Strategies for Minimizing Foreign Body Response in Bioelectronics: From Molecular Mechanisms to Clinical Translation
This article provides a comprehensive analysis of innovative strategies to mitigate the foreign body response (FBR) against implantable bioelectronic devices.
Strategies for Minimizing Foreign Body Response in Bioelectronics: From Molecular Mechanisms to Clinical Translation
Abstract
This article provides a comprehensive analysis of innovative strategies to mitigate the foreign body response (FBR) against implantable bioelectronic devices. Targeting researchers, scientists, and drug development professionals, it synthesizes foundational knowledge of FBR immunology with cutting-edge methodological advances in biomaterial science, troubleshooting for device optimization, and comparative validation of emerging technologies. The content explores how recent breakthroughs in immunomodulatory materials, surface engineering, and device design are overcoming the critical challenge of FBR, thereby enhancing the longevity and performance of next-generation bioelectronics for therapeutic and diagnostic applications.
Understanding the Foreign Body Response: The Immune Battle Against Implanted Bioelectronics
FAQs: Understanding the Foreign Body Response
What is the Foreign Body Response (FBR) and why is it a critical problem for implantable bioelectronics?
The Foreign Body Response is an immune-mediated reaction to implanted materials, culminating in the formation of a dense, collagenous fibrotic capsule that isolates the device [1] [2]. For bioelectronics, this is a fundamental challenge because the fibrotic capsule can impair device function by disrupting the critical interface with the target tissue [3] [4]. This can lead to signal degradation in recording electrodes, increased impedance for stimulating electrodes, and ultimately, device failure [5] [6]. It is estimated that FBR contributes to the failure of approximately 30% of breast implants and about 10% of all other implantable medical devices, presenting a significant hurdle for long-term therapies [3] [7].
What are the key cellular stages of the FBR cascade?
The FBR is a sequential process that can be broken down into several key stages [1] [8]:
- Protein Adsorption: Within seconds of implantation, blood plasma proteins (e.g., albumin, fibrinogen, fibronectin) non-specifically adsorb to the implant surface, forming a provisional matrix [3] [4].
- Acute Inflammation: Neutrophils are the first responders (within hours to 2 days), attempting to clear the foreign material [1] [2]. They are quickly followed by monocytes that differentiate into pro-inflammatory M1 macrophages [1] [3].
- Chronic Inflammation and FBGC Formation: Unable to phagocytose large implants, macrophages undergo "frustrated phagocytosis" and fuse to form multinucleated Foreign Body Giant Cells (FBGCs), a hallmark of chronic FBR [1] [3].
- Fibrotic Encapsulation: Activated macrophages and other immune cells release factors like TGF-β, which drive fibroblast recruitment, their differentiation into collagen-secreting myofibroblasts, and the eventual formation of an avascular, dense fibrous capsule [1] [8].
Which signaling pathways are most critical for driving fibroblast-to-myofibroblast differentiation, and can they be targeted?
The differentiation of fibroblasts into matrix-depositing myofibroblasts is a pivotal event in fibrosis, primarily driven by the TGF-β (Transforming Growth Factor-Beta) signaling pathway [1] [8]. TGF-β activates both Smad-dependent and Smad-independent pathways (including Rho/ROCK) to promote the expression of α-smooth muscle actin (α-SMA) and collagen synthesis [8]. The IL-17 signaling pathway has also been implicated in promoting fibrosis, with senescent cells potentially exacerbating this effect [8]. These pathways are prime targets for therapeutic intervention, with research exploring drugs like tranilast (an anti-fibrotic) and ROCK inhibitors to disrupt this critical step [8].
Troubleshooting Guide: Common Experimental Hurdles in FBR Research
Problem: High Variability in Capsule Thickness Measurements in Animal Models
Inconsistent capsule thickness data can stem from uncontrolled variables related to the implant or the host [7].
- Solution:
- Standardize Implant Properties: Ensure consistency in implant size, shape, surface topography, and, critically, mechanical stiffness (modulus) across experimental groups, as all of these parameters are known to influence the degree of FBR [3] [7].
- Control for Biological Variability: Implant multiple test materials within the same animal in a controlled configuration to minimize inter-animal variability, as demonstrated in studies with mice [7].
- Follow Systematic Histology: Use standardized protocols for tissue harvesting, sectioning orientation, and staining (e.g., Masson's Trichrome for collagen, H&E for general structure). Measure capsule thickness at multiple, predefined locations around the implant circumference.
Problem: Rapid Biofouling on Sensor Surfaces Impairs Function
Non-specific protein adsorption is the initiating event of FBR and can immediately foul biosensor surfaces [2].
- Solution:
- Implement Anti-Fouling Coatings: Utilize surface modifications with hydrophilic or zwitterionic polymers (e.g., poly(2-hydroxyethyl methacrylate) pHEMA, methacryloyloxyethyl phosphorylcholine (MPC)-based polymers) that create a hydration layer to resist protein adsorption [3] [8].
- Optimize Surface Topography: Introduce micro- or nano-scale surface textures. For example, porous pHEMA scaffolds with 34 μm porosity have been shown to elicit a less dense capsule and increased vascularization compared to non-porous or differently porous versions [3].
- Consider Novel Material Platforms: Investigate the use of intrinsically anti-fouling bulk materials, such as the EVADE (easy-to-synthesize vinyl-based anti-FBR dense elastomers) platform, which has demonstrated negligible fibrotic encapsulation for up to one year in rodent models [7].
Problem: Inconsistent Macrophage Polarization in In Vitro Models
It is challenging to replicate the dynamic switch from pro-inflammatory (M1) to pro-healing/pro-fibrotic (M2) macrophage phenotypes in cell culture [1].
- Solution:
- Use Defined Polarizing Cytokines: Prime primary macrophages or cell lines with specific cytokine cocktails (e.g., IFN-γ + LPS for M1; IL-4 + IL-13 for M2) before exposing them to your material [1].
- Monitor Polarization Status: Use a combination of surface marker analysis (e.g., flow cytometry for CCR7, CD206) and cytokine secretion profiling (e.g., ELISA for TNF-α, IL-6, IL-10, TGF-β) to confirm and track polarization states [1] [7].
- Co-culture with Fibroblasts: Establish a more complex in vitro model by co-culturing macrophages with fibroblasts in the presence of the biomaterial to better mimic the cellular crosstalk that occurs in vivo [1].
Quantitative Data: FBR Timelines and Device Impact
Table 1: Key Cell Types and Their Roles in the FBR Cascade
| Cell Type | Time of Appearance | Primary Role in FBR | Key Secretions/Markers |
|---|---|---|---|
| Neutrophils | Hours to 2 days [2] [4] | First responders; release proteolytic enzymes and ROS; attempt to phagocytose debris [1] [2] | ROS, MMPs, Neutrophil Extracellular Traps (NETs) [2] |
| Macrophages (M1) | Days 2-3, peaking in acute phase [1] [4] | Pro-inflammatory; attempt phagocytosis; secrete pro-inflammatory cytokines [1] [3] | TNF-α, IL-6, CCR7 [1] [7] |
| Foreign Body Giant Cells (FBGCs) | Multiple days, chronic phase [1] [2] | Result from macrophage fusion; persistent "frustrated phagocytosis" [1] [3] | ROS, enzymes for degradation [1] [2] |
| Macrophages (M2) | Later in chronic phase, as inflammation resolves [1] [3] | Anti-inflammatory; promote tissue remodeling and fibrosis [1] [3] | TGF-β, IL-10, PDGF [1] [3] |
| Fibroblasts / Myofibroblasts | From ~day 7, numbers peak around day 28 [2] [8] | Deposit collagen and ECM; contract the capsule [1] [8] | Collagen I/III, α-SMA (myofibroblast marker) [3] [8] |
Table 2: Impact of FBR on Specific Medical Devices
| Device Category | Common FBR-Related Issues | Consequences | Reported Failure/Complication Rates |
|---|---|---|---|
| Breast Implants | Capsular contracture, granuloma formation, pain [1] [3] | Implant hardening, distortion, pain, need for revision surgery [1] [8] | 8-30% of patients experience capsular contracture; up to 54% recurrence after reoperation [1] [3] |
| Neural Interfaces | Fibrotic encapsulation of electrodes, inflammation [3] [5] | Increased electrode impedance, signal attenuation or loss, stimulation failure [5] [6] | A primary cause of chronic recording instability and failure of microelectrode arrays [5] [6] |
| Continuous Subcutaneous Infusion Catheters | Fibrosis around catheter tip [7] | Blocked fluid flow, impaired drug absorption (e.g., insulin), necessitates frequent replacement [7] | Commercial catheters often require replacement every 2-3 days due to FBR [7] |
| Cell Encapsulation Devices | Fibrotic overgrowth of the device [3] | Isolation of encapsulated cells, hypoxia, nutrient deprivation, therapeutic failure [3] | A major barrier to long-term efficacy of encapsulated cell therapies [3] |
Experimental Protocols for Key FBR Assays
Protocol: Subcutaneous Implantation and Capsule Histomorphometry in Rodents
This is a standard in vivo model for evaluating the fibrotic response to biomaterials [7].
- Material Preparation: Sterilize test materials (e.g., polymer discs, 0.5-1.0 cm diameter). Critical: Control for material stiffness, size, and surface topography to isolate the variable of interest [7].
- Surgical Implantation: Anesthetize the animal (e.g., C57BL/6 mouse) and make a dorsal midline incision. Create subcutaneous pockets by blunt dissection on both flanks. Insert one material per pocket. Close the incision with sutures or wound clips [7].
- Explanation and Tissue Harvest: Euthanize the animal at the predetermined endpoint (e.g., 2 weeks for acute inflammation, 4 weeks or longer for fibrosis). Carefully excise the implant with the surrounding tissue envelope intact.
- Histological Processing: Fix the explant in 4% paraformaldehyde, dehydrate, and embed in paraffin. Section the tissue into 5-10 μm thick slices and mount on slides.
- Staining and Analysis:
- H&E Staining: For general tissue structure and cellularity.
- Masson's Trichrome Staining: To specifically visualize collagen (stains blue) and the fibrous capsule.
- Immunohistochemistry (IHC): For specific cell types (e.g., F4/80 for macrophages, α-SMA for myofibroblasts) or proteins (e.g., S100A8/A9) [7].
- Capsule Thickness Measurement: Using stained sections, take multiple (e.g., 10-20) perpendicular measurements of the capsule thickness around the entire implant under a microscope. Calculate the average and standard deviation [7].
Protocol: Profiling Macrophage Polarization In Vitro
This protocol helps characterize the immune response to a material by assessing macrophage phenotype.
- Cell Culture: Use a primary macrophage cell line (e.g., bone marrow-derived macrophages from mice) or an immortalized line (e.g., RAW 264.7).
- Polarization and Seeding:
- Differentiate monocytes into M0 macrophages using M-CSF.
- Pre-polarize macrophages by treating with LPS + IFN-γ (for M1) or IL-4 + IL-13 (for M2) for 24 hours.
- Seed the polarized macrophages onto the material surfaces or tissue culture plastic controls.
- Analysis (24-48 hours post-seeding):
- Gene Expression: Perform qRT-PCR to analyze expression of M1 markers (e.g., iNOS, TNF-α, IL-6) and M2 markers (e.g., Arg1, CD206, TGF-β).
- Protein Secretion: Collect cell culture supernatant and analyze cytokine levels using ELISA kits for M1 (TNF-α, IL-6) and M2 (TGF-β, IL-10) associated cytokines [7].
- Surface Markers: Detach cells and analyze surface markers characteristic of M1 (e.g., CCR7) and M2 (e.g., CD206) phenotypes via flow cytometry [1].
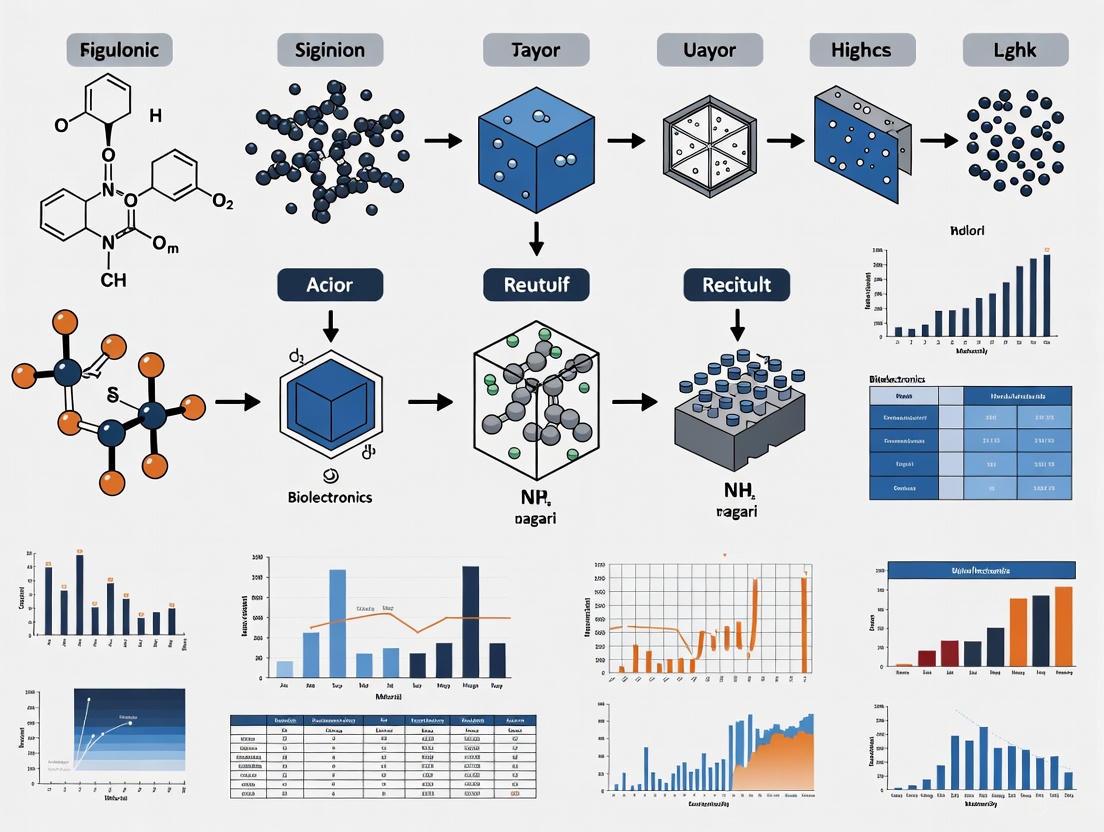
Visualization of the FBR Cascade and Key Pathways
Key Fibrogenic Signaling Pathways
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Reagents for FBR and Fibrosis Research
| Reagent / Material | Function/Application | Example Use in FBR Context |
|---|---|---|
| Recombinant Cytokines (TGF-β, IL-4, IL-13) | Directly polarize macrophages or stimulate fibroblast differentiation in vitro [1] [8]. | Used in cell culture to model the pro-fibrotic microenvironment and study myofibroblast differentiation [1]. |
| α-SMA (Alpha-Smooth Muscle Actin) Antibody | A standard marker for identifying activated myofibroblasts via immunohistochemistry or flow cytometry [3] [8]. | Critical for quantifying the number of pro-fibrotic cells in the tissue capsule surrounding an explanted device [3]. |
| Masson's Trichrome Stain | Histological stain that differentially colors collagen fibers blue, muscle fibers red, and nuclei dark brown/purple [7]. | The primary method for visualizing and quantifying the extent and density of the collagenous fibrotic capsule in tissue sections [7]. |
| EVADE Elastomers | A novel platform of immunocompatible elastomers that intrinsically resist FBR [7]. | Used as a positive control material or a next-generation substrate for devices to achieve long-term, minimal-fibrosis implantation [7]. |
| Clodronate Liposomes | A tool for in vivo depletion of macrophages [2]. | Used to experimentally confirm the central role of macrophages in FBR; macrophage depletion prevents fibrotic capsule formation [2]. |
| S100A8/A9 Inhibitors / Knockout Models | Target specific alarmin proteins implicated in the pro-inflammatory and pro-fibrotic cascade [7]. | Used to investigate the role of S100A8/A9 in FBR and as a potential therapeutic strategy to attenuate fibrosis [7]. |
The foreign body response (FBR) is an inevitable biological reaction to any implanted biomaterial or medical device. For bioelectronics researchers, understanding this process is critical to improving the long-term functionality and stability of implants. The FBR is a coordinated sequence of events involving the immune system and connective tissues, ultimately leading to the encapsulation of the device in a collagenous, scar-like capsule. This fibrotic tissue can isolate the implant from its target tissue, leading to device failure—a significant obstacle for neural interfaces, biosensors, and other implantable bioelectronics. The core cellular players driving this response are macrophages, foreign body giant cells (FBGCs), and fibroblasts. This guide provides troubleshooting advice and foundational knowledge to help researchers identify and mitigate the FBR in their experimental models.
FAQ: Understanding the Key Cellular Players
What are the main phases of the FBR?
The FBR progresses through well-defined, overlapping phases [9] [10]:
- Protein Adsorption: Within seconds of implantation, blood-derived proteins (e.g., albumin, fibrinogen) non-specifically adsorb to the biomaterial surface, forming a provisional matrix [10].
- Acute Inflammation: Neutrophils are the first responders, infiltrating the site within minutes to hours. They secrete factors that recruit monocytes [10].
- Chronic Inflammation: Monocytes arrive and differentiate into macrophages, which populate the implant interface. These cells attempt to phagocytose the material [10].
- FBGC Formation and Fibrosis: If phagocytosis fails (due to the implant's size), macrophages fuse into multinucleated Foreign Body Giant Cells (FBGCs). This phase is accompanied by the recruitment and activation of fibroblasts, which deposit collagen and other extracellular matrix (ECM) proteins, leading to the formation of a fibrous capsule [11] [9] [10].
What roles do macrophages and FBGCs play in device failure?
Macrophages are the primary coordinators of the FBR. They are highly plastic cells that can adopt different functional phenotypes, often broadly categorized as pro-inflammatory (M1) or pro-healing/anti-inflammatory (M2) [11] [9].
- M1 Macrophages: Driven by signals like LPS or IFN-γ, they secrete pro-inflammatory cytokines (e.g., TNF-α, IL-6, IL-1β) and reactive oxygen species (ROS) [9]. They dominate the early, inflammatory phase and can directly damage device materials through enzymatic degradation and oxidative stress [10].
- M2 Macrophages: Induced by cytokines like IL-4 and IL-13, they secrete anti-inflammatory cytokines (e.g., IL-10) and factors like TGF-β that promote tissue repair and fibroblast activation [11] [9]. A transition to an M2-dominated environment is associated with the fibrotic phase.
Foreign Body Giant Cells (FBGCs) form when macrophages fuse in an attempt to engulf large foreign materials, a process termed "frustrated phagocytosis" [12]. FBGCs persist at the material-tissue interface and secrete large amounts of degradative enzymes and ROS, leading to significant biomaterial deterioration [10] [12]. They also contribute to a pro-fibrotic microenvironment, stimulating fibroblasts and promoting excessive ECM deposition [12].
How do fibroblasts contribute to device failure?
Fibroblasts are recruited to the implant site by signals from macrophages and platelets [11] [9]. Their primary role in FBR is the production and remodeling of the ECM. Upon activation by factors like TGF-β, they differentiate into myofibroblasts, which express α-smooth muscle actin (α-SMA) and possess high contractile activity [9]. The excessive deposition and contraction of dense, cross-linked collagen by myofibroblasts leads to the formation of a fibrotic capsule. This capsule can:
- Isolate the device from its target tissue (e.g., neurons), severely impairing the function of recording or stimulating electrodes [10] [5].
- Contract over time, mechanically stressing both the implant and the surrounding host tissue, potentially leading to device displacement or damage [9].
Troubleshooting Guide: Common Experimental Challenges
Problem 1: Excessive Fibrous Encapsulation
Observed Issue: A thick, dense collagenous capsule forms around the implant, leading to functional isolation.
| Potential Cause | Diagnostic Tips | Mitigation Strategies |
|---|---|---|
| Prolonged M2 macrophage activity & FBGC persistence | Immunostaining for M2 markers (e.g., CD206, Arg1) and FBGCs (multinucleated cells) at the interface. | Modulate macrophage polarization using biomaterial properties (e.g., topography, stiffness) [11]. Consider local delivery of CSF1R inhibitors to disrupt FBGC formation [11] [9]. |
| Sustained TGF-β signaling | Measure TGF-β levels in peri-implant tissue via ELISA. Stain for α-SMA+ myofibroblasts. | Use biomaterials that absorb or sequester TGF-β. Explore small molecule inhibitors of TGF-β signaling pathways. |
| Excessive stiffness mismatch | Characterize the Young's modulus of your material versus the target tissue (e.g., brain ~1 kPa) [13]. | Use softer, more compliant materials like specific polymers (e.g., Polyimide, PDMS) or hydrogels to minimize mechanical activation of fibroblasts [9] [13]. |
Problem 2: Chronic Inflammation and Material Degradation
Observed Issue: Inflammation fails to resolve, and the implant material shows signs of surface degradation, cracking, or leaching.
| Potential Cause | Diagnostic Tips | Mitigation Strategies |
|---|---|---|
| "Frustrated phagocytosis" and persistent M1 activation | Immunostaining for M1 markers (e.g., iNOS), and detecting ROS/LOS production. SEM imaging of material surface. | Design smoother surface topographies or materials that evade protein fouling. Incorporate anti-inflammatory agents (e.g., IL-10) into the material coating [11]. |
| Material toxicity or inappropriate surface chemistry | In vitro cytotoxicity assays (e.g., PC-12 neural cells, NRK-49F fibroblasts) [13]. | Select biocompatible polymers with a proven track record (e.g., Polyimide, Polylactide) and avoid cytotoxic materials like some PEGDA formulations [13]. Functionalize surfaces with immunomodulatory groups [14]. |
Problem 3: Inconsistent FBR in Animal Models
Observed Issue: High variability in the severity of the FBR between subjects in a study.
| Potential Cause | Diagnostic Tips | Mitigation Strategies |
|---|---|---|
| Surgical technique and tissue trauma | Standardize and document surgical procedures meticulously. Monitor for excessive bleeding or infection. | Train all surgeons to a high level of proficiency. Use consistent implantation protocols and tools. |
| Uncontrolled host factors | Use genetically similar animal cohorts. Monitor for pre-existing conditions. | Utilize inbred rodent strains to minimize genetic variability. Ensure animals are of similar age and health status. |
| Material property variability | Characterize material surface properties (roughness, chemistry) between batches. | Implement strict quality control (QC) checks for all fabricated devices and materials. |
Experimental Protocols for Studying FBR
In Vitro Model for Macrophage Fusion and FBGC Formation
This protocol allows for the quantitative study of factors driving macrophage fusion, a key event in the FBR [12].
- Primary Cell Isolation: Isolate CD14+ monocytes from human peripheral blood using density gradient centrifugation and magnetic-activated cell sorting (MACS).
- Macrophage Differentiation: Culture monocytes in RPMI 1640 medium supplemented with 10% FBS and 25-100 ng/mL recombinant human M-CSF for 72 hours to differentiate them into macrophages.
- Fusogenic Stimulation: Replace the medium with fresh medium containing M-CSF and a fusogenic cytokine stimulus, typically IL-4 (10 ng/mL) and/or IL-13 (10 ng/mL).
- Culture and Analysis:
- Culture cells on a permissive substrate (e.g., Polyethylene Terephthalate (PET) films) for up to 28 days, replacing the media every 3-4 days.
- To quantify fusion, fix cells at desired time points and stain with May-Grünwald/Giemsa.
- Image and count nuclei. A Fusion Index can be calculated as: (Number of nuclei within multinucleated cells / Total number of nuclei counted) × 100 [12].
- FBGCs are typically defined as cells containing ≥4 nuclei.
In Vitro Coculture Model for Macrophage-Fibroblast Interactions
This model investigates the paracrine signaling between macrophages and fibroblasts [12].
- Cell Culture:
- Differentiate macrophages from monocytes as described above.
- Culture fibroblasts (e.g., NRK-49F line [13]) in standard DMEM medium.
- Setup:
- Direct Contact: Seed macrophages and fibroblasts together on the material of interest.
- Indirect Contact: Use transwell systems, where one cell type is cultured on a permeable insert and the other in the well below, allowing exchange of soluble factors but preventing physical contact.
- Analysis:
- Collect conditioned media and analyze secreted cytokines (e.g., TGF-β, PDGF, IL-10) using ELISA [12].
- Assess fibroblast activation by immunostaining for markers like α-SMA or by measuring collagen production (e.g., Sirius Red staining).
Key Signaling Pathways and Cellular Crosstalk
The progression of the FBR is governed by complex crosstalk between macrophages and fibroblasts. The diagram below illustrates the core signaling axes and cellular transitions.
Cellular and Molecular Drivers of the Foreign Body Response
A critical mechanical interaction was discovered in fibrillar collagen matrices, where contracting fibroblasts generate long-range deformation fields [15]. Macrophages can sense these mechanical cues from several hundred micrometers away and actively migrate towards the source via α2β1 integrin and stretch-activated channels, independent of chemotaxis [15]. This represents a powerful mechanical crosstalk mechanism that recruits macrophages to sites of active remodeling.
The Scientist's Toolkit: Key Reagents and Materials
The table below lists essential reagents and materials used in FBR research, based on the protocols and studies cited.
| Research Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Recombinant Human M-CSF | Differentiates isolated human monocytes into macrophages in vitro. | Used at 25-100 ng/mL to generate macrophages for fusion assays [12]. |
| Recombinant Human IL-4 / IL-13 | Key cytokines that drive macrophage polarization to an M2 phenotype and promote fusion into FBGCs. | Used at 10 ng/mL each to stimulate FBGC formation on PET films [12]. |
| Polyethylene Terephthalate (PET) | A permissive substrate used in in vitro models to study macrophage adhesion and fusion. | Sterilized PET films (0.1 mm thick) used as a standard surface for FBGC formation studies [12]. |
| TAK-242 (CLI-095) | A potent inhibitor of TLR4 signaling. Used to investigate the role of innate immune activation in macrophage fusion. | Added at 1 µg/mL to cultures to inhibit TLR4 and assess its impact on large FBGC formation [12]. |
| Anti-α-SMA Antibody | Marker for identifying activated myofibroblasts in tissue sections or cell cultures via immunostaining. | Used to quantify the extent of fibroblast-to-myofibroblast transition (FMT) in fibrotic tissue [9]. |
| Polyimide (PI) | A polymer with high biocompatibility for neural interfaces, causing minimal FBR. | Identified in a screen of 10 polymers as showing the highest compatibility with neural and fibroblast cells [13]. |
| PEGDA | A hydrogel material that can elicit a strong FBR, useful as a positive control for fibrosis studies. | Showed cytotoxic effects, low cell adhesion, and strong FBR with fibrosis in comparative studies [13]. |
| CSF1R Inhibitor | Pharmacological agent that blocks the colony-stimulating factor 1 receptor, crucial for macrophage survival and FBGC formation. | In vivo inhibition resulted in reduced fibrous encapsulation and FBGC formation [11] [9]. |
Frequently Asked Questions (FAQs)
Q1: What is the foreign body response (FBR) and why is it a critical issue for bioelectronic implants? The foreign body response (FBR) is a complex, innate immune reaction triggered by the implantation of a medical device. It begins with protein adsorption on the implant surface, followed by a cascade of immune cell recruitment (neutrophils, monocytes, macrophages), chronic inflammation, and the eventual formation of a dense, collagen-rich fibrous capsule that isolates the device [3] [16]. This response is a primary cause of long-term bioelectronic device failure. The fibrous capsule acts as an insulating barrier, severely compromising the device's ability to communicate electrically with the target tissue by increasing impedance at the tissue-device interface [3] [17]. It can also block analyte diffusion for biosensors and impede drug delivery from implantable pumps [3].
Q2: What are the direct functional consequences of the fibrous capsule on my bioelectronic device's performance? The fibrous capsule directly degrades device performance through several mechanisms:
- Increased Interface Impedance: The avascular, collagen-dense capsule electrically insulates the electrode, drastically increasing impedance and weakening signal transmission for both recording and stimulation [3] [17].
- Signal Degradation: For recording electrodes, this results in a decreased signal-to-noise ratio (SNR), making neural signals weaker and harder to resolve. For stimulating devices, more power is required to achieve the same therapeutic effect, which can drain batteries faster and cause tissue damage [6].
- Device Isolation: The capsule can physically displace the device from its intended target, further reducing signal fidelity and stimulation efficiency [3].
Q3: Beyond fibrosis, what other aspects of FBR should I be monitoring in my experiments? While collagen deposition is a key endpoint, a comprehensive assessment should include:
- Immune Cell Infiltration: Monitor the presence and polarization of macrophages. A persistent population of pro-inflammatory M1 macrophages (expressing markers like CCR7) is a driver of chronic inflammation and fibrosis, whereas a transition to anti-inflammatory M2 macrophages is associated with resolution [7] [3] [18].
- Inflammatory Cytokines: Analyze the expression of pro-inflammatory biomarkers such as S100A8/A9, TNF-α, IL-6, and IL-1β in the peri-implant tissue. Their upregulation indicates an active and damaging inflammatory phase of the FBR [7] [18].
- Myofibroblast Activation: The differentiation of fibroblasts into α-Smooth Muscle Actin (α-SMA) positive myofibroblasts is a critical step in the formation of a contractile fibrous capsule, which can mechanically distort both the tissue and the implant [3] [18].
Q4: Are certain implant materials more likely to trigger a severe FBR? Yes, the material's chemical and physical properties fundamentally dictate the severity of the FBR. Historically used rigid materials like metals and silicon (with a Young's modulus in the GPa range) have a significant mechanical mismatch with soft tissues (kPa range), promoting inflammation and fibrosis [6]. Among polymers, materials like PEGDA have been shown to elicit strong FBR, while others like polyimide (PI), polylactide (PLA), and polydimethylsiloxane (PDMS) show better, though not perfect, compatibility [13]. Emerging research focuses on intrinsically immunocompatible materials, such as certain semiconducting polymers and hydrogels, which are designed to minimize immune activation from the outset [7] [18] [19].
Quantitative Data: Documenting the Impact of FBR
The following table summarizes key quantitative findings from recent studies, illustrating the measurable impact of FBR and the efficacy of mitigation strategies.
Table 1: Quantitative Consequences of FBR and Efficacy of Mitigation Strategies
| Metric of Interest | Control / Baseline Material | Performance of Advanced Material / Strategy | Citation |
|---|---|---|---|
| Fibrous Capsule Thickness | PDMS: 45-135 μm (in mice) | EVADE Elastomer (H90): 10-40 μm (in mice) | [7] |
| Collagen Density | Control Semiconducting Polymer: ~25% | Selenophene-based Polymer with TMO side chain: ~8% (68% decrease) | [18] |
| Macrophage Population | Control Semiconducting Polymer (p(g2T-T)): Baseline | Engineered Polymer (p(g2T-Se)-TMO): ~68% decrease | [18] |
| Myofibroblast Population | Control Semiconducting Polymer (p(g2T-T)): Baseline | Engineered Polymer (p(g2T-Se)-TMO): ~79% decrease | [18] |
| Inflammatory Markers (e.g., CCR-7, TNF-α) | PDMS: Baseline (High) | EVADE Elastomer (H90): ~1/6 to 1/8 fold reduction | [7] |
| Impedance at Interface | Conventional non-adhesive interfaces prone to fibrosis | Adhesive Nonfibrotic Bioelectronics (ANB): Stable, low impedance (~0.76 kΩ at 1 kHz) maintained for 12 weeks | [19] |
Experimental Protocols for Assessing FBR
Protocol 1: In Vivo Histological and Immunohistochemical Analysis of the Tissue-Device Interface
This protocol is fundamental for characterizing the cellular and structural components of the FBR to an implanted bioelectronic device.
- 1. Device Implantation: Implant your bioelectronic device subcutaneously or at the target organ (e.g., brain, peripheral nerve) in an appropriate animal model (e.g., mouse, rat, non-human primate). Ensure a sham or a control material (e.g., PDMS, silicon) is implanted in the same animal for a paired comparison to minimize inter-subject variability [7].
- 2. Explanation and Tissue Harvest: At predetermined endpoints (e.g., 1 week for acute inflammation, 4-12 weeks for chronic fibrosis), euthanize the animal and carefully excise the implant with the surrounding tissue envelope intact [7] [13].
- 3. Tissue Fixation and Sectioning: Fix the tissue-device construct in 4% paraformaldehyde (PFA) for 24-48 hours. For stiff implants, careful decalcification may be needed. Embed the tissue in paraffin or optimal cutting temperature (OCT) compound and section it into 5-10 μm thick slices using a microtome or cryostat [13].
- 4. Staining and Imaging:
- H&E Staining: Provides a general overview of tissue structure, inflammatory cell infiltration, and the overall capsule architecture [7] [13].
- Masson's Trichrome Staining: Specifically stains collagen fibers blue, allowing for clear visualization and quantification of the fibrous capsule thickness and density [7] [18] [19].
- Immunofluorescence Staining: Use antibodies to label specific cell types and proteins. Key targets include:
- 5. Image Analysis: Use image analysis software (e.g., ImageJ, Fiji) to quantify capsule thickness, collagen density (via blue pixel density in Masson's Trichrome), and fluorescence intensity for cell counts and marker expression [7] [18].
Protocol 2: Molecular Analysis of Inflammatory Biomarkers
This protocol supplements histology by providing quantitative data on gene and protein expression related to the FBR.
- 1. Tissue Sampling: After explant, carefully dissect the tissue immediately adjacent to the implant interface. Snap-freeze the tissue in liquid nitrogen and store at -80°C [7] [18].
- 2. RNA Extraction and Quantitative PCR (qPCR): Homogenize the tissue, extract total RNA, and synthesize cDNA. Perform qPCR using primers for fibrosis-related genes (e.g., Collagen type I, Collagen type III) and inflammation-related genes (e.g., TNF-α, IL-6, IL-1β) [18]. Normalize data to housekeeping genes (e.g., Gapdh, Actb).
- 3. Protein Analysis (Antibody Array or ELISA): For a broader profiling of inflammatory mediators, use a proteome profiler antibody array to simultaneously detect the relative levels of multiple cytokines and chemokines (e.g., IFN-γ, GM-CSF, MCP-1, IL-23) in the tissue lysate [7] [18]. Alternatively, use Enzyme-Linked Immunosorbent Assays (ELISAs) for quantitative measurement of specific proteins of interest, such as S100A8/A9 [7].
The workflow for these key experimental protocols to assess FBR can be visualized as follows:
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials and Reagents for FBR Research
| Item / Reagent | Function / Application in FBR Research | Examples from Literature |
|---|---|---|
| EVADE Elastomers | A class of intrinsically immunocompatible materials used as the bulk substrate for devices to suppress FBR long-term (≥1 year in mice). | Copolymers of HPEMA and ODA (e.g., H90) [7] |
| Engineered Semiconducting Polymers | Conductive polymers with immunomodulatory backbones (e.g., Selenophene) and side chains (e.g., THP, TMO) for bioelectronics with suppressed FBR. | p(g2T-Se)-TMO, p(g2T-Se)-THP [18] [17] |
| Adhesive Hydrogel Interfaces | Bioadhesive layers (e.g., PVA/PAA-based) that create a conformal, nonfibrotic interface on nerves by preventing immune cell infiltration. | Adhesive Nonfibrotic Bioelectronics (ANB) [19] |
| Anti-CD68 Antibody | An antibody for immunofluorescence staining to identify and quantify macrophage populations in the peri-implant tissue. | Used for macrophage detection in vivo [18] |
| Anti-α-SMA Antibody | An antibody for immunofluorescence staining to identify and quantify activated myofibroblasts, the key collagen-producing cells in fibrosis. | Used for myofibroblast detection in vivo [18] |
| Proteome Profiler Antibody Array | A membrane-based array for simultaneously screening the relative levels of multiple inflammation-related cytokines and chemokines from tissue lysates. | Used to profile cytokines like CCR7, IFN-γ, IL-6 [7] [18] |
| S100A8/A9 Inhibitors | Chemical inhibitors or genetic knockout models used to investigate the specific role of these alarmin proteins in driving the fibrotic cascade. | Used in mechanistic studies to confirm S100A8/A9's role in FBR [7] |
Visualizing the FBR Cascade and Its Impact on Device Function
The core mechanism by which FBR initiates and ultimately compromises device function is summarized in the following diagram:
Implantable medical devices and biomaterials inevitably trigger a complex immune-mediated reaction known as the foreign body response (FBR). This process begins immediately upon implantation with protein adsorption and progresses through acute and chronic inflammation, ultimately resulting in fibrotic encapsulation of the device. The dense collagenous capsule that forms can isolate the implant from surrounding tissue, severely compromising the function of bioelectronic devices by impeding signal transduction, increasing interface impedance, and limiting analyte diffusion [18] [3].
For bioelectronic implants, including neural interfaces and biosensors, this fibrotic barrier presents a significant challenge to long-term performance and stability. Research indicates that approximately 90% of failures in common medical devices can be attributed to FBR, with up to 30% of implanted devices failing during their operational lifespan due to immune-mediated reactions [7]. Understanding how specific material properties initiate and modulate this immune cascade is therefore fundamental to designing next-generation bioelectronics with enhanced longevity and functionality.
Fundamental Principles: How Material Properties Guide Immune Activation
The FBR is not a single event but a carefully orchestrated sequence of immune activities. The initial seconds and minutes after implantation are critical, as the material surface immediately interacts with biological components. The following table summarizes the key stages of this process [3]:
Table 1: The Sequential Stages of the Foreign Body Response
| Stage | Time Frame | Key Cellular Events | Outcome |
|---|---|---|---|
| Protein Adsorption | Seconds to minutes | Adsorption of blood plasma proteins (albumin, fibrinogen) | Protein layer forms on material surface |
| Acute Inflammation | 1-7 days | Neutrophil infiltration, followed by monocytes | Initial immune recognition and response |
| Chronic Inflammation | Up to 3 weeks | Macrophage activation and polarization | Persistent inflammatory environment |
| Foreign Body Giant Cell Formation | Weeks | Fusion of macrophages into FBGCs | Attempt to phagocytose foreign material |
| Fibrous Encapsulation | Weeks to months | Fibroblast activation, myofibroblast differentiation, collagen deposition | Dense, avascular fibrotic capsule formation |
The properties of an implanted material directly influence the intensity and progression of each stage. Surface characteristics determine the identity and conformation of adsorbed proteins, which in turn influence subsequent immune cell behavior. The physical and chemical properties of the implant can either amplify or dampen the resulting immune response, making material design a powerful tool for modulating FBR [3].
Material Properties That Modulate the Immune Response
Chemical Composition and Molecular Design
The fundamental chemistry of implant materials plays a pivotal role in determining immune compatibility. Recent research has identified several promising molecular strategies:
Selenophene-Based Polymer Backbones: Replacing traditional thiophene units with selenophene in semiconducting polymer backbones has demonstrated significant immunomodulatory potential. This approach can reduce collagen density by approximately 50% compared to conventional materials, likely through suppression of macrophage activation and reactive oxygen species (ROS) scavenging [18] [20].
Immunomodulatory Side Chains: Functionalization of polymer side chains with specific immunomodulatory groups, such as triazole-tetrahydropyran (THP) and triazole-thiomorpholine 1,1-dioxide (TMO), can further suppress FBR. When combined with selenophene backbone engineering, this strategy has achieved reductions in collagen density of up to 68% in vivo [18].
Tetrahydropyran-Based Elastomers: New elastomer platforms (termed EVADE) incorporating tetrahydropyran ether-derived methacrylate monomers have demonstrated exceptional long-term immune compatibility, showing negligible inflammation and minimal capsule formation in both rodent and non-human primate models for over one year [7].
Physical and Structural Properties
Physical characteristics of implants significantly influence the degree of FBR, often independently of chemical composition:
Table 2: Physical Properties and Their Impact on FBR
| Property | Effects on FBR | Optimal Characteristics for Reduced FBR |
|---|---|---|
| Surface Topography | Determines protein adsorption density, cell adhesion, and macrophage fusion | Micro/nano-scale patterns that discourage focal adhesion formation |
| Stiffness/Mechanical Properties | Mismatch with surrounding tissue causes micromotion and chronic inflammation | Low modulus materials (0.1-0.5 MPa) matching tissue mechanics |
| Size and Shape | Larger implants with sharp edges trigger stronger responses | Smaller, curved geometries that minimize tissue disturbance |
| Surface Roughness | Macroscale roughness promotes fibrosis, nanoscale may reduce it | Controlled nanoscale topography similar to native tissue |
| Porosity | Dense materials prevent vascular integration | 30-160 μm porosity enhances vascularization and reduces capsule density |
The mechanical mismatch between stiff traditional implants and soft biological tissues creates a persistent inflammatory environment. Research shows that softening materials to match the modulus of target tissues (typically in the 0.1-0.5 MPa range for many applications) significantly reduces chronic inflammation and fibrotic encapsulation [7] [21].
Experimental Protocols for Assessing FBR
In Vivo Implantation and Histological Analysis
Objective: To evaluate the extent of foreign body response elicited by implant materials in a subcutaneous model.
Materials Needed:
- Test material samples (sterilized)
- Control materials (e.g., PDMS, medical-grade titanium)
- Animal model (typically C57BL/6 mice or similar)
- Surgical equipment and anesthesia
- Fixatives (4% paraformaldehyde)
- Histological staining reagents (Masson's Trichrome, H&E)
- Immunofluorescence antibodies (CD68 for macrophages, α-SMA for myofibroblasts)
Procedure:
- Fabricate test materials into standardized discs (typically 5-10mm diameter, 0.5-1mm thickness) with controlled surface properties.
- Sterilize materials using appropriate methods (ethanol, UV, or ethylene oxide).
- Anesthetize animals and perform subcutaneous implantation in dorsal regions, with each animal receiving multiple test materials to control for inter-animal variability.
- After predetermined timepoints (typically 1, 4, and 12 weeks), euthanize animals and explant materials with surrounding tissue.
- Fix tissue samples in 4% PFA for 24 hours, process, and embed in paraffin.
- Section tissues (5-7μm thickness) and perform:
- Masson's Trichrome staining to visualize collagen deposition
- H&E staining for general histology
- Immunofluorescence for immune cell markers (CD68, α-SMA)
- Quantify capsule thickness, cellular density, and collagen density using image analysis software.
- Isolate RNA from peri-implant tissue for qPCR analysis of collagen types I and III, and inflammatory markers [18] [7].
Cytokine and Proteomic Profiling
Objective: To characterize the inflammatory microenvironment surrounding implants.
Procedure:
- Implant test materials as described in Section 4.1.
- After 2-4 weeks, harvest tissue immediately adjacent to implants.
- Homogenize tissues in appropriate lysis buffers with protease inhibitors.
- Analyze inflammatory profiles using:
- Proteome profiler antibody arrays for simultaneous detection of multiple cytokines and chemokines
- ELISA for specific cytokines of interest (e.g., IL-1β, IL-6, TNF-α, IL-10)
- Quantify expression of pro-inflammatory (CCR7, IFN-γ, GM-CSF, MCP-1, IL-23, IL-6, IL-1β) and anti-inflammatory (IL-10, IL-4) biomarkers to determine the balance of immune activation [18] [7].
Functional Assessment in Bioelectronic Devices
Objective: To evaluate the functional impact of FBR on device performance.
Procedure:
- Fabricate OECTs or other bioelectronic devices using test semiconducting polymers.
- Implant devices in relevant anatomical locations (subcutaneous, neural, muscular).
- Monitor electrical performance parameters over time:
- Charge carrier mobility
- Transconductance
- Impedance at the electrode-tissue interface
- Signal-to-noise ratio for recording devices
- Correlate electrical performance metrics with histological outcomes from explanted devices.
- For sensing applications, measure analyte sensitivity and response time chronically to determine how fibrotic encapsulation affects device function [18] [20].
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagents for FBR Investigation
| Reagent/Material | Function/Application | Research Context |
|---|---|---|
| Selenophene-based polymers | Semiconductor with immunomodulatory properties | Backbone engineering for reduced macrophage activation [18] |
| THP (Triazole-tetrahydropyran) | Immunomodulatory side chain | Side-chain functionalization to downregulate inflammatory biomarkers [18] |
| TMO (Triazole-thiomorpholine 1,1-dioxide) | Immunomodulatory side chain | Side-chain functionalization for enhanced FBR suppression [18] |
| EVADE Elastomers | Tetrahydropyran-based immunocompatible materials | Long-term implantable devices with minimal fibrosis [7] |
| Anti-CD68 antibodies | Macrophage identification | Immunofluorescence staining of immune cell infiltration [18] |
| Anti-α-SMA antibodies | Myofibroblast identification | Detection of activated fibroblasts in fibrotic capsule [3] |
| Masson's Trichrome stain | Collagen visualization | Histological assessment of fibrous encapsulation [18] [7] |
| S100A8/A9 inhibitors | Alarmin pathway blockade | Mechanistic studies of fibrosis pathway [7] |
Frequently Asked Questions (FAQs)
Q1: What is the single most important material property for reducing FBR in bioelectronic implants?
While there is no single solution, the mechanical mismatch between implant and tissue is a fundamental driver of FBR. Research consistently shows that matching the elastic modulus of the target tissue (typically 0.1-1 MPa for many soft tissues) significantly reduces chronic inflammation and fibrosis. However, an integrated approach combining appropriate stiffness with immunomodulatory chemistry and topography yields the best outcomes [7] [21].
Q2: How quickly does the foreign body response initiate after implantation?
The FBR cascade begins within seconds to minutes with protein adsorption on the material surface. Neutrophil recruitment peaks within the first 2 days, followed by monocyte infiltration and macrophage differentiation. The chronic inflammatory phase typically lasts about 3 weeks, with fibrous encapsulation becoming evident by 4 weeks and maturing over several months [3].
Q3: Can we completely prevent foreign body response, or only minimize it?
Current evidence suggests that FBR can be significantly minimized but not completely eliminated. Even the most biocompatible materials still initiate some degree of immune recognition. The research goal is to develop materials that steer the immune response toward tolerance and integration rather than attempting to completely evade immune detection [22] [7].
Q4: What are the most promising new strategies for FBR-resistant bioelectronics?
Emerging approaches include: (1) Selenophene-based semiconducting polymers that suppress macrophage activation; (2) Immunomodulatory side chains (THP, TMO) that actively downregulate inflammatory pathways; (3) EVADE-class elastomers enabling long-term implantation without significant fibrosis; and (4) Biomimetic topographies that discourage fibrotic cell adhesion [18] [7] [20].
Q5: How do I determine if my material's FBR performance is improved compared to standards?
Standardized assessment should include: (1) Quantification of capsule thickness and collagen density via histology (Masson's Trichrome); (2) Immune cell profiling (macrophages, myofibroblasts) via immunofluorescence; (3) Cytokine expression analysis of both pro- and anti-inflammatory markers; and (4) Functional assessment in relevant device configurations. A >50% reduction in collagen density with maintained or improved electrical performance indicates significant improvement [18] [7].
Engineering Solutions: Material and Design Strategies to Evade the Immune System
Frequently Asked Questions (FAQs)
Q1: What is the core principle behind using selenophene backbones and immunomodulatory side chains in bioelectronic materials?
The core principle is to intrinsically design the material at a molecular level to actively suppress the foreign body response (FBR), rather than just being passively inert. This two-pronged approach incorporates selenophene into the polymer backbone to mitigate macrophage activation and adds immunomodulatory functional groups (like THP and TMO) to the side chains to downregulate the expression of inflammatory biomarkers. Together, these strategies aim to reduce chronic inflammation and subsequent fibrotic encapsulation, which can impair device function [14] [20] [17].
Q2: What quantitative improvements can be expected from these design strategies?
When implemented in a semiconducting polymer based on p(g2T-T), these immune-compatible designs have demonstrated substantial improvements in key performance metrics, as summarized below [14] [20]:
| Performance Metric | Improvement Achieved | Significance |
|---|---|---|
| Foreign Body Response | Up to 68% reduction in collagen density [14] | Indicates significantly less fibrotic scar tissue formation around the implant. |
| Electrical Performance | Charge-carrier mobility of up to 1.2 cm² V⁻¹ s⁻¹ [14] [20] | Maintains high electrical conductivity necessary for bioelectronic device function. |
| Signal Fidelity | Higher signal amplitudes maintained after 4 weeks of implantation [20] | Ensures chronic recording quality for applications like electrocardiography (ECG). |
Q3: Why is suppressing the foreign body response (FBR) critical for implantable bioelectronics?
The FBR is an immune-mediated reaction that begins with protein adsorption on the implant and culminates in the formation of a dense, avascular collagen capsule. This fibrotic tissue acts as an insulating barrier, impeding intimate contact between the device and the tissue [3] [17]. For bioelectronics, this isolation hinders signal transmission (recording and stimulation), reduces the efficiency of drug delivery, and can ultimately lead to device failure. Mitigating FBR is therefore essential for achieving long-term stability and functionality of implantable devices [14] [3].
Q4: How do these molecular designs affect macrophage behavior?
Macrophages are key immune cells in the FBR cascade. The designed polymers work by suppressing macrophage activation. Comprehensive immunological assays have shown that these materials can downregulate pro-inflammatory biomarkers (often associated with the M1 macrophage phenotype) and upregulate anti-inflammatory biomarkers (associated with the M2 phenotype). This shift in macrophage polarization from a pro-inflammatory to a pro-healing state is a key mechanism for reducing the FBR [14] [20].
Troubleshooting Guides
Issue 1: Inconsistent Foreign Body Response Suppression In Vivo
Potential Causes and Solutions:
- Cause: Variations in polymer synthesis leading to inconsistent incorporation of selenophene or immunomodulatory side chains.
- Solution: Implement rigorous characterization of each polymer batch using techniques like Nuclear Magnetic Resonance (NMR) spectroscopy to confirm molecular structure and ensure batch-to-batch consistency.
- Cause: Mechanical mismatch between the implant and the surrounding soft tissue, which can independently provoke an immune response.
- Solution: Tune the Young's modulus of the final device to better match the tissue (typically in the kPa to low MPa range). This can be achieved by adjusting the polymer composition or formulating it as a soft hydrogel composite [23].
- Cause: Inadequate sterilization of implants prior to surgery, introducing an external source of immune activation.
- Solution: Validate a sterilization protocol (e.g., ethylene oxide gas, sterile filtration) that does not degrade the polymer's electrical or immunomodulatory properties.
Issue 2: Poor Electrical Performance of the Synthesized Polymer
Potential Causes and Solutions:
- Cause: Reduced crystallinity or π-conjugation length due to the incorporation of bulky side-chain groups.
- Solution: Optimize the ratio of immunomodulatory side chains to maintain a balance between biocompatibility and electronic transport. Techniques like grazing-incidence X-ray scattering (GIXS) can be used to assess the solid-state structure and crystallinity [14].
- Cause: Inadequate doping levels, leading to low charge carrier density.
- Solution: Re-optimize the doping process (e.g., using chemical or electrochemical methods) for the new polymer structure to enhance conductivity [23].
Experimental Protocols
Protocol 1: Synthesis of Selenophene-Based Copolymer with Immunomodulatory Side Chains
This protocol outlines the synthesis of a semiconducting polymer with a selenophene backbone and tetrahydropyran (THP) functionalized side chains, adapted from recent literature [14] [7].
1. Reagents and Equipment:
- Monomer A: Selenophene-based dibromide monomer.
- Monomer B: Distannyl-functionalized comonomer bearing tetrahydropyran (THP) protected side chains.
- Catalyst: Tetrakis(triphenylphosphine)palladium(0) (Pd(PPh₃)₄).
- Solvent: Anhydrous toluene and anhydrous dimethylformamide (DMF).
- Reaction Environment: Schlenk line or glovebox for inert atmosphere (Ar/N₂).
- Purification: Methanol, acetone, Soxhlet extraction apparatus.
2. Step-by-Step Procedure: 1. Add Monomer A (0.5 mmol), Monomer B (0.5 mmol), and Pd(PPh₃)₄ (0.02 mmol) to a dry Schlenk tube inside a glovebox. 2. Evacuate and purge the tube with argon three times. 3. Add a 3:1 mixture of degassed anhydrous toluene and DMF (total volume 5 mL). 4. Heat the reaction mixture to 90-110 °C with stirring for 48-72 hours. 5. Allow the mixture to cool to room temperature. 6. Precipitate the polymer by slowly dripping the reaction mixture into vigorously stirred methanol (200 mL). 7. Collect the resulting fibrous solid via filtration. 8. Sequentially purify the polymer using a Soxhlet extractor with methanol (24 h) and acetone (24 h) to remove catalysts and oligomers. 9. Recover the final polymer by dissolving in a minimal amount of chloroform and re-precipitating in methanol. Dry the polymer under vacuum overnight.
Protocol 2: In Vivo Subcutaneous Implantation for FBR Assessment
1. Materials and Preparation:
- Polymer Films: Fabricate thin films of test and control polymers (e.g., thiophene-based analog) of standardized size and shape (e.g., 1x1 cm squares).
- Sterilization: Sterilize all films using ethylene oxide gas or exposure to UV light.
- Animal Model: C57BL/6 mice (8-12 weeks old).
2. Surgical Procedure: 1. Anesthetize the mouse according to your institution's animal care protocol. 2. Shave and disinfect the dorsal area. 3. Make a small midline incision and create subcutaneous pockets on each side of the incision using blunt dissection. 4. Implant one polymer film into each pocket, ensuring the test and control materials are randomized. 5. Close the incision with sutures or wound clips. 6. Administer post-operative analgesics and monitor animals until they fully recover.
3. Explanation and Analysis (After 4 Weeks): 1. Euthanize the animals and carefully excise the implant with the surrounding tissue. 2. Fix the tissue-implant construct in 4% paraformaldehyde for 24-48 hours. 3. Process the tissue for paraffin embedding and sectioning. 4. Perform histological staining: * Masson's Trichrome: To stain collagen fibers (fibrotic capsule) blue. * Hematoxylin & Eosin (H&E): For general tissue morphology and immune cell infiltration. 5. Image the stained sections under a light microscope. 6. Quantify the FBR by measuring the thickness of the collagen capsule (in μm) and the density of collagen around the implant using image analysis software (e.g., ImageJ) [14] [7].
Key Signaling Pathways in Foreign Body Response
The following diagram illustrates the key immune signaling pathways involved in the Foreign Body Response (FBR) and the points where selenophene backbones and immunomodulatory side chains are hypothesized to intervene.
Experimental Workflow for Material Evaluation
The diagram below outlines the core workflow for designing, synthesizing, and evaluating immunomodulatory semiconducting polymers.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and reagents used in the synthesis and evaluation of immunomodulatory semiconducting polymers.
| Item | Function / Role in Research | Example / Specification |
|---|---|---|
| Selenophene Monomers | Forms the core conjugated backbone of the polymer, providing electronic conductivity and intrinsic immunomodulatory properties by mitigating macrophage activation [14] [20]. | e.g., Selenophene-based dibromide or distannyl monomers. |
| Immunomodulatory Monomers | Introduces functional groups (e.g., THP, TMO) into polymer side chains to actively downregulate inflammatory biomarkers and suppress the FBR [14] [7]. | e.g., Monomers with tetrahydropyran (THP) ether groups. |
| Palladium Catalyst | Catalyzes key carbon-carbon coupling reactions (e.g., Stille or Suzuki polymerization) to form the conjugated polymer chain [14]. | e.g., Tetrakis(triphenylphosphine)palladium(0) (Pd(PPh₃)₄). |
| Organic Electrochemical Transistor (OECT) | A standard device architecture for evaluating the electrical performance (e.g., charge carrier mobility, transconductance) of semiconducting polymers in an electrolyte environment, mimicking biological conditions [14] [20]. | Custom-fabricated OECT devices. |
| Masson's Trichrome Stain | A histological stain used to visualize and quantify collagen deposition (fibrotic capsule) around explanted devices [14] [7]. | Standard histological staining kit. |
| Antibodies for Immunohistochemistry | Used to detect and visualize specific immune cell markers (e.g., CCR-7, TNF-α) and activation states in tissue sections surrounding the implant [7]. | e.g., Anti-CCR7, Anti-TNF-α, Anti-IL-6. |
This technical support center is designed for researchers and scientists working to minimize the Foreign Body Response (FBR) in implantable bioelectronics. The FBR—a complex cascade of inflammation, immune cell recruitment, and fibrotic encapsulation—severely compromises the long-term functionality of sensitive devices such as neural interfaces, continuous glucose monitors, and cochlear implants. This resource provides targeted troubleshooting guides, detailed experimental protocols, and FAQs focused on two primary strategies: engineering surface topographies with micro- and nano-scale features and applying non-fouling zwitterionic chemical coatings. The guidance herein is framed within the context of a doctoral thesis, aiming to bridge foundational research and practical, repeatable experimentation.
Troubleshooting Guides: Common Experimental Challenges
Zwitterionic Hydrogel Coating Application
Problem: Inconsistent or Non-Uniform Coating Coverage Observed as patchy coatings or areas where the coating delaminates from the substrate, particularly on complex geometries like electrode arrays.
- Possible Causes & Solutions:
- Cause 1: Incorrect Surface Preparation.
- Solution: Ensure the substrate (e.g., PDMS) is thoroughly cleaned and activated. Use an oxygen plasma treatment immediately prior to coating application to ensure high surface energy and reactivity [24].
- Cause 2: Sub-Optimal Photografting Parameters.
- Cause 3: Inadequate Coating Solution Formulation.
- Solution: Confirm the purity of the zwitterionic monomer (e.g., CBMA) and ensure it is freshly dissolved. Filter the solution to remove any particulates that could cause defects.
- Cause 1: Incorrect Surface Preparation.
Problem: Loss of Anti-Fouling Properties After Implantation The coating appears intact but shows increased protein adsorption or cellular adhesion in in-vivo tests compared to initial in-vitro results.
- Possible Causes & Solutions:
- Cause 1: Hydrogel Degradation or Mechanical Failure.
- Cause 2: Hydrogel Dehydration or Handling Damage.
- Solution: Always store and handle coated devices in an aqueous solution (e.g., PBS) to prevent dehydration-induced cracking. Develop specialized fixtures for implantation to minimize physical contact with the coated surface.
Micro/Nano-Patterning of Substrates
Problem: Poor Cell Adhesion or Misaligned Morphology on Micro-Patterns Mesenchymal Stem Cells (MSCs) or other target cells fail to adhere, or their morphology does not align with the intended topographic cues.
- Possible Causes & Solutions:
- Cause 1: Inadequate Protein Pre-adsorption.
- Solution: Pre-incubate the patterned substrate in cell culture medium or a relevant protein solution (e.g., serum) immediately after oxygen plasma treatment. Surface hydrophilicity and protein adsorption capacity can decay over time when stored in air [26].
- Cause 2: Pattern Dimensions are Non-Optimal.
- Solution: Redesign the pattern based on literature values. For instance, micro-gratings or pillars with an aspect ratio of 1:2 and an interspace of 2 μm have been successfully used to guide MSC orientation and migration [26].
- Cause 3: Contamination of the Pattern.
- Solution: Implement rigorous cleaning protocols post-fabrication, using solvents and techniques that do not damage the delicate micro/nano-features.
- Cause 1: Inadequate Protein Pre-adsorption.
Problem: Insufficient Bactericidal Effect of Nanotopographies Gram-negative (E. coli) or gram-positive (S. aureus) bacteria continue to colonize nanostructured surfaces.
- Possible Causes & Solutions:
- Cause 1: Nanofeature Dimensions are Incorrect.
- Solution: Ensure the nanofeatures (e.g., Moth-Eye nanocones) have sharp tips and a height/spacing that generates sufficient mechanical stress to rupture bacterial membranes upon contact. Features with contact points in the 10–100 nm range are typically required [26].
- Cause 2: Material Stiffness is Too Low.
- Solution: The mechano-bactericidal effect requires the substrate to be sufficiently rigid to prevent deformation when bacteria attach. Consider using hard PDMS (hPDMS) or PMMA instead of soft elastomers for the nanostructured layer [26].
- Cause 1: Nanofeature Dimensions are Incorrect.
Frequently Asked Questions (FAQs)
Q1: What is the primary mechanism by which zwitterionic hydrogels reduce the FBR? A1: Zwitterionic polymers, such as pCBMA, create a dense, highly ordered hydration layer via their paired positive and negative charges. This layer forms a physical and energetic barrier that significantly reduces the initial, non-specific adsorption of proteins (e.g., fibrinogen). Since protein fouling is the first step in the FBR cascade, its suppression leads to reduced macrophage adhesion, foreign body giant cell formation, and ultimately, a thinner fibrotic capsule [25] [24].
Q2: Can surface topography and chemistry strategies be combined? A2: Yes, and this is a leading-edge approach. Hierarchical surfaces that combine microtopographies (to guide host cell integration) with nanotopographies (for bactericidal effects) can be further enhanced with a zwitterionic coating. This multi-scale strategy simultaneously addresses multiple aspects of the FBR: preventing infection, directing desirable cell responses, and minimizing non-specific protein fouling [26].
Q3: How do I validate the in-vivo performance of my modified surface? A3: Beyond standard in-vitro fouling tests, subcutaneous implantation in rodent models is a common and effective validation step. Key quantitative endpoints include:
- Histomorphometry: Measure the fibrotic capsule thickness around the implant after explantation. A successful coating can reduce thickness by 50-70% compared to uncoated controls [25] [24].
- Immunohistochemistry: Stain tissue sections for specific cell markers (e.g., CD68 for macrophages, α-SMA for myofibroblasts) to qualitatively and quantitatively assess the cellular immune response.
- Functional Testing: For drug-delivery devices, measure the transport of a model drug (e.g., insulin) over time to demonstrate that the modification maintains functional efficacy [27].
Q4: My coating is stable in buffer but fails in vivo. What could be wrong? A4: The in-vivo environment is far more challenging. This failure often points to a lack of mechanical durability. The coating may be degrading, or more likely, it is being physically compromised by the compressive and shear forces exerted by the surrounding tissue and immune cells. Solutions include optimizing the cross-linking density and testing the coated device in a simulated biological mechanical environment before moving to in-vivo studies.
The following tables consolidate key quantitative findings from recent literature to aid in experimental design and benchmarking.
Table 1: In-Vivo Performance of Zwitterionic pCBMA Coatings
| Metric | Performance Data | Experimental Conditions | Source |
|---|---|---|---|
| Fibrotic Capsule Thickness Reduction | 50 - 70% | Coated vs. uncoated PDMS sheets & cochlear implants; 6 wk - 1 yr implantation in mice | [25] [24] |
| Effective Cross-linker Composition | 5 - 50 wt% | pCBMA coatings with varying PEGDMA cross-linker; maintained anti-fouling properties | [25] [24] |
| Coating Durability | > 6 months | No degradation or loss of anti-fouling function after subcutaneous implantation | [25] |
Table 2: Design Parameters for Differential Biological Responses via Topography
| Biological Target | Topography Type | Typical Feature Dimensions | Observed Outcome | |
|---|---|---|---|---|
| Bacteria (E. coli, S. aureus) | Moth-Eye (ME) Nanocones | Nanoscale sharp tips (10-100 nm contact points) | Mechano-bactericidal effect; bacteria membrane rupture | [26] |
| Mesenchymal Stem Cells (MSCs) | Low Aspect Ratio (LAR) Micropillars/Gratings | 1:2 aspect ratio (height:diameter), 2 μm interspace | Influenced cell orientation, migration, and enhanced osteogenic marker expression | [26] |
| Combined Strategy | Hierarchical (LAR + ME) | Micro-features (as above) fully covered with ME nanocones | Maintained cytocompatibility with MSCs while retaining bactericidal effect | [26] |
Detailed Experimental Protocols
Protocol: Photografting Zwitterionic Hydrogel onto PDMS
This protocol details the simultaneous photopolymerization and photografting of poly(carboxybetaine methacrylate) - pCBMA onto PDMS substrates, a key methodology for creating durable anti-fouling coatings [24].
I. Materials
- Substrate: Polydimethylsiloxane (PDMS) sheets or device.
- Monomer: (3-([2-(Methacryloyloxy)ethyl]-dimethylammonio)propionate (CBMA).
- Cross-linker: Poly(ethylene glycol) dimethacrylate (PEGDMA, MW 750 Da).
- Photo-initiator: Irgacure 2959.
- Solvent: Deionized water.
- Equipment: UV Light Source (~320–390 nm wavelength), Oxygen Plasma Cleaner, Vacuum Desiccator.
II. Step-by-Step Procedure
- Substrate Preparation: Clean PDMS substrates with sequential sonication in acetone, ethanol, and deionized water. Dry with nitrogen gas.
- Surface Activation: Treat the clean PDMS surfaces with oxygen plasma for 1-2 minutes to generate surface-reactive radicals.
- Coating Solution Preparation: In deionized water, prepare a solution containing:
- 1.0 M CBMA monomer.
- 5-50 wt% PEGDMA cross-linker (relative to monomer).
- 1.0 mM Irgacure 2959 photo-initiator.
- Dissolve completely and degas the solution using a vacuum desiccator to remove oxygen, which inhibits free-radical polymerization.
- Coating Application: Pipette the coating solution onto the activated PDMS surface, ensuring complete coverage.
- Photografting & Polymerization: Immediately place the sample under the UV lamp. Irradiate for 5-10 minutes in an inert atmosphere (e.g., under a nitrogen purge). This step simultaneously grafts the polymer network to the PDMS surface and cross-links the hydrogel.
- Post-Processing: Rinse the coated substrate thoroughly with copious amounts of sterile PBS or deionized water to remove any unreacted monomers and photo-initiator. Store hydrated until use.
III. Validation and QC Checks
- Water Contact Angle: A significant decrease in the contact angle (superhydrophilic surface) indicates successful coating application.
- In-Vitro Fouling Test: Immerse the coated substrate in a solution of fluorescently tagged fibrinogen (1 mg/mL) for 1 hour. Image using fluorescence microscopy. A successful coating will show minimal protein adsorption compared to an uncoated control.
Protocol: Creating Hierarchical Micro-Nano Topographies
This protocol outlines the process for fabricating hierarchical surfaces with micro-gratings/pillars and Moth-Eye nanocones to differentially control MSC and bacterial responses [26].
I. Materials
- Polymers: PMMA or hPDMS (hard PDMS).
- Master Templates: Silicon wafers with patterned micro- and nano-features fabricated via electron-beam or photolithography.
- Equipment: Oxygen Plasma Reactor, Soft Lithography Setup, Spin Coater.
II. Step-by-Step Procedure
- Master Fabrication (or sourcing): Obtain or fabricate a silicon master wafer containing the desired hierarchical negative pattern (e.g., micro-gratings covered with nanoconces).
- Replica Molding:
- For PMMA: Use a thermal nanoimprinting process. Heat the PMMA above its glass transition temperature and press it onto the master wafer under controlled pressure.
- For hPDMS: Mix the hPDMS prepolymer and pour it over the master wafer. Cure at elevated temperature (e.g., 65°C for 1 hour).
- Demolding: Carefully peel the solidified polymer replica from the master wafer.
- Surface Activation for Cell Culture: Immediately before cell seeding, treat the topographic substrates with oxygen plasma for ~1 minute to render them temporarily hydrophilic.
- Protein Pre-conditioning: Without delay, incubate the plasma-treated substrates in the complete cell culture medium for at least 1-5 hours to allow for the formation of a protein conditioning layer that promotes cell adhesion.
III. Validation and QC Checks
- Scanning Electron Microscopy (SEM): Image the fabricated surfaces to verify the fidelity and integrity of the micro- and nano-features.
- Water Contact Angle (WCA): Measure the WCA before and after plasma treatment to confirm increased hydrophilicity.
- Bactericidal Assay: Incubate the substrates with a known concentration of E. coli or S. aureus for several hours, then perform live/dead staining and plate counting to quantify bacterial viability.
Signaling Pathways and Experimental Workflows
Workflow for Coating Development and Validation
This diagram illustrates the end-to-end workflow for developing and validating a zwitterionic surface coating, from initial synthesis to final in-vivo assessment.
Diagram 1: Workflow for developing and validating a surface coating to minimize the Foreign Body Response (FBR), integrating both in-vitro and in-vivo stages.
Host Immune Response and Modification Strategies
This diagram maps the key biological stages of the Foreign Body Response (FBR) and aligns them with the strategic interventions provided by surface modifications.
Diagram 2: The Foreign Body Response cascade and strategic intervention points for surface modifications.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents and Materials for FBR-Mitigating Surface Research
| Category | Item / Reagent | Primary Function in Research | Key Consideration |
|---|---|---|---|
| Zwitterionic Chemistry | Carboxybetaine Methacrylate (CBMA) Monomer | Primary building block for creating ultra-low-fouling hydrogel coatings. | Purity is critical for consistent polymerization and performance. |
| Poly(ethylene glycol) dimethacrylate (PEGDMA) | Cross-linker to create a robust, stable hydrogel network from CBMA. | Molecular weight (e.g., 750 Da) and concentration (5-50 wt%) affect mesh size and stiffness. | |
| Irgacure 2959 | Photo-initiator to generate free radicals for the UV-induced grafting and polymerization process. | Must be soluble in aqueous solutions; concentration impacts initiation rate. | |
| Substrate Materials | Polydimethylsiloxane (PDMS) | A common, biocompatible elastomer used for device housing (e.g., cochlear implants). | Requires surface activation (plasma) for covalent coating attachment. |
| Poly(methyl methacrylate) (PMMA) | A rigid thermoplastic used for creating micro/nano-topographies via nanoimprinting. | Offers high stiffness, which is beneficial for mechano-bactericidal effects. | |
| Biological Assays | Fibrinogen, fluorescently tagged | Model protein for in-vitro anti-fouling validation assays. | A significant reduction in adsorption indicates a successful coating. |
| Primary Macrophages or cell lines (e.g., RAW 264.7) | Used for in-vitro assessment of the cellular inflammatory response. | Look for reduced adhesion and altered morphology on modified surfaces. | |
| Specific Antibodies (e.g., anti-CD68, anti-α-SMA) | For immunohistochemical staining of immune cells and fibroblasts in explanted tissue. | Allows quantification of the FBR in-vivo. |
Technical Support Center: FAQs & Troubleshooting Guides
This technical support center provides practical guidance for researchers developing soft, tissue-like electronics to minimize Foreign Body Response (FBR). The FAQs and protocols below address common experimental challenges within the context of bioelectronics and regenerative engineering.
Frequently Asked Questions (FAQs)
Q1: Why is mechanical mismatch a critical problem in bioelectronic implants? The pronounced mechanical mismatch between rigid conventional implants (e.g., silicon, ~180 GPa) and soft neural tissue (~1–30 kPa) prevents devices from conforming to biological substrates. This leads to physical damage during insertion, exacerbates tissue micromotion, and triggers a severe foreign body response (FBR), resulting in inflammation, glial scar encapsulation, and eventual signal degradation [28] [6].
Q2: What are the primary material strategies for achieving tissue-like softness? Strategies can be categorized into three main approaches:
- Soft Polymers and Elastomers: Use of materials like polydimethylsiloxane (PDMS), polyimide (PI), and thermoplastic polyurethane (TPU) as substrates or encapsulation [28] [13].
- Conductive Composites: Combining soft polymers with conductive fillers like carbon nanotubes, graphene, or conductive polymers (e.g., PEDOT:PSS) to create flexible conductive traces [28] [29].
- Hydrogels: Using hydrogels based on materials such as poly(2-hydroxyethyl methacrylate) (pHEMA), alginate, or gelatin, which closely mimic the hydrated environment of native tissues [3] [30].
Q3: How does surface topography influence the Foreign Body Response? Surface topography at the micro/nano level regulates protein adsorption and immune cell interaction. For instance, engineered surface roughness or specific porosity (e.g., pHEMA scaffolds with 34 μm porosity) can reduce the density of the fibrous capsule, decrease macrophage attachment, and increase local vascularization, thereby mitigating the FBR [3].
Q4: We are experiencing inconsistent cell viability when bioprinting with multiple materials. What could be the cause? Inconsistent viability in multi-material bioprinting often stems from crosslinking incompatibility or handling protocols. Different bioinks have specific, and sometimes conflicting, requirements for temperature, pH, or crosslinking agents. Ensure that the crosslinking method for one material does not adversely affect the cell-laden counterpart and rigorously standardize mixing and handling protocols across all batches [30].
Troubleshooting Common Experimental Issues
Problem 1: Chronic Inflammatory Response and Fibrous Encapsulation In Vivo
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Excessive mechanical stiffness | Measure the elastic modulus of your construct and compare it to the target tissue (typically 1-100 kPa) [29]. | Transition to softer substrates (e.g., PDMS, SEBS) or use ultra-thin, flexible geometric designs (e.g., serpentine wires, mesh structures) to reduce flexural rigidity [28] [29]. |
| Bio-incompatible material surface | Perform in vitro cytotoxicity and cell adhesion assays using relevant cell lines (e.g., neurons, fibroblasts) [13]. | Select polymers with proven biocompatibility (e.g., Polyimide, PDMS) or apply bioactive surface coatings (e.g., with extracellular matrix proteins) to improve integration [28] [13]. |
Problem 2: High Electrode Impedance and Poor Signal-to-Noise Ratio
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Insufficient conductive surface area | Perform electrochemical impedance spectroscopy (EIS) on fabricated electrodes. | Coat metal electrodes (e.g., Pt, Au) with conductive polymers like PEDOT:PSS or polypyrrole (PPy), which significantly reduce impedance and enhance charge injection capacity [28] [29]. |
| Delamination of conductive layer | Inspect the electrode-tissue interface post-explant using electron microscopy. | Improve the adhesion between layers through surface plasma treatment or by using functionalized conductive polymers that bond more strongly to the substrate [29]. |
Experimental Protocols & Methodologies
Protocol 1: In Vitro Biocompatibility and Cytotoxicity Screening of Polymer Substrates
This protocol is adapted from a comparative study of polymer toxicity [13].
1. Objective: To quantitatively evaluate the biocompatibility of polymer materials intended for neural interfaces. 2. Materials:
- Polymers: Test polymer scaffolds (e.g., Polyimide (PI), PDMS, PEGDA, PLA, TPU).
- Cell Lines: Neural model (e.g., PC-12 cell line) and fibroblast model (e.g., NRK-49F cell line).
- Equipment: Cell culture facility, SEM for surface characterization, fluorescence microscope for viability staining. 3. Methodology:
- Scaffold Fabrication: Fabricate polymer samples using consistent methods (e.g., 3D printing, molding). Sterilize all samples prior to cell culture.
- Surface Characterization: Image scaffold surfaces using Scanning Electron Microscopy (SEM) to analyze topography and porosity [13].
- Cell Seeding: Seed cells directly onto the surface of the polymer scaffolds at a standardized density.
- Cell Adhesion & Growth Assessment: After a set period (e.g., 72 hours), fix and stain cells for cytoskeletal markers (e.g., actin) and nuclei. Quantify cell adhesion density and morphological spreading using fluorescence microscopy.
- Cytotoxicity Assay: Assess cell viability using a Live/Dead assay kit. Calculate the ratio of live to dead cells to determine material toxicity [13]. 4. Expected Outcomes:
- High Biocompatibility (e.g., PI, PDMS): High cell adhesion, normal cell morphology, and high percentage of live cells.
- Low Biocompatibility (e.g., PEGDA): Poor cell adhesion, rounded cell morphology, and low cell viability, indicating cytotoxic effects [13].
Protocol 2: Fabrication of a Piezoresistive Hydrogel Sensor Integrated with Engineered Tissue
This protocol summarizes the approach used to create biohybrid constructs with built-in sensing capabilities [30].
1. Objective: To 3D bioprint a stable, conductive sensor hydrogel integrated within a cell-laden tissue construct. 2. Materials:
- Sensor Hydrogel: Polyvinyl Alcohol (PVA), Sodium Alginate (SA), Gellan Gum (GG), and conductive filler (Polypyrrole, PPy).
- Tissue Bioink: Matrigel, collagen, and primary cells (e.g., myoblasts).
- Equipment: Multi-material 3D bioprinter (e.g., BIO X6), conical 22G nozzles, tissue culture incubator. 3. Methodology:
- Pre-Bioprinting:
- Bioink Preparation:
- Sensor Hydrogel: Weigh and mix PVA, SA, GG, and PPy under controlled temperature and stirring to form a homogeneous, printable ink.
- Tissue Bioink: Mix myoblast cell pellet with Matrigel and collagen composite at a predetermined cell density. Keep on ice to prevent premature crosslinking.
- Model Preparation: Write a tailored G-code to define the architecture and spatial distribution of the two materials in the final construct [30].
- Bioink Preparation:
- Bioprinting:
- Aseptically load the two bioinks into separate cartridges.
- Calibrate the printer nozzles with high accuracy (e.g., ±0.1 mm).
- Initiate printing using optimized parameters (pressure, speed, temperature) determined from prior shape fidelity tests [30].
- Post-Bioprinting:
- Crosslinking: Apply appropriate crosslinking strategies (e.g., ionic crosslinking for alginate, thermal gelation for collagen).
- Tissue Maturation: Culture the constructs in growth medium, replacing half the medium daily. For muscle tissue, apply mechanical tension to promote maturation.
- Functional Validation: Test the sensor's performance via mechanoelectrical characterization (e.g., measuring resistance change under strain) and assess tissue viability with Live/Dead staining [30].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Developing Soft Bioelectronics
| Material / Reagent | Function / Application | Key Characteristics |
|---|---|---|
| Polyimide (PI) | Flexible substrate and insulation for neural probes [13]. | Excellent biostability, high mechanical strength, and superior in vitro and in vivo biocompatibility, supporting high cell adhesion [13]. |
| PEDOT:PSS | Conductive polymer coating for electrodes [28] [29]. | Significantly reduces electrode impedance and improves charge injection capacity; can be processed into free-standing films [28]. |
| PDMS | Elastomeric substrate for soft electronics and microfluidics [28] [13]. | High flexibility, biocompatibility, gas permeability, and easy to mold. |
| MXenes (e.g., Ti₃C₂Tₓ) | Conductive 2D material for composites and sensors [31]. | High electrical conductivity, hydrophilic surface, mechanical strength, and biocompatibility; used in wearable sensors and conductive scaffolds [31]. |
| PEGDA | Hydrogel for biofabrication and drug delivery [13]. | Caution: Can exhibit cytotoxic effects and provoke strong FBR; requires careful formulation and testing for long-term implants [13]. |
| Polypyrrole (PPy) | Conductive filler for piezoresistive sensor hydrogels [30]. | Provides stable conductivity in hydrogel composites; less prone to agglomeration compared to carbon black [30]. |
| Matrigel/Collagen | Base for cell-laden bioinks [30]. | Provides a natural, biologically active environment that supports cell proliferation and tissue formation. |
Signaling Pathways and Experimental Workflows
Foreign Body Response Signaling Cascade
In Vitro Biocompatibility Screening Workflow
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: My hydrogel coating is delaminating from the bioelectronic device. What could be the cause? Delamination often results from inadequate surface pretreatment or incorrect crosslinking. Ensure the device surface is thoroughly cleaned and functionalized to promote adhesion. Verify that crosslinking parameters (time, temperature, and initiator concentration) fall within the optimized range for your specific hydrogel formulation.
Q2: The electrical conductivity of my polymer coating is lower than expected. How can I improve it? Low conductivity can stem from several factors:
- Insufficient doping: Confirm that doping agent concentration and incorporation method are correct.
- Structural defects: Ensure polymerization conditions (e.g., temperature, solvent purity, reaction time) are strictly controlled.
- Moisture contamination: Conductive polymers are often hygroscopic; ensure all materials are stored and handled in a dry environment.
Q3: Cell adhesion on my ECM-mimicking coating is poor. What should I check? First, verify the activity and concentration of the bioactive peptides (e.g., RGD). Use a positive control, such as a commercially available coating known to support cell growth, to confirm that your cells are viable and adhesion-competent [32]. Also, check that sterilization methods have not degraded the coating's functional groups.
Q4: I am observing a strong inflammatory response in my in vivo model, contrary to the coating's design. How should I troubleshoot this? A persistent foreign body response indicates that the coating may not be adequately mimicking native tissue. Systematically review these factors:
- Coating uniformity: Ensure the coating is smooth and free of defects that could cause irritation.
- Degradation products: Analyze if the coating is degrading into pro-inflammatory byproducts.
- Control experiments: Confirm that the underlying device itself is not triggering the response by testing an uncoated control [32] [33].
Troubleshooting Guides
Troubleshooting Hydrogel Coating Formation
Unexpected results in hydrogel formation require a systematic approach to identify the variable at fault [32] [33].
| Problem | Possible Cause | Suggested Solution |
|---|---|---|
| Uneven or Brittle Hydrogel | Improper crosslinking (rate too fast) | Reduce initiator concentration or lower crosslinking temperature. |
| Poor Adhesion to Device | Inadequate surface activation | Re-optimize surface pretreatment (e.g., plasma treatment, silanization). |
| Swelling Ratio Too High/Low | Incorrect polymer or crosslinker density | Adjust the monomer-to-crosslinker ratio systematically. |
| Cell Death upon Seeding | Unreact crosslinker residues | Increase post-curing wash steps and test cytotoxicity of leachates. |
Troubleshooting Conductive Polymer Performance
When electrical performance is inadequate, a methodical review of materials and processes is essential.
| Problem | Possible Cause | Suggested Solution |
|---|---|---|
| Low Conductivity | Insufficient doping level; oxidative damage | Increase dopant concentration incrementally; ensure synthesis occurs in an inert atmosphere. |
| Poor Film Homogeneity | Aggregation during deposition; fast solvent evaporation | Switch to a different solvent or adjust spin-coating/printing parameters. |
| Loss of Function In Vivo | Delamination; biofouling | Revisit hydrogel adhesion protocol; consider incorporating anti-fouling agents like PEG. |
Troubleshooting ECM-Mimicking Coatings
For coatings designed to control cellular interaction, consistency and bioactivity are paramount.
| Problem | Possible Cause | Suggested Solution |
|---|---|---|
| Low Cell Adhesion | Bioactive ligand denaturation; low density | Source fresh ligands; confirm ligand coupling efficiency via spectroscopy. |
| Inconsistent Coating Thickness | Unoptimized deposition technique | Standardize the deposition method (e.g., dip-coater speed, spray parameters). |
| Unexpected Differentiation | Unintended signaling from coating | Profile the coated surface for other adsorbing proteins; use a more specific ligand. |
Detailed Experimental Protocols
Protocol: Fabrication of a Minimally Inflammatory Hydrogel Coating
This protocol describes the formation of a bio-inert, crosslinked hydrogel coating on a bioelectronic device to minimize the Foreign Body Response (FBR).
1. Materials
- Device Substrate: (e.g., platinum-iridium electrode).
- Hydrogel Precursors: (e.g., Poly(ethylene glycol) diacrylate (PEGDA)).
- Crosslinker: (e.g., Ammonium persulfate (APS) and Tetramethylethylenediamine (TEMED)).
- Surface Primer: (e.g., (3-Aminopropyl)triethoxysilane (APTES)).
- Buffers: Phosphate Buffered Saline (PBS), pH 7.4.
2. Methodology
- Step 1: Surface Pretreatment. Clean the device substrate with oxygen plasma for 5 minutes at 100W. Immediately immerse in a 2% (v/v) solution of APTES in ethanol for 1 hour to functionalize the surface with amine groups. Rinse thoroughly with ethanol and dry under a stream of nitrogen.
- Step 2: Hydrogel Solution Preparation. Prepare a 20% (w/v) solution of PEGDA in degassed PBS. To this, add the crosslinking initiators APS and TEMED to final concentrations of 1% (w/v) and 0.1% (v/v), respectively. Mix gently but thoroughly. Critical: Work quickly once initiators are added.
- Step 3: Coating and Crosslinking. Pipette the hydrogel solution onto the pretreated device surface. Use a spin coater at 2000 rpm for 30 seconds to achieve a uniform layer. Allow crosslinking to proceed for 30 minutes at room temperature in a humidified chamber.
- Step 4: Post-processing and Sterilization. Immerse the coated device in sterile PBS for 48 hours, changing the buffer every 12 hours, to remove any unreacted monomers. Sterilize the final product using low-temperature ethylene oxide gas or exposure to 70% ethanol, ensuring compatibility with the hydrogel.
3. Controls and Validation
- Positive Control for FBR: An uncoated device implant.
- Negative Control for Biocompatibility: A device coated with a known biocompatible hydrogel (e.g., from a commercial source).
- Validation: Perform quantitative histology at the implant-tissue interface 2 and 4 weeks post-implantation to measure capsule thickness and immune cell density (e.g., CD68+ macrophages).
Experimental Workflow and Signaling Pathways
Hydrogel Coating and FBR Minimization Workflow
Key Signaling Pathways in the Foreign Body Response
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and reagents for developing advanced biointerfaces, with a focus on minimizing the Foreign Body Response.
| Item | Function & Rationale |
|---|---|
| Poly(ethylene glycol) (PEG) | A bio-inert polymer used as a backbone for hydrogels; resists non-specific protein adsorption, a critical first step in mitigating the Foreign Body Response (FBR). |
| Conductive Polymers (PEDOT:PSS) | Provides electrical conductivity for device functionality while being more biocompatible than traditional metals; can be blended with hydrogels to create conductive composites. |
| RGD Peptide | A classic cell-adhesive peptide (Arg-Gly-Asp) grafted onto coatings to promote specific integrin-mediated cell adhesion, improving integration and reducing inflammation. |
| Anti-inflammatory Agents (e.g., Dexamethasone) | Pharmacological agents that can be incorporated into coatings for localized, controlled release to suppress the immune response at the implant-tissue interface. |
| Silane Coupling Agents (e.g., APTES) | Molecules used to functionalize inorganic device surfaces (e.g., metals, oxides) with chemical groups (e.g., amines) that enable strong bonding of polymer coatings. |
| Matrix Metalloproteinase (MMP) Cleavable Peptides | Crosslinkers that allow the hydrogel coating to be remodeled and degraded by cell-secreted enzymes, facilitating integration and reducing mechanical mismatch. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What does "EVADE" stand for and what is its primary purpose? EVADE stands for Easy-to-synthesize Vinyl-based Anti-FBR Dense Elastomers. Its primary purpose is to serve as a platform of immunocompatible elastomers that intrinsically resist the Foreign Body Response (FBR), thereby enhancing the longevity and performance of implantable medical devices [7].
Q2: My EVADE elastomer has low fracture strain and high modulus. How can I adjust its mechanical properties? The mechanical properties of EVADE elastomers are highly tunable by modifying the monomer ratio. A high content of the HPEMA monomer (e.g., H90) results in high fracture tensile strains of 500% or beyond and a low tensile modulus (0.1–0.5 MPa). If your formulation is too stiff (like H100), consider increasing the mole fraction of HPEMA. Alternatively, adding a tiny amount (less than 1 wt%) of a chemical crosslinker like ethylene glycol dimethacrylate (EGDMA) can dramatically increase the modulus and fracture stress, though at the expense of decreased fracture strain [7].
Q3: The fibrotic capsule thickness in my mouse model is highly variable. Is this normal and how can I improve the experiment? Yes, notable inter-mouse variability in capsule thickness is a common challenge, as noted in the original EVADE study [7]. To minimize undesired influences and ensure your results are material-specific, control the following factors:
- Mechanical Properties: Adjust the modulus of your control materials (e.g., PDMS) to be similar to your EVADE samples.
- Surface Topology, Size, and Shape: Ensure all sample discs have identical surface topology, size, and shape.
- In-Animal Controls: Implant all test and control samples in the same animal to directly compare performance under identical biological conditions.
Q4: Beyond EVADE, what other molecular strategies are being explored for intrinsic anti-FBR properties? Recent research has identified other promising molecular design strategies to imbue materials with intrinsic immunocompatibility:
- Selenophene Backbones: Incorporating selenophene into the backbone of semiconducting polymers can mitigate FBR by suppressing macrophage activation [18].
- Immunomodulatory Side-Chains: Functionalizing polymer side chains with groups like triazole-tetrahydropyran (THP) or triazole-thiomorpholine 1,1-dioxide (TMO) can downregulate inflammatory biomarkers [18].
- Bio-inspired Polymers: Materials like poly-DL-serine (PSer) hydrogels, inspired by low-immunogenic silk sericin, have demonstrated exceptional anti-FBR performance, surpassing even poly(ethylene glycol) (PEG) hydrogels [34].
Troubleshooting Common Experimental Challenges
Problem: Inconsistent results in subcutaneous implantation models.
- Potential Cause 1: Inadequate control of material physical properties.
- Solution: Fully characterize and match the mechanical properties (modulus, fracture strain) and physical dimensions of test and control samples before implantation. Refer to the "Key Material Properties Table" for target values.
- Potential Cause 2: Variability in the surgical implantation procedure or animal model.
- Solution: Standardize the surgical protocol, including incision site, pocket creation, and insertion technique. Use a sample size that accounts for inter-animal variability.
Problem: The synthesized elastomer lacks sufficient elasticity.
- Potential Cause: Insufficient physical cross-linking domains due to low octadecyl acrylate (ODA) content or inadequate formation of crystalline phases.
- Solution: Ensure the ODA co-monomer is included in your synthesis. The long alkyl chains of ODA form microcrystals that act as physical crosslinks. Characterize the material using X-ray diffraction (XRD) to confirm the presence of a crystalline phase [7].
Experimental Protocols & Data
Detailed Methodology: Synthesis and Characterization of EVADE Elastomers
1. Monomer Synthesis:
- Synthesize the key monomer, 2-((tetrahydro-2H-pyran-2-yl)oxy)ethyl methacrylate (HPEMA) [7].
- Acquire the co-monomer, octadecyl acrylate (ODA).
2. Copolymerization:
- Perform free radical bulk polymerization of HPEMA and ODA.
- The copolymers are designated based on the mole fraction of HPEMA. For example, a copolymer with 90 mol% HPEMA and 10 mol% ODA is designated as H90 [7].
3. Material Characterization:
- Mechanical Testing: Perform tensile tests to determine fracture strain, fracture stress, and tensile modulus. Conduct cyclic tensile tests to evaluate elastomeric behavior and hysteresis [7].
- Structural Analysis: Use X-ray diffraction (XRD) to confirm the formation of a crystalline phase from the ODA units, which is critical for physical cross-linking [7].
- Thermal Analysis: Determine the glass transition temperature (Tg) using Differential Scanning Calorimetry (DSC).
4. In Vitro Biocompatibility Assessment:
- Conduct cytotoxicity measurements per ISO 10993-5 standards using extracts from the elastomers. The EVADE materials have shown no cytotoxicity [7].
5. In Vivo FBR Evaluation (Subcutaneous Implantation):
- Sample Preparation: Fabricate material discs with controlled modulus, surface topology, size, and shape.
- Animal Model: Utilize C57BL/6 mice. Implant test and control materials (e.g., PDMS, TPU) subcutaneously in the same animal to serve as an internal control.
- Duration: Explain studies for acute inflammation (e.g., 2 weeks) and long-term fibrotic encapsulation (e.g., 1 month, 1 year).
- Histological Analysis:
- Harvest implants with surrounding tissue at designated time points.
- Process and embed tissue for sectioning and staining.
- Perform Masson's Trichrome staining to visualize and quantify collagenous fibrous capsule thickness.
- Perform H&E staining for general histology.
- Perform immunohistochemical staining for pro-inflammatory markers (e.g., CCR-7, TNF-α, IL-6) and anti-inflammatory markers (e.g., IL-10) [7].
- Proteomic Analysis: Use proteome profiler antibody arrays to quantify multiple inflammation-related cytokines and chemokines in tissues adjacent to the implants [7].
Key Material Properties and In Vivo Performance
Table 1: Mechanical Properties of EVADE Elastomers
| Material Designation | HPEMA (mol%) | ODA (mol%) | Fracture Strain (%) | Tensile Modulus (MPa) | Fracture Stress (MPa) |
|---|---|---|---|---|---|
| H100 | 100 | 0 | Low (Glassier) | High | Low |
| H90 | 90 | 10 | >500 | ~0.21 | 0.8 - 2.5 |
| H70 | 70 | 30 | >500 | 0.1 - 0.5 | 0.8 - 2.5 |
| H60 | 60 | 40 | >500 | 0.1 - 0.5 | 0.8 - 2.5 |
| H50 | 50 | 50 | >500 | 0.1 - 0.5 | 0.8 - 2.5 |
Table 2: In Vivo Fibrotic Capsule Thickness Comparison After 1 Month
| Implant Material | Average Capsule Thickness (μm) | Key Findings |
|---|---|---|
| PDMS (Control) | 45 - 135 | Significant fibrotic encapsulation observed [7] |
| EVADE (H90) | 10 - 40 | Significantly thinner capsule than PDMS in the same animal [7] |
| Polyethylene (EMA) | 35 - 160 | All common polymers triggered thicker capsules than H90 [7] |
| Polyurethane (TPU) | 35 - 160 | All common polymers triggered thicker capsules than H90 [7] |
| Polyamide (PA) | 35 - 160 | All common polymers triggered thicker capsules than H90 [7] |
Table 3: Research Reagent Solutions
| Reagent/Material | Function in Experiment | Key Notes |
|---|---|---|
| HPEMA Monomer | Main constituent providing immunomodulatory properties | Imparts tetrahydropyran ether group, which is key to anti-FBR effect [7] |
| Octadecyl Acrylate (ODA) Monomer | Co-monomer forming physical cross-linking domains | Long alkyl chain forms microcrystals, enabling elasticity without chemical crosslinkers [7] |
| Ethylene Glycol Dimethacrylate (EGDMA) | Chemical Crosslinker | Use at <1 wt% to finely tune and increase modulus; decreases fracture strain [7] |
| Polydimethylsiloxane (PDMS) | Control Material | A common medical elastomer; adjust modulus to match test samples for fair comparison [7] |
| Masson's Trichrome Stain | Histological Staining | Visualizes collagen (blue) in fibrous capsule for thickness quantification [7] |
| Anti-CCR7, TNF-α, IL-6 Antibodies | Immunohistochemistry | Labels pro-inflammatory macrophages and cytokines to quantify acute inflammation [7] |
Signaling Pathways and Experimental Workflows
EVADE Material Development and Testing Pipeline
FBR Mechanism and EVADE Intervention Points
Optimizing Bioelectronic Integration: Troubleshooting Persistent FBR Challenges
Addressing Frustrated Phagocytosis and Macrophage Polarization
Frequently Asked Questions (FAQs)
What is the foreign body response (FBR) and why is it a problem for bioelectronics? The foreign body response is an immune-mediated reaction to implanted materials. For bioelectronics, this response is critical because it typically ends with the implant being encapsulated by a dense collagenous scar tissue [18]. This fibrotic capsule acts as an insulating layer, increasing the interface impedance between the device and the tissue, which degrades the quality of recorded signals and the efficiency of electrical stimulation over time [35] [18]. This limits the functional longevity and reliability of implantable devices like pacemakers, neural interfaces, and drug delivery systems.
What is the role of macrophage polarization in the foreign body response? Macrophages are central players in the FBR. Their high plasticity allows them to differentiate into various phenotypes in response to signals from the implant microenvironment [36] [37].
- Pro-inflammatory (M1) Macrophages: These are often activated by damage signals and are highly phagocytic. They release pro-inflammatory cytokines (e.g., IL-1β, TNF-α, IL-6) and reactive oxygen species (ROS) [36] [38]. While this initial inflammatory phase is part of normal wound healing, its persistent activation by an implant can drive chronic inflammation.
- Pro-healing/Anti-inflammatory (M2) Macrophages: Induced by signals like IL-4 and IL-13, these macrophages are associated with tissue repair and the resolution of inflammation. They produce anti-inflammatory cytokines (e.g., IL-10) and pro-fibrotic factors like TGF-β, which can ultimately lead to collagen deposition and fibrosis around the implant [36] [38]. The inability of macrophages to phagocytose large implants leads to "frustrated phagocytosis," which can trigger the fusion of macrophages into foreign body giant cells (FBGCs), a hallmark of the FBR that sustains inflammation and tissue damage [39] [18].
How can we design bioelectronic materials to minimize the FBR? Recent strategies focus on creating immune-compatible materials through molecular design:
- Backbone Engineering: Incorporating specific chemical groups, such as selenophene, into the backbone of semiconducting polymers has been shown to mitigate FBR by suppressing macrophage activation, potentially through scavenging reactive oxygen species (ROS) [18].
- Side-Chain Functionalization: Attaching immunomodulatory groups like triazole-tetrahydropyran (THP) and triazole-thiomorpholine 1,1-dioxide (TMO) to polymer side chains can actively downregulate pro-inflammatory biomarkers and further decrease collagen deposition [18].
- Mechanical Properties: Designing devices with tissue-like softness and flexibility reduces mechanical mismatch, which also helps to suppress inflammatory responses [6].
Troubleshooting Guides
Problem: Excessive Fibrosis Around Implant
Potential Causes and Solutions:
| Potential Cause | Diagnostic Experiments | Solution and Mitigation Strategies |
|---|---|---|
| Persistent M1 Inflammation | • Measure pro-inflammatory biomarkers (e.g., IFN-γ, IL-6, IL-1β) via PCR or cytokine array [18].• Perform immunofluorescence staining for M1 markers (e.g., CCR7, iNOS) [18] [38]. | • Utilize materials with intrinsic immunomodulatory properties (e.g., selenophene-based polymers) [18].• Apply anti-fouling surface coatings (e.g., PEG, zwitterionic materials) to reduce initial protein adsorption [38]. |
| Dominant M2-driven Fibrosis | • Quantify collagen deposition via Masson's Trichrome staining or PCR for collagen types I and III [18].• Stain for myofibroblasts (α-SMA) and M2 macrophages (CD206, CD163) [18] [38]. | • Explore material designs that promote a balanced macrophage response rather than a strong M2 skew [38].• Consider localized delivery of agents that modulate TGF-β signaling to limit fibroblast activation. |
| Mechanical Mismatch | • Characterize the stiffness (Young's modulus) of your implant material. | • Use flexible and soft substrates that better match the mechanical properties of the target tissue (e.g., soft conductive polymers) [6]. |
Problem: Inconsistent Polarization Assays In Vitro
Potential Causes and Solutions:
| Potential Cause | Diagnostic Experiments | Solution and Mitigation Strategies |
|---|---|---|
| Inadequate Polarization Stimuli | • Validate cytokine activity and concentration. Check cell surface receptor expression. | • Use well-established, high-purity cytokines at standard concentrations (e.g., 20-100 ng/mL IFN-γ + LPS for M1; 20-50 ng/mL IL-4/IL-13 for M2) [36] [37]. Include a positive control for each phenotype. |
| Impure or Uncharacterized Cell Population | • Use flow cytometry to check for the presence of other immune cells (e.g., lymphocytes, neutrophils). | • Use well-defined cell lines (e.g., THP-1 with PMA differentiation) or highly pure primary macrophages (e.g., bone marrow-derived macrophages) [39]. |
| Using a Single Marker for Phenotype | • Analyze a panel of multiple M1 and M2 markers (surface and transcriptional) simultaneously. | • Do not rely on a single marker. Use a combination of markers (e.g., for M1: CD80, CD86, iNOS; for M2a: CD206, CD209, Arg1) to confirm polarization [36] [38] [37]. |
The following table summarizes key quantitative findings from recent research on material strategies to suppress the Foreign Body Response.
Table 1: Quantitative Efficacy of Immune-Compatible Polymer Designs In Vivo
| Polymer Design | Key Modification | % Reduction in Collagen Density (vs. Control) | % Reduction in Macrophages (CD68+ cells) | Key Biomarker Changes |
|---|---|---|---|---|
| p(g2T-Se) [18] | Selenophene in backbone | ~50% | Information Missing | Downregulation of pro-inflammatory markers (CCR7, IFN-γ, IL-6, etc.) [18] |
| p(g2T-Se)-THP [18] | Selenophene + THP side chain | ~69% | Information Missing | Further downregulation of pro-inflammatory markers; Upregulation of IL-10 [18] |
| p(g2T-Se)-TMO [18] | Selenophene + TMO side chain | ~72% | ~68% | Strongest downregulation of pro-inflammatory markers; Upregulation of IL-10 and IL-4 [18] |
| Selenophene-based + other strategies [35] | Selenophene backbone & immunomodulatory side chains | Up to 68% (average) | Information Missing | Improved electrical signal amplitude (ECG/EMG) after 4 weeks in vivo [35] |
Table 2: Common Macrophage Phenotypes and Their Markers
| Phenotype | Inducing Stimuli | Characteristic Surface Markers | Secreted Factors | Primary Functions in FBR |
|---|---|---|---|---|
| M1 (Classical) [36] [38] [37] | IFN-γ, LPS, TNF-α | CD80, CD86, MHC-II, TLR4 | IL-1β, IL-6, IL-12, TNF-α, ROS, NO | Initiation of inflammation, pathogen clearance, antigen presentation. |
| M2a (Alternative) [36] [38] | IL-4, IL-13 | CD206, CD209, CD163 | IGF, TGF-β, Fibronectin, CCL17, CCL18 | Tissue repair, fibrosis, debris clearance, constructive remodeling. |
| M2c (Acquired deactivation) [36] | IL-10, TGF-β, Glucocorticoids | CD163, CD206 | IL-10, TGF-β, CCL16 | Immunoregulation, matrix deposition, tissue remodeling. |
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Application in FBR Research |
|---|---|
| Selenophene-based conjugated polymers [18] | Semiconducting materials with intrinsic immunomodulatory properties for constructing bioelectronic interfaces that suppress FBR. |
| THP and TMO functional groups [18] | Immunomodulatory moieties for covalent attachment to polymer side chains to actively downregulate inflammatory responses. |
| Anti-CD68 antibody [18] | Immunofluorescence staining for general macrophage identification in tissue sections. |
| Anti-α-SMA antibody [18] | Immunofluorescence staining for identifying activated myofibroblasts, the primary collagen-producing cells in fibrosis. |
| Recombinant IL-4 and IL-13 [36] [37] | Cytokines used for in vitro polarization of macrophages towards an M2 phenotype. |
| Recombinant IFN-γ and LPS [36] [37] | Stimuli used for in vitro polarization of macrophages towards an M1 phenotype. |
| Masson's Trichrome Stain [18] | Histological technique to visualize and quantify collagen deposition (fibrosis) around implants. |
Signaling Pathways and Experimental Workflows
Mitigating Mechanical Mismatch and Chronic Micromotion
Troubleshooting Guide: Frequent Challenges and Solutions
FAQ 1: What are the primary causes of chronic recording failure in implantable neural electrodes?
Chronic recording failure is primarily driven by the biological foreign body response (FBR) and material failure, both of which are exacerbated by mechanical mismatch and chronic micromotion.
- Biological Failure (Foreign Body Reaction): The immune system recognizes the implant as a foreign body, triggering a cascade that leads to glial scar formation. This scar, composed of reactive astrocytes and other cells, forms a physical barrier that pushes neurons away from the recording sites, degrading the signal-to-noise ratio over time [40] [41].
- Material Failure: Mechanical strain from micromotion can cause physical damage to the electrode itself. Finite Element Modeling (FEM) shows that strain concentrates at the interfaces between different materials (e.g., iridium and silicon) and on small protrusions like electrical traces, leading to cracking, delamination, or other structural failures [42].
- Key Driver: The mechanical mismatch between rigid implant materials (e.g., silicon, Young's modulus of ~200 GPa) and soft brain tissue (Young's modulus of ~1-6 kPa) means that natural brain micromotion (up to 40 µm in rats) causes persistent strain and inflammation at the device-tissue interface [43] [44].
FAQ 2: How can I experimentally measure the strain induced by an implant in neural tissue?
A standard method is to use Finite Element Modeling (FEM) to simulate the mechanical environment. The protocol below is adapted from chronic implantation studies [42]:
- Model Development: Create a 3D model of your probe in simulation software (e.g., ANSYS). Accurately define the geometry, including substrate, conductive traces, insulation, and recording sites.
- Material Assignment: Input the mechanical properties (Young's modulus, Poisson's ratio) for all materials. For brain tissue, use a modulus of ~6 kPa and a Poisson's ratio of 0.45.
- Boundary Conditions and Loading: Fix the bottom surface of a modeled brain phantom. Apply a displacement (e.g., 1 µm) to the probe tip in both the thickness and width directions to simulate brain micromotion.
- Analysis: Solve for the von Mises Equivalent Elastic Strain, which represents the combined effective strain. The results will show areas of concentrated strain on the probe and in the surrounding tissue, highlighting vulnerable design points [42].
FAQ 3: My flexible electrodes buckle during insertion. What are the available solutions?
Buckling occurs because the critical buckling force is proportional to the microelectrode's bending stiffness. Several aiding strategies have been developed [44]:
- Bending Stiffness Modification: Use a biodegradable polymer (e.g., polyethylene glycol, sucrose) as a temporary stiffening shuttle that dissolves after implantation, leaving the flexible electrode in place [43] [44].
- Effective Length Reduction: Utilize a microdrive to slowly advance the electrode, effectively reducing the unsupported length (L) during insertion, which significantly increases the force required for buckling according to Euler's formula [44].
- Utilizing a Magnetic Field: Guide a magnetic microelectrode into position using an externally applied magnetic field, a contactless method that avoids axial compression forces [44].
FAQ 4: What material strategies are most effective for reducing the Foreign Body Response?
The most promising strategies involve softening the device and incorporating immunomodulatory chemistry.
- Mechanical Matching: Coating rigid probes with soft, compliant hydrogels (e.g., PEG-based) that closely match the modulus of brain tissue has been shown to significantly reduce local strain and glial scar formation in vivo [43].
- Immunomodulatory Materials: New semiconducting polymers can be designed with inherent immune-compatible properties. For instance, incorporating selenophene into the polymer backbone and immunomodulatory side chains (e.g., THP, TMO) can suppress macrophage activation and reduce collagen deposition (a key marker of FBR) by up to 68% [18] [35].
FAQ 5: Are there any trade-offs when using softer, more compliant materials?
Yes, the primary trade-off involves device size and handling.
- Size vs. Mechanics: While a soft hydrogel coating improves mechanical matching, it also increases the overall diameter of the implant. Research shows that increasing implant diameter alone can independently increase scarring, macrophage activation, and local blood-brain barrier permeability [43]. Therefore, design must balance the mechanical benefit against the geometric cost.
- Insertion Challenges: Softer materials have a lower bending stiffness, making them prone to buckling during implantation, which necessitates the use of insertion aids as described in FAQ 3 [44].
Data Tables for Material and Strategy Comparison
Table 1: Mechanical Properties of Common Neural Implant Materials
| Material | Young's Modulus | Key Advantages | Key Disadvantages / Trade-offs |
|---|---|---|---|
| Brain Tissue | 1 - 6 kPa [43] [41] | Native mechanical environment | - |
| PEG Hydrogel | ~ 1 - 10 MPa [43] | Excellent mechanical matching, reduces strain & scarring | Increases overall device diameter, may swell [43] |
| Thiol-ene Polymer | ~ 35 MPa (softened) [41] | Softens in vivo, low swelling, lithography-compatible | Softer than brain tissue, can increase immune activation if too large [41] |
| Silicon | ~ 200 GPa [42] [40] | Easily microfabricated, high strength | Large mechanical mismatch, focuses strain [42] |
| Iridium | 528 GPa [42] | Excellent conductor for recording sites | High stiffness creates strain concentration at interfaces [42] |
Table 2: Quantitative Performance of FBR-Mitigation Strategies
| Strategy | Key Metric | Result | Reference |
|---|---|---|---|
| Selenophene-based Polymer | Collagen Density (vs. control) | ~50% decrease [18] | [18] |
| PEG-DMA Hydrogel Coating | Glial Scarring (vs. rigid glass) | Significantly reduced [43] | [43] |
| Immunomodulatory Side Chain (TMO) | Macrophage Population (vs. control) | ~68% decrease [18] | [18] |
| Softening Thiol-ene Probe | Blood-Brain Barrier Disruption | Increased (in acute phase, for a specific design) [41] | [41] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Investigating Mechanical Mismatch
| Item | Function / Application |
|---|---|
| Polyethylene Glycol Dimethacrylate (PEG-DMA) | A hydrogel precursor used to create soft, tissue-matching coatings on neural probes to mitigate strain from micromotion [43]. |
| 3-(Trichlorosilyl)propyl methacrylate (TPM) | A silane used to functionalize glass or silicon surfaces, providing methacrylate groups for covalent bonding of hydrogel coatings [43]. |
| Selenophene-containing Semiconducting Polymers | Conductive polymers for bioelectronics. The selenophene backbone provides immunomodulatory effects, suppressing the foreign body response [18]. |
| Finite Element Analysis Software (e.g., ANSYS) | Used to build computational models simulating the mechanical strain on implants and surrounding tissue under micromotion conditions [42]. |
| Polyimide | A polymer with high biocompatibility and flexibility, often used as an insulating substrate or coating for flexible neural probes [13]. |
Experimental Protocols and Workflows
Protocol 1: Evaluating the Foreign Body Response to Implanted Materials In Vivo
This protocol is used to compare the biocompatibility of different materials, such as polymers or coated electrodes [13] [18].
- Sample Preparation: Fabricate sterile experimental scaffolds or functional probes of a standardized size and shape.
- Animal Implantation: Implant the samples into the target tissue (e.g., visual cortex of mice or rats) using aseptic surgical techniques.
- Chronic Timeline: Allow the implants to remain in situ for the desired chronic period (e.g., 4 weeks for fibrotic capsule formation).
- Perfusion and Histology: At the endpoint, perfuse the animal and extract the brain. Section the tissue containing the implant and perform immunohistochemical staining.
- Key Markers and Analysis:
- Neuronal Density: Stain for NeuN to quantify viable neurons at various distances from the implant [41].
- Glial Scar: Stain for GFAP to visualize and measure the thickness of the reactive astrocyte sheath [40] [41].
- Immune Activation: Stain for CD68 to identify activated microglia and macrophages [18] [41].
- Fibrosis: Use stains like Masson's Trichrome or quantify Collagen I/III mRNA to measure fibrotic capsule formation [18].
Protocol 2: Forming and Characterizing a Mechanically-Matched Hydrogel Coating
This protocol details the application of a soft PEG hydrogel coating to a neural probe [43].
- Substrate Functionalization:
- Clean the probe (e.g., glass capillary) in piranha solution.
- Treat the probe with a solution of TPM in heptane-CCl₄ to covalently attach methacrylate functional groups to the surface.
- Hydrogel Precursor Preparation: Dissolve PEG-DMA (e.g., 5-20% w/v) in water with a photo-initiator (e.g., 0.5% w/v Irgacure 2959).
- Coating Formation:
- Place the functionalized probe into a cylindrical glass mold.
- Fill the mold with the precursor solution.
- Expose to UV light for 60 seconds to crosslink the polymer into a solid hydrogel coating around the probe.
- Characterization:
- Mechanical Testing: Use atomic force microscopy (AFM) to confirm the elastic modulus of the hydrogel is in the kPa-MPa range.
- In Vivo Validation: Implant coated and uncoated controls and follow Protocol 1 to assess reduction in glial scarring.
Signaling Pathways and Experimental Workflows
Diagram Title: Foreign Body Response Cascade to Neural Implants
Diagram Title: Biocompatibility Testing Workflow
Scientific Background: Fibrosis and the Foreign Body Response
Fibrosis, the excessive deposition of extracellular matrix (ECM) proteins like collagen, is a critical failure mode for many implantable bioelectronic devices. This process is a hallmark of the Foreign Body Response (FBR), an immune-mediated reaction that leads to the encapsulation of implants in a fibrous scar, isolating them from their target tissue and severely compromising their function and longevity [2]. At the heart of this fibrotic cascade are key molecular biomarkers, most notably Transforming Growth Factor-Beta (TGF-β) and the damage-associated molecular pattern (DAMP) S100A8/A9.
- TGF-β: A well-known master regulator of fibrosis, TGF-β is secreted by macrophages and other immune cells at the implant site. It directly drives the differentiation of fibroblasts into highly active myofibroblasts. These myofibroblasts are characterized by their expression of Alpha-Smooth Muscle Actin (α-SMA) and are responsible for the rampant secretion and deposition of ECM proteins, such as Type I Collagen (Col1), leading to capsule formation [2].
- S100A8/A9: This heterodimer, also known as calprotectin, is predominantly released by infiltrating neutrophils and monocytes in response to tissue injury or the presence of a foreign material [45] [46]. It functions as a DAMP, alerting and activating the innate immune system. Recent research has solidified its role as a potent pro-fibrotic mediator. Studies on intrauterine adhesion (IUA) and obstructive nephropathy have demonstrated that S100A8/A9 not only promotes inflammatory cell recruitment but also directly activates fibroblasts and induces their differentiation into myofibroblasts [45] [47].
The interplay between these biomarkers creates a vicious cycle: tissue injury from implantation triggers S100A8/A9 release, which fuels inflammation and activates TGF-β-driven pathways, resulting in sustained fibroblast activation and fibrosis. Therefore, targeting these biomarkers is a promising strategy to mitigate the FBR and enhance the integration and durability of bioelectronic implants.
Key Signaling Pathways in Fibrosis
Understanding the specific signaling pathways is crucial for developing targeted interventions. The following diagrams and tables summarize the key mechanisms driven by S100A8/A9 and TGF-β.
S100A8/A9 Signaling Pathway
Diagram Title: S100A8/A9 Pro-Fibrotic Signaling via RAGE-JAK2-STAT3
Table 1: S100A8/A9 Pathway Components and Functions
| Component | Function in Pathway | Experimental Evidence |
|---|---|---|
| S100A8/A9 (DAMP) | Released by neutrophils; activates pro-fibrotic signaling. | Elevated in IUA endometrium and renal fibrosis models [45] [47]. |
| RAGE Receptor | Primary receptor for S100A8/A9-induced fibrosis. | RAGE blockade (FPS-ZM1) inhibits α-SMA and Col1 expression in hEnSCs [45]. |
| TLR4 Receptor | Binds S100A8/A9, but role in fibrosis is less clear. | TLR4 blocker (TAK-242) did not inhibit fibrosis markers in hEnSCs [45]. |
| JAK2/STAT3 | Key intracellular signaling pathway. | S100A8/A9 increases p-JAK2 and p-STAT3; inhibitor AG490 blocks fibrosis [45]. |
| Downstream Effects | Leads to cell proliferation, ECM production, and inflammation. | Increased hEnSC proliferation, Col1, α-SMA, IL-1β, and IL-6 [45]. |
TGF-β Signaling Pathway
Diagram Title: TGF-β Canonical Smad-Dependent Pro-Fibrotic Signaling
Table 2: TGF-β Pathway Components and Functions in FBR
| Component | Function in Pathway | Role in Foreign Body Response |
|---|---|---|
| TGF-β | Master cytokine regulator of fibrosis; secreted by activated macrophages. | Key factor in FBGC formation and fibroblast-to-myofibroblast transition [2]. |
| TGF-β Receptor | Serine/threonine kinase receptor. | Initiates intracellular signaling upon ligand binding. |
| Smad2/3/4 | Canonical intracellular signaling proteins. | Translocate to nucleus to activate transcription of pro-fibrotic genes. |
| Myofibroblast | Differentiated fibroblast with high contractile and secretory activity. | Primary cell type responsible for collagen deposition and capsule contraction [2]. |
| α-SMA & Collagen | Key markers and outputs of myofibroblast activity. | α-SMA provides contractility; Collagen (e.g., Col1) forms the fibrous capsule [45] [2]. |
Technical Support & Troubleshooting Guides
A. Experimental Protocols
Protocol 1: In Vitro Assessment of S100A8/A9-Induced Fibrosis in Stromal Cells
This protocol is adapted from studies on human endometrial stromal cells (hEnSCs) and is applicable for investigating fibroblast activation relevant to the FBR [45].
- Cell Isolation and Culture: Isolate primary human stromal cells (e.g., hEnSCs) from tissue specimens using established protocols. Confirm phenotype via immunofluorescence staining for Vimentin (positive) and α-SMA (negative under normal conditions).
- Treatment with S100A8/A9:
- Use recombinant human S100A8/A9 protein.
- Prepare a concentration gradient (e.g., 25, 50, 100, 200 ng/mL) in serum-free culture medium. A concentration of 100 ng/mL is often effective for stimulation, based on measured plasma levels in fibrotic conditions [45].
- Include a positive control (e.g., TGF-β at 10 ng/mL) and a vehicle control.
- Treat cells for 24-72 hours depending on the downstream assay.
- Pathway Inhibition: To confirm the role of specific pathways, pre-treat cells for 1 hour with inhibitors before adding S100A8/A9.
- RAGE Blocker: FPS-ZM1 (10 μg/mL) [45].
- JAK2/STAT3 Inhibitor: AG490.
- TLR4 Blocker: TAK-242 (10 μg/mL) as a negative control for fibrosis-specific signaling.
- Downstream Analysis:
- PCR/Western Blot: Analyze mRNA and protein levels of fibrosis markers (Col1, α-SMA) and inflammatory cytokines (IL-1β, IL-6).
- Immunofluorescence: Visualize α-SMA fiber formation and cellular morphology.
- Proliferation Assay: Use a CCK-8 assay to measure cell proliferation after 1-3 days of treatment.
Protocol 2: Validating Anti-Fibrotic Strategies in a Pre-Clinical Model
This protocol outlines key steps for evaluating biomaterials or drugs aimed at mitigating FBR, based on a porcine IUA model and mouse subcutaneous implantation studies [45] [7].
- Model Establishment:
- Large Animal (e.g., Porcine): Establish a fibrotic model via electrocautery injury to the target tissue (e.g., endometrium) to simulate implantation trauma [45].
- Rodent Subcutaneous Implantation: Implant polymer discs (e.g., PDMS vs. test material) into the backs of C57BL/6 mice. Ensure controls and test materials have similar size, shape, and mechanical properties (e.g., modulus) [7].
- Therapeutic Intervention:
- Tissue Collection and Analysis:
- Duration: Explain animals at predetermined endpoints (e.g., 1 month, 3 months, or longer for chronic FBR).
- Histology:
- Masson's Trichrome Staining: To visualize collagen deposition (blue) and measure fibrous capsule thickness.
- H&E Staining: For general tissue morphology and immune cell infiltration.
- Immunohistochemistry/Immunofluorescence:
- Stain for S100A8/A9, CD16 (neutrophil marker), α-SMA, and RAGE.
- Quantify expression levels and cellular localization.
- Protein Analysis: Homogenize tissue surrounding the implant. Use ELISA to quantify S100A8/A9 and TGF-β1 levels. Use Western Blot to analyze pathway activation (e.g., p-STAT3/STAT3).
B. Frequently Asked Questions (FAQs)
Q1: My in vitro results show that S100A8/A9 treatment does not significantly increase α-SMA in my fibroblast cell line. What could be wrong? A1: Consider the following troubleshooting steps:
- Cell Type Authenticity: Verify that your cell line is indeed a fibroblast and has not dedifferentiated. Check for Vimentin expression and confirm the source.
- S100A8/A9 Bioactivity: Ensure the recombinant protein is bioactive and correctly reconstituted. Perform a dose-response curve (25-200 ng/mL) and a time course experiment (24-72 hours). Always include a positive control like TGF-β.
- Receptor Expression: Confirm that your cells express the primary receptor RAGE via RT-PCR or Western Blot.
- Serum in Media: High serum concentrations can mask subtle effects. Consider using low-serum or serum-free conditions during stimulation.
Q2: When evaluating a new anti-fibrotic material in a mouse model, how can I distinguish a specific effect on the S100A8/A9 pathway from a general reduction in inflammation? A2: A multi-faceted analysis is key:
- Histological Correlation: Perform co-staining for S100A8/A9 and neutrophil/macrophage markers (e.g., CD16, F4/80). A specific effect would show a significant reduction in S100A8/A9* cells independent of a slight reduction in total immune cells [7].
- Pathway Analysis: Examine the downstream signaling components specifically. A material targeting S100A8/A9 should show reduced phosphorylation of JAK2 and STAT3 in the tissue surrounding the implant, even if early inflammation markers are present.
- Compare to Controls: Benchmark your material against a well-known inflammatory but fibrotic material (e.g., PDMS) and a negative control (sham surgery). This will help contextualize the specific anti-fibrotic effect.
Q3: What are the most critical controls for in vivo FBR experiments? A3:
- Sham Operation: Animals undergoing the same surgical procedure without implant placement. This controls for the effects of surgical trauma.
- Material Controls: Include implants made from a standard material known to elicit a strong FBR, such as PDMS or TPU. This is essential for benchmarking your test material's performance [7].
- Internal Control: When possible, implant multiple different materials in the same animal to reduce inter-subject variability and allow for direct comparison of capsule thickness and inflammation [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Investigating S100A8/A9 and TGF-β in Fibrosis
| Reagent / Material | Function / Application | Example & Notes |
|---|---|---|
| Recombinant S100A8/A9 Protein | To stimulate pro-fibrotic pathways in vitro. | Novoprotein (cited in [45]); use at 100 ng/mL for hEnSC stimulation. |
| Recombinant TGF-β1 Protein | Positive control for inducing fibroblast activation and differentiation. | Widely available from vendors like R&D Systems; use at 10 ng/mL. |
| RAGE Inhibitor (FPS-ZM1) | To block S100A8/A9 binding to RAGE and validate the specific pathway. | Use at 10 μg/mL for 1-hour pre-treatment in hEnSCs [45]. |
| JAK2/STAT3 Inhibitor (AG490) | To inhibit the key intracellular signaling pathway downstream of RAGE. | Validates the role of JAK2/STAT3 in S100A8/A9-mediated fibrosis [45]. |
| TLR4 Inhibitor (TAK-242) | To test the dependency of the fibrotic response on TLR4 signaling. | Used as a negative control in hEnSC studies, where it did not block fibrosis [45]. |
| Anti-S100A8/A9 Antibody | For detecting protein expression and localization in tissue via IHC/IF. | Critical for quantifying biomarker presence in pre-clinical models. |
| Anti-α-SMA Antibody | Marker for identifying activated myofibroblasts in tissue sections and cell cultures. | A primary readout for fibrotic activity [45] [2]. |
| Anti-Col1 Antibody | For detecting increased collagen I deposition, a key ECM component in fibrosis. | |
| EVADE Elastomers | Example of an immunocompatible material that suppresses S100A8/A9 expression and FBR. | Copolymer of HPEMA and ODA; showed negligible capsule formation after 1 year in mice [7]. |
Strategies for Sustained Anti-Fouling and Drug Delivery
This technical support guide provides targeted troubleshooting for researchers developing bioelectronic devices for sustained drug delivery. A primary challenge in this field is the foreign body response (FBR), a complex immune reaction that leads to the encapsulation of implanted devices in fibrotic tissue, isolating them from their target and causing functional failure [3] [10]. Furthermore, biofouling—the nonspecific adsorption of proteins and cells onto implant surfaces—initiates this response and can clog drug release mechanisms, reducing therapeutic efficacy [48] [49]. This resource addresses specific experimental issues related to minimizing the FBR and biofouling to maintain long-term device functionality.
Troubleshooting Guide: Common Experimental Challenges
FAQ 1: My implanted drug-delivery device shows a sharp drop in release efficacy after two weeks. What could be causing this?
Potential Cause: The most likely cause is fibrotic encapsulation of the device due to the foreign body response (FBR), creating a physical barrier that impedes drug diffusion [3] [10]. After implantation, protein adsorption triggers a cascade where macrophages attempt to phagocytose the device and subsequently fuse into foreign body giant cells (FBGCs). This process culminates in fibroblasts depositing a dense, avascular collagenous capsule around the implant [50] [10].
Solution: Implement surface modification strategies to create "immune-instructive" surfaces that resist protein fouling and discourage fibroblast activation.
- Surface Chemistry Modification:
- Apply Zwitterionic Polymer Coatings: Surfaces modified with polymers like poly(carboxybetaine) or poly(sulfobetaine) create a strong hydration layer via electrostatic interactions, providing excellent resistance to nonspecific protein adsorption [49] [51].
- Use High-Density Poly(Ethylene Glycol) (PEG): PEG chains create a steric and hydration barrier that prevents protein adhesion. Ensure a high density and appropriate molecular weight to form an effective "brush" regime [48] [51].
- Material Property Tuning:
- Optimize Surface Stiffness: Mimicking the mechanical properties of the surrounding host tissue can reduce the immune response. Macrophages and fibroblasts are sensitive to substrate stiffness, and a mismatch can exacerbate the FBR [3] [50].
- Incorporate Topographical Cues: Introducing micro- or nano-scale surface features can influence cell adhesion and morphology. For instance, surfaces with specific porosity (e.g., 34 µm pores in pHEMA hydrogels) have been shown to reduce capsule density and increase vascularization [3].
Experimental Protocol: Evaluating Fibrotic Encapsulation In Vivo
- Implant Material: Subcutaneously implant your drug-delivery device or a material sample into a rodent model (e.g., mouse or rat).
- Duration: Allow the implant to remain for 3-4 weeks to ensure the chronic FBR and fibrosis have developed [10].
- Explanation and Analysis: After euthanizing the animal, explant the device with the surrounding tissue.
- Histological Processing: Fix the tissue, embed it in paraffin, and section it for staining.
- Staining and Quantification:
- H&E Staining: For general observation of tissue structure and the cellular layers around the implant.
- Masson's Trichrome Staining: To specifically visualize the collagenous fibrotic capsule. The blue-stained collagen can be measured for capsule thickness using image analysis software.
- Immunohistochemistry for α-SMA: To identify activated myofibroblasts, the key cells responsible for collagen deposition and capsule contraction [3].
FAQ 2: The anti-fouling coating on my nanoparticle drug carrier is unstable in serum, leading to rapid clearance. How can I improve its stability?
Potential Cause: The instability is likely due to the displacement of the antifouling coating by serum proteins, forming a "protein corona." This corona is recognized by immune cells, particularly macrophages of the mononuclear phagocyte system (MPS), leading to opsonization and rapid clearance from the bloodstream [49] [51].
Solution: Select and apply advanced antifouling materials that form a more stable and resilient barrier against protein adsorption.
- Move Beyond Traditional PEG: While PEG is a standard, it is susceptible to oxidative damage and can trigger immune responses after multiple administrations [49]. Consider these alternatives:
- Zwitterionic Polymers: Materials like poly(2-methacryloyloxyethyl phosphorylcholine) (PCB) and poly(sulfobetaine methacrylate) (PSBMA) are highly hydrophilic and neutral, forming a more robust hydration layer than PEG and demonstrating superior antifouling performance in complex biological fluids [49] [51].
- Hydrophilic Polysaccharides: Natural polymers like dextran or hyaluronic acid can also be used as stealth coatings, though their effectiveness depends on the specific formulation and surface coverage [49].
Experimental Protocol: Analyzing Protein Corona and Nanoparticle Stability
- Incubation with Serum: Incubate your coated nanoparticles (NPs) with 100% fetal bovine serum (FBS) or mouse/rat plasma at 37°C for 1 hour.
- Isolation of Corona-Coated NPs: Separate the NPs from unbound proteins using centrifugation, size-exclusion chromatography, or magnetic separation (if applicable).
- Analysis:
- Dynamic Light Scattering (DLS): Measure the hydrodynamic diameter and zeta potential before and after serum incubation. A significant increase in size indicates protein adsorption.
- SDS-PAGE Gel Electrophoresis: Lyse the isolated NPs to desorb the corona proteins, run them on a gel, and stain (e.g., with Coomassie Blue) to visualize and semi-quantify the amount of adsorbed protein.
- Cellular Uptake Assay: Incubate serum-treated NPs with macrophage cell lines (e.g., RAW 264.7). Use flow cytometry or fluorescence microscopy (if NPs are fluorescently labeled) to quantify the percentage of cells that have internalized the NPs, which is a direct measure of "stealth" performance [51].
FAQ 3: My bioelectronic sensor loses signal sensitivity within days of implantation. How can I maintain a stable interface with the tissue?
Potential Cause: Signal loss is a classic symptom of the FBR, where an insulating layer of proteins, activated immune cells, and eventually a fibrotic capsule forms on the sensor's surface, physically blocking analyte diffusion and electrical contact with the target tissue [3] [10].
Solution: A multi-pronged approach focusing on both material properties and local immune modulation is required.
- Integrate Anti-Fouling and Fouling-Release Surfaces:
- Silicone Elastomers: Materials like polydimethylsiloxane (PDMS) with low surface energy can be used to create fouling-release surfaces, where adhered cells or biofilms are more easily detached under low shear stress [48].
- Leverage Biomimetic Designs: Surfaces that present "self" signals, such as the CD47 "don't eat me" signal, can help evade immune recognition and phagocytosis [50].
- Incorporate Localized Anti-Inflammatory Drug Delivery:
- Device Functionalization: Coat the sensor with a biodegradable polymer layer (e.g., PLGA) loaded with an anti-inflammatory agent (e.g., dexamethasone). This creates a localized, sustained release that can dampen the acute and chronic inflammatory response in the immediate vicinity of the implant without systemic side effects [50].
Experimental Protocol: Electrochemical Impedance Spectroscopy (EIS) for Monitoring Fouling
- Setup: Use a standard three-electrode system (working, counter, and reference electrodes) with your sensor as the working electrode.
- Baseline Measurement: Perform EIS in a relevant electrolyte (e.g., PBS) before implantation or exposure to a fouling solution to establish a baseline impedance spectrum.
- Fouling Challenge: Expose the sensor to a complex protein solution (e.g., 10% FBS) or implant it in vivo.
- Monitoring: Periodically measure the EIS spectrum over time.
- Data Interpretation: The increase in charge transfer resistance (
R_ct) at the electrode-electrolyte interface, observed as a widening of the semicircle in the Nyquist plot, is a direct quantitative indicator of biofouling and the formation of an insulating layer on the sensor surface.
Essential Research Reagent Solutions
Table 1: Key materials for developing anti-fouling surfaces and managing the foreign body response.
| Research Reagent | Function & Mechanism | Example Applications |
|---|---|---|
| Poly(ethylene glycol) (PEG) & Derivatives [48] [49] | Forms a hydrated steric barrier; prevents protein adsorption via high chain mobility and low interfacial energy. | Coating for nanoparticles, implant surfaces, and drug delivery systems to extend circulation time. |
| Zwitterionic Polymers (e.g., PCB, PSBMA) [49] [51] | Creates a super-hydrophilic surface bound water layer via electrostatic interactions; highly resistant to protein adhesion. | Superior alternative to PEG for stealth coatings on diagnostics and implants; used in hydrogels. |
| Silicone Elastomers (e.g., PDMS) [48] | Provides a low-modulus, low-surface-energy surface for fouling-release; weak adhesion of organisms. | Used in marine anti-fouling coatings and as a base material for soft bioelectronic implants. |
| Polyurethane Acrylate [48] | A durable polymer binder that can be engineered with fouling-release properties. | Matrix for anti-fouling paints and coatings on medical devices. |
| Dexamethasone [50] | A potent anti-inflammatory corticosteroid that suppresses macrophage activation and cytokine release. | Locally released from implant coatings to mitigate the acute and chronic inflammatory phases of the FBR. |
| Anti-CD47 Antibodies [50] | Biomimetic ligand that engages the SIRPα receptor on phagocytes, inhibiting phagocytosis ("don't eat me" signal). | Functionalization of implant surfaces to evade immune recognition by macrophages and dendritic cells. |
Critical Signaling Pathways and Experimental Workflows
Diagram: Foreign Body Response and Anti-Fouling Intervention Points
Diagram: Experimental Workflow for Anti-Fouling Coating Validation
Balancing Electrical Performance with Immune Compatibility
Troubleshooting Common Experimental Challenges
FAQ: Why does my bioelectronic implant experience significant signal degradation within weeks of implantation?
This is typically caused by the foreign body response (FBR), where immune cells recognize the implant as a foreign material, leading to collagenous fibrotic capsule formation that insulates the device [3] [35]. This avascular fibrous tissue creates a physical barrier that impedes signal transduction by increasing interface impedance and blocking efficient transport of biomolecules [35].
FAQ: Which material properties most significantly influence the foreign body response?
Both physical and chemical properties play crucial roles. Key physical parameters include size, shape, surface topography, and mechanical stiffness [3]. Chemically, surface wettability, charge, and functional groups determine protein adsorption patterns that subsequently trigger immune activation [3] [18]. Research shows that incorporating specific immunomodulatory chemical groups and optimizing surface topography can reduce collagen deposition by up to 68% [18].
FAQ: How can I test immune compatibility without resorting to expensive long-term animal studies?
Establish robust in vitro screening methods before moving to in vivo validation:
- Macrophage polarization assays: Expose primary macrophages to material extracts and quantify M1/M2 phenotype markers via PCR or flow cytometry [50]
- Cytokine profiling: Measure pro-inflammatory (IL-1β, IL-6, TNF-α) and anti-inflammatory (IL-4, IL-10) cytokine secretion using ELISA [18]
- Reactive oxygen species (ROS) detection: Use fluorescent probes to quantify oxidative stress in immune cells [18]
Experimental Protocols for Immune Compatibility Assessment
Protocol 1: Quantitative Fibrosis Measurement in Subcutaneous Implantation Model
Materials Required:
- Polymer films or devices (diameter: 5-10mm, thickness: 100-500μm)
- C57BL/6 mice (8-12 weeks old)
- Masson's Trichrome staining kit
- Imaging system with quantification software
Procedure:
- Implant test materials subcutaneously in mouse dorsal regions using aseptic technique
- After 4 weeks, euthanize animals and excise implant sites with surrounding tissue
- Fix tissue in 4% paraformaldehyde for 24 hours, process, and embed in paraffin
- Section tissues at 5μm thickness and perform Masson's Trichrome staining
- Image sections at 10x magnification and quantify collagen density using ImageJ software:
- Convert images to 8-bit grayscale
- Apply uniform threshold to isolate blue-stained collagen
- Calculate percentage of blue pixels per total tissue area
- Compare collagen density between experimental and control groups (n ≥ 5 per group)
Protocol 2: Electrochemical Impedance Spectroscopy for Interface Stability
Materials Required:
- Potentiostat with EIS capability
- Three-electrode setup (implant material as working electrode)
- Phosphate buffered saline (PBS, pH 7.4) or simulated body fluid
- Temperature-controlled cell (37°C)
Procedure:
- Mount test material as working electrode in electrochemical cell
- Immerse in electrolyte solution and maintain at 37°C
- Apply sinusoidal potential (10mV amplitude) over frequency range 0.1Hz-100kHz
- Record impedance spectra at predetermined time points (day 0, 7, 14, 28)
- Fit Nyquist plots to equivalent circuit models to extract:
- Solution resistance (Rs)
- Charge transfer resistance (Rct)
- Double layer capacitance (Cdl)
- Monitor changes in Rct over time as indicator of fibrotic tissue formation
Performance Comparison of Immune-Compatibility Strategies
Table 1: Quantitative Comparison of Material Strategies for Mitigating Foreign Body Response
| Strategy | Material System | Collagen Density Reduction | Electrical Performance | Key Immune Markers Affected |
|---|---|---|---|---|
| Selenophene backbone | Semiconducting polymer p(g2T-Se) | ~50% [18] | Charge-carrier mobility ~1 cm²V⁻¹s⁻¹ [18] | ↓ CCR7, IFN-γ, IL-6, IL-1β [18] |
| Immunomodulatory side chains (TMO) | p(g2T-Se)-TMO | ~68% [18] | Maintains electrical functionality in OECT [18] | ↓ Macrophages (~68%), ↓ myofibroblasts (~79%) [18] |
| Cell-scale porosity | MAP hydrogel | Prevents fibrous encapsulation [52] | Not electrically active | Promotes regenerative macrophage polarization [52] |
| Surface topography modification | Electrospun PTFE (1.08μm roughness) | Reduced FBGC formation [3] | Application-dependent | ↓ Macrophage attachment, ↓ FBGCs [3] |
Table 2: In Vitro and In Vivo Assessment Methods for Immune Compatibility
| Assessment Method | Parameters Measured | Timeframe | Key Advantages |
|---|---|---|---|
| Macrophage polarization assay | M1/M2 surface markers, cytokine secretion | 3-7 days | Rapid screening, mechanistic insight |
| Subcutaneous implantation | Collagen density, immune cell infiltration | 4 weeks | Gold standard for FBR evaluation |
| Electrochemical impedance spectroscopy | Interface resistance, charge transfer | Real-time monitoring | Non-destructive, functional assessment |
| Immunofluorescence staining | Macrophages (CD68), myofibroblasts (α-SMA) | Endpoint (1-4 weeks) | Spatial distribution of immune cells |
Research Reagent Solutions
Table 3: Essential Research Reagents for Immune Compatibility Studies
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| Selenophene-containing polymers | Semiconductor backbone with immunomodulatory properties | Reducing FBR through ROS scavenging [18] |
| THP & TMO side chains | Immunomodulatory functionalization | Downregulating pro-inflammatory biomarkers [18] |
| Microporous Annealed Particle (MAP) scaffolds | 3D hydrogel with cell-scale porosity | Preventing fibrous encapsulation in volumetric muscle loss [52] |
| PEG-based hydrogels | Tunable stiffness substrates | Matching tissue mechanical properties (e.g., 11.35 kPa for myotube differentiation) [52] |
| Masson's Trichrome stain | Collagen visualization in tissue sections | Quantifying fibrotic capsule thickness [18] |
Signaling Pathways in Foreign Body Response
Diagram 1: Foreign body response signaling pathway and intervention points.
Experimental Workflow for Immune-Compatible Material Development
Diagram 2: Comprehensive workflow for developing immune-compatible bioelectronic materials.
Bench to Bedside: Validating FBR Reduction and Comparing Technology Efficacy
Troubleshooting Guide: Common Challenges in Long-Term FBR Studies
Table: Troubleshooting Common Issues in Long-Term FBR Implantation Studies
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Excessive Fibrosis & Rapid Device Failure | Overly aggressive host immune response; suboptimal implant material properties. [53] [2] | Consider increasing spherical implant diameter to ≥1.5 mm. Optimize material surface chemistry with immunomodulatory moieties (e.g., selenophene, THP, TMO). [53] [18] |
| High Animal-to-Animal Variability | Inconsistent surgical implantation technique; genetic drift in animal colonies; inconsistent post-operative care. [54] | Standardize surgical protocols across all researchers. Use age- and sex-matched animals from stable genetic backgrounds. Implement blinded histopathological analysis. [55] |
| Unexpected Immune Cell Recruitment | Unaccounted for material properties (e.g., surface topography, wettability) triggering specific immune pathways. [2] [54] | Characterize material surface properties thoroughly pre-implantation. Include positive and negative control materials in the study design. Use knockout mouse models (e.g., Mac-1, SPARC) to probe specific pathways. [2] |
| Inconsistent Capsule Thickness Measurements | Non-uniform capsule formation; sub-optimal tissue sectioning or staining. [55] | Use standardized histomorphometry across multiple tissue sections. Employ quantitative methods like collagen pixel density or mRNA expression levels for collagen types I/III. [18] |
FAQs: Designing and Executing FBR Studies
Q1: What is the critical time frame for assessing a "long-term" FBR in rodents? A long-term FBR in rodents is typically assessed at 4 weeks post-implantation, by which point a mature, dense fibrous capsule has fully developed. Acute inflammatory responses are evaluated around 1 week. [18] [55] [56]
Q2: How can I quantitatively compare the severity of the FBR between different implant groups? The fibrotic response can be quantified using several methods:
- Histomorphometry: Measure the thickness and cellularity of the collagen capsule from stained tissue sections (e.g., Masson's Trichrome). [55]
- Collagen Density: Quantify the blue pixel density from Masson's Trichrome-stained sections. [18]
- qPCR: Analyze mRNA expression levels of fibrosis-related genes, such as Collagen Type I and Type III. [18]
- Immunofluorescence: Quantify the presence of key immune cells, such as macrophages (CD68+) and myofibroblasts (α-SMA+), in the tissue surrounding the implant. [18]
Q3: What are the key advantages of using non-human primate (NHP) models for FBR research? NHP models are critical for demonstrating clinical translatability. Their immune systems more closely resemble humans, providing highly relevant pre-clinical data on a material's or device's potential to mitigate the FBR, which is essential for regulatory approval. [53] [55] [56]
Q4: My bioelectronic implant requires direct electrical contact with tissue. How can I mitigate FBR without sacrificing performance? Recent strategies focus on intrinsic material modification rather than coatings that can increase impedance. Incorporating specific molecular designs, such as selenophene in the polymer backbone or immunomodulatory groups (THP, TMO) on side chains, has been shown to suppress FBR (reducing collagen density by up to 68%) while maintaining high charge-carrier mobility. [18]
Experimental Protocols for Key FBR Assessments
Protocol 1: Subcutaneous Rodent Implantation for Long-Term FBR
This is a foundational model for evaluating the FBR to biomaterials and bioelectronics. [55]
- Material Preparation: Sterilize implant materials (e.g., polymer films, hydrogels, or devices) using ethylene oxide or gamma irradiation. For spherical hydrogels, ensure precise diameter control.
- Animal Anesthesia & Preparation: Anesthetize rodents (e.g., C57BL/6 mice) and shave/sterilize the dorsal skin.
- Implantation: Make a small midline incision. Create subcutaneous pockets bilaterally via blunt dissection. Insert one implant per pocket. The control pocket should receive a sham surgery or a standard control material.
- Closure & Post-Op Care: Close the incision with surgical sutures or clips. Administer post-operative analgesics and monitor animals until they recover.
- Explanation & Analysis: At the predetermined endpoint (e.g., 4 weeks), euthanize the animal. Carefully explant the device with the surrounding tissue and process for histological and molecular analysis. [55]
Protocol 2: Quantitative Analysis of Fibrotic Encapsulation
- Tissue Fixation and Sectioning: Fix explanted tissue in 4% paraformaldehyde, paraffin-embed, and section to a 5-10 µm thickness. [55]
- Staining: Perform Masson's Trichrome (MT) staining to visualize collagen (blue), muscle/cytoplasm (red), and cell nuclei (black).
- Image Acquisition: Capture high-resolution images of the tissue-implant interface using a brightfield microscope.
- Quantification:
- Capsule Thickness: Measure the fibrous capsule width at multiple, standardized locations around the implant and calculate the average.
- Collagen Density: Use image analysis software (e.g., ImageJ) to calculate the percentage of blue-stained area (collagen) within a defined region of interest adjacent to the implant. [18]
Visualizing the Foreign Body Response Pathway
The following diagram illustrates the key cellular and molecular events in the Foreign Body Response, a critical framework for designing experiments and interpreting results.
Foreign Body Response Mechanism
The Scientist's Toolkit: Essential Reagents & Models
Table: Key Reagents and Models for FBR Research
| Reagent / Model | Function / Purpose | Key Characteristics & Examples |
|---|---|---|
| Alginate Spheres | A widely used hydrogel model for studying the effect of implant size and shape on FBR. | Spheres ≥1.5 mm significantly reduce fibrosis. Used for islet cell encapsulation to prolong graft function. [53] |
| Immunomodulatory Polymers | Semiconducting polymers designed to intrinsically suppress FBR for bioelectronics. | Polymers with selenophene backbone and THP/TMO side chains suppress macrophage activation and collagen deposition (up to 68% reduction). [18] |
| Genetically Modified Mice | To dissect the role of specific immune pathways in the FBR. | Mac-1 KO: Thinner capsule. SPARC-null: Thinner, less dense capsule. Clodronate liposomes: Deplete macrophages to prevent FBR. [2] |
| Macrophage Cell Lines | In vitro models for initial screening of material biocompatibility. | RAW 264.7 (mouse), J774A.1 (mouse), THP-1 (human). Useful for studying adhesion, polarization, and cytokine release. [56] |
| Computational (in silico) Models | Predictive tools to simulate FBR dynamics and test hypotheses. | Incorporates material properties (stiffness, immunogenicity) to predict fibrotic outcomes, complementing wet-lab experiments. [54] |
Core Quantification Metrics and Their Significance
This section details the key quantitative measurements used to assess the Foreign Body Response (FBR), providing a baseline for evaluating the performance of new bioelectronic materials.
Table 1: Key Quantitative Metrics for Assessing Foreign Body Response
| Metric Category | Specific Metric | Typical Measurement Method | Significance & Interpretation | Reported Values in Anti-FBR Studies |
|---|---|---|---|---|
| Capsule Thickness | Fibrous capsule thickness (μm) | Histological staining (e.g., H&E, Masson's Trichrome); multiple measurements per capsule [57]. | Direct indicator of fibrotic encapsulation; thinner capsules suggest lower FBR [58] [34]. | PDMS: 45-135 μm; EVADE Elastomer (H90): 10-40 μm [58]. PEG Hydrogels: ~19-27 μm; Poly-DL-serine (PSer) Hydrogels: <5 μm [34]. |
| Collagen Density | % Collagen at tissue-implant interface | Masson's Trichrome staining with image analysis (blue pixel density) [18] [34]. | Measures extent of fibrotic, collagen-based tissue deposition [57]. | PEG Hydrogels: >90%; PSer Hydrogels: 48-69% [34]. Control Polymers: ~25%; Immune-compatible Semiconducting Polymers: as low as ~8% [18]. |
| Immune Cell Infiltration | Macrophage density (cells/area) | Immunofluorescence (e.g., F4/80, CD68 staining) [18] [34]. | Identifies primary immune cells driving the FBR; lower density indicates better biocompatibility. | A 68% decrease in macrophage population was reported for an immune-compatible semiconducting polymer compared to its control [18]. |
| Myofibroblast presence (cells/area) | Immunohistochemistry (e.g., α-Smooth Muscle Actin (α-SMA) staining) [18] [57]. | Marks activated fibroblasts responsible for capsule contraction. | A 79% decrease in myofibroblasts was reported for an immune-compatible semiconducting polymer [18]. Contracted capsules show significantly greater α-SMA immunoreactivity [57]. | |
| Gene Expression | mRNA levels of collagens & cytokines | Quantitative Real-Time PCR (qRT-PCR) from harvested capsular tissue [18] [59]. | Reveals molecular activity behind fibrosis and inflammation. | Immune-compatible designs downregulate mRNA for Collagen I/III (by up to 70%) and pro-inflammatory genes (e.g., IL-6, IL-1β, TNF-α) [18]. hAD-MSCs downregulate pro-fibrotic and pro-inflammatory genes [59]. |
| Protein Biomarkers | Cytokine/Chemokine levels | Proteome profiler antibody arrays; ELISA (e.g., for TGF-β) [58] [59]. | Quantifies soluble signaling proteins that orchestrate FBR. | EVADE elastomers significantly reduce pro-inflammatory markers (CCR-7, TNF-α, IL-6) versus PDMS [58]. S100A8/A9 alarmins are identified as key proteins in fibrosis cascade [58]. |
Detailed Experimental Protocols for Key Metrics
FAQ: What is the standard workflow for histologically quantifying capsule thickness and collagen density?
The following protocol, adapted from established methods, ensures reliable and quantifiable results [57].
1. Sample Harvesting and Preparation:
- Implant Explanation: Carefully remove the implant and the surrounding capsular tissue en bloc.
- Fixation: Immediately place tissue in 10% Neutral Buffered Formalin for 24-48 hours to preserve structure.
- Processing and Embedding: Dehydrate tissues through a graded ethanol series, clear with xylene, and embed in paraffin wax.
- Sectioning: Use a microtome to cut 5 μm thick sections and mount them on glass slides.
2. Histological Staining:
- Masson's Trichrome (M&T) Staining: This is the gold standard for simultaneous visualization of tissue structure and collagen.
- Principle: Stains nuclei black, cytoplasm/muscle fibers red, and collagen blue.
- Procedure: Follow standard M&T staining kit protocols, which typically involve sequential staining with Weigert's Iron Hematoxylin, Biebrich Scarlet-Acid Fuchsin, and Aniline Blue.
- Hematoxylin and Eosin (H&E) Staining:
- Principle: Stains nuclei blue-purple and cytoplasm/extracellular matrix pink. Provides a general overview of tissue morphology and inflammatory cell infiltration.
3. Image Acquisition and Analysis:
- Microscopy: Capture high-resolution images of the capsule-tissue interface using a light microscope with a 4x to 20x objective.
- Capsule Thickness:
- On a low-magnification image (e.g., 4x), draw five to ten perpendicular lines from the implant surface to the outer edge of the capsule at evenly spaced intervals.
- Use image analysis software (e.g., Nikon NIS Elements, ImageJ) to measure the length of each line.
- Report the average thickness and standard deviation [57].
- Collagen Density:
- On high-magnification M&T images (e.g., 20x), take multiple fields of view along the implant interface.
- Using image analysis software, apply a color threshold to isolate the blue-stained collagen areas.
- Calculate the percentage of the total tissue area that is positive for blue staining (collagen density = [blue pixel area / total pixel area] * 100) [18] [34].
FAQ: How do I quantify the expression of key fibrotic and inflammatory markers at the molecular level?
Protocol: RNA Isolation and Quantitative PCR (qPCR) from Capsular Tissue
1. RNA Isolation:
- Homogenization: Lyse approximately 30 mg of harvested capsular tissue in a TRI Reagent (or similar) using a homogenizer.
- Phase Separation: Add chloroform, shake vigorously, and centrifuge. The RNA partitions into the colorless upper aqueous phase.
- RNA Precipitation: Transfer the aqueous phase to a new tube and precipitate the RNA with isopropanol.
- Wash and Resuspend: Wash the RNA pellet with 75% ethanol, air-dry, and dissolve in RNase-free water.
- Quality Control: Measure RNA concentration and purity using a spectrophotometer (e.g., Nanodrop). A 260/280 ratio of ~2.0 indicates pure RNA.
2. cDNA Synthesis:
- Use a High-Capacity cDNA Reverse Transcription Kit.
- Set up a reaction with your purified RNA template, reverse transcriptase enzyme, dNTPs, and random primers.
- Incubate according to the manufacturer's protocol (typically 10 min at 25°C, 120 min at 37°C, 5 min at 85°C).
3. Quantitative PCR (qPCR):
- Reaction Mix: Prepare reactions using SYBR Green PCR Master Mix, forward and reverse primers (e.g., for Collagen I, Collagen III, IL-6, TNF-α, TGF-β), cDNA template, and nuclease-free water.
- Cycling Conditions: Standard two-step qPCR protocol: Initial denaturation (95°C for 10 min), followed by 40 cycles of denaturation (95°C for 15 sec) and annealing/extension (60°C for 1 min).
- Data Analysis: Calculate the relative gene expression using the 2^(-ΔΔCt) method. Normalize the Ct values of your target genes to a housekeeping gene (e.g., GAPDH, β-actin) and then compare to a control group (e.g., tissue from a sham surgery or a control implant material) [18] [59].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for FBR Quantification
| Reagent / Material | Function / Application | Specific Examples / Targets |
|---|---|---|
| Primary Antibodies (IHC/IF) | Detect and visualize specific cell types or proteins in tissue sections. | α-SMA: Identifies contractile myofibroblasts [57].CD68 / F4/80: Pan-macrophage markers [18] [57] [34]. |
| SYBR Green qPCR Master Mix | Fluorescent dye for detecting amplified DNA in qPCR reactions. | Quantify mRNA expression of fibrotic (Collagen I, III) and inflammatory (TNF-α, IL-6, IL-1β) genes [18] [59]. |
| Proteome Profiler Antibody Arrays | Simultaneously detect multiple cytokines and chemokines from tissue lysates or serum. | Screen for a wide panel of inflammation-related proteins (e.g., GM-CSF, MCP-1, IL-23) to identify key players in FBR [18] [58]. |
| Masson's Trichrome Staining Kit | Differentiate collagen (blue) from muscle/cytoplasm (red) and nuclei (black) in tissue sections. | Standard method for quantifying collagen density and visualizing fibrous capsule structure [18] [57] [34]. |
| ELISA Kits | Precisely quantify the concentration of a specific soluble protein. | Measure key cytokines like TGF-β (master regulator of fibrosis) or alarmins like S100A8/A9 in serum or tissue homogenates [58] [59]. |
Troubleshooting Common Experimental Issues
FAQ: My histological samples show high background staining or non-specific signal in immunohistochemistry. What can I do?
- Problem: High background noise obscures specific signal.
- Solution:
- Titrate Antibodies: The most common cause is antibody concentration that is too high. Perform a checkerboard titration to find the optimal dilution for your primary and secondary antibodies.
- Optimize Blocking: Ensure you are using an appropriate blocking serum (from the same species as the secondary antibody) for a sufficient time (1 hour at room temperature).
- Increase Wash Stringency: Add a mild detergent like Tween-20 (0.025-0.1%) to your PBS wash buffer and increase wash frequency and duration.
- Check Endogenous Enzymes: For enzyme-based detection (e.g., HRP), quench endogenous peroxidase activity with 3% H₂O₂ before antibody incubation.
FAQ: My qPCR results show high variability between technical replicates or no amplification.
- Problem: Inconsistent or failed qPCR runs.
- Solution:
- Check RNA Integrity: Ensure RNA is not degraded. Run an aliquot on an agarose gel to check for sharp ribosomal RNA bands.
- Verify Primer Specificity: Check primer sequences using BLAST and run a melt curve after qPCR. A single, sharp peak indicates specific amplification.
- Optimize Template Concentration: Too much cDNA can inhibit the reaction, while too little leads to low signal. Test a dilution series of your cDNA to find the linear range of amplification.
- * pipetting Accuracy:* Use calibrated pipettes and master mixes to minimize volume errors between wells. Centrifuge the plate before running.
FAQ: The collagen density measurements from my image analysis are inconsistent across different sample fields.
- Problem: High variance in collagen quantification.
- Solution:
- Standardize Image Acquisition: Use identical microscope lighting, exposure time, and magnification for all images.
- Calibrate Thresholding: Apply the same color threshold settings to all images within an experimental set. Manually verify that the threshold accurately captures all collagen and excludes background for a subset of images first.
- Sample Sufficiently: Analyze multiple, non-overlapping fields of view per sample (e.g., 5-10 fields) to get a representative average.
- Blind Analysis: Have the person performing the quantification do so blindly, without knowledge of the experimental group, to eliminate bias.
The foreign body response (FBR) presents a fundamental challenge for implantable bioelectronic devices, often leading to device failure through inflammatory processes and fibrotic encapsulation. This immune-mediated reaction begins immediately upon implantation with protein adsorption to the material surface, followed by neutrophil recruitment, macrophage activation, and eventual collagen deposition that isolates the implant from surrounding tissue [60] [4]. The resulting fibrotic barrier significantly impedes signal transduction for biosensing and stimulating devices, compromising their long-term functionality and reliability [61] [4]. As the field of bioelectronics advances toward chronic implantation and precise neural interfacing, developing material strategies to mitigate FBR has become increasingly critical for clinical translation.
Material Performance Comparison Tables
Polymer Biocompatibility and Foreign Body Response
Table 1: In vivo performance of polymers for neural interfaces
| Polymer Material | Fibrous Capsule Thickness | Macrophage Response | Collagen Density | Key Findings |
|---|---|---|---|---|
| Polyimide (PI) | Minimal | Low | Low | Highest compatibility; minimal FBR [13] |
| PEGDA | Extensive | High | High | Strong cytotoxic effects; pronounced FBR [13] |
| PDMS | Moderate | Moderate | Moderate | Good biocompatibility; suitable for neural interfaces [13] |
| PLA | Moderate | Moderate | Moderate | Promising for safe neural interfaces [13] |
| TPU | Moderate | Moderate | Moderate | Good compatibility for long-term use [13] |
| Selenophene-based polymer | Significantly reduced | ~68% reduction | ~68% reduction | Substantial FBR suppression [62] [18] |
Electrical and Mechanical Properties
Table 2: Functional properties of bioelectronic materials
| Material | Charge Carrier Mobility | Young's Modulus | Key Electrical Features | Signal Stability |
|---|---|---|---|---|
| Traditional P(g2T-T) | High | MPa range | Good OECT performance | Signal degradation over weeks |
| Selenophene-engineered P(g2T-Se) | ~1-1.2 cm²V⁻¹s⁻¹ | MPa range | Enhanced transconductance | Improved chronic signal retention [18] [20] |
| PEDOT:PSS | Variable | Soft, flexible | Low impedance, coating/freestanding | Good short-term stability [63] |
| Thiophene-based semiconductors | Moderate to high | MPa range | Standard OECT operation | Standard signal degradation [62] |
Frequently Asked Questions (FAQs)
Q1: What are the primary mechanisms through which novel polymers reduce foreign body response compared to traditional materials?
Novel immunomodulatory polymers employ two primary mechanisms to reduce FBR: (1) backbone engineering with selenium-containing units like selenophene, which suppresses macrophage activation through antioxidant effects and reactive oxygen species scavenging [62] [18]; and (2) side-chain functionalization with immunomodulatory groups (THP and TMO) that downregulate pro-inflammatory biomarkers including CCR7, IFN-γ, GM-CSF, MCP-1, and various interleukins while upregulating anti-inflammatory biomarkers like IL-10 and IL-4 [18]. Traditional materials typically lack these specific immunomodulatory properties and may rely primarily on passive biocompatibility.
Q2: How does the mechanical mismatch between implant materials and neural tissue contribute to FBR, and how do novel polymers address this?
The significant mechanical mismatch between rigid traditional materials (Young's modulus of ~100-200 GPa for metals and silicon) and soft brain tissue (~1 kPa) exacerbates FBR by causing continuous tissue micromotion, inflammation, and eventual glial scar formation [63]. Novel polymers address this through tissue-like mechanical properties with Young's moduli in the kPa-MPa range, significantly reducing the mechanical mismatch [63]. Additionally, advanced material designs incorporate ultra-thin geometries, mesh structures, and stretchable serpentine patterns to further enhance mechanical compatibility with dynamic biological tissues [63].
Q3: What are the trade-offs between FBR suppression and electrical performance in novel polymer designs?
The most successful novel polymer designs demonstrate that FBR suppression and electrical performance need not be mutually exclusive. Selenophene backbone engineering in semiconducting polymers simultaneously promotes immune compatibility while maintaining high charge carrier mobility (~1-1.2 cm²V⁻¹s⁻¹) and even enhancing transconductance compared to traditional thiophene-based counterparts [18] [20]. This represents a significant advantage over coating-based FBR mitigation approaches, which often increase interfacial impedance and can limit signal transduction efficiency [18].
Troubleshooting Guides
Problem: Excessive Fibrous Encapsulation of Implants
Potential Causes and Solutions:
Cause: Material surface properties promoting protein fouling and macrophage adhesion.
Cause: Excessive mechanical mismatch causing chronic tissue irritation.
- Solution: Select materials with tissue-matching mechanical properties (Young's modulus < 1 MPa) and consider ultra-thin, flexible designs to minimize mechanical strain [63].
Cause: Lack of active immunomodulation in material composition.
Problem: Signal Degradation in Chronic Implantation
Potential Causes and Solutions:
Cause: Progressive fibrotic encapsulation increasing electrode impedance.
- Solution: Utilize drug-eluting composite coatings (e.g., PLGA microspheres in PVA hydrogel) for localized, sustained anti-inflammatory drug release [61].
Cause: Material degradation or corrosion in biological environment.
Cause: Macrophage-mediated oxidative damage to electronic components.
Experimental Protocols
Protocol for In Vivo FBR Assessment of Bioelectronic Materials
Objective: Systematically evaluate the foreign body response to novel polymer-based bioelectronic materials in a murine subcutaneous implantation model.
Materials Required:
- Polymer films (0.5-1.0 cm diameter) on SEBS substrates
- Surgical tools (forceps, scissors, needle holder)
- Isoflurane anesthesia system
- Suture materials or wound clips
- Tissue processing equipment and reagents
Procedure:
- Prepare polymer films (500 μm thickness) on circular SEBS substrates and sterilize using ethylene oxide or ethanol immersion.
- Anesthetize mice (C57BL/6, 8-12 weeks) and shave dorsal region.
- Make 1 cm incision and create subcutaneous pocket using blunt dissection.
- Implant polymer films (n=5-8 per group) and close incision with sutures or wound clips.
- After 4 weeks, euthanize animals and carefully excise implants with surrounding tissue.
- Fix tissue in 4% paraformaldehyde, process, and embed in paraffin.
- Section tissues (5 μm thickness) and perform Masson's trichrome staining for collagen visualization.
- Quantify collagen density using image analysis software (ImageJ) by calculating percentage of blue-stained area relative to total tissue area in implant-adjacent regions [18] [13].
- Perform immunofluorescence staining for macrophages (CD68) and myofibroblasts (α-SMA) to quantify immune cell recruitment.
- Isolate RNA from peri-implant tissue for qPCR analysis of collagen types I and III, and inflammatory markers.
Expected Outcomes: Novel immunomodulatory polymers should exhibit significantly reduced collagen density (>50% reduction), decreased macrophage and myofibroblast populations, and downregulation of pro-inflammatory gene expression compared to traditional materials [18] [13].
Protocol for Electrical Performance Assessment in OECT Configuration
Objective: Characterize the electrical performance and operational stability of novel semiconducting polymers in organic electrochemical transistor (OECT) configuration.
Materials Required:
- Synthesized semiconducting polymers
- Pre-patterned OECT substrates with source/drain electrodes
- Phosphate buffered saline (PBS) or physiological electrolyte
- Semiconductor parameter analyzer (Keysight B1500A or similar)
- Probe station with environmental chamber
- Ag/AgCl gate electrode
Procedure:
- Fabricate OECT devices by spin-coating or drop-casting polymer solutions onto pre-patterned substrates.
- Anneal films according to optimized conditions for each polymer.
- Mount devices in probe station and immerse gate and channel areas in PBS (pH 7.4).
- Insert Ag/AgCl gate electrode into electrolyte.
- Perform output characteristics by sweeping drain voltage (V$D$) from 0 to -0.6 V at different gate voltages (V$G$).
- Measure transfer characteristics by sweeping V$G$ from 0.4 to -0.6 V at constant V$D$ = -0.6 V.
- Extract transistor parameters: on/off ratio, transconductance (g$_m$), and volumetric capacitance (C*).
- Calculate charge carrier mobility (μ) using the equation: μ = (g$m$$^2$L$^2$)/(WC*V$D$I$_D$), where L and W are channel length and width, respectively.
- For stability assessment, continuously operate devices at physiologically relevant conditions (37°C, PBS) while monitoring performance metrics over 2-4 weeks.
Expected Outcomes: High-performance semiconducting polymers should maintain charge carrier mobility >1 cm²V⁻¹s⁻¹ with high transconductance and stable operation over several weeks in physiological conditions [18] [20].
Signaling Pathways and Experimental Workflows
Diagram Title: FBR Mechanism and Polymer Intervention Points
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential materials for FBR-suppressive bioelectronic research
| Research Reagent | Function/Application | Key Considerations |
|---|---|---|
| PLGA Microspheres | Controlled drug delivery platform for anti-inflammatories | Biodegradable; FDA-approved; tunable release kinetics [61] |
| PVA Hydrogel | Dispersing matrix for drug carriers; biocompatible coating | Physically crosslinkable; tissue-like mechanics; analyte permeability [61] |
| Selenophene-based monomers | Backbone units for immunomodulatory semiconducting polymers | Provide antioxidant properties; maintain electrical performance [62] [18] |
| THP/TMO functional groups | Side-chain modifications for immunomodulation | Downregulate pro-inflammatory biomarkers; compatible with CLIP chemistry [18] |
| Zwitterionic polymers | Low-fouling surface coatings | Resist protein adsorption; reduce macrophage adhesion [63] |
| Soft elastomers (SEBS, PDMS) | Substrates for flexible electronics | Tissue-matching mechanics; encapsulation materials [18] [63] |
Troubleshooting Guides & FAQs
Device-Specific Troubleshooting FAQs
Q1: Our implanted neural interface shows a progressive decline in signal-to-noise ratio (SNR) over weeks. What is the likely cause and how can we validate this? A: The most probable cause is the foreign body response (FBR), leading to fibrous encapsulation that increases impedance and distances the electrode from active neurons [64]. To validate:
- Histological Analysis: Explain the process for explanting the device and surrounding tissue for analysis. The tissue should be stained for macrophages (CD68), myofibroblasts (α-SMA), and collagen (e.g., Masson’s Trichrome) to quantify immune cell density and fibrotic capsule thickness [18].
- Electrochemical Impedance Spectroscopy (EIS): Detail how to perform EIS measurements in vivo or on explanted devices to track increases in interface impedance over time, which correlates with FBR progression [64].
Q2: Our subcutaneous glucose sensor exhibits inaccurate readings and increased lag time after the first few days of implantation. How can we determine if this is a biofouling issue? A: This pattern is characteristic of the acute inflammatory phase of the FBR, where protein adsorption and leukocyte infiltration create a barrier to analyte diffusion [65] [66].
- In Vitro Biofouling Simulation: Describe a protocol for incubating the sensor membrane in a solution of serum albumin or fibrinogen to model protein adsorption. A significant drop in sensitivity suggests susceptibility to biofouling.
- Analyte Permeability Testing: Outline a method using a diffusion cell to measure the glucose flux through the sensor membrane before and after biofouling simulation. A decreased flux confirms the FBR is impairing analyte transport [65].
Q3: An insulin pump integrated with a CGM fails to maintain glycemic control. The CGM readings are stable, but blood glucose is high. How do we isolate the fault? A: This points to a failure in insulin delivery, not sensing.
- Infusion Set Check: Provide steps to inspect for kinks, occlusions, or leaks in the tubing and cannula.
- In Vitro Flow Rate Validation: Specify a methodology to connect the pump to a saline reservoir and measure the delivered volume over 24 hours against the programmed rate. A discrepancy indicates a pump mechanism failure [67].
- Formulation Stability Check: Recommend testing the insulin for aggregation or degradation, which can cause occlusions and reduce bioavailability.
Quantitative Data on FBR-Suppressing Strategies
Table 1: Efficacy of Molecular Design Strategies in Suppressing Foreign Body Response
| Strategy | Material/Design | Experimental Model | Key Metric | Result | Reference |
|---|---|---|---|---|---|
| Backbone Engineering | Selenophene-based semiconducting polymer (p(g2T-Se)) | Mouse subcutaneous implant | Collagen Density (after 4 weeks) | ~50% decrease vs. control | [18] |
| Side-Chain Functionalization | p(g2T-Se) with TMO group | Mouse subcutaneous implant | Collagen Density (after 4 weeks) | ~68% decrease vs. control | [18] |
| Side-Chain Functionalization | p(g2T-Se) with THP group | Mouse subcutaneous implant | Macrophage Population (CD68+) | ~68% suppression | [18] |
| Side-Chain Functionalization | p(g2T-Se) with TMO group | Mouse subcutaneous implant | Myofibroblast Population (α-SMA+) | ~79% suppression | [18] |
| Passive Coating | Hydrogel membranes | Rodent subcutaneous implant | Fibrous Encapsulation | Significant reduction vs. uncoated | [65] |
| Physical Design | Ultra-thin, flexible neural probes | Rodent brain implant | Chronic Inflammatory Response | Mitigated vs. rigid implants | [63] [64] |
Table 2: Electrical Performance of FBR-Suppressing Polymers
| Polymer | Key Modification | Charge-Carrier Mobility (cm²V⁻¹s⁻¹) | FBR Suppression | |
|---|---|---|---|---|
| p(g2T-T) (Control) | Thiophene backbone | ~1 | Baseline | [18] |
| p(g2T-Se) | Selenophene backbone | ~1 | Moderate | [18] |
| p(g2T-Se)-TMO | Selenophene + TMO side-chain | ~1 | High | [18] |
| p(g2T-Se)-THP | Selenophene + THP side-chain | ~1 | High | [18] |
Experimental Protocols for Functional Validation
Protocol 1: In Vivo Validation of Fibrous Encapsulation for Subcutaneous Devices
This protocol is used to quantitatively assess the FBR to implanted sensors or drug delivery ports.
- Implantation: Aseptically implant the device subcutaneously in an animal model (e.g., mouse or rat).
- Explanation: After a pre-determined period (e.g., 4 weeks), euthanize the animal and carefully explant the device with the surrounding tissue.
- Fixation and Sectioning: Fix the tissue in 4% paraformaldehyde, process, and embed in paraffin. Section the tissue to a thickness of 5-10 µm.
- Staining: Perform Masson's Trichrome staining on tissue sections. This stains collagen fibers blue, muscle fibers red, and cell nuclei dark brown/black.
- Imaging and Quantification: Use bright-field microscopy to image the tissue-device interface. The collagen density can be quantified as the percentage of blue pixels in a defined region of interest using image analysis software (e.g., ImageJ) [18].
Protocol 2: In Vitro Macrophage Activation Assay for Material Biocompatibility
This protocol tests the intrinsic immunomodulatory properties of a new material.
- Material Preparation: Sterilize material samples and place them in a cell culture plate.
- Cell Seeding: Seed a macrophage cell line (e.g., RAW 264.7) onto the material samples and control surfaces.
- Stimulation: Stimulate the macrophages with a potent inflammatory trigger like lipopolysaccharide (LPS).
- Analysis:
- PCR: After 24 hours, extract RNA and perform quantitative PCR (qPCR) to measure the expression of pro-inflammatory biomarkers (e.g., IL-6, IL-1β, TNF-α) [18].
- Cytokine Assay: Collect the cell culture supernatant and analyze it using an ELISA or multiplex cytokine array to quantify the secretion of pro-inflammatory cytokines [18].
The Scientist's Toolkit
Table 3: Essential Research Reagents for FBR and Device Validation Studies
| Reagent / Material | Function in Research |
|---|---|
| Selenophene-based polymers | Semiconducting polymer backbone modification to mitigate FBR through antioxidant effects [18] [17]. |
| Immunomodulatory side chains (THP, TMO) | Chemical groups attached to polymer side chains to downregulate pro-inflammatory pathways in immune cells [18]. |
| Anti-CD68 antibody | Immunohistochemistry marker for identifying and quantifying macrophages in tissue sections [18]. |
| Anti-α-SMA antibody | Immunohistochemistry marker for identifying myofibroblasts, key cells in fibrotic capsule formation [18]. |
| Masson's Trichrome Stain | Histological stain to visualize and quantify collagen deposition (fibrosis) around explanted devices [18]. |
| PEDOT:PSS | A conductive polymer coating used to lower electrode impedance and improve the signal-to-noise ratio in neural interfaces [63]. |
| Biocompatible Hydrogels | Used as sensor membranes or soft coatings to mimic tissue mechanics and improve integration [63] [65]. |
Signaling Pathways and Experimental Workflows
Diagram Title: Foreign Body Response Signaling Pathway and Intervention Points
Diagram Title: Functional Validation Workflow for Implantable Bioelectronics
Frequently Asked Questions (FAQs)
Q1: What is the primary biocompatibility issue limiting the functional longevity of implantable bioelectronics? A1: The primary issue is the foreign-body response (FBR), an immune-mediated reaction to implanted materials. This response begins with protein adsorption, which triggers a cascade of immune cell recruitment, foreign body giant cell (FBGC) formation, and collagen deposition, eventually encapsulating the functional implant in fibrotic tissue [18] [20]. This fibrotic barrier substantially increases the device-tissue interface impedance, hindering the transduction of electrical or chemical signals and limiting the device's lifespan [17] [18].
Q2: My team has developed a novel semiconducting polymer. Beyond standard cytotoxicity tests, what specific in vivo assays are critical for a rigorous assessment of the elicited Foreign Body Response (FBR)? A2: To move beyond basic in vitro tests, a rigorous in vivo FBR assessment should include the following key methodologies [18]:
- Implantation Model: Subcutaneously implant polymer thin films (supported by a substrate like SEBS) into mouse dorsal regions for periods of one and four weeks to study both acute and chronic phases [18].
- Histological Staining and Quantification:
- Protocol: After explant, tissue sections are stained with Masson’s Trichrome (MT) to visualize collagen deposition.
- Quantification: Analyze the stained tissue sections by measuring the blue pixel density, which corresponds to collagen density at the polymer-tissue interface [18].
- Gene Expression Analysis:
- Protocol: Use quantitative PCR (qPCR) on tissue samples from the area surrounding the implant.
- Quantification: Measure the mRNA expression levels of specific biomarkers, primarily collagen type I and type III, which are the main components of the fibrotic capsule [18].
- Immunofluorescence Staining:
- Protocol: Stain tissue sections with fluorescently-labeled antibodies.
- Quantification: Image and count populations of key immune cells, such as macrophages (using CD68 antibody) and myofibroblasts (using α-SMA antibody) [18].
- Inflammatory Cytokine Profiling:
- Protocol: Analyze tissue homogenates or serum using multiplex immunoassays (e.g., ELISA or Luminex).
- Quantification: Measure the expression levels of a panel of pro-inflammatory and anti-inflammatory biomarkers, including IFN-γ, IL-6, IL-1β, MCP-1, and IL-10 [18].
Q3: We are exploring molecular design strategies to create intrinsically immune-compatible semiconducting polymers. What are some proven design elements that suppress the Foreign Body Response? A3: Recent research has identified two key molecular design strategies that intrinsically suppress FBR while maintaining electrical performance [17] [18] [20]:
- Backbone Engineering: Replace thiophene units in the polymer backbone with selenophene. This element has demonstrated antioxidant properties that mitigate FBR by suppressing macrophage activation and scavenging reactive oxygen species (ROS) [18] [20].
- Side-Chain Functionalization: Incorporate specific immunomodulatory groups at the ends of the polymer's side chains. Two groups shown to be effective are:
- Triazole-tetrahydropyran (THP)
- Triazole-thiomorpholine 1,1-dioxide (TMO) These groups downregulate the expression of pro-inflammatory biomarkers [18].
Q4: What quantitative improvements in FBR suppression and electrical performance can be expected from these immune-compatible designs? A4: The combination of backbone and side-chain engineering has shown significant quantitative improvements, as summarized in the table below.
| Performance Metric | Result with Immune-Compatible Designs | Experimental Context |
|---|---|---|
| Collagen Density | Up to 68% decrease [18] [20] | Measured via Masson's Trichrome staining after 4-week mouse implantation [18]. |
| Macrophage Population | ~68% decrease (CD68+ cells) [18] | Measured via immunofluorescence after 4-week implantation [18]. |
| Myofibroblast Population | ~79% decrease (α-SMA+ cells) [18] | Measured via immunofluorescence after 4-week implantation [18]. |
| Charge-Carrier Mobility | Maintained at ~1 cm² V⁻¹ s⁻¹ (up to 1.2 for selenophene backbone) [18] [20] | Measured in Organic Electrochemical Transistor (OECT) devices [18]. |
| In Vivo Signal Amplitude | Significantly higher signal retention after 4 weeks [20] | Chronic recording of ECG/EMG signals in live mice [20]. |
Troubleshooting Guides
Problem: High Collagen Density and Fibrotic Encapsulation Around Implanted Material
- Potential Cause 1: The chemical structure of your polymer is triggering a strong pro-inflammatory response.
- Solution:
- Potential Cause 2: A mechanical mismatch between the stiff implant and soft tissue exacerbates the FBR.
- Solution: Integrate the chemical designs above with low-modulus substrate materials (e.g., soft hydrogels or SEBS) to better mimic tissue mechanics and alleviate mechanical stress [18] [20].
Problem: Inconsistent or Poor Electrical Performance in Bioelectronic Devices After Implantation
- Potential Cause: The developing fibrotic capsule is acting as an insulating layer, increasing interface impedance and blocking signal transduction [17] [18].
- Solution:
- Implement the immune-compatible polymer designs (selenophene backbone + THP/TMO side chains) to suppress fibrotic formation from the outset [18] [20].
- Validate performance using in vivo OECT measurements over extended periods (e.g., 3 months) to demonstrate long-term stability and current retention [20].
Problem: Difficulty in Mechanistically Understanding How a Material Modification Suppresses FBR
- Potential Cause: Reliance on endpoint histology alone without profiling the dynamic immune response.
- Solution: Conduct a comprehensive analysis of inflammatory biomarkers. This will determine if your design effectively:
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in FBR Research |
|---|---|
| p(g2T-T) Polymer | A high-performance semiconducting polymer used as a base or control structure for implementing new immune-compatible designs [18] [20]. |
| Selenophene | A backbone unit that replaces thiophene to confer immunomodulatory properties, mitigating macrophage activation and FBR [18]. |
| THP (Triazole-tetrahydropyran) | An immunomodulatory group attached to polymer side chains to downregulate pro-inflammatory biomarker expression [18]. |
| TMO (Triazole-thiomorpholine 1,1-dioxide) | An immunomodulatory group attached to polymer side chains to suppress collagen deposition and immune cell recruitment [18]. |
| SEBS Substrate | A flexible polymer used as a supportive substrate for semiconducting polymer films during in vivo implantation studies [18]. |
| Antibody: Anti-CD68 | Used for immunofluorescence staining to identify and quantify macrophage populations in tissue surrounding the implant [18]. |
| Antibody: Anti-α-SMA | Used for immunofluorescence staining to identify and quantify myofibroblasts, the cells responsible for collagen production in fibrotic tissue [18]. |
Experimental Workflow and Signaling Pathways
Diagram 1: The Foreign Body Response Cascade leading to device failure.
Diagram 2: Immune-compatible polymer design strategies and outcomes.
Conclusion
The successful mitigation of the foreign body response is paramount for the future of chronic bioelectronic implants. The synthesis of research across immunology and materials science demonstrates that a multi-pronged approach—combining immunomodulatory chemistry, mechanical compatibility, and sophisticated device design—holds the key to durable device integration. Promising future directions include the refinement of 'immune-instructive' biomaterials that actively guide healing, the development of advanced in vitro human immune models for faster screening, and the clinical translation of biohybrid and 'all-living' interfaces. By systematically addressing FBR, the next generation of bioelectronics will achieve unprecedented longevity and functionality, unlocking their full potential for treating a wide range of chronic diseases.
References
- 1. Exploring the Overlooked Roles and Mechanisms of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10081717/]
- 2. Domesticating the Foreign Body Response: Recent Advances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6774350/]
- 3. Advanced strategies to thwart foreign body response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9472022/]
- 4. Foreign Body Reaction to Implanted Biomaterials and Its ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.622524/full]
- 5. Overcoming failure: improving acceptance and success of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00168-7]
- 6. Advances in bioelectronics for neural interfacing [https://link.springer.com/article/10.1557/s43579-025-00822-w]
- 7. Immunocompatible elastomer with increased resistance to ... [https://www.nature.com/articles/s41467-024-52023-z]
- 8. Decoding Fibrotic Encapsulation in Plastic Surgery implants [https://www.sciencedirect.com/science/article/abs/pii/S0927776525006988]
- 9. Macrophages and fibroblasts in foreign body reactions [https://pmc.ncbi.nlm.nih.gov/articles/PMC10494263/]
- 10. Foreign Body Reaction to Implanted Biomaterials and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8081831/]
- 11. Macrophage and Fibroblast Interactions in Biomaterial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6415913/]
- 12. Cellular and microenvironmental cues that promote ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1411872/full]
- 13. Foreign Body Reaction to Neural Implants: A Comparative ... [https://www.mdpi.com/2079-6374/15/9/599]
- 14. Immune-compatible designs of semiconducting polymers for ... [https://pubmed.ncbi.nlm.nih.gov/40247019/]
- 15. Dynamic fibroblast contractions attract remote ... [https://www.nature.com/articles/s41467-019-09709-6]
- 16. Biomimetic optimization of silicone breast implant integration [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1668930/full]
- 17. Study could point way to reducing scar tissue around ... [https://news.uchicago.edu/story/study-could-point-way-reducing-scar-tissue-around-implants]
- 18. Immune-compatible designs of semiconducting polymers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355568/]
- 19. Adhesive nonfibrotic bioelectronic interfaces on diverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12588291/]
- 20. Implantable semiconducting polymers with low foreign- ... [https://communities.springernature.com/posts/implantable-semiconducting-polymers-with-low-foreign-body-response]
- 21. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 22. Overcoming immune hurdles to implant longevity [https://www.nature.com/articles/s41551-024-01276-6]
- 23. Introductory Review of Soft Implantable Bioelectronics Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11506957/]
- 24. Reducing the foreign body response on human cochlear ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706123002581]
- 25. Reducing the foreign body response on human cochlear ... [https://pubmed.ncbi.nlm.nih.gov/37187301/]
- 26. Hierarchical micro-nano topographies to control Bacteria ... [https://www.nature.com/articles/s41598-025-08415-2]
- 27. Dynamic actuation enhances transport and extends ... [https://www.nature.com/articles/s41467-022-32147-w]
- 28. Bio-inspired electronics : Soft, biohybrid, and... | Nature Communications [https://www.nature.com/articles/s41467-025-57016-0?error=cookies_not_supported&code=7517b609-3cd0-41bd-a49f-b7c5618ecaa7]
- 29. Engineering Smart Hybrid Tissues with Built-In Electronics [https://pmc.ncbi.nlm.nih.gov/articles/PMC6994631/]
- 30. Understanding Bioelectronics [https://www.cellink.com/blog/understanding-bioelectronics/]
- 31. Bio-electric-electronics and tissue engineering applications ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894724027177]
- 32. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 33. How to Troubleshoot Experimental Protocols in the Lab [https://www.linkedin.com/advice/1/what-some-strategies-troubleshooting-experimental-jekfe]
- 34. Bio-inspired poly-DL-serine materials resist the foreign- ... [https://www.nature.com/articles/s41467-021-25581-9]
- 35. Implants better accepted by the immune system [https://pme.uchicago.edu/news/implants-better-accepted-immune-system]
- 36. Macrophage Polarization: Learning to Manage It 2.0 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10743686/]
- 37. Macrophage Polarization - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/macrophage-polarization]
- 38. Macrophage phenotypes in tissue repair and the foreign body ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8464623/]
- 39. Macrophages and fibroblasts in foreign body reactions [https://www.sciencedirect.com/science/article/pii/S2590006423002430]
- 40. Material and design strategies for chronically-implantable ... [https://www.nature.com/articles/s41427-025-00613-8]
- 41. Understanding the Effects of Both CD14-Mediated Innate ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2018.00772/full]
- 42. Mechanical failure modes of chronically implanted planar ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4312222/]
- 43. Characterization of Mechanically Matched Hydrogel ... [https://www.nature.com/articles/s41598-017-02107-2]
- 44. Neural tissue-microelectrode interaction: Brain ... [https://www.sciencedirect.com/science/article/abs/pii/S016502702100323X]
- 45. S100A8/A9 promotes endometrial fibrosis via regulating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10803310/]
- 46. S100A8/A9 in Inflammation [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.01298/full]
- 47. S100A8/A9 promotes parenchymal damage and renal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6150262/]
- 48. Polymers for anti - fouling applications: a review - Environmental... [https://pubs.rsc.org/en/content/articlehtml/2025/va/d5va00034c]
- 49. Current status, challenges and prospects of antifouling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11109453/]
- 50. Mitigating the foreign body response through 'immune ... [https://www.sciencedirect.com/science/article/abs/pii/S2468498821000032]
- 51. Antifouling Strategies of Nanoparticles for Diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8003124/]
- 52. Cell-scale porosity minimizes foreign body reaction and ... [https://www.nature.com/articles/s41536-025-00395-1]
- 53. Size- and shape-dependent foreign body immune response to ... [https://pubmed.ncbi.nlm.nih.gov/25985456/]
- 54. Towards predicting implant-induced fibrosis: A standardized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312070/]
- 55. In vitro and in vivo models for assessing the host response ... [https://www.sciencedirect.com/science/article/abs/pii/S1740675717300518]
- 56. In Vitro and In Vivo Models for Assessing the Host Response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6251320/]
- 57. Histological Characterization of Human Breast Implant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4434852/]
- 58. Immunocompatible elastomer with increased resistance to the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11364871/]
- 59. Adipose-derived mesenchymal stem cells for the prevention of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12449375/]
- 60. FOREIGN BODY REACTION TO BIOMATERIALS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2327202/]
- 61. Polymeric “smart” coatings to prevent foreign body ... [https://www.sciencedirect.com/science/article/abs/pii/S016836591200870X]
- 62. Immune-compatible designs of semiconducting... | Nature Materials [https://www.nature.com/articles/s41563-025-02213-x?error=cookies_not_supported&code=23252705-26d5-4109-9da9-7ee7e9d636ac]
- 63. Bio-inspired electronics: Soft, biohybrid, and “living” neural ... [https://www.nature.com/articles/s41467-025-57016-0]
- 64. A Materials Roadmap to Functional Neural Interface Design [https://pmc.ncbi.nlm.nih.gov/articles/PMC5963731/]
- 65. Glucose Sensor Membranes for Mitigating the Foreign ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3208860/]
- 66. Modulating the Foreign Body Response of Implants for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8217111/]
- 67. What to Do If Your Insulin Pump Malfunctions [https://www.healthline.com/health/diabetes/what-to-do-if-your-insulin-pump-malfunctions]