Strategies to Mitigate Fibrosis and Enhance Longevity in Neural Electrode Interfaces
The long-term performance of implantable neural electrodes is critically limited by the foreign body reaction (FBR), a complex immune response that culminates in fibrotic tissue encapsulation.
Strategies to Mitigate Fibrosis and Enhance Longevity in Neural Electrode Interfaces
Abstract
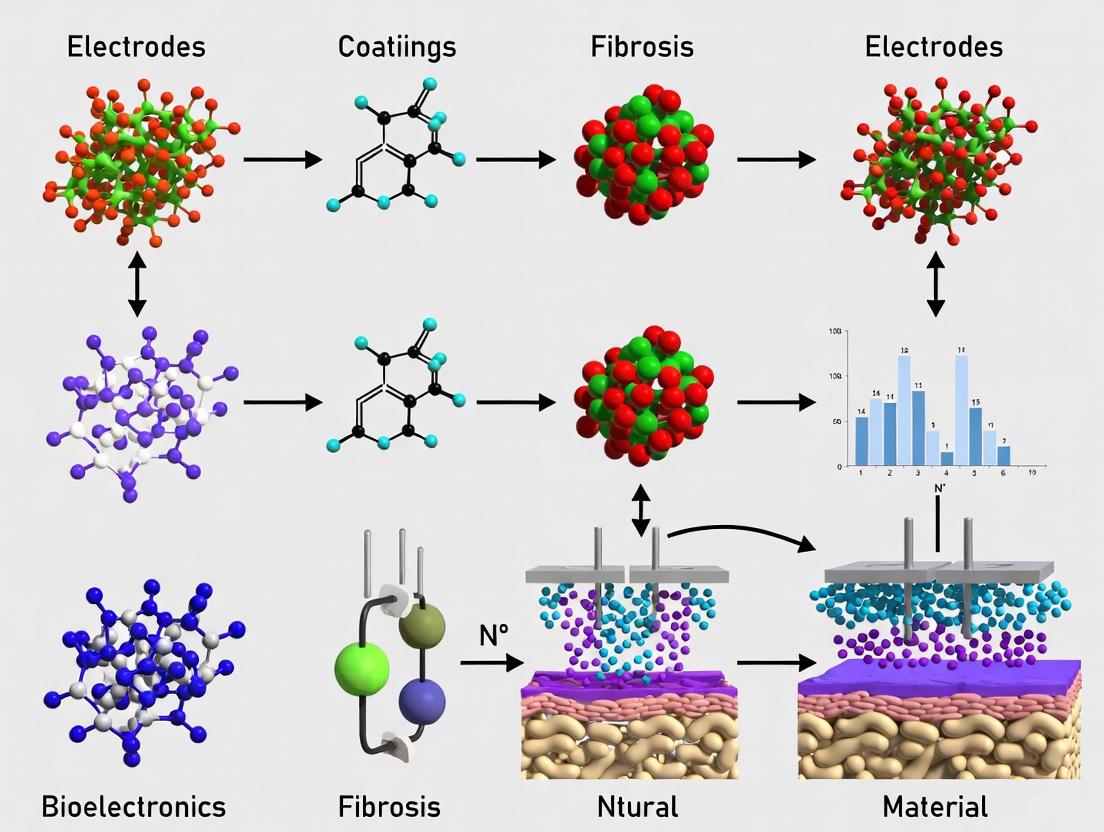
The long-term performance of implantable neural electrodes is critically limited by the foreign body reaction (FBR), a complex immune response that culminates in fibrotic tissue encapsulation. This fibrotic scar increases electrical impedance, attenuates signal quality, and ultimately leads to device failure. This article provides a comprehensive analysis for researchers and drug development professionals, exploring the foundational biology of FBR, reviewing cutting-edge material science and bioengineering strategies to counteract it, examining troubleshooting for chronic stability, and validating approaches through in vitro and in vivo models. By synthesizing recent advances in biocompatible materials, drug-delivery coatings, and intelligent electrode design, this review outlines a pathway toward developing next-generation neural interfaces with improved functional longevity.
Understanding the Foreign Body Reaction: The Biological Basis of Fibrosis
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our neural electrode recordings show a sharp increase in electrical impedance 2-3 weeks post-implantation. What is the likely cause and how can we confirm it?
A1: A sharp increase in impedance between weeks 2-4 is a classic symptom of progressing fibrous encapsulation [1] [2]. The foreign body reaction leads to the formation of a fibrotic capsule around the implant, which acts as an insulating layer [2]. To confirm:
- Histological Analysis: Explant the device and surrounding tissue for sectioning and staining. Look for the presence of a collagen-dense capsule, macrophages, and Foreign Body Giant Cells (FBGCs) at the tissue-device interface [1].
- Immunofluorescence: Stain for specific cell markers: CD68 (macrophages), α-SMA (myofibroblasts), and Collagen I/III (fibrotic capsule) [3].
Q2: We observe significant variability in fibrotic capsule thickness between our in-vivo models. What experimental factors should we standardize?
A2: Capsule thickness is highly sensitive to mechanical mismatch [3] [4]. Standardize these factors:
- Implant Stiffness (Young's Modulus): Ensure consistent material properties across implants. The goal is to match brain tissue (~1-10 kPa) [4].
- Implantation Method & Cross-sectional Area: The size and shape of the implant and the surgical technique (e.g., use of rigid shuttles) directly influence acute injury and chronic inflammation. Smaller, distributed implants cause less damage [4].
- Micromotion: Secure the device to minimize movement relative to the surrounding tissue, which exacerbates the chronic inflammatory response [4].
Q3: Which cytokines are the most critical biomarkers to monitor in the tissue surrounding the implant to track FBR progression?
A3: The FBR is driven by a cascade of cytokines. Key biomarkers to monitor include:
Table 1: Key Cytokines in the Foreign Body Reaction Cascade
| Cytokine/Chemokine | Primary Source | Primary Role in FBR |
|---|---|---|
| TGF-β | Platelets, Macrophages, FBGCs | Master regulator of fibrosis; stimulates fibroblast activation and ECM production [2] [3]. |
| CCL2 (MCP-1) | Macrophages | Key chemoattractant for recruiting monocytes/macrophages to the implant site [1] [2]. |
| IL-4 & IL-13 | Mast Cells, T-cells | Promote alternative (pro-healing) macrophage polarization and FBGC formation [1]. |
| PDGF | Platelets, Macrophages | Chemoattractant and mitogen for fibroblasts [1]. |
| TNF-α | Macrophages | Pro-inflammatory cytokine; amplifies early inflammatory response [1]. |
Q4: What are the most promising strategies to mitigate the Foreign Body Reaction for chronic neural implants?
A4: Strategies can be categorized as passive or active:
- Passive "Stealth" Strategies: Reduce the immune system's recognition of the implant. This includes using biomimetic coatings (e.g., hydrogels), optimizing device geometry to minimize cross-sectional area, and using flexible materials to reduce mechanical mismatch [2] [4].
- Active Modulation Strategies: Use the implant as a delivery vehicle to release anti-inflammatory agents (e.g., steroids like Dexamethasone) or factors that modulate the local immune environment (e.g., TGF-β inhibitors) directly to the tissue interface [4].
Troubleshooting Common Experimental Challenges
Problem: Inconsistent Macrophage Polarization In Vitro
- Issue: Difficulty in generating reproducible M1 (pro-inflammatory) and M2 (pro-healing) macrophage phenotypes for FBR studies.
- Solution:
- Protocol: Use primary bone marrow-derived macrophages (BMDMs) from consistent mouse strains for better reproducibility.
- Polarization Cocktails:
- Mechanical Cues: Culture cells on hydrogels with tunable stiffness (1-10 kPa for M2-like, >30 kPa for M1-like tendencies) to better mimic the in-vivo mechanical environment [3].
Problem: Excessive Fibrosis in Small Animal Models
- Issue: The fibrotic capsule is too thick, making it difficult to separate the device from the tissue for analysis.
- Solution:
- Optimize Implant Size: The implant's cross-sectional area should be minimized. For distributed filament electrodes, aim for widths of 10-50 μm [4].
- Pharmacological Inhibition: Consider systemic or local delivery of anti-fibrotic drugs (e.g., Losartan, an angiotensin inhibitor) to moderate the fibrotic response, but account for its broad effects in your experimental design.
- Perfusion Fixation: For histology, perform transcardial perfusion with paraformaldehyde (PFA) before explant to preserve tissue architecture and facilitate cleaner device removal.
Experimental Protocols & Data Presentation
Protocol 1: Histological Quantification of Fibrotic Capsule Thickness
Objective: To quantitatively assess the extent of fibrosis around an explanted neural device.
Materials:
- Ex-vivo tissue sample with implanted device
- 4% Paraformaldehyde (PFA)
- Paraffin embedding station or Cryostat
- Microtome
- Hematoxylin and Eosin (H&E) stain, Masson's Trichrome stain
- Light microscope with digital camera and image analysis software (e.g., ImageJ)
Methodology:
- Fixation & Sectioning: Fix explanted tissue in 4% PFA for 24-48 hours. Decalcify if necessary. Embed in paraffin and section coronally at 5-10 μm thickness. Alternatively, for cryosectioning, embed in OCT compound after sucrose gradient dehydration.
- Staining:
- Perform H&E staining for general morphology and to identify the device-tissue interface.
- Perform Masson's Trichrome staining to specifically highlight collagen fibers (will appear blue).
- Imaging & Analysis:
- Image multiple, non-overlapping fields around the entire device circumference under 10x or 20x magnification.
- Using ImageJ, calibrate the scale. Draw perpendicular lines from the device surface to the outer edge of the dense, collagen-rich capsule. Measure the thickness at regular intervals (e.g., every 100 μm).
- Calculate the average capsule thickness and standard deviation for each sample.
Protocol 2: Immunofluorescence Analysis of FBR Cellular Components
Objective: To identify and localize key cellular players in the FBR.
Materials:
- Tissue sections on glass slides
- Antigen retrieval solution (e.g., citrate buffer)
- Blocking solution (e.g., 5% normal goat serum)
- Primary antibodies: α-SMA (myofibroblasts), CD68 (macrophages), Collagen I
- Fluorophore-conjugated secondary antibodies
- DAPI solution
- Fluorescent microscope or confocal microscope
Methodology:
- Deparaffinization & Antigen Retrieval: Deparaffinize and rehydrate sections. Perform heat-induced antigen retrieval in appropriate buffer.
- Staining:
- Block sections with 5% serum for 1 hour at room temperature.
- Incubate with primary antibodies diluted in blocking buffer overnight at 4°C.
- Wash and incubate with secondary antibodies for 1 hour at room temperature (protected from light).
- Counterstain nuclei with DAPI for 5 minutes.
- Imaging: Acquire z-stack images using a confocal microscope. Use consistent laser power and exposure settings across all samples for quantitative comparison.
Table 2: Temporal Progression of Key Events in the Foreign Body Reaction [1] [2]
| Time Post-Implantation | Phase | Key Cellular Events | Key Molecular Mediators |
|---|---|---|---|
| Minutes - Hours | Protein Adsorption | Adsorption of fibrinogen, fibronectin, albumin, immunoglobulins to implant surface [1]. | Vroman Effect [1] |
| Hours - Days | Acute & Chronic Inflammation | Neutrophil infiltration, followed by monocyte recruitment and differentiation to macrophages [1]. | CCL2, CCL3, CCL5, TGF-β, PF4 [1] [2] |
| Days - Weeks | Foreign Body Reaction & Granulation Tissue | Macrophage fusion to form FBGCs; Fibroblast infiltration and neovascularization [1] [2]. | IL-4, IL-13, TGF-β, PDGF [1] |
| Weeks - Months | Fibrosis / Fibrous Encapsulation | Fibroblast-to-myofibroblast transition; Massive deposition of Collagen I/III, forming an avascular capsule [2] [3]. | TGF-β, α-SMA, Connective Tissue Growth Factor (CCN2) [3] |
Signaling Pathways and Experimental Workflows
FBR Signaling Pathway
Experimental Workflow for FBR Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for FBR Investigation
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| Polyimide-based Neural Probes | Flexible substrate for neural implants; reduces mechanical mismatch with brain tissue (Young's modulus ~2-3 GPa) [4]. | Fabrication of chronic intracortical or intraneural electrodes for long-term FBR studies [4]. |
| PEG-based Hydrogels | Tunable, biomimetic coating for implants; can be functionalized with RGD peptides to improve biocompatibility [3]. | Creating a soft, hydrated interface layer on electrodes to dampen host immune recognition [2]. |
| TGF-β Neutralizing Antibody | Inhibits the TGF-β signaling pathway, the master regulator of fibrosis [3]. | Local delivery from an implant coating to assess the specific role of TGF-β in fibrous capsule formation in-vivo. |
| IL-4 & IL-13 Cytokines | Induce alternative (M2) macrophage polarization and promote FBGC formation in vitro [1] [3]. | Treatment of primary macrophages in culture to study the effects of M2 polarization on fibroblast activation in co-culture systems. |
| α-SMA, CD68, Collagen I Antibodies | Key markers for immunofluorescence: α-SMA (myofibroblasts), CD68 (macrophages), Collagen I (fibrosis) [3]. | Staining tissue sections to quantify the key cellular components of the FBR and correlate with impedance data. |
| Losartan | An angiotensin II receptor blocker (ARB) with known anti-fibrotic effects. | Administering systemically in animal models to investigate the potential reduction of FBR-related fibrosis around neural implants. |
Frequently Asked Questions (FAQs)
What are the key cellular players in the foreign body response (FBR) to implanted neural electrodes? The foreign body response is a coordinated process involving immune and stromal cells. The key players are:
- Macrophages: Myeloid immune cells that first respond to the implant. They orchestrate inflammation and can fuse to form Foreign Body Giant Cells (FBGCs) [5] [6].
- Foreign Body Giant Cells (FBGCs): Large, multinucleated cells formed by macrophage fusion. They persist at the biomaterial-tissue interface and contribute to chronic inflammation and degradation attempts [5] [6].
- Myofibroblasts: Activated fibroblasts that are the primary effector cells for fibrosis. They are characterized by excessive deposition of collagen and other extracellular matrix (ECM) proteins, leading to the formation of a dense, scar-like capsule around the implant [5] [7] [8].
Why is the FBR a significant problem for neural electrodes? The FBR leads to the formation of a fibrotic scar and glial scar around the implant [9]. This has two major detrimental effects:
- Increased Electrode Impedance: The fibrotic tissue acts as an electrical insulator, reducing the signal quality recorded from or stimulated into neurons [9] [10].
- Neurodegeneration: The chronic inflammatory environment and physical encapsulation can lead to the loss of neurons near the electrode, further degrading interface performance [9] [10].
How do macrophages influence the development of fibrosis? Macrophages are central regulators. They exhibit plasticity and can adopt different functional phenotypes, often broadly categorized as:
- Pro-inflammatory (M1): Drive early inflammation and can recruit other immune cells and fibroblasts [5] [6].
- Pro-healing/Anti-inflammatory (M2): Promote tissue repair, but can also drive fibroblast activation and fibrosis [5] [6]. The persistence of macrophages and FBGCs at the implant site helps sustain a pro-fibrotic signaling environment, for instance, through the release of TGF-β1, a potent activator of myofibroblasts [5] [7].
What role does mechanical signaling play in the FBR? Recent research highlights that physical forces are a major driver of the FBR, independent of material chemistry [11] [12].
- Implant Stiffness: Stiffer implants generate greater mechanical stress at the tissue interface, which promotes FBGC formation and myofibroblast activation via mechanosensitive ion channels like TRPV4 [11].
- RAC2 Signaling: A 2023 study identified RAC2, a haematopoietic-specific GTPase, as a key mechanotransduction signal in myeloid cells (macrophages) that drives pathological FBR in humans. This pathway is activated by tissue-scale forces [12].
Troubleshooting Guides
Issue 1: Excessive Fibrous Encapsulation of Implants
Potential Causes and Solutions:
| Potential Cause | Supporting Evidence | Recommended Mitigation Strategies |
|---|---|---|
| Chronic macrophage activation & FBGC formation | Macrophages and FBGCs secrete pro-fibrotic signals (e.g., TGF-β) that activate myofibroblasts [5] [6]. | 1. Target Macrophages: Use a CSF1R inhibitor (e.g., PLX5622) to deplete macrophages [10].2. Modulate Phenotype: Design biomaterials that promote a pro-regenerative macrophage phenotype [5]. |
| Persistent TGF-β1 / Smad signaling | TGF-β1 is the primary cytokine driving fibroblast-to-myofibroblast differentiation via the canonical Smad pathway [7] [8]. | 1. Local Drug Delivery: Use implants coated with or eluting TGF-β receptor inhibitors [7].2. Target Downstream Signaling: Investigate inhibitors of Smad3 or other non-canonical pathways (e.g., MAPK, ERK1/2) [7]. |
| Elevated mechanical forces at implant interface | Tissue-scale forces activate RAC2 in myeloid cells, driving severe FBR. Stiffness sensing via TRPV4 promotes FBGC formation and myofibroblast differentiation [11] [12]. | 1. Reduce Implant Stiffness: Use flexible, soft materials that better match brain tissue modulus [9] [12].2. Pharmacological Inhibition: Inhibit mechanosensing pathways (e.g., TRPV4 or RAC2 inhibitors) [11] [12]. |
Issue 2: Poor Long-term Signal Quality in Neural Recordings
Potential Causes and Solutions:
| Potential Cause | Supporting Evidence | Recommended Mitigation Strategies |
|---|---|---|
| Glial scarring and neuronal loss | The FBR creates an insulating glial/fibrotic capsule and a pro-inflammatory environment that is toxic to neurons [9] [10]. | 1. Minimize Insertion Trauma: Use ultra-thin, flexible electrodes and advanced insertion systems to reduce bleeding and initial tissue damage [9] [13].2. Anti-inflammatory Drugs: Administer local steroids (e.g., dexamethasone) to suppress the inflammatory response [10]. |
| Increased electrode impedance | Fibrotic tissue, composed of collagen and other ECM proteins deposited by myofibroblasts, electrically isolates the electrode [9] [10]. | 1. Reduce Cross-section: Use neural probes with a smaller footprint to displace less tissue and minimize the FBR target [9].2. Surface Modification: Develop non-fouling surface chemistries to reduce protein adsorption and subsequent cell adhesion [5] [9]. |
Table 1: Experimental Outcomes of Macrophage Depletion on Cochlear Implant FBR Data derived from a study using the CSF1R inhibitor PLX5622 in a mouse model [10].
| Parameter | Control Diet (No PLX) | PLX5622 Diet (Macrophage Depletion) | Implication |
|---|---|---|---|
| Macrophage Infiltration | Present in implanted cochleae | Significantly reduced at all time points | Confirms efficacy of macrophage depletion strategy [10]. |
| Scala Tympani Fibrosis (α-SMA+ volume) | Evident | Not reduced | Suggests other cells or pathways can sustain fibrosis; macrophages may not be the sole driver in this context [10]. |
| Electrode Impedance | Baseline levels | Increased compared to controls | Macrophages may play a role in maintaining a conductive interface; their removal may be detrimental to signal conduction [10]. |
| Spiral Ganglion Neuron (SGN) Survival | Baseline survival | Decreased in implanted and contralateral cochleae | Highlights a critical role for macrophages in promoting neuronal survival post-implantation [10]. |
Table 2: Impact of Implant Physical Properties on the Foreign Body Response
| Property | Effect on FBR | Key Molecular Mediators | Reference |
|---|---|---|---|
| Stiffness | Stiffer implants promote FBGC formation, fibrosis, and pathological FBR. Softer, flexible implants reduce glial scarring. | TRPV4, RAC2, Cytoskeletal remodeling [11] [9] [12] | |
| Cross-sectional Size | Smaller probes displace less tissue, cause less vascular damage, and demonstrate improved integration with reduced gliosis. | N/A (Primarily a physical effect) [9] |
Detailed Experimental Protocols
Protocol A: Assessing the Role of Macrophages via Pharmacological Depletion
Objective: To determine the specific contribution of macrophages to the FBR and neural health around an implant.
Reagents:
- PLX-5622: A CSF1R inhibitor formulated into rodent chow at 1200 ppm [10].
- Control Diet: Standard AIN-76A chow.
- Animal Model: CX3CR1+/GFP reporter mice (to visualize macrophages) [10].
- Implants: Neural electrode or cochlear implant array.
Methodology:
- Pre-treatment: Begin feeding mice the PLX-5622 or control diet 7 days prior to implantation to achieve pre-depletion of macrophages [10].
- Surgical Implantation: Perform the implant surgery using aseptic techniques. Minimize insertion trauma and bleeding [9].
- Post-operative Monitoring: Continue the specialized diet for the duration of the study (e.g., 28-56 days). Monitor functional outcomes like electrode impedance and neural response thresholds [10].
- Tissue Collection & Histology: At endpoint, perfuse and harvest the implanted tissue.
- Fixation and Sectioning: Cryopreserve and section the tissue.
- Immunostaining:
- Image Analysis: Use software (e.g., IMARIS) to quantify:
Protocol B: Evaluating the Role of Mechanosensing via TRPV4 Inhibition
Objective: To investigate the contribution of stiffness-induced mechanosensing to FBGC formation and fibrosis.
Reagents:
- TRPV4 Inhibitor: e.g., GSK2193874.
- Animal Model: Wild-type and TRPV4-/- mice [11].
- Implants: Biomaterials of varying stiffness (e.g., soft vs. stiff silicone).
Methodology:
- In Vivo Implantation: Implant biomaterials subcutaneously or in the target neural tissue of wild-type mice treated with a TRPV4 inhibitor and TRPV4-/- mice [11].
- Tissue Analysis: Harvest implant capsules after a set period (e.g., 2-3 weeks).
- In Vitro Validation:
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating FBR
| Reagent | Function/Application | Example Use in FBR Research |
|---|---|---|
| PLX-5622 (CSF1R inhibitor) | Depletes macrophages and microglia by blocking a key survival signal. | Used to study the specific role of macrophages in FBR-driven fibrosis and neurodegeneration [10]. |
| Anti-α-SMA Antibody | Identifies activated myofibroblasts, the primary collagen-producing cells in fibrosis. | Critical for quantifying the extent of fibrotic encapsulation around implants via immunohistochemistry [7] [10]. |
| Recombinant TGF-β1 | The primary cytokine to induce fibroblast-to-myofibroblast transition in vitro and in vivo. | Used to activate fibroblasts and study TGF-β signaling pathways in controlled experiments [7] [8]. |
| TRPV4 Inhibitors (e.g., GSK2193874) | Blocks the mechanosensitive ion channel TRPV4. | Used to dissect the role of stiffness-sensing in FBGC formation and fibrotic activation [11]. |
| CX3CR1+/GFP Mice | Reporter mouse model where macrophages and microglia express GFP. | Allows for in vivo tracking and quantification of macrophage infiltration and localization around implants [10]. |
Signaling Pathway Visualizations
Diagram Title: Foreign Body Response Timeline
Diagram Title: Mechanosensing in FBR
The formation of fibrotic tissue around implanted electrodes is a common biological response that significantly impacts the performance and longevity of neural interfaces, cochlear implants, and other neuroprosthetic devices. This foreign body reaction, characterized by the activation of immune cells such as microglia and astrocytes, leads to the deposition of extracellular matrix components that form a dense, insulating scar tissue around the implant [4]. This fibrotic capsule acts as a physical barrier, increasing the distance between the electrode and its target neural tissue, which in turn leads to increased electrode impedance and attenuated signal quality [14] [4]. Understanding this relationship is crucial for researchers and drug development professionals working to improve the functional longevity of neural interfaces.
The following table summarizes the key performance metrics affected by fibrotic tissue formation:
Table 1: Key Performance Metrics Affected by Fibrotic Tissue Formation
| Performance Metric | Impact of Fibrosis | Consequence for Research & Therapy |
|---|---|---|
| Electrode Impedance | Increase due to insulating effect of fibrotic tissue [14] [4] | Reduced charge transfer efficiency, higher power requirements [4] |
| Signal-to-Noise Ratio (SNR) | Decrease due to increased distance from signal source [4] | Compromised accuracy of neural signal detection and decoding |
| Stimulation Threshold | Increase due to physical barrier between electrode and neurons [4] | Requires higher stimulation energy, potentially causing tissue damage |
| Long-term Stability | Gradual degradation as fibrosis progresses over time [4] [15] | Limited chronic reliability of neural interfaces |
Troubleshooting Guide: Diagnosing Fibrosis-Related Issues
Q1: How can I determine if increased impedance in my chronic experiment is caused by fibrosis?
A common challenge in long-term neural interface studies is differentiating between impedance increases caused by fibrotic encapsulation versus other factors like electrode material degradation or protein adsorption.
Diagnostic Protocol:
- Monitor Impedance Trends: Track impedance over time. A gradual, persistent increase that stabilizes after several weeks is indicative of fibrotic encapsulation, as opposed to a sudden spike which may suggest lead fracture or connector issues [15].
- Conformational Testing: For flexible electrodes, analyze the relationship between mechanical stress and impedance. Performance degradation that recovers after rest periods may indicate material fatigue rather than stable fibrosis [16].
- Post-mortem Histological Correlation: The most definitive method is to correlate terminal impedance measurements with post-mortem histology. Techniques like serial block-face imaging can precisely quantify the fibrotic tissue area and its spatial relationship to the electrode [14].
Interpretation of Results: It is critical to note that while impedance measurements can indicate the presence of an insulating layer, studies on pelvic nerve implants have shown that absolute impedance values may not correlate directly with the absolute amount of fibrotic tissue [14]. Therefore, impedance should be used as a relative indicator of interface changes rather than an absolute metric of fibrosis severity.
Q2: What are the primary failure modes observed in electrodes affected by fibrosis?
Fibrosis can lead to several distinct operational failures in neural recording and stimulation systems.
Table 2: Electrode Failure Modes Linked to Fibrosis
| Failure Mode | Description | Observable Symptoms |
|---|---|---|
| Signal Attenuation | Reduced amplitude of recorded neural signals due to increased electrode-tissue distance [4]. | Gradual decrease in spike amplitude over weeks; increased difficulty in isolating single-unit activity. |
| Increased Stimulation Threshold | More energy required to activate neurons due to the insulating fibrotic capsule [4]. | Previously effective stimulation parameters no longer elicit a neural response; higher current/voltage needed. |
| Loss of High-Frequency Information | The fibrotic tissue acts as a low-pass filter, attenuating high-frequency signal components [4]. | Deterioration in the quality of high-frequency local field potentials (LFP) and spike waveforms. |
| Chronic Inflammatory Cycle | Ongoing micro-movements of the electrode can cause persistent inflammation, worsening fibrosis [4]. | Impedance continues to slowly increase over many months without stabilization. |
Q3: What strategies can mitigate the impact of fibrosis on electrode performance?
A multi-faceted approach is required to mitigate fibrosis, focusing on material design, surgical technique, and pharmacological intervention.
Material and Geometric Strategies:
- Flexible Substrates: Use electrodes with a low Young's modulus to reduce mechanical mismatch with soft neural tissue, thereby minimizing chronic inflammatory stimuli [17] [4].
- Miniaturization: Design smaller, filament-like electrodes to reduce the cross-sectional area of implantation and acute injury [4].
- Self-Healing Materials: Investigate novel conductive polymers and composites that can autonomously recover their electrical properties after mechanical damage, thus maintaining performance despite material fatigue in dynamic implant environments [16].
Pharmacological and Surface Modification Strategies:
- Drug-Eluting Systems: Develop controlled-release coatings that deliver anti-inflammatory drugs (e.g., dexamethasone) locally to the implantation site to suppress the immune response [4] [15].
- Biocompatible Coatings: Apply surface modifications such as hydrophilic polymers or biomimetic peptides to make the electrode "invisible" to the immune system [4].
Diagram: The fibrosis cascade and mitigation strategies post-electrode implantation, showing the progression from acute inflammation to performance degradation and the points where different intervention strategies can be applied.
Detailed Experimental Protocols for Fibrosis Assessment
Protocol 1: Longitudinal Impedance Monitoring in Chronic Models
This protocol is adapted from methodologies used in cochlear implant and peripheral nerve interface studies to track impedance as a proxy for tissue response [14] [15].
Objective: To characterize the dynamics of the tissue-electrode interface over time through frequent impedance measurements.
Materials:
- Custom Sound SQL database or equivalent for data management [18]
- MATLAB (R2023b or newer) for data processing scripts [18]
- Impedance measurement system (e.g., MAESTRO software for IFT or a custom neuroprosthetic system with telemetry) [15]
Procedure:
- Baseline Measurement: Record impedance values immediately after implantation and again at the initial activation/post-operative check (typically 2-4 weeks for neural interfaces) [18] [15].
- Frequent Sampling: For high temporal resolution, collect measurements twice daily (morning and evening) to capture diurnal fluctuations and the impact of electrical stimulation onset [15].
- Data Analysis: Calculate the mean impedance across all electrode channels. Analyze the trajectory over distinct post-operative phases:
- Correlation with Stimulation: Compare impedance trends between experimental groups with and without electrical stimulation to isolate its effect on the tissue response [15].
Protocol 2: Histological Correlation of Impedance and Fibrotic Tissue
This protocol is based on a study that directly correlated electrical measurements with in-situ imaging of the electrode-nerve interface [14].
Objective: To quantitatively assess the relationship between measured impedance/evoked potential thresholds and the physical properties of the fibrotic interface.
Materials:
- Chronic in vivo electrode array (e.g., extraneural four-platinum electrode array) [14]
- Serial block-face staining and imaging setup [14]
- Standard electrophysiology setup for measuring common ground impedance, transimpedance, and electrically evoked neural thresholds [14]
Procedure:
- Chronic Implantation: Implant the electrode array on the target nerve (e.g., rat pelvic nerve) for a defined period (e.g., two weeks) [14].
- Electrical Measurements: Periodically measure common ground impedance, transimpedance, and neural thresholds throughout the implantation period [14].
- In-situ Imaging: At the study endpoint, use a serial block-face staining and imaging technique to preserve the spatial relationship between the electrode and the tissue. This allows for precise measurement of the fibrotic tissue area and the distance from the electrode surface to the neural tissue [14].
- Statistical Analysis: Perform correlation analysis between the final electrical measurements (impedance and thresholds) and the quantified histological metrics (fibrotic area, nerve distance). Studies using this method have found that while impedance indicates the presence of interface tissue, it may not correlate with the absolute amount of fibrosis, highlighting the need for direct histological validation [14].
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Research Reagents and Materials for Investigating Electrode-Fibrosis Interactions
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| PEDOT:PSS Conductive Polymer | Coating to reduce electrode impedance and improve charge transfer efficiency [17]. | Enhances interface stability but long-term durability in vivo requires further investigation. |
| Self-Healing Polymers (SHP) | Substrate for creating neural interfaces that recover from mechanical fatigue [16]. | Critical for maintaining performance in dynamic implant environments; look for low Tg and high toughness. |
| Dexamethasone | Anti-inflammatory drug incorporated into drug-eluting coatings to suppress local immune response [15]. | Effective in reducing acute inflammation; optimal release kinetics for chronic applications is an active research area. |
| Poly(L-lactic acid)-poly(trimethylene carbonate) (PLLA-PTMC) | Biodegradable substrate for temporary neural interfaces [17]. | Eliminates need for explantation; degradation rate must match the period of intended use. |
| Silk Fibroin-based Nerve Conduits | Biocompatible, degradable scaffolds providing mechanical support and promoting nerve regeneration [17]. | Offers excellent biocompatibility and tunable degradation properties. |
| Ag nanowire/Ag flake composites | Conductive fillers in self-healing bilayer electrodes for recoverable electrical percolation pathways [16]. | Pt coating is often necessary to enhance biocompatibility and charge injection capacity. |
FAQs on Fibrosis and Electrode Performance
Q: Can the immune response in one implantation site affect a subsequent site in the same subject? A: Emerging evidence suggests yes. A retrospective study on sequential bilateral cochlear implants found that the second implanted ear exhibited a more rapid increase and greater magnitude of electrode impedance. This is consistent with a robust immune response in the second ear, potentially due to immunological memory or "contralateral priming" from the first implant [18].
Q: Are there new material technologies that actively combat performance degradation? A: Yes, cutting-edge research focuses on "performance-recoverable" systems. For example, self-healing, stretchable bilayer (SSB) electrodes have been developed that can spontaneously reconstruct their electrical percolation pathways after damage or fatigue, effectively recovering their electrical performance within seconds. This is a promising strategy to counteract the chronic degradation caused by the inflammatory environment [16].
Q: How does the mechanical property of an electrode influence fibrosis? A: The mechanical mismatch between a rigid electrode and soft neural tissue is a primary driver of chronic inflammation and fibrosis. Flexible electrodes with a low Young's modulus significantly reduce this mismatch, leading to less persistent glial scarring and better long-term signal stability. The shape and implantation method must be coordinated to minimize acute injury during insertion [4].
Q: Is impedance a reliable standalone metric for fibrosis in peripheral nerve interfaces? A: Caution is advised. A study on rat pelvic nerves found no significant correlation between impedance or neural threshold and the quantified area of fibrotic tissue. While impedance indicates interface changes, it should not be used as the sole metric for fibrosis severity. Combining electrical measurements with histological validation is considered best practice [14].
Troubleshooting Guide: Chronic Inflammation and Electrode Failure
Q1: Why does a glial scar form around my implanted neural electrode, leading to signal degradation? The formation of a glial scar, or glial encapsulation, is a direct consequence of the chronic foreign body response triggered by the mechanical mismatch between the implanted electrode and the surrounding brain tissue [19]. Brain tissue is exceptionally soft, with a Young's modulus of approximately 1–10 kPa [4] [20]. When a rigid electrode (e.g., silicon at ~102 GPa or platinum at ~102 MPa) is implanted, this stiffness mismatch causes ongoing micro-movements and friction against the soft neural tissue [4]. This persistent mechanical irritation activates microglia and astrocytes. Activated microglia adopt an amoeboid shape, proliferate, and release pro-inflammatory cytokines and cytotoxic factors [19]. Astrocytes become reactive, undergo hypertrophy, and upregulate Glial Fibrillary Acidic Protein (GFAP), secreting extracellular matrix components that eventually form a dense, insulating physical barrier around the electrode [19] [4]. This scar tissue increases the distance between neurons and the electrode's recording sites, causing a rapid attenuation of neural signals and a sharp rise in impedance, ultimately leading to electrode failure [4].
Q2: What are the key cellular events following electrode implantation that lead to chronic inflammation? The tissue response unfolds over acute and chronic timescales [19]:
- Initial Injury and Acute Response (First 24-48 hours): Electrode insertion severs blood vessels, tears the extracellular matrix, and ruptures neural cell bodies and processes. This leads to bleeding, serum protein leakage, and the infiltration of blood-borne immune cells. Microglia are activated within hours, sending projections toward the injury site and migrating to surround the implant within 24 hours [19].
- Chronic Response (Weeks to Months): The sustained mechanical mismatch prevents the resolution of inflammation. Microglia remain activated, and astrocytes continue to proliferate and deposit extracellular matrix. The result is the formation of a persistent glial scar, which isolates the electrode from the functional neural tissue [19] [20].
Q3: My flexible electrode still triggers an immune response. Why? While flexible electrodes with a lower Young's modulus significantly reduce mechanical mismatch compared to rigid devices, they are not entirely invisible to the immune system [4]. The implantation method itself is a key factor. Flexible electrodes often require rigid shuttles for insertion, which temporarily recreate the problem of a stiff device penetrating the brain, causing acute injury [4]. Furthermore, the geometric design of the electrode (e.g., its cross-sectional area and shape) continues to influence the extent of chronic inflammation. Even a flexible electrode with a large cross-section can cause significant tissue displacement and sustain a chronic inflammatory response due to macroscopic movements against the tissue [4].
Q4: How can I measure the success of my strategy to reduce fibrosis? Success can be evaluated through a combination of histological, functional, and electrochemical assessments, as summarized in the table below.
Table 1: Key Metrics for Assessing Reduced Fibrosis and Improved Biocompatibility
| Assessment Category | Specific Metric | Methodology/Technique |
|---|---|---|
| Histological Analysis | Microglial Activation | Immunohistochemical staining for markers like ED1; quantify cell density and morphology around the implant [19]. |
| Astrocytic Scarring | Immunohistochemical staining for GFAP; measure the thickness and density of the GFAP-positive barrier [19]. | |
| Neuronal Survival | Staining for neuronal markers (e.g., NeuN); quantify neuronal density in the vicinity of the electrode [19]. | |
| Functional Performance | Signal-to-Noise Ratio (SNR) | Record neural signals over time; a stable or increasing SNR indicates healthy interface stability [20]. |
| Electrode Impedance | Measure impedance at 1 kHz; a stable, low impedance suggests minimal scar tissue formation [19]. | |
| Recording Longevity | Stable Single-Unit Yield | Track the number of distinct, isolatable neurons over weeks or months; extended longevity indicates reduced inflammatory encapsulation [4]. |
Experimental Protocols for Key Investigations
Protocol 1: Assessing the Acute and Chronic Tissue Response to Implanted Electrodes
- Objective: To characterize the timeline of glial activation and scar formation around an electrode with different stiffness profiles.
- Materials: Electrodes (rigid vs. flexible), animal model (e.g., rat or mouse), stereotaxic surgical setup, perfusion and fixation equipment, cryostat, antibodies (e.g., anti-Iba1 for microglia, anti-GFAP for astrocytes, anti-NeuN for neurons).
- Methodology:
- Implantation: Surgically implant the test electrodes into the target brain region(s) using aseptic techniques.
- Time-Point Sacrifice: Euthanize animals and perform transcardial perfusion with paraformaldehyde at predetermined time points (e.g., 24 hours, 1 week, 4 weeks, 8 weeks post-implantation).
- Tissue Processing: Extract brains, post-fix, cryoprotect, and section tissue into slices containing the electrode track.
- Immunohistochemistry: Label tissue sections with fluorescent antibodies against Iba1, GFAP, and NeuN.
- Imaging and Quantification: Use confocal or fluorescence microscopy to image the tissue surrounding the implant. Quantify metrics such as microglial density, astrocytic scar thickness, and neuronal density within defined radii from the electrode track [19].
Protocol 2: Evaluating Electrode Performance via Electrochemical Impedance Spectroscopy (EIS)
- Objective: To monitor the functional integrity of the electrode-tissue interface and infer scar formation.
- Materials: Implanted electrode, potentiostat/impedance analyzer, reference electrode, counter electrode.
- Methodology:
- Baseline Measurement: Perform EIS on the electrode in saline prior to implantation to establish a baseline.
- In Vivo Tracking: At regular intervals post-implantation, connect the implanted electrode to the analyzer and record the impedance spectrum, typically from 1 Hz to 100 kHz.
- Data Analysis: Focus on the impedance magnitude at 1 kHz, which is strongly influenced by the biological environment. A steady increase over time is indicative of insulating scar tissue forming around the electrode [19] [21].
Signaling Pathways in the Foreign Body Response
The following diagram illustrates the key cellular and molecular events triggered by electrode implantation.
Strategies for Mitigating Mechanical Mismatch
The diagram below outlines a strategic workflow for developing neural interfaces that minimize the foreign body response.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Neural Interface Biocompatibility Research
| Reagent / Material | Function / Application | Key Consideration |
|---|---|---|
| Flexible Polymer Substrates (e.g., Polyimide, Parylene C) | Serves as the base material for electrodes, providing a low Young's modulus that better matches brain tissue (1-10 kPa) [4] [20]. | Reduces chronic mechanical mismatch and micromotion-induced damage. |
| Conductive Coatings (e.g., PEDOT:PSS, Carbon Nanotubes) | Coated on electrode sites to improve charge transfer capacity and lower interfacial impedance, enhancing signal quality [20]. | Can improve the efficiency of stimulation and the signal-to-noise ratio of recordings. |
| Bio-Dissolvable Stiffeners (e.g., Polyethylene Glycol - PEG) | Temporarily increases the stiffness of a flexible electrode to enable penetration; dissolves post-implantation to restore flexibility [4]. | Mitigates acute implantation injury caused by rigid shuttles. |
| Anti-inflammatory Agents (e.g., Dexamethasone) | Incorporated into electrode coatings for controlled release to locally suppress the immune response post-implantation [4]. | Actively modulates the inflammatory environment to reduce glial activation. |
| Immunohistochemistry Antibodies (anti-Iba1, anti-GFAP, anti-NeuN) | Used to label and quantify microglia, astrocytes, and neurons in tissue sections for post-mortem analysis of the tissue response [19]. | Critical for validating the efficacy of any new electrode design or anti-fibrosis strategy. |
Innovative Material and Bioengineering Solutions for Anti-Fibrotic Interfaces
Technical Support Center: Troubleshooting and FAQs
This technical support center provides troubleshooting guides and frequently asked questions (FAQs) for researchers working with Polyimide, Polydimethylsiloxane (PDMS), and Polylactic acid (PLA) in the context of developing neural electrodes with reduced fibrotic response. The content is framed within a broader thesis on reducing fibrosis around neural implants.
Troubleshooting Guides
Common Experimental Challenges and Solutions
Problem: Excessive Fibrosis and Glial Scarring Around Implant
- Symptoms: Gradual degradation of neural signal quality (increased impedance, signal attenuation) over weeks to months post-implantation [4].
- Potential Causes:
- Solutions:
- Optimize mechanical properties: Blend rigid polymers like PLA with softer polymers (e.g., PCL) or design flexible, thin-film electrodes to lower the bending stiffness and better match neural tissue [22] [4].
- Apply surface modifications: Functionalize the electrode surface with bioactive coatings (e.g., PEG, laminin) or drug-eluting systems to actively suppress the immune response and promote integration [22] [4].
Problem: Uncontrolled or Unexpected Polymer Degradation
- Symptoms: Premature loss of mechanical integrity, altered surface morphology, and unexpected local tissue reactions.
- Potential Causes:
- Solutions:
- Control environmental factors: During in vitro testing, precisely control the temperature and pH of the immersion solution. A temperature increase of 50°C can accelerate PLA hydrolysis by 30-50% [22].
- Modify polymer chemistry: Copolymerize with more hydrophobic monomers or adjust crystallinity to slow down hydrolysis rates.
Problem: Poor Cell Adhesion or Cytotoxicity on Polymer Surface
- Symptoms: Low cell viability in in vitro assays, poor integration with host tissue in vivo.
- Potential Causes:
- Solutions:
- Perform rigorous extraction cytotoxicity testing: Follow ISO 10993-5 guidelines, using methods like MTT assay to ensure cell viability is typically above 70% for device extracts [23].
- Enhance bioactivity: Modify the surface with extracellular matrix (ECM) proteins (e.g., collagen, laminin) or arginine-glycine-aspartic acid (RGD) peptides to promote cell attachment [22].
Frequently Asked Questions (FAQs)
Q1: What are the key regulatory standards for biocompatibility testing of implantable neural devices? A1: The ISO 10993 series is the internationally recognized standard for the biological evaluation of medical devices [24]. Key parts for neural implants include:
- ISO 10993-1: Provides the overall framework for evaluation within a risk management process.
- ISO 10993-5: Specifies tests for in vitro cytotoxicity, a fundamental requirement for all devices [23] [24].
- ISO 10993-6: Evaluates local effects after implantation, which is critical for assessing fibrosis and tissue integration [25].
- ISO 10993-10: Covers tests for skin sensitization and irritation [24]. Always consult regional regulatory bodies like the FDA or EMA, as they provide specific guidances that align with, but may not fully recognize, all ISO standards [26] [23].
Q2: How does the "Big Three" in biocompatibility testing apply to my neural electrode made of Polyimide? A2: The "Big Three" tests—cytotoxicity, irritation, and sensitization—are required for almost all medical devices, including your Polyimide electrode [23].
- Cytotoxicity: Assesses if leachables from the Polyimide device kill cultured cells (e.g., L929 fibroblasts). This is a first-line screening test [23].
- Irritation: Evaluates the potential for the device to cause localized inflammation, which directly relates to the fibrotic response you aim to minimize.
- Sensitization: Determines if the device materials can cause an allergic reaction. These tests are typically performed on extracts of your device and are a mandatory part of the safety profile for regulatory submissions [23].
Q3: Beyond the "Big Three," what other biocompatibility tests are critical for chronic neural implants? A3: For long-term implants, additional evaluations are essential:
- Implantation Study (ISO 10993-6): This is crucial. It involves histopathological examination of the tissue surrounding the implant to quantify the immune response, fibrosis (collagen deposition), and tissue integration [25].
- Genotoxicity (ISO 10993-3): Ensures materials do not cause genetic damage.
- Systemic Toxicity (ISO 10993-11): Assesses potential effects on distant organs.
- Hemocompatibility (ISO 10993-4): Required if the device has contact with blood [24].
The following tables summarize key properties and experimental data for the polymers in the context of neural interfaces.
Table 1: Key Properties of Polyimide, PDMS, and PLA for Neural Interfaces
| Property | Polyimide | PDMS | PLA | Relevance to Neural Interfaces |
|---|---|---|---|---|
| Young's Modulus | ~2-8 GPa [4] | ~0.36-3 MPa [4] | ~1.5-3.5 GPa [22] | PDMS is closer to brain tissue (~1-10 kPa), reducing mechanical mismatch [20]. |
| Biodegradability | Non-degradable | Non-degradable | Degradable (hydrolytic/enzymatic) [22] | PLA is suitable for temporary implants; degradation rate must be controlled. |
| Key Biocompatibility Advantage | Excellent electrical insulation, high strength | High flexibility, low stiffness, gas permeable | Biocompatible, tunable degradation | PDMS minimizes chronic inflammation; PLA resorbs, avoiding a second surgery. |
| Key Biocompatibility Challenge | Can be stiff, leading to mechanical mismatch | Hydrophobic, can adsorb proteins, potential for encapsulation | Acidic degradation products may cause inflammation [22] | Surface modification is often required for PDMS and PLA to improve bio-inertness or buffer pH. |
Table 2: Summary of Key Biocompatibility Tests Based on ISO 10993
| Test Endpoint | Standard | Typical Method | Application to Neural Electrodes |
|---|---|---|---|
| Cytotoxicity | ISO 10993-5 [23] [24] | MTT/XTT assay on device extracts using L929 or Balb 3T3 cells [23] | First-line screening for leachable substances; >70% cell viability is a positive indicator [23]. |
| Sensitization | ISO 10993-10 [24] | Guinea Pig Maximization Test (in vivo) or in vitro alternatives | Assesses risk of allergic contact dermatitis from device materials. |
| Irritation | ISO 10993-10, -23 [24] | Skin irritation test (in vivo or in vitro models) | Evaluates potential for localized inflammatory response. |
| Implantation | ISO 10993-6 [25] | Histopathology of implanted site (H&E, Masson's Trichrome staining) [25] | Critical test for fibrosis; quantifies inflammation, collagen deposition, and tissue integration. |
Detailed Experimental Protocols
Protocol 1: In Vitro Cytotoxicity Testing by Extraction (Based on ISO 10993-5)
- Objective: To determine if leachables from the polymer sample are cytotoxic.
- Materials: Polymer samples (Polyimide, PDMS, PLA), cell culture medium (extraction vehicle), L929 fibroblast cells, 96-well cell culture plates, MTT reagent, incubator.
- Procedure:
- Sample Preparation: Sterilize the polymer samples and immerse in culture medium at a surface area-to-volume ratio of 3 cm²/mL or 6 cm²/mL. Incubate at 37°C for 24 hours to create the extract [23].
- Cell Seeding: Seed L929 cells in a 96-well plate and culture until near-confluent.
- Exposure: Replace the culture medium in the wells with the polymer extract. Include a negative control (medium only) and a positive control (e.g., latex extract).
- Incubation: Incubate the cells with the extract for 24 hours at 37°C.
- Viability Assessment: Add MTT reagent to the wells. Living cells will convert MTT to purple formazan crystals. After solubilizing the crystals, measure the absorbance at 570 nm.
- Analysis: Calculate cell viability as a percentage of the negative control. A reduction in cell viability by more than 30% (i.e., viability below 70%) may indicate cytotoxicity [23].
Protocol 2: Histopathological Evaluation of Tissue Response Post-Implantation (Based on ISO 10993-6)
- Objective: To qualitatively and quantitatively assess the foreign body response, including fibrosis, to the implanted polymer in vivo.
- Materials: Polymer implants, animal model (e.g., rat), fixation buffer (e.g., formalin), paraffin or resin, microtome, staining solutions (H&E, Masson's Trichrome).
- Procedure:
- Implantation: Aseptically implant the polymer sample into the target tissue (e.g., brain, muscle) for a defined period (e.g., 4, 12, 26 weeks).
- Tissue Harvesting and Fixation: At the endpoint, carefully excise the implant with the surrounding tissue and fix in formalin to preserve tissue architecture [25].
- Processing and Sectioning: Dehydrate the tissue, embed it in paraffin or resin, and section it into thin slices (3-7 µm) using a microtome. Specialized laser microtomes (e.g., Tissue Surgeon) can be used for hard polymer-tissue composites [25].
- Staining:
- Analysis and Scoring: A board-certified pathologist examines the slides semi-quantitatively. Key parameters are scored:
- Inflammation: Number and distribution of lymphocytes, plasma cells, macrophages, and giant cells.
- Fibrosis: Thickness and density of the collagen capsule around the implant.
- Necrosis: Presence of dead tissue cells.
- Advanced Analysis: Digital pathology and AI-driven histomorphometry (e.g., with Visiopharm software) can be used for precise quantification of tissue density, cell counts, and capsule thickness [25].
Research Reagent Solutions
Table 3: Essential Materials for Biocompatibility and Fibrosis Research
| Reagent / Material | Function | Example Application |
|---|---|---|
| L929 Fibroblast Cells | A standard cell line for in vitro cytotoxicity testing [23]. | Screening polymer extracts for cytotoxic leachables. |
| MTT/XTT Assay Kits | Colorimetric assays to measure cell metabolic activity and viability [23]. | Quantifying cytotoxicity in accordance with ISO 10993-5. |
| Anti-PEG Antibodies | Research tool to study immune responses to PEGylated surfaces [22]. | Investigating pre-existing or induced immunity to a common coating polymer. |
| Masson's Trichrome Stain | Histological stain that differentiates collagen (blue/green) from muscle and cytoplasm (red) [25]. | Visualizing and quantifying fibrotic capsule formation around explanted devices. |
| Visiopharm Software | AI-driven digital pathology image analysis platform [25]. | Performing precise, reproducible histomorphometry on tissue sections. |
Experimental Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for evaluating a new polymer for a neural interface, from initial concept to advanced in vivo analysis.
Polymer Evaluation Workflow for Neural Interfaces
The diagram below outlines the key biological signaling pathways activated upon implantation of a neural electrode, leading to the critical outcome of fibrosis.
Fibrosis Pathway and Mitigation Strategies
This technical support guide provides troubleshooting and methodological assistance for researchers developing conductive, flexible composites based on PEDOT:PSS and nanomaterial hybrids. The content is specifically framed within a thesis research context aimed at reducing fibrosis around neural electrodes. The mechanical mismatch between rigid conventional electrodes and soft neural tissue (Young's modulus of 1–10 kPa) is a primary driver of the foreign body response, leading to glial scar formation and signal degradation [27] [20]. The strategies discussed herein focus on creating soft, compliant interfaces to mitigate this response.
Troubleshooting Guides & FAQs
PEDOT:PSS Formulation and Processing
Q1: My pristine PEDOT:PSS film has low conductivity (<1 S/cm). How can I enhance it effectively?
- A: Low conductivity of pristine PEDOT:PSS is a common issue due to the insulating PSS shells surrounding conductive PEDOT cores [28]. The following strategies can yield significant improvements:
Table 1: Conductivity Enhancement Strategies for PEDOT:PSS
| Method | Mechanism | Typical Conductivity Achieved | Considerations for Neural Interfaces |
|---|---|---|---|
| Secondary Dopants (e.g., DMSO, EG) | Screen electrostatic attraction between PEDOT and PSS, facilitating charge hopping [29] [28]. | 10 - 1000 S/cm | Improves performance without introducing non-biocompatible nanoparticles. |
| Nanomaterial Blending (e.g., Graphene, Ag NPs) | Bridges PEDOT islands, creating additional conductive pathways [30] [28]. | Can exceed 1000 S/cm [28] | Biocompatibility check is critical. Silver nanoparticles may offer antimicrobial properties. |
| Multiple Deposition | Increases the concentration of PEDOT grains and improves film connectivity [28]. | Increases exponentially with layer number [28] | Increases film thickness, which may affect flexibility. |
| Acid Treatment (e.g., H₂SO₄) | Removes excess PSS and reorders PEDOT crystallites [29]. | Up to 4380 S/cm [29] | Harsh processing may not be suitable for all substrates; requires careful rinsing. |
Q2: My PEDOT:PSS film does not adhere well to the substrate (e.g., flexible Mylar or Si wafer). What is the solution?
- A: Poor adhesion is often due to contamination or insufficient surface energy. Implement a rigorous substrate cleaning and activation protocol [28]:
- Cleaning: Sonicate substrates in acetone for 10 minutes, followed by isopropyl alcohol (IPA) for another 10 minutes.
- Rinsing and Drying: Rinse with deionized (DI) water and blow-dry with nitrogen.
- Dehydration: Place substrates on a pre-heated hot plate at 110°C for 1-2 minutes.
- Surface Activation: Treat the cleaned substrate with oxygen plasma. This step is crucial for ensuring uniform coverage and strong adhesion for subsequent spin-coating [28].
Q3: How can I pattern PEDOT:PSS for creating microelectrodes?
- A: Standard photolithography can chemically deteriorate PEDOT:PSS. A reliable method uses a sacrificial metal layer [28]:
- Deposit a thin sacrificial metal layer (e.g., Silver) on the PEDOT:PSS film.
- Deposit and pattern a photoresist on top of the silver layer using standard lithography.
- Etch the exposed silver using a suitable etchant (e.g., nitric acid), which selectively removes the silver without damaging the underlying PEDOT:PSS.
- Etch the now-exposed PEDOT:PSS segments using oxygen plasma.
- Strip the remaining photoresist and etch the remnant silver islands, leaving behind the patterned PEDOT:PSS.
Mechanical and Biocompatibility Issues
Q4: The composite is too brittle and cracks under strain. How can I improve its stretchability?
- A: Pristine PEDOT:PSS films are flexible but only stretchable to ~10% [29]. To enhance stretchability for applications requiring tissue conformability:
- Blend with Elastomers/Plasticizers: Incorporate soft polymers (e.g., polyethylene oxide - PEO) or plasticizers to increase the elastic compliance of the composite [29] [30].
- Form Fibers or Gels: Processing PEDOT:PSS into hydrogel matrices or fibers can significantly enhance deformability and mimic the mechanical properties of neural tissue [29] [27].
- Deposit on Pre-strained Elastomers: Transfer the conductive film to a pre-stretched elastomer like PDMS. Upon release, the film forms wavy, buckled structures that can accommodate large tensile strains [29].
Q5: How can I assess the mechanical mismatch between my composite and neural tissue?
- A: The key parameter is the Young's (Elastic) Modulus. Neural tissue has a soft consistency, with a Young's modulus ranging from 1 to 10 kPa [20] [27]. Your composite should aim to be in this range. Nanoindentation or tensile testing can be used to characterize the modulus of your film. A significant mismatch with traditional materials like silicon (~180 GPa) or platinum (~170 GPa) contributes to chronic inflammation and scar tissue formation [27] [20].
Experimental Protocols for Key Experiments
Protocol: Formulating and Screen-Printing a PEDOT:PSS/Graphene Composite Ink
This protocol is adapted for creating flexible, conductive patterns on various substrates [30].
Objective: To prepare a stable, printable ink that exhibits enhanced electrical conductivity and excellent flexibility for deformable electronic devices.
Materials:
- PEDOT:PSS aqueous dispersion (e.g., Clevios PH1000)
- Graphene powder or solution
- Polyethylene Oxide (PEO) - as a viscosity modifier
- Deionized (DI) Water
- Screen printer and appropriate mesh screens
- Target substrate (e.g., oxygen plasma-treated Mylar)
Method:
- Ink Synthesis: Mix PEDOT:PSS dispersion with graphene powder at a predetermined weight ratio. Sonication or vigorous stirring is required to achieve a homogeneous dispersion.
- Viscosity Adjustment: Add PEO incrementally to the composite mixture. The ratio of PEO is critical to adjust the ink's viscosity and flowability without compromising electrical properties. A trade-off exists between ink printability, resolution, and electrical performance.
- Printing: Use the synthesized ink for screen printing onto the activated substrate. Optimize printing parameters (squeegee pressure, speed) for pattern resolution.
- Curing: Allow the printed patterns to dry and cure, typically at mild temperatures (e.g., 60-90°C) to evaporate solvents and set the film.
Troubleshooting: If the printed circuit cracks, reduce the graphene content or increase the PEO plasticizer. If the pattern resolution is poor, increase the PEO content to increase viscosity or optimize screen mesh size.
Protocol: Enhancing Biocompatibility and Reducing Fibrosis via Surface Biofunctionalization
Objective: To create a "bioactive" neural interface that minimizes the foreign body response (FBR) and glial scar formation.
Materials:
- Fabricated soft electrode (e.g., PEDOT:PSS-based composite)
- Relevant biomolecules (e.g., Laminin, Fibronectin, anti-inflammatory drugs like Dexamethasone)
- Hydrogel matrix (e.g., GelMA, agarose)
- Standard cell culture or sterile handling equipment
Method:
- Surface Coating: Physically adsorb or chemically tether biomolecules to the electrode surface. These can be peptides derived from extracellular matrix (ECM) proteins (e.g., Laminin) to promote neuronal attachment over glial cells.
- Hydrogel Encapsulation: Encapsulate the soft electrode within a hydrogel layer. Hydrogels closely match the mechanical properties of brain tissue and can be loaded with anti-inflammatory drugs for localized, sustained release to suppress the initial immune response [27].
- In-Vitro Validation: Culture the functionalized electrodes with a mixed cell population (e.g., neurons and astrocytes) to assess selective neuronal adhesion and reduced astrocytic activation.
Troubleshooting: If the coating delaminates, use stronger covalent bonding strategies (e.g., silane chemistry). If the drug releases too quickly, adjust the hydrogel cross-linking density.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials for Developing Low-Fibrosis Neural Electrodes
| Item | Function in Research | Key Consideration |
|---|---|---|
| PEDOT:PSS Dispersion | The primary conductive polymer; provides the foundation for the flexible, organic electrode [29] [28]. | Commercial sources (e.g., Clevios) vary; conductivity can be enhanced with secondary dopants. |
| Graphene / Carbon Nanotubes | Nanomaterial additives to significantly enhance the electrical conductivity and mechanical robustness of the composite [30] [27]. | Functionalization may be needed for stable dispersion in polymer matrix. |
| PDMS / Soft Elastomers | Used as flexible substrates or encapsulation layers to achieve a low elastic modulus matching neural tissue [27]. | Surface activation (e.g., oxygen plasma) is required for adhesion. |
| Polyethylene Oxide (PEO) | A polymer additive that acts as a plasticizer to improve ink printability and composite stretchability [30]. | Ratio must be optimized for a trade-off between mechanical and electrical properties. |
| Oxygen Plasma System | Critical for cleaning and activating substrate surfaces to ensure strong adhesion of PEDOT:PSS films [28]. | Standard equipment in cleanroom or microfluidic fabrication labs. |
| Laminin / Fibronectin | ECM-derived proteins for bioactive surface functionalization to promote neuronal integration and reduce glial scarring [27]. | Requires sterile handling and specific buffer conditions for coating. |
| Biocompatible Hydrogels | Used to create a soft, hydrated interface between the electrode and tissue, mitigating FBR [27]. | Choice of hydrogel (e.g., GelMA, agarose) influences drug release and cell interaction. |
Workflow and Signaling Pathways
The following diagram illustrates a recommended experimental workflow for developing and characterizing these composites, from material synthesis to in-vitro biocompatibility validation.
Figure 1: Experimental Workflow for Neural Electrode Development
Troubleshooting Guide: Common Experimental Challenges in Reducing Fibrosis
FAQ 1: Why is there a progressive decline in the signal-to-noise ratio of my neural recordings over several weeks? This is a classic sign of the foreign body response (FBR), where the body recognizes the implant as a foreign object [27]. The process begins with protein adsorption and leads to the activation of microglia and astrocytes, resulting in the formation of a protective glial scar and fibrotic tissue around the electrode [31] [32]. This fibrotic capsule electrically insulates the electrode from nearby neurons, increasing impedance and degrading signal quality [33] [34]. The chronic inflammatory response can persist for the duration of the implant, continually compromising performance [32].
FAQ 2: Our soft electrode prototypes are difficult to implant without buckling. How can this be overcome? Buckling is a common issue due to the low flexural rigidity of soft materials. Successful strategies involve the use of temporary, biodegradable stiffeners. A widely cited method uses silk fibroin, a nature-derived material, as a supportive shuttle [31]. The electrode is spin-coated with a layer of silk fibroin, which provides the necessary rigidity for insertion into neural tissue. Upon contact with physiological fluids, the silk layer dissolves, leaving the soft, flexible electrode in place, perfectly conforming to the target tissue [31].
FAQ 3: We've applied a bioactive coating, but it seems to degrade or delaminate too quickly in vivo. What are we doing wrong? Coating stability is a significant hurdle. Physically adsorbed coatings (e.g., laminin, collagen) can rapidly desorb or degrade enzymatically, diminishing their intended bioactivity [32]. To improve longevity, shift your strategy to covalent immobilization. For example, the anti-inflammatory drug dexamethasone can be covalently bound to a polyimide electrode surface, ensuring slow, local release over at least two months [35]. Similarly, the neuronal adhesion molecule L1 has been covalently immobilized on silicon, leading to improved recording yield over 16 weeks [32].
FAQ 4: Our conductive polymer coating (PEDOT:PSS) is showing signs of electrochemical instability during chronic stimulation. How can we improve its resilience? Pure conductive polymer coatings can suffer from mechanical fatigue and delamination under prolonged electrical cycling. A proven solution is to use composite materials. Doping PEDOT with negatively charged carbon nanotubes creates a nanofibrous, interpenetrating network that enhances both mechanical robustness and electrical performance [32]. This composite structure promotes cellular process ingrowth, which can further stabilize the interface and has been shown to provide stable recording and higher stimulation efficiency over 12 weeks in vivo [32].
Experimental Protocols: Key Methodologies for the Field
Protocol: Covalent Immobilization of Dexamethasone on Polyimide
This protocol is based on a recent study that demonstrated reduced immune response and improved chronic stability [35].
- Objective: To create a neural implant with a slow-release anti-inflammatory drug coating.
- Materials:
- Polyimide-based neural electrodes
- Dexamethasone
- Appropriate crosslinking agents (e.g., EDC/NHS chemistry)
- Solvents (DMF, Ethanol)
- Standard cell culture materials for biocompatibility testing (e.g., immune cell lines)
- Methodology:
- Surface Activation: Clean and activate the polyimide surface using an oxygen plasma treatment to generate reactive functional groups (e.g., carboxyl groups).
- Chemical Coupling: Incubate the activated polyimide with dexamethasone in the presence of a crosslinking agent. The study used a specific chemical strategy to enable covalent binding, ensuring the drug is not merely adsorbed [35].
- Washing and Sterilization: Thoroughly rinse the coated devices in sterile solvent to remove any unbound drug molecules. Sterilize using ethylene oxide or low-temperature plasma.
- In Vitro Validation:
- Release Kinetics: Soak the coated implant in phosphate-buffered saline (PBS) at 37°C and use high-performance liquid chromatography (HPLC) to quantify drug release over time. The cited method demonstrated release for a critical period of at least two months [35].
- Biocompatibility: Culture immune cells (e.g., macrophages) on the coated surface and assay for inflammatory markers (e.g., TNF-α, IL-1β) to confirm reduced activation.
- In Vivo Application: Implant the functionalized device in the target neural tissue (e.g., peripheral nerve). After 4-6 weeks, perform histological analysis to quantify the density of glial fibrillary acidic protein (GFAP)-positive astrocytes and IBA1-positive microglia around the implant site, comparing against uncoated controls [35].
Protocol: Characterizing the Foreign Body Response to Soft Implants
This guideline provides a framework for comprehensively evaluating new bio-inspired neural interfaces [36].
- Objective: To systematically assess the biocompatibility and functional integration of a soft neural electrode.
- Materials:
- Soft electrode (e.g., made from PDMS, SU-8, or conductive hydrogel)
- Electrochemical impedance spectrometer
- Histology reagents (fixatives, antibodies for neurons, astrocytes, microglia)
- Confocal microscope
- Methodology:
- Pre-implantation Characterization:
- Mechanical Testing: Measure the elastic modulus of your device material using a tensile tester or atomic force microscopy (AFM). Compare this to the modulus of neural tissue (~1-30 kPa) [27].
- Electrochemical Analysis: Perform cyclic voltammetry and electrochemical impedance spectroscopy (EIS) in PBS to establish baseline charge storage capacity and impedance [36].
- In Vivo Implantation: Surgically implant the device into the target neural region of an animal model (e.g., rat cortex). Ensure all procedures are approved by the relevant Institutional Animal Care and Use Committee (IACUC).
- Chronic Functional Monitoring:
- Signal Quality: Regularly record neural signals (local field potentials and/or single-unit activity) over the implantation period (e.g., 4-16 weeks). Track the number of recordable units and signal amplitude [33].
- Impedance Tracking: Periodically measure the electrode-tissue impedance at 1 kHz. A steady increase often correlates with fibrotic encapsulation [36].
- Endpoint Histological Analysis:
- Tissue Fixation and Sectioning: Perfuse the animal and extract the brain/nerve containing the implant. Section the tissue for immunohistochemistry.
- Immunostaining and Quantification: Stain tissue sections for:
- Neurons (NeuN): To quantify neuronal survival and density near the interface.
- Astrocytes (GFAP): To visualize and quantify astrocytic scarring.
- Microglia/Macrophages (IBA1): To assess the neuroinflammatory response.
- Use image analysis software to count cells and measure the thickness of the glial scar surrounding the implant track [31] [34].
- Pre-implantation Characterization:
The Scientist's Toolkit: Essential Reagents & Materials
Table 1: Key Research Reagent Solutions for Anti-Fibrosis Neural Interfaces
| Item Name | Function/Benefit | Key Considerations |
|---|---|---|
| Soft Substrates (PDMS, Polyimide) [27] | Provides flexible, tissue-matching mechanical base for electrodes (Elastic modulus ~kPa-MPa). Reduces mechanical mismatch and micromotion damage. | PDMS is gas-permeable and optically clear; Polyimide is a robust, microfabrication-friendly insulator. |
| Conductive Polymers (PEDOT:PSS) [27] [32] | Coating or stand-alone electrode material. Lowers impedance, increases charge injection capacity. Intrinsically softer than metals. | Can be doped with biologics (e.g., drugs) or mixed with nanotubes for enhanced stability [32]. |
| Dexamethasone [35] | Potent anti-inflammatory drug. Local release suppresses the foreign body response and subsequent fibrosis. | Covalent binding to the implant surface enables slow release over months, critical for long-term efficacy [35]. |
| Nature-Derived Materials (Hyaluronic Acid, Laminin, Silk Fibroin) [31] [32] | Bioactive coatings or structural elements. Mimic the extracellular matrix, providing familiar cues to neural cells and reducing inflammation. | Silk fibroin is excellent as a biodegradable stiffener. Hyaluronic acid has inherent anti-inflammatory properties [31]. |
| Zwitterionic Polymers (PSBMA) [32] | "Anti-fouling" surface coating. Creates a hydration layer that resists non-specific protein adsorption, the first step in the FBR. | Must be covalently grafted for stability. Can be further functionalized with bioactive molecules for multifunctionality [32]. |
Visualizing Core Concepts: Pathways and Workflows
Foreign Body Response Cascade
This diagram outlines the key cellular events following neural electrode implantation that lead to fibrosis and device failure.
Bio-integrative Coating Strategy Workflow
This flowchart illustrates the decision-making process for selecting and applying a bio-integrative coating to a neural device.
Understanding the Foreign Body Response (FBR) Against Neural Implants
The foreign body response is an immune-mediated reaction that leads to the rejection of implanted devices through a cascade of inflammatory events and wound-healing processes, resulting in fibrosis. This fibrotic capsule can disrupt biosensing functions, cut off nourishment for cell-based implants, and ultimately lead to device failure, presenting a fundamental challenge for chronic neural interfaces [37].
The following table summarizes the key cellular players and their roles in the FBR cascade:
Table 1: Key Cellular Events in the Foreign Body Response to Neural Implants
| Time Phase | Key Cells Involved | Primary Functions & Effects |
|---|---|---|
| Early (Hours-Days) | Neutrophils | First responders; secrete proteolytic enzymes and reactive oxygen species that can damage implants [37]. |
| Acute (Days) | Monocytes/Macrophages | Differentiate from infiltrating monocytes; secrete pro-inflammatory cytokines (IL-1, IL-8, MCP-1) and attempt to phagocytose the implant [37]. |
| Chronic (Days-Weeks) | Foreign Body Giant Cells (FBGCs) | Formed by macrophage fusion; presence indicates a persistent inflammatory state [37]. |
| Late (Weeks+) | Fibroblasts/Myofibroblasts | Produce collagen and extracellular matrix (ECM), leading to the formation of a dense, fibrotic capsule that isolates the implant [37]. |
The diagram below illustrates the key signaling pathways and cellular interactions in the FBR.
Experimental Protocols for Developing Drug-Eluting Coatings
Covalent Binding of Dexamethasone to Polyimide
This protocol details a method for creating a neural implant coating that provides sustained local release of an anti-inflammatory drug [38].
Key Reagents:
- Polyimide substrate (e.g., BPDA-PDA)
- Dexamethasone (DEX)
- Chemical agents for surface activation (e.g., linkers for covalent binding)
Methodology:
- Surface Activation: Chemically modify the surface of the polyimide electrode to create reactive groups for drug binding.
- Covalent Conjugation: Covalently bind DEX molecules to the activated surface using a specific chemical strategy. This step is crucial for achieving sustained release, as it prevents the rapid "burst release" of the drug.
- Characterization: Verify successful binding and quantify the drug loading on the surface using techniques like X-ray Photoelectron Spectroscopy (XPS) or Fourier Transform Infrared (FTIR) spectroscopy.
- Release Kinetics: Perform in vitro elution studies by incubating the coated substrate in a buffer (e.g., phosphate-buffered saline) at 37°C. Sample the buffer at regular intervals over several weeks and use High-Performance Liquid Chromatography (HPLC) to measure the concentration of released DEX, confirming a release duration of at least 9 weeks [38].
Protein Nanofilm-Based Drug Delivery System
This protocol describes a versatile method for coating implants with a drug-loaded protein nanofilm, which is also applicable to neural interfaces [39].
Key Reagents:
- Bovine Serum Albumin (BSA)
- Tris(2-carboxyethyl)phosphine (TCEP)
- Sodium Alginate (SA)
- Anti-fibrotic drug (e.g., Rapamycin)
Methodology:
- Solution Preparation: Prepare a phase transition solution by premixing BSA and SA in an aqueous solution.
- Reduction and Aggregation: Add TCEP (pH 4.5) to the BSA/SA mixture. TCEP reduces the intramolecular disulfide bonds in BSA, triggering its unfolding and aggregation into β-sheet-stacking nanoparticles.
- Coating Formation: Immerse the implant (e.g., a catheter or electrode shank) in the phase transition solution. The protein nanoparticles self-assemble at the solid-liquid interface, forming a nanofilm on the implant surface.
- Drug Loading: The anti-fibrotic drug can be incorporated into the nanofilm during the assembly process. The intrinsic nanochannels (approximately 2.16 nm) within the film provide a pathway for controlled drug diffusion [39].
- Film Characterization: Control the nanofilm thickness (10–200 nm) by adjusting BSA concentration, SA ratio, and incubation time. Confirm the structural change of BSA from α-helix to β-sheet using Circular Dichroism (CD) and FTIR.
In Vivo Evaluation of Coating Efficacy
A standardized protocol for assessing the performance of coated neural implants in animal models is critical.
Animal Model: Rats or rabbits are commonly used. For peripheral nerve implants, the sciatic nerve is a frequent target [38].
Surgical Implantation:
- Anesthetize the animal and perform an aseptic surgical procedure to expose the target nerve or brain region.
- Implant the coated device alongside appropriate controls (e.g., uncoated device, polymer-only coated device).
- Suture the wound and provide post-operative care according to approved animal welfare protocols.
Endpoint Analysis (after 4-12 weeks):
- Histological Analysis: Explant the tissue surrounding the implant. Process, section, and stain the tissue with markers for:
- Quantitative Morphometry: Measure the thickness of the fibrotic capsule and calculate the ratio of M2/M1 macrophages around the implant to quantify the immunomodulatory effect [40] [38].
- Functional Assessment: For neural electrodes, simultaneously monitor the electrical impedance and the quality of recorded neural signals over time to correlate the reduction in FBR with improved functional stability [4].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Developing Drug-Eluting Neural Implant Coatings
| Reagent/Material | Function & Rationale | Example Use Case |
|---|---|---|
| Polyimide (BPDA-PDA) | Electrically inert, flexible substrate for neural implants; provides a surface for chemical functionalization [38]. | Covalent binding of dexamethasone for sustained anti-inflammatory release [38]. |
| Dexamethasone (DEX) | Potent anti-inflammatory glucocorticoid; suppresses pro-inflammatory cytokine production and macrophage activation [38]. | Coating on polyimide to mitigate FBR, with release over 9 weeks shown to reduce fibrotic capsule thickness [38]. |
| Rapamycin | Immunosuppressant and anti-proliferative drug; inhibits mTOR pathway, reducing fibroblast proliferation and neointimal hyperplasia [39]. | Loaded into protein nanofilm coatings on catheters to prevent stricture by regulating ECM homeostasis [39]. |
| Bovine Serum Albumin (BSA) | Nature-derived protein used to form biocompatible, self-assembling nanofilms for controlled drug delivery [39]. | Base material for creating a hybrid PTB@SA nanofilm coating on various implant substrates [39]. |
| Hyaluronic Acid (HA) | Natural polysaccharide with excellent biocompatibility; mimics glycosaminoglycans in the ECM, reducing immune activation [31] [40]. | Used as a bridging polymer to create a living red blood cell (RBC) coating on PDMS, promoting M2 macrophage polarization [40]. |
| Red Blood Cells (RBCs) | Source of "self" markers (CD47, CD59); provides immune-evasive antigens that signal "don't eat me" to macrophages [40]. | Decorated onto HA-coated PDMS to create a living cell coating that actively modulates macrophage phenotype to M2, minimizing fibrosis [40]. |
Troubleshooting Guide & FAQs
Q1: My drug-eluting coating releases its payload too quickly in vitro, leading to a high initial burst release. How can I achieve a more sustained release profile?
- Problem: The drug is physically adsorbed or the coating matrix is too porous.
- Solution: Shift from physical adsorption to covalent binding of the drug to the polymer backbone, as demonstrated with dexamethasone on polyimide [38]. Alternatively, use a reservoir-type system or a denser matrix (e.g., a protein nanofilm with controlled porosity) to better control diffusion [39].
- Prevention: During development, thoroughly characterize the in vitro release kinetics in infinite-sink conditions with frequent early time-point sampling to identify burst release issues early [41].
Q2: Histological analysis shows a thick fibrotic capsule despite my anti-inflammatory drug coating. What could be wrong?
- Problem: The chosen drug or its release kinetics may not adequately target the key drivers of fibrosis.
- Solution: Re-evaluate the cellular mechanism. The FBR involves multiple cell types. Consider:
- Combination Therapy: Use a drug that targets macrophages (e.g., DEX) in combination with one that directly inhibits fibroblast proliferation (e.g., Rapamycin) [37] [39].
- Macrophage Polarization: Aim to shift macrophages from a pro-fibrotic (M1) to an anti-fibrotic, healing (M2) phenotype. Coatings incorporating "self" markers (e.g., CD47 from RBCs) have shown success in promoting M2 polarization [40].
- Investigation: Use immunohistochemistry to analyze macrophage polarization (M1 vs. M2 markers) in the tissue to diagnose if the immune response is being appropriately modulated [40].
Q3: The coating delaminates or loses mechanical integrity after implantation. How can I improve adhesion and stability?
- Problem: Poor adhesion between the coating and the implant substrate in the hydrated, dynamic physiological environment.
- Solution:
- Surface Activation: Implement robust surface activation steps (e.g., plasma treatment, chemical etching) prior to coating to create strong covalent bonds [38].
- Use of Adhesive Interlayers: Employ materials with strong interfacial adhesion properties. For example, protein nanofilms can adhere to various substrates via ligand bonding, electrostatic, and hydrophobic interactions [39].
- Mechanical Testing: Perform rigorous in vitro mechanical testing, including sonication and simulated implantation, to screen coatings for stability before moving to in vivo studies.
Q4: How do I determine the appropriate dosage of the drug for my coating?
- Problem: The local effective dose is unknown, and systemic toxicity is a concern.
- Solution: Conduct systematic dose-ranging studies in preclinical models. Implant devices with varying drug loadings and establish a dose-response relationship for both efficacy (reduction in capsule thickness) and safety (local tissue toxicity, systemic exposure) [41].
- Analysis: Measure drug concentrations in the local tissue, blood, and downstream organs (e.g., liver, kidney) at necropsy to understand the pharmacokinetic profile and safety margin [41].
The following diagram outlines a logical workflow for developing and troubleshooting a drug-eluting coating, from concept to validation.
Surface Functionalization and Biomimetic Coatings to Modulate the Immune Response
Troubleshooting Common Experimental Challenges
FAQ: Why is my surface modification failing to reduce fibrotic encapsulation in vivo?
- Potential Cause 1: Mechanical Mismatch. The underlying implant may be too stiff, causing chronic micromotion that sustains inflammation and undermines the bioactive coating.
- Potential Cause 2: Incomplete Surface Coverage. Inconsistent coating application can leave exposed areas that trigger protein adsorption and the foreign body reaction (FBR) cascade.
- Solution: Employ surface characterization techniques like X-ray Photoelectron Spectroscopy (XPS) and Atomic Force Microscopy (AFM) to verify coating uniformity. Use reliable coating methods such as chemical vapor deposition (CVD) copolymerization to create robust, continuous layers [42].
- Potential Cause 3: Coating Delamination. The coating may lack sufficient adhesive strength to the substrate, leading to peeling or degradation under physiological conditions.
- Solution: Implement surface activation pre-treatments, such as oxygen plasma treatment, to improve adhesion. Use interpenetrating polymer networks or polydopamine-based priming layers for enhanced bonding strength [42].
FAQ: My anti-inflammatory drug release system is too rapid. How can I achieve a sustained, long-term release?
- Potential Cause: The drug carrier matrix (e.g., a hydrogel) may have a low cross-linking density or be incompatible with the therapeutic molecule.
- Solution: Explore different material systems for controlled release. For instance, a polydopamine-doxorubicin-hydrophilic MPC coating has demonstrated long-term sustained drug release characteristics [42]. Alternatively, tune the degradation rate of a biodegradable polymer like Poly(L-lactic acid) (PLLA) to synchronize drug release with the timeline of the FBR [17].
FAQ: How can I accurately model and test the FBR in vitro before moving to in vivo models?
- Challenge: Traditional 2D cell cultures do not recapitulate the complex 3D cellular interactions of the FBR.
- Solution: Utilize advanced 3D in vitro models. A standardized 3D collagen hydrogel-based co-culture system with human fibroblasts and macrophages can simulate key aspects of the immune response to implant materials. This model allows for the measurement of cytokine expression and ECM remodelling over time [43].
FAQ: Why is the electrical impedance of my neural electrode increasing over time despite a conductive coating?
- Potential Cause: The formation of an insulating glial scar and fibrotic capsule around the implant, which increases the distance between the electrode and neural cells [44] [4].
- Solution: Combine conductive coatings with anti-fouling strategies. Use conductive polymers like PEDOT:PSS, which can reduce electrode impedance. Further functionalize these coatings with biomimetic motifs (e.g., CD47 peptide) or anti-inflammatory molecules to actively suppress the FBR and prevent scar tissue formation [44] [17].
Essential Experimental Protocols
Protocol 1: Creating a Biomimetic Anti-Fouling Coating via Covalent Grafting
This protocol details the creation of a stable, hydrophilic coating to resist non-specific protein adsorption.
- Substrate Preparation and Activation:
- Clean the neural electrode substrate (e.g., platinum, gold, or polyimide) thoroughly with solvents and oxygen plasma treatment. Plasma treatment cleans the surface and generates reactive oxygen-containing groups [42].
- Covalent Grafting:
- Immerse the activated substrate in a solution containing the desired hydrophilic polymer (e.g., poly(2-methacryloyloxyethyl phosphorylcholine) (MPC) or poly(ethylene glycol) (PEG) derivatives) along with appropriate coupling agents.
- Incubate for a specified duration (e.g., 4-24 hours) to allow covalent bonds to form between the surface and the polymer chains [42].
- Washing and Characterization:
- Rinse the modified substrate extensively with deionized water to remove any physisorbed molecules.
- Validate the coating using Water Contact Angle (WCA) measurement (expect a significant decrease, indicating increased hydrophilicity) and XPS to confirm surface chemistry [42].
Protocol 2: Immobilizing a Bioactive Peptide on a Neural Interface
This protocol describes how to functionalize a surface with a specific peptide to promote desired cellular responses.
- Surface Priming with a Universal Adhesive:
- Apply a thin layer of polydopamine (PDA) to the electrode surface by immersing it in a weak alkaline solution (e.g., Tris-HCl, pH 8.5) of dopamine. PDA forms a robust, versatile coating that facilitates secondary conjugation [42].
- Peptide Conjugation:
- Incubate the PDA-coated substrate in a phosphate-buffered saline (PBS) solution containing the bioactive peptide (e.g., a neurite-out promoting peptide like IKVAV or an immune-modulating peptide like CD47). The reactive quinone groups in PDA will covalently bind to amine or thiol groups on the peptide [45].
- Validation:
- Use fluorescence microscopy (if a fluorescently-tagged peptide is used) or Time-of-Flight Secondary Ion Mass Spectrometry (ToF-SIMS) to confirm peptide immobilization.
- Conduct in vitro cell culture with macrophages (e.g., RAW 264.7 cell line) to assess changes in inflammatory cytokine secretion (e.g., TNF-α, IL-6) compared to a control surface [44] [43].
Protocol 3: Establishing a 3D In Vitro Foreign Body Response Model
This protocol outlines the creation of a cost-effective 3D co-culture system to screen material biocompatibility [43].
- Hydrogel Matrix Preparation:
- Prepare a collagen type I hydrogel mixture from rat tail collagen on ice, following the manufacturer's instructions, to a final concentration of 2-4 mg/mL.
- Seed human fibroblasts (e.g., HFF-1 cells) directly into the collagen solution before gelation to achieve a final concentration of 1-2 x 10^6 cells/mL.
- Model Assembly:
- Pipette the cell-collagen mixture into transwell inserts and allow it to polymerize at 37°C for 30-60 minutes.
- In the lower chamber, seed human macrophages (e.g., THP-1-derived macrophages) at a similar density. The semi-permeable membrane allows for cytokine crosstalk while keeping the cell types spatially separated [43].
- Introduction of Test Material and Analysis:
- Add microparticles (e.g., titanium, ceramic) of the test biomaterial to the upper chamber containing the fibroblasts in the 3D matrix.
- Culture for up to 14 days, collecting media supernatants periodically for cytokine analysis (e.g., ELISA for TGF-β1, IL-6, IL-4). At endpoint, fix the hydrogel and perform immunohistochemistry for collagen deposition and cellular markers [43].
The Scientist's Toolkit: Key Research Reagents and Materials
The table below lists essential materials used in the development of immune-modulating coatings for neural interfaces.
| Research Reagent / Material | Function / Rationale in Research |
|---|---|
| Poly(3,4-ethylenedioxythiophene):Poly(styrene sulfonate) (PEDOT:PSS) | A conductive polymer used to coat electrodes; significantly reduces impedance and improves charge transfer efficiency, while its soft nature is more tissue-compliant [17]. |
| Polydopamine (PDA) | A versatile bio-adhesive primer; forms a thin, surface-independent coating that enables subsequent immobilization of peptides, polymers, or drugs via its reactive quinone groups [42]. |
| Poly(ethylene glycol) (PEG) & Zwitterionic Polymers (e.g., MPC) | Hydrophilic polymers used to create anti-fouling surfaces; resist non-specific protein adsorption, which is the critical first step in the Foreign Body Reaction [42]. |
| Self-assembled Monolayers (SAMs) | Well-ordered molecular assemblies (e.g., of alkanethiols on gold) used as model surfaces to precisely study the effect of surface chemistry (e.g., terminal functional groups) on protein and cell behavior [42]. |
| Cell Membrane-derived Vesicles | Nanoplatforms coated with native cell membranes (e.g., from red blood cells or leukocytes); confer unique biological properties, including immune evasion and enhanced targeting, to synthetic implants [46]. |
| Titanium & Ceramic Microparticles | Used in 3D in vitro FBR models to simulate the abrasive wear debris from implants and study the material-specific activation of immune cells [43]. |
| Transforming Growth Factor-beta (TGF-β1) Antibody | A key cytokine to monitor; its elevated levels are a primary driver of fibroblast activation and collagen deposition, making it a central biomarker for fibrotic response [44] [43]. |
| CD47 Peptide Mimetics | A "Self" peptide; when immobilized on a surface, it signals "don't eat me" to macrophages via the SIRPα receptor, actively suppressing phagocytosis and the FBR [44]. |
Visualizing Key Concepts
Foreign Body Reaction Cascade
This diagram outlines the sequential cellular events of the Foreign Body Reaction (FBR) to an implanted neural electrode [44].
Surface Modification Experimental Workflow
This flowchart illustrates a generalized experimental workflow for developing and testing a biomimetic surface coating [45] [42].
Material-Specific Fibrotic Response
Data from a 3D in vitro FBR model showing the fibrotic potential of different implant materials, as indicated by TGF-β1 and collagen levels [43].
| Material Type | Relative TGF-β1 Secretion | Relative Collagen Deposition | Key Cytokine Trends |
|---|---|---|---|
| Titanium (TIT) | High | High | Strong increase in TGF-β1 and IL-6, indicating high fibrotic and inflammatory potential. |
| Ceramic (CT800) | Low to Moderate | Low to Moderate | Lower levels of pro-fibrotic cytokines, suggesting higher biocompatibility. |
| Steel (STE) | Moderate | Moderate | Intermediate response between Titanium and Ceramic. |
| Control (No Particles) | Baseline | Baseline | Baseline levels of cytokines and ECM components. |
Optimizing Electrode Design and Implantation for Chronic Stability
FAQs: Core Concepts and Strategic Planning
Q1: Why is reducing the cross-sectional area of a neural electrode critical for minimizing fibrosis? A reduced cross-sectional area directly decreases the physical disruption caused during implantation and lessens the chronic foreign body response. The primary drivers of fibrosis—the body's immune response to a foreign object and the mechanical mismatch between the stiff implant and soft neural tissue—are both mitigated with a smaller, more compliant footprint. This leads to reduced activation of immune cells like microglia, decreased proliferation of astrocytes, and ultimately, less formation of an encapsulating glial scar that degrades signal quality over time [20] [33].
Q2: How does geometric design influence the long-term stability of recording signals? Geometric design is a fundamental determinant of long-term signal stability. A large, rigid implant induces significant micromotion-related damage and chronic inflammation, leading to increased local impedance and electrical isolation of the electrode from nearby neurons. Conversely, a smaller, softer footprint minimizes mechanical strain on the surrounding tissue, promoting stable integration and reducing the signal-degrading fibrotic capsule. This ensures higher quality electrophysiological recordings over extended periods [20] [47] [33].
Q3: What are the key trade-offs when minimizing an implant's footprint? Minimizing the footprint involves several key engineering trade-offs:
- Mechanical Strength vs. Flexibility: Ultra-thin, flexible designs are more biocompatible but may lack the rigidity required for self-supported insertion into neural tissue without buckling [48] [47].
- Electrical Performance: Reducing electrode site size can increase electrochemical impedance, which may degrade the signal-to-noise ratio unless conductive coatings are applied [47] [33].
- Structural Complexity: Introducing sophisticated 3D designs or high-density arrays can enhance functionality but complicates the fabrication and reliability of the device [48] [47].
Q4: Which material properties are most important for a small-footprint, fibrosis-resistant implant? The ideal material combination exhibits:
- Low Young's Modulus: To match the softness of neural tissue (~1-10 kPa) and reduce mechanical mismatch [20] [47].
- Excellent Biocompatibility: To minimize the foreign body reaction and chronic inflammatory response [20] [33].
- High Electrical Conductivity: For efficient signal transduction, often achieved using flexible conductive polymers or thin metal layers [20] [47].
Troubleshooting Guide: Common Experimental Challenges
| Problem | Potential Cause | Solution |
|---|---|---|
| Increased Electrode Impedance Post-Implantation | Formation of an insulating glial scar and protein fouling on the electrode surface [20] [33]. | Apply low-impedance conductive coatings (e.g., PEDOT:PSS, Iridium Oxide) to the electrode sites. Optimize geometry to reduce mechanical strain [48] [33]. |
| Electrode Buckling During Insertion | Insufficient stiffness of a small-footprint, flexible electrode [47]. | Use a biodegradable polymer or shuttle needle as a temporary stiffener for implantation. Alternatively, design 3D protruding structures that offer better mechanical stability [48]. |
| Unstable or Drifting Neural Recordings | Macroscopic or microscopic movement (micromotion) of the implant relative to the tissue [33]. | Implement 3D elastic designs (e.g., soft microbumps) that buffer against brain micromotion. Ensure the implant is securely anchored at the cranium, not the cortical surface [48]. |
| Chronic Inflammatory Response Despite Small Size | Surface roughness or poor biocompatibility of the material itself [20]. | Utilize ultra-smooth, bio-inert polymer substrates (e.g., specific polyimides) and consider anti-inflammatory drug-eluting coatings [20] [33]. |
Summarized Quantitative Data
Table 1: Mechanical Properties of Neural Tissues and Interface Materials
| Material / Tissue | Young's Modulus | Key Characteristics for Fibrosis |
|---|---|---|
| Brain Tissue | 1 - 10 kPa [20] | Soft, compliant reference point; significant mechanical mismatch with rigid materials causes inflammation [20]. |
| PDMS (Silicone) | ~ 750 kPa [48] | Flexible and widely used; modulus is closer to tissue than rigid materials but still significantly higher [48]. |
| Polyimide (PI) | ~ 2.5 GPa [48] | A flexible polymer substrate, but must be thinned to a few microns to achieve effective mechanical compliance [48]. |
| Platinum (Pt) | ~ 168 GPa [20] | Conventional electrode metal; extreme stiffness necessitates very small feature sizes or use as thin films on soft substrates [20] [47]. |
| Silicon | ~ 170 GPa [20] | Traditional probe material; high stiffness causes significant mechanical mismatch and chronic inflammation [20]. |
Table 2: Performance Comparison of Electrode Geometries
| Electrode Geometry | Key Feature Size | Impact on Fibrosis & Performance |
|---|---|---|
| 2D Planar Film | Thickness: a few μm [48] | Conforms better than rigid shanks, but recessed site can trap bubbles/proteins. Vulnerable to pressure from rigid cranial covers [48]. |
| 3D Soft Microbump (SMBE) | Height: ~327 μm [48] | Protruding structure improves contact, reduces impedance. Silicone base provides elastic buffering against micromotion, reducing inflammatory strain [48]. |
| Michigan-style Silicon Shank | Thickness: ~15-50 μm [47] | Rigid shank causes chronic FBR. High stiffness enables deep implantation but at the cost of long-term signal stability [20] [47]. |
| Nanoneedle / Microhole Array | Diameter: ~2 μm, Pitch: ~20 μm [47] | Ultra-small footprint minimizes disruption. Microhole structure enhances cell-electrode seal, enabling intracellular recording with minimal invasiveness [47]. |
Experimental Protocols
Protocol 1: Fabrication and Testing of a 3D Soft Microbump Electrode (SMBE)
This protocol details the creation of an elastic neural interface designed to buffer against micromotion [48].
I. Materials and Equipment
- Substrate: Polyimide precursor (e.g., PI-2611).
- Metal Layer: Cr/Au (20/200 nm) for traces and electrode sites.
- 3D Mold: Silicon wafer or glass die with laser-micromachined pits.
- Silicone: Ecoflex 0033 AF (antibacterial) and Ecoflex 0010.
- Equipment: Spin coater, photolithography setup, sputtering system, picosecond laser, oven, anisotropic conductive film (ACF) hot-press.
II. Methodology
- 2D Electrode Patterning: Use standard MEMS processes on a silicon carrier wafer. Spin-coat and cure the bottom polyimide layer. Sputter and pattern the Cr/Au metal layer to form interconnects and electrode sites. Spin-coat and cure the top polyimide insulation layer. Use photolithography and reactive ion etching (RIE) to open vias to the electrode sites and define the overall device outline, including grasping strips and slits [48].
- Mold Fabrication: Machine a glass die with pits using a picosecond laser to achieve the desired inverse shape of the microbumps. Cast PDMS into these pits to create a flexible, reusable mold [48].
- 3D Assembly (Stress-Free Preforming):
- Release the 2D electrode array from the carrier wafer.
- Align and press the electrode sites into the glass die pits using the PDMS mold.
- Thermally anneal the assembly (e.g., 180°C for 24 hours) to permanently reshape the polyimide into the 3D configuration.
- Remove the PDMS mold, leaving the preformed 3D electrode in the glass die.
- Fill the pits with a mixed silicone formulation (Ecoflex 0033 AF:0010 = 2:1 by mass), level it, and cure to form the soft, bump-supporting base [48].
- Mechanical and Electrical Validation:
- Cyclic Compression Test: Subject the SMBE to repeated compression (e.g., up to 100% strain) to validate its mechanical resilience and elastic recovery.
- Electrochemical Impedance Spectroscopy (EIS): Measure the impedance of the electrode sites before and after compression to ensure electrical stability.
- In Vivo Validation: Implant the SMBE in an animal model (e.g., rat) and perform electrophysiological recordings during sensory stimulation (e.g., whisker deflection) and application of external pressure to confirm signal stability [48].
Protocol 2: Assessing the Foreign Body Response to Implants
I. Materials and Equipment
- Animal Model: Rats or mice.
- Implants: Test devices (varying in geometry and material) and controls.
- Reagents: Paraformaldehyde (PFA), cryoprotectant (sucrose), OCT compound, primary antibodies (e.g., Iba1 for microglia, GFAP for astrocytes), fluorescent secondary antibodies, DAPI.
- Equipment: Cryostat, fluorescence microscope, vibratome.
II. Methodology
- Implantation: Stereotactically implant the neural electrodes into the target brain region according to approved animal protocols.
- Perfusion and Tissue Harvest: At predetermined time points (e.g., 1, 4, and 12 weeks post-implantation), deeply anesthetize the animal and transcardially perfuse with saline followed by 4% PFA. Extract the brain and post-fix in PFA [20] [33].
- Sectioning: For cryosectioning, cryoprotect the brain in 30% sucrose, embed in OCT, and section coronally (20-40 μm thickness) through the implant site using a cryostat. Alternatively, for free-floating immunohistochemistry, section the brain using a vibratome [49].
- Immunofluorescence Staining:
- Permeabilize and block the tissue sections.
- Incubate with primary antibodies (e.g., anti-Iba1, anti-GFAP) overnight at 4°C.
- Incubate with appropriate fluorescently-labeled secondary antibodies.
- Counterstain nuclei with DAPI and mount the sections [49].
- Imaging and Analysis: Image the tissue surrounding the implant tract using fluorescence microscopy. Quantify the foreign body response by measuring:
Visualized Workflows and Signaling
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Fabricating and Testing Low-Fibrosis Interfaces
| Category | Item | Function / Rationale |
|---|---|---|
| Substrate Materials | Polyimide (PI) | A flexible, biocompatible polymer that serves as an insulation substrate for thin-film microelectrodes [48]. |
| Polydimethylsiloxane (PDMS) | An elastic silicone used for creating soft substrates and 3D bump structures due to its low modulus and biocompatibility [48]. | |
| Conductive Materials | Gold (Au) / Chromium (Cr) | Cr/Au bilayers are standard for creating metallic traces and electrode sites on flexible polymers via thin-film deposition [48]. |
| PEDOT:PSS | A conductive polymer coating that significantly reduces electrode impedance and increases charge injection capacity, improving signal quality [48]. | |
| Iridium Oxide (IrOx) | A high-capacitance coating for electrodes that lowers impedance and allows for safe charge injection during stimulation [33]. | |
| Fabrication Aids | Biodegradable Stiffeners (e.g., Polylactic-co-glycolic acid - PLGA) | Temporarily provide rigidity for implantation of flexible probes, then dissolve, leaving a soft, compliant device behind [47]. |
| Analysis Reagents | Anti-Iba1 Antibody | Labels microglia and macrophages for immunohistochemical quantification of the innate immune response around implants [20] [33]. |
| Anti-GFAP Antibody | Labels astrocytes for immunohistochemical assessment of glial scar formation and thickness [20] [33]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary causes of fibrosis following neural electrode implantation, and how do implantation techniques influence this process? The primary cause of fibrosis is the body's foreign body response, triggered by both the initial injury during implantation and the ongoing mechanical mismatch between the implanted device and the soft neural tissue. [4] This response involves acute inflammation followed by chronic inflammation, leading to the activation of microglia and astrocytes, which ultimately form a dense glial scar and fibrotic tissue around the electrode. [4] [33] This scar tissue acts as an insulating layer, increasing the distance between neurons and electrode sites, causing signal attenuation and a sharp rise in impedance. [4]
The implantation technique directly influences the extent of this response. Acute injury is governed by the geometric and mechanical mismatch during implantation, where larger, stiffer devices cause more tissue tearing, displacement, and vascular damage. [4] Chronic inflammation is driven by persistent mechanical mismatch, where macroscopic and microscopic movements (micromotions) of the electrode cause ongoing friction and tissue damage. [4] Therefore, techniques that minimize the implantation cross-section and reduce mechanical mismatch are crucial for mitigating fibrosis.
Q2: A unified implantation of a multi-shank flexible array has failed. Post-explanation histology shows significant glial scarring at the insertion point. What are the potential causes and solutions? Potential Causes:
- Excessive Implantation Cross-Section: The unified implantation of a multi-shank array likely resulted in a large initial injury, triggering a severe acute inflammatory response. [4] The folded or bundled shanks create a thicker implant profile than a single shank.
- Ongoing Mechanical Mismatch: Despite using flexible materials, the unified structure may still be too rigid compared to brain tissue, leading to chronic micromotions that perpetuate the inflammatory cycle and glial scar formation. [4]
Recommended Solutions:
- Transition to Distributed Implantation: Consider using a system that implants electrode filaments individually. [4] This strategy minimizes the cross-sectional area of a single implantation to a subcellular level, promoting faster wound healing with minimal scarring. [4]
- Optimize Shuttle Design: Ensure the rigid shuttle used for guidance has the smallest possible diameter. For deep brain applications, a unified implantation might be necessary, but the shuttle and electrode geometry should be co-optimized to reduce the bending stiffness (EI), as defined by the material's Young's modulus (E) and the cross-sectional moment of inertia (I). [4]
Q3: During a minimally invasive implantation of a high-density cortical array using a cranial micro-slit, we observe higher-than-expected initial impedance across several channels. What steps should we take? Troubleshooting Steps:
- Verify Electrolyte Environment: A high ground path impedance can indicate a lack of conductive fluid at the electrode-tissue interface. [50] Check that the target site is sufficiently irrigated with saline or cerebrospinal fluid to complete the electrical circuit.
- Inspect for Mechanical Compression: Examine if the device is being mechanically compressed or if sutures are overly tight around any part of the implant, particularly near ground or reference electrodes, as this can disrupt electrical contact. [50]
- Check Electrode Integrity: Use intraoperative impedance testing and neural response telemetry (NRT) to check for short-circuits or open circuits in specific channels. [50] This can help determine if the issue is with the biological environment or a hardware fault.
- Confirm Array Positioning: Utilize intraoperative imaging (e.g., fluoroscopy) or endoscopy to verify the array is correctly positioned on the cortical surface and has not folded back on itself or failed to fully deploy. [51]
Q4: How can we quantitatively compare the invasiveness of different rigid shuttle systems for guiding flexible electrodes? The invasiveness of a shuttle system is largely determined by its bending stiffness, which quantifies its resistance to deformation. A lower bending stiffness generally correlates with reduced tissue damage. Bending stiffness is calculated as the product of the material's Young's Modulus (E) and the cross-sectional moment of inertia (I). [4]
Table: Bending Stiffness Formulas for Common Shuttle Cross-Sections
| Cross-Sectional Shape | Formula for Bending Stiffness (EI) | Key Variables |
|---|---|---|
| Circular (e.g., Tungsten wire) | EI = E * (π * r⁴)/4 [4] |
E: Young's Modulus, r: cross-sectional radius |
| Rectangular (e.g., SU-8 shuttle) | EI = E * (b * h³)/12 [4] |
E: Young's Modulus, b: width, h: height |
To compare systems, calculate the EI for each shuttle. The moment of inertia (I) is highly dependent on the smallest dimension (radius or height), which is why reducing the shuttle diameter from, for example, 35 µm to 7 µm dramatically reduces acute injury. [4]
Q5: What are the key differences between unified and distributed implantation strategies for flexible electrodes? Table: Comparison of Unified vs. Distributed Implantation Strategies
| Feature | Unified Implantation | Distributed Implantation |
|---|---|---|
| Description | Multiple electrodes deployed simultaneously or in a single step using a single guidance system. [4] | Electrode filaments are deployed sequentially or independently using multiple guidance systems. [4] |
| Best For | High-throughput detection in a single brain area or at different depths along the same path; deep brain detection. [4] | Expanding the detection range across a broader area; minimizing single-point injury. [4] |
| Impact on Fibrosis | Higher risk of acute injury and chronic inflammation due to larger implantation cross-section, but suitable for structures requiring coordinated placement. [4] | Minimizes acute injury per implantation site (subcellular scale), promoting individual wound healing and reducing local scar formation. [4] |
| Examples | Single-shank electrodes with multiple channels, folded multi-shank electrodes. [4] | NeuroRoots filament separation, robotic-assisted implantation of individual microwires. [4] |
Experimental Protocols
Protocol 1: Intraoperative Impedance and Neural Response Telemetry for Device Validation
This protocol is adapted from clinical cochlear implant procedures to verify the functionality of a newly implanted neural interface and diagnose common issues like short circuits or poor electrical contact. [50]
Objective: To confirm successful electrode insertion, check for hardware malfunctions, and ensure a viable electrical interface with the nervous system immediately after implantation.
Materials:
- Implanted electrode array and pulse generator/recording system with telemetry capabilities.
- Programming interface with software for impedance measurement and Neural Response Telemetry (NRT) or Electrically Evoked Compound Action Potential (ECAP) recording.
- Sterile normal saline solution.
Methodology:
- Initial Impedance Check: After device implantation and wound closure, initiate an impedance test through the programming interface. Record the impedance values for each electrode channel and the ground path.
- Interpret Initial Results:
- Expected: Stable, low-to-moderate impedance values across all channels.
- High Ground Path Impedance: This suggests an incomplete circuit, often due to a dry interface over the ground electrode or air trapped under the device. [50]
- Short Circuit on Specific Electrodes: This indicates a hardware fault or that perilymph/conductive fluid has been suctioned from around the electrodes. [50]
- Troubleshooting: If high ground path impedance is detected, inject a few milliliters of sterile normal saline between the periosteal flap and the implant's ground electrode to complete the circuit. Re-check impedance. [50]
- Neural Response Validation: Once impedances are normalized, perform NRT/ECAP. Stimulate specific electrodes and attempt to record a neural response from the auditory or other target nerve. A detectable ECAP signifies that the implant is successfully firing and evoking a neural response. [50]
- Final Validation: A successful outcome is indicated by stable, normal impedances and recordable neural responses on all active electrodes.
Protocol 2: Surgical Implantation of a High-Density Thin-Film Array via Cranial Micro-Slit
This protocol describes a minimally invasive approach for deploying a cortical surface array, avoiding a full craniotomy to reduce tissue damage and inflammation. [51]
Objective: To implant a high-channel-count microelectrode array on the cortical surface through a minimal skull opening.
Materials:
- Thin-film, flexible microelectrode array (e.g., 1024-channel array).
- Precision sagittal saw for creating a 500–900 µm wide cranial micro-slit. [51]
- Fluoroscopic or computed tomographic image guidance system.
- Neuroendoscope for monitoring insertion.
Methodology:
- Trajectory Planning: Using pre-operative MRI/CT, plan the trajectory for the micro-slit. The approach angle should be approximately tangential to the cortical surface to facilitate subdural insertion. [51]
- Micro-Slit Creation: Use the precision sagittal saw to create a narrow incision (500–900 µm) in the skull at the planned location. [51]
- Guided Array Insertion: Under fluoroscopic and endoscopic guidance, advance the flexible electrode array through the micro-slit and into the subdural space. The endoscope allows for direct visualization to ensure the array deploys correctly without damaging the cortical surface. [51]
- Array Placement: Position the array to cover the target functional region of the cortex. The flexibility of the array allows it to conform to the cortical surface.
- Closure and Securing: Secure the array and close the surgical site. The entire procedure, from skin incision to final array placement, can be performed in under 20 minutes, reducing the risk of infection and inflammation. [51]
The Scientist's Toolkit
Table: Key Research Reagent Solutions for Neural Interface Implantation
| Reagent / Material | Function in Experimentation |
|---|---|
| Polyethylene Glycol (PEG) | Used as a temporary, soluble coating to fix a flexible electrode to a rigid tungsten wire shuttle. It melts after implantation, allowing the shuttle to be retracted. [4] |
| Conductive Polymers (e.g., PEDOT:PSS) | Used for electrode surface functionalization to lower impedance and improve charge transfer efficiency, enhancing signal quality and potentially reducing the stimulation charge needed. [52] [17] |
| Sterile Normal Saline | Critical for maintaining a moist, conductive environment at the electrode-tissue interface. Used to troubleshoot high impedance by irrigating the ground electrode site. [50] |
| Flexible Substrate Materials (e.g., Polyimide, Parylene) | Form the structural base of flexible electrodes. Their low Young's modulus (matching brain tissue ~1-10 kPa) reduces chronic inflammatory responses and mechanical mismatch. [4] [52] |
| Biodegradable Polymer Scaffolds (e.g., PLLA-PTMC) | Used to create temporary neural interfaces that provide mechanical support and electrical stimulation during nerve regeneration, then naturally degrade, eliminating the need for a second removal surgery. [17] |
Analytical Workflows and Pathways
The following diagram illustrates the critical decision-making pathway for selecting an implantation strategy, based on device design and research goals, and how that choice influences the foreign body response and long-term recording stability.
Decision Pathway for Implantation Strategy and Impact on Fibrosis
Understanding Micromotion and Its Biological Consequences
What is micromotion and why is it a critical issue in chronic neural implants?
Micromotion refers to the small-scale, repetitive relative movement that occurs between an implanted neural electrode and the surrounding brain tissue [53]. This motion is driven by several physiological processes:
- Natural Body Movements: Breathing and changes in intracranial pressure cause the brain to pulsate, leading to continuous small displacements [48].
- Cardiac Pulse: The rhythmic beating of the heart contributes to cyclic tissue movement [53].
- Tethered Implants: When an electrode is fixed to the skull, any movement between the brain and the skull results in strain at the implant-tissue interface [54].
The primary consequence of this micromotion is a chronic inflammatory foreign body response [4]. The mechanical mismatch between stiff implant materials and soft brain tissue exacerbates this friction-induced stress [55] [54]. This persistent inflammation activates microglia and astrocytes, leading to the formation of a dense glial scar that encapsulates the electrode [56] [54]. This scar tissue acts as an insulating layer, increasing the electrical impedance of the electrode and physically pushing neurons away from the recording or stimulation sites, ultimately leading to a decline in device performance and eventual failure [4] [54].
Material & Design Strategies: A Quantitative Comparison
What are the primary material-based strategies to mitigate micromotion-induced damage?
The core strategy for reducing micromotion damage is to minimize the mechanical mismatch between the implant and the neural tissue. The following table summarizes the key properties and performance of different material classes used in neural interfaces.
Table 1: Comparison of Neural Electrode Materials and Their Interface Properties
| Material Class | Example Materials | Young's Modulus | Tissue Response / Performance Notes |
|---|---|---|---|
| Traditional Rigid Materials | Tungsten, Silicon [55] [56] | ~200 GPa [56] | Significant chronic inflammatory response, glial scar formation, higher cellular distortion [55] |
| Conventional Flexible Polymers | Polyimide, Parylene C [56] | ~2–5 GPa [56] | Reduced inflammatory response compared to rigid materials, but modulus is still orders of magnitude higher than brain tissue [53] |
| Ultrasoft/Elastomeric Materials | PDMS, PEDOT-PEG/PDMS composites [55] | ~360–974 kPa [55] | Significantly reduced inflammatory tissue response at 8 weeks compared to tungsten; minimal cell body distortion [55] |
| Brain Tissue (Reference) | - | ~0.4–15 kPa [56] | Target for mechanical compatibility. |
The data shows a clear progression toward softer materials. One study directly compared ultrasoft polymer microwires (Young's modulus = 974 kPa) to traditional tungsten wires. After 8 weeks of implantation, the soft implants demonstrated a significantly reduced inflammatory tissue response and less distortion of nearby neuronal cell bodies [55]. This supports the hypothesis that minimizing stiffness mismatch mitigates chronic tissue damage.
Experimental Protocols & Methodologies
What is a standard protocol for evaluating the chronic tissue response to a novel neural implant?
To systematically assess the effectiveness of a new electrode design in mitigating micromotion-induced fibrosis, researchers employ a combination of in vivo implantation, histological analysis, and quantitative cell morphology assessment. The workflow for a standard chronic implantation study is outlined below.
Diagram 1: Chronic Implant Evaluation Workflow
Detailed Methodology:
Implant Fabrication and Sterilization:
- Fabricate the test implant (e.g., from an ultrasoft conductive elastomer) and a geometrically similar control implant (e.g., a fluorosilicone-coated tungsten wire) [55].
- Ensure implants are sterilized using an appropriate method (e.g., ethylene oxide gas, cold sterilization) prior to surgery.
Animal Surgery and Implantation:
- Anesthetize the animal (e.g., rat or mouse) and secure it in a stereotaxic frame.
- Perform a craniotomy at the target coordinates.
- For flexible electrodes, use a rigid shuttle system (e.g., a stainless-steel needle) coated with a dissolvable PEG glue to guide the implant to the target brain region [55] [4].
- Retract the shuttle after implantation, leaving the flexible electrode in place.
Chronic Recovery and Perfusion:
- Allow animals to recover for pre-defined time points (e.g., 1 week for acute response and 8 weeks for chronic response) [55].
- At the endpoint, transcardially perfuse the animal with phosphate-buffered saline (PBS) followed by 4% paraformaldehyde (PFA).
- Extract and post-fix the brain for sectioning.
Histological Analysis and Quantification:
- Section the brain tissue containing the implant track using a cryostat or microtome.
- Perform immunofluorescence staining using antibodies against:
- NeuN: To label neuronal cell bodies and quantify neuronal density and distance from the implant track.
- GFAP: To label reactive astrocytes and measure glial scar thickness.
- Iba1: To label activated microglia/macrophages.
- Image the stained sections using confocal or fluorescence microscopy.
- Use image analysis software (e.g., ImageJ, Fiji) to quantify:
- Neuronal density within a fixed radius (e.g., 100 µm) from the implant track.
- The distance from the track to the nearest viable neuron.
- The thickness of the GFAP-positive glial scar.
Automated Cell Shape and Strain Analysis (Advanced):
- Develop or use an automated algorithm to analyze the shape of neuronal cell bodies (NeuN+) near the implant [55].
- Quantify metrics such as circularity or aspect ratio. A higher degree of cell body distortion is typically found next to stiff tungsten implants compared to soft polymer implants, indicating persistent mechanical strain [55].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Investigating the Foreign Body Response
| Reagent / Material | Function / Target | Application in Research |
|---|---|---|
| Anti-Iba1 Antibody | Labels microglia and macrophages | Marker for innate immune response and phagocytic activity at the implant site [54]. |
| Anti-GFAP Antibody | Labels reactive astrocytes | Marker for glial scar formation and astrocytic activation [54]. |
| Anti-NeuN Antibody | Labels neuronal nuclei | Used to quantify neuronal survival, density, and proximity to the implant track [55]. |
| Fluoropolymer-coated Tungsten Wire | Control, stiff implant | Serves as a baseline for comparing the tissue response of novel soft materials against traditional rigid electrodes [55]. |
| PEDOT-PEG/PDMS Composite | Ultrasoft conductive elastomer | Material for fabricating test neural electrodes with a Young's modulus closer to that of brain tissue [55]. |
| Polyethylene Glycol (PEG) | Dissolvable adhesive/bonding agent | Used as a temporary "glue" to secure a flexible electrode to a rigid shuttle for implantation; dissolves upon contact with tissue [55]. |
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Our flexible electrode is too floppy to penetrate the dura mater. How can we resolve this implantation issue?
Answer: This is a common challenge. The standard solution is to use a rigid shuttle system.
- Rigid Shuttle with Sacrificial Coating: Temporarily bond your flexible electrode to a rigid needle (e.g., tungsten or stainless steel) using a biodegradable adhesive like polyethylene glycol (PEG) [55] [4]. The PEG dissolves after implantation, allowing the shuttle to be retracted, leaving the flexible electrode in place.
- Stiffening Structures: Integrate a biodegradable stiffener, such as silk or sugar, directly onto the electrode shank. This provides temporary rigidity for implantation, which is lost as the material resorbs in the physiological environment.
- Micro-molded PEG Guidance: For particularly delicate mesh or filament electrodes, use a micro-molded PEG structure to unify and stiffen the array during implantation [4].
FAQ 2: Our impedance measurements are steadily increasing over several weeks post-implantation. Is this a sign of failure related to micromotion?
Answer: A steady rise in impedance is a classic symptom of the foreign body response and is often linked to chronic micromotion.
- Root Cause: The increasing impedance is likely due to the formation of a dense glial scar and fibrotic tissue around the electrode [54]. This tissue encapsulates the electrode, increasing the distance between the conductive surface and the target neurons and acting as an electrical insulator.
- Troubleshooting Steps:
- Verify Material Softness: Ensure your electrode material has a low Young's modulus (ideally in the MPa or kPa range) to minimize mechanical mismatch [55] [4].
- Check Tethering: A rigid tether between the skull and the electrode can amplify micromotion. Implement a "floating" electrode design or use flexible, low-profile interconnects to decouple the implant from skull movements [54].
- Post-mortem Histology: Correlate the electrical data with histology. Section and stain the brain tissue to confirm the presence and thickness of the GFAP-positive glial scar and measure neuronal distance [55].
FAQ 3: We observe high signal-to-noise ratio initially, but single-unit yield drops after 4-6 weeks. What are the potential causes and solutions?
Answer: This performance degradation is a hallmark of chronic inflammation and encapsulation.
- Potential Causes:
- Glial Encapsulation: The primary cause is the formation of an insulating glial sheath, which increases the distance to viable neurons [54].
- Neuronal Loss: Neurons may die or be displaced due to persistent inflammation and mechanical strain from micromotion [55] [54].
- Material Failure: In some cases, micromotion can lead to material fatigue, causing delamination of insulation or cracking of conductive traces [54].
- Solutions to Investigate:
- Surface Functionalization: Coat your electrodes with bioactive molecules (e.g., laminin, neuronal adhesion molecules) to promote neuronal attachment and survival near the interface [56].
- Anti-inflammatory Drug Delivery: Incorporate a drug-eluting system into your electrode design. A controlled-release coating containing an anti-inflammatory agent (e.g., dexamethasone) can locally suppress the foreign body response [4].
- Reduce Cross-sectional Area: Minimize the electrode's footprint. Distributed, filamentous electrodes with subcellular dimensions (e.g., NeuroRoots, nanowires) cause less acute injury and reduce chronic inflammation [4].
Technical Support Center: Troubleshooting Guides and FAQs
This technical support center addresses common experimental challenges in the development and use of multifunctional neural interfaces, with a specific focus on strategies to reduce fibrosis and improve long-term biocompatibility.
Biological Integration & Fibrosis Troubleshooting
Q1: Our chronic neural recordings show progressive signal degradation over several weeks. What could be causing this, and how can we mitigate it?
Signal attenuation often results from the foreign body response, where activated microglia and astrocytes form an insulating scar around the implant [57] [20]. This fibrotic tissue increases impedance and electrically isolates the electrode.
Diagnostic Steps:
- Measure Electrode Impedance: Track impedance over time; a steady increase suggests encapsulation.
- Histological Analysis: Post-mortem immunohistochemistry for GFAP (astrocytes) and Iba1 (microglia) can quantify glial scarring around the implant tract [20].
- Check Signal Characteristics: Loss of high-frequency neural units and preservation only of lower-frequency local field potentials can indicate encapsulation.
Solutions to Mitigate Fibrosis:
- Mechanical Compliance: Use flexible substrates like SU-8, polyimide, or soft conductive polymers that match the low Young's modulus of neural tissue (1-10 kPa) to reduce micromotion-induced inflammation [57] [17] [20].
- Anti-fouling Coatings: Coat probes with anti-inflammatory nanogels or hydrogels. One study showed a nanogel-coated neural probe allowed stable recording in rat thalamic nuclei for over 4 weeks [57].
- Local Drug Delivery: Integrate microfluidic channels for the localized release of anti-inflammatory drugs (e.g., dexamethasone) directly to the implantation site to suppress the local immune response [57] [58].
Q2: How can we validate that our interface is successfully reducing fibrosis in vivo?
A multi-modal validation approach is required, combining functional, histological, and molecular techniques.
- Functional Validation: Stable electrophysiological signals (consistent spike amplitude and signal-to-noise ratio) over weeks to months are a primary indicator of reduced fibrosis [57].
- Histological Validation: After a set implantation period, process brain sections to visualize:
- Astrocytes: Stain for Glial Fibrillary Acidic Protein (GFAP).
- Microglia: Stain for Ionized calcium-binding adapter molecule 1 (Iba1).
- Neurons: Stain for Neuronal Nuclei (NeuN) to assess neuronal density near the probe interface [20]. A successful anti-fibrosis strategy will show a thinner glial scar and higher neuronal density near the probe compared to uncoated controls.
- Molecular Validation: Use qPCR on tissue surrounding the implant to quantify expression levels of pro-inflammatory cytokines (e.g., TNF-α, IL-1β) [20].
Technical & Functional Failures
Q3: The microfluidic channels in our probe are clogged, preventing drug delivery. What are the causes and prevention strategies?
Clogging can be caused by particulate matter, drug crystallization, or protein adhesion (biofouling) within the channels [57].
- Prevention and Solutions:
- Filtration: Always filter drugs and solutions (using a 0.2µm filter) before loading into the reservoir or microfluidic system.
- Channel Design: Implement larger channel cross-sections where possible (e.g., 10x10 µm² or larger) to reduce clogging risk [57].
- Surface Passivation: Use surface treatments like PEGylation to reduce protein adhesion.
- In-line Pressure Sensor: Integrate a pressure sensor to monitor pressure drops within the channel, which can provide an early warning of clog formation.
Q4: We are experiencing large electrical artifacts during simultaneous electrical stimulation and recording. How can this be managed?
Stimulation artifacts are a common challenge because the stimulation pulse amplitude is orders of magnitude larger than neural signals [57].
- Solutions:
- Electrode Design: Physically separate recording and stimulating electrodes to reduce crosstalk.
- Reference Electrodes: Use a dedicated, low-impedance reference electrode.
- Hardware Blanking: Utilize recording systems with built-in blanking circuits that disconnect the recording amplifier during the stimulation pulse.
- Post-processing: Implement algorithmic artifact subtraction in software, using template subtraction or adaptive filtering techniques.
Q5: Our implanted device has failed prematurely. How can we systematically determine the cause of failure?
Implanted neural interfaces are complex systems where failure can be technological, mechanical, or biological [33]. Follow a systematic troubleshooting flowchart to diagnose the issue.
Experimental Protocols
Protocol 1: Coating a Neural Probe with an Anti-inflammatory Nanogel for Fibrosis Reduction
This protocol is adapted from methods that have demonstrated stable long-term recording in rodent models [57].
- Objective: To apply a uniform, adherent nanogel coating on a neural probe to improve biocompatibility and reduce the glial scar formation.
- Materials:
- Sterile neural probes
- Anti-inflammatory nanogel solution (e.g., PEG-based hydrogel loaded with dexamethasone)
- Micro-pipette or dip-coating apparatus
- UV cross-linker (if using a photopolymerizable gel)
- Sterile phosphate-buffered saline (PBS)
- Procedure:
- Probe Preparation: Clean and sterilize the neural probe according to standard protocols.
- Coating Application: Using a micro-pipette under a stereomicroscope, dispense a small volume of the nanogel solution to cover the electrode sites and probe shank. Alternatively, use a controlled dip-coating process.
- Curing: If required, expose the coated probe to UV light for a specified duration to cross-link and solidify the gel.
- Rinsing: Gently rinse the probe in sterile PBS to remove any uncured gel and confirm electrode functionality by measuring impedance in saline.
- Implantation: The probe is now ready for stereotaxic implantation.
- Validation: As described in FAQ #2, perform histology after the experiment to quantify glial scarring and neuronal loss around the coated probe versus an uncoated control.
Protocol 2: In Vivo Validation of Integrated Microfluidic Drug Delivery
This protocol ensures the microfluidic system of a multifunctional probe is operational and delivers its payload correctly in a behaving animal [57] [58].
- Objective: To verify the patency and function of microfluidic channels and confirm localized drug delivery in the brain.
- Materials:
- Multifunctional probe with integrated microfluidics
- Syringe pump or wireless pressurized reservoir system
- Drug solution (e.g., a fluorescent dye like Fluorescein for initial validation)
- Micro-volume tubing and connectors
- Fluorescence microscope or tissue spectrometer
- Procedure:
- Pre-implantation Priming: Before surgery, prime the microfluidic channel and outlet by flowing PBS to remove air bubbles. Verify there are no leaks.
- Probe Implantation: Implant the probe into the target brain region using standard stereotaxic surgery.
- Post-surgery Delivery: After recovery, connect the probe to the drug delivery system. For a wireless probe, activate the reservoir remotely [57].
- Dye Infusion: Infuse a small volume (e.g., 50-100 nL) of a fluorescent dye solution at a low flow rate (e.g., 20 nL/min).
- Perfusion and Analysis: After a short period (e.g., 30-60 minutes), perfuse the animal and extract the brain. Section the brain and image the tissue under a fluorescence microscope to confirm the localized spread of the dye from the probe's outlet.
- Troubleshooting: If no dye is observed, check for clogs as per FAQ #3. If the spread is too diffuse, optimize the infusion volume and rate.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Key materials and reagents for developing advanced multifunctional neural interfaces.
| Item | Function / Application | Key Characteristics |
|---|---|---|
| PEDOT:PSS (Poly(3,4-ethylenedioxythiophene):Poly(Styrene Sulfonate)) | Conducting polymer for electrode coating. Improves charge injection capacity for stimulation and reduces recording impedance [57] [17]. | Excellent conductivity, biocompatibility, can be electrodeposited, can be loaded with drugs for controlled release [57]. |
| SU-8 / Polyimide | Flexible polymers used as substrates for soft neural probes [57] [17]. | Photosensitive (SU-8), high insulation, mechanically compliant, reduces mechanical mismatch with tissue. |
| Iridium Oxide (IrOx) | High-performance electrode coating material [57] [33]. | High charge injection capacity, facilitates safe and effective electrical stimulation, can be sputtered or electrodeposited. |
| Silk Fibroin | Biodegradable, biocompatible substrate for transient electronics or nerve conduits [57] [17]. | Programmable deformability, dissolves after use, excellent biocompatibility, can be functionalized. |
| Anti-inflammatory Nanogels (e.g., PEG-based) | Coating for probes to reduce fouling and inflammatory response [57]. | Hydrophilic, reduces protein adsorption, can be loaded with drugs (e.g., dexamethasone) for localized release. |
| Tetro-DOpE Probes | Multifunctional platform integrating recording electrodes, optical waveguides, and microfluidic channels in a single bundle [58]. | Highly customizable, enables simultaneous electrophysiology, optogenetics, and pharmacology in behaving animals. |
Balancing Flexibility for Biocompatibility with Stiffness for Reliable Implantation
Troubleshooting Common Experimental Challenges
Q1: Our flexible electrode arrays consistently buckle during insertion, preventing precise placement in the target neural tissue. What strategies can we employ to overcome this?
A: Buckling occurs when the electrode's bending stiffness is insufficient to overcome the penetration force required for the target tissue. Implement one of these shuttle-based implantation techniques to provide temporary rigidity [4]:
- Rigid Shuttle Guidance: Temporarily attach a rigid guide, such as a tungsten wire or SU-8 polymer shank, to your flexible electrode. The shuttle provides the necessary column strength for penetration and is retracted after implantation [4].
- Bioresorbable Stiffeners: Coat or laminate your flexible electrode with a material like silk or a sugar blend. These stiffeners provide mechanical support during implantation and then dissolve upon contact with physiological fluids, leaving behind the flexible electrode without a permanent foreign body [4].
Q2: After successful implantation, our recording quality degrades over several weeks, accompanied by a rise in impedance. We suspect fibrotic encapsulation. What are the primary factors and how can we mitigate them?
A: Rising impedance and signal degradation are classic signs of the foreign body response (FBR), leading to fibrotic tissue formation. The key factors and mitigation strategies are [20] [33]:
- Mechanical Mismatch: The significant stiffness difference between traditional rigid electrodes (GPa) and soft brain tissue (1–10 kPa) causes chronic micro-motion and inflammation.
- Device Geometry: Larger, sharper implants cause more acute tissue damage during insertion.
- Solution: Minimize the cross-sectional area of electrode shanks. Consider distributed, filament-like electrodes that are subcellular in size (e.g., widths of 7–10 µm) to dramatically reduce acute injury and chronic inflammation [4].
- Biological Response: The immune system recognizes the implant as a foreign body, activating microglia and astrocytes, which eventually form an insulating glial scar.
Q3: Are measurements of electrode impedance a reliable standalone indicator of the degree of fibrosis at the neural interface?
A: No. While a significant increase in impedance often suggests the presence of a fibrotic capsule, research indicates that impedance measurements alone cannot quantify the absolute amount of fibrotic tissue [14]. Studies have shown no significant correlation between impedance values and the measured area of fibrotic tissue in chronic implants. Impedance can be influenced by other factors, including electrode material, surface chemistry, and the local ionic environment. Therefore, impedance should be used as an initial diagnostic tool, but conclusive analysis of fibrosis requires post-mortem histological validation [14].
Experimental Protocols & Methodologies
Protocol 1: Coating Flexible Electrodes with an Anti-inflammatory Drug for Local Release
This protocol details the process of creating a dexamethasone-eluting coating on a flexible neural probe to suppress the local immune response [4].
- Electrode Preparation: Clean flexible polyimide electrode arrays using a standard oxygen plasma treatment to ensure a clean, hydrophilic surface for coating adhesion.
- Coating Formulation: Prepare a solution of a biodegradable polymer, such as Poly(Lactic-co-Glycolic Acid) (PLGA), in an organic solvent (e.g., dimethyl sulfoxide). Dissolve dexamethasone into the PLGA solution at a controlled concentration (e.g., 10% w/w of polymer).
- Coating Application: Using a precise dip-coater or micro-syringe, apply a thin, uniform layer of the PLGA-dexamethasone solution onto the electrode shanks. Ensure the active recording sites are not occluded, potentially using a masking technique.
- Solvent Evaporation: Allow the solvent to evaporate slowly in a controlled vacuum desiccator for 24 hours, forming a solid, drug-embedded polymer matrix around the electrode.
- In Vitro Release Test: Characterize the drug release profile by immersing the coated electrode in phosphate-buffered saline (PBS) at 37°C and measuring dexamethasone concentration in the PBS over time using UV-Vis spectroscopy.
- Sterilization: Sterilize the coated electrodes using low-temperature ethylene oxide gas (EtO) to avoid melting the coating or drug degradation.
Protocol 2: Evaluating the Foreign Body Response to Implants via Histology
This standard methodology is used to qualitatively and quantitatively assess fibrosis and inflammation around an implant weeks to months post-insertion [4] [14].
- Perfusion and Fixation: At the predetermined endpoint, deeply anesthetize the animal and perform transcardial perfusion with saline followed by 4% paraformaldehyde (PFA) to fix the tissues in situ.
- Tissue Extraction and Sectioning: Carefully extract the brain with the implant in place. For delicate flexible electrodes, it may be necessary to perfuse with the implant intact and then carefully remove it before sectioning to avoid damage to the microtome blade. Alternatively, use specialized techniques like serial block-face imaging for in situ analysis [14].
- Staining: Cut coronal sections (e.g., 40 µm thick) containing the implant track and subject them to immunohistochemical staining.
- Astrocytes: Stain with an antibody against Glial Fibrillary Acidic Protein (GFAP).
- Microglia/Macrophages: Stain with an antibody against Ionized Calcium-Binding Adapter Molecule 1 (Iba1).
- Neurons: Stain with an antibody against Neuronal Nuclei (NeuN).
- Collagen/Fibrosis: Use a Masson's Trichrome stain or Picrosirius Red.
- Imaging and Quantification: Image the stained sections using confocal or fluorescence microscopy. Use image analysis software (e.g., ImageJ, Fiji) to quantify the intensity of GFAP and Iba1 staining around the implant site and measure the thickness of the glial scar and the distance from the electrode to the nearest neuron.
Quantitative Data for Material Selection
Table 1: Mechanical and Electrical Properties of Common Neural Electrode Materials
| Material | Young's Modulus | Key Advantages | Key Limitations for Chronic Use |
|---|---|---|---|
| Silicon (Michigan/Utah probes) | ~100 GPa [20] | High spatial resolution, well-established fabrication [47] | Extreme mechanical mismatch, promotes inflammation and scar formation [20] [47] |
| Platinum (Pt) | ~150 GPa [20] | Excellent conductivity, high charge injection capacity [33] | Stiff, prone to corrosion under chronic stimulation [20] |
| Iridium Oxide (IrOx) | N/A (typically used as coating) | Superior charge injection capacity compared to Pt [33] | Mechanical properties depend on substrate; can be fragile |
| Polyimide | 2.5 - 8.5 GPa [4] | Flexible, biocompatible, good insulator for substrates [4] [33] | Higher impedance than metals; used as substrate, not conductor |
| Parylene-C | 2.8 - 4.0 GPa | Conformal coating, biocompatible, moisture barrier [33] | Can delaminate in chronic, moist environments [60] |
| Carbon Fiber | ~200 GPa [20] | Can be fabricated into very small diameters (~7 µm) for minimal cross-section [20] [4] | High resistivity; challenging for high-density interconnect |
Table 2: Performance Comparison of Implantation Support Strategies
| Implantation Strategy | Mechanism | Impact on Acute Damage | Impact on Chronic Inflammation | Key Challenge |
|---|---|---|---|---|
| Tungsten Wire Guidance [4] | Rigid shuttle provides temporary stiffness | Moderate (depends on shuttle size) | Low (shuttle is removed) | Potential for additional tissue displacement during shuttle retraction |
| Bioresorbable Stiffeners [4] | Material dissolves post-implantation | Low to Moderate | Low (no permanent foreign body) | Optimizing dissolution kinetics to match implantation time |
| SU-8 Guidance [4] | Polymer shuttle for complex shapes | Moderate | Low (shuttle is removed) | Suitable for mesh electrodes; requires precise design |
| Unified Implantation [4] | Multiple electrodes implanted as one unit | Higher (larger cross-section) | Moderate (larger footprint) | Maximizing throughput while minimizing initial injury |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Neural Interface Biocompatibility Research
| Reagent / Material | Function in Experimental Context |
|---|---|
| Polyimide [4] [33] | A flexible polymer used as the substrate for fabricating soft microelectrode arrays. Its key function is to reduce the mechanical mismatch with neural tissue. |
| Parylene-C [33] | A polymer used as a conformal, biocompatible insulating coating for electrode traces and shanks. It acts as a moisture barrier to protect underlying electronics. |
| Dexamethasone [4] [59] | A potent anti-inflammatory drug. When incorporated into polymer coatings (e.g., PLGA), it is eluted locally to actively suppress the foreign body response and reduce glial scarring. |
| Brain-Derived Neurotrophic Factor (BDNF) [59] | A neurotrophic factor used in regenerative strategies. Its function is to initiate and promote neurite outgrowth towards the electrode, improving interface proximity and integration. |
| Iridium Oxide (IrOx) [33] | A conductive coating applied to electrode sites. Its primary function is to significantly increase the charge injection capacity of stimulation electrodes, allowing for safer and more effective stimulation. |
| Anti-GFAP Antibody [4] | An immunohistochemical marker for astrocytes. It is used to visualize and quantify astrocytic activation and glial scar formation around the implant site in post-mortem tissue analysis. |
| Anti-Iba1 Antibody [4] | An immunohistochemical marker for microglia and macrophages. It is used to identify and quantify the innate immune response and inflammation surrounding the neural implant. |
Visualizing Strategies and Relationships
Implant Failure Pathways
Biocompatibility Strategy Workflow
Preclinical Models and Comparative Analysis of Anti-Fibrotic Performance
Technical Support Center
Troubleshooting Guides
Guide 1: Cytotoxicity Assay Inconsistencies
Problem: High background noise or inconsistent results in membrane integrity cytotoxicity assays.
Solution:
- Verify Dye Selectivity: Ensure you are using dyes classified as non-permeable to live cells, such as Propidium Iodide or SYTOX Green, and confirm they do not cross intact membranes [61]. Dyes that readily penetrate live cells will produce false positives.
- Check Exposure Time: Long-term exposure (e.g., over 72 hours) of DNA-binding dyes can be cytotoxic to some cell lines, artificially increasing dead cell counts [61] [62]. Perform a dye cytotoxicity test with your specific cell type and use the shortest viable exposure time.
- Control for Fluorescence Interference: If your test compounds are fluorescent, signal interference can occur. Consider switching to a luminescence-based method, such as measuring the release of a natural enzyme like lactate dehydrogenase (LDH) with a luminometric readout, to avoid this issue [62].
Guide 2: Unclear Macrophage Polarization Status
Problem: Difficulty in confirming the M1/M2 polarization state of macrophages before applying a test stimulus.
Solution:
- Implement Multimarker Validation: Do not rely on a single marker. Use a combination of surface markers, gene expression, and cytokine secretion profiles to definitively characterize the polarization state [63] [64].
- Functional Assays: Confirm polarization with functional assays. For example, M1 macrophages should show a pro-inflammatory cytokine profile (e.g., increased IL-6, TNF-α), while M2 macrophages typically exhibit high phagocytic activity and secrete factors like CCL18 and VEGF [63] [64].
Guide 3: Poor Cell Adhesion in Migration/Invasion Assays
Problem: Cells detach during washing steps in transwell or spreading assays.
Solution:
- Validate ECM Coating: Ensure the extracellular matrix (ECM) coating (e.g., Matrigel, fibronectin) is prepared and applied correctly. Allow sufficient time for polymerization and protein adhesion to the membrane or dish [65].
- Optimize Seeding Density: A density that is too low may not provide enough cell-cell contact for stable collective migration, while a density that is too high can lead to overcrowding and detachment. Perform a seeding density optimization experiment [65].
- Confirm Serum Starvation: For chemotaxis assays, ensure the cells are properly serum-starved before the experiment to eliminate random migration driven by serum factors in the culture medium [65].
Frequently Asked Questions (FAQs)
Q1: What is the most sensitive cell viability assay for high-throughput screening? A: The bioluminescent ATP assay is generally considered the most sensitive for high-throughput workflows. ATP is rapidly degraded in dead cells, so its presence is a direct marker of viability. The assay is homogenous, has a broad linear range, and is less prone to artifacts compared to tetrazolium reduction (MTT) assays [62].
Q2: How can I distinguish between true cytotoxicity and cytostasis (growth arrest) in my assay? A: Measuring a single endpoint can confuse these two outcomes. To distinguish them, multiplex your assays. Combine a viability assay (e.g., ATP content) with a cytotoxicity assay (e.g., a membrane integrity dye). A cytostatic effect would show a decrease in the viability signal without a corresponding increase in the cytotoxicity signal, whereas a cytotoxic effect would show a strong increase in the cytotoxicity signal [61].
Q3: My research involves testing materials for neural electrodes. Which macrophage response is most relevant? A: For neural interfaces, the goal is often to minimize the chronic foreign body response, which is driven by pro-fibrotic M2-like macrophages. Your in vitro assays should focus on quantifying markers associated with the pro-inflammatory M1 state (e.g., TNF-α, IL-6, iNOS) and the pro-fibrotic M2 state (e.g., CD206, Arg-1, CCL18) [63] [64]. A desirable material would promote an initial M1 response for microbial defense and then resolve to a balanced state, avoiding a persistent M2 response that leads to fibrotic encapsulation [20] [33].
Q4: Can I perform real-time, kinetic measurements of cell death? A: Yes, using non-permeable DNA-binding dyes. However, it is critical to validate that the dye itself is not cytotoxic to your cells over the extended measurement period [61] [62]. Alternatively, real-time viability assays are available that use a pro-substrate converted to a luciferase substrate only by metabolically active cells, allowing for continuous monitoring of the same well over days [62].
Quantitative Data Tables
Table 1: Comparison of Common Cell Viability Assays
| Assay Type | Mechanism | Readout | Key Advantage | Key Limitation |
|---|---|---|---|---|
| ATP Bioluminescence [62] | Measures cellular ATP via luciferase reaction | Luminescence | High sensitivity, excellent for HTS | Requires cell lysis (endpoint) |
| Tetrazolium Reduction (MTT) [62] | Mitochondrial reductase activity in viable cells converts dye to formazan | Absorbance | Inexpensive, well-established | Long incubation; insoluble product requires solubilization |
| Resazurin Reduction [62] | Metabolic activity in viable cells reduces resazurin to fluorescent resorufin | Fluorescence | More sensitive than MTT, soluble product | Fluorescent compounds can interfere |
| Live-Cell Protease [62] | Measures protease activity unique to viable cells | Fluorescence | Can be multiplexed with other assays | Signal is dependent on protease activity levels |
| Real-Time Kinetic [62] | Viable cells reduce a pro-substrate to a luciferase substrate | Luminescence | Allows continuous monitoring of the same sample | Requires specialized reagent |
Table 2: Key Markers for Macrophage Polarization States
| Polarization State | Surface Markers | Gene/Gene Product Markers | Secreted Factors | Functional Role |
|---|---|---|---|---|
| M1 (Pro-inflammatory) [63] [64] | CD80, CD86, MHC II | iNOS, CCR7 | TNF-α, IL-6, IL-1β, IL-8 [63] | Pathogen clearance, acute inflammation [63] |
| M2 (Pro-repair/Immunoregulatory) [63] [64] | CD200R, CD163, CD206 | Arg-1, CCL18 | IL-10, TGF-β, VEGF, CCL18, CCL22 [63] | Tissue repair, inflammation resolution, fibrosis [63] |
Experimental Protocols
Protocol 1: Measuring Cytotoxicity via Lactate Dehydrogenase (LDH) Release
Principle: This assay measures the activity of LDH, a stable cytoplasmic enzyme released upon cell membrane damage, in the culture supernatant [62].
- Plate cells in a 96-well plate and treat according to your experimental design. Include a background control (culture medium only) and a maximum LDH release control (cells treated with a lysis solution).
- Centrifuge the plate at low speed to pellet cells and debris.
- Transfer a volume of the supernatant from each well to a new clear-bottom 96-well plate.
- Prepare the LDH reaction mix according to the manufacturer's instructions. A typical mixture contains lactate, NAD+, and a tetrazolium salt (like INT) or resazurin.
- Add the reaction mix to each well containing the supernatant.
- Incubate for 30 minutes at room temperature, protected from light.
- Measure absorbance (for formazan products) at ~490nm or fluorescence (for resorufin) with Ex/Em ~560/590nm.
- Calculate cytotoxicity: Cytotoxicity (%) = [(Experimental LDH - Background LDH) / (Maximum LDH - Background LDH)] x 100
Protocol 2: Macrophage Polarization and Phenotypic Assessment
Principle: Human monocytes are differentiated into macrophages (M0) and then polarized toward M1 or M2 states using specific cytokines. Their phenotype is assessed via gene expression and cytokine secretion [63].
- Isolation and Differentiation:
- Isolate human monocytes from PBMCs or use a monocyte cell line.
- Differentiate into naive macrophages (M0) by culturing for 5-7 days with 50 ng/mL Macrophage Colony-Stimulating Factor (M-CSF).
- Polarization:
- M1 Polarization: Stimulate M0 macrophages for 24-48 hours with 100 ng/mL LPS (Lipopolysaccharide) and/or 20 ng/mL IFN-γ.
- M2 Polarization: Stimulate M0 macrophages for 24-48 hours with 20 ng/mL IL-4.
- Application of Test Material: Add your test material (e.g., neural electrode material extract, conditioned medium) to the polarized macrophages for a further 24-48 hours.
- Phenotypic Analysis:
- Gene Expression: Harvest cells for RNA extraction and perform RT-qPCR for M1 (e.g., CD86, CCR7) and M2 (e.g., CD206, Arg-1, CCL18) markers [64].
- Cytokine Secretion: Collect cell culture supernatant and analyze for M1 (TNF-α, IL-6) and M2 (CCL18, VEGF) cytokines via ELISA or multiplex bead array [63].
- Surface Markers: Analyze cells by flow cytometry for M1 (CD80, CD86) and M2 (CD206, CD163) surface receptors [63].
Protocol 3: Cell Spreading and Adhesion Assay
Principle: This assay measures the capacity of cells to adhere to an extracellular matrix (ECM) and spread out, which is a key initial step in migration and integration [65].
- Coat Surfaces:
- Add a solution of ECM protein (e.g., 10 µg/mL fibronectin in PBS) to a 96-well plate or μ-Dish.
- Incubate for at least 1 hour at 37°C or overnight at 4°C.
- Aspirate the coating solution and block non-specific binding sites with 1% BSA in PBS for 30 minutes at 37°C.
- Wash once with PBS before cell seeding.
- Cell Seeding:
- Trypsinize and resuspend cells in serum-free medium.
- Seed cells at a subconfluent density (e.g., 5,000 - 20,000 cells/well in a 96-well plate) onto the coated surface.
- Allow Adhesion and Spreading:
- Incubate the cells at 37°C for a defined period (e.g., 15, 30, 60, 120 minutes).
- Fixation and Staining:
- Gently wash wells with pre-warmed PBS to remove non-adherent cells.
- Fix cells with 4% Paraformaldehyde (PFA) for 15 minutes.
- Permeabilize with 0.1% Triton X-100 (optional) and stain for F-actin with phalloidin (e.g., 1:1000) and for nuclei with HOECHST 33342 (e.g., 1 µg/mL) [65].
- Image Acquisition and Analysis:
- Image using a fluorescence or confocal microscope.
- Use image analysis software (e.g., ImageJ/Fiji) to quantify:
- Number of Adherent Cells: Count nuclei in multiple fields of view.
- Spreading Area: Measure the average cell area based on the F-actin stain.
Signaling Pathways and Workflows
MP to M1/M2 Polarization
Cytotoxicity Assay Workflow
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Featured Experiments
| Reagent / Kit | Function / Application | Example Use Case | Key Considerations |
|---|---|---|---|
| SYTOX Green [61] | High-affinity nucleic acid stain that is impermeable to live cells. | Detecting dead cells in a population via fluorescence microscopy or plate reader. | ~500x fluorescence enhancement upon DNA binding. Check for spectral overlap if multiplexing. |
| CellTiter-Glo Assay [62] | Luminescent assay for quantifying ATP as a marker of viable cells. | Determining cell viability in high-throughput screening formats. | Highly sensitive; linear over a wide cell density range. Requires cell lysis. |
| Propidium Iodide (PI) [61] | Membrane-impermeant DNA intercalating agent and fluorescent dye. | Flow cytometry analysis to distinguish dead (PI-positive) from live cells. | Commonly used; can be excited by 488nm laser. |
| Recombinant Human Cytokines (M-CSF, IL-4, IFN-γ, LPS) [63] | Polarize human monocyte-derived macrophages toward M0, M1, or M2 states. | Creating defined macrophage phenotypes for testing neural biomaterials. | Use high-quality, endotoxin-free cytokines. Optimize concentration and duration for your cell source. |
| Matrigel Basement Membrane Matrix [65] | Complex ECM protein mixture used to coat surfaces for invasion/adhesion assays. | 3D invasion assays (transwell) or to create a biologically relevant substrate for cell spreading. | Keep on ice; polymerization is temperature-dependent. Lot-to-lot variability exists. |
| Fibronectin [65] | ECM glycoprotein that promotes cell adhesion, migration, and growth. | Coating plates for cell spreading assays or to improve cell attachment. | Standardized and defined compared to Matrigel. |
| HOECHST 33342 [65] | Cell-permeable blue-fluorescent DNA stain. | Nuclear counterstain for immunofluorescence and to count total cells in adhesion assays. | Stains all cells (live and dead). Use at low concentrations to minimize cytotoxicity. |
Frequently Asked Questions
What are the key cellular players in the Foreign Body Response (FBR) I should quantify? The primary cells to quantify are fibroblasts (αSMA+), neutrophils (neutrophil elastase+), and macrophages (CD68+ for pan-macrophages; iNOS+ for pro-inflammatory phenotypes; CD206+ for anti-inflammatory phenotypes). A significant reduction in the infiltration of these cells is a key indicator of a successful anti-fibrotic strategy [66].
How does an adhesive implant-tissue interface affect fibrosis? Research demonstrates that an adhesive interface creates conformal integration with the tissue, significantly reducing the infiltration of inflammatory cells compared to non-adhesive interfaces. This reduction leads to decreased collagen deposition and can prevent the formation of an observable fibrous capsule over 12 weeks in vivo [66].
My negative control is still showing some fibrosis. Is this normal? Yes. Even non-adhesive control implants and sham procedures will trigger a foreign body reaction, resulting in a measurable fibrous capsule. The goal of your experimental groups is to show a statistically significant reduction in capsule thickness and cellular infiltration compared to these controls [67] [66].
What is a major pitfall when comparing fibrous capsule thickness between studies? A common pitfall is inconsistent measurement protocols. Thickness can be reported as an average, a maximum, or via collagen area quantification. Always clearly state your measurement method (e.g., "average thickness from 20 random locations per sample") and ensure it is consistent across all experimental groups to allow for valid comparisons [66] [68].
Beyond standard histology, what advanced methods can improve my analysis? Automated computational pathology using machine learning models can segment tissues and quantify features like cell number, tissue area ratios, and border integrity with high precision and reduced scorer variability. This method provides continuous, quantitative data that strongly correlates with traditional semi-quantitative scores [68].
Table 1: Key Metrics from Preclinical FBR Studies
| Metric | Typical Control/Non-Adhesive Implant Findings | Typical Experimental/Adhesive Implant Findings | Measurement Method | Source |
|---|---|---|---|---|
| Fibrous Capsule Thickness | Significant collagen deposition; thickness increases over time (e.g., >50µm). | Collagen layer thickness comparable to native tissue (e.g., mesothelium); often no observable capsule. | Histological section staining (e.g., H&E, Masson's Trichrome); thickness measurement. | [66] |
| Fibroblast Infiltration | High density of αSMA+ fibroblasts at the interface. | Significantly fewer αSMA+ fibroblasts. | Immunofluorescence (αSMA staining); cell counting over a defined interface width. | [66] |
| Innate Immune Cell Infiltration | High numbers of neutrophils (elastase+) and macrophages (CD68+, iNOS+). | Significantly fewer neutrophils and macrophages. | Immunofluorescence; multiplex Luminex assays for cytokines; qPCR of immune genes. | [66] |
| Adaptive Immune Cell Infiltration | Presence of T-cells (CD3+) at the interface. | Significantly fewer T-cells (CD3+). | Immunofluorescence (CD3 staining); cell counting. | [66] |
| NP Cell Number (Disc Degeneration Model) | Significant loss of NP cellularity with injury. | Machine learning models can automate count; correlates with traditional scores. | Computational pathology; H&E-stained sections; deep learning segmentation. | [68] |
Table 2: Correlation Between ML-Derived and Traditional Histological Scores
| Machine Learning (ML) Derived Measure | Correlation with Traditional Histologic Score (rho) | What It Quantifies |
|---|---|---|
| NP Cell Number | 0.65 | Loss of cellularity in the nucleus pulposus. |
| NP Area Ratio | 0.87 | Reduction in the relative size of the NP. |
| NP/AF Border Integrity | 0.79 | Disorganization and tearing at the border between NP and annulus fibrosus. |
| NP Roundness | 0.73 | Change in tissue shape due to degeneration. |
| AF Perimeter | 0.78 | Structural changes in the annulus fibrosus. |
Data derived from a rat model of disc degeneration, demonstrating the application of automated analysis for fibrotic tissue changes [68].
Experimental Protocols
Protocol 1: Histopathological Evaluation of Fibrotic Capsule Formation
This protocol is adapted from a study investigating adhesive anti-fibrotic interfaces on diverse organs [66].
- Implantation: Implant your neural electrode device (e.g., polyurethane-based) subcutaneously or in the target neural tissue of your animal model (rat, mouse, or pig). The experimental group should feature the device with an adhesive interface (e.g., composed of crosslinked poly(acrylic acid) and poly(vinyl alcohol)), while the control group uses an identical but non-adhesive device, secured with sutures if necessary.
- Explanation and Fixation: At the endpoint (e.g., 3, 7, 14, 28, and 84 days post-implantation), explant the device with the surrounding tissue. Immerse the tissue sample in 4% paraformaldehyde (PFA) for 24 hours for fixation, followed by multiple washes in phosphate-buffered saline (PBS).
- Sectioning and Staining: Process the fixed tissue for paraffin embedding. Section the blocks into thin slices (e.g., 5-15 µm) and mount them on slides. Perform standard Hematoxylin and Eosin (H&E) staining to visualize general tissue structure and collagen deposition.
- Histological Analysis: Examine the slides under a microscope. A blinded pathologist should evaluate the formation of a fibrous capsule. The key metric is the thickness of the collagenous layer at the implant-tissue interface, which should be measured and compared to both the native tissue and the control implant interface [66].
Protocol 2: Immunofluorescence Analysis of Immune Cell Infiltration
This protocol details the steps to quantify specific immune cells involved in the FBR [66].
- Sample Preparation: Follow the steps for implantation, explantation, and sectioning as described in Protocol 1.
- Antibody Staining: On the tissue sections, perform immunofluorescence co-staining using antibodies against:
- Fibroblasts: Anti-αSMA (alpha-smooth muscle actin).
- Neutrophils: Anti-neutrophil elastase.
- Macrophages: Anti-CD68 (pan-macrophage), anti-iNOS (pro-inflammatory M1 phenotype), and/or anti-CD206 (anti-inflammatory M2 phenotype).
- T-cells: Anti-CD3.
- Imaging and Quantification: Acquire high-resolution fluorescence images of the implant-tissue interface. Quantify the number of each cell type in the collagenous layer over a standardized width (e.g., 500 µm) from multiple random fields of view. Compare cell counts between experimental and control groups.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Application | Example/Note |
|---|---|---|
| Adhesive Hydrogel | Creates conformal, anti-fibrotic interface between implant and tissue. | Interpenetrating network of poly(acrylic acid) N-hydroxysuccinimide ester and poly(vinyl alcohol) [66]. |
| SRC Inhibitor (Saracatinib) | Orphan drug that inhibits SRC mechanosensor protein; can reverse fibroblast activation in fibrotic hearts when combined with TGFβ pathway suppression [69]. | Potential therapeutic agent for modulating the fibrotic response. |
| Primary Antibodies (Immunofluorescence) | Labeling and quantification of key cells in the FBR. | αSMA (fibroblasts), CD68 (macrophages), Neutrophil Elastase (neutrophils), CD3 (T-cells) [66]. |
| Machine Learning Segmentation Model | Automated, high-throughput quantification of tissue areas and cell counts from histology slides. | Deep convolutional neural network trained to identify seven distinct disc tissues; can be adapted for fibrous capsule analysis [68]. |
| Poly(lactide-co-glycolide) (PLGA) | A common, biodegradable synthetic copolymer used for constructing implantable scaffolds and devices. | Often used with trimethylenecarbonate-ε-caprolactone to form filamentous fleeces or sponge-like scaffolds for tissue engineering [67]. |
Experimental Workflow and Signaling Visualization
Frequently Asked Questions
Q1: Why is polyimide (PI) often considered superior to PEGDA for long-term neural implants?
Polyimide (PI) demonstrates excellent long-term biostability and minimal foreign body reaction, making it suitable for chronic implants. It shows high cell adhesion and growth for neural cells and fibroblasts with low cytotoxicity, leading to reduced fibrosis formation [70]. In contrast, PEGDA exhibits significant cytotoxic effects, low cell adhesion, and induces a strong foreign body reaction, including fibrosis and the formation of multinucleated cells, making it unsuitable for long-term applications [70].
Q2: What are the key mechanisms of polymer biodegradation that could affect an implant's lifespan?
The primary mechanisms are:
- Hydrolysis: Water molecules react with vulnerable bonds in the polymer chain (e.g., esters, anhydrides), causing the chain to break [71].
- Oxidation: Oxidants generated by the body's inflammatory cells diffuse into the polymer, leading to degradation [71].
- Enzymatic Degradation: Enzymes from the biological system catalyze the breakdown of the polymer chains [71]. The degradation rate depends on the polymer's chemical structure, crystallinity, and the local implantation environment [71] [72].
Q3: Which flexible polymer materials show promise for reducing the chronic inflammatory response?
Besides polyimide, several flexible materials have shown improved biocompatibility:
- Polylactide (PLA) and Thermoplastic Polyurethane (TPU) demonstrated lower pathological responses in comparative studies, making them promising for neural interfaces [70].
- Polydimethylsiloxane (PDMS) also showed good compatibility in these studies [70].
- Conductive Polymers like PEDOT:PSS can reduce electrode impedance and improve charge transfer efficiency, while materials like silk-based bioelectronics offer programmable deformability for better integration [17].
Q4: How does the Foreign Body Reaction (FBR) lead to the failure of neural electrodes?
The FBR is a major factor limiting long-term stability [70] [4]:
- Acute Inflammation: Implantation causes tissue damage, leading to the release of inflammatory factors and recruitment of immune cells [4].
- Chronic Inflammation & Scar Formation: A persistent mechanical mismatch between the implant and soft brain tissue causes ongoing micro-movements. This activates microglia and astrocytes, which proliferate and secrete extracellular matrix components [4].
- Fibrous Capsule Formation: A dense, insulating glial scar forms around the electrode, increasing the distance between neurons and the recording/stimulation sites. This attenuates signal quality and increases impedance, ultimately leading to electrode failure [70] [4].
Troubleshooting Guides
Issue: Rapid Signal Attenuation and Rising Impedance Post-Implantation
Potential Causes and Solutions:
- Cause: Extensive Fibrous Encapsulation. A thick glial scar is insulating the electrode.
- Cause: Mechanical Mis-match. The stiffness (Young's modulus) of the implant is too high compared to brain tissue (~1 kPa), causing chronic irritation [4].
- Solution: Use flexible, compliant substrates with low bending stiffness. Strategies include using ultraflexible electrodes like NeuroRoots or mesh electrodes implanted with minimally invasive techniques [4].
Issue: Observable Cytotoxicity in Cell Culture Assays
Potential Causes and Solutions:
- Cause: Leaching of Cytotoxic Compounds. Unreacted monomers, initiators, or plasticizers may be leaching from the polymer into the culture medium [70].
- Cause: Inherent Material Toxicity. The polymer itself may not be biocompatible.
- Solution: Re-evaluate material choice. Replace highly cytotoxic materials like PEGDA with more compatible alternatives like PI, PLA, or TPU based on comparative study data [70].
Table 1: Comparative Biocompatibility of Selected Polymers for Neural Interfaces
Data synthesized from a 2025 comparative study assessing in vitro and in vivo responses [70].
| Polymer Material | In Vitro Cytotoxicity | Cell Adhesion (Neural) | Foreign Body Reaction (In Vivo) | Fibrosis Formation | Suitability for Long-Term Implants |
|---|---|---|---|---|---|
| Polyimide (PI) | Low | High | Mild | Low | Excellent |
| Polylactide (PLA) | Low | Moderate | Moderate | Moderate | Promising |
| PDMS | Low | Moderate | Moderate | Moderate | Promising |
| Thermoplastic Polyurethane (TPU) | Low | Moderate | Moderate | Moderate | Promising |
| PEGDA | High | Low | Strong | High | Unsuitable |
| Nylon 618 | Moderate | Moderate | Moderate | Moderate | Potentially Usable |
| Polycaprolactone (PCL) | Moderate | Moderate | Moderate | Moderate | Potentially Usable |
Table 2: Key Properties and Degradation Mechanisms of Biomedical Polymers
Data compiled from multiple sources on polymer properties and degradation [71] [72].
| Polymer Material | Key Advantages | Primary Degradation Mechanism | Key Degradation Factors | Typical Functional Timeframe |
|---|---|---|---|---|
| Polyimide (PI) | High biostability, excellent mechanical/electrical properties [73] [74] | Slow oxidation, minimal hydrolysis [71] | Chronic inflammation, oxidants [71] | Long-term (years) |
| PEGDA | Tunable hydrogel, good for cell encapsulation | Hydrolysis | Water content, crosslink density | Short-term (weeks-months) |
| PLA | Biodegradable, good biocompatibility | Hydrolysis | Molecular weight, crystallinity [71] | Tailorable (months-years) |
| PCL | Biodegradable, slow degradation rate | Hydrolysis | Molecular weight, crystallinity | Long-term degradation (>2 years) |
Experimental Protocols
Protocol 1: In Vitro Biocompatibility Assessment via Cell Culture
Objective: To evaluate the cytotoxicity and cell adhesion properties of polymer scaffolds using neural cell lines.
Materials:
- Polymer scaffolds (e.g., PI, PEGDA, PLA, PDMS)
- Neural cell line (e.g., PC-12) and fibroblast cell line (e.g., NRK-49F)
- Standard cell culture equipment and reagents
Methodology:
- Scaffold Preparation: Sterilize polymer scaffolds (e.g., via ethanol immersion and UV exposure). Pre-condition in cell culture medium for 24 hours.
- Cell Seeding: Seed cells directly onto the scaffold surfaces at a standard density (e.g., 10,000 cells/cm²). Include a tissue culture plastic well as a positive control.
- Cytotoxicity Assay: After 24-72 hours, assess cell viability using a standard MTT or Live/Dead assay. Measure the release of lactate dehydrogenase (LDH) as a marker of cell death.
- Cell Adhesion and Morphology: Fix and stain cells with phalloidin (for actin) and DAPI (for nuclei) after 24 hours. Image using fluorescence or scanning electron microscopy (SEM) to qualitatively and quantitatively assess cell adhesion and spreading [70].
Protocol 2: In Vivo Assessment of Foreign Body Reaction to Implants
Objective: To analyze the brain tissue response, including inflammation and fibrosis, to implanted polymer scaffolds.
Materials:
- Polymer scaffolds (phantom electrodes)
- Animal model (e.g., rats)
- Stereotaxic surgical setup
- Histology reagents and equipment
Methodology:
- Implantation: Anesthetize the animal and implant the polymer scaffold into the target brain region (e.g., cortex or hippocampus) using a stereotaxic frame and aseptic technique.
- Recovery and Duration: Allow the animal to recover and maintain for a set period (e.g., 4 weeks) to observe chronic tissue response.
- Tissue Harvest and Sectioning: Perfuse the animal transcardially with paraformaldehyde. Extract the brain, post-fix, and section it coronally around the implant site using a cryostat or microtome.
- Histological Analysis:
- H&E Staining: Assess general tissue morphology and inflammatory cell infiltration.
- Immunohistochemistry: Use antibodies against Iba1 (to label activated microglia), GFAP (to label reactive astrocytes), and CD68 (for macrophages) to quantify the immune response.
- Fibrosis Assessment: Use stains like Masson's Trichrome or picrosirius red to visualize collagen deposition and fibrous capsule thickness around the implant [70] [4].
Material Interaction Pathways
Foreign Body Reaction Pathway
Polymer Biocompatibility Assessment Workflow
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Biocompatibility Testing
| Research Reagent | Function in Experiment | Key Consideration |
|---|---|---|
| PC-12 Cell Line | A model neural cell line derived from rat pheochromocytoma used to assess neural-specific cytotoxicity and adhesion on polymer scaffolds [70]. | Differentiate with NGF for a more neuronal phenotype. |
| NRK-49F Cell Line | A normal rat kidney fibroblast cell line used to evaluate the response of connective tissue cells, which are key players in the fibrotic response [70]. | Useful for modeling the fibroblast involvement in fibrosis. |
| Iba1 Antibody | A marker for activated microglia via immunohistochemistry; quantifies the innate immune response around the implant site [4]. | The density of Iba1+ cells is a key metric for neuroinflammation. |
| GFAP Antibody | A marker for reactive astrocytes via immunohistochemistry; assesses the glial scar formation component of the Foreign Body Reaction [4]. | Increased GFAP staining intensity indicates astrocyte activation. |
| MTT Assay Kit | A colorimetric assay that measures metabolic activity as an indicator of cell viability and proliferation on or near polymer samples [70]. | Detects only metabolically active cells; can be influenced by material color. |
| LDH Assay Kit | Measures lactate dehydrogenase release from damaged cells into the culture medium, quantifying cytotoxicity [70]. | Correlates directly with cell membrane damage and death. |
Troubleshooting Guide: Common Experimental Issues
Q1: Why is the electrochemical impedance of my neural electrode unexpectedly high after implantation?
High impedance often results from biofilm formation or protein adsorption on the electrode surface, which creates a barrier to charge transfer. This typically occurs during the first 2-4 weeks post-implantation as the foreign body response (FBR) progresses [2].
Troubleshooting Steps:
- Perform a Dummy Cell Test: Disconnect your electrochemical cell and replace it with a 10 kΩ resistor. Run a cyclic voltammetry (CV) scan from +0.5 V to -0.5 V at 100 mV/s. The result should be a straight line intersecting the origin with currents of ±50 μA. A correct response confirms your instrument and leads are functioning properly, indicating the problem lies with the cell itself [75].
- Check Your Reference Electrode: High impedance can stem from a clogged or damaged reference electrode. Reconnect your cell with the reference and counter electrode leads connected together to the counter electrode (2-electrode configuration). Run the CV scan again. If you now obtain a typical voltammogram, the issue is likely with your reference electrode. Check that the frit is not clogged, no air bubbles are blocking it, and it is properly immersed in the solution [75].
- Inspect the Working Electrode: If the problem persists, the working electrode surface may be compromised. For solid electrodes, recondition the surface by polishing or electrochemical treatment. For thin-film electrodes, the issue could be film detachment from the current collector or dissolution in the electrolyte [75].
Q2: My recorded neural signals have become noisy and attenuated over a 6-week implantation. What could be the cause?
Signal attenuation is frequently caused by the formation of a fibrotic scar tissue capsule around the electrode, which increases the distance between neurons and the recording sites [2] [4]. This insulating sheath elevates electrical impedance and dampens signal amplitude.
Troubleshooting Steps:
- Verify Electrochemical Stability: Perform weekly electrochemical impedance spectroscopy (EIS) and cyclic voltammetry (CV) in vivo. Consistent impedance and charge storage capacity (CSC) over time suggest the electrode itself is stable, pointing to biological factors like fibrosis as the culprit [76].
- Confirm Electrode Material Integrity: Ensure your electrode coating is designed for stability. For example, sputtered ruthenium oxide (RuOx) has been shown to maintain stable impedance and CSCc over 6 weeks, with 1 kHz impedance decreasing from a median of 1.06 MΩ to 0.68 MΩ, indicating stable interface properties [76].
- Consider Mechanical Mismatch: Evaluate the flexibility of your electrode. Flexible electrodes with a low Young's modulus (matching brain tissue at 1–10 kPa) significantly reduce chronic micromotions that exacerbate the FBR and glial scar formation [4].
Q3: The charge storage capacity of my electrode coating degrades rapidly during accelerated testing. How can I improve its longevity?
Degradation often indicates insufficient electrochemical stability of the coating material under repeated charge injection.
Troubleshooting Steps:
- Select Stable Materials: Utilize faradaic materials known for their robust charge injection, such as sputtered ruthenium oxide (RuOx) or iridium oxide (SIROF). RuOx films demonstrate remarkable stability, with one study showing no significant deviation in CSCc over 6 weeks, maintaining ~24 mC cm⁻² at a 50 mV s⁻¹ sweep rate [76].
- Explore Nanostructured Coatings: Incorporate nanomaterials to enhance performance. Molybdenum disulfide (MoS₂) nanosheets can form "nanowells" on the electrode surface that act as quantized charge storage units, dramatically improving charge storage capacity and reducing impedance [77].
- Optimize Coating Morphology: Employ porous or high-surface-area coatings. A porous RuOx structure, for instance, provides a larger electroactive surface area, which increases charge storage and injection capacity without increasing the geometric footprint of the electrode [76].
Performance Data of Electrode Materials
Table 1: Electrochemical Performance of Neural Electrode Coatings In Vivo
| Electrode Material | Test Duration | Impedance at 1 kHz | Charge Storage Capacity (CSCc) | Key Stability Findings |
|---|---|---|---|---|
| Sputtered RuOx [76] | 6 weeks | Decreased from 1.06 MΩ to 0.68 MΩ | ~24 mC cm⁻² (at 50 mV/s) | Consistent single-unit recording; 75% active-electrode yield over 6 weeks. |
| MoS₂ Nanowells [77] | Not Specified | Multifold reduction vs. bare electrode | Multifold increase vs. bare electrode | 17.7x catalytic activity improvement; reduced inflammatory response. |
| SIROF (for comparison) [76] | Chronic (Ref.) | Low & Stable | High | Established stable chronic recording benchmark. |
Table 2: Impact of Foreign Body Reaction on Electrode Performance Over Time
| Post-Implantation Phase | Key Biological Processes | Impact on Electrode Function |
|---|---|---|
| Acute (Hours-Days) | Protein adsorption; inflammation; immune cell recruitment [2]. | Transient increase in impedance; temporary signal noise. |
| Chronic (Weeks-Months) | Fibrosis; glial scar formation; encapsulation by dense collagen matrix [2] [4]. | Permanent increase in impedance; signal attenuation; potential device failure. |
Detailed Experimental Protocols
Protocol 1: Weekly In Vivo Electrochemical Characterization
This protocol is essential for monitoring the stability of implanted electrodes [76].
- Setup: Use a potentiostat (e.g., Gamry Reference 600) in a 3-electrode configuration with the implanted electrode as the working electrode, a chloridized silver pad as a reference electrode, and a sterile needle in the tail as a counter electrode.
- Electrochemical Impedance Spectroscopy (EIS):
- Apply a 10 mV RMS sinusoidal voltage signal centered at the open circuit potential.
- Sweep the frequency from 1 Hz to 100 kHz, collecting 10 points per decade.
- Monitor impedance at key frequencies: 1 Hz (local field potentials), 1 kHz (single-unit action potentials), and 30 kHz (tissue impedance).
- Cyclic Voltammetry (CV):
- Cycle the electrode potential between -0.6 V and +0.6 V vs. Ag|AgCl.
- Use at least two scan rates: a slow 50 mV/s to assess total charge storage, and a fast 50,000 mV/s to simulate stimulation pulses.
- Integrate the cathodic current over a single cycle to calculate the cathodic Charge Storage Capacity (CSCc).
Protocol 2: Assessing Functional Stability via Neural Recording
This protocol evaluates the electrode's ability to record neural signals over time [76].
- Implantation: Implant the MEA in the target region (e.g., rat motor cortex) using a slow insertion speed (e.g., 100 µm/s) and, if available, a vibrating inserter to reduce acute tissue damage.
- Data Acquisition: Weekly, record extracellular neural signals from all active channels.
- Signal Analysis:
- Single-Unit Activity: Isolate and count single-unit action potentials. Track the number of active electrodes over time (single-unit active-electrode-yield).
- Signal Amplitude: Measure the peak-to-peak amplitude (Vpp) of the recorded action potentials.
- Signal-to-Noise Ratio (SNR): Calculate the SNR for identified units. Consistent Vpp and SNR values over time indicate good functional stability.
The Fibrosis Signaling Pathway
Diagram 1: The core pathway of Foreign Body Reaction (FBR) leading to signal loss. Key cytokine TGF-β stimulates fibroblast-to-myofibroblast differentiation, driving extracellular matrix (ECM) deposition and fibrotic capsule formation [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Neural Interface Stability Research
| Material / Reagent | Function in Research | Specific Example & Rationale |
|---|---|---|
| Sputtered RuOx Coating | Faradaic electrode coating for charge injection. | Low-cost alternative to iridium oxide; demonstrates stable impedance and CSCc over 6-week implants [76]. |
| MoS₂ Nanosheets | Nanostructured coating to enhance sensitivity. | Forms "nanowells" that act as quantized charge storage units, reducing impedance and inflammatory response [77]. |
| Flexible Polymer Substrate | Base material for neural probes. | Polyimide-based electrodes reduce mechanical mismatch with brain tissue (Young's modulus ~1-10 kPa), mitigating chronic inflammation [4]. |
| Tungsten Guidance Shuttle | Temporary stiffener for implanting flexible electrodes. | Enables precise insertion of flexible electrodes with minimal cross-sectional area and acute injury [4]. |
| PEG Coating | Bioresorbable adhesive for guidance shuttles. | Melts after implantation, allowing for the retrieval of the guidance shuttle and leaving only the flexible electrode in place [4]. |
FAQs: Implementing AI for Fibrosis Prediction
1. How can we generate synthetic fibrosis data to overcome limited datasets for neural electrode research?
The limited availability of detailed human fibrosis data can be addressed using generative AI models, specifically Denoising Diffusion Probabilistic Models (DDPMs). These models learn the underlying distribution of real fibrosis patterns and can create realistic synthetic distributions for data augmentation [78].
- Experimental Protocol:
- Data Preparation: Gather a collection of real fibrosis distributions from imaging data. In cardiac research, 100 LGE-MRI distributions from patients were used. For neural interfaces, this could be adapted from histological sections or micro-CT scans of fibrotic tissue around electrodes [78].
- Model Training: Train a DDPM on these 2D representations of fibrosis. The model works by progressively adding Gaussian noise to the training images and then learning to reverse this process to generate new samples from random noise [78].
- Generation: Use the trained model to synthesize a large number of novel, realistic fibrosis distributions. A study successfully generated 1,000 synthetic distributions to expand its training dataset [78].
- Validation: Compare synthetic and real data using metrics like mean intensity values and Shannon entropy to ensure the generated data captures the variability and texture of real fibrosis [78].
2. What non-invasive biomarkers and tools can be used to assess fibrosis risk and progression?
Several AI-driven tools and biomarker-based scores can be used for non-invasive fibrosis assessment. The table below summarizes key tools, though their application for neural fibrosis requires further validation.
Table 1: Non-Invasive Tools for Fibrosis Analysis
| Tool / Score Name | Primary Application | Key Inputs / Basis | Performance / Notes |
|---|---|---|---|
| Fibro-Predict [79] | Liver fibrosis (General population screening) | Routine blood tests (e.g., hemoglobin, platelets) & demographics via Machine Learning (XGBoost) | 5-year prediction AUC: 0.81; Designed for early detection in EHR data [79]. |
| Proteomic Aging Clock [80] [81] | Biological Age & Fibrosis Link | AI model trained on protein data from blood samples (e.g., UK Biobank proteomics) | Accurately predicts biological age (R²=0.84); Shows accelerated aging in fibrotic disease [80] [81]. |
| FIB-4 Index [82] | Liver fibrosis | Age, Liver enzyme levels (AST, ALT), Platelet count | High Negative Predictive Value; useful for excluding advanced fibrosis; lower sensitivity [82]. |
| NAFLD Fibrosis Score (NFS) [82] | Liver fibrosis | Age, BMI, Diabetes status, Albumin, AST, ALT | Also has a high Negative Predictive Value [82]. |
3. Our AI model for predicting fibrosis outcomes is performing poorly. What are common troubleshooting steps?
Poor model performance can stem from several issues. Follow this structured troubleshooting guide.
Table 2: Troubleshooting Guide for AI Fibrosis Models
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low Predictive Accuracy | • Insufficient or low-quality training data.• Data leakage between training and test sets.• Model architecture not suited to the data type. | • Use generative AI (e.g., DDPMs) for data augmentation [78].• Ensure temporal or spatial separation of data splits. Use a "rolling-origin" validation method [79].• For image-like data (e.g., fibrosis distributions), use CNNs or Diffusion Models. For tabular data (e.g., blood tests), use ensemble methods like Gradient Boosted Trees (XGBoost) [79]. |
| Model Fails to Generalize | • Overfitting to the training dataset.• Dataset does not capture full patient/ tissue variability. | • Incorporate synthetic data to increase dataset diversity and better capture biological variability [78].• Apply strong regularization techniques and perform rigorous external validation on a separate cohort [79]. |
| Difficulty Identifying Key Features | • High-dimensional, complex omics data (e.g., transcriptomics).• Non-linear relationships between features. | • Use a pathway-aware or omics transformer model (e.g., ipf-P3GPT) to analyze gene expression and identify core pathways like TGF-β signaling, inflammation, and ECM remodeling [80] [81]. |
The Scientist's Toolkit: Research Reagent & Model Solutions
Table 3: Essential AI Tools and Models for Fibrosis Research
| Tool / Reagent | Function / Category | Specific Application in Fibrosis |
|---|---|---|
| Denoising Diffusion Probabilistic Model (DDPM) [78] | Generative AI Model | Creates synthetic, high-quality fibrosis distributions from a limited dataset for augmentation [78]. |
| Pathway-Aware Proteomic Aging Clock [80] [81] | AI-based Biomarker | Measures biological age from blood proteomics; identifies acceleration due to fibrotic processes [80] [81]. |
| Omics Transformer (e.g., ipf-P3GPT) [80] [81] | Generative AI for Biology | Analyzes and generates gene expression profiles from text prompts; identifies shared/unique pathways between fibrosis and aging [80] [81]. |
| Gradient Boosted Trees (XGBoost) [79] | Machine Learning Algorithm | Builds powerful predictive models from structured, tabular data (e.g., electronic health records) for risk stratification [79]. |
| TNIK Inhibitor (e.g., rentosertib) [83] | Small Molecule Inhibitor | First-in-class AI-generated therapeutic target; inhibits a key kinase involved in fibrotic pathways; exemplifies AI-driven drug discovery [83]. |
Visualizing Experimental Workflows and Signaling Pathways
Core Fibrosis Signaling Pathways
This diagram outlines the key molecular pathways involved in fibrotic progression, which are prime targets for AI-driven analysis and intervention.
AI-Driven Fibrosis Analysis Workflow
This flowchart illustrates a complete pipeline for using AI and in-silico models to predict fibrosis outcomes and test therapeutic strategies.
Conclusion
The challenge of fibrosis around neural electrodes demands a multifaceted approach that integrates foundational biology with advanced engineering. Key takeaways include the critical importance of mitigating the foreign body reaction through a combination of biocompatible, soft materials; intelligent electrode design that minimizes mechanical mismatch; and active strategies such as localized drug delivery. The future of neural interfaces lies in the continued development of biohybrid and "living" electrodes that can dynamically interact with their environment, smart materials that respond to physiological changes, and personalized approaches informed by predictive modeling. Closing the loop between preclinical validation and clinical application will be essential for translating these innovative strategies into reliable, long-lasting neuroprosthetic solutions that restore function for patients.
References
- 1. FOREIGN BODY REACTION TO BIOMATERIALS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2327202/]
- 2. Biomedical and Tissue Engineering Strategies to Control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8185207/]
- 3. Macrophages and fibroblasts in foreign body reactions [https://www.sciencedirect.com/science/article/pii/S2590006423002430]
- 4. Long-term stability strategies of deep brain flexible neural ... [https://www.nature.com/articles/s41528-025-00410-x]
- 5. Macrophage and Fibroblast Interactions in Biomaterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6415913/]
- 6. Macrophages, Foreign Body Giant Cells and Their ... - MDPI [https://www.mdpi.com/1996-1944/8/9/5269]
- 7. Myofibroblasts: Function, Formation, and Scope of Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8391320/]
- 8. Mechanical and Physical Regulation of Fibroblast ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2020.609653/full]
- 9. Engineering strategies towards overcoming bleeding and glial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8975777/]
- 10. Contribution of macrophages to neural survival and ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-023-02955-y]
- 11. Mechanosensing by TRPV4 mediates stiffness-induced ... [https://pubmed.ncbi.nlm.nih.gov/34726952/]
- 12. Allometrically scaling tissue forces drive pathological ... [https://www.nature.com/articles/s41551-023-01091-5]
- 13. Insertion Systems for Ultra-Thin Neural Electrodes [https://engineering.purdue.edu/CID/Projects/insertion-thin-neural-electrodes.html]
- 14. Correlation of Electrical Impedance and Evoked Potentials ... [https://www.sciencedirect.com/science/article/pii/S1094715925006968]
- 15. App-based daily self-measurement of impedance in ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1618031/full]
- 16. Performance‐Recoverable Closed‐Loop Neuroprosthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447059/]
- 17. Multidimensional advances in neural interface technology for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12296523/]
- 18. Electrode impedance dynamics in sequential cochlear implant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605110/]
- 19. Chronically Implanted Intracranial Electrodes: Tissue Reaction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6187588/]
- 20. Revolutionizing brain‒computer interfaces - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243264/]
- 21. Mechano-electrochemical impedance spectroscopy [https://www.sciencedirect.com/science/article/abs/pii/S2542435125003587]
- 22. Advanced Biocompatible and Biodegradable Polymers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611034/]
- 23. The “Big Three” in biocompatibility testing of medical devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800850/]
- 24. Navigating Biocompatibility: An Introduction to ISO 10993 ... [https://medinstitute.com/blog/navigating-biocompatibility-an-introduction-to-iso-10993-series-of-standards/]
- 25. Histopathology in Focus: Evaluating Implanted Medical ... [https://namsa.com/resources/blog/histopathology-evaluating-implanted-medical-devices/]
- 26. Biocompatibility Assessment Resource Center [https://www.fda.gov/medical-devices/premarket-submissions-selecting-and-preparing-correct-submission/biocompatibility-assessment-resource-center]
- 27. Bio-inspired electronics: Soft, biohybrid, and “living” neural ... [https://www.nature.com/articles/s41467-025-57016-0]
- 28. Conductive organic electrodes for flexible electronic devices [https://www.nature.com/articles/s41598-023-30207-9]
- 29. Stretchable Conductive Polymers and Composites based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6401235/]
- 30. Fabrication of flexible electronics by screen printing with ... [https://www.sciencedirect.com/science/article/pii/S2213846325000677]
- 31. Progress and challenges of implantable neural interfaces ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8077843/]
- 32. Bio-integrative Design of The Neural Tissue- Device Interface [https://pmc.ncbi.nlm.nih.gov/articles/PMC8671324/]
- 33. Overcoming failure: improving acceptance and success of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00168-7]
- 34. Revolutionizing brain‒computer interfaces: overcoming ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03573-x]
- 35. Novel method to improve the biocompatibility and chronic stability of... [https://www.news-medical.net/news/20250630/Novel-method-to-improve-the-biocompatibility-and-chronic-stability-of-neural-electrode-implants.aspx]
- 36. Guidelines to Study and Develop Soft Electrode Systems ... [https://www.sciencedirect.com/science/article/pii/S0896627320308060]
- 37. Domesticating the Foreign Body Response: Recent Advances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6774350/]
- 38. Drug-Coated Neural Implants Reduce Immune Rejection [https://neurosciencenews.com/neural-implant-rejection-29389/]
- 39. Rectifying disorder of extracellular matrix to... | Nature Communications [https://www.nature.com/articles/s41467-023-38282-2?error=cookies_not_supported&code=e7ea0ce7-5319-4c65-bbb0-be261d58cba7]
- 40. Immunomodulating Red Blood Cell Coating for Mitigation ... [https://www.sciencedirect.com/science/article/pii/S2666138125000143]
- 41. Drug-Eluting Stents in Preclinical Studies Updated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2935144/]
- 42. Surface modifications of biomaterials in different applied ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10331796/]
- 43. Biomimetic hydrogel scaffolds for stimulating fibrotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425956/]
- 44. Frontiers | Biomedical and Tissue Engineering Strategies to Control Foreign Body Reaction to Invasive Neural Electrodes [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.659033/full]
- 45. A review of biomimetic surface functionalization for bone- ... [https://www.sciencedirect.com/science/article/pii/S0079642519300702]
- 46. Cell membrane biomimetic nanoplatforms: a new strategy ... [https://www.sciencedirect.com/science/article/pii/S2590006425009147]
- 47. Advances in bioelectronics for neural interfacing [https://link.springer.com/article/10.1557/s43579-025-00822-w]
- 48. 3D soft microbump electrodes for elastic interaction with ... [https://www.nature.com/articles/s41528-025-00480-x]
- 49. Protocol for muscle fiber type and cross-sectional area ... [https://www.sciencedirect.com/science/article/pii/S2666166724005896]
- 50. Troubleshooting Cochlear Implant Malfunction Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10895891/]
- 51. Minimally invasive implantation of scalable high-density ... [https://www.nature.com/articles/s41551-025-01501-w]
- 52. Advances in Flexible High-Density Microelectrode Arrays ... [https://www.sciencedirect.com/science/article/pii/S0956566325009790]
- 53. Micromotion - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/engineering/micromotion]
- 54. Recent advances in neural electrode–tissue interfaces [https://www.sciencedirect.com/science/article/abs/pii/S2468451117300478]
- 55. Ultrasoft microwire neural electrodes improve chronic tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5512864/]
- 56. Tissue Response to Neural Implants: The Use of Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6624471/]
- 57. Recent developments in multifunctional neural probes for ... [https://www.nature.com/articles/s41378-022-00444-5]
- 58. Multifunctional Tetrode-like Drug delivery, Optical ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566324007024]
- 59. Decreasing the physical gap in the neural-electrode ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1425226/full]
- 60. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 61. Cytotoxicity Assays: In Vitro Methods to Measure Dead Cells [https://www.ncbi.nlm.nih.gov/books/NBK540958/]
- 62. The Assay Guidance Manual: A Guide for In Vitro and ... [https://www.promega.com/resources/pubhub/tpub_191-the-assay-guidance-manual/]
- 63. In Vitro Modulation of Macrophage Inflammatory and Pro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190423/]
- 64. Reprogramming macrophage polarization with a small ... [https://www.sciencedirect.com/science/article/pii/S0753332225006420]
- 65. In vitro Cell Migration, Invasion, and Adhesion Assays [https://pmc.ncbi.nlm.nih.gov/articles/PMC6587234/]
- 66. Adhesive anti-fibrotic interfaces on diverse organs [https://www.nature.com/articles/s41586-024-07426-9]
- 67. In Vivo Comparison of Synthetic Macroporous Filamentous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9496825/]
- 68. Automated Computational Pathology to Assess ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488225/]
- 69. Researchers uncover promising new strategy to treat ... [https://news.stanford.edu/stories/2025/04/cardiac-cardiovascular-fibrosis-research-study-treatment]
- 70. A Comparative Study of Polymer Toxicity and Tissue Response [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467080/]
- 71. Degradability of Polymers for Implantable Biomedical Devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC2769140/]
- 72. 16.1 Biocompatibility and biodegradation of polymers [https://fiveable.me/introduction-polymer-science/unit-16/biocompatibility-biodegradation-polymers/study-guide/s9Gl7ZG8j39AZeFG]
- 73. Biocompatibility of Polyimides: A Mini-Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6804260/]
- 74. Polyimide as a biomedical material - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2024/na/d4na00292j]
- 75. Troubleshooting Electrochemical Cell [https://redox.me/blogs/good-measurement-practices/troubleshooting-electrochemical-cell]
- 76. Electrochemical stability and neural recording with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278477/]
- 77. A nanowell-based MoS2 neuroelectrode for high-sensitivity ... [https://www.sciencedirect.com/science/article/pii/S2589004224021746]
- 78. Synthetic fibrosis distributions for data augmentation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12021809/]
- 79. Fibro predict a machine learning risk score for advanced ... [https://www.nature.com/articles/s41598-025-17534-9]
- 80. AI Tools Uncover New Link Between Idiopathic Pulmonary ... [https://www.aging-us.com/news-room/ai-tools-uncover-new-link-between-idiopathic-pulmonary-fibrosis-and-aging]
- 81. Insilico employs AI-driven tools to uncover the link between ... [https://insilico.com/tpost/5t5cdcvdj1-insilico-employs-ai-driven-tools-to-unco]
- 82. Diagnostic Performance of Fibrosis‐4 Index, Nonalcoholic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12449594/]
- 83. A generative AI-discovered TNIK inhibitor for idiopathic ... [https://www.nature.com/articles/s41591-025-03743-2]