Barostim Neo System: Comprehensive Technical Specifications for Cardiovascular Research and Device Development
This article provides a detailed technical analysis of the Barostim Neo system, a novel carotid sinus baroreceptor activation therapy for resistant hypertension and heart failure.
Barostim Neo System: Comprehensive Technical Specifications for Cardiovascular Research and Device Development
Abstract
This article provides a detailed technical analysis of the Barostim Neo system, a novel carotid sinus baroreceptor activation therapy for resistant hypertension and heart failure. Tailored for researchers, scientists, and drug development professionals, it covers the foundational biophysics of baroreflex activation, system architecture and implantation methodology, critical troubleshooting and optimization protocols for experimental studies, and comprehensive validation data versus pharmacotherapy and other device-based interventions. The review synthesizes engineering specifications with clinical evidence to inform future biomedical research and therapeutic development.
Unveiling Barostim Neo: Core Biophysics and System Architecture for Researchers
Application Notes
Baroreflex Activation Therapy (BAT) using the Barostim neo system is a novel device-based neuromodulation therapy for patients with resistant hypertension and heart failure with reduced ejection fraction (HFrEF). The therapy directly addresses autonomic imbalance, a core pathophysiological mechanism in these conditions.
Key Principles:
- Baroreceptor Function: High-pressure baroreceptors in the carotid sinus detect arterial wall stretch (pressure). Their afferent signaling to the nucleus tractus solitarius (NTS) is diminished in chronic disease states.
- BAT Mechanism: Electrical activation of these afferent fibers via an implantable system mimics natural baroreceptor signaling, restoring autonomic balance.
- Central Integration: Enhanced NTS signaling leads to increased parasympathetic (vagal) outflow and decreased sympathetic outflow from the medullary cardiovascular centers.
- Systemic Effects: The net effect is a reduction in sympathetic drive to the heart, kidneys, and peripheral vasculature, resulting in lowered heart rate, reduced vasoconstriction, improved renal function, and reverse cardiac remodeling.
Quantitative Clinical Data Summary:
Table 1: Key Efficacy Outcomes from Major BAT Clinical Trials
| Parameter | Resistant Hypertension (Rheos DEBuT-HT, Rheos Pivotal) | HFrEF (BeAT-HF Trial) | Notes |
|---|---|---|---|
| Systolic BP Reduction | -26 ± 29 mmHg (DEBuT-HT, 12 mo) | -7.2 mmHg (vs. +1.6 mmHg control) | Sustained reduction at 3 years in responder cohort. |
| NYHA Class Improvement | Not Applicable | 59% improved ≥1 class (vs. 42% control) | Significant improvement in quality of life. |
| 6-Minute Walk Distance | Not Applicable | +59.6 meters (vs. +3.7 meters control) | Primary endpoint of BeAT-HF trial. |
| NT-proBNP Reduction | Not Primary Focus | Greater reduction vs. control | Marker of cardiac wall stress and heart failure severity. |
| Heart Rate Reduction | ~5-10 bpm | Significant reduction observed | Direct indicator of reduced sympathetic tone. |
| Major Adverse Events | 17.4% procedure-related (Pivotal) | 1.6% system/procedure-related (BeAT-HF) | Safety profile improved with Barostim neo vs. earlier systems. |
Table 2: Barostim neo System Technical Specifications (Research Context)
| Component | Specification | Research Implication |
|---|---|---|
| Pulse Generator | Titanium housing, programmable (1-7.5V, 20-500µs, 20-160Hz) | Enables precise titration of electrical stimulus for dose-response studies. |
| Carotid Sinus Lead | Bipolar, steroid-eluting, minimally invasive cuff electrode (3.0mm width) | Standardized electrode interface for consistent neural activation. Target is carotid sinus adventitia. |
| System Lifespan | ~4-6 years (typical settings) | Critical for long-term chronic study design and endpoint timing. |
| Impedance Range | 300 - 2000 Ohms (typical) | Monitoring parameter for lead integrity and tissue interface stability. |
| Communication | Wireless telemetry (Radio Frequency, 402-405 MHz MICS band) | Enables remote data download and non-invasive parameter adjustment in chronic studies. |
Experimental Protocols
Protocol A: In Vivo Assessment of Acute Hemodynamic Response to BAT in an Anesthetized Large Animal Model (e.g., Porcine) Objective: To quantify the immediate changes in central hemodynamics and sympathetic nerve activity (SNA) upon BAT initiation. Materials: Anesthetized subject, Barostim neo implant kit (research version), arterial pressure catheter, femoral vein access, renal sympathetic nerve activity (RSNA) recording apparatus, ventilator, data acquisition system. Methodology:
- Anesthetize, intubate, and ventilate the subject. Maintain stable anesthesia (e.g., isoflurane/alpha-chloralose).
- Instrument subject: Insert arterial pressure catheter into femoral/ carotid artery. Isolate a renal nerve branch for multi-unit RSNA recording.
- Implant BAT electrode: Surgically expose the carotid sinus. Place the bipolar cuff electrode around the sinus adventitia. Connect to an external pulse generator simulator.
- Baseline Recording: Record 10 minutes of stable mean arterial pressure (MAP), heart rate (HR), and integrated RSNA.
- BAT Stimulation: Initiate stimulation at sub-therapeutic parameters (2.0V, 80µs, 50Hz). Increase voltage in 0.5V increments every 5 minutes.
- Data Acquisition: At each step, record the last 2 minutes of hemodynamic and neurographic data. Note threshold for MAP/HR response.
- Pharmacological Block: Administer intravenous hexamethonium (ganglionic blocker, 10 mg/kg). Repeat stimulation at maximal effective voltage to confirm neural mediation of response.
- Analysis: Plot MAP and HR vs. Stimulation Voltage. Express RSNA as percent change from baseline.
Protocol B: Ex Vivo Molecular Analysis of Myocardial Tissue Following Chronic BAT in a Heart Failure Model Objective: To evaluate reverse remodeling and changes in sympathetic signaling markers in myocardial tissue after chronic BAT. Materials: Heart failure animal model (e.g., post-MI sheep), Barostim neo system, terminal procedure kit, RNA/DNA/protein extraction kits, qPCR thermocycler, Western blot apparatus. Methodology:
- Model Induction & Group Allocation: Induce myocardial infarction (MI) via coronary occlusion. After 4 weeks, confirm HF phenotype (reduced EF by echocardiography). Randomize into: i) BAT Therapy (implant active), ii) Sham Control (implant inactive), iii) Healthy Control.
- Chronic Therapy: Implant Barostim neo system in BAT group. Program to deliver therapy 12 hours/day. Sham group has system implanted but inactivated. Monitor for 3 months.
- Terminal Tissue Harvest: At endpoint, euthanize and rapidly excise the heart. Dissect left ventricular (LV) free wall, septum, and right ventricle. Flash-freeze in liquid nitrogen for molecular analysis or preserve in formalin for histology.
- Molecular Endpoints:
- qPCR: Extract RNA. Measure expression of: Beta-1 Adrenergic Receptor (ADRB1), G-protein-coupled receptor kinase 2 (GRK2), Atrial Natriuretic Peptide (NPPA), Brain Natriuretic Peptide (NPPB), Collagen I/III (COL1A1, COL3A1). Use GAPDH for normalization.
- Western Blot: Extract protein. Analyze levels of: Phosphorylated vs. total RyR2 (ryanodine receptor), SERCA2a, Phospholamban, Connexin-43, Tyrosine Hydroxylase.
- Histology: Section formalin-fixed tissue. Perform Masson's Trichrome stain for collagen deposition (fibrosis) and calculate percentage fibrotic area.
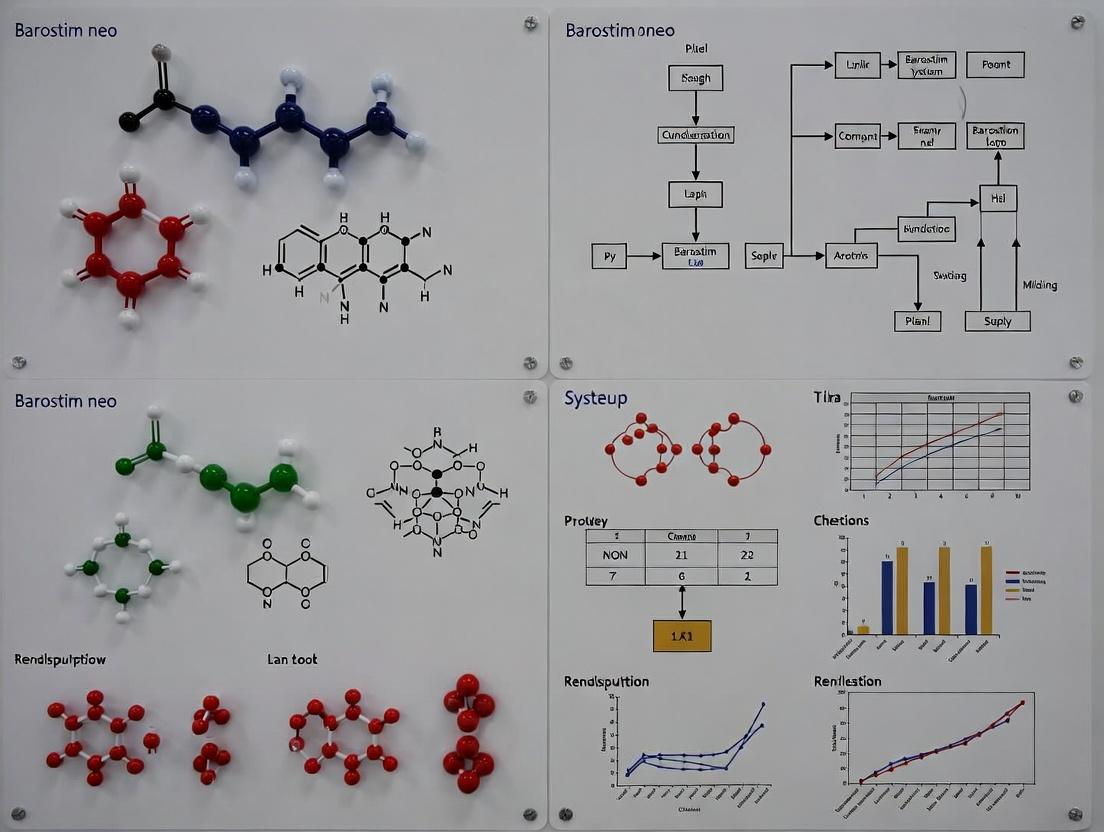
Diagrams
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Preclinical BAT Research
| Item / Reagent | Function / Application in BAT Research |
|---|---|
| Barostim neo Preclinical System | Provides the precise, programmable electrical stimulus for chronic in vivo studies. Enables translation of clinical parameters to animal models. |
| Telemetry Pressure Transmitters (e.g., DSI) | Allows continuous, ambulatory measurement of arterial blood pressure and heart rate in conscious, freely moving animals, critical for chronic efficacy studies. |
| Sympathetic Nerve Activity (SNA) Recording System | Amplifier, microelectrodes, and software for direct measurement of renal or splanchnic SNA, the gold-standard functional readout of autonomic modulation. |
| Ganglion-Blocking Agent (e.g., Hexamethonium Chloride) | Pharmacological tool to confirm the neural (vs. direct muscular) mediation of BAT-induced hemodynamic effects in acute experiments. |
| ELISA/Kits for Circulating Markers (e.g., Norepinephrine, NT-proBNP, Renin, Aldosterone) | Quantifies systemic neurohormonal changes in response to chronic BAT therapy in plasma/serum samples. |
| Primary Antibodies for Western Blot (Anti-GRK2, Anti-pRyR2, Anti-Tyrosine Hydroxylase) | Key reagents for assessing molecular changes in cardiac tissue and stellate ganglia related to sympathetic signaling and calcium handling. |
| Masson's Trichrome Stain Kit | Standard histological stain for visualizing and quantifying myocardial collagen deposition (fibrosis), a key structural endpoint in reverse remodeling. |
| Programmable External Pulse Generator | For acute or in vitro studies, allows fine control of stimulus waveform (pulse width, frequency, amplitude) independent of the full implant system. |
Application Notes
The Barostim Neo system is a carotid baroreceptor activation therapy device for the treatment of resistant hypertension and heart failure. Its technical specifications are critical for researchers investigating neuromodulation mechanisms, device-tissue interfaces, and long-term biocompatibility. The system's operation hinges on the precise integration of its three primary components: the implanted pulse generator (IPG), the lead, and the electrode. Research in this domain focuses on electrical parameter optimization, material science for chronic implantation, and the physiological decoding of baroreflex signaling pathways.
Component Specifications & Quantitative Data
Table 1: Barostim Neo Generator Specifications
| Parameter | Specification |
|---|---|
| Model | Barostim Neo (C214) |
| Dimensions | 36.5 mm x 47.5 mm x 8.1 mm |
| Weight | 20 grams (approx.) |
| Battery | Single-cell Lithium Carbon Monofluoride (Li-CFx) |
| Programmable Parameters | Pulse Amplitude (0.0 - 7.5 mA), Pulse Width (115 - 755 µs), Frequency (40 - 150 Hz) |
| Typical Output | 4.0 mA, 365 µs, 80 Hz (subject to patient programming) |
| Communications | Bidirectional RF telemetry |
| Expected Service Life | > 4 years (dependent on programmed parameters) |
Table 2: Lead and Electrode Specifications
| Component | Specification |
|---|---|
| Lead Model | Barostim Neo Lead (C213) |
| Lead Design | Unipolar, silicone insulated, helical coil conductor |
| Lead Length | 52 cm |
| Electrode Type | Cylindrical, balloon-expandable stent-like electrode |
| Electrode Material | Platinum-Iridium alloy |
| Electrode Surface Area | ~17.5 mm² |
| Fixation Mechanism | Balloon-expandable stent for carotid sinus apposition |
Experimental Protocols
Protocol 1: In Vitro Electrode Impedance and Charge Injection Capacity Testing
Objective: To characterize the electrochemical performance and safety limits of the Barostim Neo electrode. Methodology:
- Setup: Place the electrode in a 37°C phosphate-buffered saline (PBS) solution simulating physiological fluid. Use a platinum counter electrode and a Ag/AgCl reference electrode.
- Electrochemical Impedance Spectroscopy (EIS): Apply a sinusoidal voltage perturbation (10 mV RMS) across a frequency range of 0.1 Hz to 100 kHz. Measure impedance modulus and phase angle.
- Cyclic Voltammetry (CV): Sweep the electrode potential between water electrolysis limits (-0.6 V to +0.8 V vs. Ag/AgCl) at a scan rate of 50 mV/s. Calculate the real surface area from the charge under the curve.
- Voltage Transient Measurement: Deliver the device's typical waveform (4.0 mA, 365 µs, cathodic-first, biphasic) into the solution. Record the interphase voltage via the reference electrode. The access voltage is subtracted to determine the electrode polarization voltage. Ensure polarization remains within water window limits.
Protocol 2: Histomorphometric Analysis of Tissue-Electrode Interface
Objective: To assess chronic tissue response and fibrosis around the implanted carotid sinus electrode. Methodology:
- Animal Model: Implant the Barostim Neo lead/electrode in the carotid sinus of a large animal model (e.g., sheep) per surgical guidelines. Include a control (sham implant).
- Explanation: After 90-180 days, euthanize and carefully explant the carotid sinus segment with the electrode in situ.
- Fixation & Sectioning: Perfuse-fix with 10% neutral buffered formalin. Embed in methyl methacrylate (MMA) resin. Section using a diamond-blade microtome to produce ~50 µm slices adjacent to the electrode.
- Staining & Analysis: Stain sections with Hematoxylin & Eosin (H&E) and Masson's Trichrome (for collagen). Use digital image analysis to quantify fibrous capsule thickness, inflammatory cell density, and tissue integration.
Protocol 3: Quantification of Baroreflex Activation via Sympathetic Nerve Activity (SNA)
Objective: To measure the electrophysiological response to Barostim Neo stimulation. Methodology:
- Preparation: In an anesthetized animal model, isolate a postganglionic sympathetic nerve fiber bundle (e.g., renal nerve).
- Recording: Place the nerve on a bipolar platinum-iridium recording electrode. Connect to a differential amplifier, band-pass filter (100-1000 Hz), and store raw data.
- Stimulation Protocol: Implant and activate the Barostim Neo system at varying amplitudes (2-6 mA). Use a standardized on/off cycle (e.g., 30 seconds on/30 seconds off).
- Data Analysis: Full-wave rectify and integrate the raw neurogram. Calculate percent change in integrated SNA during stimulation periods versus pre-stimulation baseline. Plot stimulus-response curves.
Signaling Pathway of Carotid Baroreceptor Activation
Diagram Title: Baroreflex Neuromodulation Pathway
Experimental Workflow for Device Performance Analysis
Diagram Title: Integrated Device Research Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Reagent | Function in Barostim Research |
|---|---|
| Phosphate-Buffered Saline (PBS), 0.1M | Electrolyte solution for in vitro electrochemical testing, simulating extracellular fluid. |
| Ag/AgCl Reference Electrode | Provides a stable, non-polarizable potential reference for all electrochemical measurements. |
| Methyl Methacrylate (MMA) Embedding Kit | Hard plastic resin for embedding metal-containing tissue specimens, enabling precise sectioning near the electrode. |
| Masson's Trichrome Stain Kit | Differentiates collagen (blue/green) from muscle/cytoplasm (red), critical for fibrosis quantification. |
| Platinum-Iridium Microelectrodes (for SNA) | High-conductivity, stable electrodes for recording low-amplitude sympathetic nerve action potentials. |
| Differential Amplifier & Data Acquisition System | Isolates and amplifies the tiny neural signals from background noise for SNA quantification. |
| Custom RF Telemetry Interface | Allows researchers to non-invasively interrogate and program the implanted IPG in chronic animal studies. |
| Finite Element Modeling (FEM) Software | Simulates electric field distribution and mechanical stress at the electrode-tissue interface. |
Within the broader thesis on Barostim Neo system technical specifications research, this document details the key electrical engineering parameters—pulse width, amplitude, frequency, and duty cycle—that define its operation. These parameters are critical for researchers and drug development professionals investigating autonomic modulation, as they directly influence the system's therapeutic efficacy and safety profile. Precise control and documentation of these ranges are essential for experimental reproducibility and mechanistic understanding in preclinical and clinical research.
Parameter Definitions & Therapeutic Ranges
The Barostim Neo system delivers electrical pulses to the carotid baroreceptors. The interaction of these parameters dictates the neural stimulus.
Table 1: Barostim Neo Key Engineering Parameters & Typical Ranges
| Parameter | Definition | Typical Therapeutic Range | Units | Physiological Impact |
|---|---|---|---|---|
| Pulse Width | Duration of a single electrical pulse. | 110 - 750 | microseconds (µs) | Affects which nerve fiber types are recruited. Wider pulses may recruit smaller fibers. |
| Amplitude | Intensity or magnitude of the electrical current. | 0.5 - 7.0 | milliamps (mA) | Determines the strength of baroreceptor activation. Must be titrated to patient response. |
| Frequency | Number of pulses delivered per second. | 20 - 100 | Hertz (Hz) | Influences the sustained nature of the baroreflex activation and heart rate modulation. |
| Duty Cycle | Fraction of time the device is actively stimulating within a programmed cycle. | Typically 14% (e.g., 14s ON, 86s OFF) or continuous | Percent (%) | Allows for intermittent stimulation, potentially preventing desensitization and conserving battery life. |
Note: Specific parameter combinations are physician-programmed based on individual patient therapeutic response and are not all user-adjustable. The system operates within these predefined safety limits.
Experimental Protocol: Quantifying Autonomic Response to Parameter Variation
This protocol outlines a method for researchers to systematically assess the physiological impact of varying Barostim parameters in a controlled experimental setting.
Objective: To measure acute changes in heart rate (HR) and blood pressure (BP) in response to systematic variation of pulse amplitude and frequency.
Materials & Preparations:
- Animal Model/Surgical Prep: Anesthetized large animal (e.g., canine) instrumented for acute study.
- Barostim Neo System: Implanted with lead positioned at the carotid sinus.
- Physiological Recorders: Continuous arterial BP line, ECG leads connected to a digital acquisition system.
- Data Analysis Software: (e.g., LabChart, MATLAB) for real-time visualization and post-hoc analysis.
Procedure:
- Baseline Recording: With stimulation OFF, record stable baseline HR and BP for 10 minutes.
- Parameter Set Establishment: Set a standard pulse width (e.g., 250 µs) and duty cycle (e.g., 14%). Amplitude will be the primary variable.
- Amplitude Titration:
- Start at sub-therapeutic amplitude (e.g., 0.5 mA).
- Initiate stimulation. Record data for 5 minutes post-activation.
- Increment amplitude by 0.5 mA steps up to the maximum tolerable level (without adverse effects).
- At each step, allow a 5-minute stabilization period before the 5-minute recording window.
- Between each amplitude level, turn stimulation OFF for a 10-minute washout period to return to baseline.
- Frequency Variation (at Fixed Amplitude):
- Select an intermediate therapeutic amplitude from Step 3.
- Repeat the cycle of stimulation ON/OFF, varying frequency (e.g., 20, 40, 60, 80, 100 Hz) at this fixed amplitude.
- Data Analysis:
- For each parameter set, calculate the average HR and mean arterial pressure (MAP) during the final 3 minutes of each recording window.
- Express changes as ΔHR and ΔMAP from the immediately preceding OFF-period baseline.
- Plot dose-response curves (ΔHR vs. Amplitude; ΔMAP vs. Frequency).
Signaling Pathway Visualization
Barostim Neural Pathway from Stimulation to Physiological Response
Experimental Workflow for Parameter Optimization
Workflow for Systematic Parameter Optimization
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Materials for Barostim Parameter Studies
| Item | Function in Research |
|---|---|
| Programmer/Telemetry Wand | Enables non-invasive communication with the implanted device for real-time parameter adjustment and data retrieval in chronic studies. |
| Acute/Cronic Animal Model | Large animal model (e.g., canine, swine) providing relevant anatomy and physiology for translational baroreflex research. |
| High-Fidelity Data Acquisition System | Records continuous analog signals (arterial BP, ECG, sympathetic nerve activity) with high temporal resolution synchronized to stimulus pulses. |
| Autonomic Blocking Agents | Pharmacological tools (e.g., Atropine, Propranolol, Hexamethonium) to dissect parasympathetic vs. sympathetic contributions to the observed response. |
| Neural Recording Electrodes | Microwire or cuff electrodes for concurrent recording of afferent baroreceptor or efferent sympathetic nerve activity during stimulation. |
| Custom Analysis Scripts (MATLAB/Python) | For batch processing of stimulation-triggered averages, frequency-domain analysis (e.g., power spectral density of HR/BP), and parameter-response modeling. |
Application Notes
The long-term clinical success of implantable medical devices, such as the Barostim neo system, is fundamentally dependent on the biocompatibility and material stability of their constituent components. This research forms a core technical specification pillar, analyzing the primary materials used in active implantable device construction: Titanium (Ti, typically Grade 5 or Grade 23) for hermetic encapsulation, Platinum-Iridium (Pt-Ir, typically 90/10 or 80/20) for electrodes, and Medical-Grade Silicone (e.g., Silicone Elastomer) for insulation and encapsulation. The interaction of these materials with the physiological environment dictates the host inflammatory response, long-term device function, and the stability of the electrode-tissue interface. Key performance metrics include corrosion resistance, ion release profiles, fibrotic encapsulation, and chronic inflammatory response. The following notes detail their roles within an implantable neurostimulator context.
Titanium (Ti-6Al-4V ELI, Grade 23) Titanium serves as the primary hermetic enclosure material for the Barostim neo pulse generator. Its exceptional strength-to-weight ratio, corrosion resistance due to a stable surface oxide layer (TiO₂, 5-10 nm thick), and proven biocompatibility make it ideal. The Grade 23 (Extra Low Interstitial) alloy minimizes vanadium and aluminum ion release. The surface can be electropolished to a roughness (Ra) < 0.8 µm to minimize bacterial adhesion and promote soft tissue integration without excessive fibrous capsule formation (typically 50-200 µm thick after 12 weeks in vivo). Passive oxide layer regrowth occurs spontaneously in vivo after any micro-damage.
Platinum-Iridium Alloy (90% Pt, 10% Ir) This alloy is the standard for stimulating and sensing electrodes. Iridium addition increases tensile strength and wear resistance compared to pure platinum. The charge injection capacity (CIC) is critical; for Pt-Ir 90/10, the reversible CIC is approximately 150-350 µC/cm² for geometric surface area. Surface texturing via sputtered or activated iridium oxide films (AIROF) can increase CIC to > 1 mC/cm². The alloy's corrosion resistance under biphasic pulsing is excellent, with corrosion current densities below 10 nA/cm² in physiological saline. Chronic impedance typically stabilizes between 500-2000 Ω post-healing.
Medical-Grade Silicone Elastomer (e.g., LSR Silicone) Used for lead insulation, suture sleeves, and external coating, silicone elastomers offer excellent biostability, flexibility, and electrical insulation. High-purity, platinum-cured silicones with low levels of leachables (e.g., < 50 ppm total extractables) are required. Key concerns include long-term resistance to in vivo degradation (hydrolysis, lipid absorption) and the formation of a fibrous capsule. Silicone elastomers can absorb small molecules (lipids, drugs) which may slightly alter mechanical properties (e.g., a 1-5% swell over years in vivo).
Table 1: Material Properties and Performance Metrics
| Material/Property | Titanium (Grade 23) | Platinum-Iridium (90/10) | Silicone Elastomer (Implant Grade) |
|---|---|---|---|
| Primary Function | Hermetic Encapsulation | Electrode/Conductor | Insulation/Encapsulation |
| Density (g/cm³) | 4.43 | 21.5 | 1.12 - 1.25 |
| Tensile Strength (MPa) | 860-965 | 1240-1450 (Annealed) | 8 - 12 |
| Elongation at Break (%) | 10-15 | 20-30 | 400 - 800 |
| Corrosion Rate in PBS (µm/year) | < 0.1 | < 0.01 | Not Applicable (Degrades via swell) |
| Ion Release Rate (ng/cm²/day) | Ti: < 0.5, Al: < 0.05, V: < 0.005 | Pt: < 0.1, Ir: < 0.05 | Siloxane Oligomers: < 10 |
| Fibrous Capsule Thickness (12 weeks, avg.) | 50 - 150 µm | 100 - 250 µm (around lead) | 100 - 300 µm |
| Charge Injection Limit (µC/cm², ph. balanced pulse) | N/A | 300 - 350 (Geometric) | N/A |
| Dielectric Strength (kV/mm) | N/A | N/A | 20 - 25 |
Experimental Protocols
Protocol 1:Static Immersion Corrosion and Ion Release Profiling (ASTM F2129 & ISO 10993-15)
Objective: To quantitatively assess the corrosion behavior and metal ion release of Ti and Pt-Ir alloy samples in a simulated physiological environment.
Materials:
- Test specimens (10mm x 10mm x 1mm, polished to Ra ~0.4 µm).
- Control: 316L Stainless Steel (for comparison).
- Solution: Phosphate Buffered Saline (PBS, pH 7.4 ± 0.1) or Hanks' Balanced Salt Solution (HBSS).
- Incubation oven (37°C ± 1°C).
- Inductively Coupled Plasma Mass Spectrometry (ICP-MS).
- Electrochemical Workstation (for ASTM F2129 Scratch Test).
Methodology:
- Sample Preparation: Clean specimens ultrasonically in acetone, isopropanol, and deionized water. Sterilize via autoclave (Ti, Pt-Ir) or ethylene oxide (silicone).
- Immersion: Immerse samples in pre-warmed PBS at a surface-area-to-volume ratio of 1 cm²/mL. Use polypropylene containers. Maintain at 37°C for 30, 90, and 180 days (n=5 per time point).
- Solution Analysis: At each time point, remove and acidify 5 mL of immersion solution. Analyze via ICP-MS for Ti, Al, V, Pt, Ir ions. Express as cumulative release (ng/cm²).
- Surface Analysis: Post-immersion, examine surfaces via Scanning Electron Microscopy (SEM) and Energy Dispersive X-ray Spectroscopy (EDS) for pitting or surface oxide changes.
- (Optional) Electrochemical Testing: Perform potentiodynamic polarization per ASTM F2129 in deaerated PBS at 37°C to determine breakdown potential (Eb).
Protocol 2:Fibrous Capsule Thickness and Histomorphometry (ISO 10993-6)
Objective: To evaluate the in vivo biocompatibility and chronic inflammatory response to material implants via a subcutaneous implantation model.
Materials:
- Material discs (φ12mm x 1mm thick, with edges smoothed).
- Animal model (e.g., Sprague-Dawley rats, n=6 per material group).
- Surgical kit, sutures.
- Histology supplies: 10% Neutral Buffered Formalin, paraffin embedding, microtome, Hematoxylin & Eosin (H&E) stain, Masson's Trichrome stain.
- Light microscope with image analysis software.
Methodology:
- Implantation: Anesthetize rat. Create subcutaneous pockets dorsally. Implant one material disc per pocket (2 per animal, separated). Close wound. Maintain for 4, 12, and 26 weeks.
- Explanation & Fixation: Euthanize at endpoint. Excise implant with surrounding tissue. Fix in formalin for 48 hours.
- Histological Processing: Dehydrate, paraffin-embed. Section through implant center (5 µm thickness). Perform H&E and Masson's Trichrome staining.
- Histomorphometry: Using microscopy, measure fibrous capsule thickness at 4 equidistant points around the implant. Score inflammatory response per ISO 10993-6: 0 (none) to 4 (severe) for cell types (lymphocytes, macrophages, neutrophils, giant cells). Quantify collagen density/alignment in capsule using Trichrome-stained sections with image analysis.
Protocol 3:Electrochemical Characterization of Pt-Ir Electrodes
Objective: To determine the charge storage capacity (CSC) and charge injection limits (CIL) of Pt-Ir electrodes.
Materials:
- Pt-Ir wire electrode (φ0.5 mm, 1 cm length exposed).
- Electrochemical cell with 3-electrode setup: Pt-Ir as Working Electrode, Pt mesh as Counter Electrode, Ag/AgCl (in 3M NaCl) as Reference Electrode.
- Electrolyte: 0.167 M PBS (pH 7.4) at 37°C.
- Potentiostat/Galvanostat with electrochemical impedance spectroscopy (EIS) and cyclic voltammetry (CV) capabilities.
Methodology:
- Cyclic Voltammetry (for CSC): Scan potential between water window limits (typically -0.6 V to +0.8 V vs. Ag/AgCl) at a slow scan rate (e.g., 50 mV/s). Record current. Calculate CSC by integrating the cathodic (or anodic) current over time and dividing by scan rate and geometric surface area (mC/cm²).
- Electrochemical Impedance Spectroscopy (EIS): Apply a 10 mV RMS sinusoidal perturbation from 100 kHz to 0.1 Hz at open circuit potential. Fit data to a modified Randles circuit to determine charge transfer resistance (Rct) and double-layer capacitance (Cdl).
- Voltage Transient Measurement (for CIL): Use a biphasic, charge-balanced current pulse (0.2 ms phase width). Incrementally increase current amplitude until the electrode potential exceeds the water window (safety limit = ±0.8 V vs. Ag/AgCl, including access voltage). The CIL is the charge density of the last safe pulse (µC/cm²).
Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Biocompatibility Testing
| Item | Function & Rationale |
|---|---|
| Phosphate Buffered Saline (PBS), pH 7.4 | Standard immersion medium for in vitro corrosion/degradation studies. Provides ionic strength and pH similar to extracellular fluid. |
| Hanks' Balanced Salt Solution (HBSS) | More complex physiological simulant containing glucose, Ca²⁺, Mg²⁺, and bicarbonate ions for more realistic ion release studies. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) Standards | Certified reference solutions for Ti, Al, V, Pt, Ir, Si, etc., used to calibrate ICP-MS for precise quantification of trace metal ion release. |
| 10% Neutral Buffered Formalin | Standard histological fixative. Preserves tissue architecture and cellular detail around explanted devices for accurate scoring. |
| Hematoxylin & Eosin (H&E) Stain Kit | Routine histological stain. Hematoxylin stains nuclei blue; eosin stains cytoplasm and extracellular matrix pink. Allows cell type identification and inflammatory scoring. |
| Masson's Trichrome Stain Kit | Special stain. Colors nuclei black, cytoplasm/keratin red, and collagen fibers blue. Essential for assessing fibrous capsule maturity and collagen density. |
| Potentiostat with EIS/CV Software | Instrument to perform electrochemical tests (Cyclic Voltammetry, Electrochemical Impedance Spectroscopy) for characterizing electrode materials and corrosion rates. |
| Simulated Body Fluid (SBF) | Ion concentration solution similar to human blood plasma, used for evaluating apatite-forming ability (bioactivity) and surface degradation. |
Within the context of research on the Barostim neo system, precise electrode placement at the carotid sinus is critical for effective baroreflex activation therapy. Optimal placement requires a detailed understanding of the target neurovascular anatomy to maximize therapeutic electrical field interaction with baroreceptor nerve endings while minimizing off-target effects. This document outlines the anatomical framework and provides protocols for its experimental validation.
Table 1: Carotid Sinus Anatomical & Biophysical Parameters for Electrode Targeting
| Parameter | Typical Measurement (Mean ± SD or Range) | Relevance to Barostim Electrode Placement |
|---|---|---|
| Location (Bifurcation) | C3-C5 vertebral level (common) | Determines surgical/access approach. |
| Carotid Sinus Wall Thickness | 0.4 - 0.7 mm | Influences current penetration; thinner walls may lower stimulation thresholds. |
| Density of Baroreceptor Endings | Highest in posterolateral adventitia | Primary target zone for electrode placement. |
| Distance to Vagus Nerve (X) | 7.5 ± 3.2 mm (posteromedial) | Critical for avoiding unintended vagal stimulation (bradycardia, cough). |
| Distance to Hypoglossal Nerve (XII) | >15 mm (usually superior/medial) | Lower risk, but posterior placement requires awareness. |
| Optimal Electrode Contact Zone | 5-10 mm segment proximal to bifurcation apex | Zone of maximal baroreceptor density. |
| Typical Impedance at 1 kHz | 600 - 1200 Ω (in vivo, post-healing) | Informs pulse generator output programming. |
Experimental Protocol: Histological Mapping of Human Carotid Sinus Baroreceptors
Objective: To quantitatively map the density and distribution of baroreceptor nerve endings (using specific immunohistochemical markers) within the carotid sinus adventitia to define the optimal anatomical target for electrode contact.
Materials:
- Human carotid sinus specimens (post-mortem or from surgical procedures, with ethical approval).
- Primary Antibodies: Anti-PGP9.5 (pan-neuronal marker), Anti-Tyrosine Hydroxylase (for mechanosensory fibers).
- Secondary Antibodies: Fluorescently conjugated (e.g., Alexa Fluor 488, 594).
- Microscopy: Confocal laser scanning microscope with z-stack capability.
- Image Analysis Software: e.g., Fiji/ImageJ with cell counting plugins.
Methodology:
- Tissue Preparation: Fix specimens in 4% paraformaldehyde for 24h. Embed in paraffin or optimal cutting temperature (OCT) compound. Section serially at 5-7 µm thickness in transverse and longitudinal planes.
- Immunohistochemistry: Perform antigen retrieval. Incubate with primary antibodies (PGP9.5 & Tyrosine Hydroxylase) overnight at 4°C. Apply species-appropriate fluorescent secondary antibodies.
- Imaging & Quantification: Acquire high-resolution z-stack images from standardized zones (medial, lateral, anterior, posterolateral). Use software to count PGP9.5+/Tyrosine Hydroxylase+ nerve terminal clusters per unit area (mm²).
- Data Analysis: Generate a density heat map. Correlate peak density zones with external anatomical landmarks (e.g., bifurcation apex, muscle insertions).
Experimental Protocol: Finite Element Modeling (FEM) of Stimulation Field
Objective: To model the electrical field distribution generated by the Barostim neo electrode in a patient-specific carotid sinus anatomy and predict activation thresholds for baroreceptor fibers.
Materials:
- High-resolution CT or MRI angiography data of neck vasculature.
- FEM Software: COMSOL Multiphysics, ANSYS, or Sim4Life.
- Tissue Electrical Properties Database: Conductivity (σ) and permittivity (ε) for blood, vessel wall, fat, muscle, connective tissue.
- Barostim Neo Electrode Model: CAD geometry of the electrode array.
Methodology:
- Geometry Reconstruction: Import imaging data. Segment key structures: Common, Internal, External Carotid Arteries, carotid sinus bulge, adjacent nerves (vagus, hypoglossal), and surrounding tissues.
- Assignment of Material Properties: Assign frequency-dependent electrical properties to each tissue compartment from published literature.
- Physics & Boundary Conditions: Apply the "Electric Currents" physics interface. Define the electrode contacts as terminals with a defined current or voltage stimulus waveform (e.g., 40 µs pulse width, 1-4 mA). Set outer boundaries as ground.
- Solving & Analysis: Solve for the spatial distribution of electric potential and field strength (V/m). Plot isofield contours. Overlay modeled baroreceptor density maps to calculate the percentage of fibers within the activating field (>10 V/m threshold).
Visualization: Signaling & Workflow Diagrams
Diagram 1: Barostim Baroreflex Activation Pathway
Diagram 2: Electrode Targeting Research Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Carotid Sinus & Barostim Research
| Item / Reagent | Function / Application |
|---|---|
| Anti-PGP9.5 Antibody (UCHL1) | Immunohistochemical pan-neuronal marker to identify all nerve fibers in the carotid sinus adventitia. |
| Anti-Tyrosine Hydroxylase Antibody | Marks catecholaminergic neurons; specifically labels the afferent baroreceptor nerve endings. |
| Tissue Clearing Kit (e.g., CUBIC, CLARITY) | Enables 3D visualization of innervation architecture in intact tissue samples. |
| Patient-Specific Vascular Phantom | 3D-printed model from CT angiography for in-vitro stimulation and field mapping validation. |
| Multichannel Electrophysiology System | For recording afferent nerve signals (from carotid sinus nerve) in acute animal models during stimulation. |
| Finite Element Modeling Software | To simulate the electrical field interaction between the electrode and complex neurovascular anatomy. |
| High-Resolution Micro-CT | For ex-vivo 3D micro-architectural analysis of vessel wall and electrode-tissue interface post-implant. |
Research Implementation: Implant Protocol, Programming, and Data Acquisition Methods
This protocol provides a detailed technical guide for the surgical implantation of the Barostim neo system in preclinical large animal models. This work is framed within a broader thesis investigating the technical specifications, biomechanical integration, and long-term performance of the Barostim neo system, a carotid sinus baroreceptor activation device for the treatment of resistant hypertension and heart failure. Precise preclinical implantation is critical for generating valid data on electrode stability, signal transduction, and tissue-device interface reactions, which directly inform clinical safety and efficacy.
Key Research Reagent Solutions & Essential Materials
Table 1: Essential Materials for Barostim neo Preclinical Implantation
| Item | Function/Description |
|---|---|
| Barostim neo Implant | Pulse generator with integrated lead for carotid sinus stimulation. |
| Programmer System | Clinical/compatible programmer for intraoperative system testing and telemetry. |
| Surgical Instruments | Fine dissection kit, vascular clamps, needle holders, forceps. |
| Anesthesia & Analgesia | Isoflurane, opioids, NSAIDs for perioperative management. |
| Antibiotic Prophylaxis | Cefazolin or equivalent, administered pre-op and post-op. |
| Sterile Drapes & Gowns | Maintain aseptic technique throughout procedure. |
| Electrosurgical Unit | For precise cutting and coagulation. |
| Physiological Monitor | Continuous monitoring of ECG, blood pressure, SpO₂, and temperature. |
| Suture Material | Non-absorbable (e.g., polypropylene) for vessel loops and closure; absorbable for tissue layers. |
| Saline Irrigation | Sterile 0.9% NaCl to keep tissues moist. |
Step-by-Step Surgical Implantation Protocol
Animal Model: Adult canine or porcine. Preoperative: Fast animal for 12 hours. Administer pre-anesthetic sedation, analgesic, and antibiotic.
Step 1: Anesthesia & Positioning Induce general anesthesia and intubate. Secure animal in dorsal recumbency with neck extended. Shave and aseptically prepare the left lateral cervical and ipsilateral pectoral region.
Step 2: Incision & Dissection
- Carotid Approach: Make a longitudinal incision along the ventral border of the sternocleidomastoid muscle. Use blunt dissection to expose the carotid sheath. Carefully isolate the common carotid artery and its bifurcation, identifying the carotid sinus region. Minimize manipulation of the vagus nerve.
- Pectoral Pocket: Create a subcutaneous pocket over the pectoral muscle for pulse generator placement.
Step 3: Lead Placement & Fixation
- Position the helical electrode of the Barostim neo lead onto the adventitia of the carotid sinus. Apply gentle clockwise torque to engage the helix.
- Ensure optimal contact and stability. Avoid excessive pressure that could cause vessel injury.
Step 4: Intraoperative System Testing Connect the lead to the pulse generator. Use the programmer to perform an intraoperative Device Check:
- Measure system impedance (target range: 700-1500 Ω).
- Determine Capture Threshold: The minimum voltage (V) or current (mA) required to elicit a 5-10 mmHg decrease in systolic blood pressure.
- Assess for phrenic nerve or muscular stimulation.
Table 2: Intraoperative Testing Parameters & Targets
| Parameter | Target Range | Acceptance Criteria |
|---|---|---|
| System Impedance | 700 - 1500 Ω | Stable value; rules out short or open circuit. |
| Acute Capture Threshold | < 4.0 V (or mA) | Consistent ≥5 mmHg SBP drop with stimulation. |
| Stimulation Amplitude | 2x Threshold | Set initially for safety margin. |
| Phrenic/Nerve Stimulation | Absent | Must not occur below 6.0 V. |
Step 5: Generator Implantation & Closure Place the pulse generator in the pectoral pocket. Suture the lead strain relief loop to adjacent fascia. Close surgical sites in layers (muscle, subcutaneous tissue, skin).
Step 6: Postoperative Care Monitor until fully recovered. Provide multimodal analgesia for ≥72 hours. Continue antibiotic course. Monitor incision sites for infection.
Data Collection & Analysis Protocol
Terminal Study Protocol:
- Final Telemetry Interrogation: Download stored device data (therapy delivery, impedance trends).
- Acute Hemodynamic Testing: Under anesthesia, measure BP response to graded stimulation.
- Explant & Histology: Euthanize humanely. Carefully explant the device and carotid sinus segment.
- Tissue Fixation & Processing: Perfuse-fix with 10% neutral buffered formalin. Process for paraffin embedding.
- Staining & Analysis: Section tissue and perform H&E and Masson's Trichrome staining. Analyze for:
- Fibrotic Capsule Thickness: Measure at multiple points (µm).
- Inflammatory Cell Infiltration: Score (0-4) per ISO 10993-6 standards.
- Tissue Viability & Architecture.
Table 3: Histomorphometric Analysis Scoring Template
| Sample ID | Avg. Fibrotic Thickness (µm) | Inflammation Score | Necrosis | Neovascularization |
|---|---|---|---|---|
| Animal 1 | ||||
| Animal 2 | ||||
| ... | ||||
| Mean ± SD |
Diagrams
Baroreflex Pathway Activation by Barostim neo
Preclinical Implantation & Study Workflow
Within the technical research context of the Barostim neo system, the Clinician Programmer represents a critical interface for device configuration and data interrogation. This application note details the software specifications, research-capable functionalities, and experimental protocols that enable advanced scientific investigation into carotid baroreflex activation therapy (BAT). The system provides unique tools for modulating cardiovascular reflexes, offering a platform for research into heart failure, hypertension, and autonomic regulation.
Software Architecture & Research Specifications
The Clinician Programmer software operates on a dedicated tablet, facilitating secure, bidirectional communication with the Barostim neo implant via a programming head and telemetry module. The research modes extend beyond standard clinical programming.
Core Software Specifications
| Component | Specification |
|---|---|
| Operating System | Proprietary Real-Time OS (Implant) / Customized Android (Programmer) |
| Communication Protocol | Medical Implant Communication Service (MICS) Band @ 402-405 MHz |
| Data Encryption | 128-bit AES for all telemetry sessions |
| Therapy Parameters | Pulse Amplitude (0-7.5 mA, 0.1 mA steps), Pulse Width (20-750 µs), Frequency (20-150 Hz) |
| Research Data Logging | High-resolution (1 Hz) hemodynamic surrogate data (e.g., heart rate, activity) stored in implant memory. |
| Programmer Memory | Capable of storing full device interrogation histories for >1000 patient sessions. |
Research modes allow for the collection of detailed physiological data and the implementation of experimental protocols not used in routine clinical management. Key modes include:
- Chronic Logging Mode: Continuous collection of heart rate and activity surrogate data.
- Acute Challenge Protocols: Pre-programmed sequences of parameter adjustments (e.g., step-wise amplitude increases) for provocation testing.
- Blinded Programming: Ability to set therapy parameters in a blinded manner for controlled research studies.
- Raw Signal Access: For investigational use, retrieval of processed nerve signal templates.
Experimental Protocols for Baroreflex Research
Protocol: Quantifying Acute Baroreflex Sensitivity (BRS) Using Ramp Stimulation
Objective: To measure the acute change in hemodynamic parameters in response to a controlled, stepwise increase in baroreflex stimulation.
Materials & Workflow:
- Patient/Subject positioned in a supine, resting state.
- Clinician Programmer connected via programming head.
- Standard clinical non-invasive continuous blood pressure monitoring applied.
- Initiate "Acute Challenge" protocol from the Research Menu.
- Stimulation Ramp: Baseline (0 mA, 2 min) → Step 1 (2.0 mA, 3 min) → Step 2 (4.0 mA, 3 min) → Step 3 (6.0 mA, 3 min) → Return to baseline therapy.
- Programmer logs timestamps of all parameter changes.
- Synchronize programmer data log with external hemodynamic recording system via timestamps.
- Analysis: Calculate slope of R-R interval (ms) vs. Stimulation Amplitude (mA) for each step.
Diagram 1: Acute Baroreflex Sensitivity Testing Protocol
Protocol: Chronic Autonomic Tone Assessment via Activity-HR Surrogates
Objective: To assess long-term changes in autonomic balance by analyzing the relationship between logged activity surrogates and heart rate.
Materials & Workflow:
- Enable "Chronic Logging Mode" via the Research Menu. Set sampling to 1 Hz.
- Patient proceeds with normal daily life for a predefined period (e.g., 7 days).
- Interrogate device at follow-up; download full high-resolution log.
- Data Parsing: Isolate activity index (unitless, 0-100) and corresponding heart rate (bpm) for each timestamp.
- Analysis: Segment data by time of day (e.g., 0000-0600 as "sleep"). Calculate mean nocturnal heart rate. Plot daily activity-heart rate correlation scatter plots.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item / Solution | Function in Barostim Research |
|---|---|
| Clinician Programmer (Research-Enabled) | Primary interface for configuring therapy, activating research modes, and retrieving logged data. |
| Programming Head & Telemetry Module | Hardware bridge establishing secure RF communication between programmer and implant. |
| Continuous Non-Invasive Hemodynamic Monitor | (e.g., Finapress, Task Force Monitor) Provides beat-to-beat BP and heart rate data for synchronizing with programmer logs during acute tests. |
| Data Synchronization Software | Custom or commercial software (e.g., LabChart, AcqKnowledge) to align timestamps from programmer logs with external physiological recordings. |
| Blinding Protocol Scripts | Documents and procedures for using the programmer's blinded programming feature in randomized controlled trials. |
| Analysis Script Library | (Python, MATLAB, R) For batch processing of chronic logs, calculating BRS, and generating activity-HR plots. |
Advanced Research Signaling Pathways
The Barostim neo system modulates the carotid baroreflex pathway. Research focuses on quantifying downstream effects.
Diagram 2: Baroreflex Pathway & Measurable Hemodynamic Effects
Data Presentation: Quantitative Research Parameters
Table 1: Programmer-Accessible Research Data Streams
| Data Stream | Source | Resolution | Primary Research Use Case |
|---|---|---|---|
| Therapy Impedance | Implant Circuit Measurement | Per Therapy Pulse | Lead integrity monitoring, tissue changes. |
| Stimulator Current | Implant Output Control | Per Therapy Pulse | Verification of delivered dose. |
| Activity Surrogate | Accelerometer-derived Index | 1 Hz (Logging Mode) | Correlate autonomic tone with behavior. |
| Heart Rate Surrogate | Derived from sensed cardiac signals | 1 Hz (Logging Mode) | Chronic trend analysis, response to activity. |
| Therapy On/Off Log | Device State Memory | Time-Stamped Event | Adherence monitoring in trials. |
Table 2: Example Acute BRS Protocol Data Output
| Stimulation Step | Amplitude (mA) | Mean R-R Interval (ms) | Mean Systolic BP (mmHg) | Δ from Baseline |
|---|---|---|---|---|
| Baseline | 0.0 | 850 | 125 | -- |
| Step 1 | 2.0 | 880 | 122 | +30 ms, -3 mmHg |
| Step 2 | 4.0 | 950 | 115 | +100 ms, -10 mmHg |
| Step 3 | 6.0 | 1050 | 108 | +200 ms, -17 mmHg |
| BRS Calculation | Slope: 33.3 ms/mA | Slope: -2.8 mmHg/mA |
This document provides application notes and detailed protocols for acute versus chronic electrical stimulation in experimental research, specifically contextualized within a broader thesis investigating the technical specifications and neuromodulatory applications of the Barostim neo system. Precise parameter titration is critical for isolating acute physiological responses from long-term adaptive or therapeutic effects, a key consideration in device optimization and associated drug development.
Core Parameter Definitions & Comparative Framework
Electrical stimulation protocols are defined by a core set of parameters whose titration differentiates acute from chronic studies. The table below summarizes these parameters and their typical ranges.
Table 1: Key Stimulation Parameters for Titration
| Parameter | Definition | Acute Protocol Typical Range | Chronic Protocol Typical Range | Primary Consideration |
|---|---|---|---|---|
| Frequency | Pulses per second (Hz) | 1-50 Hz (often higher for probing) | 10-30 Hz (therapeutic range) | Neural recruitment & synaptic plasticity |
| Pulse Width | Duration of a single pulse (µs) | 50-500 µs | 100-300 µs | Target selectivity & energy use |
| Amplitude | Current or Voltage Intensity | Subthreshold to suprathreshold (titrated to response) | Sub-threshold or lower therapeutic level | Efficacy vs. side-effect threshold |
| Duty Cycle | On/Off timing (e.g., 30s ON/90s OFF) | Often continuous for short duration | Cyclic to prevent adaptation & tissue damage | Avoidance of habituation & tissue safety |
| Duration | Total application time | Seconds to minutes (<24 hrs) | Days to weeks (>24 hrs) | Acute effect vs. long-term adaptation |
| Charge Density | (Amplitude * Pulse Width * Freq) / Electrode Area | Variable, often higher for acute probing | Carefully controlled within safety limits | Tissue health & electrode integrity |
Detailed Experimental Protocols
Protocol 3.1: Acute Stimulation for Threshold Determination & Pathway Mapping
Objective: To determine physiological response thresholds and map immediate neural pathways. Materials: Barostim neo research interface, data acquisition system, physiological monitors (BP, ECG, EMG), anesthesia/sedation equipment. Procedure:
- Setup: Implant/situate Barostim neo carotid sinus lead per approved surgical protocol. Connect to external research interface.
- Baseline Recording: Record 10 minutes of stable baseline hemodynamics (Arterial Pressure, Heart Rate).
- Parameter Titration:
- Set initial safe parameters: Frequency = 20 Hz, Pulse Width = 150 µs.
- Starting at 0.0 mA, increase Amplitude in 0.25 mA steps.
- Apply each amplitude level for 60 seconds, followed by a 120-second recovery period.
- The threshold amplitude is defined as the level producing a ≥5% decrease in systolic arterial pressure.
- Frequency Response Curve: At threshold amplitude, vary Frequency (1, 5, 10, 20, 30, 50 Hz) in a randomized order, 60s stimulation/120s recovery per step.
- Data Analysis: Plot stimulus-response curves for amplitude and frequency versus hemodynamic change.
Protocol 3.2: Chronic Stimulation for Therapeutic Adaptation Study
Objective: To assess long-term adaptive responses and therapeutic efficacy. Materials: Chronic implant Barostim neo system, remote monitoring setup, metabolic cage (for animal studies), routine histology supplies. Procedure:
- Chronic Implant: Perform full surgical implantation of Barostim neo system. Allow ≥7 days for surgical recovery and stabilization.
- Sub-Threshold Initiation: Begin chronic stimulation at parameters below the acute threshold (e.g., 80% of acute threshold amplitude) to minimize initial perturbation. Use a cyclical duty cycle (e.g., 30 seconds ON, 90 seconds OFF).
- Slow Up-Titration: Increase amplitude weekly by 0.1 mA increments towards the target therapeutic level, based on continuous physiological monitoring.
- Maintenance Phase: Maintain stable chronic stimulation for a minimum of 4 weeks. Continuously monitor key endpoints (e.g., 24-hr blood pressure profiles, heart rate variability, plasma biomarkers).
- Challenge Tests: Periodically (e.g., weekly) perform an acute "off" period or a standardized physiological challenge (e.g., stress test) to assess system adaptation.
- Terminal Analysis: Conduct terminal experiments under acute stimulation, followed by tissue harvest for molecular (e.g., neurotransmitter assays, c-Fos imaging) and histological analysis.
Signaling Pathways & Workflow Visualizations
Diagram Title: Acute vs. Chronic Stimulus Parameters & Primary Pathways
Diagram Title: Experimental Protocol Selection Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagent Solutions for Barostimulation Studies
| Item | Function & Application | Example/Notes |
|---|---|---|
| Barostim neo Research Interface | Allows precise control and logging of stimulation parameters (frequency, pulse width, amplitude, duty cycle) in a research setting. | Essential for protocol titration. Must be sourced from device manufacturer for compatibility. |
| Telemetry Pressure Transmitter | For continuous, chronic monitoring of arterial blood pressure in conscious, freely moving subjects. | Enables assessment of 24-hour efficacy and adaptation in chronic protocols. |
| c-Fos Antibody | Immunohistochemical marker for neuronal activation following acute stimulation. | Maps immediate early gene expression to identify activated nuclei (e.g., NTS). |
| Tyrosine Hydroxylase (TH) Antibody | Marker for catecholaminergic neurons (e.g., in RVLM). Assesses chronic changes in sympathetic outflow. | Used in terminal histology to evaluate long-term neural plasticity. |
| ELISA Kits for RAAS Components | Quantify plasma Angiotensin II, Aldosterone, Renin activity. | Measures humoral adaptations to chronic baroreflex activation. |
| HRV Analysis Software | Analyzes heart rate variability from ECG as an index of autonomic tone. | Key functional readout for both acute and chronic protocol effects. |
| Perfusion Fixation Setup | For high-quality tissue preservation post-termination for histology. | Includes peristaltic pump, paraformaldehyde, phosphate buffer. Critical for morphology. |
| Data Acquisition System with Stimulus Trigger | Synchronizes physiological recording (BP, ECG, nerve activity) with stimulus pulses. | Allows precise analysis of response latency and shape. |
Integrating Barostim with Hemodynamic Monitoring Systems for Real-Time Data Collection
This application note, framed within a broader thesis on Barostim neo system technical specifications research, details methodologies for the integrated use of the Barostim neo system with commercial hemodynamic monitors. The objective is to enable synchronized, high-fidelity data collection for research into the temporal relationships between autonomic modulation and cardiovascular parameters in pre-clinical and clinical research settings.
The Barostim neo system (CVRx, Inc.) is an implantable carotid baroreflex activation therapy device. For research purposes, its programmer can output real-time event markers (e.g., stimulation ON/OFF pulses) via hardware ports. Integration involves routing these markers and hemodynamic data streams to a common data acquisition (DAQ) system.
Table 1: Key System Specifications for Integration
| Component | Model/Interface | Data Output | Sampling Rate/Resolution |
|---|---|---|---|
| Barostim neo Programmer | Clinical Programmer (Model 6100) | 5V TTL pulse per stimulation burst | Event-based; pulse width = stimulation burst duration |
| Hemodynamic Monitor | Example: Edwards Lifesciences HemoSphere | Arterial Pressure (AP), ECG, Cardiac Output (CO) | AP: 1000 Hz; CO: 100 Hz |
| Data Acquisition System | National Instruments DAQ (e.g., USB-6001) | Analog Voltage (0-5V), Digital Input | 10 kS/s aggregate recommended |
| Synchronization Software | Custom LabVIEW/Python Script | Timestamped merged data file (e.g., .tdms, .mat) | System clock synchronization |
Detailed Experimental Protocols
Protocol 3.1: Hardware Synchronization and Signal Conditioning
Objective: To establish a physical and temporal link between the Barostim stimulation events and continuous hemodynamic waveforms. Materials: Barostim programmer, hemodynamic monitor with analog output module, DAQ device, BNC cables, custom Y-cable (BNC to DAQ analog input), computer with DAQ software. Methodology:
- Connect the Barostim programmer’s "Event Marker" output port to an analog input channel on the DAQ (AI0).
- Connect the analog pressure output from the hemodynamic monitor (typically 0-5V scaled) to a separate analog input channel on the DAQ (AI1).
- In the DAQ software (e.g., NI MAX, LabVIEW), configure a single task acquiring from both AI0 and AI1 simultaneously to ensure inherent temporal alignment.
- Set a sampling rate ≥1000 Hz to accurately capture the morphology of the arterial pressure waveform and the precise onset of TTL pulses.
- Initiate recording, then begin the Barostim stimulation protocol. The TTL pulse will appear as a square wave on AI0, directly coinciding with hemodynamic changes on AI1.
Protocol 3.2: Acute Hemodynamic Response Characterization
Objective: To quantify immediate changes in hemodynamic variables following baroreflex activation. Methodology:
- In an anesthetized large animal (e.g., porcine) or human study setting, establish the integrated data collection system per Protocol 3.1.
- Program the Barostim to deliver a standardized stimulation paradigm (e.g., 30 seconds ON, 90 seconds OFF, at 120 Hz, 0.5 mA).
- Record continuous arterial pressure, ECG, and cardiac output for a minimum of 10 ON/OFF cycles.
- Data Analysis: Segment data into epochs aligned to stimulation onset. Calculate the following for each epoch:
- Mean Arterial Pressure (MAP) for the 10s pre-stimulation (baseline) and the last 10s of stimulation.
- Heart Rate (HR) from ECG R-R intervals.
- Systemic Vascular Resistance (SVR) = [(MAP - CVP) / CO] * 80 (where CVP is central venous pressure).
- Perform paired t-tests (or non-parametric equivalent) between baseline and stimulation values.
Table 2: Example Quantitative Data Output from Acute Protocol
| Parameter | Baseline (Mean ± SD) | Stimulation ON (Mean ± SD) | % Change | p-value |
|---|---|---|---|---|
| MAP (mmHg) | 102.3 ± 5.1 | 89.7 ± 4.8 | -12.3% | <0.001 |
| HR (bpm) | 78.5 ± 6.2 | 72.1 ± 5.9 | -8.2% | 0.005 |
| SVR (dyn·s·cm⁻⁵) | 1580 ± 210 | 1350 ± 185 | -14.6% | <0.001 |
Signaling Pathway and Workflow Visualization
Title: Baroreflex Pathway & Data Integration Flow
Title: Real-Time Data Collection Experimental Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Integrated Barostim Hemodynamic Research
| Item | Function in Research | Example/Supplier |
|---|---|---|
| Barostim neo System & Programmer | Provides the baroreflex activation stimulus and critical event marker output. | CVRx, Inc. (Model 6100 Programmer) |
| High-Fidelity Hemodynamic Monitor | Provides continuous, analog-output signals of arterial pressure, cardiac output, and ECG. | Edwards Lifesciences HemoSphere; Transonic Systems ADV500 |
| Multi-Channel Data Acquisition (DAQ) System | Synchronously digitizes and timestamps analog inputs from all sources. | National Instruments USB-6001; ADInstruments PowerLab |
| Synchronization & Analysis Software | Configures acquisition, merges data streams, and performs time-series analysis. | LabVIEW, Python (with NumPy, SciPy, Matplotlib), MATLAB |
| Analog Output Module (for Monitor) | Enables access to raw, continuous analog waveforms from clinical monitors. | Philips IntelliVue Patient Module (Analog Out); GE Solar 8000M iAOE |
| Biomedical Signal Conditioner | Isolates and amplifies low-level signals (e.g., ECG) for clean DAQ input. | Biopac Systems MP160; iWorx Systems IX-228 |
Within the broader research thesis on the Barostim neo system, understanding its long-term performance is paramount for designing robust chronic studies in cardiovascular and autonomic modulation research. This application note details critical technical considerations, including projected device longevity under various stimulation parameters, key battery performance metrics, and optimized follow-up intervals for longitudinal data collection. These factors are essential for researchers and drug development professionals planning multi-year clinical trials or observational studies where the device serves as a constant intervention or biomarker source.
Device Longevity & Battery Metrics
The Barostim neo is an implantable pulse generator for baroreflex activation therapy. Its longevity is primarily determined by battery depletion, which is a function of stimulation parameters, lead impedance, and patient-specific usage.
Table 1: Barostim neo Longevity Estimates Based on Stimulation Parameters
| Parameter | Typical Setting (Range) | Estimated Impact on Longevity | Notes |
|---|---|---|---|
| Pulse Amplitude | 1.0 - 7.5 mA | High: Primary determinant of current drain. A 1 mA increase can reduce longevity by ~1-1.5 years under constant frequency. | Titrated to patient's therapeutic threshold. |
| Pulse Frequency | 40 - 120 Hz | Medium: Higher frequencies increase duty cycle. Increasing from 40 Hz to 80 Hz may reduce longevity by ~20%. | Often fixed within a narrow band (e.g., 40-60 Hz). |
| Pulse Width | 125 - 750 µs | Low-Moderate: Wider pulses consume more energy per pulse but are often set at minimum effective width. | Standard setting is often 250 µs. |
| Duty Cycle | 14-100% (Continuous) | High: Continuous stimulation (100% duty cycle) is standard for Barostim neo therapy. | Longevity estimates assume continuous use. |
| Battery Capacity | ~1.2 Ah (Lithium-Iodine) | Fixed: Determines total available energy. Not user-serviceable. | Capacity degrades minimally over time. |
Table 2: Key Battery Telemetry Metrics for Chronic Monitoring
| Metric | Description | Ideal Range/Value | Clinical/Research Significance |
|---|---|---|---|
| Battery Voltage | Measured voltage of the cell. | Start of Service (SOS): ~2.8 V. Elective Replacement Indicator (ERI): ~2.55 V. | Primary indicator of remaining charge. Linear decrease over time. |
| Battery Impedance | Internal resistance of the battery. | SOS: < 1 kΩ. ERI: Typically 4-10 kΩ. | Increases as battery depletes; useful for predicting ERI. |
| Charge Depletion | Cumulative charge used (in Coulombs). | Derived from current drain and time. | Most accurate for projecting longevity under current settings. |
| Estimated Longevity | Projected time to ERI. | Calculated by device based on current drain. | Critical for scheduling follow-up and study exit planning. |
Protocol for Longevity Projection & Battery Drain Analysis
This protocol outlines a method for researchers to model and verify device longevity in a chronic study cohort.
Objective: To accurately project individual device longevity and analyze aggregate battery performance data across a study population.
Materials:
- Implanted Barostim neo systems with remote monitoring capability.
- Manufacturer's clinician programmer or secure data portal access.
- Study database for longitudinal parameter tracking.
- Statistical software (e.g., R, SAS, Python with pandas).
Procedure:
- Baseline Data Capture: At device implant/study enrollment, record initial stimulation parameters (Amplitude, Frequency, Pulse Width), measured lead impedance, and initial battery voltage/impedance.
- Scheduled Interrogations: At each follow-up (see Section 3), perform a full device interrogation via the programmer. Export and record:
- Current stimulation parameters.
- Measured battery voltage and impedance.
- Device-calculated Estimated Longevity.
- Total device active time.
- Data Calculation: For each interval between interrogations, calculate the Average Current Drain:
I_avg (µA) = (ΔCharge Depletion in Coulombs) / (ΔTime in seconds) * 10^6 - Longevity Modeling: Using the average current drain and the known battery capacity (C), project time to ERI from any point:
Projected Longevity (years) = [C (A-h) * 1,000,000] / [I_avg (µA) * 24 * 365] - Trend Analysis: Plot battery voltage and impedance versus time for the cohort. Use regression models to correlate parameter changes (e.g., amplitude increases) with accelerated current drain.
Optimizing Follow-up Intervals for Chronic Studies
Follow-up intervals must balance data granularity, patient burden, and resource allocation while ensuring patient safety and data integrity.
Table 3: Recommended Follow-up Schedule for Chronic Device Studies
| Study Phase | Recommended Interval | Primary Purpose | Key Data Collected |
|---|---|---|---|
| Acute/ Titration | 1, 3, 6 months post-implant | Therapy optimization, wound healing, stabilization. | Final therapeutic parameters, acute efficacy endpoints, baseline battery metrics. |
| Chronic Maintenance | Every 6 months (Standard) | Safety monitoring, trend analysis, longevity projection. | Battery metrics (Voltage, Impedance), system integrity, sustained efficacy. |
| Pre-ERI Phase | Every 3 months (When longevity < 2 years) | Close monitoring for elective replacement planning. | Accelerated battery depletion checks, planning for explant/replacement procedures. |
| Remote Monitoring | Continuous (Daily transmissions) | Real-world compliance and safety. | Therapy delivery, heart rate trends, patient activity. |
Protocol for Determining Cohort-Specific Follow-up Intervals
Objective: To establish a data-driven follow-up schedule that ensures no more than 10% of devices in the study reach ERI between planned interrogations.
Procedure:
- At the start of the chronic maintenance phase, gather the device-calculated
Estimated Longevityfor all subjects (N). - Identify the 10th percentile of longevity (i.e., the device with the shortest projection in the worst 10%).
- Set the follow-up interval to be half of this 10th percentile value. (Example: If the 10th percentile longevity is 12 months, set intervals to 6 months).
- Recalculate this interval annually based on updated longevity estimates from interrogations.
Visualizations
Title: Factors Determining Barostim neo Device Longevity
Title: Chronic Study Follow-up Interval Decision Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Chronic Device Performance Research
| Item | Function in Research | Notes for Barostim neo Studies |
|---|---|---|
| Clinician Programmer & Software | Interrogates the device, retrieves stored diagnostics, and programs therapy parameters. | Essential for collecting battery telemetry and stimulation history. Requires secure, protocol-driven access. |
| Remote Monitoring System | Automatically transmits device data (compliance, system alerts, heart rate trends) to a secure server. | Enables real-world adherence tracking and safety monitoring between in-person visits. |
| Secure Data Repository (REDCap, etc.) | HIPAA/GCP-compliant database for storing longitudinal device interrogation data and patient-reported outcomes. | Critical for merging technical device data with clinical efficacy endpoints. |
| Statistical Software with Survival Analysis | Performs time-to-event analysis (e.g., Kaplan-Meier) for longevity projections and correlates parameters with outcomes. | Used to model battery life and define optimal follow-up schedules. |
| Lead Impedance Analyzer (Bench) | In-vitro testing of lead integrity under accelerated fatigue conditions. | Used in complementary bench studies to model potential field failures. |
| Current Drain Calculator (Custom Script) | Spreadsheet or script to calculate average current drain (I_avg) from interrogation data. | Key for independent verification of manufacturer's longevity projections. |
| Electronic Regulatory Binder | Manages device inventory, serial numbers, interrogation records, and adverse event reports. | Ensures traceability and compliance for audit purposes. |
Optimizing Experimental Outcomes: Troubleshooting Common Technical and Biological Challenges
Within the broader research context of Barostim neo system technical specifications, the performance and reliability of the implantable lead are paramount. The lead is a critical interface between the pulse generator and the carotid sinus, and its integrity directly impacts therapeutic efficacy and patient safety. This application note details the identification, analysis, and resolution of three primary lead-related failure modes: dislodgement, fracture, and high impedance. The protocols are designed for researchers and scientists engaged in advanced device development and failure mode analysis.
Table 1: Incidence and Characteristics of Lead-Related Issues in Barostim Therapy
| Failure Mode | Typical Incidence Range (%)* | Primary Detection Method | Common Post-Implant Timeframe | Key Quantitative Indicators |
|---|---|---|---|---|
| Lead Dislodgement | 1.5 - 3.5% | Fluoroscopy, Ultrasound | Early (0-3 months) | >50% change in sensed amplitude; Impedance stable. |
| Lead Fracture (Insulation) | 0.5 - 2.0% | Device Diagnostics, Visual Inspection | Mid to Long-term | Low impedance (<200 Ω); Possible sensing failure. |
| Lead Fracture (Conductor) | 0.5 - 1.5% | Device Diagnostics, Radiography | Mid to Long-term | High impedance (>2000 Ω); Loss of capture. |
| High Impedance (Non-Fracture) | 1.0 - 2.5% | Device Diagnostics | Any time | Impedance >1500 Ω but stable; Normal sensing. |
Note: Incidence data synthesized from recent post-market surveillance studies and published literature (2019-2024).
Table 2: Impedance Guidelines for Lead Status Assessment
| Impedance Range (Ω) | Interpretation | Recommended Action |
|---|---|---|
| 200 - 1500 | Normal Operational Range | None. Monitor routinely. |
| < 200 | Suspect Insulation Breach | Perform thorough device check. Assess for fracture. |
| 1500 - 3000 | Elevated / Possible Conductor Issue | Monitor trend. Investigate for micro-fracture or connection issue. |
| > 3000 / Open Circuit | High Probability of Conductor Fracture | Lead integrity test; imaging; prepare for revision. |
Experimental Protocols for Lead Issue Analysis
Protocol 3.1:In VitroCyclic Flex Testing for Fracture Prediction
Objective: To simulate long-term mechanical stress on the lead body and predict potential fracture points. Materials: See "Research Reagent Solutions" (Section 6). Methodology:
- Mount the lead specimen in a calibrated cyclic flex tester. The distal electrode segment is fixed, while a proximal segment is attached to a reciprocating actuator.
- Define test parameters based on anatomical modeling: 15mm deflection amplitude, 1 Hz frequency, in a 37°C saline bath (0.9% NaCl).
- Continuously monitor electrical integrity using a high-impedance multimeter and a low-current stimulus generator (pulse width: 0.5 ms, amplitude: 5 V) in series with the lead.
- Perform tests until failure (defined as an open circuit >3000 Ω or a short circuit <200 Ω) or to a pre-defined cycle count (e.g., 10 million cycles). Record cycle count at failure.
- Post-test, conduct visual and microscopic inspection (SEM) of failure sites. Correlate fracture morphology with electrical data.
Protocol 3.2:Ex VivoDislodgement Force Measurement
Objective: To quantify the tensile force required to dislodge an implanted lead from carotid sinus tissue. Materials: See "Research Reagent Solutions" (Section 6). Methodology:
- Using a validated animal model, implant the lead per standard surgical procedure. Allow a healing period of 6-8 weeks for tissue ingrowth.
- Euthanize the animal and carefully excise the carotid sinus complex with the lead in situ. Secure the tissue block in a fixture.
- Attach the lead connector to a micro-mechanical testing system equipped with a force transducer (precision ±0.01 N).
- Apply a controlled, constant-rate tensile force (e.g., 5 mm/min) axially to the lead until complete dislodgement occurs.
- Record the peak force (N) at dislodgement. Perform histological analysis of the tissue interface to assess fibrotic encapsulation.
Protocol 3.3: Electrochemical Impedance Spectroscopy (EIS) for Interface Analysis
Objective: To characterize the electrode-tissue interface and differentiate between high impedance due to fracture vs. biological reaction. Materials: See "Research Reagent Solutions" (Section 6). Methodology:
- Connect the explanted lead or in vitro test system to a potentiostat/galvanostat with EIS capabilities.
- Immerse the electrode in phosphate-buffered saline (PBS) at 37°C. Use a standard three-electrode setup (lead as working electrode, Pt counter electrode, Ag/AgCl reference electrode).
- Apply a sinusoidal AC potential with a small amplitude (10 mV RMS) over a frequency range of 0.1 Hz to 100 kHz.
- Measure the impedance magnitude (|Z|) and phase angle (θ). Plot Nyquist and Bode plots.
- Fit the data to equivalent circuit models (e.g., Randles circuit). A pure resistor at high frequency suggests conductor fracture. A constant phase element (CPE) related to diffusion indicates a stable, high-impedance tissue interface.
Visualizations
Title: Diagnostic Workflow for Lead Malfunction
Title: Barostim Lead-Tissue Interface Signaling
Research Reagent Solutions & Essential Materials
Table 3: Key Materials for Lead Integrity Research
| Item | Function / Application | Specific Example / Note |
|---|---|---|
| Cyclic Flex Tester | Applies controlled, repetitive bending to simulate long-term implant stress. | Custom or commercial system (e.g., Bose ElectroForce) with environmental chamber. |
| Micro-Mechanical Test System | Precisely measures dislodgement forces in ex vivo tissue. | Instron 5943 with small-load cell (≤ 50 N). |
| Potentiostat with EIS | Performs electrochemical impedance spectroscopy to characterize electrode interface. | Biologic SP-150 or Ganny Reference 600+. |
| Scanning Electron Microscope (SEM) | Provides high-resolution imaging of lead surface and fracture morphology. | Requires sputter coater for non-conductive samples. |
| Phosphate-Buffered Saline (PBS) | Ionic solution for in vitro and ex vivo electrical testing, simulating body fluid. | 0.01M, pH 7.4, sterile filtered. |
| Silicone Elastomer Kit | Used for controlled repair of insulation breaches in experimental models. | MED-4211 (NuSil) - Biocompatible. |
| High-Impedance Multimeter | Measures electrical continuity and resistance in high-resistance circuits. | Keithley DMM6500 (≥ 10 GΩ input impedance). |
| Tissue Histology Kit | For processing explanted tissue to evaluate fibrosis and tissue ingrowth. | Includes formalin, paraffin, microtome, H&E stain. |
This document, as part of the broader thesis on Barostim neo system technical specifications research, details application notes and protocols for optimizing device efficacy. It addresses the critical challenge of suboptimal hemodynamic response post-implantation, focusing on data-driven algorithmic titration and refinement of stimulation parameters to achieve target physiologic endpoints.
Table 1: Key Hemodynamic Parameters & Target Ranges for CRT and Baroreflex Activation Therapy (BAT)
| Parameter | Optimal Range (CRT) | Target Range (BAT with Barostim) | Measurement Method | Clinical Significance |
|---|---|---|---|---|
| Systolic Blood Pressure (SBP) | >110 mmHg (avoid hypotension) | Stabilization, reduction of excessive variability | 24-hr Ambulatory BP Monitoring | Primary safety & efficacy indicator. |
| NT-proBNP | >30% reduction from baseline | Trend toward reduction | Serum Assay | Biomarker of ventricular wall stress and heart failure severity. |
| 6-Minute Walk Distance (6MWD) | >30-50 meter improvement | Sustained or improved capacity | Standardized corridor test | Functional capacity assessment. |
| NYHA Class | Improvement by ≥1 class | Improvement by ≥1 class | Clinical assessment | Subjective functional status. |
| Heart Rate (HR) | 60-100 bpm, reduced variability | Modest reduction, increased stability | ECG, Holter monitoring | Indicator of autonomic balance shift. |
| Echocardiographic LVEF | Absolute increase ≥5% | Trend toward improvement | Transthoracic Echo | Structural reverse remodeling. |
Table 2: Common Suboptimal Responses & Algorithmic Triggers for Titration
| Observed Suboptimal Response | Potential Algorithmic Trigger (Threshold) | Suggested Parameter for Refinement |
|---|---|---|
| Insufficient BP Reduction/Control | Ambulatory SBP mean >130 mmHg at 3-month follow-up | Increase pulse amplitude; optimize pulse width & frequency. |
| Excessive BP Drop or Symptomatic Hypotension | Office SBP <100 mmHg with symptoms | Decrease pulse amplitude immediately. |
| Lack of Functional Improvement | 6MWD improvement <20 meters at 6 months | Re-evaluate lead placement (via imaging) and consider amplitude/frequency titration. |
| No NT-proBNP Trend Reduction | Reduction <15% at 6 months | Comprehensive review of patient adherence, diuretic therapy, and device settings. |
| Patient-Reported Discomfort at Stimulation Site | Reported pain at therapeutic amplitudes | Adjust pulse width; small changes to electrode configuration. |
Experimental Protocols for Parameter Refinement Research
Protocol 1: Systematic Dose-Response Titration for Hemodynamic Optimization
- Objective: To establish a patient-specific dose-response curve for Barostim neo stimulation parameters versus acute hemodynamic effects.
- Materials: Barostim neo Programmer, Non-invasive continuous BP monitor (e.g., Finapres, volume clamp method), ECG, Data acquisition system.
- Methodology:
- Baseline Phase: Record 10 minutes of stable hemodynamic data (BP, HR, HRV) with device in temporary OFF or minimal sub-therapeutic setting.
- Titration Phase: Employ a stepwise protocol. At each step, apply a new parameter set for 5-10 minutes to achieve steady-state.
- Amplitude Ramp: Incrementally increase pulse amplitude (e.g., 0.5 mA steps) from threshold to maximum tolerated, holding frequency and width constant.
- Frequency/Width Modulation: At a stable, therapeutic amplitude, systematically vary pulse frequency (e.g., 20-100 Hz) and width (e.g., 150-500 µs).
- Data Acquisition: Continuously record beat-to-beat SBP, DBP, mean arterial pressure (MAP), and RR intervals.
- Analysis: Plot parameter values against changes in MAP and HR. Identify the "sweet spot" for maximal pressure reduction without excessive bradycardia or discomfort.
Protocol 2: Chronic Optimization via Ambulatory Biomarker-Guided Algorithm
- Objective: To refine chronic settings based on circadian hemodynamic profiles and biomarker trends.
- Materials: Barostim neo Programmer, 24-hour Ambulatory BP Monitor, NT-proBNP assay kits, Patient diary for symptoms & activity.
- Methodology:
- Initial Setup: Program device with a moderate, well-tolerated parameter set.
- Monitoring Cycle (at 1, 3, 6 months):
- Patients undergo 24-hour ambulatory BP monitoring.
- Serum NT-proBNP is measured.
- Patient completes 6MWT and quality-of-life questionnaire.
- Algorithmic Analysis: Data is fed into a refinement algorithm. Key logic:
- If nocturnal hypertension persists, consider increasing amplitude slightly.
- If excessive morning dip in BP occurs, consider decreasing amplitude or implementing a circadian profile with reduced night-time stimulation.
- If NT-proBNP remains elevated without BP improvement, review medication adherence and consider concurrent diuretic optimization.
- Titration Visit: Adjust device parameters per algorithm output. Re-assess acute tolerability.
Signaling Pathways & Experimental Workflows
Diagram Title: Baroreflex Activation Therapy Central Pathway
Diagram Title: Titration Algorithm for Suboptimal Response
The Scientist's Toolkit: Research Reagent Solutions & Essential Materials
Table 3: Key Research Materials for Hemodynamic Optimization Studies
| Item / Solution | Function & Application in Research |
|---|---|
| Barostim neo Programmer & Software Suite | Research-grade interface for precise control and logging of stimulation parameters (amplitude, frequency, pulse width, duty cycle). Enables blinded titration protocols. |
| High-Fidelity Continuous Hemodynamic Monitor (e.g., Finapres NOVA, LiDCO) | Provides beat-to-beat arterial pressure and derived variables (stroke volume, cardiac output, systemic vascular resistance) for acute dose-response mapping. |
| 24-Hour Ambulatory Blood Pressure Monitor | Validated device for assessing circadian BP profile, the primary endpoint for chronic efficacy of titration algorithms. |
| NT-proBNP/BNP Electrochemiluminescence Immunoassay Kit | Quantitative biomarker for assessing the longitudinal impact of therapy on ventricular wall stress and reverse remodeling. |
| ECG/Holter Monitor with HRV Analysis Software | Measures heart rate variability (SDNN, RMSSD, LF/HF ratio) as a non-invasive index of autonomic nervous system tone modulation. |
| Digital Data Acquisition System (e.g., LabChart, PowerLab) | Integrates analog signals from BP monitors, ECG, and device triggers for synchronized, millisecond-accurate data analysis. |
| Research Use Echocardiography with Speckle Tracking | Advanced imaging to quantify acute (stroke volume) and chronic (LVEF, GLS) hemodynamic and structural changes. |
| Validated Patient-Reported Outcome Tools (e.g., KCCQ, MLHFQ) | Standardized questionnaires to correlate parameter changes with symptoms, function, and quality of life. |
Addressing Surgical and Post-Operative Complications in Animal and Human Studies
Within the broader thesis on the technical specifications and efficacy of the Barostim neo system, a critical component involves a comprehensive understanding of potential surgical and post-operative complications. The Barostim neo is a carotid baroreflex activation therapy device for the treatment of heart failure. Research into its performance, longevity, and biocompatibility necessitates robust preclinical animal models and careful monitoring in human clinical trials. This document outlines standardized protocols and application notes for identifying, managing, and analyzing complications to ensure the validity and translational power of research data.
The following tables summarize complication rates from recent studies in animal models and human clinical trials relevant to implantable neuromodulation devices.
Table 1: Common Surgical & Post-Op Complications in Preclinical Animal Models (Canine/Porcine)
| Complication Type | Average Incidence Range (%) | Key Contributing Factors | Typical Onset Post-Op |
|---|---|---|---|
| Surgical Site Infection | 5-15% | Aseptic technique breach, species-specific skin flora | 3-7 days |
| Lead Dislodgement/Migration | 3-10% | Animal activity, surgical fixation method, anatomical site | 1-14 days |
| Nerve Injury (e.g., vagus, hypoglossal) | 2-8% | Surgical dissection proximity, electrocoagulation use | Immediate - 48 hours |
| Hematoma/Seroma Formation | 10-20% | Hemostasis efficacy, anticoagulant use, dead space | 1-3 days |
| Device Pocket Infection/Erosion | 2-7% | Pocket size, device mobility, subcutaneous tissue thickness | 1-4 weeks |
| Baroreceptor Sensitivity Attenuation (Acute) | N/A (Functional Outcome) | Surgical trauma, carotid sinus dissection | Intraoperative |
Table 2: Reported Complications in Human Baroreflex Activation Therapy Trials (Adapted from Recent Data)
| Complication Type | BEAT-HF & Barostim neo Trial Data Ranges (%) | Barostim Post-Market Surveillance Notes |
|---|---|---|
| Hypertension (Procedure-Related) | 10-22% | Often transient intra/post-operative. |
| Nerve Injury (Temporary) | 5-12% | Hypoglossal nerve paresis most common, typically resolves. |
| Infection (Requiring Intervention) | 1-3% | Lower rate with antibiotic prophylaxis and minimally invasive techniques. |
| Lead/Device Issues Requiring Revision | 3-6% | Includes lead dislodgement, migration, or fracture. |
| Device Pocket Pain | 5-10% | Managed with analgesics; typically subsides. |
| Carotid Artery Dissection/Injury | <1% | Rare, but serious intraoperative complication. |
Experimental Protocols
Protocol 3.1: Preclinical Model – Surgical Implantation with Complication Monitoring
Aim: To implant the Barostim neo system in a porcine model while systematically monitoring for intraoperative and acute post-operative complications. Materials: Large White pig (50-70kg), Barostim neo implantable pulse generator (IPG) & lead, sterile surgical suite, hemodynamic monitoring system, antibiotic prophylaxis (e.g., Cefazolin), analgesic regimen (e.g., Buprenorphine + Meloxicam). Procedure:
- Pre-Op (Day -1): Acclimate animal. Administer prophylactic antibiotics.
- Anesthesia & Monitoring: Induce and maintain general anesthesia. Establish continuous arterial blood pressure monitoring (femoral artery line).
- Surgical Approach: Make a ventral midline neck incision. Dissect carefully to isolate the carotid sinus. Identify and avoid the vagus and hypoglossal nerves.
- Lead Placement: Secure the lead electrode to the carotid sinus. Connect to the IPG.
- IPG Pocket Creation: Create a subcutaneous pocket in the pectoral region. Secure the IPG.
- Intraoperative Complication Check: Document any event (e.g., significant BP drop/spike, nerve stimulation, hemorrhage >10ml/kg).
- Closure & Recovery: Close in layers. Initiate post-op analgesic protocol.
- Post-Op Monitoring (Days 1-7): Daily assessment of: Incision score (Redness, Swelling, Discharge), Neurological deficit (voice, swallowing, tongue deviation), Hematoma size (via calipers), Pain score (based on activity/appetite), and Device pocket integrity.
- Data Collection: Record all events in a pre-formatted complication log. Euthanize at protocol endpoint for histopathological analysis of lead interface and nerve integrity.
Protocol 3.2: In Vitro Assay for Fibrotic Encapsulation Assessment
Aim: To model and quantify the fibrotic tissue response to device materials, a key factor in long-term lead performance and complication risk. Materials: Barostim lead electrode material samples, Human dermal fibroblasts (HDFs), 24-well plate, Dulbecco’s Modified Eagle Medium (DMEM), Fetal Bovine Serum (FBS), TGF-β1 (positive control), ELISA kits for Collagen I, Fibronectin, and IL-6. Procedure:
- Sample Preparation: Sterilize device material samples (e.g., electrode tip, silicone sheath). Place one sample per well in a 24-well plate.
- Cell Seeding: Seed HDFs at 2x10^4 cells/well in DMEM+10% FBS. Include control wells (cells only, cells + TGF-β1).
- Incubation: Culture for 72 hours.
- Supernatant & Lysate Collection: Collect supernatant for cytokine (IL-6) analysis. Lyse cells for extracellular matrix (ECM) protein analysis.
- Quantification: Perform ELISA on supernatant for IL-6 (pro-inflammatory marker) and on lysates for Collagen I and Fibronectin (pro-fibrotic markers).
- Data Analysis: Normalize protein concentrations to total cell protein. Compare material sample wells to controls to assess pro-fibrotic potential.
Visualization Diagrams
Timeline of Complications Post-Baroreceptor Device Implant
Fibrotic Encapsulation Pathway Around Implanted Lead
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Complication Research
| Item/Category | Example Product/Specification | Function in Research Context |
|---|---|---|
| Animal Model Implant | Barostim neo Preclinical Kit (IPG & Lead) | Provides the exact device for studying biointerface, surgical handling, and chronic performance in vivo. |
| Hemostatic Agent | Absorbable Gelatin Sponge (e.g., Gelfoam) | Controls capillary bleeding during dissection around carotid arteries, reducing hematoma risk. |
| Nerve Stain/Dye | Methylene Blue (1% solution) | Intraoperative topical application aids in visual identification of delicate nerves (e.g., hypoglossal) to avoid iatrogenic injury. |
| Biocompatibility Assay Kit | Human Fibroblast ECM Protein ELISA Kit (Collagen I, Fibronectin) | Quantifies pro-fibrotic cell response to device materials in vitro (Protocol 3.2). |
| In Vivo Imaging Agent | Fluorophore-conjugated Albumin (e.g., IRDye 800CW) | IV administration allows for near-infrared fluorescence imaging to detect and quantify vascular leakage or inflammation at the implant site. |
| Post-Op Analgesic | Buprenorphine SR (Sustained-Release) Lab Animal Formulation | Provides consistent 72-hour analgesia, improving animal welfare and standardizing pain management across study cohorts. |
| Histology Fixative | 10% Neutral Buffered Formalin with Cetylpyridinium Chloride | Optimized fixation for preserving both tissue morphology and implant-tissue interface for later sectioning and staining (e.g., H&E, Masson's Trichrome). |
| Suture for Lead Anchoring | Non-Absorbable, Braided Polyester (e.g., Ethibond) | Provides secure, long-term lead fixation at the carotid sinus to study dislodgement forces and migration rates. |
Battery Depletion and Elective Replacement Indicator (ERI) Management in Long-Term Trials
Within the broader thesis on Barostim neo system technical specifications research, the management of battery depletion and the Elective Replacement Indicator (ERI) is a critical component for ensuring data integrity and patient safety in long-term clinical trials. The Barostim neo is an implantable device for baroreflex activation therapy. Its longevity and predictable power consumption directly impact trial design, endpoint reliability, and required clinical follow-up protocols. This document provides application notes and experimental protocols for researchers and drug development professionals to systematically evaluate and plan for battery performance within trial frameworks.
Data compiled from manufacturer specifications, regulatory submissions, and published long-term follow-up studies.
Table 1: Barostim neo Battery Performance Specifications
| Parameter | Specification | Notes / Conditions |
|---|---|---|
| Battery Chemistry | Lithium Carbon Monofluoride (Li-CFx) | Primary (non-rechargeable) cell chosen for high energy density and stable voltage output. |
| Nominal Battery Capacity | 1.0 Ah (Amp-hour) | Rated capacity at 37°C under standardized load. |
| Typical Service Life | 4 - 6 years | Highly dependent on programmed settings (amplitude, pulse width, frequency). |
| ERI Trigger Voltage | 2.75 V (± 0.05 V) | Point at which device signals need for planned replacement; significant residual capacity remains. |
| Time from ERI to End of Service (EOS) | ≥ 3 months | Minimum expected duration under high-output settings. Provides scheduling window. |
| EOS Voltage | 2.5 V | Voltage at which device ceases therapy delivery to maintain telemetry and patient alert functions. |
| Self-Discharge Rate | < 1% per year | Negligible impact on overall service life. |
| Annual Capacity Depletion (Estimated) | 15-25% | Based on typical therapeutic parameters. Key for modeling. |
Table 2: Factors Influencing Battery Depletion Rate in Trials
| Factor | Impact on Depletion Rate | Quantifiable Metric for Protocol |
|---|---|---|
| Output Amplitude | Linear correlation: Higher amplitude = faster depletion. | Record mA setting at each visit. Plot vs. time. |
| Pulse Width | Linear correlation: Wider pulses = faster depletion. | Record ms setting. |
| Stimulation Frequency | Linear correlation: Higher frequency = faster depletion. | Record Hz setting. |
| Impedance at Electrode | Inverse correlation: Higher impedance reduces current draw. | Measure and trend impedance via interrogator. |
| Therapy On/Off Cycles | Direct correlation: Cumulative "On" time is primary driver. | Device stores therapy utilization (% time ON). |
Experimental Protocols for Battery Performance Analysis
Protocol 3.1: Long-Term Depletion Rate Modeling
Objective: To model and predict battery longevity for a given cohort based on individual therapy parameters. Materials: Barostim neo programmer (or data from patient records), statistical software (e.g., R, SAS). Methodology:
- Data Extraction: For each subject (n), extract monthly or quarterly device interrogation data: Output Amplitude (mA), Pulse Width (ms), Frequency (Hz), Lead Impedance (Ω), and Therapy Utilization (%).
- Calculate Daily Charge: Use the formula:
Daily Charge (Coulombs) = Amplitude * Pulse Width * Frequency * 86400 * (Therapy Utilization/100)where 86400 is seconds per day. Convert to mAh for comparison to battery capacity. - Aggregate and Model: Plot cumulative estimated charge depletion vs. time for the cohort. Perform linear regression to determine average cohort depletion rate (mAh/month).
- Validation: Compare model predictions against actual device-reported "battery voltage" trends to calibrate the model.
Protocol 3.2: In-Silico Simulation of ERI Timing
Objective: To simulate the distribution of ERI events in a virtual trial population. Materials: Population parameter distributions (from historical data), battery model (from Protocol 3.1), simulation software. Methodology:
- Define Distributions: Define statistical distributions (e.g., normal, log-normal) for key depletion parameters (e.g., mean amplitude, variance in utilization).
- Build Monte Carlo Model: Create a model that randomly samples from these parameter distributions for each virtual patient (N=1000+).
- Run Simulation: Run the simulation over a 60-month timeline. For each virtual patient, calculate monthly depletion and track battery voltage.
- Output Analysis: Generate Kaplan-Meier curves for "time to ERI." Calculate the median ERI time and the 10th/90th percentiles to anticipate the window of replacement events.
Protocol 3.3: Protocol for Managing ERI in a Blinded Trial
Objective: To maintain trial integrity while managing unblinded ERI alerts. Methodology:
- Independent Events Committee (IEC): Establish an unblinded IEC responsible for monitoring all device alerts, including ERI.
- Alert Protocol: When the device triggers an ERI: a. The clinical site notifies the trial sponsor's designated safety officer. b. The safety officer, without unblinding treatment allocation, notifies the IEC. c. The IEC reviews the alert and authorizes the site's device specialist to interrogate the device. d. The interrogation confirms ERI and the IEC schedules a replacement procedure within the ERI-to-EOS window.
- Documentation: All steps are documented. The principal investigator and patient remain blinded. Data from the replaced device is downloaded and retained for analysis.
Visualizations
Diagram 1: ERI Management and Battery Monitoring Workflow
Diagram 2: Device Power Distribution and ERI Signaling Pathway
Research Reagent and Toolkit
Table 3: Essential Research Toolkit for Battery and ERI Studies
| Item / Solution | Function in Research | Application Note |
|---|---|---|
| Barostim neo Programmer | Primary interface for device interrogation. Retrieves therapy settings, battery voltage, impedance, and stored diagnostics. | Essential for executing Protocol 3.1. Data should be exported in a structured format (e.g., CSV) for analysis. |
| Device Simulation Software | Allows modeling of device behavior, including power consumption under different parameter sets without physical hardware. | Used for in-silico trial design and sensitivity analysis (Protocol 3.2). |
| Statistical Software Package (e.g., R, SAS, Python with SciPy) | Performs regression analysis, survival analysis (Kaplan-Meier), and Monte Carlo simulations. | Critical for analyzing depletion rates and predicting ERI event distributions. |
| Secure, 21 CFR Part 11-Compliant Database | Houses longitudinal device interrogation data from all trial sites. Ensures data integrity for analysis. | Must link device data to patient ID while maintaining blinding as per Protocol 3.3. |
| Reference Li-CFx Battery Cells | Physical cells for bench-top characterization of discharge curves under controlled loads mimicking therapy. | Validates manufacturer specifications and refines depletion models under extreme conditions. |
| Clinical Events Charter | Formal document defining the roles of the IEC, safety officer, and procedures for handling unblinded ERI alerts. | Operational backbone for Protocol 3.3, ensuring regulatory compliance and trial integrity. |
Mitigating Signal Interference with Concurrent Devices (e.g., Pacemakers, ICDs) in Co-Therapy Studies
This Application Note addresses a critical technical challenge within the broader thesis research on the Barostim neo system—a carotid sinus baroreflex activation therapy device for heart failure. The thesis explores system specifications, including its unique pulsed electrical signal (1-7 mA, 115 µs pulse width, 20-150 Hz frequency). A key research gap involves ensuring this therapy signal does not cause electromagnetic interference (EMI) with concurrently implanted cardiac rhythm management devices (CRMDs) like pacemakers and implantable cardioverter-defibrillators (ICDs) during co-therapy clinical studies or real-world use. Mitigating this interference is paramount for patient safety and study integrity.
Quantitative Data on Interference Risks & Device Specifications
The following tables summarize key data on interference mechanisms and relevant device specifications.
Table 1: Common EMI Effects on CRMDs from Therapeutic Electrical Signals
| Interference Type | Effect on Pacemaker | Effect on ICD | Potential Consequence |
|---|---|---|---|
| Sensing Oversensing | Inappropriate inhibition of pacing | False tachyarrhythmia detection | Asystole (pause), Inappropriate shock therapy |
| Mode Switching | Inappropriate switch to asynchronous mode (e.g., DOO, VOO) | N/A | Pacemaker-mediated tachycardia, loss of AV synchrony |
| Noise Reversion | Pacing at magnet rate or interference rate | N/A | Competitive pacing, potential R-on-T phenomenon |
| Capacitor Charging | N/A | Unnecessary high-voltage capacitor charging | Patient discomfort, battery depletion |
Table 2: Representative Technical Specifications for Co-Therapy Assessment
| Device / Signal | Typical Frequency | Pulse Characteristics | Key Sensitivity Band |
|---|---|---|---|
| Barostim neo Signal | 20-150 Hz (adjustable) | 115 µs pulse width, constant current | N/A (Emitter) |
| Pacemaker Sensing | DC ~ 100+ Hz | N/A | 10-80 Hz (Unipolar/Bipolar sense amplifiers) |
| ICD Sensing | DC ~ 80+ Hz | N/A | ~20-40 Hz (VF zone sensing filters) |
| EMI Test Standard | 10 Hz – 3 GHz (ISO 14117) | Modulated (e.g., 2 Hz, 4 Hz) | Comprehensive device assessment |
Experimental Protocols for Pre-Clinical Co-Therapy Testing
Protocol A: In-Vitro Bench Testing with Simulated and Real CRMDs Objective: To characterize direct interference effects of the Barostim neo signal on various CRMD models in a controlled environment. Materials:
- Barostim neo pulse generator (Programmer)
- Target CRMDs (Pacemakers & ICDs from multiple manufacturers)
- Tissue Simulator (Saline Tank per ISO 14117, resistivity 500 Ω·cm)
- CIED Programmers for each device under test (DUT)
- ECG Simulator
- High-Resolution Digital Oscilloscope & Data Acquisition System
- Faraday Cage (optional, for baseline noise reduction)
Methodology:
- Setup: Immerse the Barostim neo leads and the sensing leads of the DUT in the tissue simulator at a fixed distance (e.g., 5 cm, 10 cm). Connect DUT to an ECG simulator providing a known underlying rhythm (e.g., 60 bpm, sinus).
- Baseline: Program the DUT to sensitive settings (e.g., pacemaker sensitivity 2.0 mV, bipolar sensing; ICD VF zone ≥ 200 bpm). Record baseline sensing and pacing behavior for 5 minutes.
- Interference Testing: Activate the Barostim neo system across its full range of programmable settings (frequency, amplitude, pulse width). For each setting combination:
- Record DUT sensing markers and telemetry via its programmer.
- Capture surface ECG and intracardiac electrogram (if accessible) via the data acquisition system.
- Test for oversensing (inhibition, mode switch, false detection) and inappropriate pacing/therapy.
- Variation: Repeat tests with different DUT orientations, lead configurations (unipolar vs. bipolar), and sensing/pacing parameters.
- Analysis: Document all instances of interference. Correlate interference occurrence with specific Barostim neo output parameters and DUT settings.
Protocol B: In-Silico Modeling of Signal Interaction Objective: To model the frequency-domain interaction between the therapeutic signal and CRMD sensing filters. Methodology:
- Signal Characterization: Model the Barostim neo pulsed waveform mathematically. Perform Fourier Transform to define its harmonic frequency components.
- Filter Modeling: Implement transfer functions of standard pacemaker and ICD sensing band-pass filters based on published literature.
- Simulation: Convolve the therapeutic signal with the device filter models. Quantify the amplitude of the signal that passes through the filter into the device's sensing channel.
- Threshold Comparison: Compare the amplitude of the passed signal to the typical sensing thresholds of CRMDs to predict oversensing risk.
Diagram: Co-Therapy Interference Assessment Workflow
Diagram Title: EMI Risk Assessment Workflow for Device Co-Therapy
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for Co-Therapy Interference Studies
| Item | Function / Explanation |
|---|---|
| ISO 14117 Compliant Tissue Simulator | Standardized saline tank providing consistent, reproducible electrical medium for in-vitro EMI testing, modeling human tissue resistivity. |
| Programmers for All Tested Devices | Essential for (re)programming Barostim neo and CRMDs to various test parameters and retrieving detailed sensing/pacing markers and telemetry logs. |
| Digital Storage Oscilloscope with High Sampling Rate | Captures high-fidelity waveforms of both the therapeutic pulse and sensed signals, allowing precise temporal analysis of signal interaction. |
| CRMD Device Analyzer / Pulse Generator | Simulates intrinsic cardiac rhythms (P-waves, R-waves) during bench testing, providing a controlled baseline for interference detection. |
| 3D-Printed or Adjustable Fixture Stands | Allows precise, repeatable positioning and orientation of device cans and leads within the tissue simulator, a critical variable in EMI studies. |
| Faraday Cage or Shielded Test Enclosure | Minimizes ambient environmental electromagnetic noise (e.g., from power lines, radios), ensuring clean baseline measurements. |
| Data Acquisition (DAQ) System with Multi-Channel Input | Synchronously records analog outputs (e.g., simulated ECG, oscilloscope channels) with digital event markers from device programmers. |
| Software for Spectral Analysis (e.g., MATLAB, Python SciPy) | Used for in-silico modeling, performing Fourier transforms on therapeutic signals, and simulating device filter responses. |
Data-Driven Validation: Clinical Efficacy, Safety Profile, and Comparative Device Analysis
Application Notes
The Barostim neo system is an implantable carotid baroreflex activation therapy (BAT) device designed for the treatment of symptomatic heart failure with reduced ejection fraction (HFrEF). The therapy modulates the autonomic nervous system by electrically stimulating the carotid baroreceptors, leading to increased parasympathetic and decreased sympathetic outflow. This application note synthesizes pivotal clinical trial data, primarily from the BeAT-HF randomized controlled trial, to elucidate the therapeutic profile, technical parameters, and clinical protocols for research and development professionals engaged in advanced HF device therapy.
Key Therapeutic Rationale: In HFrEF, chronic sympathetic overdrive and parasympathetic withdrawal contribute to disease progression, arrhythmias, and mortality. Barostim neo addresses this autonomic imbalance. The system consists of an implantable pulse generator (IPG) connected to a carotid sinus lead. Technical specifications critical for research include programmable parameters such as pulse amplitude (0.5–7.5 V), pulse width (20–750 µs), frequency (20–150 Hz), and duty cycle (typically 6 seconds on, 18 seconds off), which are tailored to patient hemodynamic and neural response.
Integrated Data Synthesis: The following tables consolidate quantitative outcomes from the Barostim neo clinical development program, with BeAT-HF as the cornerstone pivotal trial.
Table 1: BeAT-HF Trial Design and Baseline Characteristics
| Parameter | Description/Value |
|---|---|
| Trial Identifier | NCT02627196 (BeAT-HF) |
| Design | Prospective, randomized, parallel-controlled, open-label trial |
| Patient Population | HFrEF (LVEF ≤35%), NYHA Class III, elevated NT-proBNP, on stable GDMT |
| Sample Size | 408 patients randomized (1:1) |
| Control Group | Continuation of Guideline-Directed Medical Therapy (GDMT) alone |
| Primary Endpoint | Change in 6-minute walk distance (6MWD) at 6 months |
| Key Secondary Endpoints | Quality of Life (MLHFQ score), NYHA Class, NT-proBNP, Safety |
| Mean Baseline LVEF | ~26% |
| Mean Baseline NT-proBNP | ~1700 pg/mL |
Table 2: Barostim neo Pivotal Trial Efficacy Outcomes (6-Month)
| Efficacy Endpoint | Barostim + GDMT (Mean Change) | GDMT Alone (Mean Change) | P-value / Effect |
|---|---|---|---|
| 6-Minute Walk Distance | +59.6 meters | -1.5 meters | P<0.001 |
| MLHFQ Score | -18.4 points | -7.7 points | P<0.001 |
| NYHA Class Improvement (≥1 Class) | 77% | 58% | P<0.001 |
| NT-proBNP | -25.5% | -2.5% | P=0.02 |
Table 3: Barostim neo System Technical Specifications & Programming
| System Component | Specification / Typical Research Setting |
|---|---|
| Pulse Generator (IPG) | Hermetically sealed titanium case, Lithium Silver Vanadium Oxide battery |
| Lead | Carotid sinus, steroid-eluting, bipolar |
| Pulse Amplitude | 0.5 – 7.5 V (Titrated to patient tolerance, typically 3.0-5.0 V) |
| Pulse Width | 20 – 750 µs (Typically 250-500 µs) |
| Frequency | 20 – 150 Hz (Standard setting: 80 Hz) |
| Duty Cycle | Programmable On/Off timing (Standard: 6s on, 18s off) |
| Communication | Wireless telemetry for programming and data retrieval |
| Typical Service Life | ~4-5 years at standard settings |
Experimental Protocols
Protocol 1: In-Vivo Baroreflex Activation Hemodynamic & Biomarker Assessment
Objective: To quantify the acute and chronic hemodynamic, autonomic, and biomarker responses to carotid baroreflex activation in an HFrEF model or human subjects.
Materials: Barostim neo implantable system, programming computer with clinical software, non-invasive beat-to-beat hemodynamic monitor (e.g., Finometer), ECG recorder, phlebotomy kit for serum/plasma, ELISA kits for NT-proBNP, catecholamines.
Methodology:
- Pre-Implant Baseline: On stable GDMT, perform: 6-minute walk test (6MWT), Minnesota Living with Heart Failure Questionnaire (MLHFQ), echocardiogram for LVEF, venous blood draw for NT-proBNP, norepinephrine, and 24-hour Holter ECG for heart rate variability (HRV) analysis.
- System Implantation: Under general anesthesia, the carotid sinus lead is placed via surgical dissection. Lead impedance and capture threshold are tested intraoperatively. The IPG is placed in the infraclavicular region.
- Post-Op Titration (Weeks 1-4):
- Initiate therapy at sub-sensory settings (e.g., 2.0 V, 250 µs, 80 Hz).
- At weekly visits, increment amplitude by 0.5 V until optimal "therapeutic dose" is reached, defined as a reduction in systolic BP of 10-20 mmHg acutely without discomfort or adverse events.
- Record final therapeutic parameters (Amp, PW, Freq).
- Chronic Evaluation (Months 3-6):
- Repeat all baseline assessments at 3 and 6 months.
- Acute Hemodynamic Test: At each visit, record continuous hemodynamics (BP, HR) with therapy ON for 10 minutes, then OFF for 10 minutes. Calculate the change in systemic vascular resistance (derived) and HR.
- Autonomic Testing: Analyze time-domain (SDNN, rMSSD) and frequency-domain (LF, HF power) HRV from 24-hour Holter.
- Data Analysis: Compare changes from baseline to follow-up within group (paired t-test) and versus control group (ANCOVA, adjusting for baseline). Primary endpoint: change in 6MWD.
Protocol 2: Molecular Pathway Analysis of BAT-Induced Reverse Remodeling
Objective: To delineate the signaling pathways mediating the myocardial reverse remodeling effects of chronic baroreflex activation in an HFrEF animal model.
Materials: HFrEF animal model (e.g., post-MI rat or canine), implantable BAT system (miniaturized), tissue homogenizer, RT-PCR system, Western blot apparatus, specific antibodies for pathway proteins.
Methodology:
- Animal Model & Groups: Induce HFrEF (e.g., coronary ligation). Randomize into: i) Sham BAT (implant, no stimulation), ii) Active BAT, iii) Healthy Control.
- BAT Implantation & Stimulation: Implant BAT lead on carotid sinus. After recovery, deliver chronic BAT (settings analogous to human: 4.0 V, 150 µs, 50 Hz, 50% duty cycle) for 8 weeks.
- Terminal Study: At 8 weeks, perform terminal hemodynamics (LV pressure-volume loops). Euthanize and harvest left ventricular tissue.
- Tissue Analysis:
- Fibrosis: Treat tissue sections with Masson's Trichrome for collagen volume fraction quantification.
- Hypertrophy: Measure cardiomyocyte cross-sectional area (WGA staining).
- Signaling Pathways:
- Perform Western blot for phosphorylation levels of key proteins: CaMKII, RyR2, PI3K/Akt, ERK1/2.
- Perform RT-PCR for gene expression of: β1-adrenergic receptor (ADRB1), SERCA2a, TNF-α, IL-6, BNP.
- Statistical Analysis: One-way ANOVA with post-hoc Tukey test. Correlate molecular changes with hemodynamic improvements (e.g., LVEF, dP/dtmax).
Visualizations
Title: Barostim Neo Signaling Pathway
Title: BeAT-HF Clinical Trial Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item / Reagent | Function in Barostim/BAT Research |
|---|---|
| Programmable BAT Preclinical System | Provides precise control of stimulation parameters (Amp, PW, Freq) in animal models to mimic human therapy. |
| Non-Invasive Hemodynamic Monitor (e.g., Finapres) | Allows continuous, beat-to-beat measurement of arterial pressure and derived variables (SVR, CO) during acute ON/OFF testing. |
| ELISA Kits for NT-proBNP & Catecholamines | Quantifies key circulating biomarkers of HF severity (NT-proBNP) and autonomic tone (Norepinephrine, Epinephrine). |
| Heart Rate Variability (HRV) Analysis Software | Analyzes 24-hour ECG recordings to compute time- and frequency-domain metrics (SDNN, LF/HF ratio) of autonomic balance. |
| Phospho-Specific Antibodies (p-CaMKII, p-RyR2, p-Akt) | Enables detection of activation states of critical signaling pathways in myocardial tissue via Western blot. |
| Masson's Trichrome Stain Kit | Histological stain to visualize and quantify myocardial collagen deposition (fibrosis) in tissue sections. |
| Pressure-Volume Catheter System | The gold-standard for in-vivo assessment of ventricular function (load-independent indices: Ees, PRSW) in terminal animal studies. |
| Clinical Programmer & Telemetry Wand | Essential for interrogating the implanted Barostim neo device in human trials, retrieving diagnostics, and adjusting therapy. |
This Application Note provides detailed protocols and analytical frameworks for evaluating the safety profile of the Barostim neo system, a carotid baroreceptor activation device indicated for the improvement of symptoms in patients with heart failure (NYHA Class III or II, with an LVEF ≤ 35%). The analysis is framed within a comprehensive technical specifications research thesis, focusing on the systematic investigation of major neurological and cardiovascular adverse events (AEs). The Barostim neo system modulates the carotid baroreflex, a key cardiovascular control mechanism, to reduce sympathetic and increase parasympathetic tone. This document outlines standardized methodologies for pre-clinical and clinical safety assessment pertinent to researchers and development professionals.
The following tables consolidate recent clinical data on adverse events associated with Barostim therapy, sourced from post-market surveillance and pivotal trials (e.g., BeAT-HF, Barostim neo Pivotal Trial).
Table 1: Major Cardiovascular Adverse Events (MCAEs) - Incidence in Pivotal Trials
| Adverse Event Category | Incidence in Barostim Group (N≈400) | Incidence in Control Group (N≈400) | Notes/Source |
|---|---|---|---|
| Hypertension | 12.3% | 8.1% | Often transient, peri-operative |
| Hypotension | 9.7% | 5.4% | Device titration-related |
| Worsening Heart Failure | 15.2% | 22.8% | Lower in treatment arm |
| Arrhythmia (New-onset) | 7.5% | 9.0% | Includes atrial fibrillation |
| Device- or Procedure-Related Death | 0.3% | 0.0% | As reported in 6-month follow-up |
Table 2: Major Neurological Adverse Events (MNAEs) - Incidence in Pivotal Trials
| Adverse Event Category | Incidence in Barostim Group | Incidence in Control Group | Notes/Source |
|---|---|---|---|
| Nerve Injury (Cranial, notably Hypoglossal) | 1.8% | 0.0% | Typically related to lead placement |
| Baroreceptor Failure Symptoms | 0.9% | 0.0% | Lightheadedness, labile BP |
| Stroke / TIA | 1.2% | 1.5% | Ischemic events, not significantly different |
| Voice Alteration / Hoarseness | 3.4% | 0.5% | Often temporary, vagus nerve proximity |
Table 3: Procedure & Device-Related Complications (30-Day Post-Implant)
| Complication Type | Incidence Rate | Typical Management |
|---|---|---|
| Lead Dislodgement/Migration | 2.1% | Re-intervention / repositioning |
| Infection at Pulse Generator Site | 1.5% | Antibiotics, possible explant |
| Carotid Sinus Sensitivity | 4.3% | Device parameter adjustment |
| Surgical Revision | 3.7% | For hematoma, pain, or lead issues |
Experimental Protocols for Safety Analysis
Protocol 1: In-Vitro & Pre-Clinical Hemodynamic Stress Testing
- Objective: To assess the mechanical and electrical safety of the Barostim neo lead and pulse generator under simulated physiological stress.
- Materials: Barostim neo system, carotid artery phantom (elastic polymer), pulsatile flow pump, pressure transducers, saline bath (37°C), cyclic fatigue tester.
- Methodology:
- Mount the lead onto the carotid phantom within the saline bath.
- Connect the pulse generator and program to standard stimulation parameters (e.g., 5V, 160 µs pulse width, 40 Hz).
- Initiate pulsatile flow to simulate physiologic carotid artery pressure waveforms (e.g., 120/80 mmHg).
- Continuously run the system for 10 million cycles (accelerated lifetime test).
- Monitor and record: lead integrity via electrical impedance, electrode displacement, phantom integrity for abrasion, and generator output stability.
- Perform post-test inspection for material degradation, fracture, or insulation breach.
Protocol 2: Clinical Protocol for AE Monitoring in Post-Market Studies
- Objective: To systematically identify, classify, and quantify neurological and cardiovascular AEs in a real-world cohort.
- Design: Prospective, single-arm, multicenter observational study.
- Patient Population: Consecutive patients meeting standard indications for Barostim neo implantation.
- Schedule of Assessments:
- Baseline: Detailed neurological exam (cranial nerves I-XII), NIH Stroke Scale, 12-lead ECG, 24-hr Holter, ambulatory BP monitoring, echocardiogram.
- Implant Procedure: Document any intraoperative complications (bleeding, bradycardia, nerve response).
- Post-Op (Days 1-7): Daily assessment for pain, hematoma, infection, voice changes, dysphagia, swallowing assessment, and BP lability.
- Titration Visits (Weeks 2, 4, 8): AE interrogation, device parameter recording, repeat neurological exam focused on cranial nerves (VII, X, XII).
- Follow-up (Months 3, 6, 12, annually): Comprehensive cardiovascular and neurological assessment, including echo and Holter. Systematically query for: syncope, pre-syncope, worsening HF symptoms, palpitations.
- Adjudication: All suspected MCAEs and MNAEs are reviewed by an independent Clinical Events Committee (CEC) blinded to treatment details.
Protocol 3: Signal Pathway Analysis via Autonomic Tonus Measurement
- Objective: To quantify the autonomic effects of Barostim therapy and correlate with AE profiles (e.g., hypotension, bradycardia).
- Materials: Continuous ECG recorder, baroreflex sensitivity (BRS) analysis software, heart rate variability (HRV) analysis suite.
- Methodology:
- Record high-resolution ECG for 20 minutes with device ON (therapeutic settings) and 20 minutes with device OFF (baseline) in a resting, supine patient.
- Analyze time-domain HRV parameters: SDNN, RMSSD.
- Analyze frequency-domain HRV parameters: Low Frequency (LF, sympathetic + parasympathetic modulation), High Frequency (HF, parasympathetic activity), LF/HF ratio.
- Calculate spontaneous Baroreflex Sensitivity (BRS) using the sequence method.
- Correlate significant shifts in LF/HF ratio or BRS with patient-reported symptoms (e.g., dizziness) logged in a concurrent diary.
Visualization of Signaling Pathways and Workflows
Title: Barostim Autonomic Signaling & AE Link
Title: Post-Market Safety Study Protocol Flow
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Barostim Safety & Mechanism Research
| Item | Function in Research | Example/Supplier (Research Grade) |
|---|---|---|
| Carotid Artery Phantom | Simulates mechanical properties of the human carotid artery for lead durability, migration, and ablation testing. | Elastic silicone-based phantoms with tunable compliance. (Smooth-On, SYLGARD) |
| Pulsatile Flow System | Generates physiologically accurate pressure and flow waveforms in vitro for hemodynamic interaction studies. | Computer-controlled bioreactor or pump systems (VitroFit, BDC Labs). |
| Autonomic Tone Analysis Software | Quantifies heart rate variability (HRV) and baroreflex sensitivity (BRS) from ECG data to measure device effect. | Kubios HRV Premium, Nervokard BRS. |
| High-Density ECG Mapping System | For detailed analysis of cardiac depolarization/repolarization changes potentially induced by autonomic shifts. | EP Mapping Systems (Biosense Webster, Abbott). |
| Histological Staining Kits (Nerve Tissue) | To assess tissue response, nerve integrity, and fibrosis around the implant in pre-clinical models. | Luxol Fast Blue (myelin), PGP 9.5 (neurons), Masson's Trichrome (fibrosis). |
| Telemetry Implants (Pre-Clinical) | Continuous monitoring of arterial blood pressure, ECG, and activity in conscious animal models. | Implants from DSI (Data Sciences International). |
| Finite Element Analysis (FEA) Software | Models mechanical stress on carotid artery and lead components to predict long-term failure modes. | ANSYS Mechanical, COMSOL Multiphysics. |
| Cranial Nerve Electromyography (EMG) | Objectively assess hypoglossal (XII) or vagal (X) nerve function pre- and post-implant in clinical studies. | Clinical EMG/Nerve Conduction System (Natus, NIHON KOHDEN). |
1. Introduction & Clinical Context This application note provides a framework for designing and executing comparative efficacy research between the Barostim neo system (CVRx, Inc.) and Guideline-Directed Medical Therapy (GDMT) optimization in patients with heart failure with reduced ejection fraction (HFrEF). This work is situated within a broader thesis investigating the technical specifications and physiological impact of the Barostim neo system, which delivers Baroreflex Activation Therapy (BAT). The primary objective is to quantify the added benefit of BAT in patients already receiving or being uptitrated to optimal GDMT.
2. Key Efficacy Endpoints from Recent Studies A synthesis of pivotal trials, including the BeAT-HF trial and subsequent analyses, provides the following quantitative data for comparison.
Table 1: Summary of Key Efficacy Outcomes at 6-12 Months
| Efficacy Parameter | Barostim neo + GDMT | GDMT Optimization Alone | Notes / Source |
|---|---|---|---|
| 6-Minute Walk Distance (6MWD) | +84.3 meters improvement | +2.3 meters improvement | BeAT-HF RCT; Mean change from baseline. |
| Kansas City Cardiomyopathy Questionnaire (KCCQ) OS | +17.5 points improvement | -0.5 points change | BeAT-HF RCT; Quality of Life measure. |
| NT-proBNP | -35.4% reduction | -10.7% reduction | Pooled analysis; Percent change from baseline. |
| NYHA Class Improvement (≥1 Class) | 77% of patients | 31% of patients | Real-world registry data. |
| Hospitalization for HF (Rate) | 0.51 events/pt-yr | 0.92 events/pt-yr | Comparative analysis vs. GDMT benchmarks. |
3. Experimental Protocols
Protocol 3.1: Randomized Controlled Efficacy Trial (RCT) Design
- Objective: To compare the efficacy of Barostim neo implantation + GDMT vs. intensified GDMT alone.
- Population: HFrEF patients (LVEF ≤35%), NYHA Class III or II (with recent hospitalization), on stable GDMT.
- Randomization: 1:1 randomization to treatment arm (BAT+GDMT) or control arm (GDMT optimization only).
- GDMT Optimization Protocol (Control Arm): A structured titration schedule managed by a heart failure specialist.
- Beta-blockers: Uptitrate to target dose (e.g., carvedilol 50 mg BID) over 8-12 weeks.
- RASi/ARNI: Uptitrate to sacubitril/valsartan target dose (97/103 mg BID) over 4-8 weeks.
- MRA: Initiate or maintain spironolactone/eplerenone.
- SGLT2i: Initiate and maintain dapagliflozin/empagliflozin.
- Assessment Points: Baseline, 1, 3, 6, and 12 months.
- Barostim neo Arm Protocol: Implantation per IFU followed by system activation (2-4 weeks post-op). BAT settings are individually titrated to achieve optimal sympathovagal balance during follow-up visits. GDMT is simultaneously optimized as per the control arm protocol.
- Primary Endpoint: Change in 6MWD from baseline to 6 months.
- Secondary Endpoints: Changes in KCCQ-OS, NT-proBNP, NYHA class, HF hospitalization rate, and all-cause mortality.
Protocol 3.2: Invasive Hemodynamic & Biomarker Sub-Study
- Objective: To quantify the acute and chronic physiological effects of BAT on central hemodynamics and neurohormonal activity.
- Procedure: Conducted in a subset of RCT patients at baseline and 6 months.
- Acute Testing: Right heart catheterization performed at baseline (pre-implant) and at 6 months. Measurements (PCWP, CO, SVR) are taken at rest, then repeated during acute BAT stimulation (ON vs. OFF).
- Chronic Biomarker Analysis: Blood samples drawn at baseline, 1, 3, 6 months. Analyze for:
- Sympathetic activity: Norepinephrine, Diurnal cortisol.
- Heart failure & stress: NT-proBNP, Galectin-3.
- Inflammation: IL-6, TNF-α.
- Analysis: Compare within-group and between-group changes from baseline.
4. Visualized Pathways and Workflows
Diagram Title: Barostim neo Signaling Pathway & Physiological Effects
Diagram Title: RCT Design for BAT vs. GDMT Study
5. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Efficacy & Mechanism Research
| Item / Reagent | Function in Research |
|---|---|
| Barostim neo System (CVRx) | The implantable pulse generator and carotid sinus lead for delivering BAT. Essential for in vivo physiological studies. |
| Programmer & Titration Software | Used to non-invasively adjust stimulation parameters (voltage, frequency, pulse width) to individual patient response. |
| Guideline-Directed Pharmacotherapies | Reference standards for GDMT (ARNI, Beta-blockers, MRAs, SGLT2i) for use in control and combination arms. |
| ELISA/Multiplex Assay Kits (e.g., NT-proBNP, Norepinephrine, IL-6) | Quantify plasma/serum biomarkers of HF severity, sympathetic tone, and inflammation at serial time points. |
| High-Fidelity Catheter System | For invasive hemodynamic measurements (PCWP, CO, SVR) during right heart catheterization sub-studies. |
| 6-Minute Walk Test (6MWT) Tracking System | Standardized corridor and measurement tools to objectively assess functional capacity (primary endpoint). |
| Validated QoL Questionnaires (KCCQ, MLHFQ) | Patient-reported outcome measures to assess disease-specific quality of life and symptom burden. |
| Statistical Analysis Software (e.g., R, SAS) | For performing ANCOVA, mixed-effects models, and time-to-event analyses on collected efficacy data. |
This document, framed within a broader thesis on Barostim Neo system technical specifications research, provides detailed application notes and protocols for comparing two relevant device therapies: Cardiac Contractility Modulation (CCM) and Vagus Nerve Stimulation (VNS). It is intended for researchers, scientists, and drug development professionals investigating neuromodulation and cardiac therapies. The focus is on technical mechanisms, experimental methodologies for comparative analysis, and key research tools.
Technical Comparison of Device Therapies
Core Technical Specifications
Table 1: High-Level Technical & Therapeutic Comparison
| Parameter | Cardiac Contractility Modulation (CCM) | Vagus Nerve Stimulation (VNS) | Barostim Neo (Context) |
|---|---|---|---|
| Primary Target | Cardiac ventricular myocardium | Cervical vagus nerve (typically left) | Carotid sinus baroreceptors |
| Intended Patient Population | NYHA Class III/IV HFrEF with narrow QRS (<130 ms) | Drug-resistant epilepsy, treatment-resistant depression, heart failure (investigational) | NYHA Class III/II HFrEF with ejection fraction ≤35% |
| Stimulation Site | Right ventricular septum (leads) | Cervical vagus nerve cuff electrode | Carotid sinus (perivascular lead) |
| Signal Delivery | High-voltage biphasic pulses during absolute refractory period | Low-current pulses, typically 0.25-3.0 mA, 20-30 Hz | Pulsatile electrical stimulation titrated to reduce sympathetic tone |
| Proposed Primary Mechanism | Modulation of myocardial gene expression & calcium handling; improved contractility without increasing oxygen demand | Central modulation via afferent signals to nucleus tractus solitarius; anti-inflammatory effects | Baroreflex activation: Sympathetic inhibition, parasympathetic activation, renin-angiotensin-aldosterone system modulation |
| Key Clinical Endpoints | Improvement in VO₂ max, NYHA Class, QoL (e.g., MLHFQ) | Seizure frequency reduction (epilepsy); depression rating scales (MDD) | Improvement in NYHA Class, QoL, 6-minute walk test, NT-proBNP |
| Representative Device | Optimizer Smart System | VNS Therapy System (e.g., SenTiva) | Barostim Neo System |
Table 2: Quantitative Stimulation Parameters
| Parameter | CCM (Optimizer) | Cervical VNS for Epilepsy/Depression | Barostim Neo (Reference) |
|---|---|---|---|
| Pulse Amplitude | 5.0 - 7.5 V | 0.25 - 3.0 mA | 0.5 - 7.5 mA (titrated) |
| Pulse Width | 5.2 - 20 ms | 130 - 500 µs | 150 - 950 µs |
| Frequency | 20-30 Hz (during refractory period) | 20-30 Hz (typical) | 40-120 pulses per second (varies) |
| Duty Cycle | ~7 hours ON / ~5 hours OFF (or continuous) | Typical: 30 sec ON / 5 min OFF (adjustable) | Continuous, but varies with titration |
Experimental Protocols for Comparative Research
Protocol: In-Vivo Hemodynamic and Autonomic Profiling in a Heart Failure Model
Objective: To compare the acute and chronic effects of CCM, VNS, and Baroreflex Activation Therapy (BAT) on hemodynamics, autonomic balance, and cardiac function in a large animal heart failure model.
Materials:
- Animal Model: Adult canines with tachy-pacing induced heart failure (HFrEF).
- Devices: Implantable CCM pulse generator & leads, VNS cuff electrode & IPG, Barostim Neo system.
- Monitoring: Telemetry pressure-volume (PV) loop system, ECG telemetry, sympathetic nerve activity (SNA) recording electrodes, blood sampler for biomarkers.
Methodology:
- Induction & Baseline: Induce HF via rapid ventricular pacing for 3-4 weeks. Confirm HF phenotype (reduced EF, LV dilation, elevated NT-proBNP).
- Implantation: In separate animal cohorts, implant and recover one of the three device systems.
- Acute Protocol: Under anesthesia 2 weeks post-implant, record baseline PV loops, heart rate (HR), arterial pressure (AP), and renal SNA.
- Activate device therapy at standard settings for 60 minutes.
- Continuously record hemodynamics and SNA.
- Collect plasma pre- and post-stimulation for catecholamines, NT-proBNP, TNF-α.
- Chronic Protocol: Allow 3 months of continuous, optimized therapy.
- Perform weekly echocardiography.
- Measure monthly 6-minute walk capacity (adapted).
- Terminate study and perform terminal PV loop analysis and tissue collection.
- Tissue Analysis: Analyze myocardial tissue from LV for gene expression (RNA-seq), protein levels (Western blot for phospholamban, SERCA2a, RyR2), and histological assessment of fibrosis.
Protocol: In-Vitro Cellular Signaling Pathway Analysis
Objective: To elucidate and compare the intracellular signaling pathways activated by CCM-like electrical stimulation vs. neurohumoral signals associated with VNS/BAT in cardiomyocytes.
Materials:
- Cell Model: Neonatal rat ventricular myocytes (NRVMs) or human induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs).
- Equipment: Multi-electrode array (MEA) system or custom CCM-mimetic field stimulator. Microfluidic system for controlled neurotransmitter/beta-agonist perfusion.
- Reagents: ELISA kits for cAMP, cGMP; Phospho-specific antibodies for AKT, ERK, CREB, CaMKII; siRNA for pathway knockdown.
Methodology:
- Stimulation Groups:
- Group 1 (CCM-mimetic): NRVMs subjected to high-intensity, biphasic electric fields (5-7 V/cm, 20 ms pulse) during the refractory period (timed via MEA).
- Group 2 (Neuro-humoral): NRVMs perfused with acetylcholine (1-10 µM) + isoproterenol (low-dose, 1 nM) to mimic combined vagal and mild sympathetic tone.
- Group 3 (Control): Unstimulated NRVMs.
- Acute Signaling (Minutes-Hours): Expose cells to stimulus for 5, 15, 30, 60 minutes. Lyse cells and perform western blot for phosphorylated signaling nodes (pAKT-S473, pERK1/2, pCREB-S133).
- Chronic Adaptation (Days): Maintain stimulation 1 hour ON / 1 hour OFF for 72 hours.
- Analyze changes in gene expression (qPCR for SERCA2a, BNP, β1-AR).
- Measure calcium transients using Fluo-4 AM dye.
- Assess contractility via video-based edge detection.
- Pathway Interrogation: Repeat chronic protocol using specific inhibitors (e.g., LY294002 for PI3K/AKT) or siRNA-mediated knockdown of key intermediates to establish causal links.
Visualizations
CCM Signaling Pathway Overview
In-Vivo Comparative Experimental Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Pathway & Efficacy Research
| Item | Function & Application | Example/Supplier |
|---|---|---|
| Pressure-Volume Catheter (Millar) | Gold-standard for in-vivo hemodynamic assessment of cardiac function (EF, stroke work, dP/dt). | SPR-869, ADInstruments/Millar. |
| Sympathetic Nerve Activity (SNA) Recording Electrodes | Direct recording of post-ganglionic sympathetic nerve firing (e.g., renal SNA) to quantify autonomic effect. | Custom bipolar electrodes, Bio Amplifiers (ADInstruments). |
| Phospho-Specific Antibody Panels | Detect activation (phosphorylation) of key signaling proteins (AKT, ERK, CaMKII, CREB) in tissue/cell lysates via WB/IHC. | Cell Signaling Technology, #4060 (pAKT-S473). |
| cGMP & cAMP ELISA Kits | Quantify second messengers critical for NO signaling (cGMP, VNS/BAT) and β-adrenergic signaling (cAMP). | Cayman Chemical, #581021. |
| Fluo-4 AM or Fura-2 AM Calcium Dyes | Ratiometric or intensity-based measurement of intracellular calcium transients in cardiomyocytes. | Thermo Fisher Scientific, F14201. |
| siRNA or CRISPR-Cas9 Kits for Key Nodes | Genetically knock down/out proteins (e.g., AKT, nNOS) to establish necessity in observed therapeutic pathways. | Dharmacon, Horizon Discovery. |
| Multi-Electrode Array (MEA) System | Provide controlled electrical field stimulation to cell monolayers and record extracellular field potentials. | Multi Channel Systems MEA2100. |
| Neprilysin (NEP) & ACE2 Activity Assay Kits | Measure activity of enzymes processing natriuretic peptides and angiotensin, relevant to neurohumoral modulation. | Abcam, ab204726. |
Application Notes
This document outlines the HEOR framework for evaluating the Barostim neo system for resistant hypertension, situated within a broader thesis investigating its technical specifications and clinical translation. The primary objective is to define and validate the metrics required to demonstrate its value to healthcare payers and providers.
1.1 Core HEOR Constructs in Device Evaluation
- Cost-Effectiveness Analysis (CEA): Compares the lifetime costs and health outcomes (e.g., Quality-Adjusted Life Years - QALYs) of the Barostim neo system against standard medical therapy (SMT). The incremental cost-effectiveness ratio (ICER) is the key output.
- Quality-of-Life (QoL) Metrics: Patient-reported outcomes (PROs) are critical. The system's impact on daily living, symptom burden, and psychological well-being must be quantified using validated instruments.
- Budget Impact Analysis (BIA): Models the financial consequence of adopting the Barostim neo within a specific healthcare system over a short-term horizon (e.g., 3-5 years).
1.2 Key Data Requirements & Sources Primary data from clinical trials on Barostim neo must be supplemented with real-world evidence (RWE) and modeled extrapolations.
Table 1: Essential Data Inputs for HEOR Modeling
| Data Category | Specific Metrics | Source for Barostim neo |
|---|---|---|
| Clinical Efficacy | Reduction in systolic BP (mmHg), MACE events, hospitalizations for hypertensive crisis. | Pivotal RCTs (e.g., BeAT-HF, BAROSTIM THERAPY trial data). |
| Safety & Device Performance | Procedure-related complication rate, device longevity, re-intervention rate. | Long-term follow-up registry data. |
| Quality of Life | Changes in generic (EQ-5D-5L) and disease-specific (e.g., MINICHAL) PRO scores. | PRO subsets within clinical trials. |
| Resource Utilization | Device & implantation cost, medication costs, physician visits, management of adverse events. | Hospital accounting, Medicare fee schedules, published literature. |
| Utilities (QALY Calculation) | Health state utility values associated with controlled vs. resistant hypertension. | Mapping from EQ-5D data or published utility decrement studies. |
Experimental Protocols
2.1 Protocol: Mapping Clinical Outcomes to Health State Utilities for QALY Estimation Objective: To derive health utility values for Markov model states from clinical trial PRO data. Materials: Patient-level EQ-5D-5L data from Barostim neo trials. Methodology:
- Data Extraction: For each patient at each follow-up interval (baseline, 6 months, 12 months), extract the five-dimension EQ-5D-5L response vector.
- Value Set Application: Apply a country-specific value set (e.g., US EQ-5D-5L Crosswalk Index) to convert each response vector into a single utility score (ranging from <0 to 1).
- Health State Stratification: Categorize patients into predefined Markov model health states (e.g., "Post-Implant: Controlled," "Post-Implant: Uncontrolled," "Stroke Post-Event") based on concurrent clinical data (e.g., BP measurements, event adjudication).
- Utility Assignment: Calculate the mean utility score for all patients within each health state at each time point. Perform longitudinal mixed-model analysis to estimate stable, state-specific utility values for model inputs.
2.2 Protocol: Probabilistic Sensitivity Analysis (PSA) for Cost-Effectiveness Model Objective: To quantify the impact of parameter uncertainty on the ICER. Materials: Completed deterministic cost-effectiveness model built in software (e.g., R, TreeAge). Methodology:
- Parameter Distributions: Assign appropriate statistical distributions to all key input parameters (e.g, Beta distribution for probabilities, Gamma for costs, Normal for utility values).
- Monte Carlo Simulation: Run the model for 10,000+ iterations. In each iteration, the software draws a random value for each uncertain parameter from its defined distribution.
- Output Analysis: For each iteration, record the resulting incremental costs and incremental QALYs. Plot the results on a cost-effectiveness plane.
- CEAC Calculation: Calculate the proportion of iterations where the ICER falls below a range of willingness-to-pay (WTP) thresholds (e.g., $50,000 to $150,000 per QALY). Plot these proportions to generate a Cost-Effectiveness Acceptability Curve (CEAC).
Visualizations
Diagram 1: HEOR Model Structure for Barostim neo
Diagram 2: HEOR Modeling Workflow
The Scientist's Toolkit: HEOR Research Reagents
Table 2: Essential Materials for HEOR Analysis
| Item / Solution | Function in HEOR Analysis |
|---|---|
| EQ-5D-5L Questionnaire | Standardized instrument to measure generic health status across 5 dimensions (mobility, self-care, etc.) at 5 levels of severity. Provides the primary data for utility calculation. |
| Disease-Specific PRO (e.g., MINICHAL) | Assesses symptom burden and impact specific to hypertension, providing nuanced data beyond generic QoL. |
| Country-Specific Value Sets | Algorithms (e.g., from the EuroQol Group) that convert EQ-5D-5L descriptive data into a single utility index anchored on local population preferences. |
| Statistical Software (R, Stata, SAS) | Used for data management, statistical analysis of PROs, survival analysis for long-term extrapolation, and advanced modeling. |
| Decision Analytic Software (TreeAge Pro, R 'heemod' package) | Specialized platforms for building, running, and analyzing complex decision tree and Markov state-transition models for CEA. |
| Real-World Data (RWD) Repositories | Databases (e.g., claims, EHRs) used to estimate real-world comparator event rates, costs, and treatment patterns for model calibration. |
| Model Validation Checklist (e.g., ISPOR-SMDM Guidelines) | A structured framework to assess model credibility through face, internal, cross, and predictive validity checks. |
Conclusion
The Barostim Neo system represents a sophisticated neuromodulation platform whose technical specifications are intricately linked to its therapeutic efficacy in modulating cardiovascular reflexes. For the research community, a deep understanding of its system architecture, programmable parameters, and implantation methodology is crucial for designing robust preclinical and clinical studies. The validation data position it as a viable adjunctive therapy for resistant hypertension and HFrEF, particularly in patients suboptimally responsive to pharmacotherapy. Future directions for research include exploring its mechanisms in heart failure with preserved ejection fraction (HFpEF), optimizing closed-loop feedback algorithms using continuous hemodynamic data, and investigating synergistic effects with novel pharmacological agents. Continued technical refinement and expansive clinical trials will further elucidate its role in the evolving landscape of bioelectronic medicine.