- 52. Hydrogel-based soft bioelectronic interfaces and their ... [https://pubs.rsc.org/en/content/articlehtml/2025/tc/d4tc04150j]
- 53. Engineered hydrogels for mechanobiology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7614763/]
- 54. 3D-Printed Hydrogel for Diverse Applications: A Review [https://www.mdpi.com/2310-2861/9/12/960]
- 55. Liquid-in-liquid printing of 3D and mechanically tunable ... [https://www.nature.com/articles/s41467-023-40004-7]
- 56. Current Biomedical Applications of 3D-Printed Hydrogels [https://pmc.ncbi.nlm.nih.gov/articles/PMC10815850/]
- 57. Modulus-tunable multifunctional hydrogel ink with ... [https://pubmed.ncbi.nlm.nih.gov/38574560/]
- 58. 3D-Printed Hydrogels from Natural Polymers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942323/]
- 59. 3D printable and mechanically tunable hydrogels achieved ... [https://pubs.rsc.org/en/content/articlelanding/2024/sm/d4sm00602j]
- 60. Simple yet effective methods to probe hydrogel stiffness for ... [https://www.nature.com/articles/s41598-021-01036-5]
- 61. Unlocking superior fracture resistance in micro-ceramics ... [https://www.sciencedirect.com/science/article/pii/S1359645425007608]
- 62. Young's modulus measurement [https://bio-protocol.org/exchange/minidetail?id=987208&type=30]
- 63. Effect of Relative Humidity On the Young's Modulus of ... [https://aquila.usm.edu/fac_pubs/1732/]
- 64. Experimental Study on the Effect of Humidity on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608748/]
- 65. Structure–Transport Properties Governing the Interplay in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9955331/]
- 66. Circuit Design Tips: PCB Moisture Protection for Humid Environments [https://resources.altium.com/p/circuit-design-tips-pcb-moisture-protection-humid-environments]
- 67. Understanding elasticity and swellability of polymer gels ... [https://www.sciencedirect.com/science/article/abs/pii/S1359029424000906]
- 68. Advances in Materials with Self-Healing Properties [https://pmc.ncbi.nlm.nih.gov/articles/PMC11123491/]
- 69. Self‐Healing Materials for Bioelectronic Devices [https://www.semanticscholar.org/paper/Self%E2%80%90Healing-Materials-for-Bioelectronic-Devices-Liu-Kelley/8e3f477278ffad787537634ffccc3650d1c69ce7]
- 70. Experimental characterization of the self-healing capacity ... [https://www.sciencedirect.com/science/article/pii/S095006181830165X]
- 71. Self Healing Materials Market Size 2024-2028 [https://www.technavio.com/report/self-healing-materials-market-industry-analysis]
- 72. Review Self-healing materials for wearable electronics [https://www.sciencedirect.com/science/article/pii/S2950235725000198]
- 73. Perspectives on tissue-like bioelectronics for neural modulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10192532/]
- 74. Mechanically adaptive supercontractile polymer for soft ... [https://www.sciencedirect.com/science/article/pii/S2590238524000535]
- 75. Highly tough and conformal silk-based adhesive patches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271796/]
- 76. Electrical Safety Tests [https://www.ebme.co.uk/articles/electrical-safety/electrical-safety-tests]
- 77. Electrical Safety Standards and Basic Testing [https://www.flukebiomedical.com/blog/electrical-safety-standards-and-basic-testing]
- 78. Mechanical Testing: Types, Benefits, and Applications Explained [https://elenergylab.com/what-is-mechanical-testing/]
- 79. What is Mechanical Testing? (A Complete Guide) - TWI [https://www.twi-global.com/technical-knowledge/faqs/what-is-mechanical-testing]
- 80. Mechanical Testing - ASTM Test Methods Performed [https://www.lucideon.com/testing-characterisation/mechanical-testing/mechanical-astms]
- 81. Preclinical research models for evaluating the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628057/]
- 82. The “Big Three” in biocompatibility testing of medical devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800850/]
- 83. Regulatory considerations for animal studies of biomaterial ... [https://www.sciencedirect.com/science/article/pii/S2452199X21004497]
- 84. Recent Advances in Conductive Composite Hydrogels for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562860/]
- 85. Research Advances in Mechanical Properties and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9779336/]
- 86. Multiscale mechanical properties and enhancement ... [https://www.sciencedirect.com/science/article/pii/S0144861725002024]
- 87. Printable Conductive Hydrogels and Elastomers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12469759/]
- 88. Development of Hydrogel-Based Flexible Bio-Electronic ... [https://www.sciencedirect.com/science/article/pii/S177322472501189X]
- 89. Electrical conductivity and Young's modulus of flexible ... [https://www.sciencedirect.com/science/article/abs/pii/S1359645410006920]
- 90. Conducting materials as building blocks for electronic textiles [https://pmc.ncbi.nlm.nih.gov/articles/PMC8550728/]
- 91. Mechanics of elastomeric molecular composites - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6140500/]
- 92. The Young's Modulus as a Mechanical Biomarker in AFM ... [https://www.mdpi.com/1424-8220/25/11/3510]
- 93. Chance discovery improves stability of bioelectronic material ... [https://news.rice.edu/news/2025/chance-discovery-improves-stability-bioelectronic-material-used-medical-implants]
- 94. Challenges in Zinc-Based Biodegradable Materials for ... [https://link.springer.com/chapter/10.1007/978-981-95-2401-3_10]
- 95. Understanding the Regulatory Landscape for Medical ... [https://www.mylanguageconnection.com/understanding-the-regulatory-landscape-for-medical-translation/]