Bioelectronic Medicine: The Emerging Frontier in Targeted Neuromodulation Therapies
This article explores bioelectronic medicine, an innovative field using targeted electrical signals to interface with the nervous system and treat disease.
Bioelectronic Medicine: The Emerging Frontier in Targeted Neuromodulation Therapies
Abstract
This article explores bioelectronic medicine, an innovative field using targeted electrical signals to interface with the nervous system and treat disease. It covers foundational principles from historical devices to next-generation closed-loop systems, examines therapeutic applications across neurology, cardiology, and immunology, addresses critical stability and reliability challenges for clinical translation, and provides comparative analysis against pharmacotherapies. For researchers and drug development professionals, it synthesizes technological advances, material innovations, and clinical validation shaping this rapidly evolving therapeutic paradigm.
From Ancient Shocks to Modern Implants: The Evolution of Bioelectric Therapy
Bioelectronic medicine is an emerging interdisciplinary field that uses electronic devices to interface with the body's electrically excitable tissues to treat diseases and restore function. This therapeutic approach represents a significant departure from conventional pharmacology, offering targeted neuromodulation with potentially fewer systemic side effects [1]. The conceptual foundations of bioelectronic medicine trace back to ancient observations of natural electrical phenomena in biological organisms, particularly electric fish, which demonstrated the profound connection between electricity and biological function long before modern understanding of electrophysiology [2] [1]. These early observations established a fundamental principle: that electrical signaling is an inherent property of biological systems that can be harnessed for therapeutic purposes.
The historical development of bioelectronic medicine reveals a fascinating trajectory from observation of natural electrical phenomena to sophisticated implantable devices. This evolution required convergence of multiple scientific disciplines including physiology, materials science, electrical engineering, and neuroscience [3]. The field has matured from simple electrical stimulation to complex bidirectional interfaces capable of both recording physiological signals and delivering targeted therapy, ultimately leading to the development of modern devices such as pacemakers, cochlear implants, and neural stimulators that form the foundation of contemporary bioelectronic medicine [1] [4].
Historical Timeline: Key Developments in Bioelectronic Medicine
Table 1: Historical Evolution of Bioelectronic Medicine
| Time Period | Key Development | Contributors/Examples | Significance |
|---|---|---|---|
| 2750-2500 BC | Therapeutic use of electric fish | Egyptian Fifth Dynasty | First documented use of biological electricity for pain management |
| 18th Century | Discovery of bioelectricity | Luigi Galvani (Italy) | Established fundamental connection between electricity and muscle contraction |
| Mid-18th Century | Electrostatic medical applications | Benjamin Franklin (USA), Kratzenstein (Germany) | Early attempts to apply man-made electricity therapeutically |
| 1840 | First clinical electrotherapy department | Dr. Golding Bird, Guy's Hospital (England) | Institutionalization of electrical therapies |
| 1958 | First fully implantable pacemaker | - | Revolutionized treatment of cardiac arrhythmias |
| 1961 | First cochlear implant | - | Restored hearing through electrical stimulation |
| 1970s | FDA recognition of TENS | United States Food and Drug Administration | Formal regulatory approval for transcutaneous electrical nerve stimulation |
| 2000s | Advanced neuromodulation therapies | Vagus nerve stimulation for epilepsy and inflammation | Expanded applications to neurological and inflammatory conditions |
| 2024 | FDA approval for rheumatoid arthritis | SetPoint Medical's vagus nerve stimulator | First bioelectronic treatment approved for autoimmune disease [3] |
The historical timeline of bioelectronic medicine reveals a progressive understanding of electrical principles and their application to biological systems. Ancient civilizations utilized the powerful electrical discharges from torpedo fish (similar to electric eels) for pain relief, intuitively recognizing their therapeutic potential despite lacking scientific understanding of the underlying mechanisms [2] [1]. These early applications represented the first recorded instances of neurostimulation, establishing a foundation that would be built upon centuries later with more sophisticated technologies.
The 18th century marked a critical turning point with Luigi Galvani's seminal experiments demonstrating that electrical stimulation could induce muscular contractions in frog legs [1] [4]. This discovery of "animal electricity" provided the first experimental evidence for the electrical excitability of nervous tissue, fundamentally reshaping scientific understanding of neuromuscular physiology. Throughout the 19th and early 20th centuries, technological advances in generating and controlling electricity enabled more precise therapeutic applications, including the development of Galvanic, Faradic, and sinusoidal currents that became standard modalities in electrotherapy [2]. The mid-20th century breakthrough came with the development of fully implantable devices, beginning with cardiac pacemakers in 1958 and cochlear implants in 1961, which established the core principle of using implanted electronics to replace or modulate physiological functions [1].
Electric Fish: Nature's Blueprint for Bioelectronic Medicine
Electric fish represent remarkable natural models that demonstrate the evolutionary optimization of bioelectrical systems for sensing, communication, and defense. These organisms provided both the initial inspiration for bioelectronic medicine and continue to offer valuable insights into the principles of electrogenesis and neural control of electrical outputs. Two major groups of electric fish have been extensively studied: the strongly electric fish (such as the electric eel, Electrophorus electricus), capable of generating powerful discharges up to 600 volts for predation and defense, and weakly electric fish (including numerous species of South American knifefishes and African elephantfishes), which produce low-voltage signals for electrolocation and communication [5].
The neurophysiological mechanisms underlying electric organ function in these species reveal sophisticated biological solutions to electrical signal generation that have informed engineering approaches in bioelectronic medicine. Electric fish possess specialized electric organs derived from either muscle tissue (myogenic electric organs) or nervous tissue (neurogenic electric organs) [5]. These organs contain electrocytes – specialized cells that function similarly to neurons in generating action potentials but are optimized for producing external electrical fields rather than intracellular signaling [5]. In the electric eel (Electrophorus electricus), adults possess three distinct electric organs: the main organ, Sach's organ, and Hunter's organ, which collectively dominate the posterior 80% of the animal's body [5]. The sophisticated neural circuitry controlling these organs allows for precise modulation of discharge frequency and pattern, demonstrating nature's solution to the challenge of controlling bioelectrical outputs – a fundamental requirement for effective bioelectronic therapies.
Comparative Analysis of Electric Organs
Table 2: Electric Organ Types and Characteristics in Electric Fish
| Characteristic | Myogenic Electric Organ | Neurogenic Electric Organ |
|---|---|---|
| Tissue Origin | Muscle tissue | Nervous tissue |
| Electrocyte Type | Type A (within tail muscle) and Type B (below tail muscle) | Specialized neural tissue |
| Representative Species | Electrophorus electricus, Brachyhypopomus gauderio | Apteronotidae family (ghost knifefishes) |
| Discharge Properties | Monophasic, biphasic, or triphasic discharges | Continuous wave-type signals |
| Developmental Origin | Derived from muscle precursor cells | Derived from neural precursor cells |
| Key Proteins | Dystrophin, desmin, actin (muscle proteins) | Neural-specific proteins |
| Functional Specialization | Powerful discharges for predation/defense or weak signals for electrolocation | Primarily for electrolocation and communication |
The evolutionary convergence of electric organs across distantly related fish lineages demonstrates the fundamental advantage of electrical signaling in aquatic environments and provides nature's validation of electricity as a biological modality [5]. The anatomical structure of these organs, with electrocytes arranged in stacked columns and synchronized activation, represents a natural blueprint for designing efficient electrode arrays in bioelectronic devices. Furthermore, the precise neural control of electric organ discharges, which can be modulated by social context, reproductive state, and environmental factors, illustrates the principle of adaptive neuromodulation that underpins modern closed-loop bioelectronic systems [6] [5].
From Natural Principles to Clinical Applications: The Modern Era
The translation of principles from electric fish to human therapeutics required fundamental advances in understanding neural coding, bioelectrical phenomena, and device engineering. A critical milestone was the discovery of the inflammatory reflex by Kevin Tracey and colleagues, which revealed that the vagus nerve plays a central role in regulating immune function and inflammation [7]. This discovery provided a physiological basis for using electrical stimulation to treat inflammatory conditions, establishing a new paradigm for bioelectronic therapy beyond traditional neurological applications.
The modern era of bioelectronic medicine has been characterized by progressive technological miniaturization and increasing specificity of neural interfaces. Early implantable devices were relatively crude in their stimulation paradigms, delivering fixed patterns of electrical pulses without feedback from physiological states. Contemporary systems are evolving toward closed-loop architectures that continuously monitor physiological biomarkers and adjust stimulation parameters in real-time to maintain optimal therapy [1] [4]. This approach mirrors the adaptive control systems observed in electric fish, which modulate their electric organ discharges based on environmental context and behavioral requirements.
Current Clinical Applications and Market Landscape
Table 3: Modern Bioelectronic Medicine Applications and Market Data (2024)
| Application Area | Representative Devices | Key Conditions Treated | Market Value (2023) |
|---|---|---|---|
| Cardiac Rhythm Management | Implantable cardioverter defibrillators, cardiac pacemakers | Arrhythmia, heart failure | Largest segment of $23.54B market [8] |
| Neurological Disorders | Deep brain stimulators, vagus nerve stimulators | Parkinson's disease, tremor, epilepsy, depression | DBS: $1.41B; VNS: $479.15M [1] |
| Chronic Pain | Spinal cord stimulators, transcutaneous electrical nerve stimulators | Neuropathic pain, failed back surgery syndrome | SCS: $2.92B [1] |
| Hearing Loss | Cochlear implants | Sensorineural hearing loss | Established therapy with continuous innovation |
| Inflammatory Diseases | Vagus nerve stimulators | Rheumatoid arthritis, inflammatory bowel disease | Emerging application with recent FDA approvals [3] |
The bioelectronic medicine market has experienced substantial growth, valued at USD 23.54 billion in 2024 and projected to reach USD 33.59 billion by 2030, representing a compound annual growth rate of 6.10% [8]. This expansion is driven by multiple factors including the rising prevalence of chronic diseases, technological advancements in device miniaturization and functionality, growing awareness of the limitations of pharmacological therapies, and an aging global population that increasingly requires chronic disease management solutions [8] [1]. The recent FDA approval of SetPoint Medical's vagus nerve stimulation device for rheumatoid arthritis marks a significant milestone, representing the first bioelectronic therapy approved specifically for an autoimmune condition and validating the concept of targeting neural circuits to modulate immune function [3].
Experimental Approaches and Methodologies
The advancement of bioelectronic medicine relies on sophisticated experimental methodologies that bridge multiple disciplines from basic neuroscience to device engineering. Fundamental to progress in the field is the ability to precisely interface with neural circuits and quantify the resulting physiological effects. The following experimental protocols represent core approaches that have enabled key discoveries in bioelectronic medicine.
Vagus Nerve Stimulation (VNS) for Inflammatory Conditions
Objective: To evaluate the efficacy of vagus nerve stimulation in modulating inflammatory responses and treating inflammatory diseases.
Background: The inflammatory reflex is a neural circuit that interfaces the immune and nervous systems, with the vagus nerve serving as the primary conduit for signals that regulate cytokine production and inflammation [7]. Electrical stimulation of the vagus nerve activates this pathway, resulting in suppression of pro-inflammatory cytokines including TNF, IL-1β, and IL-6.
Materials and Reagents:
- Vagus Nerve Cuff Electrode: Multi-contact cuff electrode for selective vagus nerve stimulation
- Programmable Pulse Generator: Device capable of delivering precise current-controlled stimulation pulses
- Electrophysiology Recording System: For verifying neural activation and recording evoked potentials
- Enzyme-Linked Immunosorbent Assay (ELISA) Kits: For quantifying cytokine levels (TNF-α, IL-1β, IL-6) in serum and tissues
- Animal Model: Typically rodents or porcine models with induced inflammation (e.g., endotoxemia, rheumatoid arthritis)
- Microdissection Tools: For surgical exposure of the vagus nerve
- Histology Supplies: For verification of electrode placement and tissue response
Procedure:
- Surgically expose the cervical vagus nerve using aseptic technique
- Implant multi-contact cuff electrode around the vagus nerve
- Connect electrode to programmable pulse generator
- Apply stimulation parameters (typical settings: 0.5-2.0 mA, 100-500 μs pulse width, 10-30 Hz frequency)
- Monitor physiological parameters (heart rate, respiration) to ensure appropriate stimulation intensity
- Collect blood and tissue samples at predetermined time points for cytokine analysis
- Process samples using ELISA to quantify inflammatory mediators
- Sacrifice animals and perform histology to verify electrode placement and assess tissue response
Applications: This methodology has been successfully applied in preclinical models of rheumatoid arthritis, inflammatory bowel disease, sepsis, and other inflammatory conditions, providing the foundation for clinical trials of VNS in these diseases [7].
Characterization of Electric Organ Physiology
Objective: To analyze the electrophysiological properties and discharge characteristics of electric organs in model species.
Background: Electric fish generate species-specific electric organ discharges (EODs) through the synchronized activity of electrocytes. Understanding the mechanisms of EOD generation and modulation provides insights into fundamental principles of bioelectrogenesis that can inform device design.
Materials and Reagents:
- Aquatic Electrophysiology Setup: Tank with calibrated electrode array for EOD recording
- High-Speed Voltage Recording System: Capable of sampling at ≥100 kHz to capture EOD waveform details
- Water Conductivity Meter: For standardizing experimental conditions
- Isolated Pulse Stimulator: For direct stimulation of electric organ efferent neurons
- Microelectrodes: For intracellular recording from electrocytes (as applicable)
- Pharmacological Agents: Neurotransmitter blockers (curare, atropine), ion channel modifiers (TTX, TEA)
Procedure:
- Acclimate fish in experimental tank with controlled water conductivity
- Position recording electrodes at standardized locations relative to the fish
- Record baseline EOD activity under various behavioral conditions (rest, exploration, social interaction)
- Analyze EOD waveform parameters: amplitude, duration, phase number, frequency spectrum
- For reduced preparations, directly stimulate efferent neurons to electric organ while recording output
- Apply pharmacological agents to characterize neurotransmitter systems and ion channels
- Use intracellular recording to analyze electrocyte membrane properties and action potential characteristics
- Correlate electrophysiological data with anatomical studies of electric organ structure
Applications: This approach has revealed fundamental mechanisms of pattern generation in neural circuits, the evolution of specialized electrogenic tissues, and principles of electrical field generation in biological tissues [6] [5].
Table 4: Key Research Reagents and Technologies for Bioelectronic Medicine Research
| Research Tool | Function/Application | Examples/Specifications |
|---|---|---|
| Multi-Contact Cuff Electrodes | Selective stimulation and recording from peripheral nerves | Polyimide-based designs with 8-16 contacts for spatial selectivity [9] |
| Implantable Pulse Generators | Programmable electrical stimulation in chronic experiments | Bidirectional devices with sensing and stimulation capabilities [1] |
| Conducting Polymers | Improved electrode-tissue interface | PEDOT:PSS coatings reducing impedance and improving charge injection [1] |
| Wireless Telemetry Systems | Remote monitoring and control of implanted devices | Bluetooth Low Energy or medical implant communication service bands [1] |
| Computational Neural Models | Optimization of stimulation parameters and prediction of neural responses | ASCENT pipeline for simulating nerve responses to complex waveforms [9] |
| Flexible Bioelectronic Materials | Enhanced biocompatibility and reduced foreign body response | Stretchable electronics, hydrogels, liquid metal conductors [4] |
| Cytokine Assay Kits | Quantification of inflammatory mediators for immunomodulation studies | ELISA or multiplex bead arrays for TNF-α, IL-1β, IL-6 measurement [7] |
The development of increasingly sophisticated research tools has been instrumental in advancing bioelectronic medicine. Multi-contact cuff electrodes enable selective stimulation of specific nerve fascicles, dramatically improving the precision of neuromodulation therapies [9]. Computational models of nerve activation allow researchers to optimize stimulation paradigms in silico before validation in biological systems, accelerating the development of novel therapy approaches [9]. Advanced materials, particularly conducting polymers such as PEDOT:PSS, have significantly improved the interface between electronic devices and biological tissues by reducing impedance and enhancing charge transfer capacity [1]. These technological advances continue to push the boundaries of what is possible in bioelectronic medicine, enabling more precise, effective, and durable therapies.
Signaling Pathways and Neural Circuits
The therapeutic efficacy of bioelectronic medicine depends on precise interaction with specific neural pathways that regulate physiological processes. The inflammatory reflex represents one of the most thoroughly characterized neural circuits targeted by bioelectronic therapies.
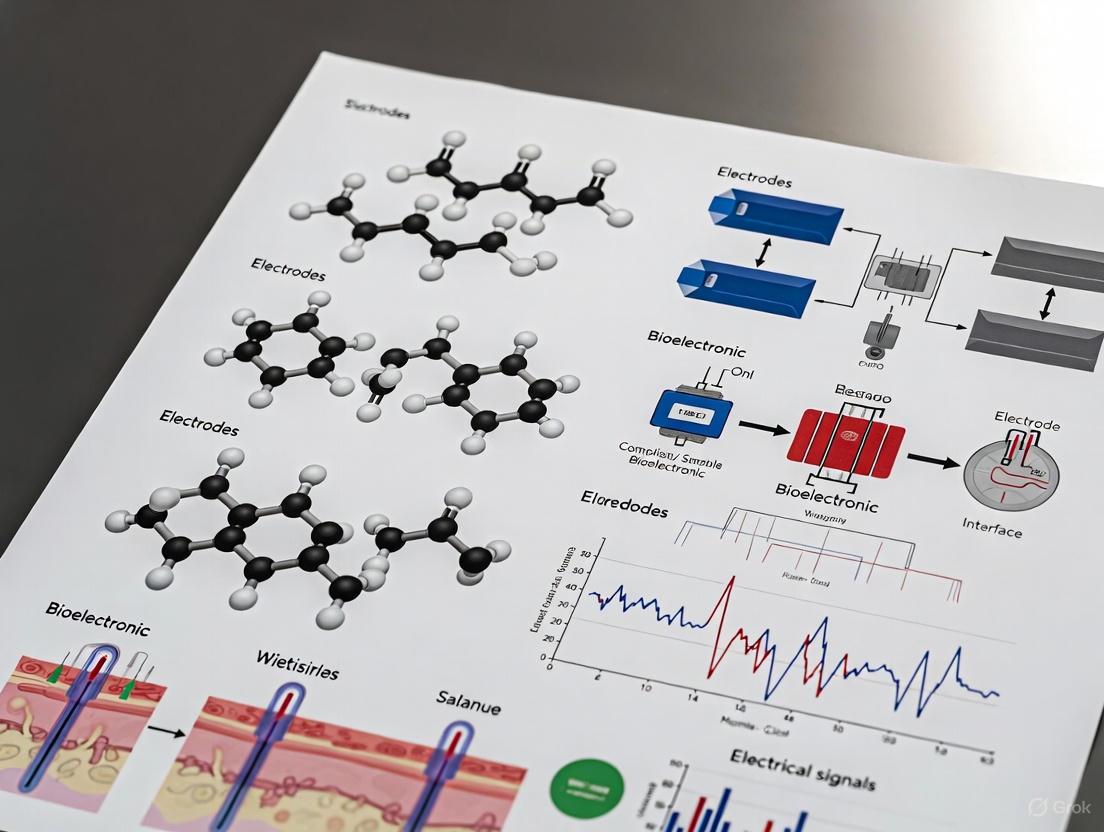
Figure 1: Neural Circuit of the Inflammatory Reflex. This diagram illustrates the neuroimmune pathway through which vagus nerve stimulation reduces inflammation. The circuit begins with peripheral inflammation detected by afferent vagus nerve fibers, integrates in the brainstem nucleus tractus solitarius (NTS), and activates efferent vagus nerve pathways that ultimately signal through the splenic nerve to trigger T-cell release of acetylcholine, which suppresses macrophage production of pro-inflammatory cytokines via α7 nicotinic acetylcholine receptors (α7nAChR) [7].
The inflammatory reflex represents a sophisticated neural feedback system that maintains immunological homeostasis. Afferent vagus nerve signals carrying information about peripheral inflammation are integrated in the brainstem nucleus tractus solitarius (NTS), which then activates efferent vagus nerve pathways [7]. These efferent signals project to the celiac-superior mesenteric ganglion, where they activate the splenic nerve, which in turn triggers norepinephrine release in the spleen [7]. Norepinephrine stimulates a specialized population of T cells expressing choline acetyltransferase (ChAT) to produce acetylcholine, which acts on macrophages via α7 nicotinic acetylcholine receptors to inhibit the release of pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 [7]. This multi-synaptic pathway demonstrates the complex interplay between the nervous and immune systems that can be therapeutically targeted with bioelectronic devices.
Future Directions and Challenges
The field of bioelectronic medicine faces several significant challenges that must be addressed to realize its full potential. Device reliability and long-term stability remain critical concerns, particularly as implants become smaller and more complex [4]. The biological environment presents unique challenges for electronic devices, including mechanical stresses from constant movement, corrosion from bodily fluids, and the foreign body response that can insulate electrodes from their target tissues [1] [4]. These factors can compromise device performance over time and limit therapeutic efficacy.
Future advances in bioelectronic medicine will depend on interdisciplinary approaches that integrate developments in multiple fields. Materials science is producing a new generation of biocompatible, flexible, and even biodegradable electronic materials that better interface with biological tissues [1] [4]. Wireless power transfer technologies are enabling smaller, battery-free implants that can operate indefinitely without requiring surgical replacement [1]. Artificial intelligence and machine learning algorithms are being integrated into closed-loop systems that can adapt therapy in real-time based on physiological feedback [8] [1]. These technological advances, combined with deepening understanding of neural circuit physiology, promise to expand the applications of bioelectronic medicine to a wider range of conditions including metabolic disorders, autoimmune diseases, and neurodegenerative conditions.
The historical foundation of bioelectronic medicine, from the early observations of electric fish to modern implantable devices, demonstrates a progressive understanding of the intimate connections between electrical signaling and biological function. As the field continues to evolve, it holds the potential to transform the treatment of chronic diseases through targeted neuromodulation, offering precisely controlled therapy with reduced side effects compared to conventional pharmacological approaches. The ongoing convergence of neuroscience, engineering, and materials science promises to accelerate this transformation, ultimately fulfilling the potential inherent in nature's earliest demonstrations of bioelectricity.
Bioelectronic medicine represents a paradigm shift in therapeutic strategies, moving from pharmaceutical compounds to the targeted modulation of neural circuits to treat disease. This field is grounded in the principle that the nervous system dynamically regulates physiological processes and organ functions through specific neural pathways. Dysregulation or pathology within these circuits can lead to a wide array of diseases, including rheumatoid arthritis, inflammatory bowel disease, cancer, diabetes, asthma, and cardiovascular conditions [3]. By mapping these circuits with high precision and developing technologies to neuromodulate their activity, researchers can develop interventions that restore healthy physiological states. This approach leverages the body's own innate control systems, offering the potential for highly specific, reversible, and adaptive treatments with fewer side effects than systemic drug administration [10].
The field is inherently interdisciplinary, integrating material science, biochemistry, biophysics, molecular medicine, neuroscience, immunology, bioengineering, electrical engineering, computer science, and artificial intelligence to decode and interface with the nervous system [3]. The ultimate focus is on understanding electrical signaling within the nervous system and developing technologies to record, stimulate, or block neural signals to affect specific molecular mechanisms. This spans from molecular-level interactions to circuit-level dynamics and whole-organism physiological outcomes, promising a new frontier in diagnosing and treating human disease [3].
Core Principles of Neural Circuit Function and Dysfunction
The functional architecture of the brain and peripheral nervous system is built upon specialized neural circuits, which are ensembles of interconnected neurons that process specific types of information and generate defined outputs. The central tenet of bioelectronic medicine is that these circuits form the structural basis for physiological control, and their dysfunction underlies numerous disease states. Several core principles govern how these circuits operate and how they can be targeted for therapeutic intervention.
Circuit Specificity and Connectional Logic: Neural circuits are not random networks but are organized with precise connectivity patterns that determine their function. The connectional logic dictates how information flows from inputs to outputs. For example, research on the retrosplenial cortex (RSC) has revealed that distinct projection pathways subserve different cognitive functions. Neurons projecting from the RSC to the secondary motor cortex (M2) are crucial for object-location memory and action planning, while those projecting to the anterodorsal thalamus (AD) are primarily involved in spatial memory [11]. This semi-autonomous operation of parallel pathways within a single brain region highlights the precision required for effective circuit-based interventions.
Excitatory-Inhibitory Balance: The dynamic interplay between excitatory and inhibitory neurons is fundamental to healthy neural circuit operation. Excitatory neurons, such as pyramidal cells, facilitate signal transmission, while diverse classes of inhibitory interneurons—including parvalbumin (Pvalb)-positive basket cells, somatostatin (SST)-positive Martinotti cells, and vasoactive intestinal peptide (VIP)-positive bipolar cells—provide precise control over timing, synchronization, and network excitability [11]. Disruption of this delicate balance is implicated in numerous neurological and psychiatric conditions, including epilepsy, schizophrenia, and autism spectrum disorders [11].
Neuroplasticity and Circuit Remodeling: Neural circuits are not static but demonstrate neuroplasticity—the ability to strengthen, weaken, or reorganize synaptic connections in response to experience, learning, or injury. This capacity for change is central to both the pathogenesis of disease and the mechanism of therapeutic recovery. Following brain injury or in neurodegenerative diseases, promoting targeted neuroplasticity through neuromodulation or stem cell therapies represents a promising strategy for circuit repair and functional recovery [11]. Understanding the molecular and cellular mechanisms that govern this plasticity is therefore critical for developing effective bioelectronic therapies.
Hierarchy, Feedback, and Redundancy in Circuit Dynamics: The neural circuits governing fundamental processes like sleep and arousal operate on principles of feedback control, hierarchical organization, and functional redundancy. Computational models of the sleep-wake cycle have identified these three aspects as fundamental to the system's stability and function [12]. Feedback loops maintain state stability, hierarchical organization allows higher-order circuits to gate the activity of lower ones, and redundant pathways ensure robustness. Dysregulation in these dynamic properties can lead to state fragmentation, as seen in narcolepsy with dysfunction of the hypocretin (orexin) system [12].
Table 1: Key Neurotransmitter Systems in State-Dependent Neural Circuits
| Neurotransmitter | Primary Source Nuclei | Role in Circuit Function | Associated Pathologies |
|---|---|---|---|
| Hypocretin (Orexin) | Lateral Hypothalamus | Controls boundaries between vigilance states, stabilizes wakefulness. | Narcolepsy, Cataplexy [12] |
| Norepinephrine (NE) | Locus Coeruleus | Promotes wakefulness and arousal; tonic activity during active wake. | Fragmented Sleep, Arousal Deficits [12] |
| Histamine (His) | Tuberomammillary Nucleus | Promotes wakefulness; diffuse projections throughout the brain. | Sleep Architecture Abnormalities [12] |
| Acetylcholine (ACh) | Basal Forebrain | Increased during wakefulness and REM sleep; critical for cortical activation. | Cognitive Impairment, Sleep Disorders [12] |
| Serotonin (5-HT) | Dorsal Raphe | Increased during wakefulness; modulates mood, arousal, and respiratory function. | Depression, Anxiety, Sleep Disorders [12] |
Methodologies for Neural Circuit Mapping and Analysis
A cornerstone of bioelectronic medicine is the ability to delineate the anatomical and functional organization of neural circuits with ever-increasing resolution and cell-type specificity. The methodologies for achieving this have evolved from gross lesion studies to sophisticated genetic and optical tools that allow for precise observation and manipulation of circuit components.
Anatomical Tracing Techniques
Anatomical tracing techniques reveal the "wiring diagram" of the brain by exploiting the natural axonal transport mechanisms of neurons.
Conventional Tracers: Early approaches used molecules like horseradish peroxidase (HRP) and fluorescent conjugates (e.g., Fluoro-Gold). These tracers are taken up by neurons and transported anterogradely (from soma to axon terminals) or retrogradely (from terminals back to the soma) to map efferent and afferent connections, respectively [13]. While useful, these methods often lack cell-type specificity.
Viral Vector-Based Tracers: Genetically modified viral vectors represent a revolutionary advance in circuit tracing. Adeno-associated viruses (AAVs) are commonly used for anterograde tracing due to their safety and efficiency. For high-resolution mapping of direct inputs to a defined neuronal population, monosynaptic rabies virus systems are employed. This involves a two-part system: an initial "helper" AAV expresses the TVA receptor and rabies glycoprotein (G) in target cells, followed by a modified rabies virus (RV-ΔG) that lacks G and is pseudotyped with EnvA. This virus only infects TVA-expressing cells and, with the supplied G, undergoes a single, monosynaptic retrograde jump to directly presynaptic partners, allowing for input mapping at single-synapse resolution [11] [13].
Functional Manipulation and Interrogation
While anatomy provides the structural map, functional tools are required to establish causal links between circuit activity and physiological or behavioral outcomes.
Optogenetics: This technique provides millisecond-precision control over genetically defined neuronal populations. Neurons are made to express light-sensitive ion channels (e.g., Channelrhodopsin-2 for excitation, Halorhodopsin for inhibition). By delivering light via optical fibers, researchers can activate or silence specific circuits with high temporal precision, allowing them to probe the necessity and sufficiency of a circuit for a given function or behavior [11] [12]. For instance, optogenetic silencing of M2-projecting RSC neurons was shown to impair object-location memory [11].
Chemogenetics (DREADDs): Designer Receptors Exclusively Activated by Designer Drugs (DREADDs) offer an alternative for remote control of neural circuits. Engineered G-protein-coupled receptors are expressed in target neurons and activated by an inert ligand (e.g., Clozapine N-oxide). This allows for sustained modulation (over minutes to hours) of neuronal activity without the need for implanted hardware, making it suitable for studying longer-term processes like neuroplasticity or inflammation [11].
Nanostructured Photonic Probes: The integration of nanotechnology with neuroscience has led to the development of ultra-high-resolution probes. These devices combine tailored optogenetic stimulation with recording capabilities, offering spatial (~100 nm) and temporal (~ms) accuracy that surpasses traditional electrodes. This enables real-time observation and modification of brain activity at cellular and subcellular levels, opening new avenues for minimally invasive neurotherapeutic diagnostics and interventions [11].
Quantitative Modeling of Neural Circuit Dynamics
To translate the vast amounts of data from mapping and interrogation studies into predictive knowledge, the field increasingly relies on quantitative computational modeling. These models help interpret complex data, assist in optimizing experimental parameters, and drive the design of next-generation experiments and therapies [12].
Data-Driven Modeling with Artificial Neural Networks: A recent trend involves using artificial neural networks (ANNs) to create data-driven models that can quantitatively learn intracellular and circuit dynamics from experimental recordings. A key architecture is the Recurrent Mechanistic Model (RMM), which is formulated as a discrete-time state-space model [14]:
C(v̂_{t+1} - v̂_t)/δ = -h_θ(v̂_t, x_t) + u_t
x_{t+1} = f_η(v̂_t, x_t)
Here, v̂_t is the predicted membrane voltage, u_t is the injected current, x_t is a vector of internal state variables, C is a membrane capacitance matrix, and h_θ and f_η are learnable functions parameterized by ANNs. This approach can accurately predict unmeasured variables, such as synaptic currents within a circuit, from voltage measurements alone, providing a powerful tool for inferring internal connectivity [14].
System-Theoretic Modeling for State Transitions: For behaviors like sleep-to-wake transitions, analytical models can encapsulate the interactions between multiple neuromodulatory circuits. These models define the system components (e.g., Hcrt, NE, His systems) and mathematically represent their input-output relationships and interactions (e.g., feedback, redundancy, hierarchy). By fitting such models to empirical data, researchers can simulate system behavior under different conditions, propose limits on biological parameters, and identify key control points for intervention [12].
Training Methodologies for Predictive Models: The performance of data-driven models depends critically on the training algorithm. Empirical assessments compare methods like:
- Teacher Forcing (TF): Trains the model using the ground-truth voltage as input at each step.
- Multiple Shooting (MS): Divides the time series into segments and trains the model to match both the initial state and the dynamics of each segment, improving stability for long predictions.
- Generalized Teacher Forcing (GTF): A hybrid approach that uses ground-truth data for a limited number of steps before switching to the model's own predictions [14]. These methods enable the creation of stable and accurate models that can be used in real-time or closed-loop experimental paradigms.
Table 2: Key Research Reagents for Neural Circuit Analysis
| Reagent / Tool | Category | Primary Function in Experimentation |
|---|---|---|
| Adeno-Associated Virus (AAV) | Viral Vector | Gene delivery vehicle for expressing sensors, actuators, or tracing components in specific neuronal populations [11] [13]. |
| Monosynaptic Rabies Virus (RV-ΔG) | Viral Tracer | Retrograde tracer for mapping direct, monosynaptic inputs to a starter population of neurons [11] [13]. |
| Channelrhodopsin-2 (ChR2) | Optogenetic Actuator | Light-gated cation channel for precise millisecond-timescale activation of targeted neurons [11] [12]. |
| Designer Receptors (DREADDs) | Chemogenetic Tool | Chemically activated engineered GPCRs for remote, sustained modulation (minutes-hours) of neuronal activity [11]. |
| Tetracysteine Display of Optogenetic Elements (Tetro-DOpE) | Multifunctional Probe | A probe that allows for real-time monitoring and modification of specific neuronal populations, enhancing intervention precision [11]. |
| Recurrent Mechanistic Model (RMM) | Computational Model | A data-driven architecture (a type of Recurrent Neural Network) for rapidly estimating and predicting intracellular neuronal dynamics from voltage data [14]. |
Therapeutic Applications and Clinical Translation
The ultimate goal of mapping and modeling neural circuits is to develop novel, effective therapies for human disease. Bioelectronic medicine is already yielding clinically approved treatments and a robust pipeline of experimental therapies.
Inflammatory and Autoimmune Diseases: The most advanced success story is the FDA approval of a vagus nerve stimulation device from SetPoint Medical for the treatment of rheumatoid arthritis [3]. This therapy is based on the pioneering scientific work that identified the inflammatory reflex—a specific circuit in which vagus nerve activity signals to the spleen to suppress the release of inflammatory cytokines like TNF [3]. This represents a paradigm of directly using a neural circuit to treat an inflammatory condition without broad immunosuppression.
Neurological and Psychiatric Disorders: Circuit-based interventions are showing great promise for a range of brain disorders.
- Depression and Anxiety: Non-invasive techniques like Transcranial Magnetic Stimulation (TMS) are approved for treatment-resistant depression and are being investigated for anxious depression and OCD. TMS is thought to work by modulating activity in circuits linking the prefrontal cortex and amygdala, improving emotional regulation [11] [10].
- Substance Use Disorders (SUDs): Repetitive TMS (rTMS) targeting the ventromedial prefrontal cortex (VMPFC)-amygdala circuit is being explored to improve emotional control and decision-making, thereby reducing impulsive drug-seeking behaviors [11].
- Stroke and Neurodegeneration: Strategies that combine stem cell therapies with neurogenesis-promoting interventions are under investigation to enhance circuit repair and functional recovery after brain injury [11].
The Future: Closed-Loop and Non-Invasive Systems: The next generation of bioelectronic medicine focuses on "closed-loop" systems that autonomously adjust therapy based on real-time physiological feedback. For example, a device paired with a biomarker sensor could titrate vagus nerve stimulation to maintain a desired level of inflammation or neural activity [10]. Furthermore, the development of non-invasive neuromodulation techniques (e.g., TMS) is a major priority, as it avoids the risks of surgery and increases the potential for widespread adoption and scale [10].
Table 3: Clinically Approved Bioelectronic Medicine Interventions
| Therapy / Device | Target Circuit / Structure | Primary Indication(s) | Key Mechanism of Action |
|---|---|---|---|
| Vagus Nerve Stimulation | Inflammatory Reflex (Vagus Nerve → Spleen) | Rheumatoid Arthritis [3] | Neuroimmunomodulation; suppression of pro-inflammatory cytokines. |
| Deep Brain Stimulation (DBS) | Subthalamic Nucleus, Globus Pallidus | Parkinson's Disease, Essential Tremor [10] | Modulation of pathological oscillatory activity in motor circuits. |
| Spinal Cord Stimulation (SCS) | Dorsal Columns of Spinal Cord | Chronic Pain, Motor Dysfunction from Injury [10] | Interference with pain signal transmission; activation of residual neural pathways. |
| Transcranial Magnetic Stimulation (TMS) | Prefrontal Cortex, Amygdala Circuitry | Depression, OCD, Migraine Pain [11] [10] | Induction of currents in superficial brain regions to modulate circuit excitability and plasticity. |
The field of bioelectronic medicine is undergoing a fundamental transformation in its core material technologies. Traditional rigid implants are increasingly being replaced by soft, flexible bioelectronic devices that bridge the mechanical mismatch with biological tissues. This whitepaper examines the technological shift toward hydrogel-based semiconductors, detailing their manufacturing processes, experimental validation, and functional advantages. We provide a comprehensive technical analysis of material properties, experimental methodologies for characterizing tissue-integrated electronics, and a practical toolkit for researchers developing next-generation bioelectronic therapies. This paradigm shift enables more seamless biointerfaces for advanced neuromodulation, biosensing, and chronic implantation applications.
Bioelectronic medicine (BEM) represents a transformative approach to treating disease through electrical modulation of electrically active tissues, primarily the nervous system [1]. By interfacing with neural circuits that innervate every organ, bioelectronic devices can selectively target and modulate organ function, potentially replacing pharmacotherapies with precise, on-demand electrical stimulation [7] [1]. This field has evolved from early electrotherapy concepts to sophisticated implantable devices including spinal cord stimulators (SCS), deep brain stimulators (DBS), and vagus nerve stimulators (VNS) that treat conditions ranging from chronic pain and Parkinson's disease to drug-resistant epilepsy and inflammatory disorders [15].
Despite considerable clinical success, traditional bioelectronic implants face significant limitations stemming from their fundamental material properties. Conventional semiconductors are inherently rigid, brittle, and hydrophobic, creating a pronounced mechanical mismatch with soft, watery biological tissues [16]. This mismatch triggers foreign body reactions (FBR), inflammatory responses that form fibrotic tissue around implants, ultimately degrading device performance over time through reduced signal quality and increased impedance [1]. The encapsulation required to protect traditional electronics from bodily fluids further exacerbates these issues, creating additional bulk and rigidity [1].
The solution lies in developing bioelectronic interfaces with tissue-like mechanical properties - soft, stretchable, and highly hydrated materials that can deform harmoniously with surrounding tissue while maintaining robust electronic functionality [16]. This whitepaper examines the pioneering materials and methodologies driving this technological shift from rigid implants to soft, flexible bioelectronics.
Hydrogel Semiconductors: A Paradigm Shift in Biomaterial Design
Material Properties and Manufacturing Breakthrough
A groundbreaking advancement in soft bioelectronics comes from the University of Chicago Pritzker School of Molecular Engineering, where researchers have created the first truly integrated hydrogel semiconductor [16]. This material represents a fundamental departure from previous approaches that merely attached conventional electronics to hydrogel substrates. Instead, the new material is both semiconductor and hydrogel simultaneously - a single integrated system with dual functionality [16].
The key innovation lies in a novel solvent exchange process that circumvents the traditional incompatibility between semiconductors and aqueous environments [16]. Rather than attempting to dissolve hydrophobic semiconductors in water, researchers first dissolved polymer semiconductors in an organic solvent miscible with water, then prepared a gel from the dissolved semiconductors and hydrogel precursors [16]. This methodology enables creation of a bluish, jelly-like material that maintains excellent semiconductive properties while achieving mechanical characteristics nearly identical to natural tissues.
Table 1: Comparative Properties of Traditional vs. Hydrogel Semiconductors
| Property | Traditional Semiconductors | Hydrogel Semiconductors |
|---|---|---|
| Mechanical Properties | Rigid, brittle | Soft, stretchable, tissue-like |
| Hydration | Hydrophobic (water-repelling) | Highly hydrated (water-loving) |
| Biocompatibility | High risk of foreign body reaction | Reduced immune response and inflammation |
| Porosity | Non-porous | Highly porous for molecular diffusion |
| Tissue Interface | Mechanical mismatch | Deforms harmoniously with tissue |
| Manufacturing Process | Standard microfabrication | Solvent exchange-based gelation |
Functional Advantages and Enhanced Biointeractivity
The unique material properties of hydrogel semiconductors translate to significant functional advantages in biological environments. The soft mechanical properties and high hydration similar to living tissue promote more intimate biointerfaces while reducing immune responses typically triggered by device implantation [16]. This enhanced biocompatibility is crucial for chronic implants that must function for 5-10 years without significant performance degradation [1].
The porous nature of hydrogel semiconductors enables elevated biosensing capabilities and stronger photomodulation effects [16]. Biomolecules can diffuse into the film, significantly increasing interaction sites for biomarkers and resulting in higher detection sensitivity. For therapeutic functions, such as light-operated pacemakers or wound dressings, the efficient transport of molecules enhances responses to light stimulation, potentially accelerating healing processes [16].
This combination of properties creates a synergistic effect where the integrated material system outperforms what either component could achieve separately - a "one plus one is greater than two" combination that represents a true paradigm shift in bioelectronic material design [16].
Experimental Characterization and Validation Methodologies
Mechanical and Electrical Property Assessment
Rigorous experimental characterization is essential to validate the performance of soft bioelectronic materials. The following methodologies provide comprehensive assessment of key material properties:
Mechanical Testing Protocol:
- Elastic modulus measurement: Perform uniaxial tensile testing using standardized specimens (e.g., 30mm × 10mm × 1mm) to determine Young's modulus under physiological strain rates (1-10% strain)
- Cyclic fatigue testing: Subject materials to repeated deformation cycles (typically 10,000+ cycles) at strains relevant to the target tissue (15-30% for peripheral nerves, 10-15% for brain tissue)
- Adhesion strength: Measure interfacial toughness between the hydrogel semiconductor and biological tissues using 90-degree peel tests or lap shear tests
Electrical Characterization Protocol:
- Impedance spectroscopy: Measure electrochemical impedance across frequency range 1 Hz-1 MHz using standard electrolyte solutions (e.g., PBS at 37°C)
- Charge storage capacity: Determine using cyclic voltammetry at physiologically relevant scan rates (1-100 mV/s)
- Stability assessment: Monitor electrical performance during continuous operation in simulated physiological conditions for extended durations (1000+ hours)
In Vitro and In Vivo Functional Validation
Beyond basic material properties, functional validation demonstrates practical efficacy in biological contexts:
In Vitro Biosensing Assessment:
- Sensitivity quantification: Immerse hydrogel semiconductor devices in solutions containing target biomarkers at physiological concentrations (e.g., cytokines, neurotransmitters)
- Selectivity testing: Evaluate response to interfering substances present in biological fluids
- Response time measurement: Monitor temporal response to sudden concentration changes
In Vivo Biocompatibility and Efficacy:
- Foreign body reaction assessment: Implant materials subcutaneously or in target neural tissues for 4-12 weeks, then histologically examine fibrotic capsule thickness, immune cell infiltration, and vascularization
- Functional efficacy: In disease models (e.g., rheumatoid arthritis, epilepsy), compare therapeutic outcomes between hydrogel-based devices and traditional implants
- Chronic stability: Evaluate device performance and tissue response over extended periods (6+ months) relevant to clinical applications
Diagram 1: Experimental characterization workflow for soft bioelectronic materials, covering mechanical, electrical, and biological validation stages.
Design Principles for Next-Generation Soft Bioelectronics
Material Selection and Device Architecture
The design of soft bioelectronic devices requires careful consideration of multiple interrelated factors to achieve optimal performance in biological environments. Future bioelectronic systems are envisioned as distributed networks across three interweaved layers: the implant layer, an optional wearable companion layer, and a user interface layer for communication with patients, physicians, or cloud services [1].
Front-End Electrode Design: Modern neural interfaces are shifting from traditional metals to advanced materials that better bridge the biological-electronic divide. Conducting polymers have emerged as particularly promising candidates due to their mixed ionic/electronic conductivity, mechanical flexibility, and enhanced biocompatibility [1]. These materials offer reduced impedance compared to traditional electrodes, enabling further miniaturization that promotes treatment selectivity while reducing off-target effects [1]. Additional materials under investigation include graphene, MXenes, and carbon nanotubes, each offering unique electronic and optical properties beneficial for specific applications [1].
Device Encapsulation Strategies: Chronic implants require packaging that maintains functionality for 5-10 years in the harsh environment of the body [1]. Traditional approaches use hermetic packages to protect electronics from bodily fluids, but these are often rigid and create mechanical mismatch. Emerging strategies include:
- Thin-film encapsulation: Using multiple layers of biocompatible polymers and inorganic barriers
- Conformal coatings: Applying precise, pinhole-free coatings that accommodate device flexibility
- "Living electrode" concepts: Integrating cell layers into bioelectronic devices as functional interfaces that minimize biotic/abiotic mismatch [1]
Power and Data Management
Miniaturization and soft form factors introduce significant challenges for power delivery and data communication in implantable devices:
Wireless Power Transfer: Battery-less implants represent an important trend in soft bioelectronics, eliminating the need for battery replacement surgeries and facilitating device miniaturization [1]. Multiple wireless powering techniques are under development:
- Inductive/electrical transfer: Using coupled coils to transmit power through tissue
- Ultrasound-based powering: Employing piezoelectric materials to convert acoustic energy to electrical energy
- Magneto-electric and optical approaches: Emerging methods showing promise for specific applications
Data Communication Systems: The choice of communication systems involves careful trade-offs between local preprocessing and data transmission [1]. As implants become more sophisticated, some therapeutic approaches may require multiple implants that communicate and synchronize with each other [1]. This necessitates circuit designs that address multiple channels while providing efficient on-board processing capabilities. Neuromorphic circuits offer particularly promising approaches due to their power-efficient information processing properties suitable for edge computing paradigms at the implant level [1].
Table 2: Comparison of Wireless Power Transfer Methods for Soft Bioelectronics
| Method | Principle | Advantages | Limitations | Suitable Applications |
|---|---|---|---|---|
| Inductive Coupling | Magnetic field coupling between coils | High efficiency at short range, well-established technology | Rapid efficiency drop with distance, sensitive to misalignment | High-power applications (neural stimulators) |
| Ultrasonic Transfer | Piezoelectric conversion of acoustic waves | Better tissue penetration, less directional | Lower power density, potential tissue heating | Deep implants, distributed sensor networks |
| Optical Powering | Photovoltaic conversion of light | High power density, precise targeting | Limited tissue penetration, requires external light source | Subdermal implants, wearable integration |
| Magneto-Electric | Magnetic field to strain to voltage | Miniaturized receivers, medium penetration | Complex material systems, developing technology | Miniature implants, neural dust concepts |
The Scientist's Toolkit: Essential Materials and Reagents
Developing soft, flexible bioelectronics requires specialized materials and reagents that enable the creation of tissue-integrated electronic devices. The following toolkit outlines essential components for research in this emerging field:
Table 3: Research Reagent Solutions for Soft Bioelectronics Development
| Category | Specific Materials | Function/Purpose | Key Characteristics |
|---|---|---|---|
| Semiconductor Polymers | DPP-based polymers, PEDOT:PSS, P3HT | Provide semiconductive properties in hydrated environment | Conjugated backbones, tailorable side chains, mixed conductivity |
| Hydrogel Matrix Materials | Polyacrylamide, Poly(ethylene glycol) diacrylate, Alginate, Gelatin methacrylate | Create hydrated, tissue-like mechanical environment | High water content, tunable modulus, biocompatibility |
| Conducting Polymers | PEDOT:PSS, PANI, PPy | Enable efficient ion-to-electron transduction at tissue interface | Mixed ionic/electronic conduction, mechanical flexibility |
| Crosslinking Agents | APS/TEMED, Irgacure 2959, LAP photoinitiators | Facilitate hydrogel formation and stability | Controlled gelation kinetics, biocompatible byproducts |
| Solvent Systems | DMSO, DMF, THF with aqueous mixtures | Enable solvent exchange processing | Water-miscible organic solvents with polymer solubility |
| Encapsulation Materials | Parylene-C, PDMS, SU-8, Silicon nitride | Protect electronic components from biological fluids | Conformal coating, barrier properties, mechanical compliance |
| Characterization Reagents | Potassium ferricyanide, PBS, synthetic interstitial fluid | Electrochemical and functional testing | Physiologically relevant ionic environment |
The technological shift from rigid implants to soft, flexible bioelectronics represents a fundamental advancement in bioelectronic medicine's core material science. Hydrogel semiconductors and other soft electronic materials bridge the mechanical mismatch between conventional electronics and biological tissues, enabling more intimate biointerfaces with reduced foreign body response. This paradigm shift, supported by novel manufacturing approaches like solvent exchange processing, facilitates devices that maintain excellent electronic functionality while achieving tissue-like mechanical properties.
Looking forward, several key challenges must be addressed to advance these technologies toward clinical application. Further material development is needed to enhance the stability and performance consistency of soft bioelectronic devices under chronic implantation conditions. Manufacturing processes must be scaled while maintaining precision and reproducibility. Regulatory frameworks need to adapt to these hybrid material systems that combine characteristics of medical devices, biologics, and drugs. Finally, standardized sterilization methods and implantation techniques must be developed specifically for these delicate, compliant devices.
The continued convergence of materials science, neural engineering, and molecular medicine will enable increasingly sophisticated bioelectronic therapies that seamlessly integrate with the nervous system. As these technologies mature, they promise to transform the treatment of chronic diseases through precise, personalized neuromodulation approaches that fundamentally improve upon both traditional pharmaceuticals and first-generation electronic implants.
Bioelectronic medicine represents a paradigm shift in therapeutic intervention, moving beyond pharmaceutical chemistry to use electrical signals for diagnosing and treating disease. This field leverages advanced neuromodulation technologies to interface with the nervous system, interpreting and manipulating neural signals to restore physiological balance. The foundational principle rests on understanding that the nervous system serves as the body's master communication network, continuously monitoring organ function and coordinating responses through precise electrical signaling. By targeting specific anatomical structures and neural pathways, bioelectronic devices can modulate everything from inflammatory responses to heart function, offering unprecedented precision in treating conditions as diverse as rheumatoid arthritis, epilepsy, depression, and inflammatory bowel disease [3] [10].
The therapeutic potential of bioelectronic medicine stems from the nervous system's inherent role as a biological interface that connects cognitive functions with peripheral physiology. This connection forms what researchers describe as the "brain–heart–immune axis," a communication network that enables centralized control over distributed bodily functions. Understanding the anatomical organization and functional specialization within this system provides the essential framework for developing targeted neuromodulation therapies that can achieve specific physiological outcomes with minimal side effects [17].
Core Neuroanatomy for Therapeutic Targeting
Central Nervous System Architecture
The central nervous system (CNS), comprising the brain and spinal cord, functions as the integrative command center for all neural processing. This system receives, processes, and responds to sensory information through highly specialized regions that can be selectively targeted for therapeutic modulation [18] [19].
Table 1: Major Central Nervous System Structures and Therapeutic Relevance
| Anatomical Structure | Primary Functions | Therapeutic Applications | Example Interventions |
|---|---|---|---|
| Cerebral Cortex | Voluntary movement, cognition, sensory processing | Stroke recovery, chronic pain, movement disorders | Transcranial direct current stimulation (tDCS), cortical implants |
| Thalamus | Sensory relay station, consciousness regulation | Chronic pain, disorders of consciousness | Deep brain stimulation (DBS) |
| Hypothalamus | Homeostasis, autonomic control, neuroendocrine function | Metabolic disorders, sleep disorders, hypertension | Focused ultrasound, implantable stimulators |
| Brainstem | Cardiorespiratory control, consciousness, cranial nerve functions | Epilepsy, depression, migraine, respiratory control | Vagus nerve stimulation (VNS), respiratory pacemakers |
| Cerebellum | Motor coordination, balance, motor learning | Movement disorders, tremor, ataxia | Cerebellar stimulation, non-invasive modulation |
| Spinal Cord | Sensorimotor relay, reflex integration | Paralysis, chronic pain, bladder control | Spinal cord stimulation (SCS), intraspinal interfaces |
| Limbic System | Emotion, memory, motivation | Depression, PTSD, addiction | Deep brain stimulation, responsive neurostimulation |
The cerebral cortex represents the most evolved region of the human brain, with different lobes specializing in distinct functions. The frontal lobe enables voluntary motor control and executive functions, the parietal lobe processes somatosensory information, the temporal lobe manages auditory processing and memory, and the occipital lobe specializes in visual processing. Each of these regions offers unique targeting opportunities for conditions ranging from stroke recovery to neuropsychiatric disorders [18].
Deeper brain structures provide additional critical targets. The thalamus serves as the central relay station for sensory information, making it ideal for pain management interventions. The hypothalamus, despite its small size, regulates fundamental processes including heart rate, blood pressure, appetite, and hormonal release through connections with the pituitary gland. The brainstem houses essential autonomic centers controlling respiration, cardiovascular function, and consciousness, while the cerebellum fine-tunes motor commands to ensure smooth, coordinated movements [18].
The spinal cord forms the final common pathway for CNS output, containing both ascending sensory pathways and descending motor pathways. This organization creates opportunities for interventions at multiple levels to restore function after injury or disease. The recent development of non-invasive spinal cord stimulation techniques has shown promise for addressing urinary dysfunction, bowel control, and sexual function following cervical spinal cord injury [17].
Peripheral Nervous System Pathways
The peripheral nervous system (PNS) connects the CNS to organs, limbs, and skin, creating the communication network that enables whole-body integration. The PNS is functionally divided into the somatic nervous system (mediating voluntary movements) and the autonomic nervous system (regulating involuntary physiological processes) [19].
The autonomic nervous system represents a particularly valuable target for bioelectronic medicine, as it controls visceral functions that are frequently disrupted in chronic disease. This system is further subdivided into sympathetic ("fight-or-flight") and parasympathetic ("rest-and-digest") branches, which generally exert opposing effects on target organs. The vagus nerve, as the primary parasympathetic nerve, has emerged as a particularly promising target given its extensive innervation of thoracic and abdominal organs and its fundamental role in regulating inflammation, heart rate, and gastrointestinal function [10] [17].
Table 2: Key Peripheral Nerves for Bioelectronic Intervention
| Nerve/Target | Innervation | Physiological Influence | Clinical Applications |
|---|---|---|---|
| Vagus Nerve | Heart, lungs, digestive tract, liver, spleen | Heart rate reduction, inflammation control, gastric motility | Rheumatoid arthritis, epilepsy, depression, inflammatory bowel disease |
| Spinal Nerves | Limbs, trunk, neck | Motor control, sensory feedback | Chronic pain, motor rehabilitation, peripheral nerve injury |
| Splanchnic Nerves | Abdominal viscera | Gastrointestinal function, visceral sensation | Irritable bowel syndrome, visceral pain |
| Sacral Nerves | Bladder, bowel, reproductive organs | Urination, defecation, sexual function | Incontinence, bladder dysfunction, fecal incontinence |
Recent advances have demonstrated that the autonomic nervous system provides a precise communication pathway between the brain and peripheral immune function. This "neuro-immune axis" enables neural modulation of inflammation, creating opportunities for treating conditions like rheumatoid arthritis through vagus nerve stimulation rather than immunosuppressive drugs. The recent FDA approval of SetPoint Medical's vagus nerve stimulation device for rheumatoid arthritis represents a landmark validation of this approach [3] [10].
Molecular Signaling and Neurotransmitter Systems
Key Neurotransmitter Pathways
Neurotransmitters serve as the chemical messengers of neural communication, converting electrical signals into chemical signals at synapses throughout the nervous system. These molecules represent critical intervention points for both pharmacological and bioelectronic approaches, as their balance directly influences neuronal excitability, information processing, and ultimately physiological outcomes [20].
Table 3: Major Neurotransmitter Systems and Modulation Strategies
| Neurotransmitter | Primary Action | Receptor Types | Role in Disease | Modulation Approaches |
|---|---|---|---|---|
| Glutamate | Primary excitatory neurotransmitter | NMDA, AMPA, kainate, metabotropic | Excitotoxicity in stroke, Alzheimer's, ALS | Receptor antagonists, release modulation |
| GABA (γ-aminobutyric acid) | Primary inhibitory neurotransmitter | GABAA (ionotropic), GABAB (metabotropic) | Epilepsy, anxiety, insomnia | Receptor agonists, reuptake inhibitors |
| Acetylcholine | Autonomic control, neuromuscular junction | Nicotinic, muscarinic | Myasthenia gravis, Alzheimer's, autonomic dysfunction | Receptor agonists/antagonists, cholinesterase inhibitors |
| Norepinephrine | Sympathetic nervous system activation | α1, α2, β1, β2-adrenergic | Depression, anxiety, hypertension | Reuptake inhibitors, receptor blockers |
| Dopamine | Motor control, reward, motivation | D1-D5 receptors | Parkinson's disease, schizophrenia, addiction | Receptor agonists, precursor supplementation |
| Serotonin | Mood, appetite, sleep | 5-HT1-7 receptors | Depression, anxiety, migraine | Reuptake inhibitors, receptor agonists |
Glutamate serves as the predominant excitatory neurotransmitter in the CNS, playing essential roles in synaptic plasticity, learning, and memory. However, excessive glutamate release can lead to excitotoxicity, a process implicated in various neurological conditions including stroke, epilepsy, and neurodegenerative diseases. The balance between glutamate and GABA, the primary inhibitory neurotransmitter, determines neuronal network stability and represents a crucial target for maintaining neural homeostasis [20].
The cholinergic system, centered around acetylcholine, deserves particular attention in bioelectronic medicine due to its fundamental role in the "inflammatory reflex"—a neural circuit through which the vagus nerve regulates immune function. Vagus nerve stimulation activates cholinergic signaling that suppresses pro-inflammatory cytokine release, providing a mechanistic explanation for the anti-inflammatory effects observed in conditions like rheumatoid arthritis [3] [17].
Signaling Pathways in Neural Circuits
The therapeutic effects of neuromodulation emerge from precisely altering activity in specific neural circuits. Understanding these circuits at both the anatomical and molecular levels enables increasingly targeted interventions.
Diagram 1: Neuro-Immune Signaling Circuit
The diagram above illustrates the inflammatory reflex circuit, a well-characterized neural pathway that connects peripheral inflammation to brain-mediated responses through the vagus nerve. This circuit begins with sensory neurons detecting inflammatory cytokines, relaying this information to CNS integration centers, which in turn activate autonomic output through the vagus nerve to suppress inflammation via cholinergic signaling to immune cells [3] [17].
Experimental Methodologies and Technical Approaches
Neural Interface Technologies
Advanced neural interfaces form the technological foundation of bioelectronic medicine, enabling precise recording and modulation of neural activity. These interfaces vary significantly in their invasiveness, spatial resolution, and target applications.
Table 4: Neural Interface Modalities and Characteristics
| Interface Type | Invasiveness | Spatial Resolution | Temporal Resolution | Key Applications |
|---|---|---|---|---|
| Non-invasive (tDCS, TMS) | Non-invasive | Low (cm) | Medium (ms) | Depression, chronic pain, stroke rehabilitation |
| Transcutaneous (tVNS, tsFUS) | Minimally invasive | Medium (mm-cm) | High (μs-ms) | Inflammation control, epilepsy, metabolic disorders |
| Peripheral Nerve Interfaces | Surgical implantation | High (μm-mm) | High (μs-ms) | Rheumatoid arthritis, IBD, blood pressure control |
| Spinal Cord Stimulators | Surgical implantation | Medium (mm) | High (μs-ms) | Chronic pain, spasticity, bladder control |
| Deep Brain Stimulators | Surgical implantation | High (μm-mm) | High (μs-ms) | Parkinson's disease, epilepsy, depression |
Non-invasive techniques like transcranial direct current stimulation (tDCS) and transcranial magnetic stimulation (TMS) modulate cortical excitability through external application of electrical currents or magnetic fields. These approaches offer the advantage of minimal risk but provide relatively limited spatial resolution and depth penetration. Recent innovations in temporal interference (TI) stimulation have enabled non-invasive targeting of deeper brain structures by using multiple high-frequency fields that interfere to create a net stimulation effect only at their intersection point [10] [17].
Implantable interfaces provide superior specificity and access to deeper neural targets but require surgical intervention. The development of closed-loop systems represents a particularly promising advance, as these devices can continuously monitor physiological or neural biomarkers and automatically adjust stimulation parameters in response. This creates self-regulating therapeutic systems that can adapt to changing patient needs in real time [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Key Research Reagents for Neural Circuit Investigation
| Reagent/Material | Category | Research Application | Experimental Function |
|---|---|---|---|
| Channelrhodopsins (ChR2) | Optogenetic actuator | Neural circuit mapping | Light-activated cation channel for neuronal excitation |
| Halorhodopsins (NpHR) | Optogenetic inhibitor | Neural circuit manipulation | Light-activated chloride pump for neuronal inhibition |
| AAV vectors | Viral delivery tool | Targeted gene delivery | Neuron-specific transduction for optogenetic/chemogenetic manipulation |
| DREADDs | Chemogenetic tool | Remote neural control | Designer receptors exclusively activated by designer drugs |
| Neurotransmitter sensors (iGluSnFR, dLight) | Molecular sensor | Neurotransmitter release monitoring | Genetically encoded fluorescent indicators of neurotransmitter dynamics |
| Multielectrode arrays | Electrophysiology tool | Neural population recording | High-density recording of extracellular neuronal activity |
| Carbon fiber electrodes | Neural interface | In vivo electrophysiology | Single-unit recording and stimulation in behaving animals |
| Neurotrophic factors (BDNF, NGF) | Biological response modifier | Neural plasticity studies | Enhancement of neuronal survival, growth, and synaptic plasticity |
The experimental workflow for investigating and validating neural targets typically begins with molecular tools for circuit mapping, progresses through physiological recording and manipulation, and culminates in behavioral or therapeutic outcome assessment. Optogenetics has revolutionized neural circuit dissection by enabling millisecond-precise control of genetically defined neuronal populations, while chemogenetic approaches like DREADDs (Designer Receptors Exclusively Activated by Designer Drugs) offer remote neuronal manipulation over longer timescales without implanted hardware [21].
Advanced electrophysiological systems provide critical readouts of neural activity, with high-density multielectrode arrays enabling simultaneous recording from hundreds of neurons. These tools are essential for deciphering the neural codes that represent sensory information, motor commands, and pathological states. The development of miniaturized, wireless recording systems has further enabled the study of naturalistic behaviors without movement constraints [17].
Diagram 2: Experimental Workflow for Target Development
The experimental workflow for target development follows a logical progression from basic anatomical identification through clinical translation. Each stage builds upon findings from the previous one, with continuous refinement of both biological understanding and technological capabilities. This iterative process ensures that therapeutic interventions are grounded in rigorous mechanistic understanding while meeting practical clinical requirements [21] [10] [17].
Emerging Frontiers and Future Directions
The field of bioelectronic medicine continues to evolve rapidly, with several emerging frontiers promising to expand therapeutic capabilities. Non-invasive neuromodulation approaches represent a particularly promising direction, as they eliminate surgical risks and can be more readily scaled for widespread clinical use. The combination of non-invasive techniques with closed-loop control systems creates opportunities for adaptive therapies that continuously optimize treatment parameters based on real-time physiological feedback [10].
Another significant frontier involves the development of pathogen-specific neuromodulation strategies. Research has revealed that the body produces unique neural response patterns to different infectious agents over time. Creating a "pathogen library" of these signature responses could enable precise identification of infectious agents and guide targeted neuromodulation interventions to impede pathogen-specific inflammatory cascades. This approach could revolutionize the management of infectious diseases and sepsis [10].
Bioelectronic approaches also show exceptional promise for addressing mental health disorders through modulation of the neuro-immune axis. Conditions including post-traumatic stress disorder, major depression, and anxiety disorders have been linked to inflammatory processes and vagus nerve pathology. The emerging ability to assess brain inflammation through techniques like autonomic neurography may enable objective stratification of mental health severity and guide precise neuromodulation treatments tailored to individual neuro-immune profiles [10].
The convergence of bioelectronic medicine with artificial intelligence and machine learning is already yielding sophisticated approaches for treatment personalization. Recent studies have demonstrated that machine learning algorithms can optimize non-invasive brain stimulation parameters for major depression and predict individual treatment responses. These computational approaches leverage high-dimensional physiological data to identify biomarkers that guide therapy selection and parameter optimization, moving beyond the traditional one-size-fits-all approach to neuromodulation [17].
As the field advances, the integration of increasingly sophisticated biological understanding with cutting-edge engineering innovations promises to unlock new therapeutic possibilities across a broad spectrum of diseases. The ongoing refinement of neural interfaces, combined with deeper insights into neural circuit function and pathology, positions bioelectronic medicine as a transformative approach that harnesses the body's inherent communication systems for precise, adaptive therapeutic intervention.
Bioelectronic medicine represents a transformative frontier in therapeutic science, founded on the interdisciplinary convergence of neuroscience, materials science, and microelectronics. This field utilizes advanced technological devices to interface with the electrically active nervous system to diagnose and treat diseases, offering a paradigm shift from conventional pharmacotherapies [1]. By establishing direct communication pathways with neural circuits, bioelectronic medicine promises targeted, personalized treatments with reduced off-target effects for conditions ranging from inflammatory diseases and metabolic disorders to paralysis and mental health conditions [3] [7] [10]. The foundational principle hinges on decoding the language of the nervous system—electrical and chemical signals—and developing sophisticated interfaces to modulate these signals with precision. This convergence has accelerated dramatically in recent years, driven by simultaneous advances in neural circuit mapping, flexible electronics manufacturing, and miniature implanted systems capable of closed-loop operation [22] [1].
The therapeutic potential of bioelectronic medicine is vast. The nervous system maintains homeostasis and health through complex reflex circuits that control involuntary processes, including immune function, inflammation, cardiovascular regulation, and metabolism [7]. Homeostatic disruptions underlying numerous diseases can be controlled by bioelectronic devices targeting central and peripheral neural circuits [7]. For instance, the inflammatory reflex—a neural circuit mediated by the vagus nerve that regulates immune function and inflammation—can be modulated using bioelectronic vagus nerve stimulation (VNS) to suppress excessive pro-inflammatory cytokine release and alleviate deleterious inflammation in rheumatoid arthritis, inflammatory bowel disease, and other chronic inflammatory conditions [3] [7]. The growing clinical translation of these approaches is evidenced by recent FDA approvals of bioelectronic devices for autoimmune diseases and the expanding markets for spinal cord stimulation, deep brain stimulation, and vagus nerve stimulation technologies [1].
Foundational Scientific Principles
Neural Signaling and Circuit Mechanisms
The nervous system functions through intricate networks of electrical and chemical signaling that maintain physiological homeostasis. Billions of neurons collectively form neural networks, transmitting information via electrophysiological signals (action potentials) and neurochemical messengers (neurotransmitters) to facilitate essential biological activities, including perception, learning, memory, and autonomic functions [22]. These signaling mechanisms enable the nervous system to regulate virtually every organ and physiological process in the body, forming the basis for bioelectronic interventions [7].
The inflammatory reflex represents a paradigmatic neural circuit for bioelectronic medicine. This vagus nerve-mediated reflex arc regulates peripheral immune function and inflammation through a well-characterized pathway [7]. Afferent (sensory) vagus nerve fibers, representing 80-85% of vagus neurons, detect peripheral inflammatory mediators and relay this information to the brainstem nucleus tractus solitarius (NTS) [7]. This sensory input is integrated within the brainstem, leading to efferent vagus nerve signaling that culminates in the release of norepinephrine in the spleen, which activates choline acetyltransferase (ChAT)-positive T cells to release acetylcholine [7]. This acetylcholine then binds to α7 nicotinic acetylcholine receptors (α7nAChR) on macrophages, suppressing the release of pro-inflammatory cytokines such as TNF [7]. This circuit provides a specific molecular target for bioelectronic intervention in inflammatory diseases.
Materials Science for Neural Interfaces
Materials science provides the critical bridge between biological tissues and electronic systems in bioelectronic medicine. Conventional rigid electronic materials exhibit significant mechanical mismatch with soft, dynamic biological tissues, often leading to tissue injury, immune reactions, and chronic inflammation that impair device performance and longevity [22]. Flexible materials and innovative structural designs address these limitations by enhancing biocompatibility, mechanical compliance, and sensing performance [22].
Carbon-based nanomaterials, including carbon nanotubes and graphene, have emerged as particularly promising materials for neural interfaces due to their high electrical conductivity, large specific surface area, and excellent biocompatibility [22]. Graphene fiber microelectrodes demonstrate significantly higher sensitivity for dopamine detection (1.54 nA/μM) compared to conventional carbon fiber microelectrodes (0.41 nA/μM), attributed to faster electron transfer rates and superior antifouling capabilities [22]. Conducting polymers represent another important class of neural interface materials, offering unique mixed ionic/electronic conductivity that seamlessly bridges the gap between biological and electronic systems [1]. Their mechanical flexibility, enhanced biocompatibility, and reduced impedance compared to traditional electrodes allow for miniaturization that promotes treatment selectivity while reducing off-target effects [1].
Table 1: Advanced Materials for Neural Interfaces
| Material Class | Representative Materials | Key Properties | Applications |
|---|---|---|---|
| Carbon-Based Nanomaterials | Carbon nanotubes, Graphene, Graphene oxide (GO), Reduced graphene oxide (rGO) | High electrical conductivity, Large specific surface area, Excellent biocompatibility, Antifouling capabilities | Dopamine detection, Neurotransmitter sensing, Multimodal neural recording |
| Conducting Polymers | PEDOT, PPy | Mixed ionic/electronic conductivity, Mechanical flexibility, Reduced impedance, Enhanced biocompatibility | Neural recording electrodes, Stimulation interfaces, Conformable neural probes |
| Metallic Composites | Gold, Platinum, Iridium oxide | High charge injection capacity, Biostability, Conformability in nanostructured forms | Microelectrode arrays, Stimulation contacts, Flexible electronics |
| Hybrid Materials | MXenes, Carbon nanotube yarns | Novel electronic/optical properties, Tunable surface chemistry, Stretchability | Multimodal sensing, Closed-loop systems, Bi-directional interfaces |
Microelectronics and System Integration
Microelectronics technology enables the miniaturization, integration, and functionality of bioelectronic devices. Modern bioelectronic systems typically comprise an implant layer with electrode arrays for tissue interfacing, electronics for signal processing and stimulation generation, communication modules for data transfer, and power management systems [1]. The trend toward bidirectional, multimodal implants that combine recording, stimulation, and sometimes drug delivery capabilities represents a significant advancement in the field [1].
Closed-loop systems constitute a particularly promising direction for bioelectronic medicine. These systems continuously monitor physiological signals and automatically adjust stimulation parameters in real-time to optimize therapeutic outcomes [22] [10]. For example, closed-loop optical stimulation systems can suppress abnormally firing neurons in the hippocampal region while activating inhibitory interneurons, effectively blocking epileptic seizure cascades in animal models with response latencies as low as 50 ms [22]. The integration of machine learning and artificial intelligence further enhances these systems by enabling dynamic adjustment of electrical stimulation parameters and developing predictive models for conditions such as seizure risk, significantly improving intervention timeliness [22].
Wireless power and communication technologies address the critical challenge of providing continuous operation without bulky batteries or percutaneous connections. Wireless powering techniques based on inductive/electrical coupling or ultrasound allow for battery-less implants that are easier to miniaturize and avoid the need for surgical battery replacements [1]. Similarly, advanced communication systems enable data transfer in and out of the body, with design trade-offs between local pre-processing and transmission bandwidth [1]. In some advanced therapeutic paradigms, multiple implants communicate and synchronize with each other, requiring sophisticated circuitries that address multiple channels and implement on-board processing functionalities [1].
Experimental Methodologies and Workflows
Multimodal Neural Signal Acquisition
Comprehensive investigation of neural function requires simultaneous acquisition of multiple signal modalities, including electrophysiological activity, neurochemical dynamics, and mechanical variations. Integrated sensing systems capable of simultaneously capturing electrophysiological, mechanical, and neurochemical signals provide multidimensional information essential for understanding complex neural mechanisms [22].
Flexible electrode arrays enable simultaneous recording of neuronal electrical activity and local stress variations. When combined with nano-piezoresistive sensors embedded in microfluidic chips, these systems achieve in situ monitoring of neurotransmitter diffusion dynamics and fluid pressure fluctuations [22]. For neurochemical monitoring, carbon fiber microelectrodes (CFMEs) and carbon nanotube yarn microelectrodes (CNTYMEs) treated with electrochemical activation methods demonstrate significantly enhanced sensitivity for cationic neurotransmitters [22]. Fast-scan cyclic voltammetry (FSCV) provides real-time measurement of dynamic changes in neurochemicals in the living brain, essential for elucidating the molecular mechanisms underlying neurophysiological and pathological processes [22].
Neural Interface Fabrication Protocols
The fabrication of advanced neural interfaces incorporates specialized materials processing and microstructuring techniques to achieve desired mechanical and electrical properties. Serpentine geometries patterned in thin (<1 μm) inorganic device layers enable inherently non-stretchable materials to achieve low bending stiffness and stretchability, enhancing their compatibility with biological tissues [22]. This structural engineering approach, combined with novel material compositions, enables the development of neural interfaces with enhanced biocompatibility and chronic stability.
Graphene fiber microelectrodes (GFMEs) are synthesized via a hydrothermal method using graphene oxide (GO) and reduced graphene oxide (rGO) [22]. The synthesis process involves:
- Preparation of graphene oxide dispersion through modified Hummers' method
- Hydrothermal assembly of GO dispersion into fiber structures at 230°C for 6 hours
- Chemical reduction using hydriodic acid to obtain rGO fibers
- Thermal annealing at 800°C under argon atmosphere to enhance crystallinity and electrical conductivity
- Electrochemical characterization using cyclic voltammetry and electrochemical impedance spectroscopy
Surface modification protocols enhance electrode performance and specificity. Electrochemical treatments using KOH on carbon fiber microelectrodes (CFMEs) and carbon nanotube yarn microelectrodes (CNTYMEs) result in approximately a twofold increase in CFME sensitivity and a two- to fourfold enhancement in CNTYME sensitivity toward cationic neurotransmitters [22]. This treatment creates negatively charged nanogap surfaces that preferentially attract cationic species while repelling anionic metabolites such as DOPAC [22].
Closed-Loop System Implementation
Closed-loop bioelectronic systems represent the cutting edge of neural interface technology, enabling adaptive, personalized therapies based on real-time physiological feedback. These systems integrate neural signal acquisition, computational analysis, and therapeutic modulation in an integrated architecture [22] [10].
A representative experimental workflow for implementing closed-loop neuromodulation involves:
- Signal Acquisition: High-density electrode arrays record neural activity from target regions (e.g., motor cortex for movement disorders, hippocampus for epilepsy)
- Feature Extraction: Real-time processing algorithms extract relevant biomarkers from recorded signals (e.g., beta band power for Parkinson's disease, high-frequency oscillations for epilepsy)
- Decision Algorithm: Machine learning classifiers detect pathological states or predict disease events based on the extracted features
- Therapeutic Stimulation: Upon detection of target states, the system delivers precisely timed electrical, optical, or chemical stimulation to specific neural circuits
- Outcome Assessment: Continuous monitoring of physiological responses enables iterative optimization of stimulation parameters
In animal models of epilepsy, closed-loop optical stimulation systems achieve seizure suppression by targeting specific neuronal populations [22]. These systems detect seizure onset from local field potential recordings and deliver brief light pulses to optogenetically-modified inhibitory interneurons, effectively blocking seizure propagation with response latencies of 50 ms [22]. Similarly, in spinal cord injury rehabilitation, implantable closed-loop systems achieve bidirectional interaction by adaptively adjusting both electrical stimulation intensity and drug release rates based on real-time biomechanical feedback, overcoming the limitations of traditional open-loop approaches [22].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagents and Materials for Bioelectronic Medicine
| Category | Specific Reagents/Materials | Function/Application | Key Characteristics |
|---|---|---|---|
| Electrode Materials | Carbon nanotubes, Graphene fibers, PEDOT:PSS, Iridium oxide | Neural recording and stimulation interfaces | High conductivity, Biocompatibility, Low impedance, Charge injection capacity |
| Flexible Substrates | Polyimide, Parylene-C, Polydimethylsiloxane (PDMS) | Structural support for flexible electronics | Mechanical compliance, Biostability, Insulating properties |
| Neurochemical Sensors | Carbon fiber microelectrodes, CNT yarn microelectrodes, Enzyme-modified electrodes | Real-time neurotransmitter detection | High sensitivity (e.g., 1.54 nA/μM for DA), Selectivity, Fast temporal response |
| Neural Modulation Tools | Optrodes, Microfluidic channels, Piezoresistive elements | Combined stimulation and sensing | Multimodal integration, Cell-type specificity (optogenetics), Mechanical sensing |
| Signal Processing Tools | FPGA boards, ASICs, Neuromorphic chips | Real-time signal analysis for closed-loop systems | Low power consumption, High processing speed, Adaptive algorithms |
| Encapsulation Materials | Silicon nitride, Silicon carbide, ALD coatings | Protection of electronics from biological fluids | Hermeticity, Biostability, Flexibility, Long-term reliability |
Quantitative Data and Performance Metrics
The performance of bioelectronic devices is characterized by quantitative metrics that guide material selection and system optimization. Sensitivity, signal-to-noise ratio (SNR), charge injection capacity, and impedance represent critical parameters for neural interfaces [22] [1].
Graphene fiber microelectrodes (GFMEs) demonstrate significantly higher sensitivity toward dopamine detection (1.54 nA/μM in Tris buffer) compared to conventional carbon fiber microelectrodes (CFMEs, 0.41 nA/μM in Tris buffer) [22]. This improvement is attributed to the GFMEs' faster electron transfer rates (indicated by a smaller ΔEp), higher redox cycling efficiency (Ir/Io approaching 1), and superior antifouling capability against serotonin [22]. Electrochemical treatments using KOH on carbon-based electrodes result in approximately a twofold increase in CFME sensitivity and a two- to fourfold enhancement in carbon nanotube yarn microelectrode (CNTYME) sensitivity toward cationic neurotransmitters [22].
Table 3: Performance Metrics for Neural Interface Technologies
| Technology/Material | Key Performance Metric | Value/Range | Context/Application |
|---|---|---|---|
| Graphene Fiber Microelectrodes | Dopamine Sensitivity | 1.54 nA/μM | Tris buffer, Superior to conventional CFMEs |
| Conventional CFMEs | Dopamine Sensitivity | 0.41 nA/μM | Tris buffer, Baseline comparison |
| KOH-treated CFMEs | Cationic Neurotransmitter Sensitivity | ~2x increase | Post-electrochemical treatment |
| KOH-treated CNTYMEs | Cationic Neurotransmitter Sensitivity | 2-4x increase | Post-electrochemical treatment |
| Closed-loop Optical Stimulation | Response Latency | 50 ms | Epileptic seizure blockade in animal models |
| Mechanical-Electrical-Chemical Systems | Motor Function Recovery Time | 40% reduction | Animal studies of spinal cord injury |
| Conducting Polymer Electrodes | Impedance Reduction | Significant decrease vs. metals | Enables miniaturization, improves safety |
Future Directions and Translational Challenges
The future evolution of bioelectronic medicine will be shaped by advances in miniaturization, intelligence, and integration. Key research directions include the development of battery-less implants powered by wireless energy transfer techniques based on inductive/electrical coupling or ultrasound [1]. These approaches facilitate device miniaturization, eliminate the need for surgical battery replacements, and improve environmental sustainability [1]. The convergence of machine learning with bioelectronic systems enables increasingly sophisticated closed-loop therapies that adapt to individual patient needs and disease states [22] [10].
Significant translational challenges remain in the path toward widespread clinical implementation. Foreign body reaction (FBR) represents a fundamental challenge for chronic implants, triggering inflammatory responses that can compromise device functionality [1]. The shift from traditional stiff electrodes to more flexible, stretchable designs helps bridge the mechanical mismatch with biological tissue, reducing FBR [1]. Innovative approaches such as "living electrodes" that integrate cell layers into bioelectronic devices show promise for minimizing biotic/abiotic mismatch [1]. Long-term biostability requires advanced encapsulation materials and techniques that protect electronic components from bodily fluids while maintaining mechanical flexibility [1]. Silicon nitride, silicon carbide, and atomic layer deposition (ALD) coatings represent promising encapsulation strategies under investigation [1].
The scaling of stimulation parameters across species presents another critical challenge for clinical translation. Recent research indicates that previous translation efforts did not adequately account for interspecies differences in nerve anatomy, leading to suboptimal parameter selection [17]. Systematic approaches to parameter translation that consider nerve morphology and functional organization are essential for successful clinical development [17]. As the field progresses, non-invasive bioelectronic techniques are gaining prominence for their potential to avoid surgical risks while enabling broader deployment [10]. Techniques such as transcranial magnetic stimulation and transcutaneous vagus nerve stimulation offer distinct advantages, including scalability and reduced regulatory barriers [10].
The interdisciplinary convergence of neuroscience, materials science, and microelectronics will continue to drive innovation in bioelectronic medicine, ultimately transforming the treatment landscape for numerous neurological, inflammatory, metabolic, and mental health disorders. Through continued collaboration across these disciplines, bioelectronic medicine promises to deliver increasingly sophisticated, personalized therapies that harness the body's innate neural circuits for therapeutic benefit.
Therapeutic Neuromodulation: Devices and Clinical Implementation
Bioelectronic medicine represents a transformative frontier in therapeutic science, focusing on modulating nervous system signals to treat a wide array of diseases. This field converges material science, biochemistry, neuroscience, immunology, and bioengineering to develop devices that record, stimulate, or block neural signaling for therapeutic purposes [3]. Implantable neurostimulation platforms constitute a cornerstone of bioelectronic medicine, delivering targeted electrical impulses to specific neural pathways to restore physiological balance and function. These platforms operate on the principle that the nervous system functions as a biological network that can be modulated with precise electrical stimuli to treat conditions ranging from movement disorders to inflammatory diseases [3] [17].
The three most established implantable neurostimulation platforms—Deep Brain Stimulation (DBS), Spinal Cord Stimulation (SCS), and Vagus Nerve Stimulation (VNS)—have evolved from rudimentary electrical therapies to sophisticated, targeted systems. The global neurostimulation devices market, valued at USD 6.21 billion in 2024, is projected to grow to USD 11.69 billion by 2032, exhibiting a compound annual growth rate (CAGR) of 8.3% [23]. This growth trajectory underscores the increasing clinical adoption and technological advancement of these platforms within the broader context of bioelectronic medicine research and application.
Global Market and Clinical Landscape
The implantable neurostimulation market demonstrates robust growth driven by technological innovations, rising prevalence of neurological disorders, and increasing preference for non-pharmaceutical interventions. The market encompasses diverse device types, with invasive devices currently dominating the landscape with approximately 95.5% market share in 2024 [23]. Pain management represents the largest application segment, accounting for 55.7% of market share, followed by movement disorders and psychiatric conditions [23].
Table 1: Global Neurostimulation Devices Market Overview
| Parameter | 2024 Status | Projected Growth |
|---|---|---|
| Market Size | USD 6.21 billion [23] | USD 11.69 billion by 2032 (CAGR 8.3%) [23] |
| Dominant Device Type | Invasive devices (95.5% share) [23] | Non-invasive segment growing at 4.5% CAGR [23] |
| Leading Application | Pain management (55.7% share) [23] | Psychiatric disorders segment growing at 8.3% CAGR [23] |
| Primary End User | Hospitals & Specialty Clinics (78.3% share) [23] | Research & Academic Institutes growing at 7.41% CAGR [23] |
| Regional Dominance | North America (44.12% share) [23] | Asia Pacific exhibiting fastest growth [23] |
North America dominates the neurostimulation landscape, holding 44.12% of the global market share in 2024 [23]. This dominance is attributed to advanced healthcare infrastructure, high disease prevalence, and supportive regulatory frameworks. The United States Deep Brain Stimulation devices market specifically is projected to reach USD 1.2 billion in 2025, growing at a CAGR of 9.8% [24]. Europe follows with a significant market share, driven by an aging population and strong research infrastructure, while the Asia-Pacific region represents the fastest-growing market due to improving healthcare access and rising awareness [23] [25].
Deep Brain Stimulation (DBS) Platforms
Deep Brain Stimulation involves the stereotactic implantation of electrodes into specific deep brain structures to deliver controlled electrical impulses for neuromodulation. Modern DBS systems consist of four key components: the implanted electrode(s), extension wires, an implantable pulse generator (IPG), and an external programmer for parameter adjustment [26] [24]. DBS technology has evolved significantly since its modern inception in 1947 with the introduction of stereotactic apparatus by Spiegel and Wycis, with subsequent refinements in electrode design, targeting precision, and programmability [26].
The primary applications for DBS include movement disorders such as Parkinson's disease, essential tremor, and dystonia, with expanding indications for psychiatric conditions including obsessive-compulsive disorder (OCD) and treatment-resistant depression [26] [24]. Parkinson's disease represents the most common application, accounting for 67.2% of DBS procedures, followed by essential tremor at 23.8% and dystonia at 3.8% [26].
Quantitative Market Data and Clinical Statistics
The global DBS devices market is projected to experience consistent growth from USD 1.3 billion in 2023 to USD 3.5 billion by 2033, at a CAGR of 10.2% [26]. This growth is fueled by technological advancements including directional leads, closed-loop systems, and AI-enabled programming algorithms that enhance therapeutic precision [24].
Table 2: Deep Brain Stimulation Market and Clinical Statistics
| Parameter | Value | Source |
|---|---|---|
| Global Market Size (2025 Projection) | USD 3.9 billion [24] | Dimension Market Research |
| Projected Market Size (2034) | USD 9.4 billion [24] | Dimension Market Research |
| Growth Rate (2025-2034) | CAGR 10.4% [24] | Dimension Market Research |
| U.S. Market Size (2025 Projection) | USD 1.2 billion [24] | Dimension Market Research |
| Procedure Volume (U.S., 1996-2017) | 72,427 discharges for DBS [26] | The Lancet |
| Most Common Indication (Parkinson's) | 67.2% of DBS procedures [26] | The Lancet |
| Robotic Surgery Adoption | 6.3% of neurostimulator-related admissions [26] | The Lancet |
The competitive landscape for DBS devices is characterized by dominance by a few key players. Abbott leads the sector with a 15% market share, closely followed by Medtronic at 14% and Boston Scientific Corporation at 13% [26]. Other significant contributors include Aleva Neurotherapeutics S.A. (11%), Nexstim (9%), and LivaNova PLC (9%) [26].
Key Experimental Protocols and Methodologies
Surgical Implantation Protocol: DBS implantation follows a standardized protocol beginning with high-resolution MRI for anatomical targeting. Following frame-based or frameless stereotactic registration, surgical planning software identifies coordinates for target structures (e.g., subthalamic nucleus for Parkinson's disease, ventral intermediate nucleus for essential tremor). Microelectrode recording is often employed for physiological confirmation before permanent macroelectrode placement. Intraoperative test stimulation assesses therapeutic effects and side effect thresholds. The procedure concludes with subcutaneous IPG implantation in the pectoral region, connected via extension wires [26] [24].
Programming and Optimization Protocol: Postoperative programming typically begins 2-4 weeks after implantation to allow for resolution of microlesion effects. Systematic parameter testing includes electrode configuration selection (monopolar/bipolar), amplitude adjustment (typically 1-4 V), pulse width (60-120 μs), and frequency (130-185 Hz for movement disorders). Outcome measures include standardized rating scales (UPDRS for Parkinson's disease, FTM for essential tremor), with optimization occurring over multiple sessions [24]. Recent advances incorporate AI-driven algorithms to predict optimal parameter combinations based on patient-specific characteristics [24].
Spinal Cord Stimulation (SCS) Platforms
Spinal Cord Stimulation systems employ epidurally implanted electrode arrays to deliver electrical impulses that modulate pain signaling pathways in the dorsal columns of the spinal cord. Modern SCS platforms have evolved from simple paresthesia-based systems to sophisticated devices offering multiple waveform options, including high-frequency, burst, and closed-loop stimulation [27]. The primary indications for SCS include failed back surgery syndrome (FBSS), complex regional pain syndrome (CRPS), diabetic peripheral neuropathy, and refractory low back pain [23] [27].
Recent technological advancements have significantly improved SCS efficacy and patient experience. Boston Scientific's FAST (Fast-Acting Sub-perception Therapy) platform, for example, demonstrates rapid onset of pain relief within minutes and sustained outcomes over two years [27]. Multiple mechanism approaches that combine different stimulation modalities have shown superior outcomes compared to single-modality systems [27].
Quantitative Clinical Outcomes and Market Position
SCS represents the largest segment within the neurostimulation devices market by device type [23]. Robust clinical evidence supports its efficacy, with recent studies demonstrating compelling outcomes. The SOLIS randomized controlled trial, published in 2025, compared SCS combined with conventional medical management (CMM) against CMM alone for non-surgical refractory back pain [28]. The trial demonstrated that 89.5% of patients receiving SCS+CMM achieved ≥50% pain relief without increased opioid use, compared to only 8.1% in the CMM-only group [28]. Additionally, disability scores (Oswestry Disability Index) improved significantly more in the SCS group (-27.5 points) versus CMM alone (-7.2 points) [28].
Table 3: Spinal Cord Stimulation Clinical Outcomes from Recent Studies
| Outcome Measure | SCS + CMM Group | CMM Alone Group | Statistical Significance |
|---|---|---|---|
| ≥50% Pain Relief (3 months) | 89.5% [28] | 8.1% [28] | p<0.0001 [28] |
| ODI Improvement (3 months) | -27.5±15.9 points [28] | -7.2±9.9 points [28] | p<0.0001 [28] |
| EQ-5D-5L Improvement (3 months) | 0.247±0.164 points [28] | 0.031±0.151 points [28] | p<0.0001 [28] |
| Pain Relief Onset (FAST Therapy) | 2 minutes [27] | N/A | N/A |
| Trial Salvage Rate | 60% [27] | N/A | N/A |
| Implant Salvage Rate | 60% [27] | N/A | N/A |
Long-term outcomes remain encouraging, with the SOLIS trial demonstrating sustained benefits at 12-month follow-up [28]. The WaveWriter Outcomes Study similarly reported durable pain relief through 24 months using systems capable of combination therapy [27].
Key Experimental Protocols and Methodologies
Trial Stimulation Protocol: SCS implementation typically begins with a percutaneous trial period using temporary electrodes connected to an external pulse generator. Under fluoroscopic guidance, electrodes are advanced to the target epidural space (typically T8-T11 for lower extremity pain, higher for upper extremity or axial pain). During the 5-7 day trial period, various stimulation parameters are tested to optimize coverage of painful areas. A successful trial, typically defined as ≥50% pain reduction, leads to permanent implantation [27] [28].
Permanent Implantation and Programming Protocol: Permanent implantation involves surgical placement of paddle-style or percutaneous electrodes connected to an implantable pulse generator. Modern programming approaches include multiple modalities: paresthesia-based programming using low-frequency stimulation (30-100 Hz); sub-perception therapy including high-frequency (1-10 kHz) and burst stimulation; and combination approaches [27]. The COMBO randomized controlled trial demonstrated that allowing patients to choose between sub-perception and paresthesia-based programming yielded superior outcomes [27]. Recent advances incorporate automated programming algorithms and personalized settings based on individual anatomical considerations [27].
Vagus Nerve Stimulation (VNS) Platforms
Vagus Nerve Stimulation systems deliver electrical impulses to the vagus nerve, primarily targeting the left cervical vagus nerve below the cardiac branch to minimize side effects. Traditional VNS requires surgical implantation of a pulse generator in the chest wall with electrodes wrapped around the vagus nerve [29]. More recently, non-invasive transcutaneous VNS (tVNS) devices have emerged, stimulating through the skin either at the cervical region or the auricular branch in the ear [29].
The established clinical applications for VNS include drug-resistant epilepsy and treatment-resistant depression [29]. Epilepsy represents the dominant application, holding a 58.89% revenue share in 2025 [29]. The therapeutic landscape is rapidly expanding to include new indications such as rheumatoid arthritis, with the FDA recently approving SetPoint Medical's bioelectronic medicine device for this application based on pioneering work in neuroimmunomodulation [3]. Additional emerging applications include inflammatory bowel disease, migraine, and anxiety disorders [29].
Quantitative Market Data and Growth Projections
The global VNS market demonstrates robust growth, valued at approximately USD 434.40 million in 2022 and projected to reach USD 970.6 million by 2030, growing at a CAGR of 10.61% [29]. Alternative projections estimate the market will expand from USD 575.81 million in 2025 to USD 974.30 million by 2034 at a CAGR of 6.06% [29]. The U.S. market specifically is expected to grow from USD 8.03 billion in 2025 to USD 18.17 billion by 2033 at a CAGR of 14.58% [29].
Table 4: Vagus Nerve Stimulation Market Segmentation and Projections
| Market Segment | 2025 Status | Growth Outlook | Notes |
|---|---|---|---|
| Overall Global Market | USD 575.81 million [29] | USD 974.30 million by 2034 (CAGR 6.06%) [29] | Alternative projection |
| U.S. Market | USD 8.03 billion [29] | USD 18.17 billion by 2033 (CAGR 14.58%) [29] | Specific regional growth |
| Product Type (Implantable) | 66.3% market share [29] | Steady growth | Dominant segment |
| Product Type (External) | Lower market share [29] | Fastest growing (CAGR 9.05%) [29] | Emerging segment |
| Application (Epilepsy) | 58.89% revenue share [29] | Steady growth | Dominant indication |
| Regional Dominance | North America (54% share) [29] | Maintained leadership | Advanced healthcare infrastructure |
The implantable VNS device segment currently dominates the market, accounting for over 59% of market share in 2022 and projected to hold 66.3% in 2025 [29]. However, the external non-invasive segment is expected to grow at the faster CAGR of 9.05%, reflecting patient preference for less invasive options [29]. North America leads the global VNS market with over 54% share in 2025, driven by high disease prevalence and advanced healthcare infrastructure [29].
Key Experimental Protocols and Methodologies
Surgical Implantation Protocol: Traditional VNS implantation is typically performed under general anesthesia via a horizontal incision in the left neck region for vagus nerve exposure and a separate infraclavicular incision for generator placement. The helical electrodes are carefully wrapped around the vagus nerve, with integrity testing conducted before wound closure [29]. Recent minimally invasive techniques reduce surgical dissection and operative time.
Stimulation Parameter Optimization: Initial programming typically begins 2 weeks postoperatively with standard parameters including output current (0.25-2.0 mA), frequency (20-30 Hz), pulse width (250-500 μs), and duty cycle (typically 30 seconds on/5 minutes off). Parameters are gradually uptitrated based on therapeutic response and side effect profile [29]. For epilepsy, magnet activation allows for additional stimulation during auras or seizure onset.
Experimental Neuroimmunomodulation Protocol: For inflammatory disorders like rheumatoid arthritis, research protocols involve distinct parameter settings targeting the cholinergic anti-inflammatory pathway. SetPoint Medical's approach uses different stimulation parameters (lower frequency, shorter pulse width) than those used for epilepsy or depression [3]. Preclinical studies typically involve electrode implantation followed by established disease models (e.g., collagen-induced arthritis), with systematic monitoring of inflammatory markers and clinical disease scores [3] [17].
Signaling Pathways and Neural Circuits
The therapeutic effects of implantable neurostimulation platforms are mediated through modulation of specific neural pathways and circuits. Understanding these mechanisms is essential for optimizing therapy and developing new applications.
Diagram 1: Neural Pathways for Neurostimulation Platforms
Deep Brain Stimulation primarily modulates dysfunctional circuits within the basal ganglia-thalamocortical network. For Parkinson's disease, high-frequency stimulation of targets like the subthalamic nucleus disrupts pathological oscillatory activity, restoring more normal movement patterns [26] [24]. The mechanisms involve both local inhibition of target structures and downstream network effects throughout the motor circuit.
Spinal Cord Stimulation operates through multiple complementary mechanisms. The traditional "gate control theory" proposes activation of large-diameter fibers inhibits nociceptive transmission in the dorsal horn [27] [28]. More recently, supraspinal mechanisms have been identified, including activation of descending pain inhibitory pathways and modulation of brain regions involved in pain perception [27].
Vagus Nerve Stimulation exerts diverse effects through its widespread central and peripheral projections. Afferent fibers project to the nucleus tractus solitarius, which connects to multiple brain regions including limbic structures (for mood regulation), thalamocortical networks (for seizure control), and autonomic centers [29] [3]. For inflammatory conditions, VNS activates the cholinergic anti-inflammatory pathway, resulting in suppression of pro-inflammatory cytokine production [3] [17].
Research Toolkit: Essential Materials and Reagents
Conducting research on implantable neurostimulation platforms requires specialized equipment, reagents, and experimental models. The following toolkit outlines critical components for preclinical and clinical investigations in this field.
Table 5: Research Reagent Solutions for Neurostimulation Studies
| Research Tool | Function/Application | Specific Examples/Models |
|---|---|---|
| Stereotactic Frames | Precise electrode positioning in DBS research | Frame-based and frameless systems for rodent and primate models |
| Microelectrode Recording Systems | Physiological confirmation of target structures | Single-unit and multi-unit recording during DBS implantation |
| Implantable Pulse Generators | Deliver controlled electrical stimulation | Rechargeable and primary cell systems with programmable parameters |
| Neural Signal Processors | Real-time analysis of neural data | High-density brain-implantable devices with processing capabilities [17] |
| Cytokine Assay Kits | Quantify inflammatory mediators in VNS studies | ELISA-based detection of TNF-α, IL-1β, IL-6 in bioelectronic medicine research [3] |
| Animal Disease Models | Preclinical testing of neurostimulation efficacy | 6-OHDA Parkinson's model, CCI pain model, kainic acid epilepsy model, collagen-induced arthritis |
| Behavioral Assessment Systems | Quantify functional outcomes in animal models | Rotarod for motor function, von Frey for pain sensitivity, seizure rating scales |
| Clinical Rating Scales | Standardized outcome measures in human trials | UPDRS for Parkinson's, VAS for pain, HAM-D for depression, seizure diaries |
Advanced research in bioelectronic medicine increasingly incorporates innovative technologies such as magnetoelectric nanoparticles for selective neural activation [17], closed-loop systems that adapt stimulation based on physiological biomarkers [17], and high-density neural interfaces capable of recording and stimulating simultaneously [17]. The field also employs sophisticated computational models to optimize stimulation parameters and predict neural responses [17].
Emerging Trends and Future Directions
The field of implantable neurostimulation is evolving rapidly, with several transformative trends shaping its future trajectory. Closed-loop systems represent a paradigm shift, moving from continuous open-loop stimulation to adaptive approaches that respond to physiological signals. In DBS, responsive neurostimulation systems can detect pathological activity (e.g., seizure precursors or movement disorder signatures) and deliver targeted therapy in real-time [24]. Similar approaches are being developed for SCS, where stimulation parameters adjust based on changes in posture or activity [27].
Miniaturization and advanced materials are enabling next-generation devices with improved biocompatibility and functionality. Thin-film electrodes, wireless power transfer, and compact electronics facilitate less invasive implantation and extended device longevity [25] [24]. The integration of artificial intelligence and machine learning algorithms enhances device personalization, with systems increasingly capable of optimizing stimulation parameters based on individual patient responses and patterns of use [25].
The therapeutic scope of neurostimulation continues to expand beyond traditional neurological and psychiatric applications. Bioelectronic medicine approaches are being investigated for autoimmune conditions (rheumatoid arthritis, inflammatory bowel disease) [3], metabolic disorders (obesity, diabetes) [17], cardiovascular diseases (heart failure, hypertension) [17], and cognitive impairment [24]. These applications leverage the anatomical connectivity and physiological regulatory capacity of the nervous system to restore homeostasis without pharmaceutical agents.
The convergence of neurostimulation with other advanced technologies creates additional opportunities. Brain-computer interfaces enable direct communication between neural systems and external devices [25]. Gene therapy combined with neurostimulation offers potential for targeted neuromodulation through optogenetic or chemogenetic approaches [3]. Non-invasive stimulation techniques, including temporal interference and focused ultrasound, may eventually provide alternatives to some surgical implantations [17].
As the field advances, key challenges remain, including reducing device costs, improving accessibility in developing regions, addressing long-term reliability concerns, and navigating complex regulatory pathways. Nevertheless, the continued innovation in implantable neurostimulation platforms promises to significantly expand therapeutic options for patients with diverse medical conditions, solidifying the role of bioelectronic medicine as a pillar of modern medical science.
Closed-loop bioelectronic systems represent a paradigm shift in therapeutic interventions, moving beyond static stimulation to dynamic, adaptive modulation based on real-time physiological feedback. These intelligent systems continuously monitor biomarker activity and automatically adjust stimulation parameters to maintain optimal therapeutic efficacy while minimizing side effects. This technical guide explores the core principles, implementation methodologies, and current applications of closed-loop architectures in bioelectronic medicine, providing researchers with a comprehensive framework for developing next-generation adaptive neuromodulation therapies. By integrating advanced sensing capabilities, machine learning algorithms, and responsive stimulation protocols, closed-loop systems offer unprecedented precision in treating neurological disorders, chronic inflammatory conditions, and cardiovascular diseases, positioning them at the forefront of personalized medicine.
Closed-loop bioelectronic systems represent a significant evolution from traditional open-loop approaches, which deliver predetermined electrical stimulation without regard to dynamic physiological states. These intelligent systems create a continuous feedback cycle where physiological biomarkers are monitored in real-time, processed through sophisticated algorithms, and used to dynamically adjust stimulation parameters for optimal therapeutic effect [30]. This self-regulating capability allows for precise titration of therapy that adapts to the patient's fluctuating needs, potentially enhancing efficacy while reducing side effects associated with constant, non-contingent stimulation [10].
The fundamental architecture of closed-loop systems comprises three core components: biosensors for continuous physiological monitoring, computational units for real-time signal processing and decision-making, and neuromodulation interfaces for delivering adaptive stimulation. This integrated approach enables the system to respond to moment-to-moment changes in disease state, medication levels, or environmental factors that influence symptom severity [31]. For conditions like Parkinson's disease, where symptom expression fluctuates throughout the day, this adaptive capability is particularly valuable for maintaining consistent therapeutic benefit across varying physiological states [31].
The transition to closed-loop paradigms reflects the broader maturation of bioelectronic medicine from simple electrical stimulation devices to sophisticated systems that interface bidirectionally with the nervous system. Where early devices like cardiac pacemakers and deep brain stimulators operated with fixed parameters, modern closed-loop systems leverage advances in materials science, microelectronics, and machine learning to achieve unprecedented precision in neuromodulation [4]. This evolution mirrors developments in other technology sectors toward intelligent, responsive systems that adapt to user needs and environmental context.
Core Principles and System Architecture
Fundamental Components and Workflow
Closed-loop bioelectronic systems operate through an integrated workflow that continuously cycles between monitoring, analysis, and intervention. The system begins with biosensing, where implanted or wearable sensors detect relevant electrophysiological signals, biochemical markers, or behavioral metrics [32]. These signals are then processed through real-time analytics that extract meaningful features correlated with disease state or symptom severity [33]. Based on this analysis, adaptive algorithms determine optimal stimulation parameters, which are executed through neuromodulation interfaces that deliver precisely titrated electrical stimulation to target neural circuits [30]. This cycle typically operates on timescales ranging from milliseconds for neural applications to minutes for inflammatory conditions, depending on the pathophysiology being targeted.
The diagram below illustrates the core operational workflow of a closed-loop bioelectronic system:
Key Technological Elements
Biosensing Platforms form the critical input layer of closed-loop systems. For neural applications, these typically include electrodes for recording local field potentials, electrocorticography, or single-unit activity [31]. Advanced systems incorporate multi-modal sensing capable of detecting electrophysiological signals, neurotransmitter release, inflammatory cytokines, and behavioral metrics [32]. Flexible bioelectronics with tissue-matching mechanical properties have significantly improved signal quality and long-term stability by minimizing inflammatory responses and motion artifacts [4].
Computational Architecture transforms raw sensor data into control signals for modulation. This involves real-time signal processing to remove noise and artifacts, followed by feature extraction to identify biomarkers relevant to disease state [33]. For Parkinson's disease, beta-band (13-30 Hz) oscillations in the subthalamic nucleus serve as a well-validated biomarker for bradykinesia and rigidity severity [31]. Machine learning algorithms increasingly enable personalized biomarker detection that adapts to individual patient signatures and long-term disease progression.
Adaptive Stimulation Interfaces deliver precisely calibrated neuromodulation based on computational outputs. Contemporary systems can adjust multiple stimulation parameters including amplitude, frequency, pulse width, and spatial targeting [31]. Advanced implementations use current steering and field shaping techniques to dynamically redirect stimulation to optimal anatomical targets as the patient moves or their disease state fluctuates. The development of soft, conformable electrodes has significantly improved the precision and stability of neural interfaces [32].
Quantitative Outcomes and Clinical Efficacy
Closed-loop systems demonstrate distinct advantages across multiple therapeutic domains, with quantitative benefits observed in both clinical outcomes and system performance metrics. The following table summarizes key efficacy data from recent studies and clinical implementations:
Table 1: Quantitative Outcomes of Closed-Loop Bioelectronic Systems
| Application Domain | Key Biomarker | Stimulation Adjustment | Clinical Outcome | Study Details |
|---|---|---|---|---|
| Parkinson's Disease (Adaptive DBS) | Subthalamic beta power (13-30 Hz) | Amplitude modulation based on beta power thresholds [31] | Significant improvement in overall well-being (5.92 to 6.73 points, p=0.007); trend toward enhanced general movement (p=0.058) [31] | 8 patients, 2-week ecological momentary assessment; 6/8 patients chose to remain on aDBS long-term [31] |
| Chronic Pain (Closed-loop SCS) | Evoked compound action potentials (ECAPs) | Stimulation intensity adjusted to maintain ECAP within therapeutic window [30] | Recent FDA approvals (2022, 2024) with reported improved pain control and reduced paresthesia compared to open-loop SCS [30] | Saluda and Medtronic systems; Onward Medical seeking DeNovo approval for spinal cord injury application [30] |
| Epilepsy (Responsive Neurostimulation) | Epileptiform activity or high-frequency oscillations | Burst stimulation triggered by detected seizure precursors [30] | Medtronic DBS System approved (2018) for adults with focal epilepsy resistant to ≥3 anti-seizure medications [30] | System detects and responds to epileptiform activity in real-time to prevent seizure progression [30] |
| Inflammatory Conditions (Non-invasive) | Autonomic tone via heart rate variability | Focused ultrasound stimulation titrated based on inflammatory cytokine levels [30] | Preclinical models show reduced inflammatory markers in sepsis and rheumatoid arthritis [30] | Emerging non-invasive approach combining autonomic neurography with splenic focused ultrasound stimulation [30] |
The implementation of closed-loop systems also introduces unique programming considerations compared to traditional open-loop approaches. The following table outlines key parameter differences:
Table 2: Programming Parameter Comparison: Open-Loop vs. Closed-Loop Systems
| Parameter | Open-Loop Systems | Closed-Loop Systems | Clinical Implications |
|---|---|---|---|
| Stimulation Amplitude | Fixed, determined during clinical programming | Dynamic range between upper and lower limits (average range: 0.58±0.19 mA) [31] | Prevents over-stimulation (side effects) and under-stimulation (breakthrough symptoms) [31] |
| Temporal Pattern | Continuous or simple cycling | Responsive to biomarker fluctuations | Reduces habituation and improves efficacy during symptom exacerbation [30] |
| Biomarker Utilization | Not used for real-time control | Control signal derived from physiological biomarkers (e.g., beta power) [31] | Enables therapy individualization and adaptation to medication cycles [31] |
| Energy Consumption | Constant power delivery | Variable based on therapeutic demand | Potential for extended battery life with equivalent or improved efficacy [4] |
| Clinical Programming | Periodic clinic visits for parameter adjustment | Initial setup with ongoing autonomous optimization | Reduced clinical burden with maintained optimization across disease progression [31] |
Implementation Methodologies and Technical Protocols
Experimental Setup and System Configuration
Implementing closed-loop bioelectronic systems requires meticulous attention to system configuration, signal processing, and parameter optimization. The following workflow outlines the key stages in establishing an effective closed-loop neuromodulation system:
Biomarker Identification and Validation represents the foundational step in closed-loop system implementation. For Parkinson's disease applications, this involves recording local field potentials from implanted electrodes, typically in the subthalamic nucleus, to identify characteristic beta oscillatory activity [31]. Patients should be evaluated in both OFF and ON medication states to characterize medication-induced modulation of biomarker power. In approximately 25% of implanted hemispheres, no clear beta peak may be visible during initial testing, necessitating evaluation of alternative biomarkers or sensing locations [31]. When double beta peaks are present (occurring in approximately 25% of subthalamic nuclei), test stimulation and medication challenge can help identify the most therapeutically relevant peak for control signals [31].
Signal Acquisition and Processing requires specialized hardware and software architecture. Modern systems utilize integrated sensing amplifiers with sampling rates typically between 250-1000 Hz for local field potentials [31]. Real-time signal processing pipelines, such as those enabled by platforms like Improv, perform bandpass filtering (e.g., 13-30 Hz for beta oscillations), power spectral density estimation, and artifact rejection [33]. Continuous data streaming over several days enables characterization of circadian rhythm influences on biomarker levels, which is essential for setting appropriate long-term control parameters [31]. Adaptive filtering techniques are particularly valuable for distinguishing true physiological signals from motion artifacts or environmental interference.
Threshold Determination and Parameter Setting involves establishing the relationship between biomarker levels and optimal stimulation parameters. Local field potential thresholds are typically set based on percentile distributions of biomarker power during representative activities, with common initial settings at the 25th and 75th percentiles of daytime levels [31]. Substantial inter-individual variability is observed in absolute threshold values (reported ranges: 225-3160 for upper thresholds, 100-2970 for lower thresholds), necessitating personalized calibration [31]. Stimulation amplitude boundaries must be determined through careful titration, evaluating both therapeutic efficacy and side effect profiles across the anticipated operating range. The minimum effective stimulation should be established in the OFF medication state to prevent undershooting during symptom exacerbation [31].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of closed-loop bioelectronic systems requires specialized materials and technical components. The following table catalogues essential research solutions and their applications:
Table 3: Essential Research Reagents and Materials for Closed-Loop Bioelectronics
| Category | Specific Materials/Components | Function/Application | Technical Considerations |
|---|---|---|---|
| Substrate Materials | Parylene-C, Polyimide, Polyethylene terephthalate (PET) [32] | Flexible substrate for conformal tissue interfaces | Ultrathin geometries (<5μm) enable van der Waals-driven adhesion without external adhesives [32] |
| Conductive Elements | Gold (Au), Platinum (Pt), Silver Nanowires, PEDOT:PSS [32] | Electrodes for signal recording and stimulation | PEDOT:PSS enables transparent, flexible OECTs with high transconductance (>400 mS) [32] |
| Sensing Platforms | Organic electrochemical transistors (OECTs), Carbon nanotube networks [32] | Amplification and processing of biosignals | OECTs on parylene-C substrates can achieve high transconductance with >90% optical transparency [32] |
| Computational Framework | Improv software platform, Apache Arrow Plasma library [33] | Real-time data analysis and experimental control | Enables concurrent execution of multiple actors for data acquisition, processing, and visualization [33] |
| Stimulation Interfaces | Directional electrodes, Multi-contact arrays [31] | Targeted delivery of neuromodulation | Allows current steering and field shaping for spatial precision [31] |
| Biocompatible Coatings | Hydrogels, Bioresorbable layers [4] | Interface between device and tissue | Minimizes foreign body response and maintains signal fidelity long-term [4] |
Technical Challenges and Implementation Barriers
Despite their considerable promise, closed-loop bioelectronic systems face significant technical hurdles that must be addressed for widespread clinical adoption. Signal Stability and Quality remains a fundamental challenge, as bioelectronic interfaces must maintain performance in dynamic biological environments characterized by mechanical stress, biochemical degradation, and evolving tissue responses [4]. Endogenous and exogenous noise sources can obscure physiological biomarkers, requiring sophisticated filtering algorithms that distinguish relevant signals from artifacts [30]. Additionally, signal drift may occur over time due to disease progression, therapy-induced neuroplasticity, or fibrotic encapsulation of electrodes, potentially compromising long-term system performance [30].
Algorithm Development and Personalization presents another substantial challenge. Effective control algorithms must balance responsiveness to acute biomarker fluctuations with stability against transient perturbations [31]. Current systems primarily utilize threshold-based controllers, but more sophisticated approaches incorporating predictive modeling and machine learning are emerging [33]. These advanced algorithms must be rigorously validated for safety, particularly regarding the risk of stimulation runaway or inappropriate therapy delivery. Personalization remains resource-intensive, requiring multiple clinical visits for parameter optimization [31]. Developing automated calibration protocols that minimize clinical burden while maintaining therapeutic efficacy is an active area of investigation.
Materials and Manufacturing constraints also impact system reliability. Few clinical systems currently achieve fully bidirectional closed-loop operation, partly due to challenges in creating chronically stable tissue interfaces [4]. The mechanical mismatch between conventional rigid electronic components and soft, dynamic biological tissues can lead to inflammation, fibrosis, and eventual device failure [32]. Emerging solutions include soft, flexible bioelectronics using advanced materials such as stretchable conductors, ultrathin substrates, and conformal electrode arrays that minimize tissue damage while maintaining signal fidelity [4]. Wireless power delivery and communication systems further enhance chronic stability by eliminating percutaneous connections that pose infection risks [32].
Future Directions and Emerging Applications
The evolution of closed-loop bioelectronic medicine is progressing toward increasingly sophisticated systems with expanded clinical applications. Multi-modal Sensing and Stimulation approaches represent a promising frontier, integrating complementary biomarkers to enhance system robustness and therapeutic precision [10]. For example, future Parkinson's disease systems may combine neural electrophysiology with inertial measurement of motor symptoms and autonomic monitoring to create comprehensive state estimation [31]. Similarly, inflammatory disorders might be targeted through integrated monitoring of neural, immune, and metabolic signals to guide vagus nerve stimulation [30].
Advanced Computational Approaches including machine learning and artificial intelligence are being increasingly integrated into closed-loop architectures. These technologies enable more sophisticated biomarker identification, particularly for conditions without well-defined oscillatory signatures [33]. Adaptive algorithms can continuously refine stimulation parameters based on therapeutic outcomes, effectively "learning" optimal settings for individual patients over time [33]. Cloud connectivity and distributed computing approaches may eventually enable population-level optimization, where systems learn from aggregated data across many patients while maintaining individual privacy and autonomy [10].
Non-invasive and Minimally Invasive Systems represent a particularly promising direction for expanding the accessibility and applications of closed-loop bioelectronic medicine. Recent advances in focused ultrasound stimulation and autonomic neurography demonstrate the potential for effective closed-loop modulation without surgical implantation [30]. These approaches could substantially broaden the therapeutic scope of bioelectronic medicine beyond current indications, potentially encompassing common conditions such as hypertension, metabolic syndrome, and inflammatory disorders [10]. Combined with wearable biosensing platforms, non-invasive closed-loop systems may eventually deliver personalized neuromodulation as a first-line therapy with significantly reduced risk profiles compared to pharmaceutical interventions or invasive procedures [30].
As the field advances, the integration of closed-loop bioelectronic systems with other therapeutic modalities—including pharmaceuticals, biologics, and lifestyle interventions—will likely create synergistic treatment approaches that address the multifaceted nature of chronic diseases. These developments position closed-loop bioelectronic medicine as a cornerstone of next-generation precision healthcare, offering dynamic, individualized therapy that adapts to each patient's evolving physiological needs.
Bioelectronic medicine represents a paradigm shift in therapeutic interventions, moving beyond pharmacological compounds to target disease pathophysiology through precise modulation of neural circuits [10]. This field leverages advancements in material science, biochemistry, immunology, neuroscience, and bioengineering to develop novel treatments for a spectrum of conditions including cancer, rheumatoid arthritis, inflammatory bowel disease, paralysis, and cardiovascular disease [3]. The foundational principle involves decoding and modulating electrical signaling within the nervous system to regulate molecular mechanisms and restore physiological balance [3].
Vagus nerve stimulation (VNS) for rheumatoid arthritis (RA) exemplifies the translational success of bioelectronic medicine. This approach leverages the "inflammatory reflex," a neural circuit that detects and regulates immune function and inflammation [34]. The recent FDA approval of SetPoint Medical's bioelectronic device for RA marks a pivotal moment, establishing neuroimmunomodulation as a valid treatment modality for autoimmune diseases [3] [35]. This milestone, based on the pioneering work of Dr. Kevin J. Tracey, demonstrates how targeted neuromodulation can offer a non-pharmacological alternative for patients with inadequate responses to conventional biologic or targeted synthetic disease-modifying antirheumatic drugs (b/tsDMARDs) [3] [34].
Mechanism of Action: The Neuroimmune Pathway
The therapeutic effect of VNS in RA is mediated through the inflammatory reflex, a hardwired neural circuit that connects the brain and immune system to maintain immunological homeostasis [34]. The following diagram illustrates this neuroimmune signaling pathway.
Figure 1. Neuroimmune signaling pathway activated by vagus nerve stimulation. Electrical stimulation of vagal efferents activates the inflammatory reflex, ultimately leading to reduced pro-inflammatory cytokine release via splenic cholinergic signaling to α7nAChR receptor-expressing macrophages.
The molecular mechanism involves acetylcholine release from cholinergic terminals in the spleen binding to α7 nicotinic acetylcholine receptors (α7nAChR) on macrophages, which inhibits nuclear factor kappa B (NF-κB) signaling and subsequent release of pro-inflammatory cytokines including tumor necrosis factor (TNF), interleukin-1β (IL-1β), and IL-6 [34]. This pathway enables the nervous system to exert precise control over systemic inflammation without causing broad immunosuppression.
Clinical Evidence and Outcomes
Efficacy Data from Pivotal Trials
The RESET-RA study, a randomized, double-blind, sham-controlled pivotal trial, established the foundation for FDA approval of the SetPoint System [36] [37]. This trial enrolled 242 patients with moderately to severely active RA who were incomplete responders or intolerant to at least one b/tsDMARD [37]. The study met its primary efficacy endpoint with statistically significant improvement in ACR20 response at 12 weeks compared to control (p=0.0209) [37].
Table 1. Clinical efficacy outcomes from the RESET-RA trial through 12 months
| Efficacy Measure | 3 Months | 6 Months | 9 Months | 12 Months | Notes |
|---|---|---|---|---|---|
| ACR20 Response | 42.4% (TNFi subgroup) | 52.1% | 51.7% | 55.8% | Primary endpoint met at 3 months (p=0.0209) [37] |
| ACR50 Response | - | - | - | 38% (TNFi subgroup) | Sustained improvement observed [37] |
| ACR70 Response | - | - | - | 16% (TNFi subgroup) | Progressive improvement over time [37] |
| DAS28-CRP LDA/Remission | Significant vs control | - | - | 49.3% | Low Disease Activity/Remission (DAS28-CRP <3.2) [37] |
| CDAI LDA/Remission | - | - | - | 47.4% | Clinical Disease Activity Index improvement [37] |
| EULAR Response | - | - | - | 77.3% | Good/moderate response [37] |
| Erosion Progression | 18.9% (treatment) vs 37.8% (control) | - | - | - | Erosive subgroup, p=0.0156 [37] |
Long-term extension studies demonstrate durable responses through 36 months. In patients with multidrug-refractory RA who had previously failed an average of 4.8 different drugs, the median change in Clinical Disease Activity Index (CDAI) from baseline to month 36 was -17.8 (SEM 4.9), with 64% (7/11) of patients achieving a CDAI response meeting or exceeding the minimal clinically important difference [38].
Safety Profile and Tolerability
The safety data from clinical trials establishes VNS as a well-tolerated intervention with a favorable risk-benefit profile for treatment-refractory RA populations.
Table 2. Safety outcomes from VNS clinical trials in rheumatoid arthritis
| Safety Parameter | Incidence | Notes |
|---|---|---|
| Device/Procedure-Related SAEs | 1.7% (n=4) | Primarily in perioperative period (first 3 months) [36] [37] |
| Post-procedure SAEs (3-12 months) | 0% | No related serious adverse events after perioperative period [37] |
| Common Side Effects | Low rate, typically mild | Hoarseness, cough, throat irritation (often stimulation-linked, transient) [34] [39] |
| Major Safety Events | 0% | No cardiac events, serious infections, or malignancies related to device [36] |
| Therapy Persistence | 97.5% at 12 months | High continuation rate indicates tolerability [37] |
| Surgical Complications | Low | No intraoperative complications, infections, or surgical revisions reported [34] |
The safety profile is particularly notable given that these patients had previously failed multiple conventional therapies, with 64% (9/14) having failed a targeted synthetic DMARD before enrollment in the long-term extension study [38].
Experimental Protocols and Methodologies
RESET-RA Trial Design and Implementation
The RESET-RA trial employed a rigorous methodology to evaluate the safety and efficacy of the SetPoint Medical neuroimmune modulation device:
Study Population: Adults with moderately to severely active RA (≥6 swollen/≥6 tender joints) with inadequate response, loss of response, or intolerance to ≥1 b/tsDMARD [37]. Patients had long-standing disease with mean duration of 10.5 years and high baseline disease activity (mean DAS28-CRP >5.5) [37].
Randomization and Blinding: Participants were randomized to active treatment or sham control in a double-blind design. The sham control involved implantation with the device programmed to deliver non-therapeutic stimulation parameters [34].
Device Implantation: The minimally invasive surgical procedure involved:
- Implantation of miniaturized pulse generator with integrated electrodes on the left cervical vagus nerve within the carotid sheath
- Surgical duration approximately 1 hour
- Silicon pod positioning the pulse generator on the vagus nerve [34]
Stimulation Parameters:
- Pulse frequency: 10 Hz
- Pulse width: 250 µs
- Stimulation duration: 60-second pulse train once daily
- Current intensity: Individualized to patient tolerance and response [34]
Assessment Schedule: Comprehensive evaluations at baseline, 4, 8, 12, 24, 36, and 52 weeks including:
- Clinical measures: ACR response criteria, DAS28-CRP, CDAI, SDAI
- Patient-reported outcomes: Pain, physical function, global assessment
- Laboratory measures: CRP, ESR, cytokine levels (TNF, IL-1, IL-6)
- Imaging: Gadolinium-enhanced MRI of hand/wrist for RAMRIS scoring [37]
Statistical Analysis: Primary endpoint was ACR20 response at 12 weeks using modified non-responder imputation for missing data. Key secondary endpoints included ACR50/70, DAS28-CRP remission, and change in tender/swollen joint counts [37].
Long-term Extension Study Methodology
The 36-month extension study implemented the following protocol:
Participant Flow: Patients completing the initial 12-week blinded period were eligible for rollover into the open-label extension [38].
Stimulation Regimen: Continued once-daily stimulation with the same parameters, though adjustments to current intensity were permitted based on efficacy and tolerability [38].
Concomitant Medications: Patients were permitted to continue stable doses of conventional synthetic DMARDs. Addition of new b/tsDMARDs was documented as therapy augmentation [38].
Safety Monitoring: Comprehensive assessment of adverse events, with particular attention to device-related events, surgical site complications, and vagus nerve stimulation-associated symptoms [38].
Efficacy Assessments: Clinical disease activity indices (CDAI, SDAI, DAS28-CRP), functional status (HAQ-DI), and patient-reported outcomes at 3-month intervals [38].
Research Toolkit: Essential Reagents and Materials
Table 3. Key research reagents and materials for investigating vagus nerve stimulation in inflammatory models
| Reagent/Material | Function/Application | Specifications/Considerations |
|---|---|---|
| Implantable Neuroimmune Modulation Device | Delivers programmed electrical stimulation to vagus nerve | SetPoint Medical device: miniaturized pulse generator with integrated electrodes, silicon positioning pod [34] |
| External Programming System | Wireless device charging and parameter adjustment | iPad application for programming pulse generator, wireless charger [34] |
| Cytokine Assay Kits | Quantification of inflammatory mediators (TNF, IL-1β, IL-6) | ELISA or multiplex platforms; essential for monitoring neuroimmune mechanism [34] |
| α7nAChR Antagonists | Experimental validation of mechanism | α-bungarotoxin or methyllycaconitine; blocks cholinergic anti-inflammatory pathway [34] |
| Vagotomy Surgical Tools | Surgical disruption of vagus nerve for control experiments | Microdissection instruments; creates negative control condition [34] |
| MRI Contrast Agents | Imaging of joint inflammation and structural damage | Gadolinium-based agents for RAMRIS scoring of synovitis, osteitis, erosion [37] |
| Electrophysiology Equipment | Verification of neural activation | Nerve conduction monitoring; confirms target engagement during stimulation [10] |
Future Directions in Bioelectronic Medicine
The successful clinical application of VNS for RA has catalyzed development of next-generation bioelectronic therapies. Current research focuses on several transformative frontiers:
Closed-Loop Systems: Unlike the open-loop SetPoint device (fixed stimulation schedule), next-generation systems incorporate real-time physiological monitoring to enable adaptive stimulation. These systems detect biomarkers of inflammatory state (e.g., cytokine levels, neural signals) and automatically adjust stimulation parameters to maintain therapeutic effect while minimizing side effects [10] [30]. The integration of biosensors with neuromodulation devices represents a paradigm shift toward autonomous, patient-specific therapy titration.
Non-Invasive Approaches: Transcranial magnetic stimulation and transcutaneous vagus nerve stimulation devices represent promising non-invasive alternatives that bypass surgical implantation [10]. These approaches leverage focused ultrasound and other energy modalities to modulate neural circuits through intact skin, potentially expanding access and reducing treatment barriers [30].
Disease Signature Detection: Research indicates the autonomic nervous system produces unique response patterns to different inflammatory stimuli and disease states [10]. Advanced analytical approaches, including machine learning algorithms, are being developed to decode these "neuroimmune signatures" for precise disease characterization and personalized stimulation parameter selection [10].
Expansion to Other Indications: Building on the success in RA, clinical trials are underway or planned for multiple sclerosis, inflammatory bowel disease, lupus, Sjögren's syndrome, and vasculitis [35]. The shared reliance on neuroimmune pathways across inflammatory conditions suggests broad therapeutic potential for bioelectronic approaches.
The convergence of bioelectronic medicine with immunology and neuroscience represents a fundamental shift in therapeutic strategy—from systemic pharmacological suppression to precise neural circuit modulation. As the field advances, bioelectronic approaches promise to expand the treatment arsenal for autoimmune diseases, offering solutions for patients with limited options while potentially reducing reliance on chronic immunosuppression.
Bioelectronic medicine represents a paradigm shift in therapeutic strategies, moving from pharmaceutical interventions to those that use electrical signals to modulate neural pathways for diagnosing and treating disease [10]. This field converges multiple disciplines, including material science, neuroscience, immunology, bioengineering, and electrical engineering to develop devices that can interface with the nervous system [3]. A significant limitation of many current implantable bioelectronic devices is their reliance on bulky batteries with finite lifespans. These batteries often necessitate subsequent replacement surgeries, introducing additional risks, costs, and patient discomfort [40]. Battery-free implants, powered by advanced wireless power transfer (WPT) systems, offer a transformative solution to this challenge. They enable the development of miniaturized, permanently implantable devices that can be deployed through minimally invasive procedures, thereby accelerating the development of next-generation bioelectronic therapies [40].
The evolution of this field is marked by a transition from invasive to non-invasive techniques and from single implants to coordinated networks. As the field progresses, the ability to power multiple, millimeter-sized implants simultaneously and efficiently becomes paramount for advanced applications such as distributed sensing and stimulation in the central or peripheral nervous system [41]. This whitepaper provides an in-depth technical examination of the core architectures enabling this future, with a specific focus on magnetoelectric coupling, metamaterial-enhanced systems, and sophisticated rectenna design.
Core Wireless Power Transfer Technologies
Fundamental Principles and Challenges
Wireless power transfer for implantable medical devices (IMDs) is fundamentally challenged by the biological environment itself. Biological tissues absorb electromagnetic energy, quantified by the Specific Absorption Rate (SAR), and FDA-imposed caps on SAR levels constrain transmitter power [40]. Furthermore, achieving sufficient coupling between the external transmitter (Tx) and internal receiver (Rx) is difficult, with efficiency dropping significantly due to tissue absorption, distance, and misalignment [40]. The primary goal of WPT system design is to maximize the Power Transfer Efficiency (PTE), which is influenced by parameters such as the spatial relationship and alignment between Tx and Rx, and the system's operating frequency [40].
Comparative Analysis of WPT Modalities
The table below summarizes the key technical characteristics of three prominent WPT modalities for implantable devices.
Table 1: Comparison of Wireless Power Transfer Modalities for Implantable Devices
| Technology | Operating Principle | Reported PTE/Performance | Key Advantages | Reported Applications |
|---|---|---|---|---|
| Magnetoelectric Networks [41] | Magnetic field coupling using magnetoelectric materials. | Total system efficiency: 0.2% (1 node) to 1.3% (6 nodes); Power per node: 2.2 mW at 1 cm. | Scalable network architecture; Efficiency improves with additional devices; Robust in biological tissues. | Distributed spinal cord stimulators; Cardiac pacing devices. |
| Metamaterial-Enhanced WPT [40] | Engineered materials (e.g., MNG, CSSRR) placed between Tx and Rx to concentrate power. | Efficiency boost: 46% to 51% (13.56 MHz system) [40]; Enhanced PTE and transmission distance. | Can enhance both near-field and far-field transfer; Overcomes tissue absorption and misalignment. | Neurostimulators; Pressure/glucose sensors; Cardiac pacemakers. |
| Dual-Band Rectenna Systems [42] | Antenna (Rx) and rectifier circuit converting RF to DC power at two frequencies. | RF-to-DC efficiency: 79.9% @ 0.915 GHz/1 dBm; 72.8% @ 2.45 GHz/3 dBm. | Harvests from multiple bands for more stable power; Compact, meandered antenna design. | General deep-implanted BIDs (e.g., for drug delivery, bio-telemetry). |
Technical Deep Dive: Magnetoelectric Architectures
Operational Principle and Experimental Validation
Magnetoelectric wireless transfer represents a significant advancement for networked implants. This approach uses magnetoelectric materials that can effectively convert magnetic energy into electrical energy at the implant site. A recent groundbreaking study demonstrated a network of millimeter-sized, battery-free bioelectronic implants where the total system efficiency increased from 0.2% with a single implant to 1.3% with six implants, with each node receiving 2.2 mW of power at a distance of 1 cm [41]. This unique property of improving system efficiency with additional devices makes it exceptionally suitable for distributed bioelectronic networks.
The experimental protocol for validating such a system typically involves the following steps:
- Fabrication of Magnetoelectric Implants: Miniature implants are fabricated incorporating magnetoelectric transducers and the necessary circuitry for stimulation or sensing.
- In Vivo Testing: Networks ranging from one to six implants are deployed in large animal models (e.g., pigs) to demonstrate proof-of-concept applications.
- Efficiency and Power Measurement: The total system efficiency is calculated by measuring the input power to the external transmitter and the resulting power received and utilized by each implant node. Physiological readouts (e.g., muscle activation, breathing rate) are monitored to confirm device functionality [41].
- Application Demonstration: The study validated the architecture by creating networks of miniature spinal cord stimulators and cardiac pacing devices, confirming robust wireless power transfer and therapeutic efficacy [41].
Figure 1: Magnetoelectric Network Power Transfer. An external transmitter creates a magnetic field that simultaneously and efficiently powers multiple, distributed magnetoelectric implants, which work in concert to produce a therapeutic effect.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Materials for Magnetoelectric and Metamaterial WPT Research
| Research Reagent / Material | Function in Experimental System |
|---|---|
| Magnetoelectric Transducer | Core material that converts external magnetic fields into local electrical energy to power the implant without a battery [41]. |
| Mu-Negative (MNG) Metasurface | A type of metamaterial with negative permeability used to enhance magnetic coupling between transmitter and receiver, boosting PTE [40]. |
| Circular Spiral Split Ring Resonator (CSSRR) | A 2D metasurface design with a high refractive index used to enlarge the effective aperture of the receiver for improved energy capture [40]. |
| Conformal Phased Surface | A flexible/stretchable electromagnetic structure using subwavelength resonant elements as a transmitter to enhance WPT efficiency and distance [40]. |
| Dual-Band Meandered Antenna | A compact implantable antenna designed to efficiently receive power at two different ISM frequency bands (e.g., 0.915 GHz and 2.45 GHz) [42]. |
| Computational Modeling Pipeline (e.g., ASCENT) | Realistic 3D models of nerves and electrodes used to simulate and optimize complex stimulation paradigms and understand mechanism of action before in vivo testing [9]. |
Technical Deep Dive: Metamaterial-Enhanced WPT
Operational Principle and Implementation
Metamaterials are engineered materials with electromagnetic properties not found in nature, such as negative permittivity or permeability. When integrated into WPT systems, they serve to manipulate and concentrate electromagnetic fields, thereby enhancing power transfer. They can be positioned between the transmitter and receiver or function as the transmitter itself [40]. The primary mechanism involves modifying the direction of the magnetic field and enhancing evanescent waves at deep sub-wavelength scales, which increases PTE through resonant coupling and effectively extends the transfer distance [40].
Various configurations have been experimentally validated:
- High-Refractive-Index CSSRR Metasurface: A circular spiral split ring resonator metasurface operating at 2.40–2.48 GHz can increase the effective aperture of the Rx coil, improving PTE. This design has been simulated and measured on a flexible substrate to conform to skin curvature [40].
- Dual-Layer MNG Metasurface: A mu-negative (MNG) metasurface placed on the skin can enhance PTE to a receiver implanted 3 mm beneath the skin. The dual-layer design increases induced current, which is transmitted to the receiver side, and can support simultaneous power and data transfer [40].
- SRR Metamaterial Array: A 5x5 array of split-ring resonator (SRR) units at 13.56 MHz can augment evanescent wave coupling. When integrated with an LC resonant tank to counteract efficiency losses from eddy currents, this configuration has been shown to boost coil efficiency from 46% to 51% [40].
Technical Deep Dive: Rectenna System Design
Core Components and Workflow
A rectenna (rectifying antenna) is a critical component for far-field WPT, consisting of an implantable antenna and a rectifier circuit. Its function is to harvest radiated RF energy and convert it into usable DC power to operate the implant or recharge a battery [42]. Dual-band rectennas are particularly advantageous as they can harvest energy from multiple frequency bands, providing more stable and reliable power for complex implants [42].
The design and validation workflow for an implantable rectenna system involves a multi-stage process, as illustrated below.
Figure 2: Implantable Rectenna Development Workflow. The process involves designing miniaturized antennas and efficient rectifiers, integrating them into a biocompatible package, and rigorously testing performance in a tissue-simulating environment.
Experimental Protocol for Dual-Band Rectenna Characterization
A detailed methodology for implementing and testing a dual-band rectenna, as referenced in the search results, is as follows [42]:
- Antenna Fabrication: Design a compact dual-band antenna (e.g., based on a meandered-resonator with a slotted ground plane) for operation at 0.915 and 2.45 GHz ISM bands. The antenna should be miniaturized (e.g., to (5 \times 5.25 \times 0.25) (\text{mm}^3)) and exhibit quasi-omnidirectional radiation patterns.
- Rectifier Circuit Fabrication: Design a dual-band rectifier using a dual-branch matching network (e.g., an L-matching network and open-circuited stub in each branch). The rectifier must be optimized for high RF-to-DC conversion efficiency at the target frequencies and input power levels.
- System Integration: Integrate the antenna and rectifier circuit inside a capsule device that simulates the final implantable package.
- In Vitro Testing Setup: Place the fabricated and encapsulated rectenna inside a phantom biological tissue (e.g., minced pork meat) to simulate the implant environment.
- Power Transmission and Measurement: Use a wideband log-periodic antenna as an external RF source (WPT transmitter), connected to an RF signal generator. Measure the resulting DC output voltage across a load resistor at the rectenna's output using a digital multimeter (DMM).
- Efficiency Calculation: Calculate the RF-to-DC conversion efficiency for each frequency band using the measured output DC power and the known input RF power. Analyze the Power Transmission Efficiency (PTE) of the complete WPT link.
The roadmap for next-generation bioelectronic medicine points toward non-invasive or minimally invasive closed-loop systems that can self-regulate based on patient-specific biomarkers [10]. The WPT architectures detailed herein are fundamental enablers for this future. Key research frontiers include:
- Closed-Loop Autonomic Neuromodulation: Developing systems that record physiological data (e.g., inflammatory biomarkers, heart rate variability) and use this feedback to automatically adjust nerve stimulation parameters in real-time, providing truly individualized therapy [10] [9].
- Advanced Computational Modeling: Using realistic computational models based on 3D nerve anatomies to optimize complex stimulation paradigms (like intermittent interferential current stimulation) and understand their mechanism of action, reducing reliance on exhaustive animal experiments [9].
- Non-Invasive Bioelectronic Diagnostics: Exploring the use of bioelectronic signals, such as autonomic neurography, to diagnose disease by identifying unique pathogen-specific "signatures" in the body's neural signals, potentially enabling early intervention [10].
In conclusion, the move away from batteries and toward sophisticated wireless power architectures is not merely a technical improvement but a necessary evolution for the field of bioelectronic medicine. Technologies like magnetoelectric networks, metamaterial-enhanced WPT, and advanced rectennas are paving the way for miniaturized, distributed, and permanently implantable devices that will enable precise, personalized, and closed-loop therapies for a wide range of chronic diseases.
Bioelectronic medicine is an emerging multidisciplinary field that uses electronic devices to diagnose, monitor, and treat disease by modulating the body's electrical signaling pathways [43]. This approach represents a paradigm shift from conventional pharmacology, offering targeted, reversible, and personalized control over physiological processes such as inflammation, mood, metabolism, and cardiovascular function [43]. The field has evolved from foundational discoveries like Luigi Galvani's 18th-century experiments on "animal electricity" to modern clinical applications including cardiac pacemakers, deep brain stimulation for Parkinson's disease, and vagus nerve stimulation for rheumatoid arthritis and inflammatory bowel disease [43].
The effectiveness of bioelectronic medicine hinges on the interface between electronic devices and biological tissues, where material innovations play a crucial role [44]. Conducting polymers and graphene-based materials have emerged as particularly promising interface materials due to their unique combination of electrical properties, mechanical characteristics, and biocompatibility [45] [46]. These materials form the critical link between traditional electronic components and the nervous system, enabling more efficient signal recording and stimulation while minimizing damage to surrounding tissues [44]. As the field advances toward miniaturized, closed-loop systems that integrate artificial intelligence for real-time adaptive therapy, the development of sophisticated biocompatible interfaces becomes increasingly essential for next-generation bioelectronic medicines [10].
Fundamental Properties of Conducting Polymers for Biomedical Interfaces
Conducting polymers (CPs) represent a unique class of organic materials that exhibit electrical and optical properties comparable to those of inorganic semiconductors and metals, while maintaining the desirable mechanical traits and processability of conventional polymers [45]. The electrical conductivity in these materials arises from a conjugated electron backbone along the polymer chain, which features alternating single and double bonds [45]. This extended π-electron system can be precisely tuned through doping processes to achieve specific electrical characteristics ranging from semiconducting to metallic behavior.
The most extensively studied conducting polymers for biomedical applications include polypyrrole (PPy), polyaniline (PANI), and poly(3,4-ethylenedioxythiophene) (PEDOT) [45]. These polymers can be synthesized through various methods including electrochemical deposition, chemical oxidation polymerization, and vapor-phase polymerization, each offering distinct advantages for creating different morphological structures such as thin films, nanotubes, nanofibers, and scaffolds [45]. The ability to process these materials into diverse architectures enables their integration with various biomedical devices and tissue engineering constructs.
Table 1: Key Conducting Polymers and Their Biomedical Applications
| Polymer | Electrical Conductivity | Key Advantages | Primary Biomedical Applications |
|---|---|---|---|
| PEDOT | ~100-1000 S/cm | High stability, low impedance, excellent charge injection capacity | Neural electrodes, biosensors, tissue engineering scaffolds |
| Polypyrrole (PPy) | 10-100 S/cm | Ease of synthesis, good biocompatibility | Drug delivery systems, nerve guides, biosensing |
| Polyaniline (PANI) | 1-100 S/cm | Tunable conductivity, environmental stability | Tissue engineering, biosensors, antimicrobial coatings |
Conducting polymers offer several critical advantages for biointerfacing applications. Their soft, flexible nature provides a better mechanical match for biological tissues compared to rigid metal electrodes, reducing mechanical mismatch and associated tissue damage [45]. Furthermore, their surface chemistry can be readily modified with biological motifs such as extracellular matrix proteins, peptides, and growth factors to enhance cellular adhesion and integration [45]. These polymers also demonstrate mixed ionic-electronic conduction, which enables efficient translation of electronic signals from devices to ionic signals in biological systems, a crucial capability for effective neural interfacing [45].
Graphene and Graphene-Based Composites for Enhanced Biointerfacing
Graphene, a two-dimensional carbon allotrope composed of a single layer of carbon atoms arranged in a hexagonal lattice, has emerged as a revolutionary material for biomedical applications due to its exceptional properties [46]. These include high electronic and thermal conductivities, superior mechanical strength, and an extremely high surface area [46]. The material's structure, characterized by a large aspect ratio and ability to interact with various molecules through physical and chemical processes, makes it particularly suitable for bioelectronic interfaces [46].
Graphene derivatives such as graphene oxide (GO) and reduced graphene oxide (rGO) have further expanded the material's applicability in biomedical contexts [46]. GO contains oxygen-containing functional groups that enhance its dispersion in solvents and polymeric matrices, while rGO offers a balance between processability and electrical conductivity [46]. These derivatives can be functionalized with metals, antimicrobial drugs, polymers, and natural compounds to create composite materials with enhanced functionality and reduced toxicity [46].
The antimicrobial mechanisms of graphene-based materials involve several pathways, making them particularly valuable for implantable devices. These mechanisms include: physical damage to bacterial cell membranes by sharp edges, leading to loss of membrane integrity and content leakage; generation of oxidative stress through reactive oxygen species (ROS)-dependent and independent pathways; and wrapping and trapping of bacterial cells, which isolates them from the environment and inhibits proliferation [46]. The antimicrobial effectiveness depends on factors such as particle size, number of layers, surface modification, and the nature of the targeted microorganism, with generally greater efficacy against Gram-positive bacteria compared to Gram-negative strains [46].
Table 2: Graphene-Based Materials and Their Key Characteristics for Biomedical Applications
| Material Type | Key Characteristics | Advantages for Biointerfaces | Limitations |
|---|---|---|---|
| Pristine Graphene | High electrical/thermal conductivity, mechanical strength | Excellent signal transduction, durability | Poor dispersibility, potential toxicity |
| Graphene Oxide (GO) | Oxygen functional groups, hydrophilic, modifiable | Enhanced biocompatibility, easy functionalization | Reduced electrical conductivity |
| Reduced Graphene Oxide (rGO) | Intermediate oxygen content, moderate conductivity | Balance between processability and performance | Potential structural defects |
| Graphene-Polymer Composites | Combined properties of components | Tunable mechanical/electrical properties | Interface compatibility challenges |
Advanced Composite Materials and Hybrid Approaches
The integration of conducting polymers with graphene-based materials has led to the development of advanced composites that synergistically combine the advantages of both material systems [44]. These hybrid approaches address limitations inherent in the individual components, such as the relatively poor mechanical stability of pure conducting polymers and the challenging processability of pristine graphene [44]. By creating composite architectures, researchers have achieved materials with enhanced electrical, mechanical, and biological properties superior to their individual constituents.
One notable example is the development of PEDOT/GO nanocomposites for neural interface applications [44]. In this system, graphene oxide serves as a dopant during the electrochemical polymerization of PEDOT, resulting in a composite film where GO sheets are uniformly distributed within the conducting polymer matrix [44]. This unique structure enhances both mechanical integrity and electrical performance—the GO component provides structural reinforcement and increases the effective surface area, while the PEDOT facilitates efficient charge transfer [44]. Studies have demonstrated that electrodes modified with PEDOT/GO exhibit nearly two orders of magnitude decrease in impedance at 1 kHz compared to bare gold electrodes, along with significantly increased charge storage capacity [44].
Additional composite strategies include the incorporation of carbon nanotubes into conducting polymers to enhance chronic neural stimulation capabilities [44], and the functionalization of graphene with antimicrobial peptides [46], silver nanoparticles [46], and biodegradable polymers [46] to create multifunctional biointerfaces. These advanced composites can be engineered to provide controlled drug delivery, reduce inflammatory responses, and promote specific cellular interactions while maintaining optimal electrical performance for bioelectronic applications.
Experimental Protocols for Material Synthesis and Characterization
Electrochemical Deposition of Conducting Polymer-Graphene Composites
The synthesis of conducting polymer-graphene composites via electrochemical deposition represents a widely employed methodology for creating uniform, adherent coatings on electrode surfaces [44]. The following protocol details the process for depositing PEDOT/GO films:
Electrolyte Preparation: Prepare an aqueous solution containing 2 mg/ml graphene oxide (GO) and 0.01 M EDOT monomer. Stir the mixture for 2 hours to ensure complete dissolution and dispersion. Purge the solution with nitrogen gas for 10 minutes to eliminate dissolved oxygen, which can interfere with the polymerization process [44].
Substrate Preparation: Clean electrode substrates (typically gold-sputtered glass slides or gold wire electrodes) using standard protocols. For gold surfaces, perform oxygen plasma treatment or piranha solution cleaning to ensure a clean, hydrophilic surface for improved film adhesion [44].
Electrochemical Deposition: Employ a three-electrode system with the target substrate as the working electrode, a platinum plate as the counter electrode, and a Ag/AgCl reference electrode. Apply constant current density of 0.2 mA/cm² for 600 seconds using a potentiostat/galvanostat system. Maintain the electrolyte at room temperature with continuous gentle stirring during deposition [44].
Post-processing: After deposition, carefully rinse the modified electrodes with deionized water to remove unreacted monomers and loosely bound GO sheets. Dry the samples under a nitrogen stream and store in a desiccator until further characterization or use [44].
Material Characterization Techniques
Comprehensive characterization of the synthesized materials is essential for evaluating their suitability for bioelectronic applications. Key characterization methods include:
Structural and Morphological Analysis:
- Scanning Electron Microscopy (SEM): Image the surface morphology of deposited films using appropriate accelerating voltages (typically 5-15 kV). Sputter-coat non-conductive samples with a thin gold or platinum layer prior to imaging [44].
- Atomic Force Microscopy (AFM): Perform tapping mode AFM to characterize surface topography and roughness using silicon cantilevers with resonant frequencies of approximately 300 kHz [44].
- Transmission Electron Microscopy (TEM): Analyze the internal structure and distribution of GO sheets within the polymer matrix at accelerating voltages of 80-200 kV [44].
Electrochemical Characterization:
- Electrochemical Impedance Spectroscopy (EIS): Measure impedance spectra over a frequency range of 1 Hz to 100 kHz with an amplitude of 10 mV at open circuit potential [44].
- Cyclic Voltammetry (CV): Perform CV scans in phosphate-buffered saline (PBS) at scan rates of 50 mV/s between potential limits of -0.6 V to 0.8 V vs. Ag/AgCl to determine charge storage capacity [44].
- Charge Injection Limit Testing: Evaluate charge injection limits using biphasic current pulses (0.2 ms pulse width) to determine maximum safe stimulation parameters [44].
Diagram 1: Experimental workflow for developing and characterizing bioelectronic materials.
Quantitative Performance Comparison of Biointerface Materials
The performance of interface materials directly impacts the efficacy and safety of bioelectronic devices. Quantitative assessment of key parameters enables informed material selection for specific applications. The following table summarizes critical performance metrics for various electrode-tissue interface materials based on experimental data from the literature.
Table 3: Quantitative Performance Comparison of Electrode-Tissue Interface Materials
| Material | Impedance at 1 kHz (kΩ) | Charge Storage Capacity (mC/cm²) | Stability (Cycles) | Cell Viability (%) |
|---|---|---|---|---|
| Bare Gold | 100-150 | 0.5-1.5 | N/A | 85-95 |
| PEDOT/PSS | 2-5 | 35-50 | 100-500 | 80-90 |
| PEDOT/GO | 1-3 | 50-100 | 1000-5000 | 85-95 |
| Iridium Oxide | 5-15 | 20-40 | 500-2000 | 75-85 |
The data demonstrate significant advantages for composite materials, particularly PEDOT/GO, which exhibits substantially reduced impedance and enhanced charge storage capacity compared to traditional interface materials [44]. This improved performance enables higher signal-to-noise ratios for neural recording and more efficient charge delivery for stimulation applications. Furthermore, the incorporation of GO nanosheets enhances the mechanical stability of the conducting polymer matrix, addressing a critical limitation of pure conducting polymer films that typically suffer from delamination and degradation under prolonged electrical stimulation [44].
Biocompatibility assessment represents another crucial evaluation parameter. Standard protocols involve culturing relevant cell lines (such as PC-12 neuronal cells or NIH/3T3 fibroblasts) on material surfaces and evaluating cell viability using MTT or Live/Dead assays [44]. Materials showing cell viability greater than 80% are generally considered biocompatible for implantable applications. The PEDOT/GO composite demonstrated excellent biocompatibility with cell viability exceeding 85%, making it suitable for long-term implantation [44].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of advanced bioelectronic interfaces requires access to specialized reagents and materials. The following toolkit summarizes essential components for research in conducting polymer and graphene-based biointerfaces.
Table 4: Essential Research Reagents and Materials for Biointerface Development
| Category | Specific Items | Function/Purpose | Example Suppliers/References |
|---|---|---|---|
| Conductive Monomers | EDOT, Pyrrole, Aniline | Building blocks for conducting polymer synthesis | Sigma-Aldrich [44] |
| Graphene Materials | Graphene Oxide, Reduced GO | Conductive filler, mechanical reinforcement | XFNano [44] |
| Electrochemical Supplies | Potentiostat/Galvanostat, Electrodes | Material synthesis and characterization | BioLogic, Metrohm |
| Characterization Tools | SEM, AFM, EIS, CV | Material property assessment | Multiple vendors [44] |
| Cell Culture | PC-12, NIH/3T3 cells | Biocompatibility assessment | ATCC [44] |
| Specialized Equipment | Plasma cleaner, Glove box | Sample preparation, controlled environments | Multiple vendors |
Signaling Pathways in Bioelectronic Medicine and Material Interfaces
Bioelectronic medicine functions through the modulation of specific neural signaling pathways that regulate physiological processes. Understanding these pathways is essential for designing effective interface materials that can precisely control neural circuits.
The cholinergic anti-inflammatory pathway represents one of the most well-characterized mechanisms in bioelectronic medicine [43]. This pathway involves efferent vagus nerve signals that suppress pro-inflammatory cytokine production through the release of acetylcholine in peripheral organs such as the spleen [43]. Electrical stimulation of the vagus nerve activates this pathway, leading to reduced levels of tumor necrosis factor (TNF) and other inflammatory mediators, providing a therapeutic approach for autoimmune conditions like rheumatoid arthritis and inflammatory bowel disease [43].
Advanced bioelectronic interfaces facilitate closed-loop systems that monitor physiological signals and automatically adjust stimulation parameters in real time [10]. These systems integrate sensing capabilities with therapeutic stimulation, creating adaptive treatments that respond to the patient's changing physiological state. Material innovations play a crucial role in these systems by enabling high-fidelity signal recording, efficient stimulation delivery, and minimal tissue damage during chronic implantation.
Diagram 2: Neural signaling pathway and bioelectronic interface mechanism in inflammation control.
The integration of conducting polymers and graphene-based materials has significantly advanced the field of bioelectronic medicine by enabling more efficient, stable, and biocompatible interfaces with neural tissues. These material innovations address critical challenges in electrode-tissue interfacing, including impedance matching, charge delivery capacity, mechanical compatibility, and long-term stability. The development of composite approaches that synergistically combine the advantages of different material systems represents a particularly promising direction, offering enhanced performance compared to single-component materials.
Future advancements in bioelectronic interfaces will likely focus on several key areas. Closed-loop systems that integrate sensing and stimulation capabilities will enable adaptive therapies that respond to real-time physiological changes [10]. The incorporation of artificial intelligence and machine learning algorithms will further enhance the precision and personalization of bioelectronic treatments [43]. Additionally, biodegradable electronic materials that safely resorb after fulfilling their therapeutic function represent an emerging frontier that could eliminate the need for device extraction surgeries [45]. As these technologies mature, bioelectronic medicine is poised to become an increasingly important therapeutic modality, offering targeted, reversible, and personalized treatments for a wide range of neurological, inflammatory, and metabolic disorders [43].
Overcoming Technical Hurdles: Stability and Reliability Challenges
Bioelectronic medicine represents a transformative approach to treating disease by using advanced devices to modulate neural circuits that control organ function and inflammation [3]. This field brings together material science, neuroscience, immunology, and bioengineering to develop implantable devices that can record, stimulate, or block neural signaling for therapeutic purposes [3]. The global bioelectronic medicine market, valued at USD 23.54 billion in 2024 and projected to reach USD 33.59 billion by 2030, reflects the significant growth and potential of this innovative field [47].
A fundamental challenge confronting all implantable medical devices (IMDs), including those for bioelectronic medicine, is the foreign body reaction (FBR)—an inevitable host response to implanted materials [48] [49]. Following implantation, local tissue damage triggers a cascade of inflammatory and fibrotic processes that can severely impair device performance and longevity [48]. For bioelectronic devices that rely on precise, stable interfaces with nerve tissue, FBR poses a particularly significant obstacle. The formation of a dense, avascular fibrous capsule can functionally isolate implants, disrupting crucial electrical signaling and leading to device failure [49] [50]. This review provides an in-depth examination of FBR mechanisms and outlines advanced strategies to enhance biocompatibility, with specific relevance to bioelectronic medicine applications.
Molecular and Cellular Mechanisms of FBR
The foreign body reaction is a dynamic, multifaceted process involving coordinated molecular signaling pathways, cellular mechanosensing mechanisms, and intercellular communication [48]. Understanding this complex timeline is essential for developing effective mitigation strategies.
The FBR Timeline
The cellular events following implantation progress through distinct but overlapping phases:
Protein Adsorption (Seconds to Minutes): Immediately upon implantation, blood plasma proteins (primarily albumin, fibrinogen, and fibronectin) nonspecifically adsorb to the material surface, creating a provisional matrix [49] [50]. Through the Vroman effect, smaller proteins are progressively replaced by larger ones over time, with the specific protein composition varying by material properties [50].
Neutrophil Recruitment (Minutes to Days): As first responders, neutrophils migrate to the implantation site, adhere to the protein layer, and release reactive oxygen species (ROS) and proteolytic enzymes [49] [50]. This initial wave of neutrophils typically disappears within two days, giving way to macrophages [50].
Monocyte Recruitment and Macrophage Differentiation (Days to Weeks): Chemical signals from neutrophils, clotting factors, and mast cells attract monocytes that differentiate into macrophages, which proliferate and populate the lesion [50]. These macrophages release pro-inflammatory cytokines including TNF-α, IL-1β, IL-6, and IL-8, sustaining the inflammatory response [50].
Frustrated Phagocytosis and FBGC Formation (Weeks): When macrophages cannot phagocytose large implants, they undergo "frustrated phagocytosis," secreting degrading enzymes and ROS in an attempt to break down the material [50]. Persistent implants promote macrophage fusion into foreign body giant cells (FBGCs) [49].
Fibrotic Encapsulation (Weeks to Months): Activated macrophages and FBGCs induce fibroblast activation and differentiation into myofibroblasts, characterized by α-smooth muscle actin (α-SMA) expression [49]. These cells secrete dense collagen fibers that form an avascular, capsule-like fibrous tissue that isolates the device from surrounding tissue [49] [50].
Key Cellular Players and Signaling Pathways
Macrophages are central regulators of FBR, exhibiting remarkable plasticity with different polarization states driving inflammatory responses:
M1 Macrophages: Predominant in early stages, these pro-inflammatory cells secrete IL-1, TNF-α, and other cytokines that amplify inflammation and recruit additional immune cells [49]. They attempt to eliminate implants through phagocytosis, releasing ROS and matrix metalloproteinases [49].
M2 Macrophages: As inflammation resolves, polarization shifts toward anti-inflammatory M2 phenotypes that upregulate tissue remodeling pathways [49]. In persistent FBR, this transition is delayed, maintaining chronic inflammation [49].
Foreign Body Giant Cells (FBGCs): Formed through macrophage fusion on material surfaces, these multinucleated cells are characteristic of chronic FBR and contribute to ongoing inflammatory signaling and material degradation attempts [49].
Fibroblasts and Myofibroblasts: Activated by macrophage-derived cytokines (including IL-4 and IL-13), fibroblasts differentiate into contractile myofibroblasts that express α-SMA and deposit dense collagen matrices, forming the fibrotic capsule [49].
The diagram below illustrates the key signaling pathways and cellular interactions in FBR:
Impact of FBR on Bioelectronic Medical Devices
The consequences of FBR are particularly detrimental for bioelectronic medical devices, which require stable, intimate interfaces with target tissues for proper function. Excessive fibrosis can compromise device performance through multiple mechanisms:
Table 1: FBR-Related Issues in Specific Bioelectronic Device Categories
| Device Category | FBR-Related Issues | Clinical Consequences | References |
|---|---|---|---|
| Neural Implants | Microelectrode recording failures, insertion trauma, giant cell formation around electrodes | Loss of signal fidelity, reduced stimulation efficacy | [49] [51] [50] |
| Cardiovascular Implants | Granulomatous reactions, fibrosis-related replacement complications, thrombosis | Device malfunction, need for replacement surgery | [49] |
| Cochlear Implants | Fibrous encapsulation, inflammation | Reduced hearing restoration efficacy | [49] |
| Vagus Nerve Stimulators | Fibrotic encapsulation of nerve electrodes | Diminished therapeutic response for epilepsy, depression, rheumatoid arthritis | [49] [3] |
For neural interfaces specifically, FBR presents several critical challenges. The fibrous capsule that forms around electrodes electrically isolates them from target neural tissue, increasing impedance and reducing signal-to-noise ratio for recording applications [50]. For stimulation devices, higher thresholds are required to activate neurons through the fibrotic layer, reducing battery life and stimulation specificity [51]. The inflammatory environment can also damage both the device materials and the surrounding tissue, potentially causing neuronal loss and further compromising device function [51] [50].
Strategies to Mitigate Foreign Body Reaction
Material Selection and Surface Modification
Strategic material selection and surface engineering represent frontline approaches for minimizing FBR. The core principle involves designing biomaterials that modulate rather than provoke immune responses.
Table 2: Polymer Biocompatibility Assessment for Neural Interfaces
| Polymer Material | Neural Cell Compatibility | Fibroblast Compatibility | Foreign Body Reaction | Suitability for Long-term Implants |
|---|---|---|---|---|
| Polyimide (PI) | High | High | Mild | Excellent |
| Polylactide (PLA) | Moderate-High | Moderate-High | Moderate | Good |
| Polydimethylsiloxane (PDMS) | Moderate | Moderate | Moderate | Good |
| Thermoplastic Polyurethane (TPU) | Moderate | Moderate | Moderate | Good |
| Polyethylene glycol diacrylate (PEGDA) | Low | Low | Severe (fibrosis, multinucleated cells) | Poor |
Recent comparative studies evaluating ten polymer materials for neural interface applications demonstrated significant differences in FBR responses. Polyimide showed the highest compatibility for both neural cells and fibroblasts, while PEGDA exhibited cytotoxic effects, low cell adhesion, and provoked severe FBR including extensive fibrosis and multinucleated cell formation [51].
Beyond bulk material properties, surface characteristics significantly influence FBR progression through several mechanisms:
Surface Topography: Micro- and nano-scale surface patterns can dramatically influence cell behavior and FBR progression. For example, electrospun polytetrafluorourethane (PTFE) with a surface roughness of 1.08 μm significantly reduced macrophage attachment and FBGC formation compared to smoother PTFE configurations [49]. Porous poly(2-hydroxyethyl methacrylate) (pHEMA) hydrogel scaffolds with 34 μm porosity elicited less dense capsule formation and increased vascularization compared to non-porous or larger-pore variants [49].
Surface Chemistry and Wettability: Material surface chemistry determines protein interaction levels and subsequent biological responses. Surface modifications that reduce protein adsorption or promote adsorption of specific proteins that minimize macrophage activation can dampen FBR initiation [49].
Mechanical Properties: Stiffness mismatches between implants and surrounding tissue create mechanical cues that influence immune cell behavior. The modulus of brain tissue is approximately 1 kPa, while many conventional electrode materials have Young's moduli of 100-200 GPa [51]. This significant mismatch contributes to chronic inflammation and FBR. Softer, more compliant materials that better match tissue mechanics reduce inflammatory responses [49] [51].
Advanced Anti-Fibrotic Strategies
Bioinspired and Biomimetic Approaches
Innovative biomimetic coating strategies represent a promising frontier in FBR mitigation. These approaches seek to create "immune-stealth" surfaces that evade host recognition:
Red Blood Cell (RBC) Coatings: A novel living RBC coating fabricated on PDMS substrates using hyaluronic acid (HA) as a bridging polymer demonstrated significant FBR reduction [52]. This bioinspired approach leveraged immune escape antigens (CD47 and CD59) naturally present on RBC membranes to actively communicate with macrophages and promote polarization toward anti-inflammatory M2 phenotypes [52]. The PDMS-HA-RBC constructs induced the least fibrosis formation compared to pristine PDMS or PDMS-HA alone, with the highest M2/M1 macrophage ratios [52].
Decellularized Matrices: Acellular dermal matrix (ADM) and acellularized bovine pericardium (ABP) have been used as biological scaffolds that provide a more natural substrate for tissue integration. These matrices replicate the structure and functional features of the native extracellular matrix, potentially facilitating more constructive tissue remodeling compared to synthetic materials [53].
Drug Delivery and Immunomodulation
Localized delivery of immunomodulatory agents represents another strategic approach to control FBR:
Anti-inflammatory Drug Elution: Controlled release of corticosteroids or NSAIDs from implant coatings can suppress the initial inflammatory response that initiates FBR [49].
Specific Pathway Inhibition: Targeting specific molecular pathways in the FBR cascade, such as integrin binding or cytokine signaling, may provide more precise control with fewer systemic side effects than broad anti-inflammatory approaches [50].
Experimental Models and Assessment Protocols
Standardized In Vivo Evaluation
Robust experimental models are essential for evaluating FBR and testing novel mitigation strategies. Well-established protocols following international standards provide reproducible frameworks for biocompatibility assessment:
ISO 10993-6 Compliance: The International Organization for Standardization defines standards for biological evaluation of medical devices, specifying implantation protocols and evaluation timelines [53]. For non-degradable materials, short-term responses are analyzed at 1-4 weeks, while long-term responses require evaluation at 12 weeks or more to distinguish surgical trauma from material-specific responses [53].
Dual-Plane Rat Model for Biomaterial Evaluation: A standardized surgical model in rats using a dual-plane technique has been developed for evaluating biomaterials in silicone implant coverage [53]. This model involves implanting miniature textured silicone prostheses (2 mL) in the submuscular region of Wistar rats, with test biomaterials superimposed on the prosthesis in the experimental group [53]. The protocol includes evaluation at multiple biological time points (1, 2, 4, 12, and 26 weeks) with detailed histological analysis using hematoxylin-eosin staining to observe inflammatory progression, tissue repair, and fibrous capsule formation [53].
In Vitro Screening Models
In vitro systems provide valuable preliminary screening platforms for evaluating material biocompatibility:
Cell Culture Toxicity Assessment: Direct culture of neural cells (e.g., PC-12) and fibroblasts (e.g., NRK-49F) on material surfaces allows evaluation of cell adhesion, growth, and potential cytotoxic compound release [51]. These assays can screen multiple materials simultaneously under controlled conditions before advancing to more complex in vivo studies.
Macrophage Polarization Assays: In vitro systems using macrophage cell lines enable specific investigation of material effects on immune cell polarization, measuring markers of M1 (pro-inflammatory) versus M2 (anti-inflammatory) phenotypes in response to material surfaces [49] [52].
The following diagram illustrates a comprehensive experimental workflow for evaluating biomaterial biocompatibility:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for FBR and Biocompatibility Studies
| Reagent/Material | Function/Application | Examples/Specifications | References |
|---|---|---|---|
| Acellular Bovine Pericardium (ABP) | Biological scaffold for tissue integration | Alternative to acellular dermal matrix (ADM) for implant coverage | [53] |
| Polymer Substrates for Neural Interfaces | Material biocompatibility screening | Polyimide, PLA, PDMS, TPU, PEGDA for toxicity and FBR assessment | [51] |
| Hyaluronic Acid (HA) | Bridging polymer for bioinspired coatings | Facilitates attachment of red blood cell coatings to PDMS substrates | [52] |
| Red Blood Cells (RBCs) | Immune-stealth coating material | Source of CD47 and CD59 immune escape antigens for macrophage modulation | [52] |
| Antibodies for Macrophage Phenotyping | M1/M2 macrophage polarization assessment | CD86 (M1 marker), CD206 (M2 marker) for immunohistochemistry | [52] |
| Histological Stains | Tissue response evaluation | Hematoxylin and eosin (H&E) for general morphology; specific stains for collagen | [53] |
The foreign body reaction remains a significant challenge for the advancing field of bioelectronic medicine, where stable, long-term interfaces with neural tissue are essential for therapeutic efficacy. A comprehensive understanding of the molecular signaling pathways, cellular interactions, and material properties that drive FBR provides the foundation for developing innovative solutions. Strategic material selection, surface engineering, biomimetic coatings, and localized immunomodulation represent promising approaches to mitigate adverse host responses. As bioelectronic medicine continues to evolve toward more sophisticated and miniaturized devices, overcoming the FBR barrier will be crucial for realizing the full potential of this revolutionary therapeutic paradigm. The integration of advanced materials science with immunology and neural engineering will enable the next generation of bioelectronic devices that maintain functional interfaces with the nervous system for chronic disease management.
Bioelectronic medicine is an emerging field that uses implantable and wearable electronic devices to interface with the body's electrically active tissues, such as nerves, the heart, and muscles, to treat a wide range of conditions [54] [1]. Unlike traditional pharmaceuticals, these devices offer precise, targeted therapies by modulating neural or muscular activity through electrical stimulation, potentially revolutionizing the management of chronic diseases like epilepsy, Parkinson's disease, chronic pain, and autoimmune disorders [54]. However, the long-term reliability and stability of these devices remain a critical challenge that must be addressed for their widespread clinical adoption [54].
A primary factor limiting device longevity is the permeation of water and ions through encapsulation barriers into the electronic components [55]. The human body presents a harsh, dynamic, and corrosive environment for implanted electronics. Body fluids contain various ions (H⁺, OH⁻, Cl⁻) that can lead to current leakage, corrosion of metallic components, performance degradation, and eventual device failure [56]. This challenge is particularly acute for next-generation soft and flexible bioelectronic devices, which require encapsulation that provides superior barrier performance while maintaining mechanical compliance with biological tissues [54] [56]. The development of robust encapsulation strategies that can withstand diverse physiological environments—from the highly acidic conditions of the gastrointestinal system (as low as pH 1.5) to the alkaline environment of chronic wounds (up to pH 8.9)—is therefore a fundamental research focus in advancing bioelectronic medicine [56].
Encapsulation Material Technologies and Performance
Encapsulation materials for bioelectronic implants must satisfy multiple demanding criteria: superior barrier properties against water and ion penetration, mechanical compatibility with soft biological tissues, and long-term stability in specific physiological environments [56]. Researchers are investigating various material systems, each with distinct advantages and limitations for different applications.
Traditional and Emerging Encapsulation Materials
Table 1: Comparison of Encapsulation Materials for Bioelectronic Implants
| Material Type | Examples | Key Advantages | Key Limitations | Typical Water Vapor Transmission Rate (WTR) |
|---|---|---|---|---|
| Inorganic Thin Films | Aluminum oxide (Al₂O₃), Silicon nitride (SiNₓ), Silicon carbide (SiC) [55] | Excellent intrinsic barrier properties, high density | Can develop micro-pinholes during fabrication; brittle, prone to cracking under strain [55] | Very low (when defect-free) |
| Traditional Polymers | Polyimide, Parylene C, Polydimethylsiloxane (PDMS) [56] [55] | Good flexibility, established processing methods | Moderate barrier properties, can fail rapidly in extreme pH [56] | ~10⁻¹ to 10⁰ g/m²/day |
| Liquid-Based Encapsulation | Oil-infused elastomers (e.g., Krytox oil in roughened PDMS) [56] | Excellent stretchability, transparency, durable barrier in broad pH range (1.5-9) [56] | Requires structured surface to lock liquid, potential long-term stability concerns at edges | Extremely low (maintained wireless function for ~2 years in vitro at pH 1.5) [56] |
| Bioresorbable Polymers | Poly(lactic-co-glycolic acid) (PLGA), Polycaprolactone (PCL) [57] | Dissolve in body, eliminate need for surgical extraction [57] | Limited operational lifetime defined by dissolution rate, challenging to achieve long-term stability | Varies with polymer composition and thickness |
Quantitative Performance of Encapsulation Strategies
Table 2: Performance Comparison of Encapsulation Strategies in Challenging Environments
| Encapsulation Strategy | Test Environment | Performance Outcome | Reference |
|---|---|---|---|
| Conventional Silicone Elastomer | Acidic environment (pH 1.5) | Complete device failure within 1.5-19 days [56] | [56] |
| Parylene C Coating | Acidic environment (pH 1.5) | Lost >20% of original performance within 1.5-19 days [56] | [56] |
| Epoxy Resin | Gastrointestinal tract (acidic) | Widely used but high modulus (GPa), thick geometry limits soft bioelectronics use [56] | [56] |
| Oil-Infused Elastomer | pH 1.5 and pH 4.5 (acidic) | Nearly 2 years of durability in soaking tests with NFC antennas [56] | [56] |
| Oil-Infused Elastomer | pH 7.4 (physiological) | Year-long performance observed with wireless optoelectronics [56] | [56] |
| Oil-Infused Elastomer | pH 9.0 (alkaline) | Robust encapsulation demonstrated [56] | [56] |
| Oil-Infused Elastomer | In vivo (freely moving mice) | Maintained robust wireless operation for 3 months [56] | [56] |
Experimental Protocols for Evaluating Encapsulation Reliability
Protocol 1: In Vitro Soaking Test for Barrier Durability
This protocol assesses the long-term stability of encapsulation barriers under controlled laboratory conditions that simulate physiological or extreme environments [56].
Materials and Reagents:
- Phosphate Buffered Saline (PBS): Standard solution for simulating physiological ionic environment.
- Buffer Solutions at Target pH: pH 1.5 and 4.5 (acidic), pH 7.4 (physiological), pH 9.0 (alkaline) to represent different body compartments [56].
- Test Samples: Encapsulated devices, ideally functional subsystems like Near-Field Communication (NFC) antennas or simple electrode structures [56].
- Control Samples: Devices encapsulated with standard materials (e.g., Parylene C, plain silicone elastomer) for benchmarking [56].
- Environmental Chamber: For maintaining constant temperature (e.g., 37°C) to simulate body conditions.
Procedure:
- Baseline Characterization: Measure the key functional parameters of all devices before immersion (e.g., impedance for electrodes, quality factor and resonance frequency for antennas).
- Immersion: Submerge test and control samples in the respective buffer solutions, ensuring complete coverage.
- Accelerated Aging: Maintain samples at an elevated temperature (e.g., 37°C or higher for accelerated testing) with continuous or periodic agitation.
- Periodic Monitoring: At predetermined intervals (e.g., daily, weekly), remove samples, rinse with deionized water, dry carefully, and re-measure the functional parameters.
- Failure Criterion: Define a failure threshold (e.g., 20% performance degradation or complete functional loss) and record the time until this threshold is reached for each sample [56].
- Data Analysis: Plot performance metrics versus time and compare the stability across different encapsulation schemes and environmental conditions.
Protocol 2: Real-Time Wireless Monitoring of Water Permeation
This advanced protocol uses a wireless, battery-free platform to monitor water permeation directly and in real-time, both in vitro and in vivo [55].
Materials and Reagents:
- Magnesium (Mg) Sensing Elements: ~200 nm thick Mg films patterned into specific designs (stripes, serpentines) and encapsulated with the test barrier [55].
- Flexible Polyimide Substrate: Serves as the base for the sensor platform.
- Titanium Adhesion Layer: A thin layer (~20 nm) between Mg and polyimide.
- Wireless Interrogator/Reader: Generates the RF carrier wave and receives the backscattered signal.
- RF Spectrum Analyzer: For analyzing the frequency shift of the backscattered signal.
Procedure:
- Sensor Fabrication: Fabricate the Mg sensors via sequential thin-film deposition (DC reactive sputtering or thermal evaporation) and UV photolithography patterning on a flexible polyimide substrate [55].
- Platform Assembly: Integrate the Mg sensor with a tunable oscillator circuit and a flexible dipole antenna to create the complete wireless platform.
- Calibration: Establish the relationship between the oscillator's output frequency and the resistance of the Mg sensor before exposure to moisture.
- Permeation Monitoring:
- In Vitro: Immerse the platform in PBS or other solutions at 37°C.
- In Vivo: Implant the platform subdermally or intramuscularly in an animal model (e.g., mice) [55].
- Data Collection: The interrogator powers the platform wirelessly. As water permeates the barrier and corrodes the Mg sensor (Mg + 2H₂O → Mg(OH)₂ + H₂), its resistance increases, causing a measurable frequency shift in the backscattered signal [55].
- WTR Calculation: Use an analytical model to convert the frequency shift data into a quantitative Water Transmission Rate (WTR) value, providing a direct measure of the encapsulation's barrier performance over time [55].
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials for Encapsulation and Reliability Research
| Category | Specific Material/Reagent | Function in Research | Key Characteristics |
|---|---|---|---|
| Substrate Materials | Polyimide (PI) [55] | Flexible substrate for devices and sensors | Young's modulus ~2.5 GPa, good electrical insulation |
| Encapsulation Materials | Polydimethylsiloxane (PDMS) [56] | Elastic, transparent encapsulation matrix | Young's modulus ~MPa range, stretchable, moderate barrier |
| Parylene C [56] [55] | Conformal thin-film coating | Good dielectric, transparent, but limited in extreme pH [56] | |
| Bioresorbable Polymers (e.g., PLGA) [57] | Temporary encapsulation for transient electronics | Dissolves in body over time, preventing need for removal [57] | |
| Liquid Barrier Agents | Krytox Oil (PFPE) [56] | Infused into elastomers for liquid-based encapsulation | Ultralow water diffusion coefficient, creates slippery surface |
| Sensor Materials | Magnesium (Mg) thin films [55] | Corroding sensing element for water detection | Resistivity ~4.6×10⁻⁸ Ω·m, reacts predictably with water |
| Adhesion Layers | Titanium (Ti) [55] | Improves adhesion between layers (e.g., Mg to PI) | ~20 nm thickness, promotes film stability |
| Test Solutions | PBS Buffer, pH-adjusted buffers [56] | Simulate physiological and extreme body environments | pH 1.5 (gastric), 7.4 (physiological), 9.0 (chronic wounds) [56] |
The journey toward achieving ultra-stable, long-lasting bioelectronic implants is intrinsically linked to solving the fundamental challenge of encapsulation and water permeation. While traditional materials often fall short, particularly in extreme pH environments or under mechanical strain, emerging technologies like liquid-based encapsulation and bioresorbable polymers offer promising pathways forward [56] [57]. The development of sophisticated, wireless monitoring techniques further provides researchers with the tools needed to quantitatively assess barrier performance in real-time and under realistic conditions [55].
Future progress will likely hinge on the development of multifunctional, smart encapsulation systems that not only provide a passive barrier but also actively respond to the local biological environment. The integration of these advanced encapsulation strategies with the ongoing trend toward soft, flexible, and miniaturized bioelectronic devices is essential. As these material and engineering challenges are met, the potential of bioelectronic medicine to provide targeted, personalized, and durable therapies for a wide spectrum of diseases will move closer to widespread clinical reality [54] [1].
Bioelectronic medicine represents a transformative frontier in therapeutic science, focusing on modulating neural circuits to treat a wide range of diseases, from rheumatoid arthritis to Parkinson's disease [3]. At the heart of this field lie neural interfaces—the crucial bidirectional communication bridges between external electronic devices and the nervous system. These interfaces enable both the recording of complex neuronal activity and the repair of damaged neural tissues [58]. However, a fundamental challenge impedes their progress: the significant mechanical mismatch between conventional rigid electronic materials and soft, delicate neural tissues.
This mechanical disparity creates a profound compatibility issue. While neural tissue exhibits a soft consistency with a Young's modulus ranging from 1 to 10 kPa, traditional electrode materials like silicon (~180 GPa) and platinum (~102 MPa) are orders of magnitude stiffer [59] [58]. This mismatch prevents seamless integration, causing mechanical trauma during insertion, exacerbating chronic inflammation through tissue micromotion, and triggering a persistent foreign body response (FBR) [59] [60]. The resulting glial scar formation encapsulates the device, increases impedance, degrades signal quality, and ultimately diminishes the functional lifespan of the implant [58]. Overcoming this mechanical mismatch is therefore not merely an engineering concern but a prerequisite for reliable, long-term bioelectronic therapies. This whitepaper details the material, structural, and bioactive strategies developed to bridge this mechanical divide and enable the next generation of soft, stretchable neural interfaces.
Material-Based Strategies: Engineering Tissue-Like Properties
The most direct approach to mitigating mechanical mismatch involves developing new conductive materials whose intrinsic mechanical properties closely resemble those of neural tissue.
Conductive Polymers and Composites
Conductive polymers offer a unique combination of electrical functionality and mechanical compliance. Poly(3,4-ethylene-dioxythiophene) polystyrene sulfonate (PEDOT:PSS) has been extensively utilized both as a coating and as a free-standing film to reduce impedance and enhance signal transduction [59]. For instance, the NeuroGrid, an ultrathin (4 μm) array with free-standing PEDOT:PSS electrodes, can detect single-cell action potentials from the cortical surface [59]. These polymers can be integrated into soft matrices like Polydimethylsiloxane (PDMS) to create composites that are both conductive and tissue-like [59] [60].
Advanced Conductive Composites for Fiber Electrodes
Fiber-based electrodes represent a promising geometry, and their performance is critically dependent on the conductive composites used in their fabrication. The table below summarizes key material classes and their properties.
Table 1: Properties of Conductive Composites for Soft Neural Interfaces
| Material Class | Example Materials | Electrical Conductivity (S cm⁻¹) | Elastic Modulus | Key Characteristics |
|---|---|---|---|---|
| Carbon-Based Materials | Carbon Nanotubes (CNT), Graphene | 2.8×10³ - 5.84×10⁴ (CNT) | 1.12×10⁵ - 7.2×10⁷ kPa (CNT) | High conductivity, excellent mechanical strength [60] |
| Conductive Polymers | PEDOT:PSS | 2 - 231 | N/A | High flexibility, low impedance, biocompatible [60] |
| Liquid Metals (LMs) | Eutectic Gallium-Indium (EGaIn) | 3.4×10⁴ | N/A | Fluidic, stretchable, self-healing properties [60] |
| Soft Polymer Substrates | PDMS, Polyimide, SU-8 | Insulating | ~1,000 - 2,000 kPa (PDMS) | Biocompatible, flexible, used as substrate/encapsulation [59] |
Design and Structural Engineering Strategies
Beyond intrinsic material properties, ingenious geometrical designs can confer softness and stretchability to otherwise rigid materials.
Ultra-Thin and Miniaturized Designs
A primary strategy involves reducing the device footprint and thickness to minimize flexural rigidity. Ultra-thin films (<10 μm) of metals or semiconductors patterned on polymeric substrates can achieve bending stiffnesses comparable to a biological axon (as low as ~1.4×10⁻¹⁶ N·m²) [59]. This approach allows the device to seamlessly conform to the irregular, dynamic surfaces of the brain or nerves with minimal force.
Fractal and Serpentine Geometries
To make non-stretchable materials stretchable, conductive traces are patterned in serpentine, mesh, or fractal layouts [59]. These designs allow the entire structure to absorb significant strain through the out-of-plane buckling or in-plane uncoiling of the meandering traces, while the functional electronic materials themselves experience minimal deformation. This principle is fundamental to many state-of-the-art flexible bioelectronic devices.
Diagram: Structural Strategies for Soft Neural Interfaces
Bioactive and "Living" Interface Strategies
The most advanced strategies move beyond passive mimicry to create biologically active, integrative interfaces.
Bioactive Surface Functionalization
Surface chemistry can be engineered to promote specific biological responses. This involves coating devices with biomolecules such as peptides, enzymes, or extracellular matrix (ECM) components like laminin [59]. These coatings can mask the device as "self," dampen the immune response, and actively promote neuronal attachment and integration by providing favorable biochemical cues from the native tissue microenvironment [59].
Biohybrid and "All-Living" Interfaces
A paradigm shift involves incorporating living cells into the interface. 'Biohybrid' neural interfaces feature a layer of living cells (e.g., neurons, stem cells) at the brain-device interface [59]. This cell layer acts as an active, biological scaffold that promotes tissue regeneration and seamless integration. Pushing this concept further, 'all-living' approaches utilize engineered biological constructs composed solely of cells and biological components to achieve synaptic-mediated control of neural circuits, thereby eliminating synthetic materials entirely [59].
Experimental Protocols and Validation
Validating the performance and biocompatibility of soft neural interfaces requires a suite of standardized experimental protocols.
In Vitro Characterization Protocol
Objective: To quantitatively assess the electrical and mechanical properties of the fabricated interface.
- Electrical Impedance Spectroscopy: Measure impedance across a frequency range (e.g., 1 Hz - 1 MHz) in physiological saline (e.g., PBS or artificial cerebrospinal fluid) to determine charge transfer capability [60].
- Cyclic Stretch Testing: Mount the device on a stretchable substrate or tensile stage. Subject it to repeated strain cycles (e.g., 10-30%, 1000+ cycles) while monitoring electrical continuity and resistance to evaluate electromechanical stability [60].
- Young's Modulus Measurement: Use a micro-indenter or tensile tester to perform stress-strain analysis on the material, calculating the elastic modulus to confirm it falls within the kilopascal range [58].
In Vivo Biocompatibility and Functional Assessment
Objective: To evaluate the foreign body response and recording/stimulation performance in a living animal model.
- Surgical Implantation: Implant the neural interface into the target region (e.g., cortex, peripheral nerve) of an anesthetized rodent or larger animal using standard stereotaxic techniques [59] [58].
- Chronic Signal Recording: Over several weeks to months, record neural signals (single-unit spikes, local field potentials). Track metrics like signal-to-noise ratio (SNR), single-unit yield, and electrode impedance over time [58].
- Histological Analysis: At endpoint, perfuse and fix the brain. Section the tissue around the implant and stain for markers of the foreign body response:
- Astrocytes (GFAP stain) to visualize glial scarring.
- Microglia (Iba1 stain) to assess immune activation.
- Neurons (NeuN stain) to quantify neuronal density and proximity to the implant site [59] [58]. A successful, soft interface will show significantly reduced glial activation and higher neuronal survival near the implant compared to rigid controls.
Diagram: Experimental Workflow for Interface Validation
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Developing Soft Neural Interfaces
| Item | Function/Application | Examples / Key Properties |
|---|---|---|
| Conductive Polymers | Low-impedance electrode coating or free-standing film; reduces FBR. | PEDOT:PSS [59] [60] |
| Soft Elastomers | Flexible substrate and encapsulation; provides mechanical match to tissue. | PDMS, Ecoflex, Polyimide [59] [60] |
| Carbon Nanomaterials | Conductive filler in composites; provides high conductivity and strength. | Carbon Nanotubes (CNTs), Graphene [60] |
| Liquid Metals | Stretchable conductor for extreme deformability. | Eutectic Gallium-Indium (EGaIn) [60] |
| Bioactive Coatings | Surface functionalization to promote neuronal integration and reduce FBR. | Laminin, Poly-L-Lysine, Peptide motifs [59] |
| Histological Markers | Labeling specific cell types for post-mortem biocompatibility analysis. | Anti-GFAP (astrocytes), Anti-Iba1 (microglia), Anti-NeuN (neurons) [59] [58] |
The journey toward overcoming mechanical mismatch in neural interfaces is propelling the field of bioelectronic medicine into a new era. The convergence of tissue-like conductive materials, innovative structural designs, and biologically active strategies is transforming rigid, foreign probes into seamless, integrative neural companions. These advancements are not merely technical improvements; they are fundamental to realizing the long-term therapeutic potential of bioelectronic devices for chronic conditions like Parkinson's disease, epilepsy, and paralysis. As these soft, stretchable interfaces continue to evolve, they promise to unlock a deeper understanding of neural circuits and enable a new generation of robust, effective, and lifelong bioelectronic therapies.
Bioelectronic medicine represents a transformative approach to treating chronic diseases by using miniaturized electronic devices to interface with the body's electrically active tissues and organs [54]. This emerging field harnesses targeted electrical stimulation to modulate neural activity, offering precise therapeutic alternatives to traditional pharmaceuticals for conditions such as Parkinson's disease, epilepsy, chronic pain, and autoimmune disorders [54] [61]. Unlike conventional drugs that act systemically, bioelectronic devices provide highly specific intervention by targeting specific neural circuits, thereby avoiding widespread side effects [54].
The effectiveness of these advanced therapies is fundamentally constrained by a critical technological challenge: power management. As the field shifts toward increasingly miniaturized, implantable, and wearable devices [54] [61], the limitations of conventional battery technology become increasingly problematic. Power sources must balance multiple competing demands including longevity, reliability, size constraints, and patient safety. This whitepaper examines the current limitations of battery technology in bioelectronic medicine, explores emerging energy harvesting solutions, and presents hybrid approaches that promise to enable the next generation of electroceuticals.
Battery Technology: Limitations and Challenges
Despite their widespread use, batteries present significant constraints for advanced bioelectronic applications, particularly for implantable and wearable devices intended for long-term therapy.
Fundamental Limitations of Battery Power
- Limited Lifespan and Capacity: Batteries possess finite energy storage capacity, necessitating periodic replacements or recharging [62]. This limitation directly contradicts the vision of "set-it-and-forget-it" medical implants, particularly for chronic conditions requiring lifelong management.
- Environmental Impact: The disposal of depleted batteries contributes significantly to electronic waste, with toxic chemicals potentially leaching into landfills and waterways [62]. This environmental burden raises sustainability concerns as the number of deployed bioelectronic devices grows exponentially.
- Resource Constraints: The minerals required for battery manufacturing (such as lithium and cobalt) are often rare and may be dubiously sourced, creating supply chain vulnerabilities and ethical concerns [62].
- Recurring Costs and Maintenance: Batteries represent a significant recurring expense for healthcare systems. Facility operators deploying numerous wireless sensors face substantial labor costs and logistical challenges for battery replacement, even when required only once every few years [62].
- Size and Form Factor Limitations: The need for rigid battery compartments often conflicts with the trend toward soft, flexible bioelectronics that conform to body tissues [54]. This mechanical mismatch can lead to patient discomfort, inflammation, and fibrotic encapsulation around implanted devices.
Clinical Implications in Bioelectronic Applications
The limitations of batteries extend beyond technical specifications to impact direct patient care and treatment efficacy. Device replacements due to battery depletion necessitate surgical interventions for implantable systems, exposing patients to repeated procedural risks and healthcare costs [54]. Furthermore, the finite nature of battery life may lead clinicians to conservatively program stimulation parameters to extend device longevity, potentially delivering subtherapeutic treatment doses. The physical presence of batteries also complicates device miniaturization, particularly for advanced applications such as injectable bioelectronics [54] and neural dust motes requiring ultra-compact form factors.
Energy Harvesting: Alternative Power Solutions
Energy harvesting technologies offer promising alternatives by capturing ambient energy from the device environment and converting it into usable electricity, enabling extended operational lifetimes and reduced battery dependence [62].
Energy Harvesting Modalities
Table 1: Comparison of Energy Harvesting Modalities for Bioelectronic Medicine
| Modality | Energy Source | Power Output Range | Suitable Applications | Key Advantages | Key Challenges |
|---|---|---|---|---|---|
| Photovoltaic | Ambient light | 10µW - 100mW (depending on size and conditions) | Wearable devices, subcutaneous implants with light transmission | Relatively high power density, established technology | Limited functionality in implanted/dark environments, requires exposure to light |
| RF Energy Harvesting | Ambient radio frequencies (Wi-Fi, cellular) | µW - mW range | Intermediate power applications, hybrid systems | Continuous power availability in urban environments, works indoors | Distance-dependent, low efficiency, variable power availability |
| Piezoelectric | Body movement, muscle contraction, blood pressure | µW - mW range (highly activity-dependent) | Pacemakers, implantable sensors, wearable patches | Direct integration with physiological movements, self-contained | Inconsistent output, requires mechanical coupling, biomechanical energy varies |
| Thermoelectric | Body heat (temperature gradients) | 10-100µW/cm² | Deep tissue implants, continuous monitoring | Continuous power from body heat, works day and night | Very low power output, requires significant temperature gradient |
| Kinetic/Motion | Body movement, limb motion | µW - mW range (activity-dependent) | Wearable neurostimulators, activity trackers | High power during patient movement, intuitive source | No power at rest, requires frequent movement, bulky mechanisms |
Technical Considerations for Biomedical Implementation
Implementing energy harvesting in bioelectronic devices requires careful consideration of several technical factors. Power management circuits must efficiently convert often irregular, low-level harvested energy into stable, usable power, necessitating sophisticated power conditioning electronics. The biological environment presents unique challenges, including the need for biocompatible encapsulation materials that protect both the energy harvester and surrounding tissues [54]. Device designers must also address the variable nature of harvested energy, implementing energy storage buffers (such as supercapacitors or rechargeable batteries) and intelligent power management algorithms that dynamically adjust device operation based on available energy. For implantable systems, energy transmission efficiency through tissue layers must be optimized, considering factors such as attenuation and heat generation.
Hybrid Approaches: Integrating Batteries with Energy Harvesting
Hybrid power systems that combine energy harvesting with batteries represent a pragmatic transitional approach, balancing reliability with sustainability [62]. These systems leverage the strengths of both technologies while mitigating their individual limitations.
Hybrid System Architectures
Two predominant architectural philosophies have emerged for hybrid power systems in bioelectronic devices:
- Energy Harvesting as Primary Source with Battery Backup: In this configuration, the device operates primarily on harvested energy, with the battery serving as a backup during periods of low ambient energy availability. This approach maximizes battery lifespan while ensuring continuous device operation [62].
- Battery as Primary Source with Harvesting Extension: Alternatively, some implementations use the battery as the main power source while employing energy harvesting to supplement power needs, thereby extending battery life. This approach reduces battery replacement frequency while maintaining predictable device operation [62].
Implementation and Clinical Workflow
Table 2: Experimental Protocol for Hybrid Power System Validation
| Testing Phase | Methodology | Measurement Parameters | Success Criteria | Duration |
|---|---|---|---|---|
| Benchtop Verification | System operation in controlled environmental chamber with simulated physiological signals | Power conversion efficiency, maximum power point tracking performance, energy storage charging efficiency | >70% power conversion efficiency, stable operation under variable input conditions | 2-4 weeks |
| In Vivo Animal Model | Implantation in appropriate animal model (e.g., porcine for vagus nerve stimulation studies) | Device functionality consistency, tissue response at interface, thermal profile during operation | Maintenance of therapeutic stimulation parameters, absence of significant tissue inflammation or necrosis | 3-6 months |
| Clinical Workflow Integration | Use in simulated clinical environment with human factors testing | Physician programming interface usability, patient quality of life impact, clinical workflow compatibility | Successful parameter adjustment by clinicians, patient satisfaction with reduced maintenance burden | 1-2 months |
Diagram 1: Hybrid Power Management System Architecture for Bioelectronic Devices. This illustrates the integrated approach combining multiple ambient energy sources with intelligent power distribution and storage.
The Scientist's Toolkit: Research Reagent Solutions
Implementing advanced power management systems in bioelectronic medicine requires specialized materials and experimental components.
Table 3: Essential Research Materials for Bioelectronic Power Management Studies
| Research Reagent/Material | Function | Application Example | Key Considerations |
|---|---|---|---|
| Flexible Lithium Polymer Cells | Thin-form-factor rechargeable energy storage | Powering soft, conformable bioelectronic patches | Cycling stability, mechanical flexibility under repeated deformation, safety profile |
| Biocompatible Encapsulation Materials (e.g., Parylene-C, PDMS, medical-grade silicone) | Protection of electronic components from biological fluids, electrical insulation | Chronic implantation studies, ensuring device longevity | Water vapor transmission rate, long-term stability in physiological conditions, fibrosis response |
| Micro-Supercapacitors | Rapid charge/discharge cycles for pulse power delivery | Buffering high-current stimulation pulses in neural stimulators | Power density vs. energy density tradeoffs, lifetime cycle count, integration complexity |
| Polymer-based Piezoelectric Materials | Conversion of mechanical deformation to electrical energy | Self-powered cardiac pacemakers harnessing heart motion | Biocompatibility, mechanical robustness, charge generation efficiency under physiological strains |
| Stretchable Conductors (e.g., EGaIn, MXene composites) | Electrical interconnects that maintain conductivity under strain | Interfacing components in flexible hybrid power systems | Resistance stability during stretching, fatigue life, manufacturing reproducibility |
| Reference Electrodes (Ag/AgCl, Pt) | Electrochemical characterization in physiological solutions | Validating biofuel cell performance in simulated body fluid | Stability in chloride-containing environments, potential drift, miniaturization capability |
Future Directions and Research Opportunities
The convergence of multiple technological domains presents exciting opportunities for advancing power management in bioelectronic medicine. Artificial intelligence and machine learning algorithms are being increasingly deployed for predictive power management, forecasting energy availability based on historical patient activity patterns and optimizing device operation accordingly [61]. Materials science innovations continue to produce novel solutions such as biodegradable power sources that safely dissolve after their useful lifespan, eliminating explanation surgeries, and nanogenerators that harvest energy from subtle physiological motions previously considered insufficient for power generation [54].
The integration of biofuel cells that directly oxidize physiological metabolites (such as glucose) represents another promising direction, potentially creating truly autonomous implants powered by the body's own chemistry [54]. As these technologies mature, standardized testing protocols and regulatory frameworks will be essential to ensure their safe clinical translation. Research should prioritize not only technical performance metrics but also long-term biocompatibility and reliability in the dynamic physiological environment.
Diagram 2: Research and Development Workflow for Power Systems in Bioelectronic Medicine. This outlines a systematic approach from requirements definition through clinical translation, including essential feedback loops for design optimization.
Bioelectronic medicine (BEM) represents a transformative approach to treating disease through targeted modulation of neural circuits using implantable or wearable electronic devices rather than pharmaceutical agents [1] [43]. This emerging field leverages the body's inherent electrical signaling language to monitor and regulate physiological processes, including inflammation, mood, metabolism, and cardiovascular function [10] [43]. The unquestionable clinical impact of bioelectronic medicine is underscored by successful translations to humans over recent decades, including applications for rheumatoid arthritis, Parkinson's disease, drug-resistant epilepsy, and inflammatory bowel disease [63] [1] [9].
At the core of advanced bioelectronic systems, particularly closed-loop architectures, lies the critical challenge of maintaining signal integrity amidst substantial noise and drift contamination. Unlike open-loop systems that deliver predetermined stimulation, closed-loop systems continuously adapt therapeutic parameters based on real-time physiological feedback [10] [1]. This creates a sophisticated bioelectronic interface that functions much like an "artificial neuron" within the body's natural control systems. However, the effectiveness of these systems depends entirely on their ability to accurately distinguish legitimate biological signals from corrupting noise and drift artifacts [64] [65]. The presence of these signal contaminants can severely degrade system performance, leading to either inappropriate therapy delivery or failure to deliver needed intervention.
Noise in bioelectronic systems manifests as random, high-frequency fluctuations superimposed on the desired physiological signals, originating from both internal sources (thermal noise, shot noise, flicker noise) and external sources (electromagnetic interference, power supply ripple) [66] [65]. In contrast, signal drift represents slow, systematic deviations in baseline signal characteristics over time, often caused by environmental factors (temperature fluctuations, humidity), component aging, mechanical stress, or biological processes like tissue encapsulation of implants [64] [65]. These phenomena present particularly formidable challenges in bioelectronic medicine due to the low-amplitude nature of neural signals and the demanding precision required for therapeutic effectiveness.
The Critical Role of Signal Processing in Closed-Loop Systems
Fundamental Architecture of Closed-Loop Bioelectronic Systems
Closed-loop bioelectronic systems represent a significant advancement over traditional open-loop approaches by creating continuous feedback circuits that automatically adjust therapeutic parameters based on real-time physiological measurements [10] [1]. These sophisticated systems typically operate across three integrated layers: the implant layer (containing electrodes and electronics for neural interfacing), an optional wearable companion layer (for additional sensing or processing), and the user interface layer (enabling communication with physicians or cloud services) [1]. The fundamental innovation lies in the system's ability to capture biological signals, process them to extract clinically relevant features, and use this information to dynamically modulate stimulation parameters in a responsive, individualized manner [1].
This architectural complexity introduces several signal processing challenges. The implant layer must perform initial signal acquisition in an electrically hostile environment characterized by low signal-to-noise ratios, while the processing components must distinguish relevant physiological patterns from contaminating artifacts. Simultaneously, the system must maintain long-term stability despite changing biological conditions and component characteristics. The presence of noise can obscure critical physiological features that trigger necessary therapy adjustments, while signal drift can cause gradual deterioration of system performance that escapes immediate detection [64] [66]. In therapeutic applications such as responsive neurostimulation for epilepsy, these signal integrity issues can mean the difference between effectively preventing a seizure and either failing to respond or delivering unnecessary stimulation [1].
Clinical Consequences of Signal Integrity Failures
The impact of inadequate noise filtering and drift compensation extends beyond technical performance metrics to direct clinical outcomes. In vagus nerve stimulation (VNS) for inflammatory conditions such as rheumatoid arthritis or Crohn's disease, inaccurate sensing of inflammatory biomarkers could lead to inappropriate stimulation dosing, potentially exacerbating the underlying condition or causing unnecessary side effects [43] [9]. Similarly, in deep brain stimulation (DBS) for Parkinson's disease, signal contamination could disrupt the precise patterning required to suppress tremors without causing adverse effects [1].
The tables below summarize the primary sources and characteristics of noise and drift in bioelectronic systems, along with their potential clinical impacts:
Table 1: Characteristics and Sources of Noise in Bioelectronic Systems
| Noise Type | Frequency Characteristics | Primary Sources | Clinical Impact |
|---|---|---|---|
| Thermal Noise | Broadband, white spectrum | Random electron motion in resistive components | Reduced signal detection sensitivity |
| Shot Noise | Broadband | Discrete nature of charge carriers in semiconductors | Decreased accuracy in spike detection |
| Flicker Noise (1/f) | Low-frequency dominance | Semiconductor interfaces, impurities | Obscures low-frequency physiological rhythms |
| Environmental EMI | Narrowband or impulsive | Power lines, wireless devices, motors | False triggering of therapeutic responses |
| Quantization Noise | Frequency-dependent | Analog-to-digital conversion limitations | Reduced dynamic range for physiological sensing |
Table 2: Characteristics and Sources of Drift in Bioelectronic Systems
| Drift Type | Temporal Characteristics | Primary Sources | Clinical Impact |
|---|---|---|---|
| Temperature Drift | Slow, correlated with thermal changes | Temperature coefficients of electronic components | Gradual therapy efficacy loss |
| Aging Drift | Very slow, often monotonic | Material degradation over time | Long-term performance deterioration |
| Biological Drift | Variable, often exponential initially | Tissue encapsulation (fibrosis), immune response | Changing stimulation thresholds & sensing sensitivity |
| Mechanical Drift | Step changes or slow creep | Physical stress on packaging or leads | Sudden performance changes or failures |
Technical Approaches to Noise Filtering
Multi-Layered Filtering Architectures
Effective noise management in bioelectronic systems requires a multi-layered approach that addresses different noise types and frequency characteristics at various stages of the signal pathway. The most successful implementations employ complementary hardware filtering at the acquisition stage followed by sophisticated digital filtering during signal processing [66] [65]. This dual approach ensures that strong interference is eliminated before analog-to-digital conversion, while more nuanced filtering operations can be applied algorithmically to the digitized signal.
Hardware filtering typically begins with proper shielding and grounding techniques to minimize electromagnetic interference, followed by analog low-pass filters that remove high-frequency noise components beyond the physiological band of interest [65]. For particularly vulnerable low-amplitude neural signals, instrumentation amplifiers with high common-mode rejection ratios (CMRR) are essential for rejecting noise that is common to both recording contacts [65]. Additionally, power supply decoupling using bypass capacitors (e.g., 0.1 μF ceramic) and bulk capacitors (e.g., 10-100 μF electrolytic) helps suppress power-borne noise that could otherwise corrupt sensitive analog front-ends [65].
Digital filtering implementations vary significantly based on the specific application requirements and computational constraints. For systems with limited processing resources, moving average filters or median filters provide computationally efficient noise reduction, with median filters being particularly effective against impulse noise [65]. More advanced systems employ Kalman filters that incorporate models of both the physiological system and noise characteristics to optimally estimate the true underlying signal [64] [66]. The recursive nature of Kalman filters makes them especially suitable for real-time implementation in resource-constrained implantable devices.
Advanced Adaptive Filtering Methodologies
Recent research has focused on adaptive filtering approaches that automatically adjust their parameters based on changing signal and noise characteristics. In nuclear magnetic resonance (NMR) sensors used for inertial measurement, innovation-based adaptive Kalman filters (AKF) have demonstrated significant improvements in noise suppression under dynamic conditions [64]. These systems continuously monitor the "innovation" sequence—the difference between predicted and actual measurements—to dynamically adjust filter gain and noise parameters, maintaining optimal performance even as signal characteristics evolve [64].
For particularly challenging noise environments, hybrid approaches that combine multiple filtering strategies have shown promise. One innovative method published in 2021 employed Multi-objective particle swarm optimization-based Variational Mode Decomposition (MOVMD) combined with Time-Frequency Peak Filtering (TFPF) [66]. This technique first decomposes the noisy signal into intrinsic mode functions (IMFs), classifies these components based on their noise characteristics using sample entropy (SE), then applies targeted filtering strategies to each component before reconstruction [66]. This parallel processing approach demonstrated remarkable noise reduction, decreasing the angle random walk in MEMS gyroscope outputs from 0.531076°/h/√Hz to 5.22502×10⁻³°/h/√Hz—a 99% improvement [66].
Figure 1: Advanced Parallel Processing Pipeline for Noise and Drift Reduction
Advanced Methodologies for Drift Compensation
Modeling Approaches for Systematic Drift
Signal drift in bioelectronic systems presents a more complex challenge than noise due to its systematic, often non-stationary characteristics. Effective drift compensation begins with accurate characterization and modeling of the underlying drift processes. The most common approach involves time-series modeling using Auto Regressive (AR), Moving Average (MA), or combined Auto Regressive Moving Average (ARMA) methodologies [64]. These models effectively capture the temporal correlations in drift phenomena, allowing for predictive compensation.
In NMR sensors, ARMA modeling has proven particularly effective for representing the complex random drift processes that emerge from interactions between optical, thermal, and magnetic field instabilities [64]. The AR component of these models captures longer-term trends and correlations in the historical data, while the MA component effectively handles transient, abrupt changes or high-noise periods [64]. When combined with Kalman filtering, these drift models serve as the state transition model, enabling real-time estimation and subtraction of drift components from the measured signals.
For temperature-induced drift—one of the most pervasive challenges in bioelectronic systems—compensation models typically establish a mathematical relationship between measured temperature and the resulting drift characteristics. These range from simple polynomial regression models that capture the nonlinear relationship between temperature and output deviation, to more sophisticated neural network approaches that can model complex, multi-factor interactions [66]. Implementation can occur through look-up tables (LUTs) stored in device memory or real-time computation of compensation parameters, with the choice dependent on processing capabilities and power constraints.
Machine Learning-Enhanced Compensation Strategies
Recent advances in drift compensation have increasingly leveraged machine learning techniques that automatically learn and adapt to individual device characteristics and usage patterns. The Beetle Antennae Search Algorithm-Elman Neural Network (BAS-Elman NN) represents one such innovative approach that has demonstrated remarkable effectiveness in compensating for temperature drift in MEMS gyroscopes [66]. This method combines the global search capabilities of the BAS optimization algorithm with the dynamic recursive properties of Elman neural networks, creating a compensation system that maintains temporal context while avoiding local minima that plague traditional backpropagation approaches [66].
Another promising development is the integration of signal stability detection (SSD) with adaptive filtering methodologies [64]. This approach recognizes that drift characteristics often vary significantly between different operational states, such as static versus dynamic conditions. By implementing real-time state detection algorithms that monitor signal variance, frequency content, and other stability metrics, these systems can apply specialized compensation strategies optimized for each operational mode [64]. In experimental implementations with NMR sensors, the SSD-AKF (Signal Stability Detection-Adaptive Kalman Filter) method demonstrated superior performance compared to conventional AKF approaches, particularly under low-dynamic conditions where traditional innovation-based adaptation struggles to distinguish drift from legitimate low-frequency signals [64].
Table 3: Performance Comparison of Drift Compensation Algorithms in Experimental Studies
| Compensation Method | Experimental System | Performance Improvement | Implementation Complexity |
|---|---|---|---|
| ARMA-Kalman Filter | NMR Sensors | Significant reduction in angular velocity error | Medium |
| BAS-Elman Neural Network | MEMS Gyroscope | Bias stability: 32.7364°/h to 0.140403°/h | High |
| MOVMD-TFPF Parallel Processing | MEMS Gyroscope | Angle random walk: 0.531076° to 5.22502×10⁻³°/h/√Hz | High |
| SSD-AKF | NMR Sensors | Improved accuracy under low dynamic conditions | Medium |
| Polynomial Temperature Compensation | General Analog Sensors | ~60-80% drift reduction | Low |
| Multi-point Calibration + LUT | General Analog Sensors | ~70-90% drift reduction | Low-Medium |
Experimental Protocols and Implementation Frameworks
Protocol: ARMA Modeling and Adaptive Kalman Filtering for Drift Suppression
Purpose: To implement and validate an ARMA-based drift model combined with an Adaptive Kalman Filter for real-time drift suppression in bioelectronic sensing systems.
Materials and Equipment:
- Bioelectronic signal acquisition system (neural recorder, biosensor interface)
- Environmental chamber for controlled temperature testing
- Reference sensors for ground truth measurement
- Computing platform for real-time signal processing (FPGA or DSP)
- Calibration equipment for system characterization
Procedure:
System Characterization and Data Collection:
- Collect continuous output from the bioelectronic sensor under stable conditions for a minimum of 2 hours to capture inherent drift characteristics.
- Record simultaneous temperature measurements using a precision thermistor placed adjacent to the sensing element.
- Repeat under varying temperature conditions (if applicable) to characterize thermal drift properties.
ARMA Model Identification:
- Preprocess the collected drift data using detrending and normalization techniques.
- Calculate autocorrelation and partial autocorrelation functions to identify potential model orders.
- Estimate parameters for candidate ARMA(p,q) models using maximum likelihood estimation or nonlinear least squares approaches.
- Validate model performance using criteria such as Akaike Information Criterion (AIC) and examination of residual whiteness.
Adaptive Kalman Filter Implementation:
- Implement the state-space representation using the identified ARMA model as the state transition model.
- Initialize process noise covariance (Q) and measurement noise covariance (R) based on characterization data.
- Implement innovation-based adaptation to continuously update noise covariances during operation.
- For systems with signal stability detection (SSD), implement additional stability metrics including:
- Moving variance calculation over 1-5 second windows
- Frequency content analysis using short-time Fourier transform
- Threshold-based state classification with hysteresis
Validation and Performance Assessment:
- Compare compensated outputs against reference measurements using metrics including:
- Allan deviation for noise characterization
- Root mean square error (RMSE) for accuracy assessment
- Spectral analysis to verify preservation of physiological signal content
- Compare compensated outputs against reference measurements using metrics including:
Protocol: Parallel Processing Model for Combined Noise and Drift Reduction
Purpose: To implement a parallel processing architecture that simultaneously addresses high-frequency noise and low-frequency drift through signal decomposition and targeted processing.
Materials and Equipment:
- High-resolution data acquisition system (≥16-bit ADC)
- Multi-objective optimization software framework (MATLAB, Python with PyMOO)
- Neural network training and deployment environment
- Signal processing library with VMD and time-frequency analysis capabilities
Procedure:
Multi-objective Optimization of VMD Parameters:
- Define optimization objectives: minimization of mode mixing and maximization of signal fidelity.
- Implement Multi-Objective Particle Swarm Optimization (MOPSO) to identify optimal VMD parameters [k, α].
- Establish parameter bounds: k typically 3-10, α range 100-5000.
- Execute optimization using recorded bioelectronic signals with known characteristics.
Signal Decomposition and Classification:
- Apply MOVMD (Multi-objective optimized VMD) to raw sensor output.
- Calculate sample entropy (SE) for each resulting Intrinsic Mode Function (IMF).
- Classify IMFs based on SE thresholds:
- Noise-dominant IMFs (SE > thresholdhigh)
- Mixed-signal IMFs (thresholdlow < SE < thresholdhigh)
- Drift-dominant IMFs (SE < thresholdlow)
Parallel Component Processing:
- Noise-dominant components: Apply selective discarding or aggressive filtering.
- Mixed-signal components: Process using Time-Frequency Peak Filtering (TFPF) with optimized window lengths.
- Drift-dominant components: Compensate using BAS-Elman neural network:
- Implement Beetle Antennae Search algorithm to optimize Elman network initial weights.
- Train network using temperature-drift correlation data.
- Deploy optimized network for real-time drift prediction and subtraction.
Signal Reconstruction and Validation:
- Recombine processed components using inverse transformation.
- Validate using ground truth measurements from reference systems.
- Quantify performance using standardized metrics (SNR improvement, drift reduction).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Bioelectronic Signal Processing Research
| Category | Specific Items | Function/Application | Example Use Cases |
|---|---|---|---|
| Signal Acquisition | Multi-contact cuff electrodes | Neural recording and stimulation | Peripheral nerve interfacing [9] |
| Microelectrode arrays | High-density neural recording | Cortical signal acquisition [1] | |
| Precision thermistors | Temperature monitoring | Thermal drift characterization [66] [65] | |
| Shielded cabling systems | Signal interconnection | EMI reduction in physiological recording [65] | |
| Processing Platforms | FPGA development kits | Real-time algorithm implementation | Custom filtering architectures [64] |
| DSP processors | Signal processing algorithms | Kalman filter implementation [64] [66] | |
| Wireless telemetry systems | Data transmission | Implantable device communication [1] | |
| Algorithm Development | Optimization toolboxes (PyMOO, MATLAB) | Algorithm parameter tuning | MOPSO-VMD implementation [66] |
| Neural network frameworks (TensorFlow, PyTorch) | Machine learning model development | BAS-Elman network training [66] | |
| Digital signal processing libraries | Filter implementation and analysis | TFPF, adaptive filtering [66] | |
| Validation Systems | Precision rate tables | Motion reference generation | Inertial sensor characterization [64] |
| Environmental chambers | Controlled temperature testing | Thermal drift assessment [65] | |
| Reference sensors | Ground truth measurement | Algorithm performance validation [64] [66] |
Figure 2: Integrated Closed-Loop System Architecture with Noise and Drift Challenges
The challenges of noise filtering and drift compensation represent fundamental barriers to the widespread clinical implementation of closed-loop bioelectronic systems. While significant advances have been made in both algorithmic approaches and implementation strategies, the field continues to evolve toward increasingly sophisticated solutions. The parallel processing model that separately addresses different signal components has demonstrated remarkable performance improvements in experimental systems, reducing angle random walk by over 99% in some implementations [66]. Similarly, the integration of signal stability detection with adaptive filtering has shown superior performance under challenging low-dynamic conditions where traditional approaches falter [64].
Future developments in this field will likely focus on several key areas. Miniaturization of processing capabilities will enable more sophisticated algorithms to be implemented directly in implantable devices, reducing latency and power consumption associated with wireless data transmission [1]. Novel sensing methodologies, including the use of multiple complementary sensors and fusion algorithms, will provide more robust reference points for drift compensation [10]. Additionally, personalized adaptation approaches that learn individual patient characteristics and patterns over extended periods will enable increasingly precise and effective therapy delivery [10] [43].
As these technological advances mature, closed-loop bioelectronic systems will become increasingly capable of maintaining signal integrity in the face of noise and drift challenges, unlocking new therapeutic possibilities across a wide range of neurological, inflammatory, and metabolic conditions. The continued convergence of signal processing expertise, biomedical engineering, and clinical insight promises to deliver increasingly sophisticated solutions to these fundamental challenges in the coming years.
Clinical Evidence and Therapeutic Value Assessment
Bioelectronic medicine represents a transformative approach to treating disease by using electronic devices to modulate neural circuits that control biological processes. This field brings together material science, biochemistry, biophysics, molecular medicine, neuroscience, immunology, bioengineering, electrical engineering, computer science, and artificial intelligence to develop new insights into the diagnosis and treatment of conditions as varied as cancer, rheumatoid arthritis, inflammatory bowel disease, obesity, diabetes, asthma, paralysis, blindness, and neurodegenerative diseases [3]. The fundamental premise rests on decoding the electrical signaling within the nervous system that regulates physiological functions, then using technological interfaces to record, stimulate, or block these neural signals to achieve therapeutic outcomes.
Assessing treatment efficacy in this emerging field requires sophisticated metrics that can capture complex physiological and clinical changes. Unlike pharmaceutical interventions with systemic molecular targets, bioelectronic approaches often work through precise neuromodulation of specific neural pathways. This necessitates a multifaceted evaluation framework encompassing molecular biomarkers, electrophysiological recordings, functional clinical scales, and patient-reported outcomes. Researchers must consider both the direct neural interface performance and the downstream biological effects to fully characterize therapeutic impact.
The growing importance of this field is underscored by recent regulatory milestones, including the FDA approval of SetPoint Medical's bioelectronic medicine device for rheumatoid arthritis treatment—a novel neuroimmunomodulation therapy targeting the vagus nerve [3]. This approval, based on the pioneering work of Dr. Kevin J. Tracey, establishes a critical precedent for the entire field and validates the potential of bioelectronic approaches to address inflammatory conditions through precisely targeted neural stimulation. Similar approaches are now being investigated for neurological disorders, creating a need for standardized efficacy metrics across both neurological and inflammatory conditions.
Efficacy Metrics for Neurological Conditions
Neuroinflammatory and Neurodegenerative Disorders
In neurological conditions, efficacy assessment requires multidimensional metrics that capture changes in neural function, inflammatory status, and clinical manifestation. Neuroinflammatory diseases such as multiple sclerosis (MS), Alzheimer's disease (AD), and Parkinson's disease (PD) involve complex interactions between neural cells and immune mediators, necessitating biomarker panels that can differentiate between distinct pathological processes [67].
Table 1: Efficacy Biomarkers in Neuroinflammatory and Neurodegenerative Conditions
| Condition | Primary Efficacy Biomarkers | Secondary Clinical Endpoints | Neuroimaging Metrics |
|---|---|---|---|
| Multiple Sclerosis | Neurofilament Light Chain (NfL) [67], IL-1β, TNF-α, IFN-γ [67], B-cell depletion levels [67] | Expanded Disability Status Scale (EDSS), relapse rate, cognitive function tests | MRI lesion load, brain atrophy rates, blood-brain barrier integrity [67] |
| Alzheimer's Disease | Amyloid-β levels, tau protein, NLR [67], CRP [67], IL-6 [67], TREM2 gene variants [67] | ADAS-Cog, MMSE, CDR, quality of life measures | Amyloid PET burden, hippocampal volume, cortical thickness |
| Parkinson's Disease | α-synuclein aggregates [67], TNF-α [67], IL-1β [67], LRRK2 gene variants [67] | UPDRS, Hoehn & Yahr staging, tremor scales, gait analysis | Dopaminergic transporter imaging, substantia nigra volumetry |
In multiple sclerosis, neurofilament light chain (NfL) has emerged as a particularly valuable biomarker for monitoring treatment efficacy, as it correlates with disease activity and neuroaxonal damage [67]. The development of B-cell depleting therapies such as ocrelizumab has demonstrated the importance of measuring specific immune cell populations alongside traditional clinical metrics [67]. For Alzheimer's disease, monoclonal antibodies targeting amyloid-beta, including Aducanumab, Lecanemab, and Donanemab, have established new efficacy standards through reduction of amyloid burden, though clinical translation has been complicated by adverse effects including amyloid-related imaging abnormalities (ARIA) [67]. Parkinson's disease assessments now incorporate inflammatory biomarkers in cerebrospinal fluid that can distinguish PD from other neurodegenerative conditions such as Alzheimer's disease and Dementia with Lewy Bodies, enabling more targeted treatment approaches [67].
Viral CNS Infections and Sequelae
Viral infections of the central nervous system represent another area where bioelectronic approaches show promise. West Nile virus neuroinvasive disease (WNND) causes significant long-term neurological sequelae in 40-60% of survivors, including muscle weakness, fatigue, depression, memory loss, and cognitive impairment [68]. These persistent symptoms provide a complex efficacy measurement challenge that requires integrated metrics spanning molecular, functional, and cognitive domains.
Research into the mechanisms of WNND sequelae has revealed that complement-mediated synaptic loss in the hippocampus contributes to cognitive deficits, providing a potential biomarker target for interventions aimed at preserving cognitive function [68]. Additionally, persistent T-cell mediated inflammation and disrupted neurogenesis appear to drive long-term symptoms, suggesting that efficacy assessments should include monitoring of specific immune cell populations and inflammatory mediators in conjunction with traditional cognitive testing [68]. The identification of regional brain atrophy in the brainstem, cerebellum, and thalamus of WNND survivors further supports the inclusion of volumetric MRI analyses in efficacy assessments for interventions targeting viral CNS infection sequelae [68].
Efficacy Metrics for Inflammatory Conditions
Rheumatoid Arthritis and Autoimmune Disorders
Inflammatory conditions have emerged as promising targets for bioelectronic medicine, particularly through vagus nerve stimulation approaches that modulate the inflammatory reflex. Rheumatoid arthritis represents a landmark indication, with the recent FDA approval of SetPoint Medical's vagus nerve stimulation device establishing a new efficacy assessment paradigm for bioelectronic interventions [3].
The inflammatory reflex, a neural circuit that regulates immune function, provides both mechanism and metrics for evaluating bioelectronic efficacy in autoimmune conditions. Key inflammatory biomarkers including C-reactive protein (CRP), tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-1 beta (IL-1β) serve as primary efficacy measures, complemented by clinical assessments such as the Disease Activity Score (DAS-28), American College of Rheumatology response criteria (ACR20/50/70), and health assessment questionnaires [3] [67]. The successful application of vagus nerve stimulation in rheumatoid arthritis demonstrates that bioelectronic approaches can achieve clinically significant improvements in these established metrics, validating their use across inflammatory conditions.
Table 2: Efficacy Metrics for Inflammatory Conditions in Bioelectronic Medicine
| Condition | Inflammatory Biomarkers | Clinical Endpoints | Functional & Quality of Life Measures |
|---|---|---|---|
| Rheumatoid Arthritis | CRP [67], TNF-α [67], IL-6 [67], IL-1β [67] | DAS-28, ACR20/50/70, joint count, radiographic progression | HAQ-DI, patient global assessment, pain VAS |
| Inflammatory Bowel Disease | Fecal calprotectin, CRP, IL-6, TNF-α | Mayo Score (ulcerative colitis), CDAI (Crohn's), endoscopic healing | IBD-Q, fatigue scales, work productivity |
| Systemic Inflammatory Response | NLR [67], cytokine panels (IFN-γ, IP-10) [68], complement factors [68] | SOFA score, organ failure assessment, survival rates | Quality of life measures, functional status |
Beyond rheumatoid arthritis, inflammatory bowel disease represents another condition where bioelectronic approaches show significant promise. Research on transcutaneous auricular vagus nerve stimulation (taVNS) in experimental models of colitis has demonstrated measurable reductions in local and systemic inflammation, establishing preclinical efficacy metrics that can inform human trial design [17]. The efficacy assessment in these models incorporates colon histopathology scores, mucosal integrity measures, and inflammatory cytokine levels alongside behavioral observations, providing a comprehensive framework for evaluating bioelectronic intervention impact.
Metabolic and Other Inflammatory Conditions
The application of bioelectronic medicine continues to expand into metabolic disorders with inflammatory components, including obesity, fatty liver disease, and diabetes-related conditions [17]. Recent research has highlighted the role of TGF-β signaling and vagus nerve innervation in these disorders, suggesting new efficacy metrics that combine traditional metabolic parameters with inflammatory biomarkers [17].
Focused ultrasound neuromodulation approaches are being investigated for conditions such as post-operative hyperglycemia, with efficacy assessments incorporating glucose tolerance tests, insulin sensitivity measures, and inflammatory markers including IL-6 and TNF-α [17]. These multidimensional assessments recognize the interconnected nature of metabolic and inflammatory pathways, providing a more comprehensive picture of bioelectronic intervention effects than traditional single-parameter metrics.
Experimental Protocols and Methodologies
AI-Guided Neural Control Protocol
Advanced experimental protocols are essential for establishing efficacy metrics in bioelectronic medicine. One cutting-edge approach involves artificial intelligence-guided neural control using deep reinforcement learning (RL) and infrared neural stimulation (INS) in rodent models [69]. This protocol enables precise closed-loop control of neural circuits, allowing researchers to establish causal relationships between specific neural firing patterns and therapeutic outcomes.
The protocol consists of several key steps:
- Chronic electrode implantation to facilitate long-term neural stimulation and recording capabilities [69]
- Thalamic infrared neural stimulation combined with cortical recordings to map neural pathways [69]
- Deep reinforcement learning implementation to drive neural firing toward desired states [69]
This methodology represents a significant advancement over traditional open-loop deep brain stimulation by incorporating real-time feedback and adaptive control algorithms. The closed-loop approach enables more precise titration of neural modulation, potentially enhancing therapeutic efficacy while minimizing side effects. For efficacy assessment, this protocol provides high-resolution electrophysiological data that can be correlated with behavioral and molecular outcomes, creating a comprehensive efficacy dataset.
Neural Interface Optimization Protocols
Improving the acceptance and success of implanted neural interfaces represents another critical methodological frontier in bioelectronic medicine. Recent protocols focus on enhancing biocompatibility, signal fidelity, and long-term stability of neural interfaces through material innovations and implantation techniques [17].
These protocols include:
- Accelerated regeneration approaches using electrical stimulation following peripheral nerve injury [17]
- Multi-system assessment methodologies for evaluating the effects of spinal cord stimulation on urinary, bowel, and sexual function [17]
- Non-invasive neuromodulation techniques including transcutaneous spinal cord stimulation (tSCS) and temporal interference (TI) approaches [17]
Each of these methodologies incorporates specialized efficacy metrics tailored to the specific intervention and target condition. For example, protocols evaluating peripheral nerve regeneration combine electrophysiological conduction studies with functional recovery assessments and histological analyses of nerve tissue [17]. Similarly, multi-system assessments after spinal cord injury require integrated evaluation of autonomic, sensory, and motor functions to fully capture intervention efficacy [17].
Signaling Pathways and Neural Circuits
Neuro-Immune Signaling Pathways
The efficacy of bioelectronic interventions depends fundamentally on their ability to modulate specific neural circuits that regulate physiological processes. In inflammatory conditions, the inflammatory reflex represents the primary neural circuit targeted by bioelectronic approaches. This circuit originates in the vagus nerve, which detects peripheral inflammation and relays this information to the brainstem, ultimately leading to efferent signals that suppress inflammatory cytokine production through mechanisms including splenic nerve activation and noradrenergic signaling to immune cells [3].
Key molecular mediators in this pathway include:
- Acetylcholine released from vagus nerve terminals that binds to α7 nicotinic receptors on macrophages
- Norepinephrine from splenic nerves that regulates lymphocyte function
- Inflammatory cytokines including TNF-α, IL-6, and IL-1β whose production is modulated by neural signals [67]
In neurological conditions, the targeted neural circuits vary by disorder but often involve cortical, subcortical, and spinal pathways. For movement disorders such as Parkinson's disease, basal ganglia-thalamocortical circuits represent primary modulation targets, with efficacy correlated to normalization of pathological oscillatory activity [67]. For cognitive disorders, hippocampal-prefrontal circuits and default mode network connectivity provide both targets and efficacy metrics for bioelectronic interventions.
Circuit Dysregulation in Disease States
Understanding the specific alterations in neural signaling pathways during disease states is essential for designing effective bioelectronic interventions and appropriate efficacy metrics. In neurodegenerative conditions, neuroinflammation involves complex interactions between neurons, microglia, and astrocytes, with disease-specific patterns of circuit dysregulation [67].
In Alzheimer's disease, amyloid-β accumulation and tau pathology trigger microglial activation through pattern recognition receptors including toll-like receptors (TLRs), initiating sustained neuroinflammation that contributes to synaptic loss and cognitive decline [67]. Efficacy metrics for bioelectronic interventions in AD must therefore account for both the primary protein pathologies and the secondary inflammatory responses.
In Parkinson's disease, α-synuclein aggregates activate microglia and promote pro-inflammatory cytokine production, leading to degeneration of dopaminergic neurons in the substantia nigra [67]. The involvement of the gut-brain axis further complicates this picture, with alterations in gut microbiota composition potentially influencing neuroinflammation through multiple signaling pathways [67]. Bioelectronic approaches targeting PD must therefore modulate these complex circuit interactions, with efficacy assessments spanning neural, inflammatory, and gastrointestinal domains.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Bioelectronic Medicine Studies
| Reagent/Category | Function/Application | Specific Examples & Technical Notes |
|---|---|---|
| Neural Interfaces | Recording and stimulation of neural activity | Chronic electrode arrays [69], vagus nerve cuffs, cortical recording devices [17] |
| Stimulation Systems | Delivery of controlled neural stimulation | Infrared neural stimulation (INS) systems [69], transcutaneous electrical stimulators [17], focused ultrasound devices [17] |
| AI & Analytics Platforms | Data processing and closed-loop control | Deep reinforcement learning algorithms [69], real-time neural signal processors [17], machine learning classifiers [17] |
| Molecular Assays | Biomarker quantification and validation | Multiplex cytokine panels [67], neurofilament light chain ELISA [67], RNA sequencing for inflammatory genes [68] |
| Animal Models | Preclinical efficacy testing | Rodent neural control models [69], large animal surgical stress models [17], autoimmune disease models [67] |
The research toolkit for bioelectronic medicine continues to evolve with technological advancements. Recent innovations include high-density brain-implantable devices capable of real-time neural signal processing, enabling unprecedented resolution in neural circuit monitoring and modulation [17]. Similarly, non-invasive neuromodulation approaches such as temporal interference (TI) stimulation and transcutaneous spinal cord stimulation (tSCS) are expanding the toolkit for human applications [17].
Machine learning and artificial intelligence platforms represent another critical component of the modern bioelectronic medicine toolkit. These systems enable pattern recognition in complex neural datasets, identification of predictive biomarkers, and implementation of adaptive closed-loop control algorithms that optimize stimulation parameters based on real-time physiological feedback [69] [17]. The integration of these computational tools with traditional biological assays creates a powerful framework for establishing comprehensive efficacy metrics across neurological and inflammatory conditions.
The establishment of robust efficacy metrics for bioelectronic medicine requires integrated assessment frameworks that span molecular, neural, physiological, and clinical domains. As the field advances toward non-invasive closed-loop autonomic neuromodulation systems [17], efficacy assessment must similarly evolve to capture the dynamic, multidimensional nature of treatment responses. Future directions include the development of biomarker panels that can predict individual treatment responsiveness, the validation of digital biomarkers derived from wearable sensors, and the standardization of efficacy metrics across clinical trials to enable cross-study comparisons.
The recent regulatory approval of bioelectronic devices for inflammatory conditions [3] establishes an important precedent for the entire field and validates the approach of targeting neural circuits to treat disease. As research continues to elucidate the complex signaling pathways connecting the nervous and immune systems [67], efficacy metrics will become increasingly sophisticated, potentially incorporating real-time neural signaling patterns alongside traditional inflammatory biomarkers. This evolution in assessment methodologies will parallel advances in bioelectronic technology itself, driving the field toward more personalized, adaptive, and effective therapeutic interventions for both neurological and inflammatory conditions.
Bioelectronic medicine represents a paradigm shift in therapeutic interventions, moving from molecular-based pharmacology to the modulation of neural signaling for disease treatment. This field uses advanced electronic devices to interface with the nervous system, targeting specific neural circuits to regulate physiological processes and restore health [3] [63]. As defined by the International Neuromodulation Society, it involves "the use of advanced medical device technology to enhance or suppress the activity of the nervous system for the treatment of disease" [63]. In contrast, pharmacological treatment relies on the administration of chemical compounds that interact with specific biological targets through molecular mechanisms, following traditional drug-receptor principles [70].
The historical context of bioelectronic medicine dates back to ancient civilizations, with records of electric fish being used to treat headaches in Egyptian and Greek medicine [63] [10]. Modern bioelectronic medicine began its significant evolution in the mid-20th century with the development of the first fully implantable pacemaker in 1958 [70] [30], followed by cochlear implants in 1961 [70]. The field has since expanded to include deep brain stimulation (DBS) for Parkinson's disease, spinal cord stimulation (SCS) for chronic pain, and vagus nerve stimulation (VNS) for conditions ranging from epilepsy to inflammatory disorders [3] [70] [63].
Fundamental Mechanisms of Action
Pharmacological Mechanisms
Pharmacological interventions operate on the principle of molecular specificity, where drugs produce therapeutic effects by interacting with specific biological targets such as receptors, enzymes, or ion channels [70]. The fundamental characteristics include:
- Systemic Distribution: Drugs are typically administered systemically (orally, intravenously) and distribute throughout the body via the bloodstream, leading to interactions with both target and off-target tissues [70].
- Biochemical Interactions: Therapeutic effects are mediated through precise biochemical interactions, such as receptor agonism/antagonism, enzyme inhibition, or interference with cellular signaling pathways [70].
- Metabolism and Elimination: Drugs undergo metabolic transformation and clearance, often producing active metabolites or presenting challenges with maintaining therapeutic windows [70].
- Fixed Dosing Regimens: Pharmacological treatments generally follow predetermined dosing schedules that are not dynamically responsive to real-time physiological changes in the patient [70].
Bioelectronic Mechanisms
Bioelectronic medicine operates through the principles of neural signaling and circuit modulation, characterized by:
- Targeted Neural Modulation: Devices interface with electrically active tissues (nerves, brain, spinal cord) to modulate neural activity in specific pathways that regulate bodily functions [70] [63].
- Bidirectional Communication: Advanced bioelectronic systems can both stimulate and record from neural tissues, enabling closed-loop control systems that respond to physiological feedback [70] [10] [30].
- Anatomical Precision: By targeting specific neural structures, bioelectronic devices can achieve organ-specific or function-specific modulation without systemic exposure [70].
- Electrical Signaling: Therapeutic effects are mediated through electrical impulses that mimic or modulate natural neural signaling patterns, exploiting the body's inherent electrical communication systems [70] [63].
Table 1: Fundamental Mechanism Comparison
| Characteristic | Pharmacological Treatment | Bioelectronic Treatment |
|---|---|---|
| Therapeutic Agent | Chemical compounds | Electrical signals |
| Delivery Method | Systemic (oral, IV, topical) | Targeted (implantable/non-invasive devices) |
| Mechanism of Action | Molecular interactions (receptors, enzymes) | Neural circuit modulation |
| Specificity | Biochemical (dependent on drug distribution) | Anatomical (dependent on device placement) |
| Dosing Control | Fixed regimens, slow adjustment | Programmable, dynamic adjustment possible |
| Onset/Duration | Dependent on pharmacokinetics | Immediate onset, programmable duration |
Key Signaling Pathways
Bioelectronic medicine often targets specific neural pathways to achieve therapeutic effects. One well-characterized pathway is the inflammatory reflex, in which vagus nerve stimulation modulates immune function through a neural circuit that connects the brain to the spleen and other immune organs [63]. This pathway involves:
- Neural Activation: Electrical stimulation of the vagus nerve activates afferent and efferent fibers [63].
- Splenic Innervation: Efferent signals travel through the splenic nerve, leading to norepinephrine release in the spleen [63].
- Immune Modulation: Norepinephrine stimulates acetylcholine-releasing T cells, which subsequently suppress macrophage production of pro-inflammatory cytokines (e.g., TNF, IL-1, IL-6) via α7 nicotinic acetylcholine receptors (α7nAchR) [63].
This neuro-immune pathway demonstrates how bioelectronic devices can achieve precise immunomodulation without systemic immunosuppression, contrasting sharply with conventional pharmacological approaches to inflammatory diseases like rheumatoid arthritis or inflammatory bowel disease [63].
Figure 1: Cholinergic Anti-inflammatory Pathway Activated by Vagus Nerve Stimulation
Comparative Therapeutic Profiles
Efficacy and Clinical Outcomes
The therapeutic efficacy of bioelectronic versus pharmacological approaches varies significantly across disease domains, with each modality demonstrating distinct advantage profiles.
Table 2: Clinical Efficacy Comparison Across Disease Domains
| Disease/Condition | Pharmacological Approach | Bioelectronic Approach | Comparative Efficacy |
|---|---|---|---|
| Rheumatoid Arthritis | DMARDs, biologics (anti-TNF) | Vagus nerve stimulation (SetPoint Medical) | Bioelectronic: FDA-approved device shows significant improvement in patients refractory to pharmacological treatments [3] |
| Parkinson's Disease | Levodopa, dopamine agonists | Deep Brain Stimulation (DBS) | Bioelectronic: Superior for managing motor fluctuations and dyskinesias in advanced disease [70] [30] |
| Drug-Resistant Epilepsy | Multiple AEDs | Vagus Nerve Stimulation (VNS) | Bioelectronic: Effective in 30-40% of pharmacoresistant patients [63] [30] |
| Chronic Pain | NSAIDs, opioids, adjuvants | Spinal Cord Stimulation (SCS) | Bioelectronic: Superior long-term outcomes for neuropathic pain, avoids opioid-related risks [70] [8] |
| Cardiac Arrhythmia | Antiarrhythmic drugs | Pacemakers, defibrillators | Bioelectronic: Gold-standard for life-threatening arrhythmias [70] [71] [30] |
Safety and Side Effect Profiles
The safety considerations for these two therapeutic paradigms differ substantially in both nature and mechanism.
Pharmacological Safety Considerations:
- Systemic Toxicity: Off-target interactions cause side effects in non-diseased tissues and organs [70].
- Metabolic Complications: Many drugs undergo hepatic metabolism, potentially causing liver toxicity or drug-drug interactions [70].
- Narrow Therapeutic Indices: Some medications require precise dosing to avoid toxicity while maintaining efficacy [70].
- Immune Reactions: Biologics and some small molecules can trigger immune responses or hypersensitivity reactions [70].
Bioelectronic Safety Considerations:
- Surgical Risks: Implantable devices carry procedural risks (infection, bleeding, tissue damage) [70].
- Device-Related Complications: Hardware malfunction, lead migration, battery failure, or foreign body reactions [70] [63].
- Stimulation-Limited Side Effects: Adverse effects are typically localized and reversible with adjustment of stimulation parameters [70].
- Long-Term Biocompatibility: Chronic tissue interface challenges include fibrosis or electrode degradation [70].
Table 3: Adverse Effect Profile Comparison
| Parameter | Pharmacological Treatment | Bioelectronic Treatment |
|---|---|---|
| Nature of Side Effects | Systemic, metabolic, immunological | Localized, device-related, stimulation-induced |
| Reversibility | Dependent on drug half-life and metabolism | Immediate with stimulation adjustment |
| Management Approach | Dose adjustment, adjunctive medications | Device reprogramming, surgical revision if needed |
| Long-Term Risks | Cumulative toxicity, organ damage | Device failure, tissue changes at interface |
| Therapeutic Window | Defined by pharmacokinetics/pharmacodynamics | Defined by stimulation parameters and target anatomy |
Technical and Methodological Approaches
Experimental Protocols in Bioelectronic Research
Vagus Nerve Stimulation for Inflammatory Conditions
Objective: To evaluate the efficacy of transcutaneous vagus nerve stimulation (tVNS) in modulating inflammatory responses and compassionate mental states in human subjects [72].
Methodology:
- Study Design: Randomized, sham-controlled, 2×2 factorial design (stimulation × imagery condition) [72].
- Participants: 120 healthy volunteers screened for neurological/psychiatric conditions [72].
- Stimulation Protocol:
- Active tVNS: Mild electrical pulses applied to the tragus (auricular branch of vagus nerve)
- Sham tVNS: Identical stimulation applied to earlobe (non-vagal innervation)
- Parameters: Customized intensity (sensory threshold without pain), pulse width 200-300μs, frequency 20-25Hz [72]
- Concurrent Intervention: Standardized self-compassionate or sham mental imagery audio instructions [72].
- Assessment Timeline:
- Lab sessions (Days 1 and 8): Pre-stimulation, peri-stimulation, and post-imagery measures
- Home sessions (Days 2-7): Self-administered stimulation with end-of-session measures [72]
- Primary Outcomes: State self-compassion scales, self-criticism measures, heart rate variability (HRV) [72].
- Secondary Outcomes: Attentional bias to compassionate faces (eye-tracking), physiological stress markers [72].
Key Technical Considerations: Credible sham control, standardized imagery scripts, objective HRV bioassay of vagal engagement, and ecological momentary assessment for real-world validity [72].
Closed-Loop Deep Brain Stimulation for Parkinson's Disease
Objective: To develop and validate adaptive deep brain stimulation (aDBS) that responds in real-time to pathological neural signatures [30].
Methodology:
- Device Platform: Medtronic Percept with BrainSense DBS system capable of simultaneous recording and stimulation [30].
- Surgical Protocol: Stereotactic implantation of quadripolar electrodes in subthalamic nucleus (STN) or globus pallidus internus (GPi) [30].
- Biomarker Identification: Local field potentials (LFPs) recorded from implanted electrodes, with specific focus on beta-band (13-30 Hz) oscillations correlated with motor symptom severity [30].
- Control Algorithm: Stimulation amplitude modulated based on real-time beta-power thresholds, with continuous adaptation to individual patient's neural signatures [30].
- Outcome Measures: Unified Parkinson's Disease Rating Scale (UPDRS) motor scores, medication reduction, stimulation-induced side effects, battery longevity [30].
Technical Innovation: First FDA-approved closed-loop DBS system that senses and adapts to neural signals in real-time, representing a significant advancement beyond open-loop stimulation [30].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Bioelectronic Medicine Investigations
| Item | Function/Application | Technical Specifications |
|---|---|---|
| Multielectrode Arrays | Neural recording and stimulation interface | High-density microelectrodes (e.g., Utah array, Michigan probe); conducting polymers (PEDOT:PSS) for improved impedance [70] |
| Implantable Pulse Generators (IPGs) | Device power and control electronics | Hermetically sealed titanium casing; programmable stimulation parameters (amplitude, frequency, pulse width) [70] |
| Wireless Power Transfer Systems | Battery-less implant operation | Inductive coupling (electromagnetic); ultrasound energy transfer; magneto-electric systems [70] |
| Biocompatible Encapsulation Materials | Chronic implant protection | Parylene-C, silicone elastomers, polyimide; flexible/substrate materials to minimize foreign body reaction [70] |
| Neural Recording Systems | Electrophysiological signal acquisition | Multi-channel amplifiers, analog-to-digital converters; real-time signal processing capabilities [70] [30] |
| Closed-Loop Control Algorithms | Adaptive stimulation delivery | Machine learning classifiers for pathological state detection; proportional control systems [10] [30] |
| Biomaterial Coatings | Improved tissue-device interface | Conducting polymers, graphene, MXenes; drug-eluting coatings for anti-inflammatory effects [70] |
Figure 2: Bioelectronic Medicine Research and Development Workflow
Clinical Implementation and Market Landscape
Adoption Trends and Market Dynamics
The bioelectronic medicine market has demonstrated substantial growth, reflecting increasing clinical adoption and technological advancement. The market was valued at approximately $23.54 billion in 2024 and is projected to reach $33.59 billion by 2030, registering a compound annual growth rate (CAGR) of 6.1% [8]. This growth trajectory significantly outpaces many traditional pharmaceutical market segments.
Table 5: Bioelectronic Medicine Market Segmentation and Growth Indicators
| Segment | 2024 Market Value | Projected Growth | Key Drivers |
|---|---|---|---|
| Implantable Devices | 55.3% market share [71] | Steady adoption | Chronic disease management, technological miniaturization |
| Cardiac Applications | Leading application segment [71] | CAGR 6.1% [8] | Aging population, rising cardiovascular disease prevalence |
| Neurological Applications | Significant market share [8] | Accelerated growth | Expansion of indications for DBS, SCS, VNS |
| Non-Invasive Devices | Emerging segment [10] | High growth potential | Patient preference, reduced regulatory barriers |
| Asian Markets | Varying penetration | CAGR 8.2% (China) [71] | Healthcare infrastructure development, rising disposable income |
Integration with Digital Health and Artificial Intelligence
A transformative trend in bioelectronic medicine is the integration with digital health platforms and artificial intelligence, enabling:
- Closed-Loop Systems: Devices that automatically adjust therapy based on real-time physiological feedback [10] [30]. For example, modern DBS systems can sense pathological neural signals and respond with appropriate stimulation patterns without clinician intervention [30].
- Predictive Analytics: AI algorithms that analyze patient data to optimize stimulation parameters and predict disease exacerbations [8].
- Remote Monitoring: Cloud-connected devices that enable continuous assessment of therapy efficacy and patient status outside clinical settings [8].
- Personalized Treatment Protocols: Machine learning approaches that tailor stimulation patterns to individual patient anatomy and disease characteristics [10] [30].
This integration represents a significant advantage over traditional pharmacological approaches, where personalization is limited by fixed dosage forms and pharmacokinetic variability between patients.
Future Perspectives and Research Directions
The future evolution of bioelectronic medicine will be characterized by several key developments:
Technological Advancements
- Miniaturization and Battery-Free Operation: Development of millimeter-scale devices powered by wireless energy transfer or bioenergy harvesting [70].
- High-Density Neural Interfaces: Electrode arrays with thousands of contacts enabling precise neural circuit mapping and modulation [70].
- Multimodal Devices: Integrated systems combining electrical stimulation, drug delivery, and biosensing capabilities [70].
- Biostable Materials: Novel composites and coatings that maintain functional integrity over decades of implantation [70].
Clinical Expansion
- Inflammatory and Autoimmune Diseases: Building on the success of VNS for rheumatoid arthritis, bioelectronic approaches are being investigated for inflammatory bowel disease, lupus, and other immune-mediated conditions [3] [63].
- Metabolic Disorders: Research exploring neuromodulation of organs involved in glucose homeostasis and energy balance for diabetes and obesity management [71] [8].
- Mental Health Applications: Investigating bioelectronic interventions for depression, PTSD, and substance use disorders through modulation of neuro-immune pathways [10] [72].
- Diagnostic Applications: Using neural signals as biomarkers for early disease detection and monitoring of treatment response [10].
Regulatory and Accessibility Challenges
Despite the promising trajectory, bioelectronic medicine faces several implementation challenges:
- Cost and Reimbursement: High initial device costs and inconsistent insurance coverage create barriers to widespread adoption, particularly in middle- and low-income countries [8].
- Technical Expertise Requirements: Device implantation and programming require specialized training, potentially limiting availability outside major medical centers [70].
- Long-Term Safety Data: While existing devices have demonstrated good medium-term safety profiles, decades-long performance data are still being accumulated [70].
- Interdisciplinary Collaboration: Optimal advancement requires seamless integration of neuroscience, engineering, materials science, and clinical medicine [63].
The comparative analysis between bioelectronic and pharmacological treatment paradigms reveals complementary rather than exclusively competitive therapeutic approaches. Bioelectronic medicine offers distinct advantages in target specificity, reversibility, personalization potential, and avoidance of systemic side effects for conditions with well-defined neural circuitry. Pharmacological approaches maintain superiority for diffuse systemic conditions, infectious diseases, and conditions where molecular targets are not neurologically accessible.
The emerging integration of bioelectronic devices with digital health technologies and artificial intelligence represents a fundamental advancement in therapeutic precision, enabling truly personalized, adaptive treatments that respond to real-time changes in patient physiology. This capability for closed-loop control represents a significant paradigm advance beyond static pharmacological dosing regimens.
As research continues to elucidate the intricate connections between neural circuits and physiological functions, the scope of addressable diseases through bioelectronic approaches will expand. The future therapeutic landscape will likely feature increasingly sophisticated combinations of bioelectronic and pharmacological treatments, leveraging the unique advantages of each modality to optimize patient outcomes across the spectrum of human disease.
Bioelectronic medicine (BEM) represents a paradigm shift in therapeutic intervention, moving from systemic pharmacology to targeted neuromodulation for disease treatment. This approach utilizes implanted electronic devices to modulate the electrical activity of specific neural pathways, which in turn regulates organ function and biological processes [1]. The fundamental thesis of bioelectronic medicine research is to decode the "neural code" of health and disease, enabling the development of precise, modifiable, and reversible treatments that address the root causes of pathology with minimal off-target effects [7] [1].
The safety profile of BEM is inherently different from that of systemic drug therapies. While pharmaceuticals achieve their effects through molecular interactions in the bloodstream and tissues—often leading to unwanted interactions with non-target tissues—BEM acts by selectively modulating neural circuits that control specific physiological functions [1]. This targeted mechanism offers the potential for reduced systemic side effects, personalized dosing, and the ability to turn off treatment instantly if adverse effects occur [1]. This technical guide provides a comprehensive comparison of safety profiles between these therapeutic modalities, with a focus on quantitative side-effect data, underlying mechanisms, and research methodologies.
Mechanisms of Action and Associated Safety Profiles
Systemic Drug Therapies: The Challenge of Off-Target Effects
Systemic drug therapies operate on the principle of mass-action molecular interactions. When administered, drugs distribute throughout the body via the bloodstream, interacting with their intended biological targets but also with structurally similar off-target sites, leading to dose-dependent side effects [1]. The safety challenges are compounded by several factors:
- Imperfect Specificity: Drug specificity is not absolute, leading to interactions with healthy tissues and resulting in toxicity [1].
- Continuous Exposure: Drugs often remain in the system for extended periods, even after their therapeutic effect is no longer needed [1].
- Non-optimized Dosing: Standardized dosing regimens often result in subtherapeutic or supratherapeutic concentrations in individual patients, leading to either poor efficacy or excessive side effects [1].
Quantitative studies demonstrate that between 38% and 100% of reported side-effects to medications are non-pharmacological in nature, instead arising from nocebo effects and treatment context [73]. Furthermore, serious adverse drug reactions are estimated to be the fourth leading cause of death in the United States, resulting in approximately 100,000 deaths annually [74].
Bioelectronic Medicine: Targeted Neuromodulation
In contrast, bioelectronic medicine treats disease by stimulating electrically active tissues, primarily components of the nervous system that innervate every organ in the body [1]. The inflammatory reflex, a well-characterized neural circuit involving the vagus nerve, exemplifies this approach [7]. Vagus nerve stimulation (VNS) modulates immune function and inflammation through a precisely mapped neural pathway:
- Efferent Vagus Nerve Signaling: Electrical stimulation activates efferent vagus nerve fibers.
- Norepinephrine Release in Spleen: These signals lead to norepinephrine release from the splenic nerve.
- T-cell Acetylcholine Production: Norepinephrine interacts with β-adrenergic receptors on choline acetyltransferase (ChAT)+ T cells.
- Macrophage Inhibition: Acetylcholine from T cells binds to α7 nicotinic acetylcholine receptors (α7nAChR) on macrophages, inhibiting pro-inflammatory cytokine release [7].
This targeted mechanism localizes the therapeutic effect to specific immune cell populations, dramatically reducing systemic exposure compared to anti-inflammatory drugs like corticosteroids or biologic agents.
Table 1: Fundamental Differences in Therapeutic Mechanisms
| Characteristic | Systemic Drug Therapies | Bioelectronic Medicine |
|---|---|---|
| Mechanism of Action | Molecular interactions in bloodstream and tissues | Electrical modulation of neural circuits |
| Specificity | Limited by biochemical similarity of targets | Determined by anatomical placement and stimulation parameters |
| Reversibility | Limited (drug must be metabolized) | Immediate (stimulation can be ceased) |
| Dosing Control | Fixed or slow-release formulations | Programmable, titratable, on-demand |
| Distribution | Systemic (throughout body) | Localized to targeted neural pathway |
Quantitative Safety and Side-Effect Comparisons
Comparative Analysis in Inflammatory Conditions
Clinical studies directly comparing bioelectronic and pharmacological interventions are emerging, particularly in rheumatology and gastroenterology. The recent FDA approval of SetPoint Medical's vagus nerve stimulation device for rheumatoid arthritis marks a significant milestone, providing the first direct comparison point [3].
In a clinical trial of rheumatoid arthritis patients, VNS demonstrated significant reduction in disease activity with side-effect profiles primarily related to the implantation procedure and device function, rather than the systemic immunosuppressive effects associated with conventional disease-modifying antirheumatic drugs (DMARDs) and biologics [3] [7]. Unlike pharmacological immunosuppressants, which increase vulnerability to infections and may have hepatic, renal, or hematological toxicity, VNS side effects are typically localized and manageable.
Comparative Analysis in Neurological and Psychiatric Conditions
Substantial safety data exists for bioelectronic treatments of neurological conditions. Deep Brain Stimulation (DBS) for Parkinson's disease and Vagus Nerve Stimulation for epilepsy have been used for decades, enabling robust safety comparisons with pharmacological treatments.
Table 2: Side-Effect Profile Comparison for Select Conditions
| Therapy Type | Condition | Common Side Effects | Serious Adverse Events | Discontinuation Due to Side Effects |
|---|---|---|---|---|
| Pharmacological (Benzodiazepines) | Insomnia | Sedation, dizziness, memory impairment | Dependency, withdrawal seizures | OR 1.79 vs. placebo [75] |
| Pharmacological (Zopiclone) | Insomnia | Metallic taste, drowsiness, dry mouth | Complex sleep behaviors, dependency | OR 2.00 vs. placebo [75] |
| Pharmacological (SSRIs) | Depression | Nausea, sexual dysfunction, weight gain | Increased suicidal ideation | 5-15% in clinical trials [73] |
| Bioelectronic (VNS) | Rheumatoid Arthritis | Hoarseness, cough, implantation site pain | Surgical risks (infection, nerve injury) | Low (device adjustable/removable) [3] [7] |
| Bioelectronic (DBS) | Parkinson's Disease | Paresthesia, speech disturbance, balance issues | Intracranial hemorrhage, device infection | 3-10% in long-term studies |
For insomnia treatments, a network meta-analysis of 154 randomized controlled trials with 44,089 participants found that benzodiazepines, eszopiclone, zolpidem, and zopiclone were consistently associated with more side effects than placebo (OR range: 1.27–2.78) [75]. Zopiclone and zolpidem specifically caused significantly more dropouts due to adverse events than placebo (OR 2.00 and 1.79, respectively) [75]. These systemic side effects contrast with the more localized and manageable adverse events associated with bioelectronic approaches.
Methodologies for Safety Assessment in Bioelectronic Medicine Research
Preclinical Models for Efficacy and Safety Evaluation
Preclinical research in bioelectronic medicine utilizes established disease models to elucidate neural circuits and assess therapeutic safety:
Inflammatory Disease Models:
- Endotoxemia Model: Administration of bacterial lipopolysaccharide (LPS) to induce systemic inflammation, followed by VNS to measure suppression of TNF and other pro-inflammatory cytokines [7].
- Collagen-Induced Arthritis (CIA) Model: Standard model for rheumatoid arthritis used to demonstrate VNS efficacy in reducing joint inflammation and damage [7].
- Dextran Sodium Sulfate (DSS) Colitis Model: Inflammatory bowel disease model used to evaluate VNS effects on intestinal inflammation [7].
Safety-Specific Methodologies:
- Neural Pathway Mapping: Anatomical and functional tracing studies (e.g., transsynaptic tracing) to identify connected neural structures and potential off-target pathways [7].
- Stimulation Parameter Titration: Systematic evaluation of stimulation intensity, frequency, and duration to identify therapeutic windows that avoid nerve damage or excessive activation [1].
- Chronic Implantation Studies: Long-term assessment of tissue response to electrodes and implants, evaluating foreign body reaction and structural integrity [1].
Clinical Translation and Safety Monitoring
Clinical trials of bioelectronic therapies employ specialized assessment protocols:
- Blinded Sham-Controlled Designs: For VNS studies, implantable devices are activated in only the treatment group, with both groups undergoing identical implantation procedures to control for placebo effects [7].
- Stimulation Titration Phase: Gradual optimization of stimulation parameters to maximize efficacy while minimizing side effects like voice changes (for cervical VNS) or muscle contractions [7].
- Long-Term Safety Follow-Up: Post-market surveillance to monitor device performance, structural integrity, and chronic tissue response [1].
Signaling Pathways in Bioelectronic Medicine
The inflammatory reflex represents the most thoroughly characterized neuro-immune pathway targeted by bioelectronic medicine. The following diagram illustrates this key regulatory circuit:
Figure 1: Inflammatory Reflex Pathway Targeted by Vagus Nerve Stimulation
This pathway demonstrates the precise cellular specificity achievable through bioelectronic modulation, contrasting with the broad systemic action of pharmacological immunosuppressants that affect immune cells throughout the body.
Experimental Workflow for Bioelectronic Safety Research
The following diagram outlines a standardized research methodology for evaluating the safety and efficacy of bioelectronic therapies:
Figure 2: Bioelectronic Therapy Development Workflow
Essential Research Reagents and Materials
Table 3: Key Research Reagents for Bioelectronic Medicine Investigations
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Multielectrode Arrays | Neural signal recording and stimulation | Flexible, stretchable electrodes; conducting polymer-coated electrodes |
| Neural Tracers | Mapping neural connectivity | Anterograde/retrograde viral tracers (PRV, AAV) |
| Specific Receptor Agonists/Antagonists | Mechanism validation | α7nAChR agonists (e.g., GTS-21), α7nAChR antagonists (e.g., α-bungarotoxin) |
| Cytokine Assays | Monitoring immune responses | ELISA, multiplex bead arrays for TNF, IL-1β, IL-6 |
| Animal Disease Models | Therapeutic efficacy assessment | Collagen-induced arthritis, DSS colitis, LPS inflammation models |
| Immunohistochemistry Reagents | Tissue analysis and localization | Antibodies for neuronal markers (c-Fos, ChAT) and immune cell markers (CD68, CD3) |
Bioelectronic medicine presents a fundamentally different safety paradigm compared to systemic drug therapies. While pharmaceutical approaches will continue to play a crucial role in medical treatment, bioelectronic approaches offer a promising alternative with more localized side effects, reduced systemic toxicity, and the advantage of tunable, reversible intervention. The documented safety profiles across multiple therapeutic areas suggest that bioelectronic medicine may offer particular value for patients requiring chronic therapy, those with medication sensitivities or contraindications, and conditions where precise temporal control of therapeutic effects is critical. As the field advances with improved electrode materials, miniaturization, and more sophisticated neural interface technologies, the therapeutic window of bioelectronic treatments is expected to widen further, potentially establishing neuromodulation as a first-line intervention for an expanding range of conditions.
Bioelectronic Medicine (BEM) represents a paradigm shift in therapeutic interventions, using miniaturized electronic devices to interface with electrically active tissues and modulate neural circuits for treating disease [4] [1]. Unlike traditional pharmaceuticals which often cause systemic side effects, BEM offers targeted, precise modulation of specific physiological functions [4]. This emerging field promises not only clinical advantages but also distinct economic benefits that warrant rigorous evaluation. The economic assessment of BEM technologies requires specialized methodologies that account for their unique characteristics: high initial investment costs coupled with potential long-term durability, reduced need for continuous drug administration, and possibilities for personalized, adaptive therapy [1]. This guide provides a comprehensive framework for conducting cost-benefit analyses and evaluating the healthcare system impact of bioelectronic medicine technologies, equipping researchers and health economists with the necessary tools for robust economic assessment.
Key Economic Concepts and Methodologies
Core Health Economic Evaluation Frameworks
Economic evaluations of BEM interventions typically employ several established methodologies. Cost-effectiveness analysis (CEA) measures costs relative to health outcomes, typically expressed as cost per quality-adjusted life-year (QALY) gained [76]. Cost-benefit analysis (CBA) monetizes health benefits to compare directly with costs. Budget impact analysis (BIA) assesses the financial consequence of adoption within a specific healthcare budget. For BEM, these frameworks must be adapted to account for device durability, replacement cycles, and unique complication profiles distinct from pharmaceutical counterparts.
The Markov model represents a particularly valuable methodology for modeling chronic conditions treated with BEM. This approach simulates disease progression through various health states over time, incorporating probabilities of transitions between states (e.g., improvement, deterioration, relapse, withdrawal from treatment) [76]. Each health state is assigned specific costs and quality-of-life weights, allowing for projection of long-term costs and outcomes. For example, in evaluating BEM for multiple sclerosis, health states might be defined by Expanded Disability Status Scale (EDSS) scores, with transitions between states modeled annually [76].
BEM-Specific Economic Considerations
Economic evaluations of BEM must incorporate several distinctive factors. Device Longevity and Replacement Costs: Unlike pharmaceuticals with continuous dosing, BEM devices may function for years before requiring replacement [4]. Models must account for implantation procedures, device lifespan, and replacement surgeries. Dynamic Therapeutic Optimization: BEM devices can be reprogrammed and optimized without additional hardware costs, creating economic value through improved outcomes over time [1]. Closed-Loop System Economics: Advanced BEM systems with closed-loop capabilities (automatic adjustment based on physiological signals) may command premium pricing but offer superior outcomes through real-time adaptation [10].
Table 1: Key Input Parameters for BEM Economic Models
| Parameter Category | Specific Parameters | Data Sources |
|---|---|---|
| Device Costs | Initial implantation cost, Device unit cost, Replacement cost, Reprogramming visits | Manufacturer pricing, Hospital cost accounting, Procedural codes |
| Clinical Outcomes | Treatment efficacy, Disease progression rates, Relapse rates, Adverse event probabilities | Clinical trials, Registry studies, Real-world evidence |
| Healthcare Utilization | Medication use, Hospitalizations, Outpatient visits, Emergency department visits | Claims data, Clinical studies, Expert opinion |
| Patient-Related | Quality of life weights, Productivity losses, Transportation costs | Patient surveys, Health state utilities, Labor statistics |
Case Study: Cost-Effectiveness Analysis of a Bioelectronic Implant for Multiple Sclerosis
A 2021 study provides a pioneering model for BEM economic evaluation, analyzing the cost-effectiveness of "Optoferon," a novel bioelectronic cell-based implant for controlled release of beta-interferon in multiple sclerosis (MS) patients [76]. The study compared this bioelectronic approach against standard injectable IFNβ1a (Avonex) using a Markov model with a 9-year time horizon from the Dutch societal perspective [76].
The model simulated a cohort of 1,000 Dutch patients with relapsing-remitting MS, with a mean starting age of 35 years and a 3:1 female-to-male ratio [76]. Health states were defined by EDSS scores (0-9), with patients able to transition between states annually, experience relapses, or withdraw from treatment to best supportive care [76]. The analysis applied annual discount rates of 4% for costs and 1.5% for health effects, in accordance with Dutch economic guidelines [76].
Key Assumptions and Input Parameters
The model incorporated several BEM-specific parameters. The Optoferon device was assumed to be implanted in a daycare setting and replaced every 3 years due to potential scar tissue formation with reimplantation [76]. While base-case analysis assumed equal disability progression and adverse event probabilities between Optoferon and Avonex, it incorporated two key differential assumptions: (1) reduced annual relapse rates for Optoferon, and (2) lower annual withdrawal rates for the implantable device compared to injectable therapy [76]. These assumptions reflect potential benefits of improved adherence and consistent drug delivery with implantable BEM technologies.
Table 2: Cost-Effectiveness Results for Optoferon vs. Avonex (Base-Case Analysis)
| Parameter | Optoferon | Avonex | Incremental Difference |
|---|---|---|---|
| Total Costs (9 years) | € | € | -€26,966 (Cost saving) |
| Total QALYs | +0.45 QALYs | ||
| Relapse Rates | Reduced | Baseline | Favors Optoferon |
| Withdrawal Rates | Reduced | Baseline | Favors Optoferon |
| ICER | Dominant strategy (cost-saving and more effective) |
Results and Sensitivity Analysis
The base-case analysis found Optoferon to be a dominant strategy, providing both cost savings (-€26,966) and health gains (0.45 QALYs) compared to injectable Avonex over the 9-year time horizon [76]. A primary driver of cost differences was the acquisition cost of Optoferon being 2.5 times lower than Avonex [76]. Sensitivity analysis revealed that the incremental cost-effectiveness ratio was most sensitive to variations in: (1) annual acquisition costs of Avonex, (2) annual withdrawal rates for both treatments, and (3) disability progression rates with Avonex [76]. Value of information analysis indicated that further research to reduce parameter uncertainty could be economically justified.
Experimental Framework for BEM Economic and Clinical Evaluation
Core Methodological Approach
Robust economic evaluation of BEM requires integration of clinical and economic data collection throughout the development lifecycle. The fundamental methodology centers on prospective economic evaluation alongside clinical trials, with extension through modeling to capture long-term value. For early-stage BEM technologies, iterative cost-effectiveness modeling (headroom analysis) informs target product profiles and development decisions [76]. Pivotal trials should incorporate detailed resource utilization tracking, patient-reported outcomes, and health state utility measures suitable for economic evaluation.
The experimental workflow for comprehensive BEM assessment involves parallel tracking of clinical efficacy, safety, resource utilization, and patient-reported outcomes throughout the study period. Economic data collection must capture both direct medical costs (device, implantation, follow-up, medications, management of adverse events) and indirect costs (productivity losses, transportation, caregiver time) [76]. For BEM technologies with learning curve effects (clinician experience with implantation), economic evaluations should account for potential improvements in efficiency and reductions in procedure time over the evaluation period.
The Scientist's Toolkit: Essential Reagents and Materials for BEM Research
Table 3: Key Research Reagent Solutions for Bioelectronic Medicine Development
| Reagent/Material | Function | Application in BEM |
|---|---|---|
| Conducting Polymers | Mixed ionic/electronic conductivity, mechanical flexibility, enhanced biocompatibility | Electrode coating to reduce impedance, allow miniaturization, improve safety and decrease energy consumption [1] |
| Soft/Stretchable Materials | Bridge mechanical mismatch with biological tissue, reduce foreign body reaction | Flexible electrodes that wrap around nerves, conform to organs, minimize inflammation and fibrosis [4] [1] |
| Genetically Programmed Cells | Controlled therapeutic protein release in response to external stimuli | Cell-based implants for optogenetic-controlled drug delivery (e.g., IFN-β1a for MS) [76] |
| Biocompatible Encapsulants | Hermetic protection of electronics from bodily fluids, maintaining biostability | Long-term functional integrity of implantable pulse generators and electronics (5-10 years) [1] |
| Wireless Power Transfer Systems | Battery-less operation through inductive, ultrasonic, or magneto-electric transfer | Miniaturized implants without battery replacement needs, improved environmental footprint [1] |
Signaling Pathways in Bioelectronic Medicine and Economic Implications
The economic value of BEM is fundamentally linked to its precise modulation of specific neurophysiological pathways. The cholinergic anti-inflammatory pathway represents a prime example, where vagus nerve stimulation activates the α7 nicotinic acetylcholine receptor (α7nAChR) on immune cells in the spleen, suppressing pro-inflammatory cytokine release [63]. This mechanism provides a direct electronic alternative to pharmaceutical immunomodulators, with potential economic benefits through reduced drug costs and side effect management.
Different BEM approaches target distinct neural pathways with varying economic considerations. Vagus nerve stimulation modulates inflammatory responses through the neuro-immune reflex, potentially treating conditions like rheumatoid arthritis and inflammatory bowel disease [63]. Spinal cord stimulation primarily targets pain pathways through segmental inhibition in the dorsal horn and activation of descending inhibitory pathways [63]. Deep brain stimulation modulates pathological neural circuits in movement and psychiatric disorders [63]. Each pathway presents unique value propositions based on the cost of alternative treatments, patient population size, and current therapeutic limitations.
Healthcare System Impact and Broader Economic Considerations
Budget Impact and System Integration
The adoption of BEM technologies carries significant implications for healthcare system planning and resource allocation. While potentially offering long-term cost savings, BEM typically requires substantial upfront investment in specialized equipment, clinician training, and infrastructure. Healthcare systems must evaluate capacity requirements for implantation procedures, postoperative management, and device programming. The economic evaluation should account for workflow implications and potential need for multidisciplinary teams including neurologists, surgeons, and programming specialists.
BEM offers potential economic advantages through reduced environmental impact compared to continuous pharmaceutical manufacturing [1]. Battery-free devices or those with long-lasting power sources minimize medical waste, while some emerging bioresorbable materials safely dissolve in the body over time, eliminating explantation surgeries [4]. These environmental benefits represent important societal economic considerations beyond direct healthcare costs.
Value-Based Pricing and Reimbursement Strategies
Establishing appropriate reimbursement mechanisms represents a critical challenge for BEM technologies. Traditional fee-for-service models may not adequately capture the comprehensive value of these interventions, particularly their potential to reduce long-term medication use and disease complications. Risk-sharing agreements between manufacturers and payers can help align financial incentives with clinical outcomes, particularly for novel BEM approaches with evolving evidence bases.
Economic evaluations should incorporate broader societal perspectives including productivity gains from improved patient functioning, reduced caregiver burden, and transportation cost savings [76]. For working-age patients with chronic conditions, the ability to maintain employment may represent a significant economic benefit not captured in traditional healthcare sector analyses. These broader impacts strengthen the value proposition for BEM technologies despite potentially higher initial device costs.
Bioelectronic Medicine represents not only a therapeutic innovation but a potential economic disruptor in healthcare. The unique characteristics of BEM – including targeted therapy, adaptability, potential durability, and reduced pharmaceutical dependence – necessitate specialized economic evaluation frameworks that capture both short-term costs and long-term value. The case study of Optoferon for multiple sclerosis demonstrates that under appropriate conditions, BEM approaches can offer dominant economic value through both cost savings and improved health outcomes [76].
Future economic assessments must evolve alongside BEM technological advancements. Next-generation systems incorporating closed-loop feedback mechanisms and non-invasive approaches present new economic considerations [10]. The emergence of soft, flexible bioelectronics may improve long-term reliability and reduce complication-related costs [4]. As the field progresses toward multimodal devices combining stimulation, recording, and drug delivery capabilities, economic evaluations must account for these integrated benefits [1]. Robust economic evidence will be essential to guide appropriate adoption, reimbursement, and continued innovation in this promising therapeutic domain.
The regulatory landscape for medical products in the United States is a structured framework designed to ensure safety and efficacy while fostering innovation. For researchers in bioelectronic medicine—a field that uses electrical signals to diagnose and treat disease—navigating this landscape is essential for translating laboratory discoveries into clinical therapies [10] [15]. The U.S. Food and Drug Administration (FDA) oversees this process through a combination of regulations, guidance documents, and approval pathways. The centerpiece of human subjects research regulation is the Good Clinical Practice (GCP) standards, which provide a unified ethical and scientific quality standard for clinical trials [77]. These regulations govern the entire lifecycle of medical product development, from initial preclinical testing through post-market surveillance, ensuring that data from clinical trials is credible and that the rights, safety, and well-being of trial subjects are protected [78].
For the field of bioelectronic medicine, this regulatory framework applies to a diverse range of devices, from implantable neurostimulators for conditions like Parkinson's disease and epilepsy to non-invasive devices for depression and inflammatory disorders [10] [15]. The recent FDA approval of a bioelectronic device for rheumatoid arthritis, which targets the vagus nerve, underscores the field's transition from experimental concept to approved therapy and highlights the importance of understanding the regulatory process [3]. This guide provides a detailed analysis of the FDA approval processes and clinical trial methodologies essential for successfully bringing bioelectronic medicines to patients.
FDA Drug and Biological Product Approvals
The Novel Drug Approval Process
The FDA's Center for Drug Evaluation and Research (CDER) is responsible for approving novel drugs, defined as new drugs never before approved or marketed in the United States [79]. The approval process is rigorous, requiring sponsors to demonstrate substantial evidence of safety and effectiveness through adequate and well-controlled clinical investigations. The pathway typically involves several stages:
- Investigational New Drug (IND) Application: Before initiating clinical trials in humans, a sponsor must submit an IND application containing preclinical data, manufacturing information, and clinical trial protocols [77].
- Clinical Trial Phases: Sponsors conduct Phase 1 (safety), Phase 2 (efficacy and dosing), and Phase 3 (confirmatory) trials under the IND [77].
- New Drug Application (NDA) or Biologics License Application (BLA): For approval, sponsors submit an NDA or BLA containing all preclinical and clinical data, proposed labeling, and manufacturing details [80].
The FDA's "Novel Drug Approvals" website serves as the authoritative source for tracking these approvals, providing a comprehensive list of new molecular entities and new therapeutic biological products that CDER has approved [79] [80].
Recent Novel Drug Approvals (2025)
The following table summarizes select novel drug approvals from 2025, demonstrating the range of therapeutic areas and technological approaches in current medical product development. These approvals represent significant advancements in their respective fields, including oncology, rare diseases, and metabolic disorders.
Table 1: Select FDA Novel Drug Approvals in 2025
| Drug Name | Active Ingredient | Approval Date | FDA-Approved Use |
|---|---|---|---|
| Hyrnuo | sevabertinib | 11/19/2025 | Locally advanced or metastatic non-squamous non-small cell lung cancer with HER2 tyrosine kinase domain mutations [79] |
| Redemplo | plozasiran | 11/18/2025 | Reduce triglycerides in adults with familial chylomicronemia syndrome [79] |
| Komzifti | ziftomenib | 11/13/2025 | Adults with relapsed or refractory acute myeloid leukemia with NPM1 mutation [79] |
| Kygevvi | doxecitine and doxribtimine | 11/03/2025 | Thymidine kinase 2 deficiency in patients with symptom onset at age 12 or younger [79] |
| Lynkuet | elinzanetant | 10/24/2025 | Moderate-to-severe vasomotor symptoms due to menopause [79] |
| Jascayd | nerandomilast | 10/07/2025 | Idiopathic pulmonary fibrosis [79] |
| Rhapsido | remibrutinib | 09/30/2025 | Chronic spontaneous urticaria in adults who remain symptomatic despite H1 antihistamine treatment [79] |
| Modeyso | dordaviprone | 08/06/2025 | Diffuse midline glioma with H3 K27M mutation with progressive disease [79] |
| Tryptyr | acoltremon | 05/28/2025 | Signs and symptoms of dry eye disease [79] |
| Journavx | suzetrigine | 01/30/2025 | Moderate to severe acute pain [79] |
These approvals highlight several important trends in drug development, including the continued growth of targeted therapies in oncology (e.g., Hyrnuo, Komzifti), advances in the treatment of rare diseases (e.g., Kygevvi, Redemplo), and new options for chronic conditions (e.g., Rhapsido, Lynkuet). For bioelectronic medicine researchers, understanding these approval patterns provides context for the evolving therapeutic landscape and helps identify potential areas where device-based therapies may address unmet medical needs.
Clinical Trial Regulations and Methodologies
Good Clinical Practice (GCP) Regulations
The FDA's regulations governing the conduct of clinical trials are primarily contained in Title 21 of the Code of Federal Regulations (CFR). These regulations establish the foundation for human subject protection and clinical trial integrity in the United States [77]. Key regulatory sections include:
- Informed Consent (21 CFR Part 50): This regulation outlines the requirements for obtaining and documenting informed consent from human subjects, ensuring they are provided with all necessary information about the study to make an informed decision about participation. Specific provisions address additional safeguards for children in clinical investigations (Subpart D) and exceptions from informed consent requirements for certain emergency research [77].
- Institutional Review Boards (21 CFR Part 56): This section establishes the standards for the composition, operation, and responsibilities of IRBs, which are independent committees that review and approve research protocols to protect the rights and welfare of human subjects. Recent regulatory developments include requirements for IRB registration and provisions allowing IRB waiver or alteration of informed consent for minimal risk clinical investigations [77].
- Financial Disclosure (21 CFR Part 54): These regulations require clinical investigators to disclose financial interests and arrangements that could potentially introduce bias in the conduct or reporting of clinical studies, ensuring the integrity of clinical trial data [77].
- Investigational New Drug Application (21 CFR Part 312): This section governs the procedures and requirements for submitting INDs and conducting clinical investigations of drugs and biologics, including regulations for clinical holds, safety reporting, and disqualification of clinical investigators [77].
The FDA also maintains a Bioresearch Monitoring (BIMO) program, which conducts on-site inspections and data audits to monitor all aspects of the conduct and reporting of FDA-regulated research, ensuring compliance with these regulations [78].
Clinical Trial Methodologies and Protocol Development
Designing robust clinical trials requires meticulous methodology and protocol development. The fundamental elements of a scientifically sound clinical trial include:
- Clear Objectives and Endpoints: Precisely defined primary and secondary endpoints that directly measure the intervention's effect on the disease or condition.
- Appropriate Study Design: Selection of a design (e.g., randomized controlled, crossover, adaptive) that minimizes bias and provides valid statistical inference.
- Statistical Considerations: A pre-specified statistical analysis plan, including sample size calculations based on power analysis.
- Risk Management Plans: Procedures for identifying, monitoring, and addressing potential risks to study participants.
Specialized training programs, such as the one offered by the National Institute of Neurological Disorders and Stroke (NINDS) Clinical Trials Methodology Course (CTMC), provide researchers with comprehensive education in clinical trial design and conduct. The 2025 CTMC course structure illustrates the comprehensive approach required for protocol development:
Table 2: Clinical Trial Methodology Course Components (2025)
| Component | Timeline | Key Activities |
|---|---|---|
| Virtual Sessions | March - June 2025 | Biweekly webinars on clinical trials expertise; small group meetings for proposal development [81] |
| Residential Meeting | June 23-26, 2025 | Intensive in-person training in Charlottesville, VA; includes presentations, small group meetings, and one-on-one sessions [81] |
| Final Protocol Development | July 2025 onward | Completion of protocol synopsis; mock study sections for proposals preparing for external funding [81] |
For bioelectronic medicine trials, specific methodological considerations include device-specific blinding techniques, appropriate sham controls, device titration protocols, and specialized endpoint selection that captures both clinical outcomes and patient-reported experiences. The emerging field of closed-loop systems in bioelectronic medicine, where devices automatically adjust therapy based on physiological feedback, introduces additional methodological complexities related to algorithm validation and adaptive trial designs [10].
Bioelectronic Medicine: Regulatory Pathways and Applications
Unique Regulatory Considerations for Bioelectronic Medicine
Bioelectronic medicine presents distinct regulatory challenges that differ from both pharmaceutical products and conventional medical devices. These novel therapies, which interface directly with the nervous system to modulate physiological functions, often fall under the FDA's device regulatory pathway but may also be regulated as combination products when they incorporate drug components [77]. Key regulatory considerations for bioelectronic medicine include:
- Device Classification: Bioelectronic devices are typically regulated under the Premarket Approval (PMA) pathway for Class III devices or the 510(k) pathway for devices demonstrating substantial equivalence to existing predicates [77].
- Biocompatibility Testing: Assessment of how device materials interact with neural tissue, particularly for implantable systems designed for long-term use.
- Software Validation: Rigorous evaluation of the software algorithms that control stimulation parameters, especially for adaptive "closed-loop" systems that automatically adjust therapy based on physiological signals [10].
- Non-Invasive Approaches: Recent advancements in non-invasive neuromodulation techniques, such as transcutaneous auricular vagus nerve stimulation (tVNS), present unique regulatory questions regarding dosing, targeting, and efficacy demonstration [10] [15].
The recent FDA approval of SetPoint Medical's bioelectronic device for rheumatoid arthritis, which uses vagus nerve stimulation to modulate inflammatory responses, represents a significant regulatory milestone for the field and provides a precedent for future devices targeting immune and inflammatory conditions [3].
Research and Development Toolkit for Bioelectronic Medicine
The multidisciplinary nature of bioelectronic medicine requires researchers to utilize a diverse array of specialized tools and methodologies. The following table outlines essential components of the research toolkit for developing and testing bioelectronic therapies:
Table 3: Research Toolkit for Bioelectronic Medicine
| Tool/Technique | Function/Application | Regulatory Considerations |
|---|---|---|
| Neural Interfaces | Record from or stimulate neural tissue; range from microelectrode arrays to cuff electrodes [15] | Biocompatibility (ISO 10993), material safety, electrical safety (IEC 60601) |
| Autonomic Neurography (ANG) | Objectively measure nerve activity to stratify patients and guide treatment parameters [10] | Device classification (typically II), analytical validation |
| Closed-Loop Systems | Automatically adjust stimulation parameters based on real-time physiological feedback [10] | Algorithm validation, cybersecurity, human factors engineering |
| Non-Invasive Neuromodulation | Modulate neural activity without implantation (e.g., tVNS, TMS) [10] [15] | Dosing determination, targeting verification, safety monitoring |
| Biomarker Assays | Measure molecular or physiological changes resulting from neuromodulation (e.g., cytokine levels) [10] | Analytical validation, clinical validation for specific contexts of use |
The development pathway for bioelectronic medicines typically proceeds from basic research understanding neural circuits, to device engineering creating the interface technology, preclinical validation in animal models, and finally clinical trials in human patients [10] [15]. Throughout this process, researchers should engage early with FDA through the Q-Submission Program to obtain feedback on proposed development plans and regulatory requirements.
Visualizing Regulatory Pathways and Methodologies
FDA Regulatory Pathway for Bioelectronic Devices
The following diagram illustrates the key stages in the regulatory pathway for bioelectronic medicine devices, from initial concept through post-market surveillance:
Clinical Trial Development Workflow
This diagram outlines the key methodological stages in developing and conducting a clinical trial for a bioelectronic medicine, highlighting the integration of regulatory requirements at each phase:
The regulatory landscape for FDA approvals and clinical trial methodologies represents a dynamic framework that balances innovation with patient safety. For researchers in bioelectronic medicine, successfully navigating this landscape requires a comprehensive understanding of both device regulations and clinical trial methodologies. The field stands at a transformative moment, with advances in non-invasive neuromodulation, closed-loop systems, and novel neural interfaces creating new therapeutic possibilities for conditions ranging from inflammatory diseases to mental health disorders [10]. As these technologies evolve, regulatory science must similarly advance to create efficient pathways that enable safe and effective bioelectronic therapies to reach patients in need. By integrating rigorous scientific methodology with regulatory compliance from the earliest stages of development, researchers can accelerate the translation of bioelectronic discoveries into approved therapies that address unmet medical needs.
Bioelectronic medicine (BEM) is an emerging multidisciplinary field that uses implantable or wearable electronic devices to interface with electrically active tissues for therapeutic purposes [70]. This approach represents a paradigm shift from conventional pharmacology, moving from broad-spectrum chemical interventions to precise, targeted modulation of neural circuits and organ function [43]. The field has evolved from foundational applications like cardiac pacemakers (first implanted in 1958) and cochlear implants (1961) to advanced neuromodulation therapies for neurological, inflammatory, and metabolic disorders [70] [4]. The global BEM market is experiencing significant growth, driven by technological advancements, increasing prevalence of chronic diseases, and growing physician acceptance of neuromodulation as a viable therapeutic modality [8] [82].
This growth trajectory is supported by substantial market validation. The global bioelectronic medicine market was valued between USD 23.54 billion and USD 25.9 billion in 2024-2025, with projections indicating expansion to approximately USD 33.59 billion to USD 47.28 billion by 2030-2034, representing a compound annual growth rate (CAGR) of 6.10% to 7.12% [8] [82] [71]. This robust growth underscores the accelerating adoption of bioelectronic therapies across clinical specialties and healthcare systems worldwide.
Market Growth Trajectory: Quantitative Analysis
The bioelectronic medicine market demonstrates consistent global expansion across all segments, fueled by technological innovation and clinical demand. The following tables summarize key market metrics and regional growth patterns.
Table 1: Global Bioelectronic Medicine Market Size and Growth Projections
| Metric | 2024-2025 Value | 2030-2035 Projection | CAGR | Source |
|---|---|---|---|---|
| Global Market Value | USD 23.54 Billion (2024) | USD 33.59 Billion (2030) | 6.10% | [8] |
| Global Market Value | USD 25.48 Billion (2025) | USD 47.28 Billion (2034) | 7.12% | [82] |
| Global Market Value | USD 25.9 Billion (2025) | USD 46.8 Billion (2035) | 6.1% | [71] |
| U.S. Market Value | USD 6.85 Billion (2025) | USD 13.42 Billion (2034) | 7.77% | [82] |
Table 2: Growth Rates by Country/Region (2025-2035 Projections)
| Country/Region | Projected CAGR | Key Growth Drivers |
|---|---|---|
| China | 8.2% | Rapid industrial growth, technology adoption, healthcare investment |
| India | 7.6% | Growing healthcare infrastructure, large patient population |
| Germany | 7.0% | Strong industrial standards, innovation focus |
| United States | 5.2%-7.77% | Advanced healthcare infrastructure, high chronic disease prevalence, strong R&D investment |
| North America (Overall) | - | 38.14% market share (2024), developed infrastructure, favorable reimbursement |
| Asia-Pacific | - | Fastest growing region, aging population, rising chronic diseases |
Market growth is primarily driven by the increasing global burden of chronic diseases, with cardiovascular diseases accounting for approximately 17.9 million deaths annually worldwide, and diabetes affecting 537 million adults in 2021 (projected to reach 643 million by 2030) [8]. The aging global population further accelerates this trend, with one in six individuals expected to be over age 65 by 2050, creating greater demand for chronic disease management solutions [8].
Technological Advancements Driving Adoption
Device Innovation and Miniaturization
The evolution of bioelectronic devices toward smaller, smarter, and more patient-friendly form factors is significantly enhancing their clinical adoption. Key innovations include:
- Ultra-miniaturized implants: Devices like Nalu Medical's implantable pulse generator, which is 27 times smaller than traditional neurostimulators, enable less invasive implantation procedures and improved patient comfort [61].
- Battery-free devices: Wireless powering techniques using inductive/electrical coupling or ultrasound energy transfer eliminate the need for battery replacements and facilitate further miniaturization [70].
- Soft and flexible bioelectronics: The shift from rigid materials to flexible, stretchable interfaces using conducting polymers, graphene, and hydrogels reduces mechanical mismatch with biological tissues, minimizing inflammation and improving long-term signal stability [4] [83].
AI Integration and Closed-Loop Systems
Artificial intelligence is transforming bioelectronic devices from static stimulators to adaptive therapeutic systems:
- Personalized stimulation parameters: Machine learning algorithms analyze patient-specific neural and physiological data to optimize stimulation parameters in real-time, improving efficacy while reducing side effects [82] [61].
- Closed-loop therapies: Devices like responsive neurostimulation (RNS) systems for epilepsy can detect abnormal brain activity and deliver stimulation only when needed, representing a significant advancement over open-loop continuous stimulation [43] [84].
- Predictive analytics: AI-enabled devices can identify patterns preceding clinical events (e.g., epileptic seizures), enabling preemptive intervention and fundamentally changing disease management paradigms [61].
Enhanced Neural Interfaces
Improvements in neural interface technology are critical for achieving precise neuromodulation:
- Multi-electrode arrays: Advanced cuff electrodes with multiple contacts enable selective targeting of specific nerve fascicles, improving therapeutic precision while reducing off-target effects [83].
- Novel electrode materials: Conducting polymers offer mixed ionic/electronic conductivity, reduced impedance, and enhanced biocompatibility compared to traditional metal electrodes [70].
- Bidirectional communication: Modern implants combine stimulation capabilities with recording functionality, creating feedback loops for automated therapy adjustment [70].
Physician Acceptance and Clinical Integration
Current Adoption Trends Across Specialties
Physician acceptance of bioelectronic medicine varies by specialty but is generally increasing as clinical evidence accumulates:
- Neurology and Neurosurgery: Deep brain stimulation for Parkinson's disease (approved by FDA in 1997) and essential tremor has established strong clinical acceptance among movement disorder specialists [43]. Vagus nerve stimulation for epilepsy and treatment-resistant depression has gained traction over the past two decades [43].
- Pain Medicine: Spinal cord stimulation has become a well-accepted modality for chronic pain management, with the SCS market valued at $2.92 billion in 2023 [70].
- Cardiology: Implantable cardioverter defibrillators and pacemakers represent the most established bioelectronic therapies, with continuous innovation (e.g., leadless pacemakers) maintaining physician confidence [8] [71].
- Otolaryngology: Cochlear implants have transformed profound hearing loss treatment, with ongoing innovation improving outcomes [8] [70].
- Rheumatology and Immunology: Emerging applications for inflammatory conditions like rheumatoid arthritis and Crohn's disease are gaining attention, with clinical trials demonstrating vagus nerve stimulation can reduce inflammatory cytokines [43].
Key Factors Influencing Physician Adoption
Several critical factors determine the rate of physician acceptance across specialties:
- Clinical Evidence Base: Robust, randomized controlled trial data remains the primary driver of physician adoption. The 5.7 hours per night usage rate reported by Inspire Medical for sleep apnea treatment provides tangible evidence of patient compliance superior to CPAP [84].
- Reimbursement Pathways: Clear reimbursement frameworks are essential for widespread adoption. As noted at the 2025 Bioelectronic Medicine Forum, the bankruptcy of Pear Therapeutics despite its $1.6 billion valuation highlights how reimbursement challenges can derail promising technologies [84].
- Specialized Training Programs: As Ray Cohen, whose leadership at Axonics culminated in a record-breaking acquisition by Boston Scientific, emphasized: understanding patient experiences before engaging physicians is critical for adoption [84].
- Device Reliability and Safety: Long-term device performance significantly impacts physician confidence. Reliability (consistent function without failure), stability (resistance to biological environmental fluctuations), durability (physical resilience), and longevity (operational lifespan) represent distinct performance aspects that clinicians evaluate [4].
Experimental Protocols and Methodologies
Preclinical Development Workflow
The development of bioelectronic therapies follows a structured preclinical pathway to establish safety and efficacy before human trials. The diagram below illustrates a generalized experimental workflow from target identification through regulatory approval.
Key Methodological Approaches
Chronic In Vivo Reliability Testing
Objective: Evaluate long-term device performance and tissue integration in relevant animal models [4].
Protocol:
- Surgical Implantation: Aseptic implantation of bioelectronic device (e.g., cuff electrode on target nerve) in anesthetized animals following institutionally approved protocols
- Stimulation Parameter Optimization: Determine threshold and suprathreshold stimulation parameters while monitoring physiological responses
- Long-Term Monitoring: Periodic assessment of device functionality and tissue response over 4-12 weeks
- Endpoint Analysis: Histological evaluation of tissue integration and foreign body response; electrochemical analysis of electrode integrity
Outcome Measures:
- Stimulation threshold stability over time
- Electrochemical impedance spectroscopy measurements
- Histological scoring of inflammation and fibrosis
- Functional efficacy in disease model
Closed-Loop System Validation
Objective: Verify automated detection and response capabilities in disease models [70] [43].
Protocol:
- Biomarker Identification: Characterize electrophysiological signatures preceding clinical events (e.g., epileptiform activity before seizures)
- Algorithm Development: Train detection algorithms on annotated electrophysiological datasets
- System Integration: Implement detection algorithm on implantable processor with predefined stimulation response
- In Vivo Validation: Test closed-loop system in relevant animal models, comparing to sham stimulation or open-loop controls
Outcome Measures:
- Detection sensitivity and specificity for target events
- Latency from detection to therapeutic stimulation
- Efficacy in preventing or aborting clinical events
- False positive rate and associated side effects
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Bioelectronic Medicine Development
| Research Tool Category | Specific Examples | Research Application |
|---|---|---|
| Electrode Materials | Conducting polymers (PEDOT:PSS), Platinum-iridium, Graphene, MXenes | Neural interface fabrication, Signal recording and stimulation |
| Encapsulation Materials | Parylene-C, Silicon rubber, Polyimide, Bioresorbable polymers | Device protection from biological fluids, Biocompatibility enhancement |
| Characterization Equipment | Electrochemical impedance spectroscope, Cyclic voltammetry apparatus, Atomic force microscope | Material property analysis, Interface characterization |
| In Vitro Test Systems | Multi-electrode arrays, Cell culture models, 3D tissue constructs | Preliminary biocompatibility testing, Mechanism investigation |
| Animal Models | Rodent neuroinflammatory models, Large animal (porcine) surgical models, Disease-specific transgenic models | Safety and efficacy evaluation, Surgical technique development |
| Computational Tools | Finite element modeling software, Neural network simulators, Circuit design tools | Stimulation field prediction, Device optimization, Algorithm development |
Challenges and Future Directions
Barriers to Widespread Adoption
Despite promising growth, several significant challenges must be addressed to accelerate market adoption:
- High Device Costs and Reimbursement Limitations: Advanced implantable devices involve complex manufacturing processes and high R&D investments, resulting in substantial costs that limit accessibility in low- and middle-income countries [8]. Inconsistent reimbursement frameworks across regions further hinder adoption, with WHO data showing that out-of-pocket medical expenses push approximately 100 million people into extreme poverty annually [8].
- Regulatory Hurdles: As highlighted at the 2025 Bioelectronic Medicine Forum, regulatory bottlenecks remain challenging, particularly biocompatibility testing requirements and disruptions in pre-submission meetings with regulatory bodies [84].
- Technical Reliability Concerns: Long-term reliability of bioelectronic implants in dynamic biological environments presents ongoing challenges, including foreign body reaction, material degradation, and maintaining stable neural interfaces over multi-year timelines [4].
- Interdisciplinary Collaboration Gaps: As Lisa Shafer of Biogen noted, siloed mentalities separating pharmaceutical and medical device sectors have limited collaboration opportunities, with vagus nerve stimulation often absent from pharmaceutical competitive analyses despite its therapeutic potential [84].
Emerging Opportunities and Strategic Directions
The future growth of bioelectronic medicine will be shaped by several key developments:
- Expansion into New Therapeutic Areas: Research is advancing beyond neurological applications to include metabolic disorders (type 2 diabetes, obesity), autoimmune conditions (rheumatoid arthritis, inflammatory bowel disease), and cardiovascular diseases (hypertension) [43] [61].
- Sustainability-Focused Design: Growing emphasis on eco-friendly materials, energy-efficient devices, and battery-free systems that reduce environmental impact while improving patient outcomes [82] [4].
- Direct-to-Consumer Models: Emerging approaches like Spark Biomedical's OhmBody for menstrual symptoms represent a shift toward consumer-friendly bioelectronic solutions that may accelerate market penetration [84].
- Global Market Expansion: While North America currently dominates with 38.14% market share (2024), the Asia-Pacific region represents the fastest-growing market, creating opportunities for tailored devices and business models [82].
The bioelectronic medicine market is on a robust growth trajectory, with projections indicating substantial expansion through 2035. Physician acceptance is increasing across specialties, driven by accumulating clinical evidence, technological advancements in device miniaturization and intelligence, and expanding therapeutic applications. The convergence of materials science, artificial intelligence, and neuroscience is creating unprecedented opportunities for precise, personalized neuromodulation therapies that address limitations of conventional pharmaceuticals.
Successful market adoption will require addressing remaining challenges related to cost, reimbursement, regulatory pathways, and long-term device reliability. As the field matures, strategic focus on interdisciplinary collaboration, economic modeling, and patient-centric design will be essential to realizing the full potential of bioelectronic medicine to transform care for chronic neurological, inflammatory, and metabolic diseases. The ongoing shift from pharmaceutical-dominated treatment paradigms to integrated bioelectronic-pharmacological approaches represents a fundamental transformation in therapeutic strategy that will increasingly engage researchers, clinicians, and drug development professionals in the coming decade.
Bioelectronic Medicine (BEM) represents a transformative approach to treating disease by using implantable electronic devices to modulate the electrical activity of electrically excitable tissues, primarily the nervous system [1]. Unlike conventional pharmaceuticals that interact with biological targets through molecular pathways, BEM interfaces directly with the body's neural circuits to achieve therapeutic effects. This field has evolved from early applications like cardiac pacemakers and cochlear implants to increasingly sophisticated neuromodulation therapies for conditions ranging from Parkinson's disease to drug-resistant epilepsy [1]. The emerging integration of artificial intelligence (AI) with bioelectronic devices is now poised to address one of the field's most significant challenges: the lack of precision and personalization in stimulation protocols. Current approaches often require months of parameter adjustments and still yield variable response rates between 50-70% for therapies like vagus nerve stimulation (VNS) [85]. The convergence of AI, advanced biosensing, and closed-loop systems is creating a new generation of "intelligent" bioelectronic devices capable of adapting therapy in real-time based on individual patient physiology and disease state.
Current Landscape and the Need for AI-Enhanced Precision
Limitations of Conventional Bioelectronic Therapies
Traditional bioelectronic systems operate predominantly in an open-loop configuration with fixed stimulation parameters that cannot adapt to dynamic physiological states. This one-size-fits-all approach fails to account for inter-patient variability in nerve morphology, disease pathophysiology, and individual response patterns. For instance, in vagus nerve stimulation therapy, the complex fascicular organization of the vagus nerve means that fibers associated with side effects (such as those innervating the larynx and pharynx) respond more readily to stimulation than those mediating desirable therapeutic effects [85]. This morphological complexity creates a "curse of dimensionality" problem where the parameter space for optimization becomes prohibitively large for manual exploration [85]. The limitations extend beyond VNS to other neuromodulation approaches where fixed stimulation protocols cannot accommodate the dynamic nature of neurological conditions, inflammatory states, or cardiovascular diseases.
The Promise of AI-Driven Personalization
Artificial intelligence, particularly machine learning (ML) and reinforcement learning algorithms, offers powerful tools to navigate complex parameter spaces and identify optimal stimulation strategies for individual patients. AI can integrate multimodal data streams—including recorded neural signals, physiological biomarkers, clinical outcomes, and even omics data—to develop personalized stimulation protocols that maximize therapeutic efficacy while minimizing side effects [86] [87]. The application of AI in biomedical sciences has grown exponentially, with machine learning emerging as the most frequently reported model across various biomedical disciplines [86]. In bioelectronic medicine specifically, AI enables a shift from static, open-loop stimulation to dynamic, closed-loop systems that can adapt therapy based on real-time physiological feedback.
Table 1: Key Challenges in Conventional Bioelectronic Therapies and AI-Enhanced Solutions
| Challenge | Impact on Therapy | AI-Enhanced Solution |
|---|---|---|
| Inter-patient variability in nerve morphology | Highly variable treatment response; prolonged dosing periods | Patient-specific computational models; personalized parameter optimization |
| Complex multi-parameter optimization | Subtherapeutic stimulation or excessive side effects | Reinforcement learning to navigate parameter space efficiently |
| Dynamic disease states | Static stimulation protocols become suboptimal over time | Closed-loop systems with real-time adaptation based on biosensor data |
| Delayed therapeutic effects | Months to achieve optimal efficacy | Predictive biomarkers for early outcome prediction |
| Multimodal data integration | Incomplete understanding of stimulation effects | AI-powered integration of neural, physiological, and omics data |
AI Technologies Driving Personalized Stimulation Protocols
Machine Learning and Reinforcement Learning Approaches
Machine learning algorithms are being deployed across multiple dimensions of bioelectronic medicine to enhance personalization. Supervised learning models can predict optimal stimulation parameters based on patient characteristics and recorded neural responses. For example, Gaussian processes (GP) and parametric regression models have been used to analyze the relationship between VNS parameters and evoked compound action potentials (eCAPs), enabling more precise fiber-type recruitment [85]. Unsupervised learning approaches can identify patient subtypes that may respond differently to stimulation protocols, allowing for stratified therapy approaches.
Reinforcement learning (RL) represents a particularly powerful paradigm for bioelectronic medicine, as it mimics the iterative dose-finding approach used by physicians. In an exemplary implementation, researchers at UC Santa Cruz developed a wearable wound healing device called "a-Heal" that uses an RL model the researchers termed the "AI physician" [88]. This system continuously images the wound, assesses the healing stage through machine learning, and automatically adjusts the delivery of either medication or electric field stimulation to optimize the healing trajectory. The RL model is designed with the goal of minimizing time to wound closure and is "rewarded" for making progress toward that goal, continually learning from the patient and adapting its treatment approach [88]. Preclinical tests demonstrated that this AI-driven closed-loop system accelerated healing by approximately 25% compared to standard care [88].
Deep Learning for Neural Signal Interpretation and Biomarker Discovery
Deep learning algorithms, particularly convolutional neural networks (CNNs) and recurrent neural networks, are enabling sophisticated analysis of complex neural and physiological signals. These approaches can identify subtle patterns in recorded neural activity that serve as biomarkers for specific physiological states or disease conditions. In cardiac bioelectronics, deep learning algorithms have been applied to electrocardiogram (ECG) and photoplethysmography (PPG) signals to enhance disease detection and guide therapy [89]. Similarly, in VNS, deep learning models can interpret recorded evoked compound action potentials (eCAPs) to characterize fiber recruitment patterns and predict physiological effects [85].
The integration of AI with bioelectronic devices has also facilitated the discovery of novel neural biomarkers for therapy personalization. For instance, researchers have used signal processing and Gaussian process models to establish relationships between specific eCAP signatures and short-term physiological responses to VNS, including cardiac and respiratory effects [85]. These neural biomarkers can then be used as proxies for therapeutic effects during dosing procedures, allowing for more efficient parameter optimization without repeatedly assessing clinical outcomes.
Table 2: AI Approaches in Bioelectronic Medicine and Their Applications
| AI Technology | Key Characteristics | Bioelectronic Application Examples |
|---|---|---|
| Reinforcement Learning | Learns optimal strategies through trial-and-error; rewards progress toward goals | "AI physician" for wound healing [88]; adaptive neuromodulation parameters |
| Deep Learning Networks | Identifies complex patterns in high-dimensional data; feature hierarchy learning | Neural signal classification [89]; physiological response prediction [85] |
| Gaussian Processes | Probabilistic models; uncertainty quantification | Modeling neural response to stimulation parameters [85] |
| Convolutional Neural Networks | Spatial hierarchy in data processing; translation invariance | Image-based assessment of healing progression [88]; ECG signal analysis [89] |
| Random Forest | Ensemble learning; handles mixed data types | Predictive modeling of immunotherapy response [90]; appendicitis diagnosis [87] |
Technical Implementation of AI-Enhanced Stimulation Protocols
Experimental Methodologies for AI-Bioelectronic Integration
The development of AI-enhanced stimulation protocols requires rigorous experimental methodologies that integrate computational modeling with empirical validation. A representative methodology for establishing personalized VNS parameters, as detailed in recent research, involves several key stages [85]:
Surgical Preparation and Neural Interface Implementation: Studies conducted in anesthetized swine (chosen for their morphological similarity to human vagus nerves) involve the implantation of multi-electrode arrays on the cervical vagus nerve. These arrays typically include both stimulating and recording electrodes to enable simultaneous stimulation and recording of evoked compound action potentials (eCAPs).
Comprehensive Parameter Space Exploration: Researchers systematically explore a wide range of stimulation parameters, including pulse width (10-500 μs), frequency (1-100 Hz), current amplitude (0.1-3.0 mA), and waveform shapes. This broad parameter exploration is essential for building comprehensive models of the input-output relationship between stimulation parameters and neural/physiological responses.
Multimodal Data Acquisition: During stimulation, multiple data streams are recorded simultaneously: (1) neural signals (eCAPs) from the recording electrodes on the vagus nerve; (2) physiological responses including ECG, respiratory rate, and laryngeal electromyography; (3) stimulation parameters for precise correlation.
Computational Modeling and Biomarker Identification: The acquired data is processed using signal processing techniques to extract features from eCAPs and physiological responses. Gaussian processes and parametric regression models are then used to establish relationships between stimulation parameters, eCAP features, and physiological effects. This modeling identifies specific eCAP biomarkers that predict desired therapeutic responses (e.g., heart rate modulation) or unwanted side effects.
Validation and Closed-Loop Implementation: The identified biomarkers and models are validated through additional stimulation experiments. Finally, closed-loop algorithms are implemented that use these real-time neural biomarkers to automatically adjust stimulation parameters to maintain therapeutic effects while minimizing side effects.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for AI-Enhanced Bioelectronic Research
| Item | Function | Technical Specifications |
|---|---|---|
| Multi-electrode Arrays | Neural recording and stimulation | Multiple contacts (≥8); flexible substrates; PtIr or conducting polymer electrodes [85] |
| Wireless Biosensing Modules | Physiological signal acquisition | ECG, respiratory, EMG capabilities; wireless data transmission [1] |
| Programmable Stimulation Hardware | Precise parameter control | Current- or voltage-controlled; wide parameter ranges (pulse width: 10-1000μs; frequency: 0.1-200Hz) [85] |
| Signal Processing Software | Neural feature extraction | eCAP analysis; noise filtering; feature classification algorithms [85] |
| Machine Learning Frameworks | AI model development | TensorFlow, PyTorch; support for reinforcement learning [88] |
| Biocompatible Encapsulation Materials | Device protection and biocompatibility | Parylene-C, silicone; flexible, moisture-resistant coatings [1] |
| Conducting Polymer Electrodes | Improved neural interface | PEDOT:PSS; lower impedance; enhanced biocompatibility [1] |
Signaling Pathways and Neural Circuits for Targeted Stimulation
The efficacy of personalized stimulation protocols depends fundamentally on understanding the neural pathways and signaling mechanisms through which bioelectronic stimulation produces therapeutic effects. The vagus nerve serves as a particularly illustrative example due to its diverse regulatory functions and complex morphology.
The vagus nerve contains approximately 80% afferent (sensory) fibers and 20% efferent (motor) fibers, with fiber types ranging from heavily myelinated A-fibers to unmyelinated C-fibers [85]. Different fiber types mediate distinct physiological functions: A-fibers primarily innervate muscles of the larynx and pharynx and are associated with side effects like cough and voice alteration; B-fibers influence cardiac function and can produce bradycardia or tachycardia; and C-fibers, along with some B-fibers, modulate inflammatory processes through the cholinergic anti-inflammatory pathway [63] [85].
The cholinergic anti-inflammatory pathway represents one of the most thoroughly studied mechanisms of bioelectronic therapy. In this pathway, VNS activates efferent fibers that synapse in the celiac ganglion, ultimately releasing norepinephrine in the spleen that activates cholinergic T-cells. These T-cells then release acetylcholine, which binds to α7 nicotinic acetylcholine receptors (α7nAChR) on macrophages, inhibiting the release of pro-inflammatory cytokines like TNF-α [63]. This neuro-immune reflex has been leveraged in clinical studies for rheumatoid arthritis and inflammatory bowel disease [63].
Other important pathways include:
- The hypothalamic-pituitary-adrenal (HPA) axis modulation for neuropsychiatric conditions
- The central autonomic network for cardiovascular regulation
- The parasympathetic control of gastric and intestinal function
- The nucleus tractus solitarius (NTS) projections for seizure control
AI-enhanced stimulation protocols can target these specific pathways by using recorded neural biomarkers to identify the recruitment of particular fiber populations and adjusting parameters to optimize engagement of the desired pathways while avoiding off-target effects.
Diagram 1: Neural signaling pathways modulated by vagus nerve stimulation
Implementation Workflow for AI-Driven Protocol Optimization
The development and implementation of personalized stimulation protocols follows a systematic workflow that integrates computational modeling, experimental validation, and clinical translation. This workflow can be conceptualized as an iterative cycle of data acquisition, model training, parameter optimization, and outcome assessment.
Diagram 2: AI-driven personalized stimulation protocol workflow
Data Acquisition and Biomarker Identification
The initial phase involves comprehensive characterization of individual patient responses to stimulation across a broad parameter space. As demonstrated in recent VNS research, this includes recording evoked compound action potentials (eCAPs) while systematically varying stimulation parameters such as pulse width, frequency, amplitude, and waveform [85]. Advanced signal processing techniques are then applied to extract features from these eCAPs that correlate with specific physiological responses. For instance, certain eCAP components may predict bradycardia while others correlate with therapeutic anti-inflammatory effects. This phase establishes the critical neural biomarkers that will serve as control signals for the personalized stimulation protocol.
Computational Model Development
With the identified biomarkers, researchers develop patient-specific computational models that predict physiological responses based on stimulation parameters. Gaussian processes are particularly valuable for this application as they provide not only predictions but also uncertainty estimates, which are crucial for safe optimization [85]. These models learn the relationship between what are termed "pulse parameters" (which primarily determine the immediate neural response and fiber recruitment) and "train parameters" (which integrate these neural responses into physiological effects) [85]. This separation of parameter types enables more efficient optimization strategies.
Closed-Loop Implementation and Refinement
The validated computational models are implemented in closed-loop systems that continuously monitor neural biomarkers and dynamically adjust stimulation parameters to maintain optimal therapeutic effects. The reinforcement learning approach enables these systems to further refine their control policies based on observed outcomes, gradually improving personalization over time [88]. This continuous adaptation is particularly important for chronic conditions where disease progression or neural plasticity may alter the response to stimulation.
Future Directions and Emerging Applications
Multimodal Integration with Other Advanced Technologies
The future of AI-integrated bioelectronic medicine lies in convergence with other transformative technologies. Nanotechnology is enabling increasingly miniaturized and precise neural interfaces with enhanced biocompatibility and functionality [90]. Advanced materials science is producing flexible, stretchable electrodes that minimize foreign body response and improve long-term stability [1]. Wireless power and communication technologies are eliminating the need for bulky implanted batteries, facilitating entirely new device form factors [91]. Meanwhile, the integration of bioelectronic devices with multi-omics data (genomics, proteomics, metabolomics) is creating unprecedented opportunities for personalized medicine approaches that consider an individual's unique biological context [90].
Expanding Therapeutic Applications
While current applications of AI-enhanced bioelectronic medicine have focused primarily on neurological, cardiovascular, and inflammatory conditions, the approach is rapidly expanding to new therapeutic areas. In oncology, AI is being integrated with bioelectronic approaches to modulate the tumor microenvironment and enhance immunotherapy responses [90]. For metabolic disorders, closed-loop bioelectronic systems are being developed to precisely regulate glucose homeostasis and energy balance. In psychiatric conditions, AI-powered neuromodulation offers new hope for treatment-resistant depression, PTSD, and addiction by adapting stimulation to moment-to-moment changes in neural circuit activity.
The integration of artificial intelligence with bioelectronic devices represents a paradigm shift in neuromodulation therapy, transforming static, one-size-fits-all stimulation protocols into dynamic, personalized treatments that adapt to individual physiology and disease state. Through machine learning approaches like reinforcement learning, Gaussian processes, and deep neural networks, these intelligent systems can navigate complex parameter spaces to optimize therapeutic efficacy while minimizing side effects. The implementation of closed-loop control based on neural biomarkers enables precise engagement of targeted pathways while avoiding off-target effects. As research advances, the convergence of AI with bioelectronic medicine promises to unlock new therapeutic possibilities across a broad spectrum of diseases, ultimately fulfilling the field's potential to provide precisely targeted, personalized therapies with minimal side effects.
Conclusion
Bioelectronic medicine represents a paradigm shift from conventional pharmacotherapy, offering targeted, programmable treatment for chronic conditions through direct neural interface. The field has evolved from basic cardiac pacemakers to sophisticated closed-loop systems capable of real-time physiological adaptation. While significant challenges remain in device longevity, biocompatibility, and system integration, emerging advances in flexible electronics, novel materials, and artificial intelligence are rapidly addressing these limitations. The convergence of bioelectronic medicine with digital health technologies promises a future of truly personalized, adaptive therapies that could revolutionize treatment for neurological, inflammatory, and metabolic diseases. For researchers and drug development professionals, this expanding field offers unprecedented opportunities to develop therapies with superior specificity, reduced systemic side effects, and potentially curative potential for previously intractable conditions.
References
- 1. The rise of bioelectronic medicine - BioMed Central [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-024-00151-8]
- 2. A Brief History of Bioelectronic Medicine and other interesting facts you probably didn't know | NuroKor BioElectronics [https://www.nurokor.com/blog/history-of-bioelectronic-medicine]
- 3. Home | Bioelectronic Medicine [https://bioelecmed.biomedcentral.com/]
- 4. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00179-4]
- 5. The diversity and evolution of electric organs in Neotropical ... [https://evodevojournal.biomedcentral.com/articles/10.1186/s13227-022-00194-5]
- 6. Vocal and Electric Fish: Revisiting a Comparison of Two ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8418312/]
- 7. Bioelectronic medicine: preclinical insights and clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10155266/]
- 8. Bioelectronic Medicine Market Research Report 2025 [https://www.globenewswire.com/news-release/2025/06/04/3093780/28124/en/Bioelectronic-Medicine-Market-Research-Report-2025-Featuring-Key-Players-Medtronic-Abbott-Boston-Scientific-Cochlear-LivaNova-Soterix-Medical-Bioinduction-GiMer-Medical-CEFALY-BioC.html]
- 9. Abstracts from the Sixth Bioelectronic Medicine Summit [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538809/]
- 10. New Paper Creates Roadmap for the Next Generation ... [https://today.ucsd.edu/story/new-paper-creates-roadmap-for-the-next-generation-of-bioelectronic-medicine]
- 11. Neural Circuit Mapping and Neurotherapy-Based Strategies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12297084/]
- 12. A Framework for Quantitative Modeling of Neural Circuits ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4341569/]
- 13. A Student's Guide to Neural Circuit Tracing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6718611/]
- 14. Quantitative prediction of intracellular dynamics and ... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2025.1515194/full]
- 15. Bioelectronic Medicine: a multidisciplinary roadmap from ... [https://www.frontiersin.org/journals/integrative-neuroscience/articles/10.3389/fnint.2024.1321872/full]
- 16. In bioelectronics breakthrough, scientists create soft, ... [https://news.uchicago.edu/story/bioelectronics-breakthrough-scientists-create-soft-flexible-semiconductors]
- 17. Articles | Bioelectronic Medicine - BioMed Central [https://bioelecmed.biomedcentral.com/articles]
- 18. Anatomy, Central Nervous System - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK542179/]
- 19. Nervous System: What It Is, Parts, Function & Disorders [https://my.clevelandclinic.org/health/body/21202-nervous-system]
- 20. Neurotransmitters—Key Factors in Neurological and ... [https://www.mdpi.com/1422-0067/23/11/5954]
- 21. Exploring the key targets and compounds that manipulate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11089239/]
- 22. Recent Advances in Flexible Sensors for Neural Interfaces [https://www.mdpi.com/2079-6374/15/7/424]
- 23. Neurostimulation Devices Market Size, Share | Growth [2032] [https://www.fortunebusinessinsights.com/industry-reports/neuromodulation-devices-market-100561]
- 24. Deep Brain Stimulation (DBS) Devices Market Size to ... [https://dimensionmarketresearch.com/report/deep-brain-stimulation-dbs-devices-market/]
- 25. Neurostimulation Market Outlook 2025 to 2035 [https://www.futuremarketinsights.com/reports/neurostimulation-market]
- 26. Deep Brain Stimulation Statistics 2025 By Devices [https://media.market.us/deep-brain-stimulation-statistics/]
- 27. Spinal Cord Stimulation (SCS) Clinical Data [https://www.bostonscientific.com/en-US/medical-specialties/pain-management/scs-clinical-data.html]
- 28. Spinal cord stimulation plus conventional medical ... [https://pubmed.ncbi.nlm.nih.gov/41047246]
- 29. vagus nerve stimulator trends 2025: Key Insights [https://www.accio.com/business/vagus-nerve-stimulator-trends]
- 30. Next generation bioelectronic medicine: making the case for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11748337/]
- 31. Chronic adaptive deep brain stimulation for Parkinson's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12397205/]
- 32. Materials strategy and device fabrication for stable closed ... [https://www.nature.com/articles/s44328-025-00045-y]
- 33. A software platform for real-time and adaptive ... [https://www.nature.com/articles/s41467-025-64856-3]
- 34. A novel neuroimmune modulation system for the treatment of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-024-00142-9]
- 35. Approval of vagus nerve stimulator may herald 'pivot point' [https://www.healio.com/news/rheumatology/20251113/approval-of-vagus-nerve-stimulator-may-herald-pivot-point-for-rheumatology]
- 36. Clinical Evidence [https://setpointmedical.com/clinical-evidence/]
- 37. SetPoint Medical to Present Data at ACR Convergence ... [https://www.biospace.com/press-releases/setpoint-medical-to-present-data-at-acr-convergence-2025-demonstrating-sustained-efficacy-and-safety-for-the-setpoint-system-to-treat-rheumatoid-arthritis]
- 38. Neuroimmune Modulation for Drug-Refractory Rheumatoid ... [https://pubmed.ncbi.nlm.nih.gov/41071520/]
- 39. Vagus Nerve Stimulator for Rheumatoid Arthritis: New FDA ... [https://empoweredarthritis.com/rheumatology/vagus-nerve-stimulator-for-rheumatoid-arthritis/]
- 40. Harnessing metamaterials for efficient wireless power transfer ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-023-00136-z]
- 41. Distributed battery-free bioelectronic implants with improved ... [https://pubmed.ncbi.nlm.nih.gov/40877535/]
- 42. Wireless power transfer system for deep-implanted ... [https://www.nature.com/articles/s41598-022-18000-6]
- 43. Singing The Body Electric: Exploring Bioelectronic Medicine [https://www.pharmasalmanac.com/articles/singing-the-body-electric-exploring-bioelectronic-medicine]
- 44. Graphene oxide doped conducting polymer ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961213014245]
- 45. The Biomedical Applications of Conductive Polymers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10145001/]
- 46. Graphene-Based Composites for Biomedical Applications [https://www.mdpi.com/2218-273X/13/11/1571]
- 47. Bioelectronic Medicine Market Research Report 2025 ... [https://finance.yahoo.com/news/bioelectronic-medicine-market-research-report-151200955.html]
- 48. Molecular Signaling in Biomaterial-induced Foreign Body ... [https://pubmed.ncbi.nlm.nih.gov/40981767/]
- 49. Advanced strategies to thwart foreign body response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9472022/]
- 50. Foreign Body Reaction to Implanted Biomaterials and Its ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.622524/full]
- 51. Foreign Body Reaction to Neural Implants: A Comparative ... [https://www.mdpi.com/2079-6374/15/9/599]
- 52. Immunomodulating Red Blood Cell Coating for Mitigation ... [https://www.sciencedirect.com/science/article/pii/S2666138125000143]
- 53. Experimental protocol for evaluation of biomaterials in an in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11441155/]
- 54. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 55. Wireless, battery-free, and real-time monitoring of water ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11358307/]
- 56. Liquid-based encapsulation for implantable bioelectronics ... [https://www.nature.com/articles/s41467-025-55992-x]
- 57. Review Bioresorbable polymers for electronic medicine [https://www.sciencedirect.com/science/article/pii/S2666386424003771]
- 58. Revolutionizing brain‒computer interfaces - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243264/]
- 59. Bio-inspired electronics: Soft, biohybrid, and “living” neural ... [https://www.nature.com/articles/s41467-025-57016-0]
- 60. Emerging fiber-based neural interfaces with conductive ... [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d4mh01854k]
- 61. Electric Medicine: A Transformative HealthTech Sub-Sector in ... [https://www.healthcare.digital/single-post/electric-medicine-a-transformative-healthtech-sub-sector-in-2025]
- 62. Batteries or Energy Harvesting - Can't It Be Both? [https://www.onio.com/article/batteries-and-harvesting-can-itbe-both.html]
- 63. Bioelectronic Medicine: a multidisciplinary roadmap from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10911101/]
- 64. Drift suppression method based on signal stability ... [https://www.sciencedirect.com/science/article/abs/pii/S1051200424004378]
- 65. Analog Sensor Woes: Dealing with Drift, Noise, and Non- ... [https://runtimerec.com/analog-sensor-woes-dealing-with-drift-noise-and-non-linearity/]
- 66. A Novel Parallel Processing Model for Noise Reduction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8625380/]
- 67. The role of inflammation in neurological disorders: a brief ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11558529/]
- 68. Sequelae of viral CNS infections including outcomes, ... [https://www.nature.com/articles/s44298-025-00160-7]
- 69. Protocol for artificial intelligence-guided neural control ... [https://www.sciencedirect.com/science/article/pii/S2666166724006610]
- 70. The rise of bioelectronic medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11337583/]
- 71. Bioelectric Medicine Market | Global Market Analysis Report [https://www.futuremarketinsights.com/reports/bioelectric-medicine-market]
- 72. A bioelectronic route to compassion: Rationale and study protocol for... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0282861]
- 73. Influencing Side-Effects to Medicinal Treatments [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2018.00775/full]
- 74. Exploring the Relationship Between Drug Side-Effects and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3900166/]
- 75. Comparative effects of pharmacological interventions for ... [https://www.sciencedirect.com/science/article/pii/S0140673622008789]
- 76. The Potential Cost-Effectiveness of a Cell-Based Bioelectronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8739553/]
- 77. Regulations: Good Clinical Practice and Clinical Trials [https://www.fda.gov/science-research/clinical-trials-and-human-subject-protection/regulations-good-clinical-practice-and-clinical-trials]
- 78. Clinical Trials and Human Subject Protection [https://www.fda.gov/science-research/science-and-research-special-topics/clinical-trials-and-human-subject-protection]
- 79. Novel Drug Approvals for 2025 [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 80. Drug Approvals and Databases [https://www.fda.gov/drugs/development-approval-process-drugs/drug-approvals-and-databases]
- 81. 2025 Course | Join Clinical Trials Training Today [https://www.ninds-ctmc.org/2025-course-1]
- 82. Bioelectric Medicine Market Size to Hit USD 47.28 Billion ... [https://www.precedenceresearch.com/bioelectric-medicine-market]
- 83. Bioelectronic medicine: wearable and implantable electronics [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00185-6]
- 84. 2025 Bioelectronic Medicine Forum Report, Lisa Shafer, Biogen ... [https://www.neurotechreports.com/pages/BMF25report.html?utm_source=phpList&utm_medium=email&utm_campaign=Neurotech+Reports+News+Updates&utm_content=HTML]
- 85. Using neural biomarkers to personalize dosing of vagus ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-024-00147-4]
- 86. Artificial Intelligence in Biomedical Sciences: A Scoping Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360964/]
- 87. Revolutionizing healthcare: the role of artificial intelligence in ... [https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-023-04698-z]
- 88. Smart device uses AI and bioelectronics to speed up ... [https://news.ucsc.edu/2025/09/smart-device-ai-bioelectronics-speed-up-wound-healing/]
- 89. Advances in cardiac devices and bioelectronics augmented ... [https://pubmed.ncbi.nlm.nih.gov/40695457/]
- 90. Revolutionizing breast cancer immunotherapy by integrating ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00173-w]
- 91. Bioelectronic devices for light-based diagnostics and therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC10903427/]