Optimizing taVNS Protocols: A Comprehensive Guide to Parameters, Efficacy, and Safety for Clinical Research
This article provides a systematic analysis of transcutaneous auricular vagus nerve stimulation (taVNS) protocols for researchers and drug development professionals.
Optimizing taVNS Protocols: A Comprehensive Guide to Parameters, Efficacy, and Safety for Clinical Research
Abstract
This article provides a systematic analysis of transcutaneous auricular vagus nerve stimulation (taVNS) protocols for researchers and drug development professionals. It synthesizes current evidence on the foundational mechanisms of taVNS, detailing its neuroanatomical basis and neuromodulatory effects. The review covers methodological considerations, including stimulation parameters (frequency, intensity, pulse width, site) and their applications across neurological and psychiatric disorders. It addresses troubleshooting and optimization strategies, focusing on parameter variability and safety profiles. Finally, the article validates findings through efficacy comparisons with other neuromodulation techniques and discusses biomarker-driven assessments. This guide aims to support the design of rigorous, reproducible clinical trials and inform future therapeutic development.
Unraveling the Science: Neuroanatomy and Core Mechanisms of taVNS
Anatomical and Neurophysiological Foundation
The auricular branch of the vagus nerve (ABVN), also known as Arnold's or Alderman's nerve, provides a unique cutaneous representation of the vagus nerve on the outer ear, serving as a non-invasive gateway for neuromodulation [1] [2]. This anatomical specialization forms the foundational principle for transcutaneous auricular vagus nerve stimulation (taVNS).
Neuroanatomical Pathway and Central Projections
The ABVN arises from the superior ganglion of the vagus nerve and receives a connecting filament from the petrous ganglion of the glossopharyngeal nerve [2]. It traverses the temporal bone via the mastoid canaliculus, crosses the facial canal, and surfaces through the tympanomastoid fissure, ultimately innervating the skin of the ear canal, tragus, tympanic membrane, and parts of the auricle [1] [2]. Crucially, afferent fibers of the ABVN project directly to the nucleus of the solitary tract (NTS) in the brainstem [3] [4]. The NTS then connects to key neurotransmitter nuclei, including the locus coeruleus (noradrenergic), raphe nuclei (serotonergic), and nucleus basalis of Meynert (cholinergic), enabling widespread modulation of cortical and subcortical brain networks [3] [4].
Cutaneous Innervation and Stimulation Targets
Anatomical studies indicate that the concha (cymba conchae and cavum conchae) and the tragus are the most densely innervated regions by the ABVN, making them the primary targets for taVNS electrode placement [1] [5]. The earlobe, which lacks significant vagal innervation, is frequently used as a control (sham) stimulation site in clinical trials [3] [5]. Computational modeling confirms that electrode placement significantly influences current flow patterns, allowing for relatively selective stimulation of ABVN-innervated regions [5].
Table 1: Key Anatomical Features of the Auricular Branch of the Vagus Nerve (ABVN)
| Feature | Description | Research/Clinical Significance |
|---|---|---|
| Origin | Superior ganglion of the vagus nerve [2] | Defines the proximal connection to the main vagal trunk. |
| Intracranial Path | Traverses temporal bone via mastoid canaliculus [2] | Explains proximity to other cranial nerves (e.g., facial nerve). |
| Cutaneous Innervation | Ear canal, tragus, tympanic membrane, auricle (concha) [1] [2] | Identifies optimal stimulation sites (tragus, concha). |
| Afferent Projection | To the Nucleus Tractus Solitarius (NTS) in the brainstem [3] [4] | Establishes the central gateway for modulating key neurotransmitter systems. |
| Fiber Composition | Myelinated Aβ, Aδ, and unmyelinated C fibers [4] | Informs parameter selection for selective fiber activation. |
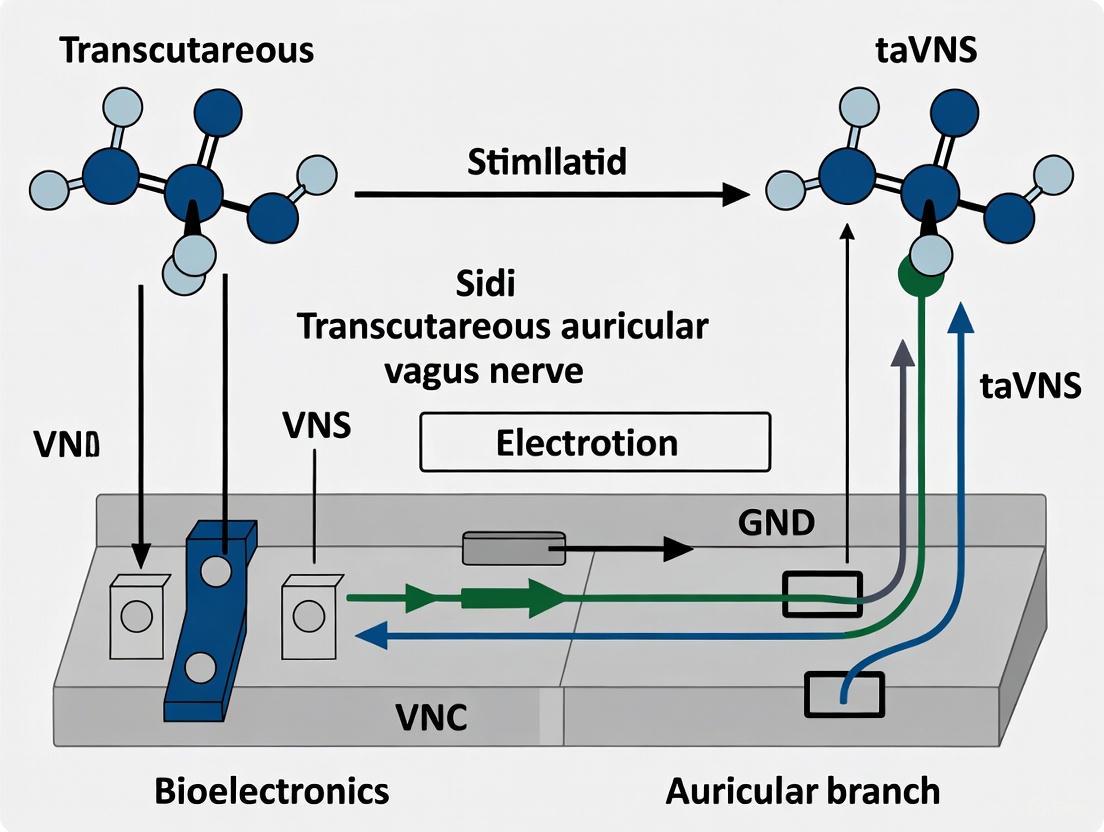
Diagram 1: Neuroanatomical pathway of ABVN and central projections activated by taVNS.
Research Applications and Physiological Mechanisms
The ABVN gateway enables taVNS to systemically modulate brain function and autonomic activity, supporting its investigation across numerous neurological and psychiatric conditions.
Key Therapeutic Applications and Associated Mechanisms
- Cognitive Enhancement: taVNS is hypothesized to improve cognitive processing speed, particularly in conditions like multiple sclerosis, by enhancing noradrenergic and cholinergic neurotransmission in cortical areas such as the prefrontal cortex and cerebellum [3]. This is the focus of ongoing clinical trials using the Symbol Digit Modalities Test (SDMT) as a primary outcome [3].
- Epilepsy Management: taVNS modulates functional brain network topology, with differential effects observed in focal versus generalized epilepsies, suggesting disease-specific mechanisms of action [6]. This network stabilization may underlie its reported antiseizure effects.
- Cardiac Function Regulation: In heart failure, taVNS improves left ventricular ejection fraction (LVEF), reduces heart rate, and lowers inflammatory markers like TNF-α, likely by restoring autonomic balance through increased parasympathetic tone [7].
- Motor Rehabilitation and Cortical Inhibition: Evidence suggests taVNS can enhance GABAergic neurotransmission, specifically GABA~A~-mediated cortical inhibition, and boost motor learning, supporting its potential application in stroke and Parkinson's disease rehabilitation [8] [9].
Table 2: Select Clinical Research Outcomes for taVNS (Based on Recent Meta-Analyses and Trials)
| Condition | Reported Outcome Measures | Key Findings / Effect Size | Proposed Mechanism |
|---|---|---|---|
| Heart Failure [7] | LVEF, 6-Minute Walk Distance (6-MWD), TNF-α, MLHFQ Score | ↑ LVEF (MD: 3.21%, p=0.0003), ↑ 6-MWD (MD: 86.6m, p<0.00001), ↓ TNF-α (MD: -1.47, p=0.001) | Autonomic nervous system rebalancing, reduced inflammation |
| Cognitive Impairment (RRMS) [3] | Symbol Digit Modalities Test (SDMT) | Primary outcome in ongoing trial; results pending | Enhanced noradrenergic & cholinergic projection to cortex |
| Epilepsy [6] | EEG-derived Functional Network Properties | Differential reorganization of global network characteristics in focal vs. generalized epilepsy | Modulation of brain network stability and robustness |
| Motor Learning [9] | Visuomotor Task Performance, SICI (TMS) | Improved learning, enhanced SICI (GABA~A~ activity) in females | Increased GABAergic cortical inhibition |
Detailed Experimental Protocols
This section provides standardized methodologies for key experiments, enabling replication and comparison across research studies.
Protocol 1: Investigating Effects on Cognitive Processing Speed in RRMS
This protocol is adapted from a registered, single-blinded, SHAM-controlled trial [3].
- Primary Objective: To evaluate the therapeutic potential of a single session of taVNS on cognitive processing speed in people with Relapsing-Remitting Multiple Sclerosis (PwRRMS).
- Subjects: 30 PwRRMS (diagnosed per McDonald criteria 2017) and 30 matched healthy controls. Age range: 18-50 years.
- Intervention:
- Active taVNS: Applied to the cymba conchae of the left ear.
- SHAM taVNS: Applied to the left earlobe.
- Stimulation Parameters:
- Duration: 30 minutes
- Pulse Width: 250 µs
- Stimulation Frequency: 25 Hz
- Duty Cycle: 30 seconds ON, 30 seconds OFF
- Intensity: Individually adjusted to tolerance threshold (just below pain threshold) [3].
- Assessment Schedule:
- Baseline Assessment: Administer primary and secondary outcome measures.
- Intervention: Apply active or SHAM taVNS.
- Post-Intervention Assessment: Re-admin primary and secondary outcome measures immediately after stimulation.
- Primary Outcome Measure: The Symbol Digit Modalities Test (SDMT). The total number of correct symbol-number pairings in 90 seconds is the primary metric. Use alternate versions to mitigate practice effects [3].
- Secondary Outcome Measures:
- Fatigue: Fatigue Scale for Motor and Cognitive Functions (FSMC).
- Depression: Beck Depression Inventory-II (BDI-II).
- Disease Severity: Expanded Disability Status Scale (EDSS) [3].
Diagram 2: Experimental workflow for a single-session taVNS cognitive study.
Protocol 2: Assessing Effects on Motor Cortex Inhibition and Learning
This protocol is adapted from research investigating the neurophysiological mechanisms of taVNS on motor learning [9].
- Primary Objective: To assess the effects of taVNS on GABA~A~-mediated intracortical inhibition and visuomotor learning.
- Experimental Design: Within-subject, cross-over design (active vs. sham taVNS) with order randomized and adequate washout period.
- Stimulation Protocol:
- Neurophysiological Assessment (TMS):
- Technique: Single- and paired-pulse Transcranial Magnetic Stimulation (TMS) over the primary motor cortex (M1).
- Key Metrics:
- SICI (Short-Interval Intracortical Inhibition): A proxy for GABA~A~ receptor activity.
- CSE (Corticospinal Excitability): Measured by Motor Evoked Potential (MEP) amplitude.
- LICI (Long-Interval Intracortical Inhibition): A proxy for GABA~B~ receptor activity.
- cSP (Cortical Silent Period).
- Timing: Measurements are taken at baseline (pre-stimulation) and immediately after the combined taVNS+task session [9].
- Behavioral Task: A computerized visuomotor adaptation or learning task is performed continuously throughout the 30-60 minute taVNS/sham stimulation period. Performance metrics (accuracy, reaction time) are recorded.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Equipment for taVNS Research
| Item Category | Specific Examples / Models | Critical Function & Application Notes |
|---|---|---|
| Stimulation Devices | NEMOS (Cerbomed); tVNS Technologies GmbH device | Deliver precisely controlled electrical pulses. Key features: adjustable intensity (mA), frequency (Hz), pulse width (µs), and duty cycle [3] [6]. |
| Electrodes | Hemispheric titanium electrodes; custom surface electrodes (various sizes) | Interface with the auricular skin. Material, size, and shape (e.g., 2x 8mm diameter) influence current density and stimulation selectivity [6] [5]. |
| Computational Modeling Software | Finite Element Method (FEM) platforms (e.g., COMSOL, SimNIBS) | Predict current flow, electric field distribution, and optimize electrode montage for sensitivity and selectivity before in-vivo testing [5]. |
| Neurophysiology & Outcome Assessment | EEG Systems (e.g., 19-channel); TMS with EMG; fMRI; SDMT; BDI-II; FSMC | Measure direct (brain activity, cortical inhibition) and indirect (behavioral, cognitive) outcomes of taVNS. Critical for validating target engagement [3] [6] [9]. |
| SHAM Control Equipment | Earlobe electrodes; placebo devices with minimal current | Provide a credible control condition by stimulating a non-vagal innervated site (e.g., earlobe) or using subliminal stimulation, essential for blinding [3] [5]. |
Transcutaneous auricular vagus nerve stimulation (taVNS) is a non-invasive neuromodulation technique that influences central nervous system function by stimulating the auricular branch of the vagus nerve [10]. Understanding the central pathways from the brainstem to cortical networks is fundamental for developing targeted taVNS protocols for neurological disorders and cognitive research. This application note details the key neural pathways, provides experimentally validated protocols, and offers practical methodological guidance for researchers investigating taVNS mechanisms and applications.
Central Pathways of taVNS
The vagus nerve serves as a critical bidirectional communication pathway between the periphery and central nervous system. taVNS primarily engages afferent (sensory) fibers, which constitute approximately 80% of its fibers [10]. Stimulation of the auricular branch initiates a cascade of neural signaling through well-defined anatomical pathways.
Core Pathway Model
The primary central pathway begins with afferent signals from the auricle projecting to the nucleus tractus solitarius (NTS) in the medulla oblongata [10]. The NTS serves as a central relay station, distributing signals to multiple key brainstem nuclei and beyond:
- Norepinephrine Pathway: The NTS projects to the locus coeruleus (LC), the brain's primary source of norepinephrine (NE) [11] [12]. The LC then broadcasts NE widely throughout the forebrain, influencing arousal, attention, and cognitive function [11].
- Serotonin Pathway: The NTS also connects with the raphe nuclei, which are the primary source of serotonin [11]. Serotonergic projections modulate mood, sleep, and aspects of cognition.
- Cholinergic Activation: Projections from the NTS to the basal forebrain, including the nucleus basalis of Meynert, activate cholinergic systems that are critical for learning, memory, and cortical plasticity [3] [13].
- Ascending Arousal Systems: The NTS influences the ascending reticular activating system (ARAS), a complex network in the brainstem that regulates wakefulness and arousal [11].
These subcortical modulatory pathways subsequently influence large-scale cortical networks. Research indicates taVNS can modulate the default mode network (DMN), salience network (SN), and fronto-parietal networks, which are essential for higher-order cognition [11] [14].
Figure 1: Central Pathways of taVNS. NE: Norepinephrine; 5-HT: Serotonin; ACh: Acetylcholine.
The Vagal Cortical Pathways Model
A comprehensive model proposes six consecutive pathways and mechanisms by which taVNS may influence consciousness and cognition, particularly in disorders of consciousness (DoC) [11]:
- Lower Brainstem Activation: Direct stimulation of the NTS.
- Upper Brainstem Activation: Subsequent activation of the ARAS.
- Norepinephrine Pathway: LC activation leading to widespread NE release.
- Serotonin Pathway: Raphe nuclei activation leading to serotonin release.
- Network Reconfiguration: Re-establishing cortico-striatal-thalamo-cortical loops.
- Network Modulation: Promoting connectivity changes between the DMN, SN, and external networks (ExN) [11].
Experimental Evidence & Quantitative Outcomes
Empirical studies using fMRI and EEG have quantified the impact of taVNS on brain activity and connectivity. The tables below summarize key findings.
Table 1: fMRI-Measured Functional Connectivity Changes Induced by taVNS
| Population | Stimulation Parameters | Key Brain Regions with Altered Connectivity | Primary Outcome | Citation |
|---|---|---|---|---|
| Mild Cognitive Impairment (MCI) | Left tragus, 25 Hz, 250 μs pulse width | Hippocampus, Temporal & Parietal Lobes | Enhanced connectivity within semantic and salience networks; hippocampal-cortical coupling. | [13] |
| Healthy Subjects | Bilateral concha, 30 Hz, 30s on/off | Right Frontal Gyrus, Fronto-Parietal Network | Significant activation in frontal regions and fronto-parietal network after 3.5 min of stimulation. | [14] |
Table 2: EEG Oscillation Changes Induced by taVNS
| Population | Stimulation Parameters | Key EEG Findings | Interpretation | Citation |
|---|---|---|---|---|
| Healthy Subjects | Single session, 25 Hz | ↑ Delta power in frontal regions; ↑ Right-hemisphere delta asymmetry. | Induction of homeostatic low-frequency activity; activation of fronto-vagal network. | [12] |
| DoC Patients* | Variable protocols | Modulation of low-frequency oscillations linked to arousal and awareness. | Potential for promoting consciousness recovery. | [11] |
DoC: Disorders of Consciousness; findings inferred from proposed mechanisms.
Detailed Experimental Protocols
Protocol 1: fMRI Investigation of taVNS-Induced Connectivity
This protocol is adapted from a study investigating taVNS effects in patients with Mild Cognitive Impairment (MCI) [13].
4.1.1 Research Question How does acute taVNS modulate functional connectivity within semantic, salience, and hippocampal-cortical networks in individuals with MCI?
4.1.2 Materials and Reagents Table 3: Essential Research Reagents & Equipment
| Item | Specification / Function | Research Application |
|---|---|---|
| taVNS Device | Certified for research (e.g., CE, FDA listed). | Precisely delivers electrical stimulation to the auricle. |
| MRI-Safe Electrodes | Bipolar, for auricular placement (tragus/concha). | Ensures safety and signal fidelity during fMRI. |
| 3T MRI Scanner | Equipped with high-resolution structural and fMRI sequences. | Measures BOLD signal for functional connectivity analysis. |
| Sham Electrodes | For placement on the earlobe (minimal vagal innervation). | Serves as a control condition for blinding. |
| Analysis Software | FSL, SPM, or CONN toolbox. | Processes fMRI data and performs seed-based connectivity analysis. |
4.1.3 Workflow
Figure 2: fMRI-taVNS Experimental Workflow.
4.1.4 Key Parameters
- Stimulation Site: Left tragus or cavum conchae.
- Control Site: Left earlobe.
- Stimulation Parameters: Frequency 25 Hz; Pulse width 200-500 μs; Current intensity individualized to tolerance threshold (e.g., 0.1-3 mA) [13] [10].
- fMRI Design: Blocked design (e.g., 30 seconds stimulation ON / 30 seconds OFF) for approximately 7-15 minutes total [14].
- Data Analysis: Preprocessing, then seed-based functional connectivity analysis using regions of interest (e.g., hippocampus, LC, thalamus).
Protocol 2: EEG Investigation of taVNS-Induced Cortical Oscillations
This protocol is based on a randomized, double-blinded, sham-controlled trial investigating taVNS effects on brain oscillations in healthy subjects [12].
4.2.1 Research Question Does a single session of taVNS alter resting-state low-frequency (delta/theta) oscillations and interhemispheric asymmetry in healthy adults?
4.2.2 Materials and Reagents Table 4: Essential Research Reagents & Equipment for EEG
| Item | Specification / Function | Research Application |
|---|---|---|
| High-Density EEG System | 64+ channels, AC coupled. | High-resolution recording of cortical electrical activity. |
| taVNS Device | Portable, with precise parameter control. | Delivers stimulation outside the lab or in a controlled setting. |
| Electro-Cap | Standardized electrode positions (10-20 system). | Ensures consistent electrode placement across subjects. |
| Sham Device | Identical to active device, delivers minimal/negligible current. | Critical for participant blinding and control condition. |
| EEG Analysis Software | EEGLAB, BrainVision Analyzer, MNE-Python. | Processes raw EEG data, filters artifacts, and computes power spectral density. |
4.2.3 Workflow
Figure 3: EEG-taVNS Experimental Workflow.
4.2.4 Key Parameters
- Stimulation Parameters: Frequency 25 Hz; Pulse width 250 μs; Cyclic stimulation (e.g., 30s on/30s off) for 30 minutes [12].
- EEG Recording: Resting-state, eyes closed, before and immediately after stimulation.
- Primary Metrics: Absolute and relative power in delta (1-4 Hz), theta (4-8 Hz), alpha (8-13 Hz), and beta (13-30 Hz) bands. Frontal asymmetry index.
- Analysis: Comparison of pre-to-post changes in power and asymmetry between active and sham groups.
The Scientist's Toolkit
Table 5: Key Research Reagent Solutions for taVNS Studies
| Category | Item | Critical Function | Research Application Notes |
|---|---|---|---|
| Stimulation Equipment | Certified taVNS Device | Precisely controls current, frequency, and pulse timing. | Select devices with research-grade output control and MRI-safe options if needed. |
| Research-Grade Electrodes | Targets vagally innervated auricular sites (tragus, cymba conchae). | Bipolar configurations minimize current spread. Material should minimize skin irritation. | |
| Control Conditions | Sham Stimulation Device | Controls for placebo effects and somatosensation. | Earlobe placement is the most validated sham site due to minimal vagal innervation [3] [13]. |
| Neuromonitoring & Outcome Measures | fMRI Scanner (3T+) | Measures BOLD signal changes to map network connectivity. | Ideal for investigating subcortical (e.g., LC, NTS) and deep cortical network engagement. |
| High-Density EEG System | Measures direct cortical oscillatory activity with high temporal resolution. | Best for capturing acute changes in brain rhythm power and asymmetry [12]. | |
| Analysis Tools | fMRI Preprocessing Pipelines (e.g., FSL, SPM) | Standardizes data for group analysis. | Corrects for motion, normalizes to standard space, and smooths data. |
| EEG Analysis Toolboxes (e.g., EEGLAB) | Processes raw EEG and computes spectral metrics. | Essential for artifact removal and time-frequency analysis. |
Transcutaneous auricular vagus nerve stimulation (taVNS) is a non-invasive neuromodulation technique that has garnered significant interest for its potential therapeutic applications in treating various neurological, psychiatric, and inflammatory conditions. By delivering electrical impulses to the auricular branch of the vagus nerve innervating the external ear, taVNS modulates central and peripheral neural circuits, leveraging the extensive projections of the vagus nerve to influence multiple physiological systems. This application note delineates the key mechanisms—neuroplasticity, anti-inflammation, and angiogenesis—underlying taVNS effects, providing detailed experimental protocols and analytical methodologies tailored for researchers, scientists, and drug development professionals engaged in neuromodulation and therapeutic development.
Key Mechanistic Pathways of taVNS
The therapeutic potential of taVNS is mediated through three primary, interconnected biological mechanisms, each supported by distinct molecular pathways and experimental evidence.
Neuroplasticity
Neuroplasticity refers to the nervous system's capacity to adapt and reorganize its structure and function in response to experience, injury, or stimulation. taVNS promotes neuroplasticity through several key mechanisms:
- BDNF-TrkB Signaling Pathway Activation: taVNS enhances the expression of Brain-Derived Neurotrophic Factor (BDNF) and its receptor, Tropomyosin receptor kinase B (TrkB). This activation is crucial for synaptic strengthening, neuronal survival, and the facilitation of long-term potentiation (LTP), a fundamental process for learning and memory [15]. Evidence indicates that taVNS enhances axonal plasticity and improves long-term neurological recovery by activating the BDNF signaling pathway via α7 nicotinic acetylcholine receptors (α7nAChR) [15].
- Modulation of Neurotransmitter Systems: taVNS influences the release of key neurotransmitters involved in plasticity. It increases the release of norepinephrine (NE) from the locus coeruleus and serotonin (5-HT) from the dorsal raphe nucleus, creating a neurochemical environment conducive to synaptic plasticity [15]. Furthermore, taVNS has been shown to boost GABAergic neurotransmission, specifically enhancing GABAA-mediated cortical inhibition, which is essential for refining neural circuits and supporting learning processes [9].
- State-Dependent Plasticity: The plasticity-inducing effects of taVNS are not spontaneous but are highly dependent on concurrent rehabilitative training. Pairing taVNS with specific tasks enhances synaptic plasticity within relevant neural circuits, leading to more robust functional recovery, as demonstrated in motor rehabilitation after stroke [15] [16].
Anti-inflammation
The anti-inflammatory effects of taVNS are primarily mediated through the cholinergic anti-inflammatory pathway (CAP), a neuro-immune reflex that modulates systemic inflammation:
- Cholinergic Anti-inflammatory Pathway (CAP): Afferent vagal signals, activated by taVNS, project to the nucleus tractus solitarius (NTS) in the brainstem. This leads to the activation of efferent vagal pathways, culminating in the release of acetylcholine (ACh) in the spleen. ACh binds to α7nAChR on macrophages, inhibiting the release of pro-inflammatory cytokines such as Tumor Necrosis Factor-alpha (TNF-α), Interleukin-6 (IL-6), and IL-1β [17] [15] [18].
- Alternative Anti-inflammatory Mechanisms: Beyond the CAP, taVNS may regulate inflammation through other pathways, including the enhancement of peroxisome proliferator-activated receptor gamma (PPAR-γ) expression and modulation of the hypothalamic-pituitary-adrenal (HPA) axis [15].
- Contextual Efficacy: It is important to note that the anti-inflammatory efficacy of taVNS in human clinical populations can be variable. A recent systematic review and meta-analysis found no consistent evidence for its anti-inflammatory effect across all studied conditions [18], while another study specifically showed no anti-inflammatory effect in people with diabetes [19]. This highlights that therapeutic outcomes may depend on factors such as patient population, disease state, and stimulation parameters.
Angiogenesis
Angiogenesis, the formation of new blood vessels from pre-existing vasculature, is a critical process for repairing damaged tissues, including after ischemic injury such as stroke.
- Promotion of New Blood Vessel Formation: Vagus nerve stimulation has been demonstrated to promote angiogenesis, which contributes to improved perfusion and recovery in ischemic tissues [16]. This mechanism is particularly relevant for conditions like stroke, where restoring blood flow to the penumbra (the area surrounding the core infarct) is crucial for salvaging neural tissue.
- Interplay with Other Mechanisms: Angiogenesis works in concert with neuroplasticity and anti-inflammatory processes. New blood vessels supply oxygen and nutrients necessary for plastic changes and support the clearance of inflammatory mediators, thereby creating a more favorable environment for recovery [16].
Table 1: Key Mechanisms and Associated Molecular Mediators of taVNS
| Mechanism | Key Molecular Mediators | Biological Outcome | Relevant Disease Models |
|---|---|---|---|
| Neuroplasticity | BDNF, TrkB, Norepinephrine, Serotonin, GABA, α7nAChR [15] [9] | Enhanced synaptic strength, improved neural circuit function, motor learning [16] [9] | Stroke, Epilepsy, Cognitive Impairment [15] [16] |
| Anti-inflammation | Acetylcholine, α7nAChR, TNF-α, IL-6, IL-1β, PPAR-γ [17] [15] | Reduction in pro-inflammatory cytokine release, immune cell modulation [17] [15] | Rheumatoid Arthritis, Inflammatory Bowel Disease, Sepsis [17] |
| Angiogenesis | Not specified in results | Promotion of new blood vessel formation, improved tissue perfusion [16] | Ischemic Stroke [16] |
Experimental Protocols for Investigating taVNS Mechanisms
To ensure reproducible and valid results in taVNS research, standardized experimental protocols are essential. The following sections provide detailed methodologies for both human and animal studies.
taVNS Application Protocol
This protocol outlines the common parameters for administering taVNS in clinical and preclinical research settings.
- Stimulation Site: The cymba conchae of the left ear, which receives exclusive innervation from the auricular branch of the vagus nerve, is the most targeted site [15] [20]. Sham stimulation is typically applied to the earlobe, which has minimal vagal innervation [3].
- Stimulation Parameters: While parameters vary, a common protocol used in clinical studies involves:
- Duration: 30 minutes per session [3].
- Frequency: 25 Hz [3] [19].
- Pulse Width: 250 μs [3].
- Intensity: Set to the individual's tolerance threshold, just below the level of pain [3] [19].
- Duty Cycle: A common pattern is 30 seconds of stimulation followed by 30 seconds off, to prevent nerve habituation and potential damage [3].
- Device: Commercially available tVNS devices (e.g., GammaCore Sapphire) or custom-built stimulators with bipolar electrodes are typically used [19] [20].
Table 2: Example taVNS Parameters from Clinical Studies
| Study Objective | Stimulation Site | Frequency | Pulse Width | Session Duration | Duty Cycle |
|---|---|---|---|---|---|
| Cognitive processing in Multiple Sclerosis [3] | Cymba Conchae | 25 Hz | 250 μs | 30 min | 30s on, 30s off |
| Anti-inflammatory effect in Diabetes [19] | Cervical (neck) | 25 Hz | 200 μs (1ms burst) | 120 s (per side) | Continuous |
| Motor Learning [9] | Cymba Conchae | Not specified | Not specified | During task | Not specified |
Protocol for Assessing Effects on Cognitive Processing
This protocol is adapted from a study investigating the effect of taVNS on cognitive processing speed in relapsing-remitting multiple sclerosis (RRMS) [3].
- Primary Outcome Measure: Cognitive processing speed, measured using the Symbol Digit Modalities Test (SDMT). The total number of correct symbol-number pair matches in 90 seconds is the primary metric [3].
- Secondary Outcome Measures:
- Depression: Beck Depression Inventory-II (BDI-II).
- Fatigue: Fatigue Scale for Motor and Cognitive Functions (FSMC).
- Disease Severity: Expanded Disability Status Scale (EDSS).
- Study Design:
- A prospective, single-center, sham-controlled, single-blinded trial.
- Participants are randomized into active taVNS or sham stimulation groups.
- Baseline Assessment: Conduct SDMT, BDI-II, and FSMC before stimulation.
- Intervention: Apply active or sham taVNS for 30 minutes using the parameters outlined in section 3.1.
- Post-Intervention Assessment: Re-administer the SDMT, BDI-II, and FSMC immediately after the stimulation session.
- Statistical Analysis: Compare changes in SDMT scores from baseline to post-intervention between the active and sham groups using ANOVA or mixed-model regression, adjusting for potential confounders like baseline fatigue and depression scores.
Protocol for Evaluating Anti-inflammatory Effects
This protocol details a method for quantifying the impact of taVNS on systemic inflammatory biomarkers [19] [18].
- Primary Outcome Measures: Plasma concentrations of pro-inflammatory and anti-inflammatory cytokines, including IL-6, IL-8, IL-10, TNF-α, and IFN-γ, quantified using multiplex immunoassay technology (e.g., Meso Scale Discovery V-PLEX panels) [19].
- Study Design:
- A randomized, double-blind, sham-controlled trial.
- Baseline Blood Sample: Collected from participants after a fasting period of at least 6 hours before initiating the taVNS intervention.
- Intervention Phase:
- Study Period 1 (Short-term, high-dose): Participants self-administer active or sham taVNS four times daily for seven days.
- Wash-out Period: A period of at least 14 days with no stimulation.
- Study Period 2 (Long-term, moderate-dose): Participants self-administer stimulation two times daily for 56 days.
- Follow-up Blood Samples: Collected after study period 1 and study period 2.
- Sample Analysis: All plasma samples are analyzed in a single batch to minimize inter-assay variability.
- Statistical Analysis: Compare cytokine levels between the active and sham groups at each time point using linear mixed models, including factors such as age, sex, diabetes type, and presence of cardiac autonomic neuropathy as covariates.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Equipment for taVNS Research
| Item | Function/Application | Example/Specifications |
|---|---|---|
| taVNS Device | Non-invasive electrical stimulation of the auricular vagus nerve. | GammaCore Sapphire [19]; custom stimulators with bipolar electrodes (e.g., silver cup electrodes) [20]. |
| ELISA/Multiplex Immunoassay Kits | Quantification of protein levels of cytokines (e.g., TNF-α, IL-6, IL-1β) and neurotrophic factors (e.g., BDNF) in plasma, serum, or tissue homogenates. | Meso Scale Discovery (MSD) V-PLEX Proinflammatory Panel 1 Human Kit [19]. |
| Neuropsychological Assessments | Behavioral measurement of cognitive, motor, and mood-related outcomes. | Symbol Digit Modalities Test (SDMT) [3], Fugl-Meyer Assessment for Upper Extremity (FMA-UE) [16], Beck Depression Inventory-II (BDI-II) [3]. |
| Transcranial Magnetic Stimulation (TMS) | Neurophysiological assessment of cortical excitability and GABAergic inhibition (via SICI, LICI, CSP). | Used to measure tVNS-induced changes in intracortical inhibition in the motor cortex [9]. |
| Functional Magnetic Resonance Imaging (fMRI) | Mapping of brain activity and functional connectivity changes in response to taVNS. | Identifies activation in NTS, locus coeruleus, insula, and other regions [3]. |
Mechanistic Pathway Diagrams
taVNS Anti-inflammatory and Neuroplasticity Pathways
Diagram 1: taVNS Anti-inflammatory and Neuroplasticity Pathways. This diagram illustrates the primary neural pathways activated by taVNS. Afferent signals from the ABVN project to the NTS in the brainstem. The NTS then activates the LC, leading to norepinephrine release and subsequent upregulation of BDNF, promoting neuroplasticity. Concurrently, efferent signals via the DMN engage the cholinergic anti-inflammatory pathway in the spleen, where acetylcholine binding to α7nAChR on macrophages suppresses the release of pro-inflammatory cytokines [17] [15] [16].
Experimental Workflow for taVNS Research
Diagram 2: Experimental Workflow for taVNS Research. This flowchart outlines a standard randomized controlled trial (RCT) design for investigating taVNS. After recruitment and baseline assessments, participants are randomized into active or sham control groups. The intervention is administered according to a predefined protocol, followed by post-intervention and follow-up assessments to measure outcomes. This design is critical for establishing causal efficacy and controlling for placebo effects [3] [19] [18].
Transcutaneous auricular vagus nerve stimulation (taVNS) has emerged as a prominent non-invasive neuromodulation technique, attracting significant research interest for its potential to treat a range of neurological and psychiatric conditions. This application note synthesizes current neurophysiological evidence, derived primarily from electroencephalogram (EEG) and functional magnetic resonance imaging (fMRI), to elucidate the brain modulation signatures elicited by taVNS. Framed within a broader thesis on taVNS protocol research, this document provides researchers and drug development professionals with a detailed overview of the mechanistic underpinnings, standardized experimental protocols, and key reagents essential for investigating and applying taVNS in both clinical and research settings. The efficacy of taVNS is believed to stem from its ability to activate the vagus nerve's afferent pathways, which project to the nucleus of the solitary tract (NTS) and subsequently influence a wide network of cortical and subcortical regions, modulating key neurotransmitter systems including norepinephrine, GABA, and serotonin [21] [3] [20].
Mechanistic Foundations and Signaling Pathways
The therapeutic potential of taVNS is grounded in its capacity to influence central nervous system activity through well-defined neuroanatomical pathways. The vagus nerve, a key component of the parasympathetic nervous system, is composed of approximately 80% afferent fibers, which transmit sensory information from the body to the brain [22]. taVNS primarily targets the auricular branch of the vagus nerve (ABVN), which is densely distributed in specific regions of the external ear, including the cymba concha, tragus, and concha [20]. Stimulation of these cutaneous afferents initiates a signaling cascade that propagates to higher brain centers.
Table 1: Key Neurophysiological Effects of taVNS
| Effect Category | Specific Outcome | Measured Parameter | Supporting Evidence |
|---|---|---|---|
| Brainstem Activation | Increased BOLD signal in NTS | fMRI | [23] |
| Cortical Inhibition | Enhanced GABAA-mediated inhibition | SICI (TMS metric) | [9] |
| Cardiac Interoception | Increased amplitude of HEP | EEG | [24] |
| Autonomic Function | Modulation of heart rate variability | HRV | [24] |
| Cognitive Performance | Improved visuomotor learning | Behavioral task accuracy | [9] |
| Arousal System | Pupil dilation (pulsed protocols only) | Pupillometry | [25] |
Afferent vagal signals first project to the NTS in the brainstem. From there, the pathway extends to other key brainstem nuclei, most notably the locus coeruleus (LC), the primary source of norepinephrine in the brain, and the raphe nuclei, which are the main source of serotonin [21] [3]. This brainstem activation leads to the subsequent modulation of cortical excitability and widespread neural networks. Recent fMRI studies have confirmed that taVNS perturbs brain signaling in the NTS, though these effects are dependent on sufficient temporal signal-to-noise ratio (tSNR) and require precise localization [23]. The resulting neuromodulatory effects include increased release of norepinephrine and GABA, which are critical for regulating attention, cognitive functions, and cortical inhibition [21] [9]. Furthermore, taVNS has been shown to influence cardiac-related interoceptive processing by increasing the amplitude of heart-evoked potentials (HEP), a potential EEG correlate of interoceptive prediction error signaling [24].
Figure 1: taVNS Central Signaling Pathway. ACC: Anterior Cingulate Cortex; PFC: Prefrontal Cortex; NE: Norepinephrine; 5-HT: Serotonin; HEP: Heart-Evoked Potential; HRV: Heart Rate Variability.
Neurophysiological Signatures: EEG and fMRI Evidence
EEG Correlates of taVNS
Electroencephalography provides high-temporal-resolution insights into the neural dynamics modulated by taVNS. A key signature is the enhancement of the heart-evoked potential (HEP), an EEG potential time-locked to the cardiac cycle. A recent study demonstrated that active taVNS, compared to sham stimulation, produced significantly higher HEP amplitudes during a cardiac interoceptive task. This enhancement is interpreted as a correlate of increased precision in processing cardiac interoceptive signals, potentially reflecting strengthened cardiac-related prediction error signals within the brain's predictive processing framework [24]. Furthermore, the same study found that the positive relationship between interoceptive accuracy and allostatic adjustments (measured via heart rate variability) was mediated by HEP amplitudes, positioning the HEP as a critical neural mediator of taVNS's effects on autonomic regulation [24].
Beyond HEP, taVNS has been shown to specifically enhance GABAA-mediated cortical inhibition. Using transcranial magnetic stimulation (TMS) to probe neurophysiology, one study found that active taVNS significantly increased short-interval intracortical inhibition (SICI), a specific TMS metric for GABAA receptor activity. This effect was particularly pronounced in female participants. Notably, the same study found that taVNS concurrently boosted performance in a visuomotor learning task, linking the neurophysiological effect to a behavioral outcome [9]. This provides direct evidence that taVNS can refine inhibitory neurotransmission, which has broad implications for treating disorders characterized by network hyperexcitability.
fMRI Correlates of taVNS
Functional MRI offers complementary high-spatial-resolution data on the brain networks modulated by taVNS. The primary afferent pathway of the vagus nerve can be visualized with fMRI, with studies confirming that taVMS increases the blood-oxygen-level-dependent (BOLD) signal in the NTS [23]. However, this effect is technically challenging to capture and is dependent on achieving a sufficient temporal signal-to-noise ratio (tSNR) within the brainstem [23].
From the NTS, activation propagates to a distributed network of cortical and subcortical regions. fMRI studies have shown that taVNS modulates activity in areas including the insula, anterior cingulate cortex (ACC), prefrontal cortex, postcentral gyrus, and cerebellum [3] [23]. The insula and ACC are key nodes of the interoceptive network, and their modulation by taVNS aligns with the observed changes in HEP amplitude and interoceptive accuracy [24]. The overlap between these taVNS-modulated areas and the networks critical for cognitive processes, such as the fronto-parietal network activated during the Symbol Digit Modalities Test, provides a plausible neural substrate for the cognitive-enhancing effects reported in some taVNS studies [3].
Table 2: EEG and fMRI Signatures of taVNS-Induced Brain Modulation
| Modality | Biomarker/Effect | Neurophysiological Interpretation | Associated Cognitive/Clinical Outcome |
|---|---|---|---|
| EEG | ↑ Heart-Evoked Potential (HEP) Amplitude | Enhanced processing of cardiac interoceptive signals; ↑ precision of prediction errors | Improved interoceptive accuracy, allostatic regulation [24] |
| EEG/TMS | ↑ Short-Interval Intracortical Inhibition (SICI) | Enhanced GABAA-mediated inhibitory neurotransmission | Improved visuomotor learning; potential for treating epilepsy [9] |
| fMRI | ↑ BOLD in Nucleus of Solitary Tract (NTS) | Successful activation of the primary afferent terminus of the vagus nerve | Validation of target engagement [23] |
| fMRI | Modulation of Insula/ACC Activity | Altered interoceptive and salience network processing | Regulation of autonomic and emotional states [24] [3] |
| fMRI | Modulation of Prefrontal Cortex/Cerebellum | Altered executive control and motor coordination networks | Potential improvement in cognitive processing speed [3] |
| Pupillometry | Pupil Dilation (Pulsed Protocols) | Phasic increase in norepinephrine release | Potential biomarker for monoaminergic engagement [25] |
Detailed Experimental Protocols
Protocol 1: Investigating taVNS Effects on Cardiac Interoception and HEP
This protocol is designed to quantify taVNS-induced changes in cardiac interoceptive processing and their neural correlates using EEG.
- Primary Objective: To assess the effect of taVNS on interoceptive accuracy and its electrophysiological correlate, the heart-evoked potential (HEP).
- Study Design: Within-subject, cross-over design with active taVNS and sham stimulation sessions, spaced at least one week apart to avoid carryover effects [24].
- Participants: Typically, healthy adult volunteers. Exclusion criteria include history of cardiovascular, neurological, or psychiatric disorders.
- Stimulation Parameters:
- Device: A transcutaneous electrical nerve stimulation (TENS) device capable of delivering low-intensity currents.
- Site: The cymba conchae of the left ear for active stimulation [24] [9]. The earlobe is a common site for sham stimulation due to its minimal vagal innervation [3] [20].
- Parameters: Pulse width ~250 μs, frequency ~25 Hz, with a duty cycle (e.g., 30s on/30s off) to prevent nerve habituation. Intensity is set just below the individual's pain threshold [24] [3].
- Procedure:
- Baseline Recording: Participants perform the Heartbeat Counting Task (HCT) without stimulation to establish a baseline for interoceptive accuracy (IAcc) [24].
- Stimulation & Task Blocks: Participants repeat the HCT task during multiple blocks of active or sham stimulation.
- EEG & ECG Recording: Continuous EEG is recorded from a 64-channel cap, and electrocardiogram (ECG) is recorded simultaneously. EEG is referenced to the left mastoid and sampled at ≥1000 Hz [24] [26].
- Data Analysis:
- IAcc: Calculated from the HCT using the formula: IAcc = 1/3 Σ [1 - (|recorded heartbeats - counted heartbeats| / recorded heartbeats)] [24].
- HEP: EEG epochs are time-locked to the R-peak of the ECG. HEP amplitude is calculated as the average amplitude in a post-R-peak window (e.g., 200-500ms) after artifact rejection and baseline correction [24].
- Statistical Analysis: Repeated-measures ANOVA or mixed models are used to compare IAcc and HEP amplitudes between active and sham conditions.
Figure 2: Protocol Workflow for taVNS and Cardiac Interoception. HCT: Heartbeat Counting Task; IAcc: Interoceptive Accuracy; HEP: Heart-Evoked Potential.
Protocol 2: Probing taVNS Effects on Cortical Inhibition and Learning with TMS-EEG
This protocol combines taVNS with TMS and EEG to investigate GABAergic mechanisms and their behavioral consequences.
- Primary Objective: To determine the effect of taVNS on GABAA-mediated intracortical inhibition and visuomotor learning.
- Study Design: Within-subject design, where each participant undergoes active and sham taVNS in separate sessions, with baseline neurophysiological assessments pre-stimulation [9].
- Participants: Healthy adults. Key exclusion criteria: contraindications to TMS, neurological or psychiatric history.
- Stimulation Parameters:
- Site: Cymba conchae of the left ear.
- Parameters: Similar to Protocol 1 (30 min, pulse width 250 μs, frequency 25 Hz, 30s on/30s off, intensity at tolerance threshold) [9].
- Procedure:
- Baseline TMS Measures: Before stimulation, single- and paired-pulse TMS is applied to the primary motor cortex (e.g., right or left M1) to measure baseline corticospinal excitability (CSE), short-interval intracortical inhibition (SICI), long-interval intracortical inhibition (LICI), and intracortical facilitation (ICF) [9].
- Concurrent taVNS & Task: Active or sham taVNS is applied while the participant performs a computerized visuomotor learning task.
- Post-Stimulation TMS Measures: TMS protocols are repeated immediately after the stimulation period to quantify changes.
- Data Analysis:
- Neurophysiology: SICI (GABAA), LICI (GABAB), and CSE are calculated from TMS-induced motor evoked potentials (MEPs). A significant increase in SICI post-active taVNS compared to baseline and sham indicates enhanced GABAA activity [9].
- Behavior: Visuomotor task performance (e.g., accuracy, reaction time) is compared across stimulation conditions and task blocks.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials and Reagents for taVNS Research
| Item Category | Specific Example/Model | Critical Function | Protocol Notes |
|---|---|---|---|
| Stimulation Device | TENS device with isolated output | Delivers precise, controlled electrical pulses to the auricular vagus nerve. | Must allow parameter control (frequency, pulse width, current) and duty cycling [3] [20]. |
| EEG System | 64-channel amplifier system (e.g., g.HIamp) with active electrodes | Records high-fidelity electrical brain activity (e.g., HEP). | High sampling rate (≥1000 Hz) and synchronized ECG recording are crucial [24] [26]. |
| fMRI Scanner | 3T MRI system with high-sensitivity head coil | Measures BOLD signal changes in deep and cortical brain structures. | High tSNR is critical for detecting brainstem activation (NTS) [23]. |
| TMS System | Magnetic stimulator with figure-of-eight coil | Probes cortical excitability and GABAergic inhibition (SICI, LICI). | Used in conjunction with EMG to record MEPs from target muscles [9]. |
| Electrocardiogram | ECG recording module | Records heartbeats for HEP analysis and HRV calculation. | Must be synchronized with the EEG system [24]. |
| Sham Electrode | Custom electrode for earlobe placement | Provides a credible sham condition by mimicking sensory aspects without significant vagal activation. | Critical for blinding participants and controlling for non-specific effects [3] [20]. |
| Neuropsychological Tests | Symbol Digit Modalities Test (SDMT), Fatigue Scale for Motor and Cognitive Functions (FSMC) | Quantifies cognitive processing speed and fatigue. | Used to assess behavioral outcomes in clinical populations (e.g., MS) [3]. |
Discussion and Future Directions
The convergence of evidence from EEG and fMRI studies provides a compelling picture of taVNS as a potent modulator of brain function. The signatures—enhanced HEP amplitudes, increased GABAergic inhibition, and modulated activity in the interoceptive and cognitive control networks—offer a neurophysiological basis for its reported therapeutic benefits. However, several challenges remain for the translation of this knowledge into standardized clinical practice. A significant issue is the lack of a standardized stimulation protocol. Parameters such as current intensity, pulse frequency, and duty cycle vary across studies, making direct comparisons difficult [20]. Furthermore, the choice of an optimal sham condition is still debated, though the earlobe is commonly used [3] [20].
Future research must prioritize large-scale, multicenter trials with standardized protocols to validate these neurophysiological signatures as biomarkers for specific clinical outcomes. The differential effects of conventional (continuous) versus pulsed stimulation protocols on physiological markers like pupil dilation [25] suggest that the temporal pattern of stimulation is a critical parameter that requires systematic exploration. Additionally, exploring state-dependent effects and individual factors, such as sex, which was shown to modulate the GABAergic response to taVNS [9], will be key to personalizing therapy. Finally, combining taVNS with other modalities like fMRI-EEG or TMS-EEG will further our mechanistic understanding and help optimize this promising non-invasive tool for both cognitive enhancement and clinical intervention in neurological and psychiatric disorders.
Protocol Design: Stimulation Parameters and Clinical Applications
Transcutaneous auricular vagus nerve stimulation (taVNS) has emerged as a promising non-invasive neuromodulation technique for a spectrum of neurological, psychiatric, and cardiovascular conditions. As a library, NLM provides access to scientific literature. Inclusion in an NLM database does not imply endorsement of, or agreement with, the contents by NLM or the National Institutes of Health. [27] Unlike invasive vagus nerve stimulation, taVNS selectively targets the auricular branch of the vagus nerve (ABVN)—the only superficially accessible vagal branch—to activate central pathways without surgical implantation. [27] The efficacy of taVNS is fundamentally governed by the precise selection of stimulation parameters, including frequency, intensity, pulse width, and duration. However, the field currently lacks standardized protocols, and parameter optimization remains a primary challenge in translating taVNS research into predictable clinical outcomes. [28] [29] This application note synthesizes current evidence to provide structured guidance on critical parameter selection for researchers and drug development professionals, framing these decisions within the context of target engagement and therapeutic objectives.
Parameter Optimization and Quantitative Evidence
Frequency and Pulse Width Selection
Stimulation frequency is a major parameter significantly impacting the neuromodulatory effects of taVNS. [30] Different frequencies appear to recruit distinct neural pathways and produce condition-specific therapeutic outcomes. The following table summarizes evidence-based frequency and pulse width combinations for various applications.
Table 1: Frequency and Pulse Width Optimization for Clinical Applications
| Clinical Target | Effective Frequency | Effective Pulse Width | Key Findings | Citation |
|---|---|---|---|---|
| Heart Rate Variability (HRV) in Healthy Adults | 10 Hz & 25 Hz | 100 µs, 250 µs, 500 µs | The combinations 10 Hz/250 µs, 10 Hz/500 µs, and 25 Hz/100 µs significantly increased SDNN, a measure of overall HRV. [29] | [29] |
| Hypertension & Blood Pressure | 100 Hz | Not Specified | 100 Hz RAVANS (Respiratory-gated Auricular Vagus Afferent Nerve Stimulation) significantly reduced diastolic and mean arterial blood pressure in Black hypertensive participants. [30] | [30] |
| Disorders of Consciousness (DOC) | Under Investigation | Not Specified | An ongoing trial is evaluating 1, 10, 25, 50, and 100 Hz; 100 Hz may elicit the strongest brainstem fMRI response. [28] | [28] |
| Post-Stroke Motor Rehabilitation | 20-30 Hz | 200-500 µs | Multiple RCTs for upper limb dysfunction used frequencies of 20-30 Hz and pulse widths of 0.2-0.5 ms, showing significant functional improvement. [27] [31] | [27] [31] |
| Chronic Insomnia & Functional Dyspepsia | 80 Hz | 100 µs | A fixed high-frequency protocol is being utilized in an RCT for elderly patients with comorbid conditions. [32] | [32] |
Intensity, Duration, and Session Parameters
Stimulation intensity and treatment duration are critical for ensuring sufficient neural activation while maintaining patient safety and tolerability. The following table consolidates common parameters derived from clinical studies.
Table 2: Intensity, Duration, and Treatment Course Parameters
| Parameter | Common Range in Clinical studies | Notes and Considerations | Citation |
|---|---|---|---|
| Stimulation Intensity | 0.1 - 3 mA | Typically adjusted to a level just below the discomfort threshold, often described as a "slight tapping sensation" without pain. [27] [12] | [27] [12] |
| Daily Session Duration | 15 - 30 minutes | Shorter sessions (e.g., 15 min) are used in acute HRV studies, while longer sessions (e.g., 30 min) are common for chronic conditions. [29] [32] | [29] [32] |
| Treatment Course | 2 weeks - 6 weeks | Clinical trials often administer stimulation over multiple weeks; 4-week courses are frequently reported in post-stroke rehabilitation studies. [27] | [27] |
| Stimulation Site | Cymba Conchae | The left cymba conchae is most commonly targeted to avoid potential cardiac side effects, as the left vagus nerve primarily innervates the atrioventricular node. [27] [33] | [27] [33] |
Detailed Experimental Protocols
Protocol for Parameter Optimization in Autonomic Function
This protocol is adapted from a randomized controlled trial investigating the acute effects of taVNS on heart rate variability in healthy adults. [29]
Objective: To systematically evaluate the acute effects of different frequency and pulse width combinations of taVNS on Heart Rate Variability (HRV) in healthy participants.
Materials:
- taVNS device with programmable frequency, pulse width, and intensity.
- ECG recording equipment for continuous HRV monitoring (e.g., SDNN, RMSSD).
- Computer for data storage and analysis.
- Electrodes for attachment to the cymba conchae of the left ear.
Procedure:
- Participant Preparation: Recruit healthy adult participants with no history of neurological, psychiatric, or cardiovascular disorders. Obtain informed consent.
- Environment Setup: Conduct sessions in a quiet, dimly lit, temperature-controlled (22–24 °C) room. Ask participants to refrain from intense exercise, alcohol, caffeine, and smoking on the test day.
- Randomization & Blinding: Employ a single-blinded, sham-controlled, randomized crossover design. Each participant undergoes all six active protocols and one sham session in randomized order, with a minimum 24-hour washout period between sessions.
- Stimulation Protocol:
- Baseline Recording: Record a 15-minute resting ECG.
- Active/Sham Stimulation: Apply one of the following protocols for 15 minutes to the left cymba conchae:
- Protocol 1: 10 Hz at 100 µs
- Protocol 2: 10 Hz at 250 µs
- Protocol 3: 10 Hz at 500 µs
- Protocol 4: 25 Hz at 100 µs
- Protocol 5: 25 Hz at 250 µs
- Protocol 6: 25 Hz at 500 µs
- Sham: Electrodes placed with no current output.
- Intensity is set to a level perceptible but not painful (e.g., 1-3 mA).
- Recovery Recording: Record a 10-minute post-stimulation ECG.
- Data Analysis: Calculate HRV metrics (SDNN, RMSSD) for baseline, stimulation, and recovery periods. Use statistical models (e.g., linear mixed-effects models) to compare the effects of each active protocol against sham.
Protocol for Clinical Efficacy Trials in Post-Stroke Rehabilitation
This protocol synthesizes methodologies from multiple RCTs on taVNS for upper limb motor dysfunction after stroke. [27] [31]
Objective: To assess the efficacy of taVNS as an adjunct to conventional rehabilitation for improving upper limb motor function in chronic stroke patients.
Materials:
- CE-marked or FDA-cleared taVNS device.
- Upper limb motor assessment scales (Fugl-Meyer Assessment for Upper Extremity - FMA-UE, Action Research Arm Test - ARAT).
- Assessment tools for activities of daily living (e.g., Modified Barthel Index - MBI).
- Robotic training equipment or conventional rehabilitation tools.
Procedure:
- Participant Screening: Recruit patients >3 months post-stroke with moderate-to-severe upper limb motor impairment. Exclude patients with other neurological conditions or contraindications for taVNS.
- Baseline Assessment: Conduct pre-intervention assessments using FMA-UE, ARAT, and MBI.
- Randomization & Blinding: Randomly assign participants to active taVNS or sham control groups in a double-blind design. The sham group receives identical procedures with minimal or no effective electrical output.
- Intervention Protocol:
- Stimulation Parameters:
- Frequency: 25-30 Hz
- Pulse Width: 200-500 µs
- Intensity: 1-3 mA, adjusted to sensory threshold
- Stimulation Site: Left cymba conchae
- Training Regimen:
- Sessions: 30-minute sessions, 5 days per week for 4-6 weeks.
- Concurrent Therapy: taVNS is applied simultaneously during structured upper limb motor training (e.g., repetitive task-oriented training or robotic-assisted therapy).
- Each stimulation burst is timed to coincide with movement attempts or therapy tasks.
- Stimulation Parameters:
- Post-Intervention Assessment: Re-administer the FMA-UE, ARAT, and MBI scales immediately after the intervention course and at follow-up timepoints (e.g., 3 months) to assess retention.
- Statistical Analysis: Compare changes in motor scores from baseline to post-intervention between the active and sham groups using appropriate statistical tests (e.g., t-tests, ANOVA).
Safety and Tolerability Profile
Understanding the safety profile of taVNS is essential for clinical protocol design and risk assessment. A systematic review and meta-analysis of 177 studies involving 6,322 subjects found taVNS to be a safe and feasible intervention. [34]
- Adverse Event Incidence: The meta-analytic overall adverse events incidence rate was low, at 12.84 per 100,000 person-minutes-days of stimulation. [34]
- Common Adverse Effects: The most frequently reported adverse effects are mild and transient, including ear pain, headache, and tingling at the stimulation site. [34] Skin irritation and redness have also been reported but typically resolve quickly after stimulation ceases. [35]
- Risk Comparison: There were no differences in the risk of developing an adverse event between active taVNS and sham control groups. [34] No causal relationship has been established between taVNS and serious adverse events. [34] [35]
- Safety in Special Populations: Studies specifically investigating taVNS in older adults with Mild Cognitive Impairment (MCI) and patients with disorders of consciousness have also confirmed its feasibility and safety, with no serious adverse events related to the intervention. [28] [33]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials and Equipment for taVNS Research
| Item | Function/Application | Example Specifications/Models |
|---|---|---|
| Programmable taVNS Device | Core equipment for delivering controlled electrical stimulation to the auricle. | Devices capable of delivering frequencies (1-100 Hz), pulse widths (50-500 µs), and adjustable current (0.1-5 mA). |
| ECG Recording System | Objective measurement of autonomic outcomes, specifically Heart Rate Variability (HRV). | Systems for continuous ECG recording; software for calculating SDNN, RMSSD, HF/LF power. |
| fMRI or fNIRS System | Assessment of central target engagement and neural mechanisms. | For measuring functional connectivity changes in the NTS, DMN, and other brain networks. [28] [12] |
| Clinical Outcome Scales | Validated tools for measuring clinical efficacy in specific patient populations. | FMA-UE, ARAT, WMFT (stroke motor function) [31]; CRS-R (disorders of consciousness) [28]; PSQI (sleep quality) [32]. |
| Sham Electrodes/Device | Critical for blinding in controlled trials, controlling for placebo effects. | Identical appearance to active device, with no or minimal (e.g., <0.1 mA) current output. [29] |
| Electrode Conductive Gel | Ensures good skin contact and consistent current delivery. | Standard water-soluble ECG or EEG gel. |
Signaling Pathways and Experimental Workflow
Central Mechanisms of taVNS
The following diagram illustrates the proposed neural pathways and mechanisms through which taVNS exerts its therapeutic effects, based on neuroimaging and neurophysiological studies. [27] [12]
Experimental Workflow for Parameter Optimization
This flowchart outlines a systematic approach for optimizing taVNS stimulation parameters in a research setting, integrating elements from the cited protocols. [28] [29]
Transcutaneous auricular vagus nerve stimulation (taVNS) is an emerging, non-invasive neuromodulation technique that delivers electrical stimulation to the auricular branch of the vagus nerve (ABVN), offering a promising alternative to invasive vagus nerve implantation [36]. The therapeutic potential of taVNS is being investigated for a wide range of conditions, including epilepsy, depression, cognitive impairment, and inflammatory disorders [37] [38] [22]. A critical factor influencing the efficacy of taVNS is the precise anatomical location of stimulation on the external ear, as the density of vagal afferents varies significantly across different auricular regions [37] [39]. This application note synthesizes current evidence to evaluate the comparative efficacy of the cymba conchae against other auricular stimulation sites, providing researchers and clinicians with evidence-based protocols for optimal taVNS application.
Anatomical and Physiological Basis for Target Selection
The rationale for auricular stimulation hinges on the unique neuroanatomy of the external ear. The auricular branch of the vagus nerve (ABVN) innervates specific parts of the ear, with the cymba conchae recognized as being exclusively innervated by the ABVN [39]. Other regions, such as the tragus, ear canal, and cavum conchae, also receive ABVN innervation, though it may be shared with other nerves like the greater auricular nerve [37] [39]. In contrast, the earlobe is primarily innervated by cervical spinal nerves (e.g., the greater auricular nerve) and is generally considered to have minimal to no ABVN projections, making it a common control site for sham stimulation in clinical trials [39] [40].
Functional MRI studies provide direct evidence for the central effects of taVNS. Stimulation of the cymba conchae, compared to earlobe stimulation, produces significant activation of the ipsilateral nucleus of the solitary tract (NTS), the primary central relay for vagal afferents [39]. This activation subsequently engages widespread "classical" central vagal projections, including the bilateral spinal trigeminal nucleus, locus coeruleus, amygdala, and parabrachial area [39]. This distinct central activation pattern confirms that stimulation of the cymba conchae accesses the central vagus pathway via the ABVN.
Quantitative Comparison of Stimulation Sites
The efficacy of different auricular targets has been quantitatively assessed using measures such as Vagal Somatosensory Evoked Potentials (VSEP) and heart rate variability (HRV).
Evoked Potential and Amplitude Data
VSEP amplitude reflects the amount of synchronized electrical activity generated along the stimulated neural pathway. A comparative study evaluating different anatomical targets and electrode sizes found:
Table 1: VSEP Response and Sensory Threshold by Stimulation Site [37]
| Stimulation Site | Successful VSEP Obtained? | Amplitude Compared to Reference (CS) | Pain Threshold | Key Findings |
|---|---|---|---|---|
| Cymba & Cavum (CC) | Yes | Significant increase | Significant increase | Most effective topography; simultaneous stimulation recruits more fibers. |
| Cymba Conchae (C) | Yes | Used as reference (CS) | -- | Active target, validated in commercial devices. |
| Earlobe (L) | No | Not applicable | Significant increase (vs. CCS) | Inactive target; no valid VSEP recorded. |
The study concluded that the simultaneous stimulation of the cymba and cavum conchae with a large electrode is the most effective topography for taVNS, as it generates higher amplitude VSEPs, indicating greater synchronized neural recruitment [37].
Autonomic Response Data
The effects of different stimulation sites on autonomic nervous system activity, as measured by heart rate variability (HRV), show a more complex picture. A recent study investigating burst stimulation found that the specific HRV metric SDNN (a global marker of autonomic tone) showed notable changes when stimulation was applied to both the cymba conchae and the earlobe [41]. This suggests that under certain stimulation protocols, the earlobe—typically considered an inert control site—may evoke measurable autonomic responses, highlighting the need for further parameter optimization [41].
Experimental Protocols for Site Comparison
Protocol 1: fMRI Validation of Central Vagus Pathway Activation
This protocol verifies target engagement by measuring activation of the NTS and downstream vagal projections using fMRI [39].
- Objective: To ascertain whether electrical stimulation of the cymba conchae activates the NTS and central vagal projections compared to a control site (earlobe).
- Materials:
- MRI-safe taVNS stimulator (e.g., Cerbomed NEMOS).
- Titanium earpiece electrodes.
- Stimulation Parameters:
- Pulse Width: 0.25 ms.
- Frequency: 25 Hz.
- Current Intensity: Individually determined to a "tingling" sensation below pain threshold (e.g., 0.3–0.9 mA).
- Stimulation Type: Continuous monophasic square waves.
- Procedure:
- Participant Setup: Place participant in the MRI scanner. Fit the earpiece to the left cymba conchae for the experimental condition and to the left earlobe for the control condition.
- fMRI Acquisition: Acquire functional images using gradient-echo EPI sequences covering the whole brain, including the medulla oblongata.
- Experimental Paradigm:
- Scan 1 (Control): 2-min rest, 7-min left earlobe stimulation, 5-min rest.
- Scan 2 (Experimental): 2-min rest, 7-min left cymba conchae stimulation, 11-min rest.
- Data Analysis: Use FMRIB's Software Library (FSL) for preprocessing and statistical analysis. Perform region-of-interest (ROI) analysis on the brainstem and forebrain vagal projections.
Protocol 2: Laboratory Assessment of VSEP and Perceptual Threshold
This protocol is used to compare the electrophysiological response and comfort of different auricular sites in a laboratory setting [37] [40].
- Objective: To define the optimal auricular target by comparing VSEP latency, amplitude, and sensory/pain thresholds across sites.
- Materials:
- Constant current stimulator (max 5 mA output).
- Ag/AgCl electrodes (e.g., 5.2 x 10.4 mm for "large" size).
- Conductive paste (e.g., Ten20 conductive paste).
- EEG recording system with electrodes placed at F3 and C3 (10-20 system).
- Stimulation Parameters:
- Pulse Width: 250-500 μs.
- Frequency: 25 Hz.
- Current Intensity: Individually determined via Perceptual Threshold (PT) procedure.
- Procedure:
- Skin Preparation: Clean target sites (e.g., cymba conchae, cavum conchae, earlobe) with abrasive paste (e.g., Nuprep) to reduce impedance.
- Electrode Placement: Fix stimulation electrodes to the sites under investigation. Ensure electrode impedance is below 2 kΩ.
- Determine Perceptual Threshold (PT):
- Set stimulator to 3 mA. Deliver a 1-second train of stimulation.
- If participant feels a "tickling" or "pricking" sensation, decrease intensity by 50%. If not felt, increase by 50%.
- Repeat until recording a minimum of 4 "YES" responses, with the 4th "YES" following a "NO" response. The intensity at this 4th "YES" is the PT.
- Stimulation & Recording: Apply stimulation at the determined PT. Record VSEPs from the scalp electrodes.
- Data Analysis: Compare the latency and amplitude of VSEP components across the different stimulation sites.
Figure 1: Experimental workflow for comparing the efficacy of different taVNS stimulation sites, incorporating fMRI, VSEP, and HRV outcome measures.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials for taVNS Research
| Item | Function/Description | Example Products/Specifications |
|---|---|---|
| taVNS Stimulator | Delivers controlled electrical pulses. Must be constant current. | Soterix Medical taVNS stimulator [36], Cerbomed NEMOS [39]. |
| Stimulation Electrodes | Interface for current delivery to the skin. | Ag/AgCl electrodes [37]; RELIfit-Tragus, RELI-Stick, EASY-Clip electrodes [36]. |
| Conductive Medium | Ensures good electrical contact and reduces skin resistance. | Electrolyte gel, conductive paste [40]. |
| Skin Prep Supplies | Reduces skin impedance for consistent current delivery. | Alcohol prep pads (70% isopropyl), Nuprep abrasive paste [37] [40]. |
| Perceptual Threshold (PT) Protocol | Standardized method for individualizing stimulation intensity. | Step-up/step-down binary parametric search [40]. |
Safety and Tolerability Profile
taVNS is generally considered a safe and well-tolerated intervention. A systematic review and meta-analysis of 177 studies concluded that there was no causal relationship between taVNS and severe adverse events [34]. The most frequently reported adverse effects are mild and transient, including:
The meta-analysis found no difference in the risk of developing an adverse event between active taVNS and control stimulation (e.g., sham earlobe stimulation), reinforcing its safety profile for research applications [34].
The evidence consolidated in this application note strongly supports the cymba conchae as a primary and highly effective target for taVNS, based on its exclusive ABVN innervation, robust fMRI-verified activation of the NTS, and superior VSEP amplitude responses [37] [39]. The simultaneous stimulation of the cymba and cavum conchae may yield even greater neural recruitment [37]. Future research should focus on standardizing stimulation parameters, exploring inter-individual variability in neuroanatomy, and conducting large-scale, multicenter trials to confirm the therapeutic superiority of specific stimulation sites for various clinical conditions.
Transcutaneous auricular vagus nerve stimulation (taVNS) has emerged as a promising non-invasive neuromodulation therapy for a spectrum of neurological and psychiatric conditions. This application note synthesizes current evidence and provides detailed protocols for researchers investigating taVNS in four key indications: stroke rehabilitation, depression, post-traumatic stress disorder (PTSD), and cognitive disorders. The content is framed within the context of a broader thesis on taVNS protocol research, emphasizing standardized methodologies, mechanistic insights, and reproducible experimental designs for the scientific community.
taVNS Protocol Tables for Specific Indications
Table 1: Key Stimulation Parameters Across Indications
| Indication | Stimulation Site | Frequency (Hz) | Pulse Width (μs) | Intensity | Session Duration | Treatment Course | Key Outcomes |
|---|---|---|---|---|---|---|---|
| Stroke Rehabilitation | Cymba conchae (left/right/bilateral) [27] | 20-30 [27] | 300-500 [27] | 0.1-3 mA [27] | 30-90 min [27] [42] | 10 days to 6 weeks [27] | Improved limb motor function, enhanced gait/balance [27] |
| Depression | Cymba conchae, tragus [42] | 20-30 [43] [42] | 200-300 [43] | Individualized to just below pain threshold [44] | 30-90 min [42] | 7-14 days to repeated cycles [43] [42] | Reduced PHQ-9, BDI scores [43] |
| PTSD & Stress Regulation | Cymba conchae [44] | 30 [44] | 200 [44] | 1.74 ± 0.06 mA (individualized) [44] | Intermittent during stress tasks [44] | Single session to repeated cycles [44] | Prevented stress escalation, modulated frontal theta/alpha power [44] |
| Cognitive Enhancement | Cymba conchae [9] | 20-30 [9] [42] | 200-300 [9] | Not specified | During cognitive tasks [9] | Variable | Enhanced motor learning, increased GABAA-mediated inhibition [9] |
Table 2: Combination Therapies and Adjunct Protocols
| Indication | Combination Therapy | Stimulation Parameters | Experimental Findings |
|---|---|---|---|
| Stroke Motor Recovery | taVNS + Robotic Training [27] | 30 Hz, 0.1-0.5 mA, 0.3 ms pulse width, 3 weeks [27] | Significantly improved upper limb motor function compared to sham [27] |
| Stroke Motor Recovery | taVNS + Conventional Rehabilitation [27] | 30 Hz, 0.3 ms pulse width, 4 weeks [27] | Greater motor improvement versus control groups [27] |
| Cognitive Enhancement | taVNS + Visuomotor Task [9] | Standard parameters during task performance [9] | Improved motor learning and enhanced GABAA-mediated cortical inhibition [9] |
Experimental Protocols & Methodologies
Stroke Motor Rehabilitation Protocol
Study Design: Randomized, sham-controlled trial with parallel groups [27].
Participant Characteristics: Chronic stroke patients (>6 months post-stroke) with moderate to severe upper limb motor impairment [27].
Stimulation Protocol:
- Device: Commercial taVNS device with surface electrodes
- Electrode Placement: Left cymba conchae for unilateral stimulation [27]
- Stimulation Parameters:
- Session Structure:
- 30-minute sessions
- 3-5 sessions per week
- Total duration: 3-6 weeks [27]
- Sham Protocol: Identical electrode placement on earlobe with minimal current insufficient to activate vagal afferents [27] [44]
Combination Therapy: Synchronize taVNS with intensive upper limb robotic training or conventional occupational therapy, delivering stimulation during active movement attempts [27].
Outcome Measures:
- Primary: Fugl-Meyer Assessment for Upper Extremity (FMA-UE)
- Secondary: Box and Block Test, Grip Strength, EEG correlates of motor cortex activation [27]
Depression Protocol (Inpatient Setting)
Study Design: Open-label feasibility trial with randomized dosing regimens [43].
Participant Characteristics: Adults with comorbid depression and anxiety admitted to inpatient psychiatric unit [43].
Stimulation Protocol:
- Device: Portable taVNS device with two stimulation electrodes [43]
- Electrode Placement: Cymba conchae bilaterally [42]
- Stimulation Parameters:
- Dosing Regimens:
- Regimen A: Three daily sessions on three consecutive days (nine sessions total)
- Regimen B: Nine taVNS sessions in one day [43]
- Session Duration: 30-60 minutes per session [43] [42]
Outcome Measures:
- Primary: Patient Health Questionnaire (PHQ-9), Beck Depression Inventory (BDI)
- Secondary: Generalized Anxiety Disorder-7 (GAD-7), Beck Anxiety Inventory (BAI) [43]
- Timing: Assessments at baseline and post-treatment [43]
Stress and PTSD Protocol
Study Design: Randomized, sham-controlled, crossover design [44].
Participant Characteristics: Healthy individuals or patients with PTSD diagnosis [44].
Stress Induction:
- Mental Arithmetic Task: Repeated subtraction of single-digit numbers from three-digit numbers for 40 trials [44]
- 2-Back Task: Working memory task with 600 trials identifying number matches [44]
- Counterbalanced task order across participants [44]
Stimulation Protocol:
- Device: Portable taVNS device with two stimulation electrodes [44]
- Electrode Placement:
- Active: Cymba conchae
- Sham: Earlobe (devoid of vagus nerve innervation) [44]
- Stimulation Parameters:
- Washout Period: 1 week between crossover sessions [44]
Assessment Methods:
- Self-Report: Perceived stress levels before and after stimulation [44]
- EEG Recording: 3-minute resting-state EEG at baseline and post-task [44]
- EEG Analysis: Power spectral density in theta (4-7 Hz), alpha (8-13 Hz), and beta (14-30 Hz) bands; whole-brain network analysis with path length metrics [44]
Cognitive Enhancement Protocol
Study Design: Randomized, sham-controlled, within-subject design [9].
Participant Characteristics: Healthy adults, with consideration for sex as a biological variable [9].
Stimulation Protocol:
- Device: Commercial taVNS device
- Electrode Placement: Left cymba conchae [9]
- Stimulation Parameters:
- Stimulation Timing: During performance of visuomotor learning task [9]
Neurophysiological Assessment:
- TMS Measures:
- Corticospinal excitability (CSE)
- Short and long intracortical inhibition (SICI, LICI)
- Cortical silent period (cSP)
- Intracortical facilitation (ICF) [9]
- Timing: Baseline (pre-tVNS) and post-active/sham tVNS [9]
Behavioral Task:
- Computerized visuomotor task assessing motor learning [9]
- Performance measured across task blocks during stimulation [9]
Signaling Pathways and Mechanisms
Diagram 1: taVNS Neurophysiological Pathways. This diagram illustrates the primary neural mechanisms through which taVNS exerts its effects across multiple indications, including modulation of key brainstem nuclei, neurotransmitter systems, and downstream functional pathways.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Equipment
| Item | Specifications | Research Function | Example Applications |
|---|---|---|---|
| taVNS Device | Portable stimulator, adjustable parameters (frequency: 20-30 Hz, pulse width: 200-500 μs, intensity: 0.1-5 mA) [27] [44] | Delivers controlled electrical stimulation to auricular vagus nerve branches | All taVNS research applications [27] [44] [43] |
| Surface Electrodes | Small, conductive electrodes for auricular placement | Targets cymba conchae (active) or earlobe (sham) [44] | Precise stimulation of vagus nerve innervation zones [27] [44] |
| EEG System | High-density caps, compatible with stimulation devices | Records neural activity changes during/following stimulation | Investigating stress regulation [44], cognitive enhancement [9] |
| TMS Apparatus | Single- and paired-pulse capability with EMG recording | Measures cortical inhibition (SICI, LICI) and excitability | Assessing GABAergic mechanisms in cognitive studies [9] |
| Sham Stimulation Device | Identical appearance to active device, subthreshold current | Controls for placebo effects in clinical trials | All randomized controlled trial designs [27] [44] [9] |
| Behavioral Task Software | Standardized cognitive tasks (n-back, mental arithmetic, visuomotor learning) | Provides objective measures of cognitive function | Stress induction [44], motor learning [9], cognitive assessment |
| HRV Analysis System | ECG recording with spectral analysis capabilities | Quantifies vagally-mediated cardiac activity | Autonomic nervous system assessment [45] [46] |
Diagram 2: Research Workflow for taVNS Studies. This diagram outlines a standardized experimental workflow for taVNS research, encompassing participant screening, intervention protocols, and multi-modal assessment methodologies relevant to all indicated conditions.
Transcutaneous auricular vagus nerve stimulation (taVNS) has emerged as a pivotal non-invasive neuromodulation technique that interfaces strategically with both rehabilitative and pharmacological treatment paradigms. By targeting the auricular branch of the vagus nerve—the only peripherally accessible vagal branch—taVNS activates central neural pathways without the surgical implantation required for traditional vagus nerve stimulation [10]. This unique accessibility, combined with its favorable safety profile and patient compliance, positions taVNS as an ideal adjunctive therapy capable of enhancing outcomes across multiple therapeutic domains.
The scientific foundation for taVNS combination therapies rests on its multimodal mechanisms of action. taVNS modulates central pathways involved in neuroplasticity, exerts anti-inflammatory effects through the cholinergic anti-inflammatory pathway, regulates neurotransmitter systems, and promotes autonomic balance [42]. These diverse mechanisms create synergistic potential when combined with physical rehabilitation, which leverages activity-dependent neuroplasticity, and with pharmacotherapy, which targets specific biochemical pathways. For researchers and drug development professionals, understanding these integrative applications is crucial for designing next-generation therapeutic protocols that maximize functional recovery while potentially reducing medication dosages and associated side effects.
Clinical Applications and Efficacy Data
The therapeutic efficacy of taVNS as an adjunctive therapy has been investigated across numerous neurological, psychiatric, and even inflammatory conditions. The structured data in the tables below synthesize quantitative outcomes and protocol parameters from recent clinical studies to provide researchers with a comprehensive evidence base.
Table 1: Clinical Efficacy of taVNS Combination Therapies Across Disorders
| Condition | Study Design | Combination Therapy | Key Efficacy Metrics | Outcomes |
|---|---|---|---|---|
| Post-Stroke Motor Recovery [10] | Multiple RCTs (n=13 studies) | taVNS + Conventional Rehabilitation/Robotic Training | Upper limb function, cortical activation, ADL performance | Significantly greater motor improvement vs. control (sham + same rehabilitation) |
| Post-Stroke Depression [10] | Double-blind RCT (n=80) | taVNS + Conventional Treatment | HAMD-17, SDS, Barthel Index | Significant reductions in depression scores and improved function at 6-month follow-up |
| Chronic Insomnia Disorder [47] | Double-blind RCT (n=40) | taVNS Monotherapy | PSQI, ISI, Total Sleep Time | Significant improvements in PSQI (-4.5±3.55), ISI (-7.6±5.23), and sleep time (584±1015 min) |
| Erythematotelangiectatic Rosacea [48] | Randomized, sham-controlled (n=72) | taVNS Monotherapy | Clinician's Erythema Assessment | Significant reduction in facial erythema (CEA: 1.56 vs. 2.47 sham); improved anxiety, depression, sleep |
| Multiple Sclerosis (Non-motor) [38] | Randomized, sham-controlled (planned n=60) | taVNS Monotherapy | Symbol Digit Modalities Test | Protocol designed to evaluate cognitive processing speed improvement (study ongoing) |
Table 2: Stimulation Parameters for taVNS Combination Protocols
| Clinical Condition | Frequency | Pulse Width | Intensity | Session Duration | Treatment Course | Auricular Site |
|---|---|---|---|---|---|---|
| Post-Stroke Motor Recovery [10] | 20-30 Hz | 0.2-0.5 ms | 0.1-3 mA (individualized) | Varies with rehabilitation session | 2-6 weeks | Left cymba conchae |
| Chronic Insomnia [47] | 25-30 Hz | 200-500 μs | Tolerance threshold | 30 min daily | 6 weeks | Left auricle |
| Multiple Sclerosis Protocol [38] | 25 Hz | 250 μs | Tolerance threshold | 30 min | Single session (assessment) | Left auricle |
| General Protocol [42] | 20-30 Hz | 200-500 μs | Individualized to tolerance | 30-90 min | 7-14 days (intensive) or cyclical | Cymba conchae/tragus |
Experimental Protocols for Research Applications
Protocol 1: taVNS Combined with Upper Limb Motor Rehabilitation
This protocol is adapted from recent clinical trials investigating taVNS as an adjunct to motor rehabilitation for post-stroke recovery [10].
Primary Objective: To evaluate the synergistic effects of taVNS paired with upper limb constraint-induced movement therapy on motor function recovery in subacute stroke patients.
Study Population: Adults 18-80 years with unilateral ischemic or hemorrhagic stroke occurring 14 days to 6 months prior, with moderate upper extremity motor impairment (Fugl-Meyer Assessment score 20-50).
Materials and Equipment:
- taVNS device with adjustable parameters (frequency, pulse width, intensity)
- Bipolar stimulation electrodes for auricular placement
- Sham taVNS device for control group (identical appearance, minimal current)
- Standardized upper limb rehabilitation equipment
- Electromyography (EMG) recording system
- fMRI capability for subset of participants
Methodology:
- Randomization and Blinding: Participants are randomly assigned to active taVNS or sham groups using computer-generated randomization with allocation concealment. Participants, therapists, and outcome assessors are blinded to group assignment.
- Stimulation Parameters: Active taVNS: 25 Hz frequency, 300 μs pulse width, intensity set to just below discomfort threshold (typically 0.5-2.5 mA), applied to left cymba conchae. Sham: Identical electrode placement with minimal current (0.1 mA) insufficient for nerve activation.
- Combined Intervention: During 60-minute upper limb therapy sessions, taVNS is administered simultaneously with task-specific training. Stimulation is delivered in 30-second ON/30-second OFF cycles synchronized with movement initiation [10].
- Treatment Schedule: Sessions are conducted 5 days/week for 4 weeks, totaling 20 combined sessions.
- Outcome Assessments: Primary outcome: Upper Extremity Fugl-Meyer Score at baseline, post-intervention, and 3-month follow-up. Secondary outcomes: Action Research Arm Test, Grip Strength, Motor Activity Log, and fMRI cortical activation in a subset.
Data Analysis: Intention-to-treat analysis using mixed-effects models to account for repeated measures, with adjustment for baseline severity and time since stroke.
Protocol 2: taVNS Adjunct to Pharmacotherapy for Depression
This protocol evaluates the potential for taVNS to enhance pharmacological treatment outcomes in post-stroke depression, based on the clinical trial by Liu et al [10].
Primary Objective: To determine whether taVNS augments the antidepressant effects of standard pharmacotherapy and reduces required medication dosages.
Study Population: Adults with major depressive disorder developing within 6 months of confirmed stroke, with HAMD-17 score ≥18.
Materials and Equipment:
- FDA-cleared taVNS device for depression
- Validated depression rating scales (HAMD-17, SDS)
- Serum biomarker analysis capabilities (BDNF, CREB, inflammatory markers)
- Pharmacotherapy adherence monitoring system
Methodology:
- Study Design: Double-blind, randomized, sham-controlled trial with 2:1 allocation (active:sham).
- Stimulation Parameters: 25 Hz frequency, 300 μs pulse width, intensity titrated to sensory threshold without pain, applied to left cymba conchae.
- Combined Intervention: All participants receive standard antidepressant therapy (SSRI, dosage standardized per protocol) with either active taVNS or sham stimulation.
- Treatment Schedule: Participants self-administer taVNS twice daily (30 minutes per session) for 6 months, with clinical assessments monthly.
- Outcome Measures: Primary: Change in HAMD-17 at 3 months. Secondary: SDS scores, Barthel Index, serum BDNF/CREB levels, cytokine profiles, medication dosage requirements.
- Tapering Protocol: After 3 months, antidepressant dosage is systematically reduced in 25% increments every 2 weeks if HAMD-17 remains <8, to assess taVNS-mediated stabilization.
Data Analysis: Mixed model repeated measures analysis with primary endpoint at 3 months, including mediator analysis to examine biomarker relationships with clinical outcomes.
Mechanism of Action: Signaling Pathways and Neural Circuits
The therapeutic effects of taVNS in combination therapies are mediated through multiple interconnected neural and humoral pathways. The following diagram illustrates the key neurophysiological mechanisms through which taVNS exerts its effects when combined with rehabilitation or pharmacotherapy:
Diagram 1: Mechanism of taVNS in Combination Therapies. This diagram illustrates the key neurophysiological pathways through which taVNS interacts with rehabilitation and pharmacotherapy to produce therapeutic effects across multiple domains.
The application of taVNS initiates a cascade of neural events beginning with activation of the auricular branch of the vagus nerve, which projects to the nucleus tractus solitarius (NTS) in the brainstem [10] [42]. From this central relay station, multiple parallel pathways are engaged:
Neurotransmitter Modulation: The NTS projects to key neuromodulatory nuclei including the locus coeruleus (noradrenaline) and raphe nuclei (serotonin), increasing release of these neurotransmitters [42]. This mechanism creates synergy with pharmacological approaches that target these same systems, potentially allowing for lower medication doses while maintaining efficacy.
Neuroplasticity Enhancement: taVNS promotes brain-derived neurotrophic factor (BDNF) expression through activation of the CREB signaling pathway [10]. When combined with physical rehabilitation, this creates an optimal environment for activity-dependent plasticity, facilitating the reorganization of neural circuits underlying motor recovery.
Anti-Inflammatory Pathway: Through the cholinergic anti-inflammatory pathway, taVNS attenuates systemic inflammation via α7 nicotinic acetylcholine receptors on macrophages, reducing pro-inflammatory cytokines including TNF-α and IL-6 [42]. This mechanism is particularly relevant for inflammatory conditions like rosacea and potentially for reducing neuroinflammation in neurological disorders.
Autonomic Regulation: taVNS increases heart rate variability (HRV), reflecting improved parasympathetic tone and autonomic balance [42]. This effect contributes to its therapeutic benefits in insomnia, anxiety, and other stress-related conditions.
Cortical Network Modulation: Functional neuroimaging studies demonstrate that taVNS modulates the activity and connectivity of key brain networks including the default mode network (DMN), central executive network (CEN), and salience network (SN) [49]. This network-level regulation underlies improvements in conditions ranging from insomnia to depression.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers designing studies on taVNS combination therapies, the following table details critical reagents, equipment, and assessment tools with their specific applications in experimental protocols:
Table 3: Essential Research Materials for taVNS Combination Studies
| Category | Item | Specifications | Research Application |
|---|---|---|---|
| Stimulation Devices | taVNS Stimulator | Adjustable parameters (0.1-30 Hz, 100-500 μs), current output 0.1-5 mA | Precise delivery of vagus nerve stimulation with parameter control for different conditions |
| Sham Stimulator | Identical appearance/output display, minimal current (0.1 mA) | Blinded control condition ensuring participant/tester blinding | |
| Electrodes | Bipolar Auricular Electrodes | Sized for cymba conchae/tragus, hydrogel interface | Targeted stimulation of vagus nerve-rich auricular regions |
| Assessment Tools | fMRI Capability | 3T minimum, resting-state and task-based protocols | Mapping central effects, network connectivity changes (DMN, CEN, SN) |
| Polysomnography | Full overnight PSG with EEG, EOG, EMG, respiration | Objective sleep architecture analysis in insomnia trials | |
| Electromyography | Surface EMG with multi-channel capability | Quantifying motor evoked potentials, muscle activation patterns | |
| Heart Rate Variability | ECG-derived HRV analysis (time/frequency domain) | Measuring autonomic nervous system effects | |
| Biochemical Assays | ELISA Kits | BDNF, CREB, TNF-α, IL-6, norepinephrine metabolites | Quantifying molecular mechanisms, neurotrophic and inflammatory factors |
| Serum Collection System | Standardized blood collection, processing, storage | Biomarker analysis across multiple timepoints | |
| Clinical Rating Scales | HAMD-17 | 17-item Hamilton Depression Rating Scale | Gold-standard depression assessment |
| Fugl-Meyer Assessment | Comprehensive stroke recovery scale | Motor function evaluation in stroke trials | |
| Pittsburgh Sleep Quality Index | Subjective sleep quality assessment | Primary outcome measure in insomnia studies |
Future Directions and Research Considerations
The integration of taVNS with established therapeutic modalities represents a promising frontier in neuromodulation, but several methodological considerations require attention in future research. Parameter optimization remains challenging due to heterogeneity in stimulation protocols across studies [42]. Future trials should systematically compare different frequencies (20-30 Hz vs. 1-10 Hz), pulse widths (100-500 μs), stimulation durations (30-90 minutes), and treatment courses (short-intensive vs. prolonged-cyclical) to establish condition-specific optima.
The timing of taVNS application relative to adjunctive therapies deserves particular attention. For motor rehabilitation, evidence suggests that synchronizing taVNS pulses with movement attempts maximizes plasticity effects [10]. For pharmacological combinations, temporal considerations regarding medication pharmacokinetics and stimulation timing may influence synergistic effects.
Individual difference factors including vagus nerve anatomy, baseline autonomic function, genetic polymorphisms affecting neurotrophic response, and disease characteristics may all moderate taVNS efficacy. Future research should incorporate these potential moderators to develop personalized taVNS approaches.
Finally, the field would benefit from standardized reporting of taVNS parameters consistent with initiatives like the TMS methodological quality checklist, which would enhance reproducibility and meta-analytic synthesis across studies. As taVNS continues to evolve as an adjunctive therapy, these methodological refinements will be essential for establishing its evidence base and clinical translation.
Overcoming Challenges: Safety, Tolerability, and Parameter Optimization
Transcutaneous auricular vagus nerve stimulation (taVNS) has emerged as a prominent non-invasive neuromodulation tool with therapeutic potential across a spectrum of neurological, psychiatric, and inflammatory conditions. As research interest grows, a systematic understanding of its safety profile becomes paramount for researchers, scientists, and drug development professionals designing clinical trials and therapeutic protocols. This application note synthesizes current evidence from systematic reviews, meta-analyses, and pooled data analyses to provide a comprehensive safety profile analysis of taVNS, detailing the incidence and nature of adverse events (AEs). The content is framed within the context of a broader thesis on taVNS protocol research, emphasizing evidence-based methodologies for safety monitoring and reporting.
Quantitative Safety Profile of taVNS
Comprehensive analyses of clinical studies confirm that taVNS carries a favorable safety profile. A systematic review and meta-analysis evaluating 177 studies involving 6,322 subjects found no statistically significant difference in the risk of developing an adverse event between active taVNS and sham control groups [34]. The meta-analytic overall incidence rate for adverse events was calculated at 12.84 per 100,000 person-minutes-days of stimulation [34]. This low incidence rate, coupled with the absence of increased risk over sham stimulation, provides a robust quantitative foundation for the safety of taVNS in research and clinical applications.
A separate pooled analysis of 488 healthy participants further reinforced this safety profile, reporting generally minimal and mild side effects across participants, with a mean adverse effect intensity of 1.86 (SD = 1.36) on a standardized questionnaire [50]. The analysis concluded that participants receiving sham stimulation were 32.4% less likely to report unpleasant feelings compared to those receiving active taVNS; however, this effect was driven primarily by low-end ratings, suggesting limited clinical relevance [50].
Nature and Frequency of Specific Adverse Events
The adverse events associated with taVNS are typically mild and transient. The table below summarizes the most frequently reported adverse events based on large-scale systematic reviews and pooled analyses.
Table 1: Common Adverse Events Associated with taVNS
| Adverse Event | Reported Frequency & Characteristics | Primary Sources |
|---|---|---|
| Ear Pain | Among the most frequently reported AEs. | [34] [51] |
| Headache | Commonly reported; generally mild and transient. | [34] [50] [35] |
| Tingling / Paresthesia | Frequent, localized to the stimulation site. | [34] |
| Skin Irritation | Includes redness at the electrode site. | [50] [35] |
| Dizziness | Reported in a minority of participants. | [50] [35] |
| Neck Pain | Less frequent; may be linked to stimulation parameters. | [50] |
Other less frequently reported side effects include nausea, muscle contractions in the neck or face, concentration fluctuations, and mood changes [50] [35]. It is critical to note that a causal relationship between taVNS and serious adverse events (SAEs) has not been established. The 2018 systematic review by Redgrave et al. identified 30 serious adverse events across 7 studies but none were confirmed to be caused by transcutaneous VNS [35]. This finding is consistently supported by subsequent reviews [34] [51].
Experimental Protocols for Safety Monitoring
Standardized Adverse Event Assessment Methodology
To ensure consistent and comprehensive safety data collection across taVNS studies, implementing a standardized assessment protocol is essential. The following workflow outlines a recommended procedure based on methodologies from large pooled analyses and systematic reviews.
Diagram 1: Safety monitoring workflow.
Procedure:
- Pre-Stimulation Baseline Assessment: Prior to the first stimulation session, record the participant's baseline health status and any pre-existing symptoms. This is crucial for accurately attributing subsequent AEs [50].
- Administer Standardized AE Questionnaire: Immediately before stimulation begins, administer a validated questionnaire to establish a pre-stimulation baseline for common symptoms. The questionnaire should assess both physical and psychological symptoms [50]. An evidence-based template, adapted from Jacobs et al. (2015) and used in a large pooled analysis, should include items on:
- Headache
- Nausea
- Dizziness
- Neck Pain
- Muscle contractions in the neck/face
- Stinging sensations under the electrode
- Skin irritation at the ear
- Concentration fluctuations
- Mood changes
- Unpleasant feelings [50] Each item should be rated on a numerical scale (e.g., 1-5) or a Likert scale (e.g., "not at all" to "very much") to quantify intensity [50].
- Apply taVNS Protocol: Conduct the stimulation session according to the defined experimental or clinical protocol (Active or Sham).
- Immediate Post-Stimulation AE Assessment: Re-administer the AE questionnaire immediately following the cessation of stimulation to capture any acute effects.
- Monitor for Delayed AEs: Follow up with participants 24 to 48 hours after the stimulation session to identify any delayed or prolonged adverse events. This can be done via a brief structured phone call or electronic survey [34].
- Document All AE Reports: Meticulously record all reported events, including their intensity, duration, and the investigator's assessment of causality (e.g., definitely, probably, possibly, unlikely related to taVNS). This detailed documentation is vital for meta-analyses and systematic reviews [34] [35].
- Data Analysis & Reporting: Analyze the data to determine incidence rates and compare AE profiles between active and sham groups. All studies, regardless of the presence or absence of AEs, should explicitly state this in their publications to avoid reporting bias [34].
Protocol for Investigating Stimulation Parameter Effects on Safety
Understanding how stimulation parameters influence the incidence and severity of AEs is key to protocol optimization. The following methodology is derived from a pooled analysis that investigated these relationships [50].
Objective: To determine the effects of stimulation type (continuous vs. interval), intensity, and duration on the occurrence and severity of taVNS-related AEs.
Experimental Design:
- A between-subjects or within-subject (cross-over) design can be employed.
- Participants are randomized to receive different stimulation paradigms, varying one parameter at a time (e.g., fixed intensity and duration, but different stimulation types).
Stimulation Parameters:
- Stimulation Type: Compare continuous stimulation versus interval stimulation (e.g., 30s on/30s off). Evidence suggests that interval stimulation may reduce the likelihood of some side effects, particularly neck pain and dizziness [50].
- Stimulation Intensity: Test a range of intensities relative to individual sensory threshold (e.g., 0.5 mA, 1 mA, 2 mA, or as a percentage of the perceptual threshold). The pooled analysis by Burger et al. found that stimulation intensity showed few statistically significant, but clinically minimal, effects on AEs [50].
- Stimulation Duration: Compare various session durations (e.g., 10 min, 20 min, 30 min). A positive relationship between stimulation duration and the likelihood of side effects has been identified [50].
Data Analysis:
- Use a cumulative link mixed model (CLMM) to analyze the ordinal AE rating data.
- Include stimulation parameters (type, intensity, duration) as fixed effects and participant ID as a random effect to account for repeated measures.
- This statistical approach allows for the determination of which parameters significantly modulate AE profiles while controlling for inter-individual variability [50].
Signaling Pathways and Mechanisms of Adverse Events
The adverse events associated with taVNS can be understood through the neuroanatomical pathways involved. The following diagram illustrates the proposed mechanisms linking stimulation to common AEs.
Diagram 2: Proposed pathways for taVNS adverse events.
Pathway Explanation:
- Stimulation Site: taVNS is applied transcutaneously at the cymba conchae of the outer ear, a region exclusively innervated by the auricular branch of the vagus nerve (ABVN) [51] [50].
- Localized AEs (Ear Pain, Tingling, Skin Irritation): These most common AEs are primarily attributed to the stimulation of somatic afferent fibers within the ABVN itself or surrounding cutaneous nerves at the stimulation site [50]. The electrical current can cause localized responses, such as increased blood flow, sensitivity, and minor skin irritation under the electrode [50] [35].
- Central AEs (Headache, Dizziness): The afferent signals from the ABVN project to the Nucleus Tractus Solitarius (NTS) in the brainstem [51] [50]. The NTS has widespread projections, including to the Locus Coeruleus (LC), a key nucleus regulating autonomic functions like blood pressure and heart rate [50]. Activation of this NTS-LC pathway is hypothesized to underlie less frequent AEs such as headache and dizziness, potentially through disruptions in autonomic regulation [50]. This pathway is also the primary mechanism for the therapeutic effects of taVNS.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing taVNS safety and efficacy studies, the following table outlines essential materials and their functions.
Table 2: Key Research Materials for taVNS Studies
| Item | Function/Application in Research |
|---|---|
| CE-Marked or FDA-Cleared taVNS Device | Delivers controlled, low-level electrical stimulation to the auricular branch of the vagus nerve. Essential for ensuring consistent and reproducible stimulation parameters (e.g., NEMOS by Cerbomed) [35]. |
| Electrode Gel (Conductive) | Ensures optimal electrical conductivity between the stimulation electrode and the skin, minimizing skin resistance and the risk of irritation. |
| Standardized AE Questionnaire | Validated tool for systematic collection of safety data. Critical for quantifying the incidence and severity of AEs and enabling cross-study comparisons [34] [50]. |
| Sham Stimulation Device | Placebo control device that mimics the active stimulation (e.g., delivering very low-current or no current at an inactive site like the earlobe) without providing meaningful neuromodulation. Crucial for blinding and controlling for placebo effects in clinical trials [34] [50]. |
| Skin Inspection Protocol | A standardized checklist or rating scale for visually assessing and documenting skin condition (redness, irritation) at the electrode site before and after stimulation sessions [35]. |
Transcutaneous auricular vagus nerve stimulation (taVNS) is a non-invasive neuromodulation technique that influences central and autonomic nervous system activity by stimulating the auricular branch of the vagus nerve (ABVN) in the cymba conchae of the outer ear [27] [8]. Despite its promising therapeutic potential across various neurological, psychiatric, and cardiovascular conditions, the efficacy of taVNS remains inconsistent across studies, largely due to substantial variability in stimulation parameters [52] [8]. The lack of consensus regarding optimal stimulation protocols presents a significant challenge for both research and clinical translation.
This application note synthesizes current evidence on frequency-dependent effects of taVNS, providing structured parameter recommendations and detailed experimental protocols to guide research in this evolving field. By systematically evaluating parameter-efficacy relationships, we aim to establish a foundation for standardized, reproducible, and effective taVNS applications across different physiological systems and patient populations.
Parameter-Efficacy Relationships in taVNS
Quantitative Analysis of Frequency and Pulse Width Combinations
The therapeutic effects of taVNS are highly parameter-dependent. Systematic investigation of different frequency and pulse width combinations reveals distinct physiological effects, particularly on heart rate variability (HRV) and autonomic function.
Table 1: Efficacy of taVNS Parameters on Heart Rate Variability (HRV)
| Frequency | Pulse Width | Effect on SDNN | Effect on RMSSD | Time Course of Effects |
|---|---|---|---|---|
| 10 Hz | 250 µs | Significant increase vs. sham [52] | No significant change [52] | First 5 min of recovery period [52] |
| 10 Hz | 500 µs | Significant increase vs. sham [52] | No significant change [52] | Second 5 min of stimulation [52] |
| 25 Hz | 100 µs | Significant increase vs. sham [52] | No significant change [52] | First 5 min of recovery period [52] |
| 25 Hz | 250 µs | No significant change [52] | No significant change [52] | Not applicable |
| 25 Hz | 500 µs | No significant change [52] | No significant change [52] | Not applicable |
The data indicate that specific parameter combinations rather than isolated parameters determine efficacy. The 10 Hz/500 µs protocol produces effects during stimulation, while 10 Hz/250 µs and 25 Hz/100 µs protocols exhibit delayed effects during recovery, suggesting different mechanistic pathways and temporal dynamics [52].
Clinical Efficacy Parameters in Neurological Disorders
In clinical populations, particularly stroke survivors, parameter optimization demonstrates significant functional improvements when combined with rehabilitation.
Table 2: Clinically Effective taVNS Parameters in Stroke Rehabilitation
| Application | Effective Frequency | Effective Pulse Width | Stimulation Site | Key Outcome Measures |
|---|---|---|---|---|
| Upper Limb Motor Recovery | 20-30 Hz [27] [31] | 200-500 µs [27] | Left cymba conchae [27] | FMA-UE, ARAT, WMFT [31] |
| Gait and Balance | 25 Hz [27] | 300 µs [27] | Left ear | Balance scales, gait metrics [27] |
| Motor Recovery with Robotics | 20-30 Hz [27] | 300 µs [27] | Left cymba conchae [27] | Fugl-Meyer Assessment [27] |
| Sensory Recovery | 30 Hz [27] | 300 µs [27] | Left and right ears [27] | Sensory scales [27] |
The consistency of effective frequencies between 20-30 Hz across multiple stroke recovery studies suggests this range optimally engages neural networks involved in motor learning and plasticity when combined with task-specific training [27] [31].
Neurophysiological Mechanisms and Signaling Pathways
The efficacy of specific frequency parameters can be understood through the neurophysiological pathways engaged by taVNS. The following diagram illustrates the primary neural mechanisms through which different stimulation frequencies modulate autonomic and central nervous system functions:
Diagram 1: Neural Mechanisms of Frequency-Dependent taVNS Effects
This pathway illustrates how different frequency parameters engage distinct neural mechanisms: lower frequencies (∼10 Hz) preferentially influence autonomic cardiac control via the dorsal motor nucleus, while higher frequencies (20-30 Hz) enhance noradrenergic signaling via the locus coeruleus, supporting cognitive and motor functions [27] [8] [12].
Detailed Experimental Protocols
Protocol 1: Autonomic Function Assessment in Healthy Adults
This protocol details the methodology for investigating frequency-dependent effects on heart rate variability, based on studies demonstrating significant parameter-specific effects [52].
4.1.1 Participant Preparation and Setup
- Recruitment: Healthy adults aged 18+ with no neurological, psychiatric, or cardiovascular disorders
- Pre-session instructions: Participants refrain from intense exercise, alcohol, caffeine, and smoking for at least 12 hours before testing
- Positioning: Supine position in a quiet, dimly lit, temperature-controlled room (22-24°C)
- Electrode placement:
- Stimulation electrodes: Cymba conchae of left ear for active taVNS; earlobe for sham stimulation
- ECG electrodes: Standard lead II configuration for continuous recording
4.1.2 Stimulation Parameters and Randomization
- Session structure: Seven randomized sessions (six active parameter combinations + sham) with minimum 24-hour washout between sessions
- Active parameters:
- Frequencies: 10 Hz or 25 Hz
- Pulse widths: 100 µs, 250 µs, or 500 µs
- All combinations of the above (2×3 design)
- Sham condition: Identical electrode placement with no current delivery
- Stimulation timing: 15-minute baseline, 15-minute stimulation, 10-minute recovery
4.1.3 Data Collection and Analysis
- Primary outcomes: HRV metrics (SDNN, RMSSD) from ECG recordings
- Analysis approach: Segment data into 5-minute epochs for time-course analysis
- Statistical methods: Linear mixed-effects models to account for within-subject repeated measures
Protocol 2: Cognitive and Stress Response Testing
This protocol evaluates taVNS effects on cognitive performance under stress conditions, incorporating EEG measures to elucidate underlying neural mechanisms [53] [44].
4.2.1 Participant Selection and Setup
- Participants: Healthy volunteers with no neurological or psychiatric history
- Stimulation device: Portable taVNS device with two stimulation electrodes
- Electrode placement:
- Active: Cymba conchae
- Sham: Earlobe (devoid of vagus nerve innervation)
- Stimulation parameters:
- Frequency: 30 Hz
- Pulse width: 200 µs
- Duty cycle: 1-minute ON, 1-minute OFF
- Intensity: Individually calibrated to just below pain threshold (typically 1.5-2.0 mA)
4.2.2 Experimental Timeline and Tasks
- Baseline period: 3-minute resting-state EEG recording
- Stress induction:
- Mental Arithmetic Task: 40 trials of serial subtraction
- 2-Back Task: 600 trials of working memory assessment
- Stimulation timing: 15 minutes pre-task + continuous during task performance
- Post-task assessment: 3-minute resting-state EEG + subjective stress ratings (visual analog scale 1-10)
4.2.3 EEG Data Processing and Analysis
- Power spectral density: Analysis of theta (4-7 Hz), alpha (8-13 Hz), and beta (14-30 Hz) bands
- Network analysis: Graph theory metrics (path length, efficiency) in whole-brain networks
- Statistical comparison: Within-subject contrasts between active and sham conditions
Protocol 3: Motor Recovery in Stroke Patients
This protocol outlines parameters for clinical application of taVNS in post-stroke motor rehabilitation, based on evidence from randomized controlled trials [27] [31].
4.3.1 Patient Selection and Stimulation Setup
- Participants: Stroke patients >1 month post-onset with upper limb motor deficits
- Stimulation site: Left cymba conchae (or bilateral for sensory recovery)
- Stimulation parameters:
- Frequency: 25-30 Hz
- Pulse width: 200-500 µs
- Intensity: Comfortable sensation without pain (typically 1-5 mA)
4.3.2 Rehabilitation Protocol
- Stimulation timing:
- 30-second stimulation ON periods alternating with 30-second OFF periods
- Synchronized with high-intensity repetitive task practice
- Total session duration: 60-90 minutes
- Treatment schedule: 5 sessions/week for 4-6 weeks
- Combined therapy: Integration with conventional rehabilitation (physical therapy, occupational therapy) or robotic training
4.3.3 Outcome Assessment
- Primary motor outcomes: Fugl-Meyer Assessment Upper Extremity (FMA-UE), Action Research Arm Test (ARAT), Wolf Motor Function Test (WMFT)
- Functional outcomes: Modified Barthel Index (MBI) for activities of daily living
- Assessment timing: Baseline, post-intervention (4-6 weeks), and long-term follow-up (3-6 months)
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Equipment and Materials for taVNS Studies
| Item | Specification | Research Application |
|---|---|---|
| taVNS Stimulation Device | Programmable for frequency (1-30 Hz), pulse width (100-500 µs), intensity (0.1-10 mA), and duty cycles [52] [44] | Precise parameter control for mechanistic studies |
| ECG Recording System | High-resolution (≥1000 Hz sampling) with HRV analysis software [52] | Assessment of autonomic effects via SDNN, RMSSD metrics |
| EEG Recording System | 32+ channels with capability for resting-state and task-related recording [44] [12] | Investigation of cortical mechanisms via spectral power and network analysis |
| Sham Stimulation Electrodes | Identical appearance to active electrodes, placed on earlobe [53] [44] | Controlled placebo condition for blinding |
| Behavioral Task Software | Mental arithmetic, n-back, PASAT protocols with response recording [53] [44] | Standardized cognitive stress induction and assessment |
| Clinical Assessment Tools | FMA-UE, ARAT, WMFT, PSQI, ISI [31] [54] | Validated outcome measures for clinical efficacy |
Optimizing taVNS frequency parameters is essential for maximizing therapeutic efficacy across different applications. The evidence indicates that lower frequencies (∼10 Hz) with specific pulse widths (250-500 µs) preferentially modulate autonomic cardiac control, while higher frequencies (20-30 Hz) enhance motor recovery in stroke and cognitive performance under stress. These frequency-dependent effects engage distinct neural pathways, necessitating precise parameter selection based on target outcomes.
Future research should focus on individual factors influencing parameter efficacy, including disease state, baseline autonomic function, and genetic predispositions. The development of closed-loop taVNS systems that dynamically adjust parameters based on physiological feedback represents a promising direction for personalized neuromodulation. Standardization of reporting for stimulation parameters and outcome measures will facilitate meta-analyses and accelerate clinical translation of this promising non-invasive therapeutic approach.
Transcutaneous auricular vagus nerve stimulation (taVNS) is an emerging, non-invasive neuromodulation technique that has shown promise for treating a spectrum of neurological and psychiatric conditions. A critical consideration in taVNS research and therapeutic application is the substantial individual variability in treatment response. This variability is influenced by a complex interplay of factors, including the patient's specific disease state, demographic characteristics, and innate physiological differences. Ignoring these factors can lead to inconsistent research outcomes and suboptimal clinical efficacy. This application note provides a detailed framework for accounting for individual variability in taVNS protocol design, featuring structured data summaries, standardized experimental methodologies, and visual guides to inform researchers and drug development professionals.
The tables below synthesize quantitative data and key factors from the current literature that contribute to individual variability in taVNS outcomes.
Table 1: Influence of Specific Disease States on taVNS Application and Outcomes
| Disease State | Relevant Patient Population Characteristics | Reported Outcome Measures | Key Protocol Parameters (from studies) |
|---|---|---|---|
| Relapsing-Remitting Multiple Sclerosis | Diagnosis per McDonald criteria; presence of cognitive impairment, fatigue, depression [38]. | Symbol Digit Modalities Test (SDMT); Fatigue Scale for Motor and Cognitive Functions; Beck Depression Inventory-II [38]. | 30 min; tolerance threshold; 25 Hz; 250 μs pulse width; 30s on/30s off [38]. |
| Insomnia Disorder | Chronic (>3 months) or short-term (<3 months) insomnia; higher prevalence in females [55]. | Pittsburgh Sleep Quality Index (PSQI); Sleep Latency (SL); Sleep Efficiency (SE) [55]. | Varies; often targets cymba conchae or tragus [55]. |
| Major Depressive Disorder | Not specified in results; typically patients with treatment-resistant depression. | Beck Depression Inventory-II; other depression rating scales [38]. | Parameter sets optimized for antidepressant effects, often similar to epilepsy protocols [55]. |
| Epilepsy (Drug-Resistant) | Not specified in results; patients unsuitable for invasive VNS. | Seizure frequency reduction [55]. | Based on parameters from FDA-approved invasive VNS [55]. |
| Healthy Population (Cognitive Studies) | No neurological/psychiatric disorders; no medications affecting CNS; specific age ranges (e.g., 18-50) [38] [56]. | P300 Event-Related Potential (ERP) amplitude; salivary alpha-amylase; behavioral task performance (e.g., oddball) [56]. | 25 Hz; 200-300 μs pulse width; continuous or interval stimulation [56]. |
Table 2: Impact of Demographic and Physiological Factors on taVNS
| Factor | Consideration for Variability | Protocol Recommendations |
|---|---|---|
| Age | Neuroplasticity, autonomic tone, and skin conductance may vary with age. Studies often restrict age range (e.g., 18-50) [38] [40]. | Stratify recruitment by age; consider age as a covariate in analysis. |
| Sex/Gender | Prevalence of certain conditions (e.g., insomnia, MS) is higher in females; hormonal cycles may influence stimulation effects [55]. | Ensure balanced recruitment; record phase of menstrual cycle. |
| Disease Severity & Phenotype | Baseline disability (e.g., EDSS in MS) and specific symptom profiles (cognitive vs. fatigue) affect treatment capacity and targets [38]. | Use stratified randomization based on key disease features. |
| Anatomical Variation | Inter-individual differences in auricular vagus nerve innervation and branch distribution [55] [40]. | Use neuroimaging (fMRI) to verify target engagement; precise electrode placement per anatomical landmarks. |
| Autonomic & Neurophysiological Baseline | Pre-existing vagal tone (e.g., via heart rate variability) and cortical excitability state influence response [57]. | Measure baseline autonomic and neurophysiological metrics (e.g., TMS-based SAI, HRV) for use as covariates. |
Table 3: Safety Profile and Adverse Event Incidence of taVNS
| Adverse Event (AE) | Reported Incidence (per 100,000 person-minutes-days) | Typical Severity | Notes on Individual Predisposition |
|---|---|---|---|
| Ear Pain | Most frequently reported | Mild to Moderate | Correlated with stimulation intensity; higher in individuals with low perceptual threshold [34]. |
| Headache | Frequently reported | Mild | May be more common in individuals with a history of migraines (often an exclusion criterion) [34] [56]. |
| Tingling Sensation | Frequently reported | Mild | Expected side-effect at stimulation site; intensity is individually calibrated [40] [34]. |
| Skin Irritation/Redness | Common | Mild | Related to electrode material and conductive gel; more likely with prolonged use or sensitive skin [40] [34]. |
| Overall AE Incidence | 12.84 | Predominantly Mild | No causal relationship found between taVNS and serious adverse events; risk same as sham [34]. |
Detailed Experimental Protocols
Protocol for Individualized Stimulation Dosing
A core methodology for accounting for individual neuroanatomical and physiological differences is the determination of the Perceptual Threshold (PT).
Methodology:
- Materials: Constant current stimulator (max 5 mA), disinfected round metal electrodes (e.g., 8mm diameter), conductive gel, alcohol preparation pads [40].
- Electrode Placement: After cleaning the target site (e.g., tragus, cymba conchae) with alcohol, attach the anode to the inner ear canal (targeting the anterior wall) and the cathode to the outer tragus. For sham control, place the anode on the earlobe [40].
- PT Determination: Using a binary search algorithm:
- Set initial current to 3 mA with pulse width of 250-500 μs and frequency of 25 Hz. Deliver a 1-second train [40].
- Ask the subject if they felt a "tickle" or "pricking" sensation.
- If YES, decrease intensity by 50%. If NO, increase intensity by 50%.
- Repeat until the fourth "YES" response is recorded, which must be preceded by a "NO" response. The current at this fourth "YES" is the individual's PT [40].
- Stimulation Intensity: The final stimulation intensity is typically set as a multiple of the PT (e.g., just above PT but below pain threshold) or at a standardized level based on safety limits and protocol design.
Protocol for a Disease-Specific Clinical Trial (e.g., Multiple Sclerosis)
This protocol outlines a sham-controlled, single-blinded trial design for assessing taVNS effects on non-motor symptoms in RRMS [38].
Methodology:
- Participant Recruitment:
- Inclusion: Patients (PwRRMS) aged 18-50, diagnosed per McDonald criteria [38].
- Exclusion: History of seizure, mood, or cardiovascular disorders; metal implants/pacemakers; pregnancy; facial/ear trauma or pain [40] [56].
- Stratification: Consider stratifying by baseline cognitive performance (SDMT score) or fatigue levels.
- Baseline Assessment:
- Clinical: Expanded Disability Status Scale (EDSS).
- Cognitive: Symbol Digit Modalities Test (SDMT).
- Patient-Reported Outcomes: Fatigue Scale for Motor and Cognitive Functions (FSMC), Beck Depression Inventory-II (BDI-II) [38].
- Stimulation Protocol:
- Active taVNS: Stimulation at the cymba conchae. Parameters: 25 Hz frequency, 250 μs pulse width, 30s on/30s off duty cycle, 30-minute duration, intensity at individual tolerance threshold [38].
- Sham taVNS: Stimulation of the earlobe (minimal vagal innervation) using identical parameters, or electrodes at active site with no current [40].
- Post-Intervention Assessment: Repeat the SDMT and self-report questionnaires immediately after the stimulation session and at follow-up intervals.
- Safety Monitoring: Actively solicit and record adverse events using a standardized questionnaire at each session [34].
Signaling Pathways and Experimental Workflows
This diagram illustrates the proposed neural pathways of taVNS and key points where individual variability (red elements) influences the signal transduction and final outcomes. ABVN: Auricular Branch of the Vagus Nerve; PFC: Prefrontal Cortex; ACC: Anterior Cingulate Cortex; NA: Noradrenaline; ACh: Acetylcholine; 5-HT: Serotonin.
This workflow diagram outlines a robust experimental protocol that incorporates steps to account for individual variability at critical stages, from recruitment and stratification to data analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for taVNS Studies
| Item | Function/Application | Specifications & Considerations |
|---|---|---|
| Constant Current Stimulator | Delivers precise electrical pulses. Must be current-controlled for safety [40]. | Max output 5 mA; capable of delivering pulsatile stimulation (pulse width: 200-500 μs, frequency: 10-25 Hz) [40] [56]. |
| Stimulation Electrodes | Interface for transcutaneous electrical stimulation. | Round conductive metal (tin, Ag/AgCl, gold) or flexible carbon; 8mm diameter common. Require disinfection between uses [40]. |
| Conductive Gel/Paste | Ensures electrical conductance between electrode and skin, reducing impedance. | Use a thin, even layer; water-soluble gels are typical to prevent skin irritation [40]. |
| Perceptual Threshold (PT) Determination Software | Automates the binary search algorithm for individualizing stimulation intensity. | Can be custom-programmed (e.g., using PEST algorithm) to increase standardization and reduce experimenter bias [40]. |
| Sham Electrode Setups | Provides a credible control condition for blinding participants. | Earlobe electrode placement is a common sham site. Alternatively, use passive control (electrodes attached, no current) [40]. |
| Standardized Outcome Measures | Quantifies symptom changes and cognitive effects. | Cognitive: Symbol Digit Modalities Test (SDMT) [38]. Sleep: Pittsburgh Sleep Quality Index (PSQI) [55]. Neurophysiology: P300 ERP [56]. |
| Adverse Event Questionnaire | Systematically records safety and tolerability data. | Evidence-based checklist for taVNS (e.g., includes ear pain, headache, tingling, skin redness) to ensure consistent reporting [34]. |
Transcutaneous auricular vagus nerve stimulation (taVNS) has emerged as a promising non-invasive neuromodulation therapy with potential applications across neurological, psychiatric, and cardiovascular disorders. However, the field faces significant standardization hurdles that impede the comparison of results across studies, replication of findings, and clinical translation. The extensive methodological heterogeneity in current taVNS research manifests in variations across stimulation parameters, outcome measurement approaches, and safety reporting practices. This application note analyzes the core sources of methodological heterogeneity in taVNS research and provides structured protocols and recommendations to enhance standardization, with particular relevance for researchers, scientists, and drug development professionals working to establish validated taVNS interventions.
Quantitative Analysis of Methodological Heterogeneity
Diversity in Stimulation Parameters Across Studies
Table 1: Documented taVNS Parameter Variations in Contemporary Research
| Parameter Domain | Representative Values Documented | Study Contexts |
|---|---|---|
| Stimulation Frequency | 10 Hz, 25 Hz | HRV modulation in healthy adults [52] |
| Pulse Width | 100 µs, 250 µs, 500 µs | Systematic parameter investigation [52] |
| Session Duration | 4-second trains, 30-minute sessions | Cognitive & autonomic studies [38] [58] |
| Stimulation Site | Cymba conchae, tragus, earlobe (sham) | Multiple clinical protocols [38] [57] |
| Current Intensity | Individual tolerance threshold, sensory threshold | Motor cortex inhibition & autonomic studies [38] [52] |
Heterogeneity in Reported Adverse Events
Table 2: Safety and Tolerability Profile Based on Systematic Review
| Safety Aspect | Quantitative Findings | Reported Incidence |
|---|---|---|
| Overall AE Incidence | 12.84 per 100,000 person-minutes-days | Meta-analysis of 35 studies [34] |
| Most Common AEs | Ear pain, headache, tingling sensation | Most frequently reported [34] |
| Severe AEs | No causal relationship with taVNS established | Systematic review [34] |
| Reporting Completeness | 55.37% of studies did not mention AEs | Analysis of 177 studies [34] |
| Risk Difference | No significant difference vs. sham controls | Meta-analysis [34] |
Standardized Experimental Protocols
Protocol for Parameter Optimization Studies
Objective: To systematically evaluate the effects of different taVNS parameters on autonomic and cognitive outcomes in a controlled setting.
Materials:
- taVNS device with programmable parameters (frequency, pulse width, intensity)
- Electrocardiography (ECG) recording equipment
- Randomized protocol sequence software
- Subjective sensation assessment scales
Methodology:
- Participant Screening: Recruit healthy adults (18-50 years) with no neurological, psychiatric, or cardiovascular disorders [52].
- Study Design: Implement a single-blinded, sham-controlled, randomized cross-over design with minimum 24-hour washout between sessions [52].
- Stimulation Parameters: Test multiple combinations systematically:
- Frequencies: 10 Hz and 25 Hz
- Pulse widths: 100 µs, 250 µs, and 500 µs
- Current: Set to individual tolerance threshold [52]
- Session Structure:
- 15-minute baseline recording
- 15-minute active/sham stimulation
- 10-minute recovery phase recording [52]
- Primary Outcomes: Heart rate variability (SDNN, RMSSD), cognitive processing speed (Symbol Digit Modalities Test) [38] [52]
- Safety Monitoring: Document any adverse events systematically using a standardized questionnaire [34]
Protocol for Cognitive Enhancement Studies
Objective: To assess the effects of taVNS on cognitive domains including executive function, memory, and perceptual decision-making.
Materials:
- taVNS device capable of brief stimulation trains
- Cognitive testing apparatus (computerized tasks)
- Pupillometry equipment (optional)
- Transcranial magnetic stimulation (TMS) setup (optional)
Methodology:
- Participant Preparation: Instructions to refrain from intense exercise, alcohol, and caffeine on test days [52].
- Stimulation Protocol:
- Apply 4-second taVNS trains during task performance
- Use cymba conchae of left ear for active stimulation
- Earlobe stimulation for sham condition [58]
- Cognitive Tasks:
- Neurophysiological Measures:
- Data Analysis:
- Drift-diffusion modeling for evidence accumulation analysis [58]
- Pre-post stimulation comparisons of cortical inhibition
Figure 1: Standardized Experimental Workflow for taVNS Studies
Neural Mechanisms and Signaling Pathways
Understanding taVNS mechanisms is essential for protocol standardization. The stimulation activates distinct neural pathways that underlie its therapeutic effects:
Figure 2: Neural Pathways and Neurotransmitter Systems Activated by taVNS
The primary mechanism involves afferent vagal fibers projecting to the nucleus tractus solitarius (NTS), which subsequently activates the locus coeruleus (LC), the primary source of norepinephrine (NE) in the brain [59]. This LC-NE activation enhances cognitive functions through multiple pathways:
- Evidence Accumulation: Increased drift rates in perceptual decision-making [58]
- Cortical Inhibition: Enhanced GABAergic neurotransmission, particularly GABA-A mediated inhibition [9]
- Autonomic Regulation: Modulation of heart rate variability through brainstem pathways [52]
Notably, taVNS does not appear to influence cholinergic circuits measured by short-latency afferent inhibition (SAI), suggesting selective neurotransmitter engagement [57].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Equipment for Standardized taVNS Research
| Category | Specific Item | Research Function | Protocol Considerations |
|---|---|---|---|
| Stimulation Device | Programmable taVNS device | Deliver precise electrical stimulation | Capable of 10-25 Hz frequency, 100-500 µs pulse width [52] |
| Electrode Configurations | Cymba conchae electrodes | Target auricular vagus nerve branches | Ensure consistent placement across sessions [38] |
| Physiological Monitoring | ECG recording system | Measure heart rate variability outcomes | Standardize recording conditions (posture, time) [52] |
| Cognitive Assessment | Symbol Digit Modalities Test | Assess cognitive processing speed | Primary outcome for MS trials [38] |
| Neurophysiology | TMS with paired-pulse protocols | Measure GABAergic inhibition (SICI, LICI) | Probe neurotransmitter mechanisms [9] |
| Safety Documentation | Standardized AE questionnaire | Systematic adverse event monitoring | Enable cross-study safety comparisons [34] |
Minimum Reporting Standards for taVNS Research
Based on analysis of methodological heterogeneity and consensus recommendations, the following minimum reporting standards should be implemented in all taVNS research publications:
Stimulation Parameter Documentation
- Complete parameter specification: Frequency, pulse width, current intensity, session duration, and electrode placement must be explicitly documented [52] [60]
- Device characteristics: Manufacturer and model should be specified, along with any custom modifications [60]
- Sham protocol details: Comprehensive description of sham control methods, including placement site and parameter differences [38] [57]
Participant Characterization
- Inclusion/exclusion criteria: Specific details regarding neurological, psychiatric, and cardiovascular health status [52]
- Sensory threshold assessment: Method for determining individual stimulation intensity [38]
- Blinding assessment: Report participant blinding success rates where feasible [60]
Outcome Measures and Safety
- Primary outcome justification: Clear rationale for selected primary endpoints [38]
- Multiple domain assessment: Include cognitive, autonomic, and safety outcomes in comprehensive trials [38] [52]
- Adverse event reporting: Systematic documentation using standardized questionnaires regardless of severity [34]
Addressing the standardization hurdles in taVNS research requires concerted effort across multiple domains of methodology and reporting. The protocols and guidelines presented here provide a framework for reducing methodological heterogeneity, enhancing reproducibility, and accelerating the clinical translation of taVNS interventions. Future work should focus on validating these standardized approaches across diverse patient populations and establishing consensus-based guidelines through professional society endorsements. For drug development professionals, these standardized protocols enable more reliable assessment of taVNS as either stand-alone or adjunctive therapies in neurological and psychiatric disorders.
Evidence and Efficacy: Validating Outcomes and Comparative Analyses
Transcutaneous auricular vagus nerve stimulation (taVNS) is a non-invasive neuromodulation technique that stimulates the auricular branch of the vagus nerve in the ear. By modulating central nervous system activity, taVNS offers promising therapeutic potential for various neurological and psychiatric conditions [61]. This document synthesizes current clinical trial evidence, focusing on meta-analyses and randomized controlled trials (RCTs) investigating taVNS efficacy, and provides detailed experimental protocols for research applications.
Therapeutic Applications & Clinical Evidence
taVNS research has expanded to encompass several therapeutic areas, with varying levels of evidence supporting its application across different disorders. Table 1 summarizes key findings from recent clinical studies and meta-analyses.
Table 1: Clinical Evidence for taVNS from Meta-Analyses and Randomized Controlled Trials
| Therapeutic Area | Reported Efficacy | Key Outcome Measures | Level of Evidence |
|---|---|---|---|
| Cognitive Flexibility | Significant improvement in task-switching under high complexity [62] [63] | Reduced switch cost in Dimensional Change Card Sorting (DCCS) task [62] | Multiple RCTs |
| Processing Speed (RRMS) | Under investigation; primary results pending [3] | Symbol Digit Modalities Test (SDMT) [3] | Registered RCT Protocol |
| Tinnitus | Inconclusive; conflicting results between studies [64] | Tinnitus Handicap Inventory (THI), Tinnitus Functional Index (TFI) [64] | Systematic Review & Meta-Analysis |
| Depression (MDD) | Reduced symptom severity in adults [61] | Hamilton Depression Rating Scale (HDRS), Beck Depression Inventory-II (BDI-II) [3] [61] | RCTs & Clinical Applications |
Detailed Experimental Protocols
Protocol for Investigating Cognitive Processing Speed in RRMS
This protocol is adapted from an ongoing, single-centre, sham-controlled, single-blinded trial [3].
- Study Population: 30 patients with Relapsing-Remitting Multiple Sclerosis (RRMS) diagnosed per McDonald criteria (2017) and 30 healthy controls, aged 18-50 years.
- Stimulation Parameters:
- Device: taVNS stimulator.
- Location: Auricular branch area of the vagus nerve in the ear.
- Duration: 30 minutes.
- Frequency: 25 Hz.
- Pulse Width: 250 μs.
- Duty Cycle: 30 seconds on, 30 seconds off.
- Intensity: Set to individual tolerance threshold.
- Sham Protocol: Stimulation applied to the earlobe, which has minimal vagal innervation [3].
- Primary Outcome Assessment:
- Tool: Symbol Digit Modalities Test (SDMT).
- Timing: Baseline and post-intervention assessment.
- Procedure: Participants are given 90 seconds to pair abstract symbols with specific numbers as quickly as possible. The total number of correct matches is the primary score [3].
- Secondary Outcome Assessments:
Protocol for Investigating Cognitive Flexibility
This protocol is based on an RCT using a within-subject design to evaluate cognitive flexibility under different task complexity levels [62].
- Study Population: 24 healthy adults, right-handed, with normal or corrected-to-normal vision.
- Stimulation Parameters:
- Device: taVNS stimulator.
- Duration: Applied throughout task performance.
- Sham Protocol: Sham stimulation using identical apparatus.
- Cognitive Task & Workflow:
- Tool: Dimensional Change Card Sorting (DCCS) task combined with a secondary auditory task.
- Procedure: The DCCS task requires participants to switch sorting rules (e.g., color vs. shape) every two trials. This is performed concurrently with an auditory task of varying difficulty (low, medium, high) to consume cognitive resources.
- Primary Metric: Switch Cost, calculated as the difference in reaction time or accuracy between switch trials and repeat trials [62].
The following diagram illustrates the experimental workflow and the neural pathways activated by taVNS during this protocol.
Signaling Pathways and Mechanisms of Action
taVNS exerts its effects through well-defined neuroanatomical pathways. The electrical stimulation targets the auricular branch of the vagus nerve, initiating a cascade of neural and neurochemical events [3] [61].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2 catalogues critical materials and tools required for conducting taVNS research, as derived from the cited protocols.
Table 2: Essential Research Reagents and Materials for taVNS Protocols
| Item Name | Function/Application | Specifications/Examples |
|---|---|---|
| taVNS Stimulation Device | Delivers controlled electrical stimulation to the auricular vagus nerve. | Programmable for frequency (e.g., 25Hz), pulse width (e.g., 250μs), and intensity; includes electrodes for auricular placement [3]. |
| Sham Stimulation Electrode | Serves as an active control by stimulating a non-vagal innervated site. | Typically placed on the earlobe; device should be identical in appearance to active taVNS device to maintain blinding [3]. |
| Symbol Digit Modalities Test (SDMT) | Assesses cognitive processing speed. | Paper-based or computerized; includes a key of paired symbols/numbers and test forms [3]. |
| Dimensional Change Card Sorting (DCCS) Task | Measures cognitive flexibility and task-switching ability. | Computer-administered; software programmed to switch sorting rules (e.g., color, shape) and record reaction time/accuracy [62]. |
| Beck Depression Inventory-II (BDI-II) | Quantifies severity of depressive symptoms. | 21-item self-report questionnaire; requires licensed manual and scoring sheets [3]. |
| Fatigue Scale for Motor and Cognitive Functions (FSMC) | Differentiates between motor and cognitive fatigue. | 20-item self-report questionnaire; provides separate sub-scores for motor and cognitive fatigue [3]. |
Transcutaneous Auricular Vagus Nerve Stimulation (taVNS) has emerged as a pivotal non-invasive neuromodulation technique, attracting significant interest for its therapeutic potential across a spectrum of neurological disorders. This application note provides a systematic comparison of taVNS against traditional invasive Vagus Nerve Stimulation (i-VNS) and other neuromodulatory methods, focusing on efficacy, safety, protocol standardization, and mechanistic insights. Framed within a broader thesis on taVNS protocol research, this document synthesizes current evidence to guide researchers, scientists, and drug development professionals in optimizing stimulation parameters and designing robust clinical trials. The non-invasive nature of taVNS, which selectively stimulates the auricular branch of the vagus nerve located in the ear, presents a compelling alternative to invasive modalities, potentially offering enhanced patient compliance, reduced procedural risks, and broader application accessibility [27] [65].
Comparative Efficacy and Safety Profiles
Quantitative Efficacy Across Indications
Table 1: Comparative Efficacy of Neuromodulation Techniques in Epilepsy
| Technique | Study Design | Population | Primary Efficacy Endpoint | Result | Citation |
|---|---|---|---|---|---|
| taVNS | RCT, n=150 | Drug-Resistant Epilepsy | Responder Rate (≥50% seizure reduction) | Significantly higher in active vs. control group at 20 weeks | [65] |
| Invasive VNS (i-VNS) | Literature Review | Drug-Resistant Epilepsy | Responder Rate | ~40-60% | [65] |
| Deep Brain Stimulation (DBS) | Systematic Review & NMA | Drug-Resistant Epilepsy | Seizure Frequency Reduction | Varied; network meta-analysis ranks efficacy | [66] |
Table 2: Efficacy in Motor Recovery Post-Stroke
| Technique | Adjunct Therapy | Stimulation Parameters | Key Motor Outcome | Citation |
|---|---|---|---|---|
| taVNS | Conventional Rehabilitation | 20-30 Hz, 0.3-0.5 ms pulse width, 4-6 weeks | Significantly improved upper limb motor function (FMA-UE) | [27] [67] |
| taVNS | Robotic Training | 20-30 Hz, 0.3 ms pulse width, 3-10 days | Improved antagonistic motor function | [27] |
| Invasive VNS | Task-Specific Rehabilitation | 0.8 mA, 100 µs, 30 Hz, 500 ms bursts (preclinical) | Enhanced forelimb motor recovery in rat models | [67] |
Table 3: Safety and Adverse Event Profile
| Technique | Common Adverse Events (AEs) | Serious Adverse Events (SAEs) | Incidence Note | Citation |
|---|---|---|---|---|
| taVNS | Ear pain, headache, tingling, skin irritation (minimal and transient) | No causal relationship to severe AEs | Overall AE incidence: ~12.84/100,000 person-minutes-days | [34] |
| Invasive VNS (i-VNS) | Hoarseness, cough, dysphagia, pain (post-surgical) | Surgical risks, infection, device malfunction, cardiac arrhythmia (e.g., bradycardia ~1/1000) | Related to surgery and efferent nerve stimulation | [65] [34] |
| DBS | Hardware-related complications, infection, intracranial hemorrhage | Surgery-related risks (e.g., stroke) | Invasive surgical procedure required | [68] |
The comparative analysis reveals a distinct efficacy-safety trade-off. For epilepsy, taVNS demonstrates a clinically significant responder rate, positioning it as an effective non-invasive alternative, particularly for patients unsuitable for surgery [65]. In post-stroke motor rehabilitation, taVNS paired with task-specific training consistently enhances upper limb recovery, with effect sizes comparable to those observed in preclinical models of invasive VNS [27] [67]. The superior safety profile of taVNS is its most defining advantage. A systematic review of 177 studies concluded that taVNS is not associated with an increased risk of adverse events compared to sham controls and has no causal link to serious adverse events [34]. In contrast, i-VNS carries inherent surgical risks and can stimulate efferent fibers leading to side effects like hoarseness, cough, and, in rare instances, cardiac arrhythmia [65] [34].
Key Signaling Pathways and Experimental Workflow
The therapeutic mechanisms of taVNS are mediated through a well-defined neuroanatomical pathway. The following diagram illustrates the central "bottom-up" signaling pathway and a standardized experimental workflow for a clinical trial.
Detailed Experimental Protocols
Protocol 1: taVNS for Drug-Resistant Epilepsy
This protocol is adapted from a randomized, double-blinded, controlled trial involving 150 patients [65].
- 1. Objective: To evaluate the superiority of add-on taVNS therapy over sham control in reducing seizure frequency in patients with drug-resistant epilepsy.
- 2. Population:
- Inclusion: Adults (18-65 years) diagnosed with epilepsy per ILAE definition, taking ≥2 ASMs for ≥2 years with ineffective control (average seizure frequency ≥4/month in the past year), and deemed unsuitable for or unwilling to undergo surgery.
- Exclusion: Status epilepticus in the past year; progressive brain diseases; serious cardiac, hepatic, or renal impairment; pregnancy; implanted cardiac pacemaker or vagus nerve stimulator.
- 3. Device & Stimulation Parameters:
- Device: Certified taVNS device (e.g., TVNS-100).
- Electrode Placement: Bipolar electrode attached to the left cymba conchae.
- Active Stimulation: Frequency = 25 Hz, Pulse Width = 250 µs, Cycle = 30 seconds on/30 seconds off.
- Dosage: 2 hours per day, divided into 4 periods of 30 minutes.
- Intensity: Maintained at the maximum tolerated intensity that causes perceptible pain but not discomfort.
- Sham Stimulation: Frequency = 1 Hz, Intensity = minimum perceptible tingling, with identical electrode placement and session duration to ensure effective blinding.
- 4. Study Design & Timeline:
- Total Duration: 28 weeks per patient.
- Baseline Period (8 weeks): Record baseline seizure frequency in a patient diary. Assess demographic information, QOL (QOLIE-31), mood (HAMA, HAMD), and cognition (MoCA).
- Treatment Period (20 weeks): Patients randomized to active (n=100) or control (n=50) groups. ASM regimens remain unchanged.
- Assessment Visits: At 4, 12, and 20 weeks during treatment. Seizure diaries are reviewed, and AEs are recorded.
- End-of-Study Assessment (Week 20): Repeat QOL, mood, and cognitive scales.
- 5. Primary Outcome: Responder rate at 20 weeks (percentage of patients with ≥50% reduction in mean seizure frequency from baseline).
- 6. Secondary Outcomes: Reduction in seizure frequency at each visit; changes in QOLIE-31, HAMA, HAMD, MINI suicide scale, and MoCA scores.
- 7. Safety Monitoring: Non-severe and severe AEs are reported by patients. Vital signs, physical examination, and 12-lead ECG are performed at visits.
Protocol 2: taVNS for Post-Stroke Motor Recovery
This protocol synthesizes methodologies from multiple RCTs and a scoping review on post-stroke arm motor recovery [27] [67].
- 1. Objective: To determine the efficacy of taVNS paired with upper limb rehabilitation in improving arm motor function in chronic stroke patients.
- 2. Population:
- Inclusion: Adult patients (>6 months post-ischemic or hemorrhagic stroke) with moderate arm motor impairment (e.g., Fugl-Meyer Assessment for Upper Extremity (FMA-UE) score between 20-50).
- Exclusion: Uncontrolled cardiac arrhythmia, significant cognitive impairment, other neurological conditions, pregnant women.
- 3. Device & Stimulation Parameters:
- Device: Portable taVNS device.
- Electrode Placement: Left auricular cymba conchae.
- Stimulation Parameters: Frequency = 25-30 Hz, Pulse Width = 300-500 µs.
- Dosage: Stimulation is delivered in brief bursts (e.g., 500 ms bursts, 0.8 mA) synchronized with goal-directed movements during therapy sessions.
- Session Duration: 30-90 minutes per session, 3-5 times per week for 4-6 weeks.
- 4. Study Design:
- Design: Randomized, sham-controlled, double-blind trial.
- Intervention Group: Active taVNS + Conventional/Robotic Upper Limb Rehabilitation.
- Control Group: Sham taVNS (identical device setup, minimal or no output) + Identical Rehabilitation.
- 5. Primary Outcome: Change in FMA-UE score from baseline to post-intervention (4-6 weeks) and at a long-term follow-up (e.g., 3 months).
- 6. Secondary Outcomes:
- Motor Function: Wolf Motor Function Test (WMFT) time and functional ability scores.
- Activities of Daily Living: Action Research Arm Test (ARAT), Box and Block Test.
- Neurophysiological Measures: Resting-state EEG to monitor changes in delta/theta power [12], fMRI for functional connectivity.
- 7. Safety Monitoring: Participants are specifically questioned about ear pain, headache, tingling, dizziness, and skin irritation at the electrode site after each session [34].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for taVNS Investigations
| Item Category | Specific Example / Function | Critical Research Application |
|---|---|---|
| Certified taVNS Device | TVNS-100; portable stimulator with ear electrodes. | Core intervention delivery; ensures consistent, reproducible stimulation parameters (frequency, pulse width) across subjects [65]. |
| Sham Stimulation Device | Identical device with 1 Hz frequency and sub-perception intensity. | Serves as an active control in RCTs; critical for blinding participants and investigators to isolate the specific effects of taVNS from placebo [65]. |
| Electrode Conductive Gel | Standard ECG or EEG gel. | Ensures optimal skin contact and current delivery at the cymba conchae; minimizes skin impedance and risk of irritation [34]. |
| Validated Clinical Scales | FMA-UE (motor), PSQI/ISI (sleep), HAMA/HAMD (mood), QOLIE-31 (quality of life). | Quantifies primary and secondary therapeutic outcomes; standardizes measurement across research sites for meta-analyses [27] [65] [54]. |
| Neurophysiology Platform | High-density EEG system (e.g., 64-channel). | Mechanistic biomarker analysis; measures taVNS-induced cortical activity changes (e.g., increased frontal delta power) [12]. |
| Adverse Event Questionnaire | Structured taVNS-specific AE form (e.g., listing ear pain, headache, tingling). | Systematic safety monitoring; allows for meta-analytic calculation of AE incidence rates and ensures patient safety [34]. |
This application note delineates the position of taVNS as a safe, feasible, and effective neuromodulation technique with distinct advantages over its invasive counterpart, particularly regarding its safety profile and accessibility. However, several challenges remain. Future research must focus on the large-scale validation of optimized stimulation parameters (intensity, frequency, dosing), the identification of predictive biomarkers of treatment response (e.g., via EEG [12]), and the execution of rigorous, multi-center trials in diverse patient populations. Furthermore, exploring the synergistic effects of taVNS with other rehabilitative strategies and pharmacotherapies will be crucial for unlocking its full therapeutic potential and solidifying its role in clinical practice and drug development pipelines.
This application note provides a structured framework for validating Heart Rate Variability (HRV), functional Magnetic Resonance Imaging (fMRI), and Electroencephalography (EEG) as objective, multimodal biomarkers to quantify the physiological and neural impact of transcutaneous auricular vagus nerve stimulation (taVNS). Robust biomarker validation is critical for substantiating target engagement and treatment efficacy in taVNS clinical trials and research protocols. The guidelines herein detail specific methodologies, data analysis techniques, and integrative approaches necessary to establish these measures as reliable indicators of taVNS-induced neurophysiological changes, thereby supporting the development of standardized, evidence-based taVNS applications.
Quantitative Biomarker Responses to Vagus Nerve Stimulation
The following tables synthesize key quantitative findings from recent studies on vagus nerve stimulation, providing a reference for expected effect sizes and outcomes.
Table 1: Biomarker Responses to Cervical and Auricular taVNS
| Stimulation Type | Biomarker | Key Findings | Effect Size/Statistical Significance | Citation |
|---|---|---|---|---|
| tcVNS (Cervical) | Auditory Performance (Gap discrimination) | 37% average improvement in performance relative to sham | p = 0.00052 | [69] |
| tcVNS (Cervical) | Visual Performance (Letter acuity) | 23% average improvement in performance relative to sham | p = 0.038 | [69] |
| tcVNS (Cervical) | Heart Rate Variability (HRV) | Increased HRV during passive viewing | p-values reported (statistically significant) | [69] |
| taVNS (Auricular) | GABAergic Cortical Inhibition (SICI) | Specific increase in GABAA-mediated inhibition, particularly in females | Significant effect of active vs. sham tVNS | [9] |
| taVNS (Auricular) | Visuomotor Learning | Improved performance across task blocks during active stimulation | Significant effect of active vs. sham tVNS | [9] |
Table 2: Diagnostic Accuracy of HRV in Mild Neurocognitive Disorder (mNCD)
| vm-HRV Parameter | Area Under Curve (AUC) | Sensitivity & Specificity | Conclusion for Screening | [70] |
|---|---|---|---|---|
| Relative Power of High Frequency (HF) | 0.68 (95% CI: 0.56, 0.81) | Calculated based on Youden's Index | Greatest AUC among parameters, but insufficient for reliable screening alone. | [70] |
| Other vm-HRV Parameters | AUC range: 0.53 - 0.61 | Not specified | Poor to moderate diagnostic accuracy. | [70] |
Detailed Experimental Protocols
This section outlines standardized protocols for acquiring and analyzing HRV, fMRI, and EEG data within taVNS research paradigms.
Protocol for HRV Acquisition and Analysis
HRV serves as a non-invasive index of vagally-mediated parasympathetic tone and is a key indicator of taVNS target engagement [71].
- Equipment Setup: Utilize a 3-lead electrocardiogram (ECG) system. A wireless, wearable sensor is acceptable if validated for clinical-grade ECG acquisition [70]. Ensure electrodes are placed for a clear R-wave signal.
- Data Acquisition:
- Conduct recordings in a quiet, temperature-controlled room.
- Participants should be in a supine or seated resting position for at least 5 minutes prior to baseline recording to stabilize heart rate.
- Record a 5-minute resting baseline followed by simultaneous recording during the entire taVNS/sham stimulation period, as per the study design in taVNS trials [71].
- Sampling rate should be ≥ 500 Hz to ensure accurate R-peak detection.
- Signal Processing & Feature Extraction:
- R-Peak Detection: Use automated algorithms with manual verification to identify R-waves and generate a series of R-R intervals (RRI).
- Artifact Removal: Apply predefined thresholds (e.g., remove RRIs differing by >20% from the previous interval) and interpolate using spline or linear methods.
- Time-Domain Analysis: Calculate rMSSD (root mean square of successive differences) and pNN50 (percentage of successive RRIs differing by >50 ms), which reflect parasympathetic activity [72].
- Frequency-Domain Analysis: Perform Fast Fourier Transform (FFT) on the RRI series. Extract High-Frequency (HF; 0.15-0.40 Hz) power, a pure marker of parasympathetic activity, and Low-Frequency (LF; 0.04-0.15 Hz) power. The LF/HF ratio is often interpreted as a marker of sympathovagal balance [72].
Protocol for fMRI Acquisition and Analysis in taVNS Studies
fMRI provides high-resolution spatial mapping of taVNS-induced brain activity and functional network changes.
- Equipment and Setup: A 3.0 Tesla MRI scanner with a standard head coil is recommended. Use simultaneous EEG-fMRI if studying epileptogenic networks, though this requires specialized equipment [73].
- Data Acquisition Parameters:
- T1-weighted anatomical scan: Use an FSPGR or MPRAGE sequence for high-resolution structural images (e.g., 1x1x1 mm³ voxels).
- Resting-state fMRI (rs-fMRI): Use a T2*-weighted gradient-echo echo-planar imaging (EPI) sequence. Key parameters: TR = 3000 ms, TE = 30 ms, voxel size = 3.75x3.75x3 mm³, 44 slices [73]. Acquire at least 10 minutes of resting-state data with participants instructed to keep their eyes closed but not fall asleep.
- fMRI Preprocessing Pipeline:
- Discard initial volumes (e.g., first 5) to allow for T1 equilibrium.
- Slice-timing correction and realignment to correct for head motion. Exclude participants with mean Framewise Displacement (FD) > 0.25 mm [73].
- Co-registration of functional and structural images.
- Spatial normalization to a standard space (e.g., MNI).
- Spatial smoothing with a 5-8 mm FWHM Gaussian kernel.
- Functional Connectivity (FC) Analysis:
- Extract mean BOLD time-series from pre-defined brain regions of interest (ROIs), such as those in the Central Autonomic Network (CAN)—including the insula, anterior cingulate cortex (ACC), and amygdala [73].
- Calculate Pearson's correlation coefficients between the time-series of different ROIs to create a whole-brain FC matrix.
- For HRV-informed analysis, employ an HRV state-dependent FC framework, binning data into high and low HRV states (e.g., based on LF-HRV or HF-HRV) to examine dynamic brain-heart interactions [73].
Protocol for EEG Acquisition and Analysis in taVNS Studies
EEG offers millisecond-level temporal resolution to capture taVNS-induced changes in cortical oscillations and cognitive processing.
- Equipment Setup: Use a high-density (64-channel) EEG system arranged according to the international 10-20 system. Dry electrode systems can be suitable for enhanced participant comfort [72].
- Data Acquisition:
- Sampling rate should be at least 500 Hz. Impedance for all electrodes should be kept below 10 kΩ.
- Record during resting state (eyes open/closed) and/or during task performance (e.g., cognitive control or emotion regulation tasks). The protocol should include a baseline and concurrent taVNS/sham stimulation.
- Signal Preprocessing:
- Apply a band-pass filter (e.g., 0.5-70 Hz) and a notch filter (50/60 Hz) to remove line noise.
- Perform Independent Component Analysis (ICA) to identify and remove artifacts related to eye blinks, eye movements, and muscle activity.
- Feature Extraction:
- Power Spectral Density (PSD): Compute the absolute or relative power in standard frequency bands: Delta (0.5-4 Hz), Theta (4-8 Hz), Alpha (8-13 Hz), Beta (13-30 Hz), and Gamma (30-70 Hz). taVNS may modulate alpha and beta power [72].
- Frontal Alpha Asymmetry: Calculate as the difference in alpha power between homologous right and left frontal electrodes (e.g., F4 - F3). This is a validated marker for emotional processing and stress [72].
- fMRI-informed Electrical Fingerprint (EFP): For targeted analysis, create a model-derived EEG metric (e.g., rIFG-EFP) that reflects activity in a specific brain region identified via prior fMRI studies, thus providing a scalable proxy for fMRI activity [74].
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the proposed neurophysiological pathways of taVNS and a standardized experimental workflow for biomarker validation.
Proposed TaVNS Neuromodulatory Pathway
Multimodal Biomarker Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Equipment for taVNS Biomarker Research
| Item | Specification/Example | Primary Function in Research |
|---|---|---|
| taVNS Stimulator | tVNS (tVNS Technologies GmbH); gammaCore (electroCore, Inc.) | Delivers controlled, transcutaneous electrical stimulation to the auricular or cervical branch of the vagus nerve. |
| EEG System | DSI-24 (Wearable Sensing); high-density 64-channel systems (e.g., BrainAmp MR+) | Records electrical activity from the scalp to measure cortical oscillations and event-related potentials with high temporal resolution. |
| ECG Amplifier | Biopac MP150 with ECG module; wireless wearable sensors | Acquires raw electrocardiogram data for subsequent HRV analysis. |
| MRI Scanner | 3.0 Tesla Scanner (e.g., GE, Siemens, Philips) | Acquires high-resolution structural (T1) and functional (T2*) images to localize brain activity and functional connectivity. |
| Simultaneous EEG-fMRI | MR-compatible EEG system (e.g., BrainAmp MR+) | Enables direct correlation of electrophysiological (EEG) and hemodynamic (fMRI) brain activity, crucial for validating EEG proxies of fMRI activity [74] [73]. |
| Analysis Software | HRV: Kubios HRV; MATLAB Toolboxes.fMRI: SPM12; FSL; AFNI.EEG: EEGLAB; ERPLAB; MNE-Python. | Provides specialized toolkits for processing, analyzing, and visualizing physiological and neuroimaging data. |
| Psychophysics Suite | MATLAB with Psychtoolbox; Presentation | Prescribes controlled sensory and cognitive tasks to quantify behavioral outcomes (e.g., sensory thresholds, reaction times) [69]. |
Transcutaneous auricular vagus nerve stimulation (taVNS) has emerged as a promising non-invasive neuromodulation therapy, demonstrating potential across a spectrum of conditions including insomnia, post-stroke rehabilitation, tinnitus, and stress-related disorders [55] [27] [75]. Despite two decades of research and documented applications for over 30 diseases, the field faces significant challenges in protocol standardization and mechanistic understanding that hinder clinical translation [76] [77]. This application note synthesizes current evidence limitations and provides detailed methodological frameworks to guide the design of future large-scale trials, with particular emphasis on standardization of stimulation parameters, validation of sham protocols, and advanced mechanistic biomarker development.
Current Evidence Gaps and Methodological Limitations
Heterogeneity in Stimulation Parameters
Table 1: Variability in taVNS Parameters Across Clinical Studies
| Condition | Stimulation Site | Frequency (Hz) | Pulse Width (μs) | Intensity | Session Duration | References |
|---|---|---|---|---|---|---|
| Insomnia | Cymba conchae, Tragus | 20-30 Hz | 100-500 μs | Comfort-titrated | 15-30 min, 8 weeks | [55] [78] |
| Post-Stroke Motor Recovery | Left cymba conchae (primarily) | 20-30 Hz | 100-500 μs | 0.1-3 mA | 15-30 min, 3-6 weeks | [27] |
| Tinnitus | Concha, tragus | 20-25 Hz | 100-300 μs | Individual tolerance | Variable protocols | [75] |
| Stress Regulation | Cymba conchae | 30 Hz | 200 μs | Just below pain threshold | 1-min on/off cycles | [44] |
| Cognitive Studies | Cymba conchae, tragus | 25 Hz | 300 μs | 0.8 mA | 30 min | [79] |
The extensive variability in stimulation parameters represents a critical barrier to comparing outcomes across studies and establishing definitive treatment protocols [76] [55]. This heterogeneity encompasses electrode placement, stimulation intensity, frequency, pulse width, and treatment duration, as detailed in Table 1. The lack of parameter optimization studies makes it difficult to determine whether negative trial results reflect true inefficacy or suboptimal stimulation protocols [55] [75].
Limitations in Sham Control Methodologies
The development of validated sham controls remains a fundamental challenge in taVNS research. Current approaches typically involve earlobe stimulation, based on the assumption that this area lacks vagal innervation [80] [44]. However, computational modeling reveals that earlobe stimulation produces distinct current flow patterns that may still activate non-vagal neural pathways, potentially undermining its validity as an inert control [80]. This methodological limitation complicates the interpretation of trial results and blinding efficacy.
Incomplete Mechanistic Understanding
While the auriculo-vagal afferent pathway (AVAP) has been proposed as the primary mechanism of action, detailed understanding of central nervous system engagement remains incomplete [55] [75]. The translation of peripheral vagal activation to specific neurophysiological effects involves complex networks including the nucleus tractus solitarius (NTS), locus coeruleus (LC), and broader autonomic regulation, but quantitative relationships between stimulation parameters and central responses are not well-established [55] [27] [79].
Proposed Experimental Protocols for Evidence Generation
Protocol for Parameter Optimization Studies
Objective: Systematically evaluate parameter combinations to identify optimal stimulation settings for specific conditions.
Study Design: Randomized, crossover, sham-controlled trial using a factorial design to test multiple parameter combinations.
Participants: Target sample of 80 participants (20 per arm) with specific condition (e.g., insomnia, post-stroke motor deficits).
Stimulation Parameters:
- Site: Cymba conchae (active) vs. earlobe (sham)
- Frequencies: 10 Hz, 20 Hz, 25 Hz, 30 Hz
- Pulse widths: 100 μs, 200 μs, 300 μs, 500 μs
- Intensities: Individualized to sensory threshold (0.5-3 mA)
- Duration: 20-minute sessions, twice daily for 4 weeks
Outcome Measures:
- Primary: Condition-specific clinical outcomes (e.g., PSQI for insomnia, Fugl-Meyer Assessment for motor recovery)
- Secondary: Physiological biomarkers (HRV, salivary alpha-amylase), neurophysiological measures (EEG, fMRI)
Statistical Analysis: Linear mixed-effects models to account for repeated measures and crossover design, with adjustment for multiple comparisons.
Protocol for Sham Validation Studies
Objective: Validate sham stimulation protocols using neuroimaging and physiological biomarkers.
Study Design: Randomized, crossover study comparing active taVNS, sham taVNS, and no stimulation.
Participants: 40 healthy volunteers.
Methods:
- Active taVNS: Cymba conchae stimulation at established parameters (25 Hz, 300 μs)
- Sham taVNS: Earlobe stimulation with identical parameters
- Assessment: fMRI to measure NTS and LC activation, pupillometry as proxy for LC activity, HRV analysis, and participant blinding assessment
Analysis: Compare neural activation patterns and autonomic responses between conditions using repeated-measures ANOVA.
Protocol for Mechanistic Biomarker Development
Objective: Establish quantitative biomarkers of taVNS target engagement.
Study Design: Prospective cohort study integrating multiple measurement modalities.
Participants: 60 participants receiving active taVNS.
Assessment Methods:
- EEG: Resting-state and event-related potentials (P3 component)
- fMRI: Resting-state functional connectivity and task-based activation
- Autonomic Measures: HRV, pupillometry, salivary alpha-amylase
- Biochemical Assays: Plasma norepinephrine, BDNF, inflammatory markers
Analysis: Multivariate models to identify associations between stimulation parameters, physiological responses, and clinical outcomes.
Visualization of taVNS Mechanisms and Experimental Workflows
Central Mechanisms of taVNS
Comprehensive Trial Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Experimental Materials
| Item | Function/Specification | Application Context |
|---|---|---|
| taVNS Stimulation Device | Programmable parameters (frequency: 1-30 Hz, pulse width: 50-1000 μs, current: 0.1-10 mA); bipolar electrodes | All intervention studies; requires FDA clearance for clinical trials |
| ECG/HRV Monitoring System | High-resolution (≥1000 Hz) recording for heart rate variability analysis | Autonomic nervous system assessment; outcome measure for target engagement |
| EEG System | 64-channel or higher with event-related potential capabilities | P3 component analysis; resting-state and task-based brain activity |
| fMRI Compatibility | taVNS device must be MRI-compatible | Neural activation studies (NTS, LC); functional connectivity analysis |
| Pseudorabies Virus (PRV) | Neurotropic tracer for neural circuit mapping | Animal studies only; neural connectivity of ABVN pathways |
| Salivary Alpha-Amylase Assay | Kit for enzymatic or spectrophotometric analysis | Non-invasive biomarker of noradrenergic activity |
| ELISA Kits | Norepinephrine, BDNF, inflammatory markers (IL-6, TNF-α) | Biochemical confirmation of mechanism; blood, saliva, or CSF samples |
| Blinding Assessment Questionnaire | Structured instrument to assess participant perception of treatment assignment | Sham control validation; typically 5-point Likert scale |
| Adverse Events Questionnaire | Standardized taVNS-specific safety monitoring tool | Safety assessment; based on systematic review recommendations [34] |
Addressing the critical evidence gaps in taVNS research requires methodologically rigorous, large-scale trials that prioritize parameter optimization, sham validation, and mechanistic biomarker development. The protocols and frameworks presented herein provide a foundation for generating high-quality evidence to advance the field. Future research should emphasize standardized outcome measures, transparent reporting, data sharing initiatives, and patient-centered trial designs to fully elucidate the therapeutic potential of taVNS across neurological and psychiatric conditions.
Conclusion
taVNS represents a promising, non-invasive neuromodulation tool with a favorable safety profile and demonstrated efficacy across multiple neurological and psychiatric conditions. The optimization of stimulation parameters—including frequency, intensity, and site—is paramount for maximizing therapeutic outcomes and is highly dependent on the target indication. Future research must prioritize large-scale, well-controlled trials to establish standardized protocols, elucidate dose-response relationships, and identify patient-specific factors influencing treatment response. For the biomedical field, taVNS offers a novel platform for exploring brain-body interactions and developing targeted neuromodulation therapies, with significant implications for drug development and personalized medicine approaches in neurology and psychiatry.
References
- 1. The anatomical basis for transcutaneous auricular vagus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7083568/]
- 2. Auricular branch of vagus nerve [https://en.wikipedia.org/wiki/Auricular_branch_of_vagus_nerve]
- 3. Effect of non-invasive transcutaneous auricular vagus nerve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598993/]
- 4. Current Directions in the Auricular Vagus Nerve ... - Frontiers [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2019.00772/full]
- 5. High-resolution computational modeling of the current flow ... [https://www.sciencedirect.com/science/article/pii/S1935861X21002278]
- 6. Transcutaneous Auricular Vagus Nerve Stimulation Differently ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9260140/]
- 7. The efficacy of transcutaneous vagus nerve stimulation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12231624/]
- 8. Transcutaneous auricular vagus nerve stimulation in ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1693907/full]
- 9. Investigating the effects of transcutaneous Vagus Nerve ... [https://www.sciencedirect.com/science/article/pii/S1053811925004999]
- 10. Clinical advances in transcutaneous auricular vagus nerve ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1676727/full]
- 11. Transcutaneous Auricular Vagal Nerve Stimulation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7477388/]
- 12. a randomized, double-blinded, sham-control trial - Nature [https://www.nature.com/articles/s41598-025-17821-5]
- 13. The Effects of Transcutaneous Vagus Nerve Stimulation on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10121945/]
- 14. Transcutaneous auricular vagus nerve stimulation can ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1368754/full]
- 15. Mechanism and Applications of Vagus Nerve Stimulation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11854789/]
- 16. Mechanisms of vagus nerve stimulation in improving motor ... [https://www.dovepress.com/mechanisms-of-vagus-nerve-stimulation-in-improving-motor-dysfunction-a-peer-reviewed-fulltext-article-NDT]
- 17. Non-invasive vagus nerve stimulation in anti-inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11599236/]
- 18. No consistent evidence for the anti-inflammatory effect of ... [https://www.sciencedirect.com/science/article/abs/pii/S0889159123003793]
- 19. Transcutaneous vagus nerve stimulation has no anti- ... [https://www.nature.com/articles/s41598-024-72139-y]
- 20. Critical Review of Transcutaneous Vagus Nerve Stimulation [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.00284/full]
- 21. A literature review on the neurophysiological ... [https://pubmed.ncbi.nlm.nih.gov/32208895/]
- 22. Transcutaneous vagus nerve stimulation: a bibliometric study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11363710/]
- 23. Brain signaling dynamics after vagus nerve stimulation [https://www.sciencedirect.com/science/article/pii/S1053811921009526]
- 24. Transcutaneous auricular vagus nerve stimulation modulates ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10879907/]
- 25. Does transcutaneous auricular vagus nerve stimulation ... [https://www.sciencedirect.com/science/article/pii/S1935861X25000245]
- 26. A multivariate comparison of electroencephalogram and ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2022.983602/full]
- 27. Clinical advances in transcutaneous auricular vagus nerve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615202/]
- 28. Optimizing the modulation paradigm of transcutaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10050378/]
- 29. The Acute Effects of Varying Frequency and Pulse Width ... [https://www.mdpi.com/2227-9059/13/3/700]
- 30. Optimization of respiratory-gated auricular vagus afferent ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2022.1038339/full]
- 31. Efficacy of Transcutaneous Auricular Vagus Nerve ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1705512/full]
- 32. Neuroregulatory and clinical efficacy of auricular vagus ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1537515/full]
- 33. Safety and feasibility of transcutaneous vagus nerve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10394887/]
- 34. Safety of transcutaneous auricular vagus nerve stimulation ... [https://www.nature.com/articles/s41598-022-25864-1]
- 35. Safety and tolerability of Transcutaneous Vagus Nerve ... [https://www.sciencedirect.com/science/article/abs/pii/S1935861X18302936]
- 36. Transcutaneous Auricular Vagus Nerve Stimulation [https://soterixmedical.com/research/tavns]
- 37. Evaluation of different vagus nerve stimulation anatomical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8613407/]
- 38. Effect of non-invasive transcutaneous auricular vagus ... [https://pubmed.ncbi.nlm.nih.gov/41213698/]
- 39. Non-invasive access to the vagus nerve central projections via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4458242/]
- 40. Laboratory Administration of Transcutaneous Auricular Vagus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6867597/]
- 41. Effects of stimulation site and protocol on autonomic ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1692530/full]
- 42. Transcutaneous Auricular Vagus Nerve Stimulation (taVNS) [https://www.lidsen.com/journals/icm/icm-10-04-043]
- 43. Accelerated Transcutaneous Auricular Vagus Nerve ... [https://www.sciencedirect.com/science/article/pii/S1094715925000327]
- 44. Effect of transcutaneous auricular vagus nerve stimulation ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1593614/full]
- 45. The efficacy of transcutaneous vagus nerve stimulation in ... [https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-025-04919-x]
- 46. The vagus nerve: a cornerstone for mental health and ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1639866/full]
- 47. Transcutaneous auricular vagus nerve stimulation ( taVNS ) improves... [https://pubmed.ncbi.nlm.nih.gov/40398066/]
- 48. Effective Rosacea Treatment Using taVNS Therapy - EMJ [https://www.emjreviews.com/dermatology/news/effective-rosacea-treatment-using-tavns-therapy/]
- 49. Transcutaneous auricular vagus nerve stimulation ( taVNS ) for insomnia [https://www.dovepress.com/transcutaneous-auricular-vagus-nerve-stimulation-tavns-for-insomnia-di-peer-reviewed-fulltext-article-NSS]
- 50. A pooled analysis of the side effects of non-invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11841445/]
- 51. Transcutaneous auricular vagus nerve stimulation in healthy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593472/]
- 52. The Acute Effects of Varying Frequency and Pulse Width of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940630/]
- 53. Effects of taVNS on physiological responses and cognitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615536/]
- 54. Transcutaneous Auricular Vagus Nerve Stimulation in ... [https://pubmed.ncbi.nlm.nih.gov/40323248/]
- 55. Transcutaneous Auricular Vagus Nerve Stimulation (taVNS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174914/]
- 56. Effects of Transcutaneous Auricular Vagus Nerve Stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274684/]
- 57. The effects of transcutaneous auricular vagus nerve ... [https://www.sciencedirect.com/science/article/pii/S1388245724003353]
- 58. Transcutaneous vagus nerve stimulation boosts accuracy ... [https://www.sciencedirect.com/science/article/pii/S1935861X25001019]
- 59. Transcutaneous Vagus Nerve Stimulation (tVNS) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10366452/]
- 60. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8040977/]
- 61. Therapeutic applications of transcutaneous auricular vagus ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.1000758/full]
- 62. Impact of transcutaneous auricular vagus nerve stimulation ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1569472/full]
- 63. Transcutaneous Vagus Nerve Stimulation May Enhance Only ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7262369/]
- 64. Efficacy and safety of transcutaneous auricular vagus nerve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11110564/]
- 65. Transcutaneous Auricular Vagus Nerve Stimulation (ta-VNS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10275831/]
- 66. Comparative Efficacy of Neuromodulatory Strategies for ... [https://www.sciencedirect.com/science/article/pii/S1878875024016334]
- 67. Mapping the role of vagus in post-stroke arm motor... nerve stimulation [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-025-01759-w]
- 68. Brain Stimulation Techniques in Research and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763832/]
- 69. Transcutaneous cervical vagus nerve stimulation improves ... [https://www.nature.com/articles/s41598-024-54026-8]
- 70. Diagnostic accuracy of heart rate variability as a screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11685156/]
- 71. Transcutaneous auricular vagus nerve stimulation to acutely ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11186228/]
- 72. Stress Analysis Based on Simultaneous Heart Rate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8407658/]
- 73. Altered Relationship Between Heart Rate Variability and ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2021.671890/full]
- 74. Neural and functional validation of fMRI-informed EEG ... [https://www.sciencedirect.com/science/article/pii/S1053811922009430]
- 75. Current status of transcutaneous auricular vagus nerve ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1405310/full]
- 76. Transcutaneous Auricular Vagus Nerve Stimulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8192665/]
- 77. Feasibility and effectiveness of transcutaneous auricular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11388527/]
- 78. taVNS for Sleep & Stress: A 2025 Practitioner's Guide [https://therawellness.us/tavns-guide/]
- 79. The Effect of Transcutaneous Auricular Vagal Nerve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7349824/]
- 80. High-Resolution Computational Modeling of the Current Flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8608747/]