Soft and Flexible Bioelectronics: Materials Design, Clinical Applications, and Future Directions for Advanced Healthcare
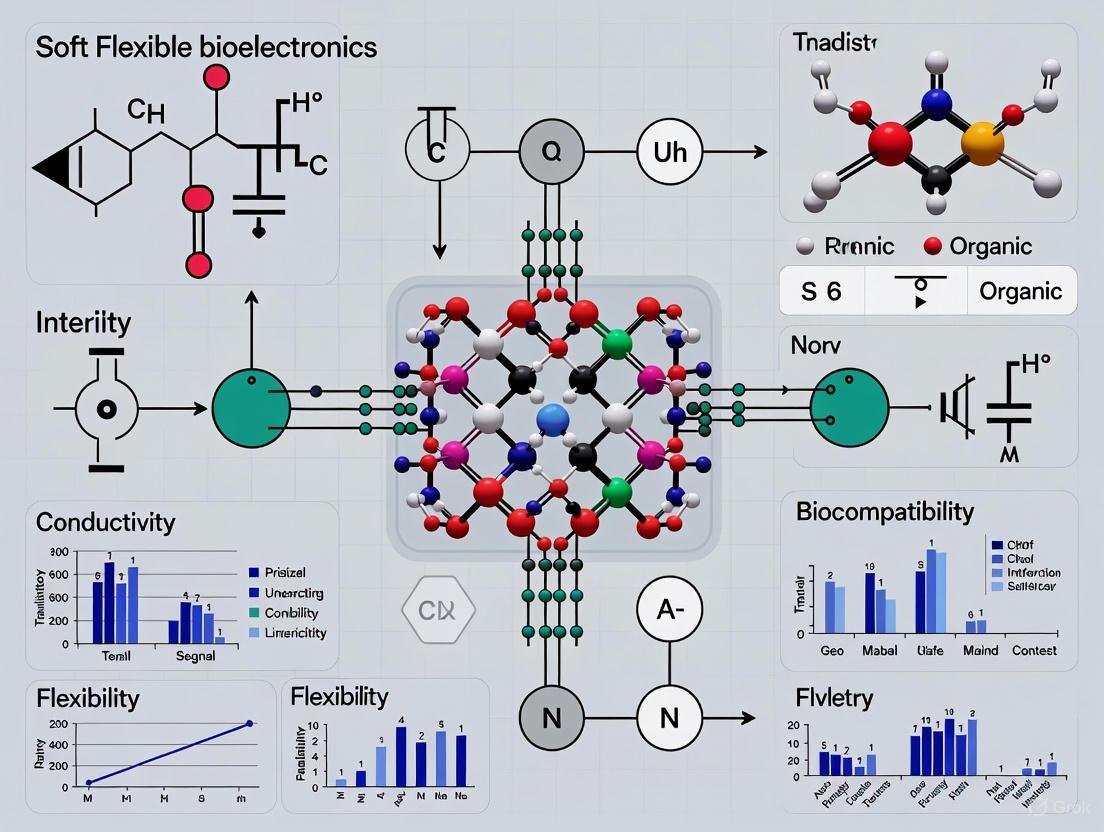
This article provides a comprehensive review of the latest advancements in soft and flexible bioelectronic materials, a field poised to revolutionize digital healthcare and biomedical research.
Soft and Flexible Bioelectronics: Materials Design, Clinical Applications, and Future Directions for Advanced Healthcare
Abstract
This article provides a comprehensive review of the latest advancements in soft and flexible bioelectronic materials, a field poised to revolutionize digital healthcare and biomedical research. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of tissue-like electronics designed to overcome the mechanical mismatch with biological systems. The scope spans from novel material designs—including hydrogels, liquid metals, and conductive polymers—to their fabrication and integration into wearable and implantable devices for continuous health monitoring and closed-loop therapeutic interventions. Further, it delves into critical challenges such as long-term stability, signal fidelity, and biocompatibility, offering troubleshooting and optimization strategies. Finally, the article presents a comparative analysis of material performance and validation frameworks essential for clinical translation, synthesizing key takeaways to outline a future roadmap for the field.
The Foundation of Soft Bioelectronics: Overcoming the Mechanical Mismatch with Biological Tissues
The development of bioelectronic devices for medical applications is fundamentally constrained by a pervasive biomechanical incompatibility: the rigid, static nature of conventional electronics is a poor match for the soft, dynamic, and water-rich environment of human tissues. This mechanical mismatch can lead to inaccurate signal acquisition, tissue damage, chronic inflammation, and device failure [1] [2]. This whitepaper delineates the core principles of this challenge, details emerging solutions centered on soft materials and innovative fabrication techniques, and provides a technical overview of the experimental methodologies and reagent solutions driving the field of soft bioelectronics forward. The content is framed within a broader thesis that overcoming this mechanical mismatch is paramount for the next generation of seamless, biocompatible human-machine interfaces.
Living tissues are soft, elastic, and constantly in motion—from the pulsations of the heart and brain to the subtle shifts of skin and muscle. The mechanical properties of these tissues, such as Young's modulus (a measure of stiffness), are typically in the kilopascal (kPa) to megapascal (MPa) range [3] [4]. In stark contrast, the silicon and metals that form the backbone of conventional electronics are rigid and brittle, with Young's moduli orders of magnitude higher (in the gigapascal, GPa, range). This stark difference creates a fundamental incompatibility at the bio-electronic interface.
When a rigid device is implanted or attached to soft tissue, the resulting mechanical mismatch can cause several critical issues:
- Reduced Treatment Effectiveness: Unstable contact leads to motion artifacts and unreliable data [1] [5].
- Tissue Damage: The persistent rubbing and pressure from a rigid device can damage delicate cellular structures [1].
- Chronic Immune Response: The body recognizes the rigid device as a foreign body, triggering inflammation and fibrotic encapsulation, which can isolate the device and degrade its performance over time [2] [6].
- Device Failure: The inability of a rigid device to withstand repeated stretching and bending can lead to mechanical fracture and electronic failure [5].
The following table quantifies the mechanical properties of various biological tissues and conventional electronic materials, illustrating the core of the challenge.
Table 1: Quantitative Comparison of Mechanical Properties between Soft Tissues and Conventional Electronics
| Material / Tissue | Young's Modulus | Key Characteristics |
|---|---|---|
| Human Soft Tissues | ||
| Human Normal Liver | ~10 kPa [3] | Soft, easily deformable |
| Human Diseased Liver | ~52 kPa [3] | Stiffer than healthy tissue |
| Breast Benign Lesion | ~146 kPa [3] | Moderately stiff |
| Breast Malignant Lesion | ~270 kPa [3] | Significantly stiffer |
| Articular Cartilage | ~0.7 - 1 MPa [3] | Resilient, load-bearing |
| Conventional Electronics | ||
| Silicon (Si) | ~130 - 190 GPa [2] | Rigid, brittle |
| Gold (Au) | ~78 GPa | Dense, malleable but not stretchable |
| Copper (Cu) | ~110 - 128 GPa | High conductivity, rigid |
Experimental Methodologies for Characterization and Validation
Overcoming the mechanical mismatch requires a deep understanding of both the tissue's properties and the device's performance under realistic conditions. The following sections describe key experimental protocols used in the field.
Protocol: Water Jet Indentation for Soft Tissue Modulus Characterization
This non-contact method is used to quantitatively image the elastic modulus of soft tissues with high resolution [3].
1. Principle: A jet of water serves as a soft indenter to deform the tissue, while high-frequency ultrasound (e.g., 50 MHz) propagating through the same water jet simultaneously measures the resulting tissue deformation and thickness.
2. Experimental Setup:
- Apparatus: A 3D translating device holds a water container connected via a pressure sensor to a nozzle and an ultrasound transducer.
- Key Parameters: Nozzle diameter (e.g., 1.7 mm), distance from nozzle to tissue (e.g., 0.95 mm), water flow speed (1-10 m/s).
3. Procedure:
- The water jet is focused on the tissue surface using the 3D translator.
- The pressure sensor records the indentation force (F), while ultrasound measures the indentation depth (d) and tissue thickness (h).
- The system performs a C-scan to obtain a modulus map of the region of interest.
4. Data Analysis - Improved Hayes' Equation:
Young's modulus (E) is calculated using a finite element (FE)-validated improvement of Hayes' equation:
E = (1 - v²) / (2a * k(v, a/h, d/h)) * (F/d)
where v is Poisson's ratio, a is the indenter radius, and k is a scaling factor dependent on v, aspect ratio (a/h), and deformation ratio (d/h). This model allows quantitative evaluation of E with an error of no more than 2% [3].
Protocol: In Vivo Performance Testing of Stretchable Bioelectronic Devices
This protocol validates the functionality and biocompatibility of novel soft devices in biologically relevant environments [1] [5].
1. Device Fabrication:
- Liquid Metal-Based Electronics: A combination of colloidal self-assembly and micro-transfer printing is used to pattern liquid metal particles (e.g., gallium-based alloys) with micrometer-scale resolution onto stretchable substrates, creating electronics that can withstand over 1,200% stretching [1].
- Organic Electrochemical Transistors (OECTs): Asymmetric transistors are fabricated from a single, biocompatible organic polymer material that interacts with biological ions. This simplifies fabrication and enhances biocompatibility [5].
2. Functional Testing:
- Strain Sensing: Devices are subjected to controlled, large deformations to validate the reliability of electrical conductivity and sensing accuracy under extreme stretching.
- Cardiac Electrophysiological Mapping: Instrumented balloon catheters with liquid metal microelectrode arrays are inflated inside explanted human hearts or animal models. Electrical impedance and the ability to acquire high-resolution maps of cardiac electrical activity are measured [1].
- Chronic Neural Recording: Soft transistor-based sensor implants are placed on the brain of developing animals. The quality of acquired neural signals is monitored over time to assess the device's ability to maintain a stable bio-interface through tissue growth and structural changes [5].
3. Biocompatibility Assessment:
- Histological analysis is performed on the surrounding tissue after a predetermined implantation period to check for signs of inflammation or fibrosis compared to controls with rigid implants.
The Scientist's Toolkit: Research Reagent Solutions
The advancement of soft bioelectronics relies on a specific set of material solutions designed to bridge the mechanical and chemical divide with biological systems.
Table 2: Essential Materials and Reagents for Soft Bioelectronics Research
| Reagent / Material | Function and Rationale |
|---|---|
| Liquid Metal Alloys (e.g., EGaIn) | Serves as a highly conductive yet deformable interconnect and electrode material; enables extreme stretchability (>1200%) while maintaining electrical function [1]. |
| Conductive Organic Polymers (e.g., PEDOT:PSS) | Provides a mixed ionic-electronic conductivity, facilitating efficient communication with biological systems (which use ions); is inherently softer and more biocompatible than inorganic semiconductors [2] [5]. |
| Functionalized Hydrogels | Acts as a hydrated, porous, and tissue-like scaffold/encapsulation; allows diffusion of biomolecules and drugs, enhancing biosensing and therapeutic functions [6]. |
| Stretchable Conductive Nanocomposites | Combines conductive nanomaterials (e.g., metal nanowires, graphene) with elastic polymers (e.g., PDMS); creates a percolation network that maintains conductivity under strain [2]. |
| Hydrogel Semiconductors | A nascent class of materials that are both semiconductor and hydrogel simultaneously; provides tissue-like mechanical properties (softness, hydration) with semiconductive ability, enabling intimate biointerfaces with augmented sensing and photo-modulation effects [6]. |
Visualizing the Development Workflow for Soft Bioelectronics
The following diagram synthesizes the logical workflow and key decision points in developing a solution to the mechanical mismatch challenge, from problem identification to functional application.
The evolution of soft and flexible bioelectronics represents a paradigm shift in the interface between artificial devices and biological systems. The fundamental challenge in this field stems from the profound mechanical mismatch between conventional rigid, planar electronics and the soft, curvilinear, and dynamic structures of biological tissues. This mechanical disparity can lead to inaccurate signal acquisition, tissue damage, and chronic inflammatory responses, ultimately causing device failure [7]. To overcome these limitations, a new class of electronic materials has emerged, defined by three core properties: stretchability, the ability to withstand mechanical deformation without functional degradation; conformability, the capacity to form stable, intimate contact with irregular biological surfaces; and tissue-mimicking softness, the replication of the low elastic modulus characteristic of biological tissues. This technical guide delineates the definitions, measurement methodologies, and material strategies for achieving these essential properties, providing a framework for the next generation of biointegrated devices.
Quantitative Definitions and Material Targets
For researchers, establishing clear quantitative targets is the first step in material selection and device design. The following tables summarize the key mechanical properties of biological tissues and the performance targets for bioelectronic materials.
Table 1: Mechanical Properties of Biological Tissues and Conventional Materials
| Material/Tissue | Young's Modulus | Key Characteristics |
|---|---|---|
| Myocardial Tissue | 10-15 kPa [7] | Represents a key target for cardiac implants. |
| Soft Bio-tissues | ~10 kPa [8] | General modulus for many internal organs and soft structures. |
| Human Skin | Varies by region and layer | Dynamic, curvilinear, and anisotropic. |
| Conventional Elastomers (e.g., PDMS, SEBS) | ~1-3 MPa [8] | 2-3 orders of magnitude stiffer than soft tissues. |
| Stretchable Electronic Materials (conductors, semiconductors) | >100 MPa [8] | Intrinsically high modulus necessitates novel softening strategies. |
| Bulk Silicon | ~100 GPa [7] | The basis of traditional electronics, fundamentally mismatched with biology. |
Table 2: Target Properties for Bioelectronic Materials and Devices
| Property | Target Value / Performance Metric | Application Implication |
|---|---|---|
| Effective Device Modulus | < 10 kPa [8] | Achieves tissue-level softness for minimized mechanical mismatch. |
| Interfacial Toughness | > 100 J m⁻² [8] | Ensures strong adhesion between device layers and to tissue. |
| Stretchability | > 100% strain without electrical/functional failure [8] | Withstands dynamic movement of organs and skin. |
| Device Thickness | < 5 μm for conformability [9] | Ultralow bending stiffness for van der Waals-driven adhesion to skin. |
Material Strategies and Experimental Methodologies
Achieving Tissue-Mimicking Softness
While material synthesis has produced softer conductors and semiconductors, a powerful generalizable strategy is the soft interlayer design [8]. This approach allows the use of existing high-performance (but relatively high-modulus) stretchable materials by engineering the mechanical structure of the device.
- Working Principle: A thin soft interlayer with an intermediate modulus is inserted between the functional electronic film (e.g., semiconductor) and an ultrasoft substrate (e.g., hydrogel). This interlayer reduces stress concentration at defect sites in the functional layer during stretching, dramatically improving its effective stretchability.
- Validated Material System:
- Functional Layer: DPPT-TT/SEBS polymer semiconductor (modulus: 19.4 MPa).
- Soft Interlayer: SEBS H1052 (modulus: 2.83 MPa).
- Ultrasoft Substrate: Ecoflex-0010 (modulus: 55 kPa) or Polyacrylamide (PAAm) hydrogel.
- Critical Design Parameters:
- Interlayer Modulus: Should be within three orders of magnitude of the functional layer.
- Interlayer Thickness: At least ten times thicker than the functional layer (e.g., 200 nm to 2 μm for a semiconductor film).
- Adhesion: Interfacial toughness should exceed 100 J m⁻².
Measuring and Ensuring Conformability
Conformability is governed by a device's bending stiffness and its adhesion to the biological surface. A key metric is the bending stiffness (D), calculated as D = Eh³ / (12(1-ν²)), where E is the elastic modulus, h is the thickness, and ν is the Poisson's ratio.
- Strategy: To achieve conformal contact on skin, devices must be engineered to be ultrathin and flexible, minimizing bending stiffness. This allows for van der Waals-driven adhesion without external adhesives [9].
- Experimental Validation:
- Method: Finite-element analysis (FEA) simulating device attachment to a rough, curved surface.
- Measurement: 180° peeling tests to quantify interfacial toughness and adhesion energy between device layers and to model biological surfaces [8].
Engineering Intrinsic Stretchability
Stretchability can be imparted through a combination of material-level and structure-level engineering.
- Intrinsically Stretchable Materials:
- Structural Engineering:
- Architectural Designs: Employing serpentine mesh layouts, kirigami/origami patterns, and horseshoe shapes to allow the device to accommodate strain through out-of-plane deformation rather than material stretching [7] [11].
- Neutral Mechanical Plane Design: Placing stiff, brittle electronic components at the neutral mechanical plane within a soft encapsulation matrix to minimize strain on these components during bending [9].
Experimental Protocols for Characterization
Protocol: Finite-Element Analysis of a Soft Interlayer Design
This FEA protocol validates the mechanical function of a soft interlayer before fabrication.
- Model Setup: Create a three-layer 2D model representing the functional film, soft interlayer, and ultrasoft substrate.
- Introduce Defect: Incorporate a notch (pre-crack) into the functional film to study stress concentration.
- Apply Boundary Conditions: Fix one end of the model and apply a uniaxial tensile strain (e.g., 100%) to the other end.
- Parameter Sweep:
- Modulus: Vary the Young's modulus of the interlayer from MPa to GPa ranges.
- Thickness: Vary the interlayer thickness from nanometers to micrometers.
- Adhesion: Model different levels of delamination (poor adhesion) around the notch.
- Output Analysis: Map the principal stress and strain energy density at the notch tip. A successful design shows a significant reduction in these stress concentration metrics compared to a no-interlayer structure [8].
Protocol: Mechanical and Electrical Characterization under Strain
This experiment quantifies the stretchability and softness of a functional electronic material or device.
- Sample Preparation: Fabricate the thin-film material or device (e.g., transistor, conductor) on the target soft substrate with the designed interlayer.
- Mounting: Clamp the sample onto a uniaxial tensile stage.
- In-Situ Measurement:
- Mechanical: Apply incremental strain steps (e.g., 10% steps up to 100% strain). Use an optical microscope or digital image correlation (DIC) at each step to record crack density and propagation.
- Electrical: Simultaneously measure the key electrical property (e.g., conductivity for a conductor, charge-carrier mobility for a semiconductor transistor) at each strain step.
- Data Analysis: Plot electrical performance versus applied strain. The strain value at which the performance degrades by a predefined threshold (e.g., 50%) defines the functional stretchability of the device [8].
Diagram 1: Workflow for FEA of a soft interlayer design.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Soft Bioelectronics Research
| Category | Material / Reagent | Function / Key Property | Example Use Case |
|---|---|---|---|
| Substrates & Encapsulation | Polyacrylamide (PAAm) Hydrogel | Ultrasoft substrate (modulus ~kPa). | Achieving tissue-level effective modulus [8]. |
| Polydimethylsiloxane (PDMS) | Conventional elastomer substrate (modulus ~MPa). | Flexible, but not tissue-soft, substrate [7]. | |
| Parylene-C | Biostable, ultrathin encapsulation/substrate. | Flexible OECTs for ECG sensing [9]. | |
| Interlayer Materials | SEBS H1052 | General-purpose soft interlayer (modulus 2.83 MPa, high adhesion). | Enabling stretchable semiconductors on ultrasoft substrates [8]. |
| Conductors | PEDOT:PSS/PFI blend | Stretchable transparent conductor. | Electrodes for biosignal recording [8] [9]. |
| Carbon Nanotube (CNT) assembly | Stretchable conductor network. | Gate, drain, and source electrodes in transistors [8]. | |
| Silver Nanowire (AgNW) | Stretchable conductor, high conductivity. | Transparent electrodes for OECTs [8] [9]. | |
| Semiconductors | DPPT-TT/SEBS blend | Stretchable polymer semiconductor. | Channel material in ultrasoft transistors [8]. |
| Characterization Tools | Peeling Test Stage | Quantifies interfacial toughness (J m⁻²). | Measuring adhesion strength between device layers [8]. |
| Tensile Stage with Microscope | Measures crack propagation under strain. | Characterizing functional stretchability [8]. |
Diagram 2: Core characterization methods for key material properties.
The convergence of stretchability, conformability, and tissue-mimicking softness is redefining the possibilities for biointegrated electronics. Moving beyond simple flexibility, the field now prioritizes an ultralow modulus to achieve seamless and stable integration with biological systems. The material strategies and experimental frameworks outlined in this guide—centered on the soft interlayer design, intrinsically stretchable composites, and ultrathin architectures—provide a foundational toolkit for researchers. The future trajectory of this field points toward the development of fully biodegradable and bioactive material systems that not only match the passive mechanics of tissue but also actively participate in biological signaling and self-repair processes [12] [7]. By adhering to the quantitative targets and rigorous characterization protocols defined herein, scientists can accelerate the development of next-generation bioelectronics for advanced diagnostics, therapeutics, and a truly symbiotic human-machine interface.
The emergence of soft and flexible bioelectronics represents a paradigm shift in the development of medical devices, diagnostic tools, and therapeutic systems. Traditional rigid electronic components face significant challenges in interfacing with biological tissues, which are inherently soft, dynamic, and aqueous. This mismatch in mechanical properties often leads to poor contact, signal interference, low signal conversion efficiency, and inflammatory responses [13]. Within this context, three key material classes—hydrogels, liquid metals, and conductive polymers—have emerged as foundational elements for next-generation bioelectronic interfaces.
These materials collectively address the critical need for mechanical compatibility with biological systems while maintaining excellent electronic functionality. Hydrogels provide tissue-like softness and biocompatibility, liquid metals offer unparalleled stretchability and self-healing capabilities, and conductive polymers bridge the gap between organic electronics and biological interfaces. This technical guide provides an in-depth examination of these three material classes, focusing on their fundamental properties, synthesis methodologies, and applications in soft bioelectronics, with particular emphasis on their roles in biomedical research and drug development.
Table 1: Core Characteristics of Key Material Classes in Soft Bioelectronics
| Material Class | Key Properties | Primary Strengths | Inherent Limitations |
|---|---|---|---|
| Hydrogels | Tissue-like softness, high water content, biocompatibility, tunable mechanical properties [14] [15] | Excellent biocompatibility, permeable to biomolecules, customizable physical properties | Low electrical conductivity (pristine), mechanical fragility, environmental instability [16] |
| Liquid Metals | Fluidic nature, high electrical (3.4×10⁶ S/m) and thermal conductivity, stretchability, self-healing [17] | Extreme deformability (>1000% strain), negligible fatigue, shape reconfigurability | Surface oxidation challenges, difficult patterning/packaging, long-term stability concerns [18] |
| Conductive Polymers | Conjugated backbone, tunable conductivity, mechanical flexibility, redox activity [19] | Chemical diversity, processability, biocompatible formulations, controllable morphology | Limited environmental/electrical stability, mechanical rigidity, processing difficulties [19] |
Hydrogels
Fundamental Properties and Classification
Hydrogels are three-dimensional, cross-linked networks of hydrophilic polymers that can absorb significant amounts of water or biological fluids without dissolving [15]. Their structure and properties are influenced by polymer composition and cross-linking methods, resulting in a diverse range of characteristics including tunable swelling/deswelling behavior, multifunctional stimuli-responsiveness, and adjustable mechanical performance [14]. The high water content of hydrogels imparts both solid and fluid mechanical characteristics, with elastic moduli comparable to those of biological tissues, thus enhancing their biocompatibility and offering significant potential for biomedical applications [14].
Based on their cross-linking mechanisms, hydrogels are classified into several categories:
- Physically cross-linked: Rely on non-covalent interactions (electrostatic interactions, hydrogen bonding, hydrophobic interactions) [14]
- Chemically cross-linked: Involve covalent bond formation between polymer chains [14]
- Hybrid cross-linked: Combine physical and chemical cross-linking mechanisms [14]
According to their origin, hydrogel materials can be further categorized as:
- Synthetic polymers: Polyacrylamide (PAAm), polyvinyl alcohol (PVA), polyethylene glycol (PEG) [16]
- Natural polymers: Chitosan, agar, fibrin, proteins, polysaccharides [15]
Performance Characteristics and Measurement
The swelling behavior of hydrogels is a critical property determined by their hydrophilic functional groups and cross-linking density. The equilibrium swelling ratio is calculated as:
[ \text{Swelling Ratio} = \frac{Ws - Wd}{W_d} ]
Where (Ws) represents the weight of swollen hydrogels and (Wd) is the weight of freeze-dried hydrogels [15]. Highly crosslinked structures exhibit lower swelling ratios, while less crosslinked structures show higher swelling ratios [15].
Stimuli-responsive "smart" hydrogels undergo significant changes in swelling behavior in response to environmental variations such as pH, temperature, electric field, light, and specific biomolecules [15]. For instance, temperature-sensitive hydrogels like poly(N-isopropyl acrylamide) (PNIPAM) exhibit swelling changes at critical solution temperatures, while pH-sensitive hydrogels based on polyacrylic acid (PAA) or polymethacrylic acid (PMAA) swell differently depending on the protonation state of their ionic groups [15].
Table 2: Key Performance Parameters of Hydrogels for Bioelectronics
| Parameter | Measurement Techniques | Typical Range | Influencing Factors |
|---|---|---|---|
| Swelling Ratio | Gravimetric analysis | 10-1000% of dry weight | Cross-linking density, polymer hydrophilicity, environmental conditions [15] |
| Elastic Modulus | Rheometry, tensile testing | 0.1-100 kPa (matching biological tissues) [14] | Polymer concentration, cross-linking density, network structure [15] |
| Degradation Rate | Mass loss monitoring, structural analysis | Days to months | Chemical composition, enzymatic activity, environmental factors [15] |
| Pore Size | Scanning electron microscopy | Nanoscale to micrometers (2-10 μm in PVA systems) [14] | Synthesis conditions, polymer concentration, freezing methods (for cryogels) |
Synthesis and Experimental Protocols
Protocol: Preparation of Anisotropic PVA/PANI Hydrogels via Low-Temperature Polymerization [16]
- Solution Preparation: Prepare a homogeneous mixture of PVA, aniline, and initiator in aqueous solution.
- Directional Freezing: Freeze the solution in a unidirectional vertical gradient to facilitate directional growth of ice crystals, forming a 3D honeycomb structure.
- Restricted Polymerization: Under these low-temperature conditions, aniline undergoes restricted polymerization at the interface between ice crystals and PVA walls.
- Scaffold Formation: Allow PANI nanofibers to slowly form a scaffold, ultimately yielding an anisotropic PVA/PANI hydrogel (APPH) with an interpenetrating network structure.
- Post-processing: Thaw the hydrogel and rinse to remove unreacted monomers, then characterize using SEM, rheometry, and electrical conductivity measurements.
This method produces hydrogels with bicontinuous phase structure consisting of ion-conducting PVA and electrochemically active PANI scaffolds with high mechanical strength and superelasticity [16].
Liquid Metals
Fundamental Properties and Composition
Liquid metals (LMs) are metals or alloys that exist in liquid state at or near room temperature. Gallium-based alloys have garnered significant attention due to their safety profile and combination of advantageous thermophysical properties compared to mercury [18]. The most common LMs for flexible bioelectronics include:
- EGaIn: Eutectic gallium-indium (75% Ga, 25% In by weight) with melting point of 15.7°C [17]
- Galinstan: Eutectic gallium-indium-tin (68.5% Ga, 21.5% In, 10% Sn by weight) [17]
These materials exhibit exceptional properties including high electrical conductivity (3.4×10⁶ S/m for EGaIn), high thermal conductivity, fluidity, stretchability, and self-healing capabilities [17]. A critical aspect of LM behavior is the formation of a thin, passivating oxide skin (primarily Ga₂O₃) upon exposure to air, which stabilizes shapes against surface tension and enables patterning [17].
Synthesis and Processing Techniques
Liquid metal composites can be prepared through physical and chemical approaches:
Physical Synthesis Methods [17]:
- Mechanical mixing of bulk LM or LM nano/microdroplets with polymer precursors, inorganic flakes, and metallic particles
- Using LMs as fillers in soft/porous matrices
- Sonication to create LM emulsion with controlled droplet size
Protocol: Preparation of LM-Based Microwires through Thermal Drawing [18]
- Co-extrusion: Co-extrude EGaIn as core element and styrene-ethylene/butylene-styrene (SEBS) as shell material
- Thermal Drawing: Apply thermal drawing to the extrudates to reduce dimensions
- Dimension Control: Vary feed speed of co-extruded materials and drawing speed to control core diameter and shell thickness
- Characterization: Assess electrical properties under stretching and kinking deformation
This process enables production of LM-based microwires with core diameters as small as 52±14 μm and shell thickness of 46±10 μm, which maintain conductivity under deformation and exhibit self-healing properties [18].
Applications in Bioelectronics
Liquid metals find applications across multiple bioelectronic domains:
- Flexible electrodes for electrophysiological signal monitoring
- Stretchable conductors for wearable sensors and electronic skins
- Thermal interface materials for heat management in implantable devices
- Drug carriers in therapeutic delivery systems [17]
The compatibility of Galinstan with diamond coatings has been demonstrated, with no penetration or corrosion observed, though long-term oxidation and hydrolysis to GaOOH remains a challenge [18].
Conductive Polymers
Fundamental Properties and Doping Mechanisms
Conductive polymers (CPs) represent a class of organic materials that combine the electrical properties of metals and semiconductors with the mechanical flexibility and processing advantages of conventional polymers [19]. The fundamental structure consists of a conjugated carbon backbone with alternating single (σ) and double (π) bonds, where highly delocalized, polarized, and electron-dense π-bonds enable charge transport [19].
A critical factor in enhancing conductivity is doping, which introduces additional charge carriers (electrons for n-type or holes for p-type) into the polymer matrix. This process generates quasi-particles that facilitate charge transport along and between polymer chains, dramatically increasing electrical conductivity while modifying electronic structure, morphology, stability, and optical properties [19].
Major Conductive Polymer Systems
Key conductive polymers for biomedical applications include:
- Polyaniline (PANI): Good environmental stability, tunable conductivity through doping
- Polypyrrole (PPy): Excellent biocompatibility, commonly used in biosensors and neural interfaces
- Poly(3,4-ethylenedioxythiophene) (PEDOT): High conductivity, stability, often used with polystyrene sulfonate (PSS) as PEDOT:PSS
- Polythiophene (PT) and derivatives: Used in organic electronics and antimicrobial coatings [19]
Table 3: Performance Characteristics of Major Conductive Polymers
| Polymer | Conductivity Range (S/cm) | Key Advantages | Primary Biomedical Applications |
|---|---|---|---|
| PANI | 10⁻¹⁰–10⁵ | Tunable conductivity, environmental stability, cost-effectiveness | Biosensors, antimicrobial coatings [19] |
| PPy | 10⁻⁸–10⁴ | Excellent biocompatibility, ease of synthesis, redox activity | Biosensors, neural interfaces, artificial muscles [19] |
| PEDOT | 10⁻⁶–10³ | High conductivity, transparency, stability (as PEDOT:PSS) | Bioelectrodes, neural interfaces, transparent conductors [19] |
| PT | 10⁻⁸–10⁴ | Structural versatility, optoelectronic properties | Biosensors, antimicrobial coatings [19] |
Synthesis and Processing for Bioelectronics
Protocol: Preparation of Conductive Polymer-Based Biosensors
- Monomer Preparation: Purify monomers (pyrrole, aniline, or EDOT) through distillation or recrystallization
- Oxidative Polymerization: Initiate polymerization using chemical oxidants (e.g., FeCl₃, ammonium persulfate) or electrochemical methods
- Doping: Introduce dopant ions during or after polymerization to enhance conductivity
- Composite Formation: Incorporate biocompatible additives or nanostructures to improve mechanical properties and biocompatibility
- Device Fabrication: Process into final form (films, coatings, patterned structures) using techniques such as spin-coating, inkjet printing, or electrodeposition
The biomedical application landscape for conductive polymers shows biosensors leading in both research and patent activity, followed by bioelectrical stimulation and neural interfaces [19]. Artificial muscles and implantable prosthetics exhibit high patent-to-journal ratios, indicating strong commercialization potential [19].
Composite Materials and Advanced Applications
Conductive Composite Hydrogels
Conductive composite hydrogels have emerged as promising materials that address the limitations of individual material systems. By introducing conductive fillers into hydrogel matrices, these composites form functional systems integrating tunable conductivity, mechanical robustness, and biocompatibility [16]. These materials can be classified based on their conductive filler type:
- Conductive polymer-based: PPy, PANI, or PEDOT incorporated into hydrogel networks
- LM-based: EGaIn or Galinstan droplets dispersed in hydrogel matrices
- Carbon-based: Graphene, carbon nanotubes, or carbon black added to hydrogels
- Metallic nanoparticle-based: Silver, gold, or other metal nanoparticles within hydrogels
Protocol: Preparation of PPy-Based Conductive Composite Hydrogels
- Hydrogel Matrix Formation: Prepare hydrogel network using natural (chitosan, gelatin) or synthetic (PVA, PAAm) polymers
- In-situ Polymerization: Incorporate pyrrole monomer into hydrogel network and initiate oxidative polymerization
- Doping: Introduce dopant anions (e.g., chloride, sulfate, polystyrene sulfonate) during polymerization
- Characterization: Evaluate electrical conductivity, mechanical properties, and biocompatibility
These composites address critical challenges in bioelectronic interfaces by providing tissue-matching mechanical properties while maintaining efficient electrical conduction for high-fidelity signal acquisition [16].
Applications in Bioelectronics and Biomedical Devices
Advanced applications of these material classes in bioelectronics include:
Electronic Skins (E-skins) based on conductive composite hydrogels can monitor physiological parameters, human motion, and environmental stimuli in real-time [16]. Their tissue-like softness and biocompatibility enable seamless integration with human skin for continuous health monitoring.
Neural Interfaces utilizing conductive polymers or LM composites provide soft, compliant electrodes that minimize foreign body response and maintain stable electrical performance for neural recording and stimulation [19] [13].
Drug Delivery Systems leverage the responsive properties of hydrogels and conductive polymers for controlled therapeutic release. For instance, electrically-triggered drug release from conductive polymer systems enables precise, localized administration of therapeutics [19].
Tissue Engineering Scaffolds incorporating conductive elements within hydrogel matrices support cell growth and regeneration while providing electrical stimulation for enhanced tissue development, particularly in electrically responsive tissues like nerve and muscle [19].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Soft Bioelectronics Material Development
| Reagent/Category | Function/Purpose | Examples/Specific Reagents |
|---|---|---|
| Hydrogel Polymers | Form primary network structure providing mechanical framework and hydration | Polyvinyl alcohol (PVA), polyacrylamide (PAAm), polyethylene glycol (PEG), chitosan, gelatin [16] [15] |
| Conductive Polymers | Provide electronic conductivity and electrochemical activity | Polyaniline (PANI), polypyrrole (PPy), PEDOT:PSS [19] |
| Liquid Metals | Create highly deformable conductive pathways | EGaIn (75% Ga, 25% In), Galinstan (68.5% Ga, 21.5% In, 10% Sn) [17] |
| Cross-linking Agents | Establish network connectivity determining mechanical properties | Glutaraldehyde, genipin, ammonium persulfate (APS), N,N'-methylenebisacrylamide (MBAA) [15] |
| Dopants | Enhance electrical conductivity through charge carrier introduction | Hydrochloric acid, camphorsulfonic acid, polystyrene sulfonate, ferric chloride [19] |
| Oxidants | Initiate polymerization of conductive polymers | Ammonium persulfate, ferric chloride, hydrogen peroxide [19] |
| Stabilizers/Surfactants | Control LM droplet formation and prevent aggregation | Sodium dodecyl sulfate, Triton X-100, polyvinylpyrrolidone [17] |
| Biocompatibility Agents | Enhance biological integration and reduce immune response | Heparin, collagen, fibronectin, laminin [15] |
Hydrogels, liquid metals, and conductive polymers represent foundational material classes that enable the development of advanced soft bioelectronic systems. Each material offers unique advantages: hydrogels provide tissue-like mechanical properties and biocompatibility, liquid metals deliver unparalleled stretchability and self-healing capabilities, and conductive polymers bridge the gap between organic electronics and biological interfaces.
The future of these materials lies in the development of sophisticated composites that combine their respective advantages while mitigating individual limitations. Key research directions include improving long-term stability under physiological conditions, enhancing biocompatibility for chronic implants, developing scalable manufacturing processes, and creating multifunctional systems that combine sensing, actuation, and therapeutic capabilities. As these materials continue to evolve, they will undoubtedly unlock new possibilities in personalized medicine, advanced diagnostics, and bioelectronic therapeutics.
The integration of these material classes—through conductive composite hydrogels, LM-polymer hybrids, and other innovative combinations—represents the forefront of soft bioelectronics research, promising to transform how we interface electronic technology with biological systems for improved healthcare outcomes.
The field of soft bioelectronics is undergoing a fundamental transformation, shifting from a design philosophy centered on permanence and durability to one that embraces transience and resorption. This paradigm, critical for next-generation medical implants and sustainable electronics, leverages bioresorbable and self-healing materials to create devices that perform their function over a clinically relevant timeframe before safely dissolving in the body or environment [20]. These transient electronics address key limitations of conventional permanent implants, including long-term foreign body response, infection risks, and the need for secondary surgical removal [21] [22]. The core principle rests on the deliberate selection and integration of materials—both functional and structural—that are designed to disintegrate upon exposure to specific triggers, such as aqueous fluids or enzymatic activity, following predictable kinetics [20].
Framed within broader soft bioelectronics research, these technologies represent a convergence of materials science with biomedical engineering, aiming to achieve seamless, biocompatible integration with biological tissues. The mechanical properties of these materials—such as softness, stretchability, and conformability—are engineered to match those of dynamic biological systems, thereby minimizing mechanical mismatch at the tissue-device interface [9] [23]. This review provides an in-depth technical examination of the material systems, degradation mechanisms, fabrication strategies, and characterization methods underpinning this emerging field, serving as a guide for researchers and scientists developing the next wave of transient biomedical devices.
Material Systems for Transient Functionality
The development of high-performance transient electronics requires a diverse palette of materials that offer both excellent electronic functionality and controlled disintegration. These materials span the categories of conductors, semiconductors, and dielectrics.
Bioresorbable Conductors and Semiconductors
Conductive elements in transient devices are typically fabricated from metals or conductive polymers that degrade into non-toxic byproducts.
- Bioresorbable Metals: Magnesium (Mg) and Zinc (Zn) are the most widely used transient conductors, serving as interconnects and electrodes. Their degradation is governed by oxidation and hydrolysis, with rates varying significantly based on the physiological environment. Mg degrades at approximately 1.2–12 µm/day in simulated body fluid (SBF) at 37°C, while Zn degrades at about 3.5 µm/day in phosphate-buffered saline (PBS) at 37°C [20]. For applications requiring longer stability, Molybdenum (Mo) and Tungsten (W) offer slower dissolution profiles of 0.001 µm/day and 0.48–1.44 µm/day, respectively [20].
- Conductive Polymers: Poly(3,4-ethylenedioxythiophene):poly(styrenesulfonate) (PEDOT:PSS) is a cornerstone material for soft, conductive layers. When combined with crosslinkers like 2,4-hexadiyne-1,6-diol (HDD) and processed with secondary dopants (e.g., methanol or H₂SO₄), it can achieve conductivities as high as ~2000 S/cm [24]. Its organic nature and tunable properties make it ideal for conformal biointerfaces.
The semiconductor layer is critical for active device operation. While single-crystalline silicon was the first major bioresorbable semiconductor discovered, the material palette is expanding.
- Silicon and Germanium: The degradation of single-crystalline silicon in aqueous environments is well-characterized, with rates highly sensitive to temperature, pH, and the presence of specific ions (e.g., HPO₄²⁻, Cl⁻) [20]. Germanium (Ge) nanomembranes and silicon-germanium (SiGe) alloys have also been successfully implemented in devices like strain and temperature sensors, offering proven biocompatibility and gas-free dissolution [20].
- Organic and Oxide Semiconductors: A composite of poly(3-hexylthiophene) (P3HT) nanofibrils within a poly(l-lactide-co-ε-caprolactone) (PLCL) matrix has been demonstrated as a solution-processable, degradable semiconductor. The optimum PLCL:P3HT ratio of 8:2 balances electrical performance with mechanical stretchability [24]. Indium–gallium–zinc oxide (IGZO) and zinc oxide (ZnO) are other promising semiconductors for transient thin-film transistors and logic circuits [20].
Table 1: Characteristics of Key Bioresorbable Semiconductor and Conductor Materials
| Material | Function | Degradation Rate | Key Properties | Applications |
|---|---|---|---|---|
| Magnesium (Mg) | Conductor | 1.2-12 µm/day (in SBF, 37°C) [20] | High conductivity, biocompatible degradation products | Electrodes, interconnects [20] |
| PEDOT:PSS | Conductor | Tunable via crosslinking & encapsulation | Up to ~2000 S/cm conductivity, soft, stretchable [24] | Conductive traces, neural interfaces [24] |
| Silicon (Si) | Semiconductor | Tunable via crystallinity & doping [20] | High-performance, well-understood dissolution | Diodes, transistors, CMOS circuits [20] |
| P3HT/PLCL Composite | Semiconductor | 0.12 μm/day (slower than PLCL) [24] | Solution-processable, elastic, degradable | Soft, stretchable thin-film transistors (TFTs) [24] |
Substrates, Encapsulants, and Self-Healing Materials
The substrate forms the structural backbone of the device, while encapsulation layers are paramount for controlling the functional lifetime.
- Biodegradable Polymers: Materials like PLCL and other biodegradable polyesters undergo hydrolysis, cleaving their ester bonds over time. The degradation rate is influenced by molecular weight (Mn), temperature, and pH. For example, higher Mn PLCL degrades faster due to a higher density of hydrolyzable bonds [24]. Poly(lactic-co-glycolic acid) (PLGA) and polycaprolactone (PCL) are also widely used for this purpose [20] [25].
- Encapsulation Strategies: Precise lifetime control is achieved through encapsulation layers that act as protective barriers. Recent work demonstrates that incorporating silicon dioxide (SiO₂) or zinc oxide (ZnO) flakes into a biodegradable polymer matrix can delay the onset of degradation, enabling devices to retain mechanical integrity for over 40 days in vivo [26]. The aspect ratio (width-to-thickness) of these filler flakes is a critical design parameter that can be modeled to fine-tune the degradation profile passively [26].
While the search results provided a stronger focus on bioresorption, the field of self-healing materials is a critical complementary paradigm for enhancing the durability and reliability of transient electronics during their operational life. These materials, often based on liquid metal alloys (e.g., gallium-based) or dynamic covalent polymer networks, can autonomously repair mechanical damage, such as cracks or breaks in conductive traces, thereby recovering electrical functionality and extending the device's usable lifetime under dynamic strain [23].
Degradation Mechanisms and Kinetics
The dissolution of transient electronic materials follows specific chemical pathways, primarily hydrolysis and enzymatic cleavage, depending on the material's chemical nature.
- Hydrolysis: This is the dominant mechanism for many polymers (e.g., PLC, PLGA) and semiconductors like silicon. For polymers, it involves the cleavage of backbone ester bonds by water molecules. For silicon, the reaction is: Si + 2H₂O → SiO₂ + 2H₂, followed by the hydration of SiO₂ to form soluble silicic acid [Si(OH)₄] [20].
- Enzymatic Degradation: Certain biopolymers, such as silk fibroin, are susceptible to enzymatic breakdown by proteases found in biological environments [20].
- Oxidation and Corrosion: Bioresorbable metals like Mg degrade via electrochemical corrosion: Mg + 2H₂O → Mg(OH)₂ + H₂. The formation of a passivating layer of Mg(OH)₂ can slow the process, but ions like Cl⁻ in physiological fluids can disrupt this layer, accelerating corrosion [20].
The kinetics of these processes are influenced by multiple external factors, allowing for programmable device lifetimes. Key influencing factors include:
- pH: Higher pH (alkaline conditions) generally accelerates the hydrolysis of polyester substrates [24].
- Temperature: Elevated temperatures significantly increase degradation rates across all material classes [20].
- Ionic Environment: The presence of specific ions, such as chloride (Cl⁻) and hydrogen phosphate (HPO₄²⁻), can catalyze the dissolution of silicon and the corrosion of magnesium [20].
The following diagram illustrates the logical relationship between material composition, environmental triggers, and the resulting degradation pathway.
Degradation Pathway Logic
Table 2: Degradation Triggers and Rates for Selected Materials
| Material | Primary Degradation Mechanism | Key Influencing Factors | Reported Degradation Rate |
|---|---|---|---|
| PLCL Substrate | Hydrolysis of ester bonds | pH, Temperature, Molecular Weight (Mn) [24] | ~0.21 µm/day (PBS, pH 7, 37°C) [24] |
| P3HT/PLCL Semiconductor | Hydrolysis (slowed by P3HT hydrophobicity) | Temperature, pH [24] | ~0.12 µm/day (PBS, pH 7, 37°C) [24] |
| Magnesium (Mg) | Corrosion/Oxidation | Ion concentration (e.g., Cl⁻), pH [20] | 1.2-12 µm/day (SBF, pH 7.4, 37°C) [20] |
| Silicon (Si) | Hydrolysis & Oxidation | Ion concentration (HPO₄²⁻, Cl⁻), Crystallinity, Doping [20] | Tunable from days to years [20] |
Fabrication and Manufacturing Strategies
A significant challenge for transient electronics is developing fabrication processes that are scalable, cost-effective, and compatible with sensitive biodegradable materials.
Monolithic 3D Fabrication via Photopatterning
Recent advances have demonstrated a solution-processable and photo-patternable approach for creating sophisticated, multi-layered devices. This strategy enables the fabrication of sensors, transistors, microheaters, and capacitors on a single, ultrathin (~3 μm) elastic substrate [24]. The workflow involves sequential, layer-by-layer deposition and patterning of optimized organic materials:
- Substrate/Insulator Formation: A biodegradable elastic polymer (e.g., UV-curable PLCL) is synthesized, spin-coated, and crosslinked via UV exposure to form the device substrate [24].
- Semiconductor Patterning: A semiconducting layer (e.g., P3HT nanofibrils in a PLCL matrix) is deposited. A diazirine crosslinker is used to form a stretchable network upon UV irradiation, enabling photopatterning of the semiconductor [24].
- Conductor Patterning: A conductive ink (e.g., PEDOT:PSS with HDD crosslinker) is cast and patterned using UV lithography. Exposure to 254 nm light induces topochemical polymerization, creating water-resistant, highly conductive traces [24].
This method offers significant advantages in resolution (down to a few microns), speed, and cost reduction compared to traditional microfabrication, making it highly suitable for producing large-area biointegrated electronic systems [24].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for Fabricating Soft Transient Electronics
| Reagent / Material | Function | Brief Explanation of Role |
|---|---|---|
| UV-PLCL (Acrylated) | Substrate/Insulator | A UV-curable, biodegradable elastomer that forms the soft, degradable backbone of the device [24]. |
| P3HT (Poly(3-hexylthiophene)) | Semiconductor | Provides the semiconducting properties. Used as nanofibrils for superior carrier mobility [24]. |
| PEDOT:PSS | Conductor | A conductive polymer complex used to form flexible, patternable electrodes and interconnects [24]. |
| 2,4,6-Trimethylbenzoyldiphenylphosphine oxide (TPO) | Photoinitiator | Generates free radicals upon UV exposure to initiate crosslinking of the UV-PLCL monomer [24]. |
| 2,4-Hexadiyne-1,6-diol (HDD) | Crosslinker | Undergoes topochemical polymerization under 254 nm UV to pattern and insolubilize PEDOT:PSS traces [24]. |
| Diazirine Crosslinker | Crosslinker | Forms carbenes under UV to create crosslinks between P3HT and the polymer matrix, enabling a patterned, stretchable semiconductor [24]. |
| Silicon Dioxide (SiO₂) Flakes | Encapsulation Filler | Mixed into polymer matrices to control the device's dissolution rate by lengthening the pathway for water ingress [26]. |
The following diagram summarizes the key steps in this monolithic fabrication process.
Monolithic 3D Fabrication Workflow
Experimental Protocols and Characterization
Rigorous characterization is essential to correlate material properties with device performance and degradation behavior. Below is a detailed methodology for key experiments cited in this field.
Protocol: In Vitro Degradation Kinetics Study
Objective: To quantitatively characterize the dissolution profile and functional lifetime of a fabricated transient electronic device under accelerated or physiologically relevant conditions [24] [26].
Materials:
- Device Under Test (DUT): e.g., a fabricated PLCL-based electrode array.
- Incubation Medium: Phosphate-buffered saline (PBS), simulated body fluid (SBF), or solutions at varying pH (e.g., pH 7.4 and pH 13 for accelerated testing).
- Environmental Chamber: Set to 37°C to mimic physiological temperature.
- Analytical Tools: Optical microscope, scanning electron microscope (SEM), impedance analyzer, scale for mass loss measurement.
Procedure:
- Baseline Characterization: Record initial mass, thickness, optical images, and electrical performance (e.g., impedance, conductivity) of the DUT.
- Immersion: Immerse the DUT in the selected incubation medium, ensuring the device is fully submerged. Maintain the environment at a constant temperature (e.g., 37°C).
- Periodic Sampling: At predetermined time intervals (e.g., daily, weekly), remove samples from the medium (n≥3 for statistical significance).
- Rinsing and Drying: Gently rinse samples with deionized water and dry under a stream of nitrogen or in a desiccator for mass loss and imaging analysis. Note: For electrical testing, measurements may be performed in-situ or on carefully blotted (not fully dried) samples to preserve the degradation state.
- Analysis:
- Mass Loss: Measure and record the mass of the dried samples to calculate the percentage of mass loss over time.
- Morphology: Use optical microscopy and SEM to document physical changes, such as cracking, delamination, and fragmentation.
- Functional Performance: Measure the electrical impedance of electrodes or the operational characteristics of transistors.
- Chemical Analysis: Use techniques like Fourier-Transform Infrared Spectroscopy (FTIR) or Gel Permeation Chromatography (GPC) to track chemical bond cleavage and molecular weight changes in polymers.
- Data Modeling: Fit the mass loss and electrical performance data to kinetic models (e.g., first-order decay) to extract degradation rate constants and predict functional lifetime.
Protocol: Electrochemical Performance of Soft Electrodes
Objective: To evaluate the electrical stability and interface impedance of soft, conductive electrodes (e.g., PEDOT:PSS) under mechanical strain and in biological fluids, a key metric for bio-sensing applications [24] [23].
Materials:
- Fabricated electrode on a soft substrate.
- Potentiostat/Galvanostat with impedance capability.
- Electrochemical cell (3-electrode setup: working electrode = DUT, counter electrode = Pt wire, reference electrode = Ag/AgCl).
- Custom-built or commercial tensile strain stage.
Procedure:
- Setup: Mount the soft electrode in the electrochemical cell containing PBS at 37°C.
- Cyclic Voltammetry (CV): Perform CV scans (e.g., from -0.2 V to 0.6 V vs. Ag/AgCl at 50 mV/s) to assess the electrochemical activity and stability.
- Electrochemical Impedance Spectroscopy (EIS): Measure impedance spectra (e.g., from 1 Hz to 100 kHz at open circuit potential with a 10 mV AC amplitude).
- Strain Testing: Repeat steps 2 and 3 while applying uniaxial tensile strain to the substrate (e.g., 0%, 10%, 30% strain) to evaluate performance under deformation.
- Data Analysis: Extract the charge storage capacity (CSC) from the CV curves. Analyze EIS data by fitting to an equivalent circuit model (e.g., a Randles circuit) to determine the interface impedance, a critical parameter for signal-to-noise ratio in sensing.
Applications in Biomedical Devices and Beyond
Bioresorbable and self-healing materials are enabling a new class of medical devices that seamlessly integrate with the body for therapeutic and diagnostic functions before safely disappearing.
- Neuromodulation and Recovery: Fully bioresorbable electrical stimulators have been developed to promote nerve regeneration after injury. These devices provide critical therapeutic stimulation during the initial healing phase and then degrade, eliminating the need for surgical removal [20]. Similarly, soft, conformable electrode arrays can be implanted on the brain cortex for electrocorticography (ECoG) monitoring and then dissolve [20] [24].
- Cardiac Rhythm Management: Temporary, battery-free, and bioresorbable pacemakers have been designed for on-demand cardiac rhythm management during the postoperative recovery period, after which the device dissolves [20] [24].
- Wound Healing and Drug Delivery: Dissolvable sensors can monitor healing parameters (pH, temperature) at wound sites and release growth factors or drugs in a spatiotemporally controlled manner, with the entire system degrading as the tissue regenerates [22] [23].
- Environmental Sensing: Beyond medicine, transient electronics are deployed as eco-friendly sensors for monitoring soil, water, or aquatic conditions. These devices perform their function and then decompose in the environment, preventing persistent electronic waste [20] [25].
The paradigm of bioresorbable and self-healing materials is fundamentally reshaping the design and application of soft bioelectronics. By engineering material systems that harmonize with biological timescales and environments, researchers are creating transient devices that eliminate the long-term risks and limitations associated with permanent implants. The progress in understanding degradation mechanisms, developing sophisticated material palettes, and establishing scalable fabrication methods like monolithic 3D photopatterning has positioned this field for significant growth.
Future research will need to tackle several key challenges to realize the full potential of this technology. These include expanding the library of high-performance biodegradable semiconductors with diverse bandgaps, developing fully biodegradable and high-energy-density power sources, and establishing standardized regulatory pathways for these dynamic devices. Furthermore, the integration of intelligent, feedback-controlled systems that can actively respond to physiological cues will pave the way for truly autonomous, closed-loop therapeutic platforms. The convergence of bioresorbable materials with self-healing capabilities and soft electronics promises a future where medical implants are not only minimally invasive and effective but also temporary and smart, ultimately dissolving away after their work is done.
From Lab to Life: Fabrication Techniques and Breakthrough Applications in Healthcare
The development of soft and flexible bioelectronics represents a paradigm shift in medical devices, demanding fabrication technologies that can bridge the mechanical mismatch between traditional rigid electronics and biological tissues. This technical guide examines three core advanced fabrication techniques—3D printing, electrospinning, and transfer printing—within the context of soft bioelectronics materials research. These methods enable the creation of devices with tissue-like mechanical properties, enhanced biocompatibility, and sophisticated functionality for applications ranging from implantable sensors to tissue engineering scaffolds and drug delivery systems. The convergence of these fabrication approaches allows researchers to overcome individual technological limitations, creating synergistic platforms that support next-generation biomedical innovations [27] [6].
Core Fabrication Technologies
Electrospinning Fundamentals
Electrospinning is a versatile technique for producing micro- and nanoscale fibers that closely mimic the native extracellular matrix (ECM). The process involves applying a strong electric field to a polymer solution or melt, which overcomes the liquid's surface tension and draws it into fine fibers that are deposited on a collector [27] [28].
Process Parameters and Setup: A basic electrospinning system consists of four main components: a high-voltage power supply (typically 10-25 kV), a solution storage unit (e.g., syringe), an ejection device (spinneret or needle), and a collection device. The applied voltage creates an electromagnetic field between the spinneret and collector, deforming the polymer solution droplet into a Taylor cone from which a charged polymer jet is ejected. This jet undergoes rapid stretching and whipping motions during its trajectory to the collector, resulting in solvent evaporation and the formation of solid fibers with diameters ranging from tens of nanometers to several micrometers [27] [28].
Critical Parameters Influencing Fiber Morphology:
- Solution Parameters: Polymer molecular weight and concentration directly affect solution viscosity. Lower molecular weights or concentrations often result in bead formation instead of uniform fibers, while higher values promote uniform fiber formation but may lead to clogging if viscosity becomes excessive. Solvent properties, particularly dielectric constant, significantly impact fiber diameter and morphology [27].
- Process Parameters: Applied voltage, flow rate, and tip-to-collector distance critically influence final fiber characteristics. Optimal voltage must be carefully determined as both insufficient and excessive voltage can cause bead formation or non-uniform fibers. Increased collector distance generally reduces fiber diameter and improves uniformity by allowing more time for solvent evaporation and jet stretching [27].
- Environmental Factors: Temperature and humidity affect solvent evaporation rates and consequently impact fiber morphology and surface characteristics [28].
Electrospinning Variants: The technology is primarily categorized into solution electrospinning (using polymer solutions) and melt electrospinning (using polymer melts). Solution electrospinning can achieve nanoscale fibers but often involves toxic organic solvents. Melt electrospinning offers a solvent-free alternative but typically produces larger diameter fibers and presents challenges related to thermal degradation and equipment complexity [28].
3D Printing Technologies
Additive manufacturing, particularly 3D printing, has revolutionized the fabrication of soft bioelectronic devices by enabling precise control over architecture and customization. Several 3D printing techniques are particularly relevant for soft devices:
Digital Light Processing (DLP): This vat polymerization technique projects 2D light patterns onto a vat of photopolymer resin, curing complete layers simultaneously. DLP offers high resolution (down to 1 μm), fast printing speeds, smooth surface finishes, and compatibility with various photocurable materials including hydrogels, elastomers, and ionogels. Recent advancements like grayscale DLP (g-DLP) enable spatial control of material properties by varying light intensity, while multi-material DLP systems facilitate heterogeneous constructs [29].
Fused Deposition Modeling (FDM): This extrusion-based method melts and deposits thermoplastic filaments layer-by-layer. FDM offers cost-effectiveness, precision, and scalability, making it suitable for creating customized scaffold structures with specific shapes and porosity. However, it typically provides lower resolution than DLP and is limited to thermoplastic materials [30].
Emerging 3D Printing Capabilities: Continuous Liquid Interface Production (CLIP) dramatically accelerates printing speed by utilizing oxygen inhibition to prevent adhesion to the vat bottom. Multi-material printing systems enable complex, heterogeneous devices with integrated functionality. Portable, low-cost DLP systems based on smartphone projectors are increasing technology accessibility [29].
Transfer Printing and Alternative Approaches
While 3D printing and electrospinning are additive processes, transfer printing techniques enable the integration of functional components onto soft, stretchable substrates. This approach is particularly valuable for creating sophisticated bioelectronic interfaces that combine the performance of semiconductor materials with the mechanical compliance of biological tissues.
Recent breakthroughs in material science have enabled alternative pathways to soft bioelectronics. The development of hydrogel-based semiconductors represents a significant innovation, creating materials that are both semiconductive and possess tissue-like mechanical properties. These materials are synthesized using a solvent exchange process where semiconductors are first dissolved in a water-miscible organic solvent before being incorporated with hydrogel precursors, resulting in a single material that combines semiconducting functionality with hydrogel properties including high hydration, porosity, and softness [6].
Another pioneering approach utilizes the giant magnetoelastic effect in soft polymer systems. This discovery enables the creation of intrinsically waterproof bioelectronic devices that operate via magnetic fields rather than direct electrical connections, overcoming the limitation of traditional electronics in high-humidity biological environments [31].
Synergistic Integration of Fabrication Techniques
Hybrid 3D Printing and Electrospinning Approaches
The integration of 3D printing and electrospinning creates complementary fabrication platforms that overcome the individual limitations of each technology. Electrospinning produces nanofibrous structures that mimic the native extracellular matrix but often lacks mechanical stability and precise geometric control. Conversely, 3D printing enables the development of tailored structures with highly controlled architecture and improved mechanical strength but struggles to achieve nanoscale resolution [27].
Combined approaches produce scaffolds and devices that integrate nanoscale features for enhanced cellular interaction with macroscale designs that provide structural integrity. These hybrid strategies have shown particular promise in tissue-specific applications including bone regeneration, skin wound healing, and nerve repair [27]. For instance, bilayered scaffolds for osteochondral repair utilize a 3D-printed base layer that provides porous mechanical support, combined with an electrospun membrane top layer that acts as a barrier against unwanted tissue infiltration [30].
The table below summarizes the complementary characteristics of these technologies and the benefits of their integration:
Table 1: Complementary Characteristics of 3D Printing and Electrospinning
| Parameter | 3D Printing | Electrospinning | Integrated Approach |
|---|---|---|---|
| Resolution | Macroscale to microscale (typically ≥50 μm) [27] | Nanoscale to microscale (50 nm - 10 μm) [28] | Multiscale architecture from nano to macro |
| Mechanical Properties | High structural strength, customizable stiffness [27] | Limited mechanical stability, high flexibility [27] | Optimized mechanical integrity with compliant interfaces |
| Architectural Control | High precision in 3D geometry, controlled porosity [29] | Random or aligned fibers, limited 3D control [27] | Precise 3D structures with biomimetic nanofeatures |
| Biomimicry | Limited at cellular level [27] | Excellent ECM mimicry, high surface area [28] | Enhanced biointegration at multiple hierarchical levels |
| Application Scope | Structural implants, custom devices [30] | Drug delivery, wound healing, filtration [28] | Advanced tissue engineering, bioactive implants |
Experimental Protocols for Hybrid Fabrication
Protocol 1: Fabrication of Bilayered Osteochondral Scaffolds
This protocol details the combined FDM 3D printing and electrospinning approach for creating functional bilayered scaffolds, as demonstrated in recent research [30]:
Materials:
- Polycaprolactone (PCL) pellets (80 kDa) and filament sticks
- Graphene nanoplatelets (GNP, 0.5 wt%)
- Osteogenon (OST) drug
- Solvents: chloroform, dimethylformamide (DMF)
3D Printing Parameters:
- Printer: Anet A8 FDM printer
- Nozzle Temperature: 190°C
- Bed Temperature: 50°C
- Layer Thickness: 0.2 mm
- Infill Pattern: Three layers of parallel bars (1 mm side length) with 0.7 mm spacing, oriented perpendicularly in adjacent layers
Electrospinning Parameters:
- Polymer Solution: PCL dissolved in chloroform/DMF (2:1 v/v) with OST incorporation
- Voltage: 15-20 kV
- Flow Rate: 1.0 mL/h
- Tip-to-Collector Distance: 15 cm
- Collector Type: Rotating mandrel for aligned fibers or static plate for random fibers
Fabrication Sequence:
- Produce GNP-modified PCL filament using injection molding with 0.5 wt% GNP incorporation
- 3D print the porous scaffold base layer using optimized FDM parameters
- Mount the 3D-printed structure on the electrospinning collector
- Electrospin the drug-loaded PCL/OST fibrous membrane directly onto the 3D-printed substrate
- Vacuum dry the bilayered scaffold for 24 hours to remove residual solvents
Table 2: Key Material Functions in Bilayered Scaffold Design
| Material | Function | Rationale |
|---|---|---|
| Polycaprolactone (PCL) | Structural polymer for both 3D printing and electrospinning | Biodegradability, excellent processability, mechanical strength [30] |
| Graphene Nanoplatelets (GNP) | Antibacterial modifier and mechanical enhancer | Antimicrobial properties via membrane damage and oxidative stress; improves ductility and crystallization [30] |
| Osteogenon (OST) | Osteoinductive drug component | Promotes bone regeneration through ossein and hydroxyapatite components [30] |
| Chloroform/DMF | Solvent system for electrospinning | Efficiently dissolves PCL, moderate volatility for controlled fiber formation [30] |
Protocol 2: DLP Printing of Soft Pneumatic Actuators
This protocol outlines the fabrication of soft pneumatic actuators with sensing capabilities using multi-material DLP printing [29]:
Materials:
- Photocurable elastomer resin (e.g., polyurethane-based)
- Conductive hydrogel resin
- Photoinitiator (e.g., phenylbis(2,4,6-trimethylbenzoyl)phosphine oxide)
- Photoabsorber (e.g., Sudan I)
DLP Printing Parameters:
- Printer Configuration: Bottom-up projection with oxygen-permeable window
- Layer Thickness: 25-50 μm
- Exposure Time: 1-5 seconds per layer (optimized for resin formulation)
- Light Intensity: 5-20 mW/cm² at 405 nm wavelength
- Multi-material Approach: Centrifugal force-assisted resin exchange for heterogeneous structures
Fabrication Sequence:
- Design actuator geometry with integrated pneumatic channels and sensing elements
- Prepare elastomer and conductive hydrogel resins with optimized viscosity (<500 cps)
- Print main actuator body using elastomer resin
- Implement resin exchange protocol for multi-material printing
- Print conductive hydrogel sensing elements at critical deformation points
- Post-cure printed structure under UV light (365 nm, 10 minutes)
- Characterize actuation performance and sensing capability
Advanced Material Systems for Soft Bioelectronics
Hydrogel-Based Semiconductors
A groundbreaking advancement in soft bioelectronics is the development of hydrogel-based semiconductors that simultaneously exhibit semiconducting functionality and tissue-like mechanical properties. These materials address the fundamental mismatch between traditional rigid semiconductors and biological tissues, enabling seamless bioelectronic interfaces [6].
The fabrication of these materials employs a novel solvent exchange process:
- Semiconducting polymers are first dissolved in a water-miscible organic solvent
- The solution is combined with hydrogel precursors and gelation agents
- Polymerization creates a unified material that maintains both semiconducting capability and hydrogel characteristics
These hydrogel semiconductors demonstrate enhanced biosensing capabilities due to their porous structure that facilitates efficient diffusion of biomolecules to interaction sites. They also exhibit reduced immune responses and inflammation when implanted, addressing critical challenges in long-term bioelectronic integration [6].
Soft Magnetoelastic Materials
The recent discovery of the giant magnetoelastic effect in soft polymer systems represents a paradigm shift in bioelectronic sensing and energy harvesting. This phenomenon, previously observed only in rigid metals and alloys, involves variations in magnetic flux density under mechanical stress [31].
- Material Composition: Soft magnetoelastic composites typically consist of magnetic nanoparticles (e.g., neodymium-iron-boron) incorporated into elastomeric matrices (e.g., silicone, polyurethane).
- Fabrication Process:
- Magnetic particles are uniformly dispersed in the uncured elastomer precursor
- The mixture is cast or printed into desired geometries
- Cross-linking is induced thermally or via UV exposure
- The material is magnetically polarized in a strong external field
- Performance Characteristics: These materials exhibit significant changes in magnetic flux density under minimal mechanical pressure (as low as 10 kPa), making them suitable for detecting physiological signals such as arterial pulse waves, respiratory movements, and cardiac cycles [31].
A key advantage of magnetoelastic bioelectronics is their intrinsic waterproofness, as magnetic fields penetrate water and biological fluids without significant signal loss. This eliminates the need for bulky encapsulation layers that typically compromise device flexibility and performance [31].
Characterization and Performance Metrics
Structural and Mechanical Characterization
Rigorous characterization of soft devices is essential to ensure performance under physiological conditions. Key metrics include:
- Structural Analysis: Scanning electron microscopy (SEM) reveals fiber morphology, pore structure, and layer integration in hybrid scaffolds. Micro-computed tomography (μCT) provides 3D visualization of internal architecture and mineral deposition in bioactive scaffolds [30].
- Mechanical Properties: Tensile testing determines elastic modulus, strain at break, and toughness. Soft bioelectronic materials typically exhibit moduli ranging from <1 kPa (matching brain tissue) to several MPa (for load-bearing applications). Hydrogel semiconductors demonstrate mechanical properties similar to native tissues, with high stretchability (often >100% strain) and toughness (up to 420 MJ/m³ for advanced formulations) [32] [6].
- Surface Characteristics: Contact angle measurements assess hydrophilicity/hydrophobicity, which influences protein adsorption and cell adhesion. FTIR spectroscopy confirms chemical composition and functional group presence [30].
Functional Performance Metrics
- Electrical Properties: Conductivity measurements evaluate performance under deformation. Advanced conductive hydrogels maintain approximately 1.2 S/cm conductivity even under 100% tensile strain, with minimal impedance increase (<9%) after 10,000 mechanical cycles [32].
- Biointeractive Performance: Implantable devices are evaluated based on signal-to-noise ratio (SNR) and foreign body response. Next-generation flexible bioelectronics demonstrate SNR of 37 dB compared to 15 dB for conventional Pt electrodes, while reducing fibrous capsule thickness to approximately 28.6 μm versus 85.2 μm for traditional materials [32].
- Antibacterial Efficacy: For antimicrobial applications, materials are tested against relevant pathogens. Graphene-incorporated scaffolds show significant antibacterial effectiveness against C. albicans and S. aureus through multiple mechanisms including physical membrane disruption and oxidative stress induction [30].
Table 3: Performance Metrics of Advanced Soft Bioelectronic Materials
| Material System | Key Performance Indicators | Values | Applications |
|---|---|---|---|
| Hydrogel Semiconductors | Electrical conductivity, Modulus, Hydration | Tissue-like modulus (<1 kPa), High porosity, Enhanced biosensing [6] | Implantable sensors, Drug delivery devices |
| Soft Magnetoelastic Composites | Pressure sensitivity, Magnetic response, Waterproofness | Detection threshold: ~10 kPa, Intrinsically waterproof [31] | Wearable sensors, Implantable monitors |
| Conductive Hydrogels | Conductivity under strain, Toughness, Cyclic stability | 1.2 S/cm at 100% strain, 420 MJ/m³ toughness, <9% impedance increase after 10,000 cycles [32] | Flexible electrodes, Strain sensors |
| PCL/Graphene Scaffolds | Antibacterial efficacy, Strain at break, Mineralization | Enhanced against S. aureus & C. albicans, Increased ductility, Rapid apatite formation [30] | Bone tissue engineering, Osteochondral repair |
Applications in Soft Bioelectronics
Tissue Engineering and Regenerative Medicine
The integration of 3D printing and electrospinning enables the creation of sophisticated scaffolds for tissue engineering that mimic the hierarchical organization of native tissues. Bilayered constructs provide distinct microenvironments for different cell types—for example, supporting both chondrogenic and osteogenic differentiation in osteochondral repair. The incorporation of bioactive molecules such as Osteogenon enhances bone regeneration, while graphene components provide antibacterial protection against postoperative infections [30].
Implantable and Wearable Bioelectronics
Advanced fabrication techniques have enabled a new generation of bioelectronic devices that seamlessly integrate with biological tissues:
- Neural Interfaces: Flexible bioelectronic systems with brain tissue-like modulus (<1 kPa) significantly reduce foreign body response and enable stable electrophysiological signal acquisition over extended periods (≥30 days). These systems can incorporate anti-inflammatory coatings that modulate macrophage polarization and suppress immune responses through reactive oxygen species scavenging [32].
- Biosensing Platforms: Hydrogel-based semiconductors enable enhanced biosensing capabilities through their porous structure that facilitates biomarker diffusion to interaction sites, significantly increasing detection sensitivity. Similarly, magnetoelastic sensors provide intrinsically waterproof operation for continuous physiological monitoring in sweaty or wet environments [6] [31].
- Soft Robotics and Actuators: DLP-printed soft pneumatic actuators with integrated sensing capabilities enable sophisticated human-machine interfaces. These systems can perform complex motions including extension, torsion, contraction, and bending, with embedded conductive hydrogels providing real-time feedback on deformation states [29].
Research Reagent Solutions
The table below provides essential materials for advanced fabrication of soft bioelectronic devices:
Table 4: Key Research Reagents for Soft Device Fabrication
| Material Category | Specific Examples | Function in Fabrication | Key Characteristics |
|---|---|---|---|
| Structural Polymers | Polycaprolactone (PCL), PLGA, Polylactic acid (PLA) | Primary scaffold material for 3D printing and electrospinning | Biodegradability, tunable mechanical properties, processability [28] [30] |
| Photocurable Resins | Polyurethane-based elastomers, Acrylated epoxies | Matrix material for DLP 3D printing | Fast curing, tunable stiffness, biocompatibility [29] |
| Conductive Materials | Conductive hydrogels, Ionogels, Graphene nanoplatelets | Enable electronic functionality in soft devices | High conductivity, stretchability, stability under deformation [32] [30] |
| Bioactive Additives | Osteogenon, Hydroxyapatite, Growth factors | Enhance biological integration and functionality | Osteoinduction, antimicrobial activity, cell signaling [30] |
| Magnetic Components | Neodymium-iron-boron particles, Ferrofluids | Enable magnetoelastic effects in soft composites | High magnetic susceptibility, biocompatible coatings [31] |
| Solvent Systems | Chloroform/DMF, Tetrahydrofuran, Water-miscible organic solvents | Dissolve polymers for electrospinning and processing | Appropriate volatility, solubility parameters, low toxicity [27] [6] |
Visualization of Workflows
Fabrication Workflow for Soft Devices
Material Design Logic for Bioelectronics
The convergence of materials science, electrical engineering, and biology is catalyzing a revolution in wearable health monitoring. Traditional rigid electronic devices face a fundamental mechanical mismatch with soft, dynamic human tissues, leading to motion artifacts, unreliable data, and tissue inflammation [7]. This whitepaper examines the next generation of wearable platforms, framed within the context of soft and flexible bioelectronics, which aim to overcome these limitations. These platforms are engineered to form conformal, biocompatible interfaces with the skin or within the body, enabling continuous, high-fidelity acquisition of electrophysiological signals—electroencephalogram (EEG), electrocardiogram (ECG), and electromyogram (EMG)—and biochemical data from metabolites in biofluids [33] [34]. The core thesis is that advances in intrinsically soft materials—such as hydrogels, elastomers, and polymer semiconductors—are the primary enablers for seamless bio-integration, transforming wearable devices from external data loggers into intimate diagnostic and therapeutic partners [32] [6] [7].
This transition is critical for applications ranging from personalized medicine and neuroprosthetics to chronic disease management. By mitigating the foreign body response (FBR) and achieving tissue-like compliance, these devices promise stable, long-term operation essential for reliable data in both clinical and ambulatory settings [35] [7]. This guide provides a technical deep dive into the material foundations, sensing modalities, data processing methodologies, and experimental protocols that define the current state-of-the-art in wearable bioelectronics.
Material Foundations for Flexible Bioelectronics
The performance and biocompatibility of wearable platforms are fundamentally determined by the materials used in their construction. The ideal material must exhibit tissue-like mechanical properties, high electrical conductivity, and stability in a physiological environment.
Key Material Classes and Their Properties
- Hydrogels and Elastomers: These materials form the backbone of soft substrates and encapsulation layers. Their low Young's modulus (often <1 kPa) and high hydration capacity mimic the mechanical properties of biological tissues, thereby minimizing FBR [7]. Recent innovations focus on incorporating self-healing properties through dynamic covalent bonds (e.g., borate ester bonds), which allow the material to recover its electrical and mechanical properties after damage, thereby enhancing device longevity [32]. For instance, research has demonstrated hydrogels that restore 90% of their conductivity within 48 hours post-mechanical failure [32].
- Conductive Composites: To render soft materials conductive, researchers embed conductive fillers or use intrinsically conductive polymers. Key materials include:
- MXenes and Graphene: These 2D materials provide high electrical conductivity and large surface areas, beneficial for sensitive biosensing and electrophysiological recording [7].
- Conductive Polymers: Poly(3,4-ethylenedioxythiophene) (PEDOT) and polypyrrole (PPy) are widely used to coat rigid electrodes, providing a soft, high-capacitance interface that improves the signal-to-noise ratio (SNR) [7].
- Hydrogel Semiconductors: A groundbreaking development is the creation of a single material that is both a semiconductor and a hydrogel. This bluish gel combines the immense information-processing ability of a semiconductor with the soft, porous, and hydrating properties of a hydrogel. This "one-plus-one-is-greater-than-two" combination reduces immune responses and enhances biosensing sensitivity due to the porous structure that allows efficient diffusion of biomolecules [6].
Table 1: Key Material Classes in Flexible Bioelectronics
| Material Class | Example Materials | Key Properties | Primary Function in Device |
|---|---|---|---|
| Soft Substrates | Polyurethane (PU), Polydimethylsiloxane (PDMS), Ecoflex, Silk Fibroin | Low Young's modulus (<100 kPa), Stretchability (up to 900%), Biocompatibility | Structural support, Encapsulation |
| Conductive Fillers | MXenes, Graphene, Carbon Nanotubes (CNTs) | High Electrical Conductivity, Large Surface Area | Electrodes, Interconnects |
| Conductive Polymers | PEDOT, PEDOT:PSS, Polypyrrole | Mixed Ionic-Electronic Conductivity, Soft Compliance | Electrode Coating, Conductive Hydrogels |
| Functional Hydrogels | Catechol-functionalized PU, Borate ester-crosslinked hydrogels | Self-Healing, Bioadhesive, Tissue-like Modulus | Substrate, Conductive Layer, Drug Reservoir |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for fabricating and testing flexible bioelectronic devices as discussed in the cited research.
Table 2: Research Reagent Solutions for Flexible Bioelectronics
| Item Name | Function/Explanation | Example from Research |
|---|---|---|
| Polyurethane (PU) Elastomer | A flexible polymer used as a substrate material. Its modulus can be tuned to match that of soft tissues. | Used as a mussel-inspired catechol-functionalized substrate with a modulus similar to brain tissue (<1 kPa) [32]. |
| Dynamic Borate Ester Bonds | A type of reversible covalent bond used as a crosslinker in hydrogels to enable self-healing properties. | Crosslinks conductive hydrogels, allowing them to recover conductivity after mechanical damage [32]. |
| MXene-Silk Fibroin Composite | A conductive (MXene) and biocompatible (silk fibroin) composite material used as an anti-inflammatory coating. | Serves as a coating that suppresses immune response by scavenging reactive oxygen species (ROS) [32]. |
| Hydrogel Semiconductor Precursors | Polymer semiconductors and hydrogel precursors dissolved in a water-miscible organic solvent. | Enables the fabrication of a single material that is both a semiconductor and a hydrogel via a solvent exchange process [6]. |
| PEDOT:PSS | A conductive polymer dispersion commonly used to coat electrodes, improving their charge injection capacity and softness. | A standard material for constructing flexible and stretchable electrodes to replace rigid metals [7]. |
Biosignal Monitoring Modalities and Performance
Wearable platforms simultaneously capture a suite of electrical and chemical signals from the body, providing a holistic view of the user's physiological state.
Electrophysiological Signal Monitoring (EEG, ECG, EMG)
Electrophysiological signals are measured by electrodes placed on the skin or implantable devices. The shift to soft materials drastically improves signal quality by ensuring a stable, conformal interface.
- EEG measures electrical activity from the brain, generated by synchronized postsynaptic currents in cortical pyramidal neurons [36]. It is crucial for brain-computer interfaces (BCIs), cognitive monitoring, and sleep studies. Flexible platforms have demonstrated stable EEG acquisition over 30 days in animal models, achieving an SNR of 37 dB, a significant improvement over the 15 dB seen with conventional platinum electrodes [32].
- ECG records the electrical activity of the heart, specifically the depolarization and repolarization of the SA node and cardiac muscle [36]. Textile-based electrodes functionalized with graphene have shown a 97.0% correlation with clinical-grade Ag/AgCl electrodes [34].
- EMG detects motor unit action potentials (MUAPs) from contracting muscle fibers [36]. It is used for neuromuscular diagnosis, rehabilitation monitoring, and controlling prosthetic limbs. Soft, tattoo-based electrodes enable robust EMG recording even during body movement.
Table 3: Performance Metrics of Electrophysiological Monitoring with Flexible Platforms
| Signal | Key Performance Metric | Rigid/Conventional Device Performance | Flexible/Bioelectronic Device Performance |
|---|---|---|---|
| EEG (Implanted) | Signal-to-Noise Ratio (SNR) | ~15 dB (Conventional Pt electrodes) [32] | ~37 dB (Self-healing bioactive interface) [32] |
| ECG (Wearable) | Correlation with Ag/AgCl Electrodes | 100% (Baseline) | 97.0% (Graphene-textile electrode) [34] |
| Motion Artifact Suppression | Root Mean Square (RMS) Error | Baseline | <15 μV (40% improvement over commercial arrays) [32] |
| Long-Term Stability | Fibrous Capsule Thickness | 85.2 ± 12.7 μm (Traditional materials) [32] | 28.6 ± 5.4 μm (Bioactive coatings) [32] |
Metabolite and Biochemical Monitoring
Continuous metabolite monitoring is achieved through microfluidic and sweat-sensing platforms [37]. These devices use capillary action to channel sweat—which contains biomarkers like glucose, lactate, cortisol, and electrolytes—to sensing electrodes functionalized with specific enzymes or chemical receptors [37]. Advances in stretchable substrates and multiplexed assays now allow for real-time, non-invasive metabolic profiling, which is valuable for athletic performance, stress tracking, and managing metabolic disorders [37]. The integration of these biochemical sensors with EEG/ECG/EMG electrodes on a single, soft platform enables multi-modal health assessment.
Data Processing and Computational Frameworks
Raw biosignals are inherently noisy. Transforming them into actionable insights requires a sophisticated processing pipeline that is increasingly powered by artificial intelligence (AI) and machine learning (ML).
The Biosignal Processing Pipeline
The journey from raw signal to insight involves three critical stages [36]:
- Pre-processing and Artifact Rejection: The raw signal is cleaned using band-pass filters to remove slow drift and high-frequency noise, and notch filters to suppress 50/60 Hz mains hum. Techniques like Independent Component Analysis (ICA) are used to remove artifacts from eye blinks (EOG) and muscle activity (EMG) [36].
- Feature Extraction: Cleaned signals are analyzed to extract quantifiable features.
- Time-domain: Mean, variance, and root mean square (RMS) for ECG and EMG.
- Frequency-domain: Power in specific bands (e.g., Alpha, Beta for EEG) [36].
- Time-Frequency-domain: Wavelet transforms to capture transient events.
- Classification and Machine Learning: Extracted features are fed into ML models for pattern recognition and classification. This includes using Support Vector Machines (SVM) and Linear Discriminant Analysis (LDA) for curated features, and Convolutional Neural Networks (CNNs) and Long Short-Term Memory (LSTM) networks for raw data analysis [33] [36]. The trend is toward on-device AI acceleration for ultra-low-power analytics and real-time, closed-loop therapeutic systems [37].
Figure 1: Biosignal Data Processing Workflow. The pipeline transforms noisy raw data into insights through sequential stages of cleaning, feature identification, and machine learning classification.
Experimental Protocols and Methodologies
This section outlines detailed methodologies for key experiments validating the performance of flexible biosensing platforms, based on recent high-impact research.
Protocol: In Vivo Validation of a Self-Healing Neural Interface
This protocol is adapted from the work by Wu et al. (2025) on a soft, bioactive bioelectronic interface [32].
- Objective: To evaluate the long-term electrophysiological recording stability, foreign body response, and self-healing capability of a flexible neural implant in a live animal model.
- Materials:
- Test Device: Multilayer electrode array comprising a catechol-functionalized polyurethane substrate, a conductive self-healing hydrogel, and an MXene-silk fibroin anti-inflammatory coating.
- Control Device: Conventional rigid electrode (e.g., Platinum or Utah array).
- Animal Model: Adult Sprague-Dawley rats.
- Equipment: Stereotaxic surgical setup, electrophysiology recording system, histological processing equipment, scanning electron microscope (SEM).
- Procedure:
- Implantation: Anesthetize the rat and secure it in a stereotaxic frame. Perform a craniotomy over the primary motor cortex. Carefully implant the test and control devices into the cortical tissue.
- Chronic Recording: Record cortical EEG signals at regular intervals (e.g., daily) for a period of 30 days. Continuously monitor the Signal-to-Noise Ratio (SNR).
- Mechanical Integrity Test: At day 10, induce a controlled, minor mechanical damage to the self-healing hydrogel layer of the test device. Continue recording and monitor the recovery of electrical conductivity over 48 hours.
- Terminal Analysis: After 30 days, perfuse the animal and extract the brain tissue surrounding the implant.
- Histology: Section the tissue and stain with H&E to measure the thickness of the fibrous capsule formed around the implant.
- Immunohistochemistry: Stain for macrophages (e.g., CD68) to quantify the level of inflammatory response.
- Key Metrics and Validation:
- Signal Quality: Compare the SNR of the test device versus the control over the 30-day period. The test device should maintain a stable SNR >35 dB [32].
- Self-Healing Efficacy: Calculate the percentage of conductivity restored post-damage. The target is >90% recovery within 48 hours [32].
- Biocompatibility: Measure the fibrous capsule thickness. The test device with bioactive coating should show a significantly reduced thickness (e.g., ~28 μm vs. ~85 μm for the control) [32].
Protocol: Fabrication of a Hydrogel Semiconductor Film
This protocol is based on the breakthrough solvent exchange process developed by Dai et al. (2024) [6].
- Objective: To synthesize a single-material film that exhibits both semiconducting and hydrogel properties.
- Materials:
- Polymer semiconductor (e.g., a relevant conjugated polymer).
- Hydrogel precursors (e.g., monomers like hydroxyethyl methacrylate, crosslinker).
- Water-miscible organic solvent (e.g., Tetrahydrofuran, DMSO).
- Initiator (e.g., Ammonium persulfate) and catalyst (e.g., TEMED) for gelation.
- Procedure:
- Dissolution: Dissolve the polymer semiconductor and the hydrogel precursors in the organic solvent. The solution should be stirred thoroughly until a homogeneous mixture is achieved.
- Gelation Initiation: Add the initiator and catalyst to the solution to initiate the cross-linking reaction of the hydrogel precursors.
- Solvent Exchange: Cast the solution into a mold and submerge it in an aqueous buffer. The organic solvent diffuses out into the water, while water diffuses in, causing the formation of a highly hydrated hydrogel network with the embedded semiconductor polymer.
- Curing and Characterization: Allow the film to fully cure.
- Electrical Characterization: Use a source meter to measure the electrical conductivity and semiconducting properties.
- Mechanical Characterization: Use a tensile tester to measure the Young's modulus and elongation at break.
- Swelling Ratio: Measure the mass of the hydrated film versus its dry mass to determine the water content.
- Key Metrics and Validation:
- Electrical Performance: Verify semiconductor behavior via transistor characteristics.
- Mechanical Properties: Confirm tissue-like softness (Young's modulus in the kPa range).
- Hydration: Achieve a high water content (>70%), confirming true hydrogel properties [6].
Figure 2: Hydrogel Semiconductor Fabrication. A solvent-exchange process creates a unified material with both semiconducting and hydrogel properties.
The field of wearable platforms for continuous physiological monitoring is being redefined by advancements in soft and flexible bioelectronics. The integration of tissue-like materials such as self-healing hydrogels, conductive composites, and now hydrogel semiconductors is directly addressing the chronic challenges of mechanical mismatch and biological rejection. This materials-centric approach is yielding devices capable of acquiring high-fidelity EEG, ECG, EMG, and metabolite data over extended periods, a capability that was previously unattainable with rigid electronics.
Looking forward, several key research trajectories are emerging. There is a strong push toward multimodal fusion, where data from various biosignals are combined using AI to provide a more comprehensive health picture [33] [37]. Furthermore, the development of closed-loop therapeutic systems—devices that not only monitor but also automatically deliver electrical stimulation or drugs in response to detected changes—represents the frontier of personalized medicine [37] [7]. Finally, overcoming remaining challenges such as long-term stability of electrical properties in wet environments and achieving scalable manufacturing will be crucial for translating these promising laboratory innovations into clinically indispensable and commercially viable tools for researchers and healthcare professionals.
The field of bioelectronics is undergoing a transformative shift from rigid, passive implants to soft, intelligent systems that integrate seamlessly with biological tissues. This evolution is driven by the fundamental mismatch between conventional electronic materials (e.g., silicon, ~180 GPa) and soft biological tissues (e.g., brain, ~1–30 kPa), which triggers foreign body responses, limits functional longevity, and ultimately causes device failure [38]. The emerging paradigm of soft bioelectronics addresses these challenges through materials and design strategies that mimic the structural, mechanical, and biological properties of native tissues. This technical guide examines three cornerstone technologies exemplifying this transition: chronic neural interfaces, programmable cardiac patches, and syringe-injectable mesh electronics. Framed within the context of soft and flexible bioelectronics materials research, these systems demonstrate how engineered materials can achieve seamless biointegration for advanced diagnostic and therapeutic applications.
Neural Interfaces: From Rigid Probes to Seamless Integration
Materials and Design for Chronic Stability
Modern neural interface design prioritizes mechanical compliance and biocompatibility to minimize the chronic foreign body response that plagues traditional rigid implants. Table 1 summarizes the key material classes and their properties for neural interfacing.
Table 1: Material Classes for Flexible Neural Interfaces
| Material Class | Example Materials | Key Properties | Applications |
|---|---|---|---|
| Polymer Substrates | Polyimide, Parylene-C, PDMS, SU-8 [38] | Flexibility, Biocompatibility, Inertness | Substrate and encapsulation for electrodes and interconnects |
| Conductive Polymers | PEDOT:PSS [38] | Mixed ionic/electronic conduction, Low impedance, Flexibility | Electrode coatings, Active sensing layers |
| Hydrogels | Alginate-PEGDA, Fibrin [9] [39] | Tissue-like modulus, High water content, Biocompatibility | Injectable matrices, Drug delivery reservoirs |
| Nanocomposites | Pt-PDMS, Carbon nanotube-polymer [38] | Tunable conductivity, Stretchability, Customizable mechanics | Soft electrodes, Stretchable interconnects |
Innovative device architectures leverage these materials to enhance integration. Ultra-thin films (<5 µm) based on parylene-C or polyimide minimize bending stiffness, allowing for conformal contact with neural tissue without causing mechanical damage [9] [38]. The NeuroGrid, for instance, is a 4 µm-thick array with free-standing PEDOT:PSS electrodes that can detect single-cell action potentials from the cortical surface [38]. Another paradigm is the open mesh electronics design, which features macroporous structures that allow neurons and neurites to infiltrate the device, facilitating seamless 3D integration and significantly reducing chronic immune responses compared to conventional flexible thin-film probes [40].
Experimental Protocol: Syringe-Injectable Mesh Electronics
The following protocol details the fabrication, injection, and validation of syringe-injectable mesh electronics for neural recording, as demonstrated by Liu et al. [40] [41].
Fabrication and Release:
- Fabricate mesh electronics via standard photolithography and deposition techniques onto a sacrificial layer. The typical structure consists of longitudinal polymer/metal/polymer elements (interconnects) and transverse polymer elements, forming an open mesh with a designed angle (α) of 45° to optimize injectability [41].
- Release the mesh from the substrate by etching the sacrificial layer. The released mesh is a free-standing, macroporous network.
Loading and Injection:
- Hydrate the mesh and load it into a glass or metal syringe needle. Needles with inner diameters as small as 100 µm can be used [41].
- Insert the needle into the target brain region.
- Initiate injection while simultaneously withdrawing the needle. This coordinated motion places the unfolded mesh electronics through the targeted neural tissue. The input/output (I/O) pads are positioned outside the tissue for external connection [41].
Interface and Validation:
- Connect the I/O pads to measurement electronics using an anisotropic conductive film (ACF) [41].
- Validate electrical functionality post-injection. Studies report >90% device yield and <12% change in key electrical properties (e.g., impedance, conductance) even after injection through 100 µm ID needles [41].
- Assess biointegration histologically. Confocal fluorescence microscopy of brain slices perpendicular and parallel to the probe axis over 2-12 weeks shows a uniform distribution of astrocytes, microglia, and neurons around the mesh, with neurons and neurofilaments penetrating the open macroporous structure, indicating minimal chronic immune response [40].
Diagram 1: Syringe-injectable mesh electronics workflow.
Cardiac Patches: Programmable Repair and Regeneration
Hydrogel-Based Systems for Myocardial Repair
Following myocardial infarction (MI), the massive loss of cardiomyocytes and subsequent pathological remodeling leads to heart failure. Hydrogel-based cardiac patches are engineered to address this by providing mechanical support, delivering therapeutic agents, and promoting tissue regeneration [42]. These patches are typically composed of natural or synthetic polymer networks that absorb large amounts of water, mimicking the native extracellular matrix (ECM) and creating a supportive microenvironment for cell infiltration and tissue repair [42].
A key advancement is the development of intelligent hydrogels that respond to specific physiological stimuli in the infarcted microenvironment. These stimuli include temperature, pH, reactive oxygen species (ROS), and specific enzymes [42]. For instance, temperature-responsive hydrogels undergo a sol-gel transition at body temperature, allowing for easy application and in situ formation. ROS-scavenging hydrogels can mitigate oxidative stress in the infarcted heart, reducing inflammation and apoptosis [42].
Experimental Protocol: TIMED Programmable Drug-Delivery Patch
The Temporal Intervention with Microparticle Encapsulation and Delivery (TIMED) system is a hydrogel patch that delivers a sequence of therapeutic agents on a pre-programmed schedule [43] [44]. The experimental workflow for its fabrication and testing is as follows:
Microparticle Fabrication:
- Create drug-loaded microparticles using the biodegradable polymer PLGA (poly(lactic-co-glycolic acid). The particles are designed as capsules with polymer "lids."
- Encapsulation Regimen: Load the capsules with a sequence of therapeutics:
- Control the drug release kinetics by varying the molecular weight of the PLGA used for the lids, which alters its degradation rate [43].
Patch Integration and Implantation:
- Embed the rows of programmed microparticles into a thin, flexible hydrogel sheet composed of alginate and PEGDA.
- In an animal model (e.g., rat), perform a thoracotomy to access the heart following an induced MI.
- Surgically implant the compact patch directly onto the infarcted area [43].
Functional Assessment:
- In vitro: Test the patch on spheres of engineered heart tissue under low-oxygen conditions. Analysis shows promoted blood vessel growth, enhanced cell survival, and reduced fibrosis [43].
- In vivo: Evaluate the patch in a rat MI model. Key outcome measures include:
- Histology: Measure the infarct size (area of damaged tissue).
- Functional Imaging: Assess cardiac output and other hemodynamic parameters via echocardiography or catheterization.
- Survival: Monitor animal survival rates over time [43].
Table 2: In Vivo Efficacy of the TIMED Cardiac Patch in a Rat MI Model
| Evaluation Metric | TIMED Patch Result | Control (IV Injection/No Treatment) |
|---|---|---|
| Animal Survival Rate | 33% higher [44] | Baseline |
| Reduction in Damaged Tissue | ~50% reduction [43] [44] | Baseline |
| Cardiac Function | Significantly improved cardiac output [43] | No significant improvement |
Diagram 2: TIMED patch therapeutic action sequence.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and implementation of the systems described rely on a suite of specialized materials and reagents. The following table details key components for replicating experiments in injectable meshes and programmable patches.
Table 3: Essential Research Reagents and Materials
| Item Name | Function/Application | Technical Notes |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer for controlled-release microparticles [43] [44] | Molecular weight controls degradation rate and drug release timing. |
| PEGDA (Poly(ethylene glycol) diacrylate) | Crosslinker for synthetic hydrogel matrices (e.g., cardiac patch substrate) [43] | Provides structural integrity and tunable mechanical properties. |
| Alginate | Natural polymer for hydrogel-based patches and injectable systems [43] [42] | Biocompatible, forms gentle gels with divalent cations (e.g., Ca²⁺). |
| PEDOT:PSS | Conductive polymer for low-impedance, flexible neural electrodes [9] [38] | Can be used as a coating or free-standing film; offers mixed ionic/electronic conduction. |
| Parylene-C | Polymer for ultra-thin, flexible substrate and device encapsulation [9] [38] | Excellent biocompatibility and conformal coating properties. |
| Neuregulin-1 | Therapeutic growth factor; promotes cardiomyocyte survival [43] [44] | Used in first release phase of TIMED patch to prevent cell death post-MI. |
| VEGF | Therapeutic growth factor; promotes angiogenesis (blood vessel formation) [43] [44] | Used in second release phase of TIMED patch to re-establish blood supply. |
| Anisotropic Conductive Film (ACF) | Electrically connects I/O pads of mesh electronics to external circuitry [41] | Enables bonding without shorting adjacent conductive lines. |
The frontier of implantable and injectable bioelectronics is defined by increasingly sophisticated and biomimetic systems. Current research is pushing beyond static, tissue-like materials toward biohybrid and "all-living" interfaces that incorporate living cells at the device-tissue interface to actively promote regeneration and seamless integration [38]. Furthermore, the integration of volumetric 3D printing and melt-electrowriting enables the fabrication of reinforced, multimaterial cardiac patches that are both suturable and regenerative, offering a scalable solution for clinical translation [39]. The convergence of these advanced fabrication techniques, intelligent materials, and biological components is paving the way for a new generation of bioelectronic medicines that can dynamically interact with and heal the human body.
The management of chronic wounds represents a significant and growing challenge in healthcare, often requiring real-time, continuous monitoring of the healing process. Conventional clinical assessments, which rely on visual inspection and bulky instruments, lack the temporal resolution and molecular specificity to accurately guide dynamic treatment strategies. Within the broader context of soft and flexible bioelectronics materials research, a paradigm shift is occurring towards the development of intelligent, conformable devices that seamlessly integrate with biological tissues. These advanced systems bridge the critical gap between the rigid, dry nature of conventional electronics and the soft, wet, and dynamic environment of biological systems [45] [46] [47]. This case study examines a groundbreaking innovation at this intersection: a wireless, soft bioelectronic device embedded with a Self-Confined Tetrahedral DNA circuit (SCTD) for high-fidelity chronic wound monitoring [48] [49].
The core challenge in chronic wound care is the accurate, continuous assessment of the healing status, which is governed by complex biochemical processes. Chronic wounds are often characterized by a prolonged inflammatory phase, with specific protein biomarkers providing crucial information about the progression from inflammation to proliferation and tissue remodeling [48]. While existing flexible sensors have focused on biophysical signals or small metabolites, the detection of low-abundance protein biomarkers such as cytokines and growth factors has remained elusive due to limitations in sensitivity, stability, and biofouling [48]. The integration of structural DNA nanotechnology with soft, breathable substrates represents a transformative approach to overcoming these limitations, offering a pathway to devices with molecular-level precision and exceptional bio-integration capabilities.
Technical Foundation: Core Components and Design Principles
The Self-Confined Tetrahedral DNA (SCTD) Circuit
The SCTD is the cornerstone of this biosensing platform, engineered to address the key challenges of sensitivity, stability, and specificity in complex wound environments. Its design incorporates several innovative features:
Tetrahedral DNA Nanostructure: A rigid, three-dimensional DNA scaffold provides a stable framework for positioning sensing elements. This defined spatial configuration ensures uniformity and reproducibility, while its structural integrity confers remarkable resistance to nuclease degradation in the harsh wound microenvironment [48] [50]. The tetrahedral geometry ensures excellent mechanical stability, demonstrated by a mere 3% signal variation after 1000 bending cycles [48].
Self-Circulation Amplification Mechanism: At the heart of the SCTD's sensitivity is a target-triggered, autonomous DNA cascade reaction. The process initiates when a target protein biomarker binds to a hairpin DNA (H1) probe modified with a methylene blue (MB) signal molecule. This binding event unfolds H1, exposing a sticky end that subsequently hybridizes with a complementary hairpin (H2) immobilized on the tetrahedral DNA scaffold. Due to a higher affinity between H1 and H2 than between H1 and the target protein, the protein is released and can cyclically participate in the reaction, leading to an accumulation of MB labels on the electrode surface and significant signal amplification [48].
Spatial Confinement and Auxiliary Nucleic Acid Pre-coating: The amplification reaction is spatially confined within defined hydrophilic areas on a nanofiber substrate. These areas are pre-coated with dry H1 powder, which dissolves upon contact with wound exudate, creating a localized reaction pool. The surrounding hydrophobic regions prevent reagent diffusion, concentrating the reaction and enhancing efficiency without the need for external fluidic handling [48]. This self-confined design decreases detection limits by an order of magnitude compared to conventional methods [48].
Soft and Breathable Substrate Integration
The electronic functionality is built upon a flexible and breathable substrate essential for non-impeded wound healing.
Material and Fabrication: The substrate is composed of electrospun polyacrylonitrile/thermoplastic polyurethane (PAN/TPU) nanofibers with an optimal 1:1 mass ratio, producing a porous mat of interwoven fibers with a uniform diameter of approximately 110 nm [48]. This nanofibrous structure provides high porosity, excellent gas permeability, and mechanical softness, conforming intimately to the irregular wound surface without causing irritation or inflammation.
Conductive Elements: A gold electrode array is deposited onto the nanofiber mat via thermal evaporation using shadow masks. This electrode exhibits outstanding electrical and electrochemical stability, with negligible changes in DC resistance after 2000 bending cycles and less than 1% variation in redox peak currents after 1000 bending cycles [48].
Multimodal Sensing Array: The platform integrates the SCTD for biochemical sensing with additional sensors for biophysical parameters. This includes polyaniline (PANI)-based electrodes for pH sensing and metal microwire-based temperature sensors, providing a comprehensive physiological profile of the wound status [48].
Table 1: Key Performance Metrics of the SCTD Biosensing Platform
| Performance Parameter | Achieved Metric | Significance |
|---|---|---|
| Detection Sensitivity | Detection limit decreased by an order of magnitude [48] | Enables monitoring of low-abundance protein biomarkers |
| Mechanical Stability | Within 3% signal variation after 1000 bending cycles [48] | Ensures reliable operation during patient movement |
| Long-term Stability | Within 8% signal attenuation over 4 weeks [48] | Suitable for long-term chronic wound monitoring |
| Anti-Biofouling | Over 50% reduction in BSA adhesion [48] | Maintains performance in protein-rich wound exudate |
| Biomarker Multiplexing | Simultaneous monitoring of TNF-α, IL-6, TGF-β1, and VEGF [48] | Provides comprehensive, stage-specific healing assessment |
Experimental Methodology and Workflow
Fabrication Protocol for the SCTD Biosensor
The construction of the integrated biosensing platform involves a multi-step fabrication process:
- Substrate Preparation: A nanofibrous mat is fabricated by electrospinning a blended solution of PAN and TPU (1:1 mass ratio) to form a flexible, breathable substrate [48].
- Electrode Patterning: A gold electrode array is thermally evaporated onto the nanofiber substrate through a shadow mask to define the conductive sensing regions [48].
- Hydrophilic Patterning: The substrate is patterned to create defined hydrophilic biosensing areas surrounded by hydrophobic boundaries. This confines the subsequent biochemical reactions [48].
- TDNA Immobilization: Tetrahedral DNA nanostructures (TDNA) are assembled and anchored to the gold electrodes via Au-Thiol (Au-S) bonding. This forms the stable, rigid scaffold for the sensing reaction [48].
- H1 Probe Loading: Hairpin DNA (H1) probes, functionalized with methylene blue (MB) and containing the target-specific aptamer sequence, are pre-coated as a dry powder onto the hydrophilic biosensing areas [48].
- Sensor Integration: The pH and temperature sensors are fabricated, and the entire multimodal array is connected to a miniaturized flexible printed circuit board (FPCB) for signal processing and wireless data transmission [48].
Characterization and Validation Procedures
Rigorous characterization is essential to validate the sensor's performance under conditions mimicking the wound environment.
- Mechanical Testing: The device is subjected to repeated bending cycles (e.g., 1000 cycles with a 3 cm radius) while monitoring electrical resistance (DC) and electrochemical performance (via Cyclic Voltammetry and Electrochemical Impedance Spectroscopy) to assess stability under deformation [48].
- Stability and Biofouling Assessment:
- Long-term Stability: The electrochemical signal is monitored over four weeks to evaluate signal attenuation [48].
- Antifouling Performance: The sensor is exposed to protein solutions like Bovine Serum Albumin (BSA), and adhesion is quantified, demonstrating over a 50% reduction compared to conventional interfaces [48].
- In Vitro and In Vivo Sensing:
- Sensitivity and Selectivity: The sensor is calibrated with solutions containing specific protein targets (TNF-α, IL-6, TGF-β1, VEGF) and potential interferents to establish calibration curves and confirm specificity [48].
- In Vivo Validation: The wireless platform is deployed on diabetic male mouse models with both non-infected and infected wounds. The healing process is tracked in real-time, and sensor data is correlated with wound status without impeding the natural healing process [48].
Performance Data and Technical Specifications
The SCTD-embedded biosensing platform demonstrates exceptional performance across multiple key parameters, as quantitatively validated through a series of rigorous experiments.
Table 2: Comprehensive Performance Characteristics of the SCTD Biosensor
| Characteristic | Method of Assessment | Key Result |
|---|---|---|
| Electrochemical Stability | Cyclic Voltammetry (CV) before/after 1000 bends | <1% variation in redox peak currents and peak potential separation [48] |
| Impedance Stability | Electrochemical Impedance Spectroscopy (EIS) before/after 1000 bends | <8% change in charge transfer resistance [48] |
| Electrical Stability | DC resistance during 2000 bending cycles | Negligible changes within 4% variation [48] |
| Breathability | Gas permeability measurement of PAN/TPU nanofiber mat | High porosity for moisture and gas exchange, preventing maceration [48] |
| In Vivo Efficacy | Monitoring of wound healing in diabetic male mice | Accurate tracking of healing status without impeding the natural healing process [48] |
The platform's capability for multiplexed biomarker detection allows for a nuanced understanding of wound status. For instance, elevated levels of the inflammatory markers TNF-α and IL-6 indicate a proinflammatory phase, while a rise in TGF-β1 and VEGF signals the transition to the repair and angiogenesis phase [48]. This stage-specific profiling enables clinicians to make data-driven treatment decisions.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and implementation of the SCTD biosensor rely on a specific set of materials and reagents, each serving a critical function in ensuring the device's performance and reliability.
Table 3: Key Research Reagent Solutions for SCTD Biosensor Fabrication
| Reagent/Material | Function/Description | Role in the System |
|---|---|---|
| Tetrahedral DNA (TDNA) | A rigid, 3D nanostructure formed by self-assembly of specifically designed DNA strands [48] [50] | Provides a mechanically stable, anti-fouling scaffold for probe immobilization; enhances nuclease resistance. |
| Hairpin DNA (H1 & H2) | Functional DNA strands; H1 contains aptamer sequence and MB, H2 is immobilized on TDNA [48] | H1 acts as the target recognition and signal transduction element. H1-H2 hybridization enables catalytic signal amplification. |
| Electrospun PAN/TPU Nanofibers | A blend of polyacrylonitrile and thermoplastic polyurethane forming a porous, flexible mat [48] | Serves as the soft, breathable substrate that conforms to the wound and prevents maceration. |
| Gold Electrodes | Thin-film conductive layers deposited via thermal evaporation [48] | Provides the electrochemical sensing interface and enables electrical connection to the readout system. |
| Methylene Blue (MB) | An electrochemical redox reporter molecule [48] | Covalently attached to H1; its accumulation on the electrode surface generates the quantifiable current signal. |
| Wireless FPCB | A miniaturized flexible printed circuit board [48] | Enables on-site signal processing, power management, and wireless transmission of data to a smartphone interface. |
Context within Soft Bioelectronics Materials Research
This innovation is a prime example of the evolution in soft bioelectronics, which aims to create devices with mechanical properties compatible with biological tissues. The SCTD platform embodies several key material design principles driving this field:
- Mechanical Compliance and Breathability: The use of electrospun nanofibers addresses the critical need for substrates that are not only flexible and stretchable but also permeable to moisture and gases. This high breathability is essential for long-term wound applications to prevent fluid accumulation and tissue maceration, a common drawback of occlusive dressings and impermeable electronics [48] [51].
- Hydrogel-Mimetic Interfaces: While this platform uses a nanofiber substrate, its operational principle of creating a localized, reactive aqueous environment mirrors the broader trend of using hydrogel-based interfaces in bioelectronics. Hydrogels are prized for their tissue-like elasticity, high water content, and biocompatibility, which promote stable integration with biological tissues and improve signal fidelity [45] [46]. The SCTD's confined hydrophilic zones function as discrete, functional hydrogel-like pools.
- Liquid-Based and Hybrid Materials: The advance towards more robust and multifunctional systems is exemplified by the exploration of organogels and organohydrogels. Organogels, which use organic solvents in their polymer networks, offer superior stability against dehydration and freezing. Hybrid organohydrogels combine the advantages of both systems, exhibiting self-healing properties and resistance to harsh environmental conditions [46]. The SCTD platform's stability in complex wound environments aligns with the pursuit of such next-generation materials.
- Intelligent Material Systems: The integration of the DNA circuit moves beyond passive sensing towards an "intelligent" material system capable of molecular computation and signal amplification directly at the bio-interface. This represents a significant step in the convergence of molecular nanotechnology and flexible electronics, creating devices that can process biochemical information locally before transmitting electronic signals [50].
This case study on the self-confined tetrahedral DNA circuit for chronic wound monitoring illustrates a sophisticated application of soft bioelectronics principles. By integrating the molecular programmability of DNA nanotechnology with a soft, breathable electronic substrate, this platform achieves a level of sensitivity, stability, and bio-integration previously unseen in wearable biosensing. It successfully addresses the critical challenges of detecting low-abundance biomarkers in the complex wound milieu while maintaining mechanical and biochemical fidelity over extended periods. For researchers and drug development professionals, this technology underscores the immense potential of interdisciplinary approaches that merge materials science, nanotechnology, and bioengineering. It establishes a new benchmark for intelligent, autonomous diagnostic systems that can provide a quantitative, comprehensive foundation for personalized therapeutic interventions in chronic wound management and beyond.
Closed-loop control systems represent a transformative approach in precision therapy, enabling the real-time monitoring of physiological conditions and automatic adjustment of treatments based on direct feedback. By seamlessly integrating sensing capabilities with on-demand therapeutic interventions, these systems offer enhanced accuracy, adaptability, and effectiveness while reducing the risks of over- or under-treatment [52]. The fundamental principle involves a continuous cycle: a biosensor detects a specific physiological signal or biomarker, a control algorithm processes this information and makes a decision, and an actuator delivers a therapeutic intervention in response, thereby creating an autonomous self-regulating medical system [53] [52].
The development of these advanced systems is intimately linked to progress in soft and flexible bioelectronics materials research. A fundamental challenge in biomedical device design has been the mechanical and chemical mismatch between traditional rigid electronic implants and soft biological tissues, which often leads to device failure through corrosion by biofluids and associated foreign body response (FBR) [32] [35]. Recent innovations in materials science have yielded soft, tissue-like composites with moduli similar to biological tissues (<1 kPa), enabling the creation of bioelectronic platforms that establish functional, stable interfaces for long-term monitoring and stimulation equipped with diagnostic/therapeutic capabilities [32] [35]. These advances are critical for implementing effective closed-loop systems across various medical applications, from diabetes management to neurostimulation and bladder disease treatment [53] [52] [54].
Soft Bioelectronics for Biomedical Integration
Material Foundations for Biointerfacing
The effectiveness of closed-loop therapeutic systems fundamentally depends on the seamless integration of biomedical devices with biological tissues. Recent breakthroughs in soft bioactive materials have focused on achieving mechanical compatibility, biochemical signaling, and sustainable energy solutions to overcome the limitations of traditional rigid implants. The core material platforms enabling this integration include self-healing hydrogels, bio-adhesive composites, and substrates with engineered microstructural topologies that actively suppress immune responses [32] [35].
Advanced material systems now integrate multiple functional layers to address various interface challenges simultaneously. One pioneering approach features a three-layer architecture: (a) mussel-inspired catechol-functionalized polyurethane elastomer substrates with brain tissue-like modulus (<1 kPa) for mechanical compatibility; (b) conductive hydrogels crosslinked by dynamic borate ester bonds, exhibiting ultrahigh toughness (420 MJ/m³) for signal transmission stability; and (c) MXene-silk fibroin composite anti-inflammatory coatings that suppress immune responses via reactive oxygen species (ROS) scavenging [32]. This multiscale design actively modulates macrophage polarization during early implantation and restores 90% conductivity within 48 hours post-mechanical damage, addressing both the mechanical and biochemical aspects of tissue integration [32].
Performance Metrics of Advanced Bioelectronic Materials
Table 1: Performance characteristics of advanced bioactive materials for closed-loop systems
| Material Platform | Key Properties | Performance Metrics | Tissue Application |
|---|---|---|---|
| Self-healing hydrogel/elastomer composites | Dynamic borate ester bonds, catechol-functionalization | 90% conductivity restoration in 48h, 1.2 S/cm conductivity under 100% strain | Neural interfaces, cardiac patches |
| Bio-adhesive composites | Mussel-inspired chemistry, tissue-like modulus (<1 kPa) | Ultrahigh toughness (420 MJ/m³), 40% improved motion artifact suppression | Cortical implants, epidermal sensors |
| Anti-inflammatory coatings | MXene-silk fibroin, ROS scavenging | Fibrous capsule thickness reduced to 28.6 ± 5.4 μm vs. 85.2 ± 12.7 μm in controls | Chronic implants, neural interfaces |
| Vascularized conductive networks | Microfluidics-assisted 3D printing | Curvature adaptation radius of 200 μm, 8.7% impedance increase after 10,000 cycles | Organ-scale interfaces, precision drug delivery |
Validation through rat cortical implantation experiments demonstrated the superiority of these advanced materials, with stable electrophysiological signal acquisition over 30 days (signal-to-noise ratio of 37 dB compared to 15 dB for conventional Pt electrodes) [32]. Compared to commercial silicon-based Utah arrays, these systems improved motion artifact suppression by 40% (RMS error <15 μV) and achieved synchronized drug release with 82% cumulative release over 72 hours, making them ideal platforms for closed-loop therapeutic applications [32].
Biosensing Technologies for Physiological Monitoring
Principles and Modalities of Biosensing
Biosensors serve as the critical detection component in closed-loop systems, functioning as analytical instruments that measure variations in biological activity and transform them into quantifiable electronic signals [54]. The escalating demand for real-time health monitoring, particularly for chronic diseases, has driven innovations in biosensor technology, with the market size estimated at USD 30.25 billion in 2024 and projected to grow at a compound annual growth rate of 8.7% from 2025 to 2034 [54]. Intravascular biosensors represent a particularly groundbreaking advancement, as they bridge traditional diagnostic approaches with practical methods for assessing physiological parameters directly within the circulatory system, enabling unparalleled opportunities for early disease detection and continuous monitoring [54].
The operational principles of biosensors vary based on their transduction mechanisms and target applications. Electrochemical biosensors leverage reactions that generate or consume electrons, typically measuring current or potential changes. Optical biosensors utilize light absorption, emission, or scattering properties. Other modalities include magnetic, acoustic, and thermal biosensors, each with distinct advantages and limitations for specific biomedical applications [54]. The selection of an appropriate sensing modality depends on factors including the target biomarker, required sensitivity and specificity, operational environment, and integration capabilities with therapeutic components.
Comparative Analysis of Biosensor Technologies
Table 2: Classification and characteristics of biosensors for closed-loop systems
| Biosensor Type | Applications | Advantages | Disadvantages | Integration Potential |
|---|---|---|---|---|
| Electrochemical | Glucose monitoring, blood pressure assessment | High sensitivity, broad applicability | Sensitivity to chemical interferences | High - compatible with miniaturized systems |
| Optical | Oxygen saturation, biomarker detection | Safety, non-invasiveness | Limited long-term durability | Moderate - requires external components |
| Magnetic | Pathogen detection, cancer biomarkers | High specificity, no optical background | Requires external magnet setups, limited commercial use | Low - challenging miniaturization |
| Acoustic (SAW, QCM) | Virus identification, small molecule sensing | Label-free, real-time, high sensitivity | Sensitive to environmental conditions | Moderate - specialized fabrication |
| Thermal | Enzyme activity, small molecule sensing | Simple readout, label-free | Low sensitivity, affected by ambient temperature | Low - thermal management challenges |
Recent advances have produced highly specialized biosensors with exceptional performance characteristics. For instance, a durable, enzyme-free glucose sensor based on a nanostructured composite electrode integrated on a printed circuit board combines highly porous gold with polyaniline and platinum nanoparticles to achieve high sensitivity (95.12 ± 2.54 µA mM−1 cm−2) and excellent stability in interstitial fluid [55]. Similarly, a terahertz surface plasmon resonance biosensor utilizing a graphene-integrated Otto configuration demonstrates exceptional phase sensitivity of up to 3.1043×10⁵ deg RIU⁻¹ in liquid sensing through active modulation of graphene's conductivity via an external magnetic field [55]. These technological improvements directly enhance the sensing capabilities available for closed-loop therapeutic systems.
Actuation Mechanisms for Therapeutic Intervention
Stimuli-Responsive Drug Delivery Systems
The actuation component of closed-loop systems delivers therapeutic interventions in response to signals from the control system. In biomedical applications, this most commonly involves controlled drug release through various mechanisms. Intravesical drug delivery, which involves administering drugs directly into the bladder via a catheter, exemplifies the advantages of localized therapeutic intervention: direct application ensures high local drug concentrations at the target site, minimizes systemic side effects, and allows for increased residence time of the drug in the bladder [53]. Similar targeted delivery approaches are being developed for various anatomical locations and clinical applications.
Stimuli-responsive materials form the foundation of advanced drug delivery mechanisms in closed-loop systems. These materials release therapeutic payloads in response to specific triggers, which can be exogenous (externally applied) or endogenous (originating from physiological changes). Ultrasound-driven systems offer non-invasive external control with precise spatial and temporal resolution. Osmosis-based approaches leverage natural physiological processes for autonomous operation. Swelling hydrogels respond to environmental changes such as pH, temperature, or specific biomarkers to modulate drug release kinetics [53]. These mechanisms enable on-demand triggering of therapeutic interventions with enhanced treatment efficacy compared to conventional continuous delivery approaches.
Experimental Protocol: Fabrication of a Stimuli-Responsive Hydrogel Drug Delivery System
Objective: To fabricate and characterize a glucose-responsive insulin delivery system for diabetes management.
Materials Required:
- Glucose oxidase enzyme
- Catalase
- pH-responsive hydrogel matrix (e.g., poly(diethylaminoethyl methacrylate))
- Phosphate buffer solution (PBS, pH 7.4)
- Insulin solution
- Diffusion cells with semi-permeable membranes
- Glucose solutions at various concentrations (50-400 mg/dL)
Methodology:
- Enzyme Immobilization: Immobilize glucose oxidase and catalase within the pH-responsive hydrogel matrix using covalent bonding via carbodiimide chemistry.
- Drug Loading: Soak the enzyme-loaded hydrogels in concentrated insulin solution (5 mg/mL) for 24 hours at 4°C to allow for equilibrium swelling and drug uptake.
- System Assembly: Encapsulate the drug-loaded hydrogel within a semi-permeable membrane that permits glucose diffusion but retains larger molecules.
- Release Kinetics Characterization: Place the assembled system in diffusion cells containing PBS with varying glucose concentrations (50-400 mg/dL). Sample the receptor compartment at predetermined time intervals and quantify insulin release using HPLC.
- Responsiveness Assessment: Calculate the release rate ratio between high glucose (400 mg/dL) and basal glucose (100 mg/dL) conditions to determine system responsiveness.
Validation Metrics:
- Response time: <10 minutes for significant release rate increase
- Release rate ratio: >3:1 (high glucose:basal glucose)
- Complete reversibility upon glucose normalization
- Maintenance of bioactivity for >30 days
This protocol exemplifies the integration of sensing and actuation functions within a single material system, creating an autonomous closed-loop therapeutic device without requiring external control electronics [53] [52].
Integrated Closed-Loop Systems in Practice
Implementation in Bladder Disease Management
Closed-loop systems show particular promise for managing chronic bladder conditions such as interstitial cystitis (IC) and bladder cancer. These conditions affect millions globally—IC impacts 3 to 8 million women and 1 to 4 million men in the United States alone, while bladder cancer represents the fourth most common cancer in men with approximately 82,290 new cases in 2023 [53]. Current treatment paradigms often require long-term administration of intravesical therapies such as Bacillus Calmette-Guérin (BCG) or chemotherapy drugs like mitomycin C, delivered directly into the bladder over several weeks or months [53].
A closed-loop system for bladder disease management integrates soft bioelectronic sensors that monitor disease-relevant parameters such as bladder pressure, volume, strain, and inflammatory biomarkers with miniaturized drug reservoirs and release mechanisms [53]. The sensors provide continuous assessment of bladder conditions, offering crucial feedback that enables adaptive therapeutic interventions. When the sensors detect predefined pathological signatures—such as those associated with inflammation or cancer recurrence—the system triggers localized drug release from integrated reservoirs. This approach minimizes the need for frequent catheterization and reduces systemic side effects by containing high drug concentrations at the target site [53].
Figure 1: Operational workflow of a closed-loop system for bladder disease management
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for developing closed-loop therapeutic systems
| Category | Specific Materials | Function/Application | Key Characteristics |
|---|---|---|---|
| Substrate Materials | Catechol-functionalized polyurethane elastomers | Mechanical compatibility layer | Tissue-like modulus (<1 kPa), self-adhesive |
| Conductive Elements | Borate ester-crosslinked hydrogels, MXene-silk fibroin composites | Signal transmission, electrode interfaces | Self-healing, high toughness (420 MJ/m³), ROS scavenging |
| Sensing Components | Glucose oxidase, oxygen electrodes, antibody-functionalized nanostars | Biomarker detection | High sensitivity, specificity, stability in biofluids |
| Drug Delivery Materials | pH-responsive hydrogels, temperature-sensitive polymers, ultrasound-triggered microparticles | Controlled release actuators | Stimuli-responsiveness, precise release kinetics |
| Fabrication Technologies | Microfluidics-assisted 3D printing | Device manufacturing | Vascularized conductive networks, 200 μm curvature adaptation |
Experimental Framework and Validation Protocols
Integrated Closed-Loop System Validation
Objective: To validate the performance of an integrated closed-loop system for management of interstitial cystitis (IC) in an animal model.
System Components:
- Soft capacitive pressure sensor with wireless readout capability
- Multiplexed electrochemical sensor array for inflammatory biomarkers (histamine, TNF-α)
- pH-responsive hydrogel drug reservoir loaded with therapeutic agent (lidocaine/heparin)
- Implantable control unit with signal processing and decision algorithms
- External reader/energy harvesting module
Experimental Protocol:
- System Calibration: Characterize sensor responses to pressure (0-100 cm H₂O) and biomarker concentrations (0-100 ng/mL) in artificial urine at 37°C.
- In Vitro Validation: Assess closed-loop operation in bladder phantom model with simulated IC flare conditions.
- Animal Model Implementation: Surgically implant the integrated system in established IC animal models (n=10) with appropriate controls.
- Triggering Threshold Definition: Program algorithm to initiate drug release when:
- Pressure exceeds 40 cm H₂O for >5 minutes, AND
- At least two inflammatory biomarkers increase >3x baseline levels
- Therapeutic Efficacy Assessment: Monitor pain behaviors (vocalization, abdominal grooming) and bladder inflammation (histology) over 28 days.
- System Performance Metrics: Record sensor stability, drug release accuracy, and foreign body response.
Validation Endpoints:
- Significant reduction in pain behaviors compared to open-loop controls (p<0.05)
- >70% decrease in inflammatory biomarkers within 6 hours of triggered drug release
- Maintenance of sensor functionality (>90% baseline sensitivity) throughout study period
- Minimal fibrous encapsulation (<50 μm thickness) at 28-day explant
This comprehensive validation framework ensures that both the technical performance and therapeutic efficacy of the closed-loop system are rigorously evaluated before clinical translation [53] [32].
Figure 2: Experimental workflow for validating closed-loop therapeutic systems
Future Directions and Challenges
Despite significant advances in closed-loop therapeutic systems, several challenges remain before widespread clinical adoption becomes feasible. Current limitations include a 23% conductivity decay after 28 days of biofluid immersion in some advanced materials, prompting research into biomimetic mineralization layers to enhance barrier functionality [32]. Long-term biostability, signal accuracy under dynamic physiological conditions, and regulatory approval processes represent critical hurdles that require continued interdisciplinary innovation [54].
Future research directions focus on enhancing both the materials and computational aspects of closed-loop systems. The integration of artificial intelligence for data analysis and prediction represents a promising avenue for improving control algorithms [54]. Similarly, the development of increasingly sophisticated bioactive interfaces that actively modulate the biological environment through controlled release of immunomodulatory factors or incorporation of endothelial cell-recruiting motifs could further enhance long-term device functionality [32] [35]. As these technologies mature, closed-loop systems are poised to transform the management of chronic diseases across multiple organ systems, advancing toward truly autonomous and personalized medicine.
The convergence of soft bioelectronics, advanced biosensing, and controlled therapeutic delivery represents a paradigm shift in medical treatment strategies. By creating systems that continuously monitor physiological states and automatically deliver appropriate interventions, closed-loop therapies offer the promise of maintaining patients within therapeutic windows with unprecedented precision, ultimately improving treatment outcomes while reducing healthcare burdens.
Ensuring Reliability and Stability: Tackling Long-Term Performance Challenges
As the field of bioelectronic medicine pivots toward soft and flexible architectures, the precise understanding of device performance metrics—reliability, stability, durability, and longevity—becomes paramount. These terms, often used interchangeably, represent distinct yet interconnected aspects critical for the clinical adoption and long-term success of implantable and wearable bioelectronic systems. This whitepaper provides a technical guide to define these concepts within the context of soft bioelectronics research, supported by quantitative data, standardized experimental protocols, and visualization tools. By establishing a clear conceptual framework, we aim to facilitate robust device development, accurate reporting of performance data, and accelerated translation of innovative bioelectronic therapeutics for researchers and drug development professionals.
Bioelectronic Medicine (BM) is an emerging field that harnesses miniaturized electronic devices to interface with the body’s electrically active tissues and organs, offering precise, targeted treatments for conditions ranging from chronic pain and epilepsy to Parkinson’s disease [56] [57]. A defining trend in recent years is the shift from rigid implants to soft and flexible bioelectronics, which aim to seamlessly integrate with the body's dynamic biological environments [56] [9] [57]. This transition, driven by advances in materials science such as stretchable electronics, ultrathin films, and hydrogels, seeks to overcome the mechanical mismatch caused by traditional rigid materials like silicon and metal, which often lead to inflammation, fibrosis, and eventual device failure [56] [57].
In this evolving landscape, ensuring the long-term performance of these sophisticated devices is a critical challenge. The complex interplay between novel soft materials and the harsh, dynamic in vivo environment necessitates a precise vocabulary to describe and quantify device performance. While the terms reliability, stability, durability, and longevity are fundamental, their conflation in scientific literature can obscure understanding and hinder progress. This guide establishes critical distinctions between these concepts, framing them within the unique demands of soft bioelectronics research to enable clearer communication, more targeted material selection, and more predictive device testing among researchers and scientists.
Core Definitions and Conceptual Framework
This section provides precise, technical definitions for the four key performance metrics, differentiating them and illustrating their interrelationships.
Individual Definitions
The following definitions are adapted from a pedagogical perspective on the reliability and stability of Bioelectronic Medicine [56] [57].
- Reliability refers to the probability that a bioelectronic device will function as intended—consistently and accurately—without failure over a specified period and under defined operating conditions. It is a statistical measure of functional performance, often quantified using metrics such as failure rates, mean time between failures (MTBF), and probability of failure. In essence, it answers the question: "Will the device work correctly every time it is needed?" [56]
- Stability denotes the ability of a device to maintain its functional and structural properties over time, including resistance to environmental and biological fluctuations. Stability can refer to electrical, chemical, or mechanical properties remaining unchanged within acceptable limits during operation. A stable device exhibits minimal drift in performance, ensuring predictable therapeutic or diagnostic outcomes for the patient [56].
- Durability pertains to the device’s physical resilience and robustness—its ability to withstand external stresses such as mechanical deformation (e.g., stretching, compression), temperature fluctuations, and prolonged exposure to bodily fluids without compromising its structural integrity or function [56].
- Longevity defines the total operational lifespan of a bioelectronic device before it becomes non-functional or requires replacement or intervention. It is the ultimate measure of a device's usable life, determined by the cumulative effect of factors such as material degradation, power supply limitations, and biological interactions [56].
Distinctions and Interrelationships
To illustrate the distinct nature of these concepts, consider the following examples [56]:
- Case I (Stable but Unreliable): A neurostimulator may function consistently within a stable operating range (i.e., its stimulation output remains constant over time) yet be unreliable due to intermittent power source failure. Its performance is stable when it works, but its inability to work consistently makes it unreliable.
- Case II (Reliable but non-Durable): A disposable ECG patch can provide highly reliable heart rate monitoring over a short period but lacks durability as its adhesive degrades quickly due to sweat and skin oils, limiting its structural integrity.
- Case III (Durable and Longevous but Unreliable): A pacemaker with a highly durable titanium housing may last a long time within the body but can be unreliable if its internal electrodes degrade or corrode, leading to intermittent performance failures.
These concepts are not isolated but exist in a hierarchical relationship, visualized below.
Diagram 1: Performance Metric Relationships. The diagram shows how Durability and Stability are foundational properties that contribute to overall Reliability, which collectively determines the device's Longevity. The dashed line indicates that Durability can influence Stability (e.g., a physically damaged device may experience electrical instability).
Quantitative Metrics and Material Considerations for Soft Bioelectronics
The mechanical and operational requirements for soft bioelectronics differ significantly from those of traditional rigid devices. The table below summarizes key performance metrics and the associated material properties that researchers must evaluate.
Table 1: Performance Metrics and Material Properties in Soft Bioelectronics
| Performance Metric | Key Quantitative Indicators | Relevant Material Properties in Soft Bioelectronics |
|---|---|---|
| Reliability | Mean Time Between Failures (MTBF); Failure Rate (%) [56] | Adhesion Strength: Peel strength (N/m) to ensure conformal contact with tissue [9]. Cyclic Loading Endurance: Number of cycles before electrical failure under strain [9]. |
| Stability | Electrical: Impedance drift (% change); Signal-to-Noise Ratio (SNR) decay [9]. Chemical: Leakage current (µA); Dissolution rate in saline (mg/day) [56]. | Water Vapor Transmission Rate (WVTR): Critical for encapsulation to prevent biofouling [56] [9]. Electrochemical Stability Window: Voltage range before material degradation [58]. |
| Durability | Fatigue Life: Cycles to fracture under applied strain (e.g., >100,000 cycles at 10-30% strain) [9]. Fracture Toughness (J/m²) [57]. | Young's Modulus: Should match target tissue (1 kPa - 1 MPa) for mechanical compliance [56] [57]. Stretchability: Ability to elongate (>10%, often >100% for ultra-soft devices) without failure [57]. |
| Longevity | Operational Lifespan (months/years) [56]. Time to 50% Performance Failure (e.g., for bioresorbable devices) [56]. | Biodegradation Rate: For resorbable implants (e.g., mass loss per week) [56]. Creep Resistance: Time-dependent deformation under constant stress [9]. |
The selection of materials is foundational to achieving these performance metrics. Soft bioelectronics rely on a different set of materials compared to conventional rigid electronics.
Table 2: Key Material Classes in Soft Bioelectronics Research
| Material Class | Function | Examples & Key Properties | Association with Performance Metrics |
|---|---|---|---|
| Elastomers & Soft Polymers | Substrate, Encapsulation | Polydimethylsiloxane (PDMS): Biocompatible, stretchable. Parylene-C: Ultra-thin, conformal, great barrier properties [9]. | Durability (Fatigue life), Stability (Encapsulation) |
| Electroactive Polymers (EAPs) | Sensing, Actuation, Conduction | PEDOT:PSS: Conducting polymer, high transconductance for OECTs [9] [59]. Polypyrrole (PPy): Used in ionic EAPs for low-voltage actuation [58] [59]. | Stability (Electrical drift), Reliability (Cyclic actuation) |
| Hydrogels & Biopolymers | Interface, Matrix | Gelatin: Thermoreversible, biocompatible, enables recyclable electrodes [60]. Ionic Gels: Used in ionic EAPs for soft actuation [59]. | Longevity (Resistance to biofouling), Stability (Hydration maintenance) |
| Nanocomposites | Conductive Fillers, Structural Reinforcement | MXene (Ti₃C₂Tₓ): High conductivity (>20,000 S/cm), processable into fibers for breathable electrodes [60]. Carbon Nanotubes (CNTs): Used to create conductive, pressure-sensitive nanofibers [9]. | Durability (Mechanical reinforcement), Reliability (Stable electrical pathways) |
Experimental Protocols for Performance Validation
Rigorous and standardized experimental validation is required to quantify the metrics defined in Section 3. The following protocols outline key methodologies for testing soft bioelectronic devices.
Protocol for In-Vitro Durability and Reliability Testing
Aim: To evaluate the mechanical durability and functional reliability of a soft electrode under simulated physiological conditions (e.g., cyclic strain, hydrated environment).
Workflow Overview:
Diagram 2: Durability Testing Workflow. This protocol subjects devices to cyclic mechanical strain while monitoring electrical performance, simulating the dynamic biological environment.
Detailed Steps:
- Sample Preparation: Fabricate the soft bioelectronic device (e.g., a conductive trace of PEDOT:PSS or a thin metal film on an elastomeric substrate like PDMS or a hydrogel).
- Mount in Bioreactor: Mount the sample in a stretchable bioreactor chamber filled with phosphate-buffered saline (PBS) at 37°C to simulate body temperature and ionic environment [9].
- Apply Cyclic Strain: Program a mechanical tester (e.g., a Bose ElectroForce or similar instrument) to apply uniaxial or biaxial cyclic strain to the substrate. A common test protocol involves 10-30% strain at 1 Hz for >100,000 cycles to simulate long-term movement [9].
- Monitor Electrical Performance: Use an impedance analyzer or source measure unit to continuously or periodically monitor the device's electrical properties.
- Reliability Metric: Record the number of cycles until electrical failure (e.g., open circuit) or a predefined increase in impedance (e.g., 50%) occurs [56].
- Durability Metric: The total number of cycles sustained before physical fracture (crack propagation) is observed.
- Post-Test Analysis: Use Scanning Electron Microscopy (SEM) to inspect for micro-cracks and profilometry to assess delamination or changes in surface topography.
Protocol for Stability Assessment
Aim: To quantify the electrical and electrochemical stability of a device under accelerated aging conditions.
Detailed Steps:
- Accelerated Aging Setup: Place devices in an environmental chamber at elevated temperature (e.g., 60-70°C) and high relative humidity (e.g., 90% RH). This accelerates the diffusion of water vapor, a primary cause of device failure.
- Water Permeation Analysis: Periodically measure the Water Vapor Transmission Rate (WVTR) of the encapsulation layer. A low WVTR is critical for long-term stability [56] [9].
- Electrochemical Characterization:
- Leakage Current: Measure the current flowing through the device's encapsulation or substrate when a small bias voltage is applied. An increasing trend indicates a breakdown of insulation and loss of chemical stability [56].
- Cyclic Voltammetry (CV): Perform CV in a saline solution to determine the electrochemical stability window. Scan the voltage and identify the potentials where oxidation and reduction currents rapidly increase, indicating the onset of Faradaic reactions and material degradation [58]. This defines the safe operating limits for stimulation.
- Electrical Drift Measurement: For sensors, monitor the baseline signal and sensitivity drift over time under constant environmental conditions. A stable device should exhibit minimal drift.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Experimental Validation
| Item | Function in Experiment | Example & Specification |
|---|---|---|
| Simulated Biological Fluid | Mimics the ionic composition and osmolarity of the body for in-vitro testing. | Phosphate Buffered Saline (PBS), pH 7.4. Artificial sweat or cerebrospinal fluid for specific applications. |
| Elastomeric Substrate | Provides a soft, stretchable base for device fabrication, matching tissue mechanics. | Polydimethylsiloxane (PDMS), e.g., Sylgard 184, with a tunable Young's modulus (e.g., 0.5 - 2 MPa) [9]. |
| Conductive Polymer Ink | Creates flexible, conductive traces for electrodes and interconnects. | PEDOT:PSS dispersion, often mixed with co-solvents (e.g., DMSO) and surfactants to enhance conductivity and film stability [9] [59]. |
| Electrochemical Cell Setup | Enables characterization of electrochemical stability and impedance. | Three-electrode cell: Working electrode (device), reference electrode (e.g., Ag/AgCl), counter electrode (e.g., Pt wire). |
| Encapsulation Material | Protects the device from the biological environment, critical for longevity. | Parylene-C, deposited via chemical vapor deposition to form a conformal, pinhole-free barrier [9]. Ultrathin epoxy or silicone layers. |
The successful development and clinical translation of next-generation soft bioelectronics hinge on a precise and universally understood lexicon for device performance. The distinctions between reliability, stability, durability, and longevity are not merely semantic; they are foundational to setting clear design goals, selecting appropriate materials, designing predictive tests, and accurately interpreting experimental data. As research pushes the boundaries with increasingly sophisticated materials—from electroactive polymers and recyclable MXene composites to fully bioresorbable circuits—adhering to these critical distinctions will be essential. By adopting this structured framework, researchers and drug development professionals can better navigate the complexities of this field, ultimately accelerating the creation of robust, long-lasting, and clinically viable bioelectronic medicines.
Soft bioelectronics represent a transformative frontier in medical technology, enabling advanced therapeutic solutions and continuous health monitoring through seamless integration with biological tissues. However, the operational longevity and fidelity of these devices are critically challenged by three persistent factors: biofouling, the unwanted adhesion of proteins and microorganisms that degrades sensor function; mechanical fatigue, the cumulative material damage from repeated deformation leading to failure; and environmental drift, performance instability under variable physiological and external conditions [57] [61] [62]. These intertwined degradation mechanisms can significantly compromise device reliability, signal accuracy, and ultimately, clinical utility. This whitepaper synthesizes current materials science and engineering strategies to mitigate these challenges, drawing upon recent advances in biomimetic design, nanostructured materials, and multifunctional composites. The solutions presented herein are essential for realizing the full potential of durable, high-fidelity bioelectronic systems for long-term biomedical applications.
Biofouling: Mechanisms and Advanced Mitigation Strategies
Biofouling occurs when proteins, cells, or microorganisms adhere to bioelectronic surfaces, forming a biofilm that impairs device function by increasing impedance, causing signal drift, and potentially inducing inflammation [61]. Effective antifouling strategies must prevent initial protein adsorption and inhibit subsequent microbial colonization.
Material and Chemical Antifouling Approaches
Table 1: Material-Based Strategies for Biofouling Mitigation
| Strategy | Key Material/Approach | Mechanism of Action | Reported Efficacy | Key Advantage |
|---|---|---|---|---|
| Tetrahedral DNA Nanostructures | Self-assembled DNA probes [48] | Creates a highly ordered, hydrophilic, and non-fouling surface that sterically hinders protein adhesion. | >50% reduction in BSA protein adhesion [48] | Inherent biocompatibility and programmability |
| Electroless Nano-Coating | Nano-copper coating on Titanium [61] | Releases copper ions that disrupt microbial cell membranes and inhibit biofilm formation. | ~95% reduction in biofilm biovolume in pilot-scale tests [61] | Durable, non-toxic anti-biofilm activity |
| Biomimetic Hydrogel Coatings | Genipin-crosslinked gelatin with tannic acid [63] | Forms a hydrated, smooth surface that creates a physical and chemical barrier to foulant adhesion. | Maintains function after 9-day in vivo ECG monitoring [63] | Excellent biocompatibility and skin conformity |
| Metal-Organic Frameworks (MOFs) | Biopolymer-based hydrogels with MOFs [61] | Controlled release of bioactive ions provides sustained antifouling and anti-corrosion effects. | Excellent inhibitory properties in fouling environments [61] | Long-term, controlled release capability |
Experimental Protocol: Assessing Antifouling Efficacy
The following protocol is adapted from methods used to evaluate nano-copper coatings on titanium condenser tubes, relevant for in vitro assessment of biofouling resistance [61].
- Sample Preparation: Fabricate the test substrate (e.g., nano-copper coated surface) and a control (e.g., pristine titanium). Sterilize all samples using UV light or ethanol immersion.
- Biofilm Cultivation: Immerse samples in a nutrient-rich microbial culture (e.g., containing sulfate-reducing bacteria (SRB) or a standard laboratory biofilm-forming strain like Pseudomonas aeruginosa) and incubate under optimal growth conditions (e.g., 37°C) for 24-72 hours to allow biofilm establishment.
- Post-Treatment Analysis:
- Microbiological Analysis: Gently rinse samples to remove non-adherent cells. Detach the biofilm via sonication or scraping, then perform serial dilution and plate counting to quantify viable cells (CFU/cm²).
- Confocal Laser Scanning Microscopy (CLSM): Stain the biofilm on the sample surface with fluorescent dyes (e.g., SYTO 9 for live cells). Image using CLSM to determine biofilm thickness, biovolume, and 3D architecture.
- Surface Analysis: Use Scanning Electron Microscopy (SEM) to visualize the topography and density of the adhered biofilm.
Mechanical Fatigue: Ensuring Long-Term Mechanical Reliability
Mechanical fatigue in soft bioelectronics results from repeated stretching, bending, and compression during use, leading to microcracks, delamination, and ultimately, electrical failure. Strategies focus on enhancing the intrinsic toughness of materials and engineering structures that dissipate strain energy.
Material and Structural Solutions for Fatigue Resistance
Table 2: Strategies for Enhanced Fatigue Resistance
| Strategy | Material/Design | Key Mechanical Properties | Reported Durability | Primary Advantage |
|---|---|---|---|---|
| Hydrogel-Elastomer Composite | Organic Hydrogel/Porous Ecoflex (OHPE) [64] | Fracture toughness: ~3540 J/m²; Low hysteresis. | >5,000 cycles with <10% residual strain [64] | Cytoskeleton-inspired; extreme robustness |
| Hierarchical Bonding Eutectogel | OMIEC Eutectogel [65] | Toughness: 4.5x conventional gels; Stretchability: >1500%. | >100,000 stretch-release cycles [65] | Autonomous self-healing; ultralow hysteresis |
| Nanofiber-Reinforced Substrate | Electrospun PAN/TPU Nanofiber with Gold Electrodes [48] | Stable DC resistance and electrochemical performance under bending. | <4% resistance variation after 2,000 bending cycles [48] | Excellent breathability and softness for wounds |
| Ultra-thin Organohydrogel Film | PU-reinforced Genipin-Gelatin Nanofilm [63] | Thickness: 392 nm; Stretchability: 166%; Toughness: 3.0 MJ/m³. | >1,000 cycles at 100% strain [63] | Skin-like conformity reduces effective strain |
Experimental Protocol: Cyclic Fatigue Testing
This protocol outlines a standard method for evaluating the mechanical and electrical fatigue resistance of soft conductive materials, such as eutectogels or hydrogel composites [64] [65].
- Sample Fabrication: Prepare the test material in a dog-bone shape using a mold or precise cutter, ensuring consistent dimensions (e.g., 50 mm × 10 mm × 1 mm).
- Setup Configuration: Mount the sample on a universal testing machine (UTM) equipped with an environmental chamber if needed. Attach a multimeter or LCR meter to the sample to monitor electrical resistance in real-time.
- Cyclic Loading: Program the UTM to apply cyclic tensile strain. Parameters should be selected based on the application (e.g., 0-50% strain for skin-worn devices, at a frequency of 1 Hz).
- Data Collection:
- Mechanical Data: Record stress-strain curves for every Nth cycle (e.g., every 100th cycle) to track changes in modulus, hysteresis, and permanent set.
- Electrical Data: Continuously log the electrical resistance (R) of the sample. Calculate the relative resistance change (ΔR/R₀).
- Failure Analysis: Continue testing until sample fracture or a predefined degradation threshold (e.g., 100% increase in resistance). Post-test, examine the fracture surfaces via SEM to identify failure mechanisms.
Environmental Drift: Stabilizing Performance in Variable Conditions
Environmental drift refers to performance instability caused by changes in temperature, humidity, and the chemical composition of the surrounding biological milieu. This can manifest as ionic conductivity changes in hydrogels or signal baseline drift in sensors.
Strategies for Environmental Resilience
A key approach involves formulating materials that maintain their properties across a wide range of conditions. Solvent replacement strategies are particularly effective, where water in hydrogels is partially replaced with non-volatile agents like glycerol or salts [63]. For instance, a sub-400 nm organohydrogel film plasticized with a glycerol/NaCl/tannic acid electrolyte demonstrated stable performance from -80°C to 150°C and at 2% relative humidity, overcoming the dehydration and freezing vulnerabilities of conventional hydrogels [63]. Furthermore, the use of deep eutectic solvents (DES) in eutectogels provides a non-volatile, ion-conducting medium that is intrinsically stable against evaporation and freezing [65].
Another critical strategy involves robust encapsulation to shield sensitive electronic components from the aqueous, ion-rich physiological environment. While soft elastomers like Ecoflex and PDMS are commonly used, recent advances focus on ultra-thin, conformal, and high-density barrier layers that prevent water and ion permeation without compromising mechanical softness [57].
Experimental Protocol: Environmental Stability Testing
- Baseline Characterization: Measure the key performance metrics of the device (e.g., impedance for a sensor, conductivity for a conductor) under standard conditions (e.g., 25°C, 50% RH).
- Environmental Chamber Testing: Place the device in an environmental chamber and subject it to defined stress cycles. A single cycle could include:
- Temperature: -20°C for 1 hour → 25°C for 1 hour → 60°C for 1 hour.
- Humidity: 2% RH for 12 hours → 90% RH for 12 hours.
- In-situ Monitoring: Continuously or intermittently monitor the performance metrics (e.g., electrical resistance, sensing signal) throughout the stress test.
- Post-Test Analysis: After a predetermined number of cycles (e.g., 100 cycles), return the device to standard conditions and perform a final characterization. Compare the results to baseline to quantify performance drift.
Integrated Design and The Scientist's Toolkit
Successful bioelectronic devices often integrate multiple strategies to simultaneously address biofouling, fatigue, and environmental drift. A prominent example is a wound monitoring patch that uses a tetrahedral DNA (TDNA) structure on a soft, breathable nanofiber substrate. The TDNA provides resistance to biofouling and nuclease degradation, while the nanofiber substrate offers mechanical durability and gas permeability, ensuring patient comfort and stable performance in the complex wound environment [48].
Table 3: Research Reagent Solutions for Fabricating Robust Soft Bioelectronics
| Reagent / Material | Function in Research | Key Property / Rationale |
|---|---|---|
| Genipin [63] | Natural crosslinker for protein-based hydrogels (e.g., gelatin). | Forms robust covalent bonds; enhances mechanical strength and thermal stability; more biocompatible than glutaraldehyde. |
| Glycerol [63] [65] | Hydrogen-bond donor in DES; plasticizer and humectant in hydrogels. | Suppresses ice crystal formation and water evaporation, conferring freeze-tolerance and long-term hydration stability. |
| Tannic Acid (TA) [63] | Multifunctional polyphenol additive. | Enhances adhesion to skin/substrates; provides antioxidant and antibacterial properties; can participate in crosslinking. |
| Polyurethane (PU) Nanomesh [63] | Electrospun reinforcement scaffold. | Imparts high mechanical toughness and tear resistance to ultra-thin films while maintaining gas permeability. |
| Choline Chloride (ChCl) [65] | Hydrogen-bond acceptor for forming Deep Eutectic Solvents (DES). | Creates a biocompatible, non-volatile, and ionically conductive liquid medium for stable eutectogels. |
| PEDOT:PSS [65] | Conductive polymer for organic mixed ionic-electronic conductors (OMIECs). | Provides high electrical conductivity and mixed conduction in hydrated/stretched states; enables high-sensitivity sensing. |
| Ecoflex Elastomer [64] | Soft, stretchable substrate or matrix. | Offers extreme stretchability (>900%), low modulus, and excellent biocompatibility for substrate and composite design. |
The path toward reliable, long-lasting soft bioelectronics hinges on a multi-faceted defense against biofouling, mechanical fatigue, and environmental drift. No single solution is sufficient; instead, a synergistic approach that combines biomimetic materials, intelligent structural design, and strategic formulation is required. The strategies detailed in this whitepaper—from DNA nanostructures and fatigue-resistant composites to environmentally stable eutectogels—provide a robust toolkit for researchers. Continued innovation in these areas is paramount for translating laboratory breakthroughs into clinical realities, ultimately enabling bioelectronic devices that patients can rely on for years, not just days.
The emergence of soft bioelectronics represents a paradigm shift in physiological monitoring, enabling seamless integration with the human body for continuous data acquisition. These devices conform to the body's soft, curvilinear structures, allowing collection of vital health parameters during daily activities with minimal discomfort. However, achieving reliable signal fidelity remains a significant challenge due to the pervasive presence of motion artifacts and electrical noise. These interference sources substantially degrade signal quality, compromising the accuracy and reliability of physiological measurements essential for both clinical diagnostics and research applications. Within the broader context of soft bioelectronics materials research, addressing these signal integrity issues is paramount for translating laboratory innovations into real-world healthcare solutions.
Soft bioelectronic systems are particularly vulnerable to motion artifacts because they are highly exposed to external forces and mechanical stress. These devices are subject to both internal mechanical stress from body movements and external environmental forces, making them susceptible to signal disruption [62]. Motion artifacts typically originate at the critical device-skin interface, where routine activities such as bending, stretching, vibration, and shear stress induce mechanical strain that alters the electrical properties of both the bioelectronics and the interface, leading to significant signal distortion [62]. For critical electrophysiological signals including electrocardiogram (ECG), electroencephalogram (EEG), and electromyogram (EMG), both active body motions (walking, running, jumping) and passive body activities (breathing, heartbeat, pulse) contribute substantially to motion artifacts [62].
Simultaneously, electrical noise from multiple sources further contaminates biosignals. Electromyography (EMG) signals, for instance, can be contaminated by various types of noise, interference, and artifacts, leading to potential data misinterpretation [66]. These contaminants include baseline noise (inherent electronic noise), interference noise (such as power-line interference and physiological crosstalk), and artifacts from multiple sources [66]. The complex interplay between motion-induced artifacts and electrical noise creates a multifaceted challenge that requires integrated solutions spanning materials science, device design, and signal processing techniques.
Understanding the specific nature and characteristics of different noise sources is essential for developing effective mitigation strategies. Contaminants in biosignals can be categorized based on their origin, spectral characteristics, and impact on signal quality.
Table 1: Classification of Primary Noise Sources in Bioelectronic Signals
| Noise Category | Subtype | Spectral Characteristics | Origin | Impact on Signals |
|---|---|---|---|---|
| Motion Artifacts | Active motion artifacts | Low frequency (< 10 Hz) | Body movements (walking, running) | Baseline wander, signal distortion |
| Passive motion artifacts | Low frequency (0.1-5 Hz) | Breathing, heartbeat, pulse | Periodic baseline fluctuations | |
| Baseline Noise | Thermal noise | Broadband uniform | Amplification systems | Decreased signal-to-noise ratio |
| Electrochemical noise | Low frequency (1/f spectrum) | Skin-electrode interface | Signal attenuation >20 Hz | |
| Interference Noise | Power-line interference | 50/60 Hz and harmonics | Ambient electromagnetic radiation | Periodic sinusoidal contamination |
| Physiological interference | Varies by source (ECG: up to 100 Hz) | Other biological signals | Signal superposition, crosstalk |
Motion artifacts manifest as low-frequency disturbances that often overlap with the spectral content of physiological signals of interest. As illustrated in Figure 1B, human mechanical motions typically occur in the frequency range below 10 Hz, which dangerously overlaps with the fundamental frequencies of key electrophysiological signals such as EEG (0.5-40 Hz) and ECG (0.5-40 Hz) [62]. This spectral overlap makes traditional filtering approaches particularly challenging, as aggressive filtering to remove motion artifacts may also eliminate crucial physiological information.
Electrical interference presents additional complications. Power-line interference (PLI) at 50/60 Hz and its harmonics introduces periodic sinusoidal contamination that can obscure physiological data [66]. Perhaps more problematic is physiological interference, such as ECG contamination in EMG signals, which manifests as a superimposed periodic signal whose energy may exceed that of the EMG signal itself, with a frequency spectrum extending up to 100 Hz [66]. Additionally, crosstalk from adjacent muscles presents a unique challenge as its spectrum is identical to the EMG signal of interest, making separation extremely difficult through conventional filtering approaches [66].
Diagram 1: Noise sources in bioelectronics and their impacts on signal fidelity. Motion artifacts and electrical noise originate from different sources but collectively degrade signal quality through various mechanisms.
Material-Level Solutions for Motion Artifact Reduction
Innovative materials strategies represent the frontline defense against motion artifacts in soft bioelectronics. These approaches focus on mitigating mechanical disturbances at their source through advanced material designs and device architectures. The development of soft conductive composites has emerged as a particularly promising avenue, with materials such as conductive polymers, functionalized hydrogels, and stretchable conductive nanocomposites enabling conformal contact with the dynamic skin surface while maintaining stable electrical properties [2].
A key advancement in this domain is the creation of selective-damping materials specifically engineered to absorb and dissipate mechanical vibrations that lead to motion artifacts. These emerging materials provide a promising route to overcome limitations in soft bioelectronics by enhancing stability during prolonged wear [62]. Selective-damping materials include viscoelastic polymers, hydrogels, and acoustic metamaterials tailored to the specific requirements of skin-interfaced bioelectronics. These materials function by filtering out low-frequency mechanical noise (typically below 10 Hz) associated with body movements while preserving the integrity of higher-frequency physiological signals [62].
Device-level design strategies have evolved along two primary philosophical approaches: strain-compliance and strain-resistance. The strain-compliance strategy aims to reduce mechanical energy transfer to the device by lowering its effective modulus through engineered structures including wavy geometries, serpentine interconnects, and Kirigami architectures [62]. These designs diffuse mechanical energy by allowing controlled deformation in noncritical regions, enabling stretchability in intrinsically non-stretchable materials. For instance, wavy, stretchable single-crystal silicon devices built on elastic substrates can withstand significant mechanical deformation without performance degradation [62]. Similarly, two-dimensional serpentine structures bonded to stretched soft elastomeric substrates and microscale Kirigami patterns have demonstrated remarkable ability to maintain electrical functionality under mechanical strain [62].
In contrast, the strain-resistance strategy strategically increases effective modulus in select regions to shield sensitive components from mechanical deformation. This approach typically employs high-stiffness "islands" or layers to protect critical electronic components, while the surrounding substrate utilizes softer, lower-modulus materials [62]. The "island-bridge" geometry, where rigid, small-footprint device islands connect through deformable serpentine or wavy interconnects, ensures that most external strain is absorbed by the compliant regions while delicate electronics on the stiff islands experience minimal mechanical stress [62]. This approach has been successfully implemented in various forms, including Ferris wheel-shaped island arrays in elastomeric substrates [62].
Table 2: Material-Level Solutions for Motion Artifact Reduction
| Strategy | Specific Approach | Key Materials | Mechanism of Action | Performance Metrics |
|---|---|---|---|---|
| Strain-Compliance | Wavy geometries | Elastic substrates (Ecoflex, PDMS) | Controlled deformation to dissipate strain | Stretchability >50% strain |
| Serpentine interconnects | Metal thin films (Au, Cu) | Out-of-plane buckling to absorb stress | Maintain conductivity at >100% strain | |
| Kirigami architectures | Polymer thin films | Strategic cutting for enhanced deformability | Direction-dependent stretchability | |
| Strain-Resistance | Island-bridge design | Rigid islands (Si) on soft substrates | Localized stiffness contrast | <5% strain on critical components |
| High-modulus layers | Composite materials | Selective mechanical shielding | 80% reduction in motion artifacts | |
| Conductive Composites | Phase-separated porous AgNWs | Silver nanowires in elastomer | Strain-insensitive conductive networks | <5% resistance change at 50% strain |
| Conductive hydrogels | PEDOT:PSS, polyacrylamide | Ionic/electronic conduction with softness | Tissue-like modulus (<10 kPa) | |
| Selective Damping | Viscoelastic polymers | Polyurethane, silicone blends | Frequency-dependent energy dissipation | Vibration attenuation >15 dB |
The development of conductive elastomeric composites represents another significant advancement for mitigating mechanical disturbances in dynamic conditions. These materials maintain high conductivity under frequent deformation, addressing a fundamental challenge in soft bioelectronics. A notable example is a conductive phase-separated porous silver nanowire (AgNW) nanocomposite that exhibits remarkable insensitivity to mechanical strain, enabling stable biosignal recording under dynamic scenarios [62]. This strain-insensitive behavior stems from the material's unique porous structure that accommodates deformation without significantly altering the conductive pathways.
Signal Processing Techniques for Noise Mitigation
When material-based approaches alone are insufficient to ensure signal fidelity, sophisticated signal processing techniques provide a complementary strategy for noise reduction. These computational methods operate on the acquired signals to separate desired physiological information from various contaminants. The most fundamental approach employs frequency-domain filtering, leveraging the distinct spectral characteristics of signals and noise. Traditional band-pass filtering has demonstrated utility in processing ECG signals under both rest and exercise conditions by attenuating frequency components outside the expected physiological range [62]. However, this approach has significant limitations when the spectral content of noise overlaps with the signals of interest, which commonly occurs with motion artifacts.
More advanced processing strategies have emerged to address these limitations. Adaptive filtering techniques dynamically adjust filter parameters based on the changing characteristics of signals and noise, making them particularly effective for non-stationary biosignals. Machine learning and deep learning models have recently shown remarkable promise in mitigating signal noise by learning complex patterns from data [62]. These data-driven approaches can identify and suppress artifacts while preserving physiological information, even when both components occupy similar frequency bands. As illustrated in Figure 1D, machine learning-based signal processing can effectively separate clean EMG signals from contaminated recordings [62].
For EMG signals specifically, various contaminant reduction methods enable full signal reconstruction without information loss. These include subtraction methods applied in the time domain, denoising methods performed after signal decomposition, and hybrid approaches that combine multiple techniques [66]. The suitability of specific methods depends on the types of contaminants present and the application requirements. When properly selected and implemented, these processing techniques can significantly improve signal quality while preserving the essential physiological information contained in the original biosignals.
A critical consideration in implementing signal processing solutions is the trade-off between noise reduction and signal integrity. Overly aggressive filtering or denoising can remove valuable physiological information along with noise, potentially leading to clinical misinterpretation. Therefore, the optimal approach often involves combining multiple complementary techniques with careful parameter selection based on the specific application requirements and signal characteristics.
Diagram 2: Signal processing workflow for noise reduction in biosignals. The systematic approach involves detection, identification, and quantification of contaminants before selecting and applying appropriate denoising methods tailored to specific noise types.
Experimental Protocols for Signal Fidelity Assessment
Rigorous experimental validation is essential for evaluating the effectiveness of signal fidelity enhancement techniques. Standardized assessment protocols enable meaningful comparison between different approaches and provide insights into their performance under various conditions. For material-based solutions, characterization should include both mechanical properties relevant to device-tissue integration and electrical performance under simulated physiological conditions.
A comprehensive experimental protocol for assessing motion artifact reduction begins with mechanical testing to quantify key parameters including effective modulus, stretchability, fatigue resistance, and adhesion strength. These tests should simulate realistic wearing conditions, including cyclic stretching comparable to skin deformation during body movements (typically 10-30% strain for most body locations). Concurrently, electronic characterization should evaluate how electrical properties including impedance, conductivity, and noise floor change under mechanical deformation. For instance, the strain-insensitive conductive porous silver nanowire nanocomposites should maintain stable impedance (preferably with less than 10% variation) across the expected strain range [62].
The critical phase of validation involves in vivo or simulated physiological testing with appropriate metrics for signal quality assessment. For electrophysiological signals such as ECG, EEG, and EMG, the signal-to-noise ratio (SNR) and signal-to-motion artifact ratio (SMR) provide quantitative measures of performance. These metrics should be evaluated under both static conditions (rest) and dynamic scenarios (exercise, movement) to comprehensively assess artifact rejection capabilities. Additionally, frequency-domain analysis can reveal specific noise components and their impact on signal integrity.
For signal processing techniques, validation should include comparison with reference "clean" signals acquired under controlled conditions where artifacts are minimized. Performance metrics may include percentage reduction in noise power, preservation of physiological information in the processed signals, and computational efficiency for real-time applications. When employing machine learning approaches, proper cross-validation procedures are essential to ensure generalizability beyond the training dataset.
A particularly informative experimental design involves simultaneously recording from conventional rigid electrodes and advanced soft bioelectronics under identical conditions to enable direct comparison. This side-by-side assessment provides clear evidence of performance improvements offered by new materials and processing techniques. Furthermore, long-term stability testing over hours or days reveals potential degradation in signal quality that might not be apparent in short-term experiments.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and implementation of advanced signal fidelity techniques requires specialized materials and reagents carefully selected for their specific properties and functions. This toolkit encompasses materials for device fabrication, characterization, and validation, forming the foundation for innovation in soft bioelectronics research.
Table 3: Essential Research Reagents and Materials for Signal Fidelity Enhancement
| Category | Specific Material/Reagent | Function/Application | Key Properties |
|---|---|---|---|
| Substrate Materials | Polydimethylsiloxane (PDMS) | Flexible device substrate | Low modulus, biocompatible, optically transparent |
| Polyurethane elastomers | Stretchable substrate | Tunable elasticity, durability, chemical resistance | |
| Ecoflex silicone | Ultra-soft substrate | Tissue-like softness, high stretchability (>900%) | |
| Conductive Materials | PEDOT:PSS | Conductive polymer electrode | High conductivity, mechanical flexibility, mixed ionic-electronic conduction |
| Silver nanowires (AgNWs) | Conductive networks | High aspect ratio, percolation networks, transparency | |
| Liquid metal alloys (e.g., EGaIn) | Stretchable interconnects | Extreme stretchability, self-healing capability | |
| Graphene & CNTs | Nanocomposite fillers | High conductivity, mechanical strength, large surface area | |
| Functional Materials | Conductive hydrogels | Soft biointerfaces | Tissue-matching modulus, high water content, ion conduction |
| Viscoelastic polymers | Selective damping | Frequency-dependent energy dissipation, tunable loss modulus | |
| Acoustic metamaterials | Mechanical filtering | Designed structures for targeted vibration attenuation | |
| Characterization Tools | Electrochemical impedance spectrometer | Interface characterization | Quantifies electrode-skin impedance across frequencies |
| Dynamic mechanical analyzer | Viscoelastic properties | Measures storage/loss moduli, damping coefficients | |
| Motion simulation systems | Artifact generation | Reproducible mechanical inputs for controlled testing |
The selection of substrate materials critically influences device mechanics and compatibility with biological tissues. Polydimethylsiloxane (PDMS) remains widely used due to its favorable combination of mechanical properties, biocompatibility, and straightforward processing [2]. For applications requiring extreme softness, Ecoflex silicone formulations offer tissue-matching modulus with exceptional stretchability. Polyurethane elastomers provide an intermediate option with enhanced durability and chemical resistance compared to silicone-based materials.
Conductive materials form the core of bioelectronic functionality. Transparent conductive electrodes based on PEDOT:PSS offer advantages including mechanical flexibility, mixed ionic-electronic conduction that facilitates signal transduction at the biological interface, and compatibility with solution processing [2]. Silver nanowire networks create deformable conductive pathways that maintain conductivity under strain, with performance dependent on nanowire aspect ratio, density, and percolation behavior [62]. For extreme stretchability requirements, liquid metal alloys based on gallium-indium systems offer unprecedented deformation capability with self-healing characteristics.
Functional materials with specialized properties enable advanced signal fidelity strategies. Conductive hydrogels bridge the gap between biological tissues and electronic systems through their high water content, tissue-matching mechanical properties, and dual ionic-electronic conduction capabilities [2]. Viscoelastic polymers engineered for selective damping provide frequency-dependent mechanical filtering, preferentially attenuating vibrations in the frequency range associated with motion artifacts while preserving signal integrity [62]. Emerging acoustic metamaterials extend this concept through carefully designed microarchitectures that manipulate mechanical wave propagation in ways not possible with conventional materials.
Future Directions and Concluding Remarks
The pursuit of enhanced signal fidelity in soft bioelectronics represents a dynamic research frontier with numerous promising directions for future investigation. The integration of multifunctional material systems that combine sensing, actuation, and signal processing capabilities within unified platforms offers particular potential. These systems could perform initial stages of signal conditioning directly at the device-skin interface, potentially reducing the burden on downstream processing components and minimizing information loss during signal transmission.
Advances in selective-damping materials specifically engineered for bioelectronic applications represent another compelling direction. The emerging class of materials that provide targeted filtering of low-frequency mechanical noise while preserving electronic functionality addresses a fundamental challenge in motion artifact reduction [62]. Future research will likely focus on optimizing these materials for specific physiological monitoring scenarios, potentially developing application-specific formulations with tailored mechanical and electrical properties.
The convergence of machine learning with materials design presents a transformative opportunity for signal fidelity enhancement. Data-driven approaches could accelerate the discovery of novel material compositions and architectures optimized for specific signal acquisition challenges. Furthermore, adaptive systems that dynamically adjust their properties in response to changing environmental conditions and motion patterns could provide robust performance across diverse real-world scenarios beyond controlled laboratory environments.
As the field progresses, standardization of evaluation methodologies and performance metrics will be essential for meaningful comparison between different approaches and facilitation of clinical translation. Establishing benchmark testing protocols that simulate realistic wearing conditions will provide more reliable predictions of real-world performance and accelerate the adoption of promising technologies in practical healthcare applications.
In conclusion, enhancing signal fidelity in soft bioelectronics requires an integrated approach spanning materials science, device engineering, and signal processing. Material-level solutions focusing on improved device-tissue interfaces and selective mechanical filtering provide the foundation for artifact reduction. These hardware strategies are usefully complemented by sophisticated signal processing techniques that separate noise from physiological information in the computational domain. As these complementary approaches continue to evolve and converge, they will enable increasingly reliable physiological monitoring in dynamic, real-world environments, ultimately transforming how we understand human health and deliver healthcare.
The advancement of soft and flexible bioelectronics represents a paradigm shift in medical therapeutics and continuous health monitoring, moving healthcare from clinical settings to personalized, daily life integration. A core challenge in this evolution lies in ensuring both the sustainable operation and biological safety of these devices during long-term implantation or wear. This technical guide examines the interconnected strategies for power management and biocompatibility that are fundamental to achieving this goal. We explore how recent breakthroughs in materials science, including the development of soft electronic materials and biodegradable components, are addressing the critical issues of the foreign body response and device longevity. Furthermore, the review details innovative energy harvesting and storage methods that promise to free devices from bulky batteries. By framing these discussions within the context of a broader thesis on soft bioelectronics materials research, this paper provides a structured framework for scientists and drug development professionals to develop the next generation of body-compliant, sustainable bioelectronic systems.
The field of bioelectronic medicine is undergoing a fundamental transformation, shifting from rigid, bulky implants toward soft, flexible devices that seamlessly integrate with the dynamic, curvilinear surfaces of biological tissues [57]. This transition to soft bioelectronics is driven by the necessity to mitigate the chronic foreign body response—an inflammatory reaction and fibrotic encapsulation triggered by the mechanical mismatch between traditional rigid implants (silicon, metals) and soft, dynamic tissues [57] [67]. This fibrotic encapsulation not only poses biocompatibility concerns but also significantly degrades device performance over time by impairing signal transduction for both sensing and stimulation applications [68].
Concurrently, the challenge of powering these devices for sustained operation without frequent surgical replacements or recharging remains a major hurdle. The ideal bioelectronic system must be both biologically invisible (fully biocompatible) and operationally self-sufficient [67] [69]. Long-term stability and sustainability therefore hinge on two pillars: (1) advanced biocompatibility achieved through physical and chemical material strategies that minimize the immune response, and (2) sophisticated power management that leverages efficient energy harvesting and storage solutions. This guide delves into the technical specifics of these intertwined strategies, providing a roadmap for researchers to develop devices that are both safe and sustainable for chronic use.
Biocompatibility: Engineering the Biological Interface
Achieving long-term biocompatibility is a multi-faceted endeavor focused on persuading the body to accept a synthetic device. The strategies can be broadly categorized into physical and chemical approaches.
Physical Biocompatibility: Mechanical Matching
The core principle of physical biocompatibility is to minimize the mechanical mismatch between the device and the host tissue to reduce micromotion-induced inflammation and fibrotic encapsulation.
- Material and Structural Softness: Utilizing materials with low Young's modulus (1 kPa – 1 MPa) and bending stiffness (< 10⁻⁹ Nm) that match the mechanical properties of soft tissues like the skin or brain [57]. This is achieved through the use of polymers, elastomers, and hydrogels in device substrates.
- Geometric Engineering: Employing designs such as ultra-thin films (< 100 µm), mesh geometries, and kirigami/origami-inspired structures that allow devices to conform to tissue surfaces, stretch with organ movement, and minimize irritation [57] [69].
- Device-Tissue Integration: Flexible devices enable conformal contact, which stabilizes the interface, reduces mechanical stress, and improves the fidelity of chronic signal recording and stimulation [57].
Chemical Biocompatibility: Material-Driven Harmony
Chemical biocompatibility addresses the molecular-level interactions at the device-tissue interface.
- Biologically Derived Materials: The use of sustainable and biocompatible materials is rising. Examples include:
- Silk Fibroin (SF): Known for its biocompatibility, toughness, and programmable biodegradability [70].
- Cellulose and its derivatives (CNF, CNC, BC): Offer excellent biocompatibility, flexibility, and are derived from abundant natural sources [70].
- Poly(lactic-co-glycolic acid) (PLGA): A biodegradable polymer widely used for its tunable degradation rate and FDA approval for certain applications [70].
- Surface Modifications: Crafting surfaces that mimic the biological environment to reduce biofouling and the foreign body response. This includes hydrogel coatings that provide a hydrous, soft interface and the immobilization of bioactive molecules like peptides to promote specific cellular interactions [67].
Table 1: Key Material Classes for Biocompatible, Soft Bioelectronics
| Material Class | Example Materials | Key Properties | Primary Applications |
|---|---|---|---|
| Elastomers | Polydimethylsiloxane (PDMS), Polyacrylamide (PAA) | Stretchable, soft, conformable | Substrates, encapsulation |
| Hydrogels | Polyvinyl alcohol (PVA), Alginate | High water content, tissue-like | Coatings, ionic conductors |
| Biodegradable Polymers | PLGA, Poly(lactic acid) (PLA), Silk Fibroin | Biocompatible, resorbable | Temporary implants, substrates |
| Cellulose-Based Materials | Bacterial Cellulose (BC), Cellulose Nanofibrils (CNF) | Sustainable, flexible, breathable | Substrates, wound dressings |
| Conductive Polymers | PEDOT:PSS, Polyaniline (PANI) | Conductive, relatively soft | Electrodes, interconnects |
The following diagram illustrates the key decision pathways and material strategies for achieving biocompatibility in implantable bioelectronics.
Power Management: Enabling Operational Sustainability
For long-term operation, especially in implantable scenarios, sustainable power management is critical. The trend is moving away from bulky, finite batteries toward energy harvesting and advanced storage.
Energy Harvesting from the Biological Environment
The body itself is a rich source of energy that can be scavenged to power low-energy electronics.
- Triboelectric Nanogenerators (TENGs): Convert mechanical energy from body movement, muscle stretching, or even blood flow into electricity via contact electrification [69] [70]. They are highly versatile and can be made from a wide range of soft polymers.
- Piezoelectric Generators (PEGs): Use materials like Poly (vinylidene difluoride) (PVDF) or Barium Titanate (BaTiO₃) to generate electrical charge in response to mechanical stress [70].
- Biofuel Cells: Utilize enzymatic or microbial catalysts to generate electricity from biochemical fuels present in bodily fluids, such as glucose from blood or interstitial fluid [69] [71]. This offers a continuous, chemically-based power source.
- Other Modalities: Thermoelectric generators (using body heat) and radiative wireless power transfer (using external sources) are also viable strategies for specific applications [67] [69].
Advanced Energy Storage Solutions
Harvested energy must be stored efficiently. Next-generation energy storage devices are being developed to align with the soft and biocompatible nature of modern bioelectronics.
- Soft and Flexible Batteries: The development of batteries using compliant components, such as hydrogel electrolytes and flexible electrodes, allows them to withstand deformation without performance loss [69].
- Biodegradable Batteries: A frontier in sustainable electronics, these batteries use materials like magnesium, iron, or polypeptides that safely dissolve in the body after their operational lifetime, eliminating the need for extraction surgery [70].
- Supercapacitors: Known for high power density and rapid charge/discharge cycles, supercapacitors are ideal for complementing energy harvesters and providing bursts of power for sensing or data transmission [69].
Table 2: Comparison of Energy Harvesting Technologies for Bioelectronics
| Energy Harvesting Method | Power Density Range | Advantages | Challenges |
|---|---|---|---|
| Triboelectric (TENG) | µW to mW / cm² | High voltage, diverse materials, high efficiency at low freq. | Long-term stability, encapsulation |
| Piezoelectric (PEG) | µW / cm² | Simple structure, relatively high power density | Brittle materials (inorganics), limited strain |
| Biofuel Cells | µW / cm² | Continuous power from bodily fluids, biocompatible | Low power density, enzyme stability |
| Thermoelectric | µW / cm² | Continuous operation, no moving parts | Low efficiency at small ΔT |
| RF Wireless Power Transfer | mW to 100s of mW | High power, well-established | Limited depth penetration, requires external emitter |
Experimental Protocols for Key Characterizations
Robust experimental validation is required to assess the success of biocompatibility and power management strategies.
Protocol: In Vivo Assessment of Foreign Body Response (FBR)
Objective: To quantitatively evaluate the chronic tissue response and fibrosis around an implanted soft electronic device.
Materials:
- Test device (soft/flexible) and control device (rigid, e.g., silicon).
- Animal model (e.g., rodent).
- Histology reagents: Formalin, paraffin, Hematoxylin and Eosin (H&E) stain, Masson's Trichrome stain.
- Immunohistochemistry (IHC) antibodies: Anti-CD68 (macrophages), Anti-α-SMA (myofibroblasts).
Methodology:
- Implantation: Surgically implant the test and control devices in subcutaneous or target tissue sites.
- Explanation: Sacrifice animals and explant the devices with surrounding tissue at multiple time points (e.g., 2, 4, 12 weeks).
- Histological Processing: Fix tissue in formalin, embed in paraffin, and section into thin slices.
- Staining and Analysis:
- H&E Staining: For general morphology and visualization of inflammatory cell infiltration.
- Masson's Trichrome: To specifically stain collagen fibers (blue) for quantitative analysis of fibrotic capsule thickness.
- IHC Staining: Use CD68 to identify total macrophages and to phenotype M1 (pro-inflammatory) vs. M2 (pro-healing) populations. Use α-SMA to identify activated myofibroblasts responsible for collagen deposition.
- Quantification: Measure capsule thickness from Trichrome slides using image analysis software. Count positively stained cells in IHC images to quantify immune response.
Protocol: In Vitro Characterization of an Energy Harvester
Objective: To measure the electrical output and mechanical reliability of a soft TENG or PEG.
Materials:
- Fabricated energy harvester device.
- Electrodynamic shaker or linear motor.
- Source meter/electrometer.
- Oscilloscope.
- Environmental chamber.
Methodology:
- Setup: Mount the device on the shaker. Connect electrodes to the source meter for current/voltage measurement and to the oscilloscope for real-time waveform visualization.
- Mechanical Input: Program the shaker to apply cyclic mechanical stimulation (e.g., compression, stretching) that mimics in vivo conditions (frequency: 1-5 Hz, strain: 5-25%).
- Electrical Output Measurement:
- Open-Circuit Voltage (Voc): Measure the voltage output without any load connected.
- Short-Circuit Current (Isc): Measure the current output when the terminals are shorted.
- Power Density: Connect a range of load resistors (e.g., 1 kΩ to 10 GΩ) and measure the voltage across them. Calculate power (P = V²/R) and normalize to the device's active area to determine power density.
- Stability Testing: Subject the device to millions of cycles in the environmental chamber (e.g., at 37°C and 90% relative humidity) to simulate long-term operation. Monitor the degradation of electrical output over time.
- Bio-Environmental Testing: Immerse the device in phosphate-buffered saline (PBS) at 37°C to test the stability of its performance and encapsulation under physiologically relevant conditions.
The following workflow diagram summarizes the key steps in characterizing a soft bioelectronic device's biocompatibility and power performance.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Soft Bioelectronics Development
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| PDMS (Sylgard 184) | Elastomeric substrate/encapsulation | Creating soft, stretchable device foundations and microfluidic channels. |
| PEDOT:PSS | Conductive polymer | Forming soft, compliant electrodes for neural interfacing or wiring. |
| PLGA | Biodegradable polymer | Fabricating temporary implants that resorb after a service period. |
| Silk Fibroin Solution | Bio-derived substrate/encapsulant | Serving as a water-soluble, biocompatible, and mechanically robust support layer. |
| IgG Anti-CD68 Antibody | Macrophage staining (IHC) | Identifying and quantifying the innate immune response to an implant. |
| Masson's Trichrome Kit | Collagen fiber staining | Visualizing and measuring the thickness of the fibrotic capsule. |
| PVDF | Piezoelectric polymer | Fabricating mechanical energy harvesters that respond to body movement. |
The trajectory of soft bioelectronics is set toward fully integrated, intelligent, and sustainable systems. Future developments will focus on closed-loop therapeutic systems that sense a physiological change, analyze the data on-board or via external communication, and deliver a tailored stimulus or drug dose in response [69]. The convergence of biocompatibility and power management will be key, exemplified by the exploration of living electronic components, such as conductive microbial nanowires from Geobacter, which offer the potential for biodegradable circuitry and power generation [71].
Furthermore, the push for sustainability will intensify, driving research into fully biodegradable device suites where sensors, processors, and power units safely dissolve after their functional lifetime, eliminating e-waste and the need for explanation surgeries [70] [71]. The integration of multimodal sensing (biophysical, biochemical, electrophysiological) onto a single, soft platform will provide a holistic view of patient health, moving us closer to the vision of personalized, predictive, and patient-centric digital health management [69] [72].
In conclusion, the safe and sustainable long-term operation of soft bioelectronics hinges on a deep, interdisciplinary understanding of the biological interface and energy autonomy. By leveraging advanced materials and clever engineering strategies for biocompatibility and power management, researchers are poised to create a new generation of bio-integrated devices that will fundamentally transform healthcare diagnostics and therapeutics.
Benchmarking Performance and Clinical Translation: A Comparative Analysis
The advancement of soft and flexible bioelectronics represents a paradigm shift in physiological monitoring, moving from clinical settings to integrated, user-centric applications in daily life. Within this framework, the electrode serves as the critical interface between the biological system and the electronic device. Its performance fundamentally dictates the fidelity of the entire system. Consequently, quantitative performance metrics, specifically Signal-to-Noise Ratio (SNR) and Electrode-Skin Impedance, are indispensable for benchmarking new electrode technologies against the clinical gold standard: silver/silver chloride (Ag/AgCl) gel electrodes. This guide provides an in-depth technical analysis of these metrics for emerging flexible bioelectrodes, offering a structured comparison and detailed methodologies to aid researchers in the development and validation of next-generation wearable sensors.
The limitations of conventional Ag/AgCl electrodes—including gel drying, skin irritation, and discomfort during long-term use—are well-documented [73]. Soft and flexible bioelectronics aim to overcome these challenges through materials and design innovations, such as flexible dry electrodes, textile-based sensors, and conductive polymers [74] [75]. However, the absence of a liquid electrolyte interface in many of these designs often leads to higher and more unstable contact impedance, which can degrade signal quality [76]. Therefore, a rigorous, quantitative comparison is essential to validate their performance and guide future material and structural optimizations.
Core Performance Metrics: Definition and Significance
Signal-to-Noise Ratio (SNR)
Signal-to-Noise Ratio (SNR) is a dimensionless metric that quantifies the level of a desired signal relative to the background noise. In the context of biopotential recording, it measures the clarity of the physiological signal (e.g., ECG, EEG) against inherent and environmental interference. It is typically expressed in decibels (dB):
SNR (dB) = 10 × log₁₀ (Psignal / Pnoise) = 20 × log₁₀ (Vsignal / Vnoise) [73]
A higher SNR indicates a cleaner, more interpretable signal. For wearable devices, which are susceptible to motion artifacts and electromagnetic interference, achieving a high SNR is a primary design objective. The QRS complex in an ECG signal is often used as the reference signal for SNR calculation due to its high amplitude and clinical significance [74].
Electrode-Skin Impedance
Electrode-Skin Impedance is the total impedance measured at the interface between the electrode and the skin. It is a complex, frequency-dependent value composed of resistive and capacitive components. Low and stable interface impedance is crucial for several reasons:
- High-Fidelity Signal Acquisition: It minimizes signal attenuation, particularly for weak, high-frequency components of biopotentials.
- Noise Immunity: A lower impedance interface is less susceptible to environmental electromagnetic noise, which can couple into high-impedance circuits [76].
- Stability: Stable impedance over time is critical for long-term monitoring, as fluctuations can introduce baseline drift and artifacts.
In conventional wet electrodes, the conductive gel penetrates the outer skin layer (stratum corneum), establishing a stable, low-impedance interface via ionic conduction. Dry and flexible electrodes, however, often rely on capacitive coupling or limited contact points, leading to inherently higher impedance, which must be managed through material and structural engineering [76] [75].
Quantitative Performance Comparison of Electrode Technologies
The following tables synthesize quantitative data from recent research, comparing the performance of various soft and flexible electrodes against standard Ag/AgCl electrodes.
Table 1: Comparative Performance Metrics of Flexible Electrodes vs. Ag/AgCl Standard
| Electrode Technology | Key Material/Feature | Reported SNR (dB) | Electrode-Skin Impedance | Reference Condition |
|---|---|---|---|---|
| Ag/AgCl (Standard) | Conductive gel | Baseline (Reference) | Low (Baseline) | Clinical gold standard [73] |
| Flexible Bioelectrode (FBE) | Moldable food-grade material | 33 dB | N/P | High-quality ECG with distinguishable QRS [74] |
| Flexible Non-contact Electrode | Capacitive coupling via FPCB | Correlation: 99.70% (rest) | N/P | High correlation to wet electrode at rest [77] |
| POLiTAG Electrode | PEDOT:PSS/PAMPS hydrogel | N/P | 20.7 kΩ·cm² | Lowest reported vs. literature & commercial gel [78] |
| CP Hydrogel Electrode | PEDOT:PSS-based polymer | SNR improved by ~2.1 dB | Reduced by nearly 10x | Improved SNR due to conformal contact [75] |
| Textile/MXene Electrode | Ti₃C₂Tₙ MXene/Gelatin non-woven | High (Qualitative) | Low | Stable ECG/EMG, high breathability [60] |
Table 2: Performance of Flexible Dry Electrodes from Material Study
| Electrode Material | Impedance Magnitude (at 10 Hz) | Normalized RMS Error (nRMSE) | Cosine Similarity (CS) | Key Finding |
|---|---|---|---|---|
| Ag/AgCl (Standard) | ~100 kΩ (Baseline) | Baseline | Baseline | Reference for comparison [73] |
| Silver-based Ink | ~10 MΩ | 0.11 | 0.99 | Signal comparable to Ag/AgCl [73] |
| Graphene-based | ~10 MΩ | 0.13 | 0.99 | Signal comparable to Ag/AgCl [73] |
| Carbon-based | ~100 MΩ | 0.16 | 0.98 | Higher impedance but good signal morphology [73] |
Note: nRMSE and CS are morphological comparison metrics against the Ag/AgCl reference signal. Lower nRMSE and higher CS (max 1.0) indicate better morphological fidelity.
Experimental Protocols for Performance Validation
Electrode-Skin Impedance Measurement
The standard method for measuring electrode-skin interface impedance is Impedance Spectroscopy.
- Equipment: Potentiostat or Impedance Analyzer.
- Electrode Configuration: A two-electrode configuration is typically used, where the working (W) and counter (C) probes carry the current, and the working sense (WS) and reference (R) probes measure the voltage drop [76].
- Setup: Two biopotential electrodes are positioned on the skin surface (e.g., the forearm) at a fixed inter-electrode distance (e.g., 4 cm). The skin should be cleansed with 70% isopropyl alcohol and allowed to dry before electrode placement [74] [76].
- Measurement Parameters: An AC excitation signal with a low voltage (e.g., 10 mV RMS) is applied to preserve linearity. A frequency sweep is performed from 0.1 Hz or 1 Hz up to 10 kHz or 100 kHz, with several measurement points per decade (e.g., 100 points/decade) [76] [73].
- Data Analysis: The impedance magnitude and phase angle are recorded across the frequency spectrum. Results are often plotted on a Bode plot (log |Z| vs. log f) or a Nyquist plot.
Signal-to-Noise Ratio (SNR) Measurement
SNR can be measured directly during in vivo biosignal acquisition.
- Equipment: Biosignal acquisition system (e.g., ECG or EEG amplifier) with a known, stable input source or a defined protocol for noise measurement.
- Direct Measurement (for defined signals): For a known periodic signal like an ECG, the SNR can be calculated by comparing the amplitude of the QRS complex (V_signal) to the root-mean-square (RMS) of the noise in a quiescent segment (e.g., the TP segment) [74]. The formula
20 × log₁₀ (V_QRS / V_noise_RMS)is applied. - Injected Signal Method (for electrode characterization): A clean sine wave of known amplitude (e.g., 100 mV, 200 mV peak-to-peak) is injected into the electrode-skin circuit via a signal generator. The output signal is measured. By subtracting the input signal from the output, the noise introduced by the electrode interface is isolated. The SNR is then calculated based on the power of the injected signal versus the power of this extracted noise [73].
In Vivo Biopotential Acquisition and Morphological Comparison
This protocol validates electrode performance under realistic conditions.
- Setup: A test electrode and a standard Ag/AgCl reference electrode are placed in close proximity on the subject's skin to acquire the same physiological signal (e.g., ECG) simultaneously [73].
- Data Acquisition: Signals are acquired synchronously for a set duration under various conditions (rest, walking, cycling).
- Signal Analysis:
- Normalized Root Mean Squared Error (nRMSE): Quantifies the absolute difference between the test and reference signals. A lower nRMSE indicates better fidelity.
- Cosine Similarity (CS): Measures the morphological similarity in the vector space. A value of 1.0 indicates identical morphology [73].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials and Reagents for Flexible Electrode R&D
| Category / Item | Example Specifics | Primary Function in R&D |
|---|---|---|
| Conductive Polymers | PEDOT:PSS (e.g., Clevios PH 1000) | Mixed ionic/electronic conductor; backbone for soft, conductive hydrogels and films [78] [9]. |
| Polymer Matrix/Additives | PAMPS Hydrogel, Triton X-100, Glycerol, LiCl | Provides ionic conductivity, softness, water-retention, and plasticization to enhance electrical and mechanical properties [78]. |
| 2D Conductive Materials | Ti₃C₂Tₓ MXene nanosheets | Provides high electrical conductivity in hydrophilic, solution-processable ink for fibers and coatings [60]. |
| Biopolymers | Gelatin | Forms thermoreversible, biocompatible, and biodegradable matrix for sustainable and recyclable electrodes [60]. |
| Substrate Materials | Polyimide (PI) film, Parylene-C, PDMS | Serves as flexible, stretchable, or ultra-thin support substrate for conductive layers [9] [79]. |
| Fabrication Equipment | Sputtering System, Laser Engraver, Wet Spinning Setup | Deposits thin metal layers (Cr/Au); patterns electrode geometries; fabricates continuous conductive fibers [79] [60]. |
| Characterization Instruments | Potentiostat, Biosignal Amplifier (e.g., ADS1299) | Measures impedance spectroscopy; acquires high-resolution electrophysiological data [77] [76]. |
The quantitative assessment of SNR and electrode-skin impedance is non-negotiable for progressing the field of soft and flexible bioelectronics. As the data demonstrates, innovative materials—from conductive polymer hydrogels like POLiTAG to MXene composites—are consistently achieving performance metrics that rival, and in some specific aspects such as stability or breathability, surpass the traditional Ag/AgCl standard. The future of this field lies in the continued refinement of these metrics through interdisciplinary material science, guided by standardized experimental protocols as outlined in this guide. The ultimate goal is the development of robust, comfortable, and clinically reliable wearable devices that enable seamless, long-term physiological monitoring.
The evolution of soft and flexible bioelectronics represents a paradigm shift in the development of medical devices, moving from rigid, monolithic systems to soft, conformable, and tissue-integrative interfaces. This transition is driven by the fundamental need to seamlessly merge electronic functionality with biological tissues, which are inherently soft, dynamic, and hydrated. The mechanical mismatch between conventional electronic materials (e.g., silicon, rigid metals) and soft tissues often leads to immune responses, signal instability, and device failure [9]. Consequently, material science has focused on developing a new class of electronic matter that is intrinsically soft, stretchable, and biocompatible.
This review provides a comparative analysis of four key material systems at the forefront of this revolution: traditional metals, hydrogels, liquid metals (LMs), and nanocomposites. Within the broader context of a thesis on soft bioelectronics, this guide delves beyond a simple catalog of properties. It offers a technical dissection of each system's underlying principles, provides detailed experimental protocols for their implementation, and presents quantitative data to guide material selection for specific applications, from wearable sensors and implantable devices to energy systems and neural interfaces.
Core Material Systems: Properties, Mechanisms, and Comparative Analysis
Metallic Materials: From Rigid Conductors to Geometrically Engineered Flexibility
Traditional metals like gold (Au), platinum (Pt), and silver (Ag) are the bedrock of electronics due to their exceptional electrical conductivity and well-established processing techniques. However, their intrinsic rigidity is a major limitation for biointerfacing.
- Mechanism and Material Forms: The primary strategy to impart flexibility and stretchability to metals involves structural engineering. This entails fabricating metals into specific geometries or dimensions that can accommodate strain without the material itself stretching.
- Serpentine Structures: In-plane, wavy patterns of thin metal films that unfurl under tensile stress [80].
- Buckling Structures: Out-of-plane wrinkles formed by bonding a thin metal film to a pre-stretched elastomeric substrate [80].
- Ultrathin Films: Reducing metal thickness to the sub-micrometer scale to minimize bending stiffness, enabling conformal contact on curved surfaces like skin [9].
- Applications: These strategies are widely used in flexible patch-type bioelectronics for electrophysiological monitoring (ECG, EEG, EMG) and in implantable arrays where high conductivity and signal fidelity are paramount [9].
Hydrogels: The Soft, Hydrated Matrix
Hydrogels are three-dimensional networks of hydrophilic polymers that can retain a large amount of water, giving them mechanical and chemical properties similar to biological tissues [81] [82].
- Mechanism and Material Forms: Their functionality stems from their hydrated, porous structure.
- Ionic Conductivity: The primary conduction mechanism in pure hydrogels, where ions in the absorbed aqueous solution facilitate charge transport.
- Stimulus-Responsiveness: They can swell, shrink, or change properties in response to environmental stimuli like pH, temperature, or specific biomarkers.
- Initiator Capability: Certain liquid metals can initiate the polymerization of hydrogel precursors, enabling novel synthesis routes [81].
- Applications: Hydrogels serve as the foundational soft matrix in composites, as injectable conductive interfaces for neural tissues, and as drug-eluting platforms in electrically stimulated therapy [83] [9].
Liquid Metals: Fluidic and Functional Conductors
Liquid metals (LMs), particularly gallium-based alloys like eutectic Gallium-Indium (EGaIn) and Gallium-Indium-Tin (Galinstan), are transformative materials that combine metallic conductivity with fluidic behavior [81] [84].
- Mechanism and Material Forms: Their key advantage is the ability to maintain conductive pathways under extreme deformation.
- Micro/Nano Droplets: LM can be probe-sonicated into droplets stabilized by surfactants, graphene, or silica, which are then dispersed into a hydrogel matrix as conductive fillers [81] [84].
- Continuous Pathways: LM can be injected into pre-formed microfluidic channels within hydrogels to create stable, stretchable wires [84].
- Applications: LM-hydrogel composites are ideal for highly stretchable sensors, soft actuators, electromagnetic interference (EMI) shielding, and energy harvesting devices due to their strain-insensitive conductivity and self-healing capabilities [81] [84].
Nanocomposites: Synergistic Material Engineering
Nanocomposites represent a synergistic approach, where nanoscale fillers are incorporated into a soft polymer or hydrogel matrix to create materials with enhanced or novel properties.
- Mechanism and Material Forms: The properties arise from the interaction between the nanofiller and the matrix.
- Conductive Networks: Fillers like carbon nanotubes (CNTs), graphene, or MXene form a percolating network for electron transport through the insulating matrix [82].
- Colloidal Crosslinkers: Nanoparticles can act as additional crosslinking sites within a hydrogel, simultaneously enhancing mechanical strength and conductivity [84] [82].
- Applications: This is a highly versatile class used in electronic skins (e-skins), human-machine interfaces (HMI), virtual reality (VR) sensors, and multifunctional wearable platforms [82].
Table 1: Quantitative Comparison of Key Material Properties in Bioelectronics
| Material System | Electrical Conductivity | Typical Elastic Modulus | Stretchability (%) | Key Functional Properties |
|---|---|---|---|---|
| Metals (Au, Pt thin films) | ~10⁶ S/cm [81] | GPa range (intrinsic) | <5% (intrinsic), up to 350% with serpentine designs [80] | High conductivity, established fabrication, excellent signal fidelity. |
| Hydrogels (Ionic) | ~0.1 - 10 S/cm (ionic) [32] | kPa - MPa range [32] [9] | Can exceed 1000% [32] | Tissue-like softness, biocompatibility, stimulus-responsiveness, drug delivery. |
| Liquid Metals (EGaIn) | 3.1 - 3.4 × 10⁶ S/cm [81] | Liquid (no modulus) | Effectively infinite (fluid) [81] [84] | Fluidic conductivity, self-healing, low toxicity, initiator for polymerization. |
| Nanocomposites (CNT-hydrogel) | Up to 100+ S/cm (electronic) [85] [82] | kPa - MPa range (tunable) | Can exceed 500% [82] | Tunable properties, multifunctionality (sensing, conduction, strength). |
Table 2: Application-Based Performance Metrics
| Application | Key Performance Metrics | Exemplary Material System & Performance |
|---|---|---|
| Wearable Electrophysiology | Signal-to-Noise Ratio (SNR), Motion Artifact Suppression | Multilayer hydrogel with MXene coating: SNR of 37 dB, 40% better motion artifact suppression than conventional electrodes [32]. |
| Implantable Neural Interface | Foreign Body Response (FBR), Long-term Stability | Soft bioadhesive interface: Reduced fibrous capsule thickness to 28.6 μm (vs. 85.2 μm for Pt), stable signal acquisition for 30 days [32]. |
| Stretchable Conductor | Conductivity Retention under Strain | LM-hydrogel composite: Conductivity of 1.2 S/cm maintained under 100% tensile strain [32]. Vertical serpentine metal: <2% resistance change under 300% strain [80]. |
| Soft Sensing & HMI | Sensitivity, Cyclic Durability | Nanocomposite hydrogel sensor: Withstood 10,000 mechanical cycles with only 8.7% impedance increase [32]. |
Experimental Protocols: A Guide to Key Methodologies
Protocol: Fabrication of LM-Hydrogel Composites via Direct Dispersion
This protocol details the creation of a conductive, stretchable composite by dispersing LM droplets within a hydrogel matrix [81] [84].
LM Droplet Synthesis (Probe Sonication):
- Materials: Eutectic Gallium-Indium (EGaIn), deionized water, vinyl monomer (e.g., acrylic acid), and optionally, a stabilizer like silica nanoparticles or a surfactant.
- Procedure: Combine EGaIn and the aqueous solution (with monomers/stabilizer) in a vial. Immerse a probe sonicator and sonicate on ice bath for 10-30 minutes at high power (e.g., 400-600 W) to form a homogeneous, grayish suspension of LM micro/nano droplets.
Hydrogel Matrix Formation:
- Materials: Hydrogel precursors (e.g., acrylamide, alginate), crosslinkers (e.g., MBAA, CaCl₂), and initiators (e.g., APS/TEMED). Note: The LM droplets themselves can act as initiators [81].
- Procedure: Mix the LM droplet suspension with the hydrogel precursors and crosslinkers. Pour the mixture into a mold and initiate polymerization via heating (e.g., 70°C for 3 hours) or UV light, depending on the initiator system. For double-network hydrogels (e.g., PAA-alginate), a secondary ionic crosslinking step in a CaCl₂ bath may follow [84].
Characterization:
- Electrical: Measure conductivity via 4-point probe, tracking resistance change under uniaxial stretching.
- Mechanical: Perform tensile tests to determine fracture strain, toughness, and elastic modulus.
- Morphological: Use scanning electron microscopy (SEM) to confirm uniform dispersion of LM droplets and assess the composite microstructure.
Protocol: Solvent-Exchange Synthesis of Intrinsic Hydrogel Semiconductors
This breakthrough protocol describes creating a single material that is both a semiconductor and a hydrogel, overcoming the classic incompatibility between the two [6].
Solution Preparation:
- Materials: A conjugated polymer semiconductor (e.g., a specific p-type semiconductor), an organic solvent miscible with water (e.g., DMSO, THF), and hydrogel precursors (e.g., PVA, a photoinitiator).
- Procedure: First, dissolve the polymer semiconductor in the organic solvent to create a concentrated stock solution. Separately, prepare the aqueous solution of hydrogel precursors.
Solvent Exchange and Gelation:
- Procedure: Slowly add the polymer semiconductor solution to the aqueous precursor solution under vigorous stirring to form a homogeneous mixture. The solvent exchange process allows the hydrophobic semiconductor to be integrated into the aqueous gel network without precipitating.
- Gelation: Cast the final mixture and induce gelation, typically via UV light exposure, to form the solid hydrogel semiconductor film.
Characterization:
- Semiconducting Properties: Fabricate OECTs or OFETs to measure transconductance, carrier mobility, and switching speed.
- Hydrogel Properties: Measure water content, swelling ratio, and elastic modulus.
- Biointerfacial Function: Test biosensing response sensitivity to biomarkers and photo-modulation efficiency for therapies like light-operated pacemakers [6].
Protocol: AI-Guided High-Throughput Doping of Conjugated Polymers
This modern protocol uses AI to efficiently optimize the electronic properties of polymers for bioelectronics [85].
Setup of DopeBot System:
- Materials: Conjugated polymer (e.g., pBTTT), dopant (e.g., F4TCNQ), a library of organic solvents.
- Procedure: An AI algorithm (e.g., Bayesian optimization) is tasked with maximizing the conductivity of the doped polymer. The system defines a multi-dimensional parameter space including solvent type, doping concentration, and processing temperature.
Iterative Experimentation:
- Procedure: The DopeBot system designs a batch of experiments (e.g., 32 conditions). The experiments are conducted by preparing doped polymer films according to the specified parameters.
- Characterization: Each sample is automatically characterized for conductivity, UV-Vis absorption (to study polaron formation), and structural order (via GIWAXS). This data is fed back to the AI.
- Loop: The AI uses the results to design the next, more optimal batch of experiments. This loop continues for several iterations.
Analysis and Validation:
- Procedure: Advanced analytics identify correlations between processing parameters, polymer structure (e.g., lamellar stacking), and electronic performance. Quantum chemical calculations are used to move from correlation to causation, revealing, for instance, that high conductivity requires ordered polymer domains with dopants located at a specific "peripheral" distance (≈1.3–1.8 nm) [85].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Their Functions in Soft Bioelectronics
| Reagent/Material | Function in Research | Exemplary Use Case |
|---|---|---|
| Eutectic Gallium-Indium (EGaIn) | A liquid metal with high conductivity and fluidity, used as a conductive filler or polymerization initiator. | Dispersed in hydrogels to create stretchable conductive composites for sensors [81] [84]. |
| Poly(3,4-ethylenedioxythiophene):Poly(styrene sulfonate) (PEDOT:PSS) | A conductive polymer, cornerstone for organic electrochemical transistors (OECTs) and conductive coatings. | Used as the active channel in ultrathin, flexible OECTs for amplifying bioelectrical signals like ECG [9]. |
| Carbon Nanotubes (CNTs) | A carbon nanomaterial providing mechanical strength and electronic conductivity to composites. | Incorporated into hydrogels as nanofillers to form conductive networks for e-skin and HMI sensors [82]. |
| F4TCNQ Dopant | A molecular p-type dopant used to tune the electronic properties of conjugated polymers. | Employed in AI-guided high-throughput screening to optimize the conductivity of pBTTT polymer [85]. |
| Dynamic Crosslinkers (e.g., Borate Esters) | Provide reversible crosslinking in hydrogels, enabling self-healing and high toughness. | Used in conductive hydrogels to achieve 90% conductivity recovery within 48 hours post-mechanical damage [32]. |
| MXene Nanosheets | Two-dimensional conductive transition metal carbides/nitrides for enhanced conductivity and functionality. | Formulated into anti-inflammatory coatings and conductive networks within hydrogels for neural interfaces [32]. |
Visualization of Workflows and Material Integration
The following diagrams illustrate key experimental workflows and the functional integration of different material systems in a composite.
Diagram 1: Fabrication of an LM-hydrogel composite via the direct dispersion method, involving sonication and in-situ polymerization.
Diagram 2: The synergistic integration of different material components within an advanced bioelectronic nanocomposite, showing the role of each element.
The comparative analysis presented herein underscores that there is no single "best" material for soft bioelectronics. Instead, the optimal choice is dictated by the specific application requirements, necessitating strategic trade-offs between conductivity, mechanical properties, biocompatibility, and functionality. The future of the field lies in the intelligent integration of these material systems, as exemplified by LM-hydrogel composites and multifunctional nanocomposites.
Emerging trends point toward several exciting frontiers. First, the use of AI and high-throughput experimentation, as demonstrated with polymer doping, will dramatically accelerate the discovery and optimization of next-generation materials [85]. Second, the development of materials with augmented biointeractive functions, such as hydrogel semiconductors [6] and self-healing bioadhesive interfaces [32], will enable more sophisticated closed-loop diagnostic-therapeutic systems. Finally, addressing challenges related to long-term stability in biofluids, scalable manufacturing of complex devices, and ensuring true biodegradability for transient electronics will be critical for the widespread clinical adoption of these transformative technologies. The journey from rigid implants to soft, tissue-integrated bioelectronics is well underway, powered by continuous innovation in material systems.
The development of soft and flexible bioelectronics represents a paradigm shift in medical technology, enabling seamless integration with biological tissues for advanced diagnostic and therapeutic applications. These devices, composed of materials with tissue-like mechanical properties, are designed to minimize foreign body response (FBR) and maintain long-term functionality. However, their path to clinical adoption requires rigorous validation frameworks that systematically assess performance from controlled laboratory settings to complex living systems. This whitepaper provides a comprehensive technical guide to validation methodologies for bioelectronic systems, with specific focus on diabetic and neurological applications. We examine key material characterization techniques, in-vitro modeling approaches, and in-vivo demonstration protocols that collectively establish safety, efficacy, and reliability for these emerging technologies.
The validation pipeline for soft bioelectronics must address unique challenges posed by their material composition and operating environments. Unlike conventional rigid implants, soft bioelectronic systems exhibit mechanical properties (Young's modulus in the kPa to MPa range) that closely match biological tissues (typically 0.5-100 kPa), significantly reducing mechanical mismatch at the biotic-abiotic interface [7] [2]. This compliance enables conformal contact with dynamic tissues but introduces new validation challenges related to long-term stability under mechanical stress, electrical performance in hydrated environments, and biological integration. This technical guide establishes a structured framework for researchers developing next-generation bioelectronic technologies for diabetes management and neurological disorders.
Material Foundations for Soft Bioelectronics
Key Material Classes and Properties
Soft bioelectronics leverage emerging material platforms that enable stable interfaces with biological tissues while maintaining electronic functionality. These materials must satisfy multiple requirements including mechanical compliance, electrical conductivity, biocompatibility, and often biodegradability or long-term stability.
Table 1: Key Material Classes for Soft Bioelectronics
| Material Class | Representative Examples | Key Properties | Applications |
|---|---|---|---|
| Conductive Polymers | PEDOT, PPy, PNAi | Conductivity (10⁻¹-10³ S/cm), Moderate stretchability | Neural electrodes, Biosensors |
| Hydrogel-Based Composites | PANI-based hydrogels, Semi-dry hydrogels | Tissue-like modulus (0.5-500 kPa), Ionic conductivity | Chronic implants, Drug-eluting electrodes |
| Conductive Nanocomposites | Graphene, MXenes, CNTs | High conductivity (10³-10⁵ S/cm), Tunable mechanical properties | High-density arrays, Flexible circuits |
| Soft Encapsulation Materials | PDMS, Ecoflex, Parylene C | Low water permeability, Flexibility | Chronic implantation, Insulation layers |
| Biodegradable Substrates | PCL, PLGA, PGA | Programmable degradation rates | Transient implants, Temporary monitors |
These material systems form the foundation for bioelectronic devices with engineered mechanical properties. For instance, recent advances have produced conductive hydrogels with Young's moduli as low as 3-5 kPa, closely matching neural tissue (1-5 kPa) and enabling minimally disruptive interfaces [7]. Similarly, silicon-based thin-film membranes with structural dimensions at the nanometer scale provide flexibility while maintaining semiconductor performance [7]. The validation of these materials requires specialized protocols that assess both electronic and biological performance under physiologically relevant conditions.
Research Reagent Solutions
Table 2: Essential Research Reagents for Bioelectronics Validation
| Reagent/Category | Function/Purpose | Application Context |
|---|---|---|
| Self-Confined Tetrahedral DNA (SCTD) Circuit | Signal amplification for low-abundance biomarkers; provides mechanical stability and anti-fouling properties | Wearable wound biosensors for diabetic patients [48] |
| SMOTE (Synthetic Minority Oversampling Technique) | Computational resampling to address class imbalance in medical datasets | Diabetes prediction models from imbalanced clinical data [86] |
| SHAP (SHapley Additive exPlanations) | Model interpretability framework for explaining feature contributions in ML predictions | Explainable AI for diabetes risk assessment [86] |
| Electrospun PAN/TPU Nanofibers | Breathable, flexible substrate with programmable hydrophilic/hydrophobic patterning | Wearable wound monitoring patches [48] |
| Neuropixels Probes | High-density neural recording (960-5120 electrodes) with single-spike resolution | Large-scale neural recording in animal models and organoids [87] |
| Retinoic Acid (RA) & FGF Signaling Molecules | Patterning cues for regional specification in neural organoid differentiation | Spinal cord organoid development [87] |
| PEDOT:PSS Conductive Polymer | Low-impedance neural interface material with mechanical flexibility | Neural recording and stimulation electrodes [7] |
Validation Frameworks for Diabetic Models
In-Vitro Analytical Validation
The validation pipeline for diabetes-focused bioelectronics begins with rigorous in-vitro characterization of sensing modalities, particularly for non-invasive glucose monitoring technologies. Analytical validation must address the unique challenges of biological media, where multiple interferents can compromise specificity.
Recent research on non-invasive glucose measurement has highlighted the limitations of directly applying the Lambert-Beer Law to complex biological samples like blood due to non-linear behavior in organic solutions [88]. A validated methodology for determining the extinction coefficient of glucose in blood requires spectrophotometric analysis across the 700-1400 nm range, with optimal sensitivity observed at approximately 975 nm [88]. The experimental protocol involves:
Sample Preparation: Whole blood and plasma samples from multiple donors with varying glucose and insulin concentrations measured using gold-standard methodologies.
Instrumentation Setup: Spectrophotometer with tungsten lamp source for infrared and visible regions, quartz cuvettes with rectangular geometry and polished faces to minimize refraction errors.
Extinction Coefficient Calculation: Iterative optimization process to determine glucose extinction coefficients (αg), ranging from -0.0045 to -0.0053, and insulin coefficients (αi), ranging from 0.000075 to 0.000078, with inter-individual variations assessed for stability.
Model Validation: Development of regression models that differentiate glucose from insulin concentration by considering cuvette thickness and sample absorbance at 965, 975, and 985 nm.
For electrochemical sensors, validation includes assessment of linearity (typically 1-30 mM glucose range), sensitivity (μA/mM/cm²), response time (<60 seconds), and selectivity against interferents like acetaminophen, uric acid, and ascorbic acid through methods such as addition-recovery experiments.
In-Vivo Demonstration in Diabetic Models
Transitioning from in-vitro validation to in-vivo demonstration requires careful consideration of biological variables including skin heterogeneity, blood flow dynamics, and metabolic processes. Recent advances in soft bioelectronics have enabled novel form factors for in-vivo validation in diabetic models.
A notable example is the development of soft, breathable bioelectronics embedded with Self-Confined Tetrahedral DNA (SCTD) circuits for chronic wound monitoring in diabetic mice [48]. The validation framework for this technology includes:
Device Fabrication: Creation of breathable sensing patches using electrospun polyacrylonitrile/thermoplastic polyurethane (PAN/TPU) nanofibers with defined hydrophilic biosensing areas that serve as reaction pools while preventing reagent diffusion.
Biomarker Panel Selection: Simultaneous monitoring of multiple wound healing-related proteins (TNF-α, IL-6, TGF-β1, and VEGF) and biophysical parameters to comprehensively assess diabetic wound status.
In-Vivo Testing: Implementation on diabetic male mice with both non-infected and infected wounds, demonstrating accurate in-situ monitoring without hindering the healing process.
Performance Metrics: Evaluation of mechanical stability (<3% variation after 1000 bending cycles), prolonged stability (<8% signal attenuation over 4 weeks), and reduced biofouling (>50% BSA adhesion reduction).
For glucose monitoring specifically, in-vivo validation requires correlation with blood glucose reference measurements (typically via venous blood or implanted microdialysis), with statistical analysis including Mean Absolute Relative Difference (MARD) <15%, Clarke Error Grid analysis (>99% in zones A+B), and consistency during glycemic excursions.
Validation Frameworks for Neurological Models
In-Vitro Validation Using Neural Organoids
Neural organoids have emerged as powerful in-vitro models that partially recapitulate the structural and functional complexity of the human nervous system, providing a biologically relevant platform for validating neuromodulation technologies [87]. These 3D constructs, derived from pluripotent stem cells (iPSCs) or embryonic stem cells (ESCs), offer several advantages over traditional 2D cultures, including improved cellular communication and more physiologically relevant microenvironments.
The validation workflow for brain-targeted bioelectronics using neural organoids includes:
Organoid Generation: Employing either unguided methods (relying on self-assembly and intrinsic differentiation capacities) or guided approaches (using specific exogenous components to constrain self-patterning and generate region-specific organoids).
Functional Maturation Assessment: Confirming the development of key neural features including ventricular zone formation, spontaneous electrical activity, and network synchronization through calcium imaging and electrophysiological recording.
Device-Organoid Integration: Implementing 3D bioelectronic interfaces that accommodate organoid architecture without disrupting internal organization, enabling long-term functional monitoring.
Multimodal Characterization: Combining electrophysiological recording with molecular analysis to comprehensively assess neural network development and function.
Advanced bioelectronic interfaces for organoids include high-density multi-electrode arrays (HD-MEAs) with up to 4,096 platinum-black electrodes integrated into CMOS chips, enabling simultaneous recording from thousands of neurons and mapping of synaptic connections [87]. These platforms have demonstrated capability to capture over 70,000 synaptic connections among approximately 2,000 neurons, classifying synaptic types and enabling re-accessing of the same neuron over time.
In-Vivo Validation of Neural Interfaces
In-vivo validation of neural interfaces requires demonstration of stable long-term performance in biologically active environments. Conventional rigid implants often trigger chronic inflammation, glial scarring, and signal degradation, highlighting the need for soft bioelectronic solutions [89] [7].
The validation framework for implantable neural interfaces includes:
Biocompatibility Assessment: Evaluation of foreign body response through histological analysis of implantation sites, quantification of glial fibrillary acidic protein (GFAP) expression for astrocyte activation, and assessment of neuronal loss around implant sites.
Electrophysiological Performance: Measurement of signal-to-noise ratio (SNR), spike sorting accuracy, and recording stability over extended periods (weeks to months), with comparison to established standards like Utah arrays and Michigan probes.
Mechanical Integration Analysis: Assessment of device-tissue integration through immunohistochemistry and analysis of micromotion-induced tissue damage.
Functional Efficacy Testing: Demonstration of therapeutic benefit in disease models, such as vagus nerve stimulation for inflammatory conditions [90] or cortical interfaces for motor restoration.
Recent advances include Neuropixels probes, which integrate 960-1,280 densely packed electrodes along silicon shanks, enabling simultaneous tracking of neuronal activity across multiple brain regions with single-spike resolution [87]. These high-density platforms have been validated in freely behaving small animals, maintaining stable performance during chronic implantation.
For peripheral nerve interfaces, validation includes assessment of stimulation selectivity using multiple contact cuff electrodes (MCEs) and computational models based on 3D anatomies of reconstructed nerves to optimize stimulation paradigms [90]. These models can be combined with physiological data from in vivo experiments to estimate unknown nerve anatomy and optimize stimulation protocols before extensive animal testing.
Integrated Validation Frameworks and Clinical Translation
Cross-Platform Validation Metrics
Establishing standardized metrics for soft bioelectronics performance enables meaningful comparison across platforms and accelerates clinical translation. Key validation parameters span multiple domains:
Table 3: Cross-Platform Validation Metrics for Soft Bioelectronics
| Performance Category | Key Metrics | Target Values | Assessment Methods |
|---|---|---|---|
| Mechanical Compliance | Young's modulus, Stretchability, Bend radius | 0.5-500 kPa (matching target tissue), >20% strain | Tensile testing, Cyclic deformation |
| Electrical Performance | Impedance at 1 kHz, Charge injection capacity, Signal-to-noise ratio | <100 kΩ, >1 mC/cm², >10 dB for neural recording | Electrochemical impedance spectroscopy, Cyclic voltammetry |
| Biological Safety | Cytotoxicity (ISO 10993-5), Hemocompatibility, Foreign body response | >70% cell viability, Minimal inflammation | In-vitro toxicity assays, Histology post-explantation |
| Functional Stability | Performance retention, Baseline drift, Biofouling resistance | <5% signal attenuation after 30 days, <50% protein adhesion | Accelerated aging, In-vivo long-term studies |
| Clinical Correlation | Sensitivity, Specificity, Accuracy | >90% for diagnostic devices | Comparison to gold-standard measurements |
Pathway to Clinical Deployment
The transition from laboratory validation to clinical implementation requires additional rigorous assessment frameworks. A notable example comes from diabetes prediction models, where despite achieving high cross-validated performance (Random Forest with SMOTE: 96.91% accuracy, AUC of 0.998), researchers emphasize that such results should be regarded as methodological proof-of-concept rather than clinically generalizable evaluation [86]. The recommended pathway includes:
Methodological Proof-of-Concept: Initial development and validation on curated datasets, with careful attention to prevent data leakage (e.g., applying SMOTE exclusively within training folds) [86].
External Validation: Testing on independent populations with different demographic characteristics and disease prevalence.
Clinical Plausibility Assessment: Structured review of model explanations (e.g., SHAP outputs) by domain experts to assess biological plausibility and guideline consistency [86].
Prospective Clinical Trials: Evaluation in real-world clinical settings with predefined endpoints relevant to clinical decision-making.
For bioelectronic medicines, recent clinical examples include baroreflex activation therapy (BAT) for heart failure with reduced ejection fraction (HFrEF), which demonstrated significant reduction in inflammatory biomarkers (TNF-α and IFN-γ) and 94% decrease in heart failure hospitalizations in clinical studies [90]. Similarly, transcutaneous auricular vagus nerve stimulation (taVNS) has shown promise in pediatric Crohn's disease when combined with biologics, with reported mucosal healing and normalized fecal calprotectin levels [90].
Validation frameworks for soft bioelectronics must evolve to address the unique characteristics of these technologies while maintaining scientific rigor. The integration of advanced in-vitro models (including neural organoids and tissue-mimicking substrates) with robust in-vivo assessment creates a comprehensive pathway from concept to clinical application. For both diabetic and neurological applications, multidisciplinary approaches that combine materials science, electrical engineering, biology, and clinical medicine are essential to establish safety and efficacy. As the field advances, standardized validation protocols and reporting standards will accelerate the translation of soft bioelectronics from research laboratories to clinical practice, ultimately enabling new diagnostic and therapeutic options for patients with diabetes, neurological disorders, and other chronic conditions.
Soft and flexible bioelectronics represents a paradigm shift in medical devices, offering the potential for seamless integration with the human body for diagnostic, therapeutic, and monitoring applications. Unlike traditional rigid electronics, these devices leverage advanced materials and structural designs to achieve tissue-like mechanical properties, enabling conformal contact with biological tissues and minimizing adverse immune responses [57] [91]. The field has evolved significantly from early implantable devices like pacemakers and cochlear implants to sophisticated systems capable of closed-loop operation, where sensing and stimulation are dynamically coordinated [57]. This progression toward soft, conformable interfaces is driven by the fundamental recognition that the human body is composed of soft, dynamic, and continuously moving tissues, making mechanical compatibility a critical requirement for long-term device functionality [57] [7].
Despite remarkable advances in materials science and device engineering, the path to widespread clinical adoption and commercialization remains fraught with technical and regulatory challenges. The mechanical mismatch between conventional electronic materials and biological tissues can lead to inflammation, fibrosis, and eventual device failure [7]. Furthermore, issues related to long-term stability in hydrated physiological environments, efficient power management, and scalable manufacturing processes continue to impede translation from laboratory demonstrations to clinically viable products [57] [92]. This whitepaper assesses the current state of soft bioelectronics, identifies persistent barriers to clinical implementation, and outlines the multidisciplinary strategies required to bridge the gap between promising research and widespread commercialization for researchers, scientists, and drug development professionals invested in this rapidly evolving field.
Technical Hurdles in Clinical Translation
Material-Tissue Interface Challenges
The interface between bioelectronic devices and biological tissues presents one of the most significant challenges for long-term stability and functionality. The foreign body response (FBR) constitutes a primary failure mechanism, where the immune system recognizes the implant as a foreign entity, triggering a cascade of events including protein adsorption, inflammatory cell recruitment, and ultimately fibroblast encapsulation that can electrically isolate the device from its target tissue [7] [32]. This process is significantly exacerbated by mechanical mismatch, where conventional electronic materials like silicon and metals have Young's moduli in the gigapascal range, while biological tissues such as brain and myocardial tissue typically exhibit moduli in the kilopascal range [7]. This several-orders-of-magnitude difference in stiffness creates micromotion-induced damage and chronic inflammation that compromises both device function and tissue health.
Beyond mechanical mismatch, chemical mismatches at the biointerface further complicate long-term stability. Many high-performance electronic materials lack the necessary hydrophilicity or biochemical compatibility to integrate seamlessly with biological systems. Conventional encapsulation materials often fail to prevent water and ion permeation over extended implantation periods, leading to device corrosion and failure [57] [7]. The resulting signal drift, increased impedance, and reduced charge injection capacity diminish the therapeutic efficacy of stimulation devices and the accuracy of recording devices. These challenges are particularly pronounced in chronic implantation scenarios, where devices must remain functional for years or decades despite the aggressive physiological environment.
Power and Data Transmission Limitations
Sustainable power delivery and efficient data transmission represent additional critical hurdles for implantable soft bioelectronics. Traditional batteries possess limited lifespan, contain potentially toxic materials, and add undesirable rigidity and bulk to otherwise flexible systems. While wireless power transfer (WPT) systems offer a promising alternative, their efficiency within the human body remains suboptimal, with challenges in energy transfer depth, alignment sensitivity, and thermal effects [93]. Recent research has explored metamaterials to enhance WPT efficiency for implantable medical devices, but these approaches have yet to achieve widespread clinical implementation [93].
Similarly, data transmission from deep-tissue implants faces significant obstacles. The body's conductive tissues attenuate radio frequency signals, necessitating higher power consumption for reliable wireless communication, which in turn generates more heat and shortens battery life. Multiplexed signal acquisition and local signal processing have emerged as strategies to reduce data transmission loads by preprocessing information before transmission [93]. However, implementing complex signal processing in ultra-thin, flexible formats with minimal power consumption remains technically challenging. These power and data constraints fundamentally limit the functionality, miniaturization, and longevity of fully implantable soft bioelectronic systems.
Table 1: Key Technical Barriers to Clinical Adoption of Soft Bioelectronics
| Challenge Category | Specific Technical Barriers | Impact on Clinical Translation |
|---|---|---|
| Material-Tissue Interface | Foreign body response (FBR), Mechanical mismatch, Water/ion permeation | Reduced device longevity, Signal instability, Tissue inflammation and damage |
| Power Management | Limited battery life, Inefficient wireless power transfer, Thermal effects | Frequent replacement surgeries, Limited device functionality, Safety concerns |
| Data Transmission | Signal attenuation in tissue, High power requirements for wireless communication | Reduced sampling rates, Limited channel counts in neural interfaces, Shorter operational lifespan |
| Manufacturing & Scalability | Complex fabrication processes, Limited yield of stretchable components, Integration challenges | High production costs, Difficulty in mass production, Variable device performance |
| Long-Term Stability | Material degradation in biofluids, Mechanical fatigue at interconnects, Delamination of layers | Uncertain device reliability, Safety concerns for chronic implantation, Limited clinical adoption |
Signal Fidelity and Stability in Dynamic Environments
Maintaining high signal-to-noise ratio (SNR) in dynamically moving biological environments presents a persistent challenge for soft bioelectronics. While rigid devices maintain stable electrical properties, the continuous deformation of stretchable conductors and semiconductors can introduce electrical noise, impedance variations, and signal drift [57]. For diagnostic and closed-loop therapeutic applications, these instabilities can compromise treatment efficacy and safety. In electrophysiological recording, motion artifacts often overwhelm biologically relevant signals, necessitating advanced signal processing algorithms and stable mechanical interfaces.
Validation through rat cortical implantation experiments has demonstrated the potential of advanced materials, with one study reporting stable electrophysiological signal acquisition over 30 days with a signal-to-noise ratio (SNR) of 37 dB compared to 15 dB for conventional Pt electrodes [32]. However, maintaining this performance over longer periods (years) required for many clinical applications remains unproven. Additionally, the trade-offs between mechanical compliance and electrical performance continue to challenge researchers, as increasing stretchability often comes at the cost of reduced conductivity or charge carrier mobility [91].
Emerging Materials and Design Strategies
Advanced Material Platforms
The development of intrinsically soft electronic materials represents a cornerstone strategy for enhancing tissue-device integration. Hydrogels have emerged as particularly promising platforms due to their high water content, tunable mechanical properties, and compatibility with biological tissues. A breakthrough from the University of Chicago demonstrated a hydrogel semiconductor that combines the electronic properties of traditional semiconductors with the tissue-like mechanical properties of hydrogels [6]. This material, created through a novel solvent exchange process rather than conventional water-based synthesis, achieves both semiconducting functionality and hydrogel design in a single integrated material, enabling improved biosensing response and stronger photo-modulation effects [6].
Conductive polymers such as PEDOT:PSS and polypyrrole have gained significant attention for their ability to combine electronic functionality with mechanical flexibility and biocompatibility [7] [9]. When processed with appropriate additives or in composite formations, these materials can achieve conductivities suitable for many bioelectronic applications while maintaining stretchability. Similarly, carbon-based materials including graphene, carbon nanotubes (CNTs), and MXenes offer attractive electrical, mechanical, and chemical properties for flexible electronics [7] [51]. These materials can be formulated into inks for printing processes or integrated into composite materials to create conductive pathways that remain functional under strain.
Table 2: Emerging Material Classes for Soft Bioelectronics
| Material Class | Key Representatives | Typical Properties | Advantages | Limitations |
|---|---|---|---|---|
| Conductive Hydrogels | Polyurethane-based catechol-functionalized elastomers, Borate ester-crosslinked hydrogels | Modulus <1 kPa, Conductivity ~1.2 S/cm, Self-healing | Tissue-like modulus, High water content, Enhanced biointegration | Conductivity decay in biofluids (e.g., 23% after 28 days) |
| Intrinsically Stretchable Conductors | Liquid metals (e.g., Gallium alloys), Conductive polymer composites | Stretchability >100%, Self-healing ability, High conductivity | Maintain conductivity under strain, Patternable, Durability | Potential toxicity concerns, Complex processing |
| Conductive Polymers | PEDOT:PSS, Polypyrrole, Polyaniline | Moderate conductivity (10-1000 S/cm), Tunable mechanical properties | Biocompatibility, Mixed ionic-electronic conduction, Solution processability | Batch-to-batch variability, Long-term stability concerns |
| Carbon Nanomaterials | Graphene, MXenes, Carbon nanotubes | High conductivity, Mechanical strength, Large surface area | Excellent electrical properties, Chemical stability, Transparency | Potential persistence in tissue, Dispersion challenges |
Structural Engineering Approaches
Beyond intrinsically soft materials, structural design innovations provide alternative pathways to achieving mechanical compatibility with biological tissues. Geometrical designs such as serpentine interconnects, island-bridge structures, and kirigami/origami-inspired patterns enable conventional electronic materials to become stretchable by distributing strain in ways that prevent material failure [91] [51]. These approaches leverage well-established semiconductor materials while achieving mechanical performance compatible with dynamic biological environments.
Ultra-thin device geometries represent another powerful structural approach to enhancing conformality. By reducing device thickness to the micrometer or sub-micrometer range, bending stiffness decreases dramatically, allowing devices to conform to tissue surfaces through van der Waals forces alone without external fixation [9]. This approach has been successfully demonstrated in epidermal electronic systems and neural interfaces, where sub-micrometer thickness enables conformal contact with minimal inflammatory response [9]. However, ultra-thin devices present handling challenges during implantation and may exhibit reduced durability under cyclic loading conditions.
Bioactive and Self-Healing Materials
Recent advances in bioactive interfaces focus on modulating the biological response to implanted devices rather than merely minimizing it. Materials featuring anti-inflammatory coatings, such as MXene-silk fibroin composites, can actively suppress immune responses through reactive oxygen species (ROS) scavenging and modulation of macrophage polarization [32]. These approaches recognize that the tissue-device interface is a dynamic biological environment that can be actively managed rather than simply tolerated.
Self-healing materials represent another frontier in enhancing the longevity and reliability of soft bioelectronics. These systems can autonomously repair mechanical damage and restore electrical functionality after failure [32] [51]. One demonstrated system integrated a mussel-inspired catechol-functionalized polyurethane elastomer substrate with conductive hydrogels crosslinked by dynamic borate ester bonds, achieving restoration of 90% conductivity within 48 hours post-mechanical damage [32]. Such capabilities are particularly valuable in applications experiencing repetitive mechanical stress, such as wearable sensors or implants in moving tissues.
Experimental Assessment Methodologies
In Vitro Characterization Protocols
Comprehensive material characterization forms the foundation for assessing potential bioelectronic materials. Standardized protocols for evaluating electrical, mechanical, and biological properties enable meaningful comparison between different material systems. Electrical characterization should include impedance spectroscopy (typically from 1 Hz to 1 MHz), current-voltage measurements, and stability tests under cyclic mechanical strain. For semiconductors, charge carrier mobility and transconductance measurements provide critical performance parameters [9].
Mechanical testing must encompass tensile tests to determine Young's modulus, elongation at break, and cyclic fatigue resistance under conditions mimicking the intended implantation environment. The use of phosphate-buffered saline (PBS) or other physiologically relevant solutions at body temperature (37°C) during mechanical testing provides more clinically relevant data than ambient conditions. Accelerated aging studies through elevated temperature or mechanical cycling can provide preliminary insights into long-term stability, though their predictive value for actual implantation performance remains limited.
Table 3: Standard Experimental Parameters for Material Validation
| Test Category | Key Parameters | Standard Protocols | Target Values for Clinical Use |
|---|---|---|---|
| Electrical Characterization | Impedance (1kHz), Charge injection capacity, Conductivity/resistivity, Operational stability | Cyclic voltammetry, Electrochemical impedance spectroscopy, 4-point probe measurements | Impedance <10 kΩ at 1kHz, Charge injection >1 mC/cm², Stable operation >10^6 cycles |
| Mechanical Testing | Young's modulus, Fracture strain, Toughness, Fatigue resistance (cycles to failure) | Tensile testing, Cyclic strain tests, Nanoindentation | Modulus matching target tissue (0.1-100 kPa), Strain >20%, Fatigue resistance >10^5 cycles |
| Biocompatibility Assessment | Cytotoxicity (ISO 10993-5), Cell adhesion/proliferation, Hemocompatibility | ISO 10993 series, Live/dead assay, MTT assay, Hemolysis assay | >90% cell viability, No significant hemolysis, Confluent cell layers |
| Barrier Properties | Water vapor transmission rate, Electrolyte permeability, Adhesion to substrates | Calcium test, Permeability cells, Peel tests | WVTR <10^-4 g/m²/day, Stable adhesion >1 J/m² |
In Vivo Validation Models
Animal models remain essential for evaluating the performance and safety of soft bioelectronic devices in physiologically relevant environments. Rodent models provide accessible platforms for initial proof-of-concept studies, particularly for neural interfaces where cortical implantation can assess both electrophysiological recording quality and tissue response [32]. Larger animal models, including porcine and primate models, may be necessary for devices requiring human-scale anatomy or more complex physiological integration.
Critical parameters for in vivo validation include:
- Electrophysiological performance: Signal-to-noise ratio, recording stability, and stimulation efficacy over implantation periods of at least 30 days, with chronic studies extending to 6-12 months for devices intended for long-term use [57] [32].
- Histological analysis: Quantitative assessment of foreign body response, including fibrous capsule thickness, immune cell infiltration, and tissue damage at predetermined endpoints. One study demonstrated a reduction in fibrous capsule thickness to 28.6 ± 5.4 μm compared to 85.2 ± 12.7 μm for conventional Pt electrodes [32].
- Functional outcomes: Behavioral assessments or physiological measurements relevant to the device's intended therapeutic application, such as recovery of motor function in neural stimulation studies or normalization of physiological parameters in organ-specific applications.
Manufacturing and Scalability Considerations
Fabrication Techniques for Soft Bioelectronics
Translating laboratory demonstrations to clinically viable products requires manufacturing approaches that balance performance, scalability, and cost. Traditional microfabrication processes, including photolithography, thin-film deposition, and etching, offer high precision and compatibility with established semiconductor manufacturing infrastructure [7]. These methods are particularly suitable for creating ultra-thin devices and precise electrode arrays with feature sizes down to the micrometer scale. However, they often involve harsh chemicals and high temperatures that may be incompatible with some soft materials.
Printing technologies present attractive alternatives for scalable manufacturing of soft bioelectronics. Screen printing enables cost-effective, high-volume production of conductive traces and electrodes on flexible substrates [94]. Aerosol jet printing and inkjet printing offer digital patterning capabilities without the need for physical masks, facilitating rapid prototyping and customization [94]. Recent advances in 3D printing and microfluidics-assisted fabrication enable complex, multi-material structures with integrated functionality, such as vascularized conductive networks with curvature adaptation radii as small as 200 μm [32]. These additive approaches provide unprecedented design freedom but face challenges in resolution, material compatibility, and production throughput.
Integration and Packaging Strategies
Robust packaging and encapsulation represent critical challenges for commercial soft bioelectronics, particularly for chronic implantation. The encapsulation must prevent water and ion ingress while maintaining mechanical flexibility and biocompatibility. Traditional hermetic packaging using titanium or ceramic cases provides excellent barrier properties but introduces undesirable rigidity. Thin-film encapsulation using alternating layers of polymers and inorganic materials offers a more flexible alternative, though achieving long-term stability in the body remains difficult [57].
System integration poses additional challenges, particularly for devices incorporating multiple functionalities such as sensing, stimulation, power management, and wireless communication. Stretchable interconnects must maintain electrical continuity under strain while withstanding millions of motion cycles. Innovative approaches such as liquid metal embedded in elastomers, buckled nanostructures, and composite conductors help address these challenges but add complexity to the manufacturing process [91] [51]. As system complexity increases, design for reliability and manufacturability becomes increasingly crucial for commercial viability.
Commercialization Landscape and Market Outlook
Current Market Dynamics
The stretchable and conformal electronics market is experiencing rapid growth, driven by increasing demand for wearable technology and advancements in flexible materials. Market analysis indicates the global stretchable and conformal electronics market size was valued at USD 2.6 billion in 2024 and is predicted to increase to approximately USD 10.28 billion by 2034, expanding at a compound annual growth rate (CAGR) of 14.74% from 2025 to 2034 [94]. This growth is fueled by material science innovations and expanding applications across healthcare, consumer electronics, and automotive sectors.
The healthcare segment represents a major driver and adoption area for soft bioelectronics, with applications including electronic skin patches, implantable devices, smart wound dressings, and continuous health monitoring systems [94]. The transition from intermittent clinic-based measurements to continuous, real-time physiological monitoring represents a paradigm shift in disease management, particularly for chronic conditions such as cardiovascular diseases, diabetes, and neurological disorders. The medical and biomedical devices segment is anticipated to grow at the fastest CAGR in the coming years, reflecting the significant unmet clinical needs addressable by soft bioelectronic technologies [94].
Translation Pathways and Regulatory Considerations
Successful commercialization of soft bioelectronics requires careful navigation of regulatory pathways that vary by intended application, risk classification, and geographical region. For implantable devices, standards such as ISO 10993 for biological evaluation of medical devices provide frameworks for assessing biocompatibility. However, the novel materials and form factors employed in soft bioelectronics may not fit neatly into existing regulatory categories, necessitating early engagement with regulatory bodies such as the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA).
Clinical validation remains a significant hurdle in the translation process, requiring substantial investment and strategic trial design. For novel neuromodulation devices, demonstrating not only safety but also clinically meaningful efficacy outcomes adds complexity and cost to the development process. The integration of artificial intelligence and machine learning algorithms into closed-loop systems introduces additional regulatory considerations regarding algorithm transparency, validation, and adaptation over time. Companies pursuing commercialization must balance innovation with regulatory strategy to efficiently navigate these complex requirements.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for Soft Bioelectronics
| Category | Specific Materials | Function/Application | Key Considerations |
|---|---|---|---|
| Substrate Materials | Polydimethylsiloxane (PDMS), Polyimide, Parylene-C, Polyurethane elastomers | Structural support, Encapsulation, Determining mechanical properties | Modulus matching, Biostability, Processing compatibility |
| Conductive Materials | PEDOT:PSS, Gold nanostructures, Liquid metals (e.g., Gallium alloys), MXenes, Graphene | Electrodes, Interconnects, Sensing elements | Conductivity under strain, Biocompatibility, Processing methods |
| Semiconductor Materials | Organic semiconductors (e.g., PBTTT), Silicon nanomembranes, Hydrogel semiconductors | Active components for transistors, Amplifiers, Switches | Charge carrier mobility, Operational stability, Stretchability |
| Encapsulation Materials | SiO₂, Si₃N₄, SU-8, Medical-grade silicones, Self-healing polymers | Barrier against biofluids, Electrical insulation, Mechanical protection | Water vapor transmission rate, Adhesion, Flexibility |
| Bioactive Coatings | MXene-silk fibroin composites, Catechol-functionalized polymers, Anti-inflammatory drugs | Immune modulation, Enhanced integration, Drug delivery | Controlled release kinetics, Stability, Bioactivity |
| Characterization Tools | Electrochemical impedance spectrometers, Tensile testers, AFM, SEM with EDX | Material property assessment, Device performance evaluation | Measurement precision, Biological relevance, Standardization |
Future Perspectives and Concluding Remarks
The field of soft bioelectronics stands at the threshold of transformative clinical impact, with the potential to revolutionize patient monitoring, diagnosis, and therapy. However, realizing this potential requires addressing persistent challenges in materials stability, manufacturing scalability, and clinical validation. Future research directions will likely focus on enhancing the longevity of soft bioelectronic interfaces through improved barrier materials and self-healing systems, developing more efficient power solutions through advanced energy harvesting and wireless power transfer, and creating more sophisticated closed-loop systems that autonomously adapt therapy to patient needs.
The convergence of soft bioelectronics with artificial intelligence represents a particularly promising frontier, enabling intelligent analysis of complex physiological data and personalized therapeutic interventions [94]. Additionally, the development of bioresorbable electronics that safely dissolve after a predefined operational period could address applications requiring temporary monitoring or stimulation without the need for extraction surgery. As these technologies mature, interdisciplinary collaboration between materials scientists, electrical engineers, biologists, and clinicians will be essential to navigate the complex path from laboratory innovation to clinical implementation.
The roadmap to widespread clinical adoption requires not only technical innovation but also thoughtful consideration of regulatory pathways, reimbursement strategies, and clinical workflows. By addressing these multifaceted challenges through integrated approaches spanning fundamental materials research to clinical implementation, soft bioelectronics can fulfill their promise as transformative tools for healthcare, ultimately bridging the gap between electronic and biological systems to improve patient outcomes across a broad spectrum of diseases and conditions.
Conclusion
The development of soft and flexible bioelectronics marks a paradigm shift from rigid, intrusive devices to seamless, tissue-integrated systems that promise to redefine preventive medicine and personalized therapeutics. The key takeaways from this review underscore that success hinges on a multidisciplinary approach, combining advanced materials science with innovative engineering to solve fundamental challenges in mechanical matching, signal stability, and long-term biocompatibility. Future progress will likely be driven by the convergence of intelligent, closed-loop systems with artificial intelligence for data analysis, the refinement of minimally invasive deployment strategies such as injectable electronics, and a intensified focus on sustainable and bioresorbable materials. For researchers and drug development professionals, these advancements open new frontiers for exploring disease mechanisms in highly realistic physiological models and developing more precise, adaptive treatments, ultimately accelerating the transition of bioelectronic medicine from pioneering research to mainstream clinical practice.
References
- 1. Medical Electronics that Match the Stretchability of Human ... [https://viterbischool.usc.edu/news/2025/09/medical-electronics-that-match-the-stretchability-of-human-tissue/]
- 2. Advances in Soft Bioelectronics for Brain Research and ... [https://www.sciencedirect.com/science/article/pii/S2590238520305749]
- 3. Quantitative Imaging of Young's Modulus of Soft Tissues from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3426275/]
- 4. Inverse finite element characterization of soft tissues [https://www.sciencedirect.com/science/article/abs/pii/S1361841502000853]
- 5. UC Irvine, Columbia University researchers invent soft ... [https://news.uci.edu/2025/01/14/uc-irvine-columbia-university-researchers-invent-soft-bioelectronic-sensor-implant/]
- 6. In bioelectronics breakthrough, scientists create soft, ... [https://news.uchicago.edu/story/bioelectronics-breakthrough-scientists-create-soft-flexible-semiconductors]
- 7. Recent Progress of Soft and Bioactive Materials in Flexible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12038164/]
- 8. Achieving tissue-level softness on stretchable electronics ... [https://www.nature.com/articles/s41467-023-40191-3]
- 9. Materials strategy and device fabrication for stable closed ... [https://www.nature.com/articles/s44328-025-00045-y]
- 10. Advances in Stretchable Functional Materials for Soft ... [https://www.semanticscholar.org/paper/Advances-in-Stretchable-Functional-Materials-for-Koo/44febbd095e6344e52197a8f5a273d10138e1e17]
- 11. Review Strategies for body-conformable electronics [https://www.sciencedirect.com/science/article/pii/S2590238522000571]
- 12. Leveraging biomimetic materials for bioelectronics [https://www.sciencedirect.com/science/article/abs/pii/S2590238525000049]
- 13. Hydrogel-based soft bioelectronic interfaces and their ... [https://pubs.rsc.org/en/content/articlehtml/2025/tc/d4tc04150j]
- 14. Recent Progress in Hydrogel Synthesis and Biomedical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12192526/]
- 15. Hydrogels: Properties, Classifications, Characterizations, ... [https://www.clinicsearchonline.org/article/hydrogels-properties-classifications-characterizations-and-biomedical-applications]
- 16. Recent Advances in Conductive Composite Hydrogels for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562860/]
- 17. Review Advances in liquid metal composites: properties ... [https://www.sciencedirect.com/science/article/abs/pii/S2589597423002654]
- 18. Liquid Metals: From Fundamentals to Applications [https://www.mdpi.com/journal/materials/special_issues/RZD7M2W4A3]
- 19. From batteries to biosensors: Conductive polymers make ... [https://www.cas.org/resources/cas-insights/conductive-polymers]
- 20. Transient electronics for sustainability: Emerging technologies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12415906/]
- 21. Biodegradable Implantable Electronics with Wireless ... [https://pubmed.ncbi.nlm.nih.gov/41001961/]
- 22. Biodegradable Electronics Reshaping MedTech Markets [https://www.linkedin.com/pulse/disruptive-design-biodegradable-electronics-reshaping-huh9c]
- 23. Soft skin-interfacing electrodes for wearable bioelectronics [https://www.sciencedirect.com/science/article/abs/pii/S2590238525004527]
- 24. Solution-processable and photo-curable system for low ... [https://www.nature.com/articles/s41467-025-64256-7]
- 25. Biodegradable electronic materials for promoting ... [https://link.springer.com/article/10.1007/s43939-025-00381-w]
- 26. Biodegradable electronics may advance with ability to ... [https://www.psu.edu/news/engineering/story/biodegradable-electronics-may-advance-ability-control-dissolve-rate]
- 27. Converging Electrospinning and 3D-Printing Technologies [https://www.mdpi.com/2079-6439/13/6/83]
- 28. Recent Progress in the Application of Electrospinning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12295322/]
- 29. Digital light processing 3D printing of flexible devices [https://www.nature.com/articles/s41378-025-00885-8]
- 30. 3D Printing and Electrospinning of Drug- and Graphene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12028827/]
- 31. Aug 12, 2025 | Professor Jun Chen Receives 2025 ACS Nano ... [https://cnsi.ucla.edu/aug-12-2025-professor-jun-chen-receives-2025-acs-nano-lectureship-award/]
- 32. Recent progress of soft and bioactive materials in flexible ... [https://www.eurekalert.org/news-releases/1103092]
- 33. Biosignal Sensing Analysis (EEG, EMG, ECG, PPG) (2nd ... [https://www.mdpi.com/journal/sensors/special_issues/3UGO719OW5]
- 34. Advances in healthcare wearable devices [https://www.nature.com/articles/s41528-021-00107-x]
- 35. Recent Progress of Soft and Bioactive Materials in Flexible ... [https://pubmed.ncbi.nlm.nih.gov/40302943/]
- 36. Types of Biosignals: EEG, ECG, EMG, and Beyond [https://www.nexstem.ai/blogs/types-of-biosignals-eeg-ecg-emg-and-beyond]
- 37. A Comprehensive Survey on Wearable Computing for ... [https://www.mdpi.com/2079-9292/14/17/3443]
- 38. Bio-inspired electronics: Soft, biohybrid, and “living” neural ... [https://www.nature.com/articles/s41467-025-57016-0]
- 39. Volumetric 3D Printing and Melt-Electrowriting to Fabricate ... [https://pubmed.ncbi.nlm.nih.gov/40761175/]
- 40. Syringe-injectable mesh electronics integrate seamlessly ... [https://pubmed.ncbi.nlm.nih.gov/28533392/]
- 41. Syringe injectable electronics - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4591029/]
- 42. The Role of Hydrogel in Cardiac Repair and Regeneration for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9952459/]
- 43. A new patch could help to heal the heart [https://news.mit.edu/2025/new-patch-could-help-heal-heart-1104]
- 44. Drug-Releasing Heart Patch Implant Shows Promise After ... [https://www.insideprecisionmedicine.com/topics/precision-medicine/drug-releasing-heart-patch-implant-shows-promise-after-myocardial-infarction/]
- 45. Hydrogel-based soft bioelectronic interfaces and their ... [https://pubs.rsc.org/en/content/articlelanding/2025/tc/d4tc04150j]
- 46. Emerging roles of hydrogels, organogels, and their hybrids ... [https://www.nature.com/articles/s44328-025-00055-w]
- 47. Emerging electronic materials for next generation soft ... [https://www.eurekalert.org/news-releases/1060973]
- 48. Soft bioelectronics embedded with self-confined ... [https://www.nature.com/articles/s41467-025-63927-9]
- 49. Soft bioelectronics embedded with self-confined ... [https://pubmed.ncbi.nlm.nih.gov/41057299/]
- 50. Soft Bioelectronics with DNA Circuit Monitor Wounds [https://bioengineer.org/soft-bioelectronics-with-dna-circuit-monitor-wounds/]
- 51. Materials, structure design, performances of multifunctional ... [https://www.sciencedirect.com/science/article/abs/pii/S0079642525000696]
- 52. Multifunctional Biomedical Devices with Closed-Loop ... [https://pubmed.ncbi.nlm.nih.gov/40583499/]
- 53. Close-loop therapy with continuous sensing and on- ... [https://link.springer.com/article/10.1007/s44258-025-00058-2]
- 54. Recent Advances in Micro- and Nano-Enhanced Intravascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12349352/]
- 55. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 56. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00179-4]
- 57. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 58. A Review on Electroactive Polymer–Metal Composites [https://pmc.ncbi.nlm.nih.gov/articles/PMC10607043/]
- 59. A Review of Electroactive Polymers in Sensing and ... [https://www.mdpi.com/2076-0825/14/6/258]
- 60. Soft, breathable, and recyclable MXene fabrics for wearable ... [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d5mh00831j]
- 61. A synergistic strategy for effectively tackling biofouling in ... [https://www.sciencedirect.com/science/article/abs/pii/S0959652625012673]
- 62. Selectively damping materials for next-generation motion ... [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d5mh00700c]
- 63. Sub-400 nanometer-thick skin and environment adaptable ... [https://www.nature.com/articles/s41467-025-65089-0]
- 64. Bionics-inspired highly robust and fatigue-resistant ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725047576]
- 65. Ultrastretchable, fatigue-resistant eutectogel with ... [https://link.springer.com/article/10.1007/s42114-025-01395-x]
- 66. Reducing Noise, Artifacts and Interference in Single-Channel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10059683/]
- 67. Implantable bioelectronics toward long-term stability and ... [https://www.sciencedirect.com/science/article/pii/S2590238521000564]
- 68. Clinical challenges and opportunities related to the ... [https://www.sciencedirect.com/science/article/pii/S1742706124007566]
- 69. Multimodal bioelectronics: A pathway to digital health ... [https://www.sciencedirect.com/science/article/abs/pii/S2590238525000918]
- 70. Sustainable electronic biomaterials for body-compliant ... [https://www.sciencedirect.com/science/article/pii/S2211285524000843]
- 71. Could Microbes Help Create Sustainable Electronics? [https://asm.org/articles/2024/november/could-microbes-help-create-sustainable-electronics]
- 72. Convergence of biocompatible printed electronics and ... [https://www.nature.com/articles/s41528-025-00421-8]
- 73. Characterization and Validation of Flexible Dry Electrodes ... [https://www.mdpi.com/1424-8220/23/3/1468]
- 74. Flexible Bioelectrodes-Integrated Miniaturized System for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12252470/]
- 75. Material and structural considerations for high-performance ... [https://www.nature.com/articles/s43246-024-00490-8]
- 76. Dependence of Skin-Electrode Contact Impedance on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9656728/]
- 77. Flexible Non-contact Electrodes for Wearable Biosensors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9209699/]
- 78. A highly stable electrode with low electrode-skin ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566322007965]
- 79. A comparative study of flexible electrode design on the ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1632279/full]
- 80. Intrinsically soft electronics using conducting ... [https://www.nature.com/articles/s41427-025-00621-8]
- 81. Smart hydrogels with liquid metals: Structural design, ... [https://www.sciencedirect.com/science/article/abs/pii/S0032386125001570]
- 82. Recent progress of nanomaterials-based composite ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11954787/]
- 83. Bioelectronics: Emerging trends and applications [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d5tb90077h]
- 84. Liquid Metal–Polymer Hydrogel Composites for ... [https://www.mdpi.com/1420-3049/30/4/905]
- 85. Designing Polymers for Use in Next-Generation Bioelectronics [https://news.ncsu.edu/2025/10/engineering-polymer-electronics/]
- 86. Interpretable Machine Learning Framework for Diabetes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563896/]
- 87. Bioelectronic Interfaces and Sensors for Neural Organoids [https://www.nature.com/articles/s41378-025-01038-7]
- 88. Validation of Analytical Models for the Development of Non ... [https://www.mdpi.com/2079-6374/15/10/669]
- 89. Advances in bioelectronics for neural interfacing [https://link.springer.com/article/10.1557/s43579-025-00822-w]
- 90. Abstracts from the Sixth Bioelectronic Medicine Summit [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538809/]
- 91. Advances in Stretchable Functional Materials for Soft ... [https://www.e-jfpe.org/archive/view_article?doi=10.56767/jfpe.2024.3.2.179]
- 92. Towards robust flexible electronics: Fabrication ... [https://www.sciencedirect.com/science/article/pii/S0924424725008593]
- 93. Bioelectronic medicine: wearable and implantable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12447594/]
- 94. Stretchable and Conformal Electronics Market Size to Hit ... [https://www.precedenceresearch.com/stretchable-and-conformal-electronics-market]