Validating Neurostimulation Protocols: A Computational Modeling Approach for Enhanced Precision and Efficacy
This article provides a comprehensive examination of computational model validation for neurostimulation protocols, a critical step in translating theoretical simulations into reliable clinical and research applications.
Validating Neurostimulation Protocols: A Computational Modeling Approach for Enhanced Precision and Efficacy
Abstract
This article provides a comprehensive examination of computational model validation for neurostimulation protocols, a critical step in translating theoretical simulations into reliable clinical and research applications. Aimed at researchers, scientists, and drug development professionals, it explores the foundational principles underpinning model credibility, details advanced methodological workflows for application, addresses key troubleshooting and optimization challenges such as parameter personalization and handling biological variability, and establishes robust frameworks for validation and comparative analysis against experimental data. By synthesizing current literature and emerging trends, this review serves as a strategic guide for enhancing the predictive power and clinical feasibility of in-silico neurostimulation studies, ultimately aiming to improve reproducibility and therapeutic outcomes.
The 'Why' and 'What': Establishing the Bedrock for Credible Models
In the rapidly evolving field of computational neurostimulation, model validation represents a critical process for ensuring that virtual representations of neural systems accurately reflect biological reality. As defined by the American Academy of Actuaries and applied to computational neuroscience, model validation is "the practice of performing an independent challenge and thorough assessment of the reasonableness and adequacy of a model based on peer review and testing across multiple dimensions" [1]. For researchers and drug development professionals working with neurostimulation protocols, rigorous validation transforms theoretical models from speculative tools into reliable platforms for therapy optimization and device design.
The fundamental challenge driving the need for robust validation frameworks is the inherent complexity of neural systems and their interactions with electrical stimuli. Without proper validation, model risk—defined as the potential for misrepresenting intended relationships through flawed implementation or misuse—can lead to failed clinical translations and costly research dead ends [1]. This guide examines the key concepts, terminology, and experimental approaches defining model validation in neurostimulation research, providing a comparative analysis of emerging methodologies that are shaping the future of personalized neuromodulation therapies.
Core Principles of Model Validation
Effective model validation in neurostimulation research rests on eight core principles established by the North American CRO Council and adapted for computational neuroscience applications [1]:
- Model Design Consistency: The model construction must align with its intended purpose, whether for predicting neural tissue damage, optimizing stimulation parameters, or understanding fundamental mechanisms.
- Independent Validation: The validation process must be conducted separately from model development to eliminate confirmation bias.
- Designated Ownership: A single individual should be accountable for validation results and serve as the point of contact.
- Appropriate Governance: A formal framework must define roles, responsibilities, and maintenance procedures.
- Proportionality: Validation efforts should focus on areas of greatest materiality and complexity.
- Component Validation: Input data, computational logic, and output formats each require specific validation approaches.
- Limitation Acknowledgement: The inherent constraints of the validation process must be explicitly documented.
- Comprehensive Documentation: All processes, findings, and limitations must be recorded for future reference.
In Bayesian inference frameworks commonly used in neurostimulation research, validation extends beyond computational accuracy to assess whether modeling assumptions adequately capture relevant system behaviors [2]. This involves quantifying error in posterior expectation value estimates and performing posterior retrodictive checks to determine how well the posterior distribution recovers features of the observed data [2].
Table 1: Core Components of Model Validation in Neurostimulation
| Validation Component | Key Questions | Common Techniques |
|---|---|---|
| Input Validation | Are assumptions biologically plausible? Is source data reliable? | Expert judgment, benchmarking against literature, back-testing [1] |
| Calculation Validation | Does model logic correctly incorporate inputs? Are computations stable? | Sensitivity testing, dynamic validation, boundary case testing [1] |
| Output Validation | Do results align with experimental observations? Is presentation clear? | Comparison with existing models, historical back-testing, peer review [1] |
Comparative Analysis of Validation Approaches
Cardiovascular Neurostimulation Model
The Lehigh University team developed a computationally tractable model of the human cardiovascular system that integrates the processing centers in the brain that control the heart [3]. This model was specifically designed to predict hemodynamic responses following atrial fibrillation (AFib) onset and guide neurostimulation dosage decisions.
Validation Methodology: The team employed clinical data comparison, validating their model against real-patient data for heart rate, stroke volume, and blood pressure metrics [3]. The model's prediction of the atrioventricular node as a strong stimulation candidate provided additional validation, as this area is already an established target for ablation therapy [3].
Key Advantage: The model's computational efficiency makes it suitable for rapid testing and potential real-time use, creating a practical "digital twin" framework for personalized cardiac care [3].
Digital Twin Framework for Viscerosensory Neurostimulation
A 2025 study established a digital twin approach for predictive modeling of neuro-hemodynamic responses during viscerosensory neurostimulation [4]. This framework focuses on the computational role of the nucleus tractus solitarius (NTS) in the brainstem, capturing stimulus-driven hemodynamic perturbations through low-dimensional latent space representation of neural population dynamics [4].
Validation Methodology: Researchers implemented simultaneous extracellular single-unit NTS recordings and femoral arterial blood pressure measurements in rats (n=10) during electrical pulse train stimulation [4]. They analyzed cross-correlations and shared variances among NTS neurons (n=192), finding significantly higher couplings in measured data (83% shared variance) compared to dummy data (27% shared variance), validating that heterogeneous responses stem from interconnected neural populations [4].
Key Advantage: This approach enables individually optimized predictive modeling by leveraging neuro-hemodynamic coupling, potentially facilitating closed-loop neurostimulation systems for precise hemodynamic control [4].
Machine Learning Model for Tissue Damage Prediction
NeurostimML represents a novel machine learning approach for predicting electrical stimulation-induced neural tissue damage [5]. This model addresses limitations of the traditional Shannon equation, which relies on only two parameters and has demonstrated 63.9% accuracy compared to the Random Forest model's 88.3% accuracy [5].
Validation Methodology: Researchers compiled a database with 387 unique stimulation parameter combinations from 58 studies spanning 47 years [5]. They employed ordinal encoding and random forest for feature selection, comparing four machine learning models against the Shannon equation using k-fold cross-validation [5]. The selected features included waveform shape, geometric surface area, pulse width, frequency, pulse amplitude, charge per phase, charge density, current density, duty cycle, daily stimulation duration, daily number of pulses delivered, and daily accumulated charge [5].
Key Advantage: NeurostimML incorporates multiple stimulation parameters beyond charge-based metrics, enabling more reliable prediction of tissue damage across diverse neuromodulation applications [5].
Table 2: Comparative Performance of Neurostimulation Validation Approaches
| Model/Platform | Primary Validation Method | Key Performance Metrics | Computational Requirements |
|---|---|---|---|
| Lehigh Cardiovascular Model [3] | Clinical data comparison | Matched heart rate, stroke volume, and blood pressure to patient data | Low computational cost; suitable for rapid testing |
| Digital Twin NTS Framework [4] | Latent space analysis of neural populations | 83% shared variance in neuronal responses; accurate BP prediction | Medium requirements for latent space derivation |
| NeurostimML Random Forest [5] | k-fold cross-validation against historical data | 88.3% accuracy in damage prediction vs. 63.9% with Shannon equation | Higher requirements for training; efficient prediction |
Experimental Protocols for Model Validation
AI-Guided Neural Control Protocol
A detailed protocol for artificial intelligence-guided neural control in rats provides a framework for validating closed-loop neurostimulation systems [6]. This approach integrates deep reinforcement learning to drive neural firing to desired states, offering a validation methodology for neural control algorithms [6].
Key Steps:
- Perform chronic electrode implantations in rats to facilitate long-term neural stimulation
- Implement thalamic infrared neural stimulation and cortical recordings
- Apply deep reinforcement learning for closed-loop control of neural firing states
- Compare model-predicted outcomes with empirical neural recordings
This protocol emphasizes adherence to local institutional guidelines for laboratory safety and ethics throughout the validation process [6].
Multi-Target Electrical Stimulation Validation
Research published in Scientific Reports details the simulation and experimental validation of a novel noninvasive multi-target electrical stimulation method [7]. This approach addresses the challenge of achieving synchronous multi-target accurate electrical stimulation in deep brain regions.
Experimental Validation Workflow:
- Establish a simulation model based on magneto-acoustic coupling effect and phased array focusing technology
- Create an experimental system for transcranial magneto-acoustic coupling electrical stimulation (TMAES)
- Compare simulated and experimental results for multi-target focused electrical field distribution
- Quantify focal point size (achieving average of 5.1 mm per target) and location accuracy
The study demonstrated that multi-target TMAES could non-invasively achieve precise focused electrical stimulation of two targets, with flexibility to adjust location and intensity through parameter modification [7].
Model Validation Workflow in Neurostimulation Research
Essential Research Reagents and Materials
The execution and validation of neurostimulation models requires specific experimental setups and computational tools. The following table details key research solutions employed in the featured studies.
Table 3: Essential Research Reagents and Solutions for Neurostimulation Model Validation
| Reagent/Solution | Function in Validation | Example Applications |
|---|---|---|
| Chronic Electrode Implants [6] | Facilitate long-term neural stimulation and recording in animal models | AI-guided neural control protocols in rats [6] |
| Extracellular Recording Systems [4] | Capture single-unit neural activities during stimulation | NTS neuronal population recording (192 neurons across 10 rats) [4] |
| Hemodynamic Monitoring [3] [4] | Measure cardiovascular responses to neurostimulation | Femoral arterial BP measurement in rat models [4] |
| Finite Element Modeling Software [8] | Simulate electric field distributions in neural tissue | Patient-specific computational models of spinal cord stimulation [8] |
| Machine Learning Algorithms [5] | Predict tissue damage and optimize stimulation parameters | Random Forest classification for damage prediction [5] |
| Digital Twin Platforms [3] [4] | Create virtual replicas for personalized prediction | Cardiovascular digital twin for AFib therapy optimization [3] |
Signaling Pathways in Neurostimulation Validation
The validation of neurostimulation models requires understanding of key neural pathways involved in stimulus response. The nucleus tractus solitarius (NTS) pathway has been identified as crucial for cardiovascular control during viscerosensory neurostimulation [4].
NTS Pathway in Neurostimulation Response
The validation of computational models in neurostimulation research represents a multifaceted process that integrates computational techniques with experimental verification. As the field progresses toward more personalized medicine approaches, including digital twin frameworks [3] [4], robust validation methodologies become increasingly critical for clinical translation. The comparative analysis presented in this guide demonstrates that while validation approaches may differ across applications—from cardiovascular control to neural tissue damage prediction—they share common foundational principles that prioritize biological plausibility, computational accuracy, and experimental corroboration.
Future directions in neurostimulation model validation will likely involve greater integration of machine learning techniques [5], more sophisticated digital twin platforms [4], and standardized validation frameworks that can keep pace with rapid technological innovations. For researchers and drug development professionals, adhering to rigorous validation principles remains essential for transforming computational models from theoretical constructs into reliable tools for advancing neuromodulation therapies.
Computational models have become indispensable tools in the development and optimization of neurostimulation therapies, bridging the gap between theoretical concepts and clinical applications. The credibility of these models hinges on the faithful integration of two core components: accurate geometric representations of anatomy and robust physics-based simulations of underlying phenomena. This guide compares the performance of predominant modeling approaches used in the field, from traditional methods to modern machine learning-assisted techniques, providing researchers with a framework for validating models within neurostimulation protocol research.
In neurostimulation, computational models provide a critical platform for investigating mechanisms of action and optimizing therapy, fulfilling roles that would be difficult, time-consuming, or ethically challenging to perform through experimentation alone [9]. Their development is a multi-disciplinary endeavor, requiring the synthesis of anatomical geometry, the physics of bioelectric fields, and the neurophysiology of neural targets. A model's credibility is determined by its ability to not just replicate empirical data, but to predict outcomes in novel scenarios, such as a new patient anatomy or a previously untested stimulation parameter. This is particularly vital as the field advances toward multi-target therapies for complex neurological diseases, where intuitive parameter selection becomes impossible [10]. The following sections dissect the core components of these models, providing a comparative analysis of methodologies and the data that underpins their validation.
Comparative Analysis of Geometric Representation Methodologies
The choice of how to represent anatomy digitally is a foundational step that directly impacts a model's computational cost, biological fidelity, and ultimate utility. The table below compares the most common geometric representations used in computational models for neurostimulation.
Table 1: Comparison of Geometric Representation Methodologies in Computational Modeling
| Representation Type | Core Description | Typical Data Sources | Advantages | Limitations | Exemplary Use-Cases in Neurostimulation |
|---|---|---|---|---|---|
| Mesh-Based (e.g., Finite Element Meshes) | 3D geometry discretized into small elements (e.g., tetrahedra, hexahedra); physics are solved over this mesh. | MRI, CT, histological cross-sections [9] | High physical accuracy; well-established mathematical foundation; suitable for complex, inhomogeneous domains. | Very high computational cost; model construction is labor-intensive; solution time scales with mesh resolution. | Patient-specific models of the spinal cord for predicting electric field spread in SCS [9]. |
| Point Clouds & Voxels | Unstructured set of points in 3D space (point clouds) or a 3D grid of volumetric pixels (voxels). | 3D scanning, MRI/CT segmentation | Simpler to generate than meshes; directly output from many imaging modalities. | Lacks connectivity information; can be high-dimensional; not directly suitable for physics simulation without further processing. | Initial digital capture of anatomical structures before conversion to a simulation-ready format. |
| Implicit/SDF (Signed Distance Function) | A continuous function that defines the distance from any point in space to a surface; the surface is the set of points where SDF=0 [11]. | CAD models, algorithmic generation | Compact, continuous representation; easy to perform Boolean operations and check collisions. | Less intuitive for direct manipulation; can be computationally expensive to evaluate for complex shapes. | Representing smooth, synthetic geometries in preliminary design explorations for implantable leads. |
| Latent Representations (via LGM) | A low-dimensional vector learned by an AI model (e.g., VAE) that encodes the essential features of a high-dimensional geometry [11]. | Large datasets of existing 3D geometries (e.g., meshes) | Extremely compact (e.g., 512 dimensions); enables fast design optimization and surrogate modeling; filters out mesh noise. | Requires significant upfront investment to train the model; "black box" nature can reduce interpretability. | Rapidly exploring the design space of a new component or optimizing a geometry within a learned, valid manifold [11]. |
Comparative Analysis of Physics Integration and Solution Methods
Once the geometry is defined, the physical principles governing the system must be integrated and solved. The choice of solution method involves a trade-off between computational speed and physical rigor.
Table 2: Comparison of Physics Integration and Solution Methods in Neurostimulation Models
| Solution Method | Underlying Principle | Typical Software/Tools | Advantages | Limitations | Key Fidelity Metrics |
|---|---|---|---|---|---|
| Finite Element Method (FEM) | Solves partial differential equations (PDEs) by dividing the domain into small elements and finding approximate solutions per element [9]. | COMSOL, Abaqus, FEniCS | High accuracy for complex geometries and material properties; gold standard for electric field calculations. | Computationally intensive; requires expertise in mesh generation and convergence testing. | Electric field strength accuracy, convergence on mesh refinement. |
| Finite Volume Method (FVM) | Solves PDEs by calculating fluxes across the boundaries of control volumes. | OpenFOAM, ANSYS Fluent | Conserves quantities like mass and momentum by construction; robust for fluid dynamics. | Less common for bioelectric problems compared to FEM. | Conservation property adherence, solution stability. |
| Hodgkin-Huxley Formalism | A set of nonlinear differential equations that describes how action potentials in neurons are initiated and propagated [9]. | NEURON, Brian, custom code | Biologically realistic model of neuronal excitability; can model ion channel dynamics. | High computational cost at scale; requires detailed knowledge of channel properties. | Action potential shape accuracy, firing rate prediction. |
| Data-Driven FEM (DD-FEM) | A framework merging traditional FEM structure with data-driven learning to enhance scalability and adaptability [12]. | Emerging/Research Codes | Aims for FEM-level accuracy with reduced computational cost; potential for broader generalization. | Emerging methodology; lacks the established theoretical guarantees of traditional FEM [12]. | Generalization across boundary conditions, extrapolation accuracy in time/space [12]. |
| Surrogate Modeling (e.g., with Gaussian Processes) | Trains a lightweight statistical model on data generated from a high-fidelity simulator (e.g., FEM) to make fast predictions [11]. | GPy, scikit-learn, MATLAB | Extremely fast evaluation; built-in uncertainty quantification (e.g., confidence intervals) [11]. | Accuracy is limited by the training data; may not extrapolate well outside the training domain. | Prediction error vs. ground truth simulator, quality of uncertainty estimates. |
Validating the Integrated Model: Protocols and Performance Metrics
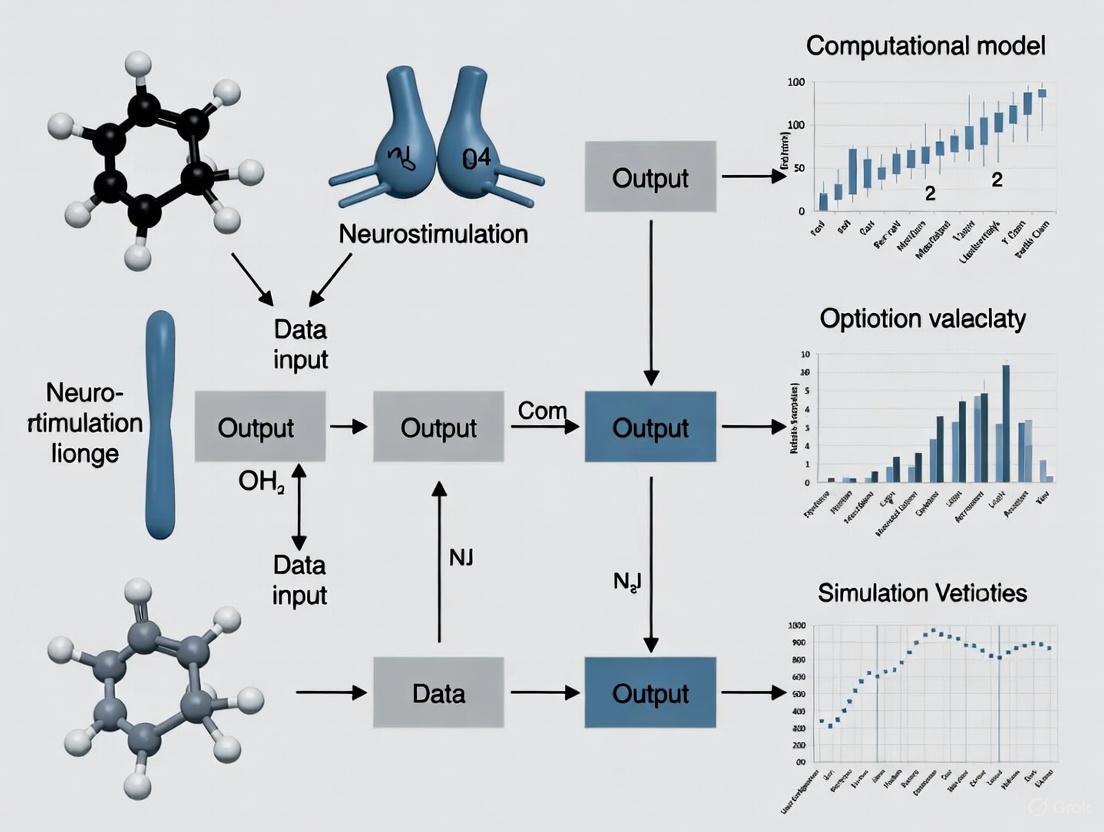
An integrated model combining geometry and physics is only as good as its validation. This process involves comparing model predictions against experimental and clinical data. The following diagram illustrates a standard workflow for building and validating a neurostimulation model, incorporating the components discussed in the previous sections.
Model Development and Validation Workflow
Key Validation Experiments and Performance Data
The credibility of a model is quantified by its performance against validation benchmarks. The table below summarizes key experimental protocols and the resulting performance data from recent credible computational models, particularly in the context of neurostimulation.
Table 3: Experimental Validation Protocols and Model Performance Benchmarks
| Validation Experiment | Experimental Protocol & Workflow | Key Outcome Measures | Reported Model Performance |
|---|---|---|---|
| Cardiovascular Neurostimulation (AFib) | 1. Develop closed-loop model integrating cardiovascular system & brain neurophysiology.\n2. Input clinical AFib episode data.\n3. Simulate neurostimulation and predict hemodynamic response.\n4. Compare predictions to empirical patient data [13]. | Heart rate (HR), stroke volume (SV), blood pressure (BP) profiles [13]. | Model output showed "robust concordance" with empirical patient data; identified AV node as a key neurostimulation target, aligning with clinical ablation practice [13]. |
| Spinal Cord Stimulation (SCS) for Pain | 1. Create patient-specific FEM model from medical images.\n2. Simulate electric field for a given lead design and stimulus.\n3. Use axon cable models to predict fiber activation.\n4. Correlate predicted activation with patient-reported pain relief [9]. | Neural activation thresholds of dorsal column fibers, spatial extent of activation, clinical pain ratings. | Models have "dramatically" improved lead designs and programming procedures; used commercially to focus stimulation on desired targets [9]. |
| SCS for Motor Control | 1. Couple electromagnetic model with neurophysiology.\n2. Simulate epidural stimulation and predict which neural pathways are recruited.\n3. Validate predictions via electrophysiology in animal models [8]. | Recruitment of sensory afferents vs. motor neurons, EMG responses, limb movement kinematics. | Models predicted and experiments confirmed that SCS primarily recruits large sensory afferents, not gray matter cells directly [8]. Model-driven biomimetic bursts restored movement in rats, monkeys, and humans [9]. |
| Surrogate Modeling via LGM | 1. Pre-train a Large Geometry Model (VAE) on millions of geometries.\n2. Encode new designs into a low-dimensional latent vector (z).\n3. Train a Gaussian Process regressor to map latent vector (z) to performance metric (c).\n4. Optimize in latent space and decode to full geometry [11]. | Prediction error of performance metrics (e.g., drag coefficient), geometric reconstruction accuracy. | Approach reduces overfitting risk vs. direct mesh-based models; provides uncertainty quantification; enables efficient high-dimensional design optimization [11]. |
Building and validating credible computational models requires a suite of specialized "research reagents" – both digital and physical.
Table 4: Essential Reagents and Resources for Computational Neurostimulation Research
| Tool/Reagent | Category | Primary Function in Research | Representative Examples / Notes |
|---|---|---|---|
| Medical Imaging Data | Data | Provides the anatomical geometry for constructing patient-specific or population-average models. | MRI, CT scans; essential for defining model geometry and assigning tissue boundaries [9]. |
| Volume Conductor Model | Software/Algorithm | Computes the distribution of extracellular electric potentials generated by neurostimulation in complex tissues [9]. | Often implemented with Finite Element Method (FEM) software; the core of the physics simulation. |
| Hodgkin-Huxley Type Models | Software/Algorithm | Simulates the response of individual neurons or axons to the applied electric field, predicting action potential generation [9]. | Implemented in platforms like NEURON; adds neurophysiological realism to the physical model. |
| Tissue Electrical Properties | Data | Critical input parameters for the volume conductor model that significantly influence the predicted electric field. | Conductivity values for cerebrospinal fluid (CSF), gray matter, white matter, and bone [9]. |
| Large Geometry Model (LGM) | AI Model | Learns a compact, low-dimensional representation of complex geometries to accelerate design and surrogate modeling [11]. | A pre-trained variational autoencoder (VAE); requires a large dataset of geometries for training. |
| Gaussian Process (GP) Regressor | Software/Algorithm | A lightweight machine learning model used as a surrogate for expensive simulations; provides fast predictions with uncertainty estimates [11]. | Used after an LGM to map latent geometric vectors to performance metrics. |
The journey toward a credible computational model in neurostimulation is a structured integration of precise geometry and robust physics. As evidenced by the comparative data, there is no single best approach; rather, the choice depends on the specific research question, balancing fidelity with computational feasibility. Traditional FEM-based biophysical models remain the gold standard for mechanistic insight and patient-specific prediction, while emerging AI-driven methods like LGMs and surrogate models offer transformative potential for rapid exploration and optimization of neurostimulation therapies. Ultimately, rigorous validation against experimental and clinical data is the non-negotiable final step that confers credibility, transforming a complex simulation into a trusted tool for scientific discovery and clinical innovation.
In computational neurostimulation, the transition from theoretical models to effective clinical protocols is fraught with uncertainties that stem directly from unvalidated assumptions. Model validation provides the critical framework for testing these assumptions, ensuring that computational predictions translate to reliable, effective neuromodulation treatments. Without rigorous validation, even the most sophisticated models risk being guided by unverified premises, leading to variable patient outcomes and failed clinical translations [14] [15].
The field of neurostimulation is experiencing rapid growth, with the global market for neurostimulation devices projected to reach USD 23.24 billion by 2034, expanding at a CAGR of 12.84% [16]. This growth is paralleled by an increasing recognition of neural variability not as noise to be minimized, but as a fundamental functional feature that must be accounted for in personalized stimulation protocols [17]. This shift necessitates advanced validation approaches that can address both inter-individual and intra-individual variability in response to non-invasive brain stimulation (NIBS).
This guide examines the core methodologies for addressing model uncertainties in neurostimulation research, providing a structured comparison of validation techniques, experimental protocols, and computational tools essential for developing reliable, clinically translatable neuromodulation interventions.
Theoretical Foundation: From Neural Variability to Personalized Protocols
The Probabilistic Framework for Neurostimulation
Traditional neurostimulation approaches often employed a "one-size-fits-all" methodology, which ignored fundamental biological variations between individuals. Contemporary research demonstrates that neural variability serves as a core functional property that underpins brain flexibility and adaptability [17]. This variability manifests across multiple dimensions:
- Inter-individual variability: Structural and functional brain differences between subjects
- Intra-individual variability: Fluctuating brain states within the same individual
- State-dependent plasticity: Variation in response to stimulation based on current neural activity
A probabilistic framework for personalization incorporates this variability through detailed brain activity recordings and advanced analytical techniques, optimizing non-invasive brain stimulation (NIBS) protocols for individual brain states [17]. This approach represents a paradigm shift from minimizing neural variability to strategically leveraging it for improved treatment outcomes.
The Closed-Loop Neurostimulation Paradigm
Closed-loop systems address fundamental uncertainties in neurostimulation by continuously adapting stimulation parameters based on real-time biomarkers. This approach contrasts sharply with traditional open-loop systems, where stimulation parameters remain fixed without regard to ongoing neural activity [15].
Table 1: Comparison of Open-Loop vs. Closed-Loop Neurostimulation Systems
| Feature | Open-Loop Systems | Closed-Loop Systems |
|---|---|---|
| Parameter Adjustment | Fixed based on prior empirical evidence | Dynamically adjusted based on real-time feedback |
| Brain State Consideration | No accommodation for non-stationary brain activities | Continuously monitors and responds to brain state fluctuations |
| Individualization | Limited personalization capabilities | Highly personalized through continuous optimization |
| Validation Requirements | Primarily model-based assumptions | Requires real-time biomarker validation |
| Clinical Flexibility | Rigid protocol structure | Adapts to individual patient responses |
The fundamental architecture of closed-loop systems follows a control engineering paradigm where the brain represents the "plant" whose state is constantly monitored via treatment response biomarkers [15]. These biomarkers, recorded through tools like fMRI or EEG, serve as proxies for the current brain state, which is compared against a desired state, with the difference driving the optimization of stimulation parameters through a dedicated controller.
Core Methodologies: Validation Techniques for Neurostimulation Models
Foundational Model Validation Approaches
Validation techniques provide the critical foundation for testing model assumptions and quantifying prediction uncertainties in neurostimulation research:
Holdout Validation Methods involve partitioning data into distinct subsets for training and testing models. The train-test split divides data into two parts (typically 70-80% for training, 20-30% for testing), while the train-validation-test split creates three partitions (e.g., 60% training, 20% validation, 20% testing) to avoid overfitting during parameter tuning [14]. For smaller datasets (common in neurostimulation research with limited subject pools), holdout methods may produce unstable estimates, necessitating more advanced techniques.
Cross-Validation addresses limitations of holdout methods by partitioning the dataset into multiple folds. The model is trained on combinations of these folds and tested on the remaining fold, repeating this process multiple times. This approach provides more robust performance estimates, especially valuable for detecting overfitting in complex neurostimulation models with limited data [14] [18].
Advanced Validation Frameworks for Neurostimulation
Beyond foundational methods, neurostimulation research requires specialized validation approaches:
Real-Time fMRI (rtfMRI) Validation integrates brain stimulation with simultaneous neuroimaging to establish closed-loop tES-fMRI systems for individually optimized neuromodulation. This methodology addresses the critical challenge of inter- and intra-individual variability in response to NIBS [15]. The system optimizes stimulation parameters by minimizing differences between the model of the current brain state and the desired state, with the objective of maximizing clinical outcomes.
Brain-State-Specific Validation incorporates the understanding that stimulation effects are not uniform but depend on the underlying brain state at the time of stimulation. This approach requires measuring baseline brain states and customizing stimulation protocols accordingly, moving beyond static models to dynamic, state-dependent validation frameworks [17].
Experimental Protocols: Methodologies for Addressing Key Uncertainties
Closed-Loop tES-fMRI Experimental Protocol
The integration of transcranial electrical stimulation (tES) with real-time fMRI represents a cutting-edge methodology for validating and optimizing neurostimulation protocols:
Objective: To establish a closed-loop system that individually optimizes tES parameters based on real-time fMRI biomarkers of target engagement [15].
Equipment and Setup:
- MRI-compatible tES device with real-time parameter control
- 3T MRI scanner with capability for real-time BOLD signal processing
- Biomarker detection software for continuous monitoring of target brain regions
- Closed-loop controller hardware/software for parameter optimization
Procedure:
- Baseline Assessment: Acquire 10-minute resting-state fMRI to identify individual functional connectivity patterns.
- Target Identification: Define target brain regions based on individual functional connectivity maps.
- Controller Setup: Implement optimization algorithm with predefined desired brain state.
- Stimulation Phase: Apply tES while continuously monitoring BOLD signal in target regions.
- Parameter Adjustment: Dynamically adjust stimulation intensity (0.5-2.0 mA) and location based on error signal between current and desired brain state.
- Iteration: Repeat steps 4-5 until predefined error threshold is reached or maximum iteration count is completed.
- Outcome Assessment: Evaluate both neural target engagement and behavioral/cognitive outcomes.
Validation Metrics: Target engagement magnitude, stability of maintained brain state, behavioral correlation with target engagement, and comparison to open-loop stimulation [15].
Probabilistic Personalization Protocol for NIBS
This protocol addresses individual variability by incorporating probabilistic frameworks into neurostimulation personalization:
Objective: To develop personalized NIBS protocols that account for inter-individual and intra-individual variability through probabilistic modeling [17].
Equipment and Setup:
- High-density EEG or fMRI equipment for brain state recording
- NIBS device (TMS, tDCS, or tACS) with neuronavigation capability
- Advanced analytical software for variability indices calculation
- Machine learning algorithms for probabilistic model training
Procedure:
- Multi-Modal Assessment: Collect structural MRI, functional connectivity (resting-state fMRI), and neurophysiological measurements (TMS-evoked potentials).
- Variability Quantification: Calculate neural variability indices through repeated measurements across multiple sessions.
- Model Training: Develop probabilistic models linking individual neural features to stimulation outcomes using machine learning.
- Protocol Optimization: Customize stimulation parameters (location, intensity, timing) based on individual probabilistic predictions.
- Validation: Test model predictions against actual outcomes in iterative refinement cycles.
- Longitudinal Tracking: Monitor changes in neural variability and adjust protocols accordingly.
Validation Metrics: Precision of outcome predictions, reduction in inter-individual response variability, stability of effects across sessions, and generalizability across clinical populations [17].
Computational Tools: The Research Toolkit for Model Validation
Essential Research Reagent Solutions
Table 2: Essential Research Toolkit for Neurostimulation Model Validation
| Tool/Category | Specific Examples | Function in Validation | Considerations |
|---|---|---|---|
| Neurostimulation Devices | Clinical-grade tDCS (Activadose), TMS with neuronavigation | Deliver precisely controlled stimulation for testing model predictions | Ensure compatibility with imaging equipment; verify precision of targeting |
| Neuroimaging Systems | Real-time fMRI, high-density EEG, fNIRS | Provide biomarkers for target engagement and treatment response | Balance spatial vs. temporal resolution based on validation objectives |
| Computational Modeling Platforms | Finite element head models, neural mass models | Simulate electric field distributions and neural population dynamics | Incorporate individual anatomical data; validate against empirical measurements |
| Closed-Loop Control Systems | Custom MATLAB/Python toolboxes, specialized neurotechnology | Enable real-time adjustment of stimulation parameters | Optimize latency for effective closed-loop intervention; ensure robust signal processing |
| Data Analysis Frameworks | Machine learning libraries, statistical packages | Identify patterns, build predictive models, quantify uncertainties | Address multiple comparison problems; implement appropriate cross-validation |
Emerging Technologies in Validation Research
Brain-Computer Interfaces (BCIs) are advancing beyond motor restoration to include emotional regulation and cognitive enhancement, providing new avenues for validating neurostimulation models. Recent developments include Neuralink's human implants that enable thought-controlled external devices, representing sophisticated platforms for closed-loop validation [16].
AI-Powered Diagnostic Tools leverage machine learning to analyze vast amounts of patient data, offering personalized treatment recommendations and creating new validation paradigms through predictive modeling of stimulation outcomes [16] [19].
Comparative Analysis: Validation Outcomes Across Modalities
Quantitative Comparison of Validation Approaches
Table 3: Performance Comparison of Neurostimulation Validation Methods
| Validation Method | Individualization Capacity | Implementation Complexity | Evidence Strength | Clinical Translation Potential |
|---|---|---|---|---|
| One-Size-Fits-All | Low | Low | Limited, highly variable outcomes | Poor, declining acceptance |
| Holdout Validation | Medium | Low to Medium | Moderate, dependent on dataset size | Moderate for large datasets |
| Cross-Validation | Medium to High | Medium | Strong, robust performance estimates | Good for protocol optimization |
| Closed-Loop rtfMRI | High | High | Emerging, highly promising | Excellent, though resource-intensive |
| Probabilistic Framework | High | High | Theoretical support, growing empirical | Excellent long-term potential |
Impact of Proper Validation on Clinical Outcomes
The critical importance of addressing model uncertainties through rigorous validation is demonstrated by comparative clinical outcomes:
Treatment-Resistant Depression: The Stanford neuromodulation therapy (SNT) paradigm utilizing individualized functional connectivity-guided targeting through resting-state fMRI demonstrated significantly improved outcomes compared to sham stimulation [15]. This approach highlights how validating the assumption that individual connectivity differences matter can dramatically impact clinical efficacy.
Chronic Pain Management: Spinal cord stimulation systems employing validated closed-loop approaches provide more consistent therapeutic effects compared to open-loop systems. Abbott's BurstDR technology demonstrated sustained relief for chronic back and leg pain, with 91% of patients preferring it over traditional methods after long-term use [19].
Parkinson's Disease: Medtronic's BrainSense Adaptive deep brain stimulation system, which received CE mark approval in 2025, uses sensing-enabled technology to provide personalized, closed-loop stimulation, representing a significant advancement over static stimulation paradigms [19].
Visualizing Workflows: Signaling Pathways and Experimental Frameworks
Closed-Loop Neurostimulation Workflow
Figure 1: Closed-Loop Neurostimulation Control Framework
Model Validation Methodology Decision Pathway
Figure 2: Model Validation Methodology Selection
The progression from unvalidated assumptions to rigorously tested computational models represents the critical path toward effective, reliable neurostimulation therapies. The evidence clearly demonstrates that models acknowledging and incorporating neural variability through probabilistic frameworks and closed-loop validation outperform traditional one-size-fits-all approaches [17] [15]. As the neurostimulation device market advances toward USD 23.24 billion by 2034 [16], the value of comprehensive model validation will only increase, particularly with emerging technologies like brain-computer interfaces and AI-powered diagnostics creating new opportunities for personalized neuromodulation.
The future of neurostimulation research lies in developing increasingly sophisticated validation frameworks that can address the multifaceted uncertainties inherent in computational models of brain function and stimulation effects. By implementing the comprehensive validation methodologies outlined in this guide—from basic holdout techniques to advanced closed-loop systems—researchers can systematically address model uncertainties, leading to more predictable outcomes and successful translations from computational models to clinical applications that reliably improve patient lives.
The Critical Role of Validation in Bridging In-Silico Findings and Real-World Outcomes
In silico methods, comprising biological experiments and trials carried out entirely via computer simulation, represent a transformative approach across biomedical research and development [20]. These computational techniques span from molecular modeling and whole-cell simulations to sophisticated virtual patient trials for medical devices and neurostimulation therapies [20] [21]. As these methods generate increasingly complex predictions, the critical challenge lies in establishing robust validation frameworks that ensure computational findings reliably translate to real-world biological and clinical outcomes. Without rigorous validation, in silico predictions remain theoretical exercises rather than trustworthy evidence for decision-making.
The validation imperative is particularly acute in neurostimulation research, where computational models simulate interactions between medical devices and the human nervous system [22]. These simulations aim to predict everything from cellular responses to treatment efficacy across diverse patient populations. Bridging this gap from digital prediction to physical reality demands meticulous validation protocols that verify models against experimental and clinical data, quantify uncertainties, and establish credibility for specific contexts of use [21]. This article examines the methodologies, standards, and evidence frameworks essential for transforming in silico models from intriguing hypotheses into validated tools for scientific discovery and clinical application.
Validation Frameworks and Regulatory Standards
Credibility Assessment Frameworks
Regulatory agencies have established structured approaches for assessing computational model credibility. The FDA's Credibility Assessment Framework provides guidance for evaluating models based on risk categorization—whether the computational model presents low, moderate, or high risk to regulatory decision-making [21]. This framework aligns with the ASME V&V 40 standard, which offers a structured approach to verification and validation of computational models used in medical applications [21]. These guidelines emphasize that model credibility depends not on universal validity but on sufficiency for the specific context of use, requiring researchers to define the model's intended purpose explicitly before establishing validation requirements.
The three-pillar model assessment framework endorsed by regulatory agencies encompasses model verification, validation, and uncertainty quantification [21]. Verification ensures that computational models correctly implement their intended mathematical representations through code verification, mesh convergence studies, and numerical accuracy assessments. Validation demonstrates accurate representation of real-world phenomena through comparison with experimental data, clinical outcome correlation, and sensitivity analysis across parameter ranges. Uncertainty quantification involves managing model parameter uncertainty from variability in material properties, model structure uncertainty from mathematical limitations, and numerical uncertainty from computational approximations.
Application in Medical Device Development
For medical device development, the Medical Device Development Tools (MDDT) program has created a pathway for qualifying computational models as regulatory-grade tools that multiple sponsors can use [21]. This program facilitates the acceptance of in silico evidence in regulatory submissions, as demonstrated by the VICTRE breast imaging simulation study, which the FDA accepted as evidence supporting imaging device performance, effectively replacing a traditional clinical study [21]. The emergence of such qualified virtual clinical trials represents a significant milestone in regulatory acceptance of in silico methods.
The International Medical Device Regulators Forum (IMDRF) continues working toward global harmonization of these approaches, though acceptance remains inconsistent across regulatory bodies [21]. While the FDA has made significant strides in accepting computational evidence, the EU MDR and EMA have not fully caught up to this level of acceptance, creating regulatory complexity for global device manufacturers. This evolving landscape underscores the importance of early regulatory engagement through Q-Sub meetings to establish the acceptability of proposed computational approaches, required validation evidence, and strategies for integrating with traditional testing methods [21].
Experimental Protocols for Model Validation
Multi-Scale Validation in Neurostimulation
Validation of neurostimulation models requires a multi-scale approach spanning from cellular responses to clinical outcomes. The following workflow illustrates a comprehensive validation framework for computational models in neurostimulation research:
Diagram 1: Model validation workflow
The validation workflow begins with computational model development, proceeds through verification and multiple validation stages, and culminates in regulatory-grade evidence generation. This systematic approach ensures models produce reliable predictions across biological scales.
Advanced research platforms enable rigorous validation through cloud-based workflows. For instance, the o²S²PARC and Sim4Life platforms allow researchers to create, execute, and automate computational pipelines that couple high-fidelity electromagnetic exposure modeling with neuronal dynamics [22]. These platforms facilitate validation through direct comparison between simulated neurostimulation effects and experimental measurements across spatial scales—from single-cell responses to brain network dynamics. Validation protocols typically include electromagnetic-neuro interactions across spatio-temporal scales covering the brain, spine, and peripheral nervous system [22].
Clinical Outcome Validation
For neurostimulation devices targeting chronic pain, validation against comprehensive clinical outcomes is essential. The Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) criteria recommend a multidimensional assessment of chronic pain outcomes beyond simple pain intensity scores [23]. These criteria specify six core outcome domains that should be consistently reported: (1) pain intensity, (2) physical function, (3) emotional function, (4) participant ratings of improvement or satisfaction with treatment, (5) adverse events, and (6) participant disposition [23].
A systematic review of randomized clinical trials on neurostimulation for chronic pain revealed substantial variability in adherence to these complete outcome measures, with universal reporting of pain intensity but inconsistent assessment of other domains like emotional function and physical functioning [23]. This validation gap highlights the need for more comprehensive outcome reporting when validating computational models against clinical data. Models predicting neurostimulation efficacy should ideally output metrics across all IMMPACT domains to enable thorough validation against clinical trial results.
Comparative Analysis of Validation Methods
Cross-Technique Validation Approaches
Each validation approach offers distinct strengths and limitations for bridging in silico findings with real-world outcomes. The table below summarizes the primary validation methodologies employed across computational life sciences:
Table 1: Comparison of Validation Methods for In Silico Findings
| Validation Method | Key Applications | Strengths | Limitations |
|---|---|---|---|
| In Vitro Experimental Correlation [24] | Enzyme function studies; Cellular response prediction | Controlled conditions; Direct mechanistic insight; High-throughput capability | May not capture full biological complexity; Limited physiological context |
| In Vivo Experimental Correlation [20] | Whole-organism response; Systemic effects | Full physiological context; Clinical relevance | Ethical considerations; High cost; Complex interpretation |
| Retrospective Clinical Analysis [25] | Drug repurposing; Treatment outcome prediction | Real-world human data; Large sample potential | Confounding factors; Data quality variability |
| Literature Validation [25] | Hypothesis generation; Model benchmarking | Broad knowledge base; Rapid implementation | Inconsistent data quality; Reporting biases |
| Prospective Clinical Trial Correlation [23] | Medical device efficacy; Therapeutic optimization | Gold standard evidence; Controlled conditions | Resource intensive; Ethical considerations; Time constraints |
Validation in Drug Discovery and Development
In computational drug discovery and repurposing, validation strategies typically follow a structured pipeline. The rigorous drug repurposing pipeline involves making connections between existing drugs and diseases needing treatments based on features collected via biological experiments or clinical data [25]. After hypothesis generation through computational prediction, validation employs independent information not used in the prediction step, such as previous experimental/clinical studies or independent data resources about the drug-disease connection [25].
Studies with strong validation provide multiple forms of supporting evidence, often combining computational methods (retrospective clinical analysis, literature support, public database search) with non-computational methods (in vitro, in vivo experiments, clinical trials) [25]. This multi-modal validation approach reduces false positives and builds confidence in repurposed drug candidates. For example, a comprehensive review of computational drug repurposing found that only 129 out of 732 studies included both computational and experimental validation methods, highlighting the validation gap in current practice [25].
Case Studies: Validation Successes and Gaps
Medical Device Innovation
In silico trials have demonstrated particular success in medical device innovation, where computational models simulate device performance within virtual anatomical environments. Cardiovascular device developers now routinely use computational fluid dynamics models to simulate blood flow patterns around stents, predicting areas where restenosis might occur and optimizing strut geometry accordingly [21]. These simulations undergo rigorous validation through comparison with benchtop testing and clinical outcomes, creating validated predictive tools that can reduce the need for extensive physical prototyping.
In transcatheter aortic valve replacement, virtual testing helps predict paravalvular leak and optimal sizing across diverse patient anatomies [21]. Rather than relying solely on limited bench testing or small pilot studies, manufacturers can explore thousands of anatomical variations digitally, with validation against clinical performance data ensuring predictive accuracy. This approach enables both device optimization and personalized patient selection, with validation studies demonstrating improved clinical outcomes compared to traditional methods.
Limitations in Predictive Accuracy
Despite advances, significant validation gaps persist. A striking example comes from a study comparing in silico predictions with in vitro enzymatic assays for galactose-1-phosphate uridylyltransferase (GALT) variants [24]. The research revealed significant discrepancies between computational predictions and experimentally measured enzyme activity. While in vitro assays showed statistically significant decreases in enzymatic activity for all tested variants of uncertain significance compared to native GALT, molecular dynamics simulations showed no significant differences in root-mean-square deviation data [24]. Furthermore, predictive programs like PredictSNP, EVE, ConSurf, and SIFT produced mixed results that were inconsistent with enzyme activity measurements [24].
This validation study highlights that even sophisticated in silico tools may not reliably predict biological function, particularly for missense mutations affecting protein activity. The authors concluded that the in silico tools used "may not be beneficial in determining the pathogenicity of GALT VUS" despite their widespread use for this purpose [24]. Such validation gaps emphasize the continued importance of experimental confirmation for computational predictions, especially in clinical decision-making contexts.
Research Reagent Solutions
Implementing robust validation protocols requires specialized computational and experimental resources. The table below outlines key research reagent solutions essential for validating in silico findings in neurostimulation and computational life science research:
Table 2: Essential Research Reagent Solutions for Model Validation
| Tool/Resource | Primary Function | Validation Application | Key Features |
|---|---|---|---|
| o²S²PARC Platform [22] | Cloud-native computational pipeline development | Build, share, reproduce complex modeling workflows from MRI to neuronal dynamics | Browser-based access; Pre-built computational workflows; High-fidelity EM modeling |
| Sim4Life [22] | Image-based, regulatory-grade simulations | Create anatomically detailed human body models with embedded nerve and brain networks | Multi-scale modeling; Coupled physical phenomena; Automated compliance checking |
| Modelscape Validate [26] | Model validation workflow management | Document validation protocols; Ensure traceability and reproducibility | Customizable templates; Automated documentation; Integration with development workflows |
| ASME V&V 40 Standard [21] | Credibility assessment framework | Structured approach to verification and validation for medical applications | Risk-informed validation planning; Context-of-use evaluation; Uncertainty quantification |
| IMMPACT Criteria [23] | Clinical outcome assessment | Multidimensional pain outcome measurement for neurostimulation trials | Six core domains; Patient-centered metrics; Regulatory recognition |
Validation Workflow Implementation
The following diagram illustrates the implementation of a comprehensive validation strategy integrating computational and experimental approaches:
Diagram 2: Integrated validation strategy
This integrated validation approach ensures computational models undergo rigorous testing across multiple evidence domains, strengthening the bridge between in silico predictions and real-world outcomes.
The critical role of validation in bridging in silico findings with real-world outcomes continues to evolve alongside computational methodologies. While significant progress has been made in establishing validation frameworks and regulatory pathways, the persistent gaps between computational predictions and experimental measurements highlight the need for continued validation science development. The integration of artificial intelligence with traditional physics-based models opens new possibilities through surrogate modeling, optimal configuration identification, and performance forecasting across diverse patient populations [21].
The future of computational life sciences undoubtedly includes expanded use of in silico methods, but their impact will be determined by the rigor of their validation. As regulatory agencies increasingly accept computational evidence, the establishment of model qualification databases as shared repositories of validated computational models will be essential [21]. By advancing validation science across multiple evidence domains—from molecular simulations to clinical outcomes—researchers can fully realize the potential of in silico methods to accelerate discovery, reduce costs, and improve patient outcomes across neurostimulation and biomedical research.
From Theory to Practice: Workflows for Building and Applying Validated Models
Validation is a critical component of research and development, ensuring that methodologies produce reliable, reproducible, and clinically meaningful results. This guide examines and compares the validation workflows from two distinct neurostimulation domains: Deep Brain Stimulation (DBS) for neuropsychiatric disorders and Transcranial Electrical Stimulation (tES) for non-invasive brain modulation. While DBS involves invasive surgical implantation with intensive long-term clinical monitoring, tES utilizes non-invasive techniques requiring precise parameter reporting. By analyzing their structured approaches to equipment qualification, parameter control, and outcome validation, researchers can extract valuable frameworks applicable to computational model validation in neurostimulation research. The protocols from these fields demonstrate how rigorous, step-by-step validation processes bridge the gap between theoretical models and clinical applications, ultimately supporting the development of safer and more effective neurostimulation therapies [27] [28] [29].
Experimental Protocols and Methodologies
Deep Brain Stimulation (DBS) for Neuropsychiatric Disorders
DBS clinical trials for conditions like treatment-refractory major depressive disorder require multi-year relationships between participants and study staff, involving frequent interactions and high participant burden. The validation protocol emphasizes patient safety, ethical considerations, and methodological rigor throughout the therapeutic intervention [27].
Key Methodological Components:
- Multidisciplinary Team Structure: Trials are conducted by experienced multidisciplinary teams mandatory for ethical research, including stereotactic and functional neurosurgery, psychiatry, neurology, neuropsychology, neuroethics, clinical research coordinators, and neural signal processing experts [27].
- Stimulation Protocol: DBS involves surgical implantation of electrodes and an implantable pulse generator delivering therapeutic stimulation to targeted brain regions. Programming adjustments typically occur 3-11 times within the first six months post-surgery, with more frequent visits in research settings [27].
- Trial Design Considerations: Due to ethical constraints against sham surgeries, randomized controlled trials often use within-participant crossover designs (AB/BA) where each participant receives both active and sham stimulation. Protocols include explicit criteria for prematurely exiting sham conditions due to patient decompensation [27].
Table: DBS Clinical Trial Activities and Frequency
| Activity Type | Frequency | Purpose |
|---|---|---|
| Clinical assessments | Weekly to monthly | Monitor psychiatric symptoms and side effects |
| DBS programming sessions | 3-11 times in first 6 months | Optimize stimulation parameters |
| Neuropsychological testing | Every 3-6 months | Assess cognitive changes |
| Neuroimaging (MRI/fMRI) | Pre-op and annually | Verify lead placement and brain changes |
| Adverse event monitoring | Continuous | Ensure participant safety |
Transcranial Electrical Stimulation (tES) Reporting Standards
The Report Approval for Transcranial Electrical Stimulation (RATES) checklist was developed through a Delphi consensus process involving 38 international experts across three rounds. This initiative identified 66 essential items categorized into five groups, with 26 deemed critical for reporting [28].
Development Methodology:
- Delphi Process: The three-round Delphi technique used interquartile deviation (>1.00), percentage of positive responses (>60%), and mean importance ratings (<3) to assess consensus and importance for each item [28].
- Systematic Review Foundation: A separate CoRE-tES initiative (Consolidated Guidelines for Reporting and Evaluation of studies using tES) begins with a systematic review of recent tES literature to assess methodological and reporting quality, informing preliminary checklist items [29].
Critical Reporting Domains: The RATES checklist categorizes essential reporting items into five domains: participants (12 items), stimulation device (9 items), electrodes (12 items), current (12 items), and procedure (25 items). Even slight variations in these parameters can notably change stimulation effects, including reversal of intended outcomes [28].
Comparative Analysis of Validation Approaches
Quantitative Data Comparison
Table: Performance Metrics Comparison Across Validation Types
| Validation Aspect | DBS Clinical Validation | tES Technical Validation | Pharmaceutical Equipment Validation |
|---|---|---|---|
| Timeframe | Months to years | Single sessions to weeks | Days to weeks |
| Primary Success Metrics | Clinical symptom reduction, functional improvement | Effect size, reproducibility | Accuracy, precision, repeatability |
| Parameter Controls | Electrode location, stimulation parameters | Electrode montage, current intensity, duration | Calibration, operational parameters |
| Acceptance Criteria | Statistical vs. clinical significance | Statistical significance, adherence to protocol | Predetermined acceptance criteria vs. URS |
| Key Challenges | Participant retention, placebo effects | Heterogeneity, blinding integrity | Impact assessment, avoiding over-qualification |
Workflow Visualization
DBS and tES Validation Workflows: This diagram illustrates the parallel yet distinct validation pathways for Deep Brain Stimulation (DBS) and Transcranial Electrical Stimulation (tES) protocols, highlighting their unique methodological approaches while demonstrating convergent validation objectives.
Essential Research Toolkit
Table: Research Reagent Solutions for Neurostimulation Validation
| Item/Category | Function in Validation | Specific Examples |
|---|---|---|
| DBS Electrodes | Deliver targeted stimulation to deep brain structures | Directional DBS leads with multiple contacts |
| tES Devices | Generate controlled electrical currents for transcranial stimulation | tDCS, tACS, and tRNS stimulators with precision current control |
| Electrode Materials | Interface between device and biological tissue | Ag/AgCl electrodes, conductive gels for tES; Platinum-iridium for DBS |
| Computational Modeling Platforms | Simulate neurostimulation effects and optimize parameters | Closed-loop cardiovascular-neural models, electric field models |
| Clinical Assessment Tools | Quantify therapeutic outcomes and side effects | Standardized depression scales (MADRS, HAM-D), cognitive batteries |
| Neuroimaging | Verify placement and monitor neural effects | MRI for DBS lead localization, fMRI for network effects |
| Data Collection & Monitoring | Ensure protocol adherence and data integrity | Electronic clinical outcome assessments, remote symptom monitoring |
Discussion: Implications for Computational Model Validation
The validation workflows from DBS and tES protocols offer complementary frameworks for computational model validation in neurostimulation research. DBS emphasizes clinical integration and adaptive long-term validation, while tES focuses on parameter standardization and reporting transparency. Together, they provide a robust foundation for developing computational approaches that are both clinically relevant and methodologically rigorous [27] [28].
Recent advances in computational modeling, such as the closed-loop human cardiac-baroreflex system for optimizing neurostimulation therapy for atrial fibrillation, demonstrate how biological system simulations can predict intervention outcomes before clinical implementation. This model successfully identified the atrioventricular node as a promising neurostimulation target, showcasing how computational approaches can generate testable clinical hypotheses [13].
For researchers developing computational models for neurostimulation, integrating both DBS and tES validation principles creates a comprehensive framework:
- Structured Parameter Reporting adapted from RATES checklist ensures model inputs and assumptions are transparent and reproducible [28].
- Clinical Outcome Alignment from DBS protocols grounds models in patient-relevant endpoints rather than theoretical constructs [27].
- Iterative Validation Cycles mirroring DBS parameter optimization processes enable continuous model refinement based on emerging data [27] [13].
- Multidisciplinary Integration essential to both protocols ensures models incorporate diverse expertise from engineering, clinical medicine, and basic science [27] [13].
The step-by-step validation workflows from DBS and tES protocols provide invaluable roadmaps for establishing robust methodological standards in computational neurostimulation research. DBS protocols demonstrate the critical importance of long-term clinical integration, multidisciplinary teams, and adaptive parameter optimization, while tES standardization efforts highlight the necessity of comprehensive parameter reporting and consensus-driven methodological guidelines. By synthesizing the strengths of both approaches—clinical relevance from DBS and methodological transparency from tES—researchers can develop computational models and validation frameworks that accelerate the development of safer, more effective, and personalized neurostimulation therapies. As computational approaches increasingly inform clinical device development, these integrated validation principles will be essential for bridging the gap between theoretical models and real-world therapeutic applications.
The validation of computational models for neurostimulation protocols presents a significant challenge in modern neuroscience. The efficacy of such models hinges on their ability to predict neurological and behavioral outcomes accurately, a task that requires integrating diverse, high-dimensional data types. This guide objectively compares the performance of primary neuroimaging and biosensing modalities—Magnetic Resonance Imaging (MRI), Electrochemical Impedance Spectroscopy (EIS), and behavioral assessment—within the specific context of model validation. Individually, these techniques provide valuable but incomplete insights; functional connectivity (FC) derived from fMRI has emerged as a robust feature for predicting behaviors like cognition and age [30], while EIS offers a powerful, label-free method for detecting biochemical biomarkers [31] [32]. However, their integration offers a more comprehensive validation framework. We summarize experimental data into structured tables, detail key methodologies, and diagram workflows to provide researchers with a clear comparison of how these modalities can be synergistically combined to enhance the precision and reliability of neurostimulation models.
Performance Comparison of Multimodal Data
Table 1: Comparison of Primary Modalities for Model Validation
| Modality | Key Measured Features | Spatial Resolution | Temporal Resolution | Primary Data Output | Performance in Behavior Prediction |
|---|---|---|---|---|---|
| Functional MRI (fMRI) | Functional Connectivity (FC), Graph Power Spectral Density, Regional Activity [30] | High (mm) | Moderate (seconds) | Brain network maps and time-series data [30] [33] | FC is best for predicting cognition, age, and sex; Graph power spectral density is second best for cognition and age [30]. |
| Electrochemical Impedance Spectroscopy (EIS) | Biomarker-receptor interaction (e.g., proteins, hormones) on electrode surface [31] [32] | N/A (Bulk measurement) | High (milliseconds to seconds) | Nyquist/Bode plots providing equivalent circuit parameters [32] [34] | Detects biomarkers for ocular/systemic diseases (e.g., Alzheimer's, cancer); high sensitivity for target analytes [31]. |
| Behavioral Outcomes | Cognitive scores, mental health summaries, processing speed, substance use [30] | N/A | Continuous to discrete | Quantitative scores and categorical classifications [30] | Serves as the ground-truth target for predictive modeling from neuroimaging and biomarker data [30] [35]. |
Table 2: Scaling Properties and Integration Potential
| Modality | Scaling with Sample Size | Scaling with Acquisition Time | Key Integration Challenge | Complementary Role in Validation |
|---|---|---|---|---|
| fMRI | Performance reserves for better-performing features (e.g., FC) in larger datasets [30]. | Important to balance scan time and sample size; longer times can improve signal [30]. | High dimensionality of data (e.g., 37,401 features from FC) requires robust machine learning [30]. | Provides macroscale network dynamics and correlates of consciousness and behavior [30] [33]. |
| EIS | Enables high-throughput, point-of-care screening when integrated into portable biosensors [31] [32]. | Provides rapid, real-time measurements on living systems with wearable technology [31]. | Translating biomarker concentration from tear fluid to functional brain state [31]. | Offers molecular-level, personalized biomarker data that can ground models in physiological states [31]. |
| Behavioral Outcomes | Larger samples improve statistical power and model generalizability [30] [35]. | Longitudinal assessment captures dynamic adaptations and long-term effects. | Subjectivity of some measures (e.g., pain ratings) requires objective correlates [8]. | Serves as the ultimate endpoint for validating the functional output of neurostimulation [8] [35]. |
Experimental Protocols for Key Methodologies
Protocol 1: Predicting Behavior from fMRI Features
This protocol is adapted from a large-scale study comparing fMRI features for brain-behavior prediction [30].
- Dataset & Preprocessing: The study utilized 979 subjects from the Human Connectome Project (HCP) Young Adult dataset. Structural T1 images were processed with Connectomemapper3 and parcellated using the Lausanne 2018 atlas (274 regions). Functional images were minimally preprocessed, followed by confound regression (motion parameters and derivatives), detrending, and high-pass filtering at 0.01 Hz. Time series were parcellated by averaging voxel signals within each atlas parcel [30].
- Feature Extraction: Nine feature subtypes were extracted from the preprocessed fMRI data. These included:
- Functional Connectivity (FC): The Pearson correlation coefficient between the time series of every pair of brain regions was calculated. The upper triangle of the resulting FC matrix was vectorized, yielding 37,401 features per subject [30].
- Region-wise features: Measures such as the mean and standard deviation of the BOLD signal, mean square successive difference (MSSD) for BOLD variability, and the fractional amplitude of low-frequency fluctuations (fALFF) [30].
- Graph Signal Processing (GSP) features: Metrics derived using the brain's structural connectivity, including the graph power spectral density and the structural decoupling index (SDI) [30].
- Prediction & Scaling Analysis: Behavioral targets (cognition, mental health, processing speed, substance use, age, and sex) were predicted from the features using machine learning models. The study systematically investigated how prediction performance scaled with different combinations of sample size and scan time [30].
Protocol 2: Impedimetric Detection of Biomarkers via EIS
This protocol outlines the use of EIS for detecting disease biomarkers, relevant for correlating physiological states with neurostimulation outcomes [31] [32].
- Biorecognition Element Immobilization: A biosensor is constructed by immobilizing a specific biorecognition element (e.g., an antibody, enzyme, or nucleic acid) onto the surface of a working electrode. This element is chosen for its selective interaction with the target biomarker [31] [32].
- Sample Collection and Application: In the context of neurological research, tear fluid is a promising source of biomarkers. It can be collected non-invasively using a glass microcapillary tube placed at the inferior temporal tear meniscus, minimizing stimulation of reflex tears. The collected sample is then applied to the biosensor surface [31].
- Impedance Measurement: An alternating current (AC) voltage signal, typically with a small amplitude (e.g., 5-10 mV), is applied across a range of frequencies (e.g., from 0.1 Hz to 100 kHz). The resulting current is measured, and the complex impedance (Z), comprising magnitude and phase shift, is calculated for each frequency [32] [34].
- Data Analysis & Equivalent Circuit Modelling: The impedance data is plotted on a Nyquist plot. An appropriate equivalent electrical circuit model (e.g., the Randles circuit) is fitted to the data. The change in a key parameter like the charge transfer resistance (Rct) before and after biomarker binding is used as the quantitative signal for biomarker detection [32] [34].
Protocol 3: Quantifying Consciousness State with Integration-Segregation Difference
This protocol uses fMRI to calculate a metric that can validate neurostimulation effects on brain state [33].
- Data Acquisition and Preprocessing: Subjects are scanned under different conditions (e.g., awake vs. anesthetized) using resting-state fMRI. Standard preprocessing steps are applied, including head motion correction, normalization, and band-pass filtering [33].
- Dynamic Functional Connectivity: The preprocessed fMRI time series is divided into sliding windows. For each window, a functional connectivity matrix is calculated, often using Pearson correlation between regional time series [33].
- Graph Theory Metrics: For each connectivity matrix, two key graph theory metrics are computed:
- Integration (Multi-level Efficiency): Measures how readily information can be exchanged across the entire brain network.
- Segregation (Multi-level Clustering Coefficient): Measures the degree to which brain nodes form tightly interconnected groups or modules [33].
- Calculate Integration-Segregation Difference (ISD): The ISD metric is computed for each time window as follows: ISD = Integration - Segregation. This metric has been shown to reliably index states of consciousness, with higher negative values indicating a more segregated (less conscious) state [33].
Workflow Visualization for Data Integration
The following diagrams illustrate the logical relationships and workflows for integrating multimodal data to validate computational models of neurostimulation.
Diagram 1: Multimodal validation workflow.
Diagram 2: fMRI brain state calculation.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials for Featured Experiments
| Item | Function/Description | Example Application |
|---|---|---|
| High-Density MRI Atlas (e.g., Lausanne 2018) | Provides a parcellation scheme to divide the brain into distinct regions for time-series extraction and network analysis [30]. | Standardizing feature extraction from fMRI data across subjects for brain-behavior prediction studies [30]. |
| Graph Signal Processing (GSP) Toolkit | A principled computational approach for extracting structure-informed functional features from neuroimaging data using the underlying structural connectivity network [30]. | Generating novel fMRI features beyond standard FC to predict behavioral variables like cognition [30]. |
| Electrochemical Biosensor with Biorecognition Element | The core of an EIS setup. The electrode is functionalized with a receptor (e.g., antibody) that selectively binds the target biomarker, transducing a biochemical event into a measurable electrical signal [31] [32]. | Label-free detection of disease-specific proteins (e.g., tau for Alzheimer's) in biofluids like tear fluid [31]. |
| Equivalent Circuit Model (e.g., Randles Circuit) | A theoretical electrical circuit used to model the electrochemical processes at the electrode-electrolyte interface. Fitting this model to EIS data allows quantification of biomarker binding [32] [34]. | Quantifying the change in charge transfer resistance (Rct) to determine the concentration of a target biomarker [32]. |
| Non-Invasive Biofluid Collector (e.g., Microcapillary Tube) | Enables the collection of biomarker-rich biofluids like tears with minimal stimulation or damage to the ocular surface, preserving sample integrity [31]. | Gathering tear fluid samples for the analysis of systemic disease biomarkers in conjunction with neurological assessments [31]. |
Leveraging AI and Bayesian Optimization for Personalized Protocol Tuning
The development of effective neurostimulation protocols and drug therapies is often hampered by significant individual variability in treatment response. Personalized protocol tuning aims to overcome this by tailoring interventions to individual patient characteristics, thereby optimizing therapeutic outcomes. Within this paradigm, Bayesian Optimization (BO) has emerged as a powerful artificial intelligence (AI) framework for efficiently navigating complex parameter spaces. This guide provides an objective comparison of BO-based personalization strategies against standard alternatives, focusing on their application in computational model validation for neurostimulation and drug development. The performance data, drawn from recent research, demonstrates how these methods are advancing personalized medicine.
Performance Comparison of Personalization Strategies
The following tables summarize experimental data comparing the performance of Bayesian Optimization and other AI-driven methods against standard non-personalized and alternative personalized approaches across key applications.
Table 1: Performance in Neurostimulation Personalization
| Application | Method | Key Performance Metric | Result | Source |
|---|---|---|---|---|
| Sustained Attention Augmentation (tRNS) | Personalized BO (pBO) | Improvement in attention (A') for low baseline performers | Significantly outperformed sham and one-size-fits-all tRNS (β = 0.76, p=0.015) | [36] |
| One-Size-Fits-All tRNS (1.5 mA) | Improvement in attention (A') for low baseline performers | No significant effect compared to sham | [36] | |
| Motor Recovery in Early Stroke (rTMS) | Bilateral rTMS (BL-rTMS) | SUCRA* for improving upper extremity motor function | 92.8% (end of intervention); 95.4% (3-month follow-up) | [37] |
| Low-Frequency rTMS (LF-rTMS) | SUCRA for improving lower extremity motor function | 67.7% | [37] | |
| Treatment-Resistant Depression (rTMS) | Accelerated iTBS (e.g., SAINT) | Remission Rates | Demonstrated high efficacy; specific protocols require more standardization | [38] |
| Standard once-daily rTMS | Remission Rates | Established efficacy, but practical limitations remain | [38] |
*SUCRA: Surface Under the Cumulative Ranking Curve (higher % indicates higher probability of being the best intervention)
Table 2: Performance in Drug Discovery and AI Model Tuning
| Application | Method | Key Performance Metric | Result | Source |
|---|---|---|---|---|
| Antibacterial Candidate Prediction | CILBO (Random Forest with BO & class imbalance handling) | ROC-AUC | 0.917 (Avg., 5-fold CV); 0.99 (Final Model) | [39] |
| Deep Learning (Graph Neural Network by Stokes et al.) | ROC-AUC | 0.896 | [39] | |
| Olanzapine Drug Concentration Prediction | LSTM-ANN with BO | RMSE (Validation Set) | 29.566 | [40] |
| Traditional PopPK Model (NONMEM) | RMSE (Validation Set) | 31.129 | [40] | |
| DRL Hyperparameter Tuning (LunarLander) | Multifidelity Bayesian Optimization | Average Total Reward | Outperformed standard BO in convergence and stability | [41] |
| Standard Bayesian Optimization | Average Total Reward | Lower average reward compared to multifidelity BO | [41] | |
| Chemical Reaction Yield Optimization | Reasoning BO (Direct Arylation) | Final Yield | 94.39% (vs. 76.60% for Vanilla BO) | [42] |
| Vanilla Bayesian Optimization | Final Yield | 76.60% | [42] |
Detailed Experimental Protocols
To ensure reproducibility and provide clear methodological insights, this section details the experimental protocols from key studies cited in the performance comparison.
Protocol: AI-Personalized Home-Based Neurostimulation
This protocol was designed to enhance sustained attention using transcranial random noise stimulation (tRNS) personalized with Bayesian Optimization [36].
- Objective: To determine if an AI-driven personalized BO (pBO) algorithm could remotely adjust neurostimulation parameters to enhance sustained attention in a home-based setting.
- Participants: Healthy adults.
- Personalization Parameters: tRNS current intensity was personalized based on individual baseline cognitive performance and head circumference.
- BO Setup: The pBO algorithm used a Gaussian Process as a surrogate model to identify an inverted U-shaped relationship between current intensity and baseline performance, finding the optimal "sweet spot" for each individual.
- Experimental Groups:
- Experiment 1: Developed the pBO algorithm.
- Experiment 2: Used in silico modeling to compare pBO against Random Search and non-personalized BO.
- Experiment 3: A double-blind, sham-controlled study comparing pBO-tRNS against one-size-fits-all tRNS (1.5 mA) and sham tRNS in a new sample.
- Outcome Measures: Primary outcome was sustained attention performance (A'—a sensitivity measure for correctly detecting a stimulus). Reaction times were also analyzed to rule out speed-accuracy trade-offs.
Protocol: Class Imbalance Learning with Bayesian Optimization (CILBO) in Drug Discovery
This protocol addresses the common challenge of imbalanced datasets in drug discovery, where active compounds are vastly outnumbered by inactive ones [39].
- Objective: To improve the prediction performance of interpretable machine learning models for antibacterial candidate discovery by handling class imbalance with BO.
- Data: The same dataset used by Stokes et al. was employed, containing 2,335 molecules with only 120 confirmed antibacterials.
- Model: A Random Forest classifier was chosen for its interpretability and resistance to overfitting.
- CILBO Pipeline: Bayesian Optimization was used not only for standard model hyperparameters but also to find the best strategy for handling class imbalance (e.g.,
class_weightandsampling_strategy). - Feature Representation: The RDK fingerprint computed by RDKit was used as the molecular feature.
- Validation: The model was evaluated using 30 repetitions of five-fold cross-validation. The final model was tested on a hold-out set and an external compound library (Drug Repurposing Hub).
Protocol: Reasoning BO for Chemical Synthesis Optimization
This protocol enhances standard BO by integrating the reasoning and knowledge-management capabilities of Large Language Models (LLMs) [42].
- Objective: To optimize a chemical reaction (Direct Arylation) yield while generating interpretable scientific hypotheses.
- Framework Components:
- Reasoning Model: An LLM integrated into the BO loop. It generates scientific hypotheses and assigns confidence scores to candidate parameters proposed by the BO's acquisition function.
- Knowledge Management: A dynamic system with knowledge graphs and vector databases stores domain rules and assimilates new experimental findings.
- Candidate Filtering: Proposed parameters are filtered based on LLM confidence and scientific plausibility before expensive experimental evaluation.
- Comparison: The performance of Reasoning BO was directly compared to Vanilla BO on the same optimization task, with yield as the primary outcome.
Workflow and Signaling Pathways
The following diagrams illustrate the core logical workflows underlying AI-driven personalized tuning, as described in the experimental protocols.
Bayesian Optimization for Protocol Personalization
Personalized Neurostimulation Protocol Development
The Scientist's Toolkit: Research Reagent Solutions
This section details key computational tools and resources essential for implementing AI and Bayesian Optimization for protocol personalization.
Table 3: Essential Tools for AI-Driven Protocol Tuning
| Tool/Resource | Type | Primary Function | Application Example |
|---|---|---|---|
| Gaussian Process (GP) | Statistical Model | Serves as a probabilistic surrogate model in BO to approximate the unknown objective function. | Modeling the relationship between neurostimulation parameters and cognitive outcomes [43] [36]. |
| Expected Improvement (EI) | Acquisition Function | Guides the BO search by quantifying the potential utility of evaluating a new point, balancing exploration and exploitation. | A standard choice for selecting the next set of parameters to test in drug yield optimization [43] [42]. |
| Random Forest | Machine Learning Model | An interpretable classifier; when combined with BO for hyperparameter and imbalance tuning, it achieves deep learning-level performance. | Predicting antibacterial candidates with the CILBO pipeline [39]. |
| Long Short-Term Memory (LSTM) Network | Deep Learning Model | A type of recurrent neural network capable of learning long-term dependencies in sequential data. | Predicting time-series drug concentrations (e.g., Olanzapine) [40]. |
| RDKit | Cheminformatics Library | Generates molecular fingerprints and descriptors that serve as feature representations for machine learning models. | Converting molecular structures into features for the antibacterial prediction model [39]. |
| Transcranial Random Noise Stimulation (tRNS) | Neurostimulation Modality | A non-invasive brain stimulation technique that modulates cortical excitability via application of random electrical noise. | Personalized enhancement of sustained attention in home-based settings [36]. |
| Repetitive Transcranial Magnetic Stimulation (rTMS) | Neurostimulation Modality | Uses magnetic fields to induce electrical currents in targeted cortical regions, modulating neural activity. | Application of various protocols (HF, LF, bilateral, iTBS) for stroke recovery and depression [37] [38]. |
| Large Language Model (LLM) | AI Model | Provides reasoning capabilities, incorporates domain knowledge, and generates hypotheses within an optimization framework. | Enhancing BO in the "Reasoning BO" framework for chemical reaction optimization [42]. |
Deep Brain Stimulation (DBS) is an established therapy for Parkinson's disease (PD) that delivers electrical stimulation to specific brain targets to alleviate motor symptoms. Conventional high-frequency DBS at 130 Hz provides significant therapeutic benefits but operates with limited understanding of its network-level mechanisms and lacks personalization for individual symptom profiles. Computational models offer a powerful approach to explore these mechanisms and optimize stimulation protocols in silico. This case study investigates the application of a validated thalamocortical microcircuit (TCM) spiking network model to evaluate and optimize DBS strategies for Parkinson's disease. The TCM model serves as a biophysically realistic platform for testing novel stimulation patterns that could potentially enhance therapeutic efficacy while reducing energy consumption and side effects. By bridging computational neuroscience with clinical application, this approach demonstrates how in-silico testing can accelerate the development of personalized neuromodulation therapies.
The Thalamocortical Model: Structure and Validation
Model Architecture and Dynamics
The thalamocortical microcircuit (TCM) model is a spiking neuronal network that incorporates 540 subthreshold noise-driven spiking neurons obeying Izhikevich neuronal dynamics [44] [45]. These neurons are connected via Tsodyks-Markram synapses, which incorporate short-term synaptic plasticity, a key mechanism underlying synaptic suppression during high-frequency stimulation [44] [46]. The network architecture is organized into specific populations:
- Cortical excitatory populations distributed across three layers: supragranular/surface (S, 100 neurons), granular/middle (M, 100 neurons), and infragranular/deep (D, 100 neurons) [44]
- Cortical inhibitory population (CI, 100 neurons) shared across cortical layers [45]
- Thalamic populations including thalamocortical relay nucleus (TCR, 100 neurons, excitatory) and thalamic reticular nucleus (TRN, 40 neurons, inhibitory) [46]
The network dynamics are described by a set of differential equations that capture membrane potential and recovery variables for each neuron [44]. The improved model corrects numerical issues in noise term integration and implements matrix-based computation for enhanced efficiency, enabling simulations with larger numbers of neurons through parallel computing and GPU acceleration [45].
Modeling Parkinsonian Pathology and Validation
The TCM model reproduces key neurophysiological features of Parkinson's disease through specific alterations in synaptic weights within and between thalamus and cortex [44] [46]. These manipulations result in:
- Elevated beta power (~13-30 Hz oscillations) in the motor cortex [46]
- Exaggerated synchronization of spiking neurons [45]
- Formation of pathological neuronal clusters [44]
The model has been validated against neurophysiological recordings from animal models and human studies, demonstrating its capability to manifest known DBS cortical effects despite its relative simplicity [45]. The incorporation of short-term synaptic plasticity as a fundamental mechanism of DBS action further enhances its biological realism and predictive power [46].
Experimental Protocols for DBS Optimization
Conventional and Novel DBS Protocols
The TCM model enables systematic testing of various DBS protocols to compare their efficacy in suppressing pathological network activity. The following experimental approaches were implemented:
Conventional DBS Protocol:
- Continuous high-frequency stimulation at 130 Hz [46]
- Applied as an intracellular transmembrane current to 50% of neurons in the deep cortical layer (layer D) [46]
- Intensity calibrated to maximize suppression of pathological beta oscillations
Novel Pulsing Strategies: Two novel pulsing patterns designed to maximize synaptic suppression while minimizing the number of stimuli were tested [46]:
- Pattern A: Incorporates changes in pulsing frequency
- Pattern B: Utilizes on/off pulsing periods Both patterns were derived from theoretical calculations leveraging short-term synaptic plasticity principles to maintain neurotransmitter depletion with minimal stimulation [46].
Control Condition:
- Low-frequency DBS at 20 Hz to demonstrate resonance effects and unwanted harmonics that occur with non-therapeutic frequencies [45]
Protocol Implementation and Testing Workflow
Table: Experimental Protocol Parameters Tested in the TCM Model
| Protocol Type | Stimulation Frequency | Pulsing Pattern | Intensity Calibration | Key Mechanism |
|---|---|---|---|---|
| Conventional DBS | 130 Hz | Continuous | Optimized for beta suppression | Synaptic suppression |
| Novel Pattern A | Variable frequency | Intermittent frequency changes | Careful tuning required | Maximized neurotransmitter depletion |
| Novel Pattern B | High-frequency bursts | On/off cycling | Balanced for efficacy | Minimal stimulus count |
| Control (20 Hz) | 20 Hz | Continuous | Same as 130 Hz | Demonstrates resonance |
The experimental workflow involved simulating each protocol for 12 seconds of model time with DBS initiation at the 6-second mark [45]. The improved computational efficiency of the model, including parallel processing and GPU acceleration, facilitated multiple simulation runs to establish statistical significance of findings [44] [45].
Diagram 1: Experimental workflow for testing DBS protocols in the thalamocortical model, showing the sequence from parameter setup through simulation to analysis and optimization.
Quantitative Results and Performance Comparison
Effects on Pathological Oscillations and Synchronization
The TCM model provides quantitative metrics to evaluate DBS efficacy, including power spectral densities for oscillatory activity and Morgera's index of synchrony (M) to measure network synchronization levels [46]. Simulation results demonstrate distinct performance patterns across stimulation protocols:
Table: Quantitative Comparison of DBS Protocol Effects on Parkinsonian Network Activity
| Protocol Type | Beta Power Reduction | Synchronization (Morgera's Index) | Neuronal Cluster Formation | Therapeutic Efficiency |
|---|---|---|---|---|
| 130 Hz Conventional DBS | Significant suppression | Strong desynchronization | Excited and inhibited clusters | High efficacy, continuous energy use |
| Novel Pattern A | Significant suppression | Strong desynchronization | Similar cluster patterns | Comparable efficacy, reduced stimuli |
| Novel Pattern B | Significant suppression | Strong desynchronization | Similar cluster patterns | Comparable efficacy, reduced stimuli |
| 20 Hz Control | Increased or unchanged | Sustained synchronization | Pathological clusters maintained | No therapeutic benefit |
Both novel pulsing strategies achieved similar suppression of exaggerated beta power and desynchronization of network spike patterns compared to conventional 130 Hz DBS when applied with careful tuning of stimulation intensities [46]. The raster plots in Figure 1 of the improved model publication visually demonstrate the desynchronization effect of 130 Hz DBS in contrast to the sustained synchronized activity with 20 Hz stimulation [45].
Clinical Translation and Symptom-Specific Optimization
Beyond oscillatory activity, DBS optimization must address the diverse symptom profile of Parkinson's disease. Recent research on symptom-specific networks provides a framework for personalizing stimulation:
Table: Symptom-Specific White Matter Tracts for Targeted DBS Optimization
| Symptom Domain | Associated White Matter Tracts | Connected Cortical Regions | STN Subregion |
|---|---|---|---|
| Tremor | Cerebellothalamic pathway, connections to primary motor cortex | Primary motor cortex, cerebellum | Posterior motor STN |
| Bradykinesia | Connections from medial STN surface | Supplementary motor area (SMA) | Anterior premotor STN |
| Rigidity | Anterior subthalamic premotor connections | Pre-supplementary motor area | Anterior premotor STN |
| Axial Symptoms | Lateral STN connections, brainstem pathways | Supplementary motor cortex, pedunculopontine nucleus | Lateral STN |
Studies with 237 patients across five centers revealed that tremor improvements correlated with stimulation of tracts connected to primary motor cortex and cerebellum, while axial symptoms responded to tracts connected to supplementary motor cortex and brainstem [47]. This symptom-tract library enables the development of algorithms that personalize stimulation parameters based on individual patient symptom profiles [47].
Research Toolkit for Thalamocortical DBS Modeling
Implementing and extending the TCM model requires specific computational tools and resources. The following research reagents and solutions form the essential toolkit for this field:
Table: Essential Research Tools for Thalamocortical DBS Modeling and Optimization
| Tool Category | Specific Solution | Function in Research | Implementation Notes |
|---|---|---|---|
| Computational Modeling | Improved TCM Code [44] | Biophysically realistic network simulations | Matrix-based computation, GPU acceleration support |
| Neuron Dynamics | Izhikevich Model [46] | Efficient spiking neuron implementation | Balances biological realism and computational efficiency |
| Synaptic Plasticity | Tsodyks-Markram Synapses [46] | Short-term plasticity and neurotransmitter release | Captures synaptic suppression mechanism |
| Clinical Translation | Lead-DBS Toolbox [48] [49] | Electrode reconstruction and VTA modeling | Integrates with patient imaging data |
| Stimulation Modeling | OSS-DBS [48] [49] | Electric field and volume of tissue activated calculations | Fast, adjustable calculations for target coverage |
| Connectome Analysis | DBS Tractography Atlas [47] | Symptom-specific pathway identification | Enables network-based targeting |
The improved TCM model code is implemented in MATLAB and includes functions such as updateTimeStep.m for efficient matrix-based computation at each simulation time step [44] [45]. The model supports both CPU (multicore and multithread) and GPU processing, with GPU implementation particularly advantageous for larger networks exceeding several hundred neurons [45].
Integration with Clinical Workflows and Personalization Approaches
Geometry-Based Optimization Algorithms
The computational insights from the TCM model can be translated to clinical practice through geometry-based optimization approaches that leverage routinely collected medical imaging data [48] [49]. These methods calculate a geometry score for each electrode contact based on:
- Euclidean distance to the motor STN centroid [49]
- Rotation angle between directional contacts and the centroid relative to electrode axis [49]
- Clinical review scores incorporating rigidity, akinesia, and tremor improvements [49]
In a retrospective analysis of 174 implanted electrode reconstructions from 87 Parkinson's patients, this algorithmic approach demonstrated superior target structure coverage (Wilcoxon p < 5e-13, Hedges' g > 0.94) and reduced electric field leakage to neighboring regions (p < 2e-10, g > 0.46) compared to expert manual parameter settings [49].
Network-Based Personalization Framework
Diagram 2: Network-based personalization framework for DBS optimization, showing how patient-specific data integrates with symptom-network mapping and computational validation.
The "network blending" approach leverages a library of symptom-response circuits to suggest optimal stimulation parameters based on individual patient symptom profiles [47]. This method addresses the limitation of one-size-fits-all DBS programming by simultaneously targeting multiple symptom-specific networks with a single electrode through complex parameter configurations [47]. The TCM model serves as a computational testbed for validating these personalized parameter sets before clinical implementation.
Discussion and Future Directions
This case study demonstrates how validated thalamocortical models can bridge computational neuroscience and clinical practice to optimize DBS for Parkinson's disease. The TCM model provides a biophysically realistic platform for testing novel stimulation patterns that achieve similar therapeutic effects to conventional high-frequency DBS while potentially reducing energy consumption through minimized stimulus delivery [46].
The integration of symptom-specific network mapping [47] with geometry-based optimization algorithms [48] [49] creates a comprehensive framework for personalizing DBS therapy. This approach moves beyond trial-and-error programming toward computationally guided, patient-specific parameter selection based on individual symptom burden and unique neuroanatomy.
Future developments should focus on incorporating long-term synaptic mechanisms such as spike-timing dependent plasticity (STDP) into the TCM model [44], enabling more naturalistic input patterns to thalamus [45], and validating model predictions against larger clinical datasets. As DBS technology evolves with directional electrodes and current fractionation capabilities, computational models will play an increasingly vital role in harnessing these technological advances for improved patient outcomes.
The synergy between computational modeling and clinical innovation holds promise for transforming DBS from a generally effective but broadly applied therapy into a precisely targeted, symptom-specific treatment tailored to each individual's unique Parkinsonian phenotype and neural circuitry.
Navigating Challenges: Strategies for Optimizing Protocols and Improving Model Fidelity
The field of therapeutic neurostimulation is characterized by a fundamental paradox: while possessing immense potential for treating conditions from chronic pain to cognitive disorders, its clinical application is often marked by inconsistent and unpredictable outcomes. This variability stems not from a failure of the underlying principle, but from the application of one-size-fits-all protocols to uniquely individual human nervous systems. The efficacy of neurostimulation is profoundly influenced by a myriad of subject-specific factors, which traditional methods have struggled to quantify and incorporate. Research indicates that often only 50% or fewer of study participants exhibit the expected response to a given neurostimulation protocol, classifying the remainder as "non-responders" [50]. This high degree of inter-individual variability has necessitated a paradigm shift towards personalized approaches. The emergence of sophisticated computational modeling and artificial intelligence (AI) now provides a robust framework to systematically account for these sources of variability, transforming neurostimulation from an art into a quantitative science. This review compares the leading computational strategies being developed to solve the variability problem, focusing on their approaches to two core dimensions: individual neuroanatomy and baseline neurophysiological performance.
The Dual Pillars of Variability: Anatomy and Baseline State
The response to neurostimulation is not a fixed property but a dynamic interplay between the stimulus and the recipient's biological and functional characteristics. These factors can be categorized into two primary groups, as detailed in the table below.
Table 1: Key Sources of Inter-Individual Variability in Neurostimulation
| Category | Specific Factor | Impact on Neurostimulation | Supporting Evidence |
|---|---|---|---|
| Anatomical Factors | Skull Thickness & Composition | Thinner skull regions (e.g., temporal bone) allow more current to reach the cortex, increasing electric field strength [50]. | tDCS studies using computational models [50]. |
| Scalp-to-Cortex Distance | A greater distance reduces current density at the target, diminishing the effective stimulus [50]. | MRI-based electric field modeling [50]. | |
| Cortex Folding & Morphology | Individual gyral patterns alter the direction and magnitude of the induced electric field, affecting which neural populations are activated [50]. | Patient-specific finite element models [9]. | |
| Functional & State-Based Factors | Baseline Performance Level | Individuals with lower baseline cognitive or physiological performance often show greater improvement, exhibiting an inverted U-shaped response to intensity [36]. | AI-optimized tRNS for sustained attention [36]. |
| Brain State & Engagement | Alertness, hormonal cycles, and task engagement modulate neural excitability and the resulting effects of stimulation [50]. | tDCS studies on motor and cognitive tasks [50]. | |
| Genetic Profile | Variations in genes related to neurotransmitter function (e.g., BDNF, COMT) influence plasticity mechanisms engaged by stimulation [50]. | Analyses of tDCS responders vs. non-responders [50]. |
Computational Approaches to Tame Variability
To address the challenges outlined in Table 1, researchers have developed several computational approaches that move beyond generic protocols.
Table 2: Comparison of Computational Modeling Approaches for Personalization
| Approach | Core Methodology | Advantages | Limitations | Representative Applications |
|---|---|---|---|---|
| Patient-Specific Biomechanical Modeling | Uses medical imaging (MRI, CT) to construct digital replicas of an individual's anatomy for electric field simulation [9]. | High anatomical fidelity; identifies optimal electrode placement and dosage; useful for implantable devices [8] [9]. | Resource-intensive (requires medical imaging); does not directly model dynamic neural response [9]. | Spinal Cord Stimulation (SCS) for pain [9], Deep Brain Stimulation (DBS). |
| AI-Driven Bayesian Optimization | Employs algorithms to iteratively adjust stimulation parameters based on measured physiological or behavioral outcomes [36]. | Does not require medical imaging; optimizes for real-world outcomes; efficient parameter space exploration [36]. | Requires many data points per individual; performance can degrade with high measurement noise [36]. | Home-based cognitive enhancement with tRNS [36]. |
| Digital Twin Neural Circuit Modeling | Develops a computational model of the target neural circuit's dynamics, which is then calibrated to individual response data [4]. | Provides a mechanistic explanation of responses; can predict temporal dynamics; powerful for closed-loop control [4]. | High complexity; requires precise individual calibration data that can be invasive to acquire [4]. | Viscerosensory neurostimulation for blood pressure control [4]. |
Experimental Protocols and Workflows
The implementation of these approaches relies on distinct experimental and computational workflows.
Protocol for Patient-Specific SCS Modeling: This protocol is used to optimize epidural spinal cord stimulation for pain management [9].
- Data Acquisition: Obtain high-resolution MRI (and sometimes CT) scans of the patient's spinal column.
- Model Construction: Segment the medical images to identify different tissues (vertebrae, cerebrospinal fluid, gray matter, white matter). Assign tissue-specific electrical conductivities.
- Finite Element Analysis (FEA): Use FEA software to compute the electric field generated in the spinal cord by specific electrode configurations and stimulation parameters.
- Neural Activation Estimation: Combine the computed electric field with biophysical models of axons to predict which neural pathways are activated.
- Clinical Application: Use the model to pre-operatively plan lead placement or post-operatively select stimulation parameters that maximize target engagement and avoid side effects.
Protocol for AI-Optimized Transcranial Random Noise Stimulation (tRNS): This protocol was used to enhance sustained attention in a home-based setting [36].
- Baseline Assessment: Measure the participant's baseline performance (
A'sensitivity index) on a sustained attention task and record basic anatomical data (e.g., head circumference). - Algorithm Setup: Initialize a personalized Bayesian Optimization (pBO) algorithm that uses baseline performance and head size to inform its initial parameter searches.
- Iterative Optimization: Over multiple sessions, the pBO algorithm selects a current intensity (e.g., 0.5 mA, 1.0 mA, 1.5 mA) for that day. The participant receives tRNS while performing the attention task, and their performance is recorded.
- Model Update: The pBO algorithm uses the input-output pair (stimulation intensity, performance change) to update its internal model of the individual's dose-response curve.
- Convergence: The algorithm converges on a personalized current intensity that maximizes the participant's sustained attention performance, often following an inverted U-shape function.
The following diagram illustrates the core logical relationship of the AI-driven optimization workflow, which can be deployed in clinical or even home settings.
Quantitative Data Comparison
The effectiveness of these personalized approaches is demonstrated by quantitative improvements in experimental outcomes.
Table 3: Experimental Efficacy of Personalized vs. Standard Neurostimulation
| Experiment / Condition | Subject Group | Key Outcome Measure | Result: Personalized vs. Control | Statistical Significance |
|---|---|---|---|---|
| AI-tRNS for Attention [36] | Low Baseline Performers | Sensitivity Index (A') | pBO-tRNS outperformed both one-size-tRNS and sham. | β = 0.76, SE = 0.29, p = 0.015 |
| AI-tRNS for Attention [36] | Low vs. High Baseline Performers | Improvement in Sensitivity Index | Low performers improved more than high performers under pBO-tRNS. | t(21) = 2.28, p = 0.03, Cohen’s d = 0.95 |
| Digital Twin for BP Control [4] | Rat Model (n=10) | Accuracy of Blood Pressure Prediction | Model based on NTS collective dynamics accurately predicted stimulus-driven hemodynamic perturbations. | High correlation between predicted and observed BP changes. |
| Computational AFib Model [13] | In-silico Simulation | Identification of AV node target | The closed-loop model identified the AV node as a promising neurostimulation target, consistent with clinical practice. | Model outputs showed robust concordance with empirical patient data. |
Advancing research in this field requires a suite of computational and experimental tools.
Table 4: Key Research Reagents and Solutions for Computational Neurostimulation
| Tool / Resource Name | Type | Primary Function in Research | Example Context |
|---|---|---|---|
| Finite Element Method (FEM) Software (e.g., COMSOL, ANSYS) | Computational Modeling | To calculate the distribution of electric fields and currents within complex, patient-specific anatomical models derived from MRI/CT scans [9]. | Building volume conductor models of the spinal cord for SCS [9]. |
| Personalized Bayesian Optimization (pBO) Algorithm | AI/Machine Learning | To efficiently search for optimal stimulation parameters by iteratively updating a model of an individual's dose-response relationship [36]. | Remote optimization of tRNS current intensity for sustained attention [36]. |
| Hodgkin-Huxley Formalism | Biophysical Neural Model | To simulate the activation and firing of neurons or axons in response to the computed extracellular electric field [9]. | Predicting the activation thresholds of dorsal column axons during SCS [9]. |
| Rion TR-06 Electrogustometer | Clinical Stimulation Device | To provide a calibrated, clinically validated method for electrically stimulating nervous tissue, often used as a reference in research [51]. | Comparing tongue sensation from a test battery device in taste research [51]. |
| Digital Twin Framework | Computational Modeling | To create a patient-specific virtual replica of a neural circuit (e.g., in the brainstem) that can predict dynamic physiological responses to stimulation [4]. | Predicting blood pressure changes during viscerosensory neurostimulation in rats [4]. |
Integrated Signaling and Workflow in a Digital Twin Framework
The most complex personalization involves creating a "digital twin" of a neural circuit. The following diagram illustrates the signaling pathway and workflow from a study that developed a digital twin for brainstem neurostimulation to control blood pressure, integrating both anatomical and functional variability [4].
Discussion and Future Directions
The evidence overwhelmingly confirms that accounting for individual anatomy and baseline performance is not merely beneficial but essential for unlocking the full potential of neurostimulation therapies. The comparative analysis reveals that no single computational approach is universally superior; rather, the choice depends on the clinical application and available resources. Patient-specific biomechanical models are indispensable for guiding the physical placement of electrodes in invasive procedures, while AI-driven optimization offers a powerful and accessible method for personalizing non-invasive protocols based on functional outcomes. The emerging digital twin paradigm represents a frontier where mechanistic understanding and personalization converge, promising unprecedented control over complex physiological functions like cardiovascular regulation [4].
Future progress hinges on standardizing model validation and developing more efficient methods for calibrating models to individuals. Furthermore, the field is undergoing a conceptual shift: rather than viewing neural variability as noise to be overcome, it is increasingly seen as a functional feature that can be harnessed. The future of neurostimulation lies in flexible, state-dependent protocols that can dynamically adapt to an individual's changing neurophysiology, moving us closer to a era of truly precise and effective neuromodulation therapies [17].
Overcoming Non-Linear and Paradoxical Effects of Stimulation Parameters
Neurostimulation therapies represent a groundbreaking approach for treating neurological disorders, but their development is complicated by inherently non-linear biological systems and occasional paradoxical responses to stimulation parameters. The success of therapeutic electrical stimulation for conditions spanning inflammatory, cardiovascular, cognitive, metabolic, and pain disorders depends on appropriate modulation of targeted neurons [52]. However, neural responses to stimulation are highly nonlinear, influenced by the delivered electrical signal, physical electrode-tissue relationships, and neuronal biophysics [52]. Computational models have become indispensable in advancing our understanding and control of neural responses to electrical stimulation, yet traditional approaches suffer from computational bottlenecks that limit their utility for real-time applications and sophisticated optimization [52].
This review examines the challenges posed by non-linear and paradoxical effects across major neuromodulation modalities, compares computational and experimental approaches to overcome these challenges, and provides validation frameworks for developing reliable neurostimulation protocols. Understanding these complex dynamics is crucial for researchers and drug development professionals seeking to create more effective, personalized neuromodulation therapies.
Manifestations of Paradoxical Effects in Clinical Settings
Case Evidence of Paradoxical Neurophysiological Responses
Paradoxical modulation of neural activity—where clinical improvement occurs despite neurophysiological responses that contradict established biomarkers—presents significant challenges for treatment personalization. A notable case study involving deep brain stimulation (DBS) for Parkinson's disease (PD) demonstrated this phenomenon clearly [53].
The patient exhibited a paradoxical increase in beta power (13-35 Hz oscillations) following administration of L-dopa and pramipexole (MEDS condition), but an attenuation in beta power during DBS and MEDS+DBS conditions, despite clinical improvement of 50% or greater under all three therapeutic conditions [53]. Specifically, total power in the beta-band significantly increased in the MEDS condition compared to OFF, yet decreased in both DBS and MEDS+DBS conditions relative to OFF [53]. This case highlights the variability in physiological presentation among PD patients and underscores the importance of personalized approaches to developing biomarker-based DBS closed-loop algorithms [53].
Table 1: Documented Cases of Paradoxical Responses to Neurostimulation
| Condition | Stimulation Type | Paradoxical Response | Clinical Outcome |
|---|---|---|---|
| Parkinson's Disease [53] | Medication (L-dopa) | Increased beta power | 50% improvement in motor symptoms |
| Parkinson's Disease [53] | DBS | Decreased beta power | 50% improvement in motor symptoms |
| Parkinson's Disease [53] | Medication + DBS | Decreased beta power | 80% improvement in motor symptoms |
Non-Linear Dynamics in Neural Systems
Computational models reveal fundamental mechanisms through which neural networks exhibit non-linear behaviors that complicate stimulation parameter optimization. Research using Wilson-Cowan-inspired networks of inhibitory and excitatory populations has shown that neural systems can demonstrate sudden transitions into oscillatory dynamics similar to transitions to seizure states [54]. These transitions occur via passage through a cascade of dynamical instabilities called bifurcations, mediated by parameters encapsulating "neuronal excitability" [54].
Such non-linear systems display multi-stability (coexistence of multiple dynamic states), where subtle changes in stimulation parameters can trigger dramatic shifts in network behavior [54]. This mathematical framework provides insights into why neurostimulation often produces non-intuitive, non-linear responses that complicate parameter optimization. Understanding these fundamental dynamics is essential for designing stimulation protocols that maintain neural circuits in therapeutic states while avoiding sudden transitions to pathological dynamics.
Computational Approaches for Parameter Optimization
Surrogate Modeling and Machine Learning
Recent advances in machine learning have enabled the development of highly efficient surrogate models that accelerate parameter optimization while accounting for non-linear dynamics. The AxonML framework implements a surrogate myelinated fiber (S-MF) model that accurately predicts spatiotemporal responses to electrical stimulation orders-of-magnitude more quickly than conventional methods [52].
This approach generates a several-orders-of-magnitude improvement in computational efficiency (2,000 to 130,000× speedup over single-core simulations in NEURON) while retaining generality and high predictive accuracy (R² = 0.999 for activation thresholds) [52]. The model successfully designed stimulation parameters for selective stimulation of pig and human vagus nerves using both gradient-free and gradient-based optimization approaches [52].
Table 2: Comparison of Computational Optimization Approaches
| Method | Computational Efficiency | Accuracy | Applications | Limitations |
|---|---|---|---|---|
| Surrogate Fiber Models (S-MF) [52] | 2,000-130,000× speedup | R² = 0.999 | Peripheral nerve stimulation, VNS | Requires extensive training data |
| Deep Learning fMRI Pipeline [55] | Reduces optimization from ~1 year to hours | 96% classification accuracy | DBS for Parkinson's disease | Limited to trained stimulation targets |
| Conventional NEURON Models [52] | Baseline (1×) | Gold standard | Research applications | Computationally prohibitive for optimization |
| Waveform Design Principles [56] | Moderate | High for specific applications | Energy-efficient stimulation | Limited to waveform optimization |
fMRI-Based Deep Learning Optimization
For deep brain stimulation, a deep learning and fMRI-based pipeline has shown promise for rapid parameter optimization. This approach uses an unsupervised autoencoder (AE)-based model to extract meaningful features from blood oxygen level dependent (BOLD) fMRI datasets, which are then fed into multilayer perceptron (MLP)-based parameter classification and prediction models [55].
This method has demonstrated remarkable accuracy in classifying optimal versus non-optimal DBS parameters (96% ± 4% accuracy, 0.95 ± 0.07 precision, 0.92 ± 0.07 recall) [55]. The pipeline has the potential to reduce optimization duration from approximately one year to a few hours during a single clinical visit, addressing a critical bottleneck in DBS therapy [55].
Model-Based Waveform Design
Computational models provide powerful tools for designing stimulation waveforms that maximize efficiency and selectivity while accounting for non-linear neural responses. Model-based analysis has revealed that waveform shape significantly influences both selectivity and efficiency of neural stimulation [56].
Key principles for waveform design include:
- Short duration pulses increase spatial selectivity by minimizing threshold changes from current redistribution [56]
- Asymmetric charge-balanced waveforms can increase stimulation selectivity between local cells and passing axons compared to conventional monophasic or symmetric biphasic waveforms [56]
- No single waveform shape is simultaneously charge-, power-, and energy-optimal, requiring careful definition of objective functions for specific applications [56]
Energy-optimal neural stimulation has practical implications for battery lifetime in implanted pulse generators, with improved efficiency potentially extending device longevity and reducing replacement surgeries [56].
Experimental Protocols for Validation
Protocol for Intensive Theta-Burst Stimulation
Novel intensive stimulation protocols are being developed to overcome limitations of conventional approaches. The personalized, functional connectivity-guided accelerated intermittent theta-burst stimulation (PAiT) protocol, modeled after Stanford neuromodulation therapy, represents an innovative approach for treatment-resistant depression [57].
This protocol involves:
- 10 sessions per day over 5 days (total 50 sessions, 90,000 pulses)
- Personalized targeting based on negative functional coupling between subgenual anterior cingulate cortex and dorsolateral prefrontal cortex
- Neuronavigation for precise coil placement [57]
In comparison, standard 10 Hz rTMS involves:
- Once daily sessions for 6 weeks (total 30 sessions, 90,000 pulses)
- Beam-F3 method for dorsolateral prefrontal cortex targeting
- Similarly, neuronavigation for coil placement [57]
This protocol is currently being evaluated in a randomized controlled trial (D-DOTT) comparing cost-effectiveness with standard rTMS, with results expected in 2027 [57].
Network Stabilization Experiments
Computational and mathematical analyses provide experimental frameworks for understanding how neurostimulation stabilizes neural networks. Research using Wilson-Cowan-motivated networks has revealed that high variance and/or high frequency stimulation waveforms can prevent multi-stability, a mathematical harbinger of sudden changes in network dynamics [54].
Key findings from this research include:
- Stimulation stabilizes neural activity through selective recruitment of inhibitory cells
- Both noisy and periodic stimuli exert stabilizing influences on network responses
- Stimulation parameters can be tuned to optimize this stabilizing effect [54]
These findings provide theoretical underpinnings for neuromodulatory approaches to stabilize neural microcircuit activity and prevent transitions to pathological states like seizures.
Comparative Effectiveness Protocol for Early Stroke
A comprehensive network meta-analysis protocol has been developed to compare different neuromodulation approaches for early stroke rehabilitation. This methodology includes:
- Bayesian network meta-analysis of randomized controlled trials comparing tDCS and rTMS protocols
- Evaluation of multiple outcomes: upper and lower extremity motor function (Fugl-Meyer Assessment), activities of daily living (modified Barthel index), neurological function (NIH Stroke Scale), and safety (adverse events)
- Surface under the cumulative ranking curve (SUCRA) analysis to estimate probabilities of each intervention being optimal [37]
Preliminary results from this approach indicate that bilateral application of high- and low-frequency rTMS (BL-rTMS) performs best in improving upper extremity motor function (SUCRA: 92.8-95.4%) and activities of daily living (SUCRA: 85.6-100%) in early stroke patients [37].
Verification, Validation, and Uncertainty Quantification
Regulatory Science Frameworks
Establishing credibility for computational models requires rigorous verification, validation, and uncertainty quantification (VVUQ) processes. The ASME VVUQ standards provide structured approaches for assessing computational model credibility across various applications, including medical devices [58].
Key components of this framework include:
- Verification: Determining if the computational model correctly implements the mathematical description
- Validation: Assessing if the computational simulation agrees with physical reality
- Uncertainty Quantification: Evaluating how variations in numerical and physical parameters affect simulation outcomes [58]
These processes are essential for regulatory acceptance of computational models used in medical device development and optimization.
Threshold-Based Validation Approach
The FDA has developed a "threshold-based" validation method that provides a mechanism for determining acceptance criteria for computational model validation [59]. This approach is particularly valuable for situations where threshold values for safety or performance are available for the quantity of interest.
The method involves:
- Inputs: Mean values and uncertainties in validation experiments, model predictions, and safety thresholds
- Process: Comparison of model predictions to established safety thresholds
- Output: A measure of confidence that the model is sufficiently validated from a safety perspective [59]
This approach helps address a key gap in validation methodology by providing a well-defined acceptance criterion for comparison error between simulation results and validation experiments.
Table 3: Essential Research Tools for Neurostimulation Optimization
| Tool/Resource | Function | Application Context |
|---|---|---|
| AxonML Framework [52] | GPU-accelerated surrogate modeling | Peripheral nerve stimulation parameter optimization |
| fMRI with DBS Cycling [55] | Mapping brain responses to stimulation | DBS parameter classification and prediction |
| NEURON Simulation Environment [52] | Gold-standard neural simulation | Generating training data for surrogate models |
| ASME VVUQ Standards [58] | Model credibility assessment | Regulatory submission for computational models |
| Threshold-Based Validation [59] | Acceptance criterion determination | Safety validation of computational models |
| Wilson-Cowan Network Models [54] | Studying network-level effects | Understanding paradoxical stabilization mechanisms |
| Personalized Neuronavigation [57] | Precise stimulation targeting | Accelerated theta-burst stimulation protocols |
| Bayesian Network Meta-Analysis [37] | Comparative effectiveness research | Evaluating multiple stimulation protocols simultaneously |
Overcoming non-linear and paradoxical effects of stimulation parameters requires integrated computational and experimental approaches that account for the complexity of neural systems. Computational models, particularly machine learning-based surrogate models and fMRI-guided optimization pipelines, offer powerful tools for navigating high-dimensional parameter spaces and identifying optimal stimulation protocols despite non-linearities. Experimental evidence from clinical and computational studies demonstrates that paradoxical responses represent genuine biological phenomena rather than measurement artifacts, necessitating personalized approaches to neuromodulation therapy.
Robust verification, validation, and uncertainty quantification frameworks provide essential methodologies for establishing model credibility and regulatory acceptance. As neurostimulation technologies continue to evolve toward more sophisticated, closed-loop, and personalized approaches, addressing these non-linear and paradoxical effects will be crucial for developing more effective and reliable therapies for neurological and psychiatric disorders.
Optimizing Electrode Montage and Current Flow for Target Specificity
In non-invasive brain stimulation, the therapeutic efficacy and experimental outcomes of techniques such as transcranial Direct Current Stimulation (tDCS) and transcutaneous auricular Vagus Nerve Stimulation (taVNS) are fundamentally governed by the precise distribution of electric current in targeted neural tissues. The electrode montage—defined by the number, size, placement, and current flow of electrodes—directly determines the intensity, focality, and specificity of the resulting electric field within the brain or peripheral nervous structures. Inconsistent outcomes and variable effect sizes reported in the literature are frequently attributable to the use of ad hoc, non-optimized montages that yield suboptimal current flow patterns [60]. Consequently, optimizing montage and current parameters is a critical prerequisite for advancing the rigor, reproducibility, and clinical utility of neurostimulation protocols.
Computational current flow modeling, typically implemented using the Finite Element Method (FEM) on detailed anatomical reconstructions derived from magnetic resonance imaging (MRI), has emerged as an indispensable tool for montage optimization. These models simulate how tissue geometry and conductivity shape the electric field, enabling researchers to rationally design stimulation protocols in silico before empirical application [61] [62] [63]. This guide provides a comparative analysis of optimization approaches for central and peripheral stimulation targets, detailing associated experimental protocols, quantitative outcomes, and the essential toolkit for implementation.
Comparative Analysis of Optimization Approaches and Outcomes
Central Stimulation: Conventional vs. Optimized and Multichannel tDCS
Conventional tDCS often employs a single pair of large pad electrodes. While simple to implement, this approach produces diffuse electric fields with poor spatial specificity, potentially stimulating both target and non-target regions simultaneously [64] [60]. Optimization strategies aim to overcome this limitation.
Table 1: Comparative Performance of tDCS Montages for Central Targets
| Montage Type | Typical Electrode Configuration | Key Advantage | Quantitative Electric Field Outcome | Associated Experimental Finding |
|---|---|---|---|---|
| Conventional Bipolar | Single anode over target (e.g., C3 for hand motor cortex), large cathode over contralateral supraorbital region [64] [63]. | Simplicity of setup and application. | Diffuse electric field; serves as a baseline for comparison (0% improvement) [63]. | High inter-individual variability in outcomes; mixed results in cognitive studies [64] [65]. |
| Optimized Bipolar | Computationally optimized positions for both anode and cathode to maximize field in target [63]. | Increased intensity at the target region using standard, low-cost electrodes. | 20% to 52% stronger electric field in the hand motor region compared to conventional montage in stroke patients [63]. | Potential for enhanced therapeutic effects in motor rehabilitation; clinical trials ongoing [63]. |
| High-Definition (HD-tDCS) | A central "active" electrode surrounded by a ring of 4 return electrodes (4x1 ring montage) [66] [60]. | Superior focality, constraining the electric field to a smaller cortical volume. | Categorically increased focality; electric field intensity can be more concentrated under the central electrode [66] [60]. | Can induce changes in neural oscillatory power correlated with baseline working memory performance [64]. |
| Multichannel Optimized | Arrays of multiple small electrodes (e.g., 19 or 64) with individually optimized current intensities [62] [66]. | Maximum steering capability; can target deep or irregularly shaped structures while avoiding specific regions. | Can direct current toward targets like the inferior frontal gyrus (IFG) or accumbens that are hard to reach with bipolar montages [62] [67]. | Shown to induce significantly greater motor cortex excitability changes than bipolar tDCS [64]. |
Individual anatomy significantly influences current flow. For example, a simulation study on stroke patients revealed that cerebrospinal fluid (CSF)-filled lesions alter current paths, often reducing the electric field intensity in the target region. Patient-specific optimized montages were able to overcome this, increasing the electric field in the hand motor region by an average of 20% and up to a maximum of 52% compared to the conventional montage [63]. Furthermore, the optimal electrode positions were unique to each patient, underscoring the importance of personalization [63].
The benefits of optimization extend beyond motor regions to cognitive networks. Studies targeting the frontoparietal network for working memory have demonstrated that the effectiveness of a given montage is not universal but interacts with an individual's innate cognitive capacity. Specifically, individuals with lower baseline working memory performance tend to benefit more from stimulation, and different montages (e.g., conventional prefrontal vs. frontoparietal network stimulation) can produce divergent outcomes depending on this baseline [64] [65].
Peripheral Stimulation: Targeting the Auricular Vagus Nerve with taVNS
The principles of optimization are equally critical for peripheral targets. In taVNS, the goal is to activate the auricular branch of the vagus nerve, which has a non-uniform density across the ear's sub-regions [61].
Table 2: Sensitivity and Selectivity of Example taVNS Electrode Montages
| Target Ear Region | Electrode Montage (Example) | Sensitivity (Peak Electric Field) | Selectivity (Spatial Restriction) | Notes on Use |
|---|---|---|---|---|
| Tragus | Bipolar electrodes placed across the tragus [61]. | High electric field focused on the tragus. | High; significant electric field is largely restricted to the tragus [61]. | Commonly used as an active control site in experimental studies. |
| Cymba Concha | Anode placed in the cymba concha, cathode on earlobe or neck [61]. | High, but dependent on electrode size and current. | Selective for the cymba concha, a region with high vagal nerve innervation. | A primary target for intended vagus nerve activation. |
| Earlobe | Bipolar electrodes placed on the earlobe [61]. | High electric field at the earlobe. | Moderate; significant field can spread to the antitragus [61]. | Often considered a control site due to low vagal innervation. |
High-resolution computational modeling (0.47 mm) of the ear has revealed that current flow patterns are highly specific to the chosen montage [61]. A key finding is that for a fixed current amplitude, reducing electrode size increases the current density and peak electric field in the underlying tissue, thereby enhancing sensitivity. Furthermore, each montage demonstrated relative selectivity for one or two auricular regions, a result that was robust across assumptions of nerve activation thresholds and tissue properties [61]. This allows researchers to select montages that not only target a desired region but also avoid off-target stimulation, thereby improving the interpretability of experimental results.
Experimental Protocols for Montage Validation
The transition from an optimized computational model to an empirically validated protocol requires a structured experimental workflow. The following methodologies are representative of high-quality studies in the field.
Protocol 1: High-Resolution Computational Modeling of taVNS
This protocol outlines the creation of a computational model to analyze current flow in the ear for taVNS [61].
- Head Model Construction: Acquire high-resolution (0.47 mm) T1 and T2-weighted MRI scans of a subject's head, with a focused field-of-view on the ear. Segment the images into distinct tissues (skin, fat, cartilage, bone, muscle, brain, CSF, blood vessels) and further segment the ear into 6 regions of interest (ROIs: cavum concha, cymba concha, crus of helix, tragus, antitragus, earlobe) based on anatomical landmarks and nerve densities.
- Electrode Placement and Meshing: Model electrodes and conductive gel (1 mm thick) in simulation software (e.g., COMSOL Multiphysics). Manually place electrodes over the target ear regions (e.g., tragus, cymba concha). Generate a high-quality, adaptive tetrahedral mesh (>970,000 elements) ensuring solution accuracy.
- Simulation and Analysis: Assign electrical conductivities to all tissues from published literature. Solve the Laplace equation (∇ ⋅ (σ ∇V) = 0) to compute the electric field. Analyze the 99th percentile and mean electric field in each ROI. Calculate sensitivity and selectivity for each montage, considering a range of assumed neural activation thresholds (e.g., 6.15 to 24.6 V/m).
Protocol 2: Optimized tDCS for Motor Cortex in Stroke
This protocol describes a within-subject simulation study to compare optimized and conventional tDCS for stroke patients [63].
- Patient-Specific Model Creation: Use T1-weighted MRI scans of stroke patients. Segment the images into brain tissues (gray matter, white matter), CSF, skull, skin, and the stroke lesion using specialized software (e.g., Neurophet tES LAB). Assign conductivity values, with the stroke lesion typically assigned a conductivity higher than normal brain tissue.
- tDCS Simulation: For the conventional montage, place 5x5 cm electrodes using the 10-20 EEG system (anode on C3/C4 of the affected hemisphere, cathode on the contralateral hemisphere). For the optimized montage, use an optimization algorithm (e.g., a grid search on the scalp surface) to find the anode and cathode positions that maximize the average electric field in a spherical target ROI (e.g., 2 mm radius) centered on the hand knob of the motor cortex.
- Electric Field Comparison: Quantify the average electric field magnitude within the target ROI for both montages. Calculate the percentage improvement of the optimized over the conventional montage. Quantify the difference in electrode positions using Euclidean distance.
Protocol 3: Assessing Montage Effects on Working Memory
This experimental protocol evaluates how different tDCS montages affect cognitive training outcomes [65].
- Participant Selection and Baseline Assessment: Recruit healthy participants and assess their baseline working memory capacity using a standardized task (e.g., a change detection or n-back task).
- Stimulation and Training: Employ a randomized, sham-controlled, crossover design. Participants receive different stimulation conditions (e.g., conventional F4-anode/cheek-cathode, frontoparietal network stimulation, sham) in separate sessions. Stimulation is applied for 20-30 minutes while participants engage in a distractor inhibition (DIIN) training task.
- Post-Stimulation Assessment and Analysis: After stimulation, measure working memory performance again using a transfer task different from the training task. Analyze data using linear mixed-effect modeling to investigate the interaction between electrode montage, baseline working memory capacity, and performance gains.
Workflow Visualization of the Optimization and Validation Pipeline
The following diagram synthesizes the protocols above into a generalized workflow for optimizing and validating an electrode montage, from initial computational design to experimental assessment.
Optimization and Validation Workflow
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of the protocols above relies on a suite of specialized software, hardware, and analytical tools.
Table 3: Essential Research Toolkit for Montage Optimization and Validation
| Tool Category | Specific Examples | Primary Function | Key Consideration |
|---|---|---|---|
| Imaging & Segmentation | 3-T MRI Scanner (e.g., Siemens Prisma); T1/T2-weighted MPRAGE sequences; Segmentation Software (Simpleware ScanIP, FreeSurfer, Neurophet tES LAB) [61] [62] [63]. | Provides anatomical data for constructing realistic head models. | High-resolution scans (e.g., <1 mm) and accurate tissue segmentation are critical for model fidelity. |
| Simulation & Modeling | Finite Element Method (FEM) Solvers (COMSOL Multiphysics, SimNIBS, custom software) [61] [66] [63]. | Solves the Laplace equation to predict current flow and electric fields in the head/ear model. | Software should handle complex geometries and assign anisotropic conductivities (e.g., for white matter). |
| Stimulation Hardware | tDCS/taVNS/tES Stimulator; Ag/AgCl electrodes (large pad or small HD); Conductive gel or paste [61] [28]. | Delivers controlled, low-intensity electrical current to the subject. | Device reliability and safety features (current ramping, impedance monitoring) are paramount. |
| Electrode Design | Rectangular sponges (e.g., 5x5 cm); Circular discs (e.g., 1-3 cm diameter for taVNS); 4x1 HD-ring electrodes [61] [63]. | Determines contact area and initial current density on the skin. | Smaller electrodes generally increase focality but may reduce subject comfort. |
| Experimental Control | EEG 10-20 System Cap; Sham Stimulation Mode; Behavioral Task Software (e.g., PsychoPy, E-Prime) [63] [65] [28]. | Ensures precise, reproducible electrode placement and enables blinding. | Proper sham protocols are essential for controlling for placebo effects. |
| Reporting Guidelines | RATES (Report Approval for Transcranial Electrical Stimulation) Checklist [28]. | Standardizes the reporting of stimulation parameters and study procedures. | Enhances reproducibility and allows for meaningful cross-study comparisons. |
Optimizing electrode montage and current flow is not a mere technical refinement but a fundamental component of rigorous neurostimulation research. As comparative data demonstrates, optimized and high-definition montages can yield electric fields in target structures that are over 50% more intense or substantially more focal than those produced by conventional approaches [61] [63]. The interplay between montage type and individual factors—from brain anatomy to baseline cognitive performance—further underscores the necessity of a personalized, model-informed approach [64] [63] [65]. By adhering to detailed experimental protocols and leveraging the computational and experimental tools outlined in this guide, researchers can enhance the target specificity, efficacy, and reproducibility of neurostimulation protocols, thereby accelerating their translation into validated clinical and research applications.
The Role of In Silico Modeling in Pre-empting Clinical Trial Failures
In silico modeling is fundamentally reshaping the clinical trial landscape by providing powerful computational tools to predict and prevent failures before they occur. By creating digital simulations of diseases, patients, and interventions, researchers can now identify risks related to safety, efficacy, and operational feasibility months before traditional trials would reveal them [68]. This paradigm shift from reactive problem-solving to proactive risk mitigation is particularly valuable in neurostimulation research, where personalization and model validation are critical for success.
Quantitative Comparison of In Silico Applications
Table 1: Performance Comparison of In Silico Modeling Applications in Clinical Trials
| Application Area | Reported Impact | Key Performance Metrics | Therapeutic Area Focus |
|---|---|---|---|
| Trial Failure Prediction | Flags doomed protocols months before first-patient-in [68] | Predicts screen failure, variance inflation, retention collapse [68] | Cross-therapeutic (Oncology, Neurology, Cardiology) |
| Digital Twin Trials | Reduces sample size needs and shortens timelines [69] | 85% predictive accuracy in simulating neuronal responses (Stanford) [70] | Oncology, Neurology, Cardiology [70] |
| Adverse Event Prediction | Addresses 17% of clinical trial failures due to safety concerns [71] | F1-score of 56% for ADE prediction using LLMs [71] | Cross-therapeutic (2,497 drugs evaluated) [71] |
| Personalized Neurostimulation | Significant effects in low baseline performers (p=0.003) [36] | Bayesian Optimization outperforms one-size-fits-all approaches [36] | Neurology (Cognitive Enhancement) |
| Operational Risk Mitigation | Cuts mis-sited starts, avoids month-long customs stalls [68] | Predicts randomization velocity, ePRO fatigue risk, site throughput [68] | Cross-therapeutic |
Table 2: In Silico Trial Adoption by Therapeutic Area and Development Phase
| Therapeutic Area | Market Share (2024) | Projected CAGR | Most Common Trial Phase Application |
|---|---|---|---|
| Oncology | 25.78% [70] | 6.9% [70] | Phase II (34.85% of deployments) [70] |
| Neurology | Fastest-growing discipline [70] | 15.46% [70] | Phase I (13.78% CAGR) [70] |
| Cardiology | Significant segment [70] | Not specified | Phase II and Phase III [70] |
| Infectious Diseases | Established segment [70] | Not specified | Phase I and Phase II [70] |
Experimental Protocols and Methodologies
Protocol 1: AI-Driven Clinical Trial Failure Prediction
This methodology integrates diverse data streams to generate early warnings of trial operational failures [68].
Workflow:
- Data Layer Integration: Combine four data streams: start-up & regulatory (import permits, ethics SLAs), site operations (historical throughput, deviation patterns), patient tech signals (smart-pill ingestion, passive biomarkers), and financials (burn vs. enrollment) [68].
- Feature Engineering: Create leading indicators including predicted randomization velocity by site, weekend ePRO failure risk, ingestion-verification roll-up, and PV precursor rates [68].
- Model Training: Implement a stacked ensemble using gradient boosting for tabular operational signals, temporal models for adherence sequences, and causal forests for "what-if" resiting analysis [68].
- Decision Activation: Trigger pre-specified playbooks when predictions exceed thresholds, such as adding backup sites, widening protocol windows, or changing monitoring modes [68].
AI Failure Prediction Workflow
Protocol 2: Digital Twin-Enhanced Randomized Clinical Trials
This approach uses AI-generated digital twins to create synthetic control arms and optimize trial design, reducing the need for traditional placebo groups [69].
Workflow:
- Data Collection & Virtual Patient Generation: Gather comprehensive patient data including symptoms, biomarkers, imaging, genetic profiles, and lifestyle factors. Augment with historical control datasets from previous trials and real-world evidence [69].
- Virtual Cohort Simulation: Create two complementary groups: synthetic controls (digital twins receiving standard care) and virtual treatment groups (digital twins receiving investigational therapy) [69].
- Predictive Modeling & Optimization: Continuously refine digital twins using predictive modeling techniques. Employ SHapley Additive exPlanations (SHAP) for model transparency and interpretability [69].
- Validation & Integration: Rigorously validate digital twins against real-world clinical trial data. Integrate findings with traditional trial data to enhance statistical power and generalizability [69].
Digital Twin Trial Workflow
Protocol 3: AI-Optimized Personalized Neurostimulation
This protocol validates computational models for neurostimulation parameters using Bayesian optimization to enhance sustained attention in home-based settings [36].
Workflow:
- Algorithm Development: Develop a personalized Bayesian Optimization (pBO) algorithm that establishes the relationship between current intensity and baseline cognitive performance, accounting for individual anatomical differences like head circumference [36].
- In Silico Modeling: Compare pBO against alternative optimization methods (Random Search, non-personalized Bayesian Optimization) using the Ackley function to evaluate performance under varying noise conditions [36].
- Experimental Validation: Conduct a double-blind, sham-controlled study comparing pBO-optimized tRNS against one-size-fits-all tRNS and sham stimulation in a new participant sample [36].
- Analysis: Use mixed-effects linear regression with random effects for participant and session to evaluate effects on sustained attention performance, with separate analysis for high and low baseline performers [36].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagents and Computational Tools for In Silico Modeling
| Tool/Reagent | Function/Purpose | Example Applications |
|---|---|---|
| ClinicalTrials.gov Dataset | Provides structured clinical trial results for model training and validation [71] | Adverse drug event prediction benchmarks (CT-ADE) [71] |
| MedDRA Ontology | Standardized medical terminology for adverse event classification [71] | System Organ Class and Preferred Term level ADE labeling [71] |
| AlphaFold2 Models | AI-predicted protein structures for drug target analysis [72] | GPCR structure-based drug discovery [72] |
| Digital Twin Platforms | Create virtual patient cohorts for simulation and control arms [69] [70] | Synthetic control arms in oncology trials [70] |
| SHAP Analysis | Explains machine learning model outputs and feature importance [69] | Model transparency in digital twin validation [69] |
| Bayesian Optimization Algorithms | Personalizes intervention parameters based on individual response [36] | Neurostimulation parameter optimization for sustained attention [36] |
| ASME V&V 40 Framework | Provides standardized verification and validation principles for computational models [70] [73] | Regulatory submission preparation for in silico evidence [70] |
In silico modeling represents a transformative approach to clinical development, offering researchers powerful tools to pre-empt multiple failure pathways. The integration of digital twins, AI-based predictive analytics, and rigorously validated computational models enables unprecedented capabilities in risk identification and mitigation. For neurostimulation research specifically, the combination of personalized optimization algorithms with robust validation frameworks provides a pathway to more effective and reliable therapeutic outcomes. As regulatory acceptance grows and methodologies standardize, these computational approaches will become increasingly integral to efficient and successful clinical development across therapeutic areas.
Benchmarks and Standards: Assessing Model Performance Against Established Metrics
In computational model validation for neurostimulation protocols research, quantifying predictive accuracy is not merely a procedural step but a fundamental requirement for scientific credibility and clinical applicability. Predictive accuracy is formally defined as the success of a predictive model in forecasting outcomes based on past data [74]. In the high-stakes domain of neurostimulation, where computational models guide therapeutic interventions, a model's performance on unseen data separates theoretical promise from practical utility. The validation process determines how well a hypothesis or model fits new, unseen data, measured as the expected log-likelihood for newly sampled data generated by the true hypothesis [74].
The challenge researchers face is validity shrinkage—the nearly inevitable reduction in predictive ability that occurs when a model derived from one dataset is applied to a new dataset [75]. This phenomenon is particularly relevant in computational neuroscience, where biological variability, measurement noise, and individual patient differences can significantly impact model generalizability. Under some circumstances, predictive validity can be reduced to nearly zero, rendering clinically deployed models ineffective or even dangerous [75]. This article provides a comprehensive framework for quantifying validation success through appropriate metrics, methodologies, and reporting standards specifically contextualized for neurostimulation research.
Classification Metrics: Evaluating Categorical Outcomes
Core Metrics and Their Clinical Interpretation
Classification models in neurostimulation research often predict categorical outcomes such as treatment response categorization, stimulation efficacy thresholds, or adverse event risk stratification. The confusion matrix provides the foundation for most classification metrics by summarizing correct and incorrect predictions for each class [74] [76]. The table below summarizes key classification metrics and their research applications.
Table 1: Classification Metrics for Predictive Model Validation
| Metric | Formula | Research Application | Advantages | Limitations |
|---|---|---|---|---|
| Accuracy | (TP+TN)/(TP+TN+FP+FN) [76] | Overall model performance assessment; initial screening metric | Intuitive interpretation; provides single-figure summary [76] | Misleading with class imbalance; insensitive to error type costs [74] [76] |
| Recall (Sensitivity) | TP/(TP+FN) [76] | Identifying true responders to neurostimulation; safety monitoring for adverse events | Emphasizes false negative reduction; crucial when missing positives is costly [76] | May increase false positives; fails to account for incorrectly classified negatives |
| Precision | TP/(TP+FP) [76] | Confirming true treatment effects; validating target engagement | Measures prediction reliability; important when false positives are costly [76] | Does not account for false negatives; can be high even with many missed positives |
| F1 Score | 2×(Precision×Recall)/(Precision+Recall) [76] | Balanced assessment in imbalanced datasets; comprehensive single metric | Harmonic mean balances precision and recall; better for imbalanced data than accuracy [76] | Obscures which metric (precision or recall) is weaker; assumes equal cost for FP and FN |
| Specificity | TN/(TN+FP) [76] | Ruling out non-responders; identifying patients unlikely to benefit | Measures ability to identify true negatives; complements sensitivity | Not focused on positive class identification; may be less relevant for rare events |
| AUC-ROC | Area under ROC curve [74] | Overall discriminative ability across all thresholds; model comparison | Threshold-independent; measures separability between classes [74] | Can be optimistic with class imbalance; does not reflect calibration performance |
Metric Selection Guidelines for Neurostimulation Research
Choosing appropriate classification metrics requires careful consideration of the clinical and research context. For neural activation prediction or treatment response classification, recall (sensitivity) often takes priority when false negatives carry significant clinical risk, such as failing to identify patients who would benefit from therapy [76]. Conversely, precision becomes critical when false positives could lead to unnecessary interventions with potential side effects [76].
In imbalanced datasets common in neurostimulation research (where non-responders may outnumber responders), the F1-score provides a more meaningful measure than accuracy, as it balances precision and recall [74] [76]. For example, in a dataset where only 10% of patients are responders, a model that predicts all patients as non-responders would achieve 90% accuracy while being clinically useless. The Area Under the Receiver Operating Characteristic Curve (AUC-ROC) offers a comprehensive threshold-independent measure of a model's ability to discriminate between classes, making it particularly valuable for comparing different modeling approaches [74].
Regression Metrics: Evaluating Continuous Outcomes
Metric Definitions and Research Applications
Regression models in neurostimulation research typically predict continuous outcomes such as stimulation intensity parameters, symptom reduction scores, or neural activation volumes. Unlike classification metrics that focus on correctness categories, regression metrics quantify the magnitude of prediction errors. The table below compares essential regression metrics for model validation.
Table 2: Regression Metrics for Predictive Model Validation
| Metric | Formula | Scale | Research Application | Interpretation |
|---|---|---|---|---|
| Mean Absolute Error (MAE) | Σ|yi-ŷi|/n [77] [74] | Same as outcome variable | Error magnitude in clinically meaningful units (e.g., mA, mV) | Average absolute prediction error; easily interpretable |
| Mean Squared Error (MSE) | Σ(yi-ŷi)²/n [77] [74] | Squared units of outcome | Emphasizing larger errors; optimization objective | Punishes larger errors more severely; less intuitive units |
| Root Mean Squared Error (RMSE) | √MSE [74] | Same as outcome variable | Clinical error assessment with emphasis on outliers | More sensitive to outliers than MAE; preserves units |
| R-squared (R²) | 1 - (SSres/SStot) [77] [74] | 0 to 1 (or 0-100%) | Proportion of variance explained; model utility assessment | Proportion of outcome variance explained by predictors |
| Adjusted R-squared | 1 - [(1-R²)(n-1)/(n-k-1)] [75] | 0 to 1 (or 0-100%) | Variance explained with parameter penalty | Adjusts for number of predictors; prevents overfitting |
Clinical Interpretation of Regression Metrics
In neurostimulation research, the clinical relevance of regression metrics must guide their interpretation. Mean Absolute Error (MAE) provides the most intuitive measure as it represents the average magnitude of prediction errors in the original units of measurement (e.g., milliamps for stimulation intensity) [77]. Mean Squared Error (MSE) and Root Mean Squared Error (RMSE) give greater weight to larger errors, which is crucial when significant deviations from predicted values could lead to adverse events or therapeutic failure [74].
The R-squared (R²) value indicates the proportion of variance in the outcome explained by the model, helping researchers determine whether a model captures meaningful relationships or merely describes noise [77] [74]. However, R² can be artificially inflated by adding predictors, making Adjusted R-squared preferable for comparing models with different numbers of parameters [75]. For computational models predicting neural activation volumes, even modest R² values may represent significant scientific advances given the complexity of neural systems.
Validation Methodologies: Ensuring Reliable Performance Estimation
Core Validation Techniques
Proper validation methodologies are essential for accurate performance estimation, as they quantify the expected validity shrinkage when models are applied to new data [75]. The diagram below illustrates a comprehensive validation workflow for neurostimulation computational models.
Figure 1: Comprehensive Validation Workflow for Predictive Models
Holdout validation involves splitting data into separate training and testing sets, providing an straightforward estimate of how the model will perform on unseen data [74] [75]. The key advantage is simplicity, but the results can be highly sensitive to how the data is partitioned, particularly with smaller datasets common in neurostimulation research.
Cross-validation, particularly k-fold cross-validation, provides more robust performance estimates by partitioning the data into k subsets and repeatedly training the model on k-1 subsets while testing on the remaining subset [77] [75]. This process is repeated k times, with each subset serving as the test set once. Leave-one-out cross-validation (LOOCV) represents an extreme case where k equals the number of observations, providing nearly unbiased estimates but with high computational cost [75].
Bootstrap validation involves drawing multiple random samples with replacement from the original dataset, providing information on the stability and variability of performance estimates [75]. Bootstrap methods are particularly valuable for calculating confidence intervals around performance metrics and applying bias correction to address optimistic performance estimates.
Advanced Considerations for Neurostimulation Research
In neurostimulation research, temporal validation is often necessary when models predict outcomes across time, requiring specific validation approaches that respect temporal ordering. Similarly, spatial validation is crucial for models predicting effects across different brain regions or electrode configurations.
External validation represents the gold standard, where models are tested on completely independent datasets collected under different conditions, at different sites, or with different patient populations [75]. For example, a computational model of deep brain stimulation effects validated on rodent data showed approximately 32.93% variation in the volume of tissue activated across different characterized electrodes, highlighting the importance of electrode-specific validation [78].
Experimental Protocols for Validation
Standardized Experimental Workflow
Rigorous validation requires standardized experimental protocols to ensure reproducible and comparable results. The diagram below outlines a comprehensive protocol for validating computational models in neurostimulation research.
Figure 2: Experimental Protocol for Model Validation
The experimental protocol begins with pre-modeling planning, where researchers define the hypothesis to test and select appropriate statistical tools before embarking on experiments [79]. This includes determining sample size requirements, ensuring adequate statistical power, and planning for potential confounding factors specific to neurostimulation research, such as individual neuroanatomical variations or electrode placement uncertainties.
During the modeling phase, feature engineering and selection techniques help identify the most relevant predictors while reducing redundancy [74]. Hyperparameter optimization methods, such as grid search with cross-validation, systematically identify optimal parameter combinations to maximize model performance [74]. For computational models of deep brain stimulation, this might include optimizing parameters related to tissue conductivity, electrode geometry, or neural activation thresholds.
The validation phase implements the methodologies described in Section 4, with particular attention to avoiding optimistic bias. Researchers should explicitly test statistical assumptions, including normality of data distribution and independence of samples, as violations can significantly impact the validity of conclusions [79]. In neurostimulation research, where repeated measurements are common, specialized statistical tests for dependent data (e.g., ANOVA with repeated measures) may be necessary [79].
Finally, the reporting phase requires comprehensive documentation of all metrics, validation procedures, and clinical implications. Transparent reporting of both successful and failed validation attempts enables the research community to accurately assess model utility and build upon existing work.
Research Reagent Solutions for Neurostimulation Validation
Table 3: Essential Research Reagents and Tools for Neurostimulation Model Validation
| Category | Specific Tool/Technique | Function in Validation | Example Applications |
|---|---|---|---|
| Statistical Software | R, Python (scikit-learn) | Implementation of validation metrics and procedures | Cross-validation, bootstrap, performance metric calculation |
| Computational Modeling | Finite Element Method (FEM) Solvers | Simulation of neurostimulation electric fields | Predicting volume of tissue activated in DBS [78] |
| Data Collection Tools | Impedance Spectroscopy | Electrode characterization and validation | In vitro electrode model validation before implantation [78] |
| Validation Frameworks | Custom Validation Pipelines | Structured validation workflow implementation | Integrating multiple validation methods for robust assessment |
| Performance Metrics | Classification/Regression Metrics | Quantitative performance assessment | Accuracy, precision, recall, MAE, R² calculation |
| Visualization Tools | MATLAB, Python (Matplotlib) | Results presentation and interpretation | ROC curves, residual plots, prediction visualizations |
Addressing Common Challenges in Predictive Validation
Mitigating Overfitting and Underfitting
Overfitting occurs when a model captures noise in the training data rather than the underlying relationship, resulting in excellent training performance but poor generalization to new data [77] [74]. In neurostimulation research, this might manifest as a computational model that perfectly predicts neural activation in the training dataset but fails with new electrode configurations or patient anatomies.
Strategies to mitigate overfitting include:
- Regularization techniques (L1/L2 penalties) that constrain model complexity [74]
- Feature selection to eliminate redundant predictors [77] [74]
- Ensemble methods (bagging, boosting) that combine multiple models to reduce variance [74]
- Simplifying model architecture when working with limited data
Conversely, underfitting occurs when models are too simplistic to capture underlying relationships, characterized by high bias and low variance [77] [74]. This might manifest as a stimulation model that fails to account for non-linear neural responses. Addressing underfitting typically requires increasing model complexity, adding relevant features, or reducing regularization.
The bias-variance tradeoff represents the balance between these two extremes, where models with high bias underfit and those with high variance overfit [77] [74]. Finding the optimal balance requires iterative validation with appropriate metrics.
Handling Imbalanced Datasets
Imbalanced datasets, where one class is significantly underrepresented, present particular challenges in neurostimulation research. For example, serious adverse events may be rare but critically important to predict. In such cases, standard accuracy metrics become misleading, as a model that always predicts "no adverse event" would achieve high accuracy while being clinically useless [74] [76].
Strategies for imbalanced datasets include:
- Metric selection: Preferring F1-score, precision-recall curves, or weighted accuracy over standard accuracy [74] [76]
- Resampling techniques: Oversampling the minority class or undersampling the majority class
- Cost-sensitive learning: Assigning higher misclassification costs to the minority class
- Anomaly detection approaches: Treating the problem as outlier detection rather than classification
Managing Data Dependency and Generalizability
Data dependency occurs when a model's predictions rely heavily on specific correlated variables, reducing generalizability across different populations or conditions [74]. In neurostimulation research, this might manifest as a model that works well for specific electrode geometries but fails with different designs.
Techniques to improve generalizability include:
- Feature engineering to create more robust representations [74]
- Domain adaptation methods to adjust models for new conditions
- Incorporating domain expertise to identify biologically plausible features
- Multi-center validation to ensure performance across different populations
Comprehensive reporting of validation results is essential for advancing neurostimulation research. Researchers should:
- Report multiple metrics to provide a complete picture of model performance, including both discrimination and calibration measures [76] [75]
- Always estimate and report expected validity shrinkage using cross-validation, bootstrap methods, or adjusted performance metrics [75]
- Provide confidence intervals for performance metrics to communicate estimation uncertainty
- Contextualize performance relative to clinical requirements and existing alternatives
- Document the entire validation protocol to enable replication and comparison
For computational models in neurostimulation research, validation should become an iterative process throughout model development rather than a final step before publication. By adopting rigorous, standardized approaches to quantifying predictive accuracy, researchers can develop more reliable models that accelerate progress in neuromodulation therapies and improve patient outcomes.
Comparative Analysis of Neurostimulation Modalities (tDCS, TMS, TI) Using Validated Models
The evolution of non-invasive brain stimulation has been marked by a continuous effort to overcome the fundamental trade-off between stimulation depth and spatial resolution. Traditional techniques like transcranial direct current stimulation (tDCS) and transcranial magnetic stimulation (TMS) have provided neuroscientists with valuable tools for neuromodulation but face inherent limitations in precisely targeting deep brain structures without affecting superficial cortical regions [80]. The emergence of temporal interference (TI) stimulation represents a significant advancement, utilizing the interference pattern of multiple high-frequency electric fields to generate a amplitude-modulated envelope that can selectively stimulate deep neural tissues [81] [82]. Within this context, computational models have become indispensable for validating stimulation protocols, predicting electric field distributions, and optimizing parameters for specific neural targets before clinical implementation [78]. This review provides a comparative analysis of these neurostimulation modalities through the lens of computational model validation, examining their respective mechanisms, experimental efficacy, and protocol standardization for research and clinical applications.
Fundamental Principles and Mechanisms
Comparative Technical Specifications
Table 1: Fundamental characteristics of major neurostimulation modalities.
| Feature | tDCS / HD-tDCS | TMS | Temporal Interference (TI) |
|---|---|---|---|
| Primary Mechanism | Modulates neuronal membrane potential via constant low-intensity direct current [81] [83] | Induces neuronal firing via rapidly changing magnetic fields generating intracranial electric currents [80] | Uses interfering high-frequency electric fields (e.g., 2 kHz & 2.02 kHz) to create a low-frequency envelope (e.g., 20 Hz) [81] [82] |
| Spatial Resolution | Limited (HD-tDCS offers improved focality) [81] | Moderate (diffusion with depth) [80] | High (theoretically superior focality for deep targets) [81] [82] |
| Stimulation Depth | Superficial cortical layers [81] | Cortical and shallow subcortical regions [80] | Designed for deep brain regions (e.g., hippocampal formation, basal ganglia) [82] [80] |
| Cell Specificity | Low (affects all neural elements in field) [80] | Low [80] | Low (inherent to electrical stimulation) [80] |
| Computational Validation Role | Predicting current flow and optimal electrode montages [81] | Modeling magnetic field-to-electric field coupling and distribution [80] | Critical for predicting the locus and shape of the interference envelope [78] [82] |
Signaling Pathways and Neuronal Activation
The following diagram illustrates the fundamental mechanisms through which each modality interacts with neural tissue.
Figure 1: Key signaling pathways for tDCS, TMS, and TI stimulation. The diagram illustrates how each modality initiates distinct physical processes (constant current, induced fields, or field interference) that ultimately converge on the modulation of spontaneous neuronal activity, leading to changes in brain function and behavior. The "low-pass filter" effect is critical for TI, where neurons respond to the low-frequency interference envelope while ignoring the high-frequency carriers [82] [80].
Experimentally Validated Protocols and Outcomes
Key Experimental Methodologies
Validation of computational models requires comparison with robust empirical data. The following experimental protocols represent validated approaches for evaluating the effects of different neurostimulation techniques.
Protocol 1: Comparative Modulation of Spontaneous Neuronal Activity (fMRI) This protocol directly compares TI and HD-tDCS using resting-state functional MRI (fMRI) [81].
- Participants: 40 right-handed healthy adults.
- Design: Randomized, crossover design with a 48-hour washout period.
- Stimulation Parameters:
- TI: Targeting left primary motor cortex (M1) via electrode square (4 cm sides). Channels: 2000 Hz and 2020 Hz at 2 mA each, generating a 20 Hz envelope.
- HD-tDCS: 4×1 ring configuration centered on C3, with current weights: C3: 2000 μA; P3: -774 μA; T7: -684 μA; Cz: -542 μA.
- Duration: 20 minutes per session, including 30-second ramp-up/down.
- Data Acquisition: Resting-state fMRI collected pre-stimulus, during first/second half of stimulation, and post-stimulus.
- Key Metrics: Regional Homogeneity (ReHo), dynamic ReHo (dReHo), fractional amplitude of low-frequency fluctuations (fALFF), and dynamic fALFF.
- Computational Link: fMRI outcomes provide a physiological benchmark for validating models that simulate the electric field's impact on neural network activity.
Protocol 2: TI for Lower Limb Motor Function This protocol validates TI's ability to modulate deep motor areas controlling lower limbs [82].
- Participants: 46 healthy males, randomized into TI or sham groups.
- Stimulation Parameters: Electrodes at F3-P3 (2000 Hz) and F4-P4 (2020 Hz), 2 mA peak-to-peak, 20 Hz envelope difference. Target: M1 leg area in the longitudinal fissure.
- Design: Double-blinded, sham-controlled. Real stimulation: 20 minutes twice daily for 5 days. Sham: identical setup with 30-second ramp-up/down only.
- Outcome Measures: Vertical jump height (Countermovement Jump, Squat Jump), dynamic postural stability (Y-balance test).
- Computational Link: Electric field simulations of the electrode montage (e.g., using SimNIBS) are used to confirm field overlap and maximal intensity in the targeted deep leg area.
Table 2: Experimentally observed effects of different neurostimulation protocols.
| Modality / Protocol | Neural/Biomarker Outcomes | Behavioral/Task Performance Outcomes | Sustained Effects |
|---|---|---|---|
| TI (M1, 20 Hz) | Significantly increased ReHo and fALFF in sensorimotor regions during and after stimulation [81]. Enhanced functional connectivity between M1 and secondary motor areas [82]. | Improved motor learning [81]. Significant increase in vertical jump height (CMJ: F=8.858, p=0.005; SJ: F=6.523, p=0.015) [82]. | Effects on spontaneous neuronal activity persisted into post-stimulation period [81]. 5-day repetitive protocol induced lasting behavioral change [82]. |
| HD-tDCS (M1) | Enhanced fALFF in real-time, but less pronounced than TI. Impact on ReHo was more limited and less sustained [81]. | Modulates cognitive function and neurophysiological activity [81]. | Significant activity was not maintained post-stimulation [81]. |
| tDCS (Prefrontal, 2 mA) | Modulates activity in dlPFC and default mode network connectivity [83]. | Mixed results on sustained attention and inhibitory control; combination with VR mindfulness showed non-significant cognitive effects [83]. | Typically requires repeated sessions for lasting effects. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key materials and computational tools for neurostimulation research.
| Item / Solution | Function / Application | Representative Examples / Notes |
|---|---|---|
| TI Stimulation System | Generates and delivers two or more high-frequency alternating currents with precise frequency and amplitude control. | Custom systems using MATLAB, converters (e.g., National Instruments USB-6361), and stimulus isolators (e.g., WPI A395) [82]; Commercial devices (e.g., Soterix Medical) [81]. |
| HD-tDCS System | Delivers transcranial direct current via multiple compact electrodes for focused stimulation. | DC-STIMULATOR PLUS (NeuroCnn) with 4×1 ring electrode configuration [81]. |
| Computational Modeling Software | Predicts electric field distribution, optimizes electrode placement, and validates targeting pre-experiment. | SimNIBS [81]: Finite element method for tDCS/TMS/TI field modeling. Custom models for TI interference envelope prediction. |
| MRI-Compatible Electrodes | Allows for concurrent brain stimulation and functional or structural MRI data acquisition. | MRI-compatible rubber electrodes for HD-tDCS [81]. |
| Validation & Calibration Workflow | Reduces model uncertainty by incorporating empirical electrode characterization and in vivo impedance. | Microscope and impedance spectroscopy for electrode geometry validation; in vivo calibration [78]. |
| AI Personalization Algorithm | Optimizes stimulation parameters (e.g., current intensity) based on individual anatomy and baseline performance. | Personalized Bayesian Optimization (pBO) using head circumference and baseline cognitive scores [36]. |
Computational Validation Workflow
The reliability of neurostimulation models depends on rigorous validation workflows, as illustrated below.
Figure 2: Computational model validation workflow. This iterative process, essential for credible predictions, involves building a simulation from anatomical data, then refining it using empirical electrode characterization and in vivo measurements. This workflow can increase tissue activation prediction accuracy by up to ~33% [78].
Discussion and Future Directions
The comparative analysis indicates that TI stimulation offers a theoretically superior profile for targeting deep brain structures with potentially higher spatial precision compared to tDCS and TMS. Experimental evidence confirms its capacity to induce significant and sustained modulation of spontaneous neuronal activity and to enhance motor performance, validating initial computational predictions [81] [82]. However, the technology is still exploratory, with human trials producing sometimes inconsistent results, necessitating further refinement of stimulation regimens [7] [82].
The critical role of computational models in this evolution cannot be overstated. As evidenced, workflows that integrate ex vivo characterization and in vivo calibration are paramount, significantly enhancing the predictive power for neural activation [78]. Future developments will likely involve the convergence of multiple advanced technologies. These include:
- Novel Multi-Target Techniques: Methods like transcranial magneto-acoustic coupling electrical stimulation (TMAES) are being developed to achieve synchronous multi-target focused electrical stimulation in the deep brain, addressing a key limitation of existing techniques [7].
- AI-Driven Personalization: The integration of artificial intelligence, such as personalized Bayesian Optimization (pBO), allows for the automatic adjustment of stimulation parameters based on individual anatomy and baseline performance, moving beyond "one-size-fits-all" approaches [36].
- Enhanced Model Specificity: Future models must evolve to predict not just the location and intensity of the electric field, but also its effects on specific cell types and neural circuits, potentially by integrating multimodal data.
In conclusion, while tDCS, TMS, and TI each occupy a unique niche in the neuromodulation landscape, the continued validation and refinement of their underlying computational models are essential for translating their theoretical advantages into safe, effective, and reliable protocols for both scientific research and clinical treatment.
In the rapidly advancing fields of computational model validation and neurostimulation protocols research, the challenge of reproducibility represents a significant barrier to scientific progress and clinical translation. Reproducibility ensures that research findings can be independently verified, a fundamental principle of scientific integrity that is particularly crucial when developing therapeutic interventions for human health. Within transcranial electrical stimulation (tES) research specifically, subtle variations in experimental parameters can dramatically alter outcomes, potentially reversing the intended effects of stimulation [28]. This sensitivity underscores why standardized reporting is not merely an academic exercise but an essential requirement for building a reliable evidence base.
The scientific community has responded to reproducibility challenges by developing specialized reporting checklists that provide structured frameworks for documenting research methodologies. These tools aim to enhance transparency, improve the interpretability of findings, and facilitate meaningful comparisons across studies. The Report Approval for Transcranial Electrical Stimulation (RATES) checklist emerges from this landscape as a consensus-based solution specifically designed for tES research [28]. Similar initiatives have been developed for related fields, including the TECH-VER checklist for health economic models [84] and the CONSORT-iNeurostim extension for randomized controlled trials of implantable neurostimulation devices [85]. Each represents a targeted approach to addressing the unique reproducibility challenges within their respective domains.
The RATES Checklist: Development and Structure
Consensus-Based Development Methodology
The RATES checklist was developed through a rigorous, systematic process designed to achieve expert consensus. Researchers employed a Delphi approach conducted across three rounds involving 38 international experts in tES research [28]. This methodological choice is particularly significant, as the Delphi technique is specifically recognized for its effectiveness in building consensus among experts on complex topics through sequential questionnaires interspersed with controlled feedback [28]. The development process began with a comprehensive literature review to identify potential reporting items, which were then categorized into five domains: participants, stimulation device, electrodes, current, and procedure [28].
Throughout the Delphi process, experts rated the importance of each potential item using a five-point Likert scale and had opportunities to suggest new items or revisions to existing ones [28]. The steering committee utilized specific metrics to assess consensus, including interquartile deviation, percentage of positive responses, and mean importance ratings. This systematic approach led to the retention of 66 out of an initial 70 items, which were subsequently distilled into a shorter version containing 26 items deemed essential for reporting [28]. The consensus-driven development methodology ensures that the resulting checklist represents collective expert opinion rather than the perspective of any single research group, enhancing its credibility and likely adoption across the field.
Comprehensive Structure and Reporting Domains
The RATES checklist organizes reporting requirements across five critical domains of tES research, providing a comprehensive framework that addresses the technical complexity of stimulation protocols. The complete checklist includes 66 items distributed as follows: participants (12 items), stimulation device (9 items), electrodes (12 items), current (12 items), and procedure (25 items) [28]. This extensive coverage ensures that researchers document all parameters that could potentially influence stimulation effects and study outcomes.
The essential version of the checklist condenses these requirements to 26 critical items, prioritizing parameters that most substantially affect outcomes and reproducibility. For example, the electrodes domain includes specifications for electrode size, shape, placement, and orientation, while the current domain addresses waveform parameters, current intensity, and duration [28]. The detailed procedural domain encompasses aspects such as participant preparation, blinding methods, and environmental conditions during stimulation. This structured yet flexible approach allows researchers to focus on the most crucial reporting elements while maintaining the option for more comprehensive documentation when necessary.
Comparative Analysis of Reporting Standards
Tabular Comparison of Neurostimulation Reporting Guidelines
Table 1: Comparison of Key Reporting Guidelines in Neurostimulation and Computational Modeling
| Checklist | Primary Application | Development Method | Number of Items | Key Focus Areas |
|---|---|---|---|---|
| RATES [28] | Transcranial electrical stimulation (tES) | Delphi consensus (38 experts, 3 rounds) | 66 (full), 26 (essential) | Participants, stimulation device, electrodes, current, procedure |
| CONSORT-iNeurostim [85] | Implantable neurostimulation device trials | Delphi survey (132 respondents), consensus meeting | 7 new items + 14-item sub-checklist | Neurostimulation intervention, blinding, temporary trial phases, programming parameters |
| TECH-VER [84] | Health economic decision models | Systematic review + iterative testing | 5 domains | Input calculations, event-state calculations, result calculations, uncertainty analysis, overall checks |
| GRADE Checklist [86] | Evidence quality assessment for healthcare interventions | Logic model development + validation | Variable by application | Risk of bias, inconsistency, indirectness, imprecision, publication bias |
Specialized Applications and Methodological Approaches
Each reporting guideline presented in Table 1 addresses distinct aspects of the reproducibility challenge through specialized methodological approaches. The RATES checklist focuses specifically on the technical parameters of non-invasive stimulation techniques such as tDCS, tACS, and tRNS, which have gained substantial momentum as both research and therapeutic tools [28]. In contrast, CONSORT-iNeurostim addresses the unique methodological challenges of implantable neurostimulation devices, including aspects such as the role of temporary trial phases in participant enrollment and detailed programming parameters [85].
The TECH-VER checklist employs a fundamentally different approach tailored to computational model verification, recommending specific testing methodologies including black-box testing (checking if model calculations align with a priori expectations), white-box testing (line-by-line code examination), and model replication [84]. Meanwhile, the GRADE checklist system focuses on rating the quality of evidence across studies, addressing factors such as risk of bias, inconsistency, indirectness, imprecision, and publication bias [86]. This diversity of approaches highlights how reporting standards must be tailored to specific research methodologies while sharing the common goal of enhancing reproducibility and scientific rigor.
Experimental Evidence Supporting Standardized Reporting
Quantitative Assessment of Reporting Completeness
Table 2: Documented Improvements from Implementing Reporting Guidelines
| Reporting Guideline | Documented Impact | Evidence Source |
|---|---|---|
| CONSORT Statement | Improved quality of RCT reporting; reduced methodological deficiencies | Systematic reviews of clinical trials [85] |
| RATES Checklist | Addressing methodologically induced variability of stimulation effects | Expert consensus on parameter optimization [28] |
| TECH-VER Checklist | Systematic identification of model implementation errors and root causes | Application to models built in different software by various stakeholders [84] |
| GRADE Approach | More transparent judgements about quality of evidence; improved consistency | Evaluation of inter-rater agreement [86] |
Methodological Framework for Verification and Validation
The experimental support for standardized reporting extends beyond simple completeness metrics to encompass sophisticated methodological frameworks for verification and validation. The TECH-VER checklist, for instance, provides a systematic approach to technical verification of health economic models through a hierarchical testing structure [84]. This framework begins with black-box testing to verify that model calculations align with expectations, proceeds to white-box testing with detailed code examination when unexpected results occur, and resorts to model replication only when necessary to resolve persistent issues [84].
In finite element analysis (FEA) for biomechanical investigations, reporting checklists have been developed specifically to address verification and validation processes, aiming to minimize serious errors in computational modeling and improve credibility in clinical applications [87]. Similarly, in artificial intelligence research, reproducibility checklists require documentation of computing infrastructure, hyperparameter specifications, statistical testing methods, and code availability [88]. These methodological frameworks share a common emphasis on transparency, comprehensive documentation, and independent verifiability as essential components of reproducible science.
Implementation Workflow for Reporting Standards
Diagram 1: Research workflow integrating reporting standards at key stages. Implementation begins with selecting appropriate domain-specific guidelines and continues through comprehensive documentation and verification processes.
Essential Research Toolkit for Neurostimulation Studies
Critical Materials and Methodological Components
Table 3: Essential Research Reagent Solutions for Neurostimulation Studies
| Tool/Resource | Function/Purpose | Implementation Example |
|---|---|---|
| Stimulation Device | Generates and delivers precise electrical currents to target neural tissue | tES devices capable of delivering tDCS, tACS, or tRNS with precise parameter control [28] |
| Electrode Assembly | Interfaces between device and subject, determining current flow and distribution | Electrodes of specific size, shape, composition, and positioning via montage-specific holders [28] |
| Computational Models | Predict current flow and optimize stimulation parameters for target engagement | Finite element models of current propagation; dose-control algorithms [28] |
| Blinding Protocols | Minimize participant and experimenter bias through controlled conditions | Sham stimulation capabilities with automated fading; separate staff for programming and application [85] |
| Parameter Documentation | Ensures comprehensive reporting of all relevant stimulation details | RATES checklist implementation; laboratory-specific standard operating procedures [28] |
Integration of Verification and Validation Tools
Beyond the physical components listed in Table 3, successful implementation of reporting standards requires integration of specialized verification and validation tools. For computational model validation, the TECH-VER checklist provides a structured approach to identifying implementation errors through systematic testing protocols [84]. Similarly, for finite element analysis in biomechanical investigations, specialized reporting checklists have been developed to define recommendations for verification and validation processes, addressing issues that commonly arise when using computational models in clinical applications [87].
In the context of artificial intelligence and machine learning applications, reproducibility checklists require documentation of computing infrastructure, including GPU/CPU models, memory specifications, operating systems, and software library versions [88]. They also mandate detailed reporting of hyperparameters, evaluation metrics, and statistical testing methods. These tools collectively form an essential ecosystem for ensuring that neurostimulation research meets the highest standards of methodological rigor and reproducibility, regardless of the specific techniques or technologies employed.
The implementation of structured reporting standards such as the RATES checklist represents a fundamental shift toward enhanced reproducibility in neurostimulation and computational modeling research. By providing comprehensive, consensus-based frameworks for documenting critical methodological details, these checklists address the pervasive challenge of methodologically induced variability that has hampered progress in these fields. The experimental evidence demonstrates that standardized reporting not only improves the transparency and completeness of individual studies but also enables more meaningful comparisons across studies and more reliable meta-analytic approaches [28] [85].
As the field continues to evolve, the ongoing development and refinement of reporting standards will be essential for maintaining scientific integrity and public trust. The successful implementation of these guidelines requires collective commitment from researchers, reviewers, journal editors, and funding agencies to establish a culture where comprehensive reporting is recognized as essential rather than optional. Through this collaborative effort, the neurostimulation research community can accelerate the translation of scientific discoveries into effective clinical applications while upholding the fundamental principles of scientific rigor and reproducibility.
The field of neurostimulation is undergoing a rapid transformation, moving beyond conventional methodologies to a new era defined by novel protocols and advanced computational tools. This evolution is critical for refining therapeutic outcomes for chronic neurological and pain conditions. Framing this progress within the context of computational model validation ensures that innovations are not merely empirical but are grounded in robust, predictable science. This guide provides an objective, data-driven comparison of next-generation neurostimulation protocols against established conventional methods, focusing on efficacy, methodological rigor, and the tools that underpin modern research.
Quantitative Efficacy Comparison: Novel vs. Conventional Neurostimulation
Direct comparisons from randomized controlled trials (RCTs) provide the most compelling evidence for the superiority of novel neurostimulation algorithms. The data below summarize key findings in spinal cord stimulation (SCS), a domain with well-defined conventional and novel paradigms.
Table 1: Comparative Long-Term Efficacy of Spinal Cord Stimulation (SCS) Protocols
| Stimulation Protocol | Theoretical Basis | Key Parameters | 24-Month Back Pain Responder Rate* | 24-Month Leg Pain Responder Rate* | Key Advantages |
|---|---|---|---|---|---|
| Conventional SCS | Gate Control Theory | 40-60 Hz, 300-600 μs [89] | 49.3% [89] | 49.3% [89] | Long-standing clinical history |
| Novel Protocol: HF10 SCS | Paresthesia-free, undefined novel mechanism | 10,000 Hz, 30 μs [89] | 76.5% [89] | 72.9% [89] | Superior, durable pain relief; paresthesia-free |
| Novel Protocol: Burst SCS | Targets affective pain components | Bursts of 5 pulses at 500 Hz, delivered at 40 Hz [90] | Data from crossover studies [91] | Data from crossover studies [91] | Reduces emotional component of pain |
*A responder is defined as a patient achieving ≥50% reduction in pain intensity on the Visual Analog Scale (VAS) [89].
The data demonstrates the clear and sustained efficacy gains of novel protocols like HF10 SCS. A pivotal RCT showed HF10 SCS provided a 27.2% absolute increase in back pain responder rates and a 23.6% increase in leg pain responder rates over traditional SCS at 24 months, with statistical superiority (P < 0.001) [89]. Furthermore, mean pain reduction was substantially greater with HF10 SCS (66.9% vs. 41.1% for back pain) [89].
Experimental Protocols and Methodological Frameworks
Pivotal Trial Design: Direct Comparison (HF10 vs. Conventional SCS)
The long-term efficacy data presented in Table 1 originates from a prospective, randomized, controlled pivotal trial [89].
- Objective: To demonstrate the non-inferiority and superiority of paresthesia-free HF10 therapy versus traditional paresthesia-based SCS for chronic intractable back and leg pain [89].
- Participants: 198 subjects were randomized (101 to HF10, 97 to traditional SCS). Subjects had an average VAS score of ≥5.0 cm for both back and leg pain and were refractory to conservative therapy [89].
- Intervention: The HF10 group received stimulation at 10,000 Hz with 30 μs pulse width. The traditional SCS group received stimulation at 40-60 Hz with 300-600 μs pulse width, programmed to produce paresthesia overlapping the painful areas [89].
- Primary Endpoint: The primary endpoint was the responder rate for back pain at 3 months, with long-term follow-up continuing to 24 months [89].
Multi-Waveform Crossover Trial (MULTIWAVE Study)
For direct, head-to-head comparison of multiple novel waveforms, the MULTIWAVE study protocol offers a robust framework [91].
- Design: A prospective, randomized, double-blinded, crossover trial in Failed Back Surgery Syndrome (FBSS) patients [91].
- Protocol: After a 2-month tonic conventional stimulation (TCS) period, patients are randomized to one of six sequences. Each sequence exposes the patient to three 1-month periods of TCS, Burst SCS, and High-Frequency SCS (HF) in a varying order. This is followed by a 12-month period where the patient chooses their preferred modality [91].
- Outcomes: The primary outcome is the change in the average global VAS of pain. Secondary outcomes include leg and back pain intensity, functional disability, quality of life, and patient satisfaction [91]. This design allows for intra-patient comparison, reducing inter-subject variability and providing high-quality evidence on patient preference and relative efficacy.
Non-Invasive Protocol: tDCS for Cannabis Use Disorder (CUD)
Novel protocols are also being validated in non-invasive neuromodulation. A pilot RCT protocol pairs transcranial direct current stimulation (tDCS) with cognitive reappraisal training for CUD [92].
- Intervention: Participants receive either active or sham 1.5 mA anodal tDCS over the right dorsolateral prefrontal cortex for 20 minutes, paired with cognitive reappraisal training, across five weekly sessions [92].
- Primary Outcomes: Changes in cannabis use (via daily SMS surveys), electroencephalogram (EEG) brain activity in response to cannabis cues, and self-reported craving intensity [92].
- Computational Validation Angle: The incorporation of EEG provides objective, quantifiable neurophysiological biomarkers (e.g., P300, LPP, frontal theta power) to validate the mechanistic effects of the intervention beyond subjective reports [92].
Diagram 1: Experimental workflow for clinical validation of neurostimulation protocols, highlighting key trial designs such as parallel-group RCTs and multi-period crossover studies.
Computational Model Validation and Reporting Standards
The transition from empirical to model-driven neurostimulation requires rigorous validation frameworks. Key to this is the standardization of reporting, which ensures that computational models are built on high-quality, reproducible data.
The SPIRIT-iNeurostim and CONSORT-iNeurostim Extensions
To address common methodological and reporting deficiencies in implantable neurostimulation trials, the international SPIRIT-iNeurostim and CONSORT-iNeurostim guidelines were developed [93]. These extensions provide a checklist of essential items to report in trial protocols and results publications, respectively. Key new items include [93]:
- Specifying the neurostimulation intervention using a 14-item sub-checklist detailing device and procedure parameters.
- Stating the intended position of the neurostimulation in the treatment pathway.
- Reporting funding sources for device costs.
These guidelines are a foundational component of computational model validation, as they enforce the completeness and transparency of input data used to build and test predictive simulations.
Automating Evidence Synthesis with Large Language Models (LLMs)
The validation of computational models against the entire body of clinical evidence is hampered by the labor-intensive nature of systematic reviews. Recent benchmarking demonstrates the efficacy of multi-agent LLM ensembles for automated data extraction [94].
- Performance: A five-model LLM ensemble achieved near-perfect agreement (Fleiss κ ≈ 0.94) with expert human extractors on core stimulation parameters like brain stimulation use and primary target [94].
- Efficiency Gain: The automated pipeline retrieved 83 aging-related tDCS trials—roughly double the yield of a conventional keyword search [94].
- Role in Validation: This technology enables the rapid, comprehensive synthesis of structured data from clinical trial registries like ClinicalTrials.gov, providing the large-scale datasets necessary for robust computational model training and validation [94].
Diagram 2: Computational model validation pipeline leveraging automated data extraction. This workflow transforms unstructured clinical text into structured data for model training and testing.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution and validation of neurostimulation research require a suite of specialized tools and reagents. The following table details key components referenced in the cited literature.
Table 2: Essential Research Reagents and Solutions for Neurostimulation Studies
| Item / Solution | Function / Role in Research | Example in Context |
|---|---|---|
| Programmable SCS Systems | Enables delivery of conventional and novel waveforms (HF, Burst) in comparative studies. | Precision Spectra SCS System used in the MULTIWAVE study [91]. |
| tDCS Stimulator | Non-invasive application of weak direct current to modulate cortical excitability. | Used to stimulate the dorsolateral prefrontal cortex in CUD research [92]. |
| High-Density Electrode Leads | Provides targeted and focused electrical field delivery for spinal cord stimulation. | 32-contact surgical lead used for precise field shaping [91]. |
| EEG System with ERP Capability | Records high-temporal-resolution brain activity to objectively measure neurophysiological effects. | Used to capture P300/LPP and theta power during craving regulation tasks [92]. |
| Reporting Guidelines (RATES Checklist) | Standardizes reporting of tES study parameters to enhance reproducibility and meta-analysis. | Consensus-based checklist with 66 items covering device, electrodes, and current [28]. |
| Multi-LLM Ensemble Pipeline | Automates extraction of structured data from clinical trial registries and publications. | Benchmarked pipeline that doubled trial retrieval yield for tDCS studies [94]. |
Conclusion
The rigorous validation of computational models is not merely an academic exercise but a fundamental prerequisite for developing effective, reliable, and personalized neurostimulation protocols. This synthesis demonstrates that a multi-faceted approach—combining foundational rigor, advanced methodological workflows, proactive troubleshooting, and standardized comparative validation—significantly enhances the predictive power of in-silico models. Future directions must prioritize the integration of real-world, at-home application data, the development of more sophisticated multi-scale models that capture network-level effects, and the establishment of universally accepted validation benchmarks. By closing the loop between model prediction and experimental outcome, validated computational frameworks will accelerate the translation of neurostimulation from a promising tool to a precise and mainstream therapeutic intervention, ultimately advancing both biomedical research and clinical care for neurological disorders.
References
- 1. A Beginner's Guide to Model Validation [https://axenehp.com/beginners-guide-model-validation/]
- 2. Model Checking/Validating Best Practices - The Stan Forums [https://discourse.mc-stan.org/t/model-checking-validating-best-practices/29443]
- 3. Lehigh team develops computational model to guide ... [https://engineering.lehigh.edu/news/article/lehigh-team-develops-computational-model-guide-neurostimulation-therapy-atrial]
- 4. Predictive modeling of hemodynamics during viscerosensory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019394/]
- 5. NeurostimML: A machine learning model for predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10614958/]
- 6. Protocol for artificial intelligence-guided neural control ... [https://www.sciencedirect.com/science/article/pii/S2666166724006610]
- 7. The simulation and experimental validation of a novel ... [https://www.nature.com/articles/s41598-024-61571-9]
- 8. A computational outlook on neurostimulation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7247210/]
- 9. A systematic review of computational models for the design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10259770/]
- 10. Multitarget Neurostimulation of the Deep Brain - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453607/]
- 11. How Latent Representations Transform Geometric ML [https://www.physicsx.ai/newsroom/foundational-geometry-models-how-latent-representations-transform-geometric-ml]
- 12. Defining Foundation Models for Computational Science [https://arxiv.org/html/2505.22904v2]
- 13. Lehigh University Researchers Create Computational ... [https://bioengineer.org/lehigh-university-researchers-create-computational-model-to-optimize-neurostimulation-therapy-for-atrial-fibrillation/]
- 14. Model Validation Techniques, Explained: A Visual Guide ... [https://towardsdatascience.com/model-validation-techniques-explained-a-visual-guide-with-code-examples-eb13bbdc8f88/]
- 15. Closing the loop between brain and electrical stimulation [https://www.nature.com/articles/s41398-023-02565-5]
- 16. Neurostimulation Devices Market to Climb USD 23.24 ... [https://www.towardshealthcare.com/insights/neurostimulation-devices-market-sizing]
- 17. Harnessing neural variability: Implications for brain ... [https://www.sciencedirect.com/science/article/pii/S0149763425003136]
- 18. Evaluating Model Performance: A Comprehensive Guide [https://medium.com/@zhonghong9998/evaluating-model-performance-a-comprehensive-guide-6f5e7c11409f]
- 19. U.S. Neurological Devices Market & Trends Analysis | 2025 ... [https://idataresearch.com/product/neurological-devices-market-united-states/]
- 20. In Vitro vs. In Vivo vs. In Silico: Preclinical Assay Differences [https://www.zeclinics.com/blog/differences-between-in-vitro-in-vivo-and-in-silico-assays-in-preclinical-research]
- 21. In Silico Trials - Transforming Medical Device Innovation [https://www.biomedstat.com/knowledge-base/in-silico-trials-medical-device]
- 22. Advanced Computational Life Science Applications at CNS ... [https://zmt.swiss/news-and-events/news/sim4life/2025/advanced-computational-life-science-applications-at-cns2025/]
- 23. Randomized Clinical Trials on Neurostimulation for ... [https://www.sciencedirect.com/science/article/abs/pii/S1094715925010323]
- 24. Comparison of In Vitro and In Silico Assessments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9910814/]
- 25. Validation approaches for computational drug repurposing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785886/]
- 26. Modelscape Validate - MATLAB & Simulink [https://in.mathworks.com/help/risk/modelscape-validate.html]
- 27. Best practices for clinical trials of deep brain stimulation ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1572972/full]
- 28. expert recommendation based on a Delphi consensus study [https://www.nature.com/articles/s41596-025-01259-0]
- 29. Developing consolidated guidelines for reporting and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587907/]
- 30. Comparing and scaling fMRI features for brain-behavior ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434381/]
- 31. Emerging Applications of Electrochemical Impedance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9599721/]
- 32. Applications of electrochemical impedance spectroscopy in ... [https://www.sciencedirect.com/science/article/pii/S2666053924000213]
- 33. Measuring the dynamic balance of integration and ... [https://www.nature.com/articles/s41467-024-53299-x]
- 34. A Review of Impedance Spectroscopy Technique [https://www.mdpi.com/2076-3417/14/13/5754]
- 35. Computational models of adaptive behavior and prefrontal ... [https://www.nature.com/articles/s41386-021-01123-1]
- 36. Personalized home based neurostimulation via AI ... [https://www.nature.com/articles/s41746-025-01744-6]
- 37. Comparison of the efficacy of different protocols of repetitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12084249/]
- 38. Comparison between accelerated and standard or sham ... [https://www.sciencedirect.com/science/article/abs/pii/S014976342500140X]
- 39. Class imbalance learning with Bayesian optimization ... [https://www.nature.com/articles/s41598-022-05717-7]
- 40. Deep Learning Methods Applied to Drug Concentration ... [https://pubmed.ncbi.nlm.nih.gov/37111625/]
- 41. Multifidelity Bayesian optimization for hyperparameter ... [https://ojs.acad-pub.com/index.php/CAI/article/view/2923]
- 42. Reasoning BO: Enhancing Bayesian Optimization with the ... [https://arxiv.org/html/2505.12833v2]
- 43. A hybrid deep learning-Bayesian optimization model for ... [https://www.sciencedirect.com/science/article/pii/S3050483X25000292]
- 44. The improved thalamo-cortical spiking network model of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380790/]
- 45. The improved thalamo-cortical spiking network model of ... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2025.1662598/full]
- 46. Computational analysis of two novel deep brain stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546198/]
- 47. Deep brain stimulation of symptom-specific networks in ... [https://www.nature.com/articles/s41467-024-48731-1]
- 48. Patient-specific and interpretable deep brain stimulation ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1661987/full]
- 49. Patient-specific and interpretable deep brain stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586115/]
- 50. Inter-Individual Variability in tDCS Effects: A Narrative Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9139102/]
- 51. A Comparison of Two Electric Taste Stimulation Devices - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4972032/]
- 52. Highly efficient modeling and optimization of neural fiber responses to electrical stimulation | Nature Communications [https://www.nature.com/articles/s41467-024-51709-8]
- 53. Paradoxical Modulation of STN Beta-Band Activity with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10843006/]
- 54. Neurostimulation stabilizes spiking neural networks by disrupting seizure-like oscillatory transitions | Scientific Reports [https://www.nature.com/articles/s41598-020-72335-6]
- 55. Deep Learning and fMRI-Based Pipeline for Optimization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11379443/]
- 56. Model-Based Analysis and Design of Waveforms for Efficient Neural Stimulation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4772858/]
- 57. Comparison of 5-Day Multidaily Neuronavigated Theta- ... [https://www.researchprotocols.org/2025/1/e70121]
- 58. Verification, Validation and Uncertainty Quantification ... [https://www.asme.org/codes-standards/publications-information/verification-validation-uncertainty]
- 59. A "Threshold-based" Approach to Determining an Acceptance ... [https://cdrh-rst.fda.gov/threshold-based-approach-determining-acceptance-criterion-computational-model-validation]
- 60. Computational models and tES dose optimization [https://bio-protocol.org/exchange/minidetail?id=2091660&type=30]
- 61. High-Resolution Computational Modeling of the Current Flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8608747/]
- 62. Target Optimization in Transcranial Direct Current Stimulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC3474130/]
- 63. Electric field simulation and appropriate electrode ... [https://www.nature.com/articles/s41598-024-52874-y]
- 64. Individual Baseline Performance and Electrode Montage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7506510/]
- 65. Individual response to transcranial direct current ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2023.1134632/full]
- 66. Optimization of montages and electric currents in tDCS [https://www.sciencedirect.com/science/article/abs/pii/S0010482520303292]
- 67. Target optimization in transcranial direct current stimulation [https://pure.johnshopkins.edu/en/publications/target-optimization-in-transcranial-direct-current-stimulation-4]
- 68. How AI Will Predict Clinical Trial Failures Before They ... [https://ccrps.org/clinical-research-blog/how-ai-will-predict-clinical-trial-failures-before-they-happen-2025-insights]
- 69. Enhancing randomized clinical trials with digital twins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494699/]
- 70. In Silico Clinical Trials Market Size & Share Forecast 2030 [https://www.mordorintelligence.com/industry-reports/in-silico-clinical-trial-market]
- 71. An Evaluation Benchmark for Adverse Drug Event ... [https://www.nature.com/articles/s41597-025-04718-1]
- 72. AI meets physics in computational structure-based drug ... [https://www.nature.com/articles/s44386-025-00019-0]
- 73. Practical Perspectives on Enhancing Predictive Modeling ... [https://link.springer.com/article/10.1007/s40495-025-00426-x]
- 74. Predictive Accuracy - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/computer-science/predictive-accuracy]
- 75. The Importance of Prediction Model Validation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4826636/]
- 76. Classification: Accuracy, recall, precision, and related metrics [https://developers.google.com/machine-learning/crash-course/classification/accuracy-precision-recall]
- 77. How to Evaluate the Accuracy of Predictive Models [https://businessanalyticsinstitute.com/how-to-evaluate-the-accuracy-of-predictive-models/]
- 78. Improving computational models of deep brain stimulation ... [https://www.sciencedirect.com/science/article/pii/S0165027024002656]
- 79. 5 key practices for data presentation in research [https://www.elsevier.com/connect/5-key-practices-for-data-presentation-in-research]
- 80. Review of Noninvasive or Minimally Invasive Deep Brain ... [https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2021.820017/full]
- 81. Comparative Effects of Temporal Interference and High ... [https://www.mdpi.com/2076-3425/15/3/317]
- 82. Repetitive temporal interference stimulation improves jump ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-024-01336-7]
- 83. The impact of transcranial direct current stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538427/]
- 84. TECH-VER: A Verification Checklist to Reduce Errors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6860463/]
- 85. Reporting guidelines for randomised controlled trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11600657/]
- 86. A checklist designed to aid consistency and reproducibility of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4124503/]
- 87. Reporting checklist for verification and validation of finite ... [https://www.sciencedirect.com/science/article/pii/S1350453321000345]
- 88. Reproducibility Checklist - AAAI [https://aaai.org/conference/aaai/aaai-23/reproducibility-checklist/]
- 89. Comparison of 10-kHz High-Frequency and Traditional Low ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5058646/]
- 90. Conventional and Novel Spinal Stimulation Algorithms [https://www.sciencedirect.com/science/article/abs/pii/S1094715921033341]
- 91. Comparison of conventional, burst and high-frequency spinal ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-04587-6]
- 92. Study protocol of a pilot randomized controlled trial of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0328205]
- 93. the SPIRIT-iNeurostim extension - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC11602573/]
- 94. Benchmarking Multiple Large Language Models for ... [https://www.mdpi.com/1999-4893/18/5/296]