Biocompatibility Testing for Organic Electronic Materials: A Comprehensive Guide for Researchers and Developers
This article provides a thorough examination of biocompatibility testing specifically for organic electronic materials, which are pivotal for the next generation of implantable and wearable medical devices.
Biocompatibility Testing for Organic Electronic Materials: A Comprehensive Guide for Researchers and Developers
Abstract
This article provides a thorough examination of biocompatibility testing specifically for organic electronic materials, which are pivotal for the next generation of implantable and wearable medical devices. It covers the foundational principles that make these materials—such as conjugated polymers and biocompatible elastomers—uniquely suited for biointegration, detailing their mechanical and charge transport properties. The scope extends to established and emerging testing methodologies aligned with ISO 10993 standards, strategies for troubleshooting common challenges like inflammatory responses and material degradation, and the critical processes for in vitro and in vivo validation. Aimed at researchers, scientists, and development professionals, this guide synthesizes current research, innovative testing platforms, and real-world case studies to navigate the path from material design to clinically safe bioelectronic devices.
The Fundamentals of Organic Electronic Materials and Biocompatibility
Defining Biocompatibility in the Context of Medical Devices and ISO Standards
Biocompatibility is defined as the "ability of a medical device or material to perform with an appropriate host response in a specific application" [1]. It is not an intrinsic property of a material but a conditional one, heavily dependent on the device's intended use and the nature of its interaction with the body [2]. The evaluation of biocompatibility is a critical pillar in the development of any medical device, ensuring that devices which contact patients—from simple surgical masks to complex implantable sensors—do not cause unacceptable adverse biological reactions [3] [4].
The international benchmark for managing biological risk is the ISO 10993 series of standards, titled "Biological evaluation of medical devices" [3] [1]. This series provides a consistent, science-based framework for biological safety evaluations, used by regulators, notified bodies, and manufacturers worldwide [3]. The core of this framework, ISO 10993-1, establishes that biocompatibility must be assessed within a risk management process aligned with ISO 14971, emphasizing hazard identification, risk estimation, and control [3] [5]. In the United States, the Food and Drug Administration (FDA) provides its own guidance on the use of ISO 10993-1, requiring evaluation for devices with direct or indirect body contact and assessing the final finished device in its entirety [4].
The ISO 10993-1 Framework: Evaluation Principles and Endpoints
ISO 10993-1 is the cornerstone standard of the series, providing the overarching principles and requirements for biological evaluation [3]. Its fundamental purpose is to guide manufacturers in identifying, assessing, and managing the biological risks associated with a device's materials, design, and tissue contact during its intended use [3]. The evaluation process is not a simple checklist of tests but a structured risk assessment that begins with a thorough characterization of the device material and its chemical constituents [3] [5].
The standard requires manufacturers to establish a biological evaluation plan, which systematically considers the nature and duration of body contact to determine the necessary biological endpoints for evaluation [1]. The nature of body contact is categorized as surface device, externally communicating device, or implant device, with further sub-divisions based on specific tissues (e.g., intact skin, mucosal membrane, blood, bone) [1]. The contact duration is classified as limited (≤24 hours), prolonged (>24 hours to 30 days), or permanent (>30 days) [1]. This categorization is used to determine which biological endpoints require evaluation. The matrix below summarizes the required and additional endpoints based on device categorization.
Table: ISO 10993-1 Endpoints for Consideration Based on Device Categorization (Adapted from FDA-Modified Matrix) [1]
| Nature of Body Contact | Contact Duration | Cytotoxicity | Sensitization | Irritation | Systemic Toxicity | Genotoxicity | Implantation | Hemocompatibility |
|---|---|---|---|---|---|---|---|---|
| Surface Device (Intact Skin) | A - Limited | X | X | X | ||||
| B - Prolonged | X | X | X | |||||
| C - Permanent | X | X | X | |||||
| Mucosal Membrane | A - Limited | X | X | X | ||||
| B - Prolonged | X | X | X | O | O | O | ||
| C - Permanent | X | X | X | O | O | X | O | |
| Blood Path, Indirect | A - Limited | X | X | X | X | |||
| B - Prolonged | X | X | X | O | O | X | ||
| C - Permanent | X | X | O | O | X | O | X | |
| Implant Device (Tissue/Bone) | A - Limited | X | X | X | O | |||
| B - Prolonged | X | X | X | O | X | X | ||
| C - Permanent | X | X | X | O | X | X | O |
X = ISO 10993-1 recommended endpoints for consideration; O = Additional FDA recommended endpoints for consideration. This is a simplified excerpt; the full matrix includes additional endpoints like chronic toxicity, carcinogenicity, and reproductive toxicity. [1]
The following diagram illustrates the logical workflow for the biological evaluation of a medical device as prescribed by ISO 10993-1 within a risk management framework.
The "Big Three" and Other Key Biocompatibility Tests
Among the numerous biological endpoints, three tests—cytotoxicity, sensitization, and irritation—are considered the "Big Three" because they are required for almost all medical devices, regardless of their categorization [6]. These tests are often the first line of in vitro screening, with additional tests required based on the device's contact and duration.
Table: Summary of Key Biocompatibility Tests and Their Methodologies
| Test Endpoint | Relevant ISO Standard | Common Test Methods & Protocols | Key Assessment Criteria |
|---|---|---|---|
| Cytotoxicity | ISO 10993-5 [6] | - Direct contact- Agar diffusion- Extract dilution (elution) using MTT, XTT, or Neutral Red Uptake assays [2] [6]. | Cell viability, morphological changes, cell lysis, and detachment. ≥70% cell viability is often a positive sign [6]. |
| Sensitization | ISO 10993-10 [5] | - Guinea Pig Maximization Test (GPMT)- Local Lymph Node Assay (LLNA)- In vitro methods [6]. | Potential for a material to cause an allergic hypersensitivity response upon repeated exposure. |
| Irritation | ISO 10993-23 [5] | - Skin irritation tests (in vivo or in vitro)- Intracutaneous reactivity test [6]. | Localized inflammatory response not involving an immune mechanism at the contact site. |
| Genotoxicity | ISO 10993-3 [5] | - In vitro assays for gene mutations (e.g., Ames test) and chromosomal aberrations [5]. | Assessment of potential damage to genetic material, which may lead to carcinogenesis. |
| Implantation | ISO 10993-6 [5] | - Device or material is surgically implanted in an animal model (e.g., muscle, bone) for a specified period [5]. | Local effects on living tissue, including inflammation, fibrosis, and encapsulation at the implant site. |
Detailed Experimental Protocol: In Vitro Cytotoxicity Testing (ISO 10993-5)
Cytotoxicity testing assesses whether a device's materials or extracts cause damage to living cells [6]. The following is a generalized protocol for the extract dilution method, one of the most common approaches.
1. Sample Preparation (Refer to ISO 10993-12):
- The test device or a representative sample is prepared under clean conditions.
- An extraction is performed using a suitable solvent(s) such as cell culture medium with serum (for polar substances) and vegetable oil or saline (for non-polar substances) [6].
- Extraction conditions (e.g., 37°C for 24-72 hours) are selected based on the device's nature and intended use to simulate clinical exposure.
2. Cell Culture:
- Mammalian cell lines, typically fibroblasts (e.g., L929, Balb 3T3), are cultured in standard conditions [6].
- Cells are seeded into multi-well plates and allowed to attach and grow until they form a near-confluent monolayer.
3. Exposure to Extract:
- The culture medium is replaced with the prepared device extract (neat or diluted).
- Control groups are included: negative control (fresh culture medium, extraction solvent), and positive control (e.g., a solution containing known cytotoxic agents like latex or zinc diethyldithiocarbamate) [6].
- Cells are incubated with the extract for approximately 24 hours at 37°C [6].
4. Assessment of Cytotoxicity:
- Cell Viability Quantification: A reagent like MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl-2H-tetrazolium bromide) is added. Metabolically active cells convert MTT to a purple formazan product. The absorbance of the dissolved formazan is measured spectrophotometrically; the intensity correlates with the number of viable cells [6]. Alternative assays include XTT and Neutral Red Uptake.
- Qualitative Morphological Assessment: Cells are examined under a microscope for signs of toxicity, including rounding, detachment from the substrate, cell lysis, and vacuolization [6].
5. Data Interpretation:
- Results are compared to controls. A reduction in cell viability below a certain threshold (e.g., <70% for neat extract) may indicate cytotoxicity [6].
- Any cytotoxic effect requires further investigation and risk assessment within the context of the device's intended use.
Biocompatibility of Organic Electronic Materials
Organic electronic materials represent a frontier in medical device technology, particularly for implantable bioelectronics and biosensors [2] [7]. These materials, which include conducting polymers like PEDOT and semiconducting polymers like DPPT-TT, offer unique advantages for biointegration [2] [7] [8]. Their mechanical properties, such as a low Young's modulus, can be engineered to closely match that of human tissues (e.g., ~10 kPa for the cortex), significantly reducing the mechanical mismatch that often leads to inflammation and fibrous encapsulation around traditional rigid implants [2]. Furthermore, their primary charge carriers can be both electrons and ions, facilitating efficient transduction of signals across the biotic-abiotic interface [2].
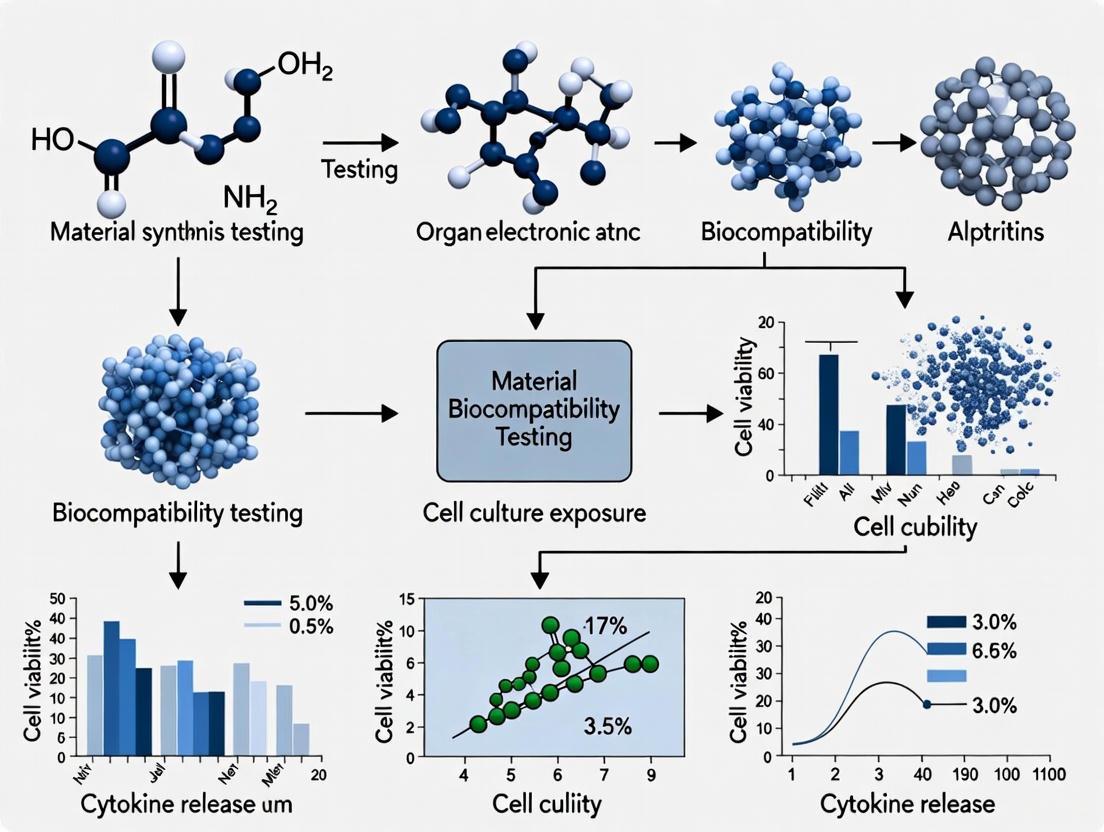
The evaluation of these novel materials follows the same ISO 10993 principles but presents specific challenges and considerations. The following diagram outlines a typical workflow for evaluating a new organic electronic material, from initial screening to in vivo validation.
A recent study exemplifies this process, developing a highly biocompatible and stretchable organic field-effect transistor (sOFET) for implants [7]. The researchers used a blend of a semiconducting polymer (DPPT-TT) and a medical-grade elastomer, bromo isobutyl–isoprene rubber (BIIR), which is known to meet ISO 10993 standards [7]. The material's vulcanization process was carefully controlled to preserve electrical properties while achieving mechanical stability under 50% strain. In vitro assessments with human dermal fibroblasts and macrophages showed no adverse effects on cell viability, proliferation, or migration [7]. Subsequent in vivo implantation studies in mice demonstrated no major inflammatory response or tissue damage, confirming its potential for long-term integration [7]. This highlights the trend of moving beyond "bio-inert" materials to those that can form a more intimate and stable interface with biological tissues.
Table: Comparison of Material Properties: Abiotic, Organic Electronic, and Biotic Tissue
| Aspect | Abiotic Electronic Materials | Organic Electronic Materials | Biotic Living Tissue |
|---|---|---|---|
| Composition | Inorganic metals & semiconductors | Organic molecules & polymers (e.g., PEDOT, DPPT-TT) | Complex mixture of water, proteins, lipids |
| Physical State | Hard solids | Soft solids | Extremely soft solids |
| Young's Modulus | ~100 GPa | 20 kPa - 3 GPa (tunable) | ~10 kPa (cortex) |
| Charge Carriers | Electrons & holes | Electrons, holes, & ions | Ions |
| Primary Biocompatibility Challenge | Mechanical mismatch, chronic inflammation | Long-term stability in physiological environment, biofouling | N/A |
Data synthesized from [2] and [7].
The Scientist's Toolkit: Key Reagents and Materials for Biocompatibility Research
Table: Essential Research Reagent Solutions for Biocompatibility Testing
| Reagent / Material | Function in Biocompatibility Evaluation |
|---|---|
| L929 or Balb 3T3 Fibroblast Cell Lines | Standardized mammalian cell lines used for in vitro cytotoxicity testing (ISO 10993-5) [6]. |
| MTT/XTT/Neutral Red Reagents | Tetrazolium-based dyes or uptake assays used to quantitatively measure cell viability and proliferation in cytotoxicity tests [2] [6]. |
| Cell Culture Media with Serum | A polar solvent used for extracting devices to simulate the leaching of hydrophilic chemical constituents [6]. |
| Vegetable Oil or Dimethyl Sulfoxide (DMSO) | Non-polar solvents used for extracting devices to simulate the leaching of lipophilic chemical constituents [6]. |
| Medical-Grade Elastomers (e.g., BIIR) | Biocompatible base materials that serve as an elastic matrix for creating soft, implantable electronic devices, ensuring compliance with ISO 10993 [7]. |
| Conducting Polymers (e.g., PEDOT, PPy) | Organic mixed ionic/electronic conductors that form the active sensing/ stimulating component in bioelectronic devices, enabling efficient interface with biological tissues [2] [8]. |
Defining and demonstrating biocompatibility is a rigorous, context-dependent process governed by the internationally recognized ISO 10993 series. The framework moves beyond simple pass/fail testing, mandating a risk-based evaluation that considers the complete device in its final form. For the burgeoning field of organic bioelectronics, this standard provides the essential pathway to clinical translation. While materials like conducting polymers offer inherent advantages for biointegration due to their soft mechanics and mixed conduction, they must still undergo the same systematic evaluation—from the "Big Three" tests to long-term implantation studies. As research progresses, the synergy between innovative material design and robust standardized evaluation will continue to be the foundation for developing the next generation of safe and effective medical devices.
Why Organic? The Unique Properties of Conjugated Polymers for Biointegration
The emergence of organic bioelectronics represents a paradigm shift in the design of medical and diagnostic devices, effectively bridging the electronic world of semiconductors with the soft, ionic world of biology. Within this field, conjugated polymers have emerged as a premier material class for biointegration, offering a unique combination of electronic functionality and biological compatibility that traditional inorganic materials like silicon and metals lack. These carbon-based semiconductors share a similar chemical "nature" with biological molecules, enabling more seamless integration with living tissues and biological systems [9]. The fundamental challenge in biointegration involves creating interfaces that allow for efficient electronic communication with biological systems without triggering adverse immune responses or mechanical mismatches. Conjugated polymers address this challenge through their tunable chemical, electrical, and mechanical properties, making them ideal candidates for applications ranging from biosensors and neural interfaces to drug delivery systems and tissue engineering scaffolds [9] [10]. This review examines the unique properties that render conjugated polymers exceptional materials for biointegration, with specific comparisons to traditional alternatives and detailed experimental methodologies for evaluating their performance.
Unique Properties of Conjugated Polymers for Biointegration
Mechanical Compatibility with Biological Tissues
The mechanical mismatch between conventional electronic materials and soft biological tissues often leads to fibrotic encapsulation, reduced signal fidelity, and chronic inflammation. Conjugated polymers address this fundamental challenge through their inherent flexibility and tunable mechanical properties.
Table 1: Mechanical Properties of Electronic Materials vs. Biological Tissues
| Material Category | Specific Material | Young's Modulus (GPa) | Tensile Strength (MPa) | Fracture Strain (%) | Key Characteristics |
|---|---|---|---|---|---|
| Traditional Electronics | Silicon | 160-180 | 7000 | <1 | Brittle, rigid |
| Gold | 78 | 220 | <5 | Dense, stiff | |
| Conjugated Polymers | PEDOT:PSS (dry) | 2-4 | 50-80 | 10-30 | Ductile, flexible |
| PEDOT:PSS (hydrogel) | 0.001-0.1 | 1-10 | 50-200 | Soft, stretchable | |
| Poly(3-hexylthiophene) | 0.5-2 | 30-60 | 5-15 | Thermoplastic | |
| Biological Tissues | Brain Tissue | 0.0005-0.003 | - | 50-100 | Ultra-soft, viscoelastic |
| Skin | 0.015-0.085 | 5-30 | 35-115 | Fibrous, anisotropic | |
| Cardiac Tissue | 0.02-0.5 | 50-150 | 10-15 | Contractile |
Conjugated polymers can be engineered into various forms, including hydrogels with Young's moduli similar to those of soft tissues, significantly reducing mechanical mismatch at the biointerface [9]. This tunability enables the design of devices that minimally impair natural tissue function and reduce foreign body responses. Furthermore, certain conjugated polymers can be processed into three-dimensional architectures because of their solution processability, creating scaffolds that provide structural support while enabling integrated sensing or stimulation within engineered tissues themselves [9].
Mixed Ionic-Electronic Conduction
Biological systems predominantly use ionic conduction for signal transmission, whereas traditional electronics rely solely on electronic conduction. Conjugated polymers uniquely bridge this fundamental divide.
Table 2: Charge Transport Properties in Electronic Materials
| Material Type | Electronic Conductivity (S/cm) | Ionic Conductivity (S/cm) | Charge Carriers | Coupling Efficiency |
|---|---|---|---|---|
| Metals | 10⁴-10⁶ | Negligible | Electrons | Poor |
| Inorganic Semiconductors | 10⁻⁶-10³ | Negligible | Electrons/Holes | Poor |
| Traditional Conducting Polymers | 10⁻¹⁰-10³ | 10⁻⁶-10⁻³ | Electrons/Holes | Moderate |
| Organic Mixed Ionic-Electronic Conductors | 10⁻³-10³ | 10⁻⁴-10⁻¹ | Both ions and electrons | Excellent |
Organic mixed ionic-electronic conductors (OMIECs), such as the widely used PEDOT, constitute a special class of materials exhibiting simultaneous electronic and ionic conductivity [10]. This unique combination enables more efficient signal transduction across the biology-electronics interface, as the polymers can directly translate ionic fluxes from biological systems into electronic signals for external devices, and vice versa [9] [10]. Leveraging ion redistribution inside a conjugated polymer upon application of an electrical field and its coupling with electronic charges enables the development of advanced devices such as organic electrochemical transistors (OECTs) that can be engineered to act as artificial neurons or synapses with complex, history-dependent behavior [9].
Chemical Tunability and Functionalization
The molecular structure of conjugated polymers provides unparalleled opportunities for chemical modification to enhance biointegration and introduce specific functionalities. Unlike inorganic semiconductors with fixed crystalline structures, conjugated polymers offer synthetic versatility that enables precise control over their properties through molecular design [9] [11]. Their biological properties can be controlled using a variety of functionalization strategies, including the incorporation of biomimetic peptides, enzyme-sensitive linkages, or anti-fouling molecules to direct specific cellular responses or minimize non-specific protein adsorption [9]. Furthermore, the development of conjugated polyelectrolytes and the ability to incorporate various side chains and functional groups allows researchers to fine-tune solubility, surface energy, and interaction with biological components without compromising electronic functionality [9].
Processability and Form Factor Versatility
Conjugated polymers can be processed using a variety of techniques that enable the creation of devices with form factors conducive to biointegration. These materials are solution-processable, allowing for deposition through low-cost, low-temperature methods such as spin-coating, inkjet printing, and 3D printing, unlike inorganic semiconductors that require high-temperature processing [12] [11]. This enables fabrication on flexible substrates compatible with biological systems. Additive manufacturing techniques allow for the creation of complex three-dimensional structures that can mimic tissue architecture, moving beyond the two-dimensional constraints of traditional electronics [11]. Finally, organic electronic materials can be integrated with a variety of mechanical supports, giving rise to devices with form factors that enable seamless integration with biological systems, including wearable, implantable, and transient electronics [9].
Experimental Characterization and Biocompatibility Assessment
Electrical Performance Characterization
Evaluating the electrical properties of conjugated polymers under biologically relevant conditions is essential for assessing their suitability for biointegration.
Table 3: Standardized Experimental Protocols for Electrical Characterization
| Test Parameter | Experimental Method | Biological Context Protocol | Key Metrics | Relevance to Biointegration |
|---|---|---|---|---|
| Electronic Conductivity | 4-point probe measurement | Measurements in physiological buffer (PBS, 37°C) | Sheet resistance, bulk conductivity | Signal fidelity in wet environments |
| Ionic-Eronic Coupling | Electrochemical impedance spectroscopy | Frequency sweep 0.1-10⁶ Hz in cell culture media | Charge storage capacity, interfacial impedance | Efficiency of biological signal transduction |
| Operational Stability | Continuous cycling in OECT configuration | 10⁴-10⁶ cycles in simulated body fluid | On/off current retention, threshold voltage shift | Device longevity in implantable applications |
| Charge Injection Capacity | Cyclic voltammetry | Scanning at 50 mV/s in relevant potential window | Volumetric capacitance, redox stability | Safety and efficacy of stimulation |
Biocompatibility Testing Workflow
The biological safety evaluation of conjugated polymers follows a structured approach aligned with regulatory frameworks such as ISO 10993, which outlines the required tests for medical devices based on the nature and duration of body contact [13] [14].
The FDA's "Chemical Analysis for Biocompatibility Assessment of Medical Devices" draft guidance emphasizes that chemical characterization forms the foundation of the biological safety assessment [14]. This involves a process of data gathering concerning the materials of construction, their chemical ingredients, and chemical residues originating from the manufacturing process. For conjugated polymers, this includes identifying and quantifying monomers, oligomers, catalysts, dopants, and processing aids that might leach out during device operation. The guidance recommends using multiple analytical techniques (HS-GC/MS, GC/MS, LC/MS, ICP/MS) to profile both organic and elemental extractables, with testing conducted on three separate batches to account for material variability [14].
Experimental Protocol: Cytocompatibility Assessment
Objective: To evaluate the in vitro cellular response to conjugated polymer samples using standardized cytotoxicity and cell adhesion assays.
Materials:
- Sterilized conjugated polymer films (e.g., PEDOT:PSS, PPy, PANI) on appropriate substrates
- Control materials (tissue culture plastic, reference materials)
- Relevant cell line (e.g., NIH/3T3 fibroblasts for general cytotoxicity, PC12 neurons for neural interfaces)
- Complete cell culture medium with serum
- Cell viability assay reagents (MTT, AlamarBlue, or PrestoBlue)
- Immunocytochemistry reagents (fixative, permeabilization buffer, primary/secondary antibodies)
Methodology:
- Sample Preparation: Prepare sterile test samples in 24-well plate format. Include positive control (e.g., latex extract) and negative control (culture medium only).
- Direct Contact Test: Seed cells directly onto test materials at standard density (e.g., 10,000 cells/well) and culture for 24-72 hours.
- Extract Testing: Prepare extracts by incubating materials in culture medium (3 cm²/mL) for 24-72 hours at 37°C. Apply extracts to pre-seeded cells.
- Viability Assessment: After exposure period, add viability indicator and measure according to manufacturer's protocol.
- Cell Morphology Analysis: Fix cells, stain for actin cytoskeleton and nuclei, and image using fluorescence microscopy.
- Data Analysis: Calculate percentage viability relative to negative control. Assess cell morphology and adhesion quality.
Interpretation: Cell viability >70% relative to negative control is generally considered non-cytotoxic. Additionally, observe cell morphology - well-spread cells with normal morphology indicate good biocompatibility, while rounded cells suggest toxicity or poor adhesion.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Materials for Conjugated Polymer Biointerface Research
| Category | Specific Material/Reagent | Function in Research | Key Considerations |
|---|---|---|---|
| Conjugated Polymers | PEDOT:PSS | Benchmark OMIEC for bioelectronics | Commercial formulations vary; often require optimization |
| Polyaniline (PANI) | pH-responsive conducting polymer | Conductivity dependent on doping state and pH | |
| Polypyrrole (PPy) | Biocompatible polymer for neural interfaces | Typically electropolymerized for device fabrication | |
| Dopants/Additives | Tosylate, PSS | p-type dopants for enhanced conductivity | Impact on biocompatibility must be assessed |
| Ionic liquids | Processing additives and conductivity enhancers | Can improve mechanical properties and stability | |
| Polyethylene glycol (PEG) | Biocompatibility enhancer | Reduces protein fouling, improves wettability | |
| Characterization Tools | Electrochemical workstation | Critical for electrical/electrochemical characterization | Must include impedance capability |
| Quartz crystal microbalance | Monitoring mass changes during swelling/protein adsorption | Combined with electrochemical measurements (EQCM) | |
| Surface plasmon resonance | Label-free monitoring of biomolecular interactions | Provides kinetic binding information | |
| Cell Culture | Primary neurons | Relevant for neural interface development | Requires specialized culture conditions |
| Fibroblasts (e.g., NIH/3T3) | General cytotoxicity screening | Standardized, well-characterized model | |
| Metabolic activity assays | Quantitative cytotoxicity assessment | Multiple platforms available (MTT, AlamarBlue, etc.) |
Conjugated polymers offer a compelling materials platform for biointegration due to their unique combination of mechanical compliance, mixed ionic-electronic conduction, chemical tunability, and versatile processing. These properties enable the development of bioelectronic devices that form more seamless interfaces with biological systems, minimizing foreign body responses while maintaining high electronic performance. As the field progresses, the emphasis is shifting from simply demonstrating biocompatibility to designing multifunctional materials that actively direct desired biological responses. The ongoing development of standardized characterization methodologies and regulatory frameworks will be crucial for translating these promising materials from laboratory research to clinical applications, ultimately enabling new generations of implantable, wearable, and transient bioelectronic devices for healthcare and medical research.
The development of bioelectronic devices for neural interfaces, wearable monitors, and implantable systems demands materials that seamlessly integrate with biological tissues. The fundamental challenge lies in the mechanical and chemical mismatch between conventional electronics and living systems. Traditional rigid electronic materials, such as silicon and metals, possess Young's moduli in the gigapascal range (GPa), while biological tissues like the brain are orders of magnitude softer, with moduli in the kilopascal range (kPa). This mismatch often triggers chronic inflammatory responses, fibrosis, and device failure. Consequently, the field has increasingly turned to soft, organic electronic materials that can bridge this divide. Among these, conductive polymers like PEDOT:PSS and biocompatible elastomers such as Bromo Isobutyl-Isoprene Rubber (BIIR) have emerged as leading candidates. This guide objectively compares the performance, properties, and biocompatibility of these key material classes, providing researchers with the experimental data and methodologies needed for informed material selection.
Material Class Comparison: Properties and Performance
The following table summarizes the key characteristics of major biocompatible material classes for organic electronics, highlighting their respective advantages and limitations.
Table 1: Comparison of Key Biocompatible Electronic Material Classes
| Material Class | Specific Example | Key Electrical Properties | Key Mechanical Properties | Biocompatibility & In Vivo Performance | Primary Applications |
|---|---|---|---|---|---|
| Conductive Polymers | PEDOT:PSS (PILC Ink) [15] | High conductivity (~286 S/cm) | Storage modulus ~105 Pa; Yield stress ~103 Pa | No post-treatment needed; successful in vivo sciatic nerve stimulation & brain recording [15]. | 3D-printed circuits, on-skin e-tattoos, implantable bioelectrodes [15] [16]. |
| PEDOT:PSS (with additives) [16] | Conductivity up to ~4176 S/cm (when annealed) | Young's modulus tunable from kPa to MPa | High biocompatibility; minimizes foreign-body response [16] [17]. | Neural electrodes for brain monitoring and modulation [16] [18]. | |
| Biocompatible Elastomers | BIIR (Medical Grade) [7] | Semiconductor blend mobility maintained under strain | Young's modulus similar to human tissues (∼107.7 to 108.8 Pa); stable at 50% strain | In vivo studies show no major inflammatory response or tissue damage; meets ISO 10993 [7]. | Skin-like implantable transistors, logic circuits (inverters, NOR/NAND gates) [7]. |
| Hydrogels | PEGDA-GelMA [19] | Primarily ionic conduction | Elastic modulus suitable for soft tissues | Permissive glial layer, induces neovascularization, attracts neuronal progenitors [19]. | Regenerative scaffolds for brain lesions, tissue engineering [19]. |
| Metallic Biomaterials | Ti-6Al-4V (LPBF) [20] | N/A (Conductive substrate) | High strength and corrosion resistance | Good osseointegration; surface roughness and wettability critical for cell adhesion [20] [21]. | Orthopedic implants, load-bearing components, structural supports for bioelectronics [20]. |
Experimental Protocols for Biocompatibility Assessment
Rigorous biocompatibility assessment is paramount for the clinical translation of organic electronic materials. The following protocols detail key methodologies referenced in the literature.
In Vitro Cytotoxicity and Cell Viability Assay
This protocol assesses the short-term toxicological response of cells to material extracts or direct contact, as performed in studies on BIIR elastomers and neural probes [7] [18].
- Principle: To determine if leachable substances from a material affect cell survival, proliferation, and metabolic activity.
- Materials:
- Test Material: Sterilized samples of PEDOT:PSS film, BIIR blend, or other material.
- Cell Line: Relevant cell types such as human dermal fibroblasts, macrophages, or neuronal cell lines.
- Culture Reagents: Cell culture medium, fetal bovine serum, penicillin-streptomycin, phosphate-buffered saline.
- Assay Kits: AlamarBlue, MTT, or Live/Dead viability/cytotoxicity kit.
- Procedure:
- Extract Preparation: Incubate the sterile test material in cell culture medium at 37°C for 24 hours to create an extract. Use culture medium alone as a negative control.
- Cell Seeding: Seed cells in a 96-well plate at a standard density and allow them to adhere for 24 hours.
- Treatment: Replace the medium in the test wells with the material extract. Negative and positive control wells receive fresh medium and a cytotoxic substance, respectively.
- Incubation: Incubate the plate for 24-72 hours.
- Viability Measurement:
- Metabolic Activity: Add AlamarBlue reagent to each well, incubate for 2-4 hours, and measure fluorescence/absorbance.
- Live/Dead Staining: Incubate cells with calcein-AM and ethidium homodimer-1, then visualize under a fluorescence microscope.
- Data Analysis: Cell viability is expressed as a percentage relative to the negative control. A viability of >70-80% is typically considered non-cytotoxic.
In Vivo Implantation and Histological Evaluation
This protocol evaluates the chronic tissue response and functional integration of a material, as used in assessments of PEGDA-GelMA scaffolds and BIIR transistors [19] [7].
- Principle: To monitor the foreign body response, inflammation, and tissue remodeling over time following device implantation.
- Materials:
- Animal Model: Rats or mice, approved by an institutional animal care and use committee.
- Test Device: Sterilized bioelectronic device or material scaffold.
- Surgical Equipment: Stereotaxic apparatus for brain implants or standard surgical tools for subcutaneous implantation.
- Histology Reagents: Paraformaldehyde, sucrose, optimal cutting temperature compound, hematoxylin and eosin stain, antibodies for immunofluorescence.
- Procedure:
- Implantation: Anesthetize the animal and perform a sterile surgical procedure to implant the test material into the target site (e.g., brain, subcutaneous pocket). A sham surgery or inert material implant can serve as a control.
- Monitoring: Allow the animal to recover and monitor behavior and health for a predetermined period (e.g., 4-12 weeks).
- Perfusion and Tissue Harvest: At the endpoint, deeply anesthetize the animal and transcardially perfuse with saline followed by 4% paraformaldehyde. Excise the tissue containing the implant.
- Sectioning and Staining: Cryopreserve the tissue, section it using a microtome, and mount on slides. Perform staining:
- H&E Staining: For general morphology and identifying fibrotic capsules and inflammatory cell infiltration.
- Immunofluorescence: Use antibodies against markers like GFAP (astrocytes), Iba1 (microglia), CD68 (macrophages), and NeuN (neurons) to assess specific cellular responses.
- Data Analysis: Histological sections are scored semi-quantitatively for inflammation, fibrosis, and specific cell presence. A minimal glial scar, low macrophage activation, and presence of neurons near the interface indicate high biocompatibility [19].
Visualization of Experimental Workflows
The following diagram illustrates the key decision points and methodologies in the biocompatibility assessment pipeline for organic electronic materials.
Biocompatibility Testing Workflow for Organic Electronic Materials
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research and development in this field rely on a suite of specialized reagents and materials. The following table details key components and their functions.
Table 2: Essential Research Reagents and Materials for Biocompatible Electronics
| Reagent/Material | Function | Example Use-Case |
|---|---|---|
| PEDOT:PSS Colloids | Conductive polymer base for inks; provides mixed ionic-electronic conduction [15] [16]. | Formulation of 3D printable PILC inks for neural probes and e-tattoos [15]. |
| EMIM:TCB Ionic Liquid | Additive to enhance conductivity and induce phase separation in PEDOT:PSS [15]. | Creating highly conductive (286 S/cm), printable PEDOT:PSS colloids without post-treatment [15]. |
| Medical Grade BIIR | Biocompatible elastomer matrix for stretchable semiconductors; provides mechanical compliance [7]. | Fabrication of implantable field-effect transistors with stable performance under strain [7]. |
| DPPT-TT Semiconductor | Donor-acceptor polymer providing charge transport pathways within an elastomer matrix [7]. | Blending with BIIR to create a vulcanized, semiconducting nanofiber network for sOFETs [7]. |
| Phe-Phe Dipeptide | Biocompatible coating to mitigate inflammatory response and tissue rejection at the neural interface [18]. | Coating neural probes via PVD to improve signal-to-noise ratio and biocompatibility in vivo [18]. |
| GelMA (Gelatin Methacrylate) | Photopolymerizable, cell-adhesive hydrogel that promotes tissue integration [19]. | Combining with PEGDA to create biocompatible scaffolds for brain tissue regeneration [19]. |
| Ti-6Al-4V Powder | High-strength, biocompatible metal for structural components and implants [20]. | Laser Powder Bed Fusion (LPBF) 3D printing of patient-specific implant geometries [20]. |
The field of implantable electronics holds transformative potential for continuous health monitoring and therapeutic intervention. A significant challenge, however, lies in the fundamental mechanical mismatch between conventional rigid electronic components and soft, dynamic biological tissues. This mismatch can lead to tissue damage, chronic inflammation, and device failure, ultimately limiting the long-term efficacy of biomedical implants [7]. The extracellular matrix (ECM) of natural tissues is a complex, hydrated milieu that exhibits a wide range of mechanical properties, which are critical for regulating cell behavior, survival, and function [22]. Therefore, achieving tissue-level softness and stretchability is not merely an engineering goal but a biological imperative for seamless biointegration.
This guide objectively compares leading strategies developed to bridge this mechanical gap. By framing the discussion within the broader context of biocompatibility testing for organic electronic materials, we will analyze and compare specific approaches based on their achieved mechanical properties, underlying design principles, and experimental validation. The focus is on providing researchers and scientists with quantitative data and methodologies to inform the selection and development of materials for next-generation bioelectronic devices.
Quantitative Comparison of Mechanical Properties
The mechanical properties of biological tissues provide the critical benchmark for designing compatible electronics. The table below summarizes key mechanical metrics for natural tissues and state-of-the-art soft electronic devices.
Table 1: Mechanical Properties of Biological Tissues and Soft Electronic Devices
| Material / Tissue | Young's Modulus | Stretchability | Key Characteristics |
|---|---|---|---|
| Natural ECM Components [22] | Wide range (kPa to GPa) | Varies by component | Complex, hierarchical protein networks; dynamic and bioactive. |
| Collagen I [22] | Stiff structural protein | Low breaking strain | Gradual stiffening with increasing strain until failure. |
| Elastin [22] | Entropically elastic | High elasticity | Critical for energy storage in tissues like skin and lungs. |
| Conventional Elastomers (e.g., PDMS, SEBS) [23] | MPa range (∼0.5-3 MPa) | High | Orders of magnitude stiffer than most soft tissues. |
| BIIR-based Transistor [7] | ∼107.7 - 108.8 Pa (∼60-800 kPa) | Up to 100% strain | Medical-grade, biocompatible elastomer; stable electrical performance at 50% strain. |
| Soft-Interlayer Design [23] | < 10 kPa (e.g., 5.2 kPa) | > 100% strain | Generalizable design using an intermediate-modulus interlayer to achieve tissue-level softness. |
Analysis of Strategic Approaches
Approach 1: Intrinsically Soft and Biocompatible Elastomeric Composites
This strategy focuses on developing new electronic materials that are intrinsically soft by blending semiconductors with medically approved elastomers.
- Material Design: This approach utilizes a vulcanized blend of a semiconducting polymer (e.g., DPPT-TT) and a medical-grade bromo isobutyl–isoprene rubber (BIIR) elastomer. The surface energy disparity between the components leads to the formation of an interconnected semiconducting nanofiber network within the elastic BIIR matrix [7].
- Key Experimental Findings: Devices maintained stable electrical performance under 50% strain and showed excellent mechanical durability, with consistent mobility after 1,000 stretching cycles at 100% strain. In vitro assessments with human dermal fibroblasts and macrophages showed no adverse effects on cell viability, proliferation, or migration. In vivo implantation in mice showed no major inflammatory response or tissue damage [7].
- Advantages and Limitations:
- Advantages: High biocompatibility certified to ISO 10993 standards; excellent chemical and aging resistance; stable performance under strain.
- Limitations: The Young's modulus, while reduced, remains in the hundreds of kPa range, which is still higher than some ultra-soft tissues.
Approach 2: A Generalizable Soft-Interlayer Design
This approach is a device-level strategy that enables existing stretchable electronic materials with relatively high moduli to be integrated onto ultra-soft substrates.
- Mechanical Principle: A thin interlayer with an intermediate modulus (e.g., SEBS at 2.83 MPa) is inserted between the functional electronic film and an ultra-soft substrate (e.g., hydrogel or soft silicone). This interlayer suppresses stress concentration at defect sites in the electronic film during stretching by providing a more gradual mechanical transition, thereby drastically improving stretchability [23].
- Key Experimental Findings: The addition of a 1.2 μm-thick SEBS interlayer on a polyacrylamide (PAAm) hydrogel substrate resulted in an effective device modulus of 5.2 kPa—over two orders of magnitude lower than devices on conventional elastomers. This design enabled transistor arrays that maintained functionality under over 100% strain [23].
- Advantages and Limitations:
- Advantages: Achieves tissue-level moduli (< 10 kPa); generalizable to various conductors and semiconductors; improves conformability on dynamic, irregular surfaces.
- Limitations: Adds complexity to the device fabrication process; requires strong adhesion between all layers.
Experimental Protocols for Validation
Protocol: In Vitro Biocompatibility Assessment
This protocol is critical for evaluating the biological safety of new electronic materials as per ISO 10993 standards [7].
- Cell Culture: Use relevant cell lines, such as human dermal fibroblasts and macrophages.
- Direct Contact Test: Place sterilized samples of the electronic material (e.g., the BIIR/DPPT-TT blend film) in direct contact with cultured cells.
- Viability Assay: After a standard incubation period (e.g., 24-72 hours), perform a cell viability assay such as AlamarBlue or MTT to quantify metabolic activity.
- Proliferation Assay: Monitor cell proliferation over several days using DNA quantification or direct cell counting.
- Migration Assay: Use a scratch assay or similar method to assess if the material or its leachates affect cell migration.
- Analysis: Compare results against positive (e.g., tissue culture plastic) and negative (e.g., a toxic material) controls. A biocompatible material will show no significant adverse effects on viability, proliferation, or migration compared to the positive control [7].
Protocol: Mechanical and Electrical Performance Under Strain
This protocol evaluates the robustness of soft electronic devices during mechanical deformation [7] [23].
- Device Fabrication: Fabricate the stretchable electronic device (e.g., a transistor or conductor) on a stretchable substrate.
- Mounting on Stretcher: Mount the device on a uniaxial or biaxial mechanical stretcher integrated with electrical measurement probes.
- Baseline Measurement: Record the baseline electrical performance (e.g., conductivity for electrodes, mobility and ON/OFF ratio for transistors).
- Static Strain Test: Apply incremental static strains (e.g., 0%, 10%, 20%, ... up to 100%) and measure the electrical performance at each step.
- Cyclic Strain Test: Subject the device to repeated stretching cycles (e.g., 1,000 cycles at a set strain like 50% or 100%) while monitoring the electrical performance periodically to assess durability.
- Failure Analysis: Use techniques like optical microscopy or scanning electron microscopy (SEM) post-testing to inspect for microcracks or delamination.
Essential Research Reagent Solutions
The table below lists key materials used in the featured research for developing tissue-like soft electronics.
Table 2: Research Reagent Solutions for Soft Electronics
| Material / Reagent | Function in Research | Specific Example |
|---|---|---|
| Medical-Grade Elastomers | Biocompatible matrix for intrinsic soft composites; provides shock absorption and low reactivity. | Bromo Isobutyl–Isoprene Rubber (BIIR) [7]. |
| Conjugated Polymers | Provides semiconducting functionality; allows for charge transport in the soft device. | DPPT-TT [7] [23]. |
| Soft Interlayer Material | Enables ultra-soft devices by mitigating stress in functional layers on low-modulus substrates. | Polystyrene-ethylene-butylene-styrene (SEBS H1052) [23]. |
| Ultra-Soft Substrates | Mimics the mechanical environment of soft biological tissues for device integration. | Polyacrylamide (PAAm) Hydrogel, Ecoflex-0010 [23]. |
| Biocompatible Conductors | Create stretchable and corrosion-resistant interconnects and electrodes for implants. | Dual-layer Silver/Gold (Ag/Au) metallization [7]. |
Visualization of the Soft-Interlayer Mechanism
The following diagram illustrates the working mechanism of the soft-interlayer design, which allows high-modulus functional films to achieve excellent stretchability on ultra-soft substrates.
The pursuit of tissue-like softness and stretchability is a cornerstone of modern biocompatible electronics. Researchers have two powerful, validated strategies at their disposal: the development of new intrinsically soft and biocompatible composite materials, and the implementation of a generalizable soft-interlayer design. The choice between an intrinsic material solution versus a device-level engineering approach depends on the specific application requirements, including the target tissue's modulus, the necessary electrical performance, and fabrication constraints. The experimental protocols and data provided herein offer a framework for the objective comparison and further development of these technologies, paving the way for electronics that can seamlessly integrate with the human body for advanced diagnostics and therapies.
The emergence of bioelectronics represents a paradigm shift in medical devices, diagnostic tools, and therapeutic interventions. Unlike conventional electronics that operate exclusively in the realm of electron flow, bioelectronic devices must function within biological environments dominated by ionic charge carriers. This interface creates a fundamental challenge: establishing seamless communication between electronic systems (which conduct electrons and holes) and biological systems (which conduct ions such as Na⁺, K⁺, Ca²⁺, and Cl⁻). Organic electronic materials have emerged as the pivotal solution to this challenge due to their unique ability to conduct both electronic and ionic species, a property known as mixed ionic-electronic conduction [24].
The significance of this field extends across multiple domains, including implanted neural interfaces, wearable health monitoring devices, tissue engineering scaffolds, and sophisticated drug delivery systems [24]. For researchers and drug development professionals, understanding charge transport mechanisms in biological environments is essential for designing next-generation medical devices and therapeutic platforms. This guide provides a comprehensive comparison of charge transport mechanisms, experimental methodologies, and material considerations for developing effective bioelectronic interfaces, with particular emphasis on their biocompatibility testing context.
Fundamental Charge Transport Mechanisms: A Comparative Analysis
Electronic Versus Ionic Conduction
In biological environments, charge transport occurs through distinct yet sometimes interconnected mechanisms. Electronic conduction involves the movement of electrons and holes through extended states or hopping between localized states, while ionic conduction involves the movement of charged atoms or molecules through fluids, tissues, and materials [25]. Mixed ionic-electronic conductors (OMIECs) represent a special class of materials that can support both transport mechanisms simultaneously, making them particularly valuable for biointerfacing applications [26].
Table 1: Fundamental Properties of Charge Carriers in Biological Environments
| Property | Electronic Conduction | Ionic Conduction | Mixed Conduction |
|---|---|---|---|
| Charge Carrier | Electrons/Holes | Ions (Na⁺, K⁺, Ca²⁺, Cl⁻) | Both electrons and ions |
| Transport Mechanism | Band transport or hopping | Drift/diffusion in electrolytes | Coupled ionic-electronic transport |
| Speed | Fast (approaching speed of light) | Slow (limited by ion mobility) | Intermediate |
| Typical Mobility | 10⁻⁵ - 10 cm²/V·s [27] | 10⁻⁷ - 10⁻³ cm²/V·s [25] | Varies with composition |
| Temperature Dependence | Decreases with temperature | Increases with temperature | Complex dependence |
| Dominant in | Conventional electronics | Biological systems | Bioelectronic interfaces |
Material Classes for Bioelectronic Interfaces
Different material classes exhibit distinct charge transport properties that determine their suitability for biological applications. Understanding these differences is crucial for selecting appropriate materials for specific bioelectronic devices.
Table 2: Charge Transport Properties of Materials for Biological Environments
| Material Class | Example Materials | Charge Transport Mechanism | Key Characteristics | Biocompatibility Considerations |
|---|---|---|---|---|
| Organic Mixed Ionic-Electronic Conductors | PEDOT:PSS, PANI [24] | Mixed ionic-electronic conduction | High flexibility, biocompatibility, volumetric capacitance >30 F/cm³ [26] | Excellent biocompatibility; require leaching tests for residual monomers [28] |
| Inorganic Semiconductors | Silicon, Germanium [29] | Primarily electronic conduction | Rigid, band-like transport, high mobility (0.1-10 cm²/V·s) [27] | Often require surface modification for biocompatibility [21] |
| Bio-sourced Materials | Conductive protein fibers, eumelanin [30] [25] | Mixed protonic-electronic conduction | Sustainable, often contain mobile ions and protons | Naturally biocompatible; may require cross-linking |
| Metallic Biomaterials | Titanium alloys, Stainless Steel 316L [21] | Electronic conduction | High strength, excellent conductivity | Good corrosion resistance; potential metal ion release |
| Conductive Hydrogels | PEG-based hydrogels, conductive polymer composites | Primarily ionic with electronic pathways | High water content, tissue-like mechanical properties | Excellent biocompatibility; tunable degradation |
Experimental Characterization Methodologies
Electrical Transport Measurements
Characterizing charge transport in biological environments requires specialized methodologies that account for the unique properties of biological systems. DC electrical measurements provide foundational information about steady-state conductivity but cannot distinguish between different charge carrier types without complementary techniques [30]. For protein-based conductive materials like M13 bacteriophage and engineered aromatic curli fibers, time-domain analysis of DC measurements can reveal transient ionic transport phenomena alongside steady-state electronic conductivity [30].
Impedance spectroscopy extends these capabilities by measuring material response across a frequency spectrum, enabling researchers to deconvolute ionic and electronic contributions to overall conductivity. This technique is particularly valuable for characterizing OMIECs, where the volumetric capacitance (cᵥ) and electronic mobility (μₑ) jointly determine device performance [26]. The characteristic impedance (z₀) of OMIEC channels can be modeled using RC series circuits with the relationship z₀ = 1/(jωcᵥWtₕ) + (ρᵢₒₙtₕ)/W, where W is width, tₕ is thickness, and ρᵢₒₙ is ionic resistivity [26].
Biocompatibility Assessment Protocols
For materials intended for biological environments, comprehensive biocompatibility testing is essential according to ISO 10993 standards [21]. These assessments evaluate multiple aspects of material-biological system interactions:
- Cytotoxicity testing assesses material effects on cell viability and proliferation
- Sensitization assays evaluate potential allergic responses
- Irritation tests examine local inflammatory responses
- Systemic toxicity evaluation assesses material effects on entire organisms
- Implantation studies evaluate material performance in realistic biological environments over extended periods [21]
Materials characterization forms the foundation of biocompatibility assessment, beginning with chemical characterization through infrared analysis, aqueous physicochemical tests, and chromatographic methods to identify potential leachables [28]. These tests determine nonvolatile residue, residue on ignition, buffering capacity, and heavy metal content, establishing baseline material properties before biological testing [28].
Signaling Pathways and Transport Models
Signal Propagation in Mixed Conductors
In organic mixed ionic-electronic conductors (OMIECs), signal propagation involves complex interactions between electronic and ionic charge carriers. When a voltage is applied to an OMIEC channel immersed in an electrolyte, the moving potential front alters local charge distribution through ejection of mobile cations, which electrostatically couple with fixed acceptors in the material's ionic phase [26]. This process results in capacitive ionic currents flowing from the OMIEC layer into the surrounding electrolyte, dissipating a portion of the electronic current traveling along the channel.
The propagation of electrical signals through mixed-conducting channels can be modeled using a transmission line model derived from the drift-diffusion equations [26]. This model describes how voltage signals travel through OMIEC thin films with specific length (L), width (W), and thickness (tₕ) parameters. The propagation constant (γ) is defined as γ = √(r₀/z₀) = √[(jωcᵥρₑₗ)/(1+jωcᵥρᵢₒₙtₕ²)], where r₀ is electronic resistance per unit length, z₀ is characteristic impedance, ω is frequency, cᵥ is volumetric capacitance, and ρₑₗ and ρᵢₒₙ are electronic and ionic resistivities, respectively [26].
Biological Signal Transduction Pathways
In biological systems, signal transduction involves conversion between ionic and electrical signals. Voltage-gated ion channels in excitable cells (neurons, muscle cells) open in response to membrane potential changes, allowing specific ions to flow down their electrochemical gradients [24]. This ionic flux alters the local membrane potential, propagating signals along cell membranes. Bioelectronic interfaces interact with these native signaling pathways through multiple mechanisms:
- Capacitive coupling involves displacement currents from ionic charge redistribution
- Faradaic coupling involves electron transfer across the electrode-electrolyte interface
- Electrostatic modulation uses applied electric fields to influence channel gating
- Electrothermal effects leverage localized heating to alter membrane properties
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research into charge transport in biological environments requires specialized materials and characterization tools. The following table outlines essential components of the experimental toolkit for researchers in this field.
Table 3: Research Reagent Solutions for Charge Transport Studies in Biological Environments
| Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Conductive Polymers | PEDOT:PSS, PANI [24] | Mixed ionic-electronic conduction for biointerfaces | Require purification to remove cytotoxic synthetic byproducts |
| Bio-sourced Materials | M13 bacteriophage, engineered curli fibers [30] | Sustainable bioelectronic materials | Exhibit both transient ionic and steady-state electronic transport |
| Characterization Electrodes | Interdigitated micro-electrodes, Ag/AgCl reference electrodes [30] | DC and AC electrical characterization | Electrode geometry affects current distribution and field lines |
| Electrolytes | Phosphate buffered saline (PBS), artificial cerebrospinal fluid (aCSF) | Simulating biological environments | Ionic composition affects charge transport mechanisms |
| Biocompatibility Assessment Tools | Cell culture models, extraction fluids [21] [28] | Evaluating biological safety | Include both aqueous and alcohol extracts for comprehensive profiling |
| Structural Characterization | FTIR, HPLC, GC-MS [28] | Material composition and purity analysis | Identify potentially cytotoxic leachables and degradation products |
Performance Comparison and Optimization Strategies
Key Performance Metrics Across Material Systems
Evaluating bioelectronic materials requires multidimensional assessment across electronic, ionic, mechanical, and biological compatibility parameters. The following comparative analysis highlights trade-offs and optimization opportunities across material classes.
Table 4: Comprehensive Performance Comparison of Bioelectronic Materials
| Performance Metric | Organic Mixed Conductors | Inorganic Semiconductors | Bio-sourced Materials | Metallic Biomaterials |
|---|---|---|---|---|
| Electronic Mobility (cm²/V·s) | 10⁻⁵ - 10⁻¹ [27] | 0.1 - 10 [27] | <10⁻³ [25] | >1 |
| Ionic Conductivity (S/cm) | 10⁻³ - 10⁻¹ | <10⁻⁶ | 10⁻⁵ - 10⁻² [25] | Not applicable |
| Young's Modulus (GPa) | 0.001 - 1 [24] | 50 - 200 | 0.1 - 10 | 100 - 200 |
| Biocompatibility | Excellent [24] | Good with surface modification | Excellent [25] | Good (varies by alloy) |
| Stability in Physiological Environments | Months to years | Years | Days to months | Years to decades |
| Signal Propagation Speed | Intermediate [26] | Fast | Slow | Fast |
| Tunability | High through side-chain engineering | Limited | Moderate through genetic engineering | Limited |
Optimization Strategies for Enhanced Performance
Based on current research, several strategies have emerged for optimizing charge transport in biological environments:
- Molecular engineering of conjugated polymers with ethylene glycol side chains enhances ion uptake and volumetric capacitance, critical figures of merit for OMIEC performance [26]
- Nanostructuring of conductive materials increases surface area-to-volume ratios, improving interfacial contact with biological tissues
- Composite material systems combine advantageous properties of individual components, such as conductive polymers with hydrogels for enhanced ionic transport
- Surface functionalization with biological recognition elements (peptides, enzymes) facilitates specific interactions with target tissues
- Device geometry optimization balances signal propagation speed with energy dissipation, guided by transmission line models [26]
For researchers developing new bioelectronic materials, the most successful approaches often involve iterative design cycles that combine computational modeling of charge transport with empirical biocompatibility assessment. This integrated methodology ensures that materials meet both electronic performance requirements and biological safety standards essential for clinical translation.
Methodologies and Applications: From ISO Standards to Advanced Testing Platforms
The ISO 10993 series, developed by the International Organization for Standardization (ISO) Technical Committee 194, provides a globally harmonized framework for evaluating the biological safety of medical devices [6]. As medical devices increasingly incorporate advanced materials like organic electronic components, this standard offers the foundational principles for assessing their biocompatibility within a structured risk management process [3]. The evaluation process mandated by ISO 10993-1 requires manufacturers to identify, assess, and manage biological risks associated with device materials, design choices, and tissue contact during intended use [3]. For researchers developing implantable organic electronics, this standard provides the critical pathway for demonstrating device safety and achieving regulatory compliance across international markets [7] [31].
The significance of this framework has grown with the recent publication of ISO 10993-1:2025, which represents a substantial evolution from the 2018 version [32] [33]. This latest revision further aligns the biological evaluation process with the risk management principles of ISO 14971, emphasizing a more science-based approach that can reduce unnecessary animal testing while ensuring patient safety [3] [6]. For the field of organic bioelectronics, where materials must seamlessly interface with biological tissues, understanding this framework is not merely a regulatory requirement but a fundamental component of responsible device development [7] [34].
Core Principles and Key Updates in ISO 10993-1:2025
Risk Management Integration
The 2025 revision of ISO 10993-1 establishes a tighter connection with ISO 14971, making biological evaluation a dedicated component within the overall risk management process [32]. The standard now explicitly requires the identification of biological hazards, definition of biologically hazardous situations, and establishment of potential biological harms [32]. This alignment extends to requiring biological risk estimation based on the severity and probability of harm, mirroring the methodology described in ISO 14971 [32]. The updated framework introduces a structured biological evaluation process that follows ISO 14971's lifecycle approach, ensuring biological safety is assessed continuously from design through post-market surveillance [32].
Practical Application Considerations
The revised standard introduces several important practical changes that affect how biological evaluations are planned and executed. Reasonably foreseeable misuse must now be considered during device categorization, including scenarios such as "use for longer than the period intended by the manufacturer" [32]. The determination of exposure duration has been refined with new definitions for "total exposure period," "contact day," "daily contact," and "intermittent contact," replacing the previous approach of simply summing contact seconds [32]. Additionally, the standard introduces new considerations for bioaccumulation, stating that if a chemical known to bioaccumulate is present in the device, the contact duration should be considered long-term unless otherwise justified [32].
Table 1: Key Changes in ISO 10993-1:2025 Revision
| Aspect | ISO 10993-1:2018 | ISO 10993-1:2025 | Impact on Organic Electronics Research |
|---|---|---|---|
| Risk Management Integration | General alignment with ISO 14971 | Tightly integrated framework with specific biological risk estimation requirements | Requires more rigorous documentation of risk-benefit analysis for novel materials |
| Device Categorization | Based on nature of body contact & duration | Simplified contact groups; eliminated externally communicating devices category | Streamlined classification for implantable organic electronics |
| Foreseeable Misuse | Focused primarily on intended use | Must consider systematic misuse scenarios | Broader safety assessment for wearable/organic electronic devices |
| Exposure Duration Determination | Used "transitory" for very brief contact | "Very brief contact" remains; any contact >1 minute defaults to one-day exposure | Important for transient organic electronic devices that may have short but repeated contact |
| Systemic Toxicity Evaluation | Based on contact duration and nature | Should reflect duration of use | Critical for biodegradable organic electronic implants |
| Genotoxicity Assessment | Required for certain contact categories | Now applies to all devices with prolonged contact (unless intact skin only) | Expanded testing likely needed for most implantable organic electronic materials |
The "Big Three" Biocompatibility Tests: Foundation of Safety Assessment
Cytotoxicity Testing
Cytotoxicity testing evaluates whether a medical device's materials or components can cause damage to living cells, serving as the first line of screening in biological safety assessment [6]. According to ISO 10993-5:2009, this testing typically involves exposing cultured mammalian cells (such as Balb 3T3, L929, or Vero cell lines) to extracts of the medical device for approximately 24 hours [6]. The methodology involves preparing device extracts using appropriate solvents (physiological saline, vegetable oil, or cell culture medium) under standardized conditions, then exposing the cells to these extracts [6]. Key assessment endpoints include cell viability (measured via MTT, XTT, or neutral red uptake assays), morphological changes, cell detachment, and cell lysis [6]. While ISO 10993-5 doesn't define strict acceptance criteria, cell survival of 70% or higher is generally considered a positive indicator, particularly when testing neat extract [6].
Irritation and Sensitization Testing
Irritation testing assesses the localized inflammatory response that can occur at the contact site between a device and body tissues, while sensitization testing evaluates the potential for materials to cause allergic reactions [6]. These tests are particularly relevant for organic electronic devices that may incorporate novel polymers, elastomers, or conductive materials that have not been previously used in medical applications. The experimental protocols for these assessments may utilize in vitro methods, though the medical device industry has been slower to adopt alternatives to animal testing compared to other sectors [6]. For organic electronic materials, which often contain complex aromatic compounds or metal nanoparticles, thorough irritation and sensitization assessment is crucial for identifying potential biological reactions before clinical use.
Table 2: The "Big Three" Biocompatibility Tests for Medical Devices
| Test Type | Purpose | Standard Methods | Key Endpoints | Relevance to Organic Electronics |
|---|---|---|---|---|
| Cytotoxicity | Assess cell damage potential | ISO 10993-5:2009; In vitro cell culture | Cell viability, Morphological changes, Cell detachment | Critical for ensuring novel semiconductors and elastomers aren't toxic to surrounding tissues |
| Irritation | Evaluate localized inflammatory response | In vitro and in vivo models | Tissue inflammation, Erythema, Edema | Important for wearable organic electronics and implantable devices with sustained tissue contact |
| Sensitization | Assess allergic reaction potential | Guinea pig maximization, Local lymph node assay | Allergic response, Immune activation | Essential for devices containing potential allergens like certain metals or organic compounds |
Application to Organic Electronic Materials Research
Biocompatibility Challenges in Organic Bioelectronics
Organic electronic materials present unique biocompatibility challenges that require careful consideration within the ISO 10993 framework. While these materials offer advantageous properties like flexibility, softness, and compatibility with biological tissues, their complex chemical structures and potential degradation products necessitate thorough safety assessment [34]. Traditional inorganic semiconductors face issues of mechanical mismatch with biological tissues, potentially leading to tissue damage, inflammation, fibrosis, and necrosis over time [7]. Although organic semiconductors better match the mechanical properties of tissues, many industrial-grade elastomers used in stretchable organic field-effect transistors (sOFETs) are not certified for biocompatibility and may induce chronic foreign body reactions [7].
Recent research has demonstrated promising approaches to these challenges. The development of elastomeric organic transistors using medical-grade bromo isobutyl–isoprene rubber (BIIR) blended with semiconducting polymers shows how material selection can enhance both performance and biocompatibility [7]. These devices have exhibited stable electrical performance under mechanical strain (up to 50% elongation) while demonstrating compatibility with human dermal fibroblasts and macrophages in vitro, and showing no major inflammatory response or tissue damage in mouse implantation studies [7]. Such advances highlight how the ISO 10993 framework guides the development of safer organic electronic implants through systematic biological evaluation.
Material Selection and Characterization Strategies
Successful biological evaluation of organic electronic devices begins with strategic material selection. Medical-grade elastomers like BIIR, which meet stringent biocompatibility standards set by ISO 10993 and European Pharmacopoeia, provide advantageous starting points for device development [7]. These materials offer excellent mechanical properties including shock absorption, low permeability, aging resistance, and high physical strength, alongside high chemical resistance and low reactivity with microorganisms [7]. The material characterization process for organic electronic devices should include thorough analysis of potential leachables and degradation products, particularly for devices intended for long-term implantation where bioaccumulation potential must be assessed [32].
Experimental Protocols for Biocompatibility Assessment
Cytotoxicity Testing Protocol (Based on ISO 10993-5)
The standardized methodology for cytotoxicity testing provides a reproducible approach for evaluating organic electronic materials. The extraction process involves immersing the test material in extraction solvents (such as physiological saline and vegetable oil) at a surface area-to-volume ratio of 3-6 cm²/mL, then incubating at 37°C for 24 hours [6]. The cell culture preparation requires seeding appropriate mammalian cell lines (L929 fibroblasts are commonly used) in 96-well plates and incubating until approximately 80% confluent [6]. For the extract exposure, culture medium is replaced with device extracts (neat and diluted) and incubated for 24±2 hours at 37°C in a 5% CO₂ atmosphere [6]. The viability assessment typically uses the MTT assay, where yellow MTT tetrazolium salt is reduced to purple formazan in metabolically active cells; absorbance is measured at 570 nm, with cell viability calculated as a percentage of negative control values [6].
In Vivo Implantation Study Protocol
For implantable organic electronic devices, in vivo assessment provides critical safety data not obtainable through in vitro methods. The sample preparation involves sterilizing test and control materials using validated methods that don't alter material properties [7]. The surgical implantation typically uses rodent models, with materials implanted subcutaneously or in muscle pockets according to standardized surgical protocols [7]. The study duration depends on the intended use of the device, with explanation timepoints at 1, 4, 12, and 26 weeks to assess tissue response over time [7]. The histopathological evaluation involves embedding explanted tissues in paraffin, sectioning, and staining with hematoxylin and eosin (H&E) for evaluation of inflammatory cell response, fibrosis, necrosis, and tissue integration [7]. A scoring system is used to semi-quantitatively assess the biological response, comparing test articles to negative and positive controls [7].
Table 3: Essential Research Reagents for Biocompatibility Testing of Organic Electronics
| Reagent/Cell Line | Function in Biocompatibility Assessment | Application Example | Standard Reference |
|---|---|---|---|
| L929 Fibroblast Cell Line | In vitro cytotoxicity testing | Assessment of cell viability after exposure to device extracts | ISO 10993-5 [6] |
| Physiological Saline | Polar extraction solvent | Extraction of hydrophilic compounds from organic electronic devices | ISO 10993-12 [6] |
| Vegetable Oil | Non-polar extraction solvent | Extraction of lipophilic compounds from organic electronic devices | ISO 10993-12 [6] |
| MTT Tetrazolium Salt | Cell viability indicator | Quantitative measurement of metabolic activity in cytotoxicity testing | ISO 10993-5 [6] |
| Medical-Grade Elastomers (BIIR) | Biocompatible substrate material | Creating stretchable semiconductor films for implantable transistors [7] | ISO 10993-1 [7] |
| Dulbecco's Modified Eagle Medium (DMEM) | Cell culture medium | Maintaining cell cultures during extract exposure studies | ISO 10993-5 [6] |
The ISO 10993 series provides an essential framework for navigating the complex biological evaluation requirements for medical devices, with particular relevance for the emerging field of organic bioelectronics. The recently published ISO 10993-1:2025 standard reinforces the risk-based approach to biological safety assessment, offering a more structured pathway for evaluating novel materials and devices [32] [33]. For researchers developing organic electronic implants, understanding this framework is not merely a regulatory hurdle but a fundamental component of responsible device development that ensures patient safety while facilitating global market access [3] [31].
Successful implementation requires early integration of biological safety considerations into the material selection and device design process, thorough chemical characterization to identify potential biological risks, and strategic testing that addresses both standard requirements and device-specific considerations [32] [6]. As the field advances, the continued development of alternative testing methods that reduce animal use while maintaining scientific rigor will be essential for addressing the unique challenges posed by organic electronic materials [6]. By embracing the structured approach provided by the ISO 10993 series, researchers can more efficiently translate innovative organic electronic technologies from laboratory concepts to clinically viable medical devices.
The development of safe and effective organic electronic medical devices, from implantable neural interfaces to smart wound dressings, hinges on rigorous biocompatibility testing [35] [36]. For researchers and drug development professionals, demonstrating that these novel materials do not provoke adverse biological reactions is a critical step in the translation from laboratory to clinical application. The international standard ISO 10993 series provides the foundational framework for this evaluation, mandating a risk-based assessment strategy [37] [38]. Within this framework, three core in vitro tests—cytotoxicity, sensitization, and irritation—form an essential triad of preliminary safety assessments required for almost all medical devices [6] [39]. This guide objectively compares the methodologies, experimental data, and protocols for these "Big Three" assays, providing a vital reference for the safety evaluation of innovative organic electronic materials.
The "Big Three" tests are considered fundamental because they screen for the most immediate and critical biological risks: cell death, allergic response, and localized inflammation [6]. Cytotoxicity assesses whether a material or its extracts are toxic to living cells, potentially causing cell death or inhibiting cell growth [39]. Sensitization evaluates the potential of a material to cause an allergic reaction, specifically a delayed (Type IV) hypersensitivity response, upon repeated exposure [37] [39]. Irritation testing determines if a material causes localized, reversible inflammatory effects on skin or other tissues, without involving the immune system in an allergic capacity [39]. The transition towards New Approach Methodologies (NAMs), including validated in vitro and in silico methods, is a key trend driven by ethical imperatives, scientific innovation, and regulatory support, such as the U.S. FDA Modernization Act 2.0 [37].
Table 1: Core Comparison of the "Big Three" Biocompatibility Tests
| Test Endpoint | Primary Objective | Governing ISO Standard | Commonly Used In Vitro Methods | Key Measured Parameters |
|---|---|---|---|---|
| Cytotoxicity | To determine if a material causes toxicity to cells, leading to cell death or inhibited growth [39]. | ISO 10993-5 [6] [39] | MEM Elution Test, MTT/XTT Assay, Direct Contact, Agar Diffusion [38] [40] | Cell viability (%), morphological changes, cell lysis, detachment [6] [39] |
| Sensitization | To assess the potential to induce a delayed-type (Type IV) allergic skin reaction [37] [39]. | ISO 10993-10 [37] [38] | GARDskin Medical Device, Direct Peptide Reactivity Assay (DPRA), h-CLAT [37] | Lymphocyte proliferation, peptide reactivity, biomarker expression (e.g., CD86) [37] |
| Irritation | To evaluate the potential for a material to cause localized, reversible skin or mucosal inflammation [39]. | ISO 10993-23 [37] [38] | Reconstructed Human Epidermis (RhE) models [37] | Cell viability (%), release of inflammatory mediators (e.g., IL-1α, IL-6, IL-8, PGE2) [37] |
Detailed Experimental Protocols and Data Analysis
Cytotoxicity Testing (ISO 10993-5)
Experimental Protocol: MTT Assay for Cytotoxicity The MTT assay is a widely used quantitative method for assessing cell viability and metabolic activity [41].
- Sample Preparation: Prepare an extract of the test material (organic electronic film, polymer, etc.) as per ISO 10993-12. Typically, the material is immersed in a cell culture medium (e.g., DMEM) supplemented with serum (e.g., 5-10% Fetal Bovine Serum) to solubilize both polar and non-polar constituents. Extraction is performed at 37°C for 24 hours (devices with contact ≤24 hours) or 72 hours (devices with prolonged contact) [40].
- Cell Culture: Seed a mammalian cell line, such as L-929 mouse fibroblasts or Vero cells, into a multi-well culture plate and incubate until a confluent monolayer forms [6] [41].
- Exposure: Replace the culture medium in the wells with the prepared extract fluid. Include control wells with culture medium only (negative control) and a known cytotoxic agent, such as zinc diethyldithiocarbamate (ZDEC) or benzalkonium chloride (BAK) (positive control) [42].
- Incubation: Incubate the cells in the extract for 24 to 72 hours at 37°C with 5% CO₂ [40].
- MTT Application: After incubation, add the MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) to each well. Living cells with active mitochondria reduce the yellow MTT to insoluble purple formazan crystals [41].
- Solubilization and Measurement: Dissolve the formazan crystals with an organic solvent like isopropanol or DMSO. Measure the absorbance of the solution at a wavelength of around 492 nm using a spectrophotometer [41].
- Data Analysis: Calculate cell viability as a percentage compared to the negative control group [40].
Cell Viability (%) = (Absorbance of Test Sample / Absorbance of Negative Control) × 100
Data Interpretation and Experimental Results A material is generally considered non-cytotoxic if cell viability is ≥ 70% for the MTT/XTT test [40]. The MEM Elution test, a qualitative method, involves microscopic evaluation of cell morphology and reactivity, where a score of 0 (no reactivity) to 4 (severe reactivity) is assigned; a score of 2 or less is typically acceptable [40]. Experimental data from a study on a Mg-1%Sn-2%HA composite for implants demonstrated a dose-response relationship, where cell viability of L-929 fibroblasts increased with extract dilution: 71.51% (undiluted), 84.93% (50%), 93.20% (25%), and 96.52% (12.5%), confirming its non-cytotoxic nature [41].
Cytotoxicity MTT Assay Workflow
Sensitization Testing (ISO 10993-10)
Experimental Protocol: GARDskin Medical Device Assay This NAM is an in vitro method that assesses the key initial steps in the skin sensitization pathway [37].
- Principle: The assay exposes a human-derived dendritic-like cell line to the test substance and uses genomics to measure changes in the expression of a biomarker signature associated with the sensitization process [37].
- Sample Exposure: Prepare extracts of the test material using both polar (e.g., saline) and non-polar (e.g., vegetable oil) vehicles as per ISO 10993-12. The GARDskin assay is designed to test these medical device extracts directly [37].
- Cell Culture and Dosing: Culture the proprietary cell line and expose it to the test extract for a defined period.
- RNA Extraction and Analysis: After exposure, extract RNA from the cells and analyze it using a targeted RNA-Seq platform to quantify the expression of the genomic biomarker signature.
- Prediction Model: The gene expression profile is evaluated using a previously trained prediction model to classify the test material as a sensitizer or non-sensitizer.
Data Interpretation and Regulatory Status The output is a binary prediction (Sensitizer/Non-Sensitizer). These in vitro sensitization methods, including GARDskin, DPRA, and h-CLAT, are recognized in Annex C of ISO 10993-10 as valid alternatives. Ongoing efforts aim to integrate them fully into the normative sections of the standard [37]. This shift is crucial for organic electronics research, as it provides a human-relevant, mechanistic understanding of sensitization potential without the ethical and interspecies extrapolation concerns of traditional animal models like the Guinea Pig Maximization Test (GPMT) or Murine Local Lymph Node Assay (LLNA) [37] [39].
Irritation Testing (ISO 10993-23)
Experimental Protocol: Reconstructed Human Epidermis (RhE) Model Validated in vitro skin models, such as EpiDerm or EpiSkin, are now formally recognized for irritation testing [37].
- Sample Preparation: Apply the test material or its extract directly onto the surface of the 3D RhE model. A negative control (e.g., saline) and a positive control (e.g., Triton X-100) are run in parallel.
- Exposure and Post-Treatment: The test substance remains in contact with the tissue for a defined period (e.g., 1 hour). The tissue is then rinsed, and post-treatment medium is added.
- Cell Viability Measurement: After a total incubation period (e.g., 42 hours), tissue viability is determined using the MTT assay. The MTT is added, and the resulting formazan salt is extracted and measured spectrophotometrically.
- Cytokine Analysis (Optional): The post-treatment culture medium can be collected and analyzed for the release of pro-inflammatory cytokines such as IL-1α, IL-6, IL-8, and PGE2, providing a more comprehensive profile of the inflammatory response [42].
Data Interpretation According to ISO 10993-23, if the tissue viability relative to the negative control is below 50%, the test material is classified as an irritant. If viability is above 50%, it is classified as a non-irritant [37]. Research on silicone materials treated with toxins like ZDEC and BAK shows that irritation can also be characterized by a change in the release profile of inflammatory cytokines, which may not always linearly correlate with the reduction in cell metabolic activity [42].
In Vitro Irritation Test Workflow
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Research Reagents for In Vitro Biocompatibility Testing
| Reagent / Material | Function in Assays | Specific Examples & Notes |
|---|---|---|
| Mammalian Cell Lines | In vitro model systems for cytotoxicity and metabolic activity assessment [6]. | L-929 (mouse fibroblasts), Balb/3T3, Human Lens Epithelial Cells (HLEC), Vero cells [6] [42]. |
| Cell Culture Media & Supplements | Provides nutrients for cell growth and acts as a polar extraction vehicle [41] [40]. | Dulbecco's Modified Eagle Medium (DMEM), supplemented with Fetal Bovine Serum (FBS) to aid extraction of non-polar constituents [41] [40]. |
| Viability/Cytotoxicity Assay Kits | Quantify cell health, proliferation, or death via colorimetric, fluorometric, or luminometric readouts [41]. | MTT, XTT, AlamarBlue (Resazurin), Neutral Red Uptake, Lactate Dehydrogenase (LDH) Assay [6] [41] [42]. |
| Reconstructed Human Epidermis (RhE) | 3D in vitro model for replacement of animal-based skin irritation testing [37]. | Commercially available tissues (EpiDerm, EpiSkin). Viability is measured via MTT assay [37]. |
| In Vitro Sensitization Assays | Mechanistic, non-animal methods to predict the skin sensitization potential of chemicals and extracts [37]. | GARDskin Medical Device, Direct Peptide Reactivity Assay (DPRA), h-CLAT [37]. |
| Cytokine Detection Kits | Measure the release of inflammatory mediators to profile the immune response to a material [42]. | Multiplex immunoassays (e.g., Mesoscale Discovery platform) for IL-1β, IL-6, IL-8, TNF-α [42]. |
| Reference Control Materials | Verify assay performance and responsiveness [42]. | Negative Control: High-Density Polyethylene (HDPE); Positive Control: ZDEC, BAK, Triton X-100 [42]. |
For researchers pioneering organic electronic materials, a deep understanding of the "Big Three" in vitro biocompatibility tests is indispensable. Cytotoxicity, sensitization, and irritation assays provide the first critical line of evidence that a new material is safe for biological contact. The experimental data and protocols outlined here demonstrate a clear industry movement towards human-relevant New Approach Methodologies (NAMs), which offer greater biological insight, reduced ethical concerns, and alignment with evolving global regulations like the EU MDR and FDA guidance [37] [40]. By integrating these standardized, robust testing strategies early in the R&D pipeline, scientists can de-risk the development pathway and accelerate the arrival of safe, advanced bioelectronic devices to the market.
The development of implantable organic electronic devices, from neural interfaces to health monitors, hinges on a critical step: comprehensive biocompatibility assessment. For researchers and drug development professionals, evaluating the local effects of these materials through implantation tests and histopathological analysis is paramount for ensuring patient safety and regulatory approval. These tests determine how the body responds at the tissue level to implanted materials, predicting long-term integration success and identifying potential failure modes. The mechanical and chemical properties of organic semiconductors—including their softness, flexibility, and mixed ionic-electronic conduction—make them particularly promising for biomedical applications, as they more closely match biological tissues than traditional rigid electronics [2]. However, their novel chemistries necessitate rigorous biological evaluation according to established international standards, primarily ISO 10993, which provides the framework for assessing the local effects of implantable materials [2] [43].
This guide compares key methodological approaches for implantation testing and subsequent histopathological analysis, providing experimental protocols and data comparison frameworks essential for researchers working at the intersection of organic electronics and medical device development.
Fundamentals of Implantation Testing
Implantation testing evaluates the local effects of biomaterials on surrounding living tissue. These tests are conducted by surgically implanting material samples into appropriate animal models, then retrieving the samples and surrounding tissue for analysis after predetermined periods. The ISO 10993-6 standard provides the core framework for these evaluations, specifying test durations based on intended clinical application and categorizing devices based on contact type (surface, external communicating, or implant) and contact duration (limited, prolonged, or permanent) [2] [43].
When a biomaterial is implanted, it interacts with biological tissues in one of four primary ways: toxic responses cause cell death and inflammation; bioinert materials have minimal interaction but may become encapsulated; bioactive materials form intimate connections with host tissue; and bioresorbable materials gradually dissolve and are replaced by native tissue [2]. The goal for most organic electronic implants is to achieve either bioinert or bioactive responses, minimizing fibrous encapsulation that could impair device function over time.
Table 1: Tissue Response Categories in Implantation Testing
| Response Type | Key Characteristics | Impact on Device Function |
|---|---|---|
| Toxic | Cell death, immunological response, inflammation | Device rejection or failure |
| Bioinert | Minimal interaction, potential fibrous encapsulation | Potential signal attenuation over time |
| Bioactive | Intimate connection with host tissue | Stable long-term interface |
| Bioresorbable | Material dissolves and is replaced by host tissue | Temporary function only |
The duration of implantation studies depends on the material's intended use and degradation profile, ranging from acute (≤ 10 days) to chronic (weeks, months, or years) [2]. For permanent implants, long-term studies extending 6-12 months or longer are typically required to assess chronic tissue response and material stability.
Histopathological Analysis as the Gold Standard
Histopathological analysis provides the definitive method for evaluating local tissue effects following implantation. This microscopic examination of harvested tissue remains the gold standard for diagnosing tissue response, inflammation, and healing processes [44] [45]. The process involves fixing, dehydrating, embedding, sectioning, and staining tissue samples containing the implant and surrounding structures, then systematically evaluating them for signs of toxicity, inflammation, fibrosis, and tissue integration.
The analytical power of histopathology lies in its ability to characterize both architectural features and cellular morphology. Pathologists assess multiple parameters, including: type and origin of tissue response; presence of inflammatory cells; vascular changes; fibrous capsule formation; and criteria of malignancy when appropriate [44]. Different staining protocols reveal distinct tissue elements: Hematoxylin and Eosin (H&E) provides overall cellular structure; Masson's Trichrome distinguishes connective tissue; toluidine blue highlights bone morphology; and specialized stains identify specific cell types like osteoclasts or macrophages [45].
A critical consideration in histopathological assessment is its inherent subjectivity, with documented interobserver variability in interpretation [44]. Studies comparing first and second opinions found partial disagreements (changes to grade or subtype) in 20-34% of cases, and complete disagreements (changes between benign and malignant or different diagnoses) in 10-19% of cases [44]. These discrepancies significantly altered prognosis or treatment in 17-39% of cases, highlighting the importance of multiple reviews when clinical and histopathological findings diverge.
Comparative Analysis of Testing Methodologies
Implant Site Preparation Techniques
The method used to create implant sites significantly influences subsequent tissue response and healing capacity. Conventional drilling remains widely used but causes measurable histological changes including microcracks, uneven bone margins, osteocyte damage, and thermal injury [46]. Controlled studies comparing drilling parameters reveal that rotational speed and cooling techniques dramatically affect bone bed quality.
Table 2: Comparison of Implant Site Preparation Methods
| Method | Key Histological Findings | Advantages | Limitations |
|---|---|---|---|
| Conventional Drilling | Microcracks, thermal damage, irregular margins | Efficiency, predictability | Potential osteonecrosis |
| Piezoelectric Surgery | Fewer microcracks, minimal inflammation | Precision, reduced trauma | Longer procedure time |
| Laser Preparation | Minimal debris, antibacterial effects | Minimal thermal spread | Specialized equipment |
| Osteodensification | Denser bone formation, compaction | Enhanced primary stability | Technique sensitivity |
Recent research demonstrates that alternative techniques (piezoelectric, laser, osteodensification) generally produce superior histological outcomes compared to conventional drilling, with fewer microcracks, reduced inflammation, and denser, more regular bone formation [46]. However, drilling with optimized parameters—particularly lower rotational speeds (800-1200 rpm) with effective cooling—can minimize adverse effects [47]. One study found the Hiossen ET system achieved optimal bone bed quality at 1200 rpm with 4°C saline cooling, producing smooth osteotomy walls with minimal thermal damage (p = 0.003), while the Paltop system performed best at 800 rpm with similar cooling, reducing tissue compression and microcracks (p = 0.012) [47].
Material-Specific Tissue Responses
Different implant materials elicit distinct tissue responses that histopathological analysis can quantify. Traditional inorganic materials like silicon often trigger chronic foreign body responses, leading to fibrous encapsulation that increases impedance at the electrode-tissue interface [2]. In contrast, appropriately engineered organic electronic materials can achieve superior biocompatibility.
Comparative studies between different surface technologies demonstrate measurable differences in tissue integration. Research comparing oxidized (OX) implants versus hydrophilic sand-blasted and acid-etched (HSBA) surfaces found significantly higher bone-implant contact (BIC) for HSBA implants after 10 days (p < 0.01), though OX implants showed higher BIC after 6 weeks (p < 0.001) [48]. The HSBA implants also demonstrated higher shear strength after 3 weeks (p < 0.001) and 6 weeks (p < 0.01), suggesting faster early-stage integration [48].
Advanced organic electronic materials show particular promise. Recent developments in elastomeric organic field-effect transistors using blends of semiconducting nanofibers and biocompatible elastomers (specifically bromo isobutyl-isoprene rubber, BIIR) exhibit Young's modulus values similar to human tissues (approximately 10⁷·⁷ Pa to 10⁸·⁸ Pa), significantly reducing mechanical mismatch [7]. In vivo implantation studies of these devices in mice showed no major inflammatory response or tissue damage, indicating excellent biocompatibility potential for next-generation implantable electronics [7].
Experimental Protocols and Workflows
Standardized Implantation Test Protocol
The following protocol for implantation testing with histopathological analysis aligns with ISO 10993-6 requirements and can be adapted for evaluating organic electronic materials [43]:
Sample Preparation: Prepare test materials in clinically relevant form and sterilization. For organic electronics, this may include complete devices or material samples with appropriate geometries.
Animal Model Selection: Choose appropriate models (typically rodents for initial screening) and implantation sites (subcutaneous, intramuscular, or bone).
Surgical Implantation: Aseptically implant test materials following predetermined spatial distribution to prevent interference between sites.
In-life Observations: Monitor animals for clinical signs, weight changes, and local reactions at predetermined intervals.
Necropsy and Tissue Harvest: Euthanize animals at study endpoints (acute: ≤10 days; chronic: weeks to months). Perform gross necropsy observations and harvest implant sites with surrounding tissue.
Tissue Processing: Fix tissues in 10% neutral buffered formalin, followed by dehydration through graded alcohol series, clearing, and embedding in paraffin or resin [45].
Sectioning and Staining: Cut thin sections (typically 5-15 μm) using a microtome, mount on slides, and stain with appropriate dyes (typically H&E for general assessment).
Histopathological Evaluation: Systematically evaluate slides for inflammation, fibrosis, necrosis, and tissue integration using semi-quantitative scoring systems.
Diagram 1: Implantation Test and Histopathology Workflow
Advanced Histomorphometric Analysis Protocol
For quantitative assessment of tissue integration, particularly for bone-implant interfaces, histomorphometry provides objective measurement of key parameters:
Specimen Preparation: Embed undecalcified bone-implant samples in methylmethacrylate or similar rigid polymer to maintain interface integrity during sectioning [45].
Sectioning and Grinding: Cut thick sections (approximately 200-300 μm) using a diamond saw, then grind and polish to final thickness (approximately 20-30 μm).
Staining Protocol: Apply specialized stains appropriate for the tissue type:
- Toluidine blue for bone morphology assessment
- Masson-Goldner trichrome for distinguishing mineralized bone and osteoid
- Modified Gram stain for infection assessment when needed
Microscopy and Image Capture: Acquire digital images using light microscopy at standardized magnifications (typically 40x-200x).
Quantitative Analysis: Use image analysis software (e.g., ImageJ, CellProfiler) to measure:
- Bone-Implant Contact (BIC): Percentage of implant surface in direct contact with bone
- Bone Area (BA): Percentage of total area occupied by bone within defined regions
- Osteoblast/Osteoclast counts: Cellular activity at the interface
Statistical Analysis: Compare parameters between test and control materials using appropriate statistical tests (ANOVA with post-hoc comparisons for multiple groups).
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Implantation Histopathology
| Reagent/Material | Function | Application Notes |
|---|---|---|
| 10% Neutral Buffered Formalin | Tissue fixation preserves architecture | Standard fixation for most tissues; 24-48 hours optimal |
| Paraffin Embedding Medium | Tissue support for sectioning | Suitable for most soft tissues; not for undecalcified bone |
| Methylmethacrylate Resin | Embedding for undecalcified bone | Preserves bone-implant interface; requires specialized sectioning |
| Hematoxylin and Eosin (H&E) | General tissue staining | Standard initial assessment; nuclei (blue), cytoplasm (pink) |
| Masson's Trichrome Stain | Connective tissue differentiation | Collagen (blue), muscle fibers (red) |
| Toluidine Blue | Bone morphology assessment | Highlights cement lines and cellular details |
| ISO 10993-12 Extracts | Control materials for testing | Polyethylene negative controls, tin-stabilized PVC positive controls |
Data Interpretation and Analytical Considerations
Accurate interpretation of histopathological data requires understanding several analytical challenges. Tissue shrinkage during processing represents a significant consideration, with studies reporting 10-36% size reduction between surgical excision and histological measurement [44]. This shrinkage can critically affect margin assessment, particularly for tumors requiring precise clearance measurements.
When evaluating implant-tissue interfaces, consider these key parameters:
Inflammation Scoring: Grade cellular infiltrates (lymphocytes, plasma cells, macrophages, giant cells) on standardized scales (e.g., 0-4).
Fibrous Capsule Formation: Measure thickness and character of fibrous tissue at material interface.
Tissue Integration: Quantify direct contact between living tissue and implant surface.
Necrosis and Apoptosis: Identify and quantify cell death in peri-implant regions.
For organic electronic materials, additional functional assessments may include electrical performance before and after implantation, corrosion resistance in biological fluids, and mechanical property changes following in vivo exposure [2] [7]. The integration of a biocompatible dual-layer silver and gold metallization in recent organic transistor designs demonstrates strategies for creating robust, stretchable, and biofluid-corrosion-resistant electrodes [7].
Implantation tests with histopathological analysis provide indispensable data for evaluating the local effects of organic electronic materials. As the field advances toward increasingly sophisticated implantable devices, rigorous biological evaluation remains essential for translating laboratory innovations into clinical applications. The comparative data and standardized protocols presented in this guide offer researchers a framework for assessing material biocompatibility, optimizing implant design, and ultimately ensuring the safe integration of organic electronics with biological systems. Future directions will likely include more sophisticated in vitro models that better predict in vivo performance, advanced imaging techniques for real-time interface monitoring, and standardized protocols specific to biodegradable organic electronic materials.
The field of biocompatibility testing for organic electronic materials is undergoing a profound transformation, moving away from traditional two-dimensional cell cultures and animal models toward more physiologically relevant and human-predictive platforms. Next-generation testing platforms, primarily organ-on-a-chip (OoC) and advanced 3D tissue models, are redefining how researchers evaluate material-biological interactions, drug responses, and toxicological profiles [49]. These microphysiological systems (MPS) represent a significant leap forward by extending the life span of cell cultures, adding critical physiological complexity, and enabling long-term pharmacokinetic and pharmacodynamic evaluations [50]. For researchers working with organic electronic materials, these technologies offer unprecedented opportunities to study material-tissue interfaces, host responses, and long-term biocompatibility in controlled microenvironments that closely mimic human physiology.
The emergence of these platforms coincides with growing regulatory receptivity to innovative testing methodologies that can reduce reliance on animal studies while improving predictive accuracy for human responses [49] [51]. This review provides a comprehensive comparison of organ-on-a-chip and 3D tissue model technologies, examining their operating principles, applications in biocompatibility assessment, experimental protocols, and their specific value for evaluating organic electronic materials in biomedical applications.
Organ-on-a-Chip Systems: Engineering Physiological Microenvironments
Organ-on-a-chip technology represents a highly engineered approach to replicating human organ functions using microfluidic devices designed to simulate tissue-tissue interfaces, mechanical forces, and chemical gradients found in living organs [50]. These systems typically feature transparent microchannels fabricated from materials like polydimethylsiloxane (PDMS) or newer minimally drug-absorbing plastics, lined with living cells that are often separated by semipermeable membranes or embedded in extracellular matrix (ECM) gels [50] [52].
The fundamental innovation of OoC platforms lies in their ability to replicate dynamic microenvironments with controlled perfusion systems that supply nutrients, remove waste, and establish biochemical gradients [50]. This setup enables the reproduction of physiological processes such as rhythmic contractions in heart tissue, alveolar gas exchange in lungs, and filtration in kidney models [50]. Recent advancements include the integration of sensors for real-time monitoring of cellular parameters and the application of controlled mechanical forces to simulate specific physiological conditions like fluid shear stress and cyclic stretching [53].
For biocompatibility testing of organic electronic materials, OoC systems offer particular advantages in studying the interface between materials and vascular systems, monitoring barrier integrity changes in real-time, and assessing the effects of mechanical stresses on material-tissue integration.
3D Tissue Models: Recapitulating Native Tissue Architecture
Three-dimensional tissue models encompass a spectrum of technologies ranging from self-assembling organoids to scaffold-based tissue constructs. Organoids are 3D structures derived from the self-organization of stem cells (either adult stem cells or induced pluripotent stem cells) under specific culture conditions that recapitulate the cellular organization, heterotypic interactions, and at least some functions of native organs [50] [51]. These models typically range from several hundred micrometers to millimeters in size and develop through processes mimicking organogenesis [51].
The development of organoids relies on the innate self-organizing capacity of stem cells grown in a gel-like matrix, often Matrigel, which provides structural and biochemical support resembling the native extracellular matrix [50]. Non-adherent microwell plates and hanging drop cultures are also used to facilitate 3D growth [50]. The culture environment requires specific media formulations tailored to the target organ type, often involving multiple growth factors and signaling inhibitors to direct cellular differentiation along desired lineages [50].
Scaffold-based 3D models utilize engineered substrates like the Alvetex Advanced platform, which provides a structural framework that enables cells to establish more natural cell-cell and cell-matrix interactions than possible in conventional 2D cultures [54]. These systems allow researchers to control culture depth, adjust medium volumes, and raise tissues to the air-liquid interface—a critical capability for modeling skin and other epithelial tissues [54].
Comparative Analysis of Key Technological Features
Table 1: Comparison of fundamental characteristics between Organ-on-Chip and 3D Tissue Models
| Feature | Organ-on-a-Chip | 3D Tissue Models (Organoids) |
|---|---|---|
| Fundamental Principle | Engineering of microphysiological environments through microfluidics [50] | Self-organization of stem cells in 3D matrices [50] [51] |
| Physiological Flow | Yes, controlled perfusion systems [50] [53] | Limited, typically static cultures [50] |
| Mechanical Stimuli | Can incorporate shear stress, stretching, compression [53] | Usually absent unless specifically engineered [50] |
| Tissue Complexity | Focus on specific functional units [50] | Higher cellular diversity and organizational complexity [50] [51] |
| Throughput Potential | Moderate, improving with new platforms [52] | High, amenable to multi-well formats [51] |
| Scalability | Challenging, requires sophisticated engineering [50] | Relatively straightforward expansion [51] |
| Vascularization | Can be engineered [50] | Limited innate vascularization [50] |
| Lifespan | Weeks to months [50] | Potentially long-term (months) [50] |
| Reproducibility | High with standardized chips [52] | Variable due to self-organizing nature [50] |
| Cost Factors | Higher initial equipment investment [50] | Lower startup costs [50] |
Table 2: Performance metrics in biocompatibility and drug testing applications
| Parameter | Organ-on-a-Chip | 3D Tissue Models (Organoids) |
|---|---|---|
| Predictive Accuracy for Human Response | High for ADME and barrier function [50] [52] | High for patient-specific drug response [51] |
| Biocompatibility Assessment Capabilities | Real-time barrier integrity, immune cell recruitment [52] | Histological analysis, cellular organization [50] |
| Drug Absorption Prediction | Excellent, with flow-enabled ADME [52] | Moderate, limited by absence of flow [50] |
| Toxicity Detection Sensitivity | High, can detect cell-specific effects [50] [51] | High, maintains metabolic functions [51] |
| Integration with Analytical Methods | Compatible with TEER, imaging, -omics [53] [52] | Excellent for histology, imaging, -omics [51] [54] |
| Personalized Medicine Potential | Moderate, with patient-derived cells [50] | High, especially with patient-derived organoids [51] |
| Multi-organ Interaction Studies | Yes, through linked systems [50] | Limited, typically single organ focus [50] |
| Regulatory Acceptance | Growing, with FDA engagement [51] | Established in specific applications [51] |
Experimental Protocols and Methodologies
Standardized Workflows for Biocompatibility Assessment
The experimental workflow for evaluating organic electronic materials in these platforms follows a structured approach to ensure reproducible and biologically relevant results. Below are detailed protocols for assessing material biocompatibility using both OoC and 3D tissue models.
Organ-on-a-Chip Material Testing Protocol
Phase 1: Chip Preparation and Cell Seeding
- Chip Sterilization: For PDMS chips, sterilize using autoclaving or UV ozone treatment. For plastic chips like the Chip-R1, use gamma irradiation or ethanol sterilization followed by PBS rinsing [52].
- Surface Coating: Apply appropriate extracellular matrix proteins (e.g., collagen IV, fibronectin) through microfluidic perfusion at 0.1-0.5 μL/s for 30 minutes, followed by incubation at 37°C for 1-2 hours [53].
- Cell Introduction: Introduce cell suspensions at optimized densities (typically 1-5×10^6 cells/mL for endothelial cells, 0.5-2×10^6 cells/mL for epithelial cells) through controlled flow rates (0.5-1 μL/s) to ensure uniform distribution [53].
- Barrier Formation: Maintain cells under static conditions for 6-24 hours to allow attachment, then initiate perfusion at gradually increasing flow rates (from 0.1 to 10 μL/s over 24-48 hours) to promote polarization and barrier formation [52].
Phase 2: Material Exposure and Assessment
- Test Material Introduction: Introduce organic electronic materials as particles (0.1-10 μm range), thin films, or as substrate-integrated components using precise flow control to mimic physiological exposure scenarios [53].
- Real-time Monitoring: Measure transepithelial/transendothelial electrical resistance (TEER) using integrated electrodes, track barrier integrity with fluorescent dextran permeability assays, and monitor metabolic activity through effluent analysis [53] [52].
- Endpoint Analysis: Following exposure period (typically 1-14 days), assess cell viability (live/dead staining), inflammatory marker expression (ELISA of effluents), and morphological changes (immunofluorescence imaging) [53] [52].
3D Tissue Model Biocompatibility Assessment
Phase 1: Model Establishment
- Scaffold Preparation: For scaffold-based models, hydrate Alvetex Advanced or similar scaffolds with culture medium according to manufacturer specifications. For Matrigel-based organoids, prepare growth factor-reduced matrix on ice [54].
- Cell Seeding: Seed primary cells or stem cells at optimized densities (typically 0.5-2×10^6 cells/mL for organoids, 0.1-0.5×10^6 cells/mL for scaffold models) using gentle centrifugation if required for scaffold penetration [54].
- 3D Culture Maintenance: Maintain cultures with specific medium formulations tailored to target tissue type, with regular medium changes (every 2-3 days) and morphological assessment [50] [54].
- Tissue Maturation: Allow 7-28 days for tissue maturation, with timing dependent on model complexity. For air-liquid interface models, raise inserts to interface at specified timepoints [54].
Phase 2: Material Biocompatibility Testing
- Material Exposure: Apply test materials to established 3D tissues as particles in suspension, as overlaying films, or as embedded components within the matrix. For organoids, materials can be introduced during formation or after maturation [51].
- Viability and Function Assessment: Quantify metabolic activity using AlamarBlue or MTT assays, assess tissue integrity through histology (H&E staining), and evaluate specific functions (e.g., albumin production for liver models, contractility for cardiac tissues) [51].
- Molecular Analysis: Process tissues for RNA/protein extraction for transcriptomic or proteomic analysis, or fix for immunohistochemical evaluation of marker expression and inflammatory responses [51] [54].
Advanced Analytical Methodologies
Both platforms support sophisticated analytical approaches that yield quantitative data on material biocompatibility:
Barrier Integrity Assessment: In OoC systems, this is continuously monitored through TEER measurements using integrated electrodes, with values typically ranging from 50-500 Ω×cm² depending on the barrier type [52]. For 3D models, barrier function is assessed through tracer flux studies using molecules like FITC-dextran [54].
Metabolic Competency Evaluation: Hepatic models are assessed for albumin production (0.1-20 μg/day/10^6 cells for OoC systems), urea synthesis (10-100 μg/day/10^6 cells), and cytochrome P450 activity (measured with substrate-specific probes) [50] [51]. Metabolic activity in 3D models is typically 2-5 times higher than in 2D cultures [51].
Histological and Morphological Analysis: Standard histotechnical processing followed by H&E staining reveals overall tissue architecture, while immunofluorescence for specific markers (e.g., ZO-1 for tight junctions, albumin for hepatocytes) confirms functional specialization [51]. Image analysis algorithms quantify morphological parameters like spheroid size distribution, nuclear orientation, and marker expression patterns [51].
Multi-omics Integration: RNA sequencing of chips and organoids reveals transcriptomic responses to material exposure, while LC-MS-based proteomics of effluents or tissue lysates identifies protein-level changes and secreted biomarkers [52] [51].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of next-generation testing platforms requires specific reagents, materials, and instrumentation. The following table details essential components for establishing these systems in a research setting.
Table 3: Essential research reagents and materials for next-generation testing platforms
| Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Base Matrices | Matrigel, Collagen I, Fibrin | Provide 3D structural support mimicking native ECM [50] | Matrigel concentration typically 5-10%; collagen 1-3 mg/mL [50] |
| Synthetic Scaffolds | Alvetex Advanced, PEG-based hydrogels | Engineered scaffolds with controlled properties [54] | Alvetex allows air-liquid interface establishment [54] |
| Specialized Media | IntestiCult, HepatiCult, STEMdiff | Organ-specific differentiation and maintenance [50] | Contain precise growth factor combinations [50] |
| Cell Sources | iPSCs, primary cells, organ-specific stem cells | Provide biological component of models [50] [51] | iPSCs enable patient-specific models [50] |
| Characterization Tools | TEER electrodes, fluorescent tracers, metabolic assays | Functional assessment of model performance [53] [52] | TEER values validate barrier integrity [52] |
| Microfluidic Chips | PDMS chips, Chip-R1, Chip S1 | Housing for OoC models with controlled flow [50] [52] | Chip-R1 minimizes drug absorption [52] |
| Flow Control Systems | Peristaltic pumps, pressure controllers | Maintain physiological flow conditions [50] [53] | Typical flow rates: 0.1-100 μL/min [53] |
| Imaging-Compatible Hardware | Custom microscope mounts, environmental chambers | Enable live imaging during experiments [53] [52] | Maintain 37°C, 5% CO2 during imaging [52] |
Applications in Organic Electronic Materials Research
The integration of OoC and 3D tissue models into the development pipeline for organic electronic materials addresses critical challenges in biocompatibility assessment, particularly for implantable devices, biosensors, and neural interfaces.
Specific Application Areas
Implantable Electronics Biocompatibility: OoC systems enable real-time assessment of foreign body responses to organic electronic materials through controlled introduction of immune cells and monitoring of cytokine secretion profiles [49] [52]. For instance, Lymph Node-Chip models have demonstrated capability to predict antigen-specific immune responses, providing valuable insights for materials intended for long-term implantation [52].
Blood-Brain Barrier Penetration for Neural Interfaces: BBB-Chip models incorporating primary human brain microvascular endothelial cells, astrocytes, and pericytes enable evaluation of material effects on this critical barrier [52]. These systems have been used to study nanoparticle penetration and barrier disruption, directly relevant to neural interface materials [52].
Cutaneous and Subcutaneous Sensor Biocompatibility: Advanced skin models using Alvetex technology allow formation of multilayered, differentiated epidermis for testing wearable and implantable sensor materials [54]. The ability to raise these models to air-liquid interface enables realistic exposure scenarios for materials intended for cutaneous application [54].
Cardiac Patch Integration Assessment: Heart-on-chip models that replicate cardiac mechanical properties enable evaluation of conductive polymer patches on cardiac tissue function, including contractility, electrophysiology, and biomarker release [50] [52].
Quantitative Performance Data
Recent studies provide compelling performance data for these platforms:
- Liver-Chip systems have demonstrated 87% accuracy in predicting drug-induced liver injury in humans, significantly outperforming conventional 2D cultures (55%) and animal models (65%) [52].
- Kidney-Chip models have successfully predicted nephrotoxicity of antisense oligonucleotides, with biomarker release (KIM-1, NGAL) correlating with clinical observations [52].
- Patient-derived organoid models in cancer research have shown 88% positive predictive value and 100% negative predictive value for clinical treatment response, highlighting their accuracy in personalized therapeutic assessment [51].
- Intestine-Chip models have replicated complex immune responses to therapeutic interventions in inflammatory bowel disease, accurately predicting clinical efficacy and identifying previously unrecognized mechanisms of action [52].
Emerging Trends and Future Directions
The field of next-generation testing platforms continues to evolve rapidly, with several emerging trends particularly relevant to organic electronic materials research:
Technology Convergence
The distinction between OoC and 3D tissue models is blurring with the development of Organoids-on-a-chip—hybrid systems that integrate the organizational complexity of organoids with the physiological relevance of microfluidic control [50]. These platforms provide enhanced reproducibility through controlled perfusion while maintaining the cellular diversity of self-organizing systems [50]. For organic electronic materials research, this convergence enables more standardized assessment of material effects on complex tissues under flow conditions.
Advanced Sensing Integration
Next-generation platforms increasingly incorporate embedded sensors for real-time monitoring of oxygen levels, pH, metabolic activity, and specific biomarkers [53]. This capability is particularly valuable for organic electronic materials themselves, as they can potentially function as built-in sensors within these systems, creating a closed-loop assessment platform [53].
Personalized Medicine Applications
The use of patient-specific induced pluripotent stem cells (iPSCs) in both OoC and organoid models enables creation of personalized testing platforms that account for individual genetic variations in material responses [50] [51]. This approach is particularly valuable for identifying hypersensitive populations who might exhibit adverse reactions to specific material compositions [51].
Regulatory Science Advancement
Regulatory agencies including the FDA are increasingly engaging with these technologies through initiatives like the Innovative Science and Technology Approaches for New Drugs (ISTAND) pilot program, which considers MPS as potential tools for regulatory decision-making [51]. This growing acceptance signals the transition of these platforms from research tools to validated components of the biocompatibility assessment pipeline.
Organ-on-a-chip and 3D tissue models represent complementary yet distinct approaches to advancing biocompatibility assessment for organic electronic materials. OoC systems excel in replicating dynamic tissue interfaces, mechanical forces, and fluid flow conditions, making them particularly valuable for evaluating vascular integration, barrier function, and materials subject to mechanical stress [50] [53]. In contrast, 3D tissue models capture higher organizational complexity and cellular diversity, making them ideal for assessing chronic exposure effects, metabolic competency, and patient-specific responses [50] [51].
The choice between these platforms depends heavily on specific research questions, with OoC technology providing greater control over microenvironmental parameters and 3D models offering more native tissue architecture. For comprehensive biocompatibility assessment of organic electronic materials, a combined approach leveraging both technologies provides the most robust evaluation pipeline, addressing both functional integration and tissue-level responses.
As these technologies continue to mature through improved standardization, enhanced analytical capabilities, and growing regulatory acceptance, they are poised to fundamentally transform the preclinical evaluation paradigm for organic electronic materials, enabling more predictive safety assessment, reduced animal testing, and accelerated development of innovative biomedical devices.
In the field of organic bioelectronics, the drive to develop devices that can seamlessly integrate with biological systems places immense importance on material biocompatibility and interfacial properties. Surface characterization techniques are indispensable for designing and validating these advanced materials. This guide provides a comparative analysis of three cornerstone techniques—Atomic Force Microscopy (AFM), Scanning Electron Microscopy (SEM), and X-ray Photoelectron Spectroscopy (XPS)—focusing on their application in biocompatibility testing for organic electronic materials. By comparing their operational principles, outputs, and specific applications in recent research, this guide aims to assist researchers in selecting and applying the most appropriate techniques for their development of next-generation bio-integrated devices.
Atomic Force Microscopy (AFM) is a scanning probe technique that provides topographical images by physically scanning a sharp tip across a sample surface. It can operate in various modes (e.g., contact, tapping) to characterize surface morphology and mechanical properties under physiologically relevant conditions, including liquid environments [55]. A key advantage is its ability to perform nanoindentation to measure local mechanical properties like Young's modulus, which is critical for ensuring a mechanical match with soft biological tissues [7] [56] [55].
Scanning Electron Microscopy (SEM) generates high-resolution images by scanning a focused electron beam across a surface and detecting secondary or backscattered electrons. It provides detailed information on surface topography and microstructure. However, traditional high-resolution SEM imaging is time-intensive, as it requires sequential scanning of large areas to find rare features. Recent advancements use artificial intelligence (AI) for resolution enhancement, enabling a 16-fold acceleration in imaging speed [57].
X-ray Photoelectron Spectroscopy (XPS), also known as Electron Spectroscopy for Chemical Analysis (ESCA), is a surface-sensitive analytical technique that uses X-rays to eject core electrons from a material. By measuring the kinetic energy of these electrons, XPS provides quantitative elemental composition and chemical state information from the outermost ~10 nanometers of a material [58] [59]. This is crucial for understanding surface chemistry, which directly influences biological interactions [7] [59].
Table 1: Core Characteristics and Applications of AFM, SEM, and XPS
| Feature | Atomic Force Microscopy (AFM) | Scanning Electron Microscopy (SEM) | X-ray Photoelectron Spectroscopy (XPS) |
|---|---|---|---|
| Primary Output | 3D surface topography, nanomechanical properties | 2D high-resolution surface imaging | Quantitative elemental & chemical state analysis |
| Lateral Resolution | Sub-nanometer | Sub-nanometer (with advanced techniques) [57] | ~10 micrometers (with micro-focused sources) |
| Analysis Depth | Surface topology (angstrom level) [55] | Several nanometers to microns | ~10 nm |
| Key Strength | Measures mechanical properties; operates in liquid | High-resolution imaging of large areas | Provides chemical bonding information |
| Sample Environment | Air, liquid, vacuum [55] | Vacuum | Ultra-high vacuum (UHV) |
| Key Bio-relevant Metric | Young's modulus (DMT modulus) [7] [56] | Microstructural voids, phase boundaries [57] | Surface chemical composition & states [7] [59] |
| Role in Biocompatibility | Assesses stiffness matching with tissues [7] | Inspects structural integrity and coatings | Verifies surface chemistry for bio-inertness |
Table 2: Performance in Biocompatibility Testing for Organic Electronics
| Analysis Goal | AFM Applications | SEM Applications | XPS Applications |
|---|---|---|---|
| Surface Morphology | Quantifies nanoscale roughness affecting cell adhesion [56] [59] | Images micro-scale features and film homogeneity | Not applicable |
| Chemical Composition | Not applicable (indirect via phase imaging) | Not directly applicable | Quantifies elemental makeup; confirms bio-inert coatings [7] |
| Mechanical Property | Measures Young's modulus (e.g., ~107.7-108.8 Pa for tissue-like transistors [7]) | Not directly applicable | Not applicable |
| Protein/Cell Adhesion | Studies cell-surface interactions in liquid [56] | Images cell morphology on materials | Analyzes protein adsorption on surfaces [56] |
| Material Degradation | Tracks surface erosion and swelling in liquid | Identifies micro-cracks and structural defects | Monitors chemical changes during degradation [59] |
Experimental Protocols for Biocompatibility Assessment
To ensure the reliability and reproducibility of surface characterization in biocompatibility studies, standardized yet adaptable experimental protocols are essential. The following workflows are synthesized from recent research on organic electronic materials.
Protocol for AFM Nanoindentation of Soft Electronic Films
This protocol is critical for developing implantable electronics with a mechanical modulus similar to human tissues to prevent inflammation and tissue damage [7].
1. Sample Preparation: Spin-coat or drop-cast the polymeric semiconductor film (e.g., a blend of DPPT-TT and bromo isobutyl–isoprene rubber) onto a clean, flat substrate. For in-liquid measurements, ensure the film is stable in aqueous environments [56].
2. Cantilever Selection: Choose a cantilever with a low spring constant (typically 0.1 - 1 N/m) suitable for soft materials. Calibrate the cantilever's spring constant and the optical lever sensitivity prior to measurement using a standard method (e.g., thermal tune).
3. Data Acquisition:
- Engage the tip with the surface in force spectroscopy mode.
- Acquire force-distance curves by extending and retracting the piezoelectric scanner at multiple, randomly selected locations across the sample surface.
- For each curve, record the cantilever deflection as a function of the sample displacement.
4. Data Analysis:
- Convert force-distance curves into force-indentation curves.
- Fit the retraction curve's slope in the elastic region using the Derjaguin-Muller-Toporov (DMT) model to calculate the local Young's modulus [7] [56] [55].
- Generate a modulus map by performing this analysis over a grid of points.
Protocol for XPS Analysis of Implantable Electronics
This protocol is used to verify the surface composition and stability of conductive electrodes and semiconducting polymers in bioelectronic devices [7].
1. Sample Preparation: Mount the sample (e.g., a film with Ag/Au electrodes or a semiconducting polymer) on a standard XPS holder using double-sided conductive tape. Avoid any contact with the analysis area.
2. Instrument Setup:
- Transfer the sample to the ultra-high vacuum (UHV) introduction chamber and outgas until a stable pressure is reached.
- Move the sample to the analysis chamber.
- Use a monochromatic Al Kα X-ray source.
- Set the analyser pass energy to 20-50 eV for high-resolution scans and 100-160 eV for survey scans.
3. Data Acquisition:
- Acquire a wide survey scan (e.g., 0-1200 eV binding energy) to identify all elements present.
- Acquire high-resolution scans for regions of interest (e.g., Ag 3d, Au 4f, S 2p, C 1s, O 1s).
- For depth profiling, use an ion gun (e.g., Ar+) to sputter the surface intermittently between XPS scans.
4. Data Analysis:
- Process the spectra using dedicated software (e.g., CasaXPS, Avantage).
- Apply a Shirley or Tougaard background subtraction.
- Use charge referencing, typically by setting the C 1s peak for adventitious carbon to 284.8 eV.
- Perform peak fitting to deconvolute chemical states (e.g., different sulfur species in a semiconducting polymer) [7].
Integrated Workflow for Comprehensive Material Characterization
A multi-technique approach is often necessary to fully understand a material's suitability for biointegration. The following workflow, common in advanced studies, illustrates how AFM, SEM, and XPS can be used complementarily [7] [56] [59].
1. Macroscopic Screening with SEM: Use SEM for initial, rapid inspection of large sample areas to check for film homogeneity, gross defects, and the integrity of micro-patterned features. AI-based resolution enhancement can be applied to accelerate this process [57].
2. Surface Chemistry Verification with XPS: Perform XPS analysis on the same sample to quantitatively determine the surface elemental composition and confirm the presence of specific chemical states or functional groups (e.g., verifying a protective gold coating on electrodes or identifying chemical changes after immersion in bio-fluids) [7].
3. Nanoscale Topography and Mechanics with AFM: Use AFM to obtain detailed 3D topography of regions identified as interesting by SEM. Subsequently, perform nanoindentation measurements to map the local mechanical properties, ensuring they match the softness of target biological tissues [7] [56].
4. Correlative Data Interpretation: Correlate data from all three techniques. For instance, a change in surface chemistry (XPS) after degradation might correlate with an increase in surface roughness (AFM) and the appearance of micro-cracks (SEM) [59].
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table lists key materials and their functions as derived from recent research on characterizing and developing biocompatible organic electronic materials.
Table 3: Key Materials for Biocompatible Organic Electronics Research
| Material/Reagent | Function in Research | Relevant Technique(s) |
|---|---|---|
| DPPT-TT (Semiconductor) | Donor-acceptor polymer providing charge transport in stretchable transistors [7]. | AFM, XPS |
| BIIR (Bromo Isobutyl–Isoprene Rubber) | Medical-grade elastomer matrix for biocompatibility and stretchability [7]. | AFM (Mechanical testing) |
| BBL (Poly(benzimidazobenzophenanthroline)) | n-type conductive polymer evaluated for neuronal cell interfacing [56]. | AFM, XPS, SEM |
| PLL (Poly-L-Lysine) | Protein coating applied to polymer surfaces to promote cell adhesion and growth [56]. | QCM-D, AFM, XPS |
| Ag/Au Dual-Layer Metallization | Creates stretchable, conductive, and biofluid-corrosion-resistant electrodes [7]. | XPS (Depth profiling) |
| Selenophene-based Polymers | Conjugated polymer backbone modification to mitigate foreign-body response [60]. | XPS, AFM |
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer for drug delivery and scaffolds; model for degradation studies [59]. | XPS, DRIFT, AFM, SEM |
AFM, SEM, and XPS are not mutually exclusive tools but rather complementary pillars of modern surface analysis in bioelectronics. AFM is unparalleled for its ability to probe nanomechanical properties under physiological conditions, a critical factor for tissue integration. SEM offers unparalleled topographical detail at the micro- and nanoscale, with AI-enhanced methods dramatically improving throughput. XPS uniquely provides definitive chemical intelligence about the outermost surface layers, which dictate primary biological responses. The convergence of data from these techniques—correlating chemical composition from XPS with topological features from SEM and AFM, and mechanical properties from AFM—enables a holistic understanding of material-biosystem interactions. This integrated approach is fundamental to rationally designing the next generation of immune-compatible, high-performance implantable electronic devices.
The development of implantable bioelectronic devices represents a frontier in modern medicine, offering the potential for continuous health monitoring, targeted therapy, and advanced neural interfaces. A significant barrier to their widespread adoption has been the mechanical and biological mismatch between conventional rigid electronic components and soft, dynamic biological tissues. This mismatch can lead to tissue damage, inflammation, and device failure [7]. The research objective of this case study is to analyze the development of a truly biocompatible and stretchable organic transistor that overcomes these limitations, focusing on the materials selection, fabrication methodology, and rigorous biocompatibility testing required for successful implantation.
This case study is framed within a broader thesis on biocompatibility testing for organic electronic materials. It will objectively compare the performance of a novel elastomeric organic field-effect transistor (OFET) against other emerging technologies, using quantitative data from recent peer-reviewed studies. The analysis will provide researchers with a comprehensive understanding of the current state of stretchable transistor technologies, their relative performance metrics, and the experimental protocols essential for validating both electrical functionality and biological safety.
Performance Comparison of Stretchable Transistor Technologies
To objectively evaluate the landscape, the following table compares the key performance characteristics of four prominent stretchable transistor technologies documented in recent literature. The data is synthesized from studies on elastomeric OFETs, all-gel Organic Electrochemical Transistors (OECTs), collagen-based OFETs, and earlier-generation stretchable OECTs.
Table 1: Performance Comparison of Stretchable Transistor Technologies for Bio-Integration
| Technology Type | Key Materials | Max Stretchability (%) | Electrical Performance | Biocompatibility & Degradation | Best Suited Applications |
|---|---|---|---|---|---|
| Elastomeric OFET [7] | DPPT-TT / BIIR Elastomer | >100% | Stable operation under 50% strain; High ON/OFF ratio | Excellent: No adverse effects on cell viability; No major inflammatory response in vivo (mouse model, 30 days) | Long-term implantable circuits & sensors |
| All-Gel OECT [61] | PEDOT:PSS/PAM Gel, Ionogel Electrolyte | 50% | Ultra-high transconductance (~86.4 mS); ON/off ratio: 1.2×10⁵ | Implied by gel materials; Immune compatibility reported | Wearable electronic skin; Tactile sensors; Gas sensors |
| Collagen-Based OFET [62] | Collagen, Semiconducting Polymer | Flexible (Bending) | Stable under bending strain | Biocompatible & Biodegradable: ~48% mass loss in days; HEK cell viability confirmed | Temporary, resorbable implants |
| Stretchable OECT (Earlier Gen.) [63] | DPP-g2T (Honeycomb) | 140% | Stable performance at 140% strain | Compatible with bodily fluids (sweat, plasma) | Wearable epidermal sensors |
The data reveals a clear trade-off between different technological approaches. The Elastomeric OFET demonstrates a superior combination of high stretchability, stable electrical performance under strain, and proven long-term biocompatibility in implantable scenarios, making it ideal for robust, chronic implants [7]. In contrast, the All-Gel OECT achieves unparalleled electrical amplification (transconductance) but with lower demonstrated stretchability, positioning it as a prime candidate for high-performance wearable sensors [61]. The Collagen-Based OFET offers a unique value proposition with its demonstrated biodegradability, suitable for applications where device removal is undesirable [62].
Experimental Protocol: Fabrication and Validation of the Elastomeric OFET
This section details the experimental methodology for developing and validating the highlighted elastomeric OFET, providing a reproducible protocol for researchers.
Material Fabrication and Device Integration
The core innovation lies in creating a stretchable semiconducting composite film.
- Solution Preparation: A blend of the semiconducting polymer poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] (DPPT-TT) and the medical-grade elastomer bromo isobutyl–isoprene rubber (BIIR) is prepared in a compatible solvent system. The optimal weight ratio for balancing electrical and mechanical properties was determined to be 3:7 (DPPT-TT:BIIR) [7].
- Vulcanization: The blend film undergoes a chemical vulcanization process using sulfur (crosslinker), dipentamethylenethiuram tetrasulfide (DPTT, accelerator), and stearic acid (initiator). This process crosslinks the BIIR chains, enhancing the film's elasticity and mechanical robustness without disrupting the conjugated structure of the DPPT-TT semiconductor. Successful vulcanization is confirmed via Fourier Transform Infrared (FTIR) spectroscopy by observing the reduction in C–Br peaks at 667 cm⁻¹ [7].
- Nanofiber Network Formation: Due to surface energy disparity, the DPPT-TT self-assembles into an interconnected nanofibre network embedded within the BIIR elastomer matrix. This structure is critical for maintaining a continuous charge transport pathway even under mechanical deformation [7].
- Biocompatible Metallization: Electrodes are fabricated using a dual-layer metallization of silver (Ag) and gold (Au). Ag provides excellent electrical contact, while a top layer of Au offers robust resistance to corrosion from biofluids, ensuring long-term stability [7].
Electrical and Mechanical Performance Testing
The fabricated transistors are subjected to a battery of tests to characterize their performance.
- Electrical Characterization: Transfer and output characteristics are measured using a semiconductor parameter analyzer. Key metrics such as field-effect mobility and ON/OFF ratio are extracted. For the vulcanized 3:7 blend film, these properties remain stable even when the transistor is stretched up to 100% strain on a rigid substrate [7].
- Mechanical Durability Testing: Devices are mounted on a stretchable substrate and subjected to cyclic strain tests. The transistors demonstrate stable electrical performance with negligible change in mobility after 1,000 stretching cycles at 100% strain, confirming their mechanical durability [7].
- Morphological Analysis: Atomic Force Microscopy (AFM) and Conductive-AFM (C-AFM) are performed on films under strain. These analyses show the alignment of the DPPT-TT nanofibres along the strain direction, visually confirming the preservation of the conductive network that enables strain-insensitive performance [7].
Biocompatibility Assessment Protocol
The biological safety of the device is validated through a multi-tiered testing protocol, which is a cornerstone of implantable materials research.
- In Vitro Cytotoxicity (ISO 10993-5):
- Cell Culture: Human dermal fibroblasts and macrophages are cultured in standard conditions.
- Extract Preparation: The device material is incubated in a cell culture medium to create an extract.
- Viability Assay: Cells are exposed to the extract, and viability is measured after 24-72 hours using assays like MTT or PrestoBlue. The material is deemed non-cytotoxic if cell viability exceeds 70-80% compared to controls. The DPPT-TT/BIIR blend showed no adverse effects on cell viability, proliferation, or migration [7].
- In Vivo Implantation Study:
- Animal Model: Devices are subcutaneously implanted in a mouse model.
- Histopathological Analysis: After a set period (e.g., 30 days), the implantation site and surrounding tissue are explanted, fixed, sectioned, and stained (e.g., with H&E). The tissue is examined under a microscope for signs of inflammation, fibrosis, necrosis, or other tissue damage. The reported transistor showed no major inflammatory response or tissue damage after 30 days [7].
The workflow below visualizes the complete experimental pathway from material synthesis to final validation.
Figure 1: Experimental workflow for transistor development
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs the key materials and reagents used in the development of the featured elastomeric OFET, serving as a reference for experimental design.
Table 2: Essential Research Materials for Biocompatible Stretchable Transistors
| Material / Reagent | Function (in this context) | Research-Grade Example / Specification |
|---|---|---|
| DPPT-TT Semiconductor | Forms the charge-transporting nanofibre network within the elastomer matrix. | High-purity donor-acceptor polymer (e.g., >99.5% purity from specialty chemical suppliers) [7]. |
| BIIR (Bromo Isobutyl–Isoprene Rubber) | Medical-grade elastomer matrix; provides stretchability and primary biocompatibility. | Medical-grade elastomer meeting ISO 10993 and European Pharmacopoeia standards [7]. |
| Vulcanization Kit | Chemically crosslinks the BIIR matrix to enhance mechanical robustness. | Sulfur (crosslinker), DPTT - Dipentamethylenethiuram tetrasulfide (accelerator), Stearic Acid (initiator) [7]. |
| Ag/Au for Metallization | Creates stretchable, corrosion-resistant electrodes. Ag for conductivity, Au for biofluid resistance. | High-purity (e.g., 99.99%) Ag and Au targets for physical vapor deposition (sputtering/evaporation) [7]. |
| Cell Lines for In Vitro Test | Assess cytocompatibility per ISO 10993-5. | Immortalized human cell lines: Dermal Fibroblasts (HDF), Macrophages (e.g., THP-1) [7]. |
| Animal Model | Assess the in vivo biological response and long-term integration potential. | Immunocompetent mouse model (e.g., C57BL/6) for subcutaneous implantation [7]. |
This case study demonstrates that the development of viable biocompatible and stretchable transistors is an interdisciplinary endeavor, merging materials science, electrical engineering, and biology. The analyzed elastomeric OFET, based on a vulcanized DPPT-TT/BIIR blend, presents a compelling solution by successfully balancing high stretchability, stable electrical performance under strain, and proven biocompatibility in both in vitro and in vivo settings [7].
The performance comparison reveals that the choice of technology is application-dependent. While elastomeric OFETs are superior for long-term implants, all-gel OECTs offer higher signal amplification for wearables, and collagen-based OFETs open the door for transient electronics [61] [62]. The future of this field lies in further enhancing the material properties, scaling down device dimensions, and integrating these transistors into more complex, multifunctional bioelectronic systems. Furthermore, the convergence of such hardware advances with artificial intelligence for data analysis promises a new generation of smart, adaptive, and self-learning implantable medical devices [64].
Troubleshooting and Optimization: Overcoming Biocompatibility Challenges
The long-term success of implantable biomedical devices, from neural interfaces to orthopaedic implants, is critically limited by the foreign body response (FBR), a complex immunological reaction to implanted materials [65]. This response typically culminates in fibrous encapsulation, isolating the implant from surrounding tissues and often causing device failure [66]. Within the specific context of organic electronic materials research, understanding and mitigating the FBR is paramount for developing advanced biointegrated devices that maintain stable functionality over time. This guide objectively compares current material and surface engineering strategies, focusing on their performance in modulating immune responses and supporting experimental data from relevant biocompatibility testing protocols.
Core Mechanisms of the Foreign Body Response
The FBR is a sequential process initiated immediately upon implantation. It begins with the adsorption of host proteins onto the biomaterial surface, creating a provisional matrix that guides subsequent immune cell recruitment [65] [66].
- Inflammatory Cell Recruitment: Neutrophils are the first responders, attempting to phagocytose the material. They are quickly followed by monocytes and tissue-resident macrophages [65] [66].
- Macrophage Polarization and Fusion: Macrophages are central orchestrators of the FBR. Their phenotypic state, influenced by local cytokine cues and material properties, dictates pathological versus reparative outcomes. Pro-inflammatory M1 macrophages dominate early stages, secreting cytokines like TNF-α and IL-6. A transition to anti-inflammatory, pro-healing M2 macrophages is crucial for positive outcomes. Under stimuli such as IL-4 and IL-13, macrophages on the material surface undergo fusion to form foreign body giant cells (FBGCs), a hallmark of the FBR [65] [66].
- Fibrous Encapsulation: FBGCs and macrophages drive fibrosis by secreting factors that activate fibroblasts, leading to the deposition of a collagen-rich, avascular capsule that walls off the implant [65] [66].
The following diagram illustrates this key cellular pathway.
Comparative Analysis of Material Strategies
Synthetic Polymer Biocompatibility
Different polymers elicit distinct cellular and tissue responses. A comparative study of ten polymers for neural interfaces evaluated their toxicity and FBR, with key quantitative findings summarized below [67].
Table 1: In Vitro and In Vivo Biocompatibility of Polymers for Neural Interfaces
| Polymer Material | Neural Cell (PC-12) Adhesion & Growth | Fibroblast (NRK-49F) Adhesion & Growth | In Vivo Fibrosis & FBR (4 weeks post-implant) |
|---|---|---|---|
| Polyimide (PI) | Highest compatibility | Highest compatibility | Lowest pathological response |
| Polylactide (PLA) | High | High | Low FBR; promising |
| Polydimethylsiloxane (PDMS) | High | High | Low FBR; promising |
| Thermoplastic Polyurethane (TPU) | High | High | Low FBR; promising |
| Polycaprolactone (PCL) | Moderate | Moderate | Lower pathological response |
| Polyethylene glycol diacrylate (PEGDA) | Cytotoxic effects | Low cell adhesion | Strongest FBR; fibrosis & multinucleated cells |
Advanced Composite Materials for Electronics
The development of elastomeric organic field-effect transistors (sOFETs) highlights the move toward materials that match the mechanical properties of biological tissues. A recent breakthrough involves a semiconductor blend of poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] (DPPT-TT) and the medical-grade elastomer bromo isobutyl–isoprene rubber (BIIR) [7].
- Biocompatibility Performance: This vulcanized blend film exhibits a Young's modulus similar to human tissues. In vitro assessments with human dermal fibroblasts and macrophages showed no adverse effects on cell viability, proliferation, or migration. Furthermore, in vivo implantation studies in mice revealed no major inflammatory response or tissue damage, confirming its high biocompatibility for implantable electronics [7].
- Electrical Performance: The composite film maintained stable electrical performance under mechanical strain up to 50% and after 1,000 stretching cycles at 100% strain, demonstrating its mechanical durability and operational stability for bioelectronic applications [7].
Surface Engineering Strategies for Immunomodulation
Biomimetic Surface Coatings
Rather than altering the bulk material, surface coatings can effectively camouflage implants from the immune system.
- Red Blood Cell (RBC) Coating: A living RBC coating fabricated using hyaluronic acid (HA) as a bridging polymer on a PDMS substrate demonstrated significant immunomodulatory effects [68].
- Performance Data: The PDMS-HA-RBC implant resulted in minimum fibrosis formation compared to pristine PDMS and PDMS-HA. Immunohistological analysis showed the RBC coating actively polarized macrophages towards the pro-healing M2 phenotype, evidenced by the highest M2/M1 ratio and the highest intensity of the M2 marker CD206. This effect is attributed to immune escape antigens (e.g., CD47, CD59) present on the intact RBC membrane [68].
The experimental workflow for creating and testing this biomimetic coating is detailed below.
Functional Polymer Coatings for Drug Delivery
Polymer coatings serve as versatile platforms for the localized delivery of immunomodulatory agents. Techniques like dip coating, spray coating, and spin coating allow precise control over coating thickness and composition, enabling tailored drug release profiles to mitigate the FBR [69]. The controlled release of anti-inflammatory drugs (e.g., corticosteroids) from these coatings can significantly dampen local inflammation, reduce adverse immune responses, and promote better integration of the implant with host tissues [69].
Experimental Protocols for Biocompatibility Testing
Robust experimental validation is essential for evaluating new materials. The following protocols are standard in the field.
In Vitro Cell Culture Assays
Objective: To assess material toxicity, cell adhesion, and proliferation on material surfaces [67].
- Material Sterilization: Sterilize polymer scaffolds (e.g., via UV irradiation or ethanol immersion).
- Cell Seeding: Seed relevant cell types (e.g., neural PC-12 cells, fibroblast NRK-49F cells) onto the material surfaces at a standard density (e.g., 10,000 cells/cm²) in appropriate culture media.
- Cytotoxicity Assessment: After an incubation period (e.g., 24-72 hours), perform assays like MTT or Live/Dead staining to quantify cell viability and metabolic activity.
- Cell Morphology and Adhesion: Use scanning electron microscopy (SEM) or fluorescence microscopy (after phalloidin/DAPI staining) to visualize cell attachment and spreading on the material surface.
In Vivo Implantation and Histological Analysis
Objective: To evaluate the tissue-level FBR to an implanted material [67] [7].
- Animal Implantation: Surgically implant material scaffolds or devices into an appropriate animal model (e.g., rats for brain implants, mice for subcutaneous implants). Include sham operations as controls.
- Explanation and Fixation: After a predetermined period (e.g., 4 weeks), euthanize the animals, retrieve the implants with surrounding tissue, and fix the tissue in formalin.
- Sectioning and Staining: Process fixed tissue into paraffin blocks, section into thin slices (5-10 µm), and mount on slides. Perform histological staining:
- H&E Staining: For general tissue morphology and identifying immune cell infiltration.
- Masson's Trichrome Staining: For visualizing collagen deposition (fibrosis).
- Immunofluorescence (IF) Staining: To identify specific cell phenotypes.
- Use primary antibodies against CD86 (for M1 macrophages) and CD206 (for M2 macrophages).
- Use fluorescently-labeled secondary antibodies for detection.
- Quantify fluorescence intensity or positive cell counts to determine M2/M1 ratios [68].
- Fibrous Capsule Measurement: Using stained images, measure the thickness of the collagenous capsule surrounding the implant at multiple locations for statistical comparison [68].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for FBR and Biocompatibility Research
| Reagent / Material | Function in Experimental Protocol | Example Application |
|---|---|---|
| Polydimethylsiloxane (PDMS) | A common, versatile silicone-based polymer used as a model substrate for implant studies. | Fabrication of medical devices and as a control/test substrate in FBR studies [68]. |
| Polyimide (PI) | A high-performance polymer with excellent stability and biocompatibility. | Used as an insulating substrate or encapsulation layer for chronic neural implants [67]. |
| Hyaluronic Acid (HA) | A natural polysaccharide used as a bioactive polymer coating or bridging layer. | Serves as an interlayer to facilitate the attachment of cell coatings (e.g., RBCs) to implant surfaces [68]. |
| Anti-CD86 Antibody | A primary antibody that binds to a surface marker expressed on pro-inflammatory M1 macrophages. | Immunofluorescence staining to identify and quantify the M1 macrophage population in tissue sections [68]. |
| Anti-CD206 Antibody | A primary antibody that binds to a surface marker expressed on anti-inflammatory M2 macrophages. | Immunofluorescence staining to identify and quantify the pro-healing M2 macrophage population [68]. |
| Masson's Trichrome Stain | A three-color staining protocol that differentially colors collagen fibers blue. | Histological evaluation of the extent of fibrous encapsulation around an explained implant [68] [67]. |
Preventing Biofouling and Fibrous Encapsulation for Sustained Device Function
The long-term performance of implantable medical devices and sensors is fundamentally constrained by the host organism's biological reactions, primarily biofouling and fibrous encapsulation. Biofouling initiates with the rapid, non-specific adsorption of proteins onto implanted surfaces, forming a conditioning film that facilitates the adhesion of cells and microorganisms [70] [71]. This triggers a complex foreign body response (FBR), often culminating in the development of a dense, collagenous fibrous capsule that isolates the device from surrounding tissue [70] [72]. For organic electronic materials, this capsule acts as an electrical and diffusion barrier, severely compromising the signal fidelity of biosensors and the delivery efficiency of bioelectronics-based therapeutic devices.
Within the context of biocompatibility testing for organic electronic materials, understanding and mitigating these responses is paramount. The field is shifting from inert, "passive" materials towards "active," smart materials that can dynamically modulate the host immune response. This guide provides a comparative analysis of contemporary anti-fouling and anti-fibrotic strategies, detailing the experimental protocols and key reagents essential for evaluating their performance in a rigorous, pre-clinical research setting.
Comparative Analysis of Leading Anti-Fouling and Anti-Fibrotic Technologies
The following table summarizes the operational principles, key performance data, and comparative advantages of current state-of-the-art technologies designed to prevent biofouling and fibrous encapsulation.
Table 1: Comparison of Anti-Fouling and Anti-Fibrotic Technologies for Implantable Devices
| Technology / Strategy | Mechanism of Action | Reported Efficacy/Performance Data | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| AIM Copolymer Coatings [73] | Synergistic combination of zwitterionic (anti-fouling) blocks and HTS-derived immunomodulatory monomers. | Superior fibrosis resistance over 1 month in immunocompetent mice; architecture-dependent performance. | Dual-action strategy; versatile substrate grafting (elastomers, ceramics, metals). | Efficacy highly dependent on specific polymer chain architecture (random/block). |
| Adhesive Tissue Interfaces [72] | Creates conformal, mechanical integration with tissue, minimizing inflammatory cell infiltration. | No observable fibrous capsule on abdominal wall, colon, stomach, lung, and heart over 12 weeks in rats. | Prevents capsule formation on diverse organs; enables long-term bidirectional electrical communication. | Requires specific chemical composition (e.g., PAA-NHS/PVA); suture points can still induce focal fibrosis. |
| Surface Topography (Textured Implants) [70] | Modulates immune response via physical cues; promotes tissue ingrowth that disrupts fibrous architecture. | Textured implants show reduced capsule thickness and lower contracture rates clinically versus smooth surfaces. | Physical, non-pharmacological intervention; well-established in clinical practice (e.g., breast implants). | Risk of particulate debris from texturing; can trigger phagocytosis and inflammation. |
| Biocompatible Elastomeric OFETs [7] | Uses medical-grade elastomers (BIIR) with tissue-mimetic modulus to reduce mechanical mismatch. | Stable electrical performance under 50% strain; no major inflammatory response or tissue damage in mice. | Intrinsic material property; certified biomedical-grade materials (ISO 10993); stable operation in vivo. | Focus on material bulk properties rather than surface-specific intervention. |
| Sustainable Antifouling Coatings (Marine) [74] [75] | Biocide-free coatings (e.g., fiber-based, polyramic) or non-chemical methods (ultrasound, UVC). | AI-powered robots enable autonomous cleaning; ultrasound prevents 80-90% of fouling. | Eco-friendly; addresses regulatory restrictions; can be highly effective for macrofouling. | Primarily developed for marine environments; less focus on mammalian FBR. |
Detailed Experimental Protocols for Efficacy Validation
To objectively compare the performance of technologies like those listed in Table 1, standardized and detailed experimental protocols are essential. Below are methodologies adapted from key studies.
Protocol for In Vivo Fibrosis and Biocompatibility Assessment
This protocol is foundational for evaluating implant-tissue integration and is based on the methodology used to validate the adhesive implant interface [72].
- Objective: To quantitatively assess the extent of fibrous capsule formation and chronic foreign body reaction to an implanted material over a 12-week period.
- Materials:
- Test articles (e.g., coated/uncoated implants, ~1 cm² disks).
- Animal model (e.g., rat or mouse models, n ≥ 5 per group).
- Surgical tools, sutures.
- Procedure:
- Implantation: Anesthetize animals and create a subcutaneous pocket on the dorsum or place the implant on the surface of a target organ (e.g., abdominal wall). Secure the implant either with sutures or via its adhesive properties.
- Explanation: At predetermined endpoints (e.g., 7, 28, and 84 days post-implantation), euthanize the animals and carefully excise the implant with the surrounding tissue.
- Histological Processing: Fix the explant in 10% neutral buffered formalin, process for paraffin embedding, and section into 5 µm thick slices.
- Staining and Analysis: Stain sections with:
- Masson's Trichrome: To visualize collagen (fibrous capsule, stained blue) and measure capsule thickness.
- Hematoxylin and Eosin (H&E): For general histopathological assessment.
- Immunofluorescence Staining: To characterize the cellular immune response.
- Label sections with antibodies against: α-SMA (for myofibroblasts), CD68 (pan-macrophages), CD206 (M2 macrophages), iNOS (M1 macrophages), and CD3 (T cells).
- Use DAPI for nuclear counterstaining.
- Image using confocal microscopy and quantify cell counts in a standardized area at the implant-tissue interface.
- Key Outcome Measures:
- Average fibrous capsule thickness (µm).
- Density and phenotype of key immune cells at the interface.
- Presence of foreign body giant cells.
Protocol for Evaluating Electrical Performance Stability
This protocol is critical for validating the functional stability of organic electronic implants, as demonstrated in the development of biocompatible OFETs [7].
- Objective: To measure the stability of key electrical parameters of an organic electronic device under simulated physiological conditions and mechanical strain.
- Materials:
- Fabricated organic electronic devices (e.g., OFETs, OECTs).
- Phosphate-buffered saline (PBS) or simulated body fluid (SBF) at 37°C.
- Mechanical stretching/strain apparatus.
- Semiconductor parameter analyzer (e.g., Keysight B1500A).
- Procedure:
- Baseline Characterization: In ambient conditions, measure the transfer (Id-Vg) and output (Id-Vd) characteristics of the devices to extract baseline parameters: field-effect mobility (µ), ON/OFF current ratio, threshold voltage (Vth), and transconductance (gm).
- Stability in Biofluid: Submerge the devices in PBS (pH 7.4) at 37°C. At regular intervals (e.g., 1, 7, 14 days), remove the devices, rinse gently with deionized water, dry under a nitrogen stream, and re-measure the electrical characteristics.
- Performance Under Strain: Mount the devices on a calibrated strain stage. Measure the electrical parameters at incremental static strain levels (0%, 10%, 25%, 50%) and after repeated cyclic stretching (e.g., 1000 cycles at 20% strain).
- Key Outcome Measures:
- Percentage retention of field-effect mobility and ON/OFF ratio after immersion.
- Percentage change in mobility and transconductance as a function of applied strain.
- Device failure rate after cyclic loading.
Visualization of Key Biological Pathways and Workflows
Understanding the molecular underpinnings of the foreign body response is crucial for developing targeted interventions. The following diagrams map this process and a generalized experimental workflow.
The Foreign Body Response and Fibrosis Pathway
This diagram illustrates the sequential cellular and molecular events that lead to fibrous encapsulation, highlighting potential intervention points.
Diagram Title: Foreign Body Response to Implants
Biocompatibility Testing Workflow
This flowchart outlines a standardized experimental workflow for evaluating new anti-fouling materials or coatings.
Diagram Title: Biocompatibility Testing Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on a suite of specialized reagents and materials. The following table details key components for developing and testing anti-fouling strategies.
Table 2: Essential Research Reagents and Materials for Anti-Fouling Studies
| Reagent / Material | Function / Role | Specific Example(s) / Notes |
|---|---|---|
| Zwitterionic Monomers [73] | Form highly hydrophilic, neutral surfaces that resist non-specific protein adsorption, the critical first step of biofouling. | Sulfobetaine methacrylate (SBMA), carboxybetaine acrylamide (CBAA). Used as building blocks in AIM copolymers. |
| Medical-Grade Elastomers [7] | Provide the bulk mechanical properties (low modulus, stretchability) that match biological tissues, minimizing mechanical mismatch. | Bromo isobutyl-isoprene rubber (BIIR), Polydimethylsiloxane (PDMS). BIIR is certified per ISO 10993 biocompatibility standards. |
| HTS-Derived Antifibrotic Monomers [73] | Actively modulate the host immune response to downregulate pro-fibrotic pathways, directly targeting fibrosis. | Specific chemistries are often proprietary; identified from high-throughput screening of immune cell responses to polymer libraries. |
| Adhesive Hydrogel Components [72] | Create stable, conformal interfaces that integrate implants with wet tissue surfaces, preventing inflammatory cell infiltration. | Poly(acrylic acid) N-hydroxysuccinimide ester (PAA-NHS) and Poly(vinyl alcohol) (PVA) for interpenetrating networks. |
| Antibodies for Immunofluorescence [72] [71] | Enable precise identification and quantification of specific cell types involved in the foreign body response in tissue sections. | α-SMA (myofibroblasts), CD68 (macrophages), CD206 (M2 macrophages), iNOS (M1 macrophages), CD3 (T cells). |
| Fluorescently-Labelled Proteins [72] | Allow for quantitative in vitro assessment of the initial protein fouling on a material surface. | Albumin and Fibrinogen, the most abundant proteins in plasma and key initiators of the FBR. |
The pursuit of sustained device function requires a multi-faceted approach that moves beyond inert encapsulation. As evidenced by the comparative data, emerging strategies like AIM copolymers and adhesive interfaces show remarkable promise by actively engaging with and modulating the biological environment. For researchers in organic electronic materials, the integration of these surface-focused anti-fouling technologies with the inherent softness and compliance of materials like BIIR-based OFETs represents a powerful path forward [7] [73] [72]. Validating these advanced materials demands a rigorous, multi-modal approach combining the quantitative histological and functional protocols outlined herein. By leveraging this comprehensive toolkit of strategies, assays, and reagents, the scientific community can accelerate the development of next-generation bioelectronic devices that maintain seamless, long-term communication with the body.
Strategies for Enhancing Long-Term Stability and Corrosion Resistance
In the rapidly advancing field of biocompatible organic electronics, the long-term stability and corrosion resistance of materials are paramount for the successful development of implantable biosensors, neural interfaces, and wearable health monitoring devices. These devices must operate reliably within harsh physiological environments characterized by the presence of moisture, ions, and varying pH levels, which can degrade electronic components and leach harmful materials into surrounding tissues. This guide objectively compares the performance of leading material strategies—including conductive polymers, metal-organic frameworks (MOFs), and organic-inorganic composites—in enhancing device longevity. By presenting synthesized experimental data and detailed methodologies, we provide researchers and drug development professionals with a clear framework for selecting and validating materials that meet the dual demands of electronic performance and biological safety.
Comparative Analysis of Material Strategies
The pursuit of stable organic electronics has yielded several strategic approaches to corrosion protection. The following table provides a high-level comparison of the primary strategies, their mechanisms, and their performance characteristics.
Table 1: Comparison of Key Strategies for Stability and Corrosion Resistance
| Strategy | Key Materials / Components | Protection Mechanism | Reported Performance Data | Key Advantages | Limitations / Challenges |
|---|---|---|---|---|---|
| Conductive Polymer Blends & Coatings | PEDOT:PSS, Polyaniline (PANI), DPPT-TT with BIIR elastomer [7] | Formation of a passive oxide layer; barrier protection; inherent biocompatibility and mechanical matching [7] [76]. | • Stable electrical performance under 50% strain.• No major inflammatory response in vivo (mice) [7]. | High flexibility; excellent biocompatibility; suitable for implantable, stretchable electronics [7] [17]. | Potential degradation at voltages >0.5 V; long-term stability under continuous electrical bias requires careful design [77]. |
| Metal-Organic Frameworks (MOFs) | ZIF-8, UiO-66, MIL-53 [78] [79] | Acts as nanofiller to enhance barrier properties; functions as a nanocontainer for corrosion inhibitors; provides hydrophobic surfaces [78] [79]. | • Improved corrosion resistance in epoxy coatings.• Responsive, self-healing inhibitor release [78] [79]. | Tunable porosity and functionality; high surface area; multifunctional platform [78] [79]. | Challenges in scalability and production cost; long-term stability of MOFs themselves in coatings [79]. |
| Organic-Inorganic Nanocomposites | HQZn-doped Polyaniline (HQZn-PA) in epoxy [76] | Synergistic anodic (PANI) and cathodic (Zn²⁺) protection; organic inhibitor (HQ) provides self-healing [76]. | • Corrosion rate reduced by 450x vs. neat epoxy.• Impedance modulus of 1.03 × 1010 Ω·cm² after 40 days in saline.• 99.28% self-healing efficiency [76]. | High, quantifiable corrosion resistance; active self-healing capability; strong synergistic effect. | Complex synthesis; dispersion stability in the polymer matrix can be challenging. |
| Hybrid Organic-Inorganic Coatings | Plasma Electrolytic Oxidation (PEO) layer sealed with Thiourea [80] | PEO base layer provides initial barrier; organic inhibitor (Thiourea) blocks micropores and provides secondary protection [80]. | • Clear decrease in corrosion current in electrochemical tests.• Effective pore sealing observed via SEM [80]. | Excellent adhesion to metal substrates (e.g., Mg alloys); leverages well-established PEO process. | Multi-step fabrication process; performance dependent on uniformity of organic sealing layer. |
Detailed Experimental Protocols and Performance Data
To ensure the reproducibility of corrosion protection studies, researchers employ standardized electrochemical and environmental testing protocols. The workflows and resulting data provide critical validation for new materials.
Standard Electrochemical Corrosion Testing
Electrochemical tests are the cornerstone for quantifying corrosion protection performance in simulated physiological conditions.
Table 2: Key Electrochemical Tests for Evaluating Corrosion Resistance
| Test Method | Standard Protocol | Key Measured Parameters | Interpretation of Results | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Electrochemical Impedance Spectroscopy (EIS) | • ASTM G59/G102 [76].• 3-electrode cell (Ag/AgCl reference, Pt counter, coated sample as working electrode).• Frequency range: 105 Hz to 10-1 Hz [76] [80].• Disturbance signal: 5-10 mV [76] [80]. | Impedance modulus ( | Z | ), Phase Angle, Coating Pore Resistance (Rpo), Charge Transfer Resistance (Rct). | A higher | Z | value at low frequency (e.g., 0.1 Hz) indicates better barrier protection. A stable or increasing | Z | over long immersion times signifies superior long-term stability [76]. |
| Potentiodynamic Polarization (PDP) | • Scan from -0.3 V to +0.4 V vs. Open Circuit Potential (OCP) [80].• Scan rate: 1 mV/s [80].• Environment: 3.5% NaCl solution [76] [80]. | Corrosion Potential (Ecorr), Corrosion Current Density (Icorr). | A positive shift in Ecorr and a significant decrease in Icorr indicate improved corrosion resistance. Icorr is directly related to the corrosion rate [80]. | ||||||
| Open Circuit Potential (OCP) Monitoring | • Measure the potential of the working electrode vs. reference over time without an applied current. | Stability of OCP over time. | A stable OCP suggests a passive, protective surface. Fluctuations can indicate localized corrosion or coating breakdown. |
Figure 1: Experimental workflow for standard electrochemical corrosion testing, combining EIS and PDP measurements for a comprehensive performance assessment.
Accelerated Aging and In-Operando Stability Testing
For organic electronics, testing under operational conditions is critical. A 2025 study on biocompatible elastomeric transistors established a robust protocol for assessing in-operando stability [7]. The methodology involves fabricating stretchable organic field-effect transistors (sOFETs) from a blend of DPPT-TT semiconducting nanofibers and bromo isobutyl–isoprene rubber (BIIR), followed by in-vivo implantation in mice. Key stability tests include:
- Electrical Performance under Strain: Characterizing field-effect mobility and ON/OFF ratio at 0% to 100% strain to ensure mechanical robustness [7].
- Cyclic Endurance Testing: Subjecting devices to 1,000 stretching cycles at 100% strain and monitoring for degradation in electrical performance [7].
- In-Vivo Biocompatibility and Stability: Implanting devices in animal models (e.g., mice) for extended periods to monitor inflammatory response, tissue damage, and device functionality through histological analysis and electrical characterization [7].
Protection Mechanisms and Material Functionality
The most effective strategies often employ multiple mechanisms to combat corrosion. The following diagram illustrates the synergistic action of a self-healing nanocomposite coating.
Figure 2: Multifunctional protection mechanism of an organic-inorganic nanocomposite coating like HQZn-PA, showing synergistic anodic, barrier, and self-healing effects [76].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on a specific set of materials and reagents, each serving a distinct function in developing and testing stable, corrosion-resistant organic electronics.
Table 3: Essential Reagents and Materials for Research and Development
| Material / Reagent | Function in Research | Specific Examples / Notes |
|---|---|---|
| Conductive Polymers | Form the active semiconducting or conducting layer in devices; can provide inherent corrosion protection. | PEDOT:PSS: Often used with additives (ethylene glycol) or post-treatments (H₂SO₄) to enhance conductivity and stability [77] [10].Polyaniline (PANI): Used in its emeraldine salt form; can be doped with acids or inhibitors (e.g., HQZn) for enhanced functionality [76] [10]. |
| Biocompatible Elastomers | Provide flexible, stretchable, and biocompatible matrix for electronic components; reduce mechanical mismatch with tissue. | Bromo Isobutyl–Isoprene Rubber (BIIR): A medical-grade elastomer meeting ISO 10993 standards; blended with semiconductors for implantable devices [7]. |
| Corrosion Inhibitors | Provide active corrosion protection by forming a protective layer on the metal substrate; can be released in a self-healing mechanism. | 8-Hydroxyquinoline (8-HQ) and derivatives: Organic chelators that form insoluble complexes with metal ions (e.g., Zn²⁺, Mg²⁺) [76].Thiourea: Contains S and N heteroatoms that adsorb onto metal surfaces, blocking active corrosion sites [80]. |
| Metal-Organic Frameworks (MOFs) | Act as smart nanofillers or nanocontainers in protective coatings; can be loaded with inhibitors. | ZIF-8, UiO-66: Popular for their good chemical stability; can be modified for better dispersion in polymer matrices like epoxy [78] [79]. |
| Electrochemical Cell Components | Essential for conducting standardized corrosion tests (EIS, PDP). | Electrolyte: 3.5% NaCl solution simulates a saline/physiological environment [76] [80].Electrodes: Ag/AgCl reference electrode, Platinum counter electrode, coated metal sample as working electrode [76]. |
| Metal Substrates | Serve as the base material for coating development and testing. | Q235 Steel: Common low-carbon steel for industrial testing [76].AZ31 Mg Alloy: Used for testing coatings for lightweight biodegradable implants [80]. |
The comparative data presented in this guide demonstrates that no single strategy universally surpasses all others; rather, the optimal choice is dictated by the specific application requirements. For implantable electronics requiring direct tissue integration, biocompatible conductive polymer blends like DPPT-TT/BIIR offer an unparalleled combination of electrical performance, mechanical compliance, and documented in-vivo stability [7]. For applications demanding the highest possible corrosion resistance in harsh environments, organic-inorganic nanocomposites like HQZn-PA provide exceptional, quantifiable protection and self-healing functionality [76]. MOF-based coatings represent a promising, tunable platform for "smart" corrosion protection but require further development to overcome cost and scalability challenges [78] [79]. As the field progresses, the integration of machine learning for material design and a intensified focus on eco-friendly, scalable synthesis methods will be crucial to advance these technologies from the laboratory to industrial and clinical real-world applications.
In the field of biocompatibility testing for organic electronic materials, the evaluation of leachables and extractables (E&L) represents a critical frontier in ensuring patient safety and device functionality. Organic electronic materials, including conducting polymers and semicrystalline materials, present unique challenges and opportunities in E&L assessment due to their complex chemical structures and interactions with biological systems [2]. Unlike traditional abiotic electronic materials, organic semiconductors facilitate mixed ionic and electronic charge transport, creating interfaces that more closely mimic biological tissue but require sophisticated characterization approaches [2].
The mechanical and charge transport properties of organic semiconductors make them particularly suitable for bioelectronic applications, with Young's modulus ranging from 20 kPa to 3 GPa – much closer to living tissue (~10 kPa) than inorganic semiconductors (~100 GPa) [2]. This mechanical compatibility, however, necessitates rigorous evaluation of potential chemical migration under physiological conditions. As the medical device industry evolves under the EU Medical Device Regulation (MDR) and other global standards, comprehensive chemical characterization has become not merely beneficial but mandatory for regulatory compliance [81].
This guide examines the current methodologies, standards, and experimental approaches for E&L assessment, with particular emphasis on their application to emerging organic electronic materials used in drug delivery systems, implantable devices, and other biomedical applications.
Fundamental Concepts and Definitions
Extractables and Leachables: Core Definitions
Understanding the distinction between extractables and leachables is fundamental to proper chemical characterization:
Extractables are compounds that can be released from a medical device or material when extracted under laboratory conditions, typically using aggressive solvents and exaggerated temperature and time parameters. This represents a "worst-case scenario" to identify potential chemical migrants [82] [83] [84].
Leachables are chemical compounds that actually migrate from a device into a patient or drug product during normal clinical use conditions. Leachables are typically a subset of extractables, though not always [82] [85] [83].
Regulatory Significance in Biocompatibility
For organic electronic materials, E&L assessment forms a crucial component of the biological safety evaluation required by ISO 10993 standards [82] [81]. The chemical characterization process outlined in ISO 10993-18 provides the foundation for toxicological risk assessment, which in turn addresses multiple biocompatibility endpoints [82]. This is particularly relevant for organic electronic materials, where the potential for electrochemical degradation or polymer breakdown must be evaluated alongside conventional material concerns [2].
The migration of chemicals from device materials can lead to multiple adverse outcomes, including direct patient toxicity, degradation of device performance, and compromised drug efficacy [83] [84]. For sensitive bioelectronic applications such as neural interfaces or implantable sensors, even minimal leaching could interfere with device functionality or elicit inflammatory responses that compromise the device-tissue interface [2].
Analytical Techniques for Chemical Characterization
Comprehensive Analytical Approaches
A combination of analytical techniques is required to fully characterize the diverse range of potential extractables and leachables from organic electronic materials. The following table summarizes the core techniques employed in comprehensive E&L studies:
Table 1: Analytical Techniques for Extractables and Leachables Characterization
| Technique | Application | Compounds Detected | Key Considerations |
|---|---|---|---|
| Headspace GC-MS (HS-GC-MS) [82] [84] [81] | Volatile organic compounds (VOCs) | Residual solvents, monomers, degradation products | Requires no solvent interference; ideal for low-boiling point compounds |
| GC-MS (Gas Chromatography-Mass Spectrometry) [82] [83] [84] | Semi-volatile organic compounds (SVOCs) | Plasticizers, antioxidants, stabilizers, hydrocarbons | Excellent for thermally stable, semi-volatile compounds |
| LC-MS (Liquid Chromatography-Mass Spectrometry) [82] [83] [84] | Non-volatile organic compounds (NVOCs) | Polymer additives, degradation products, intentionally added compounds | Handles thermally labile compounds; compatible with diverse compound polarities |
| ICP-MS/OES (Inductively Coupled Plasma-Mass Spectrometry/Optical Emission Spectroscopy) [82] [83] [81] | Elemental impurities/metals | Catalysts, fillers, pigment residues, inorganic additives | Extremely sensitive to trace metals; requires specialized sample preparation |
| IC (Ion Chromatography) [82] [81] | Dissolved ions | Anionic and cationic species, extractable ions | Complementary to organic techniques; important for biological response assessment |
Advanced and Emerging Techniques
As organic electronic materials increase in complexity, advanced analytical approaches are being employed:
High Resolution Accurate Mass (HRAM) LC-MS provides superior capability for identifying unknown compounds through exact mass measurement, crucial for characterizing complex polymer formulations and degradation products [84].
Differential Scanning Calorimetry (DSC) and Fourier Transform Infrared Spectroscopy (FTIR) complement the primary techniques by providing information about material properties and functional groups that may influence extraction behavior [82].
Combined targeted and non-targeted screening approaches enable simultaneous quantification of specific compounds of concern while maintaining the capability to discover unexpected leachables, particularly important for novel material formulations [86].
For organic electronic materials specifically, additional considerations include the potential for electrochemical leaching under operating conditions and the evaluation of polymer-specific impurities that may not be present in conventional medical device materials [2].
Experimental Design and Methodologies
Extraction Study Design
Proper extraction study design is critical for meaningful E&L assessment. The International Organization for Standardization provides guidance in ISO 10993-12 and ISO 10993-18 for selecting appropriate extraction conditions based on device characteristics and clinical use [82] [81].
Table 2: Extraction Conditions Based on Device Contact Duration
| Contact Duration | Extraction Approach | Typical Conditions | Rationale |
|---|---|---|---|
| Limited (< 24 hours) [81] | Simulated use conditions | 37°C for 24-72 hours [81] | Mimics actual clinical exposure conditions |
| Prolonged (24 hours - 30 days) [81] | Exhaustive or exaggerated conditions | 50-121°C for 24-72 hours [82] [81] | Accelerates extraction to represent maximum potential exposure |
| Long-term (> 30 days) [81] | Exhaustive conditions | Repeated extractions until <10% additional extraction by mass [82] | Determines the total potential extractables pool |
Solvent selection must account for the device's material composition and clinical use environment. Typically, multiple solvents with varying polarities are employed to ensure comprehensive extraction of compounds with different chemical properties [81]. Common solvents include:
- Polar solvents: Water, saline (simulating aqueous physiological fluids)
- Semi-polar solvents: Ethanol, isopropanol (simulating lipid-containing tissues)
- Non-polar solvents: Hexane, heptane (evaluating lipophilic compounds)
For organic electronic materials, additional consideration should be given to electrically conductive solutions that simulate the operational environment, particularly for devices that will be actively functioning during implantation [2].
Experimental Workflow
The following diagram illustrates the comprehensive workflow for E&L assessment, integrating both chemical characterization and risk assessment components:
E&L Assessment Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for E&L Studies
| Item | Function | Application Notes |
|---|---|---|
| Reference Standards [82] | Compound identification and quantification | Include FDA CLAP dataset compounds; internal standards for GC/MS and LC/MS |
| Solvent Systems [81] | Extraction media | Polar (water/saline), semi-polar (ethanol), non-polar (hexane) to cover solubility range |
| Quality Control Materials [82] | Method validation | Positive controls, system suitability standards, blank matrices |
| Solid Phase Microextraction (SPME) Fibers [85] | Solventless extraction | Particularly useful for volatile compounds; minimizes solvent interference |
| ICP-MS Tuning Solutions [85] [84] | Instrument calibration | Ensure accuracy and sensitivity for elemental impurities |
| Column Chemistry Suite [86] [85] | Chromatographic separation | Reverse-phase, HILIC, GC columns with varying stationary phases |
Risk Assessment Frameworks and Methodologies
Toxicological Risk Assessment Principles
The toxicological risk assessment (TRA) process transforms analytical chemistry data into meaningful safety conclusions. This process involves several key components:
Analytical Evaluation Threshold (AET) Establishment: The AET is a concentration limit derived from toxicological concerns that determines which analytes require identification and quantification [81]. The AET is calculated based on the device's contact category, duration of body contact, and the number of devices a user would be exposed to daily [81].
Permitted Daily Exposure (PDE) and Threshold of Toxicological Concern (TTC): These concepts establish safety thresholds for compounds without specific toxicity data [86]. The TTC represents a generic exposure level considered to pose negligible risk, while PDE is compound-specific [86].
Compounds of Specific Concern: Certain compounds, such as nitrosamines, polycyclic aromatic hydrocarbons (PAHs), and metals like cadmium and lead, require special consideration due to their potent toxicity even at low concentrations [86] [83].
Risk Assessment Using ICH Q9 Framework
The ICH Q9 quality risk management framework provides a structured approach to leachables risk assessment, comprising risk identification, risk analysis, and risk evaluation [87].
The following diagram illustrates the risk assessment process within the broader risk management framework:
Risk Assessment in Risk Management
Risk Scoring and Evaluation
Risk analysis involves scoring identified risks based on severity and probability dimensions:
Severity Scoring evaluates the potential consequences of a hazard, considering factors such as compound-specific toxicity, concentration levels, and patient population susceptibility [87].
Probability Scoring estimates the likelihood that a risk will occur, considering factors such as extraction studies data, material composition knowledge, and clinical use conditions [87].
Table 4: Example Risk Scoring Matrix
| Severity → Probability ↓ | Low (1) | Medium (3) | High (6) | Very High (10) |
|---|---|---|---|---|
| Very Low (1) | 1 | 3 | 6 | 10 |
| Low (3) | 3 | 9 | 18 | 30 |
| High (6) | 6 | 18 | 36 | 60 |
| Very High (10) | 10 | 30 | 60 | 100 |
The resulting Risk Priority Number (RPN) guides risk evaluation and control decisions. Generally, RPN scores ≥ 28 or individual severity/probability scores of 10 require immediate risk mitigation measures [87].
Special Considerations for Organic Electronic Materials
Unique Material Properties and Challenges
Organic electronic materials present distinctive considerations for E&L assessment compared to conventional medical device materials:
Mixed Ionic-Electronic Conduction: The ability of organic semiconductors to transport both electronic and ionic charges creates unique interfaces with biological tissues but may also facilitate different leaching profiles compared to inert materials [2].
Electrochemical Degradation: Under operational conditions, organic electronic materials may undergo electrochemical reactions that generate degradation products not observed in conventional extraction studies [2].
Dynamic Material Properties: The soft, flexible nature of organic semiconductors (with Young's modulus of 20 kPa to 3 GPa) may lead to material changes under physiological conditions that affect leaching behavior [2].
Complex Dopant Systems: Intentionally added dopants necessary for electronic functionality may represent new classes of potential leachables requiring specialized analytical approaches [2].
Emerging Challenges and Future Directions
The field of E&L assessment for organic electronic materials continues to evolve with several emerging areas of focus:
Per- and Polyfluoroalkyl Substances (PFAS): Increased scrutiny on PFAS compounds migrating from fluoropolymer components used in single-use systems and device packaging [86].
Combination Products: Complex drug-device combination products, particularly those involving biologics, present unique challenges due to the potential interactions between leachables and sensitive therapeutic agents [83].
Advanced Modeling Approaches: Mass transport modeling and in silico (Q)SAR methods are increasingly used to complement experimental data, particularly when experimental analysis is challenging or when screening multiple material formulations [86] [87].
Standardization Efforts: Organizations such as ELSIE (Extractable/Leachable Safety Information Exchange) are working to establish best practices and improve consistency in E&L studies across different laboratories [86] [87].
The chemical characterization and risk assessment of leachables and extractables represent a critical component in the development of safe and effective medical devices utilizing organic electronic materials. As these innovative materials enable new generations of bioelectronic therapies, robust and scientifically rigorous E&L assessment methodologies must evolve in parallel.
The framework presented in this guide integrates current regulatory expectations with practical experimental approaches, emphasizing the unique considerations for organic electronic materials. By adopting a systematic approach to E&L assessment—from proper material characterization through comprehensive toxicological risk assessment—researchers and device developers can effectively manage potential chemical risks while advancing the field of organic bioelectronics.
The continuing evolution of international standards, analytical technologies, and risk assessment methodologies will further enhance our ability to ensure the safety of these promising biomedical technologies while accelerating their translation from research to clinical application.
The field of organic bioelectronics represents a paradigm shift in medical device technology, offering unprecedented opportunities for seamless integration of electronics with biological systems. Unlike traditional inorganic electronics that rely on rigid materials like silicon, organic electronics utilize carbon-based molecules and polymers that demonstrate mechanical flexibility, biocompatibility, and tunable electronic properties [88]. These characteristics enable the development of devices that can conform to the human body and interface seamlessly with biological tissues, making them ideal for wearable health monitors, implantable sensors, and therapeutic systems [88] [2].
The central challenge in this rapidly advancing field lies in balancing two critical requirements: manufacturing scalability and biological compatibility. While organic materials offer inherent advantages for biointegration, their translation from laboratory prototypes to commercially viable products requires manufacturing processes that can be scaled cost-effectively without compromising the stringent biocompatibility standards demanded by regulatory agencies [2] [89]. This balance is particularly crucial for applications involving long-term implantation or direct tissue contact, where material degradation products must be non-toxic and device performance must remain stable under physiological conditions [2] [90].
The growing market for organic electronics, projected to reach $721.84 billion by 2033, underscores the commercial significance of resolving these manufacturing-biocompatibility challenges [89]. This review systematically compares current manufacturing approaches, their compatibility with biocompatibility requirements, and provides experimental frameworks for evaluating novel materials destined for biomedical applications.
Manufacturing Approaches: Scalability and Biocompatibility Considerations
Comparative Analysis of Manufacturing Techniques
Table 1: Comparison of manufacturing techniques for organic bioelectronics
| Manufacturing Technique | Scalability Potential | Biocompatibility Considerations | Resolution | Cost Efficiency | Key Applications |
|---|---|---|---|---|---|
| Solution-based Processing & Photopatterning [91] | High | Excellent (uses biocompatible/degradable materials) | Few microns | High | Transient implants, wearable sensors |
| Printed Electronics [36] | High | Good (compatible with soft, conformable substrates) | 10-100 microns | Medium-High | Smart wound dressings, skin patches |
| Fiber-Based Fabrication [92] | Medium-High | Excellent (minimal tissue disruption) | N/A (fiber-level) | Medium | Implantable sensors, smart sutures |
| Vacuum Deposition [89] | Medium | Variable (requires additional biocompatibility layers) | Sub-micron | Low-Medium | OLED displays, high-performance OFETs |
| Cleanroom Microfabrication [36] | Low | Variable (often requires surface modification) | Sub-micron | Low | High-density neural interfaces |
Emerging Strategies for Scalable Biocompatible Manufacturing
Recent advances in manufacturing have focused on techniques that simultaneously address scalability and biocompatibility requirements. Solution-processable and photo-patternable approaches represent particularly promising directions, as they enable monolithic 3D fabrication of soft, stretchable transient electronics using biodegradable organic insulators, semiconductors, and conductors [91]. This methodology employs direct solution-casting of materials to fabricate sensors with various modalities and transistors, demonstrating compatibility with wafer-scale production while maintaining biocompatibility [91].
Printed electronics have emerged as another scalable approach, harnessing stretchable foils, bio-derived functional materials, and organic electronics to develop biodegradable and bioresorbable monitoring systems [36]. The compatibility of printing techniques with soft, conformable substrates enables the creation of devices that minimize mechanical mismatch with biological tissues, thereby reducing inflammatory responses [2] [36].
Fiber-based electronic devices (FEDs) offer unique advantages for biomedical applications, as their fine diameter and mechanical flexibility facilitate minimally invasive implantation and chronic stability with minimal immune reactions [92]. These devices can be integrated into smart sutures containing electrochemical or mechanical sensors, enabling both diagnostic functionality and structural support while simplifying surgical workflows [92].
Biocompatibility Testing Frameworks: Standards and Methodologies
Regulatory Framework and Testing Classifications
Biocompatibility assessment for organic electronic materials follows internationally recognized standards, primarily the ISO 10993 series (Biological evaluation of medical devices), which specifies testing requirements based on the type of body contact and duration of exposure [2]. According to these standards, biocompatibility is not an intrinsic material property but rather "a condition met by a biomaterial or medical device usually based on the tissue response elicited by an implant in an animal model" [2]. This context-dependent definition underscores the importance of tailoring testing strategies to specific application environments.
The interaction between implanted bioelectronic devices and host tissues can be categorized into four distinct responses:
- Toxic: The material induces adverse effects on surrounding tissue, including cell death, immunological response, or inflammation
- Bioinert: Non-toxic but biologically inactive materials that may still provoke fibrous encapsulation
- Bioactive: Non-toxic materials that form intimate connections with host tissue
- Bioresorbable: Non-toxic materials that dissolve in host tissue and are eventually replaced by native tissue [2]
Organic semiconductors often demonstrate advantages over traditional abiotic materials by matching the mechanical and conduction properties of biotic tissue more closely, potentially reducing adverse immune responses [2].
Experimental Workflow for Biocompatibility Assessment
The following diagram illustrates a standardized workflow for assessing the biocompatibility of organic electronic materials, incorporating both in vitro and in vivo evaluation stages:
Biocompatibility Assessment Workflow
Standardized Testing Protocols
In Vitro Cytotoxicity Testing (ISO 10993-5)
Purpose: To identify potential toxic effects of material extractables or direct contact on cultured cells.
Methodology:
- Cell Lines: Use primary cells or immortalized cell lines relevant to the target tissue
- Direct Contact Assay: Place material specimens directly on cell monolayers and incubate for 24-72 hours at 37°C
- Extract Dilution Assay: Prepare extracts of materials using appropriate solvents (saline, culture media) and apply to cell cultures
- Assessment Methods:
- Mitochondrial dehydrogenase performance measurement (MTT assay)
- XTT (tetrazolium dye) cell proliferation assay
- Neutral red uptake cytotoxic assay
- Colony formation cytotoxic assay [2]
Acceptance Criteria: Materials demonstrating >70% cell viability relative to negative controls are generally considered non-cytotoxic.
In Vivo Implantation Testing (ISO 10993-6)
Purpose: To evaluate the local tissue response to implanted materials over extended periods.
Methodology:
- Animal Model: Select appropriate species (typically rodents or larger mammals) based on intended application
- Implantation: Insert material specimens or functional devices into subcutaneous tissue or site-specific locations
- Duration: Acute (1-12 weeks) or chronic (12-104 weeks) based on intended use
- Assessment:
- Histopathological evaluation of tissue response at explanation
- Scoring of inflammation, fibrosis, and tissue integration
- Immunohistochemical analysis of immune cell markers [2]
Interpretation: Compare tissue response to negative (medical-grade materials with known biocompatibility) and positive controls (materials known to elicit adverse reactions).
Material Performance Comparison: Quantitative Analysis
Electrical and Mechanical Properties of Organic Electronic Materials
Table 2: Performance comparison of organic electronic materials for biomedical applications
| Material | Charge Carrier Mobility (cm²/V·s) | Young's Modulus | Biocompatibility Profile | Degradation Timeline | Key Applications |
|---|---|---|---|---|---|
| PEDOT:PSS [2] [91] | 0.1 - 10 | 20 kPa - 2 MPa (gels) | Excellent (stable for >7 months in vivo) | Non-degradable (stable) | Neural interfaces, electrodes |
| P3HT-based Semiconductors [91] | 0.01 - 1 | Tunable with PLCL ratio | Good (compatible with transient electronics) | Controllable degradation (0.12 μm/day) | Transient implants, biosensors |
| UV-PLCL Substrates [91] | N/A (insulator) | 0.1 - 2 MPa (tunable) | Excellent (biodegradable, biocompatible) | pH-dependent (0.21 μm/day at pH 7) | Substrates for transient electronics |
| Pentacene [89] | 0.1 - 10 | ~100 MPa - 3 GPa | Variable (requires encapsulation) | Non-degradable | OFETs, high-performance devices |
| PLCL-P3HT Composite [91] | 0.05 - 0.5 | 1 - 100 MPa | Excellent (bioresorbable) | Programmable degradation | Soft, stretchable transistors |
Performance Limitations and Trade-offs
While organic electronic materials offer compelling advantages for biomedical applications, they face performance limitations compared to conventional inorganic semiconductors. The charge carrier mobility in state-of-the-art organic semiconductors typically ranges between 0.1 cm²/V·s and 10 cm²/V·s, significantly lower than crystalline silicon which exhibits mobilities exceeding 1,000 cm²/V·s [89]. This limitation restricts the operational frequency of organic field-effect transistors (OFETs) to below 100 MHz, making them unsuitable for high-speed computing applications but sufficient for most bio-sensing and stimulation purposes [89].
The operational lifetime of organic electronic devices represents another consideration, particularly for implantable applications. Under continuous usage, OLED lifetimes typically range between 20,000 to 50,000 hours, considerably lower than LED or LCD counterparts [89]. Similarly, organic photovoltaic cells can experience efficiency losses up to 20% within five years without adequate protection from environmental exposure [89]. These limitations necessitate advanced encapsulation strategies for long-term implantable devices.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for biocompatible organic electronics
| Reagent/Material | Function | Application Examples | Biocompatibility Considerations |
|---|---|---|---|
| PEDOT:PSS [2] [91] | Conductive polymer | Electrodes, neural interfaces, biosensors | Excellent biocompatibility; stable in physiological environments |
| P3HT (Poly(3-hexylthiophene)) [91] | Organic semiconductor | Transistors, photovoltaics, sensors | Requires encapsulation or blending with biodegradable polymers |
| PLCL (Poly(l-lactide-co-ε-caprolactone)) [91] | Biodegradable substrate/insulator | Temporary implants, flexible substrates | Tunable degradation rate; biocompatible degradation products |
| UV-PLCL [91] | Photo-patternable biodegradable elastomer | Monolithic 3D device fabrication | Biocompatible with programmable dissolution profiles |
| Poly(3,4-ethylenedioxythiophene) (PEDOT) [2] | Neural interface material | Deep brain stimulation, recording electrodes | Demonstrates stability for over 7 months in vivo |
| Diazirine Crosslinker [91] | Semiconductor crosslinking agent | Enhancing mechanical properties of semiconducting films | Biocompatible at optimal concentrations (~2 ratio) |
| Zonyl FS-300 [91] | Surfactant | Improving processability of organic semiconductors | Requires cytotoxicity testing at application-specific concentrations |
The successful development of organic bioelectronic devices requires careful balancing of manufacturing scalability with stringent biocompatibility requirements. Solution-processable and printable approaches offer the most promising path forward, enabling cost-effective production while maintaining compatibility with delicate biological environments. As the field advances, key considerations include the development of standardized testing protocols specific to organic electronic materials, improved encapsulation technologies to enhance device lifetime, and continued innovation in biodegradable conductive and semiconducting materials.
Future research should focus on establishing clearer structure-property relationships between material composition, processing parameters, and biological responses. Additionally, closer collaboration between academic researchers, industry partners, and regulatory bodies will be essential for creating standardized frameworks that accelerate the translation of promising laboratory innovations into clinically viable products. By systematically addressing these challenges, the field of organic bioelectronics can realize its potential to revolutionize healthcare monitoring, diagnostics, and therapeutics.
Validation and Comparative Analysis: From In Vitro to In Vivo Performance
Designing Robust In Vitro to In Vivo Correlation Studies
In the fields of pharmaceutical development and biomedical engineering, the establishment of a robust In Vitro-In Vivo Correlation (IVIVC) is a critical milestone. IVIVC is defined as a predictive mathematical model describing the relationship between an in vitro property of a dosage form and a relevant in vivo response [93]. For researchers working with advanced materials like organic electronic implants, developing a valid IVIVC is particularly challenging yet immensely valuable. It enables the prediction of in vivo performance based on controlled in vitro experiments, thereby reducing development costs, minimizing animal testing, and accelerating the translation of new technologies to clinical applications [93] [94].
The context of biocompatibility testing for organic electronic materials introduces unique complexities to IVIVC development. These materials, which include conductive polymers and elastomeric semiconductors, are designed to interface seamlessly with biological systems [7] [17]. Unlike conventional pharmaceuticals, the performance of bioelectronic devices depends not only on drug release kinetics but also on electronic properties, mechanical compatibility, and long-term stability under physiological conditions. This article provides a comprehensive comparison of IVIVC methodologies, experimental protocols, and research tools essential for creating robust correlations that can reliably predict the in vivo behavior of biomedical products.
Understanding IVIVC Levels and Applications
Classification of IVIVC Levels
The United States Pharmacopeia (USP) defines IVIVC as "the establishment of a rational relationship between a biological property, or a parameter derived from a biological property, produced by a dosage form, and a physicochemical property or characteristic of the same dosage form" [93]. Regulatory agencies recognize multiple levels of IVIVC, each with different predictive strength and regulatory utility [93]:
Table: Levels of In Vitro-In Vivo Correlation
| Correlation Level | Description | Regulatory Utility | Application Context |
|---|---|---|---|
| Level A | Point-to-point relationship between in vitro dissolution and in vivo input rate | Highest; can support bioequivalence waivers | Ideal for formulations where release controls absorption |
| Level B | Comparison of mean in vitro dissolution time to mean in vivo residence time | Limited; uses statistical moment analysis | Useful for formulation ranking during development |
| Level C | Relationship between single dissolution time point and pharmacokinetic parameter (AUC, Cmax) | Moderate; multiple Level C may approach Level A | Supports formulation optimization and quality control |
| Multiple Level C | Expands Level C to multiple dissolution time points and PK parameters | Higher than single Level C | Justifies certain post-approval changes |
| Level D | Qualitative analysis without formal correlation | No regulatory value; developmental guidance | Preliminary formulation screening |
Applications in Drug Delivery and Biomaterials
IVIVC methodologies have been successfully applied across various formulation types. For lipid-based formulations (LBFs), which are crucial for enhancing the oral bioavailability of poorly water-soluble drugs, IVIVC enables rational formulation design despite complex processes involving lipid digestion, solubilization, and permeation [93]. Similarly, for vaginal drug delivery systems, IVIVC relationships combined with Physiologically Based Pharmacokinetic (PBPK) modeling have supported the establishment of virtual bioequivalence (VBE) and dissolution safe space limits [95] [96].
In the emerging field of organic bioelectronics, IVIVC principles are being adapted to correlate material properties with biological performance. For instance, the development of biocompatible elastomeric organic transistors requires correlation between in vitro biocompatibility assays and in vivo tissue response [7]. These devices must maintain electrical functionality under physiological conditions while minimizing inflammatory responses, necessitating robust testing methodologies that can predict long-term implantation outcomes [7] [17].
Experimental Design for IVIVC Development
Core Methodological Framework
Establishing a valid IVIVC requires a systematic approach encompassing in vitro characterization, in vivo studies, and mathematical modeling. The following workflow outlines the key stages in developing and validating IVIVC for complex delivery systems and biomaterials:
In Vitro Tools for Complex Formulations
The selection of appropriate in vitro methods is critical for establishing meaningful IVIVC. Different formulation categories require specialized characterization approaches:
Table: In Vitro Characterization Methods for Different Formulation Types
| Formulation Category | Primary In Vitro Methods | Key Measured Parameters | Technical Considerations |
|---|---|---|---|
| Lipid-Based Formulations (LBFs) | USP dissolution tests; pH-stat lipolysis assays; combined dissolution-permeation models | Drug release kinetics; extent of lipolysis; precipitation tendency | Must account for digestive processes; media composition critical |
| Self-Nanoemulsifying Systems (SNEDDS) | Dispersion tests; droplet size analysis; dynamic lipolysis models | Emulsification efficiency; nanoemulsion stability; drug distribution | Correlation often fails without digestive components [93] |
| Organic Electronic Implants | Electrical performance under strain; accelerated aging in simulated biofluids; cell viability assays | Conductivity stability; mechanical integrity; cytotoxicity | Requires physiological conditions; mechanical strain cycling [7] |
| Vaginal Delivery Systems | Release testing in simulated vaginal fluid; permeation studies | Daily release rate; polymer swelling; drug permeation | MechVAM PBPK model can support IVIVR [95] |
For lipid-based formulations, traditional dissolution tests often fail to predict in vivo performance due to their inability to simulate lipid digestion processes. The pH-stat lipolysis model provides a more biorelevant approach by simulating intestinal lipolysis, though its predictive value varies. As noted in one review, of eight drugs studied using the pH-stat lipolysis device, only half correlated well with in vivo data [93]. Case studies on fenofibrate formulations demonstrated failures in distinguishing between LBFs administered in fasted versus fed states, highlighting the method's limitations [93].
For organic electronic materials, in vitro testing must evaluate both biological compatibility and electronic functionality. This includes assessing electrical performance under mechanical strain (up to 50% elongation for subcutaneous electronics), measuring stability in physiological solutions, and conducting comprehensive biocompatibility tests using human dermal fibroblasts and macrophages to evaluate cell viability, proliferation, and migration [7].
In Vivo Study Design Considerations
The design of in vivo studies for IVIVC development requires careful consideration of model system relevance and experimental conditions:
Animal Model Selection: The choice of animal model significantly impacts IVIVC translatability. For conventional pharmaceuticals, species with similar gastrointestinal physiology (e.g., dogs for LBFs) are often employed. However, for organic electronic implants, rodent models typically serve initial biocompatibility evaluation, though their relevance for long-term performance assessment may be limited [93] [7].
Study Conditions: Physiological variables such as fed versus fasted state dramatically influence the performance of lipid-based systems. Despite this, many in vitro models fail to account for these differences, leading to poor IVIVC. As evidenced in fenofibrate studies, formulations that showed different performance in fasted versus fed states in vivo could not be distinguished using standard in vitro tests [93].
Endpoint Selection: For drug delivery systems, conventional pharmacokinetic parameters (AUC, Cmax, Tmax) serve as primary endpoints. For bioelectronic implants, additional endpoints including inflammatory response, fibrous capsule formation, and device functionality over time are equally important [7].
Case Studies in IVIVC Development
Lipid-Based Formulations: Successes and Limitations
Lipid-based formulations present particular challenges for IVIVC due to the dynamic processes of digestion, solubilization, and permeation. The Lipid-Based Formulation Classification System (LFCS) categorizes LBFs into four types based on composition, with increasing hydrophilic content from Type I to Type IV [93]. This classification helps rationalize formulation behavior but doesn't guarantee predictable IVIVC.
A comprehensive review of IVIVC for LBFs highlighted several notable failures. Studies on fenofibrate formulations using in vitro dispersion data failed to distinguish between LBFs in fasted versus fed states and showed no correlation with in vivo results in rats [93]. Similarly, research on cinnarizine formulations in dogs achieved only Level D (qualitative) correlation, with observed precipitation during in vitro lipolysis that didn't correspond to differences in in vivo performance [97]. These cases underscore the need for more sophisticated in vitro models that better capture the complexity of in vivo lipid processing.
Organic Bioelectronics: Biocompatibility Correlation
Recent advances in organic bioelectronics demonstrate the adaptation of IVIVC principles to biomaterials. Researchers developing an elastomeric organic field-effect transistor for implantable electronics employed a comprehensive testing strategy [7]. The in vitro assessment included:
- Electrical performance under strain: Evaluating mobility retention under 50% strain and after 1,000 stretching cycles
- Biocompatibility screening: Using human dermal fibroblasts and macrophages to assess cell viability, proliferation, and migration
- Environmental stability: Testing performance in physiological conditions
The in vivo validation involved implantation in mice with evaluation of inflammatory response and tissue damage. The results showed no major inflammatory response or tissue damage, correlating well with the favorable in vitro biocompatibility results [7]. This successful correlation demonstrates that robust IVIVC can be established for bioelectronic materials through appropriate test method selection.
Vaginal Delivery Systems: PBPK-Guided IVIVC
A recent study on progesterone vaginal rings demonstrated an advanced approach to IVIVC through the development of an in vitro-in vivo relationship (IVIVR) supported by PBPK modeling [95] [96]. Researchers used the Mechanistic Vaginal Absorption & Metabolism (MechVAM) model in Simcyp Simulator to simulate plasma concentrations following vaginal administration. The established IVIVR enabled virtual bioequivalence (VBE) assessment, with results comparable to actual bioequivalence clinical trials [96].
This approach allowed the establishment of in vitro release safe space limits (-7.36% to +9.40% mg/day release on specific days), providing a practical tool for post-approval changes without additional clinical studies [95]. This case illustrates how combining in vitro release data with mechanistic modeling can create powerful predictive tools that reduce the need for human trials.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful IVIVC development requires specialized materials and reagents tailored to the formulation type and biological interface. The following table details essential components for IVIVC studies in different research domains:
Table: Essential Research Materials for IVIVC Studies
| Category | Specific Materials/Reagents | Function in IVIVC Development | Application Notes |
|---|---|---|---|
| In Vitro Digestion Models | Pancreatin extract; bile salts; digestion electrolytes | Simulates gastrointestinal lipolysis for LBFs | Critical for predicting performance of lipid-based systems [93] |
| Biocompatible Elastomers | Bromo isobutyl-isoprene rubber (BIIR); Medical-grade PDMS | Provides flexible, biocompatible matrix for bioelectronics | BIIR meets ISO 10993 biocompatibility standards [7] |
| Organic Semiconductors | DPPT-TT; PEDOT:PSS; Polyaniline (PANI) | Creates conductive pathways in flexible bioelectronics | Enable seamless tissue-device integration [7] [17] |
| Dissolution Media | Simulated gastric/intestinal fluids; biorelevant media with lipids | Provides physiologically relevant dissolution environment | Media composition significantly impacts dissolution profile [93] |
| Cell Culture Models | Human dermal fibroblasts; macrophages; Caco-2 cell monolayers | Assesses biocompatibility and permeability | Essential for preliminary safety screening [7] |
| PBPK Modeling Platforms | Simcyp Simulator; GI-Sim; PK-Sim | Supports IVIVR development through mechanistic modeling | Enables virtual bioequivalence assessments [95] |
Advanced Modeling Approaches in IVIVC
Quantitative In Vitro to In Vivo Extrapolation (QIVIVE)
Beyond traditional IVIVC, Quantitative In Vitro to In Vivo Extrapolation (QIVIVE) approaches have emerged to predict in vivo toxicity using in vitro data. This methodology addresses the critical challenge of differing bioavailability between in vitro systems and living organisms [97]. QIVIVE incorporates mass balance models that account for chemical distribution across various compartments, including media constituents, extracellular matrix, test system materials, and cellular components.
Comparative analysis of four major QIVIVE models (Fischer, Armitage, Fisher, and Zaldivar-Comenges) revealed that predictions of media concentrations were more accurate than cellular concentrations, with the Armitage model demonstrating slightly better overall performance [97]. Sensitivity analysis identified chemical property-related parameters as most influential for media predictions, while cell-related parameters were additionally important for cellular predictions.
PBPK Modeling for IVIVC Enhancement
Physiologically Based Pharmacokinetic (PBPK) modeling represents a powerful approach for strengthening IVIVC, particularly for complex delivery routes. The MechVAM model for vaginal drug delivery exemplifies this application, enabling the establishment of IVIVR for progesterone vaginal rings and gels [95]. This methodology successfully supported virtual bioequivalence assessments, with simulation results aligning closely with actual clinical trial outcomes.
The integration of PBPK modeling with IVIVC provides a mechanistic framework to account for physiological variables, potentially reducing the need for extensive clinical testing. For organic electronic implants, similar mechanistic approaches could correlate material properties with tissue response, though such models are still in development.
Establishing robust In Vitro-In Vivo Correlations remains challenging yet achievable through careful experimental design and appropriate method selection. The cases examined demonstrate that while IVIVC success varies across formulation types, systematic approaches incorporating biorelevant in vitro models and mechanistic modeling can significantly enhance predictive capability.
For lipid-based formulations, this means embracing complex digestion models that better simulate intestinal processing. For organic electronic materials, it requires comprehensive testing under physiologically relevant conditions with attention to both biological response and functional performance. Across all domains, the integration of advanced computational approaches like PBPK modeling and QIVIVE strengthens correlation development.
As emerging biomedical technologies continue to evolve, so too must IVIVC methodologies. The continued refinement of these approaches will accelerate the development of safer, more effective therapies and medical devices while reducing reliance on animal testing and costly clinical trials.
In the field of organic electronic materials research, rigorous biocompatibility testing is paramount for the development of safe and effective implantable devices. Evaluating cell-material interactions provides critical data on how biological systems respond to synthetic components. This guide objectively compares the performance of key experimental methods used to assess three fundamental aspects of biocompatibility: cell viability (the proportion of healthy cells), proliferation (the ability of cells to divide and grow), and adhesion (the initial attachment and spreading of cells on a material's surface). Understanding the strengths and limitations of these assays allows researchers to build a robust, multi-faceted framework for validating new organic electronic materials, such as those used in neural interfaces, biosensors, and other implantable technologies.
Comparative Analysis of Key Viability and Proliferation Assays
Selecting the appropriate assay is crucial for generating accurate and meaningful data in biocompatibility testing. The following section compares common techniques based on their underlying principles, providing a clear overview of their specific applications, advantages, and limitations.
Table 1: Comparison of Cell Viability and Cytotoxicity Assays
| Assay Name | Measurement Principle | Applications in Biocompatibility | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Flow Cytometry (FCM) [98] [99] | Multi-parametric staining (e.g., Hoechst, Annexin V, PI) to classify viable, apoptotic, and necrotic cell populations based on membrane integrity and phospholipid distribution. | High-resolution analysis of cell death pathways (apoptosis vs. necrosis) in response to material extracts or direct contact. | High-throughput, quantitative, provides statistical data on heterogenous cell populations, can distinguish early and late apoptosis [98]. | Requires cell suspension, specialized instrumentation, higher cost, complex data analysis [98]. |
| Fluorescence Microscopy (FM) [98] | Fluorescent dyes (e.g., FDA/PI, acridine orange/propidium iodide) visualize live and dead cells attached to a material surface. | Direct imaging of cell attachment and spatial distribution of live/dead cells on material surfaces. | Direct visualization, confirms cell adhesion and morphology, accessible instrumentation [98]. | Lower throughput, potential for sampling bias, semi-quantitative, material autofluorescence can interfere [98] [100]. |
| Lactate Dehydrogenase (LDH) Release [101] | Measures the activity of a cytosolic enzyme released upon cell membrane damage. | Quantifying cytotoxicity and membrane integrity following exposure to material leachables or degradation products. | Simple protocol, colorimetric readout, high-throughput compatible. | Can have high background in untreated samples, may underestimate cytotoxicity in certain co-cultures, measures only membrane damage [101]. |
| MTT Assay [100] | Measures the reduction of a yellow tetrazolium salt to purple formazan by metabolically active cells. | Assessing metabolic activity and proliferation of cells cultured on or with biomaterials. | Widely adopted, colorimetric readout, does not require cell lysis. | Endpoint assay, formazan crystals can be insoluble, results can be influenced by material-cell interactions and environmental conditions [101]. |
| Trypan Blue Exclusion [99] [101] | Dye exclusion by intact membranes of live cells; dead cells with compromised membranes take up the dye. | Quick assessment of overall viability in cell suspensions, often used after cell harvesting from materials. | Rapid, low-cost, simple protocol [99]. | Manual counting is subjective and low-throughput; short incubation time can lead to underestimation of dead cells [101]. |
| Automated Cell Counters (e.g., Vi-Cell BLU, Cellometer) [99] | Image-based or flow-based systems that automate trypan blue or fluorescent dye (AO/PI) analysis. | Rapid, reproducible viability and concentration measurement for cell products and samples from material interactions. | High reproducibility, audit trail, reduced user bias, good for routine testing [99]. | Initial instrument cost, may have issues with cryopreserved samples containing debris [99]. |
Table 2: Comparison of Cell Proliferation and Adhesion Assays
| Assay Name | Measurement Principle | Applications in Biocompatibility | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Molecular Dynamics (MD) Simulation [100] | Computational modeling of atomistic interactions between proteins (e.g., fibronectin, laminin) and material surfaces. | Predicting protein adsorption behavior and cell adhesion potential of new material compositions in silico before fabrication. | Guides optimal material design, reduces experimental trial-and-error, provides nanoscale insights into protein conformation [100]. | Requires computational expertise, results need experimental validation, simplified models may not capture full biological complexity [100]. |
| Cell Adhesion Assays [100] | Qualitative (e.g., SEM imaging) or quantitative assessment of attached cells on a material after a set time. | Directly evaluating the ability of a material surface to support cell attachment, a critical first step for integration. | SEM provides high-resolution detail on cell morphology and spreading. | Quantitative methods can be labor-intensive; results are influenced by surface chemistry, topography, and protein adsorption [100]. |
Experimental Protocols for Assessing Biocompatibility
To ensure reproducibility and reliability, detailed experimental methodologies are essential. Below are protocols for key techniques used in evaluating cell-material interactions for organic electronics.
Flow Cytometry for Multiparametric Viability Analysis
This protocol is adapted from studies on particulate biomaterials and cellular products, providing a robust method to distinguish between viable, apoptotic, and necrotic cell populations after exposure to material extracts [98] [99].
- Cell Seeding and Treatment: Seed osteoblast-like cells (e.g., SAOS-2) or other relevant cell lines in standard culture plates. Once ~70% confluent, treat cells with leachables or degradation products from the test material (e.g., organic semiconductor particles in culture medium at various concentrations) for a predetermined time (e.g., 3h and 72h) [98].
- Cell Harvesting and Staining:
- Gently detach cells using a non-enzymatic cell dissociation buffer to preserve membrane markers.
- Transfer cell suspension to flow cytometry tubes and wash with PBS.
- Resuspend cell pellets in a staining solution containing multiparametric dyes. A common combination includes:
- Hoechst 33342: Stain for all nucleated cells.
- Annexin V-FITC: Binds to phosphatidylserine, exposed on the outer leaflet of the cell membrane during early apoptosis.
- Propidium Iodide (PI): Enters cells with compromised membranes, indicating late apoptosis or necrosis [98].
- Incubate for 15-20 minutes at room temperature in the dark.
- Data Acquisition and Analysis:
- Acquire samples on a flow cytometer equipped with lasers suitable for the fluorophores used (e.g., 405nm, 488nm).
- Use unstained and single-stained controls to calibrate the instrument and set compensation.
- Analyze data using flow cytometry software (e.g., FACSDiva, FlowJo). Gate on the cell population based on forward and side scatter, then classify cells into subpopulations:
Fluorescence Microscopy for Live/Dead Staining
This protocol allows for direct visualization of cell viability and attachment on the material surface itself, which is crucial for assessing the biointerface [98] [100].
- Sample Preparation and Cell Culture:
- Sterilize the test material (e.g., a film of organic semiconductor) and place it in a culture well.
- Seed cells directly onto the material surface at a defined density and culture for the desired period.
- Staining and Imaging:
- Prepare a working solution of fluorescent dyes in culture medium. A standard combination is:
- Calcein-AM (2µM): Metabolized by esterases in live cells, producing green fluorescence.
- Propidium Iodide (PI) (4µM): Labels dead cells with red fluorescence.
- Remove the culture medium from the samples and gently wash with PBS.
- Add the dye solution to cover the material and incubate for 30-45 minutes at 37°C in the dark.
- Carefully remove the dye solution and replace with PBS for imaging.
- Immediately image using a fluorescence microscope with appropriate filter sets. Capture multiple random fields of view for statistical analysis [98].
- Prepare a working solution of fluorescent dyes in culture medium. A standard combination is:
- Image Analysis:
- Use image analysis software (e.g., ImageJ) to count the number of green (live) and red (dead) cells.
- Calculate the percentage of cell viability: (Number of live cells / Total number of cells) × 100.
Molecular Dynamics Simulation for Predicting Cell Adhesion
This computational protocol helps predict the cell adhesion potential of new material compositions by simulating the interaction between the material surface and key extracellular matrix (ECM) proteins [100].
- System Setup:
- Model Construction: Build atomic models of the material surface (e.g., a blend of Bombyx mori silk fibroin and thermoplastic polyurethane) and the ECM protein of interest (e.g., fibronectin or laminin).
- Solvation: Place the constructed protein and surface models in a simulation box and solvate with water molecules.
- Neutralization: Add ions (e.g., Na+, Cl-) to neutralize the system's charge.
- Simulation Execution:
- Energy Minimization: Perform energy minimization to remove steric clashes and unfavorable interactions in the initial system.
- Equilibration: Run simulations in the NVT (constant Number, Volume, Temperature) and NPT (constant Number, Pressure, Temperature) ensembles to equilibrate the system's temperature and density.
- Production Run: Conduct a prolonged molecular dynamics simulation (typically hundreds of nanoseconds) using software like Material Studio. Apply a suitable force field (e.g., Dreiding) to calculate potential energy, including bonded (bond stretching, angle bending) and non-bonded (van der Waals, electrostatic) interactions [100].
- Data Analysis:
- Adhesion Energy: Calculate the adhesion energy between the protein and the material surface. A higher (more negative) adhesion energy indicates stronger binding and potentially better cell adhesion.
- Protein Conformation: Analyze the final conformation of the adsorbed protein. A more spread-out conformation that maintains its structural integrity is typically favorable for cell adhesion [100].
Visualizing Experimental Workflows
The following diagrams illustrate the logical sequence of key experimental and computational processes described in this guide.
Live/Dead Fluorescence Microscopy Workflow
Multiparametric Viability Analysis by Flow Cytometry
Molecular Dynamics Simulation for Adhesion Prediction
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation relies on high-quality, well-characterized reagents and materials. The following table lists key solutions used in the featured methodologies.
Table 3: Key Research Reagent Solutions for Biocompatibility Testing
| Reagent/Material | Function in Experiment | Example Use-Case |
|---|---|---|
| Propidium Iodide (PI) [98] [99] [101] | Nucleic acid stain that penetrates cells with damaged membranes, labeling dead cells. | Used in flow cytometry and fluorescence microscopy as a dead cell marker. |
| Annexin V-FITC [98] | Binds to phosphatidylserine exposed on the outer membrane of cells undergoing apoptosis. | Used in flow cytometry to detect early apoptosis, often in conjunction with PI. |
| Hoechst 33342 [98] | Cell-permeant blue fluorescent dye that binds to DNA in all nucleated cells. | Used in flow cytometry to identify the total cell population and gate out debris. |
| Calcein-AM [98] | Cell-permeant dye converted by intracellular esterases to green fluorescent calcein in live cells. | Used in fluorescence microscopy as a live cell marker, often with PI. |
| Acridine Orange (AO) / Propidium Iodide (PI) [99] | AO stains all nucleated cells (green), while PI stains only dead cells (red). | Used in automated image-based counters (e.g., Cellometer) for viability assessment. |
| 7-Aminoactinomycin D (7-AAD) [99] | DNA intercalator that penetrates dead cells; used as a viability probe in flow cytometry. | An alternative to PI for dead cell discrimination in multicolor flow panels. |
| Trypan Blue [99] [101] | Diazo dye excluded by viable cells; dead cells with compromised membranes are stained blue. | Used for manual or automated viability counting (e.g., Vi-Cell BLU analyzer). |
| MTT Reagent [100] | Yellow tetrazolium salt reduced to purple formazan by metabolically active mitochondria. | Added to cell cultures to assess metabolic activity as a surrogate for viability/proliferation. |
| LDH Assay Kit [101] | Measures lactate dehydrogenase enzyme released from the cytosol upon cell lysis. | Used to quantify cytotoxicity in a colorimetric, high-throughput format. |
| Fibronectin & Laminin [100] | Key extracellular matrix (ECM) proteins that mediate cell adhesion to surfaces. | Used in molecular dynamics simulations to predict the cell adhesion potential of new materials. |
| Bombyx mori Silk Fibroin (SF) [100] | Natural polymer with exceptional biocompatibility, used in hybrid scaffold fabrication. | Blended with synthetic polymers (e.g., TPU) to create biocompatible vascular graft scaffolds. |
| Thermoplastic Polyurethane (TPU) [100] | Synthetic biodegradable polymer with superior mechanical properties and blood compatibility. | Combined with natural polymers to create scaffolds with tailored structural and bioactive properties. |
| DPPT-TT / BIIR Blend [7] | A blend of a semiconducting polymer (DPPT-TT) and a medical-grade elastomer (BIIR). | Forms the core stretchable, biocompatible semiconductor film in implantable organic transistors. |
A comprehensive approach to evaluating cell-material interactions is non-negotiable for advancing the field of biocompatible organic electronics. No single assay can provide a complete picture; instead, a combination of techniques is required. Flow cytometry offers unparalleled quantitative precision in dissecting cell death mechanisms, while fluorescence microscopy provides essential spatial context of cells on the material surface. Molecular dynamics simulations represent a powerful tool for in silico prediction of cell adhesion, guiding material design before costly and time-consuming experimental trials. By carefully selecting and integrating these methods—from computational prediction to high-resolution cytometric analysis—researchers can robustly validate the safety and functionality of next-generation organic electronic materials, ensuring their successful translation from the laboratory to clinical applications.
The successful long-term integration of implantable electronic devices with biological tissues is a paramount challenge in advancing modern healthcare technologies such as continuous physiological monitors, neural interfaces, and smart drug delivery systems. For researchers and drug development professionals, the core obstacle remains the foreign body reaction—a complex immune response to implanted materials that often culminates in fibrous capsule formation, isolating the device and compromising its functionality [72] [102]. This cascade begins with protein adsorption onto the implant surface, followed by infiltration of inflammatory cells (neutrophils, monocytes, macrophages), and can result in a collagen-rich fibrous capsule that physically separates the implant from the native tissue [102]. Within the specific context of organic electronic materials research, the imperative extends beyond mere biological inertness. The ideal implant must achieve seamless biointegration while maintaining stable electrical performance over time, a dual requirement that demands careful material selection and innovative interface engineering [88] [7].
This guide provides a comparative analysis of recent strategic approaches evaluated through long-term in vivo implantation studies, with a specific focus on quantitative metrics of inflammation and tissue integration. We objectively evaluate emerging data on adhesive interfaces, surface-modified biomaterials, and a new class of intrinsically soft, biocompatible organic electronic devices, providing researchers with a structured framework for assessing next-generation implantable technologies.
Comparative Analysis of Implant Integration Strategies
The following section compares three distinct strategic approaches for enhancing the biocompatibility and long-term performance of implantable devices, summarizing key experimental findings and quantitative outcomes.
Table 1: Comparison of Strategic Approaches for Long-Term Implant Integration
| Strategy | Core Mechanism | Key Materials | Experimental Model | Study Duration | Key Efficacy Findings |
|---|---|---|---|---|---|
| Adhesive Biointerfaces [72] | Conformal mechanical integration prevents inflammatory cell infiltration. | Poly(acrylic acid) N-hydroxysuccinimide ester & Poly(vinyl alcohol) | Rats, Mice, Humanized Mice, Pigs | 12 weeks | No observable fibrous capsule on abdominal wall, colon, stomach, lung, heart. |
| Surface Modification [103] | Plasma treatment enhances surface properties to improve tissue integration. | Vacuum Plasma-treated Silicone & Human Acellular Dermal Matrix (hADM) | In vivo rat model | 8 weeks | Significant reduction in capsule thickness; enhanced fibroblast infiltration and neovascularization. |
| Intrinsically Soft Electronics [7] | Mechanical modulus matching to soft biological tissues. | DPPT-TT semiconducting polymer & Bromo Isobutyl–Isoprene Rubber (BIIR) elastomer | In vivo mice model | 2 weeks | No major inflammatory response or tissue damage; stable electrical performance under strain. |
Table 2: Quantitative Histological and Immunological Outcomes
| Assessment Method | Adhesive Interface [72] | Plasma-Treated hADM [103] | Elastomeric Transistor [7] |
|---|---|---|---|
| Capsule Thickness | Collagen layer thickness comparable to native mesothelium over 12 weeks. | 45.0 ± 4.5 μm (Untreated) vs. 30.3 ± 7.4 μm (Treated) at 8 weeks. | Not explicitly measured, but study reported "no major inflammatory response". |
| Immune Cell Infiltration | Significantly fewer fibroblasts, neutrophils, macrophages, T cells at all time points (3, 7, 14 days). | No significant difference in acute macrophage (CD68) infiltration at 1 week. | In vitro: No adverse effects on fibroblast and macrophage viability, proliferation, or migration. |
| Tissue Integration Markers | Not Applicable | ↑ Cellular infiltration (9.9% to 30.0%); ↑ Neocollagenesis; ↑ Neovascularization (7.1 to 25.2 vessels/mm²). | Stable operation in logic circuits under physiological conditions. |
| Key Analytical Techniques | Histology, Immunofluorescence, qPCR, RNA-seq, Luminex assays. | Histology, Immunohistochemistry (CD68, CD31), Herovici staining. | Electrical performance testing under strain, in vitro co-culture with cells, in vivo implantation. |
Detailed Experimental Protocols for Key Studies
Protocol: Evaluating Adhesive Anti-Fibrotic Interfaces
1. Implant Preparation:
- Adhesive Implants: Composed of a polyurethane mock device and an adhesive layer of crosslinked poly(acrylic acid) N-hydroxysuccinimide ester and poly(vinyl alcohol) [72].
- Non-Adhesive Controls: Identical in chemical composition but rendered non-adhesive by pre-swelling in phosphate-buffered saline (PBS) before implantation. These controls were sutured onto organ surfaces [72].
2. Surgical Implantation:
- Animal Models: Rats, mice, humanized mice, and pigs.
- Procedure: Both adhesive and non-adhesive implants were implanted on the surfaces of multiple organs, including the abdominal wall, colon, stomach, lung, and heart. The adhesive implants formed a conformal integration without sutures, while non-adhesive controls were sutured [72].
- Duration: Studies were conducted for up to 84 days (12 weeks) [72].
3. Post-Explanation Analysis:
- Histological Analysis: Explanted tissues were processed and stained for blinded evaluation by a pathologist to assess fibrous capsule formation and tissue integration [72].
- Immunofluorescence Staining: Performed on days 3, 7, and 14 post-implantation for specific cell types: αSMA (fibroblasts), neutrophil elastase (neutrophils), CD68 (pan-macrophages), iNOS/vimentin (pro-inflammatory macrophages), CD206 (anti-inflammatory macrophages), and CD3 (T cells). Cell numbers in the implant–tissue interface were quantified over a 500 µm width [72].
- Molecular Analysis: Quantitative PCR (qPCR) and RNA-sequencing were used to profile immune-cell-related gene expression. Cytokine levels were quantified using multiplex Luminex assays [72].
Diagram 1: Adhesive interface evaluation workflow.
Protocol: Assessing Plasma-Surface Modified Implants
1. Implant Preparation and Treatment:
- Materials: Silicone implants and Human Acellular Dermal Matrix (hADM).
- Surface Modification: Implants were treated with vacuum plasma. Untreated implants served as controls [103].
2. Surgical Implantation and Analysis:
- Animal Model: In vivo rat model.
- Procedure: Plasma-treated and untreated implants were inserted subcutaneously into the dorsal skin of rats [103].
- Duration: Tissue samples were collected at 1, 4, and 8 weeks post-implantation [103].
3. Histological and Immunohistochemical Evaluation:
- Capsule Thickness Measurement: The fibrous capsule surrounding the explanted implants was measured to assess the chronic inflammatory response [103].
- Cellular Infiltration and Neocollagenesis: Cellular infiltration within hADM implants was quantified. Herovici staining was used to detect and quantify newly synthesized collagen (neocollagenesis) [103].
- Neovascularization Assessment: Immunohistochemical staining with CD31 antibody (a marker for endothelial cells) was performed. Blood vessel density was quantified both within the hADM and in the surrounding tissue [103].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Biocompatibility Testing
| Item / Reagent | Function / Application | Specific Examples from Research |
|---|---|---|
| Adhesive Hydrogel | Creates conformal, anti-fibrotic implant-tissue interface. | Crosslinked poly(acrylic acid) N-hydroxysuccinimide ester and poly(vinyl alcohol) [72]. |
| Biocompatible Elastomer | Matrix for soft electronics; provides mechanical compliance. | Bromo Isobutyl–Isoprene Rubber (BIIR), a medical-grade elastomer [7]. |
| Organic Semiconductor | Enables electronic functionality in soft, stretchable devices. | DPPT-TT polymer, forming a nanofibre network within an elastomer [7]. |
| Histological Stains | Visualizes tissue structure, collagen, and cellular components. | Herovici staining for differentiating new vs. mature collagen [103]. |
| Immunostaining Markers | Identifies and quantifies specific immune and tissue cells. | CD68 (macrophages), CD31 (endothelial cells, angiogenesis), αSMA (fibroblasts) [72] [103]. |
| Molecular Biology Kits | Profiles gene expression and cytokine levels in tissue. | qPCR for immune genes (e.g., Nos2); Multiplex Luminex assays for cytokines (e.g., G-CSF, IL-12p70) [72]. |
Analysis of Integration Pathways and Immune Modulation
The comparative data reveals distinct biological pathways through which different strategies mediate tissue integration. The adhesive interface functions primarily as a physical barrier to cell infiltration, effectively preventing the initial stages of the foreign body reaction. This is evidenced by significantly reduced levels of protein adsorption and subsequent decreased infiltration of neutrophils, monocytes, macrophages, and T cells at the adhesive implant–tissue interface compared to non-adhesive controls [72]. Notably, while the acute inflammatory phase on day 3 showed a higher level of Nos2 expression (associated with iNOS+ neutrophils) in the adhesive group, this response shifted dramatically by day 7, with the adhesive interface exhibiting significantly lower expression of all profiled immune-cell-related genes compared to controls [72]. This suggests the strategy does not abolish inflammation but rather modulates its trajectory to a more favorable, resolved state.
In contrast, plasma treatment and intrinsically soft materials employ bioactive and biopassive modulation, respectively. Plasma treatment alters the surface energy and chemistry of existing biomaterials like silicone and hADM, making them more conducive to tissue acceptance. This results in a significantly enhanced pro-regenerative response, characterized by increased fibroblast infiltration, neocollagenesis, and neovascularization, without aggressively stimulating the immune system [103]. The elastomeric transistor exemplifies a biomimetic approach, where the material's properties (Young's modulus) are engineered to match those of human tissue. This mechanical compatibility minimizes the initial irritant signal that triggers the foreign body reaction, thereby avoiding a major inflammatory cascade and tissue damage from the outset [7].
Diagram 2: Strategy mechanisms and biological outcomes.
The direct comparison of quantitative long-term data confirms that the strategic design of the implant-tissue interface is a critical determinant of biocompatibility success. While surface modification of conventional materials like silicone and hADM can significantly improve their integration profile, the emerging paradigms of adhesive biointerfaces and intrinsically soft, biocompatible electronics represent a fundamental shift toward more integrated and functional long-term implants.
For researchers in organic electronic materials, the path forward is multifaceted. It requires the continued synthesis of novel semiconductors certified for biocompatibility, the development of standardized long-term in vivo testing protocols that simultaneously monitor electrical and biological performance, and a deeper investigation into the specific immune signaling pathways modulated by these new materials. The ultimate goal is a generation of "bio-invisible" electronic implants that the body not only tolerates but seamlessly accepts, enabling reliable, lifelong diagnostic and therapeutic functions.
The development of bioelectronic devices, which form an interface between electronic systems and biological tissues, represents a frontier in medical and materials science. The core challenge in this field lies in bridging the fundamental gap between the rigid, electronic world of conventional semiconductors and the soft, ionic environment of biological systems. This article provides a comparative analysis of organic and traditional inorganic semiconductor interfaces, framed within the context of biocompatibility testing for organic electronic materials research. As bioelectronic applications expand to include neural implants, wearable sensors, and retinal prostheses, the biocompatibility of the interfacing materials becomes paramount. We examine the fundamental properties, performance characteristics, and biological responses to both material classes, supported by experimental data and standardized testing methodologies relevant to researchers and drug development professionals.
Fundamental Properties and Comparative Analysis
The intrinsic properties of organic and inorganic semiconductors stem from their distinct chemical structures and material compositions, which in turn dictate their performance in biointerfacing applications. Table 1 summarizes the key characteristics of both material classes.
Table 1: Fundamental Properties of Organic and Inorganic Semiconductors for Biointerfaces
| Property | Organic Semiconductors | Traditional Inorganic Semiconductors |
|---|---|---|
| Composition | Carbon-based molecules/polymers (e.g., PEDOT, DPPT-TT) [2] [7] | Inorganic crystals (e.g., Silicon, Gallium Arsenide) [104] [2] |
| Physical State | Soft solids [2] | Hard solids [2] |
| Young's Modulus | 20 kPa - 3 GPa (as solids); 20 kPa - 2 MPa (as gels) [2] | ~100 GPa [2] |
| Charge Carriers | Electrons, holes, and ions [2] | Electrons and holes [2] |
| Mechanical Mismatch with Tissue | Low (Similar modulus to soft tissue) [2] [7] | High [2] [7] |
| Typical Fabrication | Solution-based processing, printing [104] [12] | High-temperature, high-vacuum processes [104] [105] |
| Surface Structure | Tunable, from flat to "fuzzy" [2] | Nearly flat [2] |
The mechanical compatibility of a biointerface is critically determined by its Young's modulus, a measure of stiffness. Organic semiconductors, with a Young's modulus range that overlaps with that of living tissue (cortex ~10 kPa), significantly reduce the mechanical mismatch compared to rigid inorganic semiconductors [2]. This reduced mismatch minimizes strain-induced tissue damage, chronic inflammation, and fibrous encapsulation, which are common failure modes for rigid implants [7]. Furthermore, the ability of organic semiconductors to facilitate mixed ionic and electronic conduction enables efficient signal transduction across the biotic-abiotic divide, a feat challenging for conventional inorganics whose operation is primarily based on electronic carriers only [2].
Performance in Bioelectronic Applications
When deployed in physiological environments, the two classes of semiconductors exhibit markedly different performance and stability profiles. Table 2 compares their key performance metrics relevant to biointerfacing.
Table 2: Performance and Biocompatibility Comparison at the Biointerface
| Aspect | Organic Semiconductors | Traditional Inorganic Semiconductors |
|---|---|---|
| Biocompatibility | High (e.g., no adverse effects on cell viability/proliferation) [7] [106] | Variable; many materials are not biocompatible [2] |
| Long-term Tissue Response | Reduced inflammation and fibrous encapsulation; stable interface for over 7 months demonstrated in vivo [2] [7] | Chronic foreign body response, leading to fibrous encapsulation and interface failure [2] |
| Stability in Physiological Conditions | Stable operation in logic circuits under physiological conditions demonstrated [7] | High intrinsic stability, but biofluid corrosion can degrade metal contacts [7] |
| Charge Injection Efficiency | High, due to mixed ion/electron transport and large effective surface area [2] | Lower, requires high voltages for effective neural stimulation [2] |
| Primary Failure Mode | Potential degradation of electronic performance over long periods [88] | Fibrous tissue encapsulation severing the interface with target cells [2] |
A critical advantage of organic semiconductors is their ability to form a stable, intimate interface with neural tissue. For instance, an organic semiconductor-based nerve interface using PEDOT demonstrated functional stability for over 7 months in vivo [2]. In contrast, interfaces based on silicon, a staple of inorganic electronics, elicit a chronic tissue response that leads to fibrous encapsulation, progressively increasing impedance and ultimately isolating the electronic device from the target tissue [2]. Recent advancements in material design have yielded elastomeric organic transistors that show no adverse effects on cell viability, proliferation, or migration in vitro, and no major inflammatory response or tissue damage after in vivo implantation [7].
Experimental Protocols for Biocompatibility Assessment
The evaluation of material biocompatibility follows internationally recognized standards, primarily the ISO 10993 series, which outlines a battery of tests based on the type and duration of body contact [2]. The following protocols are fundamental to assessing the biocompatibility of semiconductor materials for bioelectronic applications.
In Vitro Cytotoxicity Assays
In vitro tests provide an initial, cost-effective screening of new materials or devices before progressing to complex in vivo studies [2].
- Objective: To determine if a biomaterial contains harmful extractables that cause death or damage to isolated cells.
- Method Selection: The Direct Contact Assay is often the most appropriate for organic semiconductors, as it avoids potential compromises to device functionality that can occur with agar diffusion, and is not limited by the maintenance of cell culture conditions as in extract dilution studies [2].
- Procedure:
- The test material is placed directly in contact with a monolayer of either primary cells or immortalized cell lines.
- The co-culture is incubated for a defined period, typically up to 10 days for "acute" testing.
- Cell damage is assessed using quantitative endpoints.
- Key Endpoint Assays:
- MTT Assay: Measures mitochondrial dehydrogenase activity as an indicator of cell metabolism and viability.
- XTT Assay: A tetrazolium dye-based test for cell proliferation.
- Neural Red Uptake Cytotoxic Assay: Evaluates the ability of cells to incorporate and bind the supravital dye neutral red, a marker of lysosomal integrity and overall health.
- Colony Formation Assay: Assesses long-term cell damage by measuring the ability of a single cell to grow into a colony.
- Outcome Interpretation: Comparable cell viability between cultures established on the test material and a standard control (e.g., glass) is a standard indicator of biocompatibility [106].
Morphological Biocompatibility Analysis
Beyond simple viability, the functional integration of a material with neural tissue requires intimate cell adhesion and neurite outgrowth.
- Objective: To analyze the morphological compatibility of cells, specifically neuronal cells, cultured on the test material.
- Procedure:
- Human retinal cell cultures (or other relevant primary neuronal cells) are established on the organic semiconductor substrate and a control surface [106].
- Cells are immunostained with specific markers for neuronal cells (e.g., retinal ganglion cells) and their neurites.
- High-resolution imaging (e.g., confocal microscopy) is performed over time.
- Neurite Elongation: The length of neurite outgrowths is quantified and compared between the test material and control.
- Significance: Differences in morphological compatibility, even when cell viability is comparable, have critical implications for the quality of the neural interface and must be assessed separately [106].
In Vivo Implantation Studies
In vivo testing is essential for evaluating the long-term ("chronic") tissue response to an implant under realistic physiological conditions.
- Objective: To assess the chronic tissue response, inflammatory reaction, and functional stability of the bioelectronic interface.
- Procedure:
- The bioelectronic device is implanted into an appropriate animal model (e.g., mice, rats).
- The implantation site is monitored over weeks, months, or even years.
- Histological Analysis: After sacrifice, the tissue surrounding the implant is harvested, sectioned, and stained to evaluate:
- Inflammation: Presence and density of immune cells.
- Tissue Damage: Signs of necrosis or micro-injury.
- Fibrous Encapsulation: Thickness of fibrous tissue layers formed around the implant.
- Functional Stability: The electrical performance of the device (e.g., impedance, signal-to-noise ratio) is tracked throughout the implantation period [2] [7].
- Outcome Interpretation: A successful implant shows no major inflammatory response or tissue damage and maintains stable electrical performance over the intended duration [7].
The following workflow diagram illustrates the progression of key experiments in a comprehensive biocompatibility assessment:
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and testing of organic semiconductor biointerfaces rely on a specific set of materials and reagents. Table 3 details key components used in the featured research.
Table 3: Key Research Reagents and Materials for Organic Bioelectronics
| Reagent/Material | Function/Description | Example Use Case |
|---|---|---|
| PEDOT (Poly(3,4-ethylenedioxythiophene)) | A conducting polymer renowned for its high stability and excellent mixed conduction properties [2]. | Neural interface coatings to improve charge injection and stability [2]. |
| DPPT-TT | A high-performance donor-acceptor semiconducting polymer used as the active component in transistors [7]. | Semiconducting nanofibers in elastomeric organic field-effect transistors (sOFETs) [7]. |
| BIIR (Bromo Isobutyl–Isoprene Rubber) | A medical-grade elastomer that serves as a biocompatible and stretchable matrix [7]. | Blended with DPPT-TT to create intrinsically stretchable and biocompatible semiconductor films [7]. |
| Primary Human Retinal Cells | Cell cultures derived directly from human tissue, providing a physiologically relevant model for biocompatibility testing [106]. | Assessing morphological biocompatibility and cell viability for artificial retina applications [106]. |
| Vulcanization Additives (Sulfur, DPTT, Stearic Acid) | A chemical cocktail used to crosslink (vulcanize) elastomers, enhancing their mechanical properties and stability [7]. | Crosslinking BIIR in blend films to improve elasticity and durability without disrupting the semiconductor [7]. |
| Dual-layer Ag/Au Metallization | A strategy to create robust, stretchable, and biofluid-corrosion-resistant electrodes [7]. | Ag provides excellent electrical contact, while Au offers protection against corrosion in physiological environments [7]. |
| Twisted π-Conjugated Molecules | A new class of 3D-shaped organic semiconductors designed for multi-directional charge transport [107]. | Exploring novel semiconductor architectures to overcome limitations of planar molecular orientation control [107]. |
The comparative analysis reveals that organic and inorganic semiconductors offer complementary strengths for biointerfacing applications. Inorganic semiconductors, with their superior charge carrier mobility and established manufacturing, remain indispensable for high-performance computing. However, for applications requiring direct, stable integration with biological tissue, organic semiconductors present a compelling advantage. Their inherent softness, mechanical compatibility, mixed ionic-electronic conduction, and demonstrated biocompatibility enable the formation of intimate neural interfaces that minimize chronic immune responses. While challenges in long-term operational stability and manufacturing scalability persist, ongoing research in material design, such as 3D-shaped molecules and vulcanized biocompatible blends, is steadily addressing these limitations. The future of bioelectronics will likely see an increased reliance on organic semiconductors, particularly for a new generation of implantable and wearable devices that seamlessly merge with the human body.
The successful translation of bioelectronic interfaces from laboratory research to clinical practice hinges on rigorous real-world validation. These devices, which form critical bridges between biological tissue and electronic systems, must demonstrate not only high performance but also long-term stability and biocompatibility in living environments. This guide objectively compares the validation methodologies and performance outcomes for three principal categories of bioelectronic interfaces: neural, cardiac, and skin. A fundamental challenge across all these domains is the mechanical and biological mismatch between conventional electronic materials and dynamic biological tissues. Organic electronic materials have emerged as promising candidates to address these limitations due to their softness, flexibility, and mixed ionic-electronic conduction properties, which more closely mimic biological systems [2]. This review synthesizes experimental data and validation protocols from recent clinical and pre-clinical studies to provide researchers and product developers with a comparative framework for assessing interface technologies within the critical context of biocompatibility.
Neural Interfaces
Performance Comparison of Neural Interface Technologies
Table 1: Performance Metrics for Implantable Neural Interfaces
| Interface Type | Primary Materials | Key Performance Metrics | Recorded Signal Quality | Chronic Stability & Biocompatibility |
|---|---|---|---|---|
| Michigan-style Si Probes | Silicon, Platinum | High spatial resolution (~15-40 µm), Multi-electrode arrays | Single-unit recordings in animal models | Significant foreign body response, glial scarring [108] |
| Utah Electrode Arrays | Silicon, Iridium oxide | High electrode density (100+ channels) | Local field potentials, multi-unit activity | Fibrous encapsulation, chronic inflammation [108] |
| Organic Polymer-Based Electrodes | PEDOT, CNTs, Graphene | Lower impedance, improved charge injection capacity | Enhanced signal-to-noise ratio in chronic settings | Reduced inflammation, stable for up to 7 months in vivo [2] [108] |
| Carbon Fiber Electrodes | Carbon fibers | Ultra-small diameter (7 µm), high-density arrays | Single-unit recordings with high spatial resolution | Flexible, reduced mechanical mismatch [108] |
Experimental Protocols for Neural Interface Validation
The validation of neural interfaces employs a multi-stage methodology:
- In Vitro Biocompatibility Screening: Initial assessment using primary neuronal cultures or cell lines (e.g., PC12 cells). Cytotoxicity is evaluated via ISO 10993-5 compliant assays (e.g., MTT, XTT, neutral red uptake) over acute periods (typically up to 10 days) [2].
- Electrical Functionality Testing: Characterization of electrode impedance, charge storage capacity, and charge injection limits in simulated physiological solutions (e.g., phosphate-buffered saline) at 37°C [2] [108].
- In Vivo Implantation and Recording: Surgical implantation of electrodes into target brain regions (e.g., motor cortex) of animal models (e.g., rodents, non-human primates). Neural signals (single-unit, multi-unit, local field potentials) are recorded during specific tasks or at rest. Signal-to-noise ratio (SNR), single-unit yield, and amplitude are quantified [108].
- Histological Analysis for Biocompatibility: Post-sacrifice, brain tissue is sectioned and stained for markers of neuronal nuclei (NeuN), astrocytes (GFAP), and microglia (Iba1). The thickness of the glial scar and neuronal density around the implant site are measured and quantified to assess the foreign body response [108].
Signaling Pathways in Foreign Body Response
The following diagram illustrates the key biological pathways activated upon implantation of a neural interface.
Cardiac Interfaces
Performance Comparison of Cardiac Monitoring Technologies
Table 2: Real-World Performance of Cardiac Monitoring Algorithms
| Device / Algorithm | Clinical Use Case | Study Design | Sensitivity (%) | Specificity / Accuracy | Key Performance Findings |
|---|---|---|---|---|---|
| ILR-ECG Analyzer (AI) | Arrhythmia Detection (ICM) | Retrospective analysis of 879 episodes [109] | 98.6 | Specificity: 76.0% (FP reduction) | Reclassified 76% of false positives as normal [109] |
| WHRM Algorithm (PPG) | Heart Rate Monitoring | Prospective, 25 subjects, 82 sequences [110] | N/A | Overall Accuracy: 92.0% (±5 BPM) | MAE: 2.01 BPM; Most challenging during walking/cycling [110] |
| AI in Cardiology (Review) | Various (Imaging, EF, Arrhythmia) | Systematic review, 64 studies [111] | Variable by task | 68.75% showed clinical improvement | 92.2% of studies published after 2020; 11 RCTs identified [111] |
Experimental Protocols for Cardiac Algorithm Validation
Robust validation of cardiac monitoring technologies follows structured protocols:
- Data Collection Protocol: For wearable heart rate monitors, data is collected using a defined activity protocol (e.g., "Maxim sports protocol") that includes resting (lying, sitting), walking, running, and cycling activities. Data is synchronously recorded from the test device (e.g., PPG sensor) and a certified reference device (e.g., ECG chest strap) [110].
- Algorithm Training: For AI-based tools like the ILR-ECG Analyzer, a development dataset of thousands of ICM episodes, diagnosed by a panel of expert cardiac electrophysiologists, is used to train and validate the algorithm. This often involves a combination of expert-defined features (morphological and frequential analyses of QRS and P waves) and a 1D Convolutional Neural Network (CNN) [109].
- Performance Metrics Calculation:
- Sensitivity and Specificity: For arrhythmia detection, calculated by comparing AI classifications to an adjudication committee's review of episodes [109].
- Mean Absolute Error (MAE) and Error-Band Accuracy: For heart rate monitoring, the absolute difference between the algorithm output and the reference device is calculated per second. The percentage of data points within a ±5 BPM error band is reported [110].
- Real-World/Clinical Validation: The final step involves testing the algorithm on entirely separate, real-world datasets collected from daily life activities to assess performance in the presence of non-periodic and irregular motion [110].
Skin Interfaces
Performance Comparison of Skin-Interfaced Sensors
Table 3: Material Properties and Performance of Skin-Interfaced Sensors
| Sensor Type | Core Materials | Target Analytes / Signals | Key Characteristics | Experimental Performance Data |
|---|---|---|---|---|
| Optical PPG Sensors | Organic PDs (NFA), Perovskite PDs, AuNWs, Graphene | Heart rate, Pulse Oximetry (SpO2) | Flexibility, Stretchability, Transparency | Organic NIR PDs: Responsivity >0.5 A/W [112]; Perovskite PDs: Functionality at 60° bending [112] |
| Physical Motion Sensors | CNTs, Ag-Au Core-Sheath NWs, Liquid Metals | Kinematics, Muscle activity, Pulse Wave Velocity (PWV) | High conductivity, Strain-insensitivity | CNT-silk E-tattoo: Stable for electrophysiological sensing [113] |
| Biochemical Sensors | MOFs, rGO, Functionalized Polymers | Metabolites (Glucose, Lactate), Electrolytes in sweat | Selective biomarker recognition, Microporosity | BP@LEG composite: High strain sensitivity, durability over 18,400 cycles [113] |
Experimental Protocols for Skin Sensor Validation
Validation of skin-interfaced electronics focuses on electrical, mechanical, and biosensing performance:
- Electrical and Mechanical Characterization:
- Responsivity and Detectivity: For photodetectors, measured under calibrated light sources at specific wavelengths (e.g., NIR) [112].
- Sheet Resistance and Conductivity: Measured using a four-point probe on flexible substrates. Changes are monitored under mechanical strain (e.g., using a tensile stage) [113].
- Cyclic Strain Testing: Devices are subjected to repeated stretching cycles (e.g., thousands of cycles) to assess electrical and mechanical durability [113].
- On-Body Signal Fidelity Testing: Sensors are applied to human subjects (e.g., wrist, chest). The quality of the recorded signal (e.g., PPG, ECG) is compared against a clinical-grade reference device. Parameters like Signal-to-Noise Ratio (SNR) and correlation coefficient are calculated [112] [110].
- Skin Conformability and Biocompatibility Assessment:
- Adhesion Strength: Measured via peel-off tests on human skin or skin models [114].
- Breathability: Evaluated by measuring moisture vapor transmission rate [114].
- Skin Irritation: Patches are worn by human volunteers for extended periods (e.g., 24-48 hours), and the skin site is graded for redness and irritation using established scales [114].
Experimental Workflow for Skin Sensor Validation
The following diagram outlines the standard workflow for developing and validating a skin-interfaced sensor.
The Scientist's Toolkit: Research Reagents & Materials
Table 4: Essential Materials for Bioelectronic Interface Research
| Category | Specific Material / Reagent | Critical Function in R&D | Key Considerations |
|---|---|---|---|
| Conductive Materials | PEDOT:PSS [2] [113] | Stable, biocompatible conducting polymer for electrodes and traces | Mixed ionic-electronic conductor; requires biocompatibility testing per ISO 10993 [2] |
| Gold Nanowires (AuNWs) [113] | High-conductivity, biocompatible material for flexible electrodes | Superior stability vs. AgNWs/CuNWs; high cost [113] | |
| Carbon Nanotubes (CNTs) [113] | Conductive filler for composites; high mechanical robustness | Excellent electrical/thermal conductivity; used in E-tattoos [113] | |
| 2D Materials | Graphene & rGO [113] | Ultrasensitive, transparent, and flexible sensing element | High carrier mobility; used in strain and biochemical sensors [113] |
| MXene [113] | Highly conductive 2D material for rapid electron transfer | Tunable surface chemistry; good for electrochemical sensing [113] | |
| Flexible Substrates/Encapsulants | Polydimethylsiloxane (PDMS) [113] [114] | Encapsulation and stretchable substrate | Tunable modulus, good optical clarity; can limit breathability [114] |
| Polystyrene-block-poly(ethylene-ran-butylene)-block-polystyrene (SEBS) [113] | Polymer matrix for stretchable conductive composites | Excellent elasticity and environmental stability [113] | |
| Biocompatibility Assays | ISO 10993-5 [2] [115] | International standard for biological safety evaluation | Defines tests for cytotoxicity, sensitization, and irritation [2] [115] |
| MTT/XTT Assay [2] | Colorimetric assay for cell viability and cytotoxicity | Measures mitochondrial dehydrogenase activity [2] | |
| Cell Lines/Tissues | Reconstructed Human Epidermis (RhE) [115] | In vitro model for skin irritation testing | FDA-recognized alternative to animal testing for skin irritation [115] |
Conclusion
The successful integration of organic electronic materials into medical devices hinges on a rigorous, multi-stage biocompatibility assessment that spans from foundational material properties to in vivo validation. The unique advantages of organic materials—including their mechanical compliance and mixed conduction—offer unparalleled opportunities for seamless biointegration, as evidenced by recent breakthroughs in stretchable transistors and imperceptible electronic fibers. However, navigating the foreign body response and ensuring long-term stability remain critical challenges. The future of the field points toward increasingly sophisticated testing paradigms, including AI-driven predictive modeling, personalized biocompatibility assessments based on patient-specific data, and a stronger emphasis on sustainable material life cycles. By adhering to a comprehensive testing framework and leveraging emerging technologies, researchers can accelerate the development of safer, more effective bioelectronic therapies that truly harmonize with the human body.
References
- 1. ISO 10993 [https://en.wikipedia.org/wiki/ISO_10993]
- 2. Organic Bioelectronics: Materials and Biocompatibility - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6121695/]
- 3. ISO 10993-1:2018 - Biological evaluation of medical devices [https://www.iso.org/standard/68936.html]
- 4. Basics of Biocompatibility: Information Needed for ... [https://www.fda.gov/medical-devices/biocompatibility-assessment-resource-center/basics-biocompatibility-information-needed-assessment-fda]
- 5. Navigating Biocompatibility: An Introduction to ISO 10993 ... [https://medinstitute.com/blog/navigating-biocompatibility-an-introduction-to-iso-10993-series-of-standards/]
- 6. The “Big Three” in biocompatibility testing of medical devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800850/]
- 7. A biocompatible elastomeric organic transistor for ... [https://www.nature.com/articles/s41928-025-01444-9]
- 8. Organic Electronics in Biosensing: A Promising Frontier for ... [https://www.mdpi.com/2079-6374/13/11/976]
- 9. Conjugated Polymers in Bioelectronics [https://pubmed.ncbi.nlm.nih.gov/29874033/]
- 10. Organic Electronics in Biosensing: A Promising Frontier for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10669243/]
- 11. Organic electronics: pioneering the future of sustainable and ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra04656d?page=search]
- 12. Organic Electronics in 2025: Innovations That Will Change ... [https://www.signalintegrityjournal.com/articles/3907-organic-electronics-in-2025-innovations-that-will-change-your-life]
- 13. North American Biocompatibility Summit [https://nabiocompsummit.com/]
- 14. Navigating the FDA's New Draft Guidance on Chemical ... [https://www.intertek.com/blog/2025/01-24-new-draft-guidance-on-chemical-analysis-for-medical-devices/]
- 15. 3D printable and biocompatible PEDOT:PSS-ionic liquid ... [https://www.nature.com/articles/s41467-024-50264-6]
- 16. PEDOT:PSS-based bioelectronics for brain monitoring and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075682/]
- 17. Organic Bioelectronics: Diversity of Electronics Along with ... [https://www.mdpi.com/2079-6374/15/9/587]
- 18. Biocompatible dipeptide coated on Pt/PEDOT:PSS ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400524016216]
- 19. In vivo biocompatibility assessment of 3D printed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11541680/]
- 20. Engineering biocompatibility and mechanical performance ... [https://www.sciencedirect.com/science/article/abs/pii/S1526612525009454]
- 21. Biocompatibility assessment of biomaterials used in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8461597/]
- 22. A Comparison of the Mechanical Properties of ECM ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12023840/]
- 23. Achieving tissue-level softness on stretchable electronics ... [https://www.nature.com/articles/s41467-023-40191-3]
- 24. Organic Bioelectronics: Diversity of Electronics Along with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467551/]
- 25. Electronic and protonic transport in bio-sourced materials [https://pubs.rsc.org/en/content/articlehtml/2021/ma/d0ma00579g]
- 26. Dissipative charge transport in organic mixed ionic- ... [https://www.nature.com/articles/s41467-025-57528-9]
- 27. A Comparison of Charge Carrier Dynamics in Organic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11469080/]
- 28. Materials Characterization as an Integral Part of Global ... [https://www.mddionline.com/materials/materials-characterization-as-an-integral-part-of-global-biocompatibility]
- 29. Review on Charge Carrier Transport in Inorganic and ... [https://www.mdpi.com/2079-6412/13/9/1657]
- 30. Mixed Ionic and Electronic Charge Transport in Conductive ... [https://pubmed.ncbi.nlm.nih.gov/40913445/]
- 31. Use of International Standard ISO 10993-1, "Biological ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/use-international-standard-iso-10993-1-biological-evaluation-medical-devices-part-1-evaluation-and]
- 32. ISO 10993-1:2025 Updates —Top 10 Biological Evaluation ... [https://namsa.com/resources/blog/iso-10993-12025top-10-biological-evaluation-essentials-in-the-update/]
- 33. Navigating revision to ISO 10993-1: Biological evaluation ... [https://www.labcorp.com/education-events/articles/navigating-revision-iso-10993-1-biological-evaluation-medical-devices]
- 34. Organic bioelectronics: materials and biocompatibility [https://openresearch.newcastle.edu.au/articles/journal_contribution/Organic_bioelectronics_materials_and_biocompatibility/29027228]
- 35. Organic Bioelectronics: Materials and Biocompatibility [https://www.mdpi.com/1422-0067/19/8/2382]
- 36. Convergence of biocompatible printed electronics and ... [https://www.nature.com/articles/s41528-025-00421-8]
- 37. Biocompatibility testing of medical devices [https://senzagen.com/2025/08/19/biocompatibility-testing-of-medical-devices/]
- 38. Biological Testing Methods of Medical Devices [https://namsa.com/resources/blog/biological-testing-methods-of-medical-devices/]
- 39. Cytotoxicity, Sensitization & Irritation Testing Explained [https://nabi.bio/cytotoxicity-sensitization-and-irritation-testing-what-do-they-involve/]
- 40. Cytotoxicity Testing for Medical Devices: A Guide to ... [https://www.mddionline.com/testing/cytotoxicity-testing-for-medical-devices-a-guide-to-compliance-best-practices]
- 41. A review of cytotoxicity testing methods and in vitro study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534221/]
- 42. In vitro assessment of the biocompatibility of chemically ... [https://www.nature.com/articles/s41598-022-08443-2]
- 43. Implant Study with Histopathology Tests [https://www.nelsonlabs.com/testing/implantation-with-histopathologytests/]
- 44. Histology: The gold standard for diagnosis? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10031787/]
- 45. Histological Analysis - an overview [https://www.sciencedirect.com/topics/engineering/histological-analysis]
- 46. Histological and Histomorphometric Insights into Implant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249557/]
- 47. Comparative Analysis of the Histological Characteristics ... [https://www.mdpi.com/2077-0383/14/7/2161]
- 48. An experimental comparison of two different clinically used ... [https://pubmed.ncbi.nlm.nih.gov/22487460/]
- 49. Next-Gen Biocompatibility Testing: Innovations in Medical ... [https://ebi.bio/next-gen-biocompatibility-testing-innovations-in-medical-devices-labs/]
- 50. Organoids VS Organ-on-a-chip: A Comparative Review ... [https://elveflow.com/microfluidic-reviews/organoids-vs-organ-on-a-chip/]
- 51. Organoids and organs-on-chips: Recent advances ... [https://www.sciencedirect.com/science/article/abs/pii/S2666634025000947]
- 52. Expanding the Frontiers of Human Biology with Organ-on-a ... [https://emulatebio.com/expanding-the-frontiers-of-human-biology-with-organ-on-a-chip-technology-highlights-from-the-2025-mps-world-summit/]
- 53. State-of-the-Art Organ-on-Chip Models and Designs for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383757/]
- 54. REPROCELL Launches Next-Generation System for 3D ... [https://www.reprocell.com/news/reprocell-launches-next-generation-system-for-3d-bioengineered-tissues]
- 55. Atomic Force Microscopy on Biological Materials Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6535871/]
- 56. Evaluation of the Biocompatibility of Poly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11798344/]
- 57. Resolution enhancement of scanning electron micrographs ... [https://www.sciencedirect.com/science/article/pii/S0264127525003752]
- 58. X-Ray Photoelectron Spectroscopy Market Size, Share [2032] [https://www.fortunebusinessinsights.com/x-ray-photoelectron-spectroscopy-market-113298]
- 59. Insights from XPS, DRIFT, and AFM Techniques [https://link.springer.com/article/10.1007/s10924-025-03578-5]
- 60. Immune-compatible designs of semiconducting polymers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355568/]
- 61. Stretchable all-gel organic electrochemical transistors [https://www.nature.com/articles/s41467-025-59240-0]
- 62. Design and Development of Biocompatible, Flexible, ... [https://pubmed.ncbi.nlm.nih.gov/40407559/]
- 63. Stretchable Organic Transistors for Biomedical Applications [https://www.aps.anl.gov/APS-Science-Highlight/2022-11-21/stretchable-organic-transistors-for-biomedical-applications]
- 64. 💡 A Biocompatible and Stretchable Transistor for Next-Generation Implantable Devices [https://quantum-server-materials.blogspot.com/2025/09/biocompatible-and-stretchable.html]
- 65. Foreign body response to synthetic polymer biomaterials and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9159526/]
- 66. Mitigating Foreign Body Reaction and Promoting Tissue ... [https://www.mdpi.com/2079-6412/15/9/1026]
- 67. Foreign Body Reaction to Neural Implants: A Comparative ... [https://www.mdpi.com/2079-6374/15/9/599]
- 68. Immunomodulating Red Blood Cell Coating for Mitigation ... [https://www.sciencedirect.com/science/article/pii/S2666138125000143]
- 69. Functionalization of Implantable Systems for Controlled ... [https://link.springer.com/article/10.1007/s40883-025-00401-4]
- 70. Decoding Fibrotic Encapsulation in Plastic Surgery implants [https://www.sciencedirect.com/science/article/abs/pii/S0927776525006988]
- 71. SMI-Capsular Fibrosis and Biofilm Dynamics: Molecular ... [https://www.mdpi.com/1422-0067/25/21/11675]
- 72. Adhesive anti-fibrotic interfaces on diverse organs [https://www.nature.com/articles/s41586-024-07426-9]
- 73. Antifouling Immunomodulatory Copolymer Architectures That ... [https://pubmed.ncbi.nlm.nih.gov/39722171/]
- 74. AI Takes on Biofouling Prevention and Removal in 2025 [https://maritime-innovations.com/ai-takes-on-biofouling-prevention-and-removal-in-2025/]
- 75. Progress in anti-biofouling materials and coatings for the ... [https://www.sciencedirect.com/science/article/abs/pii/S1001074225003109]
- 76. Enhanced long-term corrosion resistance and self-healing ... [https://www.nature.com/articles/s41598-025-92158-7]
- 77. Long-Term Stability in Electronic Properties of Textile ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10003982/]
- 78. Recent progress in metal-organic frameworks for corrosion ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854525005454]
- 79. Research progress and prospects of metal–organic ... [https://pubs.rsc.org/en/content/articlelanding/2025/cc/d5cc04529k]
- 80. Enhanced Corrosion Protection Performance by Organic ... [https://www.nature.com/articles/s41598-018-29299-5]
- 81. Extractables and Leachables Testing for Medical Devices [https://measurlabs.com/blog/medical-device-extractables-and-leachables-testing/]
- 82. Medical Device Extractables and Leachables Testing Lab [https://namsa.com/services/testing/biocompatibility-testing/iso-10993-18-extractables-leachables-testing/]
- 83. Extractables and Leachables: Best Practices & Key ... [https://adragos-pharma.com/extractables-and-leachables-best-practices-and-key-considerations/]
- 84. Extractables & Leachables Testing for Device Safety [https://nabi.bio/insights-into-extractables-leachables-testing-ensuring-medical-device-safety/]
- 85. Extractables and Leachables Testing [https://www.intertek.com/pharmaceutical/analysis/extractables-leachables/]
- 86. 5th Annual Extractables & Leachables Summit 2025 [https://www.uventia.com/event/5th-annual-extractables-leachables-summit-2025/?srsltid=AfmBOorSwPfUEnNTTsIS37FORsiRABcI7iQ2p7oa_ZA77zywQvLyOaqL]
- 87. Risk Assessment [https://elsiedata.org/risk-assessment/]
- 88. Organic semiconductors based wearable bioelectronics [https://www.sciencedirect.com/science/article/pii/S2950235725000034]
- 89. Organic Electronics Market Size, Share, 2033 [https://www.marketdataforecast.com/market-reports/organic-electronics-market]
- 90. Current and emerging strategies for biocompatible ... [https://www.sciencedirect.com/science/article/pii/S2666386424000778]
- 91. Solution-processable and photo-curable system for low-cost ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12528392/]
- 92. Advances and perspectives in fiber-based electronic ... [https://www.nature.com/articles/s41528-025-00465-w]
- 93. Improving In Vitro–In Vivo Correlation (IVIVC) for Lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567226/]
- 94. Ivivc Conversion Final 2025 | PDF | Bioavailability | In Vitro [https://www.scribd.com/document/896652915/Ivivc-Conversion-Final-2025]
- 95. Demonstration of in vitroin vivo relationship (IVIVR) and ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354925005003]
- 96. Demonstration of in vitro-in vivo relationship (IVIVR) and ... [https://pubmed.ncbi.nlm.nih.gov/41173270/]
- 97. Comparative Analysis of Chemical Distribution Models for ... [https://www.mdpi.com/2305-6304/13/6/439]
- 98. Evaluating cell viability assessment techniques: a comparative ... [https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-025-01452-y]
- 99. Assessment and Comparison of Viability Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10872314/]
- 100. A study on the cellular adhesion properties of a hybrid ... [https://www.nature.com/articles/s41598-025-01545-7]
- 101. An Overview of the Current State of Cell Viability ... [https://www.mdpi.com/1422-0067/26/1/220]
- 102. Biological responses to biomaterials: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12068782/]
- 103. Enhancing Tissue Integration and Reducing Inflammation ... [https://www.mdpi.com/1422-0067/26/12/5854]
- 104. Organic vs Inorganic Semiconductors: Which Has More ... [https://eureka.patsnap.com/article/organic-vs-inorganic-semiconductors-which-has-more-potential]
- 105. Research and Progress on Organic Semiconductor Power ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11243007/]
- 106. Design Parameters and Human Biocompatibility Assessment... - Peeref [https://www.peeref.com/works/27750025]
- 107. Add a Twist to π-molecules! A New Design Strategy for ... [https://www.ims.ac.jp/en/news/2025/06/0625_1.html]
- 108. Revolutionizing brain‒computer interfaces - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243264/]
- 109. Improved diagnostic performance of insertable cardiac ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10787483/]
- 110. Validation and Performance of a Wearable Heart-Rate ... [https://www.analog.com/en/resources/technical-articles/validation-and-performance-of-a-wearable-heartrate-monitoring-algorithm.html]
- 111. Prospective Human Validation of Artificial Intelligence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11450923/]
- 112. State-of-the-art wearable sensors for cardiovascular health [https://www.nature.com/articles/s44325-025-00090-6]
- 113. Skin-Interfaced Electronics: A Promising and Intelligent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10085866/]
- 114. Design strategies for skin-interfaced sensors [https://www.sciencedirect.com/science/article/abs/pii/S0924424724006654]
- 115. Biocompatibility and Toxicology Program: Research on ... [https://www.fda.gov/medical-devices/medical-device-regulatory-science-research-programs-conducted-osel/biocompatibility-and-toxicology-program-research-medical-devices-biocompatibility-and-toxicology]