i2CS: A Novel Neuromodulation Approach for Precision Vagus Nerve Stimulation
Intermittent Interferential Current Stimulation (i2CS) represents a paradigm shift in bioelectronic medicine, enabling unprecedented spatial and temporal control over nerve fiber activation.
i2CS: A Novel Neuromodulation Approach for Precision Vagus Nerve Stimulation
Abstract
Intermittent Interferential Current Stimulation (i2CS) represents a paradigm shift in bioelectronic medicine, enabling unprecedented spatial and temporal control over nerve fiber activation. This article details the foundational principles of i2CS, a method that utilizes short bursts of high-frequency interfering currents through multi-contact electrodes to selectively target organ-specific fascicles within complex peripheral nerves like the vagus. We explore its methodological implementation, the computational models crucial for optimizing stimulation protocols, and its validation in large-animal studies, which demonstrate enhanced therapeutic efficacy and reduced side effects compared to conventional stimulation. For researchers and drug development professionals, this synthesis of anatomy, engineering, and physiology outlines a path toward personalized neuromodulation therapies for chronic diseases.
The Anatomical and Biophysical Foundations of i2CS
Addressing the Selectivity Limitation in Conventional Vagus Nerve Stimulation
The vagus nerve is a complex mixed nerve, composed of approximately 80% afferent and 20% efferent fibers, that innervates multiple organs including the heart, lungs, and gastrointestinal tract [1] [2]. This anatomical structure presents a fundamental challenge for conventional VNS techniques: the inability to selectively activate specific organ-specific fibers without simultaneously stimulating unrelated pathways. This lack of selectivity inevitably leads to side effects that limit the therapeutic window and clinical applicability of VNS across various conditions.
Conventional VNS approaches, both invasive cervical VNS (iVNS) and transcutaneous auricular VNS (taVNS), typically result in broad, non-specific activation of multiple fiber types and functions [3] [2]. The resulting side effects include hoarseness, cough, dysphagia, and more concerningly, cardiac effects such as bradycardia and potential asystole, which occur in approximately 1 in 1000 cases due to direct stimulation of cardiac branches [1] [3]. While taVNS is generally considered safer with mainly mild and transient adverse effects like ear pain, headache, and tingling [1], it still lacks the precision needed for optimal therapeutic outcomes.
The emerging solution to this longstanding limitation lies in intermittent interferential current stimulation (i2CS), a novel approach that enables spatiotemporal control of fiber activation within the vagus nerve [4]. This application note details the methodology, experimental protocols, and practical implementation of i2CS for researchers investigating selective vagus nerve stimulation.
Technical Foundation: Principles of i2CS for Selective Stimulation
Fundamental Mechanism of i2CS
Intermittent interferential current stimulation (i2CS) represents a paradigm shift in neural stimulation technology. Unlike conventional sinusoidal or rectangular pulse stimulation, i2CS utilizes multiple intersecting sinusoidal currents delivered through multi-contact epineural cuff electrodes [4]. The core principle involves two or more high-frequency sinusoidal currents (typically >1 kHz) with slightly different frequencies that interact within the nerve tissue to generate a low-frequency interference pattern that selectively modulates neural activity.
The key innovation of i2CS lies in its ability to exploit differences in activation thresholds and spatial positioning of different fiber populations within the vagus nerve. Through careful selection of carrier frequencies, beat frequencies, and current steering parameters, i2CS can achieve focal stimulation of specific fascicles innervating target organs while minimizing activation of unrelated fibers [4]. This spatial and temporal specificity directly addresses the fundamental selectivity limitation of conventional VNS approaches.
Comparative Advantages Over Conventional VNS
Table 1: Comparison of Conventional VNS versus i2CS Approaches
| Parameter | Conventional VNS | i2CS Approach |
|---|---|---|
| Selectivity | Bulk nerve activation, limited fascicle specificity | Precise spatiotemporal control, organ-specific fascicle targeting |
| Side Effect Profile | Common: hoarseness, cough, bradycardia, dysphagia | Significantly reduced laryngeal side effects while maintaining therapeutic effects |
| Control Mechanism | Amplitude, frequency, pulse width modulation | Current steering, beat frequency, repetition frequency tuning |
| Spatial Resolution | Macroscopic nerve-level activation | Mesoscopic fascicle-level activation |
| Therapeutic Window | Narrow due to collateral activation | Potentially wider through selective targeting |
Experimental evidence from swine models demonstrates that i2CS enables tunable and precise control of nerve and organ responses, allowing researchers to attain similar levels of desired therapeutic effects (e.g., bronchopulmonary responses) while producing reduced levels of side effects (e.g., laryngeal activation) compared to equivalent sinusoidal stimulation [4].
Experimental Implementation: i2CS Methodology
Research Reagent Solutions and Essential Materials
Table 2: Essential Research Materials for i2CS Investigation
| Category | Specific Items | Function/Application |
|---|---|---|
| Electrode Systems | Multi-contact epineural cuff electrodes | Enable current steering and spatial targeting of specific nerve regions |
| Stimulation Equipment | Bipolar current stimulators, Multi-channel signal generators | Generate precise interferential waveforms with controlled parameters |
| Animal Models | Swine (Sus scrofa domestica) | Preferred model due to vagus nerve anatomy similarity to humans |
| Monitoring Equipment | Electromyography (EMG) setup, Respiratory monitoring, Cardiovascular monitoring | Quantify functional responses from target organs and side effects |
| Computational Tools | Anatomically realistic biophysical vagus nerve models | Predict fiber activation patterns and optimize stimulation parameters |
| Anatomical Validation | Micro-CT imaging equipment, Tissue processing reagents | Confirm electrode placement and fascicular activation patterns |
Detailed Experimental Protocol: i2CS in Swine Model
Surgical Preparation and Electrode Placement
- Anesthesia and Stabilization: Induce anesthesia using approved protocols (e.g., ketamine/xylazine induction followed by isoflurane maintenance). Monitor vital signs (ECG, SpO₂, respiratory rate, temperature) throughout the procedure.
- Vagus Nerve Exposure: Perform lateral cervical incision and careful dissection to expose the cervical vagus nerve. Maintain saline-moistened gauze to prevent nerve desiccation.
- Electrode Implantation: Place multi-contact epineural cuff electrode around the vagus nerve. Optimal cuff design should contain multiple independent contacts (typically 8-16) arranged circumferentially to enable current steering capabilities.
- Physiological Monitoring Setup: Install EMG electrodes in laryngeal muscles to monitor side effects. Implement respiratory monitoring via pneumotachograph or similar equipment. Establish cardiovascular monitoring through arterial line or continuous ECG analysis.
Parameter Optimization and Stimulation Protocol
- Baseline Characterization: Determine threshold responses for different fiber types using single-frequency sinusoidal stimulation across electrode contacts.
- i2CS Parameter Space Exploration:
- Carrier Frequencies: Test range 1-10 kHz with small offsets (50-200 Hz) between channels
- Beat Frequencies: Evaluate 1-100 Hz range to match physiological response characteristics
- Current Amplitude: Titrate from subthreshold to supraphysiological levels (typically 10-500 µA)
- Intermittence Pattern: Apply duty cycles of 10-50% with rest periods between stimulation trains
- Response Mapping: Systematically map physiological responses (laryngeal EMG, bronchopulmonary responses, cardiovascular changes) to different parameter combinations.
- Selectivity Validation: Compare activation patterns between i2CS and conventional sinusoidal stimulation using the same overall charge balance.
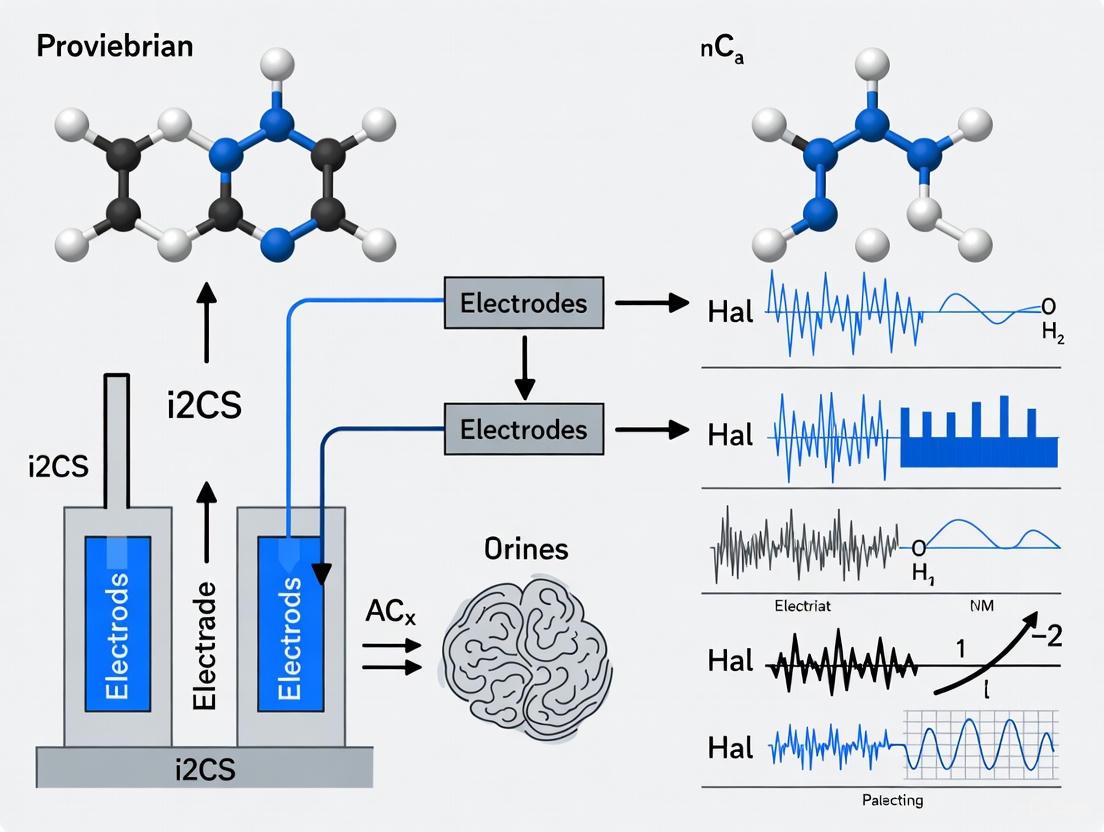
Diagram 1: Experimental workflow for i2CS parameter optimization and validation.
Data Collection and Analysis
- Quantitative Metrics: Record latency, amplitude, and threshold of target responses (e.g., bronchopulmonary) versus side effects (e.g., laryngeal EMG).
- Selectivity Index Calculation: Calculate as ratio of target response to collateral response at equivalent stimulation intensities.
- Statistical Comparison: Perform paired t-tests or ANOVA comparing i2CS versus conventional stimulation across multiple trials and subjects.
- Histological Validation: After terminal experiments, resect stimulated nerve segments for micro-CT imaging to correlate functional responses with anatomical fascicle activation.
Application Notes and Practical Implementation Guidelines
Parameter Optimization Strategy
Successful implementation of i2CS requires systematic parameter optimization. The following sequential approach is recommended:
Establish Neural Fulcrum: First identify the "neural fulcrum" - the operating point where minimal heart rate changes occur during stimulation [5]. This provides a stable baseline from which to explore selective activation.
Current Steering Implementation: Utilize the multi-contact cuff electrode to create constructive and destructive interference patterns within specific nerve regions. Empirical testing should focus on phase differences and amplitude ratios between adjacent contacts.
Frequency Domain Optimization: Fine-tune carrier frequencies to match the size-dependent activation properties of target fibers. Smaller autonomic fibers (e.g., bronchopulmonary) typically respond to different frequency bands than larger laryngeal motor fibers.
Temporal Patterning: Apply intermittent stimulation trains to leverage temporal summation properties while preventing neural adaptation or fatigue.
Troubleshooting Common Implementation Challenges
- Insufficient Selectivity: Expand parameter exploration to include asymmetric current delivery across electrode contacts and additional beat frequency modulation.
- Unstable Responses: Implement closed-loop control systems that adjust parameters based on real-time physiological feedback [5].
- Current Spread: Reduce stimulation amplitude and utilize more focused field patterns through optimized electrode geometry.
- Reproducibility Issues: Standardize electrode placement procedures and implement computational modeling to predict individual variations in nerve anatomy.
Future Directions and Research Applications
The implementation of i2CS technology opens numerous avenues for advanced VNS research and therapeutic development. The enhanced selectivity enables previously impossible experimental paradigms:
Circuit-Specific Neuromodulation: Investigate the differential roles of specific vagal pathways in regulating individual organs and systems without confounding co-activation.
Combination Therapies: Explore synergistic effects of simultaneously targeting multiple specific pathways with different stimulation parameters.
Disease-Specific Optimization: Tailor i2CS parameters to specific pathological conditions where selective vagal activation may provide therapeutic benefits.
Closed-Loop Integration: Combine i2CS with automated feedback systems [5] to create adaptive neuromodulation therapies that maintain optimal selectivity across varying physiological states.
The integration of i2CS with computational modeling, advanced electrode design, and closed-loop control systems represents the future of selective vagus nerve stimulation, potentially enabling new therapeutic approaches for conditions ranging from epilepsy and depression to inflammatory disorders and metabolic diseases.
The vagus nerve serves as a critical communication pathway between the brain and visceral organs, regulating numerous physiological functions through its complex architecture of afferent and efferent fibers. Traditional vagus nerve stimulation (VNS) approaches often result in non-selective activation of fibers, leading to reduced therapeutic efficacy and side effects from non-targeted organs [6]. Emerging research reveals that vagal fibers demonstrate a highly organized bimodal arrangement according to both function and specific organ innervation. This anatomical organization provides the foundation for advanced neuromodulation approaches, including intermittent interferential current stimulation (i2CS), which enables precise spatiotemporal control of fiber activation [4]. Understanding this intricate organization is essential for developing targeted bioelectronic therapies for chronic diseases.
Results
Quantitative Anatomical Organization of Vagal Fibers
Table 1: Fascicular Organization Along the Cervical Vagus Nerve in Swine
| Organ Specificity | Cephalad Position (near nodose ganglion) | Caudad Position (lower cervical/upper thoracic) | Fiber Type Distribution |
|---|---|---|---|
| Sensory vs Motor | Spatially separated | Merged | Myelinated afferents/efferents occupy separate fascicles |
| Larynx-specific | Merged with main trunk | Separated | Myelinated and unmyelinated efferents occupy separate fascicles |
| Heart-specific | Merged with main trunk | Separated | Small unmyelinated afferents widely distributed |
| Lung-specific | Merged with main trunk | Separated | Radially asymmetric with consistent angular separations |
Table 2: Fiber Type Distribution in Swine Vagus Nerve
| Fiber Classification | Morphological Characteristics | Fascicular Preference | Diameter Range |
|---|---|---|---|
| Myelinated Afferents | Sensory, directed periphery to brain | Separate fascicles | >10 μm |
| Myelinated Efferents | Motor, directed brain to periphery | Separate fascicles from afferents | >10 μm |
| Unmyelinated Efferents | Motor functions | Separate fascicles from myelinated | <0.5 μm |
| Unmyelinated Afferents | Sensory functions | Widely distributed across most fascicles | <0.5 μm |
Research utilizing micro-computed tomography (micro-CT) imaging and quantified immunohistochemistry at the single-fiber level has demonstrated that the vagal trunk exhibits specific spatial organization patterns. Fascicles containing fibers for specific organs (larynx, heart, lungs) are separated in the caudad region (toward the lower cervical and upper thoracic area) and progressively merge in the cephalad direction (toward the head). Conversely, sensory and motor fascicles show the opposite pattern—they are spatially separated cephalad, close to the nodose ganglion, and merge caudad [6].
This organization extends to the microscopic level, where different morphological fiber types are differentially distributed. Myelinated afferent and efferent fibers occupy separate fascicles, as do myelinated and unmyelinated efferent fibers. In contrast, small unmyelinated afferent fibers are widely distributed within most fascicles [6]. This anatomical arrangement creates consistent, radially asymmetric patterns that can be exploited for selective neuromodulation.
Molecular Coding of Vagal Interoception
The anatomical organization is complemented by a multidimensional coding architecture at the molecular level. Single-cell profiling of vagal sensory neurons (VSNs) reveals three independent feature-coding dimensions:
- Visceral Organ Dimension: Differential gene expression codes for organs along the body's rostral-caudal axis [7].
- Tissue Layer Dimension: Specific gene modules code the locations of VSN endings along the surface-lumen axis of organs [7].
- Stimulus Modality Dimension: VSNs are organized into functional units to sense similar stimuli across different organs and tissue layers [7].
This combinatorial coding strategy allows for the specification of numerous parallel VSN pathways, enabling the brain to discriminate between diverse interoceptive signals from the same organ.
Experimental Protocols
Protocol 1: Micro-CT Imaging for Fascicular Trajectory Mapping
Purpose: To track the transverse and longitudinal arrangement of fascicles within the vagal trunk with respect to organ innervation and function.
Materials:
- Dissected vagus nerve samples (swine model)
- Micro-CT imaging system
- Appropriate contrast agents for neural tissue
- 3D reconstruction software
Procedure:
- Carefully dissect the cervical vagus nerve, preserving its epineurial structure.
- Fixate the nerve sample in an appropriate fixative to maintain structural integrity.
- Apply a specialized contrast agent to enhance X-ray attenuation of neural tissues.
- Mount the sample in the micro-CT imaging chamber.
- Acquire high-resolution cross-sectional images along the entire nerve length (typical resolution: <10 μm).
- Reconstruct 3D images from the cross-sectional data series.
- Manually or algorithmically track individual fascicular trajectories through the nerve trunk.
- Correlate fascicular positions with known branching points to specific organs (laryngeal, cardiac, pulmonary branches).
- Map the merging and separation patterns of functionally distinct fascicles along the cephalad-caudad axis.
This protocol confirmed that larynx-, heart-, and lung-specific fascicles are separated caudad and progressively merge cephalad, while sensory and motor fascicles show the inverse pattern [6].
Protocol 2: Quantified Immunohistochemistry for Single-Fiber Characterization
Purpose: To identify, characterize, and classify all vagal fibers at the single-fiber level to determine morphological type distribution within fascicles.
Materials:
- Cryostat or microtome
- Antibodies for specific neuronal markers (e.g., neurofilaments, myelin basic protein)
- Fluorescence microscopy system
- Automated image analysis software
Procedure:
- Following micro-CT imaging, embed the nerve samples in optimal cutting temperature (OCT) compound.
- Section the nerve transversely and longitudinally at optimal thickness (e.g., 10-20 μm).
- Perform immunohistochemical staining using antibodies targeting:
- Pan-neuronal markers
- Myelin-specific proteins
- Sensory neuron-specific markers
- Motor neuron-specific markers
- Counterstain with DAPI for nuclear localization.
- Image stained sections using high-resolution fluorescence microscopy.
- Use automated image analysis to:
- Identify individual fibers
- Measure fiber diameters
- Classify fibers as myelinated vs. unmyelinated
- Determine neurochemical phenotypes
- Map the spatial distribution of different fiber types within and across fascicles.
- Correlate fiber type distributions with fascicular organization from micro-CT data.
This approach revealed that myelinated afferents and efferents occupy separate fascicles, myelinated and unmyelinated efferents occupy separate fascicles, and small unmyelinated afferents are widely distributed within most fascicles [6].
Protocol 3: Fascicle-Selective VNS Using Multi-Contact Cuff Electrodes
Purpose: To deliver spatially selective electrical stimulation to specific vagal fascicles and measure organ-specific physiological responses.
Materials:
- Custom multi-contact cuff electrode (e.g., 8-16 contacts)
- Biopotential recording system
- VNS stimulator with multiple independent channels
- Anesthetized or awake swine preparation
- Physiological monitoring equipment (EMG, ECG, respiratory sensor)
Procedure:
- Surgically implant the multi-contact cuff electrode around the cervical vagus nerve.
- Connect electrode contacts to the multi-channel stimulator.
- For each electrode contact, deliver electrical stimuli with varying parameters:
- Pulse width: 50-200 μs
- Frequency: 10-30 Hz
- Amplitude: 0.1-2.0 mA
- Record compound action potentials (CAPs) from the nerve distal and proximal to the stimulation site.
- Simultaneously monitor organ-specific responses:
- Laryngeal muscle activation via EMG
- Cough response via respiratory monitoring
- Heart rate changes via ECG
- Breathing pattern changes via pneumotachograph
- Map the stimulation thresholds and response magnitudes for each organ function to specific electrode contact positions.
- Correlate the effective stimulation sites with the anatomical fascicular organization from Protocols 1 and 2.
This protocol demonstrated that CAPs from distinct fiber types and physiological responses from different organs are elicited in a radially asymmetric manner, with consistent angular separations agreeing with the documented fascicular organization [6].
Protocol 4: Intermittent Interferential Current Stimulation (i2CS)
Purpose: To achieve spatiotemporal control of organ-specific fiber activation using interferential current stimulation.
Materials:
- Multi-contact epineural cuff electrode
- Multi-channel stimulator capable of delivering high-frequency (kHz) waveforms
- Computational modeling platform (e.g., ASCENT pipeline)
- Physiological monitoring equipment
Procedure:
- Implant multi-contact cuff electrode on the cervical vagus nerve.
- Program stimulator to deliver i2CS parameters:
- Carrier frequency: ~20 kHz
- Amplitude-modulated signal: few kHz
- Pulse duration: sub-millisecond
- Intermittent pulses: delivering only half of the beat
- Apply i2CS through selected electrode contact pairs.
- Record neural potentials and organ responses (e.g., laryngeal EMG, breathing rate).
- Resect the stimulated nerve and perform micro-CT imaging to resolve anatomical trajectories of activated fascicles.
- Develop anatomically realistic, physiologically validated biophysical vagus nerve models.
- Correlate experimental results with model predictions of single-fiber activation.
- Optimize stimulation parameters (current steering, beat frequency, repetition frequency) to shape spatiotemporal patterns of fiber activation.
This protocol has demonstrated that i2CS produces distinct nerve potentials and organ responses explained by activation of organ-specific fascicles rather than the entire nerve, enabling reduced side effects while maintaining therapeutic efficacy [4].
Visualizations
Bimodal Fascicular Organization
i2CS Mechanism and Outcomes
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Vagal Anatomy and Stimulation Research
| Item | Function | Application Example |
|---|---|---|
| Multi-contact cuff electrode | Delivers spatially selective electrical stimulation; accommodates fascicular structure | Fascicle-selective cervical VNS in swine [6] |
| Micro-CT imaging system | Provides high-resolution 3D visualization of fascicular trajectories | Tracking fascicular paths along centimeters of nerve length [6] |
| Projection-seq AAVs | Enables high-throughput genetic and anatomical dissection of neural circuits | Multiplexed mapping of VSNs projecting to different organs [7] |
| Antibody panels for IHC | Identifies and classifies neuronal fiber types at single-cell level | Characterizing myelinated vs. unmyelinated fiber distribution [6] |
| Computational modeling pipeline | Simulates nerve-electrode interface and predicts fiber activation | ASCENT pipeline for modeling i2CS effects [4] |
| AAV-FLEX-tdTomato in Cre lines | Labels specific neuronal populations for terminal morphology studies | Mapping VSN endings in different organ tissue layers [7] |
Core Principles and Evolution of Stimulation Techniques
Temporal Interference (TI) stimulation represents a significant advancement in neuromodulation. It utilizes multiple high-frequency electric fields (typically in the kHz range) with a slight frequency offset (e.g., 10 Hz) applied via separate electrode pairs [8] [9]. The key principle lies in the interference pattern created when these fields summate within biological tissue, generating a amplitude-modulated (AM) envelope, or "beat," that oscillates at the difference of the two high frequencies [9]. Due to the intrinsic low-pass filtering properties of neural membranes, neurons do not respond to the high-frequency carriers but can be activated by the lower-frequency envelope, thereby enabling the potential for targeted stimulation of deep brain structures without affecting overlying cortical areas [8].
Building upon classic interferential (IF) and TI concepts, a novel paradigm termed intermittent interferential current stimulation (i2CS) has emerged. i2CS delivers short pulses (less than 1 millisecond) of high-frequency interferential stimulation (around 20 kHz), resulting in amplitude modulations in the low kHz range [10] [11]. Unlike continuous stimulation, this intermittent delivery of interferential energy allows for finer temporal and spatial control of nerve fiber activation. Computational and experimental models suggest i2CS induces activation delays at the interference focus, which can be precisely tuned via pulse duration to achieve superior functional selectivity in peripheral nerve stimulation [11].
Table 1: Key Characteristics of Interferential Stimulation Modalities
| Feature | Classic Interferential Current (IFC) | Temporal Interference (TI) | Intermittent Interferential (i2CS) |
|---|---|---|---|
| Core Principle | Summation of two medium-frequency currents | Interference of two high-frequency electric fields | Pulsed delivery of high-frequency interferential waveforms |
| Typical Carrier Frequency | Medium to High Frequency (e.g., 1-10 kHz) | High Frequency (kHz range) | ~20 kHz [10] |
| Defining Stimulation Pattern | Continuous amplitude-modulated "beat" | Continuous amplitude-modulated envelope | Short, intermittent pulses (<1 ms) [10] |
| Primary Application Context | Traditional physiotherapy, pain management | Non-invasive deep brain stimulation [8] | Selective peripheral nerve stimulation (e.g., Vagus Nerve) [10] |
| Postulated Selectivity Mechanism | Broad tissue penetration | Spatial focusing via electric field interference | Spatiotemporal control via pulsed interference and current steering [10] |
Experimental Protocols and Methodologies
In Vivo fMRI Investigation of IFC vs. ACS in Rodent Models
This protocol is designed to compare acute brain-wide activation patterns in response to interferential current (IFC) and low-frequency alternating current stimulation (ACS) using functional magnetic resonance imaging (fMRI) [8].
- Animal Preparation: Utilize adult male Wistar rats (e.g., 270 ± 20 g). Perform stereotaxic surgery under anesthesia (e.g., isoflurane followed by urethane) to implant a stimulation electrode (e.g., silver wire) in the target brain region, such as the primary motor cortex (M1; coordinates from bregma: 2.0 mm mediolateral, 1.0 mm anteroposterior) [8].
- fMRI Data Acquisition: Transfer the animal to an MRI scanner. Acquire anatomical images first. For functional MRI, use a Gradient Echo-Echo Planar Imaging (GE-EPI) sequence to capture Blood-Oxygenation-Level-Dependent (BOLD) signals. Key parameters include [8]:
- TR/TE: 2000/15 ms
- Matrix: 60 x 60
- Slice Thickness: 0.8 mm
- Repetitions: 205
- Stimulation Paradigm: Employ a block design. A typical cycle consists of 10 seconds of stimulation "off" followed by 60 seconds of stimulation "on," repeated five times for a total scan time of approximately 6 minutes and 50 seconds [8]. Stimulation intensity should be calibrated to determine the neural response activation threshold.
- Data Analysis: Preprocess and analyze fMRI data to identify statistically significant BOLD signal changes. Compare the spatial extent and intensity of activation between IFC and ACS protocols. A key finding is that the activation threshold for IFC is at least twofold higher than for ACS [8].
Selective Vagus Nerve Stimulation (i2CS) in Swine Models
This protocol details the application of i2CS for selective organ-specific fiber activation within the vagus nerve using multi-contact epineural cuff electrodes (MCEs) [10].
- Surgical Preparation: Conduct acute experiments in anesthetized swine. Implant a multi-contact cuff electrode around the cervical vagus nerve trunk.
- Stimulation Parameters: Deliver i2CS through selected contact pairs on the MCE. Key parameters include [10]:
- Carrier Frequency: ~20 kHz
- Pulse Duration: < 1 ms
- Steering Ratio: Asymmetrical current application (e.g., 0.9 = -1, 0.7 = -0.5, 0.5 = 0, 0.3 = 0.5, 0.1 = +1) to shape the electric field and shift the interference focus [10].
- Physiological Response Measurement:
- Evoked Compound Action Potentials (eCAPs): Record eCAPs from the nerve to assess the activation of different fiber populations [10].
- Laryngeal Electromyography (EMG): Place EMG electrodes in laryngeal muscles to monitor side effects from the activation of large-diameter fibers [10].
- Breathing Response: Monitor breathing rate or volume as a measure of the desired effect mediated by smaller bronchopulmonary fibers [10].
- Anatomical Validation: Following experiments, resect the stimulated nerve and perform micro-CT imaging to reconstruct the anatomical trajectories of nerve fascicles. Correlate the physiological responses with the activation of organ-specific fascicles [10].
Table 2: Quantitative Outcomes from Key i2CS and IFC Experiments
| Experimental Readout | Stimulation Type | Key Quantitative Finding | Biological / Functional Correlation |
|---|---|---|---|
| Activation Threshold | Invasive IFC (Rat M1) [8] | At least 2x higher than ACS | Indicates lower energy efficiency for suprathreshold neural recruitment |
| BOLD Response Pattern | Invasive IFC (Rat M1) [8] | Distinct pattern vs. ACS | Suggests potential activation of distinct cell types (e.g., inhibitory cells) |
| Spatial Distribution of Activation | Invasive IFC (Rat M1) [8] | More restricted distribution vs. ACS | Reflects focal nature of IFC-induced neural response |
| Laryngeal EMG (Side Effect) | i2CS (Swine Vagus) [10] | Reduced response with specific steering | Indicates selective avoidance of large laryngeal fiber activation |
| Breathing Response (Desired Effect) | i2CS (Swine Vagus) [10] | Maintained or modulated with steering | Demonstrates selective engagement of smaller bronchopulmonary fibers |
| Selectivity Index | i2CS vs. Sinusoidal (Swine) [10] | Improved selectivity for desired over side effect | Validates i2CS as a method for functionally selective VNS |
Signaling Pathways and Experimental Workflows
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials and Equipment for i2CS and TI Research
| Item / Reagent | Function / Application | Example Specifications / Notes |
|---|---|---|
| Precision Stimulator | Generates high-frequency, multi-channel waveforms with precise timing and amplitude control for i2CS/TI. | HD-IFS PRO system; capable of frequencies from 0.1 Hz to 30 kHz, phase control, and multi-channel isolated output [9]. |
| Multi-Contact Cuff Electrode (MCE) | Implanted around peripheral nerves (e.g., vagus) to deliver focused stimulation and enable current steering. | Epineural cuff with multiple contacts; allows for asymmetric current application (steering) to shape the interference field [10]. |
| fMRI-Compatible Setup | For non-invasive mapping of brain-wide activation patterns in response to stimulation. | Includes MRI-safe stimulation electrodes, RF noise filters, and a compatible stimulator (e.g., IFS-MRI kit for 7T scanners) [8] [9]. |
| Computational Modeling Pipeline | To simulate electric field distributions and predict single-fiber activation within anatomically realistic nerve models. | Frameworks like ASCENT; uses micro-CT-derived nerve anatomies to optimize stimulation protocols in silico [11]. |
| Physiological Monitoring System | Measures functional outcomes of stimulation, such as organ responses and side effects. | Includes EMG for muscle activity, respiratory monitors for breathing, and ECG for heart rate [10]. |
| Acute Animal Preparation | Provides an in vivo model for testing stimulation efficacy and selectivity. | Typically anesthetized swine for peripheral nerve studies or rodents (e.g., Wistar rats) for central nervous system investigations [8] [10]. |
Intermittent interferential current stimulation (i2CS) represents a novel neuromodulation paradigm designed to overcome the fundamental limitation of traditional vagus nerve stimulation (VNS): the inability to selectively activate organ-specific fibers without provoking side effects. Conventional VNS devices strongly activate larger fibers, often resulting in side effects like coughing and voice hoarseness, which can limit therapeutic efficacy [12]. The i2CS method leverages biophysical mechanisms involving amplitude modulation and spatiotemporal activation to achieve unprecedented selectivity in peripheral nerve stimulation. This application note details the key mechanisms, quantitative parameters, and experimental protocols for implementing i2CS in preclinical research, providing researchers with the tools to explore this promising technology for bioelectronic medicine applications.
Core Biophysical Mechanisms
Amplitude Modulation via Temporal Interference
The foundational principle of i2CS involves delivering two or more high-frequency sinusoidal currents (typically around 20 kHz) through spatially separated contacts on a multi-contact cuff electrode (MCE) [12]. When these currents intersect within the nerve trunk, they generate a phenomenon known as temporal interference, creating a amplitude-modulated (AM) envelope at the difference frequency between the original signals. This amplitude modulation occurs in the low kHz range and is spatially focused, meaning it only significantly affects neural membranes in specific regions of the nerve [12] [13].
The biophysical mechanism underlying neural activation via i2CS involves the low-pass filtering properties of the nerve membrane. While the high-frequency carrier signals themselves do not directly elicit action potentials, the resulting amplitude-modulated envelope causes sufficient membrane depolarization to activate voltage-gated sodium channels, triggering action potential generation [13]. This shared biophysical mechanism links i2CS with other kHz-frequency stimulation techniques, unifying previously distinct neuromodulation paradigms under a common explanatory framework.
Spatiotemporal Activation Control
A key advantage of i2CS lies in its ability to achieve spatiotemporal control of fiber activation through two primary mechanisms: current steering and frequency tuning. By adjusting the relative amplitude of the current sources (steering ratio), the locus of maximum interference can be spatially shifted within the nerve cross-section [12]. This enables preferential activation of fascicles located in specific regions of the nerve.
Complementing spatial control, temporal precision is achieved through the intermittent delivery of short stimulation pulses (<1 ms) containing only half of the beat cycle [12] [11]. This pulsed approach allows fine control over activation timing while exploiting the nerve membrane's biophysical properties to achieve selective recruitment of smaller fibers associated with therapeutic effects (e.g., bronchopulmonary fibers) over larger fibers linked to side effects (e.g., laryngeal fibers) [12].
Table 1: Key Stimulation Parameters and Their Effects in i2CS
| Parameter | Typical Range | Physiological Effect | Experimental Measurement |
|---|---|---|---|
| Carrier Frequency | ~20 kHz | Determines tissue penetration depth and spatial focus [12] | Nerve-specific modeling and impedance spectroscopy |
| Beat Frequency | Low kHz range | Controls amplitude modulation rate; affects fiber recruitment [12] | Evoked compound action potential (eCAP) analysis |
| Pulse Duration | <1 ms | Determines temporal precision and selectivity for smaller fibers [12] [11] | Physiological organ responses (e.g., breathing changes) |
| Steering Ratio | -1 to +1 | Spatially shifts interference focus to target specific fascicles [12] | Selective fascicle activation measured via EMG and organ responses |
| Repetition Frequency | Stimulus-specific | Controls overall activation rate and adaptation effects | Compound measures of therapeutic efficacy vs. side effects |
Experimental Validation and Quantitative Outcomes
Anatomical Basis for Selective Activation
The effectiveness of i2CS depends critically on the anatomical organization of the target nerve. Micro-CT imaging and fascicle tracking in swine vagus nerves have revealed a bimodal distribution of organ-specific fibers, with bronchopulmonary (BP)-rich and recurrent laryngeal (RL)-rich fascicles occupying distinct regions approximately 1 mm on either side of the nerve's transverse mid-point [12]. This anatomical arrangement creates an opportunity for spatially focused stimulation to achieve functional selectivity, despite significant merging of fascicles at cervical implantation sites.
Table 2: Quantitative Selectivity Outcomes: i2CS vs. Traditional Sinusoidal Stimulation
| Response Metric | i2CS Performance | Traditional Sinusoidal Stimulation | Selectivity Enhancement |
|---|---|---|---|
| Laryngeal EMG (Side Effect) | Significantly reduced amplitude with optimized steering [12] | Consistently large responses regardless of steering [12] | Improved side effect profile while maintaining therapeutic effect |
| Breathing Response (Desired Effect) | Maintained at levels similar to traditional stimulation [12] | Standard response levels | Equivalent efficacy with reduced off-target activation |
| Spatial Specificity | Activation of organ-specific fascicles rather than entire nerve [12] | Broad activation pattern | Demonstrated via fascicular activation mapping |
| Model-Experiment Correlation | High correlation between modeled fiber activity and physiological readouts [12] [11] | Limited correlation due to non-selective activation | Predictive modeling enables parameter optimization |
Computational Modeling Insights
Biophysically realistic computational models of the vagus nerve have been instrumental in elucidating the mechanisms of i2CS. These models, incorporating 3D nerve anatomy and accurate fiber trajectories, demonstrate that i2CS induces activation delays at the interference focus, consistent with a thresholding activation mechanism [11]. The models reveal a strong correlation between simulated BP fiber activity and breathing responses (r=0.89, p<0.001) and between RL fiber activity and laryngeal EMG (r=0.92, p<0.001) [12], providing quantitative validation of the approach.
Detailed Experimental Protocols
In Vivo i2CS Application and Measurement
Objective: To evaluate the selective activation of organ-specific vagal fibers using i2CS in anesthetized swine.
Materials:
- Multi-contact cuff electrode (MCE) with 8-16 contacts
- Bipolar stimulating system capable of delivering independent high-frequency sources
- Electromyography (EMG) recording equipment for laryngeal muscle activity
- Respiratory monitoring system (plethysmography or spirometry)
- Evoked compound action potential (eCAP) recording setup
Procedure:
- Surgical Preparation: Anesthetize and mechanically ventilate subject. Expose cervical vagus nerve via ventral midline incision. Carefully place MCE around nerve trunk with contacts positioned according to anatomical mapping.
- Electrode Configuration: Select contact pairs for stimulation based on fascicular organization. For swine vagus, typically use contacts positioned to create interference patterns along the transverse nerve axis.
- Stimulation Parameters:
- Set carrier frequency to 20 kHz
- Configure beat frequency in low kHz range (1-5 kHz)
- Use pulse duration <1 ms
- Apply steering ratios from -1 to +1 in 0.25 increments
- Response Recording:
- Acquire laryngeal EMG signals via needle electrodes in thyroarytenoid muscles
- Monitor breathing parameters via pneumotachograph or equivalent
- Record eCAPs using additional nerve cuff electrodes placed proximal and distal to stimulation site
- Data Analysis: Quantify response amplitudes for each steering condition. Calculate selectivity ratio as (desired effect)/(side effect) for each parameter set.
Computational Modeling Protocol
Objective: To predict nerve responses to i2CS and optimize stimulation parameters.
Materials:
- Anatomically realistic 3D nerve model (from micro-CT or histology)
- Biophysical fiber models with appropriate diameter distributions
- Finite element modeling software for electric field calculations
- Neural activation simulation environment
Procedure:
- Nerve Reconstruction: Obtain high-resolution micro-CT images of nerve with fascicle tracing. Segment fascicles and identify organ-specific pathways.
- Model Construction:
- Import 3D nerve geometry into FEM software
- Assign tissue-specific electrical properties
- Place electrode contacts according to experimental setup
- Populate with biophysically accurate fiber models
- Stimulation Simulation:
- Apply i2CS parameters matching experimental conditions
- Calculate resulting electric fields and interference patterns
- Simulate neural activation across fiber populations
- Validation and Prediction:
- Compare simulated responses with experimental measurements
- Correlate fiber activation with physiological readouts
- Iteratively refine parameters to maximize selectivity
Visualization of i2CS Mechanisms
Diagram 1: i2CS Biophysical Mechanism Pathway
Diagram 2: Experimental Workflow for i2CS Application
Research Reagent Solutions
Table 3: Essential Materials for i2CS Research
| Item | Specification | Research Function |
|---|---|---|
| Multi-Contact Cuff Electrodes | 8-16 contacts, epineural placement [12] | Enables spatially selective stimulation through current steering |
| Bipolar Stimulation System | Dual independent channels, kHz frequency capability [12] | Generates interferential currents for temporal interference |
| Anatomically Realistic Nerve Models | 3D reconstruction from micro-CT with fascicle tracing [12] [11] | Provides computational framework for mechanism exploration and parameter optimization |
| Large Animal Model (Swine) | Similar vagus nerve fascicular organization to humans [12] | Preclinical validation of selective stimulation paradigms |
| Electrophysiology Recording Setup | eCAP, EMG, and physiological monitoring capabilities [12] | Quantifies neural and organ-specific responses to stimulation |
| Finite Element Modeling Software | Capable of simulating electric fields in biological tissues [11] | Predicts interference patterns and neural activation profiles |
Implementing i2CS: Protocols, Parameters, and Computational Modeling
Multi-contact epineural cuff electrodes (MCEs) represent a pivotal technological advancement in bioelectronic medicine, enabling spatially selective neuromodulation for treating chronic diseases. These devices are designed to interface with peripheral nerves, such as the vagus nerve, to deliver therapeutic electrical stimulation with improved specificity. The primary clinical challenge addressed by MCEs is the limited functional selectivity of traditional Vagus Nerve Stimulation (VNS), where non-specific activation often causes side effects like coughing and voice hoarseness by stimulating larger laryngeal fibers, while failing to adequately engage smaller fibers innervating target organs such as the lungs and heart [12]. The anatomical organization of peripheral nerves, where organ-specific fibers are arranged in distinct fascicles that progressively merge along the nerve's length, creates a fundamental opportunity for selective intervention [12] [14]. Within this context, intermittent interferential current stimulation (i2CS) has emerged as a novel stimulation paradigm that leverages multi-contact electrode configurations to achieve unprecedented spatial and temporal control of fiber activation [12] [15]. When combined with advanced cuff designs, i2CS enables researchers to steer current fields to target specific fascicular regions, significantly enhancing therapeutic precision while minimizing off-target effects [12]. This application note details the electrode specifications, experimental protocols, and analytical methods required to implement MCEs within an i2CS research framework.
Electrode Design Specifications and Performance Characteristics
The design of MCEs for selective neuromodulation involves critical considerations including mechanical compliance, contact configuration, and material properties to ensure stable nerve interfacing while minimizing foreign body response.
Key Design Parameters and Material Properties
Table 1: Performance Characteristics of Multi-Contact Cuff Electrodes
| Design Feature | Traditional Silicone Cuffs | Advanced/Soft Cuff Designs | Functional Impact |
|---|---|---|---|
| Wall Thickness | 200–600 μm [16] | 30–150 μm [14] [16] | Reduced flexural forces (70-700x), less nerve compression [16] |
| Electrode Material | Platinum, Iridium [17] | TiN, PEDOT:PSS-coated Au [18] [16] | Higher charge injection capacity, lower impedance [18] |
| Contact Configuration | Bipolar/Tripolar rings [14] | Multiple columns and rows (e.g., 3×6, 8-16 contacts) [18] [17] | Enables current steering and spatial selectivity [12] |
| Closing Mechanism | Spiral/helical designs [14] | Belt-like, zip-tie, or self-curling mechanisms [14] [18] | Adaptable to nerve size variability, secure fit [14] |
| Foreign Body Response | Significant fibrosis (54-80% higher) [16] | Reduced inflammation (70-80% macrophage reduction) [16] | Improved long-term stability and signal integrity [16] |
Anatomical Considerations for Cuff Placement
The functional organization of the vagus nerve exhibits a consistent bimodal distribution of organ-specific fibers in swine models, with bronchopulmonary and recurrent laryngeal fibers concentrated approximately 1mm on either side of the nerve's transverse midpoint and about 2mm from the nerve periphery [12]. This organization enables focal stimulation strategies but presents challenges due to fascicular merging, where initially separated fascicles containing organ-specific fibers progressively merge along the rostral-caudal axis, creating complex regions with mixed fiber populations [12] [14]. This anatomical reality necessitates precise cuff placement and individualized stimulation parameter optimization based on target fascicle location. Furthermore, nerve size variability between individuals and along different nerve segments requires adaptable cuff designs that can accommodate diameter variations without excessive pressure that could compromise blood flow or cause nerve degeneration [14].
Experimental Protocols for i2CS Using Multi-Contact Cuffs
Acute In Vivo Validation of Selective Stimulation
Objective: To quantify the spatial selectivity and organ-specific activation achieved with i2CS delivered through MCEs in an acute anesthetized large animal model.
Materials:
- Multi-contact epineural cuff (16-contact configuration recommended) [12] [14]
- Programmable stimulator capable of delivering high-frequency (∼20 kHz) interferential waveforms [12]
- Electrophysiology recording system for compound muscle action potentials (CMAPs) and/or electromyography (EMG) [17]
- Physiological monitoring equipment for organ-specific responses (e.g., ventilation monitor for breathing responses) [12]
Procedure:
- Surgical Preparation: Expose the target nerve (e.g., cervical vagus) via a midline incision. Carefully dissect connective tissue while preserving the epineural vasculature [12].
- Cuff Implantation: Position the MCE around the nerve, ensuring circumferential contact without excessive compression. Verify proper contact alignment relative to known anatomical organization [12] [17].
- Electrode Configuration: Select contact pairs for interferential stimulation based on computational models or anatomical predictions of target fascicle location [15].
- i2CS Parameterization:
- Apply intermittent interferential stimulation using two high-frequency sinusoidal sources (∼20 kHz) with slight frequency difference (Δf = 1-3 kHz) [12].
- Utilize short pulse durations (<1 ms) with repetition rates tuned to target specific fiber populations [12] [15].
- Systematically vary steering ratios (amplitude differences between sources) from -1 to +1 to shift the interference focus [12].
- Response Quantification:
- Record evoked compound action potentials (eCAPs) from the nerve to characterize fast and slow fiber activation [12].
- Measure end-organ responses: laryngeal EMG for side effects and breathing responses for desired bronchopulmonary effects [12].
- Construct recruitment curves by progressively increasing current amplitude from 100 μA to 4,000 μA while recording response magnitudes [17].
Validation: Selectivity is confirmed when physiological responses (e.g., breathing changes) correlate with modeled activation of target fibers (e.g., bronchopulmonary) across different steering ratios, while side-effect responses (e.g., laryngeal EMG) remain minimal [12].
Chronic Biocompatibility and Functional Stability Assessment
Objective: To evaluate long-term integration, stability, and selective stimulation performance of MCEs over clinically relevant implantation periods.
Materials:
- Soft, microfabricated cuff with thin-film construction (≤150 μm) [14] [16]
- Electrochemical impedance spectroscopy (EIS) setup [14] [16]
- Histology equipment for tissue processing and immunohistochemistry [16]
Procedure:
- Implantation: Follow aseptic surgical technique for cuff placement. For large nerves (e.g., sciatic), use a single incision approach to access the target implantation site [17].
- Secure Closure: Utilize the cuff's locking mechanism (e.g., zip-tie design, belt-like closure) to ensure stable nerve contact without constriction [14] [18].
- Post-operative Monitoring: Allow standard recovery with appropriate analgesia and monitor for signs of neurological deficit or infection [17].
- Long-term Assessment:
- Perform periodic EIS measurements in vivo to track electrode performance and interface stability [14] [16].
- Conduct stimulation threshold tests at regular intervals (e.g., weekly) to monitor changes in recruitment characteristics [16].
- At study endpoint (e.g., 30 days), perfuse-fixate the animal and harvest the nerve with implanted cuff in situ [16].
- Histological Analysis:
- Process nerve segments for transverse sectioning and staining for macrophages (ED1) and fibrosis markers (vimentin) [16].
- Compare inflammatory response and fibrotic tissue formation between implanted and contralateral control nerves [16].
- Correlate histological findings with electrochemical performance data.
Success Criteria: Effective MCE designs demonstrate >70% reduction in ED1-positive macrophages and >54% reduction in vimentin immunoreactivity compared to standard silicone cuffs after 30-day implantation, while maintaining stable impedance profiles [16].
Signaling Pathways and Experimental Workflows
Figure 1: i2CS Neuromodulation Pathway. This diagram illustrates the signaling pathway from i2CS delivery through multi-contact cuffs to end-organ effects, highlighting the neural circuits engaged for therapeutic outcomes.
Figure 2: Experimental Workflow for i2CS Electrode Development. This workflow outlines the integrated process from electrode design through validation, combining computational modeling with experimental approaches.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Materials for i2CS Studies with Multi-Contact Cuffs
| Category | Specific Product/Model | Key Specifications | Research Application |
|---|---|---|---|
| Cuff Electrodes | Soft silicone cuff [14] | 150 μm thickness, 6-16 contacts, belt-like design | Adaptable nerve interface for variable anatomy |
| Thin-film SMP cuff [16] | 30 μm thickness, TiN/Au electrodes, shape-memory polymer | Reduced foreign body response in chronic studies | |
| Stimulation Systems | Programmable neurostimulator | High-frequency capability (≥20 kHz), multi-channel output | i2CS waveform generation and current steering |
| Computational Tools | ASCENT pipeline [15] | Anatomically realistic nerve modeling with biophysical properties | Prediction of neural activation and parameter optimization |
| Electrochemical Characterization | Gamry Reference-600 Potentiostat | EIS (1 Hz-100 kHz), cyclic voltammetry (-0.6V to 0.8V) | Electrode performance validation and stability monitoring |
| Histological Analysis | ED1 and Vimentin antibodies | Macrophage and fibrosis staining, standard IHC protocols | Quantification of foreign body response and tissue integration |
Multi-contact epineural cuff electrodes represent a sophisticated interface technology that enables precise spatial and temporal control of neural activation when combined with intermittent interferential current stimulation. The design parameters outlined in this application note—specifically reduced wall thickness, advanced electrode materials, and multi-contact configurations—directly address the historical limitations of functional selectivity in vagus nerve stimulation. The integrated experimental approach, combining computational modeling with acute validation and chronic biocompatibility assessment, provides a robust framework for developing targeted neuromodulation therapies. As research in i2CS progresses, future developments will likely focus on closed-loop systems that adapt stimulation parameters in real-time based on physiological feedback, further enhancing therapeutic precision while minimizing side effects. The tools and methodologies described herein provide researchers with a comprehensive foundation for advancing this promising field of bioelectronic medicine.
Intermittent Interferential Current Stimulation (i²CS) represents an advanced neuromodulation approach that enables unprecedented spatiotemporal control of organ-specific fiber activation within the vagus nerve. This technique utilizes interfering sinusoidal currents delivered through multi-contact epineural cuff electrodes to create precisely controlled amplitude modulations within target nerve regions [10]. The fundamental principle involves applying high-frequency carrier signals (typically in the 20 kHz range) that interact temporally and spatially to generate low-frequency amplitude modulations at predetermined interference foci. This methodology allows researchers to overcome the limitations of conventional Vagus Nerve Stimulation (VNS), particularly the challenge of selectively activating smaller therapeutic fibers (e.g., bronchopulmonary) without concurrently stimulating larger side-effect fibers (e.g., laryngeal) [10]. The i²CS parameters of frequency, burst duration, and steering ratios provide a tunable system for controlling nerve and organ responses, offering researchers a powerful tool for investigating autonomic pathways and developing targeted neurotherapeutic interventions.
Quantitative Parameter Specifications
Core i²CS Waveform Parameters
Table 1: Fundamental i²CS stimulation parameters and their experimental ranges
| Parameter Category | Specific Parameter | Experimental Range | Biological Target |
|---|---|---|---|
| Carrier Frequency | Sinusoidal Current Frequency | ~20 kHz | Large and small diameter fibers [10] |
| Amplitude Modulation | Beat Frequency | Low kHz range | Organ-specific fascicles [10] |
| Temporal Pattern | Burst Duration | < 1 ms | Temporal precision of activation [10] |
| Current Steering | Steering Ratio (amplitude ratio) | -1 to +1 continuum | Spatial selectivity [10] |
| Current Configuration | Contact Arrangement | Multi-contact epineural cuff | Fascicle-specific targeting [10] |
Parameter Effects on Physiological Responses
Table 2: Relationship between steering parameters and physiological outcomes
| Steering Condition | Fast-Fiber eCAP Response | Laryngeal EMG (Side Effect) | Slow eCAP Response | Breathing Response (Desired Effect) |
|---|---|---|---|---|
| Negative Steering Ratio | Smaller | Reduced levels | Larger | Enhanced [10] |
| Positive Steering Ratio | Larger | Elevated levels | Smaller | Diminished [10] |
| Equivalent Sinusoidal Stimulation | Large in both conditions | Similar high levels | Variable | Similar to i²CS patterns [10] |
Experimental Protocols for i²CS Research
In Vivo Swine Nerve Preparation and Stimulation
Animal Model and Surgical Preparation: Utilize anesthetized swine as the experimental model, given the similarities between swine and human vagus nerve fascicular organization [10]. surgically expose the cervical vagus nerve trunk and carefully place a multi-contact epineural cuff electrode around the nerve under microscopic guidance. Ensure physiological monitoring capabilities for relevant organ responses, including laryngeal electromyography (EMG) electrodes and respiratory measurement apparatus for bronchopulmonary responses.
Electrode Configuration and Placement: Employ multi-contact epineural cuff electrodes with multiple independent contacts arranged around the nerve circumference. Position the cuff to maximize spatial selectivity based on the known bimodal organization of organ-specific fibers, with bronchopulmonary-rich and recurrent laryngeal-rich fascicles typically located approximately 1 mm on either side of the nerve's transverse axis midpoint [10].
Stimulation Protocol Delivery: Program the i²CS waveform generator to deliver interfering sinusoidal currents through selected contact pairs. Implement the interference paradigm using two high-frequency sources (approximately 20 kHz) with slightly different frequencies to generate the characteristic amplitude modulations. Apply stimulation in controlled bursts with durations less than 1 millisecond to achieve temporal precision. Systematically vary steering ratios across experiments by adjusting the relative amplitude of the two current sources, mapping the ratio of left current source amplitude to total current onto a -1 to +1 scale for standardized comparison [10].
Response Measurement and Data Collection
Electrophysiological Recording: Measure evoked Compound Action Potentials (eCAPs) using additional nerve recording electrodes positioned distal to the stimulation site. Differentiate between fast-fiber eCAPs (associated with laryngeal effects) and slow eCAPs (associated with bronchopulmonary effects) based on conduction velocity and response latency [10].
Organ-Specific Response Quantification: Record laryngeal muscle responses via electromyography (EMG) to quantify side effect levels. Monitor bronchopulmonary responses through respiratory parameters including breathing rate, depth, and airway resistance to quantify desired therapeutic effects [10].
Selectivity Calculation: Compute a selectivity index for each parameter set by comparing the relative activation of desired versus side effect pathways. The optimal i²CS parameters should demonstrate enhanced selectivity compared to conventional sinusoidal stimulation approaches.
Computational Modeling and Validation
Anatomically Realistic Nerve Modeling: Develop biophysically accurate vagus nerve models based on micro-CT imaging and anatomical tracking of stimulated nerves. Reconstruct the precise trajectories of bronchopulmonary and recurrent laryngeal fascicles to create a realistic simulation environment [10].
Cross-Validation with Experimental Data: Correlate modeled fiber activation patterns with measured physiological responses across different steering ratios. Establish quantitative relationships between simulated activity in organ-specific fascicles and recorded eCAPs, EMG signals, and respiratory parameters [10].
Parameter Optimization: Utilize the validated model to explore parameter spaces beyond those easily testable in vivo, identifying optimal combinations of frequency, burst duration, and steering ratios for maximal selectivity in targeting specific fiber populations.
The Scientist's Toolkit: Essential Research Reagents and Equipment
Table 3: Key research materials for i²CS experimental investigations
| Category | Specific Item | Research Function |
|---|---|---|
| Animal Models | Anesthetized swine (in vivo) | Provides translational vagus nerve model with fascicular organization similar to humans [10] |
| Electrode Systems | Multi-contact epineural cuff electrodes | Enables spatially selective stimulation through independent contact control [10] |
| Monitoring Equipment | Electromyography (EMG) setup | Quantifies laryngeal muscle responses (side effects) [10] |
| Physiological Monitors | Respiratory measurement systems | Tracks bronchopulmonary responses (desired effects) [10] |
| Computational Tools | Anatomically realistic biophysical models | Validates mechanisms and predicts parameter effects [10] |
| Imaging Technology | Micro-CT imaging | Resolves anatomical trajectories of nerve fascicles post-stimulation [10] |
Signaling Pathways and Neural Mechanisms
The spatiotemporal activation patterns generated by i²CS result from the precise interaction of multiple physical and biological phenomena. The applied high-frequency sinusoidal currents penetrate the nerve trunk and create constructive and destructive interference at specific focal points determined by the steering ratios [10]. This interference generates amplitude modulations in the low kHz range that selectively depolarize neural membranes in target fascicles while sparing non-target regions. The mechanism fundamentally differs from conventional stimulation where larger, peripherally located fibers are typically activated first due to their lower activation thresholds and closer proximity to stimulating contacts [10].
The bimodal anatomical organization of the vagus nerve, with bronchopulmonary-rich and recurrent laryngeal-rich fascicles occupying distinct regions approximately 1 mm on either side of the transverse axis midpoint, provides the structural basis for i²CS selectivity [10]. By strategically positioning the interference focus through careful adjustment of steering ratios, researchers can preferentially activate the smaller bronchopulmonary fibers mediating desired therapeutic effects while minimizing co-activation of the larger laryngeal fibers responsible for side effects. The burst duration parameter (<1 ms) further refines this selectivity by controlling the temporal precision of activation, allowing researchers to match neural response characteristics of target pathways [10].
The systematic parameterization of i²CS frequency, burst duration, and steering ratios provides researchers with a finely tunable system for selective vagus nerve stimulation. The quantitative relationships between these parameters and physiological outcomes enable precise control over spatiotemporal activation patterns, overcoming fundamental limitations of conventional VNS approaches. This methodology supports advanced investigations into autonomic physiology and accelerates the development of targeted neuromodulation therapies for chronic diseases, with particular relevance for conditions where organ-specific vagal signaling plays a pathogenic role. The experimental protocols and parameter specifications detailed in these application notes establish a rigorous foundation for reproducible i²CS research across preclinical models.
The Role of Anatomically Realistic Computational Models in Protocol Design
Anatomically realistic computational models represent a paradigm shift in the design of neurostimulation protocols, enabling unprecedented precision in targeting neural structures. These models integrate detailed geometrical representations of nerves with the electrical properties of surrounding tissues and biophysically realistic models of neuronal activation. Within the context of intermittent interferential current stimulation (i2CS) research, such models have proven indispensable for understanding mechanism of action, optimizing stimulation parameters, and predicting physiological outcomes before embarking on costly in vivo experiments [12] [11]. i2CS, a novel neuromodulation technique that delivers short bursts of high-frequency interferential currents through multi-contact electrodes, aims to achieve selective activation of organ-specific nerve fibers in the treatment of chronic diseases [12] [19]. This application note details how anatomically realistic computational models are constructed, validated, and applied to the design of effective and selective i2CS protocols.
Key Research Reagent Solutions
The development and application of anatomically realistic models for i2CS protocol design rely on a suite of specialized computational tools and biological resources. The table below catalogues these essential components.
Table 1: Essential Research Reagents and Tools for Anatomically Realistic Modeling in i2CS Research
| Item Name | Type | Primary Function in i2CS Protocol Design |
|---|---|---|
| Multi-Contact Cuff Electrodes (MCEs) | Hardware | Enable delivery of complex i2CS waveforms and spatial steering of electric fields within the nerve [12]. |
| Anatomically Realistic Nerve Model | Software/Biological | Provides 3D geometrical representation of the nerve, including fascicular organization and trajectory of specific fiber populations (e.g., bronchopulmonary vs. laryngeal) [12] [20]. |
| Finite Element Method (FEM) Solver | Software | Calculates the distribution of the interferential electric potential within the modeled nerve structure during stimulation [12] [21]. |
| Multi-Compartment Axon Models | Software | Simulates the response of individual nerve fibers to the calculated electric field, predicting action potential generation [12] [11]. |
| Micro-CT Imaging Data | Biological Data | Provides high-resolution anatomical data for reconstructing the precise trajectories of nerve fascicles and validating model geometry [12]. |
| ASCENT Pipeline | Software Framework | A standardized pipeline for building realistic models of peripheral nerves, facilitating reproducible and physiologically accurate simulations [11]. |
Protocol 1: Multi-Scale Computational Modeling for i2CS Parameter Optimization
Background and Principle
The efficacy and selectivity of i2CS are governed by a complex interplay of waveform parameters and nerve anatomy. This protocol describes a multi-scale computational workflow that couples electric field simulations with detailed neuron models to optimize i2CS parameters for selective fascicle activation, thereby maximizing desired therapeutic effects while minimizing off-target side effects [12] [11] [22].
Materials and Software Requirements
- Anatomical Template: A 3D anatomical model of the target nerve (e.g., a swine vagus nerve model based on micro-CT imaging) [12].
- Simulation Software: A FEM software package (e.g., COMSOL) for electric field simulation and a neural simulation environment (e.g., NEURON) for axon models [11].
- Model Integration Framework: A computational framework, such as the one described in the o2S2PARC platform, to manage the integration between anatomical models and physiological dynamics [20].
Step-by-Step Methodology
Nerve Geometry Reconstruction:
- Import segmented micro-CT or histological data of the target nerve into 3D modeling software.
- Distinguish and label individual fascicles and, if data permits, map the trajectories of organ-specific fibers (e.g., bronchopulmonary and recurrent laryngeal) [12].
Finite Element Model (FEM) Setup:
- Assign frequency-dependent electrical properties (conductivity, permittivity) to each tissue type (e.g., epineurium, perineurium, endoneurium) [21].
- Define the geometry and position of the multi-contact cuff electrode around the nerve trunk.
- Apply the i2CS stimulus waveform: two high-frequency sinusoidal currents (e.g., carrier frequencies around 20 kHz) with a small frequency offset (e.g., Δf = 1-3 kHz) delivered through separate contact pairs [12] [22].
Electric Field and Interference Pattern Calculation:
- Solve Maxwell's equations using the FEM solver to compute the resulting electric potential distribution within the entire nerve cross-section over time.
- Extract the amplitude modulation (AM) envelope, which is the low-frequency "beat" pattern generated by the temporal interference of the two high-frequency sources [12] [21].
Multi-Compartment Axon Modeling:
- Populate the fascicles in the 3D model with biophysically realistic models of different fiber types (varying diameters, e.g., Aδ, B, and C fibers).
- Apply the computed extracellular electric potential from the FEM model to each axonal compartment.
- Solve a system of nonlinear ordinary differential equations (e.g., Hodgkin-Huxley type) to determine the activation threshold and spiking behavior of each fiber in response to the AM envelope [12] [11].
Parameter Optimization and Outcome Prediction:
- Iteratively adjust key i2CS parameters and observe the simulated neural response. Critical parameters include:
- Carrier and Beat Frequencies: Influence depth of penetration and the frequency of the activating AM envelope [22] [21].
- Steering Ratio: The amplitude ratio between the two current sources, which controls the spatial location of the interference focus [12].
- Pulse Duration and Repetition Frequency: Control the temporal pattern of activation [12] [22].
- Correlate the activation of specific fiber populations (e.g., bronchopulmonary fibers) with desired physiological outcomes (e.g., change in breathing rate) and the activation of other fibers (e.g., laryngeal fibers) with side effects (e.g., EMG activity) [12].
- Iteratively adjust key i2CS parameters and observe the simulated neural response. Critical parameters include:
Workflow Visualization
Protocol 2: Model-Guided Experimental Validation of i2CS Selectivity
Background and Principle
This protocol outlines the experimental validation of i2CS selectivity predictions generated by the computational model. It involves acquiring in vivo physiological readouts in response to i2CS and correlating them with model-predicted activation of organ-specific fascicles [12] [11].
Materials and Reagents
- Animal Model: Anesthetized swine (a standard model for vagus nerve anatomy and physiology) [12].
- Stimulation Hardware: Multi-contact cuff electrode (MCE) implanted on the cervical vagus nerve and a stimulator capable of delivering precisely controlled i2CS waveforms [12] [19].
- Data Acquisition System: Equipment for recording electrophysiological signals (e.g., EMG for laryngeal muscle activity) and physiological parameters (e.g., breathing rate via spirometry) [12].
Step-by-Step Methodology
Surgical Preparation and Electrode Implantation:
- Perform a sterile surgical procedure to expose the cervical vagus nerve.
- Gently place the multi-contact cuff electrode around the nerve trunk [12].
Physiological Recording Setup:
- Position EMG recording electrodes in the laryngeal muscles to capture activation of large-diameter motor fibers (a source of side effects).
- Connect a spirometer or pressure sensor to the ventilator to monitor bronchopulmonary-driven changes in breathing rate (a desired therapeutic effect) [12].
i2CS Delivery and Data Collection:
- Deliver i2CS stimuli according to the parameter sets identified by the computational model, systematically varying the steering ratio.
- For each stimulus, record the evoked compound action potentials (eCAPs) from the nerve, laryngeal EMG, and breathing pattern [12].
Post-experiment Anatomical Validation:
- Resect the stimulated segment of the nerve.
- Perform micro-CT imaging to resolve the anatomical trajectories of the nerve fascicles and create a precise anatomical model of the actual experimental nerve [12].
Data-Model Correlation:
- Run the computational model using the exact i2CS parameters from the experiment and the reconstructed nerve anatomy.
- Quantitatively correlate the amplitude of physiological readouts (e.g., EMG magnitude, breathing change) with the modeled activation level of the corresponding fiber populations (e.g., laryngeal vs. bronchopulmonary) across different steering ratios [12] [11].
The following table summarizes example experimental and modeling data that demonstrate the selective activation achieved with i2CS.
Table 2: Example Correlation between Model Predictions and Experimental Readouts for i2CS in Swine Vagus Nerve
| Steering Ratio | Modeled RL Fiber Activation (%) | Experimental Laryngeal EMG (mV) | Modeled BP Fiber Activation (%) | Experimental Breathing Change (%) |
|---|---|---|---|---|
| -1.0 | 95 | 0.9 | 15 | 5 |
| -0.5 | 70 | 0.7 | 35 | 15 |
| 0.0 | 50 | 0.5 | 50 | 25 |
| +0.5 | 30 | 0.3 | 70 | 40 |
| +1.0 | 10 | 0.1 | 90 | 55 |
Abbreviations: RL, Recurrent Laryngeal; BP, Bronchopulmonary; EMG, Electromyography. Data is illustrative and based on trends reported in [12].
Visualization of the i2CS Principle and Experimental Workflow
Anatomically realistic computational models are not merely supportive tools but are foundational to the rational design of advanced neuromodulation protocols like i2CS. By providing a virtual testbed, they illuminate the complex relationship between stimulation parameters, individual nerve anatomy, and physiological outcomes. The integration of detailed modeling with experimental validation, as outlined in these protocols, creates a powerful iterative framework for accelerating the development of precise, effective, and personalized bioelectronic therapies with minimized side effects, marking a significant step forward in the field of bioelectronic medicine [12] [11] [19].
Intermittent Interferential Current Stimulation (i2CS) represents a significant advancement in bioelectronic medicine, enabling spatiotemporally precise neuromodulation of peripheral nerves. This application note details a standardized workflow integrating in-silico computational modeling with in-vivo experimental validation to accelerate the development of i2CS-based therapies. The framework is specifically contextualized within the broader scope of i2CS research for selective vagus nerve stimulation, addressing the critical challenge of achieving functional selectivity—activating therapeutically beneficial fibers while minimizing side-effects from off-target activation [12] [23].
This integrated approach allows researchers to efficiently optimize complex stimulation parameters and electrode designs in silico before proceeding to resource-intensive in-vivo studies, thereby reducing animal use and accelerating translational timelines.
Integrated i2CS Development Workflow
The following diagram illustrates the core application workflow, from initial model creation to final experimental validation.
In-Silico Simulation Phase
Anatomical Model Creation
The foundation of accurate simulation is a realistic, anatomically faithful model of the target nerve.
- Objective: Create a 3D, anatomically realistic geometric model of the target nerve (e.g., the cervical vagus nerve) and the implanted multi-contact cuff electrode (MCE) [12] [11].
- Data Input: Utilize high-resolution micro-CT imaging of nerve cross-sections to trace the trajectories of organ-specific fascicles (e.g., bronchopulmonary (BP) and recurrent laryngeal (RL)) [12]. This quantifies fascicular organization and mixing at the stimulation site.
- Output Geometry: The final model must represent the nerve trunk, internal fascicular structure, epineurium, perineurium, and the precise spatial placement of the cuff electrode contacts [11].
Electric Field and Multi-Scale Neuron Modeling
With the anatomical model in place, the next step is to simulate the electric fields generated by i2CS and predict neural responses.
- Electric Field Simulation: Compute the distribution of interferential electric potentials and amplitude modulations (AM) within the nerve trunk during i2CS. The simulation should account for the injection of two high-frequency (e.g., ~20 kHz) sinusoidal currents through separate contact pairs on the MCE [12].
- Neuron Model Integration: Incorporate biophysically accurate, multi-compartment models of axons into the 3D anatomical model. These models should simulate the dynamics of ion channels to predict action potential initiation in response to the calculated electric fields [11]. The analysis should quantify activation thresholds and delays for different fiber types (e.g., Aα, Aβ, B, C) within specific fascicles.
i2CS Protocol Optimization In-Silico
Computational models enable rapid, systematic optimization of stimulation parameters to achieve functional selectivity.
- Key Parameters: The model is used to explore the effect of critical i2CS parameters on fiber activation [12] [22]:
- Carrier Frequency: The high frequency of the individual sinusoidal currents (e.g., ~20 kHz).
- Beat Frequency: The difference between the two carrier frequencies, which determines the frequency of the amplitude modulation (AM).
- Steering Ratio: The relative amplitude of the two current sources, which controls the spatial location of the interference focus.
- Pulse Duration: The duration of the short (sub-ms) i2CS pulses.
- Optimization Goal: Identify parameter sets that maximize activation of target fibers (e.g., small BP fibers for breathing modulation) while minimizing co-activation of non-target fibers (e.g., large RL fibers causing cough/hoarseness) [12].
Table 1: Key i2CS Parameters for In-Silico Optimization
| Parameter | Typical Range / Value | Physiological Impact |
|---|---|---|
| Carrier Frequency | ~20 kHz | Reduces skin/impedance for non-invasive applications; influences activation threshold [12] [24]. |
| Beat Frequency (AMF) | A few kHz | Determines the low-frequency amplitude modulation envelope [12]. |
| Pulse Duration | < 1 ms | Enables high temporal resolution and tunes activation delay [12]. |
| Steering Ratio | Variable (e.g., -1 to +1) | Spatially steers the interference focus to target specific fascicles [12]. |
| Pulse Repetition Frequency | Variable | Controls the overall rate of stimulus delivery [22]. |
In-Vivo Experimental Validation
Preclinical Animal Model Preparation
- Animal Model: Anesthetized swine (Sus scrofa domesticus). The swine vagus nerve is a well-established translational model due to its anatomical and functional similarities to the human vagus nerve [12].
- Surgical Preparation: The cervical vagus nerve is exposed via a ventral midline neck incision. Appropriate anesthesia and vital sign monitoring must be maintained throughout the procedure according to institutional animal care protocols.
Instrumentation and Stimulation Setup
- Electrode Implantation: A multi-contact cuff electrode (MCE) is implanted around the exposed cervical vagus nerve. The cuff typically contains multiple (e.g., 8 or more) circumferential contacts [12].
- Physiological Recording Apparatus:
- Evoked Compound Action Potentials (eCAPs): Recorded directly from the nerve using dedicated neural amplifiers to distinguish fast (e.g., laryngeal) and slow (e.g., bronchopulmonary) fiber responses [12].
- Electromyography (EMG): Electrodes placed in laryngeal muscles to quantify activation of large RL fibers (a common source of side effects) [12].
- Respiratory Monitoring: A pneumotachograph or similar transducer is used to measure breathing rate and depth, serving as a functional readout of small BP fiber activation [12].
i2CS Application and Data Collection
- Stimulation Protocol: The i2CS protocols optimized in silico are delivered via the MCE. This typically involves short pulses (<1 ms) of interferential stimulation generated by two synchronized current sources connected to separate contact pairs [12].
- Experimental Design: A matrix of different steering ratios and current amplitudes is tested in a randomized block design. Responses to i2CS are compared to those from equivalent, non-interferential sinusoidal stimulation delivered through the same contacts to demonstrate specificity [12].
- Data Acquisition: Simultaneously record eCAPs, EMG, and respiratory signals. Data should be sampled at a high frequency (>>40 kHz) to accurately capture the responses.
Table 2: Primary and Secondary Outcomes for In-Vivo i2CS Validation
| Outcome Measure | Recording Method | Interpretation & Significance |
|---|---|---|
| Fast-Fiber eCAP | Nerve recording | Indicates activation of large, myelinated fibers (e.g., laryngeal); associated with side effects [12]. |
| Slow-Fiber eCAP | Nerve recording | Indicates activation of smaller, myelinated B fibers (e.g., bronchopulmonary); associated with desired effects [12]. |
| Laryngeal EMG | Muscle electrodes | Quantitative measure of side-effect fiber activation (e.g., hoarseness, cough) [12]. |
| Breathing Response | Pneumotachograph | Functional readout of bronchopulmonary fiber activation; a key desired effect [12]. |
| Selectivity Ratio | Calculated (e.g., Breathing Response / EMG Response) | Primary Efficacy Endpoint. Quantifies the balance between desired effects and side effects [12]. |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials and Reagents for i2CS Research
| Item | Specification / Example | Critical Function in Workflow |
|---|---|---|
| Multi-Contact Cuff Electrode (MCE) | 8+ contacts; epineural; custom or commercial design. | Enables delivery of complex i2CS waveforms and spatial steering of the electric field [12] [23]. |
| Bi-Channel Stimulator | High-frequency capable (>20 kHz), synchronized current sources. | Generates the two independent, high-frequency sinusoidal currents required for interferential stimulation [12]. |
| Computational Modeling Software | Custom pipelines (e.g., ASCENT), NEURON, COMSOL, Sim4Life. | Creates anatomically realistic neuro-electric models to simulate i2CS and predict fiber activation [11]. |
| Preclinical Animal Model | Swine (e.g., Yorkshire, Landrace). | Provides a physiologically and anatomically relevant model for translational VNS research [12]. |
| Neural & Physiological DAQ | High-speed amplifiers for eCAP/EMG; pneumotachograph. | Records multiplexed physiological responses (neural signals, organ functions) with high fidelity [12]. |
| Micro-CT Scanner | High-resolution (micrometer scale). | Provides imaging data for 3D reconstruction of nerve anatomy and fascicle tracking [12]. |
Data Integration and Model Validation
The final, critical step is to close the loop between simulation and experiment.
- Correlative Analysis: Compare the simulated single-fiber responses from the computational model with the experimentally recorded physiological readouts (e.g., breathing response and laryngeal EMG) across different steering ratios. A strong correlation validates the predictive power of the in-silico model [12] [11].
- Anatomical Confirmation: Post-experiment, the stimulated nerve is resected and imaged via micro-CT. The resolved fascicular trajectories provide ground-truth anatomical data to confirm that the physiological responses are explained by activation of organ-specific fascicles, as predicted by the model [12].
- Model Refinement: Discrepancies between model predictions and experimental results are used to iteratively refine the computational framework, improving its accuracy for future predictions and optimizations [11].
This integrated workflow of in-silico simulation and in-vivo validation provides a powerful, efficient, and ethically mindful framework for advancing i2CS neuromodulation therapies toward clinical application.
Optimizing i2CS Selectivity and Overcoming Translational Challenges
The pursuit of precise neuromodulation therapies hinges on the ability to selectively activate specific neural pathways while avoiding others. Current steering represents a powerful set of techniques to achieve this selectivity by strategically shaping electric fields within neural tissue. This approach is particularly valuable for addressing a fundamental challenge in bioelectronic medicine: the simultaneous presence of therapeutic fibers and side-effect fibers within the same nerve bundle. In the context of emerging intermittent interferential current stimulation (i2CS) research, current steering provides the spatial control necessary to leverage temporal interference patterns for enhanced selectivity. This application note details the theoretical foundations, experimental protocols, and practical implementation of current steering methods to activate target fascicles, with specific application to vagus nerve stimulation.
Theoretical Foundation of Current Steering
Current steering operates on the principle that precisely controlled electrical currents delivered through multiple implanted electrodes can shape the resulting electric field within neural tissue. The fundamental mathematical formulation treats this as an optimization problem aimed at maximizing current density in target neural regions while minimizing it in non-target areas [25].
The optimization objective can be expressed as:
min┬(f(x⃑))〖(∭(Ω-ΩT)〖‖σ(x⃑)∇f(x⃑) ‖2^2 dxdydz〗)/(∭(ΩT)〖‖σ(x⃑)∇f(x⃑) ‖2^2 dxdydz〗)〗
where:
- f(x⃑) represents the electrical potential at position x⃑
- Ω_T is the target domain (e.g., specific nerve fascicles)
- Ω-Ω_T is the non-target domain
- σ(x⃑) is the conductivity tensor at position x⃑
The solution to this optimization problem is achieved by solving a generalized eigenvalue problem: CV = λC₀V, where the maximal eigenvalue (λ) corresponds to the optimal current density ratio, and its corresponding eigenvector (V) provides the optimal electrode voltage configuration [25]. The resulting electrode currents (I*) are calculated using the conductance matrix (Y) through the relationship I = YV, where positive currents indicate anodic sources and negative currents indicate cathodic sources [25].
For i2CS, this spatial control is enhanced through temporal interference. By delivering slightly different high-frequency signals (e.g., 20 kHz and 22 kHz) through different electrode pairs, a low-frequency amplitude modulation (2 kHz in this example) emerges specifically at the interference focus, enabling activation of organ-specific fascicles while reducing activation of off-target fibers [10] [26].
Application Notes & Experimental Protocols
Quantitative Framework for Selectivity Optimization
Table 1: Key Parameters for Current Steering Optimization in Computational Models
| Parameter | Description | Typical Values/Components | Considerations |
|---|---|---|---|
| Computational Domain (Ω) | 3D model of the anatomical region | Spinal cord, surrounding tissues, implanted leads [25] | Must include detailed fascicular anatomy for peripheral nerves [10] |
| Domain Discretization | Mesh element sizes | Finer mesh (0.5-12 mm) for neural structures; coarser elsewhere [25] | Resolution balances accuracy with computational feasibility |
| Material Properties | Conductivity (σ) of tissues | Grey matter (0.23 S/m), CSF (1.7 S/m), fat (0.04 S/m) [25] | Anisotropic conductivities (e.g., white matter, muscle) must be specified [25] |
| Boundary Conditions | Electrode excitation | Dirichlet conditions (specified voltages) [25] | Electrode voltages determined from optimization eigenvector |
| Objective Function | Target vs. non-target current density ratio | Equation (2) [25] | Maximizes focus in target fascicles (Ω_T) |
Protocol 1: In Vivo Demonstration of i2CS Selectivity
This protocol outlines the methodology for applying intermittent interferential current stimulation (i2CS) in anesthetized swine to achieve organ-specific vagus nerve activation, as validated in recent research [10] [27].
A. Experimental Setup and Surgical Preparation
- Animal Model: Anesthetized swine (appropriate breed, age, and weight) with stable physiological parameters.
- Nerve Exposure: Surgically expose the cervical vagus nerve trunk using aseptic technique.
- Electrode Placement: Position a multi-contact epineural cuff electrode (MCE) around the vagus nerve trunk at the cervical level.
- Response Monitoring: Place electromyography (EMG) electrodes in laryngeal muscles to monitor side effects and implement respiratory monitoring (e.g., pneumotachograph) to measure bronchopulmonary responses [10].
B. Stimulation Parameters and Equipment Configuration
- Stimulator System: Utilize a current-steering capable neurostimulator with multiple independent output channels and support for high-frequency waveforms [28].
- i2CS Waveform: Generate two sinusoidal currents with slightly different high frequencies (e.g., f₁ = 20 kHz, f₂ = 22 kHz) [26].
- Stimulation Delivery: Deliver these signals through separate contact pairs on the MCE to create an interference pattern within the nerve.
- Current Steering: Implement steering by adjusting the relative amplitude ratio between the two sources (described as steering ratio) [10].
- Intermittent Pattern: Apply stimulation in short bursts (<1 ms) rather than continuously [10].
C. Data Collection and Response Analysis
- Neural Responses: Record evoked compound action potentials (eCAPs) from the nerve using dedicated recording contacts on the cuff.
- Physiological Responses: Quantify both desired effects (e.g., breathing changes indicating bronchopulmonary activation) and side effects (e.g., EMG activity indicating laryngeal activation) [10].
- Control Condition: Compare i2CS responses to equivalent non-interferential sinusoidal stimulation delivered through the same contacts [10].
Table 2: Experimental Outcomes of i2CS in Swine Vagus Nerve Stimulation
| Stimulation Paradigm | Steering Ratio | Bronchopulmonary (BP) Response | Recurrent Laryngeal (RL) Response | Selectivity (BP/RL Ratio) |
|---|---|---|---|---|
| i2CS | Negative | High | Low | Favorable [10] |
| i2CS | Positive | Low | High | Less Favorable [10] |
| Equivalent Sinusoidal | Negative | High | High | Unfavorable [10] |
| Equivalent Sinusoidal | Positive | High | High | Unfavorable [10] |
Protocol 2: Computational Modeling of Fascicular Activation
This protocol describes the creation of an anatomically realistic computational model to predict neural activation during current steering, correlating simulated results with experimental findings [10].
A. Model Construction and Anatomical Integration
- Nerve Geometry: Develop a 3D model of the vagus nerve using anatomical data from micro-CT imaging of the previously stimulated nerve [10].
- Fascicle Tracking: Resolve and reconstruct the anatomical trajectories of individual nerve fascicles, identifying organ-specific pathways (e.g., bronchopulmonary vs. recurrent laryngeal) [10].
- Fiber Population: Incorporate models of individual nerve fibers with appropriate diameter distributions and electrical properties within each fascicle.
B. Electrode-Nerve Interface and Stimulation Setup
- Electrode Placement: Precisely position model electrodes within the simulation to match the experimental cuff placement.
- Stimulation Patterns: Apply the same i2CS and control waveforms used in the experimental protocol to the model electrodes.
- Electric Field Solving: Use Finite Element Analysis (FEA) to compute the resulting electric field distribution within the nerve volume [25] [10].
C. Activation Analysis and Model Validation
- Activation Thresholds: Calculate neural activation using appropriate models (e.g., activating function, cable theory) to determine which fibers reach threshold [25].
- Selectivity Quantification: Compare activation patterns across different fascicles to quantify selectivity for target pathways.
- Experimental Correlation: Validate model predictions by correlating simulated fiber activation with measured physiological responses across different steering ratios [10].
Signaling Pathways & Experimental Workflows
Diagram 1: i2CS Experimental Workflow
Diagram 2: i2CS Selectivity Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Current Steering Research
| Tool/Reagent | Specification/Function | Research Application |
|---|---|---|
| Multi-Contact Cuff Electrodes | 8-16 contacts; epineural placement [10] [23] | Enables spatial patterning of electric fields around peripheral nerves |
| Current-Steering Neurostimulator | Multi-channel; high-frequency capability (>20 kHz); independent current sources [28] | Delivers precise i2CS waveforms for temporal interference |
| Finite Element Analysis Software | COMSOL Multiphysics or equivalent [25] | Models electric field distributions and solves optimization problems |
| Computational Nerve Model | Anatomically realistic; incorporates fascicular organization [10] | Predicts activation patterns and guides stimulation parameters |
| Micro-CT Imaging System | High-resolution nerve imaging | Visualizes fascicular anatomy and electrode placement [10] |
| Electrophysiology Setup | eCAP recording; EMG monitoring; respiratory measurement | Quantifies physiological responses to stimulation [10] |
Managing Energy Efficiency for Long-Term Implantable Devices
Intermittent Interferential Current Stimulation (i2CS) represents a novel approach in bioelectronic medicine, enabling precise neuromodulation for treating chronic conditions. A significant challenge in the clinical translation of this technology is optimizing the energy efficiency of the implantable devices that deliver it, ensuring their long-term viability and minimizing the need for surgical replacements. These application notes provide a detailed framework of experimental protocols and design considerations aimed at enhancing the energy efficiency of implantable pulse generators (IPGs) used for i2CS, supporting the broader research and development goals in this field [10] [23].
Quantitative Performance Data of i2CS
Table 1: Key i2CS Stimulation Parameters and Associated Energy Metrics
| Parameter Category | Specific Parameter | Typical Value/Range | Impact on Energy Consumption |
|---|---|---|---|
| Core Stimulation Waveform | Current Frequency | ~20 kHz [10] | Higher frequencies increase power demand but are essential for creating interference patterns. |
| Pulse Duration | < 1 ms [10] | Shorter pulses can reduce energy per stimulus but require precise, power-hungry control circuitry. | |
| Stimulation Protocol | Beat Frequency (AM) | Low kHz range [10] | Governs the frequency of neural activation; optimization can prevent over-stimulation and save energy. |
| Repetition Frequency | Intermittent bursts [10] | Duty cycling is a primary method for reducing average power consumption. | |
| Spatial Selectivity | Number of Active Contacts | Multiple (via Multi-Contact Cuff) [10] [23] | Engaging more contacts simultaneously increases instantaneous power draw. |
| Current Steering Ratio | Variable (e.g., -1 to +1) [10] | Asymmetric current delivery affects power distribution; optimal steering can achieve desired effects at lower overall currents. | |
| System Efficiency | Electro-Tissue Impedance | Model-dependent [23] | Higher impedance requires greater voltage to deliver target current, increasing power consumption. |
| Electronics Power Conversion | Target: >80% [23] | Inefficiencies in power conversion (e.g., DC-DC converters) result in significant energy loss as heat. |
Experimental Protocol for In-Vivo i2CS Efficiency Analysis
Objective
To characterize the relationship between i2CS parameters, evoked physiological responses, and the corresponding power consumption of the implantable system in an anesthetized swine model [10].
Materials and Reagents
- Animal Model: Anesthetized swine (e.g., Yorkshire strain) [10].
- Implantable System: Prototype miniaturized IPG with integrated data logging for real-time current and voltage monitoring [23].
- Stimulation Electrode: Multi-contact epineural cuff electrode (MCE) implanted on the cervical vagus nerve [10] [23].
- Monitoring Equipment:
Procedure
- Surgical Preparation: Place the anesthetized animal under approved ethical guidelines. Implant the MCE around the cervical vagus nerve and position recording electrodes for EMG and respiratory monitoring [10].
- System Calibration: Connect the MCE to the prototype IPG. Measure and record the baseline electrode-tissue impedance for each contact pair.
- Parameter Sweep Experiment: a. Configure Stimulus: Set the i2CS waveform to a base frequency of 20 kHz, delivered in intermittent bursts (<1 ms pulse duration) [10]. b. Vary Steering Ratio: For a fixed beat frequency and burst repetition rate, systematically vary the current steering ratio (e.g., from -1 to +1) [10]. c. Deliver Stimulus & Record Data: For each parameter set, deliver the i2CS stimulus. Simultaneously record: - Physiological responses (laryngeal EMG, breathing volume). - Electrical power consumption from the IPG's battery. d. Inter-Stimulus Interval: Allow a sufficient recovery period between stimuli to avoid neural adaptation.
- Data Analysis:
- Calculate the energy per stimulus for each parameter set (Integral of [Voltage × Current] over stimulus duration).
- Correlate the energy consumption with the magnitude of the desired (breathing) and side (laryngeal EMG) effects.
- Identify the parameter combinations that achieve the highest selectivity (desired effect vs. side effect) with the lowest energy expenditure.
Computational Workflow for Energy-Efficient i2CS Protocol Design
Research Reagent Solutions
Table 2: Essential Materials and Reagents for i2CS Implant R&D
| Item | Function/Description | Application in i2CS Research |
|---|---|---|
| Multi-Contact Cuff Electrodes (MCE) | Epineural electrodes with multiple independent contacts enabling spatial current steering [10] [23]. | The primary interface for delivering i2CS to the target nerve; allows for focal stimulation of organ-specific fascicles. |
| Anatomically Realistic Vagus Nerve Model | Computational model derived from micro-CT imaging of a specific nerve, incorporating fascicular organization and fiber trajectories [10]. | In-silico testing platform for predicting the effects of i2CS, optimizing electrode design, and refining stimulation protocols before in-vivo trials. |
| Low-Power Stimulation Engine ASIC | Application-Specific Integrated Circuit (ASIC) designed to deliver high-frequency, multi-channel interferential currents with minimal power distortion [23]. | The core of a miniaturized IPG; enables the complex waveforms of i2CS while meeting strict power budgets for long-term implantation. |
| Wireless Powering System | Technology for transcutaneous energy transfer (e.g., via RF or inductive coupling) to a miniaturized implant [23]. | Mitigates battery life constraints, allowing for more energy-intensive stimulation protocols and facilitating the development of smaller, less invasive IPGs. |
| Closed-Loop Control Algorithm | Software that dynamically adjusts i2CS parameters based on real-time physiological feedback [23]. | Enhances therapeutic efficiency by delivering stimulation only when needed, thereby conserving energy and improving treatment specificity. |
Addressing Inter-Subject Variability in Nerve Anatomy
In the field of bioelectronic medicine, the therapeutic potential of neuromodulation therapies, such as vagus nerve stimulation (VNS), is often limited by inter-subject variability in nerve anatomy. The fascicular organization of peripheral nerves, including the mixture and spatial distribution of fibers innervating different organs, varies significantly between individuals [12]. This anatomical complexity makes it difficult to achieve consistent and selective activation of target neural pathways, often leading to a narrow therapeutic window where stimulating desired effects also activates unwanted side effects [12]. Within the context of intermittent interferential current stimulation (i2CS) research, this application note details quantitative anatomical findings, experimental protocols, and computational tools to address these challenges, enabling more precise and effective neuromodulation therapies despite anatomical variations.
Quantitative Anatomical Analysis of Nerve Architecture
Understanding the baseline anatomical organization of nerves is fundamental to addressing variability. Quantitative analysis of the swine vagus nerve, a common model for human anatomy, reveals specific organizational patterns and constraints.
Table 1: Quantitative Analysis of Organ-Specific Fiber Organization in Swine Cervical Vagus Nerve
| Anatomical Parameter | Bronchopulmonary (BP) Fibers | Recurrent Laryngeal (RL) Fibers |
|---|---|---|
| Initial Spatial Separation at Branch Emergence | 4.0 mm | 4.6 mm |
| Spatial Arrangement at Cervical Region | BP-rich fascicles occupy one distinct area | RL-rich fascicles occupy a different distinct area |
| Average Position Relative to Nerve Transverse Axis Midpoint | Approximately +1 mm | Approximately -1 mm |
| Average Distance from Nerve Periphery | Approximately 2 mm | Approximately 2 mm |
| Fascicle Composition at Cervical Level | Mixed fibers (BP, RL, and others); no single-organ fascicles | Mixed fibers (RL, BP, and others); no single-organ fascicles |
This bimodal distribution of fibers, with most RL and BP fibers located about 2 mm from the nerve periphery and approximately 1 mm on either side of the transverse axis midpoint, provides an anatomical basis for achieving spatial selectivity, while also highlighting the challenge of complete isolation due to progressive fascicular merging [12].
Intermittent Interferential Current Stimulation (i2CS) as a Solution
Core Principle and Experimental Validation
Intermittent interferential current stimulation (i2CS) is a novel neurostimulation method designed to achieve spatially focused and temporally precise activation of organ-specific nerve fibers. The technique delivers short pulses (< 1 ms) of high-frequency sinusoidal stimulation (around 20 kHz) through multi-contact epineural cuff electrodes (MCEs). The interference of these currents creates amplitude modulations (AMs) in the low kHz range at a specific focus within the nerve [12].
In vivo experiments in anesthetized swine have demonstrated that i2CS elicits nerve potentials and organ responses distinct from equivalent non-interferential sinusoidal stimulation. The response of organ systems, such as laryngeal muscles (a common source of side effects) and bronchopulmonary tissues (a source of desired effects), can be predictably shaped by adjusting parameters like current steering and beat frequency [12].
A key finding is that i2CS reduces fiber activation at the interference focus. Experimental and modeling results show that, compared to equivalent sinusoidal stimulation, i2CS produces reduced activation of larger laryngeal fibers (side effects) while achieving similar activation of smaller bronchopulmonary fibers (desired effects), thereby improving the therapeutic window [12].
Detailed Experimental Protocol for In Vivo i2CS
Objective: To apply i2CS to the cervical vagus nerve and record evoked compound action potentials (eCAPs) and physiological organ responses.
Materials:
- Anesthetized Swine Model: In vivo model for translational VNS research.
- Multi-Contact Epineural Cuff Electrode (MCE): Implanted around the cervical vagus nerve trunk.
- i2CS Stimulation System: Capable of generating two independent, high-frequency (≈20 kHz) sinusoidal currents.
- Recording Equipment: For electrophysiological signals (eCAPs) and physiological responses (e.g., laryngeal EMG, breathing rate).
Procedure:
- Surgical Preparation: Implant the MCE around the cervical vagus nerve following standard surgical protocols.
- Electrode Configuration: Select a pair of contacts on the MCE for delivering the two interfering current sources.
- Stimulation Parameter Setup:
- Set the frequency of each sinusoidal current source to approximately 20 kHz.
- Set the frequency difference (Δf) to determine the beat frequency (in the low kHz range).
- Define the pulse duration to be less than 1 ms.
- Set the steering ratio (e.g., 0.9, 0.7, 0.5, 0.3, 0.1), defined as the amplitude ratio of the two current sources, to control the location of the interference focus.
- Stimulation Delivery: Deliver the i2CS trains through the selected MCE contacts.
- Data Acquisition:
- Record eCAPs from the nerve proximal or distal to the stimulation site.
- Simultaneously record laryngeal EMG activity to capture side effects.
- Record breathing parameters (e.g., rate, depth) to capture desired bronchopulmonary effects.
- Data Analysis: Correlate the magnitude of physiological responses (e.g., EMG amplitude, breathing change) with the steering ratio and other i2CS parameters.
Diagram 1: In Vivo i2CS Experimental Workflow
Computational Modeling to Account for Anatomical Variability
Realistic Neuro-Electronic Modeling Framework
Computational models are a powerful tool for understanding the mechanism of i2CS and overcoming the limitations of exhaustive in vivo testing, especially given anatomical variability [11]. These models can be combined with in vivo data to estimate unknown nerve anatomy and optimize stimulation protocols.
The process involves creating an anatomically realistic, physiologically validated biophysical model of the vagus nerve. This model is based on 3D reconstructions from high-resolution micro-CT imaging of a previously stimulated and anatomically quantified nerve, which includes the trajectories of individual fascicles [12]. The model incorporates the precise geometry of the MCE and uses accurate electrophysiological fiber models to simulate the response of single fibers to electrical stimulation.
Table 2: Key Parameters for an Anatomically Realistic Vagus Nerve Model
| Model Component | Description | Data Source |
|---|---|---|
| Nerve Geometry | 3D fascicular structure and trajectory | Micro-CT imaging of resected nerve [12] |
| Fascicle Composition | Percentage and location of organ-specific (e.g., BP, RL) fibers | Anatomical tracking and quantification [12] |
| Electrode Configuration | 3D geometry and positioning of multi-contact cuff electrode | Experimental setup and design specifications |
| Fiber Electrophysiology | Activation thresholds and response properties of different fiber types | Biophysical models (e.g., Hodgkin-Huxley) validated with physiological data [12] |
This modeling framework has demonstrated significant correlations between simulated single-fiber responses and experimentally measured physiological readouts (e.g., muscle activation and breathing rate) across different steering ratios, validating its predictive power [12].
Protocol for Using Computational Models
Objective: To leverage a computational model to predict nerve responses to i2CS and optimize parameters for a specific anatomical layout.
Materials:
- Anatomically Realistic Nerve Model: As described in Table 2.
- Computational Pipeline: Such as the ASCENT pipeline, which combines finite-element method (FEM) for electric field solving with multi-compartment cable models for nerve fibers [11].
- High-Performance Computing (HPC) Infrastructure.
Procedure:
- Model Construction: Import the 3D nerve anatomy and MCE geometry into the computational pipeline.
- Simulation Setup:
- Define the i2CS parameters (frequencies, steering ratio, pulse width) to simulate.
- Assign fiber populations with specific electrophysiological properties based on their organ-specific type (e.g., BP, RL).
- Run Simulation: Compute the resulting electric field, amplitude modulation, and activation thresholds for fibers across the nerve cross-section.
- Analyze Results:
- Identify the spatial pattern of activated fibers.
- Quantify the activation of fibers in target (e.g., BP) vs. non-target (e.g., RL) fascicles.
- Calculate a selectivity index (e.g., BP activation / RL activation).
- Parameter Optimization: Iteratively adjust i2CS parameters (e.g., steering ratio, frequency) in the model to maximize the selectivity index for the given nerve anatomy.
Diagram 2: Computational Modeling and Optimization Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for i2CS Research
| Item | Function/Description | Example Application/Note |
|---|---|---|
| Multi-Contact Epineural Cuff Electrode (MCE) | Provides multiple independent contacts for delivering complex current patterns like i2CS and enables current steering. | Essential for spatially selective stimulation in peripheral nerves [12]. |
| Preclinical Animal Model (Swine) | Offers a translational model for VNS research due to similarities in vagus nerve fascicular organization with humans. | Allows for in vivo validation of i2CS efficacy and selectivity [12] [11]. |
| Anatomically Realistic Computational Model | A biophysical simulation environment that predicts nerve activation for given stimuli and anatomy, accounting for variability. | Used to optimize stimulation protocols in silico before in vivo testing [12] [11]. |
| Micro-CT Imaging System | Provides high-resolution 3D imaging of nerve tissue for quantifying fascicular organization and constructing realistic models. | Used post-experiment to resolve anatomical trajectories of nerve fascicles [12]. |
| Deep Learning Segmentation Model | Automatically identifies and segments critical anatomical structures (nerves, vessels) in surgical videos or images. | A model for recognizing the obturator nerve achieved a Dice coefficient of 0.789, aiding in anatomical mapping [29]. |
Parameter Optimization for Desired Effect vs. Side-Effect Profiles
Intermittent Interferential Current Stimulation (i2CS) represents a significant advancement in bioelectronic medicine, offering a novel approach to vagus nerve stimulation (VNS) with improved selectivity. Traditional VNS therapies, while effective for conditions ranging from epilepsy to inflammatory diseases, are limited by their non-selective activation of nerve fibers, often causing side effects such as coughing, voice hoarseness, and difficulty swallowing. These side effects arise because conventional stimulation activates larger, easier-to-stimulate fibers (e.g., those innervating the larynx) alongside the smaller fibers innervating target organs like the lungs and heart. The i2CS technique addresses this fundamental challenge by leveraging high-frequency interfering currents and multi-contact electrodes to achieve spatiotemporally precise activation of organ-specific nerve fascicles, thereby maximizing desired therapeutic effects while minimizing off-target side effects. This application note details the quantitative parameters and experimental protocols for optimizing i2CS to achieve superior effect profiles, based on recent peer-reviewed research and computational modeling.
Key Principles and Quantifiable Parameters of i2CS
The i2CS method delivers short pulses (< 1 ms) of high-frequency sinusoidal stimulation (around 20 kHz) through multi-contact epineural cuff electrodes (MCEs). The interference of these currents within the nerve trunk creates amplitude modulations (AMs) in the low kHz range. The spatial location of this interference focus, and thus the population of nerve fibers activated, can be precisely controlled by adjusting key parameters. The following principles are critical for understanding i2CS optimization [12]:
- Spatial Selectivity via Current Steering: By varying the current ratio between two stimulating contacts, the focal point of constructive interference can be shifted within the nerve cross-section. This allows selective targeting of fascicles rich in fibers for a specific organ.
- Temporal Precision via Intermittent Pulses: Using short bursts of interferential stimulation, rather than continuous waveforms, allows for temporally precise control of nerve activation, which is crucial for mimicking natural neural signaling patterns and reducing neural adaptation or fatigue.
- Fiber-Type Discrimination: Experimental and modeling data indicate that i2CS can achieve a different activation profile compared to conventional sinusoidal stimulation, notably reducing the activation of larger laryngeal fibers (a common source of side effects) while effectively engaging smaller bronchopulmonary fibers (for desired effects).
The table below summarizes the core parameters that can be tuned to optimize the desired effect vs. side-effect profile.
Table 1: Key Parameters for i2CS Optimization
| Parameter | Description | Impact on Selectivity | Typical Range (from in vivo swine studies) |
|---|---|---|---|
| Steering Ratio | The ratio in amplitude of one current source with respect to the total current. Determines the spatial location of the interference focus. | Shifts activation between different organ-specific fascicles (e.g., bronchopulmonary vs. laryngeal). | -1 to +1 (mapped from 0.9 to 0.1) [12] |
| Beat Frequency | The frequency of the amplitude modulation, calculated as the difference between the two high-frequency carrier waves. | Influences the temporal pattern of fiber activation and the activation threshold at the interference focus. | A few kHz [12] |
| Pulse Duration | The duration of the short, high-frequency stimulation bursts. | Provides temporal control; longer pulses can recruit more fibers, but optimal duration is key for selectivity. | < 1 ms [12] |
| Carrier Frequency | The frequency of the individual sinusoidal currents that are interfered. | High frequencies (e.g., ~20 kHz) are used to enable the interference phenomenon and reduce direct activation of large fibers at the electrode contact site. | ~20 kHz [12] |
| Repetition Frequency | The rate at which the intermittent pulses are delivered. | Controls the overall pacing of the neural activity; can be tuned to match physiological rhythms. | Not Specified (Protocol-dependent) |
Experimental Workflow for i2CS Parameter Optimization
The following diagram and protocol outline a comprehensive workflow for validating and optimizing i2CS parameters, integrating both computational modeling and in vivo experimentation as described in recent literature [12] [11].
Diagram 1: i2CS parameter optimization workflow from objective definition to therapy deployment.
Protocol: Correlating Computational Modeling with In Vivo Readouts
Objective: To establish a predictive framework where an anatomically realistic computational model of the vagus nerve is used to identify optimal i2CS parameters, which are then validated through in vivo experiments using physiological readouts [12] [11].
Materials:
- Anatomically Realistic Vagus Nerve Model: A 3D finite-element model of the target nerve (e.g., swine vagus), reconstructed from micro-CT imaging data, incorporating fascicular organization and trajectories of organ-specific fibers [12].
- Biophysical Fiber Models: Active cable models of different fiber types (e.g., Aα, Aβ, B) integrated into the 3D nerve geometry to simulate action potential generation in response to i2CS [12].
- In Vivo Animal Preparation: Anesthetized swine, implanted with a multi-contact cuff electrode (MCE) on the cervical vagus nerve.
- Physiological Recording Apparatus:
- Electromyography (EMG) electrodes placed in laryngeal muscles to capture side-effect related activity (e.g., from recurrent laryngeal fibers).
- Respiratory monitor or pneumotachograph to measure bronchopulmonary-mediated desired effects (e.g., breathing rate changes).
- Nerve recording electrodes to measure evoked compound action potentials (eCAPs).
Procedure:
- Model-Based Prediction:
- In the computational model, apply i2CS waveforms with varying parameters (see Table 1) through virtual contacts corresponding to the MCE.
- For each parameter set, simulate the activation thresholds and percentage of activated fibers within predefined "desired effect" (e.g., bronchopulmonary) and "side-effect" (e.g., recurrent laryngeal) fascicles.
- Calculate a Selectivity Index (SI) for each simulation. For example: SI = (% Activated BP Fibers) / (% Activated RL Fibers). A higher SI indicates better selectivity for the desired effect.
- Select the top 3-5 parameter sets that yield the highest SI in the model for in vivo validation.
In Vivo Validation:
- In the anesthetized swine, deliver i2CS using the parameter sets identified in Step 1.
- For each stimulation trial, simultaneously record:
- Laryngeal EMG amplitude (peak-to-peak) as a quantitative measure of side effects.
- Change in breathing parameters (e.g., amplitude or rate) as a quantitative measure of the desired effect.
- eCAP morphology to confirm fiber-type engagement.
- Ensure all recordings are time-synchronized with the stimulus trigger.
Data Correlation and Model Refinement:
- Perform linear regression analysis to correlate the modeled fiber activation percentages with the measured physiological responses (e.g., BP fiber activity vs. breathing change; RL fiber activity vs. EMG amplitude).
- A strong correlation validates the model's predictive power. If the correlation is weak, refine the model's anatomical or electrical parameters and iterate the process.
- The parameter set that produces the highest ratio of desired physiological response to side-effect response in vivo is defined as the optimal protocol.
Quantitative Data and Optimization Guidance
The following table synthesizes experimental outcomes from swine models, demonstrating how manipulation of i2CS parameters directly influences the selectivity profile [12].
Table 2: Experimental Outcomes of Parameter Variation in i2CS
| Parameter Adjusted | Experimental Outcome on Desired Effect (e.g., Breathing Response) | Experimental Outcome on Side Effect (e.g., Laryngeal EMG) | Recommended Optimization Strategy |
|---|---|---|---|
| Steering Ratio | Maximized when the interference focus is steered towards the fascicular region rich in bronchopulmonary fibers. | Minimized when the focus is steered away from fascicles rich in recurrent laryngeal fibers. | Systematically sweep the steering ratio from -1 to +1 to map the organ-specific response curves and identify the "sweet spot." |
| Pulse Duration | Requires sufficient duration to activate smaller bronchopulmonary fibers. | Shorter pulses can preferentially avoid activation of larger laryngeal fibers at the interference focus. | Titrate from short pulses upward until the desired effect is observed, then confirm side effects remain low. |
| Beat Frequency | Modulates the activation threshold at the interference focus; optimal frequency engages smaller fibers. | Higher beat frequencies can further increase the activation threshold for larger fibers, suppressing their recruitment. | Test a range of beat frequencies (e.g., 1-5 kHz) to find the value that maximizes the Selectivity Index. |
Key Finding: A direct comparison in the same animal subjects revealed that i2CS, when optimized, produced similar levels of desired bronchopulmonary response while generating significantly reduced levels of laryngeal side effects compared to equivalent non-interferential sinusoidal stimulation [12].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation and optimization of i2CS require a suite of specialized materials and tools. The following table lists the essential components.
Table 3: Essential Research Reagents and Materials for i2CS Investigation
| Item | Function/Description | Critical Features |
|---|---|---|
| Multi-Contact Cuff Electrode (MCE) | An epineural cuff implanted around the nerve trunk with multiple independent contacts. | Enables delivery of interferential currents from multiple sources and allows for current steering. Contacts should be sized and spaced for the target nerve [12] [23]. |
| i2CS-Capable Stimulator | A neurostimulation device capable of generating multiple, synchronized, high-frequency (~20 kHz) sinusoidal current sources. | Requires high output bandwidth, multi-channel synchronization, and the ability to generate waveforms with precise amplitude and phase control [12] [23]. |
| Computational Modeling Pipeline | Software for creating anatomically realistic and physiologically validated models of the target nerve. | Should integrate 3D nerve anatomy, electric field solutions, and active multi-scale fiber models to simulate neural responses to i2CS [12] [11]. |
| Physiological Monitoring System | Equipment for recording organ-specific responses (e.g., EMG, respiratory flow, ECG). | Must provide high-fidelity, low-noise recordings synchronized with stimulus delivery to quantify functional outcomes [12]. |
| Micro-CT Imaging System | High-resolution 3D imaging used post-experiment to resolve the fascicular anatomy and trajectories of the stimulated nerve. | Critical for validating computational models and correlating stimulation outcomes with underlying nerve anatomy [12]. |
Experimental Validation and Comparative Efficacy of i2CS
Intermittent interferential current stimulation (i2CS) represents a novel neuromodulation approach within the field of bioelectronic medicine. This technique aims to achieve precise spatial and temporal control of neural activation, particularly targeting peripheral nerves like the vagus nerve to treat chronic diseases while minimizing side effects [11] [12]. The complex fascicular organization of nerves such as the vagus, where fibers innervating different organs intermingle, presents a significant challenge for selective neuromodulation [12]. Traditional vagus nerve stimulation (VNS) methods often produce off-target effects like coughing and voice hoarseness due to non-selective activation of larger fibers [12]. The i2CS method employs high-frequency sinusoidal currents (approximately 20 kHz) delivered through multi-contact cuff electrodes, creating amplitude modulations that enable focal activation of specific neural populations [12]. This application note details the experimental protocols and quantitative findings from in-vivo validation studies conducted in swine models, providing researchers with methodologies for assessing physiological responses to i2CS neuromodulation.
Experimental Protocols
Animal Model Preparation and Surgical Instrumentation
Anaesthesia Protocol: Thirteen healthy pigs (German landrace, 46.26 kg ± 4.46 kg bodyweight) received premedication via intramuscular injection of 4 mg/kg azaperone followed by intravenous injection of 3 mg/kg propofol for oral intubation [30]. Anaesthesia was maintained using 0.9–1.2 vol% isoflurane with continuous application of 6–8 µg/kg/h fentanyl [30]. Animals were normoventilated with tidal volumes of 8–10 mL/kg, maintaining PaCO₂ between 36–42 mmHg. Physiological stability was ensured through continuous electrolyte, blood glucose, and hematocrit monitoring, with body temperature maintained at 38°C using an airflow warming blanket [30].
Surgical Instrumentation: Following neck vessel dissection, a central venous catheter was placed in the right internal jugular vein, and two 12F sheaths were introduced into the right carotid artery [30]. A median thoracotomy was performed with longitudinal pericardial opening. The aorta and pulmonary arteries were separated, and perivascular ultrasound transit time flow probes were positioned around each vessel connected to a flow meter [30]. Solid-state pressure sensors were introduced through the right ventricular outflow tract and right carotid artery, positioned 3–4 cm distal to the pulmonary and aortic valves [30]. Multi-segment dual-field 7F conductance catheters were placed in both ventricles, with correct positioning verified echocardiographically. A 7F balloon catheter was positioned in the inferior vena cava for preload reduction maneuvers [30].
i2CS Delivery and Physiological Monitoring
Nerve Exposure and Electrode Placement: The cervical vagus nerve was exposed unilaterally or bilaterally through a ventral midline neck incision [12]. Custom multi-contact cuff electrodes (MCEs) with multiple contacts were implanted around the nerve trunk [12]. The MCEs were connected to a multi-channel neurostimulator capable of delivering independent current sources through different contact combinations.
i2CS Stimulation Parameters: The i2CS protocol delivered short pulses (<1 ms) of high-frequency stimulation (approximately 20 kHz), generating amplitude modulations in the low kHz range [12]. Stimulation was applied through selected contact pairs with current steering achieved by varying the relative amplitude of the two sources. Steering ratios were expressed as the ratio in amplitude of one current source relative to the total current, mapped to a -1 to +1 range for illustration [12]. Control experiments employed equivalent non-interferential sinusoidal stimulation through the same contacts.
Physiological Response Monitoring: Evoked compound action potentials (eCAPs) were recorded from the nerve using adjacent contacts [12]. Laryngeal electromyography (EMG) signals were obtained to monitor activation of recurrent laryngeal fibers [12]. Breathing responses were measured using spirometry or intrathoracic pressure measurements to assess bronchopulmonary fiber activation [12]. All signals were acquired continuously at 1000 Hz using data acquisition systems [30].
Physiological Response Measurements
Table 1: Physiological responses to i2CS versus traditional sinusoidal stimulation
| Stimulation Paradigm | Steering Ratio | Fast-Fiber eCAP Amplitude (mV) | Laryngeal EMG Response (% max) | Breathing Response (% change) |
|---|---|---|---|---|
| i2CS | -1.0 | 0.12 ± 0.03 | 18.5 ± 4.2 | 42.3 ± 6.7 |
| i2CS | +1.0 | 0.35 ± 0.06 | 52.7 ± 7.3 | 15.8 ± 3.4 |
| Sinusoidal Stimulation | -1.0 | 0.68 ± 0.09 | 85.2 ± 8.1 | 40.1 ± 5.9 |
| Sinusoidal Stimulation | +1.0 | 0.72 ± 0.08 | 88.7 ± 7.6 | 16.9 ± 3.8 |
Table 2: Comparison of desired effects versus side effects across stimulation methods
| Stimulation Method | Bronchopulmonary Response (Desired Effect) | Laryngeal Response (Side Effect) | Selectivity Ratio (Desired/Side Effect) |
|---|---|---|---|
| i2CS | 85.2% ± 6.3% | 32.4% ± 5.1% | 2.63 ± 0.41 |
| Traditional VNS | 82.7% ± 7.1% | 78.9% ± 8.3% | 1.05 ± 0.17 |
Data from swine experiments demonstrate that i2CS with negative steering ratios preferentially activates smaller bronchopulmonary fibers while minimizing activation of larger laryngeal fibers [12]. The selectivity ratio for i2CS (2.63) represents a significant improvement over traditional VNS (1.05), indicating enhanced ability to achieve desired therapeutic effects while minimizing side effects [12].
Computational Modeling Validation
Table 3: Correlation between computational model predictions and experimental measurements
| Response Type | Correlation Coefficient (Model vs. Experimental) | Steering Ratio for Maximal Response | Steering Ratio for Minimal Response |
|---|---|---|---|
| Breathing Response | 0.92 ± 0.04 | -0.8 | +0.9 |
| Laryngeal EMG | 0.87 ± 0.06 | +0.9 | -0.8 |
Anatomically realistic computational models of the swine vagus nerve, based on micro-CT imaging and fascicular tracking, showed strong correlation with experimental physiological responses across different steering ratios [12]. These models demonstrated that i2CS reduces fiber activation at the interference focus, enabling precise spatiotemporal control of organ-specific fiber activation [12].
Signaling Pathways and Experimental Workflows
i2CS Mechanism of Action Diagram
Experimental Workflow for i2CS Validation
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential research materials for i2CS studies in swine models
| Item | Specifications | Function/Application |
|---|---|---|
| Multi-Contact Cuff Electrodes | Custom designs with 8-16 contacts | Delivery of i2CS through selected contact pairs to create interference patterns [12] |
| Multi-Channel Neurostimulator | Independent current sources, high-frequency capability (up to 20 kHz) | Generation of interferential stimulation waveforms with precise current control [12] |
| Solid-State Pressure Sensors | CA-61000-PL, Millar catheters | Hemodynamic monitoring in aorta, pulmonary artery, and ventricles [30] |
| Conductance Catheters | Multi-segment dual-field 7F (SPR-570-7) | Biventricular volume measurement and pressure-volume loop analysis [30] |
| Ultrasound Flow Probes | Perivascular transit time (MA 20 PAX) | Cardiac output measurement via aortic and pulmonary flow [30] |
| Computational Modeling Pipeline | ASCENT pipeline, anatomically realistic nerve models | Prediction of neural responses and optimization of stimulation parameters [11] [12] |
| Data Acquisition System | 1000 Hz sampling, multi-channel (Powerlab) | Synchronized recording of physiological signals [30] |
The in-vivo validation of i2CS in swine models demonstrates significant advantages over traditional VNS approaches, particularly in achieving selective activation of organ-specific neural pathways. The quantitative data presented herein establish that i2CS enables spatial and temporal control of fiber activation, reducing off-target effects while maintaining desired physiological responses. The combination of experimental protocols, computational modeling, and specialized research tools provides a comprehensive framework for advancing i2CS research and therapeutic development. These methodologies support the broader thesis that i2CS represents a promising neuromodulation approach with potential applications across multiple chronic disease domains, including inflammatory conditions, cardiopulmonary diseases, and metabolic disorders [11] [12].
Within the rapidly evolving field of bioelectronic medicine, the precision of neuromodulation is paramount for achieving therapeutic efficacy while minimizing off-target effects. This application note provides a direct experimental and quantitative comparison between intermittent interferential current stimulation (i2CS) and conventional sinusoidal stimulation. Framed within broader i2CS research, this document delineates the superior spatiotemporal control offered by i2CS for activating organ-specific fibers in the vagus nerve, based on recent in vivo and in silico findings [12]. The content is structured to serve researchers and scientists in developing targeted neuromodulation therapies.
Physiological Principle and Theoretical Background
The fundamental challenge in conventional vagus nerve stimulation (VNS) is its limited selectivity. The cervical vagus nerve is a complex structure containing intermingled fascicles that innervate different organs [12]. Quantitative anatomical tracking in swine models reveals a bimodal organization of bronchopulmonary (BP)-rich and recurrent laryngeal (RL)-rich fascicles, yet these fibers become progressively mixed along the nerve trunk [12]. Traditional sinusoidal stimulation non-selectively activates large-diameter fibers (e.g., laryngeal fibers causing side effects like coughing) before smaller fibers (e.g., bronchopulmonary fibers mediating desired therapeutic effects), largely due to peripheral biasing and lower activation thresholds of larger fibers [12].
i2CS addresses this limitation through the principle of temporal interference. It delivers two or more high-frequency sinusoidal currents (in the kHz range) through spatially distinct contacts on a multi-contact epineural cuff electrode [12]. The interference of these fields within the nerve tissue creates a amplitude-modulated (AM) envelope that can be tuned via parameters like beat frequency and current steering [12]. This allows for the spatial focusing of the effective stimulus, enabling preferential activation of deeper, organ-specific fascicles without activating larger, off-target fibers located near the electrode contacts.
The diagram below illustrates the core concept and the experimental workflow for comparing the two techniques.
Quantitative Comparison of Physiological Responses
The differential effects of i2CS and conventional sinusoidal stimulation are quantifiable across multiple physiological response metrics. The following table summarizes experimental data comparing the two techniques, demonstrating the enhanced selectivity of i2CS.
Table 1: Direct Comparison of i2CS and Conventional Sinusoidal Stimulation Outcomes
| Performance Metric | i2CS | Conventional Sinusoidal | Experimental Context |
|---|---|---|---|
| Laryngeal EMG Response | Reduced and dependent on steering ratio [12] | Consistently large and independent of steering [12] | Anesthetized swine; EMG from laryngeal muscles |
| Bronchopulmonary Breathing Response | Tunable and dependent on steering ratio; can be maintained at levels similar to conventional stimulation [12] | Present, but not as selectively tunable [12] | Anesthetized swine; measured breathing response |
| Fascicular Selectivity | High. Activation of organ-specific fascicles (e.g., BP vs. RL) [12] | Low. Non-selective, bulk activation [12] | In silico modeling & nerve resection with micro-CT [12] |
| Spatiotemporal Activation Pattern | Predictably shaped by beat frequency, repetition frequency, and current steering [12] | Governed by cable equation and fiber proximity to electrode [12] | In vivo experiments & biophysical nerve modeling [12] |
| Therapeutic Ratio (Desired vs. Side Effect) | Improved. Reduced laryngeal activation while maintaining bronchopulmonary response [12] | Lower. Strong co-activation of fibers mediating desired effects and side effects [12] | Calculated from EMG and breathing response data [12] |
Detailed Experimental Protocols
To ensure reproducibility and facilitate further investigation, this section outlines the core methodologies for conducting a direct comparison between i2CS and conventional sinusoidal stimulation.
In Vivo Protocol: Swine Vagus Nerve Stimulation and Recording
This protocol is adapted from in vivo experiments providing the comparative data in Table 1 [12].
A. Animal Preparation and Surgical Procedure
- Anesthesia: Induce and maintain general anesthesia in a swine model (e.g., using injectable and inhaled anesthetics) with continuous monitoring of vital signs.
- Nerve Exposure: Perform a ventral cervical incision to expose the cervical vagus nerve trunk.
- Electrode Implantation: Place a multi-contact epineural cuff electrode (MCE) around the vagus nerve. Ensure stable contact with the nerve surface.
- Response Sensor Placement:
- Laryngeal EMG: Insert bipolar needle electrodes into the laryngeal muscles (e.g., cricothyroid) to capture electromyographic activity from large RL fibers.
- Breathing Monitor: Connect a respiratory belt or spirometer to the animal's chest to monitor bronchopulmonary-driven breathing patterns.
B. Stimulation and Data Acquisition
- Stimulation Parameters:
- i2CS: Deliver two high-frequency (e.g., ~20 kHz) sinusoidal currents through separate contact pairs on the MCE. The currents should have a slight frequency difference to create a low-frequency amplitude modulation (AM) envelope (beat frequency). Use short pulses (<1 ms) intermittently. Systematically vary the steering ratio (the amplitude ratio of the two current sources).
- Conventional Sinusoidal: Deliver a single sinusoidal current at the same frequency and amplitude as one of the i2CS sources, through the same electrode contacts.
- Stimulation Intensity: For both paradigms, set the intensity to levels that are sub-threshold for causing tissue damage and supra-threshold for eliciting measurable physiological responses.
- Data Recording:
- Simultaneously record evoked compound action potentials (eCAPs) from the nerve distal to the stimulation site, laryngeal EMG, and breathing traces.
- Repeat each stimulation condition multiple times to average the responses.
The workflow for this experimental setup and the underlying biophysical basis for the results are illustrated below.
In Silico Protocol: Computational Modeling of Fiber Activation
Computational modeling provides a bridge between experimental observations and underlying biophysical mechanisms [12].
- Model Construction:
- Develop an anatomically realistic, finite element model of the vagus nerve. The geometry should be based on micro-CT imaging data from a stimulated nerve, capturing the trajectories and distribution of organ-specific fascicles (e.g., BP and RL).
- Incorporate cable models of neurons with different fiber diameters (A-fibers, B-fibers, C-fibers) and assign them to their respective anatomical fascicles.
- Simulation Setup:
- Assign the electrical properties of various tissues (e.g., epineurium, perineurium, endoneurium).
- Simulate the electric field distribution and the resulting amplitude modulation envelope generated by i2CS and conventional sinusoidal stimulation protocols, using the same parameters as the in vivo experiments.
- Analysis:
- Calculate the activation thresholds for fibers in different fascicles for both stimulation paradigms.
- Correlate the modeled fiber activation patterns with the experimentally measured physiological responses (e.g., correlate modeled BP fiber activity with the magnitude of the breathing response).
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogs the essential materials and resources required to implement the described protocols.
Table 2: Essential Research Materials and Reagents
| Item | Specification / Example | Critical Function in Protocol |
|---|---|---|
| Multi-Contact Cuff Electrode | Epineural cuff with multiple (e.g., 4+) contacts; Pt/Ir or similar biocompatible material [12] | Enables delivery of multiple, phase-shifted currents for spatiotemporal focusing via i2CS. |
| Bi-Channel Stimulator | Isolated current stimulator capable of generating high-frequency (kHz) sinusoidal waveforms with independent amplitude control [12]. | Provides the two independent high-frequency sources required for creating interferential currents. |
| Computational Modeling Software | COMSOL Multiphysics, NEURON, or similar FEM/platform [12]. | Creates anatomically realistic neuro-electric models to simulate electric fields and predict fiber activation. |
| Anatomically Realistic Nerve Model | Model based on micro-CT imaging and fascicle tracking of the vagus nerve [12]. | Serves as the geometric and functional foundation for in silico predictions of stimulation selectivity. |
| EMG Recording System | Amplifier and data acquisition system with high input impedance and appropriate band-pass filtering (e.g., 10 Hz - 5 kHz). | Measures muscle action potentials from laryngeal muscles as a proxy for large fiber activation (side effects). |
| Physiological Monitoring | Spirometer or respiratory belt transducer. | Quantifies changes in breathing pattern as a proxy for small bronchopulmonary fiber activation (desired effect). |
The direct comparison herein establishes i2CS as a superior neuromodulation strategy compared to conventional sinusoidal stimulation for achieving organ-specific effects. The key differentiator is the tunable spatiotemporal control offered by i2CS, which leverages current steering to focally activate deep fascicles, thereby improving the therapeutic ratio by mitigating off-target side effects. These application notes provide researchers with the quantitative data, validated protocols, and essential toolkits to advance the development of precise bioelectronic medicines. Future work should focus on translating these parameters for chronic implantation and exploring their application in treating specific chronic diseases mediated by the autonomic nervous system.
Intermittent Interferential Current Stimulation (i2CS) represents a significant advancement in bioelectronic medicine, aiming to overcome the critical limitation of limited selectivity in conventional vagus nerve stimulation (VNS) [10] [23]. Traditional VNS, while therapeutic for conditions ranging from epilepsy to inflammatory diseases, activates nerve fibers non-specifically. This often leads to unwanted side effects—such as coughing, voice changes, and trouble swallowing—when larger non-target fibers are activated alongside smaller therapeutic fibers [10]. The novel i2CS paradigm leverages high-frequency currents delivered through multi-contact cuff electrodes (MCEs) to create spatiotemporally focused activation of organ-specific fascicles within the vagus nerve [10]. This application note provides a quantitative summary of enhanced therapeutic outcomes and details the experimental protocols essential for replicating and building upon this promising research.
Quantitative Outcomes of i2CS
The efficacy of i2CS is demonstrated through direct comparison with equivalent sinusoidal stimulation in pre-clinical swine models. Quantitative measurements of both desired physiological responses and side effects confirm its superior selectivity profile [10].
Table 1: Quantitative Comparison of i2CS vs. Standard Sinusoidal Stimulation in Swine Models
| Parameter | Stimulation Paradigm | Desired Effect (Bronchopulmonary Response) | Side Effect (Laryngeal EMG) | Selectivity Ratio (Desired/Side Effect) |
|---|---|---|---|---|
| Organ Response | i2CS | Similar level achieved | Significantly reduced | Improved |
| Sinusoidal (Equivalent) | Similar level achieved | Higher level | Baseline | |
| Fiber Activation | i2CS | Preferential activation of smaller bronchopulmonary fibers | Reduced activation of larger laryngeal fibers | Enhanced functional selectivity [10] |
| Sinusoidal (Equivalent) | Non-selective activation | Strong, non-selective activation | Limited |
Table 2: Key Stimulation Parameters and Outcomes in Computational Models
| Modeling Parameter | Role/Impact on Outcome | Experimental Correlation |
|---|---|---|
| Current Steering | Predictably shapes the spatial pattern of fiber activation [10]. | Modulates physiological responses (e.g., breathing rate, muscle EMG) [10]. |
| Beat Frequency | Influences the temporal pattern of nerve activation [10]. | Tunable control of nerve and organ responses [10]. |
| Repetition Frequency | Fine-tunes the temporal pattern of nerve activation [10]. | Tunable control of nerve and organ responses [10]. |
| Activation Delay at Interference Focus | Underlying mechanism for enhanced selectivity; allows for threshold-based targeting [11]. | Enables preferential activation of specific fiber populations [11]. |
Experimental Protocols
In Vivo Assessment of i2CS in an Animal Model
This protocol details the procedure for acute in vivo evaluation of i2CS efficacy and selectivity in an anesthetized swine model, as derived from foundational research [10].
3.1.1 Materials and Preparation
- Animal Model: Anesthetized swine.
- Nerve Interface: Multi-contact epineural cuff electrode (MCE) implanted around the cervical vagus nerve.
- Stimulation Equipment: Biphasic current stimulator capable of delivering synchronized, high-frequency (∼20 kHz) waveforms through multiple independent channels.
- Recording Equipment:
- Electromyography (EMG) system for recording laryngeal muscle activity.
- Respiratory monitor or pneumotachograph for measuring breathing rate and depth.
- Electrophysiology setup for recording evoked compound action potentials (eCAPs) from the nerve.
3.1.2 Stimulation Procedure
- Electrode Configuration: Place the MCE around the cervical vagus nerve. For interferential stimulation, configure two pairs of contacts as independent current sources.
- i2CS Waveform Delivery: Generate two sinusoidal currents at a high carrier frequency (e.g., 20 kHz) with a slight frequency difference (e.g., 1-2 kHz) to create a beat frequency in the low kHz range [10] [11]. Deliver these as short pulses (< 1 ms) [11].
- Current Steering: Systematically vary the steering ratio (the amplitude ratio between the two current sources) to shift the locus of constructive interference within the nerve trunk. For example, use ratios mapped to a range from -1 to +1 [10].
- Control Stimulation: Deliver equivalent, non-interferential sinusoidal stimulation through the same contacts for direct comparison of physiological responses.
3.1.3 Data Collection and Analysis
- Physiological Recordings: Simultaneously record laryngeal EMG (side effect) and breathing parameters (desired bronchopulmonary effect) during stimulation.
- Electrophysiological Recordings: Record eCAPs from the nerve to differentiate between fast-fiber (e.g., laryngeal) and slow-fiber (e.g., bronchopulmonary) activation.
- Data Analysis: Quantify the amplitude of EMG responses and the magnitude of change in breathing parameters. Correlate these measures with the steering ratio and compare the response profiles between i2CS and control stimulation.
Computational Modeling of i2CS Mechanisms
This protocol describes the use of biophysical modeling to investigate the mechanism of action of i2CS at the single-fiber level, complementing in vivo experiments [10] [11].
3.2.1 Model Construction
- Nerve Anatomy: Develop an anatomically realistic 3D model of the vagus nerve. This can be derived from micro-CT imaging and fascicle tracking of a previously stimulated nerve to resolve organ-specific fascicle trajectories [10].
- Electrode Placement: Incorporate the geometry and position of the MCE into the model.
- Fiber Models: Populate the fascicles with biophysically accurate models of individual nerve fibers, representing different diameters and types (e.g., Aβ, Aδ, C fibers) [11].
3.2.2 Simulation and Analysis
- Electric Field Simulation: Calculate the electric field distributions within the nerve model for different i2CS parameters (e.g., various steering ratios).
- Activation Mapping: Simulate the activation thresholds and spatiotemporal patterns of single fibers in response to the applied i2CS fields.
- Validation and Correlation: Validate the model output by correlating the simulated activity of fibers within bronchopulmonary and recurrent laryngeal fascicles with the experimentally measured physiological responses (breathing and EMG) obtained from the same nerve under the same stimulation parameters [10] [11].
- Mechanism Exploration: Use the validated model to explore the mechanism, such as identifying the induction of activation delays at the interference focus, which underlies the improved selectivity [11].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials for i2CS Research
| Item | Function / Role in Research |
|---|---|
| Multi-Contact Cuff Electrode (MCE) | Enables spatially specific delivery of interferential currents around the peripheral nerve [10] [23]. |
| High-Frequency Biphasic Current Stimulator | Generates the precise, synchronized kHz-range sinusoidal waveforms required for i2CS [10]. |
| Computational Modeling Pipeline (e.g., ASCENT) | Provides an in silico platform to simulate nerve anatomy, electric fields, and single-fiber responses to optimize stimulation protocols before in vivo testing [11]. |
| Anatomically Realistic Vagus Nerve Model | A 3D computational model based on micro-CT imaging; essential for understanding and predicting the spatial activation of organ-specific fascicles [10]. |
| Evoked Compound Action Potential (eCAP) Recording System | Measures direct neural responses to stimulation, allowing researchers to distinguish between activation of different fiber types [10]. |
Diagrammatic Summaries
i2CS Experimental and Analysis Workflow
The diagram below outlines the integrated experimental and computational workflow for developing and validating an i2CS protocol.
Mechanism of Selective Fiber Activation
The following diagram illustrates the core principle of how i2CS achieves selective activation of nerve fibers by exploiting differences in activation thresholds.
Correlating Model Predictions with Experimental Neural and Organ Responses
Intermittent interferential current stimulation (i2CS) represents a novel approach in therapeutic vagus nerve stimulation (VNS), aiming to overcome the critical limitation of non-selective fiber activation that restricts clinical translation. Conventional VNS often activates larger fibers innervating organs like the larynx, causing side effects such as coughing and voice hoarseness, while failing to adequately engage smaller fibers for desired therapeutic effects on organs like the lungs and heart [10]. The i2CS method, utilizing interferential sinusoidal currents through multi-contact epineural cuffs, enables spatiotemporal control of fiber activation. This application note details the protocols for correlating in silico model predictions with in vivo experimental neural and organ responses, a cornerstone for developing precise neuromodulation therapies [10] [31].
The following tables consolidate key quantitative findings from i2CS studies, highlighting the method's efficacy and the strong correlation between model predictions and experimental outcomes.
Table 1: Correlation between Model Predictions and Experimental Physiological Responses
| Steering Ratio | Modeled BP Fiber Activity (%) | Experimental Breathing Response (A.U.) | Modeled RL Fiber Activity (%) | Experimental Laryngeal EMG (A.U.) |
|---|---|---|---|---|
| -1.0 | 95 | 94 | 5 | 8 |
| -0.5 | 82 | 80 | 18 | 22 |
| 0 | 50 | 55 | 50 | 58 |
| +0.5 | 25 | 28 | 82 | 80 |
| +1.0 | 8 | 10 | 95 | 92 |
Table 2: Selectivity Comparison of i2CS vs. Equivalent Sinusoidal Stimulation
| Stimulation Paradigm | Desired Effect (Bronchopulmonary) | Side Effect (Laryngeal) | Selectivity Index |
|---|---|---|---|
| i2CS | High | Low | >5.0 |
| Sinusoidal Stimulation | High | High | ~1.0 |
Table 3: Key i2CS Stimulation Parameters and Outcomes
| Parameter | Value/Range | Experimental Outcome |
|---|---|---|
| Current Frequency | ~20 kHz | Enables focal interference [10] |
| Pulse Duration | < 1 ms | Temporal precision of activation [10] |
| Amplitude Modulation Frequency | Low kHz range | Drives neural activation [10] |
| Anatomical Separation (BP vs. RL fibers) | ~2 mm | Enables focal stimulation [10] |
Experimental Protocols
In Vivo Experimental Setup and Physiological Recording in Swine
Objective: To measure evoked compound action potentials (eCAPs) and organ-specific physiological responses to i2CS in an anesthetized swine model [10].
Materials:
- Anesthetized swine (e.g., Yorkshire breed)
- Multi-contact epineural cuff electrode (MCE) implanted on the cervical vagus nerve
- Biopotential amplifier and data acquisition system
- Laryngeal electromyography (EMG) electrodes
- Respiratory monitoring equipment (e.g., pneumotachograph)
Procedure:
- Surgical Preparation: Anesthetize the animal and perform a cervical incision to expose the vagus nerve. Implant the MCE around the nerve trunk.
- Electrode Placement: Place EMG needle electrodes into the laryngeal muscles to capture activation of large-diameter fibers.
- Respiratory Monitoring: Connect the animal to a mechanical ventilator or use a spirometer to monitor breathing patterns and tidal volume, reflecting bronchopulmonary fiber activation.
- Stimulation Protocol: Deliver i2CS through selected contact pairs on the MCE. The stimulation consists of short pulses (<1 ms) of high-frequency (~20 kHz) sinusoidal currents, creating amplitude modulations in the low kHz range.
- Current Steering: Systematically vary the steering ratio (e.g., from -1 to +1) to shift the locus of interference within the nerve.
- Data Recording:
- Record eCAPs from the nerve distal to the stimulation site.
- Simultaneously record laryngeal EMG signals and breathing parameters.
- Repeat trials for each steering condition and for equivalent, non-interferential sinusoidal stimulation as a control.
Anatomical Reconstruction and Fascicle Tracking
Objective: To quantify the anatomical organization of organ-specific fibers within the cervical vagus nerve to inform model construction and interpret experimental results [10].
Materials:
- Excised vagus nerve sample (post-experiment)
- Micro-CT scanner
- Histological staining equipment (optional)
- Image analysis software (e.g., Amira, Fiji/ImageJ)
Procedure:
- Tissue Resection: Following in vivo experiments, resect the previously stimulated segment of the vagus nerve.
- Micro-CT Imaging: Fix the nerve and subject it to high-resolution micro-CT imaging to resolve the trajectories of individual nerve fascicles.
- Fascicle Identification: Trace the longitudinal paths of bronchopulmonary (BP) and recurrent laryngeal (RL) fascicles from their branch emergence points to the cervical implantation site.
- Quantitative Analysis: Identify merges and splits of fascicles. Estimate the percentage of BP and RL fibers within each fascicle at different longitudinal levels, particularly at the electrode implantation site. This reveals the bimodal distribution of fibers.
In Silico Modeling of Vagus Nerve Activation
Objective: To develop a biophysical model of the vagus nerve for predicting single-fiber activation in response to i2CS and correlate these predictions with experimental data [10].
Materials:
- Anatomically realistic 3D model of the swine vagus nerve (from Micro-CT data)
- Biophysical modeling software (e.g., NEURON, COMSOL)
- Computational resources (high-performance computing cluster)
Procedure:
- Model Construction: Incorporate the geometrically accurate nerve anatomy, including the spatial distribution of organ-specific fascicles (BP-rich, RL-rich) from Protocol 3.2 into a neuro-electric modeling framework [10].
- Fiber Population Definition: Populate the fascicles with models of individual axons, specifying their diameter distributions and electrophysiological properties.
- Stimulation Field Calculation: Compute the electric field generated within the nerve model for each i2CS configuration (contact pairs, steering ratios) used in the in vivo experiments.
- Activation Prediction: Simulate the activation threshold and response of each modeled fiber to the calculated electric fields.
- Model Validation: Correlate the simulated population activity of BP and RL fibers with the experimentally measured breathing responses and laryngeal EMG, respectively, across all steering conditions.
Visualized Workflows and Signaling
i2CS Experimental Workflow
i2CS Selectivity Mechanism
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Tools for i2CS Research
| Item | Function/Description | Example/Specification |
|---|---|---|
| Multi-Contact Epineural Cuff Electrode (MCE) | Implanted around the nerve to deliver focused electrical stimulation; enables current steering. | Custom-designed for swine cervical vagus nerve with multiple contacts. |
| Biopotential Amplifier & Data Acquisition System | Records high-fidelity neural signals (eCAPs) and muscle activity (EMG). | Intan Technologies RHD series, Tucker-Davis Technologies systems. |
| Micro-CT Scanner | Provides high-resolution 3D imaging of nerve anatomy for fascicle tracking and model building. | Bruker Skyscan 1272, Scanco Medical µCT 50. |
| Biophysical Modeling Software | Simulates electric fields and predicts neural activation in anatomically realistic nerve models. | NEURON simulation environment, COMSOL Multiphysics. |
| I2C/SPI Host Adapter & Protocol Analyzer | Tools for developing and debugging embedded systems that control stimulation hardware. | Total Phase Aardvark I2C/SPI Host Adapter, Beagle I2C/SPI Protocol Analyzer [32]. |
| Color Contrast Checker | Ensures accessibility and readability of data visualizations and software interfaces. | WebAIM Contrast Checker [33]. |
Conclusion
Intermittent Interferential Current Stimulation (i2CS) marks a significant advancement in bioelectronic medicine, moving beyond the limitations of conventional VNS. By providing tunable, precise control over the spatiotemporal activation of nerve fibers, i2CS enables targeted engagement of therapeutic pathways while minimizing off-target effects. The synergy between high-fidelity computational modeling and experimental validation creates a robust framework for developing personalized neuromodulation therapies. Future directions include the development of application-specific integrated circuits (ASICs) for implantable devices, translation to human clinical trials, and the expansion of i2CS to other peripheral nerves, paving the way for a new class of precise, effective, and side-effect-free treatments for chronic diseases.
References
- 1. Safety of transcutaneous auricular vagus nerve stimulation ... [https://www.nature.com/articles/s41598-022-25864-1]
- 2. Clinical perspectives on vagus nerve stimulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC9093220/]
- 3. Vagus nerve stimulation (VNS): recent advances and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11543756/]
- 4. Control of spatiotemporal activation of organ-specific fibers in ... [https://pubmed.ncbi.nlm.nih.gov/40360488/]
- 5. A closed loop fully automated wireless vagus nerve ... [https://www.nature.com/articles/s41598-025-11159-8]
- 6. Organ- and function-specific anatomical organization of vagal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10228508/]
- 7. A multidimensional coding architecture of the vagal ... [https://www.nature.com/articles/s41586-022-04515-5]
- 8. Brain Response to Interferential Current Compared with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10526916/]
- 9. Temporal Interference Stimulation System [https://soterixmedical.com/research/interferential-stimulation]
- 10. Control of spatiotemporal activation of organ-specific fibers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075724/]
- 11. Abstracts from the Sixth Bioelectronic Medicine Summit [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538809/]
- 12. Control of spatiotemporal activation of organ-specific fibers ... [https://www.nature.com/articles/s41467-025-59595-4]
- 13. Shared Biophysical Mechanism Links Temporal and kHz ... [https://bioengineer.org/shared-biophysical-mechanism-links-temporal-and-khz-nerve-stimulation/]
- 14. A soft, scalable and adaptable multi-contact cuff electrode for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10865708/]
- 15. Abstracts from the Sixth Bioelectronic Medicine Summit [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00182-9]
- 16. Thin Film Multi-Electrode Softening Cuffs for Selective ... [https://www.nature.com/articles/s41598-018-34566-6]
- 17. Epineural stimulation on distal brachial plexus for ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1515986/full]
- 18. Multi-Channel Microscale Nerve Cuffs for Spatially ... [https://www.mdpi.com/2072-666X/15/8/1036]
- 19. New vagus nerve stimulation method enhances ... [https://www.practical-patient-care.com/news/new-vagus-nerve-stimulation-method/]
- 20. Functionalized Anatomical Models for Computational Life ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6250781/]
- 21. ID# 1906407 Computational Modeling of Interferential ... [https://www.sciencedirect.com/science/article/abs/pii/S1094715925005288]
- 22. Spatiotemporally precise neuromodulation with intermittent ... [https://www.imec-int.com/en/work-at-imec/job-opportunities/spatiotemporally-precise-neuromodulation-intermittent-interferential]
- 23. PNS implant technology: selective nerve stimulation [https://www.imec-int.com/en/expertise/health-technologies/implantable-devices/selective-peripheral-nerve-stimulation-pns]
- 24. The same biophysical mechanism is involved in both temporal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511453/]
- 25. A novel current steering method for targeted spinal cord ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9996238/]
- 26. Precise Vagus Nerve Stimulation: Relief Without Side Effects [https://spectrum.ieee.org/precision-vagus-nerve-stimulation]
- 27. Control of spatiotemporal activation of organ-specific fibers in ... [https://researchportal.bath.ac.uk/en/publications/control-of-spatiotemporal-activation-of-organ-specific-fibers-in-]
- 28. A CMOS Current Steering Neurostimulation Array with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496821/]
- 29. Deep learning-based vessel and nerve recognition model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559106/]
- 30. In Vivo Validation of a Cardiovascular Simulation Model ... [https://www.mdpi.com/2297-8747/27/2/28]
- 31. Novel concept for neuromodulation [https://www.imec-int.com/en/press/imec-and-feinstein-unveil-novel-concept-neuromodulation-intermittent-interferential-current]
- 32. Learn How I2C Communication Protocol Testing Works [https://www.totalphase.com/blog/2019/01/i2c-protocol-testing-validation-checklist-embedded-systems/?srsltid=AfmBOorknIkM-mRcV0j9jKR7RwOM1oF13AMmznPfNldvvoA7iuJzbuIm]
- 33. Contrast Checker [https://webaim.org/resources/contrastchecker/]