Bioelectronic Medicine vs. Pharmaceutical Outcomes: A Comparative Analysis for the Future of Therapeutics
This article provides a comprehensive comparison for researchers and drug development professionals on the evolving paradigms of bioelectronic medicine and traditional pharmaceuticals.
Bioelectronic Medicine vs. Pharmaceutical Outcomes: A Comparative Analysis for the Future of Therapeutics
Abstract
This article provides a comprehensive comparison for researchers and drug development professionals on the evolving paradigms of bioelectronic medicine and traditional pharmaceuticals. It explores the foundational principles of bioelectronic devices, which use electrical signals to modulate neural circuits, contrasting them with systemic drug actions. The analysis covers current methodologies, key applications in neurology and cardiology, and addresses critical challenges including device reliability, cost, and regulatory hurdles. By evaluating clinical and economic outcomes, this review synthesizes evidence on where bioelectronic therapies offer superior precision, reduced side effects, and long-term value, outlining a future where integrated approaches could redefine disease management.
Principles and Paradigms: Understanding the Core Mechanisms of Bioelectronic and Pharmaceutical Therapies
The pursuit of effective therapies has historically been dominated by pharmaceuticals, which rely on systemic chemical interactions. In contrast, bioelectronic medicine represents a paradigm shift, using targeted energy to modulate neural circuits. This guide provides an objective comparison of these two approaches, focusing on their mechanisms, applications, and experimental validation for researchers and drug development professionals.
Systemic drug action involves the administration of chemical compounds that distribute throughout the body via the bloodstream to interact with biological targets, while targeted neuromodulation uses electrical, magnetic, or other forms of energy to precisely modulate the activity of specific neural circuits or nerves [1]. The fundamental distinction lies in their therapeutic delivery: drugs act chemically and systemically, whereas neuromodulation acts physically and locally. Understanding their comparative profiles is crucial for selecting appropriate therapeutic strategies for specific conditions and advancing biomedical research.
Mechanisms of Action: From Molecular Diffusion to Circuit Precision
Systemic Drug Pharmacology
Systemic drugs produce their effects through pharmacokinetic (what the body does to the drug) and pharmacodynamic (what the drug does to the body) processes. After administration, drugs undergo absorption, distribution, metabolism, and excretion, leading to widespread circulation. Their therapeutic effects emerge from interactions with molecular targets such as receptors, enzymes, and ion channels [2].
For example, the newly approved drug suzetrigine, a non-opioid analgesic, exerts its effect by selectively blocking the NaV1.8 voltage-gated sodium channel in peripheral sensory neurons, inhibiting pain signal generation [3]. Similarly, acoltremon, a treatment for dry eye disease, acts as an agonist of transient receptor potential melastatin 8 (TRPM8) thermoreceptors on corneal sensory nerves, triggering increased basal tear production [3]. These molecular interactions, while specific, occur wherever the drug distributes, potentially leading to off-target effects.
Neuromodulation Mechanisms
Neuromodulation techniques interface with electrically active tissues to restore dysfunctional neural circuitry. These approaches can be broadly categorized into invasive and non-invasive modalities:
- Non-invasive techniques include repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS). rTMS uses alternating magnetic fields to induce electric currents in superficial cortical neurons according to Faraday's law of electromagnetic induction, with stimulation frequency determining the direction of neuroplastic changes [4].
- Invasive techniques such as deep brain stimulation (DBS) involve surgical implantation of electrodes to deliver electrical pulses to deep brain structures [5].
The therapeutic effect arises from modulating neural pathway activity rather than chemical receptor binding. For substance use disorders, both invasive and non-invasive neuromodulation target components of the mesocorticolimbic pathways, including the ventral striatum, nucleus accumbens, and prefrontal cortex [4]. Advanced approaches are evolving toward "closed-loop" systems that monitor physiological signals and adjust stimulation parameters in real-time for personalized therapy [6].
Table 1: Fundamental Mechanisms of Action
| Feature | Systemic Drug Action | Targeted Neuromodulation |
|---|---|---|
| Primary Mechanism | Chemical interaction with molecular targets | Physical energy modulation of neural activity |
| Therapeutic Specificity | Molecular target specificity | Anatomical and circuit specificity |
| Distribution | Systemic via bloodstream | Focal or targeted delivery |
| Reversibility | Dependent on drug half-life | Instantaneously adjustable |
| Metabolism | Hepatic metabolism and renal excretion | No metabolic processing required |
Comparative Performance Data: Quantitative Outcomes Analysis
Efficacy Metrics Across Indications
Substance Use Disorders (SUDs): Neuromodulation shows promising efficacy for challenging conditions like opioid and stimulant use disorders. For methamphetamine use disorder, a large randomized controlled trial of 126 participants found that intermittent theta burst stimulation to the dorsolateral prefrontal cortex (DLPFC) significantly reduced cue-induced craving compared to sham treatment [5]. For cocaine use disorder, systematic reviews indicate that high-frequency (≥5 Hz) rTMS protocols targeting the left DLPFC significantly reduced self-reported cue-induced craving, impulsivity, and, in some cases, cocaine use compared to controls [4].
Pain Management: The newly approved non-opioid analgesic suzetrigine demonstrated significant pain reduction in surgical pain trials. In abdominoplasty and bunionectomy patients, suzetrigine (100 mg initially, then 50 mg every 12 hours) showed significantly greater pain reduction (SPID48 values of 118.4 and 99.9, respectively) compared to placebo (70.1 and 70.6) [3]. This performance was similar to hydrocodone/acetaminophen in one trial but slightly lower in another, offering a non-addictive alternative with a different safety profile.
Neurological Disorders: Deep brain stimulation has established efficacy for movement disorders, with long-term outcomes (15 years) showing sustained benefits for Parkinson's disease patients [7]. Spinal cord stimulation, representing a market value of $2.92 billion in 2023, demonstrates the economic and therapeutic significance of neuromodulation for chronic pain [1].
Table 2: Quantitative Efficacy Comparison Across Therapeutic Areas
| Condition | Therapeutic Approach | Efficacy Outcomes | Evidence Level |
|---|---|---|---|
| Cocaine Use Disorder | High-frequency rTMS to left DLPFC | Significant reduction in craving and impulsivity | Systematic review of 8 RCTs [4] |
| Methamphetamine Use Disorder | Theta burst stimulation to DLPFC | Significant decline in cue-induced craving | RCT of 126 participants [5] |
| Moderate-to-Severe Acute Pain | Suzetrigine (50-100 mg) | SPID48: 118.4 (abdominoplasty), 99.9 (bunionectomy) | Two controlled trials (N=2,191) [3] |
| Dry Eye Disease | Acoltremon 0.003% solution | >40% patients with >10-mm increase in Schirmer score | Two Phase III trials (N=930) [3] |
| Parkinson's Disease | Deep Brain Stimulation | Significant improvement in tremors, bradykinesia, rigidity | Long-term 15-year outcomes [7] |
Safety and Tolerability Profiles
Systemic drugs frequently exhibit class-specific adverse effects. Suzetrigine demonstrates side effects including itching, rash, muscle spasms, increased creatine phosphokinase, and decreased estimated glomerular filtration rate [3]. Acoltremon primarily causes instillation-site pain (50% of patients), though less than 1% discontinue due to these sensations [3].
Neuromodulation safety profiles differ substantially. Non-invasive approaches like rTMS and tDCS are generally well-tolerated, with no serious adverse events reported in systematic reviews of SUD applications [4]. Invasive DBS carries risks associated with surgical implantation, including infection and hardware complications, but avoids systemic pharmacological side effects [5]. The bioelectronic medicine field is addressing safety through technological advances in soft, flexible bioelectronic devices that minimize mechanical mismatch with biological tissues, reducing inflammation and improving long-term biocompatibility [6].
Experimental Methodologies: Protocols for Validation
Clinical Trial Designs for Neuromodulation
Randomized, sham-controlled, double-blind trials represent the gold standard for evaluating neuromodulation therapies. In rTMS trials for substance use disorders, common methodologies include:
- Stimulation Parameters: High-frequency (≥5 Hz) protocols for increasing cortical excitability versus low-frequency (≤1 Hz) for decreasing excitability [4]
- Target Localization: Neuronavigation systems using individual MRI scans for precise targeting of the dorsolateral prefrontal cortex or other regions [5]
- Sham Conditions: Placebo coils that replicate the sound and superficial sensation without delivering active neural stimulation [4]
- Outcome Measures: Primary endpoints including self-reported craving scales, cognitive function assessments, and biological measures of substance use [4]
For example, recent rTMS studies employ accelerated paradigms compressing full treatment courses into 5 days rather than traditional 4-6 week regimens, improving retention and feasibility [5]. Theta burst stimulation protocols deliver patterned high-frequency stimulation in shorter sessions while maintaining efficacy comparable to conventional rTMS [5].
Drug Development and Validation Protocols
Pharmaceutical validation follows established regulatory pathways with specific adaptations for novel mechanisms:
- Phase III Trial Designs: For suzetrigine, two controlled trials in acute surgical pain models (abdominoplasty and bunionectomy) using the SPID48 (sum of pain intensity differences over 48 hours) primary endpoint with active (hydrocodone/acetaminophen) and placebo comparators [3]
- Biomarker Validation: For targeted therapies, demonstration of target engagement through functional imaging or electrophysiological measures
- Dosing Optimization: Identification of minimal effective doses and maximum tolerated doses through phase II dose-ranging studies
Novel drug classes require specialized validation approaches. For instance, drugs like acoltremon first require establishing proof of concept for novel targets (TRPM8 receptors) before progressing to large efficacy trials [3].
Signaling Pathways and Neural Circuits: Visualization Frameworks
Systemic Drug Signaling Pathways
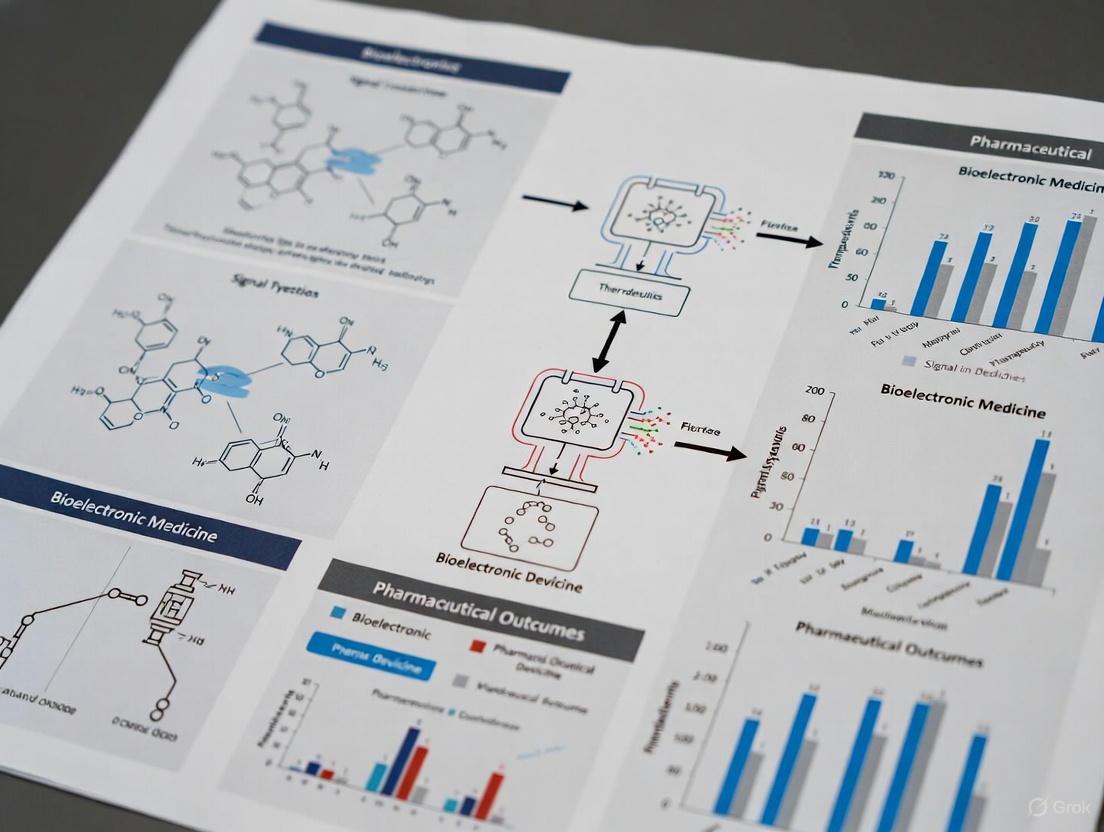
Diagram 1: Systemic Drug Action Pathway
Neuromodulation Neural Circuitry
Diagram 2: Targeted Neuromodulation Circuit
Experimental Platforms and Reagents
Table 3: Research Toolkit for Therapeutic Development
| Tool Category | Specific Technologies | Research Applications | Key Functions |
|---|---|---|---|
| Drug-Target Databases | HCDT 2.0, BindingDB, PharmGKB [8] | Drug discovery, target identification | Curated drug-gene, drug-RNA, drug-pathway interactions |
| Neuromodulation Devices | Deep TMS systems, tDCS devices, DBS implants [4] [5] | Circuit mapping, therapeutic testing | Precise neural stimulation with varying penetration depths |
| Genetic Targeting Tools | Optogenetics, Chemogenetics, Magnetogenetics [9] [7] | Cell-type specific modulation | Selective manipulation of defined neuronal populations |
| Bioelectronic Materials | Conducting polymers, Graphene, Carbon nanotubes [1] | Device development, tissue interface | Improved biocompatibility and signal transduction |
| Computational Modeling | QSP models, Machine learning, PBPK modeling [2] | Predictive therapeutic optimization | Simulation of drug effects and neuromodulation parameters |
The comparison between systemic drug action and targeted neuromodulation reveals complementary rather than competing therapeutic profiles. Pharmaceuticals offer molecular precision with systemic distribution, while neuromodulation provides anatomical precision with localized effects. The emerging field of bioelectronic medicine represents a convergence of these approaches, leveraging advances in materials science, microelectronics, and neural circuit understanding to develop increasingly sophisticated therapeutic platforms [6] [1].
Future therapeutic development will likely integrate both modalities, with pharmaceuticals potentially enhancing or being enhanced by targeted neuromodulation approaches. For researchers and drug development professionals, understanding the comparative strengths, limitations, and methodological requirements of each approach is essential for designing optimal treatment strategies for specific conditions and patient populations. The growing market for bioelectronic medicine, projected to reach $33.59 billion by 2030, reflects the increasing importance of these technologies in the therapeutic landscape [10].
Electroceuticals, or bioelectronic medicine, represent a transformative class of therapies that use electrical signals to modulate the body's electrically active tissues—such as nerves, the heart, and the brain—to treat disease [11] [1]. This approach stands in contrast to traditional pharmaceuticals, which rely on systemic chemical interactions. The core premise is that by precisely interfacing with the nervous system, which innervates every organ in the human body, bioelectronic devices can selectively modulate organ function, offering targeted treatment with the potential for reduced side effects compared to drug administration [1]. The global market for these therapies is expanding rapidly, valued at USD 23.54 billion in 2024 and projected to reach USD 33.59 billion by 2030, reflecting a compound annual growth rate (CAGR) of 6.10% [10]. This growth is driven by the rising prevalence of chronic diseases, an aging population, and continuous technological innovations [10] [12].
This guide objectively traces the evolution of electroceuticals from ancient anecdotes to modern implantable devices, framing this progression within the broader research context comparing bioelectronic and pharmaceutical outcomes. It is structured to provide researchers, scientists, and drug development professionals with a clear comparison of device performance across historical periods, detailed experimental methodologies, and essential research tools.
Historical Timeline and Technological Progression
The development of electroceuticals has progressed from foundational discoveries of bioelectricity to sophisticated, intelligent implants. The timeline below visualizes this journey through key milestones.
Figure 1: Evolution of electroceuticals from ancient times to the modern era, highlighting key technological transitions.
Ancient Origins and Foundational Discoveries
The earliest records of bioelectronic medicine date back to ancient civilizations, including Egypt and Greece, where electric fish were used to deliver therapeutic shocks for ailments like headaches, migraines, and gout [1] [13]. This constituted the first documented instance of non-invasive neuromodulation. The field's scientific foundation was laid in the late 18th century by Luigi Galvani, whose experiments demonstrated that electrical stimulation could cause muscle contraction in frog legs, introducing the concept of "bioelectricity" [6] [1] [13]. Alessandro Volta's subsequent development of the battery further enabled the therapeutic application of electricity for conditions such as paralysis and pain relief [13].
The Dawn of Modern Implants
The mid-20th century marked the transition from concept to clinical device. The first fully implantable pacemaker was developed in 1958 by Åke Senning and Rune Elmqvist, providing a reliable, long-term solution for cardiac arrhythmias and representing a pivotal moment for fully implantable bioelectronic systems [1] [13]. This was followed by the first cochlear implant for profound deafness in 1961 [1]. These early devices were open-loop systems, meaning they delivered fixed stimulation patterns without responding to the body's changing physiological needs [13].
The Rise of Neuromodulation
From the 1980s to the 2000s, the scope of bioelectronic medicine expanded beyond the heart and ears to the central and peripheral nervous systems. Deep Brain Stimulation (DBS) emerged as a reversible and adjustable therapy for movement disorders like Parkinson's disease, receiving FDA approval for essential tremor in 1997 [1] [13]. Vagus Nerve Stimulation (VNS) was developed for treatment-resistant epilepsy and depression, later showing promise for modulating immune responses and inflammation in conditions like rheumatoid arthritis [11] [13]. This period also saw the advent of rate-responsive pacemakers, which could adapt to a patient's activity level, representing an early step toward closed-loop systems [13].
The Modern Era of Intelligent Bioelectronics
The 21st century has ushered in the current generation of "intelligent" electroceuticals, characterized by four key trends:
- Closed-Loop Systems: Devices like the Medtronic Percept DBS system and closed-loop spinal cord stimulators can sense physiological signals and adjust stimulation parameters in real time, moving from continuous to on-demand, responsive therapy [12] [13].
- Miniaturization and Wireless Power: Devices are becoming smaller, with some pacemakers now smaller than a grain of rice. The shift toward battery-free implants, powered by wireless energy transfer methods like inductive coupling and ultrasound, eliminates the need for replacement surgery and improves device longevity [14] [1].
- Soft and Flexible Bioelectronics: Researchers are shifting from rigid materials to soft, conformable devices using stretchable electronics and hydrogels. This reduces the mechanical mismatch with biological tissues, minimizing inflammation and improving long-term signal stability [6].
- Integration with AI and Digital Health: Artificial intelligence is being leveraged to analyze patient data for personalized treatment protocols, while wearable companions and cloud connectivity enable remote monitoring and therapy adjustment [15] [10].
Comparative Performance Analysis of Electroceuticals
The evolution of device technology has directly translated into improved clinical performance and patient outcomes. The table below provides a structured comparison of key electroceutical devices across different stages of development.
Table 1: Performance and Outcome Comparison of Representative Electroceutical Devices
| Device / Therapy | Era of Adoption | Key Technological Parameters | Reported Efficacy Outcomes | Advantages over Pharmacological Counterparts |
|---|---|---|---|---|
| Cardiac Pacemaker [11] [13] | 1958 (First Implant) | Fixed-rate pacing; Early devices were open-loop. | Restored heart rhythm in patients with complete heart block. | Provided a life-saving intervention where drugs were often ineffective for complete heart block. |
| Rate-Responsive Pacemaker [13] | 1980s | Integrated sensors for activity; Early closed-loop feedback. | Improved quality of life and survival by adapting to patient activity. | More physiological response compared to fixed-rate pacing; superior to chronotropic drugs. |
| Deep Brain Stimulation (DBS) for Parkinson's [1] [12] [13] | 1990s-2000s (Clinical Adoption) | Adjustable frequency, amplitude, pulse width; Initially open-loop. | Significant reduction in tremor and rigidity in majority of patients. | Reversible and adjustable alternative to ablative surgery; reduced motor symptoms where drugs lost efficacy. |
| Closed-Loop DBS (Medtronic Percept) [12] [13] | 2020 (FDA Approval) | Sensing and stimulation with BrainSense technology; adaptive stimulation. | Real-time adjustment based on neural signals for improved symptom control. | Personalized therapy; potential for managing non-motor symptoms; more efficient energy use. |
| Vagus Nerve Stimulation (VNS) for Epilepsy [11] [12] | 1990s-2000s | Implantable pulse generator with programmable output. | Meaningful seizure reduction in a significant portion of drug-resistant patients. | Effective for drug-resistant epilepsy; non-pharmacological mechanism of action. |
| VNS for Depression [12] | 2000s | Similar to epilepsy devices, with different stimulation parameters. | 71% of treatment-resistant patients achieved meaningful symptom relief. | Durable option for treatment-resistant depression (TRD), where multiple drug classes fail. |
| Closed-Loop Spinal Cord Stimulation (SCS) for Pain [12] | 2022-2024 (FDA Approvals) | Real-time adjustment based on physiological feedback. | 93% pain-reduction success in chronic pain cases. | Superior pain control and reduced opioid reliance compared to conventional SCS and systemic opioids. |
Experimental Protocols in Modern Electroceutical Development
The advancement of modern electroceuticals relies on rigorous experimental methodologies. Below are detailed protocols for two key areas: evaluating wireless power transfer and assessing efficacy in chronic wound healing.
Protocol: Evaluating Wireless Power Transfer for Implantable Devices
Objective: To systematically investigate and optimize radiation efficiency and in-body path loss for robust wireless links in implantable systems [16].
Materials:
- Transmitting Coil/System: External power transmitter (e.g., RF signal generator, ultrasonic transducer).
- Implantable Receiver: Miniaturized receiving coil or antenna integrated into the device.
- Tissue Simulant: A medium that mimics the dielectric properties of human tissue (e.g., saline solution, specialized phantom gel).
- Network Analyzer: To measure S-parameters and calculate power transfer efficiency.
- Thermocouples: To monitor localized temperature changes and ensure safety limits are not exceeded.
Methodology:
- System Setup: The implantable receiver is embedded within the tissue simulant at a predetermined depth and orientation. The external transmitter is positioned at a specified distance from the simulant surface.
- Frequency Sweep: The operating frequency of the external transmitter is swept across a defined range (e.g., kHz to GHz for RF, MHz for ultrasound) while the network analyzer records the power received by the implant.
- Efficiency Calculation: The radiation efficiency is calculated as the ratio of the power received by the implant to the power input to the transmitter, accounting for losses in the intervening medium [16].
- Parameter Optimization: The process is repeated while varying key parameters, including:
- Source Type: Comparing inductive coupling, ultrasonic, and magneto-electric transfer [14] [1].
- Encapsulation Size and Material: Evaluating the impact of the device's hermetic package on efficiency [16].
- Alignment: Assessing the effect of angular and lateral misalignment between transmitter and receiver [14].
- Validation: The optimized configuration is validated in ex vivo or in vivo models to confirm performance in a biological environment. The goal is to achieve a 5- to 10-fold improvement in radiation efficiency or gain [16].
Protocol: Assessing Electrostimulation Efficacy in Chronic Wound Healing
Objective: To determine the effect of controlled micro-electrostimulation on reactivating endogenous bioelectric activities and cellular processes critical for healing chronic wounds [17].
Materials:
- Electroceutical Device: A wearable, wireless stimulator (e.g., a triboelectric nanogenerator (TENG) or an inductively powered patch) [14] [17].
- Animal Model: Diabetic (e.g., db/db) mice or other validated models of impaired wound healing.
- Electrodes: Biocompatible, flexible electrodes placed in the wound periphery.
- Histology Equipment: For tissue fixation, sectioning, and staining (H&E, Masson's Trichrome).
- Immunofluorescence Microscopy: For visualizing specific cell types and proteins.
Methodology:
- Wound Creation: A full-thickness cutaneous wound is created on the dorsum of anesthetized animals.
- Group Allocation: Animals are randomly assigned to:
- Treatment Group: Receives active electrical stimulation via the implanted device.
- Control Group: Wears an identical but inactive device (sham stimulation).
- Stimulation Parameters: The treatment group receives stimulation using predefined parameters, typically Pulsed Current (e.g., 1.2–1.5 mA), which is better suited for wound healing due to lower side effects compared to direct current [17]. Common settings include low-frequency pulses (e.g., 50-100 Hz) for a set duration daily.
- Outcome Measures:
- Primary: Wound closure rate, measured by tracing the wound area daily until complete healing.
- Secondary: Histological analysis of granulation tissue thickness, collagen deposition, and re-epithelialization. Immunofluorescence is used to quantify key cells (e.g., macrophage transition from M1 to M2 phenotype) and markers of angiogenesis (e.g., CD31) [17].
- Data Analysis: Wound healing times and histological scores are compared between groups using statistical tests (e.g., t-test, ANOVA). A successful outcome is a statistically significant acceleration of wound healing in the treatment group, coupled with evidence of enhanced cellular proliferation and migration.
Research Toolkit: Essential Materials and Reagents
The following table details key materials and technologies that are foundational to current research and development in the field of bioelectronic medicine.
Table 2: Essential Research Toolkit for Advanced Bioelectronic Device Development
| Item / Technology | Category | Primary Function in R&D |
|---|---|---|
| Conducting Polymers (e.g., PEDOT:PSS) [1] | Electrode Material | Seamlessly bridge biotic/abiotic interface; reduce impedance for safer device miniaturization; mixed ionic/electronic conductivity improves signal fidelity. |
| Soft & Stretchable Materials (e.g., Hydrogels, Elastomers) [6] [14] | Substrate/Encapsulation | Minimize mechanical mismatch with tissue; reduce foreign body reaction (FBR) and fibrosis; enable conformable, long-lasting implants. |
| Triboelectric Nanogenerators (TENGs) [14] [17] | Power Supply | Harvest mechanical energy (e.g., body movement, ultrasound) to generate electrical stimulation; enable self-powered, battery-free devices. |
| Inductive Coupling Systems [11] [14] | Power Transfer | Wirelessly transfer power over short ranges via magnetic fields; standard method for powering and triggering implanted electronic circuits. |
| Closed-Loop Feedback Controller [1] [13] | System Electronics | Processes real-time recorded biosignals to automatically adjust stimulation parameters; core component for adaptive, personalized therapy. |
| Bioresorbable Materials [14] | Device Framework | Create temporary implants that safely dissolve in the body after a therapeutic period; eliminate need for surgical extraction. |
| Autonomic Neurography [13] | Sensing/Monitoring | Precisely detects and titrates inflammatory immune responses via the autonomic nervous system; enables biomarker-driven neuromodulation. |
The historical evolution of electroceuticals demonstrates a clear trajectory from gross electrical application to precise, intelligent neuromodulation. When framed within the context of pharmaceutical outcomes research, the distinct value proposition of bioelectronic medicine lies in its target specificity, adaptability, and potential for reduced systemic side effects [1].
For researchers and drug development professionals, the future landscape presents several strategic imperatives. First, the convergence of miniaturized hardware, closed-loop sensing, and on-board artificial intelligence is creating devices that can fine-tune therapy dozens of times per second, opening the door to precision treatment for complex neurological and cardiovascular disorders [12]. Competitive differentiation will increasingly depend on algorithmic intelligence and reliable power management rather than production scale alone.
Second, the field is expanding beyond traditional neurological and cardiac indications into oncology, metabolic disorders, and autoimmune diseases [12]. For instance, Tumor Treating Fields have shown promise in disrupting cancer cell division, while targeted vagal modulation is being explored for inflammatory bowel disease [12]. This diversification offers new avenues for intervention where pharmaceuticals may have limitations.
Finally, the regulatory and reimbursement landscape is evolving. Regulatory agencies are streamlining breakthrough-device pathways, accelerating time-to-market for novel platforms [12]. Simultaneously, payers are shifting toward value-based contracts, favoring therapies that can document real-world outcome improvements and lower lifetime treatment costs compared to chronic drug regimens [12]. For the research community, this underscores the importance of generating robust clinical and health-economic data to support the adoption of next-generation electroceuticals as a pillar of 21st-century healthcare.
In the intricate landscape of disease pathways, two fundamental signaling modalities govern physiological processes and therapeutic interventions: chemical interactions and electrical signaling. Chemical transmission relies on molecular ligands—from small molecules to biologics—binding to cellular receptors to modulate biochemical pathways, forming the basis of most pharmaceutical interventions [18]. In contrast, electrical signaling operates through the movement of ions and changes in membrane potentials, enabling rapid communication within and between electrically excitable cells [19] [20]. The emerging field of bioelectronic medicine represents a paradigm shift, leveraging electrical signaling to modulate neural circuits that control organ function and disease processes, potentially offering alternatives to traditional pharmacotherapeutics [21] [22].
Understanding the distinct mechanisms, temporal profiles, and functional consequences of these communication modes provides critical insights for developing targeted therapeutic strategies. This comparison guide examines the fundamental principles, experimental approaches, and therapeutic applications of chemical and electrical signaling mechanisms in disease contexts, providing researchers with a framework for selecting and optimizing intervention strategies.
Fundamental Mechanisms and Biological Roles
Chemical Transmission Mechanisms
Chemical signaling operates through several distinct modalities with different spatial and temporal characteristics. Synaptic chemical transmission occurs at specialized junctions where neurotransmitters are released from presynaptic terminals into the synaptic cleft (typically 35-50 nm wide) and bind to receptors on the postsynaptic membrane [18]. This wiring transmission provides point-to-point communication with high privacy and safety, operating with a transmission delay in the millisecond range [18]. The concentration of chemical neurotransmitters in the synapse is typically high (micromolar range), with receptor affinities for endogenous neurotransmitters usually ranging from high nanomolar to micromolar [18].
Volume transmission represents a more diffuse chemical signaling mode where neurotransmitters and modulators diffuse through the extracellular fluid to reach remote target cells [19] [18]. This paracrine signaling operates over longer distances (seconds to minutes) and is characterized by transmitter-receptor mismatches at the anatomical level [18]. The extracellular space serves as the substrate for volume transmission, with specialized pathways along myelinated fiber bundles and blood vessels facilitating diffusion and flow [18].
Table 1: Characteristics of Chemical Signaling Modalities
| Feature | Synaptic Transmission | Volume Transmission |
|---|---|---|
| Velocity | Fast (milliseconds) | Slow (seconds to minutes) |
| Spatial Scale | Localized (synaptic cleft) | Diffuse (extracellular space) |
| Concentration | High (μM range) | Low (nM range) |
| Receptor Affinity | Low (high nM to μM) | High (low nM) |
| Divergence | Low | High |
| Safety | High | Low |
At the molecular level, chemical transmission involves complex cascades. Neurotransmitters bind to either ionotropic receptors (ligand-gated ion channels) that directly alter membrane potential, or metabotropic receptors (G-protein coupled receptors) that act indirectly through secondary messengers [19]. This allows chemical synapses to transform presynaptic signals through amplification and adaptation to diverse functional requirements [19].
Electrical Signaling Mechanisms
Electrical transmission occurs through two primary mechanisms. Electrical synapses are mediated by gap junctions—clusters of intercellular channels that directly connect the cytoplasm of adjacent cells [19] [23]. These gap junctions form low-resistance pathways that allow bidirectional passage of electrical currents and small molecules (up to 1-2 kDa) including ions, cAMP, IP₃, and calcium [19] [20]. Gap junction channels are formed by the docking of two hexameric connexin hemichannels (in vertebrates) or innexins (in invertebrates), with connexin 36 (Cx36) being the primary neuronal connexin in mammals [19].
Ephaptic transmission represents a distinct electrical signaling mode where synaptic currents generate electrical fields that can modulate chemical transmission in nearby neurons without direct physical contact [18]. This field effect coupling enables another layer of neuronal communication independent of both chemical synapses and gap junctions.
Electrical synapses are particularly efficient at detecting coincident subthreshold depolarizations within neuronal groups, promoting synchronous firing [19]. They also enable rapid signal transfer with minimal delay, making them particularly valuable in escape response networks across both invertebrates and vertebrates [19]. Unlike chemical transmission, electrical synapses operate in a bi-directional manner and do not require action potentials for analog signal transfer [19].
Table 2: Properties of Electrical Signaling Modalities
| Property | Electrical Synapses | Ephaptic Coupling |
|---|---|---|
| Structural Basis | Gap junctions | Extracellular electrical fields |
| Transmission Delay | Instantaneous | Instantaneous |
| Directionality | Bidirectional | Field-dependent |
| Signal Fidelity | High (analog) | Context-dependent |
| Molecular Transfer | Small molecules (<1-2 kDa) | None |
| Primary Function | Synchronization, rapid signaling | Modulation of excitability |
Integrated Signaling in Neural Systems
Rather than operating independently, chemical and electrical synapses functionally interact during both development and adult neural function [19]. Many synapses are "mixed," featuring both gap junctions and neurotransmitter release sites [20]. These interactions enable sophisticated computational capabilities that neither modality could achieve alone. For instance, electrical synapses can detect coincident activity necessary for strengthening specific chemical synaptic connections through Hebbian plasticity mechanisms [19].
The turn-over of gap junction channels is surprisingly dynamic, with half-lives estimated at 1-3 hours, allowing functional regulation of electrical coupling strength [19]. This dynamic regulation enables neural circuits to maintain flexibility in their computational properties, balancing the reliability of electrical synapses with the plasticity of chemical transmission.
Experimental Methodologies and Assessment Approaches
Investigating Chemical Signaling Pathways
Advanced techniques for profiling chemical signaling have evolved to capture complexity at single-cell resolution. Multiplexed Activity Profiling (MAP) combines phospho-specific flow cytometry with fluorescent cell barcoding to simultaneously measure multiple hallmark cellular functions in response to chemical perturbations [24]. This high-throughput approach enables deep structure-activity relationship studies (SAR-MAP) by quantifying bioactivity across numerous signaling nodes simultaneously.
A typical MAP experimental workflow involves:
- Cell Preparation and Barcoding: Cells are treated with compounds of interest and labeled with unique fluorescent dye signatures (FCB) [24]
- Fixation and Staining: Cells are fixed, permeabilized, and stained with fluorescent antibodies against phospho-proteins and functional markers [24]
- Flow Cytometry Acquisition: Multiparameter data is collected using modern cytometers capable of detecting 20+ parameters [24]
- Computational Analysis: Bioactivity is quantified using inverse hyperbolic sine fold changes in median fluorescence intensity versus vehicle controls [24]
Key measurable endpoints include:
- Apoptosis (cleaved CAS3)
- DNA damage response (γH2AX)
- Pathway activation (p-STAT3, p-STAT5, p-ERK, p-AKT, p-S6)
- Cell cycle status (p-HH3, Ki67)
- Membrane integrity (Ax700 uptake)
- Morphological parameters (forward/side scatter) [24]
For spatial control of chemical signal delivery, 3D-printed picoliter droplet networks enable patterned release of chemical inducers with ≈50 μm resolution [25]. These networks interface with cell populations through lipid bilayers containing engineered pores (α-hemolysin) that control molecular flux, allowing precise manipulation of gene expression patterns in underlying cells [25].
Assessing Electrical Signaling Function
Electrical signaling assessment requires specialized electrophysiological and imaging approaches. Paired intracellular recordings directly measure electrical synaptic strength by injecting current into one cell while recording voltage changes in coupled neighbors [19]. The coupling coefficient (postsynaptic/pre-synaptic voltage change) quantifies functional connectivity.
Gap junction permeability assays utilize fluorescent tracer molecules of different sizes (Lucifer yellow, neurobiotin) to assess molecular transfer between coupled cells [19]. This approach reveals both the presence and functional permeability of electrical synapses.
Immunohistochemical and ultrastructural techniques localize specific connexins using antibodies and visualize gap junctions at electron microscopic resolution [19] [23]. These morphological approaches provide anatomical correlates for functional electrical coupling.
Advanced approaches combine optogenetic control with electrophysiology to probe electrical synaptic function in complex networks. Transgenic animals expressing fluorescently tagged connexins (e.g., Cx36-GFP) enable visualization of electrical synapse distribution and dynamics in living tissue [19].
Diagram 1: Experimental assessment approaches for electrical and chemical signaling (47 characters)
Comparative Therapeutic Targeting in Disease Pathways
Pharmaceutical Targeting via Chemical Interactions
Small molecule therapeutics exert effects by structurally engaging biomolecular targets. Rocaglates, a class of translation inhibitors, exemplify structure-guided design where specific methoxy substitutions on pyrimidinone rings dictate anti-leukemia activity and cell-type selectivity [24]. Using SAR-MAP approaches, researchers identified that discrete structural features drive distinct bioactivity profiles in leukemia cells versus healthy leukocytes, enabling rational optimization of therapeutic indices [24].
Chemical therapeutics exhibit characteristic exposure-response relationships governed by:
- Target binding affinity (Kd values typically nM-μM)
- Pharmacokinetic parameters (Cmax, Tmax, AUC, half-life)
- Tissue penetration and metabolism
- Mechanism-based toxicity thresholds
The temporal dynamics of chemical interventions range from rapid receptor modulation (minutes) to chronic adaptive responses (days-weeks) involving transcriptional and translational changes [24]. This creates both opportunities for sustained effects and challenges from off-target accumulation.
Bioelectronic Interventions via Electrical Signaling
Bioelectronic medicine devices interface with neural circuits through several mechanism classes. Vagus nerve stimulation (VNS) modulates inflammatory reflexes by targeting specific fiber populations, reducing TNFα production in conditions like rheumatoid arthritis and Crohn's disease [22]. Deep brain stimulation (DBS) delivers targeted electrical currents to basal ganglia circuits, restoring movement control in Parkinson's disease by modulating pathological oscillations [21] [6]. Spinal cord stimulation (SCS) interferes with pain signal transmission, providing analgesia for chronic pain conditions [21] [6].
Modern bioelectronic systems increasingly feature closed-loop control where embedded sensors detect physiological states (e.g., seizure precursors) and trigger responsive stimulation, creating dynamic therapeutic adaptation [21] [6]. Advanced devices incorporate bidirectional communication, multimodal stimulation, and drug delivery capabilities [21].
Table 3: Therapeutic Applications of Electrical and Chemical Modalities
| Disease Area | Chemical/Pharmaceutical Approach | Bioelectronic/Electrical Approach |
|---|---|---|
| Inflammatory Disorders | Anti-TNFα biologics (e.g., Humira), immunosuppressants | Vagus nerve stimulation to modulate inflammatory reflex [22] |
| Movement Disorders | Dopamine precursors (L-DOPA), dopamine agonists | Deep brain stimulation of basal ganglia [21] [6] |
| Chronic Pain | NSAIDs, opioids, gabapentinoids | Spinal cord stimulation [21] [6] |
| Cardiac Arrhythmias | Beta-blockers, calcium channel blockers | Implantable pacemakers, defibrillators [21] |
| Epilepsy | Anticonvulsants (e.g., valproate, levetiracetam) | Responsive neurostimulation, vagus nerve stimulation [21] |
Comparative Therapeutic Profiles
Electrical and chemical therapeutic modalities demonstrate distinct characteristic profiles. Precision and localization: Bioelectronic approaches can theoretically achieve greater spatial precision by targeting specific neural circuits, though current applications are limited to larger nerves [22]. Chemical approaches distribute systemically but can achieve cellular specificity through receptor expression patterns. Temporal control: Electrical stimulation offers millisecond-precision modulation with instantaneous onset/offset, while chemical effects develop over longer timescales with prolonged clearance kinetics [21] [22]. Adaptability: Closed-loop bioelectronics can dynamically adjust therapy based on physiological feedback, while chemical dosing typically follows fixed regimens [21]. Invasiveness: Bioelectronic approaches require surgical implantation with associated risks, while chemical administration is generally less invasive [22]. Reversibility: Electrical effects cease immediately upon stimulation termination, while chemical effects persist until clearance or metabolic inactivation [22].
Diagram 2: Therapeutic intervention mechanisms (34 characters)
Key Reagents and Research Solutions
Table 4: Essential Research Tools for Signaling Studies
| Research Tool | Function/Application | Representative Examples |
|---|---|---|
| Phospho-Specific Flow Cytometry | Multiplexed measurement of signaling pathway activation at single-cell resolution | Antibodies against p-STAT3, p-ERK, p-AKT, p-S6, c-CAS3, γH2AX [24] |
| Fluorescent Cell Barcoding (FCB) | Sample multiplexing for high-throughput signaling studies | Pacific Orange, Alexa Fluor dyes for sample multiplexing before antibody staining [24] |
| 3D-Printed Droplet Networks | Spatially patterned chemical signal delivery with micrometer resolution | Picoliter droplet networks with α-hemolysin pores for controlled inducer release [25] |
| Connexin-Specific Antibodies | Localization and quantification of gap junction proteins | Anti-Cx36 for neuronal electrical synapses, anti-Cx43 for astrocytic gap junctions [19] [23] |
| Tracer Molecules | Assessment of gap junction permeability | Neurobiotin, Lucifer Yellow, fluorescent dextrans of varying sizes [19] |
| Genetically Encoded Voltage Indicators | Optical monitoring of electrical activity | ASAP-family sensors, Archon indicators for all-optical electrophysiology |
| Microelectrode Arrays | Extracellular recording of network activity | Multielectrode arrays for in vitro and in vivo electrophysiology |
Experimental Model Systems
Different model systems offer complementary advantages for studying signaling mechanisms. Primary neuronal cultures enable reductionist investigation of synaptic mechanisms in controlled environments [19]. Acute brain slices maintain native circuitry while allowing precise pharmacological and electrophysiological manipulation [19]. In vivo animal models provide physiological context for assessing therapeutic interventions and network-level effects [22]. Human cell lines and organoids offer translational relevance for human-specific signaling mechanisms and therapeutic screening [24].
The choice of model system involves trade-offs between experimental control, throughput, and physiological relevance. Increasingly, researchers employ multiple complementary models to establish robust, translatable findings across biological scales.
Chemical interactions and electrical signaling represent complementary therapeutic paradigms with distinct mechanistic foundations and application landscapes. Chemical therapeutics leverage molecular recognition for selective target engagement, while bioelectronic approaches interface with endogenous neural circuits to modulate physiological processes. The optimal therapeutic strategy depends on multiple factors including disease pathophysiology, target accessibility, temporal requirements, and risk-benefit considerations.
Future progress will likely involve increased integration of these modalities, such as device-guided drug delivery systems and neuromodulatory small molecules. Advanced materials science enabling softer, more biocompatible interfaces will expand bioelectronic applications [6], while increasingly sophisticated chemical biology approaches will enhance specificity of pharmacological interventions [24]. For researchers and drug development professionals, understanding both chemical and electrical signaling mechanisms provides a more comprehensive toolkit for addressing diverse disease pathways and developing next-generation therapeutics.
The healthcare landscape is witnessing a pivotal transformation, moving from broad-spectrum pharmacological interventions to targeted, device-driven therapies. Bioelectronic medicine (BEM) represents this shift, using implantable or wearable electronic devices to interface with electrically active tissues—such as nerves, the heart, and the brain—to treat a wide array of diseases [21]. This approach modulates neural circuits to influence organ function, offering an alternative to systemic drugs. The convergence of an aging global population, a rising burden of chronic diseases, and rapid technological advancements is propelling the BEM market forward. This guide provides an objective comparison for researchers and drug development professionals, framing BEM within the broader context of therapeutic outcomes research compared to traditional pharmaceuticals.
Quantitative Market Driver Analysis
The expansion of the bioelectronic medicine market is quantitatively linked to three interdependent macro-trends. The data below summarizes key metrics and their direct impact on the BEM sector.
Table 1: Key Market Drivers and Quantitative Impact on Bioelectronic Medicine
| Market Driver | Key Quantitative Data | Direct Impact on BEM Market |
|---|---|---|
| Aging Global Population | • By 2030, 1.4 billion (1 in 6) people will be 60 or older [26].• By 2050, the population 80+ will triple to 426 million [26]. | Creates a larger patient base for age-related chronic conditions (e.g., arrhythmia, Parkinson's) treatable with BEM devices like pacemakers and deep brain stimulators [10] [21]. |
| Rising Chronic Disease Burden | • CVDs: Lead to ~17.9 million deaths annually [10].• Diabetes: Affected 537 million adults in 2021, projected to rise to 643 million by 2030 [10].• Pharmaceutical Consumption: Antidiabetic (+50%) and antidepressant (+40%) use rose sharply from 2013-2023 [27]. | Drives demand for non-pharmacological alternatives due to limitations of conventional drugs, including systemic side effects and variable patient response [21] [6]. |
| Technological Convergence | • AI & Digital Health: Enables real-time data analysis and personalized stimulation parameters [10] [28].• Materials Science: Soft, flexible electronics improve biocompatibility and long-term stability [6]. | Enhances BEM device efficacy, safety, and patient comfort, facilitating the development of closed-loop, adaptive systems [21] [29]. |
Comparative Therapeutic Outcomes: BEM vs. Pharmaceuticals
A core thesis in modern therapeutics research is the comparison between device-based and drug-based interventions. The following analysis contrasts their mechanisms, outcomes, and limitations across several key indications.
Table 2: Bioelectronic Medicine vs. Pharmaceutical Outcomes for Select Indications
| Disease / Indication | Bioelectronic Medicine (BEM) Approach | Reported BEM Outcomes & Challenges | Pharmaceutical Approach | Reported Pharmaceutical Outcomes & Challenges |
|---|---|---|---|---|
| Cardiac Arrhythmia | Implantable Pacemaker / ICD: Provides electrical pulses to regulate heart rhythm [21]. | Efficacy: Established, life-saving gold standard for rhythm control [28].Challenges: Surgical implantation risk, device infection, lead failure [6]. | Antiarrhythmic Drugs (e.g., Amiodarone): Systemically modulate cardiac ion channels. | Efficacy: Effective for rhythm control in many patients [27].Challenges: Systemic side effects (e.g., thyroid, pulmonary toxicity); imperfect specificity [21]. |
| Parkinson's Disease & Essential Tremor | Deep Brain Stimulation (DBS): High-frequency stimulation of specific brain targets (e.g., STN) [21] [29]. | Efficacy: Reduces tremor, rigidity; improves motor function in select patients [29].Challenges: Invasive procedure; requires expert programming; device-related complications [6]. | Levodopa/Carbidopa: Oral precursor to dopamine to replenish depleted levels. | Efficacy: Highly effective for symptom control, especially initially.Challenges: Wearing-off effects, dyskinesias, and on-off fluctuations over time; non-physiological dopamine delivery [21]. |
| Type 2 Diabetes / Obesity | Research-Stage Neuromodulation: Vagus nerve stimulation to modulate metabolism/appetite [21] [28]. | Efficacy: An emerging area; aims for direct gut-brain axis modulation [28].Challenges: Primarily experimental; long-term efficacy and optimal parameters not yet defined. | GLP-1 Receptor Agonists (e.g., Semaglutide): Subcutaneous or oral drugs mimicking incretin hormones. | Efficacy: Powerful reduction in HbA1c and body weight [30].Challenges: High cost, high discontinuation rates (~50-70%) often due to GI side effects; requires chronic administration [30]. |
| Chronic Pain (e.g., Back Pain) | Spinal Cord Stimulation (SCS): Delivers low-voltage electrical stimulation to the spinal cord [21]. | Efficacy: Provides significant pain relief for many patients with failed back surgery syndrome [21].Challenges: Requires surgery, tolerance can develop, and device may require revision [6]. | Opioids (e.g., Oxycodone), NSAIDs: Systemically act on CNS and peripheral pain pathways. | Efficacy: Potent analgesia.Challenges: High risk of addiction, tolerance, and overdose with opioids; GI/renal/cardiovascular risks with chronic NSAID use [21]. |
| Drug-Resistant Depression | Vagus Nerve Stimulation (VNS) / Transcranial Magnetic Stimulation (TMS): Invasive or non-invasive neuromodulation [29]. | Efficacy: VNS and TMS are FDA-approved for treatment-resistant cases, offering a durable response [29].Challenges: VNS is invasive; TMS requires repeated clinic visits; response can be delayed [29]. | SSRIs/SNRIs (e.g., Sertraline, Venlafaxine): Systemically increase monoamine levels in the brain. | Efficacy: First-line treatment, effective for many patients [27].Challenges: 30-40% of patients do not respond; side effects (e.g., sexual dysfunction, weight gain, nausea) lead to discontinuation [27]. |
Comparative Efficacy and Limitations Analysis
The data in Table 2 reveals distinct profiles. BEM often excels in providing targeted, reversible, and adjustable therapy for specific patient subsets, particularly those refractory to pharmacotherapy, with effects that are not dependent on systemic pharmacokinetics [21] [29]. Its limitations often involve invasiveness, upfront costs, and a defined set of device-related risks. Pharmaceuticals offer broad accessibility and non-invasiveness but are frequently limited by systemic side effects, imperfect target specificity, and adherence challenges stemming from both side effects and dosing regimens [21] [30]. The high discontinuation rates for chronic condition drugs like GLP-1s highlight a significant gap that BEM aims to address through its implantable, "always-on" therapeutic potential.
Experimental Protocols for BEM Device Validation
For researchers developing new BEM technologies, rigorous and standardized testing is paramount. The following protocols outline critical pathways for evaluating long-term device performance, a major focus of current R&D.
Protocol 1: Accelerated Life Testing for Implant Reliability
This protocol evaluates the mechanical and electrical longevity of implantable systems under simulated physiological conditions [6].
- Objective: To predict the functional lifespan and identify primary failure modes of a hermetic implantable pulse generator (IPG) or a flexible electrode array.
- Materials:
- Device Under Test (DUT): Sealed IPG or flexible electrode array.
- Saline Bath: Phosphate-buffered saline (PBS) at pH 7.4, maintained at 37°C.
- Environmental Chamber: For controlled temperature and humidity cycling.
- Electrochemical Impedance Spectroscopy (EIS) Station.
- Mechanical Cyclers: For applying repetitive strain to flexible components.
- Methodology:
- Step 1: Perform baseline electrical characterization (impedance, stimulation output voltage/current).
- Step 2: Submerge DUT in a 37°C PBS bath, with options for:
- Static Soak: For assessing corrosion and fluid ingress.
- Accelerated Temperature/Humidity Cycling: (e.g., -20°C to +60°C, 90% RH) to induce thermo-mechanical stress.
- Step 3: For flexible implants, mount on a mechanical cycler to simulate in vivo movement (e.g., 100 million cycles at 1-2 Hz strain).
- Step 4: Periodically remove DUT for intermediate EIS and functional testing to monitor for performance drift or failure.
- Step 5: Upon failure or study conclusion, perform failure analysis (e.g., microscopic inspection, leak testing) to identify root cause.
- Outcome Measures: Mean Time Between Failures (MTBF), failure rate, specific failure modes (e.g., insulation breach, electrode corrosion, electronic malfunction) [6].
Protocol 2: In Vivo Biocompatibility and Functional Stability
This protocol assesses the foreign body response (FBR) and chronic performance of a BEM device in an animal model.
- Objective: To quantify the chronic tissue response and recording/stimulation stability of a novel soft neural interface.
- Materials:
- DUT: Soft, flexible electrode array (e.g., based on conducting polymers like PEDOT:PSS or polyimide substrates).
- Animal Model: Rodent or large animal model per IACUC protocol.
- Surgical equipment and stereotaxic frame.
- Histology Reagents: Paraformaldehyde (4%), cryostat, antibodies for immunohistochemistry (IHC: GFAP for astrocytes, Iba1 for microglia, NeuN for neurons), and appropriate fluorescent secondary antibodies.
- Neural recording and stimulation system.
- Methodology:
- Step 1: Aseptically implant the DUT into the target tissue (e.g., cortex, peripheral nerve).
- Step 2: Over a 12-week period, periodically measure:
- Electrical Performance: Electrode impedance, signal-to-noise ratio (SNR) of recorded neural signals, stimulation charge injection limits.
- Step 3: At terminal time points, perfuse-fixate the animal and explant the tissue with the implanted device.
- Step 4: Process tissue for histology: section, and stain with H&E and IHC markers.
- Step 5: Image and quantitatively analyze the FBR: glial scar thickness, neuronal density around the implant, and extent of microglia activation compared to unimplanted control tissue [6].
- Outcome Measures: Glial scar thickness (µm), neuronal density (neurons/mm²), chronic impedance (kΩ), and SNR stability over time.
Diagram 1: Experimental workflow for BEM device validation, integrating in-vivo and ex-vivo protocols.
The Scientist's Toolkit: Essential Research Reagents and Materials
Developing and testing next-generation BEM devices requires a specialized suite of materials and reagents. The table below details key items critical for advancing the field.
Table 3: Essential Research Reagents and Materials for BEM Development
| Item / Reagent | Category | Primary Function in BEM Research |
|---|---|---|
| Conducting Polymers (e.g., PEDOT:PSS) | Electrode Material | Bridges biology-electronics gap; improves charge injection, reduces impedance, enhances biocompatibility vs. metals [6]. |
| Flexible/Stretchable Substrates (e.g., Polyimide, PDMS) | Device Substrate | Provides soft, conformal interface with tissue; minimizes mechanical mismatch and chronic FBR [6]. |
| IHC Antibodies (GFAP, Iba1, NeuN) | Biological Reagent | Quantifies foreign body response and neuronal health around implants post-explantation [6]. |
| Phosphate-Buffered Saline (PBS) | Laboratory Reagent | Simulates ionic body fluid environment for in-vitro accelerated aging and corrosion tests [6]. |
| Hermetic Encapsulation (e.g., SiC, Al2O3) | Packaging Material | Protects "dry" electronics from corrosive bodily fluids, ensuring long-term device functionality and biostability [21] [6]. |
| Wireless Power/Data Transfer Coils | System Component | Enables battery-less operation and communication with implanted devices, crucial for miniaturization [21]. |
The convergence of market drivers and technological innovation is setting the stage for the next generation of BEM. Key future directions include the development of closed-loop systems that use real-time biosensor data to automatically adjust therapy, truly realizing personalized medicine [29] [6]. Further, the expansion into new disease areas, particularly inflammatory and autoimmune disorders via the "neuro-immune axis," represents a frontier for non-drug intervention [29]. Finally, the push towards battery-less devices powered wirelessly and made from bioresorbable materials will address challenges related to device lifetime, surgical retrieval, and long-term environmental impact [21] [6].
For the research community, the comparison between bioelectronic and pharmaceutical outcomes is not about declaring a winner, but about defining the optimal therapeutic context for each. BEM offers a compelling, targeted, and adjustable modality for a range of chronic conditions, particularly where pharmaceuticals face challenges with specificity, adherence, or systemic toxicity. As the field overcomes hurdles related to device longevity, biocompatibility, and cost, its role as a complementary pillar to pharmacotherapy is poised to expand significantly, driven irrevocably by demographic shifts, chronic disease prevalence, and relentless technological convergence.
The Shift Towards Personalized, On-Demand Therapies and Reduced Environmental Impact
The healthcare landscape is undergoing a significant transformation, moving from a traditional one-size-fits-all model toward more tailored approaches. This guide objectively compares two distinct pathways in this evolution: bioelectronic medicine, which uses electrical signals to modulate nervous system activity, and pharmaceutical therapies, particularly those with personalized applications. The comparison examines their mechanisms, therapeutic outcomes, and environmental footprints to inform research and development strategies. Bioelectronic medicine represents a shift toward device-based, on-demand therapies that can be adjusted in real-time, while pharmaceutical outcomes research continues to evolve with more targeted biological agents. Understanding the distinctions between these approaches is crucial for researchers, scientists, and drug development professionals navigating the future of therapeutic intervention.
Comparative Analysis: Mechanisms and Environmental Impact
Table 1: Direct Comparison of Bioelectronic Medicine and Pharmaceutical Therapies
| Comparison Parameter | Bioelectronic Medicine | Personalized Pharmaceuticals |
|---|---|---|
| Therapeutic Mechanism | Modulation of neural signals and specific nerve pathways [31] | Chemical interaction with molecular targets (e.g., receptors, enzymes) [32] |
| Personalization Approach | Programmable stimulation parameters; adaptive algorithms [28] [31] | Tailored to individual genetic, proteomic, or metabolic profiles [32] |
| Dosage/Application Control | On-demand, adjustable, and reversible stimulation [31] | Fixed-dose regimens based on patient characteristics [32] |
| Onset of Action | Typically rapid (milliseconds to seconds) | Variable (minutes to hours) |
| Environmental Impact (CO2e) | Device manufacturing and energy use [33] | High emissions from manufacturing, distribution, and supply chain [33] |
| Primary Waste Stream | Electronic waste (e-waste) from devices [33] | Pharmaceutical waste, single-use plastics, and lab waste [33] |
| Key Advantage | Non-pharmacological, avoids systemic side effects [31] | High specificity for molecular targets [32] |
| Key Limitation | Requires invasive procedures for implantable devices [31] | Environmental footprint from production and disposal [33] |
Table 2: Quantitative Environmental Impact Comparison
| Impact Category | Bioelectronic Medicine (Example Data) | Pharmaceuticals/Therapeutics (Example Data) |
|---|---|---|
| Carbon Footprint (per course) | Data limited; device manufacturing and energy use contribute [33] | Radiotherapy (as proxy): 4,310 kg CO2e for 25-fraction course [34] |
| Contributing Factors | Patient transit, facility energy use, device manufacturing [33] | Patient transit, facility energy, medical supplies, manufacturing [34] |
| Waste Generation | E-waste from devices and components [33] | Significant plastic and medical waste [33] |
| Potential Mitigation | Hypofractionation, renewable energy, efficient devices [34] | Hypofractionation, sustainable packaging, waste recycling [33] [34] |
Experimental Data and Supporting Evidence
Bioelectronic Medicine Workflow and Outcomes
Experimental Protocol for Neuromodulation Therapy:
- Patient Selection: Identify patients with a confirmed diagnosis of a neuromodulation-responsive condition (e.g., drug-resistant epilepsy, Parkinson's tremor, chronic pain).
- Target Identification: Use imaging (MRI, CT) to anatomically locate the target nerve or brain region.
- Device Implantation: Surgically implant the bioelectronic device (e.g., vagus nerve stimulator, deep brain stimulation leads).
- Parameter Programming: Set initial electrical stimulation parameters (frequency, pulse width, amplitude) based on established protocols and individual patient anatomy.
- Dose Titration: Adjust stimulation parameters in a controlled setting to optimize efficacy and minimize side effects.
- Efficacy Assessment: Monitor therapeutic outcomes using standardized clinical scales (e.g., reduction in seizure frequency, improvement in tremor scores, pain scales).
- Long-term Follow-up: Assess device functionality, battery life, and long-term therapeutic maintenance [31].
Supporting Data: Studies on Vagus Nerve Stimulation (VNS) show a median of 50% reduction in seizure frequency is achieved in a significant proportion of patients with drug-resistant epilepsy after 12 months of therapy, demonstrating a non-pharmacological option for a challenging patient population.
Pharmaceutical Outcomes and Personalized Approaches
Experimental Protocol for Targeted Drug Therapy:
- Biomarker Identification: Obtain patient biospecimen (tissue, blood) for genetic or proteomic analysis.
- Molecular Profiling: Sequence specific genes or assay protein levels to identify targetable mutations or biomarkers (e.g., EGFR in lung cancer, BRCA in breast cancer).
- Therapy Selection: Prescribe a pharmaceutical agent that specifically targets the identified molecular alteration.
- Dosing Regimen: Administer the drug according to a weight-based or fixed-dose schedule, as per clinical guidelines.
- Therapeutic Drug Monitoring: Measure drug levels in blood, if applicable, to ensure therapeutic range and avoid toxicity.
- Efficacy Assessment: Use radiographic imaging (e.g., RECIST criteria for oncology) and clinical evaluation to assess treatment response.
- Toxicity Monitoring: Record and manage drug-related adverse events [32].
Supporting Data: The use of Ivacaftor for cystic fibrosis patients with specific G551D mutations in the CFTR gene demonstrates the power of personalized pharmaceuticals. Clinical trials showed significant and sustained improvements in lung function (FEV1) compared to placebo, validating a genotype-driven treatment approach [32].
Visualization of Therapeutic Pathways
Diagram Title: Contrasting Therapeutic Pathways
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents and Materials for Investigative Studies
| Reagent/Material | Primary Function | Application Context |
|---|---|---|
| Multi-electrode Arrays | Record and stimulate electrical activity in neural tissues. | In vitro and in vivo studies of neurostimulation efficacy and safety [31]. |
| Biocompatible Encapsulants | Protect implanted electronics from the biological environment and ensure device longevity. | Development of chronic bioelectronic implants for human use [31]. |
| Genotyping Kits | Identify specific genetic variations in patient DNA samples. | Patient stratification for targeted drug trials and pharmacogenomic studies [32]. |
| Cytokine Assay Panels | Quantify protein biomarkers of inflammation and immune response. | Monitoring systemic effects of both neuromodulation and drug therapies [31]. |
| Target-Specific Antibodies | Detect and measure expression levels of protein targets. | Validation of target engagement in drug development and molecular diagnostics [32]. |
This comparison guide outlines a clear divergence in the mechanisms, applications, and environmental considerations of bioelectronic medicine and personalized pharmaceutical therapies. Bioelectronic medicine offers a unique value proposition with its on-demand, adjustable, and non-pharmacological mechanism of action, potentially leading to a different environmental impact profile centered on device manufacturing and energy use. In contrast, personalized pharmaceuticals provide exquisite molecular specificity but face challenges related to a significant environmental footprint from manufacturing and waste. For researchers and drug development professionals, the choice between these paradigms—or their potential convergence—will be guided by the disease target, the desired mode of action, and an increasing responsibility to consider environmental sustainability alongside therapeutic efficacy.
Therapeutic Applications and Technological Frontiers: From Pacemakers to Closed-Loop Systems
The management of cardiac arrhythmias represents a cornerstone of bioelectronic medicine, which harnesses implantable devices to interface with electrically active tissues, offering a therapeutic alternative to pharmacotherapies [1]. Unlike systemic drugs that can cause off-target effects, bioelectronic devices such as pacemakers and implantable cardioverter-defibrillators (ICDs) provide precise, targeted treatment by directly modulating the heart's electrical system [6]. This approach has evolved significantly from the first fully implantable pacemaker in 1958 to sophisticated closed-loop systems that adapt to patient needs in real time [13]. Within the broader context of bioelectronic medicine versus pharmaceutical outcomes, these devices offer a compelling value proposition: they provide continuous, responsive therapy without the chemical side effects or variable pharmacokinetics associated with antiarrhythmic drugs, potentially revolutionizing care for patients with rhythm disorders [1].
Device Comparison: Pacemakers vs. Implantable Defibrillators
While both pacemakers and implantable defibrillators are crucial for arrhythmia management, they serve distinct functions and are indicated for different patient populations [35]. Understanding their complementary roles is essential for optimizing therapeutic strategy within a bioelectronic treatment paradigm.
Pacemakers are primarily designed to regulate slow or irregular heartbeats (bradycardia) by delivering low-energy electrical pulses to maintain a steady rhythm [35]. They continuously monitor the heart and provide stimulation only when the natural rhythm becomes too slow or pauses.
Implantable Cardioverter-Defibrillators (ICDs) serve a different purpose – they are specialized for terminating life-threatening rapid arrhythmias (tachycardia) such as ventricular tachycardia (VT) or ventricular fibrillation (VF) [36] [35]. These devices constantly monitor heart rhythms and deliver high-energy shocks to reset the heart to a normal rhythm when detected dangerous arrhythmias [35].
The table below summarizes the key differences between these device classes:
Table 1: Performance Comparison of Pacemakers and Implantable Defibrillators
| Feature | Pacemakers | Implantable Defibrillators (ICDs) |
|---|---|---|
| Primary Function | Regulates slow heart rhythms [35] | Stops dangerous fast rhythms [35] |
| Energy Output | Low-energy pulses [35] | High-energy shocks [35] |
| Main Conditions Treated | Bradycardia, heart block, atrial fibrillation with slow ventricular response [35] | Ventricular tachycardia, ventricular fibrillation, sudden cardiac arrest [35] |
| Patient Risk Profile | Moderate risk of fainting or fatigue from bradycardia [35] | High risk of sudden cardiac death [35] |
| Activation Mechanism | Continuously monitors and paces as needed [35] | Activates only during dangerous arrhythmias [35] |
| Battery Longevity | Typically 8-15 years [35] | Typically 5-10 years [35] |
| Therapeutic Paradigm | Chronic rhythm support | Emergency life-saving intervention |
Indications and Clinical Evidence
Device selection is guided by robust clinical evidence and appropriate use criteria established in recent guidelines [37].
Pacemaker Indications:
- Symptomatic bradycardia
- Advanced heart block
- Sinus node dysfunction
- Atrial fibrillation with prolonged pauses [35]
ICD Indications:
- Secondary Prevention: For patients who have survived sudden cardiac arrest due to VT/VF or experienced hemodynamically unstable VT [36]. Clinical trials including AVID, CASH, and CIDS demonstrated a 20-39% reduction in mortality with ICDs compared to antiarrhythmic drugs in this population [36].
- Primary Prevention: For patients with ischemic or nonischemic cardiomyopathy, left ventricular ejection fraction (LVEF) <35%, and New York Heart Association Class II/III symptoms on optimal guideline-directed medical therapy [36]. Landmark trials including MADIT, MADIT-II, and SCD-HeFT demonstrated significant mortality reduction with primary prevention ICDs [36].
Advanced ICD Technologies and Performance Data
The technological landscape of ICDs has evolved significantly, with current systems offering various configurations tailored to individual patient needs [36].
ICD System Architectures
Transvenous ICDs (TV-ICDs) represent the traditional approach with leads placed through the venous system into the heart [36]. These are further categorized by chamber configuration:
- Single-Chamber (SC) ICDs: One lead in the right ventricle [36]
- Dual-Chamber (DC) ICDs: Leads in both the right atrium and right ventricle [36]
- Cardiac Resynchronization Therapy Defibrillators (CRT-D): Leads in right atrium, right ventricle, and coronary sinus to synchronize ventricular contraction [36]
Subcutaneous ICDs (S-ICDs) feature a lead implanted just under the skin along the left side of the chest, without intravascular components, reducing certain procedural risks [36] [35].
Extravascular ICDs (EV-ICDs) represent the latest advancement, with leads placed outside the heart but within the chest, enabling antitachycardia pacing without transvenous leads [38].
Comparative Performance Data
Recent studies provide quantitative comparisons of ICD technologies and their performance:
Table 2: Comparative Performance of Contemporary ICD Technologies
| Technology | Inappropriate Shock Rates | Therapeutic Efficacy | Complication Profile |
|---|---|---|---|
| Single-Chamber TV-ICD | Similar to DC-ICDs with modern discriminators [36] | APPRAISE ATP trial: 28% relative risk reduction in time to first all-cause shock with ATP enabled [38] | Lower rate of device-related complications compared to DC-ICDs without pacing indication [36] |
| Dual-Chamber TV-ICD | Historically lower, but contemporary studies show mixed results [36] | APPRAISE ATP trial: ATP success demonstrated in primary prevention [38] | Higher rate of pneumothorax, hemothorax, and lead dislodgement without pacing indication [36] |
| Subcutaneous ICD (S-ICD) | Comparable to transvenous systems with modern programming | MODULAR ATP: 61.3% ATP success rate when combined with leadless pacemaker [38] | Avoids lead-related cardiac complications; higher risk of pocket infections |
| ICD with Floating Atrial Dipole | Retrospective studies show modest reduction in inappropriate shocks [36] | Maintains single-chamber system simplicity while enabling better rhythm discrimination [36] | Similar to single-chamber systems; avoids additional lead complications |
MRI-Conditional ICDs represent another technological advancement, with the global market valued at approximately USD 1,750 million in 2025 and projected to reach USD 3,400 million by 2034, growing at a CAGR of 7.64% [39]. These devices incorporate special shielding and filters to safely undergo magnetic resonance imaging, addressing a significant limitation of earlier devices [39].
Experimental Protocols and Methodologies
APPRAISE ATP Trial Protocol
The Assessment of Primary Prevention Patients Receiving an ICD- Systematic Evaluation of ATP (APPRAISE ATP) study represents the largest head-to-head trial of antitachycardia pacing (ATP) in primary prevention patients with transvenous ICDs [38].
Objective: To evaluate the role of ATP by measuring time to first all-cause shock in primary prevention patients with TV-ICDs using contemporary programming [38].
Methodology:
- Study Design: Prospective, randomized controlled trial
- Population: Primary prevention patients with transvenous ICDs
- Intervention: Patients randomized to standard therapy (ATP and shock) versus shock-only treatment
- Primary Endpoint: Time to first all-cause shock
- Programming: Contemporary device programming protocols were utilized
- Follow-up: Regular device interrogation and remote monitoring
Key Findings:
- The ATP and shock arm demonstrated a 28% relative risk reduction in time to first all-cause shock
- This represents an absolute reduction in first all-cause shock in approximately 1% of primary prevention TV-ICD patients per year [38]
MODULAR ATP Clinical Trial Protocol
The MODULAR ATP trial evaluated the safety, performance, and effectiveness of a modular cardiac rhythm management system consisting of the EMBLEM S-ICD System and the EMPOWER Leadless Pacemaker [38].
Objective: To assess the first modular, intra-body, communicating subcutaneous defibrillator-leadless pacemaker system for tachycardia therapy [38].
Methodology:
- Study Design: Prospective clinical trial
- System Configuration: Modular system with S-ICD and leadless pacemaker components
- Communication Protocol: Intra-body communication between subcutaneous defibrillator and leadless pacemaker
- Primary Endpoints:
- Leadless pacemaker complication-free rate
- Communication success rate from S-ICD to leadless pacemaker
- Pacing capture thresholds
- ATP success rate
- Follow-up: Regular device interrogation and performance assessment
Key Findings:
- Leadless pacemaker complication-free rate of 97.5%
- Communication success rate of 98.8% from S-ICD to leadless pacemaker
- Low and stable pacing capture thresholds (≤2.0 V at 0.4 ms) in 97.4% of patients
- ATP success rate of 61.3%
- No patient requests for deactivation of ATP or bradycardia pacing due to pain or discomfort [38]
Research Reagent Solutions and Experimental Tools
The following table details essential research materials and methodologies used in device performance evaluation and clinical trials:
Table 3: Essential Research Toolkit for Device Performance Evaluation
| Research Tool | Function/Application | Experimental Context |
|---|---|---|
| Device Interrogation Systems | Retrieval of stored device data including arrhythmia episodes, therapy delivery, and lead parameters [40] | Routine follow-up in APPRAISE ATP and MODULAR ATP trials [38] [40] |
| Remote Monitoring Platforms | Transmission of device data to healthcare providers for timely assessment of system integrity and arrhythmia detection [40] | Standard of care in contemporary device trials including MODULAR ATP [38] |
| Lead Impedance Measurement | Assessment of lead integrity and detection of conductor fractures or insulation breaches [40] | Component of device interrogation in performance studies [40] |
| Pacing Threshold Testing | Determination of minimum energy required for reliable cardiac capture [40] | Evaluated in MODULAR ATP (≤2.0 V at 0.4 ms in 97.4% of patients) [38] |
| ATP Success Rate Assessment | Evaluation of antitachycardia pacing efficacy in terminating ventricular tachycardia without shock delivery [38] | Primary endpoint in APPRAISE ATP and MODULAR ATP trials [38] |
| Signal Discrimination Algorithms | Differentiation of ventricular from supraventricular tachyarrhythmias to prevent inappropriate therapy [36] | Critical component in single-chamber vs. dual-chamber ICD comparisons [36] |
Decision Pathways and System Workflows
Clinical Decision Pathway for Device Selection
The following workflow illustrates the clinical decision process for selecting the appropriate bioelectronic device for arrhythmia management:
Clinical Decision Pathway for Device Selection
Modular ICD System Communication Workflow
The MODULAR ATP trial demonstrated a novel system architecture with communication between subcutaneous and leadless components:
Modular ICD System Communication Workflow
The evolution of pacemakers and implantable defibrillators exemplifies the transformative potential of bioelectronic medicine in managing cardiovascular disease [13]. These devices offer targeted, responsive therapy that complements or replaces pharmaceutical approaches, particularly for life-threatening arrhythmias where drug efficacy may be limited or side effects prohibitive [1]. Current research demonstrates continued innovation in device technology, from modular systems that combine subcutaneous defibrillation with leadless pacing to advanced algorithms that reduce inappropriate therapies [38]. The integration of digital health technologies and artificial intelligence promises further enhancement of device functionality, potentially enabling more personalized and adaptive therapies [10] [39]. As the field advances, these bioelectronic approaches stand to play an increasingly important role in the therapeutic landscape, offering solutions that bridge the gap between pharmaceutical interventions and invasive surgical procedures for arrhythmia management.
Bioelectronic medicine represents a paradigm shift in therapeutic strategies, moving from systemic pharmacological interventions to the targeted modulation of specific neural circuits. This approach uses implanted or external devices to deliver electrical impulses to the nervous system to treat neurological and psychiatric disorders. For researchers and drug development professionals, understanding the performance data, protocols, and mechanisms of these technologies is crucial for positioning future R&D investments. This guide provides a comparative analysis of two established bioelectronic therapies: Deep Brain Stimulation (DBS) for Parkinson's disease and Vagus Nerve Stimulation (VNS) for treatment-resistant depression (TRD) and epilepsy. The objective data presented herein, including direct comparisons with pharmaceutical outcomes, offer a foundation for evaluating the role of bioelectronic medicine in the modern therapeutic arsenal.
Deep Brain Stimulation (DBS) for Parkinson's Disease
Clinical Performance and Outcomes
DBS, particularly targeting the subthalamic nucleus (STN), is a well-established intervention for Parkinson's disease (PD) not adequately controlled by medication. A 2025 large-scale multicenter cohort study offers robust evidence for its efficacy across different disease stages [41].
Table 1: Two-Year Outcomes of STN-DBS in Parkinson's Disease by Disease Duration [41]
| Outcome Measure | Short Duration (<5 years) | Mid Duration (5-10 years) | Long Duration (≥10 years) | Overall Improvement (Mean) |
|---|---|---|---|---|
| MDS-UPDRS-III (OFF-Meds) | Significant Improvement | Greatest Improvement (8.0% vs. short; 5.6% vs. long) | Significant Improvement | 46.7% ± 14.1% (MD 25.1) |
| Quality of Life (PDQ-39) | Significant Improvement | Significant Improvement | Significant Improvement | 47.9% ± 17.8% (MD 28.0) |
| Hamilton Anxiety (HAM-A) | Significant Improvement | Greatest Improvement vs. long duration | Significant Improvement | 54.4% ± 22.4% (MD 8.0) |
| Hamilton Depression (HAM-D) | Significant Improvement | Greatest Improvement vs. long duration | Significant Improvement | 43.4% ± 22.6% (MD 6.3) |
| Key Prognostic Factor | Levodopa response (adjusted β 0.42) | Levodopa response (adjusted β 0.17); Baseline MDS-UPDRS-III (adjusted β 0.10) | Levodopa response (adjusted β 0.20); Baseline MDS-UPDRS-III (adjusted β 0.30) | Levodopa response is a unified positive factor |
A 2025 network meta-analysis compared DBS with magnetic resonance-guided focused ultrasound (MRgFUS) and medication alone, providing a relative efficacy ranking [42]. For motor symptoms in the OFF-phase, STN-focused ultrasound (STNFUS) ranked highest (SUCRA 79.6%), followed by combined STN-GPiDBS (73.7%) and STNDBS (69.1%). For quality of life, however, GPiDBS was the top-ranked intervention (SUCRA 77.2%), followed by STN_DBS (67.3%) [42].
Recent innovations include adaptive DBS (aDBS), which dynamically adjusts stimulation based on neurophysiological feedback. A 2025 study of beta-guided aDBS reported significantly improved overall well-being compared to continuous DBS (cDBS), with a trend toward enhanced general movement. Within-subject analysis showed significant improvement in three of eight patients, and six of eight chose to remain on aDBS long-term [43].
Experimental Protocol and Workflow
The cited 2025 cohort study [41] provides a representative methodology for large-scale DBS outcomes research:
- Study Design: Multicenter retrospective cohort analysis (DBS-PD Chinese Collaboration-2).
- Participants: 1,717 patients with idiopathic PD who underwent STN-DBS between 2011-2020 across seven national centers. Patients were classified by disease duration.
- Primary Assessments: Conducted at 2-year follow-up using:
- Movement Disorder Society-sponsored revision of the Unified Parkinson's Disease Rating Scale, Part III (MDS-UPDRS-III) in the OFF-medication state.
- Hamilton Anxiety (HAM-A) and Depression (HAM-D) Rating Scales.
- Parkinson's Disease Questionnaire-39 (PDQ-39) for quality of life.
- Statistical Analysis: Relative changes in scores were analyzed for within- and between-group comparisons. Prognostic factors were identified via multivariable linear regression.
The workflow for aDBS programming, as detailed in a 2025 clinical report [43], involves a multi-step process to transition from continuous to adaptive stimulation, which can be visualized in the diagram below.
The Scientist's Toolkit: Key Reagents and Materials for DBS Research
Table 2: Essential Research Materials for DBS Investigations
| Item | Function/Application in Research | Example/Note |
|---|---|---|
| DBS Systems with Sensing | Enables chronic recording of local field potentials (LFPs) for adaptive stimulation and biomarker discovery. | Medtronic Percept PC platform allows simultaneous sensing and stimulation [43]. |
| Local Field Potential (LFP) Data | Primary biomarker for adaptive DBS; beta band power correlates with bradykinesia and rigidity. | Used as feedback control signal in aDBS; analyzed via "BrainSense Streaming" [43]. |
| Movement Disorder Society-Sponsored Revision of the Unified Parkinson's Disease Rating Scale (MDS-UPDRS) | Gold-standard clinical tool for assessing motor symptom severity in Parkinson's disease. | Part III (Motor Examination) is primary outcome in most DBS trials [41] [42]. |
| Levodopa Challenge Test | Standardized test to assess dopaminergic response; a key predictor of DBS motor outcome. | Preoperative response is a unified positive prognostic factor across disease durations [41]. |
| Parkinson's Disease Questionnaire-39 (PDQ-39) | Patient-reported outcome measure assessing health-related quality of life. | Critical for evaluating the holistic impact of DBS beyond motor symptoms [41] [42]. |
Vagus Nerve Stimulation (VNS) for Depression and Epilepsy
Clinical Performance and Outcomes
VNS is an established therapy for drug-resistant epilepsy (DRE) and treatment-resistant depression (TRD). Its efficacy, particularly the improvement over long-term use, is a critical differentiator from pharmaceutical options.
Table 3: Long-Term Efficacy of VNS in Drug-Resistant Epilepsy (DRE) [44] [45]
| Follow-up Period | Responder Rate (≥50% Seizure Reduction) | Seizure-Free Rate | Study Details |
|---|---|---|---|
| 12 Months | 33.4% (33/99 patients) | 7.1% (7/99 patients) | Single-center retrospective study (n=99) [44]. |
| 24 Months | 40.0% (32/80 patients) | 15.0% (12/80 patients) | Efficacy increases over time [44]. |
| 36 Months | 51.4% (36/70 patients) | 15.7% (11/70 patients) | Clear trend of improving response [44]. |
| 5 Years | 55.1% (27/49 patients) | 16.3% (8/49 patients) | Long-term sustainability demonstrated [44]. |
| 5 Years (tVNS) | 30% (Responder Rate) | Not Specified | Retrospective cohort comparing iVNS & tVNS [45]. |
| 5 Years (iVNS) | 32% (Responder Rate) | Not Specified | iVNS and tVNS showed comparable effects [45]. |
For TRD, a 2025 systematic review of long-term efficacy (≥2 years) found that VNS provides sustained clinical benefits for a severe patient population characterized by insufficient improvement after multiple antidepressant trials and long-standing illness [46]. The review, synthesizing over 900 cases, highlighted that VNS response and remission rates increase over the course of months to years, a pattern distinct from the often-waning effects of sequential pharmacotherapy [46].
The choice of stimulation laterality (left vs. right VNS) is a key consideration. Left-sided VNS (L-VNS) is the historical standard, primarily due to cardiac safety concerns regarding the right vagus nerve's proximity to the sinoatrial (SA) node [47]. However, emerging evidence suggests right-sided VNS (R-VNS) may be a viable and potentially advantageous approach for selected indications like heart failure, with studies reporting improvements in NYHA class and left ventricular function [47].
Experimental Protocol and Workflow
The methodology for evaluating long-term VNS outcomes in epilepsy is exemplified by a 2025 retrospective study [44]:
- Study Design & Participants: Retrospective analysis of DRE patients who underwent VNS stimulator implantation (2016-2019) and had >1 year follow-up data.
- Stimulator & Surgery: Implantation of a pulse generator and electrode cuff on the left vagus nerve under general anesthesia.
- Stimulation Parameters: Activated two weeks post-op. Initial settings: 0.20 mA current, 500 μs pulse width, 30 Hz frequency, 30 s on, 5 min off. Current was titrated upwards every two weeks.
- Efficacy Evaluation: Based on seizure frequency diaries. Response defined as ≥50% reduction in seizure frequency at 1-year post-implantation.
- Statistical Analysis: Logistic regression was used to identify efficacy predictors, with structural etiology identified as a negative predictor (OR = 0.35) [44].
The mechanism of VNS involves modulating central nervous system circuits via afferent vagal pathways, which can be visualized as follows:
The Scientist's Toolkit: Key Reagents and Materials for VNS Research
Table 4: Essential Research Materials for VNS Investigations
| Item | Function/Application in Research | Example/Note |
|---|---|---|
| Implantable VNS (iVNS) System | Surgical system for chronic cervical vagus nerve stimulation; the gold-standard for invasive VNS research. | Consists of a pulse generator (e.g., from LivaNova) and electrode cuff [46] [47]. |
| Transcutaneous VNS (tVNS) Device | Non-invasive alternative using surface electrodes on the ear (taVNS) or neck (tcVNS) for exploratory studies. | Nemos stimulator is used for taVNS research; allows for blinded sham-controlled trials [45]. |
| Seizure Frequency Diary | Primary outcome measure for epilepsy studies; used to calculate responder rates. | Standardized patient-reported logs are critical for determining ≥50% responder rates [44]. |
| Hamilton Rating Scales (HAM-D/A) | Clinician-administered scales to quantify depression (HAM-D) and anxiety (HAM-A) severity. | Standard outcomes in TRD trials to measure mood effects beyond seizure control [41] [46]. |
| Structural Neuroimaging (MRI) | Used for etiology classification and as a potential predictor of VNS outcome. | Structural etiology is a identified negative predictor of VNS effectiveness in epilepsy (OR=0.35) [44]. |
Integrated Discussion: Positioning vs. Pharmaceutical Outcomes
The data reveals distinct profiles for DBS and VNS compared to pharmacological interventions. The primary advantage of these bioelectronic therapies lies in their sustained and often improving efficacy over decades, contrasting with the common challenges of tachyphylaxis or long-term side effects associated with many chronic drug regimens.
DBS vs. Pharmacotherapy for PD: While levodopa remains the cornerstone of PD treatment, DBS offers a powerful alternative when motor complications emerge. The evidence shows that DBS not only improves motor control by ~47% but also significantly enhances quality of life (~48%) and mood [41]. The timing of intervention is critical; patients with mid-duration PD (5-10 years) derived the greatest benefit, suggesting an optimal therapeutic window that balances disease progression with preserved neural circuitry for modulation [41].
VNS vs. Pharmacotherapy for TRD and DRE: For DRE, VNS offers a progressive increase in responder rates, reaching over 50% after three years—a pattern not seen with sequential ASM trials [44]. Similarly, for TRD, VNS provides a long-term maintenance therapy for a population that has exhausted multiple pharmaceutical options [46]. The non-pharmacological mechanism avoids systemic side effects and drug-drug interactions, a significant advantage in these complex patient populations.
The convergence of bioelectronic medicine with artificial intelligence and device miniaturization is a key trend, pushing the field toward intelligent, closed-loop systems [43] [48]. aDBS and the exploration of novel stimulation sites represent a move towards truly personalized, adaptive therapies that can respond in real-time to a patient's physiological state, a level of personalization difficult to achieve with conventional pharmaceuticals.
For researchers and drug development professionals, the data underscores that DBS and VNS are not merely last-resort options but are specialized therapies with validated efficacy and predictable outcomes. The choice between bioelectronic and pharmaceutical strategies is not one of replacement but of strategic integration. Bioelectronic medicine excels in specific niches: DBS for advanced, medication-responsive Parkinson's disease, and VNS for the long-term management of drug-resistant epilepsy and depression. The future of neurotherapeutics lies in identifying the right patient, the right target, and the right timing for each modality, leveraging the unique strengths of both bioelectronic and pharmaceutical approaches to improve patient outcomes.
The management of chronic pain presents a formidable challenge for healthcare systems worldwide. For decades, pharmaceutical approaches, particularly opioids, have been a cornerstone of treatment, despite well-documented risks of dependence, tolerance, and systemic side effects [49]. In contrast, bioelectronic medicine offers a fundamentally different strategy by using targeted electrical stimulation to modulate the nervous system's activity. Spinal Cord Stimulation (SCS) is a leading bioelectronic therapy for chronic pain, acting as a non-pharmacologic intervention that directly interferes with pain signal transmission [49]. This guide provides an objective, data-driven comparison of SCS against opioid therapy, contextualized within the broader framework of bioelectronic versus pharmaceutical outcomes research.
Quantitative Outcomes Comparison
Clinical outcomes for SCS and opioid therapy are measured across multiple domains, including pain relief, functional improvement, and reduction in concomitant treatments. The tables below summarize key quantitative data from recent studies.
Table 1: Key Efficacy and Opioid-Reduction Outcomes from SCS Studies
| Study / Therapy | Patient Population | Follow-up Period | Pain Reduction (>50%) | Opioid Reduction / Cessation | Functional Improvement |
|---|---|---|---|---|---|
| SCS with Multiple Waveforms (WaveWriter System) [50] | Chronic Back & Leg Pain | 2 years | 60% responder rate sustained | N/A | High functional success sustained |
| Closed-Loop SCS (Inceptiv SCS) [51] | Chronic Pain | N/A | 84% responder rate at 12 months (with DTM therapy) | N/A | N/A |
| SCS for Failed Back Surgery Syndrome (FBSS) [52] | FBSS (on opioids) | 2 years | N/A | 23% discontinued all opioids; 39% discontinued strong opioids | N/A |
| Noninvasive SCS (ARC-EX System) [53] | Chronic Spinal Cord Injury | 16 weeks + 6 months follow-up | N/A | N/A | 72% responded in both strength and function; gains persisted post-therapy |
Table 2: Comparative Risks and Limitations
| Parameter | Spinal Cord Stimulation (SCS) | Long-Term Opioid Therapy |
|---|---|---|
| Primary Mechanism | Modulation of pain pathways in spinal cord [49] | Binding to CNS opioid receptors |
| Common Risks/Complications | Lead migration, device explantation/revision (22.1% over 2 yrs), pocket pain, tolerance [49] [54] | Constipation, respiratory depression, tolerance, dependence, misuse, overdose |
| Real-World Opioid Use Impact | No significant reduction in chronic opioid use vs. CMM at 2 years [54] | N/A (Inherent to therapy) |
| Typical NNT for >50% Pain Relief | 1.2 to 2 [49] | 4 to 10 [49] |
| Cost Considerations | High initial cost; first-year costs ~$39,000 higher than CMM [54] | Lower initial cost; long-term costs associated with management of side effects and potential addiction |
Abbreviations: NNT, Number Needed to Treat; CNS, Central Nervous System; CMM, Conventional Medical Management.
Experimental Protocols and Methodologies
A critical evaluation of SCS efficacy relies on understanding the design of key clinical trials. Below are the methodologies for two pivotal types of studies.
Protocol: Randomized Controlled Trial (RCT) for SCS Waveforms
Objective: To compare the long-term pain relief efficacy of a multiple-waveform SCS system (e.g., Boston Scientific's WaveWriter) against conventional medical management [50].
- Study Design: Prospective, multicenter, open-label, randomized controlled trial.
- Participants:
- Inclusion: Subjects with chronic, intractable back and leg pain.
- Exclusion: Typically includes comorbidities that interfere with study participation or inability to use the device.
- Randomization: Subjects are randomized to either the SCS therapy group or the control group receiving conventional medical management.
- Intervention:
- SCS Group: Subjects undergo a trial stimulation period. Those with a successful trial (typically >50% pain relief) proceed to permanent implant of the SCS system.
- Control Group: Subjects continue to receive conventional medical management, which may include medications, physical therapy, and injections.
- Outcome Measures (Assessed at 3, 6, 12, and 24 months):
- Primary: The proportion of subjects achieving ≥50% reduction in pain from baseline (responder rate).
- Secondary: Patient-reported outcomes (e.g., Oswestry Disability Index - ODI, Quality of Life - SF-36), opioid dosage quantification, and subject satisfaction.
- Data Analysis: Intent-to-treat analysis using statistical methods (e.g., t-tests, chi-square) to compare responder rates and secondary outcomes between groups at each time point.
Protocol: Real-World Comparative Effectiveness Research
Objective: To determine the long-term outcomes of SCS versus conventional medical management (CMM) in a real-world patient cohort, using administrative claims data [54].
- Data Source: Retrospective analysis of a large administrative claims database (e.g., Optum Labs Data Warehouse) containing longitudinal medical and pharmacy claims.
- Cohort Selection:
- Inclusion: Insured adults with incident diagnoses of chronic pain conditions (e.g., Failed Back Surgery Syndrome, Complex Regional Pain Syndrome).
- Exclusion: Patients without continuous insurance coverage, or with diagnoses for other neuromodulation indications.
- Propensity Score Matching:
- Patients receiving permanent SCS implants are identified.
- Each SCS patient is matched with up to five CMM-only patients based on propensity scores, which model the probability of receiving an SCS implant using baseline characteristics (e.g., demographics, comorbidities, prior healthcare utilization). This creates a balanced cohort for comparison.
- Outcome Measures:
- Primary: Chronic opioid use (defined as ≥90 days' supply within a time window) and use of epidural/facet corticosteroid injections.
- Secondary: Rates of spine surgery, radiofrequency ablation, device-related complications, and total costs of care.
- Statistical Analysis: Logistic regression is used to calculate adjusted odds ratios for binary outcomes (e.g., chronic opioid use) between the SCS and CMM groups during specific follow-up periods (e.g., 1-12 months and 13-24 months).
Signaling Pathways and Mechanisms of Action
The therapeutic effects of SCS and opioids are achieved through distinct biological pathways. The diagram below illustrates these fundamental differences.
Figure 1: Mechanisms of Pain Modulation. SCS (left) acts by stimulating large-diameter A-beta fibers in the dorsal column, which then inhibits pain signal transmission from A-delta and C-fibers in the dorsal horn of the spinal cord, preventing pain signals from reaching the brain [49]. Opioids (right) bind to μ-opioid receptors in the central nervous system, causing neuronal hyperpolarization and reduced release of pain neurotransmitters [49].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Technologies for SCS Research
| Research Tool | Function / Application in SCS Studies |
|---|---|
| Implantable Pulse Generator (IPG) | The core device housing the battery and electronics that generate electrical pulses; can be rechargeable or non-rechargeable [1]. |
| Multipolar Epidural Leads | Electrode arrays implanted in the epidural space to deliver electrical stimulation to specific spinal cord segments; enable targeted neural dosing [50]. |
| Closed-Loop Sensing System | Technology (e.g., Medtronic's Inceptiv) that measures Evoked Compound Action Potentials (ECAPs) to automatically adjust stimulation in real-time, maintaining consistent therapy [51]. |
| Clinical Outcome Assessments | Validated patient-reported outcome measures (PROMs) like Visual Analog Scale (VAS) for pain, Oswestry Disability Index (ODI), and EQ-5D for quality of life [50] [54]. |
| Programming Software/App | Customizable interfaces (e.g., ARC-EX PRO) used by clinicians to define stimulation parameters (amplitude, frequency, pulse width) tailored to individual patients [53]. |
The evidence demonstrates that SCS represents a potent bioelectronic alternative to pharmaceutical opioids for chronic pain. SCS offers a favorable risk-benefit profile for specific indications like FBSS and CRPS, with Level I evidence supporting its superiority over medical management for pain relief and some studies showing significant opioid-weaning effects [52] [49] [55]. However, real-world data also tempers this outlook, indicating that SCS does not universally eliminate opioid use and carries its own risks, including device-related complications and revisions [54]. The choice between these modalities must be guided by patient-specific factors, including pain etiology, previous treatments, and personal preference. Future research should focus on optimizing patient selection, improving device durability, and developing next-generation closed-loop and personalized stimulation paradigms to solidify the role of bioelectronic medicine in the pain treatment landscape.
Closed-loop systems, often termed adaptive neuromodulation or automated insulin delivery in therapeutic contexts, represent a transformative approach in bioelectronic medicine. These systems create a continuous cycle of monitoring and treatment by integrating real-time biosensing with adaptive stimulation, enabling precise therapeutic interventions that dynamically respond to the body's changing physiological state. Unlike traditional open-loop systems that deliver predetermined therapy, closed-loop systems continuously monitor physiological signals, process this information through sophisticated algorithms, and automatically adjust therapeutic output to maintain optimal physiological parameters [56] [13]. This self-regulating paradigm marks a significant departure from both conventional bioelectronic medicine and pharmaceutical interventions, offering unprecedented precision in disease management.
The fundamental architecture of all closed-loop therapeutic systems comprises three core components: a biosensor that continuously monitors physiological signals, an algorithm that processes this information and makes therapeutic decisions, and an actuator that delivers the appropriate therapy, typically electrical stimulation or drug delivery [56] [1]. This integrated approach allows for personalized, on-demand treatments that can potentially achieve superior outcomes with reduced side effects compared to static therapeutic regimens. The following diagram illustrates the core operational workflow of a generic closed-loop system:
Bioelectronic Medicine vs. Pharmaceutical Outcomes: A Paradigm Comparison
The emergence of closed-loop systems occurs at the intersection of two distinct therapeutic paradigms: bioelectronic medicine and pharmaceutical outcomes research. Bioelectronic medicine utilizes implantable or wearable electronic devices to interface with the body's electrically active tissues—nerves, heart, muscles—to modulate their activity for therapeutic purposes [6] [1]. This approach harnesses the body's innate electrical signaling pathways to achieve precise, targeted effects. In contrast, pharmaceutical outcomes research focuses on measuring the results of drug-based interventions in patient populations, evaluating clinical, economic, and humanistic outcomes to inform healthcare decisions [57] [58].
The fundamental distinction between these approaches lies in their mechanism of action and therapeutic delivery. Bioelectronic medicine, particularly closed-loop systems, offers localized, electrical intervention that can be instantly adjusted or terminated, potentially reducing systemic side effects [1]. Pharmaceutical interventions typically involve systemic chemical distribution throughout the bloodstream, which often leads to off-target effects and limits specificity [1]. While pharmaceuticals require repeated administration and face challenges with patient adherence, closed-loop bioelectronic systems can provide continuous, automated therapy once implanted. From an outcomes perspective, pharmaceutical research employs methodologies like pharmacoeconomics and comparative effectiveness research to evaluate treatments across populations [58], whereas bioelectronic medicine is advancing toward highly personalized therapies that adapt to individual physiological responses in real-time [13].
The economic and environmental considerations also differ substantially. Pharmaceutical treatments typically require continuous manufacturing, distribution, and administration, creating ongoing costs and environmental impact from production and waste [1]. Bioelectronic implants, particularly battery-free devices powered by wireless technologies, could provide long-term treatment with minimal maintenance, potentially offering cost efficiencies over chronic drug therapies, especially for lifelong conditions [6] [1].
Clinical Applications and Comparative Performance Data
Diabetes Management: Closed-Loop Insulin Delivery
The most advanced and clinically validated application of closed-loop technology is in managing Type 1 Diabetes (T1D) through Hybrid Closed-Loop (HCL) systems and Advanced Hybrid Closed-Loop (AHCL) systems. These systems combine a continuous glucose monitor (CGM), an insulin pump, and a control algorithm that automates insulin delivery based on real-time glucose readings [59] [60]. The following table summarizes key performance metrics from clinical studies comparing these systems with open-loop alternatives:
Table 1: Performance Comparison of Closed-Loop vs. Open-Loop Systems in Type 1 Diabetes
| System Type | Study Population | Time in Range (TIR) % | HbA1c (%) | Hypoglycemia Events | Ketoacidosis Events |
|---|---|---|---|---|---|
| Hybrid Closed-Loop | 7,088 patients (ages 2-20) | 64% | 7.34% | Lower rate of hypoglycemic coma (0.62 vs. 0.91 per 100 patient-years) | Higher rate (1.74 vs. 0.96 per 100 patient-years) [59] |
| Open-Loop | 6,834 patients (ages 2-20) | 52% | 7.50% | Reference rate: 0.91 per 100 patient-years | Reference rate: 0.96 per 100 patient-years [59] |
| Advanced HCL | 30-year-old female with intellectual disability | Improved from <50% to 70-80% | Improved from 9.0-10.0% to <7.0% | No increase | Eliminated hospitalizations for ketoacidosis [61] |
The performance advantage of closed-loop systems is particularly evident in challenging clinical scenarios. A case study involving a patient with T1D and intellectual disability demonstrated remarkable improvement after transitioning from open-loop to closed-loop systems. With a sensor-augmented pump (open-loop), the patient consistently had HbA1c levels of 9.0-10.0% and experienced frequent diabetic ketoacidosis requiring hospitalization. After implementing an AHCL system (MiniMed 780G), her time in range improved to 70-80%, HbA1c dropped below 7.0%, and she had no further hospitalizations for ketoacidosis over two years [61].
Neurological and Inflammatory Applications
Beyond diabetes, closed-loop bioelectronic systems are advancing rapidly in neurological and inflammatory disorders. Closed-loop deep brain stimulation (DBS) systems for Parkinson's disease, such as Medtronic's Percept with Brainsense, can record neural signals while providing stimulation, allowing the device to adapt therapy based on real-time brain activity [13]. Similarly, closed-loop spinal cord stimulation (SCS) systems for pain management modulate electrical signals based on physiological feedback, enhancing therapeutic precision [13].
The emerging frontier involves autonomic nervous system modulation for inflammatory conditions. Early research demonstrates the potential for closed-loop vagus nerve stimulation to regulate immune function and inflammation by responding to real-time physiological and molecular signals [13]. While still primarily in research phases, these systems represent the next evolution toward dynamically adaptive bioelectronic therapies for conditions like rheumatoid arthritis and other inflammatory disorders.
Experimental Protocols and Methodologies
Clinical Validation of Hybrid Closed-Loop Systems
Robust clinical trial methodologies have been developed to validate the safety and efficacy of closed-loop systems. The following experimental protocol is representative of recent pivotal trials:
Study Design: Randomized parallel-group or crossover trials comparing closed-loop systems against standard care (sensor-augmented pump therapy or multiple daily injections) [60].
Participants: Recruitment across diverse age groups (pediatric to geriatric) with Type 1 diabetes duration of at least one year. Sample sizes typically range from approximately 100 to over 200 participants across multiple centers [60].
Intervention: Participants are randomized to use either hybrid closed-loop systems or control therapy for a specified period (typically 12-26 weeks). Closed-loop systems include devices such as MiniMed 780G, Tandem Control-IQ, or CamAPS FX [60].
Primary Outcomes:
- Change in Time in Range (TIR): Percentage of time sensor glucose values remain between 70-180 mg/dL
- HbA1c change from baseline
- Hypoglycemia metrics: Time below range (<70 mg/dL and <54 mg/dL) and severe hypoglycemia event rates [60]
Secondary Outcomes:
- Glycemic variability (coefficient of variation)
- Patient-reported outcomes (quality of life, sleep quality, fear of hypoglycemia)
- Safety endpoints (diabetic ketoacidosis events, device-related adverse events) [60]
Statistical Analysis: Mixed-effects models adjusting for baseline values, with sensitivity analyses to test robustness of findings. The studies typically power to detect clinically meaningful differences in TIR (≥5 percentage points) [60].
Preclinical Development of Novel Closed-Loop Bioelectronics
The development cycle for innovative closed-loop bioelectronic devices involves sophisticated preclinical testing protocols:
In Vitro Characterization:
- Electrochemical profiling of biosensors using techniques like cyclic voltammetry and electrochemical impedance spectroscopy to assess sensitivity, selectivity, and stability [56]
- Accelerated aging studies to predict long-term reliability and failure modes of implantable components [6]
- Biocompatibility testing per ISO 10993 standards to evaluate material safety and foreign body response [6]
In Vivo Animal Studies:
- Proof-of-concept demonstrations in relevant disease models (e.g., rodent models of epilepsy, inflammation, or metabolic disorders)
- Dose-response characterization to establish therapeutic windows for electrical stimulation parameters
- Chronic implantation studies to assess device stability, foreign body reaction, and long-term therapeutic efficacy [6] [56]
Signal Processing and Algorithm Development:
- Feature extraction from recorded physiological signals to identify biomarkers predictive of disease states
- Control algorithm refinement using machine learning approaches to optimize stimulation parameters
- System integration testing to validate seamless operation between sensing, processing, and stimulation components [56] [13]
Technological Infrastructure and Research Reagents
The development and implementation of closed-loop systems require specialized technological components and research tools. The following table details essential elements of the closed-loop research and development toolkit:
Table 2: Essential Research Tools for Closed-Loop System Development
| Component Category | Specific Tools/Technologies | Function in Research & Development |
|---|---|---|
| Biosensing Modalities | Chemical sensors (glucose, cytokines), Electrophysiological sensors (neural signals), Physical sensors (pressure, temperature) [56] | Detect and quantify physiological parameters of interest for feedback control |
| Control Algorithms | Proportional-Integral-Derivative (PID) controllers, Model Predictive Control (MPC), Artificial Pancreas algorithms, Neural signal decoding algorithms [60] [13] | Process sensor data and compute appropriate therapeutic responses in real-time |
| Therapeutic Actuators | Microfluidic drug delivery systems, Multi-electrode arrays for neural stimulation, Insulin pumps, Neuromodulation electrodes [56] [1] | Deliver precise therapeutic interventions (electrical stimulation or drug delivery) based on algorithm commands |
| Advanced Materials | Conducting polymers (PEDOT:PSS), Graphene-based electrodes, MXenes, Soft hydrogel interfaces [6] [1] | Improve biocompatibility, signal fidelity, and device longevity at the tissue-device interface |
| Data Sources for Outcomes Research | Diabetes Prospective Follow-up (DPV) Registry, MarketScan databases, MEPS, PHARMetrics [59] [57] | Provide real-world evidence for comparative effectiveness and safety outcomes |
Signaling Pathways in Closed-Loop Bioelectronic Medicine
The therapeutic efficacy of closed-loop bioelectronic systems relies on their ability to interface with and modulate specific physiological pathways. Two particularly important signaling circuits are the inflammatory reflex and the neural circuits involved in deep brain stimulation for movement disorders. The inflammatory reflex pathway represents a key mechanism through which bioelectronic devices can modulate immune function:
Future Directions and Research Challenges
Despite significant advances, closed-loop bioelectronic medicine faces several important challenges that represent opportunities for future research and development. Long-term reliability and stability of implantable devices remains a critical hurdle, with issues including foreign body reaction, material degradation, and signal drift over time impacting device performance [6]. The field is addressing these challenges through development of softer, more flexible bioelectronic interfaces that better match the mechanical properties of biological tissues, thereby reducing inflammation and improving long-term integration [6] [1].
Another significant challenge involves algorithm refinement and personalization. Current systems demonstrate variable effectiveness across different individuals, highlighting the need to identify predictors of treatment response and develop adaptive algorithms that can learn and optimize therapy for each patient [60] [13]. Research is increasingly focusing on multi-input systems that incorporate diverse data streams (neural signals, hormone levels, cytokine concentrations) to create more comprehensive physiological models and improve control strategies [13].
Access and equity represent additional concerns, as current closed-loop technologies remain expensive and inaccessible to many patient populations. Addressing these disparities will require not only cost reduction but also development of systems appropriate for diverse healthcare environments and populations with varying technical capabilities [60]. Future research directions include fully closed-loop systems requiring minimal user input, bioresorbable electronics that eliminate the need for surgical extraction, and novel non-invasive approaches using technologies like focused ultrasound for autonomic neuromodulation [6] [13].
The convergence of bioelectronic medicine with pharmaceutical outcomes research methodologies promises to accelerate the development and optimization of closed-loop systems. By applying rigorous outcomes assessment frameworks—including cost-effectiveness analyses, quality-of-life measurements, and real-world evidence generation—researchers can more comprehensively demonstrate the value of these innovative therapies and guide their appropriate integration into healthcare systems [57] [58].
The evolution of bioelectronic medicine represents a fundamental shift from pharmaceutical-dominated therapies toward electronically mediated treatments that modulate neural circuits. This emerging field uses miniaturized electronic devices to interface with the body's electrically active tissues, offering targeted therapeutic interventions for conditions ranging from chronic inflammation to movement disorders [6] [62]. Unlike conventional pharmaceuticals that act systemically and often cause off-target effects, bioelectronic therapies achieve precision through localized electrical modulation of specific neural pathways, enabling reversible, adjustable treatment with potentially fewer side effects [62] [1].
A critical barrier to the long-term success of implantable bioelectronic devices has been the mechanical mismatch between traditional rigid electronic components and soft, dynamic biological tissues. This mismatch can trigger foreign body reactions, inflammation, fibrosis, and eventual device failure [6] [63]. In response, material science has pioneered a new generation of soft, flexible, and biocompatible electronics engineered to seamlessly integrate with biological systems. These innovations promise to enhance device reliability (consistent function without failure) and stability (maintenance of properties over time), which are crucial for widespread clinical adoption [6]. This guide objectively compares the performance of these emerging soft electronic materials against conventional alternatives, providing researchers and drug development professionals with experimental data to evaluate their potential in complementing or replacing pharmaceutical outcomes.
Comparative Performance Analysis of Electronic Materials
The transition toward soft electronics necessitates a clear understanding of how these new materials perform relative to established options. The following tables summarize key quantitative comparisons based on recent experimental studies.
Table 1: Comparison of Mechanical and Biocompatibility Properties
| Material Type | Representative Materials | Young's Modulus (Approx.) | Stretchability | Biocompatibility & Foreign Body Response |
|---|---|---|---|---|
| Soft/Elastomeric Electronics | DPPT-TT/BIIR blend [63] | ~100 kPa - 1 MPa [63] | Up to 100% strain without cracking [63] | No adverse effects on cell viability; no major inflammatory response in vivo [63] |
| Conventional Rigid Electronics | Silicon, Metals (e.g., Pt, Ir) [63] | ~10 GPa - 100 GPa | Typically <5% strain [6] | Can lead to microinjury, chronic inflammation, and fibrosis [63] [1] |
| Conductive Polymers | PEDOT:PSS [1] | ~1 MPa - 1 GPa | Moderate | Enhanced biocompatibility; reduced impedance [1] |
Table 2: Comparison of Electrical Performance and Stability
| Material Type | Representative Materials | Key Electrical Metric | Performance Under Strain | Stability in Physiological Conditions |
|---|---|---|---|---|
| Soft Organic Field-Effect Transistors (sOFETs) | DPPT-TT/BIIR blend [63] | Field-effect mobility maintained across blend ratios [63] | Negligible change in mobility under 0-100% strain [63] | Stable operation demonstrated in physiological conditions [63] |
| Rigid Inorganic Electronics | Silicon-based transistors | High intrinsic mobility | Performance degrades or fails under minimal strain | Stable but requires hermetic packaging; failure if packaged is compromised [1] |
| Soft Organic Electrochemical Transistors (sOECTs) | PEDOT-based devices [63] | High transconductance | Operate under strain | Prone to high OFF currents and crosstalk; risk of undesired neural activation [63] |
Table 3: Emerging Sustainable and Edible Electronic Materials
| Material Category | Example Components | Primary Function | Key Findings & Performance |
|---|---|---|---|
| Edible Electronics Substrates | Starch, proteins, polysaccharides, food waste (e.g., fruit peels) [64] | Biodegradable substrate/sensor | LC sensors function after exposure to artificial saliva; pH-sensitive films change color to monitor freshness [64] |
| Sustainable Energy-Storing Material | Peptide-plastic hybrid nanoribbons [65] | Ferroelectric/Piezoelectric charge storage | Matches performance of standard polymer PVDF; operates at low voltages [65] |
Experimental Protocols for Evaluating Soft Electronics
To ensure the validity and reproducibility of data, researchers follow standardized experimental protocols for characterizing new soft electronic materials. The methodology for testing the DPPT-TT/BIIR blend transistor, a representative example of a high-performance soft electronic device, is detailed below [63].
Material Synthesis and Fabrication
- Film Preparation: The semiconducting polymer (DPPT-TT) and medical-grade elastomer (Bromoisobutyl-isoprene rubber, BIIR) are blended in a 3:7 weight ratio using a solution-processing technique. This ratio was optimized to balance electrical performance and mechanical stretchability [63].
- Vulcanization: The blend film is chemically crosslinked via a vulcanization process. This involves adding sulfur (crosslinker), dipentamethylenethiuram tetrasulfide (accelerator), and stearic acid (initiator), followed by a thermal treatment. This process enhances the film's elasticity and mechanical integrity without disrupting the conjugated structure of the semiconductor [63].
- Electrode Fabrication: Biocompatible and stretchable electrodes are created using a dual-layer metallization of silver (Ag) for electrical contact and gold (Au) for corrosion resistance [63].
Mechanical and Electrical Characterization
- Stress-Strain Tests: The vulcanized blend film is subjected to uniaxial tensile stress to measure its crack-onset strain and elongation at break. The film's Derjaguin–Muller–Toporov (DMT) modulus is mapped using atomic force microscopy (AFM) to confirm its similarity to human tissue [63].
- Electrical Performance under Deformation: Transistors are fabricated on stretchable substrates. Their electrical characteristics, including field-effect mobility and ON/OFF ratio, are measured while the substrate is statically stretched to various strains (e.g., 0%, 50%, 100%) and during cyclic stretching (e.g., 1,000 cycles at 100% strain) [63].
- Surface Morphology Imaging: Conductive AFM (C-AFM) is used to visualize the alignment and integrity of the semiconducting nanofibre network within the elastomer matrix under applied strain [63].
Biocompatibility Assessment
- In Vitro Testing: Human dermal fibroblasts and macrophages are cultured with the material. Cell viability, proliferation, and migration are assessed using standard assays (e.g., MTT for viability) to ensure no adverse effects [63].
- In Vivo Testing: The device is subcutaneously implanted in an animal model (e.g., mice). After a set period, the implant site is histologically examined for signs of major inflammatory response, tissue damage, or fibrosis, confirming biocompatibility [63].
Experimental Workflow for Soft Electronics
The Scientist's Toolkit: Essential Research Reagents and Materials
Developing and testing soft, biocompatible electronics requires a specialized set of materials. The following table catalogs key reagents and their functions in this field.
Table 4: Essential Research Materials for Soft Bioelectronic Development
| Material/Reagent | Function in Research | Specific Example & Rationale |
|---|---|---|
| Medical-Grade Elastomers | Provides a soft, stretchable, and biocompatible matrix for the electronic component. | Bromo isobutyl–isoprene rubber (BIIR): Meets ISO 10993 biocompatibility standards; offers shock absorption and biofluid resistance [63]. |
| Semiconducting Polymers | Forms the active layer for charge transport in transistors. | DPPT-TT: A donor-acceptor polymer that forms a nanofibrous network within the BIIR matrix, maintaining conductivity under strain [63]. |
| Conductive Polymers | Used for creating soft, low-impedance electrodes for tissue interfacing. | PEDOT:PSS: Mixed ionic/electronic conductor that reduces voltage overshoot during stimulation, improving safety and energy efficiency [1]. |
| Crosslinking Agents | Enhances the mechanical robustness and elasticity of polymer blends. | Sulfur/DPTT/Stearic Acid: A vulcanization system that crosslinks BIIR chains without disrupting the semiconductor's conjugation [63]. |
| Biocompatible Metallization | Creates corrosion-resistant, conductive traces and electrodes. | Dual-layer Ag/Au: Silver provides excellent conductivity, while a gold outer layer protects against corrosion from biofluids [63]. |
| Natural Polymer Substrates | Serves as biodegradable and edible substrates for transient electronics. | Starch, Cellulose, Gelatin: Derived from food-grade substances; enable the creation of ingestible sensors and devices [64]. |
Signaling Pathways and Therapeutic Mechanisms
Bioelectronic medicine operates by modulating the body's innate neural signaling pathways. A prime example is the inflammatory reflex, a key circuit targeted for treating autoimmune diseases.
Cholinergic Anti-inflammatory Pathway
This pathway illustrates how bioelectronic devices like vagus nerve stimulators (VNS) achieve therapeutic effects. By electrically stimulating the vagus nerve, these devices artificially activate this reflex, leading to a reduction in pro-inflammatory cytokines like tumor necrosis factor (TNF) [13] [62]. This offers a targeted alternative to broad-acting immunosuppressive drugs. The efficacy of this approach has been demonstrated in clinical trials for rheumatoid arthritis and Crohn's disease, showcasing the potential of bioelectronic medicine to treat conditions traditionally managed by pharmaceuticals [62].
The data and comparisons presented in this guide underscore a significant trend: innovations in soft, flexible, and biocompatible electronics are directly addressing the core challenges of reliability and stability that have long hindered the broader application of bioelectronic medicine [6]. Materials like the DPPT-TT/BIIR blend demonstrate that it is possible to achieve mechanical compatibility with human tissues without sacrificing electrical performance, leading to improved device longevity and reduced foreign body response [63].
For researchers and drug development professionals, these advancements signal a pivotal moment. The convergence of material science and neuromodulation is creating a new therapeutic category capable of delivering precise, reversible, and personalized treatments. As these technologies mature, they will not only provide alternatives to pharmaceuticals but also enable entirely new "closed-loop" systems that diagnose, monitor, and treat disease in real-time [13] [62]. This progress firmly establishes bioelectronic medicine as a complementary and, in some cases, superior modality to conventional pharmacotherapies, particularly for conditions where targeted intervention and minimal systemic side effects are paramount.
Navigating Challenges: Reliability, Cost, and Adoption Barriers in Bioelectronic Medicine
Ensuring Long-Term Device Reliability and Stability in the Biological Environment
In the evolving landscape of therapeutic interventions, bioelectronic medicine (BEM) presents a paradigm shift from pharmaceutical-based treatments by using miniaturized electronic devices to interface with the body's electrically active tissues [6]. Unlike pharmaceuticals, which act through systemic chemical interactions, bioelectronic devices achieve specificity through precise electrical modulation of neural circuits and organs [21]. However, the long-term reliability and stability of these implanted devices present distinct challenges that must be critically evaluated against the established frameworks of pharmaceutical outcomes research.
For researchers and drug development professionals evaluating these technologies, understanding the fundamental concepts of device performance is crucial. Reliability refers to the probability that a bioelectronic device will function as intended without failure over a specified period under expected operating conditions, often quantified using metrics such as mean time between failures (MTBF) [6]. Stability denotes the device's ability to maintain its functional and structural properties over time, including resistance to environmental and biological fluctuations [6]. These concepts form the critical evaluation parameters when comparing bioelectronic medicine with pharmaceutical interventions.
Comparative Analysis: Bioelectronic Medicine vs. Pharmaceutical Outcomes
Fundamental Divergences in Therapeutic Approach
Table 1: Core Distinctions Between Bioelectronic and Pharmaceutical Therapeutic Approaches
| Evaluation Parameter | Bioelectronic Medicine | Pharmaceutical Interventions |
|---|---|---|
| Mechanism of Action | Electrical modulation of neural pathways and electrically active tissues [6] | Chemical interactions with biological targets via systemic distribution [21] |
| Specificity | High potential for anatomical targeting through electrode placement and stimulation parameters [6] | Limited by molecular specificity and distribution patterns, often leading to off-target effects [21] |
| Adaptability | Programmable systems capable of closed-loop adjustment based on physiological feedback [6] | Generally fixed dosing regimens with limited real-time adjustability [21] |
| Reversibility | Immediate cessation upon stimulation termination | Dependent on pharmacokinetic profiles and elimination half-lives |
| Material Concerns | Device encapsulation, electrode corrosion, mechanical failure [6] | Chemical stability, shelf life, metabolic pathways |
| Outcomes Measurement | Direct neural recording, physiological parameter monitoring [6] | Biomarker assessment, clinical symptom scales [66] |
Outcomes Research Methodologies and Evidence Generation
Table 2: Outcomes Research Frameworks in Bioelectronic Medicine and Pharmaceuticals
| Research Dimension | Bioelectronic Medicine | Pharmaceuticals |
|---|---|---|
| Primary Evidence Source | Controlled clinical trials of devices with engineering reliability data [6] | Randomized controlled trials (RCTs) with placebo/comparator arms [66] |
| Real-World Evidence | Device longevity reports, failure mode analysis, explant studies [6] | Phase IV studies, observational databases, pharmacovigilance systems [67] [58] |
| Economic Evaluation | Device cost, implantation procedure, replacement surgery, programming time [58] | Drug pricing, administration costs, side effect management [58] |
| Timeframe Assessment | Accelerated aging tests, predictive modeling of device lifespan [6] | Long-term extension studies, registry data [67] |
| Failure Mode Analysis | Material degradation, lead fracture, battery depletion, foreign body reaction [6] | Loss of efficacy, adverse events, drug interactions, tolerance development [68] |
Experimental Approaches to Assessing Device Reliability
Standardized Testing Protocols for Bioelectronic Devices
Accelerated Aging Protocols: Simulating long-term implantation through elevated temperature and humidity exposure based on the Arrhenius model, which predicts device lifespan by measuring performance degradation under stressed conditions [6]. Testing includes cyclical mechanical stress to replicate bodily movements and thermal cycling between 25°C and 45°C to simulate physiological variations.
Electrochemical Impedance Spectroscopy (EIS): Regular monitoring of electrode-tissue interface integrity using frequency response analysis. This method detects increasing impedance that may indicate fibrosis or electrode corrosion, with measurements typically taken across a frequency range of 1 Hz to 100 kHz [6].
Chronic Stimulation Testing: Continuous pulsed stimulation at levels exceeding typical clinical parameters (e.g., 2-4× threshold current) for minimum 30-day periods to assess electrode stability under operational load. Charge density limits are maintained below material-specific thresholds (typically 30-50 μC/cm² for platinum electrodes) to prevent dissolution [6].
Foreign Body Reaction (FBR) Assessment: Histological evaluation of tissue integration post-explantation, quantifying collagen capsule thickness, inflammatory cell density (macrophages, lymphocytes), and neovascularization. Current research focuses on surface modifications that reduce capsule thickness below 50μm, significantly improving long-term signal fidelity [21].
Quantitative Reliability Data for Bioelectronic Interfaces
Table 3: Experimental Reliability Metrics for Bioelectronic Device Components
| Device Component | Testing Methodology | Performance Metrics | Current Benchmark Data | Failure Threshold |
|---|---|---|---|---|
| Conventional Metal Electrodes | Cyclic voltammetry, impedance monitoring | Charge injection capacity, impedance stability | 0.8-1.2 mC/cm² initial; >50% impedance increase in 6 months [6] | Voltage transients >±1.5V, impedance increase >100% |
| Conducting Polymer Electrodes | Accelerated aging in PBS, continuous stimulation | Capacitance retention, adhesion strength | 15-25 mC/cm² initial; >80% capacitance retention after 10⁶ cycles [21] | Delamination, >30% capacitance loss |
| Hermetic Packaging | Helium leak testing, moisture ingress monitoring | Water vapor transmission rate | <5×10⁻⁴ g/m²/day at 37°C [6] | Moisture sensor activation, functionality loss |
| Flexible Interconnects | Mechanical flex testing, resistance monitoring | Resistance change during cycling | <5% resistance change after 100,000 bends at 10mm radius [6] | Open circuit, resistance increase >20% |
| Soft Encapsulation | Adhesion testing, barrier property evaluation | Interface adhesion strength | >10 J/m² to substrate after 6 months immersion [6] | Delamination, electrical failure |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Critical Research Materials for Device Reliability Studies
| Research Material | Function in Reliability Testing | Key Performance Characteristics | Representative Examples |
|---|---|---|---|
| Phosphate Buffered Saline (PBS) | Simulates ionic biological environment for in vitro testing | pH stability (7.4), ionic concentration matching extracellular fluid | Thermo Fisher (catalog #10010023), Sigma-Aldrich (catalog #P3813) |
| Electrochemical Workstation | Measures electrode-electrolyte interface properties | Frequency range (μHz-MHz), current resolution (pA) | Biologic VSP-300, Ganny Reference 600+ |
| Accelerated Test Chambers | Environmental stress application for lifespan prediction | Temperature control (±0.5°C), humidity control (±3% RH) | Thermotron 3800, Cincinnati Sub-Zero Z-32 |
| Histological Staining Kits | Tissue response evaluation post-explantation | Specificity for collagen, inflammatory cells | Masson's Trichrome (collagen), H&E (cellularity), Iba1 (macrophages) |
| Flex Testing Systems | Mechanical durability assessment of flexible components | Cycle rate, bend radius control, position accuracy | Instron 5900 Series, Tinus Olsen Flex tester |
| Conducting Polymers | Advanced electrode materials with enhanced interfaces | Mixed ionic/electronic conductivity, mechanical compliance | PEDOT:PSS, polyaniline, polypyrrole [21] |
Material Science Innovations for Enhanced Device Stability
Advanced Materials Addressing Biological Environment Challenges
The shift toward soft and flexible bioelectronics represents a fundamental innovation addressing the mechanical mismatch between traditional rigid implants and dynamic biological tissues [6]. This materials revolution encompasses several key developments:
Conducting Polymers: Materials such as PEDOT:PSS offer mixed ionic/electronic conductivity, enabling more efficient charge transfer at the tissue-device interface while providing mechanical properties closer to natural tissues [21]. These polymers demonstrate reduced impedance compared to traditional metal electrodes, allowing for further miniaturization while maintaining signal fidelity [21].
Liquid Metal Composites: Gallium-based alloys embedded in elastomeric matrices create stretchable conductors that maintain conductivity at >500% strain, addressing the critical challenge of mechanical compliance in dynamic biological environments [6].
Bioresorbable Materials: Electronic systems fabricated from materials that safely dissolve after a designated operational period eliminate the need for surgical extraction and reduce long-term complication risks [6]. These materials are engineered to maintain functionality during the therapeutic window while exhibiting predictable degradation profiles.
Experimental Data on Novel Material Performance
Graphene and 2D Materials: Ultra-thin graphene-based electrodes demonstrate exceptional stability with less than 10% signal variation during chronic implantation in rodent models, attributed to their chemical inertness and minimal mechanical footprint [21].
Hydrogel Coatings: Swellable hydrogel interfaces reduce foreign body response by 60% compared to uncoated controls, as quantified by reduced macrophage density and thinner collagen capsules in porcine models [6].
MXene Electrodes: Two-dimensional transition metal carbides/nitrides achieve charge injection capacities exceeding 2 mC/cm² while maintaining stability over 10 million stimulation cycles in accelerated testing [21].
Integrated Assessment Framework for Therapeutic Decision-Making
Comparative Outcomes Analysis: Bioelectronic vs. Pharmaceutical Interventions
For researchers and development professionals evaluating therapeutic strategies, a comprehensive understanding of both approaches requires examining their respective evidence generation frameworks:
Pharmaceutical Outcomes Validation: Relies heavily on randomized controlled trials (RCTs) with strict methodological controls to establish efficacy [66]. However, these studies often suffer from limited generalizability due to restrictive patient selection criteria [66]. Effectiveness studies (pragmatic trials) attempt to bridge this gap by evaluating treatments under real-world conditions with more diverse patient populations, though they introduce methodological challenges including confounders that increase variance and reduce signal-to-noise ratios [66].
Bioelectronic Medicine Validation: Requires dual assessment of both therapeutic efficacy and device reliability [6]. While early feasibility studies may focus on technical performance, comprehensive outcomes assessment must integrate traditional clinical endpoints with engineering reliability metrics. This dual requirement creates a more complex evidence generation pathway but offers the potential for continuous optimization through software updates and algorithmic improvements without device replacement.
Future Directions: Closed-Loop Systems and Personalized Bioelectronic Therapies
The convergence of advanced materials, miniaturized electronics, and intelligent control systems points toward next-generation bioelectronic therapies with enhanced reliability profiles [6]. Closed-loop systems that continuously monitor physiological signals and automatically adjust stimulation parameters represent a fundamental advancement beyond static pharmaceutical dosing regimens [6]. These systems potentially address the critical challenge of inter-patient variability that often undermines pharmaceutical effectiveness [66].
Battery-free devices powered through wireless energy transfer or bioenergy harvesting eliminate a primary failure point in current implants while reducing environmental impact through decreased replacement frequency [6]. Similarly, the development of standardized core outcome sets for bioelectronic interventions—mirroring advancements in pharmaceutical outcomes research—will enable more meaningful cross-study comparisons and accelerate therapeutic optimization [68].
For the research community, the ongoing challenge remains balancing innovation with reliability assurance, requiring interdisciplinary collaboration across materials science, electrical engineering, clinical medicine, and outcomes research methodology. Only through this integrated approach can bioelectronic medicine fulfill its potential as a robust therapeutic modality complementing and extending beyond conventional pharmaceutical interventions.
Addressing High Capital and Procedural Costs and Reimbursement Hurdles
Bioelectronic medicine represents a paradigm shift in therapeutic interventions, moving from broad-acting pharmaceuticals to targeted neuromodulation of specific neural circuits [31]. While this approach offers the potential for precise treatment of chronic conditions with reduced systemic side effects, its path to widespread clinical adoption is fraught with significant economic challenges [10]. The field must navigate the complex landscape of high development costs for sophisticated implantable and wearable devices, substantial procedural expenses for implantation surgeries, and inconsistent reimbursement frameworks across global healthcare systems [10]. These financial barriers are particularly pronounced when compared to established pharmaceutical development pathways, creating a critical juncture for researchers, developers, and healthcare policymakers. This analysis examines the cost structures and reimbursement hurdles facing bioelectronic medicine, providing comparative data with pharmaceutical alternatives and outlining methodological frameworks for evaluating their economic and therapeutic value in the context of chronic disease management.
Cost Structure Analysis: Bioelectronic Medicine vs. Pharmaceuticals
The economic models for bioelectronic medicine and pharmaceuticals differ substantially in their allocation of expenses across the development and deployment lifecycle. Bioelectronic medicine incurs significant upfront costs driven by sophisticated device engineering, materials science innovation, and surgical implantation procedures, whereas pharmaceuticals typically distribute costs more evenly across discovery, clinical trials, and ongoing manufacturing [10]. The table below summarizes key comparative cost components:
Table 1: Comparative Cost Structures of Bioelectronic Medicine and Pharmaceuticals
| Cost Component | Bioelectronic Medicine | Traditional Pharmaceuticals |
|---|---|---|
| R&D Expenses | High (device engineering, materials science, biocompatibility testing) [31] [10] | High (compound screening, preclinical studies) |
| Manufacturing | Complex micro-fabrication; specialized facilities [31] | Chemical synthesis/biologics production; scaling challenges |
| Procedure/Administration | Surgical implantation costs; specialist fees [10] | Minimal (oral) to moderate (injectable/infusion) |
| Long-term Management | Device maintenance, potential replacement surgeries [31] | Chronic prescription refills, monitoring for side effects |
| Reimbursement Landscape | Inconsistent coverage; device-specific approval processes [10] | Established formularies; tiered pricing models |
Market analysis indicates the bioelectronic medicine sector was valued at $23.54 billion in 2024 and is projected to reach $33.59 billion by 2030, growing at a compound annual growth rate (CAGR) of 6.10% [10]. This growth occurs despite the economic challenges, reflecting the therapeutic potential of these technologies. A primary economic barrier includes the "high cost of devices and limited reimbursement coverage," particularly for advanced implantable devices like neurostimulators and defibrillators that involve "complex manufacturing processes and high R&D investments" [10]. These economic challenges are most pronounced in low- and middle-income countries, where such treatments often "remain out of reach for a significant portion of the population" [10].
Comparative Clinical Outcomes and Economic Value
When evaluating cost-effectiveness, bioelectronic medicine demonstrates distinctive value propositions in specific therapeutic areas. The following table compares clinical outcomes and associated economic impacts for conditions treated with both modalities:
Table 2: Clinical Outcome and Economic Impact Comparison
| Condition | Therapeutic Approach | Clinical Outcomes | Economic Impact |
|---|---|---|---|
| Rheumatoid Arthritis | Vagus nerve stimulation (SetPoint Medical) | Targeted neuroimmunomodulation; reduced systemic side effects [31] [69] | FDA-approved device; initial investment vs. potential long-term biologic drug savings |
| Crohn's Disease | Non-invasive auricular vagus nerve stimulation (taVNS) plus ustekinumab | Case report: mucosal healing and clinical remission achieved [70] | Combination therapy potential; reduced medication dependence over time |
| Heart Failure with Reduced Ejection Fraction (HFrEF) | Baroreflex Activation Therapy (BAT) | 94% decrease in HF hospitalizations; improved quality of life [70] | Significant reduction in hospitalization costs offsetting device investment |
| Treatment-Resistant Depression | Vagus nerve stimulation | Reduced symptom burden in medication-resistant cases | Avoided costs of repeated medication trials and inpatient care |
| Chronic Pain | Spinal cord stimulation | Reduced opioid dependence; functional improvement [31] | Decreased medication costs; improved productivity |
Recent research provides compelling data on specific economic and clinical outcomes. Baroreflex Activation Therapy (BAT) for heart failure with reduced ejection fraction demonstrated a "94% decrease of HF hospitalizations 12-months after implantation" alongside significant improvements in quality of life measures [70]. This reduction in acute care utilization represents a substantial economic value that partially offsets the initial device and implantation costs. Similarly, a case report on transcutaneous auricular vagus nerve stimulation (taVNS) for pediatric Crohn's disease documented successful long-term use in combination with biologics, resulting in "complete mucosal healing (endoscopic and histologic healing)" [70]. The integration of bioelectronic approaches with pharmaceutical regimens suggests potential for optimized therapeutic efficacy with possible dose reduction of expensive biologic agents over time.
Experimental Framework for Economic and Outcomes Research
Methodology for Cost-Effectiveness Analysis
Research into the economic value of bioelectronic medicine requires standardized methodologies to enable valid comparisons across therapeutic modalities. The following experimental protocol provides a framework for generating comparable data:
Study Design: Prospective, randomized controlled trials or propensity-matched observational studies comparing bioelectronic interventions against standard pharmaceutical care.
Population Definition: Clearly defined patient cohorts with specific chronic conditions (e.g., rheumatoid arthritis inadequate responders to biologics, treatment-resistant depression).
Data Collection Parameters:
- Direct medical costs: Device/implantation, medications, hospitalizations, procedures
- Indirect costs: Productivity measures, caregiver burden
- Clinical outcomes: Disease-specific metrics, quality of life measures, adverse events
- Healthcare utilization: Hospital days, emergency visits, outpatient consultations
Analysis Methods:
- Cost-effectiveness analysis (CEA): Calculation of incremental cost-effectiveness ratios (ICERs)
- Budget impact modeling: Projected system-level financial impact
- Quality-adjusted life years (QALYs): Standardized utility measures for cross-condition comparison
Time Horizon: Minimum 12-month assessment with modeling for device longevity (typically 5-10 years for implants) versus chronic pharmaceutical treatment.
Methodology for Comparative Efficacy Studies
Objective Comparison of bioelectronic versus pharmaceutical outcomes requires rigorous experimental design:
Protocol 1: Neuroimmunomodulation Assessment
- Objective: Quantify inflammatory biomarker response to vagus nerve stimulation versus biologic therapy [70]
- Methods: Serial measurement of TNF-α, IFN-γ, IL-6 in response to controlled stimulation versus drug dosing
- Controls: Sham stimulation, standard of care medications
- Outcomes: Magnitude and duration of biomarker suppression, side effect profile
Protocol 2: Long-term Therapeutic Durability
- Objective: Compare sustainability of treatment response over 24-month period
- Methods: Regular assessment of clinical symptoms, biomarker levels, and functional status
- Analysis: Time-to-treatment-failure, dose escalation requirements, rescue medication use
Research Reagent Solutions and Methodological Tools
The following table details essential research tools and methodologies for conducting comparative studies in bioelectronic medicine:
Table 3: Essential Research Methodologies and Tools for Comparative Studies
| Research Tool/Methodology | Function/Application | Specific Examples/Parameters |
|---|---|---|
| Multi-contact Cuff Electrodes | Selective peripheral nerve stimulation for targeted therapy [70] | Optimization of stimulation waveforms; measurement of neural target engagement |
| Computational Nerve Modeling | Prediction of neural responses to stimulation parameters; reduces animal experimentation [70] | ASCENT pipeline; 3D anatomy reconstruction of nerves and cuff geometries |
| Inflammatory Biomarker Panels | Quantification of immunomodulatory treatment effects [70] | TNF-α, IFN-γ monitoring; correlation with clinical outcomes |
| Heart Rate Variability Analysis | Assessment of autonomic nervous system function in response to neuromodulation [70] | Time- and frequency-domain analysis; correlation with inflammatory markers |
| Quality of Life Metrics | Standardized measurement of patient-reported outcomes across modalities [70] | Minnesota Living with Heart Failure Questionnaire (MLHFQ); other validated instruments |
| Activation Threshold Mapping | Determination of optimal stimulation parameters for selective neural targeting [70] | Single-fiber response analysis; precision stimulation protocols |
Reimbursement Strategy Development and Market Access
The establishment of sustainable reimbursement pathways represents a critical challenge for bioelectronic medicine. Current analysis identifies that "reimbursement frameworks for bioelectronic therapies are inconsistent across regions," and insurance frequently "does not fully cover the cost of treatment, making it financially burdensome for patients" [10]. This reimbursement challenge is quantified by data showing that "out-of-pocket medical expenses push approximately 100 million people into extreme poverty every year" [10], highlighting the systemic nature of this barrier. To address these challenges, successful market access strategies should incorporate several evidence-based components:
Value-Based Contracting: Development of outcomes-linked reimbursement models that share risk between manufacturers and payers based on real-world performance metrics.
Staged Reimbursement Pathways: Initial coverage for treatment-resistant populations where bioelectronic interventions demonstrate clear superiority, followed by expanded indications based on accumulating evidence.
Economic Argumentation Frameworks: Comprehensive cost-effectiveness models that capture both direct medical savings and indirect benefits such as productivity gains and reduced caregiver burden.
Procedure Code Establishment: Advocacy for specific device implantation and management codes that appropriately reflect the resource requirements of these interventions.
The integration of digital health technologies and artificial intelligence presents emerging opportunities to enhance the value proposition of bioelectronic medicine. The "convergence of AI, data analytics, and bioelectronic medicine is paving the way for next-generation diagnostics and therapeutics, while also facilitating remote care and expanding access to treatment" [10]. These technological synergies may ultimately strengthen the economic case for bioelectronic interventions through improved personalization, remote monitoring capabilities, and predictive maintenance of implanted devices.
Bioelectronic medicine stands at a pivotal intersection of therapeutic innovation and economic reality. While the field offers transformative potential for treating chronic diseases through targeted neuromodulation, its advancement is inextricably linked to addressing substantial cost and reimbursement challenges. The high capital investment required for device development and procedural implementation presents significant barriers to widespread adoption, particularly in resource-constrained healthcare environments. However, emerging evidence suggests that when appropriate value frameworks are applied—capturing reduced hospitalizations, decreased medication dependence, and improved quality of life—bioelectronic approaches can demonstrate compelling economic profiles over appropriate time horizons. The ongoing integration of digital health technologies and artificial intelligence further enhances the potential for personalized, cost-effective therapeutic strategies. For researchers and developers in this space, prioritizing health economic outcomes alongside clinical efficacy will be essential to establishing sustainable reimbursement pathways and ultimately realizing the full potential of bioelectronic medicine to transform patient care.
Overcoming Complex Regulatory Pathways and Device Approval Processes
The development of novel medical therapies requires navigating fundamentally different regulatory landscapes for bioelectronic devices versus pharmaceuticals. These distinct pathways reflect the unique nature of each technology: pharmaceuticals involve active chemical interactions with metabolic pathways, while bioelectronic devices are largely mechanical or electrical and achieve their effects through physical interaction with electrically active tissues [71]. For researchers and drug development professionals entering the bioelectronic medicine space, understanding these divergent regulatory philosophies, evidence requirements, and approval timelines is crucial for strategic planning and successful translation of innovations to clinical practice.
Bioelectronic Medicine (BEM) represents an emerging therapeutic approach that uses implantable electronic devices to interface with electrically active tissues, offering innovative solutions for conditions ranging from neurological disorders to autoimmune diseases [6] [1]. Unlike pharmaceuticals, which distribute chemically throughout the bloodstream and often cause systemic side effects, bioelectronic devices achieve localized effects through precise electrical modulation of neural circuits [6]. This fundamental difference necessitates tailored regulatory approaches that account for the distinct risk-benefit profiles, development cycles, and clinical validation requirements for each technology type.
Regulatory Framework Comparison: US and EU Systems
US FDA Medical Device Regulation
The US Food and Drug Administration (FDA) employs a risk-based classification system for medical devices with three primary pathways to market:
- 510(k) Premarket Notification: Requires demonstration of substantial equivalence to a legally marketed predicate device; typically takes 4-12 months with costs ranging from $100,000-$500,000 [72] [73]. Most Class II devices (moderate risk) such as infusion pumps and pregnancy tests utilize this pathway.
- De Novo Classification: For novel low-to-moderate risk devices without predicates; typically takes 8-14 months and creates a new regulatory classification for future similar devices [72].
- Premarket Approval (PMA): The most stringent pathway for high-risk Class III devices (e.g., pacemakers, heart valves); requires comprehensive clinical data demonstrating safety and effectiveness, typically taking 1.5-3+ years with costs exceeding $1 million [72] [73].
The Breakthrough Devices Program (BDP) provides expedited development and review for devices that provide more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases [74]. From 2015-2024, only 12.3% of the 1,041 BDP-designated devices received marketing authorization, reflecting the rigorous evidence requirements even within accelerated pathways [74]. Notably, BDP-designated devices received significantly faster reviews than standard approvals: mean decision times were 152 days for 510(k), 262 days for de novo, and 230 days for PMA pathways, compared to 338 days for standard de novo and 399 days for standard PMA reviews [74].
European Union MDR System
The EU Medical Device Regulation (MDR) employs a decentralized system based on conformity assessment by Notified Bodies, with key differentiators from the US system:
- Rule-Based Classification: Four device classes (I, IIa, IIb, III) determined by 22 classification rules based on invasiveness, duration of contact, and body system affected [75].
- Clinical Evaluation Mandate: Unlike the FDA's predicate-based approach for some devices, EU MDR requires clinical evaluation for all devices regardless of classification, with stricter equivalence criteria for using existing clinical data [75].
- Timeline and Cost Considerations: EU MDR typically requires 12-18 months and $500,000-$2 million for CE marking through Notified Body assessment [75].
Table 1: Comparative Analysis of US FDA and EU MDR Regulatory Pathways
| Aspect | US FDA | EU MDR |
|---|---|---|
| Regulatory Philosophy | Centralized, predicate-based for some pathways | Decentralized, performance-based |
| Primary Authority | FDA (federal agency) | Notified Bodies (multiple, designated by member states) |
| Clinical Evidence | Varies by pathway; may rely on predicate data | Always required; stricter equivalence criteria |
| Typical Timeline | 6-12 months (510(k)) to 1-5 years (PMA) [72] | 12-18 months [75] |
| Cost Range | $7,000+ (Class I) to $1M-$10M+ (Class III) [72] | $500,000-$2 million [75] |
| Accelerated Pathway | Breakthrough Devices Program [74] | No specific accelerated pathway |
Pharmaceutical Regulatory Pathways
Pharmaceutical regulation follows distinctly different pathways, with the FDA's Accelerated Approval Program allowing drugs for serious conditions to be approved based on surrogate endpoints reasonably likely to predict clinical benefit [76]. Unlike medical devices, confirmatory trials for pharmaceuticals may sometimes begin after approval, though recent guidance emphasizes the need for these trials to be underway earlier in the process [76]. First-in-class drugs often utilize these pathways, with 24 of 50 new molecular entities approved in 2024 designated as first-in-class [77].
Strategic Considerations for Bioelectronic Medicine Development
Evidence Generation and Clinical Trial Design
Bioelectronic medicine developers face unique challenges in evidence generation compared to both traditional devices and pharmaceuticals:
- Clinical Data Requirements: Unlike pharmaceuticals where randomized clinical trials are considered the gold standard, medical devices often face practical and ethical challenges with blinding and comparator selection [71]. For example, implanting a "placebo" device raises ethical concerns, and the effect of devices depends heavily on clinician skill, patient selection, and care setting [71].
- Real-World Evidence: Post-market surveillance and real-world data play a more significant role in device evaluation compared to pharmaceuticals, with structured post-market surveillance being equally important as pre-market data for assessing long-term safety and effectiveness [71].
- Endpoint Selection: Bioelectronic devices may utilize novel endpoints that differ from traditional pharmaceutical endpoints, requiring early engagement with regulatory agencies for alignment on acceptable endpoints and study designs.
Table 2: Key Differences Between Bioelectronic Medicine and Pharmaceutical Development
| Development Aspect | Bioelectronic Medicine | Pharmaceuticals |
|---|---|---|
| Innovation Cycle | 18-24 months for iterations [71] | Decades for improvements [71] |
| Therapeutic Mechanism | Physical interaction with electrically active tissues [71] | Chemical interaction with metabolic/immune systems [71] |
| Risk Profile | Primarily mechanical/electrical risks [71] | Systemic metabolic and immunological risks [71] |
| Dosing Paradigm | Electrical parameters, programmability [22] | Chemical concentration, pharmacokinetics |
| Personalization Approach | Algorithm adjustments, stimulation parameters [22] | Dosage titration, regimen modifications |
| Clinical Trial Design | Often unblinded, clinician-dependent outcomes [71] | Typically blinded, less operator-dependent |
Market Access and Reimbursement Strategy
Navigating from regulatory approval to reimbursement requires strategic planning:
- Coverage Determinations: In the US, Centers for Medicare & Medicaid Services (CMS) makes critical coverage decisions for FDA-approved devices, while in the EU, the Health Technology Assessment Regulation (HTAR) plays a key role in evaluating clinical and cost-effectiveness [74].
- Value Proposition: Bioelectronic devices often have higher upfront costs but potentially lower long-term costs compared to chronic pharmaceutical therapies, requiring creative reimbursement models that account for this cost distribution [22].
- Health Economic Evidence: Generating robust health economic data is particularly important for bioelectronic devices, as payers increasingly demand demonstration of cost-effectiveness alongside clinical efficacy.
Experimental Design and Methodological Considerations
Preclinical Testing Requirements
Comprehensive preclinical testing is essential for bioelectronic medicine development:
- Biocompatibility Testing: Following ISO 10993 standards to evaluate device-tissue interactions, particularly important for implantable components that interface with neural tissue [6].
- Accelerated Aging Studies: To demonstrate device reliability and stability over the proposed implant duration, evaluating factors like material degradation and electrical performance [6].
- Mechanical Testing: Assessing device integrity under simulated physiological conditions, especially for flexible and stretchable electronics designed to withstand dynamic biological environments [6].
Clinical Investigation Design
Designing clinical studies for bioelectronic devices requires special considerations:
- Blinding Challenges: When complete blinding isn't feasible, utilizing objective endpoints and independent endpoint adjudication committees can reduce bias [71].
- Operator Training Standardization: Accounting for the clinician-dependent nature of device outcomes through comprehensive training protocols and potentially evaluating operator learning curves [71].
- Long-Term Follow-Up: Planning for extended post-market surveillance to capture long-term performance data, particularly important for implantable devices [73].
Diagram 1: Comparative Development Pathways for Pharmaceuticals and Bioelectronic Devices. The diagram highlights parallel but distinct development processes with different regulatory requirements and study designs at key stages.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Bioelectronic Medicine Development
| Material/Reagent | Function | Application Examples |
|---|---|---|
| Conducting Polymers (e.g., PEDOT:PSS) | Interface materials with mixed ionic/electronic conductivity, mechanical flexibility, and enhanced biocompatibility [1] | Neural electrode coatings to reduce impedance and improve signal transmission [1] |
| Soft, Flexible Substrates | Minimize mechanical mismatch with biological tissues to reduce foreign body reaction [6] | Wrap-around nerve cuffs, conformal organ interfaces [6] |
| Hydrogels | Bio-integrative materials that facilitate tissue-device integration and drug delivery capabilities [6] | Multimodal devices combining stimulation and localized drug release |
| Carbon-Based Materials (graphene, CNTs) | Novel electrodes with superior electronic and optical properties [1] | High-density neural interfaces, transparent electrodes |
| Bioresorbable Materials | Temporary implants that dissolve after serving their function, eliminating need for surgical removal [6] | Temporary stimulation devices, pediatric applications |
| MXenes | Two-dimensional conductive materials with unique surface chemistry for neural interfaces [1] | High-resolution neural recording and stimulation |
The regulatory pathways for bioelectronic medicine continue to evolve as the technology advances. Key trends include increased global harmonization efforts, growing acceptance of real-world evidence, and development of novel endpoints specific to neuromodulation therapies. For researchers and developers, success requires understanding both device and pharmaceutical regulatory principles, even when working primarily in one domain.
Future developments will likely include greater convergence between regulatory systems, with the FDA transitioning to Quality Management System Regulation (QMSR) aligned with ISO 13485:2016 in 2026, creating closer alignment with EU MDR requirements [75]. Additionally, the implementation of the EU Health Technology Assessment Regulation (HTAR) beginning in 2026 will further harmonize approval processes across member states [74].
By strategically navigating these complex regulatory pathways and generating robust scientific evidence, researchers can accelerate the development of innovative bioelectronic therapies that offer new treatment options for patients with unmet medical needs. The unique advantages of bioelectronic medicine—including targeted action, programmability, and reduced systemic side effects—position this field to become an increasingly important therapeutic modality alongside pharmaceutical interventions.
Mitigating Foreign Body Reaction and Improving Biocompatibility with Advanced Materials
The development of long-term implantable bioelectronic medical devices represents a paradigm shift in the treatment of chronic diseases, offering a targeted, reversible alternative to systemic pharmaceuticals. These devices interact directly with electrically active tissues to modulate neural circuits that control processes ranging from inflammation to cardiovascular function [1] [62]. However, the clinical translation and long-term efficacy of these technologies face a fundamental biological challenge: the foreign body reaction (FBR). This inevitable host response to implanted materials begins with protein adsorption and progresses through acute inflammation to chronic fibrosis, ultimately resulting in the encapsulation of the device in a collagenous scar tissue [78]. This fibrotic capsule electrically isolates the implant from its target tissue, diminishing recording sensitivity and stimulation efficiency while increasing power requirements [78].
The mitigation of FBR has become a critical focus in bioelectronic medicine research, as the field strives to create stable, long-lasting interfaces with neural tissue. While pharmaceutical interventions typically face challenges of systemic distribution and off-target effects, bioelectronic devices offer the potential for precise, localized therapy. However, this potential can only be realized if the materials comprising these devices can overcome the host's defensive reactions. Advanced materials science has emerged as a powerful approach to addressing this challenge, with researchers designing polymers and hydrogels with specific chemical, mechanical, and structural properties that modulate the immune response rather than provoking it [79] [80]. This comparison guide examines the current landscape of these advanced materials, providing experimental data and methodologies to inform material selection for next-generation bioelectronic implants.
Comparative Analysis of Polymer Biocompatibility
In Vitro and In Vivo Performance Metrics
The quest for biocompatible materials has yielded numerous polymer candidates with varying abilities to mitigate FBR. Recent comparative studies have systematically evaluated these materials using standardized experimental models to provide directly comparable data on their performance. The table below summarizes key findings from a comprehensive assessment of ten polymer materials, highlighting their compatibility with neural interfaces based on both cellular responses and tissue integration.
Table 1: Biocompatibility Comparison of Polymer Materials for Neural Interfaces
| Polymer Material | Neural Cell Adhesion & Growth | Fibroblast Adhesion & Growth | Cytotoxicity | Fibrotic Encapsulation (4 weeks post-implant) | Overall FBR Assessment |
|---|---|---|---|---|---|
| Polyimide (PI) | High | High | None detected | Minimal | Excellent compatibility |
| Polylactide (PLA) | Moderate | Moderate | None detected | Mild | Good compatibility |
| Polydimethylsiloxane (PDMS) | Moderate | Moderate | None detected | Mild | Good compatibility |
| Thermoplastic Polyurethane (TPU) | Moderate | Moderate | None detected | Mild | Good compatibility |
| Polyethylene Terephthalate Glycol (PET-G) | Low | Low | Low | Moderate | Moderate compatibility |
| Polypropylene (PP) | Low | Low | Low | Moderate | Moderate compatibility |
| Nylon 618 (NY) | Low | Low | Low | Moderate | Moderate compatibility |
| Polyethylene Terephthalate (PET) | Low | Low | Low | Moderate | Moderate compatibility |
| Polycaprolactone (PCL) | Low | Low | Low | Moderate | Moderate compatibility |
| Polyethylene Glycol Diacrylate (PEGDA) | Very low | Very low | Significant | Severe (strong fibrosis & multinucleated cells) | Poor compatibility |
According to the study, Polyimide (PI) demonstrated the highest compatibility for both neural cells (PC-12) and fibroblasts (NRK-49F), showing excellent cell adhesion and growth with no detected cytotoxicity [79]. This was corroborated by in vivo findings, where PI implants evoked minimal fibrotic encapsulation after four weeks. Similarly, PLA, PDMS, and TPU showed promising profiles with lower pathological responses, making them potentially suitable for neural interfacing applications. In contrast, PEGDA exhibited significant cytotoxic effects, low cell adhesion, and provoked a strong foreign body reaction including fibrosis and multinucleated giant cell formation, rendering it unsuitable for long-term implantation [79].
Advanced Hydrogel Materials for FBR Mitigation
Beyond traditional polymers, hydrogel materials have emerged as particularly promising candidates for mitigating FBR due to their high water content and tissue-like mechanical properties. Recent research has introduced innovative materials that significantly outperform traditional options like polyethylene glycol (PEG), which has shown both immunogenicity and antigenicity in long-term applications [80]. The following table compares the performance of next-generation hydrogels against established materials in subcutaneous implantation models.
Table 2: Comparative Performance of Hydrogel Materials in Foreign Body Response
| Hydrogel Material | Inflammatory Response (1-2 weeks) | Collagen Capsule Thickness (4 weeks) | Blood Vessel Density (vessels/mm²) | Key Advantages | Limitations |
|---|---|---|---|---|---|
| Poly-DL-serine (PSer) | Minimal inflammatory response, low macrophage density | <5 μm | 106-126 | High water solubility (>500 mg/mL), no collagen encapsulation after 7 months | Requires photo-crosslinking for gelation |
| PEG (Control) | Significant swelling and inflammation, high macrophage density | 22-27 μm | 26-33 | Established fabrication protocols | Immunogenicity, decomposes in physiological conditions |
| β-Homoserine (β-HS) | Low inflammatory response | Not reported | Not reported | "Dual hydrogen bonding hydration" principle | Moderate water solubility (~10 mg/mL) requires organic solvents |
| Acetyl BSP (Branched Glucomannan) | Moderate, less than linear equivalent | Less than linear equivalent | Not reported | Better absorption in body, reduced pro-inflammatory cytokine release | Requires electrospinning for scaffold formation |
| Acetyl KGM (Linear Glucomannan) | Stronger FBR than branched equivalent | Greater than branched equivalent | Not reported | Natural source, established modification protocols | Stimulates pro-inflammatory cytokines |
Bio-inspired poly-DL-serine (PSer) materials have demonstrated exceptional anti-FBR properties, causing negligible inflammatory response after subcutaneous implantation and showing no obvious collagen encapsulation even after seven months [80]. This performance surpassed PEG hydrogels, which were surrounded by dense collagen layers with thicknesses of 22-27 μm and significantly lower surrounding blood vessel density [80]. The high water solubility of PSer (>500 mg/mL) enables processing without organic solvents, addressing a significant limitation of other advanced materials like β-Homoserine, which requires dimethylsulfoxide for hydrogel preparation [80].
Experimental Protocols for Assessing FBR
Standardized Methodologies for In Vitro and In Vivo Evaluation
To generate comparable data on material biocompatibility, researchers employ standardized experimental protocols that assess cellular responses in vitro and tissue integration in vivo. These methodologies provide critical insights into the host-material interactions at different stages of the FBR continuum.
In Vitro Cell Culture Assessment:
- Cell Lines: Utilize neural (e.g., PC-12) and fibroblast (e.g., NRK-49F) cell cultures to evaluate cell-type-specific responses [79]
- Cell Adhesion & Growth: Seed cells on material scaffolds at standardized densities (e.g., 10,000 cells/cm²) and quantify adhesion rates after 24 hours using imaging or metabolic activity assays [79]
- Cytotoxicity Testing: Employ assays such as MTT or LDH release to measure cell viability and membrane integrity after 48-72 hours of exposure to material extracts or direct contact [79]
- Surface Characterization: Use scanning electron microscopy (SEM) to analyze material topography and cell morphology at various magnifications (e.g., 100x to 10,000x) [79]
In Vivo Implantation and Histological Analysis:
- Animal Models: Utilize rat or mouse subcutaneous implantation models, with sample sizes of 6-8 animals per group to ensure statistical power [79] [80]
- Implantation Protocol: Aseptically implant sterile material scaffolds (typical dimensions: 5mm diameter, 1mm thickness) in subcutaneous pockets following ethical guidelines and approved protocols [80]
- Tissue Harvesting: Euthanize animals at predetermined timepoints (1, 2, 4 weeks, 3, 7 months) and excise implants with surrounding tissue [80]
- Histological Processing: Fix tissue in 4% paraformaldehyde, embed in paraffin, section at 5μm thickness, and stain with:
- Image Analysis: Quantify inflammatory cell density, collagen capsule thickness, and blood vessel density using image analysis software (e.g., ImageJ) with multiple fields per sample [80]
Evaluating Structural Influence on Immune Response
Advanced material design recognizes that FBR is influenced not only by chemical composition but also by structural characteristics. Researchers have developed specialized protocols to isolate and study the effect of structural arrangement on immune activation.
Sugar Chain Arrangement Study:
- Material Selection: Isolate linear-chain (Konjac glucomannan, KGM) and branched-chain (Bletilla striata polysaccharide, BSP) polysaccharides with similar composition and molecular weight [81]
- Chemical Modification: Perform acetylation using standardized protocols - for BSP: disperse in pyridine, add acetic anhydride:pyridine mixture; for KGM: use trifluoroacetic anhydride:acetic acid mixture [81]
- Scaffold Fabrication: Create electrospun scaffolds from 10% solutions of acetylated materials in chloroform:DMF (2:1) using consistent parameters (voltage: +12kV/-4kV, rate: 0.5mL/h) to minimize morphological differences [81]
- Macrophage Cytokine Profiling: Culture macrophages on scaffolds and measure pro-inflammatory cytokine (IL-1β, TNF-α) release using ELISA kits [81]
- In Vivo Implantation: Implant acetyl KGM and acetyl BSP scaffolds subcutaneously to compare FBR intensity through histological analysis [81]
This methodology revealed that linear-chain acKGM scaffolds stimulated stronger FBR and pro-inflammatory cytokine release compared to branched-chain acBSP, demonstrating the significant impact of nanoscale structure on immune activation [81].
Signaling Pathways in Foreign Body Response
The foreign body reaction follows a complex, coordinated sequence of cellular events mediated by specific signaling pathways. Understanding these mechanisms is essential for designing materials that can effectively modulate rather than provoke immune responses.
Figure 1: Foreign Body Reaction Cascade Timeline
The FBR cascade initiates within seconds to minutes after implantation with non-specific protein adsorption to the material surface, predominantly albumin and fibrinogen from extravasated blood [78]. This provisional matrix undergoes dynamic rearrangement through the Vroman effect, where smaller proteins are progressively replaced by larger ones [78]. Neutrophils are the first cellular responders, migrating to the implantation site within hours and releasing reactive oxygen species (ROS) and proteolytic enzymes that further promote the inflammatory process [78]. These chemical signals attract monocytes, which differentiate into macrophages upon arrival [78].
Macrophages adhere to the protein-coated implant surface primarily through αMβ2 integrin binding to adsorbed fibronectin and fibrinogen [78]. When unable to phagocytose the large foreign body, macrophages undergo "frustrated phagocytosis," releasing additional degrading enzymes and pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 [78]. These cytokines create a chemotactic gradient that recruits additional macrophages to the site in a self-sustaining cycle [78]. Over weeks, macrophages may fuse to form foreign body giant cells (FBGCs), a hallmark of chronic FBR [78]. The final stage involves fibroblast recruitment and activation, leading to deposition of collagen and other extracellular matrix components that form a dense fibrotic capsule around the implant, effectively isolating it from the surrounding tissue and compromising its function [78].
The Scientist's Toolkit: Essential Research Reagents and Materials
The systematic evaluation of material biocompatibility requires a carefully selected suite of research tools and reagents. The following table details essential solutions and their applications in FBR research.
Table 3: Essential Research Reagent Solutions for FBR Studies
| Reagent/Material | Function in FBR Research | Example Application | Key Considerations |
|---|---|---|---|
| Poly-DL-serine diacrylamide (PSerDA) | Hydrogel precursor for anti-FBR material studies | Photo-crosslinkable hydrogel formation with superior biocompatibility | High water solubility enables processing without organic solvents [80] |
| Electrospinning Solutions (e.g., acetyl glucomannan in chloroform:DMF) | Fabrication of scaffolds with controlled topography | Creating comparable surface morphologies to isolate structural effects | Parameters (voltage, humidity, rate) must be standardized for consistency [81] |
| ELISA Kits (e.g., IL-1β, TNF-α) | Quantification of pro-inflammatory cytokine release | Measuring macrophage activation in response to material surfaces | Requires cell culture supernatant collection from material-macrophage co-cultures [81] |
| Immunofluorescence Antibodies (F4/80, αSMA, CD31) | Identification of specific cell types in tissue sections | Macrophage infiltration, myofibroblast activation, and blood vessel quantification | Tissue fixation and antigen retrieval methods affect antibody binding [80] |
| Histological Stains (H&E, Masson's Trichrome) | General tissue morphology and collagen visualization | Assessing inflammatory cell infiltration and fibrotic capsule thickness | Stain consistency requires precise timing and fresh solutions [80] |
| Contact Angle Measurement | Surface wettability quantification | Correlating material hydrophilicity with protein adsorption and cell adhesion | Requires flat, uniform surfaces for accurate measurement [81] |
| SEM Preparation Reagents (glutaraldehyde, ethanol series, HMDS) | Sample preparation for surface topography imaging | Visualizing material microstructure and cell-material interactions | Critical point drying preserves delicate structures better than air drying [79] |
These research tools enable comprehensive characterization of material properties and their biological outcomes. For instance, the combination of SEM surface analysis with immunofluorescence staining of explained tissues allows researchers to correlate physical material characteristics with the resulting cellular responses [79] [80]. Similarly, ELISA-based cytokine profiling from macrophage cultures on material surfaces provides mechanistic insights into the inflammatory potential of different materials [81].
The advancement of bioelectronic medicine hinges on solving the fundamental challenge of foreign body reaction, which currently limits the long-term stability and performance of implantable devices. The comparative data presented in this guide demonstrates that material selection is not merely a passive engineering decision but an active therapeutic strategy. While traditional materials like PEG show significant limitations, emerging options such as poly-DL-serine and structurally engineered polysaccharides offer promising alternatives that actively mitigate FBR through their chemical and physical properties [80] [81].
The experimental protocols and analytical tools outlined provide a framework for standardized evaluation of new materials, enabling direct comparison and informed selection for specific applications. As the field progresses, the integration of these advanced materials with bioelectronic devices promises to create more stable neural interfaces that maintain their therapeutic efficacy over extended periods. This materials-driven approach complements the circuit-targeted specificity of bioelectronic therapies, potentially unlocking their full potential to treat chronic conditions with unprecedented precision and minimal side effects compared to systemic pharmaceuticals.
For researchers and product developers, the current evidence supports a strategic shift toward materials with demonstrated low FBR profiles, particularly those with structural characteristics that minimize immune recognition while promoting integration with host tissues. The continued refinement of these materials, coupled with deeper understanding of their interactions with immune cells, will be essential for the next generation of bioelectronic medicines that truly merge with the body's biological systems.
The evolution of implantable medical devices represents a paradigm shift from traditional pharmaceutical interventions toward precise, programmable bioelectronic therapies. A critical bottleneck in this evolution has been power management—specifically, the reliance on bulky batteries that limit device lifespan, functionality, and miniaturization. The strategic shift toward battery-less, wirelessly powered implants addresses these limitations by harnessing external energy sources, enabling devices that are smaller, longer-lasting, and capable of operating deep within the human body. This transition is not merely a technical improvement but a fundamental reimagining of therapeutic design, positioning bioelectronic medicine as a viable alternative to pharmaceutical outcomes for chronic conditions. This guide provides an objective comparison of the dominant wireless power strategies, supported by experimental data and detailed methodologies, to inform researchers and drug development professionals evaluating these transformative technologies.
Comparative Analysis of Wireless Power Transfer Technologies
The landscape of wireless power transfer (WPT) for implants is dominated by three core technologies, each with distinct operating principles, advantages, and limitations. The following table provides a structured, data-driven comparison of Near-Field Coupling, Magnetostrictive-Piezoelectric Systems, and Far-Field RF Harvesting.
Table 1: Comparative Analysis of Wireless Power Transfer Technologies for Implants
| Technology | Operating Principle | Frequency Band | Key Components | Reported Power Output & Efficiency | Optimal Implant Depth | Advantages | Limitations |
|---|---|---|---|---|---|---|---|
| Near-Field Coupling (NFC) [82] [83] [84] | Resonant magnetic coupling between external and implant coils. | 13.56 MHz | - Primary antenna (external) - Secondary antenna (implant) - Rectifier and regulator circuit | - Peak Power: 24-32 mW at 0 mm depth [82] - Depth Performance: ~8 mW at 30 mm tissue depth [82] - Data Rate: Up to 26.48 kbps (ISO/IEC 15693) [82] | Shallow to medium depth (0-30 mm) | - High efficiency at close range - Well-established safety standards (e.g., FCC, ICNIRP) - Integrated data communication | - Rapid power drop-off with distance - Sensitive to antenna alignment and tissue properties |
| Magnetostrictive-Piezoelectric (M-P) Systems [85] [86] | Conversion of magnetic fields to electrical charge via mechanical vibration. | 109 kHz (Low Frequency) | - Magnetostrictive film (e.g., Metglas) - Piezoelectric film (e.g., PZT) - Laminated electrode structure | - Power Gain: 4-5 orders of magnitude more power than metallic coil antennas of similar size (200 μm) [85] [86] - Safe Operation: Low frequency minimizes tissue heating [85] | Deep tissue (Ideal for miniaturized, injectable implants) | - Ultra-miniaturization (sand-sized) - Efficient low-frequency operation, safe for tissue - Injectable via needle, no major surgery required | - Emerging technology, long-term reliability data limited - Complex fabrication process |
| Far-Field RF Harvesting [82] [87] | Harvesting of ambient or directed radiofrequency energy. | 915 MHz (common for wearables) | - Dipole antenna - Power management circuit - Energy storage buffer (e.g., small battery) | - Harvested Power: Enables continuous operation of a wearable biosymbiotic hub [82] - Range: Up to 2 meters from transmitter [82] | Powers wearables that then power implants via NFC | - Enables at-distance charging - Greater freedom of movement for the user | - Lower power transfer efficiency - Requires an intermediate wearable device for most implants |
Experimental Protocols & Methodologies
To critically evaluate the performance claims of different WPT systems, it is essential to understand the experimental protocols used to generate key data. The following section details the methodologies from foundational studies.
Protocol: Evaluating NFC Power Transfer through Tissue
This protocol, adapted from studies on biosymbiotic hubs and osseosurface electronics, measures the efficiency of NFC power delivery through biological tissue [82].
- Objective: To quantify the power received by an NFC-enabled implant through varying thicknesses of tissue.
- Materials:
- NFC Initiator-Reader IC and antenna (e.g., serpentine-structured or circular wire-wound coil)
- Wireless, battery-free (WBF) implant prototype with integrated power measurement circuit
- Fresh porcine tissue samples of known, varying thicknesses (0-30 mm)
- Network analyzer or custom firmware to measure received voltage/current
- Signal generator and power amplifier
- Procedure:
- The NFC antenna is connected to the initiator-reader IC and placed on one side of the tissue sample.
- The WBF implant is placed on the opposite side of the tissue sample.
- The initiator-reader IC generates a 13.56 MHz field at a fixed output power.
- The voltage and current at the rectifier stage of the WBF implant are measured and used to calculate the received power.
- The Specific Absorption Rate (SAR) is simulated or measured to ensure it remains below safety limits (e.g., FCC's 1.6 W/kg) [82].
- Steps 2-5 are repeated for increasing tissue thicknesses and with the implant placed on and off bone.
- Key Metrics: Received Power (mW), Maximum Data Transfer Rate (kbps), SAR (W/kg).
Protocol: Characterizing Magnetostrictive-Piezoelectric Antenna Performance
This protocol outlines the testing of the novel injectable antenna developed by the MIT Media Lab [85] [86].
- Objective: To characterize the power harvesting capability and operational safety of a magnetostrictive-piezoelectric antenna.
- Materials:
- Fabricated M-P antenna (200 μm size)
- Alternating magnetic field generator (low-frequency, 109 kHz)
- Oscilloscope with high-impedance probes
- Phantom tissue gel simulating electrical properties of human tissue
- Thermal camera to monitor tissue heating
- Procedure:
- The M-P antenna is embedded within the phantom tissue gel at a specified depth.
- An alternating magnetic field at 109 kHz is applied externally.
- The open-circuit voltage and short-circuit current generated across the antenna's electrodes are measured directly using the oscilloscope.
- The output power is calculated from the voltage and current measurements.
- The temperature of the phantom tissue surrounding the antenna is monitored in real-time using the thermal camera during extended operation to assess heating effects.
- The output is compared against a same-sized metallic coil antenna operating in the GHz range.
- Key Metrics: Output Power (μW/mW), Power Gain vs. coil antenna, Maximum Temperature Increase (°C).
The Therapeutic Context: Bioelectronic vs. Pharmaceutical Outcomes
The drive toward battery-free implants is a cornerstone of the broader thesis of Bioelectronic Medicine (BM), which offers a distinct alternative to traditional pharmaceuticals. The table below contrasts these two therapeutic paradigms.
Table 2: Bioelectronic Medicine vs. Pharmaceutical Outcomes: A Comparative Framework
| Aspect | Bioelectronic Medicine (with WBF Implants) | Pharmaceutical Therapeutics |
|---|---|---|
| Mechanism of Action | Electrical, optical, or mechanical modulation of specific neural circuits or organs [6]. | Systemic chemical interactions with receptors, enzymes, or cellular pathways. |
| Specificity & Targeting | High specificity; can target precise neural pathways (e.g., inflammatory reflex) without influencing unrelated systems [6]. | Lower specificity; often leads to systemic side effects due to off-target interactions (e.g., immune suppression) [6]. |
| Adaptability & Dosing | Real-time, programmable adjustment of stimulation parameters based on physiological feedback (closed-loop systems) [6]. | Fixed dosing regimens; adjustments are slow and require prescription changes. |
| Long-Term Management | "One-time" implantation with potential for long-term, maintenance-free operation; no patient adherence required post-implantation [87]. | Requires continuous, lifelong patient adherence to medication schedules; risk of non-compliance [6]. |
| Environmental Impact | Reduced medical waste from battery replacements; potential for bioresorbable materials [6] [87]. | Continuous manufacturing and distribution; packaging and drug residue waste. |
Key Signaling Pathways in Bioelectronic Therapy: A prime example of BM's targeted mechanism is the use of Vagus Nerve Stimulation (VNS) to treat inflammatory diseases. Unlike systemic immunosuppressants, VNS modulates the "Inflammatory Reflex". This pathway can be diagrammed as follows:
The Research Toolkit: Essential Materials & Reagents
For research teams developing or validating wirelessly powered implants, the following table details key reagents and their functions based on the cited experimental work.
Table 3: Key Research Reagent Solutions for Wireless Power Transfer Development
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| Magnetostrictive Film (e.g., Metglas) | Core material that deforms in response to an applied magnetic field [85] [86]. | Laminated with piezoelectric film in the MIT injectable antenna to enable low-frequency power harvesting [85]. |
| Piezoelectric Film (e.g., PZT) | Converts mechanical strain from the magnetostrictive layer into electric charge [85] [86]. | The top layer in the M-P antenna laminate; generates the power for the implant [85]. |
| Platinum Electrodes | Biocompatible, high-conductivity material for neural stimulation and recording [84]. | Used in DBS probes; surface roughness engineered to reduce impedance and improve charge injection capacity [84]. |
| Polyimide / Parylene-C | Flexible, biocompatible substrates and encapsulation materials for conformal electronics [83] [84]. | Used as the structural carrier and insulating layer for flexible, subdermal implantable devices in rodents and songbirds [83] [84]. |
| Phantom Tissue Gel | Tissue-mimicking material that simulates the dielectric properties of human tissue for in-vitro testing [85] [82]. | Used to test power transfer efficiency and Specific Absorption Rate (SAR) of implants before in-vivo studies [82]. |
| Bioresorbable Materials (e.g., PLGA, Silk) | Temporary substrates and encapsulants that safely dissolve in the body over time [6] [87]. | Enables the creation of "temporary" electronic implants that do not require surgical extraction [6]. |
Visualizing the Experimental Workflow
A critical phase in the development of any wirelessly powered implant is the in-vivo validation of its powering system and functional output. The workflow for a chronic study in a freely moving animal model can be summarized as follows:
Outcomes and Economic Impact: Validating Efficacy and Cost-Effectiveness in Clinical Practice
Treatment-resistant depression (TRD), defined as a failure to respond adequately to at least two standard antidepressant therapies, represents a major clinical challenge affecting millions of patients worldwide [88]. The high global disease burden of TRD has spurred innovation across therapeutic domains, particularly in bioelectronic medicine and novel pharmaceutical approaches [31] [88]. This review systematically compares the clinical efficacy, mechanisms, and practical implementation of emerging interventions for TRD, with a specific focus on neuromodulation techniques and rapid-acting antidepressants. We synthesize quantitative outcome data from recent clinical trials to provide researchers and drug development professionals with an evidence-based framework for evaluating these transformative therapies.
Comparative Efficacy of TRD Interventions
Quantitative Outcomes Across Therapeutic Modalities
Table 1: Clinical efficacy outcomes for TRD interventions
| Intervention | Response Rate | Remission Rate | Time Course | Evidence Source |
|---|---|---|---|---|
| Deep Brain Stimulation (MFB target) | 86% (long-term) | 60% (rostral PFC target) | Rapid improvement (2 weeks), sustained over 5 years | Network meta-analysis, long-term observational study [89] [90] |
| Accelerated rTMS (left DLPFC) | 52% | 24% | Significant improvement at 3 weeks | Controlled trial, 25 patients [91] |
| Vagus Nerve Stimulation | 67.6% (5-year cumulative) | 43.3% (5-year cumulative) | Progressive improvement, optimal at 10-12 months | 5-year prospective observational study [92] |
| Mebufotenin (GH001) | Primary endpoint met (p<0.0001) | All patients in PPD trial (Day 8) | Rapid onset (Day 8) | Phase 2b RCT, proof-of-concept trials [93] |
Key Efficacy Differentiators
The quantitative data reveal fundamental differences in the therapeutic profiles of bioelectronic versus pharmaceutical approaches. DBS targeting the medial forebrain bundle (MFB) demonstrates particularly impressive durability, with follow-up data showing sustained efficacy over five years and remarkable 81% average reduction in depression severity in long-term responders [90]. This positions DBS as a potentially transformative intervention for the most severe TRD cases, though its invasive nature necessitates careful patient selection.
In contrast, novel pharmaceutical approaches like mebufotenin (GH001) demonstrate exceptionally rapid onset, with significant improvement observed within days rather than weeks [93]. The Phase 2b trial met its primary endpoint with a MADRS reduction of -15.5 points compared to placebo at Day 8 (p<0.0001), representing one of the fastest antidepressant effects documented in controlled trials. This rapidity of action presents distinct advantages for clinical scenarios requiring urgent intervention, such as severe suicidal ideation.
Non-invasive neuromodulation techniques like rTMS offer a favorable risk-benefit profile, with accelerated protocols achieving meaningful response within three weeks while maintaining minimal side effects [91]. The durability of VNS is particularly noteworthy, with 5-year cumulative response rates significantly outperforming treatment-as-usual (67.6% vs. 40.9%) [92], suggesting potential disease-modifying effects through neuroplasticity enhancement and anti-inflammatory mechanisms.
Experimental Protocols and Methodologies
Accelerated rTMS Protocol for TRD
Table 2: Research reagents and essential materials for rTMS studies
| Item | Function | Specifications in Protocol |
|---|---|---|
| TMS Machine | Generation of magnetic pulses | Capable of high-frequency (10 Hz) stimulation |
| Motor Threshold Assessment Tool | Determine stimulation intensity | Visual observation of muscle contraction |
| APB Localization Equipment | Identify motor cortex | Supra-threshold stimulation for thumb movement |
| Scalp Measurement System | Precisely locate DLPFC | 6 cm anterior to motor hotspot |
| HDRS and CGI Scales | Standardized outcome assessment | Validated depression rating instruments |
The accelerated rTMS protocol exemplifies the trend toward condensed treatment schedules that enhance patient accessibility [91]. This specific methodology involved:
Patient Population: 25 TRD patients (12 female, 13 male) with mean age 36.9 ± 10.6 years, all with history of ≥1 failed antidepressant trial and HDRS score >17 at baseline.
Treatment Parameters:
- Target: Left dorsolateral prefrontal cortex (DLPFC)
- Localization: 6 cm anterior to motor hotspot for abductor pollicis brevis
- Intensity: 120% of resting motor threshold
- Frequency: 10 Hz stimulation
- Pulse Structure: 2.4-second trains with 15-second intertrain intervals
- Treatment Schedule: 6 days over 3 weeks, with 3 daily sessions (83, 83, and 84 trains per session) separated by 15-minute breaks
- Total Pulses: 10,500 per day (63,000 total per patient)
Outcome Assessment: Standardized HDRS and Clinical Global Impression (CGI) scales at baseline and week 3, with response defined as ≥50% HDRS reduction and remission as HDRS score <7 [91].
DBS Surgical Protocol for TRD
Patient Selection: Severe unipolar depression lasting >5 years with resistance to medications, psychotherapy, and electroconvulsive therapy.
Surgical Planning:
- Target: Superolateral branch of the medial forebrain bundle (MFB)
- Imaging: Advanced tractography to map individual patient's reward circuitry
- Electrode Placement: Precision stereotactic implantation with intraoperative stimulation to identify the "sweet spot" based on immediate mood responses (increased energy, eye contact, motivation)
Stimulation Parameters: Individualized programming based on patient response, with long-term maintenance therapy [90].
Outcome Tracking: Montgomery-Åsberg Depression Rating Scale (MADRS) at 2 weeks, 12 weeks, 1 year, and up to 5 years, demonstrating sustained antidepressant effects [90].
Mebufotenin (GH001) Pharmaceutical Trial Design
Trial Structure: Randomized, double-blind, placebo-controlled Phase 2b clinical trial in TRD patients.
Administration: Proprietary inhalation approach allowing for precise dosing.
Endpoint Assessment: Primary efficacy endpoint measured as change in MADRS score from baseline to Day 8, with additional safety and tolerability monitoring throughout the trial period [93].
Mechanisms of Action: Signaling Pathways
Bioelectronic Medicine Pathways
Vagus Nerve Stimulation (VNS) operates through afferent modulation of limbic circuits, sending impulses from the left cervical vagus nerve to the nucleus tractus solitarius (NTS), which then projects to key mood-regulating regions including the locus coeruleus [92]. This pathway enhances norepinephrine release and facilitates neuroplasticity while potentially exerting anti-inflammatory effects, creating a comprehensive neuromodulatory approach that develops over months but demonstrates remarkable durability [92].
Deep Brain Stimulation of the medial forebrain bundle directly targets the brain's reward system by engaging dopaminergic pathways connecting the ventral tegmental area to the prefrontal cortex [90]. This "reboot" of the reward circuitry explains the rapid mood improvement observed within weeks of stimulation initiation and the sustained efficacy over years, particularly when targeting intact reward circuitry confirmed through advanced imaging.
Repetitive Transcranial Magnetic Stimulation applies electromagnetic induction to superficial cortical regions, with left DLPFC stimulation modulating dysfunctional neural networks through synaptic plasticity mechanisms. The accelerated high-frequency protocol (10 Hz) enhances neuroplasticity through increased pulse administration, potentially inducing more robust and rapid network reorganization [91].
Pharmaceutical Pathway
Mebufotenin (GH001) represents a novel approach targeting the glutamate system, a departure from conventional monoaminergic antidepressants [88] [93]. As an NMDA receptor modulator, it rapidly restores synaptic homeostasis and promotes neuroplasticity, explaining the dramatic antidepressant effects observed within days rather than weeks in clinical trials [93].
Research Reagent Solutions for TRD Investigations
Table 3: Essential research materials for TRD intervention studies
| Category | Specific Reagents/Tools | Research Function |
|---|---|---|
| Neuromodulation Equipment | TMS machines with H1 coils, DBS electrode systems, VNS implantable pulse generators | Precise delivery of electrical/magnetic stimulation to target neural circuits |
| Neuroimaging Materials | Tractography software, MRI-compatible localization systems | Target identification, surgical planning, and treatment individualization |
| Assessment Tools | MADRS, HDRS, CGI rating scales | Standardized quantification of treatment response and remission |
| Surgical Implantation | Stereotactic systems, implantable pulse generators, electrodes | Precise device placement for invasive neuromodulation approaches |
| Pharmaceutical Development | Mebufotenin formulation, inhalation delivery devices | Controlled administration of novel rapid-acting antidepressants |
The expanding therapeutic landscape for treatment-resistant depression demonstrates distinct complementary strengths across bioelectronic and pharmaceutical domains. Bioelectronic approaches like DBS, VNS, and rTMS offer durable, sustained relief for chronic TRD, with particularly impressive long-term outcomes observed in DBS targeting the medial forebrain bundle. In contrast, novel pharmaceuticals like mebufotenin provide unprecedented rapidity of onset, potentially revolutionizing acute intervention for severe depressive states. The optimal positioning of these interventions within treatment algorithms will depend on individual patient factors including treatment history, symptom acuity, and specific pathophysiological mechanisms. Future research should prioritize personalized medicine approaches that match specific TRD subtypes with their most appropriate intervention based on biomarker profiles and mechanistic considerations.
In the evolving landscape of modern medicine, two distinct therapeutic paradigms—pharmaceuticals and bioelectronic medicine—present fundamentally different risk profiles. Pharmaceutical outcomes research traditionally focuses on systemic drug toxicity, where chemical entities distribute throughout the body via the bloodstream, potentially causing off-target effects and organ-specific damage [94]. In contrast, bioelectronic medicine employs targeted device-specific risks, where implanted or wearable electronic devices interface with neural circuits and organs, presenting challenges related to biocompatibility, mechanical failure, and localized tissue response [31] [6]. This comparison guide objectively analyzes these divergent safety considerations through their underlying mechanisms, testing methodologies, and risk mitigation strategies, providing researchers and drug development professionals with a structured framework for evaluating these complementary therapeutic approaches within their development pipelines.
Fundamental Mechanisms: Chemical Toxicity vs. Biophysical Risks
Systemic Drug Toxicity Pathways
Pharmaceutical toxicity primarily arises from biochemical interactions at molecular targets. Investigative toxicology has evolved from descriptive observation to mechanistic understanding, focusing on how small molecules cause cellular damage through specific pathways [94]. Key mechanisms include:
- Off-target pharmacological activity: Drugs binding to unintended receptors, ion channels, or enzymes, leading to adverse physiological effects. Secondary pharmacology profiling has become standard practice to identify these interactions early in development [94].
- Cellular stress pathways: Mitochondrial dysfunction, oxidative stress, and glutathione depletion that can lead to organ damage, particularly in the liver [94].
- Bioactivation to reactive metabolites: Conversion of parent compounds to chemically reactive species that covalently bind to cellular macromolecules, causing direct cytotoxicity or immune-mediated responses [94].
- Idiosyncratic reactions: Unpredictable, non-dose-dependent toxicities that manifest only in susceptible individuals, often discovered only during clinical trials or post-marketing surveillance [94].
Bioelectronic Device Risk Mechanisms
Bioelectronic medicine risks stem from the physical presence and operation of devices within the biological environment. Unlike systemic drugs, these risks are typically localized but persistent [95]:
- Foreign body response: A cascade of immune reactions beginning with protein adsorption, followed by acute inflammation, chronic inflammation, foreign body giant cell formation, and fibrous capsule development that can isolate the device and impair function [95].
- Mechanical mismatch: Rigid or semi-rigid implants interacting with soft, dynamic tissues causing chronic irritation, inflammation, and potential tissue damage [31] [6].
- Electrochemical tissue damage: Charge injection at electrode-tissue interfaces exceeding safe charge density limits, leading to pH changes, electrode dissolution, and tissue injury [95].
- Device failure modes: Including insulation failure, conductor breakage, connector issues, and hermiticity loss in packaging that allows moisture ingress and circuit failure [95].
Table 1: Comparative Risk Mechanisms in Pharmaceuticals vs. Bioelectronic Medicine
| Risk Category | Pharmaceuticals | Bioelectronic Devices |
|---|---|---|
| Primary Mechanism | Biochemical interactions | Physical presence & operation |
| Spatial Distribution | Systemic | Localized with potential systemic effects |
| Temporal Profile | Often dose-dependent & transient | Often continuous & persistent |
| Predictive Models | In vitro cell cultures, organ-on-chip, animal models [94] | Biocompatibility testing, accelerated aging, mechanical testing [96] [95] |
| Susceptibility Factors | Metabolic polymorphisms, organ function, drug interactions | Tissue integrity, immune status, anatomical factors |
Methodological Approaches: Toxicity Testing vs. Biocompatibility Assessment
Pharmaceutical Toxicity Evaluation
Modern drug development employs a tiered approach to toxicity assessment, moving from early screening to comprehensive evaluation:
- In vitro screening systems: Including hepatocyte cultures, HepaRG cells, 3D hepatocyte spheroids, and liver-on-chip models to predict human drug-induced liver injury (DILI) [94]. These systems evaluate cytotoxicity, mitochondrial dysfunction, and bile salt accumulation.
- Secondary pharmacology profiling: Broad screening against panels of receptors, ion channels, and enzymes to identify potential off-target activities that could lead to adverse effects [94]. Standard panels often include 100+ targets with established clinical translation.
- Computational toxicology: Machine learning models trained on chemical structures and historical toxicity data to predict potential liabilities [94]. These include quantitative structure-activity relationship (QSAR) models and more recently, deep learning approaches.
- Mechanistic investigations: Follow-up studies to understand the molecular pathways underlying observed toxicities, including transcriptomics, proteomics, and metabolomics [94].
The following diagram illustrates the integrated pharmaceutical toxicity assessment workflow:
Medical Device Safety Assessment
Device evaluation follows a different pathway focused on material properties and biological responses:
- Chemical characterization: Comprehensive analysis of extractables and leachables to identify potentially harmful chemicals that might migrate from device materials [96]. This follows ISO 10993-18 standards and includes risk assessment of identified compounds.
- Biocompatibility testing: Evaluation of local tissue effects following ISO 10993 series standards, including cytotoxicity, sensitization, irritation, and implantation tests [96]. The testing matrix depends on device nature and contact duration.
- Toxicological risk assessment: Quantitative assessment of potential exposure to leachables and comparison to established safety thresholds such as allowable limits based on carcinogenicity, genotoxicity, and other toxicological endpoints [96].
- Mechanical reliability testing: Accelerated aging, fatigue testing, and integrity testing under simulated physiological conditions to predict long-term performance [95].
The contrasting workflow for device evaluation emphasizes physical and local biological effects:
Quantitative Risk Comparison: Data and Outcomes
Pharmaceutical Toxicity Data
Drug toxicity manifests across multiple organ systems with varying incidence:
Table 2: Pharmaceutical Systemic Toxicity Profiles
| Toxicity Type | Incidence in Development | Detection Methods | Typical Onset |
|---|---|---|---|
| Drug-Induced Liver Injury (DILI) | Major cause of drug attrition & post-market withdrawals [94] | Hepatocyte models, liver spheroids, liver-on-chip [94] | Days to months |
| Cardiotoxicity (hERG inhibition) | ~30% of new chemical entities show some hERG affinity [94] | hERG patch clamp, stem cell-derived cardiomyocytes | Hours to days |
| Renal Toxicity | ~20% of acute kidney injury cases in hospitalized patients [94] | Renal proximal tubule cells, 3D kidney models | Days to weeks |
| CNS Toxicity | Common in early discovery (up to 40% of compounds) [94] | Secondary pharmacology screening, neuronal cell models | Minutes to hours |
| Idiosyncratic Reactions | Rare (1 in 1,000 to 1 in 100,000) but serious [94] | Often undetected until large-scale clinical trials | Variable |
Bioelectronic Device Adverse Events
Device risks reflect different failure modes and local tissue effects:
Table 3: Bioelectronic Device-Specific Risk Profiles
| Risk Category | Incidence/Prevalence | Assessment Methods | Typical Manifestation |
|---|---|---|---|
| Foreign Body Response | Nearly universal with variations in severity [95] | Histopathology, imaging, functional assessment | Weeks to months |
| Device Failure | 5-15% over 5 years depending on device complexity [95] | Accelerated aging, electrical testing, monitoring | Months to years |
| Infection at Implant Site | 1-27% across different neural interfaces [95] | Microbial culture, inflammatory markers | Days to months |
| Mechanical Tissue Damage | Varies with implantation site and device size [31] [95] | Medical imaging, histology, functional assessment | Immediate to chronic |
| Electrode-Tissue Interface Failure | Progressive over months to years in recording electrodes [95] | Electrochemical impedance spectroscopy, signal quality | Months to years |
The Scientist's Toolkit: Essential Research Solutions
Table 4: Key Research Tools for Toxicity and Risk Assessment
| Tool/Category | Function/Application | Examples/Models |
|---|---|---|
| In Vitro Hepatocyte Models | Prediction of drug-induced liver injury [94] | Primary human hepatocytes, HepaRG cells, 3D spheroids, stem cell-derived hepatocytes |
| Organ-on-Chip Systems | Physiologically-relevant toxicity screening with human cells [94] | Liver-chip, multi-organ systems, disease models |
| Secondary Pharmacology Panels | Identification of off-target interactions [94] | CEREP, Eurofins, Panlabs standardized panels (100+ targets) |
| Chemical Characterization Platforms | Identification of extractables and leachables from devices [96] | LC-MS, GC-MS, ICP-MS following ISO 10993-18 |
| Biocompatibility Test Systems | Evaluation of local tissue effects [96] | ISO 10993-5 (cytotoxicity), ISO 10993-10 (sensitization) |
| Accelerated Aging Systems | Prediction of device longevity and failure modes [95] | Environmental chambers, electrochemical testing, mechanical fatigue testers |
| Computational Toxicology Platforms | Early prediction of chemical liabilities [94] | QSAR tools, machine learning algorithms, database mining (ChEMBL) |
Pharmaceutical and bioelectronic therapeutic approaches present fundamentally different risk paradigms that necessitate specialized assessment methodologies. Systemic drug toxicity arises from biochemical interactions that may affect multiple organ systems, often in a dose-dependent manner, with risks frequently predicted through in vitro and computational models [94]. In contrast, bioelectronic device risks stem primarily from physical presence and operation, resulting in localized tissue responses and device failure modes that require material science and engineering solutions [96] [95].
The optimal therapeutic strategy depends on multiple factors including disease pathophysiology, treatment duration, and patient-specific factors. Future convergence may emerge through combination products—devices with drug-eluting capabilities or bioelectronics with pharmacological adjuncts—that will require integrated safety assessment approaches. For researchers and development professionals, understanding these distinct risk profiles enables more informed therapeutic choices and development strategies tailored to each modality's unique characteristics and constraints.
The escalating global healthcare expenditures, which reached an estimated $4.9 trillion in the United States alone in 2023, have intensified the focus on economic evaluation frameworks for therapeutic interventions [97]. Within this context, two distinct approaches—bioelectronic medicine and pharmaceutical outcomes research—are being rigorously evaluated through the dual lenses of long-term cost efficiency and value-based reimbursement. Bioelectronic medicine represents a transformative approach that utilizes implantable or wearable electronic devices to interface with electrically active tissues, offering precise neuromodulation for conditions ranging from chronic pain to Parkinson's disease [1] [6]. Conversely, pharmaceutical outcomes research has evolved to incorporate sophisticated value-assessment methodologies, including cost-effectiveness analysis (CEA) and innovative contracting models that tie reimbursement to real-world performance [98] [99]. This analysis provides a structured comparison of the economic models, reimbursement mechanisms, and value propositions of these therapeutic paradigms, offering researchers, scientists, and drug development professionals evidence-based insights for resource allocation and research investment decisions.
Fundamental Economic Principles and Reimbursement Frameworks
Value-Based Reimbursement Fundamentals
Value-based reimbursement represents a significant departure from traditional fee-for-service models by linking payment to outcomes rather than volume of services [100]. This approach is fundamentally centered on the concept of value, defined as delivering better health outcomes without proportionally increasing costs [100]. The implementation of value-based models varies considerably, ranging from capitation (fixed payments per patient population) to bundled payments (fixed payments for entire care episodes) and outcomes-based contracts (payments tied directly to clinical results) [100] [99]. These models redistribute financial risk among stakeholders, creating incentives for delivering efficient, high-quality care while discouraging unnecessary interventions and costs.
Pharmaceutical Value Assessment
In pharmaceuticals, value assessment increasingly relies on formal cost-effectiveness analysis (CEA), which quantifies the additional cost required to gain one unit of health benefit, typically measured in quality-adjusted life years (QALYs) [97] [98]. The results are expressed as an incremental cost-effectiveness ratio (ICER), which is compared against willingness-to-pay thresholds—typically $50,000-$200,000 per QALY in the United States—to determine whether an intervention provides sufficient value [97] [98]. This methodology has become the gold standard for health technology assessment globally, though its application varies across healthcare systems and economic contexts.
Table 1: Key Economic Evaluation Metrics in Therapeutic Development
| Metric | Definition | Application in Pharmaceuticals | Application in Bioelectronic Medicine |
|---|---|---|---|
| Incremental Cost-Effectiveness Ratio (ICER) | Additional cost per unit of health benefit gained | Primary decision metric for reimbursement of new drugs [98] | Emerging application for novel bioelectronic devices [1] |
| Quality-Adjusted Life Year (QALY) | Measure of disease burden considering quality and quantity of life | Standard outcome measure in cost-utility analysis [97] [98] | Used in economic evaluations of neuromodulation therapies [1] |
| Willingness-to-Pay Threshold | Maximum amount a payer will pay for a unit of health benefit | Typically $50,000-$200,000 per QALY in the US [97] | Similar thresholds applied, but with consideration of device longevity [1] [6] |
| Budget Impact | Short-term financial consequence of adopting an intervention | Critical consideration for pharmacy budget management | Significant upfront investment with long-term offset potential [1] [10] |
Comparative Economic Analysis: Bioelectronic Medicine vs. Pharmaceuticals
Bioelectronic Medicine Economics
Bioelectronic medicine offers a distinctive economic profile characterized by substantial initial investment but potential for long-term cost efficiency. The global bioelectronic medicine market was valued at $23.54 billion in 2024 and is projected to reach $33.59 billion by 2030, growing at a compound annual growth rate (CAGR) of 6.10% [10]. This growth trajectory reflects increasing adoption driven by several economic advantages, including reduced pharmaceutical utilization through targeted neuromodulation, minimal systemic side effects that decrease management costs, and continuous therapeutic effect without repeated dosing [1]. Advanced bioelectronic systems increasingly incorporate closed-loop feedback mechanisms that automatically adjust stimulation parameters based on real-time physiological signals, optimizing therapeutic efficacy while conserving energy [6]. For chronic conditions requiring lifelong management, the one-time investment in bioelectronic devices can potentially replace decades of pharmaceutical expenditures, fundamentally altering the long-term economic equation for payers and health systems [1].
The economic case for bioelectronic medicine is further strengthened by emerging technological innovations. Battery-less implants utilizing wireless power transfer technologies reduce the need for surgical replacement and associated costs [1]. Similarly, the development of bioresorbable materials that safely dissolve in the body over time eliminates explantation procedures and related expenses [6]. The shift toward soft and flexible bioelectronics addresses the critical challenge of mechanical mismatch with biological tissues, significantly reducing inflammation, fibrosis, and device failure rates that historically compromised long-term cost efficiency [6]. These technological advances collectively enhance the durability and longevity of bioelectronic interventions, improving their economic profile through reduced complication rates and maintenance requirements.
Pharmaceutical Economics and Outcomes-Based Contracting
Pharmaceutical cost structures differ substantially from bioelectronic approaches, typically featuring ongoing per-dose costs throughout the treatment duration. In response to escalating drug prices—particularly for specialty medications and gene therapies that often exceed $100,000 per patient annually—the industry has increasingly explored value-based contracting (VBC) [99]. These arrangements, also termed outcomes-based or performance-based contracting, link drug reimbursement to real-world clinical or economic performance through various mechanisms:
- Outcomes-based agreements: Manufacturer provides rebates or refunds if therapy fails to achieve predefined clinical targets (e.g., biomarker levels, hospitalization rates) [99]
- Financial-risk arrangements: Spending caps or risk-sharing models that limit financial exposure for payers [99]
- Subscription models: Fixed fees for unlimited treatment access over a specified period, as implemented for hepatitis C therapeutics in some Medicaid programs [99]
Despite theoretical appeal, practical implementation of pharmaceutical value-based contracts faces significant challenges. A systematic evaluation found that these agreements apply to only a narrow subset of drugs and have not demonstrated conclusive evidence of reducing overall spending or improving quality [99]. Barriers include difficulty defining appropriate outcome measures, operational complexity in tracking patient results across care settings, regulatory constraints such as Medicaid "best price" rules, and contractual complexity that increases negotiation costs [99].
Table 2: Economic and Reimbursement Profile Comparison
| Characteristic | Bioelectronic Medicine | Pharmaceutical Interventions |
|---|---|---|
| Cost Structure | High upfront device and implantation costs; lower long-term maintenance [1] [10] | Ongoing per-dose costs throughout treatment duration [99] |
| Reimbursement Models | Device reimbursement under diagnosis-related groups (DRGs) or technology-specific payments; evolving outcomes-based approaches [1] [100] | Traditional volume-based pricing with evolving outcomes-based contracts [100] [99] |
| Risk Distribution | Provider/payer assumes device efficacy risk; manufacturer typically responsible for device reliability [1] [6] | Manufacturer risk-sharing through rebates for underperformance in value-based contracts [99] |
| Economic Evaluation Timeframe | Long-term (5-10+ years) to capture device longevity and replacement cycles [1] [6] | Varies by condition; often medium-term for chronic diseases [98] [99] |
| Key Cost Drivers | Device complexity, implantation procedure, battery life, follow-up programming [1] [10] | Drug acquisition price, administration, monitoring, side effect management [98] [99] |
Clinical Decision-Making and Economic Evaluation Methodologies
Cost-Effectiveness Analysis Framework
Economic evaluation of both bioelectronic and pharmaceutical interventions increasingly employs standardized cost-effectiveness analysis methodologies to enable cross-paradigm comparisons. These analyses calculate the incremental cost-effectiveness ratio (ICER) by comparing the difference in costs between interventions to the difference in their health outcomes [97] [98]. The analysis typically incorporates quality-adjusted life years (QALYs) to capture both survival and quality-of-life impacts, though therapeutic area-specific outcome measures may also be utilized [97]. Robust CEA incorporates sensitivity analyses to account for parameter uncertainty and contextual factors that may vary across healthcare systems and patient populations [97].
Experimental Protocols for Economic Evaluation
Robust economic evaluation requires standardized methodologies to ensure comparability across interventions:
Protocol 1: Time-Driven Activity-Based Costing (TDABC) for Resource Utilization
- Objective: Precisely measure resource consumption throughout the complete care cycle for specific clinical conditions [100]
- Methodology:
- Map the complete patient care pathway from diagnosis through treatment and follow-up
- Identify all personnel, equipment, space, and supply costs at each process step
- Measure time required for each activity and calculate cost based on practical capacity
- Calculate total cost by aggregating across all activities in the care pathway [100]
- Application: Particularly valuable for quantifying the true economic impact of bioelectronic device implantation versus long-term pharmaceutical management
Protocol 2: Real-World Evidence Generation for Outcomes-Based Agreements
- Objective: Collect robust clinical and economic data to support value-based contracting [99]
- Methodology:
- Define clinically meaningful, measurable endpoints appropriate for the therapeutic area
- Establish data collection infrastructure across care settings (electronic health records, claims data, patient-reported outcomes)
- Implement risk adjustment methodologies to account for patient population differences
- Define explicit performance thresholds triggering financial reconciliation [99]
- Application: Essential for implementing outcomes-based pharmaceutical contracts and emerging applications in bioelectronic medicine
Market Evolution and Future Trajectory
Bioelectronic Medicine Market Dynamics
The electroceuticals and bioelectronic medicine market demonstrates robust growth potential, projected to reach $19,350 million by 2025 with continued expansion anticipated through 2033 [101]. This growth is propelled by multiple factors, including technological advancements in device miniaturization, wireless capabilities, and closed-loop systems; increasing prevalence of chronic neurological and cardiovascular conditions in aging populations; and growing physician and patient acceptance of neuromodulation approaches [101] [10]. The competitive landscape features established medical device companies (Medtronic, Abbott, Boston Scientific) alongside emerging innovators focusing on niche applications and technological disruptions [101] [10].
North America currently dominates the bioelectronic medicine market due to high healthcare expenditure, advanced medical infrastructure, and favorable reimbursement frameworks, though the Asia-Pacific region exhibits the most promising growth trajectory driven by expanding healthcare access and rising disposable incomes [101] [10]. Therapeutically, neuromodulation for pain management and cardiac rhythm management constitute the largest application segments, reflecting the established efficacy and economic evidence for these indications [101].
Pharmaceutical Reimbursement Evolution
Pharmaceutical reimbursement is undergoing a fundamental transformation from volume-based to value-based paradigms, though implementation challenges persist. While outcomes-based contracts have generated substantial interest, they currently apply to only a small subset of drugs—primarily in therapeutic areas with clear, measurable short-term endpoints such as diabetes, cardiology, and oncology [99]. The most successful implementations have involved straightforward outcome measures (e.g., biomarker response, hospitalization avoidance) with established data collection infrastructure [99].
Future evolution of pharmaceutical reimbursement will likely be shaped by several converging trends: regulatory reforms such as the Inflation Reduction Act in the U.S. that introduce direct price negotiation; advances in real-world evidence generation through improved data interoperability and analytics; and growing political pressure to address drug pricing sustainability [99]. Additionally, the emergence of curative therapies with multimillion-dollar price tags is driving innovation in alternative financing models, including installment payments, annuities, and population-level subscription agreements [99].
Table 3: Market Characteristics and Future Outlook
| Parameter | Bioelectronic Medicine | Pharmaceuticals |
|---|---|---|
| Current Market Size | $23.54 billion (2024) [10] | $675 billion US retail spending (2021) [99] |
| Projected Growth | 6.10% CAGR (2024-2030) [10] | Varies by therapeutic class; specialty drugs growing rapidly [99] |
| Innovation Concentration | Miniaturization, closed-loop systems, battery-less devices, soft electronics [1] [6] | Targeted therapies, gene and cell therapies, orphan drugs [98] [99] |
| Adoption Barriers | High initial cost, specialized implantation expertise, device reliability concerns [6] [10] | High prices, outcomes measurement challenges, regulatory barriers to value-based contracts [99] |
| Future Directions | Bioresorbable materials, AI-optimized stimulation parameters, bidirectional neural interfaces [1] [6] | Expanded outcomes-based contracts, novel financing models for curative therapies [98] [99] |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for Economic and Therapeutic Evaluation
| Tool Category | Specific Solutions | Research Application | Relevance to Economic Analysis |
|---|---|---|---|
| Conductive Materials | PEDOT:PSS, graphene, MXenes, carbon nanotubes [1] | Neural interface development, impedance reduction | Impacts device longevity and performance - key cost drivers [1] [6] |
| Flexible Substrates | Silicones, polyimides, ultrathin films [6] | Mechanical compatibility with biological tissues | Reduces foreign body reaction and device failure - major cost factors [6] |
| Characterization Equipment | Electrochemical impedance spectroscopy, accelerated aging chambers [6] | Device reliability and stability assessment | Provides data for device longevity projections in economic models [6] |
| Computational Modeling | Markov models, microsimulation, decision trees [97] [98] | Cost-effectiveness analysis and outcomes projection | Essential for economic evaluation of both bioelectronic and pharmaceutical interventions [97] [98] |
| Real-World Data Analytics | Electronic health record systems, claims data analysis platforms [99] | Outcomes measurement for value-based contracts | Supports evidence generation for innovative reimbursement models [99] |
The comparative economic analysis of bioelectronic medicine and pharmaceutical interventions reveals distinctive yet complementary value propositions. Bioelectronic medicine offers a high initial investment profile with potential for long-term cost efficiency through durable therapeutic effects, reduced pharmaceutical utilization, and minimal systemic side effects [1] [10]. The field is rapidly evolving through technological innovations in device miniaturization, flexible electronics, and closed-loop systems that address historical limitations regarding device reliability and biocompatibility [6]. Conversely, pharmaceutical interventions are experiencing a transformation in reimbursement paradigms through value-based contracting approaches that seek to align payment with real-world clinical and economic performance [99]. Despite theoretical appeal, practical implementation of these models faces significant challenges including outcomes measurement complexity, data infrastructure limitations, and regulatory barriers [99].
For researchers, scientists, and drug development professionals, several strategic implications emerge. First, comprehensive economic evaluation must consider the full care cycle rather than isolated intervention costs, capturing downstream savings from reduced complications, hospitalizations, and concomitant treatments [100]. Second, robust real-world evidence generation is becoming increasingly crucial for demonstrating value in both bioelectronic and pharmaceutical domains, necessitating investment in data collection infrastructure and analytics capabilities [99]. Finally, therapeutic individualization represents a converging trend, with bioelectronic approaches offering programmable stimulation parameters and pharmaceutical interventions advancing through precision medicine approaches targeting specific patient subgroups [98] [99].
As both fields continue to evolve, the economic assessment framework will likely increasingly incorporate broader societal perspectives beyond direct healthcare costs, including productivity impacts, caregiver burden, and environmental considerations [1] [98]. The optimal allocation of research resources and therapeutic approaches will ultimately depend on condition-specific factors, including pathophysiology, treatment response variability, and the feasibility of targeted intervention. Through rigorous economic evaluation and innovative reimbursement models, both bioelectronic and pharmaceutical approaches can contribute to a more sustainable, value-driven healthcare system.
For researchers and drug development professionals, understanding the dynamics of patient preference and adherence is crucial when evaluating therapeutic strategies for chronic diseases. The rise of bioelectronic medicine presents a novel paradigm, challenging traditional chronic drug regimens that have long been the cornerstone of disease management. This guide provides an objective, data-driven comparison of these two approaches, focusing on their inherent challenges, adherence rates, and overall impact on clinical outcomes. The shift toward device-based interventions is driven by the need to overcome the significant limitations of pharmacological therapies, including systemic side effects, complex dosing schedules, and suboptimal long-term adherence [102] [6]. This analysis synthesizes current evidence to inform the development of more effective and patient-acceptable therapeutic solutions.
Comparative Adherence and Clinical Outcomes
Adherence is a pivotal factor determining the real-world effectiveness of any therapeutic intervention. For chronic conditions, the World Health Organization defines adherence as "the extent to which a person’s behavior—taking medication, following a diet, and/or executing lifestyle changes—corresponds with agreed recommendations from a healthcare provider" [103]. Despite its importance, non-adherence remains a pervasive challenge, contributing to suboptimal treatment results, higher complication rates, increased hospitalizations, and substantial healthcare expenditures [103].
The following table summarizes key adherence rates and corresponding clinical outcomes for both chronic drug regimens and device-based therapies across various conditions.
Table 1: Adherence Rates and Clinical Outcomes in Chronic Disease Management
| Disease/Condition | Therapy Type | Reported Adherence Rates | Impact on Clinical Outcomes | Key Supporting Evidence |
|---|---|---|---|---|
| Hypertension [103] [104] | Drug Regimen (Antihypertensives) | 53% - 71% | Poor BP control → ↑ risk of stroke, MI, heart failure, renal disease [103]. | Observational Studies |
| Type 2 Diabetes [104] | Drug Regimen (Oral Antidiabetics) | 42% - 67% (varies by region) | Better glycemic control → ↓ microvascular/macrovascular complications [103]. | Observational Studies |
| Cardiovascular Disease [103] | Drug Regimen (e.g., Beta-blockers, Statins) | Not explicitly quantified | Improved adherence → ↓ morbidity/mortality, ↓ hospital readmissions [103]. | Clinical Trial Analysis |
| Resistant Hypertension [105] | Device (Baroreflex Activation Therapy) | 50% achieved office SBP <140 mmHg at follow-up [105] | Significant reductions in systolic and diastolic BP reported [105]. | Barostim Neo Trial |
| Heart Failure [102] | Device (e.g., Implantable CRT/ICD) | Not directly measured (long-term intervention) | Reduces morbidity & mortality, promotes reverse cardiac remodeling [102]. | Pivotal RCTs (e.g., PARADIGM-HF) |
Analysis of Adherence Drivers
The disparity in adherence between pharmacological and device-based approaches can be attributed to several key factors:
- Regimen Complexity and Burden: Drug regimens for conditions like multidrug-resistant tuberculosis (MDR-TB) can involve taking multiple medications daily for 18-24 months, creating a significant burden that impacts adherence [106]. Device-based therapies, once implanted, function with minimal daily patient effort.
- Intentional vs. Unintentional Non-Adherence: With drug regimens, unintentional non-adherence (forgetfulness, confusion) is common, as is intentional non-adherence where patients consciously decide to skip doses due to fears of side effects, perceived ineffectiveness, or cost [104]. Device-based therapies largely circumvent these behavioral barriers.
- Side Effect Profiles: Fear of medication side effects is a major driver of non-adherence [104]. Bioelectronic devices, by targeting specific neural pathways, aim to offer a more localized effect with potentially fewer systemic side effects, though they carry procedural risks and unique long-term stability concerns [6].
Experimental and Methodological Approaches
Directly comparing drug and device therapies requires a robust methodological framework that accounts for their fundamental differences. The gold standard for evaluating efficacy remains the Randomized Controlled Trial (RCT), but its application varies between the two modalities.
Clinical Trial Designs and Protocols
Table 2: Key Clinical Trial Designs for Drug vs. Device Evaluation
| Aspect | Chronic Drug Regimens | Device-Based Therapies |
|---|---|---|
| Primary Trial Design | Parallel-group, double-blind, placebo-controlled RCTs. | Often single-arm or sham-controlled RCTs; blinding is challenging. |
| Control Group | Placebo is standard. | Standard of care or "sham" procedure (where ethically feasible). |
| Phases/Stages | 4 phases (I-IV), starting with healthy volunteers. | 3 stages (Early Feasibility, Pivotal, Post-Market). |
| Primary Endpoints | Survival, disease-specific clinical events, biomarker levels (e.g., HbA1c, BP). | Composite safety/effectiveness, functional improvement, technical performance. |
| Participant Population | Healthy volunteers (Phase I) then target disease population. | Only the target disease population. |
| Typical Duration | Often years per phase. | Typically shorter, more focused, but with long-term post-market surveillance. |
Drug trials typically follow a phased approach, establishing safety in healthy volunteers before progressing to large-scale efficacy trials in patients [107]. In contrast, device trials do not involve healthy volunteers and begin with small early feasibility studies (10-40 participants) to assess initial safety and device function in the target population, followed by larger pivotal studies (hundreds to thousands) designed to provide primary evidence for regulatory submission [107].
Signaling Pathways and Workflow Visualization
The fundamental mechanistic difference lies in how these therapies interact with the body's physiological systems. Drug regimens typically act through systemic biochemical pathways, whereas bioelectronic medicine targets specific neural signaling pathways to modulate organ function.
Diagram 1: Therapeutic action and adherence pathways.
The experimental workflow for evaluating these therapies in a clinical setting also differs significantly, particularly in terms of blinding, control groups, and outcome assessment.
Diagram 2: Comparative clinical trial workflows.
The Scientist's Toolkit: Research Reagent Solutions
Research into patient adherence and the comparative effectiveness of these therapies relies on a specific set of tools and methodologies.
Table 3: Essential Research Tools for Adherence and Outcomes Studies
| Tool/Reagent | Function/Application | Relevance to Therapy Type |
|---|---|---|
| Electronic Monitoring Systems [103] | Real-time tracking of medication bottle openings or device usage. | Primarily drugs; provides objective adherence data beyond self-reporting. |
| Biochemical Assays [103] | Direct measurement of drug or metabolite levels in blood/urine. | Gold standard for confirming drug ingestion; not applicable to devices. |
| Validated Adherence Questionnaires (e.g., MMAS-8) [103] | Assess patient-reported adherence behavior and beliefs. | Both drugs and devices; subject to recall and social desirability bias. |
| Sham Procedure Protocols [107] | Control intervention mimicking device implantation without active effect. | Critical for blinding in device trials to control for placebo effect. |
| Device Diagnostic Logs | Internal device data on stimulation delivery and system integrity. | Devices only; provides objective evidence of therapy delivery. |
| Ambulatory Blood Pressure Monitors [105] | 24-hour blood pressure profiling outside clinical setting. | Key for hypertension trials (both drugs and devices like BAT/RDN). |
The choice between device-based therapies and chronic drug regimens involves a complex trade-off between mechanistic precision, adherence profiles, and invasiveness. Chronic drug regimens, while minimally invasive and scalable, face significant challenges with long-term adherence due to daily burden, side effects, and cost, which ultimately compromise their clinical effectiveness [103] [104]. In contrast, device-based therapies like bioelectronic implants offer a one-time intervention with the potential for sustained, adherence-independent therapy, but introduce concerns related to long-term device reliability, stability, and initial procedural risk [105] [6].
For researchers and drug developers, this comparative analysis highlights that the future of chronic disease management may not be a choice of one over the other, but rather a strategic integration of both modalities. The growing field of bioelectronic medicine, supported by advances in materials science, flexible electronics, and closed-loop systems, presents a compelling alternative or adjunct for patients struggling with pharmacological regimens [6]. Future research should focus on predictive biomarkers to identify patients most likely to benefit from each approach, the development of next-generation, more durable bioelectronic devices, and hybrid therapeutic strategies that leverage the strengths of both paradigms to optimize patient outcomes.
The healthcare landscape is witnessing a paradigm shift with the emergence of bioelectronic medicine (BEM), a field that uses electrical signals to modulate neural circuits and biological functions to treat diseases. Also known as electroceuticals, this approach represents a fundamental departure from conventional pharmaceuticals by targeting the body's electrical signaling systems rather than molecular pathways [108] [21]. This analysis provides a comprehensive comparison between bioelectronic medicine and traditional pharmaceutical interventions, examining growth trajectories, key players, therapeutic applications, and future revenue pools. The convergence of technological innovation and clinical need is positioning bioelectronic medicine as a transformative force in managing chronic diseases, with distinct advantages and limitations compared to pharmaceutical alternatives.
Understanding this emerging field requires examining its scientific foundation. Bioelectronic medicine operates on the principle that the nervous system intricately regulates organ function and inflammatory responses through neural signals. By interfacing with electrically active tissues using implanted or wearable devices, BEM can modulate these signals with precision, offering targeted therapeutic effects without the systemic exposure characteristic of pharmaceutical compounds [21]. This targeted mechanism of action forms the basis for its comparative advantages in specific clinical contexts, particularly for chronic conditions requiring long-term management.
Comparative Market Metrics
The bioelectronic medicine market demonstrates robust growth potential, though estimates vary significantly across different analyst reports. The table below summarizes the projected market size and growth rates from multiple sources, reflecting the dynamic and evolving nature of this sector.
Table 1: Bioelectric Medicine Market Size and Growth Projections
| Source | 2024/2025 Base Value | 2030/2035 Projection | CAGR | Notes |
|---|---|---|---|---|
| Future Market Insights [108] | USD 25.9 billion (2025) | USD 46.8 billion (2035) | 6.1% | Includes implantable and non-implantable devices |
| Research and Markets [109] [10] | USD 23.54 billion (2024) | USD 33.59 billion (2030) | 6.10% | Focus on bioelectronic medicine |
| DataM Intelligence [110] [111] | USD 31.34 billion (2024) | USD 235.55 billion (2033) | 22.3% | Most aggressive growth projection |
| Precedence Research [112] | USD 25.48 billion (2025) | USD 47.28 billion (2034) | 7.12% | - |
| Coherent Market Insights [28] | USD 23.27 billion (2025) | USD 43.09 billion (2032) | 9.2% | - |
For context, the global pharmaceutical market is projected to reach approximately $1.6 trillion by 2025, excluding COVID-19 vaccine spending, growing at a CAGR of 3-6% from pre-pandemic levels [113]. This establishes the pharmaceutical industry's dominant scale while highlighting bioelectronic medicine's potential for more rapid expansion from its smaller base.
Key Market Growth Drivers
Several interconnected factors are propelling the bioelectronic medicine market forward, creating a favorable environment for its adoption and development.
Rising Prevalence of Chronic Diseases: The increasing global burden of cardiovascular, neurological, and metabolic disorders creates substantial demand for effective long-term therapies [109] [10] [110]. According to the World Health Organization, cardiovascular diseases account for nearly 17.9 million deaths annually, while the International Diabetes Federation estimates 537 million adults lived with diabetes in 2021, projected to rise to 643 million by 2030 [109] [10].
Aging Global Population: Demographic shifts toward older populations are significant, with one in six individuals expected to be over 65 by 2050 [109] [10]. Elderly patients are more vulnerable to chronic illnesses and often experience adverse drug reactions, making non-pharmaceutical alternatives particularly appealing.
Technological Advancements: Innovations in miniaturization, wireless connectivity, battery technology, and biocompatible materials are enhancing device performance, patient comfort, and treatment efficacy [108] [21] [28]. The integration of artificial intelligence allows for personalized stimulation parameters and adaptive therapy delivery [109] [10] [28].
Clinical and Regulatory Validation: Increasing regulatory approvals and growing clinical evidence supporting the efficacy of bioelectronic interventions are encouraging broader adoption in medical practice [108]. For instance, in June 2025, Fasikl received FDA 510(k) clearance for its Felix NeuroAI Wristband for essential tremor management [28].
Product and Application Landscape
Product Segment Analysis
The bioelectronic medicine market is segmented into various product categories, with implantable devices currently dominating the landscape due to their proven effectiveness in managing chronic conditions.
Table 2: Bioelectric Medicine Market by Product Segment
| Product Category | Market Share / Position | Key Applications | Representative Devices |
|---|---|---|---|
| Implantable Devices | 55.3% of market revenue (2025) [108] | Cardiovascular diseases, neurological disorders, chronic pain | Pacemakers, ICDs, DBS, SCS, VNS |
| Cardiac Pacemakers & Defibrillators | 22.3% of market revenue (2025) [108] | Arrhythmia, heart failure | Implantable cardioverter defibrillators (ICDs) |
| Neurostimulation Devices | Significant segment [109] | Chronic pain, Parkinson's, epilepsy | Spinal Cord Stimulators (SCS), Deep Brain Stimulators (DBS) |
| Cochlear Implants | Established segment [109] | Sensorineural hearing loss | Cochlear implants |
| Non-invasive Devices | Growing segment [112] | Pain management, migraine, wellness | TENS, external vagus nerve stimulators |
Implantable devices lead the market because they provide consistent, long-term therapeutic effects with minimal intervention once surgically placed [108]. Advances in materials science, wireless recharging, and miniaturization are enhancing their safety, comfort, and durability, strengthening patient acceptance. The segment's leadership is expected to continue as technology evolves with smarter sensors and AI integration [108].
Therapeutic Application Comparison
Bioelectronic medicine demonstrates distinct therapeutic profiles compared to pharmaceuticals across various conditions, with particular strength in specific clinical areas.
Table 3: Therapeutic Application Analysis: Bioelectronic Medicine vs. Pharmaceuticals
| Therapeutic Area | Bioelectronic Medicine Applications | Traditional Pharmaceutical Approaches | Comparative Advantages of BEM |
|---|---|---|---|
| Cardiovascular | Arrhythmia (19.8% market share) [108]; Heart failure | Beta-blockers, anticoagulants, antiarrhythmics | Targeted intervention; reduced systemic side effects [21] |
| Neurological | Parkinson's disease, Epilepsy, Chronic pain | Levodopa, antiepileptics, analgesics | Reversible, adjustable therapy; less dependency on medication [108] |
| Metabolic | Emerging applications for diabetes, obesity | GLP-1 agonists (e.g., semaglutide), insulin | Potential for reduced chemical side effects [21] |
| Immunology/Inflammation | Emerging for rheumatoid arthritis, IBD | Biologics, DMARDs, corticosteroids | Localized action; potentially fewer immunosuppressive effects [21] |
| Hearing Loss | Sensorineural hearing loss (cochlear implants) | Limited pharmaceutical options | Restores function where drugs are ineffective [109] |
The arrhythmia application segment dominates the bioelectronic medicine market, accounting for 19.8% of revenue in 2025 [108]. This leadership position is driven by the rising prevalence of irregular heart rhythms and the proven ability of devices like pacemakers and defibrillators to restore normal cardiac rhythm and prevent sudden cardiac death [108].
Key Players and Competitive Landscape
Market Leaders and Their Positions
The bioelectronic medicine market features a mix of established medical device companies and specialized firms driving innovation in the sector.
Table 4: Key Players in the Bioelectronic Medicine Competitive Landscape
| Company | Market Position / Focus Areas | Key Products / Technologies | Recent Developments |
|---|---|---|---|
| Medtronic | Global leader in medical devices [108] [109] | Pacemakers, deep brain stimulators, spinal cord stimulators | - |
| Abbott Laboratories | Major cardiovascular and neuromodulation player [108] [109] | Implantable cardioverter defibrillators, DBS systems | - |
| Boston Scientific | Significant cardiovascular focus [108] [109] | Implantable devices, spinal cord stimulators | FDA approval for Vercise Neural Navigator 5 software (July 2023) [110] |
| Cochlear Ltd. | Hearing loss solutions leader [108] [109] | Cochlear implants | - |
| LivaNova PLC | Specialized in neuromodulation [108] [109] | Vagus nerve stimulation systems | - |
| electroCore, Inc. | Non-invasive vagus nerve stimulation [110] [111] | TAC-STIM, Truvaga Plus | Next-gen TAC-STIM availability (June 2024); Truvaga Plus launch (April 2024) [110] [28] |
The competitive landscape extends beyond these established players to include a thriving startup ecosystem focused on innovations in neuromodulation, AI-assisted therapy optimization, and wearable devices [112]. These emerging companies are attracting investments and partnerships, accelerating the development of personalized, non-pharmacological treatments for chronic and complex diseases.
Regional Market Analysis
The adoption and development of bioelectronic medicine varies significantly across geographic regions, influenced by healthcare infrastructure, regulatory environments, and market maturity.
Table 5: Regional Analysis of Bioelectronic Medicine Market
| Region | Market Position | Growth Drivers | Country-Specific Insights |
|---|---|---|---|
| North America | Dominant (38-44% share) [112] [28] | Advanced healthcare infrastructure; high healthcare expenditure; favorable reimbursement; key player presence | U.S. market valued at USD 9.7B (2025), projected to reach USD 16.0B by 2035 [108] |
| Europe | Significant market share [108] [111] | Robust healthcare systems; leading medical device companies; favorable regulatory environments | Germany: 7.0% CAGR; UK: 5.8% CAGR; France: 6.4% CAGR [108] |
| Asia Pacific | Fastest-growing region [110] [112] [111] | Large patient population; rising healthcare investments; expanding healthcare infrastructure; growing awareness | China: 8.2% CAGR; India: 7.6% CAGR [108] |
| Latin America, Middle East & Africa | Emerging markets [108] | Improving healthcare access; increasing healthcare expenditure | Brazil: 4.6% CAGR (lowest among major countries) [108] |
North America's leadership position stems from its highly developed healthcare infrastructure, substantial investment in research and development, and the presence of major medical device manufacturers [112]. The region also benefits from early adoption of advanced therapies for chronic and neurological conditions, coupled with supportive regulatory and reimbursement policies that facilitate faster market uptake [112].
Technological and Clinical Comparison
Mechanisms of Action: Experimental Protocols
The fundamental difference between bioelectronic medicine and pharmaceuticals lies in their mechanisms of action, which can be illustrated through experimental approaches used to validate their effects.
Experimental Protocol 1: Bioelectronic Medicine Mechanism Validation
- Objective: To demonstrate targeted neural modulation of organ-specific inflammation using bioelectronic devices.
- Methodology:
- Neural Mapping: Identify specific neural pathways innervating target organs (e.g., spleen) through anatomical tracing and electrophysiological recording.
- Device Implantation: Surgically implant microelectrode arrays on identified peripheral nerves (e.g., vagus nerve) in animal models.
- Stimulation Parameters: Apply varying electrical stimulation patterns (frequency, amplitude, pulse width) while monitoring neural activity and organ function.
- Inflammatory Response Assessment: Measure cytokine levels (e.g., TNF-α, IL-1β) in target organs and systemic circulation following immune challenge.
- Control Groups: Include sham stimulation, surgical controls, and pharmaceutical comparator groups (e.g., TNF inhibitors).
- Outcome Measures: Neural signaling patterns, local versus systemic cytokine concentrations, physiological parameters, and histological analysis of target tissues.
Experimental Protocol 2: Pharmaceutical Mechanism Validation
- Objective: To characterize pharmacokinetic and pharmacodynamic properties of drug compounds and their systemic effects.
- Methodology:
- Dose-Response Studies: Administer escalating drug doses to establish efficacy and toxicity thresholds in cellular and animal models.
- Pharmacokinetic Profiling: Measure drug concentration over time in plasma and tissues to determine absorption, distribution, metabolism, and excretion.
- Target Engagement: Assess drug binding to intended molecular targets using radioligand binding assays and biomarker modulation.
- Off-Target Effects Screening: Evaluate activity against unrelated receptors, enzymes, and cellular pathways to identify potential side effects.
- Therapeutic Window Determination: Compare efficacy doses with those causing adverse effects in validated disease models.
- Outcome Measures: Drug concentration curves, biomarker modulation, histopathology of non-target tissues, clinical observation of adverse effects.
Signaling Pathway Visualization
The therapeutic mechanisms of bioelectronic medicine operate through fundamentally different pathways compared to pharmaceutical interventions, as illustrated in the following diagram:
Diagram 1: Therapeutic Mechanism Comparison
This visualization highlights the fundamental distinction between the targeted neural pathway of bioelectronic medicine and the systemic circulation pathway of pharmaceuticals, explaining their different side effect profiles.
The Scientist's Toolkit: Research Reagent Solutions
Research in bioelectronic medicine requires specialized materials and technologies that differ significantly from those used in pharmaceutical development. The following table details essential research tools and their applications in advancing the field.
Table 6: Essential Research Toolkit for Bioelectronic Medicine
| Research Tool Category | Specific Examples | Function in Bioelectronic Research |
|---|---|---|
| Electrode Materials | Conducting polymers (PEDOT:PSS), Graphene, MXenes, Carbon nanotubes [21] | Interface with neural tissue; balance conductivity with flexibility and biocompatibility |
| Implantable Electronics | Hermetically sealed pulse generators, Wireless power receivers, Signal processing units [21] | Generate and deliver controlled electrical stimulation; process recorded neural signals |
| Neural Interfaces | Microelectrode arrays, Flexible/stretchable electrodes, Utah arrays, Michigan probes [21] | Enable bidirectional communication with nervous system; record and stimulate neural activity |
| Biocompatible Encapsulation | Parylene-C, Silicon carbide, Medical-grade silicones [21] | Protect electronics from body fluids; minimize foreign body reaction |
| Signal Processing Systems | Neuromorphic circuits, AI algorithms for signal analysis, Machine learning classifiers [21] [28] | Interpret neural signals; detect disease biomarkers; optimize stimulation parameters |
| Experimental Models | Animal models of neurological disease, Isolated nerve preparations, Human organotypic cultures [21] | Validate device efficacy and safety; understand neural circuit mechanisms |
The development of advanced materials represents a particularly active research area, with conducting polymers emerging as promising candidates that seamlessly bridge the gap between biology and electronics due to their mixed ionic/electronic conductivity, mechanical flexibility, and enhanced biocompatibility [21].
Future Outlook and Strategic Implications
Emerging Trends and Revenue Pools
The future evolution of bioelectronic medicine is being shaped by several converging trends that will create new opportunities and revenue streams.
AI and Digital Health Integration: Artificial intelligence is playing an increasingly transformative role by enabling precise, personalized modulation of neural activity [109] [10] [28]. Advanced algorithms analyze bioelectrical data to identify abnormal signaling patterns and optimize stimulation parameters in real time, enhancing both efficacy and safety. The convergence of AI, data analytics, and bioelectronic medicine is paving the way for next-generation diagnostics and therapeutics while facilitating remote care and expanding treatment access [109] [10].
Expansion into New Therapeutic Areas: Bioelectronic medicine is rapidly moving beyond traditional cardiovascular and neurological applications into metabolic, inflammatory, and autoimmune disorders [21] [28]. Research is exploring conditions such as diabetes, rheumatoid arthritis, and inflammatory bowel disease, significantly broadening the addressable market. This expansion is driving innovation in device design and treatment strategies while positioning bioelectronic therapies as alternatives to conventional drugs across a wider spectrum of diseases.
Device Miniaturization and Battery-Less Systems: Technological advances are enabling smaller, smarter, and more efficient implantable and wearable devices [21] [28]. Research into battery-less implants using wireless power transfer techniques based on inductive/electrical or ultrasound methods represents a particularly promising direction [21]. These innovations support home-based care and remote patient monitoring while improving patient comfort and compliance.
Focus on Chronic Disease Management: Bioelectronic medicine presents significant opportunities in managing chronic conditions such as diabetes, cardiovascular disorders, and neurological diseases [28]. Unlike traditional pharmacological treatments, electroceutical therapies offer precise, targeted interventions that can reduce side effects. Companies can capitalize on this demand by developing specialized devices and therapy protocols tailored to different chronic conditions, thereby broadening their product portfolios and addressing unmet clinical needs [28].
Challenges and Limitations
Despite its promising trajectory, the bioelectronic medicine field faces several significant challenges that must be addressed to realize its full potential.
High Costs and Reimbursement Limitations: Advanced implantable devices involve complex manufacturing processes and high R&D investments, resulting in substantial costs that can limit accessibility, particularly in low- and middle-income countries [109] [10]. Additionally, reimbursement frameworks for bioelectronic therapies are inconsistent across regions, and insurance often doesn't fully cover treatment costs, creating financial burdens for patients [109] [10].
Technical and Biological Hurdles: Device-related complications including infections, malfunctions, and immune responses present significant challenges [110]. Foreign Body Reaction (FBR) is a process that inevitably occurs whenever foreign materials are inserted into the body, potentially leading to inflammation and reduced device efficacy over time [21]. Long-term use may require device replacements, increasing healthcare costs and patient concerns [110].
Regulatory and Adoption Barriers: Stringent regulatory requirements and lengthy approval processes can delay the introduction of new bioelectronic therapies to the market [111]. Additionally, both physicians and patients may be hesitant to adopt device-based therapies due to familiarity with pharmaceutical approaches or concerns about invasive procedures, creating adoption barriers even when clinical evidence supports efficacy.
This analysis demonstrates that bioelectronic medicine represents a distinct and rapidly evolving therapeutic modality with particular strengths in chronic disease management, especially for neurological and cardiovascular conditions. While the pharmaceutical industry continues to dominate overall healthcare spending, bioelectronic medicine is carving out significant niches where its targeted mechanism of action, reversible effects, and potential for reduced systemic side effects offer distinct advantages.
The most promising future likely involves integrated approaches that leverage the strengths of both modalities. Pharmaceutical therapies excel at systemic conditions and acute interventions, while bioelectronic approaches show particular promise for conditions with clear neural regulatory components and for patients who respond poorly to or cannot tolerate drug therapies. As technological innovations continue to address current limitations around device miniaturization, power management, and biocompatibility, and as clinical evidence continues to accumulate, bioelectronic medicine is poised to become an increasingly important component of the therapeutic arsenal, particularly in our evolving healthcare landscape that increasingly values personalized, targeted treatments with favorable side effect profiles.
Conclusion
The comparative analysis reveals that bioelectronic medicine is not a mere replacement for pharmaceuticals but a complementary pillar in the therapeutic arsenal. Its strengths lie in providing targeted, personalized, and adaptable treatment for specific conditions, often with superior side-effect profiles and potential for long-term cost savings. However, challenges related to device reliability, upfront costs, and regulatory complexity remain significant. The future of biomedical research lies in the convergence of these fields—developing hybrid therapies that combine the systemic reach of drugs with the precise neuromodulation of bioelectronics. Success will depend on interdisciplinary collaboration to advance closed-loop technologies, create sustainable business models, and generate robust real-world evidence, ultimately steering the industry towards more predictive, preventive, and patient-centric care.
References
- 1. The rise of bioelectronic medicine - BioMed Central [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-024-00151-8]
- 2. Practical Perspectives on Enhancing Predictive Modeling ... [https://link.springer.com/article/10.1007/s40495-025-00426-x]
- 3. New Drug Review 2025 [https://www.uspharmacist.com/article/new-drug-review-2025]
- 4. Invasive and Non-Invasive Neuromodulation for the Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294003/]
- 5. Emerging neuromodulation treatments for opioid and ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1570555/full]
- 6. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00179-4]
- 7. Emerging techniques for precision neuromodulation [https://www.the-innovation.org/article/doi/10.59717/j.xinn-life.2025.100150]
- 8. HCDT 2.0: A Highly Confident Drug-Target Database for ... [https://www.nature.com/articles/s41597-025-04981-2]
- 9. Genetics‐Based Targeting Strategies for Precise ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12302646/]
- 10. Bioelectronic Medicine Market Research Report 2025 ... [https://finance.yahoo.com/news/bioelectronic-medicine-market-research-report-151200955.html]
- 11. New Era of Electroceuticals - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8876842/]
- 12. Electroceuticals/Bioelectric Medicine Market Size and Share [https://www.mordorintelligence.com/industry-reports/electroceuticals-medicine-market]
- 13. Next generation bioelectronic medicine: making the case for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11748337/]
- 14. Advances in wearable and implantable devices for ... [https://link.springer.com/article/10.1007/s44291-025-00046-1]
- 15. Wireless bioelectronic devices for next-generation ... [https://www.sciencedirect.com/science/article/pii/S3050562325000455]
- 16. Physical insights and design principles for efficient wireless ... [https://www.sciencedirect.com/science/article/pii/S2666386425002267]
- 17. A Review of Wearable Electroceutical Devices for Chronic ... [https://www.mdpi.com/2079-9292/14/7/1376]
- 18. Understanding electrical and chemical transmission in the ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2024.1398862/full]
- 19. Electrical synapses and their functional interactions with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4091911/]
- 20. Synapse [https://en.wikipedia.org/wiki/Synapse]
- 21. The rise of bioelectronic medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11337583/]
- 22. Bioelectronics 'jump-start' the next wave of device ... [https://www.mckinsey.com/industries/life-sciences/our-insights/bioelectronics-jump-start-the-next-wave-of-device-therapeutics]
- 23. Electrical synapses: a dynamic signaling system that ... [https://www.sciencedirect.com/science/article/pii/S0005273604000410]
- 24. Connecting chemical structure to single cell signaling profiles [https://www.nature.com/articles/s42003-025-08545-3]
- 25. High‐Resolution Patterned Delivery of Chemical Signals From ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12272041/]
- 26. Expanding Global Work to Revolutionize Care of Older Adults [https://www.umaryland.edu/news/archived-news/january-2025/expanding-global-work-to-revolutionize-care-of-older-adults.php]
- 27. Pharmaceutical consumption: Health at a Glance 2025 [https://www.oecd.org/en/publications/2025/11/health-at-a-glance-2025_a894f72e/full-report/pharmaceutical-consumption_cd4ca729.html]
- 28. Bioelectric Medicine Market Size & Opportunities, 2025-2032 [https://www.coherentmarketinsights.com/market-insight/bioelectric-medicine-market-1757]
- 29. New paper creates roadmap for the next generation of ... [https://www.sciencedaily.com/releases/2025/01/250121162336.htm]
- 30. 2025 Pharmacy in Focus Report: GLP-1 Drugs [https://www.evernorth.com/pharmacy-in-focus-2025]
- 31. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 32. Personalized Medicine: Motivation, Challenges and Progress [https://pmc.ncbi.nlm.nih.gov/articles/PMC6366451/]
- 33. The environmental impact of data-driven precision medicine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10953742/]
- 34. Quantification of the environmental impact of radiotherapy ... [https://www.sciencedirect.com/science/article/pii/S1470204524001487]
- 35. Pacemaker vs Defibrillator: Which Device Is Right? [https://mycardiologist.net/pacemaker-vs-defibrillator-which-device-is-right/]
- 36. Implantable Defibrillators: Which Is the Best Device for Each ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530678/]
- 37. ACC/AHA/ASE/HFSA/HRS/SCAI/SCCT/SCMR 2025 ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/39808105/]
- 38. Heart Rhythm 2024 Spotlights New Developments in ... [https://www.hrsonline.org/news/hr24-spotlights-new-developments-cieds/]
- 39. MRI Safe Implantable Defibrillator Devices Market Size to ... [https://www.precedenceresearch.com/mri-safe-implantable-defibrillator-devices-market]
- 40. Pacemaker Interrogation Reports: Comparing Diagnostics ... [https://www.syncsci.com/journal/RIMA/article/view/RIMA.2025.01.002]
- 41. Deep brain stimulation surgical timing, outcomes, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12342336/]
- 42. Ameliorating motor performance and quality of life in ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1449973/full]
- 43. Chronic adaptive deep brain stimulation for Parkinson's ... [https://www.nature.com/articles/s41531-025-01124-7]
- 44. Long-term efficacy and predictors of vagus nerve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12400741/]
- 45. Long-term effects of invasive and transcutaneous vagus ... [https://link.springer.com/article/10.1007/s10309-025-00797-7]
- 46. Long-term efficacy and safety of vagus nerve stimulation in ... [https://www.sciencedirect.com/science/article/abs/pii/S0165032725019251]
- 47. Left and right vagus nerve stimulation - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339557/]
- 48. Electric Medicine: A Transformative HealthTech Sub-Sector in ... [https://www.healthcare.digital/single-post/electric-medicine-a-transformative-healthtech-sub-sector-in-2025]
- 49. addressing persistent doubts in spinal cord stimulation [https://janesthanalgcritcare.biomedcentral.com/articles/10.1186/s44158-024-00219-6]
- 50. Spinal Cord Stimulation (SCS) Clinical Data [https://www.bostonscientific.com/en-US/medical-specialties/pain-management/scs-clinical-data.html]
- 51. Medtronic receives FDA approval for Inceptiv™ closed ... [https://news.medtronic.com/2024-04-26-Medtronic-receives-FDA-approval-for-Inceptiv-TM-closed-loop-spinal-cord-stimulator]
- 52. Higher Preimplantation Opioid Doses Associated With ... [https://www.sciencedirect.com/science/article/pii/S1094715921001513]
- 53. FDA-Cleared Noninvasive Spine Stimulation System ... [https://www.embs.org/pulse/articles/fda-cleared-noninvasive-spine-stimulation-system-could-transform-spinal-cord-injury-treatment/]
- 54. Long-term Outcomes in Use of Opioids, Nonpharmacologic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9706399/]
- 55. Technical and Clinical Overview: Spinal Cord Stimulation [https://pubmed.ncbi.nlm.nih.gov/41003458/]
- 56. mechanisms and applications in closed-loop therapeutic ... [https://pubs.rsc.org/en/content/articlelanding/2024/tb/d4tb00782d]
- 57. PhD in Pharmaceutical Outcomes Research [https://pharmacy.cuanschutz.edu/degreesandprograms/phd-programs/pharmaceutical-outcomes-research]
- 58. Outcomes Research [https://www.amcp.org/concepts-managed-care-pharmacy/outcomes-research]
- 59. Type 1 Diabetes: Hybrid Closed-Loop and Open- ... [https://www.dzd-ev.de/en/press/press-releases/press-releases-2025/type-1-diabetes-hybrid-closed-loop-and-open-loop-systems]
- 60. Closed-loop therapy: recent advancements and potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7617697/]
- 61. Efficacy of an advanced hybrid closed-loop system in a ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1611540/full]
- 62. Singing The Body Electric: Exploring Bioelectronic Medicine [https://www.pharmasalmanac.com/articles/singing-the-body-electric-exploring-bioelectronic-medicine]
- 63. A biocompatible elastomeric organic transistor for ... [https://www.nature.com/articles/s41928-025-01444-9]
- 64. A state-of-the-Art review on edible electronics [https://www.sciencedirect.com/science/article/abs/pii/S0924224425000160]
- 65. Sustainable Soft Material Stores Energy for Flexible, ... [https://news.sustainability-directory.com/research/sustainable-soft-material-stores-energy-for-flexible-biocompatible-electronics/]
- 66. Effectiveness studies: advantages and disadvantages - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3181999/]
- 67. Drug outcomes research and policies [https://pmc.ncbi.nlm.nih.gov/articles/PMC11381405/]
- 68. Why clinical trial outcomes fail to translate into benefits for ... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-017-1870-2]
- 69. Bioelectronic Medicine: Home [https://bioelecmed.biomedcentral.com/]
- 70. Abstracts from the Sixth Bioelectronic Medicine Summit [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538809/]
- 71. Medical devices and pharmaceuticals: Two different worlds ... [https://www.medtecheurope.org/2015/11/04/medical-devices-and-pharmaceuticals-two-different-worlds-in-one-health-setting/]
- 72. FDA Medical Device Process: 2025 Pathway Guide [https://www.complizen.ai/post/fda-medical-device-approval-process]
- 73. The Complete Regulatory Pathway for Medical Devices: [https://synergbiopharma.com/regulatory-pathway-medical-devices/]
- 74. Regulatory landscape of accelerated approval pathways for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119601/]
- 75. EU MDR vs FDA: 2025 US-EU Medical Device Regulatory ... [https://www.complizen.ai/post/eu-mdr-vs-fda-complete-regulatory-comparison-guide-2025]
- 76. Rethinking FDA's Accelerated Approval Pathway [https://www.mcguirewoods.com/client-resources/alerts/2025/1/rethinking-fdas-accelerated-approval-pathway-new-draft-guidances-and-implications-for-drug-companies/]
- 77. Ten first-in-class drugs on track for FDA approval in 2025 [https://www.labiotech.eu/best-biotech/first-in-class-drugs-to-watch-2025/]
- 78. Foreign Body Reaction to Implanted Biomaterials and Its ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.622524/full]
- 79. A Comparative Study of Polymer Toxicity and Tissue Response [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467080/]
- 80. Bio-inspired poly-DL-serine materials resist the foreign- ... [https://www.nature.com/articles/s41467-021-25581-9]
- 81. Differential Foreign Body Reactions between Branched ... [https://www.mdpi.com/2079-4983/13/4/293]
- 82. Continuous operation of battery-free implants enables ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12063648/]
- 83. Wireless battery free fully implantable multimodal recording ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8009877/]
- 84. Wireless, battery-free, and fully implantable electrical ... [https://www.nature.com/articles/s41378-021-00294-7]
- 85. Injectable antenna could safely power deep-tissue medical ... [https://news.mit.edu/2025/injectable-antenna-could-safely-power-deep-tissue-medical-implants-1029]
- 86. MIT touts injectable antenna that could power battery-free ... [https://www.medicaldesignandoutsourcing.com/mit-researchers-develop-injectable-antenna-that-could-power-battery-free-medical-implants/]
- 87. Battery Free Implants Market Size to Hit USD 43.55 Billion ... [https://www.precedenceresearch.com/battery-free-implants-market]
- 88. Therapeutic Shifts and Scientific Influence in Treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552951/]
- 89. Deep brain stimulation for treatment-resistant major ... [https://pubmed.ncbi.nlm.nih.gov/40911913/]
- 90. Long-Term Success with Deep Brain Stimulation for Treatment ... [https://med.uth.edu/psychiatry/2025/04/07/long-term-success-with-deep-brain-stimulation-for-treatment-resistant-depression/]
- 91. Accelerated repetitive transcranial magnetic stimulation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12090592/]
- 92. Vagus Nerve Stimulation in Treatment Resistant Depression [https://www.psychiatrictimes.com/view/vagus-nerve-stimulation-in-treatment-resistant-depression-new-lines-of-thinking]
- 93. GH Research Announces Acceptance of Pharmaceutical ... [https://investor.ghres.com/news-releases/news-release-details/gh-research-announces-acceptance-pharmaceutical-pipeline]
- 94. The evolving role of investigative toxicology in ... [https://www.nature.com/articles/s41573-022-00633-x]
- 95. Overcoming failure: improving acceptance and success of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00168-7]
- 96. How medical device toxicology differs from biocompatibility [https://jordilabs.com/blog/how-medical-device-toxicology-differs-from-biocompatibility/]
- 97. The Evolution of Value-Based Care: Why Cost-Effectiveness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528593/]
- 98. Value-Based Pricing and Reimbursement in Personalised ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5618156/]
- 99. Value-Based Contracting in Pharma: Models & Challenges [https://intuitionlabs.ai/articles/value-based-contracting-pharmaceuticals]
- 100. Value-based Reimbursement as a Mechanism to Achieve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10621730/]
- 101. Electroceuticals & Bioelectric Medicine Market Analysis ... [https://www.datainsightsmarket.com/reports/electroceuticals-bioelectric-medicine-217624]
- 102. Medical Management and Device-Based Therapies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11308856/]
- 103. Enhancing Therapy Adherence: Impact on Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11766829/]
- 104. Understanding Treatment Adherence in Chronic Diseases [https://www.mdpi.com/2077-0383/14/17/6034]
- 105. Device-Based Therapy for Resistant Hypertension: An Up‐to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9523625/]
- 106. Comparing the longer regimen and the shorter ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1645820/full]
- 107. Medical Device Clinical Trials: 2025 FDA Requirements, ... [https://www.complizen.ai/post/medical-device-clinical-trials-complete-guide]
- 108. Bioelectric Medicine Market | Global Market Analysis Report [https://www.futuremarketinsights.com/reports/bioelectric-medicine-market]
- 109. Bioelectronic Medicine Market Research Report 2025 [https://www.globenewswire.com/news-release/2025/06/04/3093780/28124/en/Bioelectronic-Medicine-Market-Research-Report-2025-Featuring-Key-Players-Medtronic-Abbott-Boston-Scientific-Cochlear-LivaNova-Soterix-Medical-Bioinduction-GiMer-Medical-CEFALY-BioC.html]
- 110. Bioelectric Medicine Market Growth Rate, Industry Insights ... [https://www.datamintelligence.com/research-report/bioelectric-medicine-market]
- 111. Bioelectric Medicine Market Poised for Rapid Growth [https://natlawreview.com/press-releases/bioelectric-medicine-market-poised-rapid-growth-innovative-therapies]
- 112. Bioelectric Medicine Market Size to Hit USD 47.28 Billion ... [https://www.precedenceresearch.com/bioelectric-medicine-market]
- 113. Global Pharmaceutical Market: 2025 Analysis & Key Trends [https://intuitionlabs.ai/articles/pharmaceutical-market-analysis-trends]