Optimizing Stimulation Waveforms for Selective Neuromodulation: From Biophysical Principles to Clinical Applications
This article provides a comprehensive exploration of the strategies and challenges in optimizing electrical stimulation waveforms to achieve selective neural activation.
Optimizing Stimulation Waveforms for Selective Neuromodulation: From Biophysical Principles to Clinical Applications
Abstract
This article provides a comprehensive exploration of the strategies and challenges in optimizing electrical stimulation waveforms to achieve selective neural activation. Aimed at researchers and biomedical professionals, it synthesizes foundational biophysical principles, cutting-edge computational and experimental methodologies, and comparative analyses of emerging technologies. The content covers key aspects from overcoming the non-selective recruitment inherent in exogenous stimulation to the application of novel paradigms like temporal interference and orientation-selective stimulation. By integrating recent findings from spinal cord, peripheral nerve, and cortical stimulation studies, this review serves as a critical resource for developing next-generation, precision neuromodulation therapies for neurological disorders and restorative neurotechnology.
The Biophysical Foundation of Selective Activation: From Size Principles to Recruitment Order
Theoretical Foundations: Natural vs. Artificial Recruitment
What is Henneman's Size Principle?
Henneman's Size Principle describes the natural, orderly recruitment of motor units by the central nervous system. It states that motor units are recruited from smallest to largest based on the force requirement of a movement [1] [2].
- Orderly Recruitment: Low-force, fatigue-resistant slow-twitch (Type I) muscle fibers, innervated by smaller motor neurons, are recruited first. As force demands increase, higher-force, fatigable fast-twitch (Type II) fibers, innervated by larger motor neurons, are recruited [1].
- Physiological Benefits: This organization minimizes fatigue by using endurance fibers for low-intensity tasks and reserves high-force fibers for strenuous activities. It also ensures a smooth, linear increase in force output [1].
- Underlying Mechanism: Smaller motor neurons have a higher membrane resistance, meaning they require a lower synaptic current to reach their firing threshold and are therefore more easily excited than larger neurons [1].
How does exogenous electrical stimulation alter this natural order?
Conventional electrical stimulation (ES) often reverses or disrupts this natural recruitment hierarchy, a phenomenon critical for researchers to understand when designing experiments.
- Reversal of Recruitment: Unlike the natural system, exogenous stimulation with typical rectangular pulses tends to activate larger, fast-twitch motor units first. This occurs because the larger axons associated with these units have a lower resistance to the applied electric current [1].
- Spatially Fixed and Temporally Synchronous Activation: Some research suggests that ES creates a non-selective pattern where recruitment is not orderly but instead is both "spatially fixed and temporally synchronous" [1]. This is fundamentally different from the finely graded, asynchronous natural activation.
- Consequence for Fatigue: Recruiting the highly fatigable fibers first can lead to rapid muscle exhaustion, which is a significant limitation in therapeutic and functional electrical stimulation applications [1].
Table: Key Differences Between Natural and Electrically Induced Recruitment
| Feature | Natural Recruitment (Size Principle) | Conventional Exogenous Stimulation |
|---|---|---|
| Recruitment Order | Small → Large Motor Units | Large → Small Motor Units |
| Initial Fiber Type Activated | Slow-Twitch (Fatigue-Resistant) | Fast-Twitch (Fatigable) |
| Activation Pattern | Orderly, Asynchronous | Non-selective, Synchronous |
| Fatigue Onset | Delayed | Rapid |
| Control Mechanism | Neurological (Synaptic Input) | Electrical (Axon Properties) |
Troubleshooting Guides & FAQs
FAQ 1: Why does my electrical stimulation protocol cause rapid muscle fatigue in subjects?
Answer: The most likely cause is the reversal of Henneman's Size Principle. Your stimulation parameters are probably recruiting large, fast-twitch, highly fatigable motor units before the smaller, fatigue-resistant ones [1]. This depletes energy reserves rapidly. To mitigate this, explore waveform shapes that promote more selective or natural-order recruitment.
FAQ 2: How can I improve the selectivity of my stimulation to target specific neural elements?
Answer: Achieving selectivity is a core challenge. Consider these factors, which can be optimized using computational models [3]:
- Stimulation Waveform Shape: Moving beyond simple rectangular pulses is key. Asymmetric biphasic pulses or waveforms with sub-threshold pre-pulses can help differentiate between cell bodies and passing axons or between fiber diameters [3].
- Stimulation Frequency: Evidence suggests that sinusoidal stimulation at specific frequencies can preferentially activate different cell types (e.g., photoreceptors at 5 Hz, bipolar cells at 25 Hz, ganglion cells at 100 Hz) [4]. This frequency-dependent selectivity may be applicable in other neural tissues.
- Pulse Duration: Shorter duration pulses generally improve spatial selectivity (activating fibers close to the electrode) and fiber diameter selectivity [3].
FAQ 3: My experimental results with electrical stimulation are inconsistent. What could be the source of error?
Answer: Inconsistencies often stem from technical setup rather than the biological preparation.
- Incomplete Circuit: The most common problem is a loss of contact between electrodes, leads, and the skin. If your stimulator cuts out at low intensities (e.g., 5-6 mA), it is often a safety alert for a broken circuit. Check for damaged leads, faulty electrodes, or poor electrode-skin contact [5].
- Stimulator Artifacts: Large stimulation artifacts can obscure neural recordings. Using charge-balanced waveforms and ensuring proper grounding can help reduce these artifacts.
Experimental Protocols for Selective Activation Research
Protocol: Investigating Frequency-Dependent Selective Activation
This protocol is adapted from studies on retinal stimulation, demonstrating a method to achieve selective neural targeting [4].
Objective: To determine the optimal sinusoidal frequency for selectively activating different neuronal populations in an in vitro preparation.
Materials:
- In vitro neural tissue preparation (e.g., retinal explant, nerve bundle).
- Microelectrode for localized sinusoidal stimulation (e.g., Pt-Ir electrode, ~10 kΩ).
- Cell-attached or whole-cell patch-clamp rig for recording from individual neurons.
- Pharmacological blockers (e.g., CNQX for AMPA/Kainate receptors, CdCl₂ for synaptic transmission blockade).
- A sinusoidal waveform generator.
Method:
- Setup: Mount the tissue in a recording chamber and continuously perfuse with oxygenated physiological solution at a controlled temperature (e.g., 36°C).
- Stimulation: Position the stimulating electrode ~25 μm above the target tissue. For a focused investigation, compare electrode placement over the soma region versus over the distal axon.
- Stimulation Parameters: Apply a series of sinusoidal waveforms at different frequencies (e.g., 5 Hz, 25 Hz, 100 Hz) with a fixed duration and pressure/current.
- Recording: Simultaneously record neural responses (spiking or subthreshold potentials) from target cells.
- Pharmacology: To elucidate direct versus synaptically mediated responses, repeat the stimulation in the presence of synaptic blockers.
- Analysis: Calculate the spike probability or peak postsynaptic current for each frequency. Plot the response magnitude against stimulation frequency to identify the optimal frequency for a given cell type.
Protocol: Model-Based Optimization of Stimulation Waveforms
This protocol uses computational modeling to design and test efficient and selective stimulation waveforms, drastically reducing experimental trial-and-error [6] [3].
Objective: To use a surrogate neural fiber model to design a stimulation waveform that selectively activates target fibers within a mixed nerve.
Materials:
- High-performance computer with GPU.
- Publicly available finite element model of the target nerve and electrode.
- Computational environment like NEURON or a machine learning-based surrogate model (e.g., AxonML/S-MF) [6].
- Electrophysiology setup for in vivo or in vitro validation.
Method:
- Model Construction: Implement a realistic model of the target nerve, including the electrode geometry and the spatial distribution of different fiber types (e.g., using the MRG model for myelinated fibers) [6].
- Define Optimization Goal: Formally state the objective, such as "maximize activation of 10 μm fibers while minimizing activation of 12 μm fibers."
- Parameter Sweep & Training: Use the model to generate a dataset of fiber responses to a wide range of waveform parameters (amplitude, pulse width, shape). Train the surrogate model on this dataset [6].
- Waveform Optimization: Run a gradient-based or gradient-free optimization algorithm on the surrogate model to find the waveform parameters that best meet the defined goal.
- Validation: Test the computationally optimized waveform in a biological preparation and compare the observed selectivity with the model's predictions.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Reagents and Materials for Selective Activation Research
| Item | Function/Application | Example/Note |
|---|---|---|
| McIntyre-Richardson-Grill (MRG) Model | A validated, non-linear computational model of mammalian myelinated nerve fibers. The gold standard for predicting responses to electrical stimulation [6]. | Used to simulate AP propagation and predict activation thresholds for different waveform parameters [6]. |
| Surrogate Myelinated Fiber (S-MF) Model | A GPU-accelerated, machine-learning-based version of the MRG model. Enables rapid, high-throughput prediction of fiber responses for large-scale parameter optimization [6]. | Offers a >10,000x speedup over conventional models, making complex optimization feasible [6]. |
| TRPA1 Channel Constructs | A sonogenetic tool (e.g., hsTRPA1). When expressed in specific cells, it renders them sensitive to ultrasound stimulation, offering an alternative non-invasive control method [7]. | Allows selective activation of transfected neurons with ultrasound at frequencies like 7 MHz, which can be focused on small brain volumes [7]. |
| Sinusoidal Waveform Generator | Delivering frequency-specific stimulation to probe or exploit the frequency-dependent excitability of different neural targets [4]. | Critical for experiments investigating frequency-based selective activation [4]. |
| Synaptic Blockers | Pharmacological agents used to isolate direct neuronal stimulation from indirect, synaptically mediated responses [4]. | Examples: CNQX (AMPA receptor blocker), CdCl₂ (calcium channel blocker). |
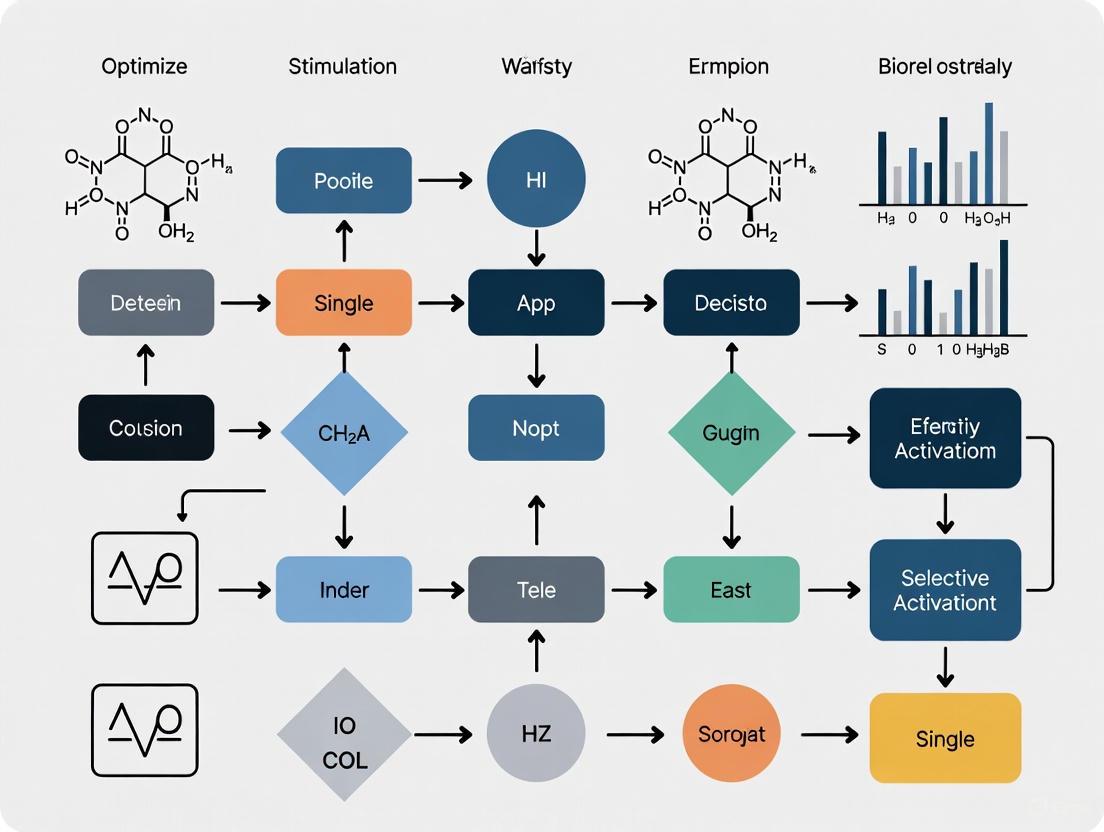
Visualization of Concepts and Workflows
Natural vs. Electrical Recruitment Order
Workflow for Selective Waveform Optimization
Frequently Asked Questions
1. Why does my model show significant errors in activation threshold when I use short-duration pulses? Traditional computational models like the Peterson surrogate can overestimate thresholds by more than 150% at short pulse widths because they do not fully capture the non-linear dynamics of ion channels, particularly the transition from sodium to potassium channel dominance at very short durations (below ~4 μs). For accurate results, use a modern surrogate model like S-MF (Surrogate Myelinated Fiber), which demonstrates a mean absolute percentage error of less than 2.5% across a wide range of pulse widths and fiber diameters by leveraging GPU acceleration and machine learning-trained biophysical properties [6] [8].
2. How can I improve the energy efficiency and selectivity of my stimulation waveforms? Conventional symmetric or monophasic pulses often trade off selectivity for high energy consumption. Employ an unconstrained optimization framework (like Particle Swarm Optimization) to design novel, asymmetric waveforms. This approach has yielded pulses with near-rectangular main phases that reduce energy loss by up to 92% compared to conventional monophasic pulses while maintaining or even improving directional selectivity, as evidenced by significant motor-evoked potential latency differences [9] [10].
3. My experimental strength-duration curve doesn't match the classical Lapicque or Weiss model. Is this normal? Yes, this is expected. The classical strength-duration models were derived for intracellular stimulation. For extracellular stimulation, the relationship is different due to the complex spatial interaction of the electric field with the axon and the distinct roles of different ion channels. The curve for extracellular stimulation typically has a slope of approximately -0.72 in log-log coordinates for pulse durations between 4 μs and 5 ms (dominated by sodium channels), which is less steep than the classical -1 slope [8].
4. What factors could be causing unexpected conduction delays in my unmyelinated axon model? Beyond standard cable properties, the presence of intracellular organelles like mitochondria can significantly impact conduction velocity. Mitochondria occupy axonal volume, increasing axial resistance. In small unmyelinated axons (e.g., ~0.4 μm diameter), a mitochondrial cross-sectional occupancy of about 26% can induce measurable delays. Ensure your computational model accounts for internal obstructions, as standard cables are often modeled as organelle-free [11].
5. How does the "strength-frequency" relationship differ from the "strength-duration" relationship? The strength-duration curve describes how the threshold current for a single pulse depends on that pulse's duration. The strength-frequency curve, relevant for repetitive stimulation like micromagnetic neurostimulation, describes how the threshold current for eliciting a response (e.g., an EPSP) changes with the frequency of the applied pulses. Generally, increasing the stimulation frequency leads to a decrease in the current amplitude threshold required for activation [12].
Troubleshooting Guides
Problem: Inconsistent Activation Thresholds Across Replicates
- Potential Cause 1: Unaccounted for biophysical variability in axonal properties.
- Solution: Standardize the state of intrinsic neural activity before testing. Axonal excitability is dynamically regulated by factors like resting membrane potential, which can inactivate potassium channels (e.g., Kv1.2, Kv1.4) and alter the action potential waveform [13].
- Potential Cause 2: Minor shifts in electrode position or orientation.
- Solution: For magnetic stimulation, carefully control the coil orientation. The effectiveness of micromagnetic neurostimulation (μMS) is highly dependent on the orientation of the μcoil relative to the neural fibers. Use a customized, easy-to-adjust holder like the "MagPen" for reproducible placement [12].
Problem: Low Spatial Selectivity During Targeted Stimulation
- Potential Cause: The stimulation waveform is not optimized for the specific neural target within the electric field.
- Solution: Implement a computational optimization workflow.
- Model: Use a multi-scale neuron model embedded in a realistic electric field distribution (e.g., from SimNIBS) [9].
- Define Objective: Establish a selectivity index, such as the ratio of activation thresholds in your target region versus the entire stimulated area [9].
- Optimize: Use a gradient-based or gradient-free (e.g., Particle Swarm) optimization algorithm to find waveform parameters that minimize this index. This can significantly improve focality from the temporal domain, even with a fixed electrode [6] [9].
- Solution: Implement a computational optimization workflow.
Problem: Excessive Coil Heating During Repetitive Stimulation Protocols
- Potential Cause: The stimulation waveform is energy-inefficient.
- Solution: Move beyond traditional biphasic or monophasic pulses. Optimize for energy loss (Joule heating) directly within your waveform design framework. As demonstrated with TMS, optimized asymmetric pulses can reduce the energy loss in the coil by up to 92%, enabling rapid-rate protocols without overheating [10].
Quantitative Data Tables
Table 1: Key Parameters from Strength-Duration Research
| Parameter | Description | Typical Value / Range | Context / Model |
|---|---|---|---|
| Rheobase | Minimum current for activation at a theoretically infinite pulse duration [14]. | 2-18 mA (clinical settings) [14]. | Clinical neurophysiology. |
| Chronaxie | Pulse duration at which the activation threshold is twice the rheobase [14]. | < 1 ms (normal muscle) [14]. | Clinical neurophysiology. |
| Short-Pulse Slope (log-log) | Slope of the strength-duration curve for extracellular stimulation with short pulses [8]. | -0.72 (for durations ~4μs-5ms) [8]. | Hodgkin-Huxley model, sodium-channel dominated. |
| S-MF Threshold Error | Mean absolute percentage error of the S-MF model vs. the NEURON MRG model [6]. | < 2.5% (across various diameters) [6]. | Machine learning surrogate model. |
| S-MF Speedup | Computational speed increase of the S-MF model over NEURON [6]. | 80x (single GPU vs. 375 CPU cores) [6]. | High-performance computing. |
Table 2: Outcomes of Waveform Optimization for Selective Stimulation
| Optimization Method | Key Achievement | Performance Outcome | Application |
|---|---|---|---|
| Gradient-Based/Free with S-MF | Selective activation in vagus nerve models [6]. | High accuracy in predicting thresholds (R² = 0.999) [6]. | Peripheral nerve stimulation (e.g., VNS). |
| Particle Swarm Optimization (PSO) | Improved TMS stimulation selectivity (temporal domain) [9]. | Reduced selectivity index (f₁), indicating more focal activation [9]. | Transcranial Magnetic Stimulation. |
| Unconstrained Asymmetric Pulse Optimization | Directional selectivity with high energy efficiency [10]. | 92% less energy loss vs. monophasic pulses; 1.79 ms MEP latency difference [10]. | Transcranial Magnetic Stimulation. |
Detailed Experimental Protocols
Protocol 1: Determining the Strength-Duration Curve Using a Computational Model
This protocol outlines how to generate a strength-duration curve using a modern, high-throughput surrogate axon model.
- Model Selection: Implement the Surrogate Myelinated Fiber (S-MF) model within the AxonML framework on a GPU-enabled system. This model accurately replicates the gold-standard MRG fiber model with a significant speedup [6].
- Setup Configuration:
- Fiber Properties: Define the diameter (e.g., 6-14 µm for myelinated fibers) and place it within a computational nerve morphology (e.g., human or pig vagus nerve model) [6].
- Electrode Configuration: Select an electrode type (e.g., cuff with monopolar or bipolar stimulation) and position it relative to the fiber [6].
- Stimulation Waveform: Define a set of rectangular monophasic pulses with durations spanning the range of interest (e.g., from microseconds to milliseconds) [6] [8].
- Threshold Determination: For each pulse duration, run a binary search algorithm to determine the minimum current amplitude (threshold) required to elicit a propagating action potential. The search should continue until the threshold is determined with a desired precision (e.g., 1%) [6].
- Data Analysis: Plot the threshold current (I) against the pulse duration (τ). Fit the data to analyze its slope in log-log space and compare it to classical (Lapicque) and modern (non-linear) expectations [8].
Protocol 2: Optimizing a Stimulation Waveform for Selectivity Using PSO
This protocol describes using an intelligent algorithm to find a waveform that selectively activates a target neuronal population.
- Define the Field: Use finite-element method (FEM) software (e.g., SimNIBS) to calculate the electric field distribution generated by your stimulator in a realistic tissue model (e.g., from an MRI) [9].
- Parameterize the Waveform: Represent the stimulation waveform as a series of levels. For a four-level TMS pulse, the parameters are the voltage (V₁-V₄) and pulse width (pw₁-pw₄) for each level, constrained by the circuit's capacitor voltages and total pulse width [9].
- Formulate the Optimization Problem:
- Decision Variables: The waveform parameters (e.g., V₁, V₂, pw₁, pw₂).
- Objective Function: A selectivity index (e.g.,
f₁ = Σ(threshEs_ROI) / Σ(threshEs_all)), where a smallerf₁indicates better selectivity. The goal is to minimizef₁[9]. - Constraints: Include practical limits like total pulse width and zero net current [9].
- Run Optimization: Employ a Particle Swarm Optimization (PSO) algorithm. The algorithm will iteratively propose new waveform parameters, simulate the neuronal response using a multi-scale neuron model, and calculate the selectivity index until a minimum is found [9].
- Validation: Test the optimized waveform in your experimental setup and measure outcomes like motor threshold and activation latency, comparing them to conventional waveforms [10].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function in Research | Brief Explanation |
|---|---|---|
| AxonML/S-MF Model | High-throughput prediction of axonal responses to electrical stimulation [6]. | A GPU-based machine learning surrogate model that dramatically accelerates simulations of neural fibers while retaining high accuracy [6]. |
| Multi-scale Neuron Model | Realistic simulation of neuron populations in a defined electric field [9]. | Integrates neuron morphology and coordinates from databases (e.g., NEURON) with electric field distributions from FEM software to predict stimulation thresholds [9]. |
| Tetrodotoxin (TTX) | Sodium channel blocker used for validation [12]. | Applying TTX blocks action potential-dependent synaptic responses. Recovery after washout confirms that recorded EPSPs are due to direct neural stimulation [12]. |
| MagPen (μCoil) | A prototype for precise micromagnetic stimulation (μMS) [12]. | A biocompatible, orientable microcoil that allows for controlled delivery of magnetic stimuli to brain slices, enabling the study of strength-frequency relationships [12]. |
| Particle Swarm Optimization (PSO) Algorithm | An intelligent algorithm for waveform parameter search [9]. | Efficiently navigates the high-dimensional parameter space of possible waveforms to find those that optimize a desired objective, such as selectivity or energy efficiency [9]. |
Experimental Workflow and Signaling Pathways
Diagram 1: Strength-Duration Relationship Determination Workflow
Diagram Title: Strength-Duration Curve Workflow
Diagram 2: Key Ion Channels Modulating Dopaminergic Axon Excitability
Diagram Title: Axonal Excitability Modulation Pathways
The Challenge of Preferential Large-Fiber Activation and Strategies for Targeting Small Diameter Fibers
Technical Troubleshooting Guides
Guide 1: Addressing Unintended Large-Fiber Activation
Problem: During experiments designed to activate small-diameter fibers (e.g., C-fibers, Aδ-fibers), you observe physiological responses indicative of concurrent large-fiber (Aα/Aβ) activation, such as muscle twitches or laryngeal EMG signals in vagus nerve studies [15].
Solutions:
- Check Electrode Configuration: Verify you are using a pin electrode setup rather than patch electrodes. Pin electrodes deliver high current density in upper skin layers and are more suitable for small-fiber activation [16].
- Adjust Pulse Duration: Increase the duration of exponential pulses to 100 ms. This leverages the accommodation properties of large fibers, which become less responsive to longer duration pulses compared to small fibers [16].
- Optimize Pulse Shape: Switch from rectangular to exponentially rising pulse shapes. Rectangular pulses preferentially activate large fibers, while slowly rising exponential pulses can elevate large-fiber activation thresholds [16].
- Modulate Stimulation Intensity: Ensure stimulation intensity is appropriately calibrated (e.g., 10 times perception threshold for maximal pain ratings in human subjects) rather than using supramaximal stimulation [16].
Guide 2: Overcoming Limited Selectivity in Vagus Nerve Stimulation
Problem: Vagus nerve stimulation elicits unwanted side effects (e.g., coughing, hoarseness, bradycardia) due to co-activation of large fibers innervating the larynx and pharynx [15].
Solutions:
- Implement Current Steering: Use multi-contact cuff electrodes and interferential current stimulation (i2CS) to create spatially focused activation fields. Adjust steering ratio to target organ-specific fascicles [17].
- Apply Anodal Block: Utilize anodic stimulation to preferentially activate orthogonal fibers approaching or leaving the electrode, which can target different fiber populations than cathodic stimulation [18].
- Utilize Kilohertz-Frequency Signals: Employ high-frequency signals (e.g., ~20 kHz) in interferential paradigms to achieve more selective activation of smaller vagal fibers [17] [15].
- Optimize Electrode Design: Ensure electrode arrays maintain proper insulation to prevent current leakage that can activate nearby large-diameter fibers with low activation thresholds [15].
Frequently Asked Questions (FAQs)
Q1: Why does conventional electrical stimulation preferentially activate large-diameter fibers instead of small-diameter fibers?
A1: This occurs due to fundamental biophysical principles. Large-diameter fibers have lower activation thresholds to exogenous electrical stimuli compared to small-diameter fibers. This creates an inverse recruitment order opposite to physiological activation (Henneman's size principle), where smaller fibers are naturally recruited before larger ones in biological systems [19]. The relationship between fiber diameter and activation threshold is well-established in computational models and experimental studies [6] [19].
Q2: What specific pulse parameters can enhance selective small-fiber activation?
A2: Research indicates several key parameters [16]:
- Pulse Shape: Exponentially rising pulses are superior to rectangular pulses
- Pulse Duration: Longer durations (≥15-100 ms) favor small-fiber activation
- Electrode Type: Pin electrodes paired with exponential pulses
- Stimulation Pattern: Single pulses may be more selective than trains for certain applications
Q3: How can I validate whether my stimulation protocol is successfully targeting small fibers?
A3: Employ these validation approaches:
- Physiological Markers: Monitor organ-specific responses known to be mediated by small fibers (e.g., bronchopulmonary responses in vagus nerve studies) [17]
- Computational Modeling: Use surrogate fiber models (e.g., S-MF) to predict activation thresholds across fiber diameters [6]
- Electrophysiological Recording: Measure evoked compound action potentials (eCAPs) to distinguish fast-fiber (large) versus slow-fiber (small) responses [17]
Q4: What are the most promising emerging technologies for selective fiber activation?
A4: Current advanced approaches include [6] [17]:
- Interferential Current Stimulation (i2CS): Uses temporal interference of high-frequency signals to create focused amplitude modulations
- Machine Learning-Optimized Stimulation: Leverages GPU-accelerated surrogate models to design selective stimulation parameters
- Anodal Block Techniques: Exploits orientation-dependent activation of fibers
- Multi-Contact Cuff Electrodes: Enables spatial targeting of specific fascicles
Table 1: Stimulation Parameters for Selective Fiber Activation
| Parameter | Large-Fiber Preference | Small-Fiber Preference | Key Findings |
|---|---|---|---|
| Pulse Shape | Rectangular | Exponential rising | Exponential pulses with 100-ms duration show maximal large-fiber accommodation [16] |
| Pulse Duration | Short (≤2 ms) | Long (≥15-100 ms) | Perception thresholds for exponential pulses increase with durations ≥15 ms, indicating large-fiber accommodation [16] |
| Electrode Type | Patch | Pin | Pin electrodes deliver high current density in upper skin layers [16] |
| Stimulation Frequency | Low frequency (≤100 Hz) | Kilohertz-frequency (∼20 kHz) | Kilohertz signals in i2CS reduce large-fiber activation at interference focus [17] |
| Polarity | Cathodic | Anodic | Anodic stimulation preferentially activates orthogonal fibers at lower thresholds [18] |
Table 2: Performance Comparison of Computational Models for Stimulation Optimization
| Model Type | Computational Speed | Accuracy | Best Applications |
|---|---|---|---|
| NEURON MRG Model | Baseline (reference) | High (gold standard) | Detailed biophysical studies, validation [6] |
| S-MF Surrogate | 2,000-130,000× faster than NEURON | R² = 0.999 for thresholds | Large-scale parameter sweeps, real-time optimization [6] |
| Peterson Surrogate | Faster than NEURON | MAPE = 31% (overestimates thresholds) | Basic threshold estimation [6] |
Experimental Protocols
Protocol 1: Preferential Small-Fiber Activation Using Exponential Currents
Based on: [16]
Objective: To establish a methodology for preferential small-fiber activation using exponentially rising electrical currents.
Materials:
- Pin electrodes and patch electrodes
- Constant current stimulator capable of generating exponential and rectangular pulses
- Perception threshold measurement system
- Pain rating scale (for human subjects)
Methodology:
- Electrode Placement: Apply both pin and patch electrodes to the target area.
- Threshold Determination: Compare perception thresholds between electrode types using single 1-100 ms exponential and rectangular pulses.
- Stimulus-Response Evaluation: Deliver pulse trains at 10 Hz using intensities from 0.1 to 20 times perception threshold.
- Data Collection: Record perception thresholds and pain ratings for both single pulses and pulse trains.
- Parameter Optimization: Apply 100-ms exponential pulses at 10 times perception threshold for maximal small-fiber activation.
Validation: Successful implementation is indicated by increased perception thresholds with longer exponential pulse durations (≥15 ms), demonstrating large-fiber accommodation.
Protocol 2: Selective Vagus Nerve Stimulation Using Interferential Currents
Based on: [17]
Objective: To achieve organ-specific fiber activation in the vagus nerve using intermittent interferential current stimulation (i2CS).
Materials:
- Multi-contact epineural cuff electrode
- Dual-channel current source capable of high-frequency (∼20 kHz) stimulation
- Recording equipment for eCAPs and physiological responses (EMG, breathing)
- Computational model for prediction (optional)
Methodology:
- Electrode Configuration: Place multi-contact cuff around cervical vagus nerve.
- Stimulation Paradigm: Deliver i2CS through contact pairs with slightly different high frequencies to create amplitude modulations.
- Current Steering: Apply uneven stimulus intensities (steering ratios from -1 to +1) to shift activation focus.
- Response Monitoring: Record eCAPs, laryngeal EMG, and breathing responses.
- Selectivity Assessment: Compare responses to equivalent non-interferential sinusoidal stimulation.
Validation: Successful selective activation is confirmed when i2CS produces distinct organ responses (e.g., bronchopulmonary vs. laryngeal) that differ from non-interferential stimulation.
Signaling Pathways and Experimental Workflows
Diagram 1: Pathways for Selective Small-Fiber Activation
Diagram 2: Experimental Optimization Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Selective Activation Research
| Item | Function/Purpose | Example Applications |
|---|---|---|
| Pin Electrodes | Deliver high current density to superficial skin layers; enhance small-fiber activation when paired with exponential pulses [16] | Cutaneous small-fiber studies, pain research |
| Multi-Contact Cuff Electrodes | Enable spatial selectivity through current steering and interferential stimulation patterns [17] | Vagus nerve studies, peripheral nerve stimulation |
| Exponential Pulse Generators | Generate slowly rising pulses that exploit accommodation properties of large-diameter fibers [16] | Preferential small-fiber activation protocols |
| Computational Models (S-MF) | GPU-accelerated surrogate models for rapid prediction of fiber responses to stimulation parameters [6] | Stimulation protocol optimization, parameter sweeps |
| High-Frequency Stimulators | Deliver kilohertz-range signals for interferential and blocking paradigms [17] | i2CS protocols, selective fiber activation |
| NEURON Simulation Environment | Gold-standard platform for modeling extracellular stimulation effects on detailed fiber models [6] [18] | Biophysical mechanism studies, model validation |
Neural Membrane Dynamics and Rectification Effects in Response to kHz Waveforms
Frequently Asked Questions (FAQs)
Q1: Why does my kHz-frequency stimulation fail to produce the expected selective activation of small fibers? This is often due to incorrect parameter combination. Selective activation of small, unmyelinated C-fibers over larger A- and B-fibers requires a specific window of frequency and intensity. For rats, use frequencies >5 kHz at intensities of 7–10 times the activation threshold (T); for mice, use 15–25 × T. Outside this window, you may get simultaneous activation of all fiber types or complete conduction block [20] [21].
Q2: My sinusoidal stimulation is causing synchronous neural firing instead of the desired desynchronization. What is wrong? The desynchronization effect of sinusoidal waveforms is highly frequency-dependent. Lower frequencies (e.g., 50-100 Hz) produce higher desynchronization across the neural population, while higher frequencies (e.g., 500-1000 Hz) can lead to more regular, synchronous firing. Ensure you are using the appropriate frequency for your application. Furthermore, consider using a Fast Amplitude Modulated Sinusoidal (FAMS) waveform, which is specifically designed to combine the benefits of low and high-frequency effects to enhance desynchronization [22].
Q3: When trying to achieve nerve conduction block, which waveform shape is most efficient? Square waveforms generally have the lowest block threshold amplitude, meaning they require less current to initiate a block. However, when efficiency is measured in charge per cycle, triangular waveforms can require the least charge. For a balance of efficacy and efficiency, both sinusoidal and square waveforms at frequencies of 20 kHz or higher are considered optimal [23].
Q4: Do the high-frequency carriers in amplitude-modulated signals (like TAMS) directly activate nerves? For carrier frequencies greater than 20 kHz, the nerve activation threshold is determined almost exclusively by the signal's offset (the low-frequency envelope), not the carrier itself. The carrier component does not offer an activation advantage over conventional rectangular pulses, which simplifies waveform design for transcutaneous stimulation [24].
Troubleshooting Guide
Common Experimental Issues and Solutions
Table 1: Troubleshooting Neural Responses to kHz Waveforms
| Problem | Potential Cause | Solution |
|---|---|---|
| Unnatural or paresthetic sensations in sensory applications [22] | Highly synchronous neural activation from rectangular pulses. | Switch to a desynchronizing waveform like a low-frequency sinusoid or FAMS [22]. |
| Inability to selectively activate C-fibers [21] | Incorrect intensity or frequency parameters. | Calibrate intensity to the specific threshold (T) for your animal model (7-10x T for rats) and use frequencies >5 kHz [21]. |
| Rapid muscle fatigue during functional stimulation [22] | Synchronous firing patterns from constant-frequency pulse trains. | Implement biomimetic, variable-frequency pulse trains or kHz-frequency amplitude-modulated waveforms to desynchronize activity [22]. |
| High block threshold or excessive power consumption [23] | Suboptimal waveform shape or electrode material. | Use square waveforms for lower block thresholds or switch to high-charge-capacity electrodes like carbon black coatings [23]. |
| Poor translation of transcutaneous stimulation depth [24] | Assumption that kHz carrier directly activates deeper nerves. | Focus on optimizing the amplitude of the low-frequency envelope; carriers >20 kHz do not directly affect activation threshold [24]. |
Optimizing Waveform Parameters
Table 2: Key Parameters for Selective Activation and Conduction Block
| Objective | Recommended Waveform | Frequency Range | Key Intensity Parameter | Model System Evidence |
|---|---|---|---|---|
| Selective C-fiber Activation [21] | Biphasic square pulse | >5 kHz | 7-10 x T (Rat); 15-25 x T (Mouse) | Rat & Mouse Vagus Nerve |
| Neural Firing Desynchronization [22] | Low-frequency sinusoid or FAMS | 50-100 Hz (Sinusoid) | 1.5 x Threshold (T) | Feline Peripheral Nerve |
| Nerve Conduction Block [23] | Square wave | 10-60 kHz | Lowest Block Threshold (Amplitude) | Rat Sciatic Nerve |
| Efficient Conduction Block [23] | Triangular wave | 10-60 kHz | Lowest Charge per Cycle | Rat Sciatic Nerve (Computational) |
| Cortical Activation (DBS) [25] | Biphasic square pulse | 1 kHz (pulse width 45 µs) | ~85 µA (current-controlled) | Awake Mouse Hippocampus/Cortex |
Detailed Experimental Protocols
Protocol 1: Establishing Selective C-Fiber Activation with kHz Stimulation
This protocol is adapted from methods to achieve selective activation of small, unmyelinated vagal C-fibers, which constitute over 80% of vagus nerve fibers [21].
1. Animal Preparation and Surgical Setup:
- Animals: Use adult male Sprague Dawley rats (300–550 g) or C57BL/6 mice (25–30 g).
- Anesthesia: Induce and maintain anesthesia using isoflurane (e.g., 4% for induction, 1.5–2% for maintenance).
- Physiological Monitoring: Maintain body temperature at 36.5–37.5 °C with a heating pad. Monitor ECG and respiration throughout.
- Nerve Exposure: Isolate the cervical vagus nerve (right cVN in rats, left in mice) via a midline neck incision. Minimize nerve manipulation by isolating only the caudal and rostral ends, leaving the middle portion within the carotid bundle.
2. Electrode Placement and Setup:
- Electrodes: Use custom tripolar cuff electrodes made with a polyimide substrate and sputter-deposited iridium oxide contacts (impedance 0.5–1.5 kΩ at 1 kHz).
- Placement: Position a stimulating cuff electrode on the nerve. Place a separate recording cuff electrode 5–6 mm away from the stimulating electrode center.
- Insulation: Apply silicone elastomer around the cuffs to minimize current leakage.
3. Stimulation and Validation of Selective Activation:
- Stimulation Waveform: Deliver symmetric, biphasic square pulses in 10-second trains.
- Key Parameters:
- Frequency: Use >5 kHz.
- Intensity: Calibrate carefully. For rats, use 7–10 times the activation threshold (T); for mice, use 15–25 x T.
- Validation with Probing Pulses: To confirm selective C-fiber activation and concurrent A/B-fiber block, interweave the kHz train with single monophasic probing pulses (100 μs for A/B-fibers, 600 μs for C-fibers). Briefly interrupt the kHz train for 30 ms (5 ms before and 25 ms after each probing pulse) to record artifact-free compound action potentials (CAPs). The presence of C-fiber CAPs with suppressed A/B-fiber CAPs indicates successful selective activation [21].
Protocol 2: Implementing FAMS for Desynchronized Neural Activation
This protocol outlines the use of the Fast amplitude-modulated sinusoidal (FAMS) waveform to evoke asynchronous, quasi-stochastic neural activity, which is useful for producing more naturalistic sensory percepts [22].
1. Computational Modeling (Initial Validation):
- Environment: Use the NEURON simulation environment.
- Neural Population: Model a heterogeneous population of sensory axons (diameters 6–12 μm) within a 100 μm² space.
- Stimulation Electrode: Model as a pair of ideal point sources.
- Waveform Definition: The FAMS waveform consists of a kHz-frequency carrier sinusoid that is amplitude-modulated at a lower frequency.
- Analysis: Compare the response to FAMS against conventional rectangular pulses. Quantify desynchronization by generating Peri-Stimulus Time Histograms (PSTHs). FAMS should produce spike timings that span the entire cathodic phase, demonstrating higher variability than the tight synchronization seen with rectangular pulses.
2. In Vivo Implementation:
- Animal Model: Utilize a feline model of peripheral nerve stimulation.
- Stimulation: Apply the FAMS waveform via a nerve cuff electrode.
- Recording and Analysis: Record neural activity and confirm that FAMS-evoked activity is more asynchronous than activity evoked by rectangular pulses, while still being controllable via simple stimulation parameters [22].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Specification / Function | Example Application |
|---|---|---|
| Tripolar Cuff Electrodes [21] | Polyimide substrate, IrOx contacts; for selective stimulation/recording. | Selective vagus nerve stimulation in rodents. |
| Programmable Stimulator [21] | Constant-current, capable of generating kHz-frequency biphasic square pulses (e.g., STG4008). | Delivery of precise kHz waveform trains. |
| High-Capacitance Electrodes [23] | Carbon black-coated electrodes; reduce block threshold and onset responses. | Efficient kilohertz nerve conduction block. |
| NEURON Simulation Environment [22] [23] | Platform for biophysical computational modeling of axons (e.g., MRG model). | Predicting neural response to novel waveforms in silico. |
| RHS2000 Controller [21] | 32-channel stim/record system for high-fidelity neural recording. | Recording compound action potentials during kHz stimulation. |
Experimental Workflow & Signaling Pathways
Diagram 1: FAMS Stimulation Experimental Workflow
Diagram 2: Selective C-Fiber Activation Principle
Diagram 3: kHz Waveform Nerve Block Mechanism
Computational and Experimental Methods for Designing Selective Waveforms
Leveraging Finite Element Models for Predicting Electric Field Distribution and Neural Activation
Frequently Asked Questions (FAQs)
Q1: What are the most common causes for a large discrepancy between my simulated electric fields and experimentally measured neural activation thresholds?
Discrepancies often arise from these key areas:
- Model Fidelity vs. Computational Cost: High-fidelity, microscopically detailed Finite Element Method (FEM) simulations are computationally intensive and can be prohibitive for large-scale parameter exploration [6] [26]. Simplifications in your model geometry may omit crucial details that affect field distribution.
- Neural Model Limitations: The accuracy of the neural activation prediction is limited by the biophysical neural model used. Simple threshold-based estimators can have errors exceeding 150%, while more complex non-linear models are computationally expensive [6].
- Biological Variability: The "electric field spatial noise" caused by microscopic physical cell structures can cause neuronal activation thresholds to vary by an average of around 10% from macroscopically homogeneous model predictions [27]. Individual anatomical differences also contribute to variability.
Q2: My model runs too slowly for parameter optimization. What strategies can I use to improve computational efficiency?
Leveraging machine learning-based surrogate models is a highly effective strategy. Researchers have achieved a 2,000 to 130,000x speedup over single-core NEURON simulations by using a GPU-based surrogate model (S-MF) of myelinated fibers. These surrogate models can generate full spatiotemporal responses to electrical stimulation orders-of-magnitude faster than conventional methods while retaining high predictive accuracy (e.g., R² = 0.999 for activation thresholds) [6]. Similarly, Graph Convolutional Networks (GCNs) can be trained on FEM data to directly predict electric potential distributions, bypassing the need for computationally intensive solvers in each iteration [26].
Q3: How can I enhance the selectivity of neural activation using waveform optimization?
Selective activation can be improved by moving beyond conventional constant-frequency pulses. Optimization algorithms like particle swarm optimization can be applied to parameterize stimulation waveforms. The key parameters to optimize include [28] [29]:
- Waveform Polarity: The ratio of the positive to negative integrated areas of the stimulation waveform.
- Temporal Pattern: The relative order and amplitude of induced electric field levels.
- Pulse Shape: Using arbitrary or irregular waveforms (e.g., sinusoidal, nested pulse, randomized).
Studies show that irregular stimulation patterns can induce neural activity states that more closely resemble natural, behaviorally relevant activity compared to the often "artificial" patterns driven by standard constant-frequency stimulation [29].
Q4: How do I validate that my computed electric fields are physically accurate?
A robust method is to derive a secondary physical quantity from your predicted field and compare it against experimental or high-fidelity simulation data. For instance, in a study using GCNs to predict electric potentials, the physical fidelity was validated by computing the capacitance matrices from the predicted fields and showing strong agreement with capacitances derived from traditional FEM fields [26]. This ensures the predicted fields are not just statistically accurate but also physically consistent.
Troubleshooting Guides
Problem 1: High Computational Demand in Large-Scale Models
Issue: Running FEM simulations for large nerve models or performing parameter sweeps is too slow.
| Solution | Description | Key Benefit |
|---|---|---|
| Implement Surrogate Models | Use machine learning models (e.g., GPU-based S-MF) trained on FEM data to approximate system responses [6]. | Massive speedup (several orders of magnitude) for simulation and optimization. |
| Use Graph Convolutional Networks (GCNs) | For electric field prediction, train a GCN on existing FEM solutions to directly output full-field distributions [26]. | Fast, one-step prediction of electric fields, enabling real-time applications. |
Workflow Diagram: Surrogate Model Implementation
Problem 2: Poor Selectivity of Neural Activation
Issue: The stimulation protocol activates non-targeted neural populations or fails to achieve specific recruitment.
Solution: Employ a closed-loop optimization framework that integrates FEM with neural response models.
- Parameterize Stimulation Waveform: Define your waveform by its amplitude, frequency, pulse width, and shape (e.g., rectangular, sinusoidal, arbitrary) [28] [29].
- Compute Electric Field: Use your FEM model to simulate the field distribution for a given set of waveform parameters.
- Predict Neural Activation: Apply the electric field to a surrogate neural model (e.g., S-MF) to predict the spatiotemporal neural response [6].
- Optimize for Selectivity: Use a gradient-based or gradient-free optimization algorithm (e.g., particle swarm) to iteratively adjust the waveform parameters. The objective function should maximize activation in target fibers and minimize activation in non-target fibers [6] [28].
Experimental Protocol: Selective Vagus Nerve Stimulation A referenced methodology for achieving selective stimulation is as follows [6]:
- Nerve Models: Use anatomically realistic FEM models of human and pig vagus nerves.
- Electrodes: Model different cuff geometries (e.g., ImThera 6-contact, LivaNova helical).
- Stimulation: Apply linear combinations of rectangular waveforms with randomized amplitudes, delays, and pulse widths.
- Neural Targets: Model myelinated fibers of various diameters (e.g., 6–14 µm) using a validated surrogate model (S-MF).
- Optimization: Implement both gradient-free and gradient-based optimization methods to find stimulation parameters that selectively activate specific fascicles.
Problem 3: Model Validation and Accuracy Concerns
Issue: Uncertainty about the real-world predictive accuracy of the coupled FEM and neural activation model.
Solution Strategy:
- Multi-Fidelity Validation: Compare your model's predictions against multiple data sources.
- Derived Quantity Analysis: As performed in electric capacitance tomography research, compute a secondary, physically relevant metric (like inter-electrode capacitance) from your model's output and validate it against experimental measurements [26].
- Benchmark Against Gold Standards: Compare your activation thresholds with those from established, high-fidelity simulation platforms like the MRG model in NEURON, which is considered a gold standard and has been experimentally validated [6].
Validation Workflow Diagram
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table: Key Computational Tools and Models for FEM-Neural Activation Research
| Item Name | Function & Application | Key Details |
|---|---|---|
| S-MF (Surrogate Myelinated Fiber) Model | A GPU-based, high-throughput model for predicting neural fiber responses to electrical stimulation [6]. | Massively parallel; offers 2,000–130,000x speedup over CPU-based NEURON models while maintaining high accuracy (R²=0.999). |
| MRG (McIntyre-Richardson-Grill) Model | A gold-standard, biophysically detailed model of mammalian myelinated fibers, implemented in NEURON [6]. | Used for validating surrogate models; basis for many clinical translation studies and FDA-approved platforms. |
| Graph Convolutional Networks (GCNs) | Machine learning models for direct, one-step prediction of electric field distributions from sensor geometry and excitation patterns [26]. | Serves as a fast surrogate for FEM solvers; enables real-time field prediction and capacitance computation. |
| Particle Swarm Optimization | A gradient-free optimization algorithm for refining stimulation waveform parameters to maximize selectivity [28]. | Effective for exploring high-dimensional parameter spaces where gradient information is unavailable or costly. |
| NEURON Simulation Environment | The industry-standard platform for computationally demanding simulations of neurons, including extracellular stimulation [6]. | Currently the primary platform supporting complex fiber ultrastructure and extracellular voltage effects. |
Table 1. Performance Comparison of Neural Simulation Methods
| Model / Method | Computational Speed | Key Advantage | Key Limitation | Predictive Accuracy (vs. Experiment) |
|---|---|---|---|---|
| FEM + NEURON (MRG) | Slow (Baseline) | High biophysical detail & validation [6] | Computationally prohibitive for optimization [6] | High (Gold Standard) [6] |
| FEM + S-MF Surrogate | 2,000 - 130,000x faster [6] | Enables large-scale parameter sweeps & optimization [6] | Requires training data from high-fidelity models [6] | Very High (R² = 0.999 for thresholds) [6] |
| Peterson Surrogate | Fast | Simplicity [6] | Limited waveform flexibility; overestimates thresholds (MAPE=31%) [6] | Moderate to Low [6] |
| GCN for E-Field | Fast (Real-time potential) | Bypasses iterative FEM solving [26] | Accuracy dependent on training data quality and scope [26] | High agreement in derived quantities (e.g., capacitance) [26] |
Table 2. Impact of Stimulation Waveform on Neural Activity
| Waveform Type | Effect on Oscillatory Power (e.g., Gamma) | Effect on High-Dimensional Activity State | Potential Clinical Implication |
|---|---|---|---|
| Constant-Frequency (Standard) | Effective entrainment [29] | Induces predominantly "artificial" patterns (dissimilar from behavior) [29] | Suitable for suppressing/enhancing a single biomarker [29] |
| Irregular Patterns (Sinusoidal, Nested Pulse, Randomized) | Similar entrainment to standard pulses [29] | Induces activity that more closely resembles natural, behavioral activity [29] | Beneficial for applications requiring complex, behaviorally-relevant state entrainment [29] |
| Optimized Arbitrary Waveforms | Information Not Available | Can achieve higher selectivity than monophasic waveforms [28] | Personalized therapy; enhanced selectivity for specific neural populations [28] |
Foundational Concepts and Definitions
What are the core components of an electrical stimulation waveform?
An electrical stimulation waveform is defined by several fundamental parameters, each controlling a specific aspect of the current delivered to the tissue. Understanding these components is essential for designing effective stimulation protocols [30].
- Amplitude: The magnitude or intensity of the current, measured in milliamps (mA) peak for neurostimulation. It directly influences the intensity of the evoked response.
- Phase Duration: The time elapsed from the beginning to the termination of a single phase of a pulse, measured in microseconds (µs). This parameter is critical for determining which neural elements are activated.
- Pulse Duration (Pulse Width): The total time from the beginning to the end of all phases within a single pulse, including any interphase interval.
- Interphase Interval: The short period of time between two successive phases of a single pulse when no electrical activity occurs. This interval can affect membrane capacitance and safety.
- Frequency (Pulse Rate): The number of pulses delivered per second, measured in Hertz (Hz). Frequency primarily modulates the temporal patterning of the neural response.
- Polarity: Refers to the direction of current flow. In monophasic pulses, current flows in one direction. In biphasic pulses, current flow alternates direction, typically featuring an active phase and a balancing phase to achieve net zero charge delivery, which minimizes the risk of skin irritation and tissue damage [30].
Parameter Effects and Quantitative Data
How do specific waveform parameters influence the amplitude and latency of evoked neural responses?
Systematic investigation, particularly in intracortical microstimulation (ICMS), has quantified how waveform parameters modulate motor-evoked potential (MEP) amplitude and onset latency. These relationships are foundational for engineering desired outcomes. The table below summarizes key findings from a study that varied parameters of a biphasic, cathode-leading waveform in the rat motor system [31].
Table 1: Effects of Stimulation Parameters on Motor-Evoked Potentials (MEPs)
| Parameter | Effect on MEP Amplitude | Effect on MEP Latency | Notable Findings |
|---|---|---|---|
| Current Amplitude | Continuous increase | No significant effect | A primary determinant of response strength. |
| Pulse Duration | Continuous increase | No significant effect | Longer durations deliver more charge per phase. |
| Stimulus Frequency | Increased up to a plateau (100-200 Hz) | Decreased with higher frequency | Higher frequencies facilitate temporal summation. |
| Train Duration | Increased up to a plateau (43-172 ms) | Decreased with longer trains | Longer trains provide more pulses to drive the response. |
| Interphase Interval | No significant effect in tested range | No significant effect in tested range | Tested from 10 µs to 640 µs; minimal influence. |
What are the clinical uses of different waveform types?
Different waveform shapes are suited to specific clinical and research applications based on their interaction with neural tissue. The selection is often a trade-off between efficacy, selectivity, and safety [30].
Table 2: Common Waveform Types and Their Clinical Applications
| Waveform Type | Clinical Uses |
|---|---|
| Monophasic (DC/Galvanic) | Iontophoresis, wound healing, denervated tissue stimulation. |
| Pulsed Galvanic | Edema reduction, wound healing, innervated muscle contraction. |
| Symmetrical Biphasic (AC) | Pain suppression (TENS), innervated muscle contraction (NMES). |
| Asymmetrical Biphasic (AC) | Pain suppression (TENS), innervated muscle contraction (NMES). Avoids net skin charge, reducing burn risk [30]. |
| Unbalanced Triphasic | Edema reduction, pain suppression. |
Experimental Protocols for Parameter Optimization
Protocol 1: Establishing a Motor Threshold and Response Curve using ICMS
This protocol is adapted from methods used to systematically map the effects of stimulation parameters on motor output [31].
- Animal Preparation: Anesthetize the rat (or other animal model) and secure it in a stereotaxic frame. Perform a craniotomy to expose the primary motor cortex.
- Electrode Implantation: Implant a microelectrode array or a single microelectrode into the forelimb region of the primary motor cortex.
- EMG Setup: Insert fine-wire electromyography (EMG) electrodes into the contralateral forelimb muscle of interest (e.g., a wrist or digit flexor).
- Stimulation and Recording:
- Set a baseline pulse waveform (e.g., cathodal-leading, biphasic pulse, 0.2 ms phase duration).
- Begin stimulation at a low current amplitude (e.g., 10 µA). Deliver short train stimuli (e.g., 13 pulses at 333 Hz).
- Simultaneously record the EMG for MEPs.
- If no MEP is observed, increase the current amplitude in small increments until a threshold response is identified.
- Parameter Variation: Once the threshold is found, systematically vary one parameter at a time (e.g., frequency from 50-400 Hz, train duration from 10-200 ms) while holding others constant. Record the amplitude and latency of the resulting MEPs for each parameter set.
- Data Analysis: Plot the MEP amplitude and latency against each parameter to generate input-output curves. Use this data to identify optimal parameters for a desired response profile.
Protocol 2: Optimizing Transcranial Magnetic Stimulation (TMS) Waveforms for Selectivity
This protocol uses intelligent optimization algorithms to design TMS pulses for improved stimulation focus [9].
- Model Setup: Establish a multi-scale neuron model based on a real human head MRI. Use simulation software (e.g., SimNIBS) to obtain the electric field distribution of a TMS coil.
- Define Objective Function: Establish a selectivity index as the optimization target. For example, the ratio of the stimulation threshold in a target region of interest (ROI) to the threshold of all neurons in the stimulated field. A lower index indicates better selectivity [9].
- Parameterize Waveform: Define the TMS coil voltage waveform using a flexible parameter set. For a multi-level waveform, this includes the amplitude and pulse width for each voltage level [9].
- Run Optimization Algorithm: Implement a particle swarm optimization (PSO) algorithm. The algorithm will iteratively test different waveform parameter combinations in the model, seeking to minimize the selectivity index.
- Validation: Select the optimized waveforms from the algorithm and test them on the model. Compare the activation of the target region versus non-target regions against conventional waveforms (e.g., monophasic or biphasic pulses).
TMS Waveform Optimization Workflow
Troubleshooting Common Experimental Issues
FAQ 1: Why is my stimulation failing to evoke a neural response despite high current amplitudes?
- Check Electrode Impedance: High impedance at the electrode-tissue interface can prevent current from reaching the target. For transcutaneous stimulation, the impedance of dry skin can be very high (e.g., ~25 kΩ for a 0.44 cm² electrode), requiring a stimulator with a high compliance voltage (e.g., ±150 V) to drive sufficient current [32]. Measure and ensure impedance is within an acceptable range.
- Verify Stimulator Specifications: Confirm your stimulator can deliver the required compliance voltage and current for your application (transcutaneous vs. invasive). Many benchtop stimulators designed for invasive use cannot output the high voltages needed to penetrate the skin [32].
- Review Pulse Parameters: The stimulus might be subthreshold. Ensure the pulse width is sufficiently long to depolarize the target neurons. Also, for motor evoked potentials, a train of pulses is often necessary; a single pulse may be insufficient [31].
- Confirm Target Location: Small errors in electrode placement over a nerve or cortical region can lead to complete failure of activation. Use anatomical landmarks, ultrasound, or stereotaxic coordinates to verify placement.
FAQ 2: How can I improve the spatial selectivity of my stimulation to avoid activating off-target areas?
- Optimize Waveform Polarity and Shape: In TMS, asymmetric (e.g., monophasic) or optimized unidirectional pulses can offer superior directional selectivity for activating specific neural populations compared to symmetric biphasic pulses [10]. Consider using algorithmic waveform optimization to design pulses that maximize activation in the target region while minimizing off-target effects [9].
- Utilize Current Steering: If using multiple electrodes, employ bipolar or multipolar configurations to steer the electric field. The shape of the electrical field is determined by the arrangement of anodes and cathodes, which can be programmed to focus current on the target [33].
- Adjust Active Electrode Contact Size and Configuration: Using a smaller active electrode contact can help concentrate current density. For spinal cord stimulation, carefully selecting and configuring the anodes and cathodes on a multi-contact lead can shape the field of paresthesia to cover the painful area [33].
FAQ 3: My stimulation is causing patient discomfort or skin irritation. What steps should I take?
- Ensure Charge Balancing: Unbalanced biphasic or monophasic waveforms can lead to a net DC current, causing electrochemical reactions at the electrode site that lead to skin irritation and potential burns. Always use a accurately charge-balanced biphasic waveform [30] [32].
- Incorporate an Interphase Interval: A short interval (e.g., 50 µs) between the cathodic and anodic phases of a biphasic pulse can allow the membrane capacitance to partially discharge, potentially improving the safety and comfort of the subsequent balancing phase [32].
- Reduce Charge Density: Lower the stimulation amplitude or pulse width. Charge density (amount of charge per unit area per phase) is a key factor in tissue damage. Calculate your charge density and ensure it is within safe limits for your electrode type and tissue.
- Check Electrode Contact and Gel: Ensure electrodes are properly attached with uniform contact. Use high-quality conductive gel to prevent hot spots from uneven current flow.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Equipment for Stimulation Research
| Item | Function / Explanation |
|---|---|
| Programmable High-Voltage Stimulator | A stimulator capable of generating biphasic, current-controlled pulses with a high compliance voltage (e.g., ±150 V) is essential for transcutaneous stimulation to overcome high skin impedance [32]. |
| Digital Potentiometer | Allows for real-time, programmatic control of stimulation amplitude via serial commands, which is crucial for closed-loop experimental paradigms [32]. |
| Multi-Scale Neuron Modeling Software (e.g., SimNIBS, NEURON) | Software that integrates realistic head models and neuron morphology to simulate the effects of electric fields on neural populations, enabling in-silico waveform testing and optimization [9]. |
| Surface EMG System | For recording motor-evoked potentials (MEPs) to quantitatively assess the output of motor stimulation protocols [31]. |
| Particle Swarm Optimization (PSO) Algorithm | An intelligent optimization algorithm used to automatically identify the best waveform parameters for a given objective, such as maximizing stimulation selectivity [9]. |
FAQs: Core Concepts for Researchers
Q1: What are the fundamental differences between SSES and OSES? SSES and OSES are advanced paradigms designed to overcome the limited spatial selectivity of Conventional Monopolar Epidural Stimulation (CMES). SSES uses multiple electrode contacts in bipolar configurations to shape the electric field spatially. In contrast, OSES controls the orientation of the electric field gradient relative to the spinal cord's neuroanatomy, typically using three contacts with currents following sinusoidal functions with 120° phase offsets to steer the field direction [34]. The core difference is that SSES focuses on the location of the field, while OSES focuses on its directional alignment with target neural pathways.
Q2: What is the primary quantitative evidence for superior selectivity with these paradigms? Evidence comes from analyses of Spinally Evoked Motor Potentials (SEMPs). Research shows that the amplitudes of SEMPs in hindlimb muscles significantly depend on the orientation of the applied electric field. Both SSES and OSES provide more selective control over SEMP amplitudes compared to CMES, as measured by the variation in response amplitudes across different stimulation configurations and orientations [34].
Q3: In what key experimental context are OSES paradigms typically applied? While the core principle is universal, the OSES paradigm was pioneered and is extensively used in Deep Brain Stimulation (DBS) research to selectively activate axonal pathways based on their orientation [35] [36]. This principle is directly translatable to spinal cord applications, where the goal is to target specific dorsal roots or other oriented structures. The foundational concept is that the maximal activation of axons occurs when the electric field gradient is oriented parallel to them [35].
Q4: What are the technical requirements for implementing OSES? Implementing OSES requires:
- A multichannel electrode array: A minimum of three electrode contacts is needed to define a plane for field orientation. Recent research has expanded this to tetrahedral (4-contact) probes for full 3D orientation control [36].
- An independent current-source stimulator: The system must deliver independently controlled currents to each channel, with the ability to precisely set amplitudes based on sinusoidal functions for field steering [34] [35].
Troubleshooting Guide: Common Experimental Challenges
Q1: We are not observing the expected variation in muscle responses with different OSES angles. What could be wrong?
- Cause 1: Incorrect lead placement relative to the target neuroanatomy. The orientation of the electrode array must align with the anatomical plane containing the target fibers.
- Solution: Verify array placement using fluoroscopy or other imaging techniques. Computational modeling of the electric field based on your specific implant geometry can help determine the optimal placement [35].
- Cause 2: Inaccurate current distribution across the electrodes.
- Solution: Recalibrate your stimulator. For OSES, ensure the relative current amplitudes (I1, I2, I3) precisely follow the functions:
I1 = I0 sin(Φ),I2 = I0 sin(Φ + 120°),I3 = I0 sin(Φ - 120°), whereI0is the amplitude andΦgoverns the stimulation angle [34] [35].
Q2: Our experimental results show high variability in SEMP latencies and amplitudes.
- Cause 1: Unstable electrode array position (lead migration).
- Solution: Ensure the array is securely fixed during implantation. In percutaneous setups, lead migration is a known challenge; regularly verify position via fluoroscopy, especially after patient movement [37].
- Cause 2: Suboptimal stimulation parameters or configuration.
- Solution: Systematically perform "spinal mapping." Test a wide range of electrode configurations (cathode/anode arrangements), pulse widths (e.g., 0.5 ms), and current amplitudes (e.g., 0.2-1.2 mA in 0.1 mA increments) to identify the optimal settings for your specific experimental goals [34] [37].
Q3: How do we define and identify the early (ER) and middle (MR) responses in SEMP data?
- Solution: Manually or algorithmically analyze the latency from the stimulus artifact.
- Early Responses (ER): Typically occur within a latency window of 1.5 to 4.5 ms. These are often attributed to the direct activation of motor axons.
- Middle Responses (MR): Typically occur within a latency window of 4.5 to 10.5 ms. These represent the activation of spinal circuits, such as mono- or disynaptic reflexes [34]. For analysis focused on spinal network activation, the MR is often the response of interest.
Table 1: Comparison of Epidural Stimulation Paradigms
| Paradigm | Abbreviation | Electrode Configuration | Key Mechanism | Key Finding in Preclinical Models |
|---|---|---|---|---|
| Conventional Monopolar EES | CMES | Single contact with a distant reference | Broad, non-selective activation | Baseline for comparison; lower spatial selectivity [34] |
| Spatial-Selective EES | SSES | Multiple contacts in 8+ bipolar configurations | Spatial shaping of the electric field | Improved selective control of SEMP amplitudes compared to CMES [34] |
| Orientation-Selective EES | OSES | Three contacts with phase-offset currents | Steering the electric field gradient | SEMP amplitudes vary systematically with the stimulation angle, allowing selective activation [34] |
| 3D Orientation-Selective DBS | 3D-OSS | Tetrahedral (4-contact) probe | 3D steering of the electric field | Evoked responses in a monosynaptically connected brain region (amygdala) depend on stimulation field orientation [36] |
Table 2: Typical Experimental Parameters for Rodent SSES/OSES Studies
| Parameter | Typical Setting | Notes / Range |
|---|---|---|
| Animal Model | Adult Sprague Dawley rats (300-350 g) | Common model for initial proof-of-concept studies [34] |
| Pulse Width | 0.5 ms | Standard for neuromodulation [34] |
| Stimulation Frequency | 0.5 Hz (for mapping) | Allows for recovery between pulses and clear SEMP analysis [34] |
| Current Amplitude | 0.2 - 1.2 mA | Tested in 0.1 mA increments to establish response thresholds [34] |
| Pulses per Trial | 10 | Allows for averaging of responses to improve signal-to-noise ratio [34] |
| Data Analysis | Amplitude & Latency of SEMPs | Amplitudes are often normalized as a percentage of the maximal response for comparison [34] |
Detailed Experimental Protocols
Protocol 1: Implementing Orientation-Selective Stimulation (OSES)
This protocol outlines the steps to set up and run an OSES experiment based on established methodologies [34] [35].
- Electrode Implantation: Implant a multi-contact electrode array (minimum 3 contacts for 2D, 4 for 3D) in the epidural space over the target spinal cord segment (e.g., lumbosacral enlargement for lower limb motor control) or deep brain region.
- Stimulator Setup: Connect the electrode contacts to a multi-channel, independent current-source stimulator (e.g., an 8-channel system like the STG4008 from Multichannel Systems).
- Define Stimulation Angles: Determine the set of angles (Φ) you wish to test (e.g., from 0° to 360° in 45° increments).
- Calculate Current Amplitudes: For each angle Φ, calculate the current for each of the three channels using the formulas:
I1 = I0 sin(Φ)I2 = I0 sin(Φ + 120°)I3 = I0 sin(Φ - 120°)whereI0is your desired peak current amplitude.
- Deliver Stimulation: For each angle, deliver a train of pulses (e.g., 10 pulses at 0.5 Hz) with the calculated current values for each channel.
- Record Responses: Simultaneously record electromyography (EMG) from target muscles (e.g., Tibialis Anterior, Gastrocnemius) or neural signals.
- Data Analysis: Analyze the amplitude and latency of the evoked responses (SEMPs) for each stimulation angle to identify the orientation that produces the most selective or robust activation.
Protocol 2: Spinal Mapping for Functional Configuration
This protocol is critical for identifying the optimal stimulation parameters to enable specific motor functions in SCI models [37].
- Lead Implantation: Permanently or temporarily implant a percutaneous or paddle lead in the epidural space.
- Systematic Configuration Testing: Test a wide array of electrode configurations, primarily varying the cathode and anode locations. Start with simple configurations (one cathode, one anode) and progress to more complex multi-contact setups.
- Parameter Variation: For promising configurations, vary stimulation parameters such as frequency (e.g., from tonic to 30-100 Hz bursts), pulse width, and amplitude.
- Functional Assessment in Multiple Contexts:
- Supine: Assess for induced tonic extensor activity or voluntary limb movement.
- Upright Supported (Standing Frame): Refine configurations that promote trunk stability and lower limb extension.
- Parallel Bars / Exoskeleton: Test the ability of the configuration to facilitate weight-bearing standing, sit-to-stand transitions, and stepping.
- Iterative Refinement: The mapping process is iterative. Configurations identified in one posture (e.g., supine) must be refined in the target functional posture (e.g., standing). An "interim mapping phase" is often required to transition from one function (e.g., standing) to another (e.g., stepping) [37].
Research Reagent Solutions
Table 3: Essential Materials and Equipment for SSES/OSES Research
| Item | Function / Application | Example / Specification |
|---|---|---|
| Multi-channel Stimulator | Delivers precise, independent currents to multiple electrodes for SSES/OSES. | STG4008 (Multichannel Systems); A-M Systems isolators with National Instruments DAC [34] [35] |
| Custom Electrode Arrays | Implantable probes for delivering oriented or spatially selective fields. | 4-channel custom arrays (SSES/OSES) [34]; Tripolar tungsten electrodes (OSS DBS) [35]; Tetrahedral 4-wire probes (3D-OSS) [36] |
| Electromyography (EMG) System | Records spinally evoked motor potentials (SEMPs) from target muscles. | Bipolar needle electrodes; systems from Medtronic or Lab Chart (AD Instruments) for amplification/filtering [34] |
| Fluoroscopic Guidance System | Ensures accurate initial placement and monitors migration of percutaneous leads. | Standard clinical or preclinical C-arm system [37] |
| Computational Modeling Software | Models the electric field distribution for predicting neural activation and optimizing array design. | Used to analyze axonal excitability for varied electric field orientation [35] |
Experimental Workflow and Signaling Pathways
Diagram 1: Experimental Workflow for SSES/OSES Optimization
Diagram 2: Signaling Pathways in Epidural Stimulation
Intelligent Optimization Algorithms and Multi-Scale Neuron Models for Waveform Design
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Why does my optimization algorithm fail to converge to a waveform that improves stimulation selectivity?
- Problem: The algorithm stalls, produces minimal improvement in the selectivity index (
f1), or suggests physically unrealistic waveform parameters. - Solution: This is often related to an inadequate objective function or incorrect parameter boundaries.
- Review the Selectivity Index Calculation: Ensure your objective function, which quantifies stimulation precision, correctly represents the biological target. The selectivity index (
f1) is often defined as the ratio of activation thresholds in the target region versus the total stimulated area [9]. A miscalculation here will misguide the optimizer. - Check Parameter Constraints: The parameters for the induced electric field waveform (e.g., voltage levels
V1-V4and pulse widthspw1-pw4) must be bounded by the physical limits of your TMS circuit topology [9]. Overly generous boundaries can lead to solutions that are not implementable. - Adjust Algorithm Hyperparameters: If using an algorithm like Particle Swarm Optimization (PSO), the convergence is sensitive to hyperparameters like swarm size and learning factors. Fine-tuning these may be necessary for your specific problem landscape [9] [38].
- Review the Selectivity Index Calculation: Ensure your objective function, which quantifies stimulation precision, correctly represents the biological target. The selectivity index (
FAQ 2: How can I validate that my multi-scale neuron model is responding realistically to the optimized waveform?
- Problem: Uncertainty about whether the model's prediction of neuronal activation is physiologically accurate.
- Solution: Employ a multi-faceted validation strategy.
- Compare to Known Results: Test your model with standard, well-documented waveforms (e.g., monophasic, biphasic) and compare the resulting activation thresholds and spatial patterns against published experimental or simulation data [39].
- Inspect Subcellular Responses: Use a toolbox like NeMo-TMS to simulate subcellular processes, such as calcium dynamics in dendrites. A realistic model should show calcium accumulation consistent with known plasticity-inducing protocols [39].
- Leverage Standardized Models: To ensure your base neuron model is sound, use and contribute to standardized, community-vetted models in repositories like the NeuroML Database (NeuroML-DB) and Open Source Brain (OSB) [40] [41]. This reduces errors in model construction.
FAQ 3: My simulation shows good selectivity, but the required stimulation intensity causes excessive coil heating. How can I balance these factors?
- Problem: The optimized waveform is effective but not practical due to hardware limitations like coil heating, calculated as ( w_{heat} = \int {RI^{2} dt} ) [9].
- Solution: Reformulate the optimization as a multi-objective problem.
- Instead of solely minimizing the selectivity index (
f1), add coil heating (w_heat) as a second objective to be minimized. - Use a multi-objective optimization algorithm like NSGA-II [42] to generate a set of Pareto-optimal solutions. These solutions represent the best possible trade-offs between selectivity and heating, allowing you to choose a waveform that is both effective and practical.
- Instead of solely minimizing the selectivity index (
FAQ 4: What are the common pitfalls when translating a natural language problem description into a mathematical model for optimization?
- Problem: The AI-generated mathematical model is syntactically correct but is inefficient for solvers or misses key constraints.
- Solution: While Large Language Models (LLMs) can help bridge the gap between natural language and mathematical formulation, their output requires expert review [43].
- Check for Missing Constraints: Domain expertise is crucial. The AI might omit subtle but critical constraints related to safety, energy, or hardware. Always manually verify the constraint set.
- Optimize for Solvability: The generated model might be mathematically correct but not formulated in a way that is efficient for Mixed Integer Programming (MIP) solvers. A domain expert should refine the model structure to enhance solving speed [43].
Detailed Experimental Protocols
Protocol 1: Intelligent Waveform Optimization using Particle Swarm Optimization (PSO)
This protocol details the process for optimizing TMS waveform parameters to improve stimulation selectivity, based on the methodology of [9].
1. Objective: To identify waveform parameters that minimize the selectivity index (f1), thereby maximizing the precision of neuronal activation.
2. Materials and Setup:
- Multi-scale Neuron Model: A model incorporating realistic neuron morphology embedded in a cortical grid, driven by an electric field distribution from a specific coil (e.g., MCB70) and head model [9] [39].
- Simulation Environment: A platform like NEURON or a custom MATLAB/SimNIBS pipeline to run the neuron simulation [9].
- Optimization Software: A PSO implementation, such as MATLAB's
particleswarmor a custom-coded variant.
3. Procedure:
- Step 1: Parameterize the Waveform. Define the waveform based on the circuit topology. For a four-level waveform from a dual-capacitor bridge circuit, the decision variables are typically
VC1,VC2,V1,V2,pw1, andpw2. The remaining parameters (V3,V4,pw3,pw4) are calculated based on constraints [9]. - Step 2: Define the Objective Function. The function should:
a. Generate the electric field waveform from the PSO's candidate parameters.
b. Apply this waveform to the multi-scale neuron model.
c. Simulate to determine the stimulation thresholds for all neurons in the Region of Interest (ROI) and the broader influenced area.
d. Calculate and return the selectivity index
f1as per Equation (2) in [9]. - Step 3: Configure the PSO. Set algorithm parameters (swarm size, maximum iterations, inertia weight) and enforce lower/upper bounds for all decision variables based on circuit limitations.
- Step 4: Run Optimization. Execute the PSO. The algorithm will iteratively update the particle positions (waveform parameters) to find the set that minimizes
f1. - Step 5: Validate Results. Select the best-performing waveform from the PSO output and run a full simulation to confirm improved selectivity and check other metrics like required stimulation intensity and coil heating.
Protocol 2: Building and Simulating a Multi-Scale Neuron Model with NeMo-TMS
This protocol outlines the steps to create a multi-scale model for predicting cellular and subcellular responses to TMS, using the NeMo-TMS toolbox [39].
1. Objective: To simulate the effects of a TMS electric field on a realistic neuron model, including membrane voltage dynamics and intracellular calcium signaling.
2. Materials and Setup:
- NeMo-TMS Toolbox: Installed from the public repository (
https://github.com/OpitzLab/NeMo-TMS). - Neuron Morphology Data: A reconstruction file (e.g., in SWC format) of the target neuron.
- Electric Field Data: The TMS-induced electric field distribution in the geometry of interest, calculated using Finite Element Method (FEM) software like SimNIBS or COMSOL.
3. Procedure:
- Step 1: Generate the Neuron Model. Use the NeMo-TMS pipeline to create a computational model from the morphological reconstruction. The toolbox automatically adds the biophysics for specific cell types (e.g., CA1 pyramidal cells) [39].
- Step 2: Export Compartment Coordinates. Export the 3D spatial coordinates of all model compartments for the field-coupling step.
- Step 3: Couple the Electric Field. Calculate the quasipotentials across all neuron compartments using the macroscopic electric field data from the FEM simulation. This integrates the spatial distribution of the TMS field into the neuron model.
- Step 4: Define the Stimulation Protocol. Generate the temporal pattern (waveform) of the rTMS pulse train to be simulated.
- Step 5: Simulate Membrane Response. Run the simulation to compute the time-varying membrane potential across the entire neuron in response to the coupled electric field.
- Step 6: Simulate Calcium Dynamics. Based on the voltage traces, solve the calcium diffusion-reaction equations to model calcium concentration changes in various subcellular compartments over time.
- Step 7: Visualize and Analyze. Use the toolbox's visualization functions to plot voltage traces, calcium transients, and spatial maps of neuronal activity.
Data Presentation Tables
Table 1: Key Performance Metrics for Waveform Optimization in Neuromodulation
| Metric | Formula / Description | Optimization Goal | Reference |
|---|---|---|---|
Selectivity Index (f1) |
( f{1} = \frac{\sum{i=1}^{n} threshEs_ROI{i} }{\sum{i=1}^{3000} threshEs_{i} } ) | Minimize | [9] |
| Stimulation Intensity | Intensity = median(threshEs_ROI_i) |
Minimize (at target efficacy) | [9] |
Coil Heating (w_heat) |
( w_{heat} = \int {RI^{2} dt} ) | Minimize | [9] |
| Waveform Polarity | ( Polarity = \frac{\sum{i=1}^{4} V{i_pos} \times \text{pw}{i_pos} }{\sum{i=1}^{4} |V{i_neg} \times pw{i_neg} |} ) | Optimize for target engagement | [9] |
| Total Product Completion Time (T) | ( T = max{p \in P} (end(p)) - min{p \in P} (start(p)) ) | Minimize (for production scheduling) | [44] |
Table 2: Comparison of Intelligent Optimization Algorithms
| Algorithm | Primary Mechanism | Best Suited For | Key Considerations |
|---|---|---|---|
| Particle Swarm Optimization (PSO) | Social collaboration of particles in search space | Continuous parameter optimization (e.g., waveform parameter tuning) [9] | Sensitive to hyperparameters; good for global search but may struggle with fine-tuning. |
| NSGA-II | Non-dominated sorting and crowding distance | Multi-objective problems (e.g., optimizing selectivity vs. heating simultaneously) [42] | Returns a set of Pareto-optimal solutions, requiring a final decision based on trade-offs. |
| Differential Evolution (DE) | Vector-based mutation and crossover | Mixed-integer, nonlinear problems (e.g., test-path scheduling in ICs) [38] | Robust and simple to implement, but performance depends on mutation strategy. |
| Arithmetic Optimization Algorithm (AOA) | Using arithmetic operators (+, -, ×, ÷) | Engineering design problems (e.g., energy management in hybrid vehicles) [38] | A relatively newer metaheuristic; general performance across problems is under evaluation. |
Workflow Visualization
The following diagram illustrates the integrated workflow for optimizing stimulation waveforms using intelligent algorithms and multi-scale models.
Integrated Workflow for Waveform Optimization
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Resources for Multi-Scale Modeling and Optimization Experiments
| Item | Function in Research | Example / Specification |
|---|---|---|
| NeuroML/LEMS | A community standard model description language for defining and sharing computational neuroscience models in a simulator-independent format. Ensures reproducibility and interoperability [40] [41]. | NeuroMLv2 with LEMS dynamics specification. |
| NeMo-TMS Toolbox | An open-source pipeline for coupling TMS-induced electric fields with realistic neuron models to simulate membrane voltage and subcellular calcium dynamics [39]. | Available at: https://github.com/OpitzLab/NeMo-TMS |
| NEURON Simulator | A widely used simulation environment for constructing and testing models of individual neurons and networks of neurons [40] [39]. | Version 7.4+; used to run multi-scale neuron models. |
| SimNIBS | A software package for calculating the electric field induced in the brain by TMS and other non-invasive brain stimulation techniques using Finite Element Methods (FEM) [9]. | Version 4.0+; used for macroscopic field modeling. |
| Open Source Brain (OSB) | A resource and platform for collaborative development, visualization, and analysis of standardized, shareable computational models in neuroscience [40] [41]. | Repository: https://www.opensourcebrain.org/ |
| PSO/NSGA-II Libraries | Pre-implemented optimization algorithms. PSO is effective for single-objective waveform parameter tuning, while NSGA-II is for multi-objective problems [9] [42]. | MATLAB Global Optimization Toolbox, PlatypUS, or custom Python implementations. |
Overcoming Practical Challenges and Fine-Tuning Stimulation Parameters
Balancing Selectivity, Efficiency, and Power Consumption in Implantable Devices
Frequently Asked Questions (FAQs)
FAQ 1: What are the primary stimulation parameters I can adjust to improve spatial selectivity? Spatial selectivity—activating target neurons while sparing non-target areas—is primarily influenced by phase duration and the use of an interphase interval (IPI). Research on epiretinal prostheses has shown that shorter phase durations (e.g., 500 µs) can achieve cortical activation at lower charge thresholds. Furthermore, incorporating an IPI and using longer phase durations (e.g., 1000-1500 µs) have been found to result in a more confined spread of cortical activation, thereby improving spatial precision [45].
FAQ 2: How does stimulation frequency impact power efficiency and neural response? Stimulation frequency directly affects both power consumption and neural response robustness. High-frequency stimulation (10-20 Hz) often leads to significant attenuation of cortical responses compared to low-frequency stimulation (1 Hz) [45]. This response attenuation can force an increase in stimulus amplitude to achieve the same effect, thereby increasing the total power delivered per unit time and exacerbating coil or tissue heating [9] [10]. For repetitive stimulation protocols, it is crucial to find the lowest effective frequency.
FAQ 3: What waveform optimization strategies can reduce power consumption? Moving beyond traditional biphasic or monophasic pulses is key to reducing power. Intelligent optimization algorithms, such as particle swarm optimization (PSO), can design novel waveforms that significantly improve energy efficiency. One study demonstrated that optimized asymmetric pulses with near-rectangular main phases achieved up to a 92% reduction in energy loss compared to conventional monophasic pulses [10]. This directly translates to lower power requirements and reduced device heating.
FAQ 4: How can I validate the selectivity of an optimized waveform in an experimental model? Validating selectivity requires a combination of computational modeling and in vivo electrophysiology. A established method involves:
- Computational Prediction: Using a multi-scale neuron model based on real brain anatomy to simulate the electric field distribution and predict neuronal activation thresholds for different waveforms [9].
- In Vivo Measurement: Implanting a multi-electrode array in the target brain region (e.g., the primary visual cortex for retinal stimulation) to record local field potentials (LFPs) and electrically evoked potentials (EEPs) in response to the stimulus [45].
- Selectivity Index Calculation: Quantifying selectivity by comparing activation thresholds in the target region (ROI) to thresholds across all neurons in the stimulated area. A lower selectivity index indicates better precision [9].
Troubleshooting Guides
Problem: Excessive Power Consumption or Rapid Battery Drain
- Potential Cause #1: Inefficient stimulation waveform.
- Solution: Utilize optimization algorithms (e.g., PSO) to design waveforms that minimize energy loss. Consider asymmetric pulses with near-rectangular phases for directional selectivity and higher efficiency [10].
- Potential Cause #2: Stimulation frequency is too high.
- Solution: Characterize the neural response attenuation at different frequencies. Reduce the stimulation frequency to the lowest level that maintains the desired therapeutic effect, as high frequencies (10-20 Hz) can lead to response attenuation, requiring more power [45].
- Potential Cause #3: High electrode-tissue impedance.
- Solution: Prior to stimulation, measure the impedance at the stimulation site. Ensure consistent electrode placement and stability, as increased impedance demands higher voltage for the same current, increasing power draw [45].
Problem: Poor Spatial Selectivity (Activation of Non-Target Regions)
- Potential Cause #1: Suboptimal pulse phase duration.
- Solution: Systematically test a range of phase durations. Implement shorter phase durations (e.g., 500 µs) to lower the activation threshold for target neurons, or use longer durations (e.g., 1500 µs) to better confine the spread of activation [45].
- Potential Cause #2: Lack of an interphase interval (IPI).
- Solution: Introduce an IPI between stimulus phases. Experimental evidence shows that an IPI can help limit the spatial extension of cortical responses, thereby improving focality [45].
- Potential Cause #3: Fixed coil geometry limiting spatial focality.
- Solution: If using transcranial magnetic stimulation (TMS), optimize the temporal waveform of the induced electric field. Intelligent waveform optimization can improve stimulation precision on a temporal scale, even with a fixed coil structure [9].
Problem: Significant Device Heating During Operation
- Potential Cause #1: High energy loss in the stimulation coil or electrode.
- Solution: This is directly linked to inefficient waveforms. Adopt optimized waveforms that drastically reduce energy loss (and thus Joule heating) in the coil. One study reported a reduction in energy loss by up to 92% [10].
- Potential Cause #2: High peak currents during stimulation.
- Solution: Waveform parameters that require high peak currents for effective stimulation will generate more heat. Optimize the waveform to reduce peak current requirements while maintaining efficacy. The heating power in a coil is proportional to the square of the current (
I²) integrated over time [9].
- Solution: Waveform parameters that require high peak currents for effective stimulation will generate more heat. Optimize the waveform to reduce peak current requirements while maintaining efficacy. The heating power in a coil is proportional to the square of the current (
Experimental Protocols for Waveform Optimization
Protocol 1: In Vivo Assessment of Stimulation Parameters in Rodent Models
This protocol outlines the key steps for evaluating electrical stimulation parameters in an animal model, such as the retinal degeneration rat model used to mimic conditions for visual prostheses [45].
Title: In Vivo Stimulation Parameter Testing Workflow
- Key Materials: Adult LE rats or retinal degenerated (e.g., F1) rats; bipolar concentric stimulating electrode (e.g., Pt/Ir, 75 µm); multi-electrode array for cortical recording; stereotaxic device; data acquisition system [45].
- Procedure:
- Animal Preparation: Anesthetize the animal and secure it in a stereotaxic device. Maintain anesthesia and body temperature (≈37.5 °C) throughout [45].
- Stimulating Electrode Placement: Insert the bipolar stimulating electrode into the target tissue (e.g., the epiretinal space). Use real-time impedance monitoring (e.g., 5-8 kΩ range for epiretinal placement) to ensure consistent electrode-tissue distance [45].
- Recording Electrode Placement: Perform a craniotomy over the target cortical area (e.g., primary visual cortex, V1). Insert a multi-electrode array to record electrophysiological signals [45].
- Recovery Period: Allow the animal to recover for approximately one hour after surgery before commencing stimulation [45].
- Stimulus Application: Apply electrical stimulation using a range of predefined parameters (see table below for specific variables).
- Data Collection: Record the resulting Electrically Evoked Potentials (EEPs) and Local Field Potentials (LFPs) from the cortical array. The key metrics are the charge threshold for eliciting a response and the spatial spread of activation across the recording electrodes [45].
- Data Analysis: Calculate the activation threshold (e.g., the current amplitude required to elicit a half-maximal cortical response) and map the cortical activation area for each parameter set.
Protocol 2: Intelligent Waveform Optimization using Particle Swarm Optimization (PSO)
This protocol describes a computational framework for designing optimal stimulation waveforms, as applied in Transcranial Magnetic Stimulation (TMS) research [9] [10].
Title: Computational Waveform Optimization with PSO
- Key Materials: Multi-scale neuron model (e.g., in NEURON/SimNIBS); computational model of the stimulation setup (e.g., TMS coil); high-performance computing workstation; PSO algorithm implementation [9].
- Procedure:
- Parametrize the Waveform: Define the waveform by its constituent parameters. For a multi-level waveform, this includes the voltage levels (V1-V4) and their respective pulse widths (pw1-pw4), often constrained by a total pulse width (PW) and circuit topology [9].
- Set Optimization Objective: Define the selectivity index (f1) as the objective function to be minimized. This index is the ratio of stimulation thresholds for neurons in the target region to thresholds for all stimulable neurons in the field [9].
- Run PSO Algorithm: Initialize a population of candidate waveforms (particles). Iteratively evaluate them using the neuron model, calculate their selectivity index, and update the population toward better solutions [9].
- Output and Validation: Once the algorithm converges, output the optimized waveform parameters. The resulting waveform should then be validated in experimental models, as described in Protocol 1 [9] [10].
Table 1: Impact of Key Stimulation Parameters on Device Performance
This table synthesizes quantitative findings on how specific parameter adjustments influence selectivity, efficiency, and power consumption.
| Parameter | Optimal Value/Strategy for Selectivity | Impact on Efficiency & Power Consumption | Key Experimental Findings |
|---|---|---|---|
| Phase Duration | Shorter durations (e.g., 500 µs) for lower charge threshold; Longer durations (e.g., 1500 µs) for confined spread [45]. | Shorter durations can reduce the charge per phase, lowering energy per stimulus. However, may require higher current amplitude. | In vivo rat studies showed shorter phases (500 µs) elicited V1 activation at lower charge thresholds. Longer phases (1000, 1500 µs) confined cortical spread [45]. |
| Stimulation Frequency | Lower frequencies (e.g., 1 Hz) maintain robust response; High frequencies cause attenuation [45]. | High frequencies (10-20 Hz) increase power delivery rate and can cause significant coil heating [9] [45]. | Cortical responses in rats were significantly attenuated at 10 Hz and 20 Hz compared to 1 Hz stimulation [45]. |
| Waveform Shape | Asymmetric pulses with near-rectangular main phases for directional selectivity [10]. | Highly significant reduction in energy loss. Optimized pulses used up to 92% less energy than conventional monophasic pulses [10]. | Optimized Unidirectional Rectangular (OUR) pulses showed similar motor thresholds to monophasic pulses but with drastically reduced energy loss [10]. |
| Interphase Interval (IPI) | Inclusion of an IPI helps limit the spatial extension of cortical responses [45]. | Minor direct impact on power. Improves efficiency by confining effects to target area, potentially allowing lower overall doses. | Application of an IPI resulted in a more confined spread of cortical activation in epiretinal stimulation [45]. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials and Tools for Stimulation Optimization Research
| Item | Function/Application | Example Specifications / Notes |
|---|---|---|
| Multi-Scale Neuron Model | Computational prediction of neuronal activation thresholds for different electric field waveforms in a realistic anatomical context [9]. | Often built using software like NEURON and SimNIBS, incorporating real head MRI data and neuron morphology [9]. |
| Bipolar Concentric Stimulating Electrode | Delivery of focal electrical stimulation to target tissues in vivo (e.g., epiretinal stimulation) [45]. | Material: Pt/Ir. Tip diameter: 75 µm. Requires real-time impedance monitoring for placement validation [45]. |
| Multi-Electrode Array (MEA) | Recording of electrophysiological responses (EEPs, LFPs) from brain regions to map activation spread and determine thresholds [45]. | Configuration: 4x4 grid. 16 electrodes, 400 µm inter-tip distance. Inserted ~800-950 µm into the cortex [45]. |
| Particle Swarm Optimization (PSO) Algorithm | An intelligent computational method to identify optimal stimulation waveform parameters that minimize a cost function (e.g., selectivity index) [9]. | Used to optimize parameters like capacitor voltages (VC1, VC2) and pulse widths to minimize the selectivity index (f1) [9]. |
| Data Acquisition System | Precise generation of stimulation waveforms and synchronous recording of high-fidelity neural signals [45]. | System (e.g., CED Micro1401) with amplifier (e.g., A-M Systems Model 3600). Sampling rate: 25 kHz with band-pass filtering [45]. |
Adjusting Pulse Width to Control Activation Depth and Volume of Tissue Activated (VTA)
Core Principles of Pulse Width and VTA
How does pulse width influence the Volume of Tissue Activated (VTA)?
Pulse width, or phase duration, is a critical parameter in electrical stimulation that directly determines the threshold for neural activation and, consequently, the spatial extent of the activated tissue. Shorter pulse widths require higher current amplitudes to excite neurons, leading to a more focal activation profile. Conversely, longer pulse widths lower the activation threshold, allowing a larger volume of tissue to be recruited at a given current amplitude due to the activation of smaller-diameter axons and neurons located farther from the electrode tip [45].
What is the relationship between pulse width and activation depth?
Activation depth is closely linked to the VTA. Longer pulse widths facilitate the recruitment of neural elements at greater distances from the stimulating electrode by reducing the current amplitude needed to reach their activation threshold. This principle is leveraged in therapeutic neuromodulation, such as Sacral Neuromodulation (SNM), where adjusting the pulse width is a standard troubleshooting step to recapture therapeutic benefit when the stimulation is felt but ineffective [46].
Quantitative Data on Pulse Width Effects
The following table summarizes key experimental findings on the effects of pulse width and related parameters on neural activation, primarily from studies on epiretinal prostheses and transcranial magnetic stimulation (TMS). These findings provide a quantitative basis for parameter selection.
Table 1: Effects of Stimulation Parameters on Neural Activation and Energy Efficiency
| Parameter | Experimental Finding | Biological / Technical Implication | Source / Model |
|---|---|---|---|
| Shorter Phase Duration (e.g., 500 µs) | Lower charge threshold for activating the primary visual cortex (V1) [45]. | Reduces the energy required to activate neural tissue, potentially increasing battery life and safety. | In vivo epiretinal stimulation in rats [45]. |
| Longer Phase Duration (e.g., 1000-1500 µs) | More confined spread of cortical activation [45]. | Can be used to achieve more focal, spatially restricted neural stimulation. | In vivo epiretinal stimulation in rats [45]. |
| Interphase Interval (IPI) | Limits the extension of cortical responses [45]. | Adds another dimension of control to shape the spatial profile of the activated neural population. | In vivo epiretinal stimulation in rats [45]. |
| Optimized Asymmetric Pulses (OUR pulses) | Up to 92% less energy loss compared to conventional monophasic pulses; significant directional selectivity (MEP latency difference of 1.79 ms) [10]. | Dramatically improves energy efficiency and enables selective activation of neural populations based on orientation. | Transcranial Magnetic Stimulation (TMS) in humans [10]. |
Diagram 1: A workflow for optimizing pulse width and amplitude to achieve a desired VTA and functional outcome.
Troubleshooting FAQs and Protocols
FAQ 1: I am not getting any neural or behavioral response despite stimulation. What should I do?
This is a common issue that requires a systematic approach to troubleshoot [47].
Verify Stimulus Delivery:
- Confirm the stimulator is on and functional.
- Check all connections and cables for damage or discontinuity.
- Ensure the stimulus amplitude is sufficiently high. In some cases, such as with obese subjects, edema, or severe neuropathy, a higher amplitude or longer pulse width may be necessary to elicit a response [47].
Check Electrode Configuration:
Confirm Recording Setup:
- If measuring an output like an Electrically Evoked Potential (EEP), ensure your recording electrodes are intact, properly placed, and have sufficient contact.
- Verify that your amplifier and data acquisition system are on and configured correctly, including parameters like gain and sweep speed [47].
FAQ 2: My stimulation produces a large artifact that obscures the neural signal. How can I reduce it?
A large stimulus artifact often points to an issue with the recording circuit or grounding [47].
- Grounding: A loose or poorly positioned ground electrode is a primary cause. Ensure the ground has excellent contact and is placed appropriately, typically between the stimulating and recording sites.
- Electrode Integrity: Check for defective recording electrodes or wires. Test them with an ohmmeter for continuity.
- Stimulus Spread: Ensure no conductive bridge exists between your stimulating electrodes.
- Cabling: Make sure recording and stimulation cables are not touching or crossed.
FAQ 3: I have lost the therapeutic effect of my stimulation, but the subject still feels the stimulus. How can I regain efficacy?
This scenario is frequently encountered in clinical neuromodulation and can be addressed through parameter adjustment.
- Reprogramming: Change the active electrode configuration or the stimulation parameters themselves. In Sacral Neuromodulation (SNM), for example, altering the pulse width and/or frequency can shift the location of the perceived stimulus and restore therapeutic benefit [46].
- Rule out Other Causes: Check for transient physiological changes that could alter the response, such as infection or swelling.
- Consider Lead Migration: If conservative reprogramming fails, consider the possibility that the stimulating electrode has moved. Imaging may be required to confirm this [46].
Experimental Protocol: Determining Threshold VTA
This protocol outlines a method for empirically determining the relationship between pulse width and VTA in a rodent model, based on methodologies used to optimize epiretinal stimulation [45].
Objective: To map the cortical activation area resulting from electrical stimulation of a specific brain region (e.g., the retina or VTA) using different pulse widths.
Materials:
- Anesthetized rodent model (e.g., Long-Evans rat).
- Stereotaxic frame.
- Bipolar concentric stimulating electrode.
- Multi-electrode array (MEA) for recording local field potentials (LFPs) in the target region (e.g., primary visual cortex, V1).
- Data acquisition system with amplifier.
- Stimulus isolation unit.
Procedure:
- Surgical Preparation: Anesthetize the animal and secure it in a stereotaxic frame. Perform a craniotomy to expose the brain region for recording (e.g., V1).
- Electrode Placement: Insert the stimulating electrode into the target structure (e.g., the ventral-temporal retina). Insert the recording MEA into the projection area (e.g., V1, contralateral to the stimulated eye).
- Impedance Check: Measure the electrode-tissue impedance to ensure consistent electrode placement and contact.
- Stimulation and Recording:
- Set the stimulation frequency to a low rate (e.g., 1 Hz) to avoid response attenuation seen at higher frequencies [45].
- Begin with a fixed, sub-threshold current amplitude.
- Deliver a train of stimuli while systematically varying the pulse width (e.g., 100 µs, 500 µs, 1000 µs).
- Record the LFPs from all channels of the MEA simultaneously.
- Data Analysis:
- Measure the amplitude of the initial negative peak of the LFP (the EEP) on each channel.
- For each pulse width condition, create a spatial map of the EEP amplitude across the recording array.
- Define an activation threshold (e.g., 50% of the maximum recorded amplitude) and calculate the cortical surface area where the response exceeds this threshold. This area serves as a proxy for the VTA.
Expected Outcome: Shorter pulse widths will require higher current amplitudes to reach threshold and will produce a smaller activated area. Longer pulse widths will produce a larger activated area at the same current amplitude.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials and Equipment for VTA Stimulation Research
| Item | Function / Application | Example from Literature |
|---|---|---|
| Bipolar Concentric Electrode | Delivers focal electrical stimulation to neural tissue while minimizing current spread. | A 75 µm Pt/Ir bipolar concentric electrode was used for epiretinal stimulation in rats [45]. A similar electrode (250 µm) was used for stimulating the bed nucleus of the stria terminalis (vBNST) [49]. |
| Multi-electrode Array (MEA) | Records population-level neural activity (e.g., LFPs) from multiple sites simultaneously to map the spatial extent of activation. | A 4x4 grid electrode array was used to record electrically evoked potentials (EEPs) in the primary visual cortex [45]. |
| Cre-dependent Channelrhodopsin (ChR2) Mouse Lines | Enables optogenetic identification and manipulation of specific neuronal populations (e.g., dopamine neurons) during electrophysiology experiments. | DAT-Cre mice crossed with Ai32 (ChR2) mice were used to identify and record from genetically defined VTA dopamine neurons [50]. |
| EAA Receptor Antagonists | Pharmacological tools to dissect the contribution of glutamatergic signaling (via NMDA and non-NMDA receptors) to neural circuit activation. | AP-5 (NMDA antagonist) and CNQX (non-NMDA antagonist) were microinfused into the VTA to block synaptic activation of dopamine neurons [49]. |
| Kynurenic Acid | A broad-spectrum excitatory amino acid (EAA) receptor antagonist used to block glutamatergic transmission. | Microinfusion of 3mM kynurenic acid into the VTA significantly reduced activation of DA neurons by vBNST stimulation [49]. |
Diagram 2: The logical relationship between stimulation parameters, the resulting VTA, and the final functional outcome, highlighting key biological factors that modulate this process.
Mitigating Non-Physiological Recruitment and Muscle Fatigue in Motor Stimulation
Frequently Asked Questions
What is non-physiological recruitment and why is it a problem in motor stimulation? Non-physiological recruitment refers to the synchronous, rather than natural asynchronous, activation of motor units (MUs) and muscle fibers during electrical stimulation. This occurs because conventional NMES techniques often use current pulses that simultaneously depolarize a large number of motor neuron axons. This pattern renders the stimulated muscle highly susceptible to fatigue and causes a rapid decline in evoked force, which limits the effectiveness of stimulation therapies [51].
How can improper electrode placement affect my stimulation outcomes? Incorrect electrode placement is a major source of poor outcomes. Placing electrodes in suboptimal locations, often based on generic anatomical charts rather than individual physiology, requires higher current levels to excite motor branches. This not only results in weaker evoked muscle tension but also causes greater excitation of pain-afferent fibers, leading to increased discomfort and poor patient tolerance [52]. The muscle motor point—the skin area where a twitch is evoked with the least current—varies between individuals and can shift with joint movement [52].
My setup is producing a large stimulus artifact that obscures the EMG response. How can I fix this? A large stimulus artifact can be caused by several factors. Systematically check the following: ensure the ground electrode is functioning correctly and has adequate paste; verify that all recording electrodes are defect-free and properly connected; check for an electrode paste bridge between the stimulating electrodes; and ensure that the recording and stimulation cables are not crossed or touching each other [47].
Why is the recorded muscle potential abnormal in voltage? If the recorded potential has an abnormal voltage, try moving the stimulating electrodes in small increments to find the best position over the nerve. Always ensure that the stimulus strength is supramaximal. Also, check the recording electrodes to confirm they are over the appropriate muscle and that the amount of electrode paste is adequate to avoid a "cream bridge" effect [47].
Troubleshooting Guides
Problem 1: Rapid Muscle Fatigue During Sustained Stimulation
- Description: The evoked muscle force decays rapidly during a stimulation session, reducing treatment efficacy.
- Possible Causes & Solutions:
- Cause: Synchronous Activation. Conventional stimulation pulses cause all motor units to fire simultaneously [51].
- Solution: Utilize novel waveform designs. Implement an asymmetric random (aSymR) stimulation waveform, which introduces random fluctuations to reduce the synchronization of axonal activation. Studies show this significantly reduces the muscle fatigue rate compared to symmetric (Sym) stimulation [51].
- Solution: Employ multi-pathway stimulation. Use a multichannel stimulator with electrodes placed over the motor points of different muscles or muscle portions. This allows for asynchronous, non-synchronous activation of different muscle volumes, which delays the onset of fatigue compared to single-channel synchronous stimulation [52].
Problem 2: Excessive Discomfort or Pain During Stimulation
- Description: The subject or patient reports significant pain at the stimulation site, limiting the tolerable intensity and duration of therapy.
- Possible Causes & Solutions:
- Cause: Suboptimal Electrode Placement. Stimulation is causing excessive activation of pain-afferent fibers [52].
- Solution: Identify the individual motor point. Perform an electrophysiological mapping procedure using a pen-electrode to find the skin area above the muscle where the motor threshold is lowest. Placing the electrode on this spot maximizes evoked tension while minimizing the required current and discomfort [52].
- Cause: High-Frequency Stimulation. Certain high-frequency protocols can exacerbate pain [51].
- Solution: Switch to an asymmetric random waveform. Research indicates that an aSymR waveform can achieve reduced muscle fatigue while also relieving the pain associated with other high-frequency stimulation modes [51].
Problem 3: Insufficient or No Muscle Contraction
- Description: Stimulation is delivered, but no visible muscle contraction or evoked force is detected.
- Possible Causes & Solutions:
- Cause: Inadequate Stimulation Parameters or Setup.
- Solution: Follow a systematic checklist:
- Verify the stimulator is delivering an impulse and that all connections are secure.
- Confirm the anatomical location of the stimulating electrodes is correct.
- Check for too much or too little electrode cream; dry the skin if there is a bridge between anode and cathode.
- Increase the stimulus strength and/or duration, which is often necessary in obese individuals, those with edema, or severe nerve disease [47].
- Cause: Incorrect Joint Position. The muscle motor point location changes with muscle length [52].
- Solution: Ensure the muscle length (joint angle) is the same during stimulation as it was during the motor point mapping procedure [52].
Experimental Protocols & Data
Protocol 1: Motor Point Identification for Optimized Electrode Placement
This protocol ensures stimulation electrodes are placed for maximum efficiency and comfort [52].
- Subject Positioning: Position the subject so the target muscle is in a relaxed, neutral state. Note and maintain this joint angle throughout the procedure.
- Electrode Setup: Use a stimulator with a pen-electrode (active, ~1 cm²) and a larger dispersive electrode (~tens of cm²) placed over an antagonist muscle or opposite to the active electrode.
- Stimulation Parameters: Set the stimulator to a low frequency (1-2 Hz) and a pulse width of 100–200 μs. Start with a low current amplitude (e.g., 1 mA).
- Skin Mapping: Gently press the pen-electrode on the skin overlying the target muscle. Hold for 3-5 seconds, then move to an adjacent area.
- Identify Response: Slowly increase the current amplitude in small steps (e.g., 1 mA) and repeat scanning until a clear muscle twitch or tendon movement is observed.
- Refine and Mark: Once a response is found, decrease the current to a level where a minimal twitch is only detectable when the pen-electrode is directly over the motor point. Mark this skin location. This point serves as the centroid for the stimulation electrode.
Protocol 2: Evaluating Waveforms for Reduced Fatigue and Pain
This protocol compares the anti-fatigue performance of different stimulation waveforms [51].
- Subject Preparation: Secure the forearm and attach force transducers to the fingers and high-density EMG electrode arrays over the relevant flexor muscles (e.g., FDS, FDP).
- Stimulation Setup: Place a 2x8 array of stimulation electrodes beneath the short head of the biceps brachii along the median and ulnar nerves.
- Stimulation Paradigm: Apply two different high-frequency narrow pulse cluster waveforms (e.g., Symmetric/Sym vs. Asymmetric Random/aSymR) to the nerve bundle. The stimuli should be calibrated to elicit the same initial contraction level.
- Fatigue Induction: Maintain each stimulation mode for a sustained period (e.g., 5 minutes) to induce muscle fatigue.
- Data Recording: Continuously record finger force, high-density EMG signals, and subjective pain scores throughout the stimulation period.
- Data Analysis: Characterize muscle fatigue by analyzing the force decay rate, absolute force decay, and plateau force. Compare EMG amplitudes and pain scores between the two waveform conditions.
The table below summarizes quantitative findings from recent research on key stimulation strategies:
Table 1: Comparison of Stimulation Strategies for Mitigating Fatigue and Improving Selectivity
| Strategy | Key Parameters | Primary Effect | Quantitative Outcome / Mechanism |
|---|---|---|---|
| Asymmetric Random (aSymR) Waveform [51] | Cluster of narrow pulses, 10 kHz carrier frequency, asymmetric random pattern | Reduces fatigue and pain | Slower force decay rate, greater plateau force, and increased delay for different nerve fibers to reach activation threshold. |
| Multipath/Multi-electrode NMES [52] | Multiple active electrodes over different muscle MPs, asynchronous stimulation | Delays fatigue onset | Activates different muscle volumes asynchronously, preventing repeated activation of the same muscle units. |
| Dorsal Epidural (dEES) vs. Ventral Epidural (vEES) [53] | Monopolar configuration, 50 Hz | Differing selectivity and thresholds | dEES has lower thresholds; vEES achieves higher muscle selectivity via direct motor axon activation. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials and Equipment for Stimulation Optimization Research
| Item | Function / Application |
|---|---|
| Programmable Multi-Channel Stimulator [51] | Allows delivery of complex, customized stimulation waveforms (e.g., aSymR) and multipath stimulation paradigms. |
| Stimulation Pen-Electrode [52] | Crucial for performing precise motor point identification mapping on the skin surface. |
| High-Density EMG (HD-EMG) System [51] | Records spatial distribution of muscle activation, allowing analysis of motor unit recruitment synchronization. |
| Miniature Load Cells / Force Transducers [51] | Precisely measures the evoked contraction force from individual fingers or limbs to quantify fatigue. |
| Finite Element Model & Nerve Fiber Cable Model [51] [53] | Computational tools to simulate extracellular potentials and axon activation, providing mechanistic insights into waveform effects. |
Experimental Workflows and Mechanisms
The diagram below illustrates the experimental workflow for comparing stimulation waveforms.
Waveform Comparison Workflow
This diagram outlines the logical relationship between stimulation strategy, its mechanism of action, and the final physiological outcome.
Strategy and Outcome Mechanism
Addressing Trade-offs Between Spatial Specificity and Stimulation Intensity
Frequently Asked Questions
FAQ 1: What is the fundamental trade-off between spatial specificity and stimulation intensity? In neural stimulation, a fundamental challenge exists where increasing the stimulation intensity to ensure reliable activation of deeper or less accessible neuronal targets often leads to a larger, less focused electric field. This results in the unintended activation of off-target neural populations, thereby reducing spatial specificity. The goal of optimization is to find a stimulation waveform that provides sufficient intensity to activate the desired population while minimizing the spread of activation to adjacent, non-targeted areas [54].
FAQ 2: Why is spatial specificity critical for clinical applications like neuroprosthetics? Spatial specificity is paramount for conveying biologically realistic percepts and for the effective operation of sensory and cortical prostheses. For instance, a prosthetic hand must encode unique signals for various sensations like pressure, texture, and heat. If stimulation is not selective, these distinct sensations cannot be evoked, severely limiting the device's functionality and natural feel. Improved specificity helps in reducing side effects and enhancing the therapeutic efficacy of clinical devices [54].
FAQ 3: How can computational modeling help overcome this trade-off? Computational modeling allows researchers to characterize the effects of key variables, such as stimulus parameters, nanoparticle concentration, and their spatial distribution, on neural activation before conducting physical experiments. For example, in silico models can predict how different concentrations of magnetoelectric nanoparticles (MENPs) influence the electric field distribution and the subsequent likelihood of activating specific axons. This reduces experimental time and resources by focusing in-vivo work on the most promising parameter spaces [55].
FAQ 4: What are the advantages of using novel materials like Magnetoelectric Nanoparticles (MENPs)? MENPs offer a promising path for minimally invasive and highly selective neural stimulation. Once delivered to a target site, these nanoparticles can convert an external magnetic field into a localized electric field, directly stimulating nearby neurons. Their nanoscale size and the ability to be tuned via magnetic fields allow for precise spatial targeting that is difficult to achieve with conventional electrode-based stimulation, potentially offering a better balance between specificity and effective stimulation intensity [55].
FAQ 5: My experimental results are inconsistent across sessions. What could be the cause? Inconsistencies, particularly in techniques like fNIRS, can often be traced to two common issues: variations in probe placement and insufficient signal quality control. Even slight changes in the position of stimulation or recording equipment (e.g., optodes or electrodes) across sessions can lead to measurements from different brain regions. Furthermore, a lack of robust real-time preprocessing to remove noise and artifacts can mean that your system is reacting to non-neural signals, leading to unreliable outcomes [56].
Troubleshooting Guides
Issue 1: Low Selectivity of Electrical Stimuli Problem: Your electrical stimulation protocol is activating a broad, non-specific population of neurons instead of the targeted sub-population. Solution:
- Implement a Closed-Loop Optimization Routine: Use an automated search algorithm, such as Powell’s conjugate direction method, to efficiently find the optimal stimulus waveform [54].
- Exploit Natural Neural Variation: Different neurons have characteristic strength-duration curves. The optimization algorithm should be designed to exploit these differences to find waveform parameters that maximize activation of target neurons while minimizing off-target activation [54].
- Actionable Protocol:
- Define Your Target: Identify the desired activation pattern (e.g., which neurons to activate and which to avoid).
- Choose a Search Algorithm: Implement Powell's method, which is resistant to noise in neuronal responses [54].
- Iterate and Model: In a closed-loop fashion, deliver a stimulus, measure the evoked response, and update the model of neuronal activation. The algorithm uses this model to select the next, potentially more selective, stimulus waveform [54].
Issue 2: Unpredictable Activation with Nanoparticle-Based Stimulation Problem: The stimulation effect of nanoparticles like MENPs is variable and does not consistently evoke a neural response. Solution:
- Systematically Model Concentration and Distribution: Computational studies show that both the concentration (w/v %) and the stochastic spatial distribution of nanoparticles significantly impact the generated electric field and subsequent neural activation [55].
- Actionable Protocol:
- Characterize Single Particle Performance: Use finite element method (FEM) software (e.g., COMSOL Multiphysics) to model the electric potential generated by a single nanoparticle [55].
- Model Multiple Particles: Simulate the aggregate electric field generated by multiple nanoparticles at different concentrations (e.g., 0.1%, 1%, 10% w/v) [55].
- Account for Randomness: Run multiple simulations (e.g., 50 iterations) for each concentration, with nanoparticles randomly distributed within a tissue volume, to statistically assess the probability of successful axonal activation [55].
Issue 3: Poor Spatial Targeting in Functional Brain Imaging (fNIRS) Problem: Inconsistent targeting of specific brain regions across repeated measurement sessions. Solution:
- Improve Anatomical Registration: Use individual MRI data to guide the placement of optodes to ensure they are consistently over the same region of interest (ROI) in every session [56].
- Utilize High-Density Arrays: Employ high-density fNIRS setups, which provide better spatial sampling and can help in discriminating signals from adjacent cortical areas [56].
- Standardize Placement: Use reliable scalp landmarks and measurement procedures. Consider using 3D-printed custom caps that are individually fitted for each subject to ensure repeatable placement [56].
Data Presentation
Table 1: Influence of MENP Concentration on Stimulation Capability
This table summarizes simulation data on how different weight/volume (w/v) concentrations of nanorod-shaped magnetoelectric nanoparticles (NRs) affect their ability to stimulate peripheral nerves. The findings are based on 50 stochastic distributions for each concentration level [55].
| NR Concentration (w/v) | Impact on Electric Field | Stimulation Capability (Myelinated Axons) | Stimulation Capability (Unmyelinated Axons) | Key Interpretation |
|---|---|---|---|---|
| 0.1% | Low magnitude, highly dependent on random particle distribution. | Low | Very Low | Stimulation is unreliable and highly sensitive to the exact spatial arrangement of NRs. |
| 1% | Moderate magnitude, more consistent across different distributions. | Moderate | Low | A practical threshold for more reliable activation may be reached, especially for excitable fibers. |
| 10% | High magnitude, less variability due to averaging effect. | High | Moderate | Higher concentrations significantly increase the probability of activating target axons, including less excitable unmyelinated ones. |
Table 2: Comparison of Neuromodulation Techniques on Key Metrics
This table provides a comparative overview of classical and emerging neuromodulation techniques, highlighting their inherent trade-offs between spatial resolution (specificity) and other factors like invasiveness [57].
| Technique | Spatial Resolution | Invasiveness | Key Mechanism | Primary Trade-off Consideration |
|---|---|---|---|---|
| Deep Brain Stimulation (DBS) | Moderate (mm) | High (surgical implantation) | Electrical stimulation via implanted electrodes. | High invasiveness for direct, deep brain access. |
| Transcranial Direct Current Stimulation (tDCS) | Low (cm) | Non-invasive | Modulation of neuronal membrane potentials via scalp electrodes. | Poor spatial specificity due to diffuse electric fields. |
| Magnetoelectric Nanoparticles (MENPs) | High (µm) | Minimally invasive (injection) | Conversion of magnetic field to localized electric field. | Balance between nanoparticle concentration/distribution and stimulation intensity. |
| Closed-Loop Electrical Optimization | High (single cell possible) | Dependent on electrode placement | Algorithmic search for selective stimulus waveforms. | Requires real-time feedback and is constrained by the natural differences in neuronal excitability. |
Experimental Protocols
Protocol 1: Powell's Conjugate Direction Method for Waveform Optimization
This protocol details the closed-loop methodology for optimizing stimulus waveform parameters to achieve selective neuronal activation [54].
1. System Setup:
- Hardware: Prepare a microelectrode array (MEA) with cultured neurons. You will need a stimulator (e.g., STG-2004) and an amplifier (e.g., MEA-1060-Up-BC) for delivering biphasic current pulses. Use optical imaging (e.g., calcium imaging) for measuring neuronal responses [54].
- Software: Use a programming environment (e.g., MATLAB) to control hardware synchronization, data acquisition, and implement the Powell's method algorithm [54].
2. Initialization:
- Define the stimulus parameter space to be searched (e.g., pulse amplitude and pulse width).
- Choose an initial guess for the stimulus waveform.
- Define the selectivity function, which quantifies the goal of activating target neurons while sparing non-target neurons [54].
3. Closed-Loop Execution:
- Stimulate: Deliver the selected stimulus waveform to the culture via a designated electrode.
- Measure: Record the evoked response from multiple neurons simultaneously using optical imaging.
- Update Model: Fit a sigmoid activation model and strength-duration curve to the measured response data for each neuron.
- Search: Apply Powell's conjugate direction method to determine the next set of stimulus parameters that is predicted to improve selectivity.
- Iterate: Repeat the Stimulate-Measure-Update-Search cycle until the selectivity function is maximized or converges [54].
Protocol 2: In Silico Analysis of MENP Concentration and Distribution
This protocol describes a computational framework to quantify how MENP concentration and spatial distribution affect neural activation [55].
1. Single Particle Multiphysics Modeling:
- Software: Use a finite element method (FEM) simulator like COMSOL Multiphysics.
- Model Geometry: Create a model of a single nanorod-shaped MENP (e.g., Cobalt Ferrite core, Barium Titanate shell) embedded in a volume representing biological tissue.
- Physics Setup: Configure the model to characterize the direct magnetoelectric effect, applying an external magnetic field to calculate the resulting electric potential on the nanoparticle's surface [55].
2. Multi-Particle Electric Field Simulation:
- Define a Volume: Model a small volume of neural tissue (e.g., within a fascicle).
- Stochastic Distribution: For a chosen concentration (e.g., 1% w/v), randomly distribute a corresponding number of NR models within the tissue volume. Repeat this to create multiple (e.g., 50) unique spatial configurations.
- Solve: For each configuration, simulate the aggregate electric field generated by all NRs within the tissue [55].
3. Hybrid Neuronal Response Modeling:
- Integrate with Neuronal Models: Import the computed electric field maps into a neural simulation environment (e.g., NEURON).
- Simulate Axonal Response: Use detailed biophysical models of different axon types (myelinated and unmyelinated) to calculate the membrane response and determine if the MENP-induced electric field is sufficient to trigger an action potential.
- Quantify Success: Across all stochastic distributions, calculate the percentage that led to successful activation for each axon type and concentration [55].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Benefit |
|---|---|
| Microelectrode Array (MEA) | Provides a high-density grid of electrodes for simultaneous stimulation and recording from multiple sites in a neuronal culture [54]. |
| Magnetoelectric Nanoparticles (MENPs) | Core-shell nanoparticles (e.g., CFO-BTO) that convert an applied magnetic field into a localized electric field, enabling wireless and precise neuromodulation [55]. |
| COMSOL Multiphysics Software | A finite element analysis tool for simulating the multiphysics behavior of MENPs, including magnetoelectric coupling and the resulting electric field distributions in tissue [55]. |
| Powell's Conjugate Direction Algorithm | A deterministic optimization algorithm used in closed-loop systems to efficiently search through multi-dimensional parameter spaces (e.g., stimulus waveforms) to find a maximum (e.g., for selectivity) [54]. |
| Strength-Duration Curve Model | A two-parameter mathematical model (threshold vs. amplitude and pulse width) that describes the activation probability of a neuron in response to a rectangular current pulse. Essential for modeling the input-output relationship in optimization routines [54]. |
Workflow and Signaling Diagrams
Optimization Workflow
MENP Signaling
Comparative Analysis and Validation of Stimulation Technologies
The following table summarizes the core performance characteristics of Dorsal (dEES) and Ventral (vEES) Epidural Electrical Stimulation, highlighting their distinct mechanisms and outcomes.
| Performance Characteristic | Dorsal Epidural Stimulation (dEES) | Ventral Epidural Stimulation (vEES) |
|---|---|---|
| Primary Neural Target | Aα-sensory fibers in the dorsal root [58] | α-motor fibers in the ventral root [58] |
| Activation Mechanism | Indirect, polysynaptic; modulates spinal circuits [58] [59] | Direct, non-synaptic; bypasses spinal circuits [58] |
| Activation Threshold | Lower [58] | Higher [58] |
| Saturation Amplitude | Lower [58] | Higher [58] |
| Muscle Selectivity | Lower [58] | Higher [58] |
| Typical Role in Therapy | Neuromodulation; promotes network plasticity and long-term recovery [59] | Direct muscle control; provides immediate muscle recruitment [58] |
Mechanisms of Action: Signaling Pathways
Dorsal and ventral epidural stimulation engage the spinal cord through fundamentally different neural pathways.
Pathway Explanation: The dorsal approach (dEES) provides indirect, polysynaptic activation by first stimulating sensory fibers, which then synaptically drive motor neurons via spinal interneurons. This process preserves natural intraspinal circuitry and promotes plasticity [58] [59]. In contrast, the ventral approach (vEES) bypasses spinal circuits entirely by directly depolarizing motor neuron axons, resulting in immediate, non-physiological muscle recruitment that can lead to faster fatigue without interleaved stimulation [58].
Experimental Protocols for Performance Comparison
Computational Modeling of Stimulation Effects
Objective: To quantitatively compare activation thresholds, saturation amplitudes, and selectivity indices for dEES and vEES using a validated computational model [58].
Materials:
- Software: COMSOL Multiphysics (v.6.0) or equivalent finite element analysis software [58]
- Model: 3D rat spinal cord model (L2-S1 segments) incorporating gray matter, white matter, roots, CSF, and surrounding tissues [58]
- Nerve Fibers: Integrated models of Aα-sensory and α-motor fibers with appropriate diameter and trajectory [58]
Workflow: The experimental workflow for computational comparison involves sequential modeling stages from geometry creation to quantitative analysis.
Methodology Details:
- Volume Conductor Model: Develop a geometrically accurate model of the lumbosacral enlargement (L2-S1) including distinct tissue compartments with anisotropic conductivity values [58].
- Electrode Configuration: Simulate three stimulation modes for both dorsal and ventral placements:
- Monopolar (5 configurations)
- Bipolar (10 configurations)
- Tripolar (10 configurations) Electrode dimensions: 1000 μm × 300 μm, placed at the center of each spinal segment [58].
- Physics Setup: Apply the quasi-static approximation to solve Laplace's equation for potential distribution: ( \overrightarrow{\nabla} \cdot (\sigma \overrightarrow{\nabla} V) = 0 ) [58]
- Analysis: Calculate activation thresholds for target muscles (e.g., Vastus Medialis, Semitendinosus), determine saturation amplitudes, and compute selectivity indices for each configuration [58].
In Vivo Electrophysiological Validation
Objective: To empirically validate computational predictions of differential muscle recruitment and selectivity using electromyographic (EMG) recordings.
Materials:
- Animal Model: Rat model of spinal cord injury
- Electrodes: Implanted epidural electrode arrays for both dEES and vEES
- Recording System: Multi-channel EMG system for simultaneous recording from antagonistic muscle pairs (e.g., Tibialis Anterior and Gastrocnemius) [58]
Protocol:
- Surgical Preparation: Implant stimulating electrodes on both dorsal and ventral aspects of the spinal cord at lumbosacral segments [58].
- EMG Electrode Placement: Insert fine-wire EMG electrodes into target hindlimb muscles.
- Stimulation Protocol: Apply graded stimulation intensities (0-500 μA) across different electrode configurations (monopolar, bipolar, tripolar) for both dEES and vEES.
- Data Collection: Record compound muscle action potentials (CMAPs) from all target muscles simultaneously.
- Data Analysis: Calculate motor thresholds, recruitment curves, and selectivity indices (ratio of target to non-target muscle activation) for each condition.
Quantitative Performance Data
Electrode Configuration Comparison
The following table summarizes how different electrode configurations affect key stimulation parameters based on computational modeling data [58].
| Electrode Configuration | Effect on Current Density | Impact on Thresholds | Effect on Selectivity |
|---|---|---|---|
| Monopolar | Focused at single segment | Lower thresholds | Higher target muscle selectivity |
| Bipolar | Dispersed across two segments | Moderate thresholds | Reduced selectivity vs. monopolar |
| Tripolar | Widely dispersed across multiple segments | Higher thresholds | Lowest selectivity |
Stimulation Parameter Optimization
The following table summarizes the effects of key stimulation parameters based on experimental findings from both animal and human studies [58] [60].
| Stimulation Parameter | Effect on Neural Activation | Impact on Selectivity | Clinical/Research Consideration |
|---|---|---|---|
| Frequency (50-100 Hz) | Higher frequencies in dEES reduce required intensity [58] | Minimal direct effect on selectivity [58] | 50 Hz commonly used for robust, fatigue-resistant activation [58] |
| Pulse Width | Narrow pulse widths require higher amplitudes [33] | Influences spatial spread of activation [33] | Determines how broadly stimulation is felt [33] |
| Waveform Type | Monophasic vs. biphasic affects membrane polarization [60] | Alters muscle recruitment patterns [60] | Charge-balanced waveforms recommended for safety [60] |
| Carrier Frequency (1-10 kHz) | Higher frequencies increase tolerance but require more current [60] | Higher frequencies (>5 kHz) activate fewer muscles [60] | Can improve comfort but reduces efficiency [60] |
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function/Application | Example Use Case |
|---|---|---|
| Finite Element Modeling Software | Simulates electric field distribution in complex spinal cord geometries [58] | Predicting neural activation thresholds for novel electrode designs [58] |
| Multi-Channel Electrophysiology System | Records simultaneous EMG responses from multiple muscles [58] | Quantifying selectivity indices across muscle groups during stimulation [58] |
| Epidural Electrode Arrays | Delivers precisely controlled electrical stimulation to spinal targets [58] | Comparing dEES vs. vEES in animal models of spinal cord injury [58] |
| Computational Neuron Models | Simulates responses of different fiber types to applied electric fields [61] | Testing mechanisms of dorsal horn interneuron polarization [61] |
Troubleshooting Guides & FAQs
Problem: Inadequate Muscle Recruitment
Possible Causes and Solutions:
- Cause #1: Suboptimal electrode configuration. Solution: Test multiple configurations (monopolar, bipolar, tripolar); monopolar typically provides highest selectivity [58].
- Cause #2: Stimulation intensity below threshold. Solution: Systematically increase amplitude while monitoring EMG responses; vEES typically requires higher intensities than dEES [58].
- Cause #3: Incorrect electrode placement. Solution: Verify placement using imaging; for leg muscles, electrodes should be positioned at lumbosacral enlargement [59].
Problem: Poor Muscle Selectivity
Possible Causes and Solutions:
- Cause #1: Current spread to non-target segments. Solution: Use focused multipolar configurations or reduce stimulation intensity [58].
- Cause #2: Incorrect pulse width setting. Solution: Narrow pulse widths may improve selectivity but require higher amplitudes [33].
- Cause #3: Suboptimal frequency parameters. Solution: Higher carrier frequencies (>5 kHz) may reduce off-target activation but require more current [60].
Problem: Rapid Muscle Fatigue During vEES
Possible Causes and Solutions:
- Cause: Non-physiological recruitment order with direct motor axon activation. Solution: Implement interleaved stimulation across multiple sites to mitigate fatigue [58].
Frequently Asked Questions
Q: What are the key anatomical differences that explain the performance variations between dEES and vEES? A: The dorsal roots contain sensory nerve fibers (Aα-sensory fibers) that enter the spinal cord, while the ventral roots contain motor fibers (α-motor fibers) that exit the spinal cord. Additionally, the ventral white matter is thicker than the dorsal white matter, causing greater attenuation of currents applied from the ventral side. The different curvature trajectories of these fiber types also significantly impact threshold and selectivity outcomes [58].
Q: How does stimulation frequency affect selectivity in dEES and vEES? A: Stimulation frequency has little direct effect on selectivity in both dEES and vEES. However, in dEES, higher frequencies can reduce the stimulation intensity required to achieve maximum selectivity [58].
Q: What is the recommended workflow for optimizing stimulation parameters in a new experimental setup? A: Begin with systematic testing at fixed pulse width and frequency while varying electrode configurations, starting with monopolar configurations first. Methodically test different contacts while carefully documenting reported sensations or EMG responses to define optimal multicolumn contact configurations [33].
Q: Why might vEES be preferred despite its higher activation threshold? A: vEES achieves significantly higher muscle selectivity, which is critical for precise motor control applications. This higher selectivity may justify the increased power requirements in scenarios where targeted muscle activation is the primary research or therapeutic objective [58].
Evaluating Conventional Monopolar Stimulation Against Novel Multi-Electrode Configurations
Frequently Asked Questions
Q1: What are the primary functional differences between monopolar and bipolar electrode configurations?
Monopolar and bipolar configurations differ fundamentally in how electrical current flows, which directly impacts stimulation efficiency and focality.
- Monopolar Configuration: Uses a single active electrode near the target tissue and a distant reference electrode (often a grounding pad on the skin). Current flows from the active electrode through the body to the distant reference. This configuration is generally more robust and effective for stimulating larger areas but offers less focused stimulation [62] [63].
- Bipolar Configuration: Uses two closely spaced electrodes where one acts as the stimulation source and the other as the reference. Current flows primarily through the tissue between these two adjacent points. This configuration confines the electric field to a more localized region, typically resulting in more selective or focal stimulation, though it may be less efficient for activating broad neural populations [62] [63].
Q2: My computational models are slow, making large-scale parameter sweeps impractical. What solutions exist?
Computational bottlenecks are a major challenge in neural stimulation optimization. A highly effective solution is to use machine learning-generated surrogate models. These are simplified, data-driven models that emulate the behavior of complex, biophysically realistic models (like the MRG nerve fiber model implemented in NEURON) but run orders of magnitude faster.
- Solution: Implement a GPU-accelerated surrogate model. For example, the S-MF ("smurf") surrogate model of the MRG fiber can generate spatiotemporal responses to electrical stimulation with a speedup of 2,000 to 130,000 times compared to single-core NEURON simulations, while maintaining high predictive accuracy (R² = 0.999 for activation thresholds) [6]. This allows for rapid large-scale parameter exploration and sophisticated optimization that was previously computationally prohibitive.
Q3: How does electrode geometry influence stimulation efficiency and selectivity?
Electrode shape and size are critical design parameters that directly affect performance [63].
- Stimulation Efficiency: Sharper electrodes and smaller electrodes generally enhance stimulation efficiency. This reduces the power required to activate neurons, which is crucial for miniaturized and implantable devices.
- Stimulation Focality: Sharper electrodes can also help localize activation. Furthermore, for most shapes, a bipolar configuration stimulates neurons more locally compared to a monopolar configuration.
The table below summarizes the integrative effects of electrode design on stimulation outcomes:
Table 1: Impact of Electrode Parameters on Stimulation Performance [63]
| Parameter | Impact on Stimulation Efficiency | Impact on Stimulation Focality |
|---|---|---|
| Sharpness | Enhanced with sharper electrodes | Improved with sharper electrodes |
| Size | Enhanced with smaller electrodes | Varies with configuration |
| Configuration | Bipolar with <1mm separation is more efficient than monopolar; Bipolar with >100µm center-to-vertex distance shows enhanced efficiency | Bipolar configuration is generally more focal than monopolar |
Q4: What precautions are necessary when using monopolar electrocoagulation near implanted electronic devices like cochlear implants?
Monopolar electrocoagulation carries a high risk of damaging nearby implanted electronic devices because the electrical current can travel through the body and induce damaging voltages in the implant's internal components [62].
- Primary Precaution: Whenever possible, use bipolar electrocoagulation instead, as it confines the current flow to a very localized area between the two tips of the forceps, significantly reducing the risk to the implant.
- If Monopolar is Medically Necessary: If monopolar coagulation is essential for the procedure (e.g., for major spinal surgery), strict safety measures must be implemented [62]:
- The patient's head (where the cochlear implant is located) should be isolated on a non-conductive substrate.
- The coagulation should be applied as far from the implant coil and electrodes as possible (e.g., below the Th3 segment for spinal surgery).
- Use the lowest effective power setting (e.g., 30W).
- Perform pre- and post-operative device checks, including electrode impedance and neural response telemetry (NRT).
Troubleshooting Guides
Issue 1: Poor Stimulation Selectivity
Problem: The electrical stimulation is activating off-target neurons or fascicles instead of being confined to the specific target region.
Possible Causes and Solutions:
- Cause: Inappropriate Electrode Configuration.
- Solution: Switch from a monopolar to a bipolar configuration. Computational studies show that bipolar configurations typically provide more localized stimulation, confining the activation field between the two electrodes [63].
- Cause: Suboptimal Electrode Geometry.
- Solution: Redesign electrodes to be sharper and smaller. Modeling data indicates that sharper electrodes with higher perimeter-to-area ratios (e.g., fractal or serpentine designs) can locally activate neurons and improve stimulation efficiency [63].
- Cause: Non-optimized Stimulation Waveform.
- Solution: Use intelligent optimization algorithms to tailor the temporal waveform. Research in transcranial magnetic stimulation (TMS) has shown that using particle swarm optimization (PSO) to design multi-level waveforms can significantly improve the selectivity index, activating target regions while minimizing off-target activation [9].
Issue 2: Inaccurate or Slow Computational Predictions
Problem: Simulations do not match experimental outcomes, or the computational time is too long for practical design cycles.
Possible Causes and Solutions:
- Cause: High Computational Cost of Biophysical Models.
- Solution: Replace high-fidelity models (e.g., in NEURON) with a machine learning-based surrogate model for rapid parameter screening. Frameworks like AxonML and models like S-MF run on GPUs and can achieve speedups of over 10,000x while maintaining high accuracy in predicting spatiotemporal responses and activation thresholds [6].
- Cause: Inaccurate Activation Threshold Predictions.
- Solution: Ensure your computational model accounts for the full nonlinear neural response. Simple threshold estimators can have large errors (>150%). The S-MF surrogate model, which is trained on full MRG model data, achieves a mean absolute percentage error (MAPE) of less than 2.5% across various fiber diameters and waveforms [6].
Experimental Protocols & Data
Protocol 1: Computational Workflow for Evaluating Electrode Configuration Performance
This protocol outlines a methodology for comparing monopolar and bipolar configurations using finite element method (FEM) simulations [63].
- Model Construction: Build a 2-D or 3-D model of the electrode and the surrounding neural tissue (e.g., gray matter) in a simulation environment like COMSOL.
- Parameter Definition: Define the electrode parameters:
- Shape: Model as regular polygons with varying numbers of edges (e.g., 4, 6, 8, 10).
- Size: Define by center-to-vertex distance (e.g., 50, 100, 500, 1000 µm).
- Configuration: Model both monopolar and bipolar setups. For bipolar, set the separation distance between electrodes (e.g., 0.25, 0.5, 1, 2 mm).
- Simulation Setup: Assign a cathodic stimulus (e.g., -1 V) to the active electrode. Set the reference electrode to 0 V (bipolar) or set the model boundary as ground (monopolar). Use a fine mesh for discretization.
- Solve and Analyze: Solve for the electric potential (V) and electric field (E = -∇V). Calculate the Activation Function (AF), which predicts where a neuron will be activated, using the formula: ( AF = \sqrt{ \left( -\frac{\partial Ex}{\partial x} \right)^2 + \left( -\frac{\partial Ey}{\partial y} \right)^2 } ) [63].
- Quantify Metrics:
- Stimulation Efficiency: Use the magnitude of the AF.
- Stimulation Focality: Calculate the Full Area at Half Maximum (FAHM) of the AF, which represents the area of neural tissue that exceeds the activation threshold.
Protocol 2: Intelligent Optimization of Stimulation Waveforms
This protocol describes how to optimize waveforms for selective activation using intelligent algorithms, as demonstrated in TMS research [9].
- Define the Optimization Goal: Establish a quantitative selectivity index. For example: ( f1 = \frac{\sum threshEs_ROIi}{\sum threshEsi} ), where a smaller ( f1 ) indicates better selectivity (ROI = Region of Interest) [9].
- Parameterize the Waveform: Represent the stimulation waveform using a flexible parametrization. For a multi-level waveform, parameters can include the voltage amplitude (V1-V4) and pulse width (pw1-pw4) for each level.
- Set up the Neuron Model: Use a multi-scale neuron model embedded in a realistic tissue geometry (e.g., from an MRI) to simulate the response to the parameterized waveform.
- Run the Optimization Algorithm: Employ an algorithm like Particle Swarm Optimization (PSO). The PSO will iteratively search for the waveform parameters (VC1, VC2, V1, V2, pw1, pw2, etc.) that minimize the selectivity index ( f_1 ).
- Validate the Optimized Waveform: Test the final waveform from the optimization process in the neuron model to confirm improved selectivity and record other key metrics like required stimulation intensity and coil heating.
Table 2: Quantitative Comparison of Monopolar vs. Bipolar Configuration [63]
| Performance Metric | Monopolar Configuration | Bipolar Configuration |
|---|---|---|
| Stimulation Efficiency | Less efficient for small separations | More efficient when electrode separation is < 1 mm |
| Stimulation Focality | Less focal; broader activation area | More focal and selective in most cases |
| Typical Use Cases | Cochlear implants, stimulating larger areas [63] | Selective stimulation for neuroscience research, microstimulation [63] |
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Tools for Computational Optimization of Neural Stimulation
| Item / Solution | Function / Description | Example Use in Research |
|---|---|---|
| AxonML Framework | A framework for implementing and efficiently executing GPU-based models of peripheral nerve fibers [6]. | Provides the foundation for high-throughput surrogate models like S-MF, enabling large-scale parameter sweeps and optimization. |
| S-MF Surrogate Model | A machine learning-based surrogate of the MRG myelinated fiber model. Offers a massive speedup (>>1000x) while retaining high accuracy [6]. | Used for rapid prediction of neural responses (activation, block) to a wide variety of stimulation protocols and for optimizing selective VNS. |
| Multi-Scale Neuron Model | A model that incorporates realistic neuron morphology and distribution within a tissue model derived from medical imaging (e.g., MRI) [9]. | Provides a biologically grounded platform to evaluate the effects of different electric field waveforms on neuronal populations for TMS and other applications. |
| Particle Swarm Optimization (PSO) | An intelligent optimization algorithm that searches for optimal parameters by simulating the social behavior of a flock of birds [9]. | Used to find the best waveform parameters (e.g., from a multi-level discharge circuit) that maximize a selectivity index in stimulation. |
| Activation Function (AF) | A mathematical function derived from the second spatial derivative of the extracellular electric potential; it predicts where an axon is most likely to be activated by extracellular stimulation [63]. | A key metric in computational studies to quickly assess and compare the efficiency and focality of different electrode designs and configurations without running full neural simulations. |
Visualized Workflows and Relationships
The following diagram illustrates the core computational workflow for optimizing stimulation parameters, integrating both electrode configuration and waveform design.
This diagram outlines the logical relationship between key concepts in electrode design and its impact on experimental outcomes.
Fundamental Principles and Mechanisms
What are the core mechanistic differences between TI and conventional kHz stimulation?
The fundamental difference lies in how each technique modulates neural activity. Temporal Interference Stimulation (TIS) relies on the interference pattern created by multiple high-frequency electric fields, while conventional kHz stimulation uses single-source high-frequency trains to directly interact with neural membranes.
Table 1: Core Mechanism Comparison
| Feature | Temporal Interference (TIS) | Conventional kHz Stimulation |
|---|---|---|
| Primary Mechanism | Interference of multiple kHz fields (e.g., 2 kHz & 2.01 kHz) creates low-frequency envelope (e.g., 10 Hz) at target [64] | Direct application of single-source kHz-frequency trains (e.g., 1-10 kHz) [21] [25] |
| Neural Target Specificity | Focality achieved through interference pattern focusing on deep brain regions [64] [65] | Fiber-type selectivity based on size and myelination; can block conduction in larger fibers [21] |
| Neural Response | Low-frequency envelope modulates neural activity in deep brain areas [64] | Can activate or block conduction depending on parameters; may preferentially activate C-fibers at specific intensities [21] |
| Spatial Precision | Can target deep brain structures non-invasively; requires individual optimization for focal stimulation [64] [65] | Typically requires implanted electrodes; precision depends on electrode placement and waveform parameters [21] [6] |
Figure 1: Mechanism pathways for TI and conventional kHz stimulation
Troubleshooting Common Experimental Challenges
Why does my TI stimulation lack focality across different subjects?
Inter-individual variability in head anatomy and tissue conductivity significantly affects TI focality. Using a common electrode montage across different subjects can reduce focality by up to 4.4 cm compared to individually optimized montages [65]. The non-linear nature of TI physics means that small changes in montage can cause focality variations up to 9.3 cm [65].
Solution: Implement individual optimization for each subject using computational head models based on individual anatomy. Use electrode arrays rather than simple electrode pairs to improve optimization potential [65].
How can I achieve selective activation of specific fiber types?
Conventional kHz stimulation can achieve selective activation through parameter optimization. In vagus nerve stimulation, intermittent kHz trains (≥5 kHz) at specific intensity ranges (7-10× threshold in rats; 15-25× threshold in mice) can activate small, unmyelinated C-afferents while blocking larger A- and B-fibers [21].
Table 2: Selective Activation Parameters
| Fiber Type | Diameter | Conduction Speed | Selective kHz Parameters | Physiological Role |
|---|---|---|---|---|
| C-afferents | 0.2-1.5 μm | 0.2-2 m/s | 5-10 kHz, 7-25× threshold intensity [21] | Sensory arc for gut, lungs, heart, immune system [21] |
| A/B-fibers | Larger diameters | Faster conduction | Blocked at above parameters [21] | Motor functions and faster signal transmission |
| Myelinated fibers | 6-14 μm | Variable | Responsive to TI stimulation envelope [64] [6] | Various CNS and PNS functions |
Why do I observe inconsistent neural responses to kHz stimulation?
Neural responses to electrical stimulation are highly nonlinear and influenced by multiple factors including waveform shape, amplitude, frequency, electrode-tissue interface, and neuronal biophysics [6]. Single neurons show heterogeneous responses even to the same stimulation parameters, with some displaying immediate calcium increases and others showing decreases [25].
Solution: Use computational models to predict responses across the parameter space. The S-MF (surrogate myelinated fiber) model can accurately predict activation thresholds with <2.5% mean absolute percentage error while providing 2,000-130,000× speedup over conventional methods [6].
Experimental Protocols and Methodologies
Protocol: Measuring Cellular Responses to kHz Stimulation Using Calcium Imaging
This protocol enables quantification of single-neuron responses to electrical stimulation while avoiding electrical artifacts [25].
Figure 2: Calcium imaging protocol for kHz stimulation
Key Parameters:
- Stimulation waveforms: Current-controlled cathode-leading biphasic square waves
- Frequencies: 40 Hz (200 μs/phase), 140 Hz (200 μs/phase), 1 kHz (45 μs/phase)
- Charge density limits: Below tissue-damaging threshold (≤276.3 μC/cm²/phase for lower frequencies) [25]
Protocol: Stimulation Artifact Suppression for Early Spike Recovery
Stimulation artifacts can obscure neural responses for milliseconds to hundreds of milliseconds after stimulation [66]. This protocol enables recovery of neural spikes within 2 ms post-stimulation.
Hardware Configuration:
- Use DC-coupled low gain amplifier (e.g., Gain 10 V/V, AD823)
- Implement 1st order low-pass filter (f_c = 8 kHz)
- Use 24-bit ADC system for wide dynamic range [66]
Software Processing:
- Apply digital filtering to remove slowly decaying baseline
- Use artifact subtraction algorithms (SALPA, RLOESS, or L1 trend filtering)
- Template subtraction method effective when all artifacts share similar underlying shape [67] [66]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Computational Tools
| Tool/Reagent | Function/Purpose | Example Applications | Key Features |
|---|---|---|---|
| GCaMP7f | Genetically encoded calcium indicator for monitoring neural activity | Cellular calcium imaging during electrical stimulation [25] | Enables optical measurement free from electrical artifacts |
| AxonML Framework | GPU-based modeling of peripheral nerve fibers [6] | Optimization of stimulation parameters for selective activation | 2,000-130,000× speedup over NEURON simulations |
| S-MF (Surrogate Myelinated Fiber) | Simplified cable model with non-linear ionic conductances [6] | Predicting neural responses to various stimulation protocols | High predictive accuracy (R² = 0.999 for thresholds) |
| Dual-Mode Stimulation Buffers | Can operate in voltage-only or current/voltage controlled modes [68] | Precise electrical stimulation with controlled parameters | Prevents Faradaic processes by controlling electrode voltage |
| Custom Tripolar Cuff Electrodes | Neural interface for stimulation and recording [21] | Selective vagus nerve stimulation studies | Low impedance contacts (0.5-1.5 kΩ); stable stimulation characteristics |
Frequently Asked Questions
Can kHz stimulation truly activate neurons despite the neural membrane low-pass filtering?
Yes, experimental evidence confirms that 1 kHz stimulation evokes robust cellular responses in awake mice. Calcium imaging shows precisely timed somatic calcium changes in many individual neurons comparable to conventional 40 Hz and 140 Hz stimulation [25]. However, the population-level dynamics differ, with 1 kHz producing more balanced excitatory and inhibitory effects in cortex compared to conventional frequencies [25].
What is the maximum temporal precision I can achieve when recording post-stimulation neural responses?
With optimized hardware and signal processing, neural responses can be recorded as early as 2 ms after the stimulus at the stimulating electrode itself [66]. Key requirements include:
- DC-coupled low gain amplifier configuration
- High-resolution (24-bit) ADC system
- Advanced artifact subtraction algorithms (SALPA, RLOESS, or L1 trend filtering)
How critical is individual optimization for TI stimulation?
Extremely critical. Using a common montage across different individuals can reduce focality by up to 4.4 cm compared to individually optimized montages [65]. The optimization should account for individual head anatomy, tissue conductivity, and target location. Computational models predict that focality variability can reach 1.2 cm at the same target across 25 subjects due to inter-individual differences [65].
What computational tools can accelerate stimulation parameter optimization?
The AxonML framework with S-MF models provides several-orders-of-magnitude improvement in computational efficiency while maintaining high predictive accuracy [6]. These tools enable large-scale parameter sweeps and sophisticated optimization of waveform shape, amplitude, frequency, and active contact configuration for selective activation.
Validating Computational Predictions with In Vivo Electrophysiological Recordings
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
FAQ 1: What are the most critical steps to ensure a successful validation of my computational model against in vivo data? A successful validation hinges on several key steps. First, ensure your computational model is calibrated with high-fidelity to clinically observable data, a process that should be streamlined and automated for reliability [69]. Second, carefully select your in vivo electrophysiological recording protocols (e.g., VEPs, EEPs) to match the specific physiological process your model predicts [69] [70]. Finally, employ a robust optimization framework, such as Particle Swarm Optimization (PSO), to iteratively adjust model parameters to minimize the discrepancy between predicted and recorded signals [9].
FAQ 2: My in vivo recorded signals show high variability. How can I determine if this is biological noise or a flaw in my computational prediction? High variability can stem from multiple sources. Begin by ensuring your data acquisition quality is optimal; for electrophysiological signals, use cepstral analysis or similar methods to quantify recording quality [69]. Furthermore, incorporate the known variability of human anatomy and physiology into your computational framework. Using virtual cohorts or digital twin models that capture patient variability can help distinguish between model inaccuracies and expected biological differences [69] [71]. Running your model with a population of inputs, rather than a single average, can provide a range of predicted outcomes for more robust comparison.
FAQ 3: How can I optimize stimulation waveforms for selective neural activation, and what metrics should I use for validation? Optimizing waveforms requires a defined optimization objective and a flexible parametrization of the waveform. Define a selectivity index that quantifies the precision of activation in your target region versus non-target areas [9]. Then, use an intelligent algorithm like PSO to find waveform parameters that minimize this index [9]. For validation, key metrics include the stimulation threshold required to activate target neurons, the spatial spread of activation measured via cortical potentials, and the energy efficiency (heat dissipation) of the waveform [9] [10] [45].
FAQ 4: What are the advantages of combining AI with traditional biophysical models for prediction validation? The combination of "fuzzy" AI and "exact" biophysics can yield powerful new insights. AI and machine learning are excellent at uncovering patterns in new or unstructured data, which can help in generating hypotheses or processing complex experimental recordings [69] [71]. Meanwhile, biophysical models provide a mechanistic understanding of the underlying processes. AI can also augment digital twins by generating data required for personalization that may not be directly available from a specific individual, thus enhancing the validation process [69].
Troubleshooting Common Experimental Issues
Issue 1: Low Signal-to-Noise Ratio in Cortical Recordings
- Problem: Electrically Evoked Potentials (EEPs) or Visual Evoked Potentials (VEPs) are obscured by noise, making it difficult to compare with computational predictions.
- Solution:
- Verify Electrode Impedance: Prior to recording, measure electrode-retinal impedance in real-time using a potentiostat. An impedance value between 5–8 kΩ has been correlated with proper electrode placement and better signal quality in retinal stimulation studies [45].
- Optimize Signal Processing: Employ a band-pass filter (e.g., 0.3–300 Hz for EEPs) during acquisition [45]. For post-processing, use cepstral analysis to quantify the periodicity and quality of your signal [69].
- Averaging: For transient responses like VEPs, ensure the stimulation rate is sufficiently slow so each response completes before a new stimulus begins, and average multiple repetitions to enhance the signal [70].
Issue 2: Discrepancy Between Predicted and Actual Spatial Spread of Activation
- Problem: Your computational model predicts a confined area of neural activation, but in vivo recordings (e.g., cortical LFP maps) show a much broader and diffuse activation pattern.
- Solution:
- Check Stimulation Parameters: Adjust key stimulation parameters. Longer phase durations (e.g., 1000–1500 µs) and the inclusion of an interphase interval (IPI) have been shown to result in a more confined spread of cortical activation [45].
- Calibrate the Neuron Model: Ensure your multi-scale neuron model incorporates real anatomical data, such as neuron morphology and coordinates from MRI, and is embedded into a realistic cortical grid to accurately simulate the electric field distribution [9].
- Validate with Simple Protocols: Before testing complex waveforms, validate your setup with standard protocols (e.g., pattern-reversal VEPs) which have well-established normative waveform characteristics and peak times [70].
Issue 3: High Energy Loss and Coil Heating in Magnetic Stimulation Experiments
- Problem: The optimized stimulation waveform effectively activates the target region but causes excessive coil heating, making it unsuitable for prolonged or repetitive protocols.
- Solution:
- Optimize for Energy Efficiency: Incorporate energy loss, calculated as ( W_{heat} = \int RI^{2} dt ), as a direct constraint in your waveform optimization framework [9].
- Explore Asymmetric Waveforms: Move beyond traditional symmetric pulses. Research shows that optimized, highly asymmetric electric field pulses can achieve up to 92% reduction in energy loss compared to conventional monophasic pulses while maintaining directional selectivity [10].
Issue 4: Failure to Replicate Selective Activation in Disease Models
- Problem: A stimulation strategy that works in a healthy animal model fails to produce selective activation in a model of disease (e.g., retinal degeneration).
- Solution:
- Re-baseline Stimulation Thresholds: Recognize that disease pathophysiology alters stimulation thresholds. Perform in vivo experiments in both healthy and diseased models to establish new baseline parameters [45].
- Re-optimize Parameters for Disease State: Do not rely on parameters optimized for healthy tissue. Use your computational framework to re-optimize phase duration, frequency, and IPI specifically for the degenerated tissue, as the charge thresholds and cortical activation patterns will differ [45].
Experimental Protocols for Key Experiments
Protocol 1: In Vivo Validation of Retinal Stimulation Efficiency
This protocol details the methodology for assessing the effect of electrical stimulation parameters on visual cortex activation in rodent models, adapted from in vivo studies on retinal degenerated rats [45].
- Objective: To optimize key electrical stimulation parameters (phase duration, frequency, interphase interval) for enhancing visual cortex activation via epiretinal stimulation.
- Animals: Adult wild-type (e.g., Long-Evans) and retinal degenerated (e.g., F1) rats.
- Preparative Surgery:
- Anesthetize animals and secure in a stereotaxic device.
- Epiretinal Electrode Implantation: Incise the sclera and insert a bipolar concentric stimulating electrode (e.g., Pt/Ir, 75 µm diameter) into the ventral-temporal region of the retina. Use an articulated holder for precision.
- Impedance Monitoring: Continuously monitor electrode-retinal impedance with a potentiostat (e.g., 10-mV AC sinusoid at 100 kHz). An impedance of 5–8 kΩ indicates optimal proximity to the epiretinal surface [45].
- Craniotomy: Perform a craniotomy over the primary visual cortex (V1) contralateral to the stimulated eye.
- Recording Electrode Array Implantation: Insert a 4x4 grid electrode array (e.g., 16 electrodes, 400 µm spacing) approximately 800–950 µm deep into V1.
- Stimulation and Recording:
- Stimulation: Apply biphasic current pulses to the retina. Systematically vary parameters:
- Phase Duration: 500 µs, 1000 µs, 1500 µs.
- Frequency: 1 Hz, 10 Hz, 20 Hz.
- Interphase Interval (IPI): 0 µs vs. 50-100 µs.
- Recording: Record Local Field Potentials (LFPs) and Electrically Evoked Potentials (EEPs) from the V1 electrode array. Use a sampling frequency of 25 kHz with a band-pass filter of 0.3–300 Hz [45].
- Stimulation: Apply biphasic current pulses to the retina. Systematically vary parameters:
- Data Analysis:
- Measure the charge threshold required to elicit a cortical response.
- Map the spatial spread of cortical activation across the electrode array for different parameter sets.
- Compare response attenuation between low and high-frequency stimulation.
Protocol 2: Optimization and Validation of TMS Waveforms
This protocol describes an intelligent optimization method for Transcranial Magnetic Stimulation (TMS) waveforms to improve stimulation selectivity, based on a computational-in vivo loop [9].
- Objective: To identify TMS waveform parameters that maximize stimulation selectivity for a target brain region.
- Computational Setup:
- Multi-scale Neuron Model: Use a model that incorporates real head MRI data and neuron morphologies from databases like NEURON. Simulate the electric field distribution of a TMS coil (e.g., MCB70 figure-of-eight) in SimNIBS [9].
- Waveform Parametrization: Parameterize the induced electric field waveform based on a dual-capacitor bridge circuit topology, defining variables for voltage levels (V1-V4) and pulse widths (pw1-pw4) [9].
- Define Selectivity Index: Establish an objective function, ( f_1 ), representing the selectivity index. This is the ratio of the stimulation thresholds of neurons in the Region of Interest (ROI) to the thresholds of all stimulable neurons in the influenced area [9].
- Optimization Process:
- Algorithm: Employ a Particle Swarm Optimization (PSO) algorithm. Decision variables are VC1, VC2, V1, V2, pw1, pw2.
- Iteration: For each particle (waveform parameter set), calculate the resulting voltage/current waveform and apply it to the multi-scale neuron model.
- Evaluation: Calculate the selectivity index ( f1 ). The PSO algorithm iteratively guides the population towards parameter sets that minimize ( f1 ) [9].
- In Vivo Validation:
- Motor Threshold Measurement: In human subjects, compare the motor thresholds and motor-evoked potential (MEP) latencies elicited by the optimized waveform against conventional monophasic pulses [10].
- Directional Selectivity: A significant MEP latency difference (e.g., 1.79 ms) between anterior-posterior and posterior-anterior electric field directions confirms improved directional selectivity [10].
Data Presentation
Table 1: Effects of Electrical Stimulation Parameters on Cortical Activation
| Parameter | Tested Values | Key Finding on Cortical Activation | Clinical Implication |
|---|---|---|---|
| Phase Duration | 500 µs, 1000 µs, 1500 µs | Shorter durations (500 µs) lower charge threshold; longer durations (≥1000 µs) confine spatial spread [45]. | Balances activation efficiency with stimulus precision. |
| Stimulation Frequency | 1 Hz, 10 Hz, 20 Hz | Significant response attenuation at high frequencies (10/20 Hz) vs. low frequency (1 Hz) [45]. | Informs design of repetitive stimulation protocols. |
| Interphase Interval (IPI) | 0 µs vs. with IPI | Inclusion of an IPI limits the extension of cortical responses [45]. | A potential strategy to improve spatial resolution. |
| Waveform Asymmetry | Monophasic vs. Optimized Asymmetric | Optimized asymmetric pulses reduce energy loss by up to 92% and offer directional selectivity [10]. | Enables selective rapid-rate rTMS with reduced heating. |
Table 2: Key Metrics for Validating Optimized Stimulation Waveforms
| Metric | Definition / Formula | Interpretation |
|---|---|---|
| Selectivity Index (f₁) | ( f1 = \frac{\sum{i=1}^{n} threshEs_ROI{i} }{\sum{i=1}^{3000} threshEs_{i} } ) [9] | A smaller value indicates better selectivity (target neurons are easier to activate than non-target ones). |
| Stimulation Intensity | Intensity = median( threshEs_ROIᵢ ) [9] | The median stimulation threshold required to activate 50% of neurons in the target region. |
| Coil Heating / Energy Loss | ( W_{heat} = \int RI^{2} dt ) [9] | Quantifies power consumption and coil heating; lower values are better for device safety and efficiency. |
| MEP Latency Difference | Latency(AP) - Latency(PA) | A significant difference (e.g., >1.5 ms) confirms directional selectivity of neural activation [10]. |
Visualization of Workflows and Relationships
Core Validation Workflow
Computational-Experimental Integration
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Stimulation Optimization Research
| Item / Solution | Function / Description | Example Use Case |
|---|---|---|
| Multi-scale Neuron Model | A computational model that simulates neuronal electrical activity across different spatial scales, from single cells to tissue networks. | Predicting neuronal activation thresholds and spatial spread for different electric field waveforms [9]. |
| Particle Swarm Optimization (PSO) Algorithm | An intelligent computational method used to iteratively search for optimal parameters that minimize or maximize a defined objective function. | Identifying TMS waveform parameters that maximize the selectivity index (f₁) [9]. |
| Bipolar Concentric Stimulating Electrode | A fine electrode used for focal electrical stimulation in neural tissue, allowing for precise delivery of current. | Epiretinal stimulation in rodent models to evoke cortical responses [45]. |
| Multi-electrode Array (MEA) | A grid of electrodes used for recording electrophysiological signals from multiple sites simultaneously. | Mapping the spatial distribution of evoked potentials in the primary visual cortex (V1) [45]. |
| Potentiostat with Impedance Monitoring | An instrument that measures the electrical impedance at the electrode-tissue interface in real-time. | Ensuring consistent and optimal distance between the stimulation electrode and the target tissue (e.g., retina) [45]. |
| SimNIBS Software | An open-source software package for simulating the electric field generated by TMS coils in realistic head models derived from MRI. | Calculating the electric field distribution for a given coil position and waveform [9]. |
| Selectivity Index (f₁) | A quantitative metric defined as the ratio of stimulation thresholds in the target region to thresholds in the entire stimulated area. | The primary objective function for optimizing stimulation waveform selectivity [9]. |
Conclusion
The pursuit of optimized stimulation waveforms for selective activation represents a convergence of biophysics, computational modeling, and clinical insight. Key takeaways confirm that tailoring parameters like pulse width, frequency, and interphase interval can significantly enhance spatial precision and mimic physiological recruitment order. The comparative success of paradigms like SSES and OSES demonstrates the value of accounting for functional neuroanatomy. Future directions must focus on closing the loop with responsive neuromodulation systems, developing personalized waveform profiles based on individual anatomy, and translating these precise control strategies into robust clinical outcomes for a wider range of neurological conditions. The integration of intelligent optimization algorithms promises to accelerate this transition, ushering in an era of truly targeted and adaptive bioelectronic medicine.
References
- 1. Henneman's size principle [https://en.wikipedia.org/wiki/Henneman%27s_size_principle]
- 2. The Size Principle [https://gymaware.com/the-size-principle/]
- 3. Model-Based Analysis and Design of Waveforms for Efficient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4772858/]
- 4. Selective Activation of Neuronal Targets With Sinusoidal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2997038/]
- 5. Troubleshooting your Electrical Stimulation Machine | PFE - [https://www.pelvicfloorexercise.com.au/resources/post/troubleshooting-your-electrical-stimulation-machine?srsltid=AfmBOooabjnUuQf07qhDMRI8LHivXz8ACNCacu77n8phApu5xbFFGfyd]
- 6. Highly efficient modeling and optimization of neural fiber ... [https://www.nature.com/articles/s41467-024-51709-8]
- 7. Sonogenetic control of mammalian cells using exogenous ... [https://www.nature.com/articles/s41467-022-28205-y]
- 8. Strength–Duration Relationship for Extracellular Neural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2957463/]
- 9. An Intelligent Optimization Method for Transcranial ... [https://link.springer.com/chapter/10.1007/978-981-96-4856-6_4]
- 10. Optimal asymmetric electric field pulses for selective ... [https://www.sciencedirect.com/science/article/pii/S1935861X25003286]
- 11. Mitochondria delay action potential propagation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420829/]
- 12. Strength-frequency curve for micromagnetic ... [https://pubmed.ncbi.nlm.nih.gov/35030549/]
- 13. Intrinsic and synaptic regulation of axonal excitability in ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1681044/full]
- 14. SD curve (Strength Duration Curve) | PPTX [https://www.slideshare.net/slideshow/sd-curve-strength-duration-curve/248483908]
- 15. Selective Neuromodulation of the Vagus Nerve [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2021.685872/full]
- 16. Investigating stimulation parameters for preferential small- ... [https://pubmed.ncbi.nlm.nih.gov/31461369/]
- 17. Control of spatiotemporal activation of organ-specific fibers ... [https://www.nature.com/articles/s41467-025-59595-4]
- 18. Anodic stimulation misunderstood: preferential activation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6889961/]
- 19. Size principles governing selective neuromodulation and ... [https://www.sciencedirect.com/science/article/abs/pii/S246845112500008X]
- 20. kHz-frequency electrical stimulation selectively activates ... [https://www.sciencedirect.com/science/article/pii/S1935861X22002248]
- 21. kHz-frequency electrical stimulation selectively activates small ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10164362/]
- 22. High-frequency amplitude-modulated sinusoidal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10888888/]
- 23. Effects of waveform shape and electrode material on KiloHertz ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9327420/]
- 24. Nerve excitation using an amplitude-modulated signal with ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-016-0171-4]
- 25. Kilohertz electrical stimulation evokes robust cellular ... [https://www.nature.com/articles/s42003-024-07447-0]
- 26. Direct Estimation of Electric Field Distribution in Circular ECT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567922/]
- 27. Enabling electric field model of microscopically realistic brain [https://www.sciencedirect.com/science/article/pii/S1935861X24013913]
- 28. Waveform Optimization and Analysis for Enhancing ... [https://ui.adsabs.harvard.edu/abs/2025IEEEA..1374868Z/abstract]
- 29. Irregular optogenetic stimulation waveforms can induce ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212926/]
- 30. About Waveforms [https://www.medi-stim.com/overview/waveforms.html]
- 31. Intracortical Microstimulation Parameters Dictate the ... [https://www.sciencedirect.com/science/article/abs/pii/S1935861X15012188]
- 32. A portable, programmable, multichannel stimulator with ... [https://www.nature.com/articles/s41598-023-30545-8]
- 33. Approach to Spinal Cord Stimulation Programming [https://asra.com/news-publications/asra-updates/blog-landing/legacy-b-blog-posts/2024/02/13/approach-to-spinal-cord-stimulation-programming-a-problem-based-learning-discussion]
- 34. Selective Activation of the Spinal Cord with Epidural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274919/]
- 35. Orientation Selective Deep Brain Stimulation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5440185/]
- 36. Orientation selective stimulation with tetrahedral electrodes ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1147547/full]
- 37. A case study of percutaneous epidural stimulation to ... [https://www.nature.com/articles/s41467-023-37845-7]
- 38. Intelligence Optimization Algorithms and Applications [https://www.mdpi.com/journal/mathematics/special_issues/Intell_Optim_Algorithms_Appl]
- 39. Multi-scale Modeling Toolbox for Single Neuron and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8608742/]
- 40. The NeuroML ecosystem for standardized multi-scale ... [https://elifesciences.org/reviewed-preprints/95135]
- 41. The NeuroML ecosystem for standardized multi-scale ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11723582/]
- 42. Intelligent Optimization Design of a Phononic Crystal Air ... [https://www.mdpi.com/1996-1944/16/17/5812]
- 43. Artificial intelligence for optimization: Unleashing the ... [https://www.sciencedirect.com/science/article/abs/pii/S0377221725006666]
- 44. An improved intelligent optimization algorithm for small- ... [https://www.nature.com/articles/s41598-024-71963-6]
- 45. Optimizing electrical stimulation parameters to enhance ... [https://www.nature.com/articles/s41598-025-08657-0]
- 46. Troubleshooting Interstim Sacral Neuromodulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6105247/]
- 47. Troubleshooting [https://teleemg.com/manual/troubleshooting/]
- 48. Troubleshooting your Electrical Stimulation Machine | PFE - [https://www.pelvicfloorexercise.com.au/resources/post/troubleshooting-your-electrical-stimulation-machine?srsltid=AfmBOorR-gv_Ner1yH1lUe2iMPV0YnRnvCrE3Wuvpw8acwgUw5cr2jjv]
- 49. Activation of Ventral Tegmental Area Cells by the Bed Nucleus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6757737/]
- 50. Ventral tegmental dopamine neurons control the impulse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7590264/]
- 51. Delayed muscle fatigue during electrical stimulation of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128545/]
- 52. Muscle motor point identification is essential for optimizing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3938308/]
- 53. Comparison of activation and selectivity in dorsal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518515/]
- 54. Optimization of Stimulation Parameters for Targeted Activation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8340624/]
- 55. In Silico analysis of concentration and spatial distribution ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00187-4]
- 56. Optimizing spatial specificity and signal quality in fNIRS [https://pmc.ncbi.nlm.nih.gov/articles/PMC11188482/]
- 57. Emerging techniques for precision neuromodulation [https://www.the-innovation.org/article/doi/10.59717/j.xinn-life.2025.100150]
- 58. Comparison of activation and selectivity in dorsal and ... [https://www.nature.com/articles/s41598-025-19555-w]
- 59. Recent advances in potential mechanisms of epidural ... [https://www.sciencedirect.com/science/article/pii/S0014488625001943]
- 60. The effects of stimulation waveform and carrier frequency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056781/]
- 61. Computational Optimization of Spinal Cord Stimulation for ... [https://www.sciencedirect.com/science/article/abs/pii/S1094715925000285]
- 62. Use of Monopolar Coagulation and Transcranial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12147387/]
- 63. Computational analysis of electrode structure and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11208352/]
- 64. Advances in the application of temporal interference stimulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12162641/]
- 65. On the need of individually optimizing temporal ... [https://www.sciencedirect.com/science/article/pii/S1935861X25002748]
- 66. Recovery of early neural spikes from stimulation electrodes ... [https://www.sciencedirect.com/science/article/abs/pii/S0165027018301171]
- 67. Remove stimulus artefact [https://www.st-andrews.ac.uk/~wjh/dataview/tutorials/remove-artefact.html]
- 68. Stimulation and Artifact-suppression Techniques for in-vitro ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6711758/]
- 69. Editorial: Computational methods in cardiac ... [https://www.frontiersin.org/articles/10.3389/fphys.2023.1231342/full]
- 70. ISCEV standard for clinical visual evoked potentials (2025 ... [https://link.springer.com/article/10.1007/s10633-025-10042-1]
- 71. State of the Art of Artificial Intelligence in Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123071/]