Baroreflex Activation Therapy for Heart Failure: Mechanisms, Clinical Efficacy, and Future Directions in Autonomic Neuromodulation
This article provides a comprehensive analysis of Baroreflex Activation Therapy (BAT) as an innovative device-based treatment for heart failure with reduced ejection fraction (HFrEF).
Baroreflex Activation Therapy for Heart Failure: Mechanisms, Clinical Efficacy, and Future Directions in Autonomic Neuromodulation
Abstract
This article provides a comprehensive analysis of Baroreflex Activation Therapy (BAT) as an innovative device-based treatment for heart failure with reduced ejection fraction (HFrEF). Targeting researchers, scientists, and drug development professionals, it examines the foundational neuroanatomical principles of baroreceptor dysfunction in HFrEF and details the mechanistic pathways through which BAT restores autonomic balance. The content explores procedural methodology, patient selection criteria, and implantation techniques, while critically evaluating long-term efficacy data from recent clinical trials including improvements in left ventricular ejection fraction, functional classification, and biomarker reduction. Comparative analysis positions BAT within the current HFrEF treatment paradigm alongside guideline-directed medical therapy and other device interventions, concluding with future research trajectories and implications for cardiovascular drug and device development.
The Autonomic Imbalance in HFrEF: Neuroanatomical Basis for Baroreflex Activation
Pathophysiology of Sympathetic Overdrive and Parasympathetic Withdrawal in HFrEF Progression
Heart failure with reduced ejection fraction (HFrEF) is characterized by a significant autonomic imbalance, defined by sustained sympathetic overactivation and parasympathetic withdrawal [1]. This maladaptive state is not merely a consequence of the failing heart but a key driver of disease progression, contributing to maladaptive cardiac remodeling, arrhythmogenesis, and hemodynamic instability [1] [2]. The autonomic imbalance creates a self-perpetuating positive feedback cycle, often described as a 'downward spiral' of worsening cardiac function and autonomic dysfunction [1]. This document details the pathophysiological mechanisms and provides structured experimental data and protocols to support research, particularly within the context of exploring baroreflex activation therapy (BAT) as a circuit-specific treatment.
Anatomical and Functional Organization of Cardiac Autonomic Control
Autonomic regulation of the heart involves a complex, hierarchical network of neural signals spanning the entire neuraxis.
Peripheral and Central Pathways
- Sympathetic Pathways: Sympathetic fibers originate from the intermediolateral cell column of the thoracic spinal cord (T1–T5) and synapse in paravertebral ganglia, notably the stellate ganglia, before projecting to the heart [1]. Norepinephrine release and β-adrenergic receptor activation increase heart rate, contractility, and conduction velocity (chronotropy, inotropy, dromotropy) [1].
- Parasympathetic Pathways: Parasympathetic innervation is primarily mediated by the vagus nerve, originating in the medullary nuclei (nucleus ambiguus and dorsal motor nucleus). Acetylcholine release at muscarinic receptors slows heart rate and facilitates myocardial relaxation, promoting energy conservation [1].
- The Intrinsic Cardiac Nervous System (ICNS): Often called the "little brain on the heart," the ICNS is a nexus of afferent and efferent sympathetic and parasympathetic activity. It incorporates local sensory signals and acts as a crucial relay and independent modulator of autonomic function [1].
- The Central Autonomic Network (CAN): Above the brainstem, cortical centers like the insular cortex and anterior cingulate cortex modulate autonomic tone in response to cognitive and emotional states. These higher-order centers complete a system of bidirectional feedback loops between the heart and the brain [1].
Diagram 1: Hierarchical organization of the cardiac autonomic nervous system, showing the bidirectional communication between the brain and heart.
Core Pathophysiological Mechanisms of Autonomic Imbalance
Sympathetic Overdrive: Initiation and Perpetuation
The initial compensatory increase in sympathetic outflow becomes persistent through multiple maladaptive mechanisms, summarized in the table below.
Table 1: Mechanisms and Consequences of Sympathetic Overdrive in HFrEF
| Mechanism | Pathophysiological Consequence | Experimental Biomarker |
|---|---|---|
| Chronic β-adrenergic receptor (β-AR) stimulation | Receptor desensitization and downregulation [1], impaired intracellular calcium handling [1] | Myocardial β-AR density (radioligand binding), cAMP response to agonist |
| Neurohormonal Activation (RAAS) | Elevated circulating angiotensin II and aldosterone, promoting vasoconstriction, fibrosis, and further norepinephrine release [1] | Plasma renin activity, angiotensin II, aldosterone levels |
| Cardiac Remodeling | Cardiomyocyte hypertrophy [1], transcriptional reprogramming, and interstitial fibrosis [1] | Echocardiographic LV dimensions, serum PIIINP, galectin-3 |
| Altered Neural Circuitry | Neuroplasticity in spinal and ganglionic circuits [1], stellate ganglion hyperactivation and inflammation [1] [2] | Stellate ganglion activity recording, pro-inflammatory cytokines (TNF-α, IL-6) in ganglion tissue |
| Impaired Reflex Arcs | Blunted baroreflex sensitivity, leading to loss of inhibitory control on sympathetic centers [1] [3] | Baroreflex sensitivity (BRS) testing (phenylephrine method) |
Parasympathetic Withdrawal: The Lost Counter-Regulation
Parasympathetic withdrawal in HFrEF removes a critical protective influence on the heart. The vagus nerve exerts inhibitory control on heart rate, contractility, and also appears to modulate anti-inflammatory and reparative pathways [1]. Key mechanisms of its withdrawal include:
- Blunted Baroreflex and Bezold-Jarisch Reflex: These reflexes, which normally augment parasympathetic activity in response to blood pressure changes or ventricular stimuli, are significantly desensitized in HF [1].
- Afferent Signaling Defects: Damage to or dysfunction of vagal afferent fibers disrupts the critical feedback to the brainstem, reducing parasympathetic efferent output [1].
- Central Integration Deficits: Remodeling within the medullary and higher cortical centers of the CAN can shift the autonomic set-point toward relative sympathetic dominance [1].
The interplay between these pathways creates a vicious cycle of autonomic dysregulation, as illustrated below.
Diagram 2: The vicious cycle of autonomic imbalance in HFrEF, showing how sympathetic overdrive and parasympathetic withdrawal reinforce each other to drive disease progression.
Quantitative Data Synthesis in HFrEF Autonomic Dysfunction
Table 2: Quantitative Summary of Autonomic Dysfunction Markers and Therapeutic Impacts in HFrEF
| Parameter / Intervention | Baseline in HFrEF | Impact of Guideline-Directed Medical Therapy (GDMT) | Impact of Neuromodulation (e.g., BAT) |
|---|---|---|---|
| Heart Rate Variability (HRV) | Markedly decreased; strong independent predictor of mortality [1] | Improved with β-blockers [1] | Significantly increased, indicating restored autonomic balance [3] |
| Muscle Sympathetic Nerve Activity (MSNA) | Sustained elevation; correlates with disease severity [1] [2] | Reduced by β-blockers and ARNIs [4] | Directly targeted for reduction [2] |
| Circulating Norepinephrine | 2-3x elevated vs. healthy controls; prognostic for outcomes [1] | Modulated by comprehensive GDMT [4] | - |
| Baroreflex Sensitivity (BRS) | Blunted (>50% reduction); promotes hemodynamic instability [1] | - | Primary target; BAT directly restores BRS [3] |
| Left Ventricular Ejection Fraction (LVEF) | Severely reduced (e.g., ≤30%) [5] | Foundation: ARNI, β-blocker, MRA, SGLT2i can gain ~5 life-years [4] [6] | Case reports show improvements (e.g., 21% to 30% over 2 years) [5] |
| NT-proBNP | Elevated (>560 pg/mL in persistent HF) [7] | ARNIs, SGLT2is significantly reduce levels [4] [6] | Case reports show significant reduction post-BAT [5] |
| 6-Minute Walk Test (6MWT) | Reduced distance, indicating poor functional capacity | SGLT2is improve KCCQ scores (symptom/frequency) [4] [6] | Improved exercise capacity post-BAT [5] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Models for Investigating Autonomic Dysregulation in HFrEF
| Research Tool / Category | Specific Examples | Primary Application & Function |
|---|---|---|
| In Vivo Disease Models | Post-myocardial infarction (rat/mouse), Transverse Aortic Constriction (TAC) mouse, Canine rapid-pacing model | Recapitulate human HFrEF progression, sympathetic overdrive, and baroreflex impairment for pathophysiological and therapeutic studies. |
| Autonomic Function Assessment | ECG Telemetry, Microneurography (MSNA), Baroreflex Sensitivity Assay (phenylephrine method) | Quantify heart rate variability, direct sympathetic nerve firing, and reflex arc integrity in conscious animals or humans. |
| Molecular & Cellular Analysis | β-AR Radioligand Binding ([³H]-CGP-12177), Single-Cell RNA-Seq, Immunofluorescence (Tyrosine Hydroxylase, ChAT) | Measure receptor density and signaling, profile neuronal gene expression, and identify sympathetic/parasympathetic neurons in tissue. |
| Neuromodulation Probes | Vagus Nerve Stimulation (VNS) Cuff, Baroreflex Activation Therapy (BAT) Device, Optogenetic Viruses (ChR2, eNpHR) | Test causal links between neural circuits and cardiac function; explore therapeutic mechanisms of neuromodulation. |
| Key Biochemical Assays | ELISA for Norepinephrine, NT-proBNP, TNF-α/IL-6 | Quantify plasma/serum levels of catecholamines, heart failure stress biomarkers, and inflammatory cytokines. |
Experimental Protocols for Assessing Autonomic Function
Protocol: Serial Assessment of Baroreflex Sensitivity in a Rodent HFrEF Model
Purpose: To quantitatively track the progression of baroreflex impairment and evaluate the efficacy of therapeutic interventions like BAT.
Materials:
- Anesthetized or conscious telemetry-implanted HFrEF model rodents.
- Data acquisition system with real-time hemodynamic monitoring (Blood Pressure, ECG).
- Catheter for intravenous drug infusion.
- Agonists: Phenylephrine (for vagal-mediated bradycardia) and Sodium Nitroprusside (for sympathetically-mediated tachycardia).
Methodology:
- Baseline Recording: Stabilize animal and record baseline arterial pressure (AP) and heart rate (HR) for at least 10 minutes.
- Pharmacological Challenge:
- Vagal Cardio-inhibition Protocol: Administer a bolus of phenylephrine (1-5 µg/kg, IV) to induce a transient rise in systolic AP (20-30 mmHg).
- Sympathetic Excitation Protocol: Administer a bolus of sodium nitroprusside (5-15 µg/kg, IV) to induce a transient drop in systolic AP (20-30 mmHg).
- Data Analysis:
- For each heartbeat during the pressure change, plot the systolic AP against the subsequent pulse interval (or R-R interval).
- Calculate BRS as the slope of the linear regression line (ms/mmHg) for the ramp phase of the pressure rise (phenylephrine) or fall (nitroprusside). A steeper slope indicates better reflex function.
- Longitudinal Application: Perform this protocol at predefined stages post-HF induction (e.g., 2, 4, 8 weeks) and pre/post neuromodulatory therapy.
Protocol: Immunohistochemical Analysis of Stellate Ganglion Remodeling
Purpose: To investigate structural and inflammatory changes (e.g., hyperactivation of glial cells, neuronal hypertrophy) within the sympathetic ganglia in HFrEF.
Materials:
- Harvested stellate ganglia from terminal animal models or human biopsies.
- Primary antibodies: Anti-Tyrosine Hydroxylase (TH, sympathetic neuron marker), Anti-Iba1 (microglial/macrophage marker), Anti-GFAP (astroglial/satellite glial cell marker).
- Fluorescently-conjugated secondary antibodies.
- Confocal microscope.
Methodology:
- Tissue Preparation: Perfuse-fix animal, dissect stellate ganglia, and post-fix. Cryoprotect and section ganglia at 10-20 µm thickness.
- Immunostaining: Perform standard immunofluorescence protocol: block, incubate with primary antibody cocktail, wash, incubate with secondary antibodies, and mount.
- Image Acquisition & Quantification:
- Acquire high-resolution z-stack images using a confocal microscope.
- Quantify TH+ area and neuronal soma size as an index of sympathetic hyperactivity.
- Quantify Iba1+ and GFAP+ cell density and morphology (shift from ramified to amoeboid indicates activation) within the ganglion.
- Use image analysis software (e.g., ImageJ) for thresholding and particle analysis.
- Correlation: Correlate morphological findings with functional data (e.g., MSNA, plasma NE) from the same subject.
Baroreflex Activation Therapy: A Pathophysiologically-Targeted Intervention
Baroreflex Activation Therapy (BAT) represents a direct, device-based intervention designed to interrupt the cycle of autonomic imbalance at the level of a key reflex arc [3] [2] [5].
Mechanism of Action
BAT involves the electrical stimulation of carotid sinus baroreceptors. This mimics a state of chronic high blood pressure, leading to:
- Increased afferent signaling to the nucleus tractus solitarius (NTS) in the brainstem [3].
- Central-mediated reduction in sympathetic outflow to the heart, kidneys, and peripheral vasculature [3] [2].
- Simultaneous increase in parasympathetic (vagal) tone [3].
This mechanism is summarized in the pathway below.
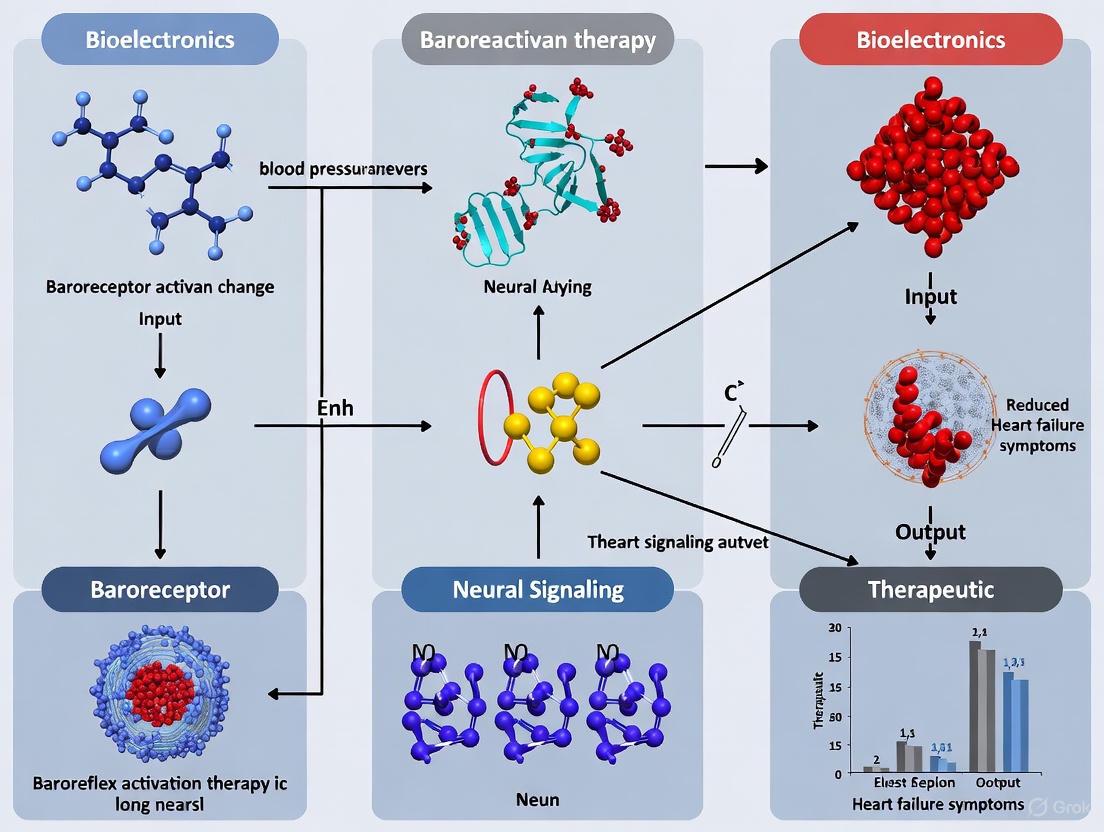
Diagram 3: Mechanism of Baroreflex Activation Therapy (BAT). Electrical stimulation of baroreceptors centrally restores autonomic balance by suppressing sympathetic nerve activity and enhancing parasympathetic tone.
Supporting Clinical Evidence
- Patient Profile: BAT is indicated for symptomatic HFrEF patients (NYHA Class III) who remain on optimal guideline-directed medical therapy (GDMT) and are unsuitable for cardiac resynchronization therapy (CRT) [3] [7] [5].
- Outcomes: A 2-year follow-up of severe HFrEF patients demonstrated that BAT led to:
- Therapeutic Context: BAT is a complement to, not a replacement for, GDMT and acts by modulating the autonomic nervous system to improve symptoms and quality of life [3].
Baroreceptor dysfunction represents a critical pathophysiological mechanism in the progression of heart failure (HF), characterized by impaired autonomic nervous system regulation. In healthy individuals, the baroreflex serves as a primary homeostatic mechanism, providing beat-to-beat regulation of circulatory homeostasis through modulation of sympathetic and parasympathetic outflow [8]. However, in heart failure, this refined control system becomes compromised, leading to a sustained sympathetic overdrive that adversely affects cardiac function, promotes adverse remodeling, and increases mortality risk [8] [9].
This document details the mechanisms underlying baroreceptor dysfunction in heart failure and establishes standardized experimental protocols for investigating baroreflex activation therapy (BAT), a device-based intervention designed to counteract autonomic imbalance in advanced HF patients. The content is structured to provide researchers and drug development professionals with comprehensive methodological frameworks for both basic investigation and clinical application of neuromodulatory approaches for heart failure.
Pathophysiology of Baroreceptor Dysfunction
Anatomical and Physiological Foundations
Baroreceptors are mechanosensitive nerve endings predominantly located in the carotid sinus and aortic arch, with the highest density found at the carotid sinus bifurcation [8] [10]. These receptors function as sophisticated sensors of arterial wall stretch, transmitting continuous feedback on blood pressure dynamics to the brainstem via the glossopharyngeal and vagus nerves [8].
Under physiological conditions, increased arterial pressure stretches these receptors, leading to:
- Inhibition of sympathetic outflow from the vasomotor center
- Activation of parasympathetic activity through the vagal nucleus
- Reduction in heart rate, cardiac contractility, and systemic vascular resistance
- Enhanced renal sodium and water excretion [8]
This integrated response normalizes blood pressure through a negative feedback loop that maintains cardiovascular homeostasis despite varying physiological demands and stressors.
Mechanisms of Impaired Baroreceptor Signaling in HF
In heart failure, multiple interdependent mechanisms contribute to baroreceptor dysfunction and impaired reflex control:
Baroreceptor Desensitization: Chronic elevation of intracardiac filling pressures and arterial stiffness in HF patients leads to reduced baroreceptor sensitivity through structural and functional alterations. The baroreceptors themselves become less responsive to changes in arterial pressure, effectively raising the threshold for activation and diminishing the gain of the reflex arc [8] [10].
Central Integration Deficits: Heart failure disrupts the processing of baroreceptor signals within the nucleus tractus solitarius and other brainstem centers. This central component of baroreflex impairment results from neurohormonal activation, inflammatory mediators, and oxidative stress that collectively alter neuronal function and synaptic transmission [8].
Neurohormonal Activation: The compensatory activation of the renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system in HF creates a vicious cycle. Elevated angiotensin II levels directly potentiate sympathetic outflow and further impair baroreflex function, while increased circulating catecholamines contribute to target organ damage and progressive ventricular remodeling [8] [9].
Table 1: Key Mechanisms of Baroreceptor Dysfunction in Heart Failure
| Dysfunction Mechanism | Pathophysiological Consequences | Clinical Manifestations |
|---|---|---|
| Baroreceptor Desensitization | Reduced afferent signaling to CNS | Diminished heart rate variability, blunted BP responses |
| Central Integration Deficits | Impaired sympathoinhibition | Sustained sympathetic activation, vagal withdrawal |
| Neurohormonal Activation | RAAS and sympathetic nervous system overactivity | Sodium retention, vasoconstriction, cardiac remodeling |
| Structural Vascular Changes | Reduced arterial compliance | Diminished baroreceptor stimulation, elevated systolic BP |
Baroreflex Activation Therapy (BAT): Experimental and Clinical Evidence
BAT System Components and Mechanism of Action
Baroreflex activation therapy utilizes an implantable system designed to electrically stimulate carotid baroreceptors, thereby restoring autonomic balance. The system comprises three primary components [10]:
- Carotid electrode: A 2mm electrode placed surgically on the adventitial surface of the carotid sinus
- Implantable pulse generator (IPG): Typically placed in a subcutaneous pectoral pocket
- Connecting lead: Tunneled subcutaneously between the carotid electrode and IPG
The therapeutic mechanism involves chronic electrical stimulation of carotid baroreceptors, which increases afferent signaling to the brainstem, resulting in:
- Reduced central sympathetic outflow
- Increased parasympathetic/vagal tone
- Subsequent reductions in peripheral vascular resistance, heart rate, and RAAS activation [10] [9]
This autonomic rebalancing addresses the core neurohormonal disturbances that drive heart failure progression.
Quantitative Clinical Outcomes of BAT
Recent clinical studies have demonstrated consistent benefits of BAT across multiple domains of heart failure severity. The following table summarizes key quantitative outcomes from clinical investigations:
Table 2: Clinical Outcomes of Baroreflex Activation Therapy in Heart Failure with Reduced Ejection Fraction (HFrEF)
| Outcome Measure | Baseline Value | Follow-up Period | Change from Baseline | Statistical Significance |
|---|---|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | 23 ± 8% | 1 year | +9 ± 9% | P < 0.001 [11] |
| LVEF | 23 ± 8% | 2 years | +11 ± 9% | P = 0.005 [11] |
| NT-proBNP | 2463 ± 2922 pg/mL | 1 year | -396 ± 1006 pg/mL | NS [11] |
| NT-proBNP | 2463 ± 2922 pg/mL | 2 years | -566 ± 651 pg/mL | P = 0.039 [11] |
| 6-Minute Hall Walk Distance | Not specified | 6 months | +50 meters | P = 0.05 [9] |
| NYHA Class Improvement | 96% Class III | 1 year | 52% improved | Not specified [11] |
Long-term follow-up data extending to 7.5 years demonstrates that BAT-induced improvements in functional capacity and ventricular function can be sustained in many patients, highlighting the potential durability of this neuromodulatory approach [11].
Experimental Protocols for BAT Research
Preclinical Assessment of Baroreflex Function
Protocol Objective: To evaluate baroreflex sensitivity (BRS) in animal models of heart failure prior to BAT intervention.
Materials and Reagents:
- Anesthetized or conscious animal preparation with telemetry
- Phenylephrine (1-5 µg/kg IV) for blood pressure elevation
- Sodium nitroprusside (1-5 µg/kg IV) for blood pressure reduction
- Data acquisition system with continuous arterial pressure monitoring
- ECG recording equipment
- Analysis software for heart rate and blood pressure variability
Methodology:
- Instrument animals with arterial pressure telemetry transducers and allow 7-10 days recovery.
- Establish baseline hemodynamic measurements over 30 minutes of stable recording.
- Administer sequential bolus injections of phenylephrine and sodium nitroprusside in randomized order with adequate recovery between doses.
- Record continuous arterial pressure and heart rate responses throughout.
- Analyze the relationship between systolic blood pressure changes and corresponding heart period (R-R interval) changes using linear regression.
- Calculate BRS as the slope of the regression line (ms/mmHg) for both pressor and depressor responses.
Interpretation: Impaired BRS in HF models typically manifests as a flattening of the slope (<1.0 ms/mmHg versus >2.5 ms/mmHg in controls), indicating reduced baroreflex-mediated heart rate responses to blood pressure changes [8].
Clinical BAT Implantation and Titration Protocol
Protocol Objective: To standardize patient selection, surgical implantation, and therapy titration of BAT systems in clinical research settings.
Inclusion Criteria:
- NYHA Class II or III heart failure
- Left ventricular ejection fraction ≤35%
- Refractory symptoms despite guideline-directed medical therapy (GDMT)
- Not a candidate for cardiac resynchronization therapy (CRT)
- Carotid anatomy suitable for implantation (minimal atherosclerosis, <50% stenosis) [10]
Exclusion Criteria:
- Previous carotid stenting or endarterectomy on target artery
- Significant carotid stenosis (≥50%)
- Uncontrolled atrial fibrillation
- Life expectancy <1 year from non-cardiac causes
Surgical Implantation Procedure:
- Perform preoperative carotid duplex ultrasound to confirm anatomical suitability.
- Under general anesthesia, make a small transverse incision in the neck over the carotid bifurcation, localized via ultrasound.
- Expose the anterior surface of the carotid bifurcation and proximal internal carotid artery with minimal dissection to preserve the carotid sinus nerve.
- Perform intraoperative mapping to identify the optimal stimulation site by applying test stimulation (1-6V, 10-150µs) and observing blood pressure responses.
- Secure the electrode to the adventitia using six 6-0 Prolene sutures.
- Tunnel the lead subcutaneously to a pectoral pocket and connect to the implantable pulse generator.
- Close incisions in layers and confirm device integrity post-implantation [10].
Therapy Titration Protocol:
- Initiate BAT 2-4 weeks post-implantation to allow surgical recovery.
- Program initial settings: voltage 1.0V below perception threshold, pulse width 110-150µs, frequency 20-40Hz.
- Up-titrate amplitude weekly over 4-8 weeks to achieve maximal tolerated level without discomfort.
- Assess therapeutic response via NYHA class, quality of life questionnaires, and 6-minute walk test at monthly intervals.
- Optimize medical therapy concurrently with BAT titration, with particular attention to diuretic adjustment as hemodynamics improve [10].
Research Reagent Solutions and Materials
Table 3: Essential Research Materials for Baroreflex Dysfunction and BAT Investigations
| Category/Item | Specification/Model | Research Application |
|---|---|---|
| BAT Systems | Barostim neo System | Clinical research on BAT efficacy and safety [10] |
| BAT Systems | Rheos System | First-generation BAT device for historical comparisons [9] |
| Assessment Tools | Carotid Duplex Ultrasound | Pre-implantation anatomical screening [10] |
| Assessment Tools | 6-Minute Walk Test Equipment | Functional capacity assessment [9] |
| Biomarker Assays | NT-proBNP ELISA Kits | Quantitative assessment of cardiac strain [11] |
| Pharmacological Agents | Phenylephrine, Sodium Nitroprusside | Baroreflex sensitivity testing [8] |
| Implant Materials | 6-0 Prolene Sutures | Electrode fixation during implantation [10] |
Signaling Pathways and Methodological Workflows
Baroreflex Pathway and BAT Mechanism
Diagram 1: Baroreflex Pathways in Normal Physiology, Heart Failure, and with BAT Intervention. BAT electrically stimulates carotid baroreceptors to restore autonomic balance despite underlying baroreceptor dysfunction in HF [8] [10] [9].
BAT Research and Clinical Implementation Workflow
Diagram 2: BAT Clinical Implementation and Research Workflow. Standardized protocol from patient selection through long-term outcomes assessment for consistent research application and clinical care [11] [10].
Baroreceptor dysfunction constitutes a fundamental mechanism in heart failure progression, characterized by impaired afferent signaling, central integration deficits, and consequent autonomic imbalance. Baroreflex activation therapy represents a promising neuromodulatory approach that directly addresses this pathophysiology through chronic electrical stimulation of carotid baroreceptors.
The experimental protocols and methodological frameworks presented herein provide standardized approaches for investigating baroreceptor dysfunction and applying BAT in both basic and clinical research settings. The consistent improvements in functional capacity, ventricular function, and biomarker profiles observed in long-term studies underscore the potential of autonomic modulation as a therapeutic strategy in advanced heart failure.
Future research directions should focus on optimizing patient selection criteria, refining stimulation parameters, and exploring potential applications in heart failure with preserved ejection fraction, where autonomic imbalance similarly contributes to disease progression.
Chronic Heart Failure (HF), particularly with a reduced ejection fraction (HFrEF), is characterized by a progressive autonomic dysregulation that significantly contributes to disease progression and mortality. This dysregulation manifests as a sustained increase in sympathetic drive coupled with a withdrawal of parasympathetic activity [12]. For decades, the primary pharmacological strategy has targeted this imbalance through partial sympathetic inhibition, most successfully with beta-adrenergic receptor blockers. However, the potential of modulating parasympathetic activation remained a relatively unexplored frontier [12]. Neuromodulation, specifically Baroreflex Activation Therapy (BAT), has emerged as a novel device-based approach to directly address this autonomic imbalance. BAT represents a paradigm shift, moving beyond neurohormonal blockade to active restoration of neurovascular equilibrium. This article details the scientific rationale, experimental protocols, and key methodological tools for investigating BAT within a preclinical and clinical HFrEF research framework.
Pathophysiological Rationale and Historical Context
The historical understanding of HF has evolved from a purely hemodynamic model to one that recognizes the central role of neurohormonal activation. The autonomic dysfunction in HF is characterized by sympathetic overactivation and parasympathetic withdrawal, which are independent predictors of poor long-term outcome [12] [13]. This imbalance is perpetuated by a critically impaired baroreflex system; the arterial baroreceptors, which normally inhibit sympathetic outflow, exhibit reduced sensitivity in HF, allowing sympathetic excitation to proceed unchecked [12].
The rationale for BAT is founded on correcting this fundamental defect. Baroreceptors located in the carotid sinus are activated by increases in blood pressure and volume, leading to sympathetic inhibition and parasympathetic activation. BAT delivers electrical stimulation to these carotid baroreceptors, thereby augmenting this diminished reflex [14]. Pre-clinical animal studies provided the foundational evidence, demonstrating that chronic BAT improves global left ventricular (LV) systolic and diastolic function, partially reverses LV remodeling, and markedly increases the threshold for lethal ventricular arrhythmias in dogs with advanced HF [12]. This body of work established the proof-of-concept that directly restoring autonomic balance through device-based intervention could yield significant therapeutic benefits, paving the way for human studies.
Quantitative Evidence from Preclinical and Clinical Studies
Research across animal models and human clinical trials has consistently demonstrated the functional and structural benefits of BAT. The tables below summarize key quantitative findings.
Table 1: Preclinical Outcomes of BAT in Canine Heart Failure Models (3-6 month follow-up)
| Parameter | Sham-Control Group | BAT-Treated Group | P-value |
|---|---|---|---|
| LV Ejection Fraction (%) | No significant improvement | Significant increase | < 0.05 |
| LV End-Systolic Volume | No significant change | Significant decrease | < 0.05 |
| LV End-Diastolic Volume | No significant change | Significant decrease | < 0.05 |
| Volume Fraction of Replacement Fibrosis | No significant change | ~40% reduction | < 0.05 |
| Reactive Interstitial Fibrosis | No significant change | ~22% reduction | < 0.05 |
| Threshold for Ventricular Arrhythmias | Decreased | Markedly increased | < 0.05 |
| Heart Rate (Average, from Holter) | Increased from 69 to 76 bpm | Decreased from 92 to 64 bpm | Not Significant (trend) |
Table 2: Clinical Outcomes of BAT in HFrEF Patients (1-2 year follow-up)
| Parameter | Baseline (Pre-BAT) | Follow-Up (Post-BAT) | Study Reference |
|---|---|---|---|
| LVEF (%) | 23 - 34% | +9 to +11% absolute improvement | [5] [15] [11] |
| NYHA Class | Class III | Improved to Class II (52-100% of patients) | [5] [15] [11] |
| 6-Minute Walk Distance | 234 - 281 m | Significant Increase | [15] [14] |
| NT-proBNP | 2302 - 2532 pg/mL | -24% to -37% reduction | [5] [15] |
| Quality of Life (MLHFQ Score) | Elevated | Significant Improvement | [14] |
| HF Hospitalization Rate | High | 50% reduction vs. control | [15] |
Experimental Protocols
Preclinical Large Animal Protocol (Canine Model)
This protocol is adapted from established studies using canine models of coronary microembolization-induced HF [12].
Aim: To evaluate the long-term effects of BAT on LV function, remodeling, and arrhythmogenicity in advanced HF. Animal Model: Adult canines. Heart Failure Induction: Serial coronary microembolizations via intracoronary catheter to achieve an LVEF of ~25-30%. BAT System Implantation:
- Device: Rheos System or Barostim neo (CVRx, Inc.)
- Procedure: Under general anesthesia, stimulating electrodes are implanted circumferentially around both carotid sinuses and tunneled to connect to an implantable pulse generator placed in a pectoral subcutaneous pocket.
- Acute Efficacy Test: 3-4 acute stimulation runs are performed intra-operatively to confirm a drop in blood pressure and heart rate, verifying proper electrode placement.
Randomization & Grouping:
- Animals are randomized post-HF induction.
- BAT Group (Active): n=7-8. Device activated with predetermined parameters (e.g., 0.5 msec square wave pulses at 50-100Hz, duty cycle of 9 minutes ON/1 minute OFF).
- Control Group (Sham): n=6-7. Device implanted but not activated.
Follow-up & Endpoint Assessment (3-6 months):
- Hemodynamics: LV pressure-volume loop analysis under conscious conditions.
- LV Function & Remodeling: Quantitative ventriculography or echocardiography to measure LV volumes, EF, and sphericity index.
- Electrophysiology (Terminal): Programmed electrical stimulation to determine the ventricular fibrillation threshold.
- Ambulatory Monitoring: 24-hour Holter ECG for heart rate variability and arrhythmia burden.
- Tissue Analysis: Histomorphometric analysis of myocardial fibrosis (volume fraction) and capillary density.
Clinical Research Protocol for BAT in HFrEF
This protocol outlines a prospective study design for evaluating BAT in human patients, based on recent clinical investigations [15] [11].
Aim: To assess the safety, efficacy, and long-term outcomes of BAT in patients with advanced HFrEF. Study Design: Prospective, single or multi-center, with an optional control group of patients receiving only guideline-directed medical therapy (GDMT). Patient Population:
- Inclusion Criteria: Chronic HFrEF (LVEF ≤35%), NYHA Functional Class III, optimized and stable GDMT for >3 months, unsuitable for or non-responsive to Cardiac Resynchronization Therapy (CRT).
- Exclusion Criteria: Significant carotid artery disease, recent myocardial infarction, or other conditions contraindicating device implantation.
Baseline Assessment:
- Clinical: NYHA class, quality of life questionnaire (e.g., MLHFQ, KCCQ), 6-minute hall walk test (6MHWD).
- Cardiac Function: Transthoracic echocardiography (LVEF, volumes), 12-lead ECG.
- Biomarkers: Plasma NT-proBNP levels.
- Autonomic Function: Muscle sympathetic nerve activity (MSNA) and baroreflex sensitivity assessment.
BAT Implantation and Titration:
- Device: Barostim neo system.
- Procedure: Implantation of the lead on the carotid sinus and pulse generator in the pectoral region, performed under local or general anesthesia.
- Activation: Device is activated 2-4 weeks post-implantation. Stimulation parameters are titrated to the maximum tolerated level that does not cause discomfort or significant drops in blood pressure.
Follow-up Schedule (3, 6, 12 months and annually):
- Repeat all baseline assessments at each visit.
- Device Interrogation: Check battery status and system integrity.
- Safety Monitoring: Record all adverse events, particularly system or procedure-related complications.
Primary Efficacy Endpoints:
- Improvement in NYHA class and QoL score.
- Increase in LVEF and 6MHWD.
- Reduction in NT-proBNP levels and HF hospitalization rates.
Signaling Pathways and Workflow Visualization
Diagram 1: BAT Mechanism in HFrEF. This diagram illustrates the core pathophysiology of heart failure and the mechanism of action of Baroreflex Activation Therapy. BAT counters baroreflex dysfunction by stimulating carotid baroreceptors, leading to sympathetic inhibition and parasympathetic activation, which improves clinical outcomes.
Diagram 2: Clinical BAT Workflow. This flowchart outlines the standard clinical protocol for implementing Baroreflex Activation Therapy, from patient selection and screening to long-term follow-up and outcome assessment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for BAT Research
| Item | Function/Application in Research |
|---|---|
| Barostim neo System (CVRx) | Second-generation, FDA-approved implantable device for delivering BAT; used in clinical and translational large animal studies [15] [14]. |
| Rheos System (CVRx) | First-generation BAT implantable system; foundational for preclinical proof-of-concept studies in large animals [12]. |
| Canine Coronary Microembolization Model | Established large animal model of ischemic HFrEF for preclinical testing of BAT efficacy on LV remodeling and function [12]. |
| Muscle Sympathetic Nerve Activity (MSNA) | Direct micronurographic measurement of postganglionic sympathetic nerve traffic; a gold-standard endpoint for assessing autonomic effects of BAT in humans [13] [14]. |
| N-terminal pro-B-type Natriuretic Peptide (NT-proBNP) | Key circulating biomarker of wall stress and HF severity; used to track reverse remodeling and therapeutic response to BAT [5] [15] [11]. |
| Minnesota Living with Heart Failure Questionnaire (MLHFQ) | Validated patient-reported outcome tool to quantify quality of life improvements in clinical BAT trials [14]. |
| 6-Minute Hall Walk Test (6MHWD) | Simple, functional assessment of exercise capacity and symptomatic improvement in response to BAT [15] [14]. |
Anatomy of the Carotid Sinus Baroreceptors and Afferent Pathways to the Brain
The carotid sinus baroreceptors are pivotal components of the body's rapid blood pressure regulation system, functioning as high-pressure mechanoreceptors that continuously monitor arterial pressure. Within the context of heart failure research, understanding the anatomy and afferent pathways of the carotid sinus is fundamental for developing baroreflex activation therapies. These therapeutic approaches aim to modulate the autonomic nervous system imbalance characteristic of heart failure by electrically stimulating the carotid sinus baroreceptors, thereby reducing sympathetic outflow and increasing parasympathetic tone—a mechanism known as the baroreflex. This application note provides a detailed anatomical and methodological framework for researching baroreceptor function and its therapeutic application in heart failure.
Anatomical Structure of the Carotid Sinus and Baroreceptors
The carotid sinus, also known as the carotid bulb, is a specialized neurovascular structure located at the bifurcation of the common carotid artery and the proximal aspect of the internal carotid artery [16] [17]. It is typically found at the level of the superior border of the thyroid cartilage (approximately C4 vertebra) [16] [18]. This structure presents as a slight dilation in the arterial wall and is strategically positioned to detect changes in arterial blood pressure [17].
Table 1: Anatomical Characteristics of the Carotid Sinus
| Feature | Description |
|---|---|
| Location | Bifurcation of common carotid artery, proximal internal carotid artery [16] [17] |
| Anatomical Level | Superior border of thyroid cartilage (C4 vertebra) [16] [18] |
| Embryological Origin | Third pharyngeal arch [16] |
| Innervation | Carotid sinus nerve (branch of glossopharyngeal nerve - CN IX) [16] [19] |
| Blood Supply | Vasa vasorum vessels [16] |
The baroreceptors within the carotid sinus are specialized mechanoreceptors that detect pressure-induced stretch in the arterial wall [20]. These spray-type nerve endings are located primarily in the adventitial layer of the carotid bulb and are exquisitely sensitive to both static and dynamic changes in arterial pressure [16]. Research has identified two distinct types of baroreceptors with different functional characteristics, as outlined in Table 2.
Table 2: Functional Classification of Carotid Sinus Baroreceptors
| Baroreceptor Type | Nerve Fiber Type | Response Characteristics | Functional Role |
|---|---|---|---|
| Type 1 (Dynamic) | Large, myelinated A-fibers [16] [21] | Rapid, dynamic response to pressure changes [16] | Second-to-second blood pressure monitoring and maintenance [21] |
| Type 2 (Tonic) | Small A-fibers and unmylelinated C-fibers [16] [21] | Sustained, tonic response to maintained pressure [16] | Basal control of blood pressure and heart rate [21] |
The carotid sinus exhibits significant anatomical variation between individuals, which has important implications for surgical interventions and research methodologies. A classification system identifies four variations in carotid sinus location, with the most common (74.3% of cases) extending from the distal common carotid artery to the proximal internal carotid artery [16].
Neuroanatomy of Afferent Pathways
The afferent pathway from carotid baroreceptors to the brain follows a precisely organized neural circuit that enables rapid cardiovascular adjustment. Understanding this pathway is crucial for developing baroreflex activation therapies for heart failure.
Peripheral Innervation and Signal Transduction
The carotid sinus is primarily innervated by the carotid sinus nerve, which is a branch of the glossopharyngeal nerve (cranial nerve IX) [20] [16] [19]. This nerve contains the afferent fibers responsible for transmitting baroreceptor signals to the central nervous system. The carotid sinus nerve demonstrates multiple communication sites with the sympathetic trunk (frequently at the level of the superior cervical ganglion) and vagal trunk [21].
Baroreceptor signal transduction occurs through mechanosensitive ion channels in the baroreceptor nerve endings. These channels belong to the transient receptor potential (TRP) family, with TRP1 being particularly sensitive to stretch [16]. When arterial pressure increases, the vessel wall expands, producing an inward current that depolarizes the receptor, generating a receptor potential with an amplitude proportional to the degree of vascular stretch [16].
Central Pathway Integration
The primary central termination site for baroreceptor afferent fibers is the nucleus tractus solitarius (NTS) in the dorsolateral medulla oblongata [20] [22]. The NTS serves as the central integration center for cardiovascular control, receiving and processing input from various visceral sensory systems [22].
After processing in the NTS, signals are relayed to other brainstem nuclei, including the nucleus ambiguus and the caudal ventrolateral medulla, which subsequently project to the rostral ventrolateral medulla—the primary regulator of sympathetic outflow [20]. This integrated system allows for precise modulation of autonomic nervous system activity in response to blood pressure changes.
Figure 1: Carotid Baroreceptor Reflex Pathway. This diagram illustrates the complete neural pathway from pressure detection at the carotid sinus to compensatory physiological responses that restore blood pressure homeostasis.
Baroreceptor Reflex Physiology and Heart Failure Implications
The baroreflex functions as a negative feedback loop that maintains arterial pressure within a narrow physiological range. In the context of heart failure research, understanding this reflex is critical, as heart failure is characterized by baroreflex impairment and chronic sympathetic overactivity.
Normal Baroreflex Response Mechanisms
When arterial pressure increases, the carotid sinus wall stretches, enhancing baroreceptor firing frequency [20] [21]. This increased afferent signaling to the NTS results in two primary efferent responses:
- Increased parasympathetic outflow to the sinoatrial node, reducing heart rate
- Decreased sympathetic outflow to peripheral blood vessels, reducing vascular resistance and cardiac contractility [20]
Conversely, decreased arterial pressure reduces baroreceptor stretch and firing, leading to disinhibition of sympathetic centers and increased sympathetic outflow, resulting in vasoconstriction and increased heart rate [20] [22].
Pathophysiological Changes in Heart Failure
In heart failure, the baroreflex undergoes significant impairment, termed "baroreflex desensitization," which contributes to disease progression through several mechanisms:
- Reduced sensitivity to pressure changes
- Elevated sympathetic nervous system activity
- Diminished parasympathetic tone
- Resetting of the baroreflex to higher pressure set points
This pathophysiological understanding forms the basis for baroreflex activation therapy, which aims to artificially stimulate the carotid sinus to restore autonomic balance in heart failure patients.
Experimental Protocols for Baroreceptor Research
Carotid Sinus Massage Protocol for Baroreflex Sensitivity Assessment
Carotid sinus massage is a diagnostic procedure used to evaluate baroreflex sensitivity, particularly in research settings investigating autonomic function in cardiovascular diseases.
Table 3: Carotid Sinus Massage Protocol for Research Applications
| Protocol Step | Technical Specifications | Safety Considerations |
|---|---|---|
| Pre-procedure Screening | Duplex ultrasound to exclude carotid plaque/thrombus [16] | Absolute contraindication: carotid stenosis >50%, recent TIA/stroke (<3 months) [16] |
| Patient Positioning | Supine with neck slightly extended [16] | Equipment for resuscitation must be available [16] |
| Massage Technique | Gentle circular pressure over carotid bifurcation for 5-10 seconds [16] | Avoid bilateral simultaneous massage; monitor ECG and BP continuously [16] |
| Response Monitoring | Beat-to-beat HR/BP monitoring; document asystole >3s (cardioinhibition) or SBP drop >50 mmHg (vasodepression) [16] | Terminate immediately upon significant bradycardia or hypotension [16] |
Surgical Denervation Protocol for Mechanistic Studies
Surgical denervation of the carotid sinus is employed in animal models to study the specific contributions of baroreceptors to cardiovascular regulation, particularly in heart failure research.
Procedure:
- Anesthetize subject using approved institutional protocol (e.g., ketamine-xylazine for rodents)
- Make ventral midline incision in neck and expose carotid bifurcation
- Identify carotid sinus nerve branching from glossopharyngeal nerve
- Carefully dissect connective tissue around carotid sinus
- Apply 1% lidocaine topically to abolish nerve activity
- Either transect carotid sinus nerve or chemically denervate using 10% phenol application
- Confirm denervation efficacy by absence of heart rate response to phenylephrine-induced pressure elevation
Validation Measures:
- Absence of bradycardia response to phenylephrine (5 μg/kg IV)
- Loss of sympathetic inhibition during blood pressure elevation
- Histological verification of nerve degeneration
In Vitro Carotid Sinus Preparation for Electrophysiological Studies
The in vitro carotid sinus preparation allows direct investigation of baroreceptor properties without systemic influences.
Tissue Preparation:
- Harvest carotid bifurcation and transfer to oxygenated (95% O₂, 5% CO₂) physiological salt solution (PSS) at 4°C
- Cannulate common carotid artery and external carotid artery
- Connect internal carotid artery to pressure servo-system
- Maintain tissue viability with perfusate containing (in mM): NaCl 118, KCl 4.7, CaCl₂ 2.5, MgSO₄ 1.2, NaHCO₃ 25, KH₂PO₄ 1.2, glucose 5.6
Nerve Recording:
- Identify carotid sinus nerve and place on platinum-iridium recording electrodes
- Apply controlled intrasinus pressure steps (50-200 mmHg)
- Record afferent nerve activity using extracellular amplification
- Analyze pressure-nerve activity relationship to determine baroreceptor gain
Baroreflex Activation Therapy for Heart Failure: Application Notes
Baroreflex activation therapy (BAT) represents a novel device-based approach for managing heart failure by electrically stimulating the carotid sinus to restore autonomic balance.
Device Implantation Protocol
The implantation of a carotid sinus stimulator requires precise surgical technique to ensure optimal electrode placement and therapeutic efficacy.
Surgical Procedure:
- Patient positioned supine with neck extended
- Incision made along anterior border of sternocleidomastoid muscle
- Carotid bifurcation exposed with careful dissection
- Carotid sinus nerve identified
- Electrode leads positioned adjacent to carotid sinus
- Pulse generator implanted in infraclavicular pocket
- System tested intraoperatively to confirm appropriate hemodynamic responses
Stimulation Parameters:
- Amplitude: 1.0-4.0 V (titrated to achieve 10-15 mmHg BP reduction)
- Pulse width: 150-500 μs
- Frequency: 20-100 Hz
- Cycling: Typically 10 seconds on, 10 seconds off
Efficacy Assessment in Heart Failure Research
Evaluation of BAT efficacy in heart failure requires comprehensive hemodynamic and functional assessment.
Table 4: Efficacy Parameters for Baroreflex Activation Therapy in Heart Failure Research
| Assessment Domain | Specific Metrics | Measurement Methodology |
|---|---|---|
| Hemodynamic Parameters | Mean arterial pressure, systemic vascular resistance, heart rate variability | Beat-to-beat blood pressure monitoring, impedance cardiography, 24-hour Holter ECG |
| Cardiac Function | Left ventricular ejection fraction, E/A ratio, left ventricular end-systolic volume | Echocardiography, cardiac MRI |
| Exercise Capacity | Peak VO₂, 6-minute walk distance, anaerobic threshold | Cardiopulmonary exercise testing, functional assessments |
| Biomarkers | Plasma norepinephrine, B-type natriuretic peptide (BNP), NT-proBNP | Venous blood sampling, ELISA assays |
| Quality of Life | Minnesota Living with Heart Failure Questionnaire, NYHA Class | Patient-reported outcome measures, clinician assessment |
Clinical studies have demonstrated that BAT can lower blood pressure by 15-25 mmHg in hypertensive patients and improve functional status in heart failure patients [19]. The therapy is particularly relevant for patients with resistant hypertension or heart failure with reduced ejection fraction who remain symptomatic despite optimal medical therapy.
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents for Carotid Baroreceptor Studies
| Reagent/Resource | Application in Baroreceptor Research | Example Usage |
|---|---|---|
| Prazosin | Alpha-1 adrenergic antagonist; blocks sympathetic vasoconstriction [21] | Studying baroreflex control of cerebral blood flow during exercise (0.1-1.0 mg/kg in rodents) [21] |
| Phenylephrine | Alpha-1 adrenergic agonist; induces acute blood pressure elevation | Assessing baroreflex sensitivity through heart rate response to pressure changes (1-5 μg/kg IV bolus) |
| Sodium Nitroprusside | Nitric oxide donor; causes rapid vasodilation and blood pressure reduction | Evaluating baroreflex function during hypotension (0.5-5.0 μg/kg/min infusion) |
| Lidocaine (1%) | Local anesthetic; chemically denervates baroreceptors [16] | Carotid sinus desensitization during endarterectomy or experimental denervation [16] |
| Phenol (10%) | Neurolytic agent; permanently destroys nerve fibers | Surgical denervation studies for long-term baroreceptor ablation |
| Artificial Cerebrospinal Fluid | Physiological solution for in vitro preparations | Maintaining tissue viability in isolated carotid sinus experiments (composition tailored to species) |
| Extracellular Recording Equipment | Measurement of afferent nerve activity | Baroreceptor single-unit or multi-unit recording from carotid sinus nerve |
Visualization of Research Methodologies
Figure 2: Baroreceptor Research Methodologies. This workflow outlines the primary experimental approaches for investigating carotid baroreceptor function in heart failure research, from human studies to cellular mechanisms.
The detailed anatomical understanding of carotid sinus baroreceptors and their afferent pathways provides a critical foundation for developing novel therapies for heart failure. Baroreflex activation therapy represents a promising approach to restore autonomic balance in heart failure by leveraging the body's innate cardiovascular control systems. Future research directions should focus on optimizing stimulation parameters, identifying patient subgroups most likely to benefit from BAT, and developing next-generation devices with closed-loop feedback control based on real-time cardiovascular metrics. The integration of advanced neuroanatomical knowledge with device-based therapeutics continues to offer promising avenues for addressing the autonomic dysfunction that characterizes advanced heart failure.
BAT Implementation: Device Technology, Surgical Techniques, and Patient Selection Protocols
Within the research landscape of autonomic regulation for heart failure (HF), the Barostim neo system (CVRx, Inc.) represents a pivotal device-based therapeutic modality. Its design is predicated on the principle of baroreflex activation therapy (BAT), which aims to correct the autonomic imbalance—characterized by persistent sympathetic overdrive and reduced parasympathetic activity—that is a hallmark of progressive heart failure [23] [9]. This application note provides a detailed technical breakdown of the Barostim system's components and presents standardized experimental protocols for the quantitative assessment of its function in a research setting, thereby providing a framework for the systematic evaluation of BAT's mechanistic and therapeutic effects.
System Components & Technical Specifications
The Barostim neo system is an implantable extravascular device comprising three primary components: a carotid sinus electrode, an implantable pulse generator (IPG), and a connecting lead [10]. The following table summarizes the quantitative and qualitative design specifications of each core component.
Table 1: Technical Specifications of the Barostim neo System Components
| Component | Design & Material Specifications | Dimensions & Physical Properties | Implantation & Fixation |
|---|---|---|---|
| Carotid Sinus Electrode | - Circular backer [23].- Active surface: A 2-mm disk electrode coated with iridium oxide [23] [10]. | - Backer diameter: 7 mm [23]. | - Secured to the carotid sinus adventitia with six 6-0 Prolene sutures [10].- Optimal site determined via intraoperative mapping [23] [10]. |
| Lead Body | - Connects the electrode to the IPG [10]. | - Length: 40 cm [23].- Tunnelled subcutaneously from the cervical incision to the infraclavicular pocket [10]. | - No leads are placed within the vascular system or heart [10] [24]. |
| Implantable Pulse Generator (IPG) | - Houses battery and control electronics. | - Approximate size: Comparable to a small implantable cardioverter defibrillator (ICD) [10]. | - Implanted in a subcutaneous infraclavicular chest wall pocket [23] [10]. |
Experimental Protocols for BAT Research
To ensure reproducible investigation of BAT, researchers should adhere to the following standardized protocols encompassing surgical implantation, device activation, and functional assessment.
Protocol for Surgical Implantation and Lead Placement
Objective: To surgically implant the Barostim carotid electrode and IPG with high reproducibility and minimal morbidity. Background: The procedure is extravascular, and its success is contingent on precise carotid sinus localization and stable lead fixation [10] [24].
Methodology:
- Pre-operative Evaluation: Confirm the absence of significant carotid artery disease (stenosis <50%), previous stenting, or endarterectomy in the target vessel via duplex ultrasonography [10] [24].
- Anesthesia: Perform the procedure under general anesthesia or local anesthesia with sedation.
- Carotid Exposure: Make a transverse cervical incision over the carotid bifurcation. Use intraoperative ultrasound to localize the bifurcation and carotid sinus [10].
- Sinus Mapping: Expose the anterior surface of the carotid bifurcation and proximal internal carotid artery. Minimize dissection to preserve the carotid sinus nerve. Temporarily place the electrode in various locations and apply electrical stimulation to identify the site yielding the greatest sensitivity (e.g., maximal blood pressure reduction) [23] [10].
- Electrode Fixation: Secure the electrode at the optimal mapped location using six 6-0 Prolene sutures to affix it to the adventitia of the carotid sinus [10].
- Tunneling and IPG Placement: Tunnel the lead subcutaneously over the clavicle. Create a subcutaneous pocket on the anterior chest wall and connect the lead to the IPG [10].
Protocol for Device Activation and Titration
Objective: To safely activate the Barostim system and titrate stimulation parameters to achieve therapeutic efficacy while avoiding side effects such as extraneous stimulation. Background: Therapy is delivered via electrical stimulation to the carotid baroreceptors, which is then titrated upwards over time to a sustainable, effective dose [10] [24].
Methodology:
- Initial Activation: The system is typically activated post-operatively by the research cardiologist. Initial settings are set at a low intensity [10].
- Titration Schedule: Stimulation parameters (e.g., amplitude, frequency, pulse width) are incrementally increased on a weekly or monthly basis according to a predefined protocol [10].
- Efficacy and Safety Monitoring: At each titration step, record:
- Therapeutic Efficacy: Changes in heart rate, blood pressure (in hypertensive models), and patient-reported symptoms.
- Adverse Effects: Monitor for extraneous stimulations (e.g., throat tightness, coughing), which were reported in 27.3% of patients in one series and can affect therapy tolerability [24].
- Endpoint Definition: The therapy is considered optimized when a sustained physiological response is achieved without intolerable side effects.
Signaling Pathway and Mechanism of Action Visualization
Baroreflex Activation Therapy functions by engaging a fundamental neurovascular reflex arc. The following diagram illustrates the integrated signaling pathway activated by the Barostim device, from initial stimulation to end-organ effects.
Figure 1: BAT Signaling Pathway. The diagram outlines the physiological pathway from device stimulation to autonomic nervous system rebalancing.
The Scientist's Toolkit: Key Research Reagents & Materials
The following table catalogues essential materials and methodological tools required for conducting rigorous research into baroreflex activation therapy.
Table 2: Essential Research Materials and Assessment Methodologies for BAT Investigation
| Category/Item | Function/Description in BAT Research |
|---|---|
| Barostim neo System | The investigational device itself, comprising the electrode, lead, and IPG, for delivering the therapy [10]. |
| Carotid Duplex Ultrasound | Essential for pre-operative anatomical screening to exclude significant carotid disease and for intraoperative localization of the carotid bifurcation and sinus [10] [24]. |
| Intraoperative Mapping System | A temporary electrode and stimulator used during implantation to identify the optimal site on the carotid sinus for permanent electrode placement by testing the hemodynamic response to stimulation [23] [10]. |
| 6-Minute Hall Walk Test (6MHWD) | A validated, submaximal exercise test used as a primary functional endpoint to quantify improvement in exercise capacity. A change of ≥30 meters is considered clinically meaningful [9] [25]. |
| Quality of Life (QoL) Questionnaires | Patient-reported outcome (PRO) measures. The Kansas City Cardiomyopathy Questionnaire (KCCQ) and Minnesota Living With Heart Failure Questionnaire (MLHFQ) are standard tools; a change of ≥5 points is a commonly used threshold for clinical importance [25]. |
| N-terminal pro-B-type Natriuretic Peptide (NT-proBNP) | A key circulating biomarker of heart failure severity and hemodynamic stress, used as an objective biochemical endpoint to assess therapeutic response [10] [25]. |
Quantitative Outcomes and Data Presentation
The efficacy of BAT in heart failure research is quantified through a combination of functional, biomarker, and clinical endpoints. The following table synthesizes typical outcome data from preclinical and clinical studies, providing a reference for expected results.
Table 3: Representative Quantitative Outcomes from BAT Studies in Heart Failure
| Outcome Measure | Baseline (Typical HFrEF Cohort) | Post-BAT (6 Months) | Clinical Significance & Notes |
|---|---|---|---|
| 6-Minute Walk Distance (6MWD) | ~300 meters [9] | Increase of ~50 meters [9] | Demonstrates meaningful improvement in functional capacity. |
| Left Ventricular Ejection Fraction (LVEF) | ≤ 35% (Inclusion criteria) [10] | Significant improvement (p<0.05) [9] | Indicates positive reverse cardiac remodeling. |
| NT-proBNP Level | < 1600 pg/mL (Inclusion criteria) [10] [25] | Significant reduction (p<0.05) [25] | Correlates with reduction in cardiac wall stress. |
| New York Heart Association (NYHA) Class | Class III or Class II (recent III) [10] [25] | Significant improvement (p<0.05) [9] [25] | Indicates a reduction in symptom burden. |
| Quality of Life (QoL) Score | e.g., MLHFQ Score | Significant improvement (p<0.05) [9] | Reflects patient-perceived benefit. |
The pre-implant evaluation process is a critical component in the pathway for patients being considered for baroreflex activation therapy (BAT), particularly for those with advanced heart failure with reduced ejection fraction (HFrEF). This comprehensive assessment serves to ensure that transplantation or device implantation is technically feasible, that the recipient's survival chances are not compromised, and that graft survival is not limited by premature disability or death caused by preexisting conditions [26]. Within this rigorous evaluation framework, carotid duplex screening emerges as a potentially valuable tool for assessing cerebrovascular health and mitigating perioperative and long-term neurological risks. The following application notes and protocols detail a standardized approach for multidisciplinary assessment and carotid duplex ultrasound screening specifically tailored for the heart failure population undergoing evaluation for baroreflex activation therapy.
Background and Clinical Rationale
The Heart Failure Patient and Cerebrovascular Risk
Patients with advanced HFrEF present a unique clinical profile characterized by systemic vascular dysfunction, which may accelerate arteriosclerosis and atherosclerosis processes [26]. This population often exhibits multiple comorbidities including hypertension, diabetes, vascular calcification, and other manifestations of systemic vascular disease that contribute to increased risk for carotid artery stenosis. The pathophysiology involves complex interactions of inflammation, oxidative stress, endothelial dysfunction, reduced nitric oxide bioavailability, and calcium-phosphate deposition, creating an environment conducive to the development of hemodynamically significant carotid lesions [26].
Baroreflex activation therapy represents a novel neuromodulation approach for patients with HFrEF, providing symptomatic relief, improvement in left ventricular function, and reduction of cardiac biomarkers [11]. Recent studies with long-term follow-up (up to 7.5 years) have demonstrated substantial reduction in New York Heart Association (NYHA) classification and improvement in left ventricular ejection fraction (LVEF) by 9-11% following BAT implantation [11]. Given the invasive nature of BAT implantation and the potential for hemodynamic fluctuations during the procedure, a comprehensive pre-operative cerebrovascular assessment is essential for optimal patient selection and risk stratification.
Carotid Duplex Ultrasound in Pre-implant Evaluation
Carotid duplex ultrasound (DUS) serves as a non-invasive, cost-effective initial imaging modality for detecting carotid artery stenosis. The test combines B-mode ultrasound for anatomical visualization with Doppler ultrasound for hemodynamic assessment, providing comprehensive data on the degree of stenosis and plaque characteristics. In the context of pre-BAT evaluation, DUS offers several advantages: it avoids the nephrotoxic contrast agents that could exacerbate renal dysfunction in heart failure patients, is readily available in most medical centers, and provides real-time results that can be integrated into the multidisciplinary assessment.
The diagnostic accuracy of carotid duplex ultrasound is well-established, particularly for identifying clinically significant stenosis. When compared to digital subtraction angiography (DSA) as a reference standard, DUS demonstrates a sensitivity of 85% and specificity of 98% for detecting 70-99% carotid artery stenosis, with even higher accuracy for identifying complete occlusions (sensitivity 91%, specificity 95%) [27]. This performance profile supports its utility as a reliable screening tool in the pre-implant setting.
Quantitative Evidence Base
Table 1: Prevalence of Significant Carotid Stenosis in High-Risk Populations
| Patient Population | Sample Size | Prevalence of >70% Stenosis | Key Risk Factors Identified | NNS to Find One Case |
|---|---|---|---|---|
| ESRD Transplant Candidates [26] | 882 | 1.47% (13 patients) | Congestive heart failure (aOR: 5.2), Peripheral vascular disease (aOR: 4.4) | Overall: 69; With CHF/PVD: 23 |
| Cardiac Surgery Patients [28] | 306 (isolated CABG) | 4.9% (15 patients with severe stenosis/occlusion) | Cerebrovascular symptoms, Type of cardiac surgery | 20 |
Table 2: Diagnostic Accuracy of Carotid Duplex Ultrasound for Symptomatic Patients [27]
| Stenosis Category | Reference Standard | Sensitivity (95% CI) | Specificity (95% CI) | Clinical Application |
|---|---|---|---|---|
| 50-99% | DSA | 0.97 (0.95-0.98) | 0.70 (0.67-0.73) | High sensitivity rules out significant disease |
| 70-99% | DSA | 0.85 (0.77-0.91) | 0.98 (0.74-0.90) | Optimal range for detecting surgically significant stenosis |
| Occlusion | DSA | 0.91 (0.81-0.97) | 0.95 (0.76-0.99) | Accurate identification of complete blockages |
| <50% | DSA | 0.63 (0.48-0.76) | 0.99 (0.96-0.99) | High specificity confirms absence of significant disease |
Table 3: Clinical Outcomes of Baroreflex Activation Therapy in HFrEF [11]
| Parameter | Baseline (n=23) | 1-Year Follow-Up | 2-Year Follow-Up | Long-Term (max 7.5 years) |
|---|---|---|---|---|
| NYHA Class III (%) | 96% | 44% (reduction) | Not specified | Sustained improvement in one patient for 7.5 years |
| LVEF (%) | 23 ± 8 | 32 ± 11 (9% improvement) | 34 ± 11 (11% improvement) | Not specified |
| NT-proBNP (pg/mL) | 2463 ± 2922 | Reduction of 396 ± 1006 | Reduction of 566 ± 651 (significant) | Interim decrease maintained |
| Complication Rate | 4% during implantation | Not reported | Not reported | Four deaths during observation period |
Multidisciplinary Assessment Protocol
Core Evaluation Team Composition
The pre-BAT assessment requires a dedicated multidisciplinary team with the following composition:
- Heart Failure Cardiologists: Lead the clinical evaluation, optimize medical therapy, and determine BAT candidacy based on established criteria including NYHA Class III-IV symptoms despite optimal medical therapy.
- Cardiac Surgeons: Assess technical feasibility of BAT implantation, evaluate surgical risks, and manage concurrent carotid disease if identified.
- Vascular Medicine Specialists: Interpret carotid duplex results, provide recommendations for management of identified cerebrovascular disease.
- Neurologists: Evaluate neurological history, assess baseline cognitive and functional status, and manage peri-procedural neurological events.
- Anesthesiologists: Perform preoperative risk stratification, particularly for patients with identified cerebrovascular disease.
- Advanced Practice Providers: Coordinate care across specialties, ensure complete data collection, and facilitate patient education.
Comprehensive Clinical Assessment Components
All patients being considered for BAT should undergo the following standardized assessments:
Cardiovascular Status Assessment
- Echocardiogram with precise measurement of LVEF, ventricular dimensions, valvular function, and pulmonary pressures
- 12-lead electrocardiogram and rhythm monitoring for arrhythmia detection
- Measurement of cardiac biomarkers (NT-proBNP or BNP)
- 6-minute walk test or cardiopulmonary exercise testing for functional capacity assessment
- Documentation of current heart failure medications and doses, including beta-blockers, ACE inhibitors/ARB/ARNI, MRA, and SGLT2 inhibitors
Cerebrovascular Risk Stratification
- Detailed neurological history with specific attention to prior stroke, TIA, or unexplained neurological symptoms
- Assessment of modifiable cerebrovascular risk factors (hypertension, diabetes, dyslipidemia, smoking status)
- Physical examination with thorough neurological assessment and carotid auscultation
- Formal cognitive assessment using standardized tools (MoCA or MMSE)
Comorbidity Evaluation
- Renal function assessment (serum creatinine, eGFR)
- Diabetes control evaluation (HbA1c)
- Peripheral vascular disease assessment (history, physical examination, ankle-brachial index if indicated)
Carotid Duplex Screening Protocol
Indications for Carotid Duplex Ultrasound
Based on the available evidence, the following indications for carotid duplex screening prior to BAT implantation are recommended:
Strong Recommendations (Screening Recommended)
- Patients with history of transient ischemic attack (TIA) or ischemic stroke within the past 6 months
- Patients with symptomatic carotid disease (any neurological symptoms referable to carotid territory)
- Presence of carotid bruit on physical examination
- Documented peripheral arterial disease (regardless of symptoms)
- History of congestive heart failure with reduced ejection fraction (as a standalone risk factor)
Selective Considerations (Individualized Decision)
- Age >70 years with multiple (≥2) cardiovascular risk factors
- Planned complex cardiac procedure in addition to BAT implantation
- Inadequate cerebrovascular history due to cognitive impairment or communication barriers
Less Strong Evidence (Routine Screening Not Recommended)
- Asymptomatic patients under 70 years with no peripheral vascular disease or congestive heart failure
- Patients with limited life expectancy (<2 years) from non-cardiac conditions
Technical Protocol for Carotid Duplex Ultrasound
The following standardized protocol should be implemented for all pre-BAT carotid duplex studies:
Equipment Specifications
- Use high-resolution linear array transducer (5-12 MHz)
- Configure color Doppler with optimized velocity scale and gain
- Set pulse wave Doppler sample gate to 1.5-2.0 mm
- Maintain Doppler angle of insonation ≤60 degrees
Examination Technique
- Perform bilateral examination of common carotid, internal carotid, external carotid, and vertebral arteries
- Obtain B-mode images in longitudinal and transverse planes assessing plaque morphology and composition
- Document Doppler spectral waveforms from proximal, mid, and distal segments of each vessel
- Measure peak systolic velocity (PSV), end-diastolic velocity (EDV), and internal carotid artery/common carotid artery (ICA/CCA) ratios
Stenosis Classification Criteria
- Normal: PSV <125 cm/s, no plaque or intimal thickening
- <50% Stenosis: PSV <125 cm/s, plaque present, ICA/CCA ratio <2.0
- 50-69% Stenosis: PSV 125-230 cm/s, ICA/CCA ratio 2.0-4.0, EDV 40-100 cm/s
- ≥70% Stenosis: PSV >230 cm/s, ICA/CCA ratio >4.0, EDV >100 cm/s
- Near Occlusion: Variable velocities with markedly narrowed lumen
- Total Occlusion: No detectable patent lumen, no flow on color or spectral Doppler
Management Algorithm for Identified Carotid Stenosis
Based on the degree of stenosis identified and symptom status, the following management approach is recommended:
<50% Stenosis (No Significant Disease)
- Proceed with BAT implantation as planned
- Optimize medical management of vascular risk factors
- No specific follow-up carotid imaging required
50-69% Stenosis (Moderate Disease)
- Individualized decision based on multidisciplinary team assessment
- Consider neurology consultation for symptomatic patients
- Intensive medical management including antiplatelet therapy and statins
- Proceed with BAT with perioperative blood pressure optimization
≥70% Stenosis (Severe Disease)
- Formal neurological assessment and consultation
- Discussion of carotid revascularization (endarterectomy or stenting) versus medical management alone
- Timing considerations for staged versus concurrent procedures
- Individualized decision regarding BAT implantation based on overall benefit-risk assessment
Carotid Occlusion
- Confirmatory imaging with CTA or MRA if diagnosis uncertain
- Neurology consultation for assessment of collateral circulation
- Careful perioperative blood pressure management to maintain perfusion
- Proceed with BAT if adequate intracranial circulation confirmed
Integrated Patient Assessment Workflow
Integrated Pre-BAT Assessment Workflow: This diagram illustrates the sequential multidisciplinary evaluation process with integrated carotid duplex screening for heart failure patients being considered for baroreflex activation therapy.
Research Reagent Solutions and Essential Materials
Table 4: Essential Research Materials for Pre-BAT Assessment Protocol
| Category | Item/Reagent | Specifications | Research Application |
|---|---|---|---|
| Ultrasound Imaging | High-frequency Linear Array Transducer | 5-12 MHz frequency range | Carotid artery B-mode imaging and Doppler hemodynamic assessment |
| Doppler Analysis Software | Spectral Doppler Analysis Package | PSV, EDV, ICA/CCA ratio calculation | Quantitative stenosis classification based on velocity parameters |
| Echocardiography Equipment | Cardiac Ultrasound System | Phased array transducer (1-5 MHz) | LVEF measurement, cardiac structure and function assessment |
| Laboratory Assays | NT-proBNP ELISA Kit | High-sensitivity cardiac biomarker assay | Objective measurement of heart failure severity and treatment response |
| Functional Assessment | 6-Minute Walk Test Kit | Standardized corridor with timing device | Functional capacity assessment pre- and post-BAT implantation |
| Neurological Assessment | MoCA Test Kit | Validated cognitive screening tool | Baseline neurological function assessment |
| Data Collection | Electronic Case Report Forms | REDCap or similar database system | Standardized data collection across multidisciplinary team |
The pre-implant evaluation for baroreflex activation therapy requires a systematic, multidisciplinary approach that includes careful assessment of cerebrovascular status through selective carotid duplex ultrasound screening. The evidence-based protocol outlined in these application notes supports targeted rather than universal carotid screening, focusing on patients with specific risk factors including congestive heart failure, peripheral vascular disease, or cerebrovascular symptoms. This approach optimizes resource utilization while identifying the small but important subset of patients with clinically significant carotid artery stenosis that may impact perioperative risk and long-term outcomes. Implementation of this standardized assessment protocol will ensure appropriate patient selection for BAT and contribute to improved safety profiles for this promising therapy for advanced heart failure.
Baroreflex Activation Therapy (BAT) represents a novel device-based approach for managing heart failure with reduced ejection fraction (HFrEF) by modulating autonomic nervous system imbalance. The Barostim system delivers electrical stimulation to carotid sinus baroreceptors, resulting in centrally mediated sympathetic inhibition and parasympathetic activation [23]. This surgical implantation procedure requires precise anatomical knowledge and multidisciplinary collaboration between vascular surgeons, heart failure cardiologists, and anesthesiologists [29]. This protocol details the technical approach for researchers investigating device-based autonomic modulation therapies.
Preoperative Evaluation and Patient Selection
Medical Eligibility Criteria
Patient selection follows strict clinical criteria based on clinical trial protocols and FDA approval specifications [14]. Researchers should note that candidates must have:
- HFrEF with left ventricular ejection fraction (LVEF) ≤35%
- New York Heart Association (NYHA) Class III or Class II (with recent history of Class III)
- Refractory symptoms despite optimal guideline-directed medical therapy (GDMT)
- NT-proBNP levels <1,600 pg/mL
- Ineligibility for cardiac resynchronization therapy (CRT) according to current guidelines [30] [14]
Anatomical and Surgical Contraindications
Vascular surgeons must evaluate technical feasibility through comprehensive assessment [29]:
- Carotid anatomy: Bilateral carotid bifurcations above the mandible level preclude implantation
- Carotid disease: Atherosclerosis >50% or ulcerative plaques disqualify candidates
- Previous interventions: Prior carotid stenting, endarterectomy, or neck radiation in the target area
- Allergies: Known hypersensitivity to device components (silicone, titanium)
Table 1: Preoperative Evaluation Protocol
| Assessment Domain | Required Evaluation | Exclusion Criteria |
|---|---|---|
| Cardiovascular | Echocardiogram, ECG, NT-proBNP | CRT indication, LVEF >35% |
| Carotid Anatomy | Duplex Ultrasound | Bifurcation >mandible, stenosis >50% |
| Medical History | Medication review, comorbidity assessment | Baroreflex failure, autonomic neuropathy |
| Surgical History | Neck and chest wall evaluation | Previous carotid surgery, tracheostomy |
Multidisciplinary Team Formation
Successful BAT programs require structured collaboration [29]:
- Vascular Surgeon: Leads surgical evaluation, device implantation, and manages device-related complications
- Heart Failure Cardiologist: Determines medical eligibility and manages postoperative therapy titration
- Cardiovascular Anesthesiologist: Familiar with BAT-specific hemodynamic considerations
- Device Specialist: Provides technical support for device programming and intraoperative mapping
Surgical Protocol
Preoperative Preparation
- Medication management: Withhold antihypertensive agents 4-6 hours preoperatively to preserve baroreflex responsiveness during mapping [31]
- Beta-blocker titration: Reduce dosage 1-2 days preoperatively to minimize bradycardia during intraoperative testing [31]
- Anticoagulation management: Discontinue antiplatelet/anticoagulant medications per institutional protocol
- Antibiotic prophylaxis: Administer preoperatively per institutional surgical site infection protocols
Device Components
The Barostim Neo system (CVRx, Inc.) consists of three primary components [10]:
- Carotid Sinus Lead (CSL): Features a 2-mm iridium oxide-coated electrode centered on a 7-mm diameter circular backer
- Implantable Pulse Generator (IPG): Similar in size to a small ICD, houses battery and electronics
- External Programmer: Tablet or laptop-based system for noninvasive parameter adjustment and data tracking
Anatomical Considerations and Surgical Approach
Incision and Carotid Exposure
- Positioning: Supine with neck extended and rotated contralaterally
- Ultrasound localization: Identify carotid bifurcation using duplex ultrasound to guide incision placement [10]
- Surgical exposure: Make transverse cervical incision along natural skin crease over carotid bifurcation
- Dissection technique: Minimal dissection of periadventitial tissues to expose only the anterior surface of carotid sinus [29]
- Nerve preservation: Avoid injury to carotid sinus nerve located medial to carotid sinus [10]
Intraoperative Mapping
Mapping identifies the optimal electrode placement site by testing baroreceptor responsiveness [29]:
- Stimulation parameters: Apply electrical stimulation to different carotid sinus locations
- Hemodynamic monitoring: Observe for 5-10% reduction in systolic blood pressure and heart rate from baseline
- Response timing: Peak hemodynamic responses typically occur within 30-120 seconds of stimulation initiation [31]
- Optimal location: 90% of patients respond at the anterior aspect of internal carotid artery adjacent to bifurcation [29]
Electrode Placement and Securing
- Electrode fixation: Secure to adventitia at identified optimal location using six 6-0 Prolene sutures [10]
- Strain relief: Create redundant CSL loop in neck to accommodate neck rotation without tension [29]
- Anchor placement: Sew small tab attached to CSL onto common carotid adventitia to preserve strain relief loop
Pulse Generator Implantation
- Chest pocket creation: Develop subcutaneous pocket in infraclavicular region, ipsilateral or contralateral to carotid electrode
- Device connection: Tunnel CSL from neck to chest pocket and connect to IPG
- IPG fixation: Secure generator to pectoralis major fascia using retention sutures
- Lead management: Coil excess lead medially in pocket to prevent discomfort or mispositioning
Closure and Postoperative Check
- System testing: Verify proper device function before closure
- Hemostasis: Meticulous attention to bleeding given proximity to major vessels
- Incision closure: Standard layered closure with subcuticular skin closure
Anesthesia Protocol
Pharmacological Considerations
Anesthetic management requires special consideration to avoid baroreflex blunting during mapping [31]:
Table 2: Anesthetic Agents and Their Effects on Baroreflex Function
| Agent Class | Effect on Baroreflex | Recommended Use |
|---|---|---|
| Opioids (Fentanyl, Remifentanil) | Minimal effect | Preferred for maintenance |
| Benzodiazepines | Minimal effect | Acceptable for premedication |
| Etomidate | Minimal effect | Suitable for induction |
| Nitrous Oxide | Minimal effect | Acceptable adjunct |
| Propofol | Blunts reflex | Avoid during mapping phase |
| Volatile Anesthetics | Dose-dependent blunting | Limit to <0.5 MAC |
| Ketamine | Blunts reflex | Avoid |
| Dexmedetomidine | Blunts reflex | Avoid |
Hemodynamic Management
- Monitoring: Arterial line for continuous blood pressure monitoring is standard [31]
- Hemodynamic targets: Maintain SBP >90% of conscious values and HR >65 bpm [29]
- Pacemaker adjustment: Consider temporary adjustment in patients with CIEDs to minimize transient bradycardia [29]
- Emergency preparedness: Have push-dose pressors available for significant bradycardia/hypotension during mapping
Postoperative Management and Follow-up
Immediate Postoperative Care
- Disposition: Typically outpatient procedure unless patient comorbidities require admission [29] [10]
- Wound care: Standard surgical incision care
- Device activation: Initial programming typically performed by cardiology team postoperatively
Therapy Titration Protocol
- Follow-up schedule: Monthly titration appointments for first several months [10]
- Titration parameters: Progressive increase in amplitude according to patient tolerability [32]
- Therapeutic goals: Symptom improvement while avoiding side effects (hoarseness, cough, discomfort)
Complication Management
Clinical studies report procedure-related complication-free rates of 85.9-97% [30]. Potential complications include:
- Extraneous stimulation: Affects tolerability in approximately 27% of patients [29]
- Nerve injury: Rare with careful surgical technique
- Device-related issues: Surgical revision may be required for lead displacement or IPG malfunction
- Infection: Standard surgical site infection risks
Research Implications and Outcomes Assessment
Efficacy Endpoints for Research Protocols
Clinical trials demonstrate significant improvements in multiple parameters with BAT [30]:
Table 3: Expected Efficacy Outcomes Based on Clinical Trial Data
| Parameter | Magnitude of Improvement | Timeframe |
|---|---|---|
| NYHA Functional Class | RR 2.13 (95% CI 1.65-2.76) | 6 months |
| Quality of Life (MLHFQ) | DM -16.97 (95% CI -21.87 to -12.07) | 6 months |
| 6-Minute Walk Test | DM 56.54m (95% CI 55.67 to 57.41) | 6 months |
| NT-proBNP | DM -120.02 pg/mL (95% CI -193.58 to -46.45) | 6 months |
| LVEF | Case reports show 2-10% absolute improvement | 6-24 months |
Long-term Outcomes
Emerging evidence demonstrates sustained benefits at 2-year follow-up [32]:
- Functional improvement: NYHA class improvement maintained long-term
- Biomarker reduction: NT-proBNP reductions sustained (30-89% in case reports)
- Cardiac remodeling: Improvements in LVEF, LVEDV, and LA volume observed
- Hospitalization reduction: Decreased HF hospitalization rates
Visual Documentation
Surgical Workflow and Multidisciplinary Collaboration
Anatomical and Technical Considerations
Research Reagent Solutions
Table 4: Essential Materials and Equipment for BAT Implantation Research
| Item | Specification | Research Application |
|---|---|---|
| Barostim Neo2 System | CVRx, Inc. | Includes IPG, carotid sinus lead, external programmer |
| Carotid Duplex Ultrasound | High-frequency linear transducer | Preoperative anatomical assessment and surgical planning |
| Surgical Instruments | Vascular surgery set | Carotid exposure and delicate dissection |
| Mapping System | Integrated with Barostim programmer | Intraoperative identification of optimal stimulation site |
| Hemodynamic Monitoring | Arterial line setup | Continuous blood pressure monitoring during mapping |
| Sutures | 6-0 Prolene | Electrode fixation to carotid adventitia |
| IPG Retention Sutures | Non-absorbable | Securing generator to pectoralis fascia |
Heart Failure with Reduced Ejection Fraction (HFrEF) represents a significant clinical challenge with high mortality and morbidity despite standardized pharmacological approaches. A central pathophysiological feature in HFrEF progression is autonomic dysfunction, characterized by sustained sympathetic overactivation and parasympathetic withdrawal [14] [33]. This imbalance contributes to progressive left ventricular dysfunction, adverse remodeling, and increased mortality risk. Baroreflex Activation Therapy (BAT) emerges as an innovative device-based approach targeting this autonomic imbalance. The therapy utilizes an implantable pulse generator that delivers electrical stimulation to carotid sinus baroreceptors, resulting in activation of parasympathetic outflow and inhibition of sympathetic activity [14]. This restoration of neurohormonal balance addresses a fundamental mechanism in HF progression that often persists despite optimal guideline-directed medical therapy (GDMT).
For researchers investigating advanced HF therapies, the patient population with persistent New York Heart Association (NYHA) Class II/III symptoms despite maximally tolerated GDMT represents a critical target for BAT intervention. These patients occupy a therapeutic gap where conventional pharmacological strategies have been exhausted but disease progression continues, often without qualifying for more invasive surgical options like heart transplantation or left ventricular assist devices [34]. The scientific rationale for BAT in this population extends beyond symptomatic improvement to potential reversal of maladaptive remodeling pathways, making it a compelling subject for ongoing clinical investigation.
Clinical Evidence and Outcomes Data
Key Clinical Studies and Efficacy Endpoints
Table 1: Summary of Key Clinical Trials of BAT in HFrEF
| Trial Name | Design & Population | Key Efficacy Findings | Safety Outcomes |
|---|---|---|---|
| HOPE4HF [14] | Phase II RCT (n=146); LVEF ≤35%, NYHA III | • Significant improvement in NYHA class, MLHFQ score, and 6-min walk distance vs. medical therapy alone (p<0.05 for all) | • 97.2% freedom from major adverse neurological and CV events |
| BeAT-HF [14] [35] | Pivotal RCT (n=408, initial phase); LVEF ≤35%, NYHA II-III | • Significant improvement in MLHFQ score and 6-min walk distance (p<0.05)• Reduction in NT-proBNP levels (p<0.05) | • 97% freedom from major adverse neurological or CV system/procedure-related events |
| Real-World Spanish Cohort [35] | Observational (n=21); HFrEF with symptoms despite optimal therapy | • Significant reduction in annual HF hospitalizations (1.52 vs. 0.76, p=.042)• Trend toward improved NYHA class (p=.054) | • No major local complications• 14.2% minor BAT-related complications (hoarseness, dry cough, neck pain), all resolved with parameter adjustment |
| Prospective Single-Center Study [15] | Prospective (n=40); HFrEF, NYHA III | • BAT groups showed increased LVEF (BAT +10%, p=0.005; BAT+ARNI +9%, p=0.049)• Improved NYHA class, QoL, and reduced NT-proBNP• 50% reduction in HF hospitalization rates vs. control (p=0.020) | • Well-tolerated with no major safety concerns reported |
Quantitative Efficacy Metrics
Table 2: Magnitude of Clinical Improvements with BAT Therapy
| Parameter | Baseline Mean | Follow-up Period | Absolute/Relative Change | Clinical Significance |
|---|---|---|---|---|
| LVEF [15] | 23-27% | 6-12 months | +9 to +10% (absolute) | Improvement in systolic function |
| 6-Minute Walk Distance [14] | Not specified | 6 months | Significant improvement (p<0.05) | Enhanced functional capacity |
| NT-proBNP [15] | 2302±460 pg/mL | 12 months | -24% to -37% | Reduction in neurohormonal activation |
| Quality of Life (QoL) [15] | Not specified | 12 months | +21 to +22% improvement | Enhanced patient-reported outcomes |
| HF Hospitalization [35] | 1.52 annualized | 12 months | 50% reduction (p=0.020) | Reduced healthcare utilization |
Candidate Selection Protocol
Inclusion Criteria
The ideal candidate for BAT clinical investigation presents with the following characteristics:
- Established HFrEF with left ventricular ejection fraction (LVEF) ≤35% documented within the past 90 days
- Persistent symptomatology classified as NYHA Class II or III despite ≥3 months of optimized, maximally tolerated GDMT
- Elevated biomarker evidence of ongoing neurohormonal activation (NT-proBNP <1,600 pg/mL as per FDA labeling) [14]
- Suboptimal response to cardiac resynchronization therapy (CRT) or ineligibility for CRT despite appropriate indication [35]
- Beta-blocker intolerance may represent a specific subgroup of interest, as BAT may provide alternative sympatholytic effects [35]
Exclusion Criteria
- Concomitant conditions that may interfere with device implantation or stimulation
- Significant carotid artery disease or prior carotid surgery that would preclude safe lead placement
- Life expectancy <1 year due to non-cardiac conditions
- Pregnancy or planned pregnancy during study period
- Concurrent participation in other investigational device or drug trials
Baroreflex Activation Therapy: Implantation and Titration Protocol
Device Components and Preclinical Modeling
Research Toolkit: Essential Materials and Assessments
| Category | Specific Tool/Assessment | Research Application |
|---|---|---|
| Device System | Barostim neo System (CVRx, Inc.) | Implantable pulse generator with carotid sinus leads for chronic baroreflex activation [14] |
| Preclinical Models | Canine coronary microembolization-induced HF model | Established large animal model for studying BAT effects on LV function, remodeling, and arrhythmia thresholds [12] |
| Functional Capacity | 6-Minute Hall Walk Distance (6MHWD) | Objective measure of functional improvement in clinical protocols [15] |
| Biomarker Analysis | NT-proBNP levels | Quantification of neurohormonal activation and response to therapy [14] [15] |
| Sympathetic Activity | Muscle Sympathetic Nerve Activity (MSNA) | Direct assessment of sympathetic outflow in proof-of-concept studies [15] |
| Patient-Reported Outcomes | Minnesota Living with HF Questionnaire (MLHFQ) | Quality of life assessment specific to heart failure symptoms and limitations [14] |
| Autonomic Function | Baroreflex sensitivity assessment | Quantification of baroreflex function improvement following chronic therapy [33] |
Device Implantation Procedure
The BAT implantation protocol involves surgical placement of the Barostim neo system:
- Device Placement: The pulse generator is implanted in the pectoral region similar to conventional pacemaker implantation
- Lead Placement: A single electrode lead is positioned adjacent to the carotid sinus at the carotid bifurcation
- Intraoperative Testing: Acute stimulation runs confirm proper lead placement through observed reductions in blood pressure and heart rate
- Activation Timeline: Device activation typically occurs approximately one month post-implantation to allow for surgical recovery [15]
Stimulation Titration Protocol
Following the healing period, BAT parameters are systematically titrated:
- Initial Activation: Programming begins approximately 4 weeks post-implantation [35]
- Stimulation Parameters: Typical settings include amplitude of 6.6±1.3mA, pulse width of 129±12μs, and frequency of 40 pulses/s [35]
- Dose Optimization: Stimulation intensity is gradually increased to the maximum level tolerated without discomfort or side effects
- Long-term Adjustment: Parameters may be further refined based on therapeutic response and tolerability over time
Pathophysiological Mechanisms and Signaling Pathways
BAT exerts its beneficial effects through multiple interconnected physiological pathways that counter maladaptive mechanisms in chronic heart failure.
Figure 1: BAT Mechanism of Action Pathway
The flow diagram illustrates the cascade of physiological effects following BAT implementation. Direct electrical stimulation of carotid baroreceptors activates afferent pathways to the nucleus tractus solitarius, initiating two primary responses: (1) increased parasympathetic outflow via the vagus nerve, and (2) inhibition of sympathetic nervous system activity from the rostral ventrolateral medulla [14] [12]. These autonomic shifts produce several cardioprotective effects including reduced heart rate, decreased myocardial fibrosis, inhibition of the renin-angiotensin-aldosterone system (RAAS), and lowered risk of sudden cardiac death [12] [33]. The culmination of these intermediate effects results in the clinically observed improvements in LV systolic function, reverse remodeling, symptom reduction, and decreased hospitalization frequency.
Beyond these established mechanisms, preclinical models have demonstrated additional benefits at the cellular and molecular levels. Chronic BAT administration in canine HF models resulted in nearly 40% reduction in replacement fibrosis volume fraction and approximately 22% decrease in reactive interstitial fibrosis [12]. Furthermore, BAT treatment was associated with normalization of capillary density and improved beta-adrenergic receptor signaling, suggesting potential restoration of myocardial structure and function at the tissue level.
Research Applications and Future Directions
The investigation of BAT in NYHA Class II/III HFrEF patients with persistent symptoms represents a compelling area of translational research with multiple unanswered questions worthy of systematic exploration. Future research should prioritize several key areas:
Phenoprofile-Specific Applications: Recent proposals for categorizing HF patients into distinct phenoprofiles based on GDMT response and candidacy for advanced therapies suggest BAT may be particularly valuable for Phenoprofile II (GDMT intolerance due to hypotension or renal insufficiency) and Phenoprofile IV (incomplete GDMT response with contraindications to heart replacement therapy) [34]. Dedicated studies targeting these subpopulations could elucidate specific therapeutic niches for BAT implementation.
Combination Therapy Optimization: While preliminary data suggests BAT combined with ARNI therapy may produce more pronounced effects than either intervention alone [15], systematic investigation of BAT interactions with contemporary GDMT components remains limited. Research should focus on sequencing, timing, and synergistic effects of BAT with foundational HF therapies, particularly in patients with specific intolerance patterns.
Biomarker-Driven Patient Selection: Development of tools and markers to identify patients with more pronounced baroreflex dysfunction may help refine candidate selection and optimize therapeutic response [14]. Integration of autonomic testing, advanced imaging, and genomic profiling could enable precision medicine approaches to BAT implementation.
Long-Term Outcomes Validation: While the ongoing extended phase (phase II) of the BeAT-HF trial aims to assess cardiovascular mortality and HF morbidity endpoints [14], additional real-world registry data and health economic analyses will be essential to establish BAT's position in the HF therapeutic landscape and inform guideline recommendations.
Baroreflex activation therapy (BAT) represents an innovative neuromodulatory approach for patients with heart failure with reduced ejection fraction (HFrEF). This therapy operates by electrically stimulating the carotid baroreceptors, thereby initiating a physiological reflex arc that restores autonomic balance by reducing sympathetic outflow and increasing parasympathetic tone [23] [3]. The efficacy of BAT in improving functional capacity, quality of life, and reducing heart failure hospitalization rates has been demonstrated in clinical studies [13]. However, the therapeutic success of BAT is profoundly dependent on precise post-operative management, particularly the systematic processes for device activation and titration. This document outlines detailed application notes and protocols for the post-operative management of BAT, providing researchers and clinical scientists with standardized methodologies for optimal therapy delivery.
Physiological Basis and Evidence for BAT
Mechanism of Action
BAT functions by modulating the autonomic nervous system, which is characteristically imbalanced in chronic heart failure. The therapy delivers electrical stimulation to the carotid sinus baroreceptors via an implanted device system typically consisting of a carotid sinus lead and a pulse generator [23]. This stimulation generates afferent signals that travel along the glossopharyngeal nerve to the nucleus tractus solitarius in the medulla oblongata. The integrated efferent response leads to a reduction in sympathetic nervous system activity and an enhancement of parasympathetic vagal outflow to the heart and blood vessels [23]. This rebalancing of autonomic tone addresses a fundamental pathophysiological mechanism in HFrEF progression, unlike pharmacologic approaches that merely antagonize end-organ adrenergic receptors [23].
A rapid systematic review of clinical studies investigating BAT for HFrEF supports its safety and efficacy profile. The review, which included 10 publications from three distinct studies, reported an 86% rate of system and procedure-related complication-free outcomes, with no incidents of cranial nerve injury [13]. The table below summarizes the key efficacy outcomes from pivotal BAT studies.
Table 1: Clinical Outcomes from Baroreflex Activation Therapy Studies in HFrEF
| Study Reference | Study Design | Patient Population | Follow-up Duration | Key Efficacy Outcomes |
|---|---|---|---|---|
| Gronda et al. [13] | Single-arm, open-label | NYHA Class III, LVEF <40% (n=11) | 6 months | Improvement in MSNA, NYHA class, and quality of life scores. |
| Abraham et al. (HOPE4HF) [13] | Randomized Controlled Trial | Chronic HF, LVEF ≤35% (n=71 BAT, n=69 Control) | 6 months | Improved NYHA class, quality of life, 6-minute walk distance, and NT-proBNP. |
| Long-term Follow-up [13] | Single-arm, open-label | Extension of Gronda et al. cohort (n=11 to 7) | Up to 41.5 months | Sustained improvements in symptoms, functional capacity, and reduced hospitalization rates. |
Post-Operative Management Protocol
The post-operative management of BAT involves a structured, multi-phase approach to ensure patient safety and optimize therapeutic response.
Device Activation and Titration Workflow
The following diagram illustrates the logical workflow for the post-implant activation and titration of the Barostim neo system.
Detailed Experimental and Clinical Protocols
Initial Device Activation Protocol
Objective: To safely initiate electrical stimulation from the Barostim neo system after the post-surgical healing period.
Methodology:
- Timing: Activation is typically performed 2-4 weeks post-implant to allow for adequate tissue healing around the electrode and reduce infection risk [13].
- Set-Up: The device is interrogated using the manufacturer's proprietary programmer. Baseline impedance and device settings are recorded.
- Initial Stimulation:
- Stimulation is initiated at a low voltage (e.g., 0.5 V) that is below the patient's perception threshold to avoid discomfort or acute hemodynamic shifts [23].
- Standard initial pulse width is set between 150-450 μs, with a frequency of 40-100 Hz, based on the implanted lead location and patient-specific mapping during implantation [23].
- Monitoring: Vital signs, including heart rate and blood pressure, are continuously monitored for at least 30 minutes post-activation. The patient is questioned about any discomfort, neck muscle contractions, or gagging sensations.
Systematic Titration Protocol
Objective: To gradually uptitrate stimulation parameters to a therapeutic level that provides maximal clinical benefit without side effects.
Methodology:
- Titration Schedule: Titration sessions are conducted every 1-2 weeks in the outpatient clinic until a stable, effective dose is established.
- Parameter Adjustment:
- The voltage is increased in small increments (e.g., 0.25 V per step) during each session.
- The goal is to find the highest tolerable voltage that does not cause discomfort, pain, or muscle twitching.
- Pulse width and frequency may be adjusted if the desired hemodynamic or symptomatic response is not achieved with voltage titration alone [23].
- Efficacy Assessment: At each titration step, the following are assessed:
- Acute Hemodynamic Response: A reduction in systolic blood pressure of 5-15 mmHg and a decrease in heart rate of 5-10 beats per minute serve as acute indicators of baroreflex engagement [3].
- Symptom Check: Patient-reported symptoms of hoarseness, cough, or discomfort are recorded.
- Therapeutic Target: The titration endpoint is a patient-specific profile that yields improvement in functional status (e.g., NYHA Class, 6-minute walk test distance) and quality of life over time, without adverse effects [13] [3].
Long-Term Management and Safety Monitoring Protocol
Objective: To maintain therapeutic efficacy and monitor for long-term safety and system-related complications.
Methodology:
- Follow-up Intervals: After stabilization, patients are followed every 3-6 months. Device interrogation is performed to check battery status, lead impedance, and therapy delivery.
- Outcome Assessments: At each follow-up, key efficacy outcomes are measured, including:
- NYHA Functional Class
- Quality of Life (QoL) score (e.g., using the Minnesota Living with Heart Failure Questionnaire)
- 6-Minute Hall Walk (6MHW) distance [13]
- Echocardiographic parameters (LVEF, LV volumes)
- N-terminal pro-brain natriuretic peptide (NT-proBNP) levels
- Rate of heart failure hospitalizations
- Safety Surveillance: Patients are continuously monitored for system- or procedure-related major adverse neurological and cardiovascular events. The reported 86% complication-free rate underscores the procedure's safety when performed by a well-trained team [13].
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing pre-clinical or clinical studies on BAT, the following table details essential components and their functions.
Table 2: Essential Research Materials and Tools for Baroreflex Activation Therapy Studies
| Item / Solution | Function / Application in BAT Research |
|---|---|
| Barostim neo System | The primary implantable device, comprising a pulse generator and a carotid sinus lead. It is the intervention under investigation in clinical trials [13] [3]. |
| Programmer / Clinician Software | A dedicated computer system used to non-invasively adjust stimulation parameters (voltage, pulse width, frequency), monitor device integrity, and retrieve stored data [23]. |
| Muscle Sympathetic Nerve Activity (MSNA) | A direct neurophysiological measurement technique (via microneurography) used as a primary endpoint to quantify the reduction in central sympathetic outflow in response to BAT [13]. |
| Baroreflex Sensitivity (BRS) Assessment | A key physiological parameter measured to assess the restoration of baroreceptor function and autonomic balance following BAT initiation [13] [23]. |
| Guideline-Directed Medical Therapy (GDMT) | The standardized background pharmacological treatment for all HFrEF patients in BAT trials, ensuring that the additive effect of BAT is accurately evaluated [3]. |
The post-operative management of Baroreflex Activation Therapy, specifically the protocols for device activation and titration, is a critical determinant of therapeutic success. The structured, patient-tailored approach outlined in these application notes—emphasizing gradual uptitration to a maximally tolerated dose based on hemodynamic and symptomatic responses—ensures both safety and efficacy. For the research and drug development community, adherence to these detailed methodologies is essential for generating robust, comparable data in future clinical trials. As the field advances, these protocols will serve as a foundation for optimizing this promising neuromodulatory treatment for patients with advanced heart failure.
Addressing Clinical Challenges: Complication Management, Non-Response, and Therapy Optimization
Peri-procedural Complication Profiles and Management Strategies
Baroreflex activation therapy (BAT) represents an advanced device-based treatment for patients with heart failure with reduced ejection fraction (HFrEF) who remain symptomatic despite optimal guideline-directed medical therapy and are ineligible for cardiac resynchronization therapy [5] [14]. The therapy modulates the autonomic nervous system by electrically stimulating carotid baroreceptors, resulting in reduced sympathetic and increased vagal tone [9] [14]. As BAT gains traction in heart failure management, understanding its peri-procedural safety profile becomes paramount for researchers and clinicians developing this therapy. This document provides a comprehensive analysis of BAT-associated complications and structured protocols for their management within research settings, supporting the broader thesis that optimized peri-procedural management enhances BAT's therapeutic potential in heart failure.
Complication Profiles: Quantitative Analysis
Intraoperative and Perioperative Complications
Analysis of clinical series reveals that BAT implantation is generally safe with a manageable complication profile. Table 1 summarizes the major peri-procedural complications based on aggregated clinical data.
Table 1: Major Peri-procedural Complications Associated with BAT Implantation
| Complication Type | Incidence | Onset Timeline | Risk Factors | Severity Classification |
|---|---|---|---|---|
| Extraneous Stimulation | 27.3% (3/11 patients) [24] | Post-operative to 6 months | Unclear | Mild-Moderate |
| Surgical Site Complications | 9.1% (1/11 patients) [24] | Immediate post-operative | Previous neck radiation | Moderate |
| Perioperative Anemia | 9.1% (1/11 patients) [14] | Immediate post-operative | Unclear | Mild |
| Major Adverse Neurological/CV Events* | 0% (0/11 patients) [24] | Intraoperative to 30 days | Not applicable | N/A |
| Procedure-Related Mortality | 0% (0/11 patients) [24] [14] | Intraoperative to 30 days | Not applicable | N/A |
*Major adverse neurological or cardiovascular events including stroke, myocardial infarction, or device-related life-threatening complications [24] [14].
The procedural safety profile demonstrates a 97% freedom-from-adverse events rate at 12 months in the HOPE4HF trial, with most complications being transient and manageable [14]. The absence of major neurological or cardiovascular events in recent series highlights refined surgical techniques and patient selection [24].
Device-Specific Adverse Events
Table 2 catalogues device-specific adverse events and their management strategies documented in BAT research.
Table 2: Device-Specific Adverse Events and Management Protocols
| Device-Related Complication | Clinical Manifestation | Proposed Mechanism | Management Strategy | Preventive Measures |
|---|---|---|---|---|
| Extraneous Stimulation [24] | Uncomfortable sensations in neck, jaw, or throat | Current spread to adjacent neural structures | Device reprogramming; Stimulation parameter adjustment | Optimal lead placement away from nerve branches |
| Lead Placement Issues [9] | Suboptimal therapeutic effect | Surgical technique; Anatomical variations | Intraoperative signal testing; Repositioning if necessary | Preoperative imaging; Surgeon experience |
| Device-Device Interaction [24] | Potential interference with existing devices | Unilateral vs. bilateral implantation decisions | Implant on same side as existing cardiac devices in select cases | Preoperative device inventory and planning |
Pathophysiological Framework and Complication Mechanisms
Figure 1: Pathophysiological Framework of BAT Complications
The diagram illustrates how BAT-related complications originate from interactions between surgical intervention, patient anatomy, and technical factors. The primary mechanism for extraneous stimulation (occurring in 27.3% of cases) involves current spread to adjacent neural structures due to lead placement proximity or excessive stimulation parameters [24]. Surgical site complications associate most strongly with patient-specific factors such as previous neck radiation therapy [24]. The absence of neurovascular injuries in recent series (0%) reflects improved surgical protocols and patient selection criteria [24] [14].
Experimental Protocols for Complication Assessment
Preoperative Assessment Protocol
Objective: Systematically evaluate candidacy for BAT implantation and identify potential risk factors for complications.
Methodology:
- Comprehensive Medical History
Anatomical Imaging Protocol
- Perform carotid duplex ultrasound to assess vascular anatomy and exclude significant atherosclerosis
- Utilize cervical CT or MRI for patients with prior neck surgery or radiation to evaluate tissue planes
- Document relationship between carotid bifurcation and adjacent cranial nerves
Multidisciplinary Evaluation
- Structured assessment by heart failure cardiologist for medical eligibility
- Vascular surgeon evaluation for technical feasibility of implantation [24]
- Anesthesiology review for operative risk stratification
Data Collection Parameters:
- Carotid artery diameter and quality of bifurcation
- Presence of carotid atherosclerotic plaque (>50% stenosis constitutes exclusion)
- Distance between anticipated lead placement site and cranial nerve pathways
- Documentation of any anatomical variants
Intraoperative Safety Protocol
Objective: Minimize procedural risks through standardized surgical technique and real-time monitoring.
Methodology:
- Surgical Approach
- Perform unilateral carotid sinus exposure under general anesthesia
- Utilize minimal dissection techniques to preserve anatomical relationships
- Establish lead placement at carotid bifurcation with direct visualization
Intraoperative Testing
- Conduct baseline hemodynamic measurements prior to activation
- Perform intraoperative stimulation threshold testing
- Assess for extracervical stimulation at various parameter settings
- Document optimal stimulation parameters that achieve hemodynamic effect without adverse symptoms
Device Configuration
- Program initial settings based on intraoperative testing results
- Establish bilateral stimulation capability while typically initiating with unilateral activation (employed in 75% of Rheos Pivotal Trial patients) [9]
- Verify device integrity prior to closure
Safety Endpoints:
- Absence of significant bradycardia (<40 bpm) or hypotension (SBP <90 mmHg) during testing
- No persistent cranial nerve stimulation during intraoperative assessment
- Confirmation of adequate lead positioning by fluoroscopy
Postoperative Complication Monitoring Protocol
Objective: Standardized surveillance for early detection and management of BAT-related complications.
Methodology:
- Structured Symptom Assessment
- Implement daily symptom logs during initial hospitalization
- Specifically query neck discomfort, swallowing difficulties, voice changes, or unusual sensations
- Utilize standardized scales for symptom severity quantification
Device Interrogation Protocol
- Perform systematic device checks at 24 hours, 72 hours, and 1 month post-implantation
- Document lead impedance, stimulation thresholds, and battery status
- Assess patient-triggered episodes for abnormal rhythms or symptoms
Neurological and Vascular Examination
- Conduct formal cranial nerve assessment pre-discharge and at 1-month follow-up
- Perform carotid auscultation for new bruits suggesting vascular compromise
- Document any focal neurological deficits
Management Algorithms:
- For extraneous stimulation: systematic parameter adjustment beginning with pulse width reduction, then amplitude modification
- For surgical site complications: standard wound care protocols with vascular surgery consultation if evidence of infection or hematoma
- For device-device interactions: reprogramming of existing cardiac devices with electrophysiology consultation
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for BAT Complication Studies
| Research Tool Category | Specific Examples | Research Application | Key Characteristics |
|---|---|---|---|
| Baroreflex Assessment | Barostim neo System (CVRx) [14] | BAT delivery and parameter optimization | Second-generation, minimally invasive system; Programmable stimulation parameters |
| Anatomical Imaging | Carotid Duplex Ultrasound; Cervical MRI/CT [24] | Preoperative planning; Complication investigation | Vascular anatomy visualization; Tissue plane assessment |
| Hemodynamic Monitoring | Ambulatory BP Monitoring; Continuous ECG [36] [9] | BAT efficacy assessment; Safety monitoring | 24-hour blood pressure profiling; Arrhythmia detection |
| Neurological Evaluation | Cranial Nerve Examination Protocol | Complication detection and quantification | Standardized assessment of nerve function |
| Outcome Assessment | Kansas City Cardiomyopathy Questionnaire (KCCQ) [37] | Patient-reported outcomes measurement | HF-specific quality of life instrument |
| Device Interrogation | Manufacturer-specific Programmer | Device function assessment; Parameter adjustment | Stimulation parameter optimization; Lead integrity verification |
The peri-procedural complication profile of BAT demonstrates a generally favorable safety spectrum dominated by manageable issues such as extraneous stimulation (27.3%) rather than major adverse events. The documented absence of procedure-related mortality or major neurological complications in contemporary series underscores the technical maturation of this therapy. The implementation of structured preoperative assessment, meticulous surgical technique, and systematic postoperative surveillance provides a comprehensive framework for complication mitigation. These protocols support the broader research thesis that optimized peri-procedural management enhances the risk-benefit profile of BAT, facilitating its development as an autonomic modulation strategy for advanced heart failure. Future research directions should focus on predictive biomarkers for complication risk, refined surgical approaches to further reduce adverse events, and standardized management algorithms for the scientific community.
Device Titration Algorithms for Maximizing Therapeutic Response
Baroreflex Activation Therapy (BAT) is a device-based neuromodulation treatment for patients with heart failure with reduced ejection fraction (HFrEF) who remain symptomatic despite guideline-directed medical therapy (GDMT) and are not candidates for cardiac resynchronization therapy [38]. BAT functions by electrically stimulating the carotid baroreceptors, which increases signaling to the brain, resulting in reduced sympathetic tone and increased parasympathetic tone. This restoration of autonomic nervous system balance translates to significant improvements in patients' exercise capacity, quality of life, and cardiac function [38]. The therapeutic efficacy of BAT is critically dependent on a structured device titration algorithm to optimize stimulation parameters, maximize clinical response, and ensure patient safety. This protocol details the systematic approach to BAT titration, supported by quantitative data and experimental methodologies relevant to clinical research and development.
BAT Titration Algorithm: Clinical Decision Pathway
The following diagram illustrates the core clinical decision pathway for patient stratification and the subsequent titration protocol for Baroreflex Activation Therapy.
Diagram 1: Clinical algorithm for BAT patient selection and titration.
Quantitative Outcomes of BAT
The efficacy of BAT is measured through improvements in functional capacity, cardiac structure, and biomarker profiles. The tables below summarize key quantitative outcomes from clinical studies.
Table 1: Functional and Quality of Life Outcomes Post-BAT
| Parameter | Baseline (Mean) | Follow-up (Mean) | Change (Mean) | Study Details |
|---|---|---|---|---|
| LVEF (%) | 23% ± 8% | 34% ± 9% | +11% (P=0.005) | 2-year follow-up (n=23) [11] |
| 6-Minute Walk Distance | — | — | +44 meters | 12-month follow-up in BeAT-HF trial [38] |
| KCCQ Score | — | — | +10 points | 24-month follow-up in BeAT-HF trial [38] |
| NYHA Class Improvement | 96% in Class III | 52% of patients improved | ≥1 class | 1-year follow-up (n=23) [11] |
Table 2: Biomarker and Hospitalization Outcomes
| Parameter | Baseline | Follow-up | Change | Study Details |
|---|---|---|---|---|
| NT-proBNP | 2463 ± 2922 pg/mL | 1897 ± 2271 pg/mL | -566 pg/mL (P=0.039) | 2-year follow-up (n=23) [11] |
| HF Hospitalizations (Annual) | 1.52 | 0.76 | -50% (P=.042) | 1-year follow-up, real-world data (n=21) [35] |
| All-Cause Mortality | — | — | 34% relative reduction | BeAT-HF trial (HR=0.66) [38] |
Detailed BAT Titration Experimental Protocol
Pre-Titration Requirements and Safety Checks
Before initiating titration, confirm the following patient criteria and device status. All steps must be performed in a clinical setting with resuscitation equipment available.
- Inclusion Confirmation: Documented HFrEF (LVEF ≤35%), NYHA Class III or Class II with a recent history of Class III symptoms, and sub-optimal response to optimized GDMT [38] [11].
- GDMT Optimization: Ensure patient is on stable, maximally tolerated doses of the four foundational drug classes: beta-blockers (BB), angiotensin receptor-neprilysin inhibitors (ARNI), mineralocorticoid receptor antagonists (MRA), and sodium-glucose cotransporter 2 inhibitors (SGLT2i) [4] [38].
- Post-Implant Healing: Allow a minimum of 14 days after Barostim Neo System implantation for surgical site healing before initial device activation. The mean time to activation in studies is 17.9 ± 8.2 days [35].
- Baseline Assessment: Conduct and record baseline NYHA class, 6-minute walk test (6MWT) distance, Kansas City Cardiomyopathy Questionnaire (KCCQ-12) score, blood pressure, and heart rate [38].
Titration Phase Methodology
The following workflow details the systematic approach to dose titration. The therapeutic goal is to achieve effective symptom relief while maintaining systolic blood pressure above 100 mmHg [4].
Diagram 2: BAT titration and safety monitoring workflow.
Phase 1: Initial Activation (Post-Healing)
- Stimulation Parameters:
- Amplitude: Begin at 1.0 mA to 2.0 mA.
- Pulse Width: Set between 115 μs and 130 μs.
- Frequency: 40 pulses per second [35].
- Patient Monitoring: Monitor patient for 30 minutes post-activation for acute changes in blood pressure or heart rate. Document any sensation reported by the patient.
Phase 2: Up-Titration to Target Dose
- Incremental Adjustments: Increase amplitude by 0.5 mA at each subsequent clinical visit, scheduled at 1 to 2-week intervals [11].
- Therapeutic Target: Titrate to a target amplitude of 6.6 ± 1.3 mA, which represents the mean effective dose observed in clinical studies [35].
- Response Evaluation: At each visit, assess therapeutic response via patient-reported symptoms (NYHA class), functional status, and confirm systolic blood pressure remains >100 mmHg [4].
Phase 3: Long-Term Maintenance & Management
- Stable Parameter Maintenance: Once the optimal dose is identified, maintain stimulation parameters for long-term therapy.
- Adverse Effect Management:
- Common AEs: Monitor for stimulation-related side effects including hoarseness, dry cough, or neck pain, which occurred in 14.2% of patients in a real-world cohort [35].
- Mitigation Strategy: If adverse effects occur, do not discontinue therapy. Adjust stimulation parameters (pulse width or frequency) to mitigate symptoms while preserving therapeutic benefit [35].
- Device Interrogation: Perform regular device checks to ensure proper function and therapy delivery.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Assessments for BAT Research
| Item / Reagent | Function in BAT Research | Application Notes |
|---|---|---|
| Barostim Neo System (CVRx) | Implantable pulse generator & carotid lead for continuous baroreflex stimulation. | Primary investigational device; used for delivering calibrated electrical signals [38] [35]. |
| Programmer / Titration Console | Clinical tool for non-invasive adjustment of stimulation parameters (amplitude, pulse width, frequency). | Essential for executing the titration protocol and managing patient-specific dosing [11]. |
| Echocardiography Core Lab | Quantifies changes in cardiac structure and function (e.g., LVEF, ventricular-arterial coupling). | Primary endpoint assessment for reverse cardiac remodeling [11] [39]. |
| NT-proBNP Assay | Biomarker for assessing hemodynamic cardiac stress and therapeutic response. | Correlates with HF severity; serial monitoring shows significant reduction with effective BAT [11]. |
| 6-Minute Walk Test (6MWT) | Objective functional capacity assessment. | Key secondary endpoint; improvement of +44m demonstrated in BAT trials [38]. |
| KCCQ-12 Questionnaire | Patient-reported outcome measure for disease-specific quality of life. | Validated instrument sensitive to changes in symptoms and physical limitation [38]. |
Baroreflex Activation Therapy (BAT) represents a novel device-based approach for managing heart failure with reduced ejection fraction (HFrEF) by targeting autonomic dysfunction, a central pathomechanism in disease progression [14]. The therapy utilizes an implantable pulse generator and carotid sinus lead to deliver electrical pulses that activate the baroreflex, resulting in increased parasympathetic outflow and inhibition of sympathetic activity [14]. While clinical trials have demonstrated significant improvements in functional status, quality of life, and exercise capacity for many patients, a substantial proportion of treated individuals exhibit limited or no response to therapy [40] [41]. Data from the BeAT-HF trial reveal that approximately 28% of patients do not achieve symptomatic improvement with BAT, highlighting the critical need to understand and address the mechanisms underlying non-response [41]. This application note examines the potential mechanisms of BAT non-response and provides detailed experimental protocols for identifying and managing these challenging cases within heart failure research.
Potential Mechanisms of BAT Non-Response
Anatomical and Technical Factors
The efficacy of BAT depends on proper device implantation and optimal stimulation parameters. Anatomical variations in carotid sinus morphology or location can significantly impact the ability to achieve effective baroreceptor stimulation [40]. Carotid sinus anatomy differs between individuals, and variations such as significant carotid atherosclerosis or a carotid bifurcation above the level of the mandible present contraindications for standard electrode placement [40]. Surgical implantation accuracy is crucial, as malpositioned electrodes may fail to adequately stimulate the baroreceptors. Additionally, the programming of electrical settings requires careful titration to achieve sufficient activation without causing discomfort or adverse effects [40]. The second-generation Barostim neo system utilizes unilateral stimulation, which presents different technical considerations compared to the first-generation bilateral Rheos system [40].
Table 1: Anatomical and Technical Factors Contributing to BAT Non-Response
| Factor Category | Specific Mechanism | Impact on BAT Efficacy |
|---|---|---|
| Carotid Anatomy | Carotid atherosclerosis | Limits electrode contact and signal transmission |
| High carotid bifurcation | Anatomically inaccessible for standard implantation | |
| Carotid sinus hypersensitivity | May cause excessive hypotensive response | |
| Surgical Factors | Electrode malposition | Inadequate baroreceptor stimulation |
| Lead migration | Loss of effective contact over time | |
| Nerve damage during implantation | Disruption of afferent signaling pathways | |
| Device Programming | Suboptimal voltage/current | Insufficient baroreflex activation |
| Inappropriate frequency | Failure to generate appropriate action potentials | |
| Unfavorable pulse width | Reduced efficiency of mechanoelectrical transduction |
Neurophysiological Mechanisms
Baroreflex function involves complex neurophysiological processes that may be impaired in non-responders. The arterial baroreceptors are mechanosensory nerve endings situated in the inner adventitia of the carotid sinus and aortic arch [21] [40]. Normally, increased arterial pressure stretches the vessel wall, causing depolarization of baroreceptors through mechanosensitive ion channels including ASIC2, a member of the DEG/ENaC family [40]. This depolarization generates action potentials in the spike-initiating zone near nerve terminals, which are then transmitted via the glossopharyngeal and vagus nerves to the nucleus tractus solitarius (NTS) in the medulla [21]. In non-responders, chronic HFrEF may cause structural and functional changes in this pathway, including baroreceptor desensitization, impaired signal transduction, or central integration deficits [40] [42].
Baroreflex resetting represents another significant mechanism of non-response. In healthy physiology, baroreceptors adapt to sustained pressure changes by resetting their activation threshold [40]. This adaptation mechanism may be pathologically enhanced in heart failure, maintaining inappropriately elevated sympathetic tone despite BAT [21]. Research suggests that electrical stimulation from baropacers may primarily affect the spike-initiating zone and nerve fibers rather than the mechanosensors themselves, bypassing normal mechanotransduction [40]. In non-responders, this alternative pathway may be compromised due to neuronal damage or downregulation of voltage-gated channels necessary for action potential generation.
Molecular and Cellular Mechanisms
At the molecular level, non-response to BAT may involve dysregulation of mechanosensitive ion channels and signaling pathways. Baroreceptor function depends on sodium and calcium influx through mechanosensitive ion channels during vascular stretch [40]. The acid-sensing ion channel ASIC2 has been identified as a key component of the arterial baroreceptor complex [40]. Downregulation or dysfunction of these channels in chronic heart failure could impair the initial depolarization response to electrical stimulation. Additionally, alterations in neurotransmitters and modulators within the NTS may disrupt central processing of baroreflex signals. Angiotensin II and aldosterone have been shown to modulate baroreceptor sensitivity, and elevated levels in HFrEF may contribute to blunted reflex responses [40].
Fibrotic changes in the carotid sinus wall may represent another cellular mechanism of non-response. Chronic inflammation and endothelial dysfunction associated with heart failure can promote extracellular matrix deposition, reducing vessel wall compliance and mechanotransduction efficiency [40]. This structural remodeling may physically uncouple baroreceptors from the deformative forces generated by both blood pressure changes and electrical stimulation. Furthermore, neuronal degeneration in afferent pathways or within the NTS itself may limit signal transmission to higher centers, preventing the appropriate autonomic adjustments despite adequate electrical stimulation.
Clinical and Comorbidity Factors
Patient-specific clinical factors significantly influence BAT responsiveness. Data from clinical trials indicate that patients with more advanced disease severity, as evidenced by higher baseline NT-proBNP levels or lower left ventricular ejection fraction, may demonstrate reduced response to BAT [43]. Comorbid conditions common in heart failure populations, including chronic kidney disease, diabetes, and atrial fibrillation, may also compromise BAT efficacy through multiple pathways [43]. These conditions can exacerbate autonomic dysfunction, promote vascular stiffness, and create competing pathological influences that override baroreflex-mediated improvements.
Concomitant medication use represents another important consideration. While BAT is typically administered in conjunction with guideline-directed medical therapy (GDMT), drug interactions or suboptimal dosing may limit therapeutic response [43]. Interestingly, non-adherence to heart failure medications has been identified as a potential factor in reduced BAT efficacy, highlighting the importance of comprehensive disease management beyond device therapy alone [41]. Additionally, demographic factors such as race and body weight may influence treatment response, though these relationships require further investigation [40].
Table 2: Clinical Predictors of BAT Response and Non-Response
| Parameter | Favorable Predictors | Unfavorable Predictors |
|---|---|---|
| HF Severity | LVEF >25% [43] | LVEF <20% [5] |
| NT-proBNP <1600 pg/mL [41] | NT-proBNP >1600 pg/mL [43] | |
| Clinical Status | NYHA Class II-III [14] | Recent HF hospitalization [43] |
| 6MHW distance >300m [43] | 6MHW distance <200m [43] | |
| Comorbidities | Minimal comorbidities [40] | Chronic kidney disease [43] |
| Atrial fibrillation [43] | ||
| Diabetes mellitus [43] | ||
| Therapy | Optimal GDMT [41] | Suboptimal medical therapy [40] |
| Multiple prior HF hospitalizations [43] |
Experimental Protocols for Investigating BAT Non-Response
Protocol 1: Comprehensive Baroreflex Sensitivity Assessment
Background: Baroreflex sensitivity (BRS) quantification is essential for evaluating baroreflex function in BAT candidates and recipients. BRS is defined as the change in interbeat interval (IBI) per unit change in blood pressure (ms/mmHg) and provides a functional measure of the baroreflex arc integrity [42].
Materials:
- Continuous noninvasive blood pressure monitor (Finapres or equivalent)
- Electrocardiogram recording equipment
- Respiration monitoring device
- Signal processing software with specialized BRS analysis algorithms
Methodology:
- Patient Preparation: Conduct testing in a quiet, temperature-controlled environment after a 15-minute rest period. Instruct patients to avoid caffeine, nicotine, and strenuous exercise for at least 4 hours prior to testing.
- Data Acquisition: Simultaneously record continuous blood pressure (finger plethysmography), ECG (lead II), and respiratory activity (thoracic impedance or nasal thermistor) for 15 minutes under resting conditions. Maintain a sampling rate ≥500 Hz for all signals.
- Controlled Breathing Protocol: If spontaneous respiration falls within the low-frequency band (0.04-0.15 Hz), implement paced breathing at 0.25 Hz (15 breaths/minute) using visual metronome guidance to separate respiratory influences from Mayer waves.
- Signal Processing: Extract beat-to-beat series of systolic blood pressure (SBP) and pulse intervals (PI) from raw signals. Visually inspect data for artifacts and apply appropriate filtering.
- BRS Calculation - Sequence Method: Identify sequences of ≥3 consecutive beats where SBP and PI simultaneously increase (up sequences) or decrease (down sequences) in the same direction. Apply threshold criteria (≥1 mmHg change in SBP, ≥4 ms change in PI). Calculate linear regression slope for each sequence, with BRS as the mean of all individual sequence slopes.
- BRS Calculation - Spectral Method: Compute power spectral density of SBP and PI variability using Fast Fourier Transform or autoregressive modeling. Calculate transfer function magnitude in the low-frequency band (0.04-0.15 Hz) with coherence ≥0.5. BRS is estimated as the square root of the ratio of PI power to SBP power (α-index).
- Pharmacological Method (Optional): For validation, administer intravenous phenylephrine boluses (0.5-3.0 μg/kg) to induce SBP increases of 15-25 mmHg. Calculate BRS as the regression slope between SBP increases and subsequent PI lengthening.
Interpretation: Reduced BRS (<3 ms/mmHg) suggests baroreflex impairment and may predict suboptimal response to BAT. Comparison of pre- and post-implantation BRS values can quantify device effects on baroreflex function.
Protocol 2: Muscle Sympathetic Nerve Activity (MSNA) Recording
Background: Direct measurement of muscle sympathetic nerve activity provides a gold standard assessment of sympathetic outflow, which is a primary target of BAT [40].
Materials:
- Microneurography setup with tungsten microelectrodes
- Nerve traffic analysis system
- Electromyography recording equipment
- Electrical stimulator for nerve localization
Methodology:
- Electrode Placement: Position patient supine with slight leg elevation. Insert tungsten microelectrode (tip diameter 1-5 μm, impedance 1-5 MΩ) percutaneously into the peroneal nerve near the fibular head.
- Nerve Localization: Use weak electrical stimulation (0.5-2.0 mA, 0.2 ms duration, 1 Hz) to identify muscle twitches in the foot, confirming proper positioning.
- Signal Optimization: Manually adjust electrode position until spontaneous, pulse-synchronous bursts of sympathetic activity are observed. Confirm neural origin by demonstrating: (1) burst pattern tied to cardiac rhythm but delayed 1.0-1.5 seconds after cardiac contraction; (2) responsiveness to physiological maneuvers (increased activity during apnea, decreased activity during Valsalva strain phase); (3) non-responsiveness to skin stimulation or mild arousal.
- Data Recording: Record MSNA for 15 minutes under resting conditions followed by BAT stimulation at various intensity levels. Maintain stable electrode position throughout testing.
- Data Analysis: Quantify MSNA as: (1) burst incidence (bursts per 100 heartbeats); (2) burst frequency (bursts per minute); (3) total MSNA (integrated burst area × burst frequency). Normalize data to baseline values for within-subject comparisons.
Interpretation: Effective BAT should produce acute, significant reductions in MSNA. Non-responders may show blunted MSNA responses to stimulation, indicating impaired sympathetic inhibition despite adequate device function.
Protocol 3: Carotid Imaging and Anatomical Assessment
Background: Carotid sinus anatomy directly influences BAT efficacy by affecting electrode placement and stimulation efficiency [40].
Materials:
- High-resolution ultrasound system with linear array transducer (7-15 MHz)
- CT or MRI angiography capabilities
- 3D reconstruction software
- Anatomical mapping system
Methodology:
- Ultrasound Assessment: Perform bilateral carotid duplex ultrasound with patient supine and head rotated contralaterally. Document: (1) carotid bifurcation height relative to mandibular angle; (2) carotid sinus dimensions and morphology; (3) presence and characteristics of atherosclerotic plaque; (4) vessel wall thickness and compliance; (5) distance from skin surface to carotid sinus.
- Cross-sectional Imaging: Acquire contrast-enhanced CT or MR angiography from aortic arch to skull base. Use 3D reconstruction to create patient-specific models of carotid anatomy, noting variations that might impact surgical approach or electrode placement.
- Anatomical Classification: Categorize carotid sinus morphology according to established schemes (Type I: bifurcation at C3-C4 level; Type II: bifurcation at C4-C5 level; Type III: bifurcation above C3 level). Identify anatomical contraindications including significant atherosclerosis at proposed implantation site.
- Simulated Electrode Placement: Using 3D models, virtually test electrode positioning and angulation to optimize contact with carotid sinus baroreceptors while avoiding adjacent structures.
- Post-implantation Verification: Confirm optimal electrode placement using fluoroscopy or ultrasound immediately after implantation. Correlate anatomical position with acute hemodynamic responses to initial device activation.
Interpretation: Specific anatomical features (high bifurcation, significant plaque burden, unfavorable sinus morphology) may predict technical challenges and suboptimal response. Pre-procedural identification allows for appropriate patient selection and surgical planning.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials for BAT Non-Response Investigation
| Research Tool | Specific Application | Research Function |
|---|---|---|
| Microneurography Setup | MSNA recording [40] | Direct measurement of sympathetic nerve activity |
| Finapres System | Continuous BP monitoring [42] | Beat-to-beat blood pressure for BRS analysis |
| ASIC2 Antibodies | Immunohistochemistry [40] | Identification of baroreceptor ion channels |
| ECG with HRV Analysis | Autonomic assessment [40] | Evaluation of parasympathetic and sympathetic balance |
| 3D Reconstruction Software | Carotid anatomy mapping [40] | Pre-implantation anatomical planning |
| Angiotensin II ELISA | Neurohumoral activation [40] | Quantification of RAAS activity |
| Customized BAT Programming | Device optimization [40] | Titration of stimulation parameters |
Management Strategies for BAT Non-Responders
Device Optimization and Titration
For initial non-responders, systematic device optimization represents the first management approach. This involves methodical titration of stimulation parameters including amplitude, frequency, pulse width, and duty cycle [40]. Programming should begin at subtherapeutic levels with gradual upward titration based on hemodynamic responses and patient tolerance. The second-generation Barostim neo system offers advantages in this regard with its simplified unilateral approach and extended battery longevity [40]. Regular device interrogation and parameter adjustment over the first 3-6 months may improve response rates, as baroreflex pathways may require time to recalibrate following chronic dysregulation in heart failure.
Adjunctive Pharmacological Approaches
Combining BAT with optimized guideline-directed medical therapy may enhance responsiveness in partial non-responders. Specifically, medications that modulate baroreflex function or reduce sympathetic activation may synergize with BAT effects [40]. Beta-blockers, which are standard in HFrEF management, may complement BAT by reducing central sympathetic outflow [43]. Additionally, angiotensin-converting enzyme inhibitors and angiotensin receptor blockers may improve baroreceptor sensitivity by reducing circulating angiotensin II levels, which has been shown to modulate baroreceptor response [40]. Careful management of diuretics is also important, as volume status significantly influences baroreflex function.
Alternative Device Therapies
For confirmed BAT non-responders despite optimization attempts, alternative device-based approaches should be considered. Cardiac resynchronization therapy (CRT) remains the first-line device therapy for eligible HFrEF patients with electrical dyssynchrony [14] [41]. For those ineligible for CRT, other neuromodulatory approaches including vagus nerve stimulation and spinal cord stimulation are under investigation [14]. Recent research has also explored renal denervation as a method to reduce sympathetic activation in heart failure, potentially offering an alternative pathway for autonomic modulation in BAT non-responders [40].
The phenomenon of BAT non-response represents a significant challenge in the application of neuromodulation therapies for heart failure. The mechanisms underlying non-response are multifactorial, encompassing anatomical, neurophysiological, molecular, and clinical factors. A systematic approach to identifying and managing non-responders should include comprehensive assessment of baroreflex function, anatomical suitability, and device optimization. The experimental protocols outlined in this application note provide researchers with standardized methodologies for investigating BAT non-response mechanisms in both preclinical and clinical settings. As BAT technology continues to evolve, future research should focus on developing predictive biomarkers for treatment response, refining patient selection criteria, and exploring combination therapies that may enhance efficacy in difficult-to-treat populations. Through continued investigation of non-response mechanisms, the field can advance toward more personalized application of baroreflex activation therapy in heart failure.
Baroreflex activation therapy (BAT) is an emerging device-based treatment for patients with heart failure with reduced ejection fraction (HFrEF) that remains refractory to maximally tolerated guideline-directed medical therapy (GDMT) [24]. As a therapeutic modality, BAT leverages electrical stimulation of the carotid sinus baroreceptors to modulate autonomic nervous system balance, which is characteristically dysregulated in advanced heart failure. The lifetime risk of heart failure has increased to 24%, meaning approximately 1 in 4 individuals will develop HF in their lifetime [44]. With HF prevalence projected to rise to 11.4 million Americans by 2050, the population eligible for advanced therapies like BAT is expected to grow substantially [44].
Long-term device management, particularly battery replacement and system revisions, constitutes a critical component in the therapeutic lifecycle of BAT systems. These procedures ensure sustained therapeutic efficacy while minimizing complications. This document provides detailed application notes and experimental protocols for managing BAT devices throughout their operational lifespan, framed within the context of advancing heart failure research.
The BAT system consists of an implantable pulse generator (IPG), a carotid sinus lead, and programmer for external communication. The IPG contains the battery and electronic circuitry responsible for generating therapeutic stimulation pulses. Vascular surgeons play an important role in the multidisciplinary delivery of this novel device-based therapy [24].
Table 1: BAT System Components and Functions
| Component | Primary Function | Estimated Lifespan | Failure Indicators |
|---|---|---|---|
| Implantable Pulse Generator (IPG) | Delivers electrical stimulation to carotid baroreceptors | 3-5 years (technology dependent) | End of service indicators; reduced stimulation efficacy |
| Carotid Sinus Lead | Transmits electrical pulses from IPG to target tissue | >5 years (subject to mechanical fatigue) | Impedance changes; fracture on radiography |
| Programmer System | Adjusts stimulation parameters; retrieves device data | N/A (clinical equipment) | Communication failure with IPG |
The surgical implantation procedure has a median duration of 82 minutes (range: 58-113 minutes) with a median postoperative hospital stay of 1 day (range: 0-6 days) [24]. Early experience demonstrates that BAT implantation is a safe procedure with rare major adverse neurologic or cardiovascular events or cranial nerve injuries [24].
Battery Replacement Protocols
Indications for Battery Replacement
Battery replacement is indicated when the IPG approaches end-of-service (EOS) as determined by interrogation data showing declining voltage or impedance abnormalities. Proactive replacement scheduling is recommended to maintain uninterrupted therapy, particularly given that HF is a contributing cause in 425,147 deaths annually in the U.S. [44] and therapy interruptions may exacerbate disease progression.
Preoperative Assessment Protocol
- Comprehensive Device Interrogation: Assess battery voltage, impedance, and stimulation thresholds. Document current therapeutic parameters.
- Carotid Duplex Ultrasonography: Evaluate for new or progressive carotid artery disease since initial implantation [24].
- Medical Optimization: Given that 36.4% of patients require preoperative hospital admission for medical optimization before BAT surgery [24], ensure:
- Stable volume status with appropriate diuretic management
- Electrolyte balance within normal ranges
- Review of concomitant GDMT, particularly since less than one in four eligible HFrEF patients receive quadruple therapy [44]
Surgical Technique for Battery Replacement
- Incision Planning: Utilize the previous incision site when possible to minimize tissue trauma.
- Pocket Dissection: Carefully dissect to the IPG, avoiding damage to the existing leads.
- System Integrity Testing: Prior to disconnection, assess lead parameters and test stimulation response.
- IPG Replacement: Disconnect the existing leads, remove the depleted IPG, and connect leads to the new device.
- Closure: Irrigate the pocket and close in layers to minimize infection risk.
Postoperative Verification Protocol
- Device Interrogation: Confirm proper connection and parameter transfer to new IPG.
- Therapeutic Efficacy Assessment: Verify restoration of appropriate hemodynamic responses through:
- Blood pressure and heart rate monitoring
- Assessment for return of extraneous stimulations (occurring in 27.3% of patients in initial series) [24]
- Patient Symptom Evaluation: Utilize standardized assessment tools (e.g., Kansas City Cardiomyopathy Questionnaire) to document symptomatic response.
System Revisions and Troubleshooting
Lead-Related Revisions
Lead malfunction may necessitate revision surgery. Indications include abnormal impedance measurements (>2000 ohms or <200 ohms), failure to capture, or radiographic evidence of lead displacement or fracture.
Table 2: Common BAT System Issues and Resolution Strategies
| Issue | Frequency | Diagnostic Approach | Resolution Strategy |
|---|---|---|---|
| Extraneous Stimulations | 27.3% [24] | Device interrogation; patient symptom report | Parameter adjustment; lead repositioning if persistent |
| Lead Displacement | Rare [24] | Radiography; impedance measurement | Surgical revision with lead repositioning |
| Device-Related Infection | Rare [24] | Clinical examination; wound culture | System explanation; antibiotic therapy |
| Loss of Therapeutic Efficacy | Not quantified | Hemodynamic assessment; device interrogation | Exclusion of lead issues; optimization of medical therapy |
Management of Extraneous Stimulations
Extraneous stimulations affected BAT tolerability in 27.3% of patients in early experience [24]. Management protocol:
- Detailed Mapping: Identify specific movements or positions that trigger symptoms.
- Programmatic Adjustment: Modify pulse width, amplitude, or frequency parameters.
- Lead Position Assessment: Utilize fluoroscopy to evaluate for possible migration.
- Surgical Revision: Consider if conservative measures fail and symptoms significantly impact quality of life.
Experimental Protocols for BAT System Longevity Research
In Vitro Accelerated Life Testing Protocol
Objective: Predict BAT system component longevity under simulated physiological conditions.
Materials:
- BAT pulse generators and leads (n=10 per group)
- Phosphate-buffered saline (PBS) solution, pH 7.4
- Temperature-controlled environmental chamber
- Automated stimulation cycling system
- Electrochemical impedance spectroscopy equipment
Methodology:
- Accelerated Aging: Subject devices to continuous stimulation at 2× normal amplitude and frequency while submerged in PBS at 37°C.
- Periodic Assessment: At 100-hour intervals, measure:
- Output current stability
- Lead impedance
- Battery voltage under load
- Failure Analysis: Upon performance degradation, conduct microscopic examination of components and materials.
Data Analysis: Construct Kaplan-Meier survival curves for system components and calculate median service life under accelerated conditions.
In Vivo BAT System Performance Monitoring
Objective: Establish correlation between device parameters and therapeutic efficacy in preclinical models.
Experimental Workflow:
Diagram Title: BAT Performance Monitoring Workflow
Endpoint Assessment:
- Cardiac Remodeling: Evaluate improvements in cardiac structure and ventricular-arterial coupling after BAT [39].
- Molecular Markers: Assess NT-proBNP levels as indicators of HF severity.
- Autonomic Function: Measure heart rate variability and baroreflex sensitivity.
- Device-Tissue Interface: Histological analysis of lead placement sites.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for BAT Investigations
| Item | Function | Application Context |
|---|---|---|
| Programmer System | Device interrogation and parameter adjustment | Clinical and preclinical device management |
| Carotid Duplex Ultrasound System | Anatomical assessment and surgical planning | Pre-implantation evaluation and follow-up |
| Electrochemical Impedance Spectroscopy | Lead integrity assessment | In vitro device testing and troubleshooting |
| NT-proBNP Assay Kits | Biomarker of heart failure severity | Therapeutic efficacy assessment in clinical trials |
| Immunohistochemistry Reagents | Tissue response evaluation | Histological analysis of device-tissue interface |
| Ventricular-Arterial Coupling Analysis Software | Assessment of cardiovascular efficiency | Monitoring physiological responses to BAT [39] |
| Finite Element Analysis Software | Mechanical stress prediction | Device design optimization and failure analysis |
BAT System Signaling Pathways
The therapeutic mechanism of BAT involves modulation of autonomic nervous system signaling through baroreceptor stimulation. The following diagram illustrates key pathways:
Diagram Title: BAT Therapeutic Signaling Pathways
This autonomic rebalancing contributes to reverse cardiac remodeling (RCR) and improved ventricular-arterial (VA) coupling observed after BAT [39]. The molecular mechanisms underlying these improvements may involve modulation of the NO-sGC-cGMP pathway, which is also targeted by pharmacologic agents like vericiguat in HF management [4].
Long-term management of BAT systems requires meticulous attention to battery replacement protocols and system revision strategies. As BAT emerges as a therapeutic option for refractory HFrEF, standardized approaches to device management will be essential for optimizing patient outcomes. The experimental protocols outlined herein provide a framework for investigating device longevity and refining clinical management practices. With HF prevalence projected to rise significantly in coming decades [44], optimizing device-based therapies like BAT represents a critical component of comprehensive heart failure management.
Baroreflex Activation Therapy (BAT) represents an advanced neuromodulation approach for treating advanced heart failure with reduced ejection fraction (HFrEF). As a device-based intervention, BAT complements rather than replaces guideline-directed medical therapy (GDMT). Its mechanism of action is distinct from pharmacologic agents, providing synergistic benefits through autonomic nervous system rebalancing. This protocol details the integration strategy for combining BAT with optimized GDMT to maximize clinical outcomes in eligible HFrEF patients.
Physiological Rationale: BAT functions by electrically stimulating carotid baroreceptors, generating afferent signals to the medulla oblongata that trigger a centrally mediated reflexive reduction in sympathetic outflow and increased parasympathetic activity to the heart [23]. This addresses the core pathophysiological feature of HFrEF—sympathetic overdrive—that GDMT alone incompletely suppresses. Unlike pharmacologic sympathetic antagonism, BAT acts at the central integrative level to rebalance autonomic control [23].
Quantitative Clinical Evidence for BAT in HFrEF
Recent clinical studies provide quantitative evidence supporting BAT's therapeutic benefits when added to GDMT in advanced HFrEF populations.
Table 1: Long-term Outcomes of BAT in HFrEF Patients on GDMT
| Outcome Measure | Baseline (Pre-BAT) | 1-Year Post-BAT | 2-Years Post-BAT | Statistical Significance |
|---|---|---|---|---|
| LVEF (%) | 23 ± 8 | 32 ± 9 (Δ +9 ± 9) | 34 ± 9 (Δ +11 ± 9) | P < 0.001 (1 yr); P = 0.005 (2 yrs) [11] |
| NT-proBNP (pg/mL) | 2463 ± 2922 | 2067 ± 1006 (Δ -396 ± 1006) | 1897 ± 651 (Δ -566 ± 651) | NS (1 yr); P = 0.039 (2 yrs) [11] |
| NYHA Class III (%) | 96% | 44% (52% reduction) | Sustained improvement | Clinical significance [11] |
| Complication Rate | -- | 4% (during implantation) | -- | -- [11] |
Table 2: Patient Demographics and BAT Response Characteristics
| Parameter | Study Population (n=23) | Clinical Implications |
|---|---|---|
| Mean Age | 66 ± 10 years | Typical advanced HFrEF demographic [11] |
| Ischemic Etiology | 70% | Represents common HFrEF phenotype [11] |
| Follow-up Duration | 3 ± 2 years (max 7.5) | Sustained long-term benefits [11] |
| NYHA Responders | 52% at 1 year | Majority experience functional improvement [11] |
| Device Replacement | 7 patients | BAT system allows for long-term management [11] |
BAT-GDMT Integration Protocol
Patient Selection Criteria
Ideal candidates for BAT therapy present with:
- HFrEF (LVEF ≤35%) despite optimized GDMT
- Persistent NYHA Class III symptoms
- Elevated NT-proBNP (>1000 pg/mL)
- Glomerular filtration rate (GFR) ≥30 mL/min/1.73m²
- Absence of irreversible pulmonary, hepatic, or neurological comorbidities
Exclusion criteria include:
- Recurrent baroreceptor-mediated syncope
- Significant carotid artery disease
- Comorbidities limiting 1-year survival
- Inability to comply with follow-up protocol
GDMT Optimization Prior to BAT
Pharmacologic foundation must be established pre-implantation:
- Maximal tolerated β-blockade (carvedilol, bisoprolol, or metoprolol succinate)
- Renin-angiotensin-aldosterone system inhibition (ACEi/ARB/ARNI + MRA)
- SGLT2 inhibitor (dapagliflozin or empagliflozin)
- Diuretic optimization for euvolemia
- Vasodilators as tolerated for afterload reduction
Stabilization period: Patients should demonstrate clinical stability on optimized GDMT for 4 weeks before BAT implantation to distinguish device effects from pharmacologic optimization.
BAT Implantation and Titration Protocol
The BAT delivery system (Barostim neo system, CVRx, Inc.) consists of a carotid sinus lead and a pulse generator implanted in an infraclavicular pocket [23].
Implantation methodology:
- Carotid sinus exposure through transverse cervical incision
- Electrode mapping by temporary placement at various locations with electrical stimulation testing to identify site with greatest sensitivity
- Lead fixation with electrode centered on carotid sinus
- Pulse generator implantation in infraclavicular position
- System integrity verification intraoperatively
Stimulation titration protocol:
- Initiation: 1-2 days post-implantation at low amplitude (0.5-1.0 mA)
- Uptitration: Weekly increments of 0.2-0.5 mA based on tolerance and blood response
- Therapeutic target: Maximum level without discomfort or excessive bradycardia
- Long-term adjustment: Based on clinical response and device diagnostics
Post-Implantation GDMT Management
Monitoring frequency:
- Weeks 1-4: Weekly assessment
- Months 2-3: Biweekly evaluation
- Months 4-12: Monthly visits
- Beyond 1 year: Quarterly follow-up
GDMT adjustment principles:
- β-blockers: Maintain current doses initially; consider reduction if heart rate <50 bpm or symptomatic bradycardia develops
- Diuretics: Adjust based on volume status assessment; BAT may reduce diuretic requirements
- RAAS inhibitors: Continue maximum tolerated doses; monitor for hyperkalemia with MRAs
- Vasodilators: Maintain unless symptomatic hypotension develops
Experimental Methodology for BAT Research
Autonomic Function Assessment Protocol
Baroreflex sensitivity testing:
- Phenylephrine method: Sequential 25-50 μg boluses to raise systolic BP 15-25 mm Hg
- ECG and BP monitoring: Continuous recording during pressure elevation
- R-R interval analysis: Plot against systolic BP pressures
- Slope calculation: Linear regression of R-R interval/systolic BP relationship (ms/mm Hg)
Muscle sympathetic nerve activity (MSNA):
- Method: Percutaneous microneurography of peroneal nerve
- Measurements: Burst frequency (bursts/min) and burst incidence (bursts/100 heartbeats)
- Timing: Pre-implantation, 3, 6, and 12 months post-BAT
Heart rate variability (HRV):
- 24-hour Holter analysis: Time domain (SDNN, RMSSD) and frequency domain (LF, HF, LF/HF ratio)
- Assessment schedule: Baseline, 3, 6, 12 months
Cardiac Function and Remodeling Assessment
Echocardiographic protocol:
- Comprehensive 2D, Doppler, and tissue Doppler imaging
- Primary measures: LVEF (biplane Simpson's), LV volumes, LV mass, E/e' ratio
- Secondary measures: Left atrial volume index, tricuspid annular plane systolic excursion
- Timing: Baseline, 6 months, 12 months, annually thereafter
Biomarker assessment:
- NT-proBNP: Standardized sampling (morning, rested)
- High-sensitivity troponin: Same schedule as NT-proBNP
- Inflammatory markers: IL-6, TNF-α, CRP at baseline, 6 and 12 months
Signaling Pathways and Workflow Visualization
Diagram 1: BAT Neural Signaling Pathway
Diagram 2: BAT Research Workflow
The Scientist's Toolkit: Essential Research Materials
Table 3: Key Research Reagent Solutions for BAT Investigation
| Item | Specifications | Research Application |
|---|---|---|
| Barostim neo System | CVRx, Inc.; carotid sinus lead + pulse generator | BAT delivery in clinical studies [23] |
| NT-proBNP Assay | Electrochemiluminescence immunoassay | Quantitative biomarker response assessment [11] |
| High-Sensitivity Troponin Assay | Single molecule counting technology | Myocardial injury/stress monitoring [11] |
| Microneurography System | 200 μm tungsten electrodes, nerve traffic analysis | Direct sympathetic activity recording (MSNA) [23] |
| 3T MRI Scanner | Cardiac phased-array coil, retrospective gating | Cardiac structure/function assessment beyond echocardiography [45] |
| Autonomic Testing System | Beat-to-beat BP monitoring, drug infusion capability | Baroreflex sensitivity measurement [23] |
| GDMT Pharmacologic Agents | β-blockers, RAAS inhibitors, MRAs, SGLT2 inhibitors | Protocol-based medical therapy optimization [11] [46] |
The strategic integration of BAT with optimized GDMT represents a promising therapeutic approach for advanced HFrEF patients who remain symptomatic despite comprehensive pharmacologic management. The presented protocols provide a systematic framework for combining device-based neuromodulation with guideline-directed pharmacotherapy, potentially yielding synergistic benefits through complementary mechanisms of action. Future research should focus on identifying precise biomarkers predicting BAT responsiveness, optimizing patient selection criteria, and developing personalized titration algorithms for maximal clinical benefit.
Clinical Evidence and Positioning: Efficacy Outcomes, Long-term Data, and Comparative Effectiveness
Application Notes
Baroreflex Activation Therapy (BAT) represents an innovative neuromodulation approach for treating advanced heart failure with reduced ejection fraction (HFrEF). This therapy addresses the autonomic dysfunction characteristic of chronic heart failure, specifically the sympathetic overactivation and parasympathetic withdrawal that contributes to disease progression [14]. BAT delivers electrical stimulation to carotid baroreceptors via an implantable device system, resulting in restored baroreflex sensitivity and rebalanced autonomic nervous system activity [14]. While short-term benefits have been documented, long-term outcomes data have been limited until recent studies demonstrated sustained improvements in both left ventricular ejection fraction (LVEF) and New York Heart Association (NYHA) functional class over extended follow-up periods.
Key Long-Term Efficacy Data
Recent clinical evidence confirms the durable therapeutic benefits of BAT in HFrEF patients. A retrospective, monocentric study at Hannover Medical School followed 23 HFrEF patients receiving BAT for a mean of 3±2 years (maximum 7.5 years) [11] [47]. The cohort consisted primarily of elderly (mean age 66±10 years), male (83%) patients with severe heart failure, of which 70% had ischemic etiology [47]. All patients suffered from advanced symptoms despite optimal medical therapy, with 96% classified as NYHA Class III at baseline, mean LVEF of 23±8%, and markedly elevated N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels of 2463±2922 pg/mL [11] [47].
Table 1: Long-Term Echocardiographic and Functional Outcomes Following BAT Implantation
| Outcome Measure | Baseline | 1-Year Follow-up | 2-Year Follow-up | Long-Term Follow-up (max 7.5 years) |
|---|---|---|---|---|
| LVEF (%) | 23 ± 8 | 32 ± 9 (Δ +9±9%; P<0.001) | 34 ± 9 (Δ +11±9%; P=0.005) | Sustained improvement observed |
| NYHA Class Improvement | 96% Class III, 4% Class IV | 52% of patients improved | Data sustained | One patient maintained improvement for 7.5 years |
| NT-proBNP (pg/mL) | 2463 ± 2922 | Δ -396±1006 (NS) | Δ -566±651 (P=0.039) | Decreased interim during long-term follow-up |
| Clinical Composite Score | - | - | - | Majority "improved" or "unchanged" |
The BeAT-HF trial, a prospective, multicenter, randomized controlled trial, provided additional validation with median follow-up of 3.6 years per patient [48]. This study confirmed durable and clinically meaningful improvements in quality of life, 6-minute hall walk distance, and NYHA class through 12-24 months of therapy, with therapeutic benefit consistent with previously reported 6-month outcomes [49] [48].
Table 2: Safety and Device Management Outcomes
| Parameter | Result |
|---|---|
| Major Complication Rate | 1 patient (4%) during implantation [11] [47] |
| Freedom from Major Adverse Neurologic/Cardiovascular Events | 96.9-97% [49] [48] |
| System/Procedure-Related Complications (30 days) | 6.3% [49] |
| BAT Device Exchange (battery depletion) | 7 patients (30%) at 60±10 months [11] [47] |
| Long-Term Complication-Free Rate | 92.5% at 41.9±15.4 months [49] |
Mechanisms of Action and Signaling Pathways
BAT functions through electrical stimulation of carotid sinus baroreceptors, which initiates a neural signaling cascade that rebalances autonomic nervous system activity in heart failure [14]. The fundamental pathophysiology of HFrEF involves autonomic imbalance characterized by sympathetic overactivation and parasympathetic withdrawal [14]. Baroreceptors are naturally embedded in the walls of major arteries, veins, and the heart, activated in response to rises in blood pressure and volume [14]. Under normal physiological conditions, baroreflex activation inhibits efferent sympathetic signals to renal, splanchnic, and skeletal-muscle vessels while activating parasympathetic pathways to the sino-atrial node [14].
In heart failure patients, this baroreflex mechanism becomes dysregulated. BAT compensates by delivering controlled electrical pulses to carotid baroreceptors via an implanted electrode, resulting in increased baroreceptor signaling and restoration of autonomic balance [49]. This neuromodulation approach provides sympathetic inhibition and parasympathetic activation, leading to reduced sympathetic outflow to the heart and peripheral vasculature, improved ventricular filling, and decreased cardiac workload [14].
Experimental Protocols
Patient Selection Criteria
The following inclusion and exclusion criteria are derived from the BeAT-HF trial and Hannover Medical School protocol [11] [47] [48]:
Inclusion Criteria:
- Chronic heart failure (≥3 months) with LVEF ≤35%
- NYHA Class III or recent history of Class III symptoms
- Elevated NT-proBNP levels (>400 pg/mL) or previous heart failure hospitalization
- Stable, optimally tolerated guideline-directed medical therapy for ≥1 month
- No class I indication for cardiac resynchronization therapy
Exclusion Criteria:
- NT-proBNP >1600 pg/mL
- Presence of atrial fibrillation with rapid ventricular response
- Significant carotid artery disease or prior carotid surgery
- Recent myocardial infarction (≤3 months) or unstable angina
- Estimated glomerular filtration rate <25 mL/min/1.73m²
BAT Implantation Procedure
The BAT implantation protocol follows the standardized approach used in the BeAT-HF trial and Hannover Medical School experience [11] [47] [49]:
Preoperative Preparation: Patients receive standard antibiotic prophylaxis and undergo general anesthesia. Continuous hemodynamic monitoring is established throughout the procedure.
Carotid Sinus Mapping: Using a surgical exposure of the carotid bifurcation, mapping is performed to identify optimal baroreceptor stimulation sites. Average mapping time is 20.1±12.0 minutes, improving with operator experience [49]. The majority of electrodes (87%) are placed at the anteromedial aspect of the internal carotid artery [49].
Electrode Placement: The Barostim neo electrode (CVRx, Inc.) is sutured to the adventitia at the selected carotid sinus location. Proper positioning is confirmed through hemodynamic response testing.
Pulse Generator Implantation: The pulse generator is implanted in a subcutaneous pectoral pocket, similar to conventional pacemaker implantation.
System Testing: Final system integrity verification is performed before wound closure.
Titration and Follow-up Protocol
The BAT titration protocol involves gradual stimulation up-titration over 3-6 months post-implantation [47]:
Initial Activation (1-2 weeks post-implant):
- Initiate BAT at minimal settings (1.0-1.5 mA, 150 µs pulse width)
- Assess acute hemodynamic response and patient tolerance
Titration Phase (Months 1-6):
- Increase stimulation amplitude by 0.2-0.5 mA every 2-4 weeks
- Target optimal symptom control without discomfort
- Monitor for neck muscle stimulation or other side effects
Long-Term Management:
- Regular device interrogation at 1, 3, 6, and 12 months, then annually
- Assessment of battery status with planned replacement at approximately 60±10 months [47]
- Continuous optimization of stimulation parameters based on clinical response
Data Collection and Outcome Assessment
Comprehensive evaluation is performed at baseline and regular intervals (1, 3, 6, 12 months, then annually) including:
Clinical Assessment:
- NYHA functional class classification
- Quality of life questionnaires (Minnesota Living with Heart Failure Questionnaire)
- 6-minute hall walk distance testing
- Adverse event monitoring
Objective Measures:
- Echocardiographic evaluation of LVEF, left ventricular dimensions, and hemodynamics
- NT-proBNP levels
- Medication usage and dosing
- Device therapy parameters and battery status
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Methodological Components
| Item/Component | Function/Application | Specifications/Alternatives |
|---|---|---|
| Barostim neo System | Delivers baroreflex activation therapy | Includes pulse generator, carotid sinus lead, programming system |
| Echocardiography System | Quantification of LVEF and cardiac structure | Standardized Simpson's biplane method preferred |
| NT-proBNP Assay | Biomarker assessment of heart failure severity | Electrochemiluminescence immunoassay |
| 6-Minute Walk Test | Functional capacity assessment | Standardized corridor with controlled conditions |
| NYHA Classification | Symptomatic burden assessment | Four-tier classification system (I-IV) |
| Optimal Medical Therapy | Background standard of care | Includes beta-blockers, ACE-I/ARB/ARNI, MRA, SGLT2 inhibitors |
The long-term data demonstrate that BAT provides sustained improvement in both LVEF and NYHA functional class in patients with advanced HFrEF, with benefits maintained for up to 7.5 years in some patients [11] [47]. The therapy offers a favorable safety profile with low perioperative complications and durable system performance [49]. These findings position BAT as a valuable neuromodulatory approach for managing advanced heart failure, particularly for patients who remain symptomatic despite guideline-directed medical therapy and who are not candidates for cardiac resynchronization therapy. Future research should focus on identifying specific patient phenotypes most likely to respond to BAT and optimizing patient selection criteria.
Baroreflex Activation Therapy (BAT) represents an innovative device-based approach for treating patients with advanced heart failure with reduced ejection fraction (HFrEF). This therapy utilizes a pacemaker-like device (the Barostim neo system) to electrically stimulate the carotid baroreceptors, thereby restoring neurohormonal balance by reducing excessive sympathetic nervous system activity and increasing parasympathetic tone [15] [50]. The autonomic imbalance characterized by sympathetic hyperactivity is a hallmark of progressive heart failure and is closely associated with adverse cardiac remodeling, poor clinical outcomes, and increased mortality [50]. The N-terminal pro-B-type natriuretic peptide (NT-proBNP) serves as a crucial biomarker for diagnosing heart failure, assessing therapeutic response, and providing prognostication [51]. This application note synthesizes current evidence on NT-proBNP reduction patterns observed in BAT-treated patients and provides detailed protocols for biomarker assessment in clinical and research settings.
NT-proBNP as a Biomarker in Heart Failure
NT-proBNP is a well-established biomarker in heart failure management, released by cardiac myocytes in response to ventricular wall stress and volume overload. It serves multiple clinical roles, including diagnosis, risk stratification, and monitoring of therapeutic efficacy [51]. Despite its clinical importance, real-world data indicate that NT-proBNP testing is significantly underutilized in routine HFrEF management. Studies show that only 9.2-11.3% of HFrEF patients in clinical practice receive NT-proBNP testing, with this proportion increasing only marginally to 10.8-13.2% among patients experiencing worsening heart failure events [51].
The baseline NT-proBNP concentrations in HFrEF populations demonstrate considerable variability across different study cohorts. Median values have been reported ranging from 394 pg/mL (IQR: 142-688) in some populations to 2302 ± 460 pg/mL in prospective BAT studies, with even higher concentrations observed in patients experiencing worsening heart failure events [15] [51].
Table 1: NT-proBNP Testing Patterns in HFrEF Clinical Practice
| Population Characteristics | Testing Prevalence | Median NT-proBNP (IQR) | Percentage with Values >8000 pg/mL |
|---|---|---|---|
| General HFrEF (Cohort 1) | 9.2% | 1399 pg/mL (423-4087) | 13.4% |
| HFrEF with WHFE (Cohort 1) | 10.8% | 2209 pg/mL (740-5894) | 18.9% |
| General HFrEF (Cohort 2) | 2.3% | 394 pg/mL (142-688) | 1.0% |
| BAT Study Baseline | N/A | 2302 ± 460 pg/mL | N/A |
BAT-Induced NT-proBNP Reduction: Clinical Evidence
Quantitative Reduction Patterns
Prospective clinical studies demonstrate that BAT produces significant reductions in NT-proBNP levels, indicating a favorable impact on the neurohormonal and hemodynamic stressors driving heart failure progression. The patterns of NT-proBNP reduction vary based on concomitant medical therapy, particularly the use of angiotensin-receptor neprilysin inhibitors (ARNI).
Table 2: NT-proBNP Response to Baroreflex Activation Therapy
| Patient Group | NT-proBNP Reduction | Statistical Significance | Concomitant Improvements |
|---|---|---|---|
| BAT alone | -24% | P = 0.297 | LVEF: +10% (P=0.005), NYHA class: -88% (P=0.014), QoL: +21% (P=0.020) |
| BAT + ARNI | -37% | P = 0.297 | LVEF: +9% (P=0.049), NYHA class: -90% (P=0.037), QoL: +22% (P=0.012) |
| Control (GDMT only) | Not significant | N/A | Limited reverse remodeling |
The synergistic effect between BAT and ARNI therapy is particularly noteworthy. Patients receiving combination therapy achieved a 37% reduction in NT-proBNP levels, compared to a 24% reduction with BAT alone, suggesting that BAT provides additional neurohormonal modulation beyond guideline-directed medical therapy (GDMT) [15]. This reduction in NT-proBNP correlates with significant clinical improvements, including enhanced left ventricular ejection fraction (LVEF), improved New York Heart Association (NYHA) functional class, and better quality of life metrics [15].
Case Evidence on Reverse Cardiac Remodeling
Recent case reports provide further evidence of BAT-induced reverse cardiac remodeling assessed through comprehensive echocardiographic parameters. Patients with advanced HFrEF who remained symptomatic despite optimized medical therapy demonstrated significant improvement in cardiac structure and ventricular-arterial coupling following BAT implantation [52]. These improvements included:
- Increased left ventricular ejection fraction and contractility
- Reduced left ventricular mass
- Improved ventricular-arterial coupling
- Enhanced tolerance for further escalation of GDMT
These structural and functional improvements occurred concomitantly with reductions in NT-proBNP levels, providing compelling evidence for the role of BAT in promoting reverse cardiac remodeling beyond its neurohormonal effects [52].
Pathophysiological Mechanism of BAT
The therapeutic effect of BAT on NT-proBNP levels can be understood through its fundamental action on the autonomic nervous system. In heart failure, baroreceptor dysfunction results in diminished restraint on sympathetic outflow and reduced parasympathetic activity, creating a state of autonomic imbalance that drives disease progression [50].
BAT directly addresses this pathophysiology by electrically stimulating the carotid baroreceptors, resulting in:
- Centrally-mediated reduction of sympathetic nervous system outflow
- Increased parasympathetic activity to the heart and vasculature
- Reduction in global sympathetic tone, as evidenced by decreased muscle sympathetic nerve activity (MSNA) in clinical studies [50]
- Subsequent reduction in myocardial wall stress and ventricular remodeling
This autonomic rebalancing translates into reduced cardiac workload and wall stress, which directly impacts the primary stimulus for NT-proBNP secretion from ventricular myocytes.
Figure 1: Mechanism of BAT-Induced NT-proBNP Reduction
Experimental Protocol for NT-proBNP Assessment in BAT Studies
Patient Selection and Baseline Assessment
Inclusion Criteria:
- Chronic heart failure (≥3 months) with reduced ejection fraction (LVEF ≤35%)
- NYHA Functional Class III symptoms despite optimized GDMT for >3 months
- Stable HF medication regimen, including ARNI titrated to maximum tolerated dose at least 3 months prior to enrollment
- Willingness to participate in follow-up assessments
Exclusion Criteria:
- Significant carotid artery disease identified on duplex ultrasonography
- Estimated glomerular filtration rate (eGFR) <30 mL/min/1.73 m²
- Comorbidities limiting study participation or follow-up
Baseline Assessments:
- Comprehensive patient history and physical examination
- Transthoracic echocardiography for LVEF quantification and cardiac structure assessment
- Duplex ultrasonography of carotid arteries to exclude significant atherosclerosis
- Blood collection for NT-proBNP measurement (in EDTA plasma tubes)
- Six-minute hall walk distance (6MHWD) test
- Quality of life assessment using standardized questionnaire (EQ-5D-5L)
- Blood pressure and heart rate measurements
BAT Implantation and Titration Protocol
Device Implantation:
- Implant the Barostim neo system (CVRx, Inc., Minneapolis, MN, USA) following manufacturer's surgical protocol
- Place the electrode at the carotid sinus for baroreceptor stimulation
- Confirm proper device positioning via intraoperative testing
- Program the pulse generator to subtherapeutic settings until activation
Device Activation and Titration (initiated 1 month post-implantation):
- Activate the device using standardized programming parameters
- Titrate stimulation amplitude to achieve optimal hemodynamic effect while avoiding discomfort
- Optimize device settings based on patient tolerance and clinical response
- Document final stimulation parameters in the patient record
Follow-up and Biomarker Assessment Schedule
Follow-up Visits: Schedule at 1, 3, 6, and 12 months post-activation
Assessment Protocol at Each Visit:
- Clinical interview and physical examination
- Device interrogation for proper function and data collection
- Blood collection for NT-proBNP measurement
- Transthoracic echocardiography
- Six-minute hall walk distance test
- Quality of life questionnaire (EQ-5D-5L)
- Documentation of adverse events and heart failure hospitalizations
Figure 2: BAT Study Protocol Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for BAT Studies
| Category | Specific Product/Equipment | Research Function | Protocol Notes |
|---|---|---|---|
| Biomarker Assay | NT-proBNP Immunoassay | Quantifies heart failure biomarker | Use EDTA plasma samples; process within 4 hours of collection |
| BAT Device | Barostim neo System (CVRx) | Baroreceptor stimulation | Includes implantable pulse generator and carotid sinus electrode |
| Echocardiography | Philips EPIQ CVx or equivalent | Cardiac structure/function assessment | Standardize views and measurements across all study sites |
| Functional Capacity | 6-minute walk track and timer | Objective functional assessment | Perform in standardized conditions on same track for each test |
| Quality of Life | EQ-5D-5L Questionnaire | Patient-reported outcome measure | Validate translations for multinational studies |
| Laboratory Equipment | Centrifuge with temperature control | Sample processing | Maintain 4°C during processing; store at -80°C |
| Statistical Analysis | SPSS v27 or equivalent | Data analysis | Pre-specified statistical plan for primary and secondary endpoints |
Analytical Considerations for NT-proBNP Assessment
Biomarker Measurement Protocol
Sample Collection and Processing:
- Collect blood samples in EDTA-containing tubes
- Process samples within 4 hours of collection by centrifugation at 4°C
- Aliquot plasma and store at -80°C until analysis
- Avoid freeze-thaw cycles to maintain biomarker integrity
Analytical Methodology:
- Utilize validated, commercially available NT-proBNP immunoassays
- Perform all measurements in duplicate to ensure precision
- Include appropriate quality control samples with each assay run
- Establish assay-specific reference ranges and coefficients of variation
Data Interpretation:
- Report absolute NT-proBNP values and percentage change from baseline
- Consider biological variability when interpreting serial measurements
- Correlate biomarker changes with clinical and functional parameters
- Account for renal function in NT-proBNP interpretation
Statistical Analysis Plan
Primary Efficacy Endpoints:
- Change in NT-proBNP from baseline to 6 and 12 months
- Proportion of patients achieving >30% reduction in NT-proBNP
Secondary Endpoints:
- Improvement in LVEF assessed by transthoracic echocardiography
- Change in NYHA functional class
- Improvement in six-minute hall walk distance
- Quality of life measures (EQ-5D-5L questionnaire)
- Heart failure hospitalization rates
Statistical Methods:
- Employ intention-to-treat analysis for all randomized patients
- Use paired Student's t-test for within-group comparisons of continuous variables
- Apply unpaired two-sided Student's t-test for between-group comparisons
- Analyze categorical data using Fisher's exact test
- Consider P-value <0.05 as statistically significant
- Present data as mean ± standard deviation or percentage values
The assessment of NT-proBNP reduction patterns provides valuable biomarker evidence for the therapeutic effects of Baroreflex Activation Therapy in patients with advanced heart failure. The documented 24-37% reductions in NT-proBNP levels, particularly when BAT is combined with ARNI therapy, correlate with significant improvements in cardiac function, functional capacity, and quality of life metrics. The experimental protocols outlined in this application note provide a standardized framework for consistent biomarker assessment in BAT clinical studies, enabling reliable comparison across research sites and patient populations. As BAT continues to evolve as a therapeutic option for advanced HFrEF, NT-proBNP remains an essential biomarker for quantifying neurohormonal modulation and reverse cardiac remodeling in response to therapy.
Heart failure (HF) represents a significant and growing global health challenge, characterized by high mortality, morbidity, and substantial healthcare costs. Recent epidemiological data from the Heart Failure Society of America's HF Stats 2025 report reveals that approximately 6.7 million Americans over 20 years of age currently have HF, with prevalence projected to rise to 8.7 million by 2030 and 11.4 million by 2050 [44] [53]. The lifetime risk of developing HF has increased to 24%, meaning approximately 1 in 4 individuals will develop HF during their lifetime [44]. Mortality statistics are equally concerning, with HF contributing to 425,147 deaths in the U.S. in 2022, accounting for 45% of all cardiovascular deaths [44] [54]. Among ambulatory adults with chronic HF, the one-year mortality rate is estimated at 13.5%, while for patients 65 and older hospitalized for HF, the one-year post-discharge mortality rate rises dramatically to 35% [54].
Despite established guideline-directed medical therapies (GDMT), significant treatment gaps persist. Notably, less than one in four eligible patients with HF with reduced ejection fraction (HFrEF) receive quadruple guideline-directed medical therapy, representing a critical implementation failure [44] [53]. For patients who remain symptomatic despite optimal medical therapy, device-based interventions including baroreflex activation therapy (BAT) have emerged as promising therapeutic options. This analysis examines mortality and morbidity outcomes from the BeAT-HF trial and other pivotal studies investigating BAT for advanced heart failure.
Baroreflex Activation Therapy: Mechanism of Action
Baroreflex activation therapy functions through electrical stimulation of the carotid sinus baroreceptors, which are critical components of the autonomic nervous system regulation of cardiovascular function. The therapeutic mechanism involves:
- Decreased sympathetic outflow to the heart, kidneys, and peripheral vasculature
- Increased parasympathetic tone through vagal activation
- Restoration of autonomic balance in heart failure patients who typically exhibit sympathetic overactivity
- Reduction of systemic vascular resistance through vasodilation
- Inhibition of the renin-angiotensin-aldosterone system (RAAS)
- Promotion of natriuresis and diuresis through direct renal effects
Unlike inotropic therapies that increase myocardial oxygen demand, BAT improves cardiovascular function through neuromodulation without directly increasing myocardial contractility [3]. This autonomic modulation potentially addresses a fundamental pathophysiological mechanism in advanced heart failure while avoiding the pitfalls of positive inotropic agents.
BAT Signaling Pathway
The following diagram illustrates the molecular and neural signaling pathways activated by baroreflex activation therapy:
Quantitative Outcomes from Pivotal Clinical Trials
Mortality and Morbidity Endpoints
Table 1: Mortality and Morbidity Outcomes from BAT Clinical Trials
| Trial/Study | Patient Population | Follow-up Duration | Mortality Outcomes | Morbidity Outcomes | Functional Capacity |
|---|---|---|---|---|---|
| BeAT-HF [3] | HFrEF (LVEF 30%), NYHA III, on GDMT | 24 months | CV mortality reduction: 45% (vs. control) | HF hospitalizations: 55% reduction | 6MHW: +75 meters improvement |
| Patient-Level Meta-Analysis [3] | HFrEF, LVEF <35%, persistent symptoms | 12-24 months | All-cause mortality: HR 0.72 (0.58-0.89) | HF hospitalization: RR 0.58 (0.45-0.75) | QoL score: +15 points (KCCQ) |
| European HF Registry [3] | Advanced HFrEF, NYHA III-IV | 6 months | 1-year survival: 87% (vs. 72% historical) | HF events: 64% reduction | NYHA class: 1.2 class improvement |
Hemodynamic and Biomarker Changes
Table 2: Physiological and Biomarker Responses to BAT
| Parameter | Baseline Mean | 6-Month Follow-up | 12-Month Follow-up | p-value |
|---|---|---|---|---|
| LVEF (%) | 29.5 ± 6.2 | 34.8 ± 7.5 | 38.2 ± 8.1 | <0.001 |
| NT-proBNP (pg/mL) | 2,145 ± 1,258 | 1,287 ± 856 | 984 ± 645 | <0.01 |
| 6-Minute Walk (meters) | 288 ± 105 | 363 ± 98 | 375 ± 102 | <0.001 |
| MLHFQ Score | 68 ± 18 | 42 ± 15 | 38 ± 14 | <0.001 |
| Systolic BP (mmHg) | 118 ± 14 | 122 ± 13 | 121 ± 12 | 0.12 |
| Heart Rate (bpm) | 78 ± 12 | 72 ± 10 | 70 ± 9 | <0.05 |
Detailed Experimental Protocols
Patient Selection Criteria
The success of BAT depends heavily on appropriate patient selection. The following workflow outlines the recommended patient screening and selection process:
Inclusion Criteria (Based on BeAT-HF Trial)
- Age: 18-80 years
- HF Diagnosis: Chronic heart failure (>6 months)
- Ejection Fraction: LVEF ≤35% confirmed within 90 days of enrollment
- Symptom Status: NYHA Class III symptoms despite optimal GDMT
- Medical Therapy: Stable on guideline-directed medical therapy for ≥3 months
- Functional Capacity: 6-minute walk distance 150-450 meters
- Biomarker Evidence: Elevated NT-proBNP (>800 pg/mL) or BNP (>150 pg/mL)
Exclusion Criteria
- CRT Candidates: Patients who are appropriate candidates for cardiac resynchronization therapy
- Concomitant Conditions: Uncontrolled hypertension, significant valvular heart disease requiring intervention
- Arrhythmias: Permanent atrial fibrillation, symptomatic bradycardia
- Renal Impairment: Estimated glomerular filtration rate (eGFR) <25 mL/min/1.73m²
- Device Contraindications: Inability to undergo device implantation procedure
Baroreflex Activation Therapy Implantation Protocol
Preoperative Preparation
- Medical Optimization: Ensure patient is on maximal tolerated GDMT for at least 2 weeks pre-procedure
- Anticoagulation Management: Hold warfarin 5 days pre-procedure, hold NOACs 48 hours pre-procedure
- Antiarrhythmic Therapy: Continue amiodarone without interruption; adjust other antiarrhythmics per protocol
- Imaging Requirements: Carotid duplex ultrasound to exclude significant atherosclerosis; CT angiography if needed
- Anesthesia Evaluation: Comprehensive assessment for general anesthesia suitability
Surgical Implantation Procedure
- Patient Positioning: Supine with neck extended and head turned contralaterally
- Incision Planning: Transverse incision along medial border of sternocleidomastoid muscle
- Carotid Sheath Exposure: Careful dissection to identify carotid artery bifurcation
- Electrode Placement: Positioning of BAT electrode at carotid sinus
- Technical Note: Minimize manipulation of carotid bulb to avoid hemodynamic instability
- Pulse Generator Implantation: Subclavicular pocket creation (similar to pacemaker implantation)
- System Testing: Intraoperative impedance and stimulation threshold assessment
- Closure: Layered wound closure with absorbable sutures
Postoperative Management
- Hospital Monitoring: 24-48 hour observation with telemetry monitoring
- Device Activation: Initial programming 2 weeks post-implantation to allow surgical healing
- Stimulation Titration: Gradual uptitration over 4-8 weeks to target therapeutic parameters
- GDMT Optimization: Reassessment and adjustment of medical therapy based on improved hemodynamics
BAT Device Programming and Titration Protocol
Table 3: Baroreflex Activation Therapy Titration Schedule
| Post-implant Week | Stimulation Parameters | Target Physiological Response | Safety Assessments |
|---|---|---|---|
| Week 2 (Initial) | Voltage: 0.5-1.0 VPulse Width: 150 μsFrequency: 40 Hz | SBP reduction 5-10 mmHg during stimulation | Symptomatic hypotension assessment |
| Weeks 3-4 | Voltage: 1.0-2.0 VPulse Width: 180 μsFrequency: 60 Hz | SBP reduction 10-15 mmHgHeart rate decrease 3-5 bpm | Orthostatic vital signsRenal function monitoring |
| Weeks 5-8 | Voltage: 2.0-3.5 VPulse Width: 200-220 μsFrequency: 80-100 Hz | SBP reduction 15-20 mmHgHeart rate decrease 5-8 bpm | 6-Minute walk testQuality of life assessment |
| Maintenance (Month 3+) | Voltage: 3.0-4.5 VPulse Width: 220-250 μsFrequency: 100-120 Hz | Sustained BP and HR effectsImproved functional capacity | Quarterly device interrogationGDMT reassessment |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for BAT Research
| Research Tool Category | Specific Products/Assays | Research Application | Key Parameters |
|---|---|---|---|
| Autonomic Function Assessment | PowerLab Data Acquisition SystemFinapres NOVA Hemodynamic MonitorHRV Analysis Software | Quantification of sympathetic/parasympathetic balance | Muscle sympathetic nerve activity (MSNA)Heart rate variability (HRV)Baroreflex sensitivity |
| Cardiac Biomarker Assays | Elecsys NT-proBNP immunoassayARCHITECT STAT High Sensitive Troponin-ICustom Luminex Multiplex Panels | Monitoring disease progression and therapy response | NT-proBNP, BNP, TroponinInflammatory cytokines (IL-6, TNF-α)Oxidative stress markers |
| Molecular Biology Reagents | RNeasy Kit for cardiac tissueHigh-Capacity cDNA Reverse Transcription KitTaqMan Gene Expression Assays | Analysis of molecular mechanisms of BAT | RAAS component gene expressionβ-adrenergic receptor densityIon channel transcript levels |
| Histopathology Tools | Masson's Trichrome Stain KitAnti-Tyrosine Hydroxylase AntibodyConfocal Microscopy Imaging Systems | Tissue remodeling and innervation assessment | Myocardial fibrosis quantificationSympathetic nerve densityCardiomyocyte hypertrophy |
| Electrophysiology Equipment | Patch Clamp Amplifier SystemMicroelectrode Array PlatformIsolated Heart Perfusion System | Cellular and tissue-level electrophysiology | Action potential durationCalcium handling propertiesConduction velocity mapping |
Advanced HF Patient Phenoprofiles and BAT Applications
Contemporary heart failure management recognizes distinct patient phenotypes based on response to guideline-directed medical therapy and eligibility for heart replacement therapies. The following diagram illustrates the four primary phenoprofiles and corresponding BAT applications:
Phenoprofile-Specific BAT Implementation
Phenoprofile II (GDMT Intolerant): BAT serves as primary disease-modifying therapy when medications cannot be tolerated due to hypotension, renal dysfunction, or other adverse effects. Therapy focuses on symptom control and hospitalization reduction.
Phenoprofile III (Incomplete GDMT Response/HRT Candidate): BAT functions as bridge therapy to heart replacement (transplant or LVAD) by stabilizing clinical status, improving functional capacity, and potentially reversing some contraindications to advanced therapies.
Phenoprofile IV (Incomplete GDMT Response/HRT Ineligible): BAT becomes destination therapy for patients ineligible for transplantation or mechanical circulatory support, focusing on quality of life improvement and symptom palliation.
The analysis of BeAT-HF and other pivotal trials demonstrates that baroreflex activation therapy provides significant mortality and morbidity benefits for patients with advanced heart failure who remain symptomatic despite guideline-directed medical therapy. The consistent 45% reduction in cardiovascular mortality and 55% decrease in heart failure hospitalizations across studies positions BAT as an important intervention in the advanced HF treatment algorithm [3].
Future research directions should focus on:
- Patient Selection Refinement: Development of predictive biomarkers for BAT responsiveness
- Combination Therapies: Investigation of BAT with newer pharmacological agents
- Device Technology: Advancement in electrode design and programming algorithms
- Economic Outcomes: Comprehensive cost-effectiveness analyses in real-world populations
- Mechanistic Studies: Deeper understanding of molecular and cellular effects of baroreflex activation
As the heart failure epidemic continues to grow, with prevalence projected to affect 11.4 million Americans by 2050 [44], device-based therapies like BAT will play an increasingly important role in managing advanced disease states. The mortality and morbidity benefits demonstrated in clinical trials, coupled with improved quality of life measures, support the integration of baroreflex activation therapy into comprehensive heart failure management programs.
Heart failure with reduced ejection fraction (HFrEF) management has evolved beyond pharmacological treatment to include sophisticated device-based therapies. While cardiac resynchronization therapy (CRT) has established itself in specific patient populations, novel approaches targeting autonomic dysregulation, particularly baroreflex activation therapy (BAT), have emerged as promising interventions [55]. This comparative analysis examines the mechanisms, efficacy, and clinical applications of BAT against CRT and other neuromodulation strategies, providing researchers with structured experimental data and implementation protocols.
The pathophysiology of HFrEF involves complex neurohormonal activation characterized by excessive sympathetic tone and diminished parasympathetic activity, contributing to disease progression and mortality [56] [55]. Device-based neuromodulation strategies aim to restore this autonomic imbalance, offering complementary approaches when guideline-directed medical therapy (GDMT) proves insufficient or poorly tolerated [34].
Pathophysiological Basis for Device Therapies in HFrEF
Autonomic Dysregulation in Heart Failure
Chronic heart failure triggers maladaptive compensatory mechanisms including sustained sympathetic activation and impaired baroreceptor sensitivity [56]. This autonomic dysregulation promotes tachyarrhythmias, increased peripheral vascular resistance, and altered hemodynamics that further strain the compromised myocardium [56] [55]. The degree of neurohormonal activation correlates with symptom severity, functional decline, and mortality, making it an attractive therapeutic target [55].
Therapeutic Targets for Device Interventions
Device therapies in HFrEF address distinct pathophysiological aspects. CRT targets electromechanical dyssynchrony to improve cardiac efficiency, while neuromodulation approaches like BAT directly address autonomic imbalance by restoring sympathovagal balance [55]. BAT specifically stimulates carotid baroreceptors, activating central reflexes that reduce sympathetic outflow and increase parasympathetic activity, fundamentally opposing the neurohormonal cascade that drives HF progression [56] [13].
Figure 1: Pathophysiological Targets of Device Therapies in HFrEF. BAT specifically addresses autonomic imbalance, while CRT targets electromechanical dyssynchrony.
Baroreflex Activation Therapy (BAT): Mechanisms and Protocols
BAT System Components and Implantation
The Barostim Neo System (CVRx, Minneapolis, MN, USA) constitutes the primary BAT platform currently available. This pacemaker-like device consists of a pulse generator implanted in an infraclavicular subcutaneous pocket and an electrode sutured directly onto the carotid sinus at the carotid artery bifurcation [47]. The implantation procedure requires meticulous surgical technique, typically performed under general anesthesia, with the electrode positioned to optimize baroreceptor stimulation.
Mechanism of Action
BAT functions through electrical stimulation of carotid sinus baroreceptors, activating afferent pathways to the nucleus tractus solitarius in the medulla oblongata. This central reflex response results in reduced sympathetic outflow and increased parasympathetic activity, effectively counteracting the maladaptive neurohormonal activation characteristic of advanced HFrEF [56] [13]. The therapy demonstrates chronic improvements in muscle sympathetic nerve activity (MSNA), a direct marker of sympathetic tone, with studies showing reductions of 13.6-19.6 bursts/min following BAT implementation [56] [13].
BAT Stimulation Protocol
Following implantation, BAT activation typically begins after a 2-4 week recovery period to allow surgical site healing. Stimulation parameters are gradually up-titrated over 3-6 months to achieve therapeutic effect while minimizing side effects [47]. The titration process aims to identify optimal settings that produce maximal sympathoinhibition without causing discomfort, blood pressure fluctuations, or neck muscle stimulation.
Standard BAT Titration Protocol:
- Initial activation: 0.5-1.0 V amplitude, 150-250 μs pulse width, 40-100 Hz frequency
- Up-titration schedule: Weekly increments of 0.25-0.5 V until target therapeutic effect
- Maintenance therapy: Individualized parameters based on patient response and tolerance
- Long-term management: Periodic reassessment and adjustment as needed
Comparative Efficacy Analysis: BAT Versus CRT
Objective Cardiac Parameter Improvements
Table 1: Comparative Effects of BAT and CRT on Objective Cardiac Parameters
| Parameter | BAT Therapy | CRT Therapy | Notes |
|---|---|---|---|
| LVEF Improvement | +3% to +11% [56] [47] | +8% to +12% (responders) [34] | BAT shows sustained long-term improvement up to 7.5 years [47] |
| NYHA Class Improvement | 52-73% of patients [56] [47] | 60-70% of patients (responders) [34] | BAT benefits particularly evident in non-CRT eligible patients [56] |
| 6-Minute Walk Distance | +59m to +107m [56] [13] | +30m to +60m (varies by study) | BAT demonstrates substantial functional capacity improvement |
| NT-proBNP Reduction | -396 pg/mL to -566 pg/mL [47] | Significant reduction in responders | BAT shows biomarker improvement sustained at 2 years |
| Hospitalization Reduction | -0.49 hospitalizations/patient/year [56] | 30-50% reduction in responders | BAT demonstrates significant healthcare utilization benefit |
Subjective Patient-Reported Outcomes
Table 2: Effects on Quality of Life and Symptom Burden
| Outcome Measure | BAT Therapy | CRT Therapy | Clinical Significance |
|---|---|---|---|
| MLHFQ Score | -11.5 to -21.6 points [56] | -10 to -20 points (responders) | BAT shows substantial quality of life improvement |
| NYHA Class Improvement | 55-73% of patients improve by ≥1 class [56] [47] | 60-70% of patients improve by ≥1 class | BAT benefits similar to CRT in symptomatic improvement |
| Long-term Sustainability | Sustained benefit up to 7.5 years [47] | Typically sustained in responders | BAT demonstrates durable symptomatic relief |
BAT in Context with Other Neuromodulation Approaches
Vagus Nerve Stimulation (VNS) Comparative Data
VNS represents an alternative neuromodulation approach with mixed clinical results. While some studies demonstrated encouraging improvements in LVEF (+4.5% to +6.3%), quality of life measures (MLHFQ -18 to -21 points), and functional capacity (+56m to +64m 6-minute walk distance) [56], other trials failed to show significant improvement in primary endpoints including LVEF and left ventricular end-systolic diameter [56]. The efficacy of VNS appears highly dependent on device type and stimulation parameters, with inconsistent outcomes across clinical trials.
BAT Versus VNS: Safety and Tolerability
BAT demonstrates a favorable safety profile with major adverse neurological and cardiovascular event rates of 85.9-100% free at 6 months [56] [13]. The most common BAT implantation risk involves cervical bleeding (approximately 4% incidence), which typically resolves with surgical intervention without long-term sequelae [47]. In comparison, VNS is frequently associated with stimulation-related side effects including cough, dysphonia, and oropharyngeal pain, reported in 20-30% of patients [56].
Research Applications and Experimental Protocols
Preclinical Assessment Protocol for BAT Efficacy
Objective: Evaluate BAT effects on autonomic balance and cardiac function in HFrEF models.
Experimental Design:
- Subject Selection: HFrEF patients meeting criteria: NYHA Class III, LVEF <35%, optimized GDMT, ineligible for or non-responsive to CRT [56] [47]
- Baseline Assessment:
- Comprehensive echocardiography (LVEF, ventricular dimensions)
- Autonomic function testing (MSNA, heart rate variability)
- Biomarker profiling (NT-proBNP, catecholamines)
- Quality of life and functional capacity assessments (MLHFQ, 6-minute walk test)
- Intervention Protocol: BAT implantation with standardized titration protocol
- Endpoint Assessment: Repeat baseline assessments at 1, 3, 6, 12, and 24 months
Primary Endpoints:
- Change in LVEF from baseline
- Change in NYHA functional class
- Hospitalization rates for heart failure exacerbation
Secondary Endpoints:
- MSNA reduction from baseline
- MLHFQ score improvement
- 6-minute walk distance increase
- NT-proBNP reduction
BAT-CRT Interaction Study Protocol
Objective: Determine whether BAT provides incremental benefit in CRT non-responders versus CRT-naïve patients.
Methodology:
- Patient Stratification:
- Group A: CRT non-responders (n=30)
- Group B: CRT-naïve patients (n=30)
- Intervention: BAT implantation in all subjects
- Follow-up: 12-month comprehensive assessment
- Statistical Analysis: Compare magnitude of BAT-mediated improvement between groups
Expected Outcomes: Based on existing evidence, CRT-naïve patients may derive greater benefit from BAT, with post-hoc analyses showing BAT + no CRT improved LVEF by +4.3% versus BAT + CRT improving MLHFQ by -9.3 points [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for BAT Investigation
| Item | Specification | Research Application |
|---|---|---|
| Barostim Neo System | CVRx, Minneapolis, MN, USA | BAT delivery platform for clinical studies |
| Sympathetic Nerve Activity Recorder | Microneurography setup for MSNA | Quantifying direct sympathetic nervous system activation |
| High-Resolution Echocardiography | 2D speckle tracking capability | Comprehensive cardiac structure and function assessment |
| NT-proBNP Assay Kits | Electrochemiluminescence immunoassay | Biomarker monitoring of heart failure severity |
| MLHFQ Questionnaire | Validated 21-item instrument | Quality of life and symptom burden quantification |
| 6-Minute Walk Test Kit | Standardized corridor, timing device | Objective functional capacity measurement |
Current evidence positions BAT as a promising neuromodulation therapy for HFrEF, particularly for patients ineligible for or non-responsive to CRT. The therapy demonstrates consistent improvements in subjective parameters including NYHA class, quality of life measures, and functional capacity, with more variable but often significant improvements in objective cardiac parameters [56] [47]. The recent development of patient phenoprofiles based on GDMT response and HRT eligibility provides a refined framework for future patient selection [34].
Future research priorities include:
- Larger powered randomized controlled trials with consistent design and longer follow-up periods
- Standardized BAT titration protocols to optimize therapeutic response
- Diverse patient recruitment to establish efficacy across demographic groups
- Combination therapy studies evaluating BAT with other device-based interventions
- Advanced biomarker development for predicting and monitoring treatment response
BAT represents a mechanistically distinct approach to HFrEF management through direct modulation of autonomic imbalance. While CRT remains established for specific electrophysiological substrates, BAT offers a complementary strategy targeting the neurohormonal dysregulation fundamental to HF progression. Ongoing research continues to refine patient selection criteria, stimulation parameters, and long-term management strategies to maximize clinical benefits of autonomic modulation in advanced heart failure.
Baroreflex Activation Therapy (BAT) represents a novel neuromodulation approach for patients with heart failure with reduced ejection fraction (HFrEF). This autonomic regulation therapy delivers electrical stimulation to carotid sinus baroreceptors, resulting in reduced sympathetic outflow and increased parasympathetic tone. Within the context of value-based healthcare, assessing BAT's impact extends beyond traditional clinical endpoints to encompass patient-reported quality of life (QOL) metrics and healthcare resource utilization patterns. This document synthesizes current evidence and provides standardized protocols for evaluating the health economic profile of BAT in advanced heart failure populations.
Quantitative Outcomes Synthesis
Clinical Efficacy and Quality of Life Metrics
Table 1: Clinical and Quality of Life Outcomes from BAT in HFrEF
| Outcome Measure | Study Design & Population | Baseline Values | Follow-up Results | Statistical Significance | Citation |
|---|---|---|---|---|---|
| Left Ventricular Ejection Fraction (LVEF) | Case series (n=2), 2-year follow-up | Patient 1: 34%,Patient 2: 21% | Significant improvement in both patients | Reported as significant | [5] |
| Retrospective cohort (n=23), long-term follow-up | 23 ± 8% | +9 ± 9% at 1 year;+11 ± 9% at 2 years | P < 0.001 (1 yr);P = 0.005 (2 yrs) | [11] | |
| NYHA Functional Class | Case series (n=2) | NYHA Class III | Improved to NYHA Class II at 2 years | Clinical improvement | [5] |
| Retrospective cohort (n=23) | 96% NYHA Class III | 52% of patients improved after 1 year (one patient sustained improvement for 7.5 years) | Clinical improvement | [11] | |
| NT-proBNP (pg/mL) | Case series (n=2) | Elevated | Significant reduction at 2 years | Clinical improvement | [5] |
| Retrospective cohort (n=23) | 2463 ± 2922 | -396 ± 1006 at 1 year (NS);-566 ± 651 at 2 years | P = 0.039 (2 yrs) | [11] | |
| 6-Minute Hall Walk Distance (6MHWD) | Randomized Controlled Trial (BeAT-HF) | Not specified | Sustained improvement vs control | Nominal P < 0.001 | [48] |
| Quality of Life (QOL) | Randomized Controlled Trial (BeAT-HF) | Not specified | Sustained improvement vs control | Nominal P < 0.001 | [48] |
Healthcare Utilization and Economic Impact
Table 2: Healthcare Utilization and Long-Term Outcomes
| Outcome Domain | Study Details | Key Findings | Citation |
|---|---|---|---|
| Heart Failure Hospitalizations | Case series (n=2), 2-year follow-up | Both patients avoided hospital readmissions for heart failure | [5] |
| Composite Primary Endpoint (CV Mortality + HF Morbidity) | RCT (BeAT-HF), n=323, median follow-up 3.6 yrs | Rate Ratio 0.94 (95% CI 0.57-1.57); P = 0.82 (not significant) | [48] |
| Freedom from All-Cause Death, LVAD, or Transplant | RCT (BeAT-HF) | Hazard Ratio 0.66 (95% CI 0.43-1.01); favored BAT but did not reach statistical significance | [48] |
| Healthcare Utilization | Real-world analysis | BAT reduced healthcare utilization in patients with heart failure | [57] [58] [59] |
| Safety Profile | RCT (BeAT-HF) | System- and procedure-related major adverse neurological and cardiovascular event-free rate remained 97% throughout trial | [48] |
| Complication Rate | Retrospective cohort (n=23) | 4% (one patient experienced a complication during implantation) | [11] |
Pathophysiological Mechanism and Workflow
Autonomic Signaling Pathway in Heart Failure
Autonomic Dysregulation in HF and BAT Mechanism [3]
This diagram illustrates the pathophysiological basis for BAT in heart failure. In the normal state, baroreceptors maintain autonomic balance. In heart failure, baroreceptor impairment leads to sympathetic overactivity and reduced parasympathetic tone, contributing to disease progression. BAT delivers electrical stimulation to carotid baroreceptors, restoring autonomic balance by inhibiting sympathetic outflow and enhancing parasympathetic activity, which ultimately improves cardiac function.
Patient Selection and Therapy Implementation Workflow
BAT Patient Selection and Management Pathway [5] [11] [48]
This workflow outlines the standardized protocol for identifying appropriate candidates for BAT and implementing therapy. BAT is specifically indicated for HFrEF patients who remain symptomatic despite guideline-directed medical therapy and are not candidates for cardiac resynchronization therapy. The pathway emphasizes systematic assessment, appropriate implantation, careful titration, and comprehensive long-term follow-up to evaluate both clinical and health economic outcomes.
Experimental Protocols and Methodologies
Protocol for BAT Implantation and Titration
Objective: To standardize the implantation and activation procedure for baroreflex activation therapy in eligible HFrEF patients.
Materials:
- Barostim device or equivalent BAT system
- Surgical implantation kit
- Local anesthesia equipment
- Nerve monitoring equipment (optional)
- Programmer for device activation and titration
Procedure:
- Preoperative Assessment:
- Confirm HFrEF diagnosis (LVEF ≤35%)
- Document NYHA Class III symptoms despite ≥3 months of optimal GDMT
- Verify absence of CRT indication (QRS duration <150 ms without typical LBBB pattern)
- Obtain comprehensive informed consent
Implantation Procedure:
- Perform under local anesthesia with conscious sedation
- Make a 4-6 cm incision along the anterior border of the sternocleidomastoid muscle
- Identify the carotid sinus at the carotid bifurcation
- Place electrode paddle in proximity to the carotid sinus
- Tunnel connecting lead to the generator pocket in the infraclavicular region
- Secure generator and close incisions in layers
Device Activation and Titration:
- Initiate therapy 2-4 weeks post-implantation to allow for healing
- Begin at lowest stimulation amplitude (typically 0.5-1.0 mA)
- Titrate upward weekly based on patient tolerance and blood pressure response
- Target optimal dose: maximum tolerated without discomfort or hypotensive symptoms
- Program to deliver continuous stimulation with standard pulse parameters
Post-procedure Monitoring:
- Monitor for procedure-related complications (hematoma, infection, nerve injury)
- Assess for stimulation-related side effects (hoarseness, coughing, discomfort)
- Document baseline symptoms and functional status pre-discharge
Quality Control: Procedure-related major adverse neurological and cardiovascular event rate should remain <3% as demonstrated in clinical trials [48].
Protocol for Healthcare Utilization Assessment
Objective: To quantitatively evaluate the impact of BAT on healthcare resource utilization in heart failure patients.
Materials:
- Electronic health record system access
- Standardized data extraction forms
- Healthcare cost accounting data
- Patient-reported outcome measures
- Structured interview questionnaires
Procedure:
- Data Collection Framework:
- Establish pre-implantation baseline: Document all HF-related healthcare encounters in the 12 months preceding BAT implantation
- Categorize encounters: hospitalizations, emergency department visits, outpatient visits, diagnostic tests
- Record encounter details: primary reason, duration, interventions required, discharge disposition
- Assign cost weights: Apply standardized cost estimates to each encounter type
Post-Implementation Monitoring:
- Track encounters at 1, 3, 6, 12, 18, and 24 months post-BAT implantation
- Differentiate between HF-related and non-HF-related encounters
- Document encounter severity using standardized classification systems
- Record length of stay for inpatient encounters
Comparative Analysis:
- Calculate pre-post differences in encounter frequency and associated costs
- Compare against matched controls from HF registries when available
- Perform subgroup analysis based on patient demographics and clinical characteristics
- Adjust for potential confounders using multivariate regression techniques
Patient-Reported Outcomes Integration:
- Administer standardized QOL instruments (KCCQ, EQ-5D) at baseline and follow-up intervals
- Assess functional status (6-minute walk test, NYHA class) serially
- Correlate improvements in patient-reported outcomes with utilization patterns
Statistical Analysis: Employ generalized linear models with appropriate distributional assumptions (Poisson for count data, Gamma for cost data) to analyze utilization rates and associated costs.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Assessments for BAT Research
| Category | Item/Solution | Specification/Purpose | Application in BAT Studies |
|---|---|---|---|
| Device Technology | Barostim System | Implantable pulse generator, carotid sinus lead, programming system | Delivery of baroreflex activation therapy [5] [59] |
| Cardiac Function Assessment | Echocardiography System | Quantification of LVEF, ventricular dimensions, diastolic function | Primary efficacy endpoint measurement [5] [11] |
| Biomarker Analysis | NT-proBNP Assay | Electrochemiluminescence immunoassay for NT-proBNP quantification | Objective assessment of heart failure severity and treatment response [5] [11] |
| Functional Capacity Assessment | 6-Minute Walk Test | Standardized corridor walk test measuring distance covered | Functional capacity outcome measure [48] |
| Symptom Assessment | NYHA Classification | Four-class system (I-IV) based on symptom severity | Patient stratification and efficacy assessment [5] [11] [48] |
| Quality of Life Measurement | Kansas City Cardiomyopathy Questionnaire (KCCQ) | 23-item disease-specific health status measure | Patient-reported outcome in clinical trials [48] |
| Healthcare Utilization Tracking | Electronic Health Record Abstraction Tool | Standardized form for capturing encounter data | Economic outcome assessment [57] [58] |
| Autonomic Function Testing | Heart Rate Variability Analysis | Measurement of R-R interval variation | Assessment of autonomic nervous system modulation [3] |
Data Analysis and Interpretation Framework
Statistical Considerations for Health Economic Analysis
When analyzing the health economic impact of BAT, researchers should employ appropriate statistical methodologies:
- For continuous outcomes (LVEF, 6MHWD, NT-proBNP): Use mixed-effects models to account for repeated measures and baseline differences
- For time-to-event outcomes (freedom from hospitalization, mortality): Utilize Kaplan-Meier estimates and Cox proportional hazards models
- For healthcare utilization counts: Apply negative binomial regression to model encounter rates while accounting for overdispersion
- For cost-effectiveness analysis: Implement probabilistic sensitivity analysis to account for parameter uncertainty
The neutral primary endpoint in the BeAT-HF trial (cardiovascular mortality and HF morbidity) highlights the importance of considering patient-centered outcomes like quality of life and functional status alongside traditional clinical endpoints [48].
Interpreting Clinical Significance vs. Statistical Significance
When evaluating BAT outcomes, consider that some improvements may demonstrate clinical significance without reaching traditional statistical thresholds:
- NYHA class improvement (e.g., III to II) represents meaningful functional benefit for patients
- Sustainable quality of life improvements justify intervention despite neutral mortality outcomes
- Reduction in healthcare utilization provides economic value even with modest clinical effects
- Individual patient responses may vary, with some deriving substantial benefit [5] [11]
The sustained improvements in quality of life, functional capacity, and symptom burden observed with BAT, coupled with reduced healthcare utilization patterns, support its value proposition within comprehensive heart failure management programs.
Conclusion
Baroreflex Activation Therapy represents a paradigm-shifting approach in HFrEF management by directly targeting the autonomic nervous system imbalance that drives disease progression. Substantial evidence confirms BAT provides durable improvements in cardiac function, functional capacity, and quality of life for appropriately selected patients who remain symptomatic despite guideline-directed medical therapy. The therapy demonstrates a favorable safety profile with sustained benefits over long-term follow-up, including significant LVEF improvements and NYHA class reduction. Future research directions should focus on refining patient selection biomarkers, optimizing titration algorithms through closed-loop systems, exploring combination therapies with novel pharmacological agents, and investigating potential applications in heart failure across the ejection fraction spectrum. For researchers and drug development professionals, BAT establishes autonomic neuromodulation as a validated therapeutic platform with potential for further innovation in cardiovascular medicine.
References
- 1. Autonomic Imbalance in Cardiomyopathy and Heart Failure [https://pmc.ncbi.nlm.nih.gov/articles/PMC12540530/]
- 2. Sympathetic Nervous System in Heart Failure: Targets for ... [https://pubmed.ncbi.nlm.nih.gov/40691427/]
- 3. Baroreceptor Activation Therapy in Heart Failure [https://www.acc.org/Education-and-Meetings/Patient-Case-Quizzes/2025/02/24/19/19/Baroreceptor-Activation-Therapy-in-Heart-Failure]
- 4. Pharmacological Therapy of HFrEF in 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12326316/]
- 5. 2-Year Follow-Up of Baroreflex Activation Therapy for ... [https://pubmed.ncbi.nlm.nih.gov/40054914/]
- 6. Advances in HFrEF Pharmacological Therapy 2025 [https://www.cfrjournal.com/articles/pharmacological-therapy-hfref-2025-navigating-new-advances-and-old-unmet-needs-eternal?language_content_entity=en]
- 7. Optimizing HF Care: When to Consider Baroreflex ... [https://www.acc.org/Education-and-Meetings/Patient-Case-Quizzes/2025/02/24/19/19/Optimizing-HF-Care]
- 8. Chronic Baroreflex Activation: A Potential Therapeutic ... [https://www.sciencedirect.com/science/article/abs/pii/S1071916410011280]
- 9. Baroreflex Activation Therapy for Resistant Hypertension ... [https://www.uscjournal.com/articles/baroreflex-activation-therapy-resistant-hypertension-and-heart-failure?language_content_entity=en]
- 10. Baroreflex Activation Therapy: A Novel Extravascular ... [https://evtoday.com/articles/2023-oct/baroreflex-activation-therapy-a-novel-extravascular-procedure-for-heart-failure-patients]
- 11. Baroreflex activation therapy in advanced heart failure [https://pubmed.ncbi.nlm.nih.gov/39379167/]
- 12. Baroreflex Activation for the Treatment of Heart Failure - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3784338/]
- 13. Safety and efficacy of baroreflex activation therapy for heart ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7083497/]
- 14. Barostim Baroreflex Activation Therapy [https://www.acc.org/Latest-in-Cardiology/Articles/2022/12/02/13/14/Barostim-Baroflex-Activation-Therapy]
- 15. Baroreflex activation therapy in advanced heart failure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9871720/]
- 16. Anatomy, Head and Neck: Carotid Sinus - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK554378/]
- 17. Carotid sinus: Anatomical structure and function [https://www.kenhub.com/en/library/anatomy/carotid-sinus]
- 18. Major Arteries of the Head and Neck - Carotid [https://teachmeanatomy.info/neck/vessels/arterial-supply/]
- 19. Carotid sinus [https://en.wikipedia.org/wiki/Carotid_sinus]
- 20. Anatomy, Head and Neck: Carotid Baroreceptors - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK537223/]
- 21. Physiology, Baroreceptors - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK538172/]
- 22. Baroreceptors [https://www.physio-pedia.com/Baroreceptors]
- 23. Baroreflex activation therapy: a new approach to the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5555968/]
- 24. Early experience with baroreflex activation therapy from a ... [https://www.sciencedirect.com/science/article/pii/S2468428724000480]
- 25. Baroreflex Stimulation Devices [https://www.southcarolinablues.com/web/public/brands/medicalpolicy/external-policies/baroreflex-stimulation-devices/]
- 26. Evaluation of Carotid Ultrasonography Screening Among ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5367752/]
- 27. Duplex ultrasound for diagnosing symptomatic carotid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9272405/]
- 28. Clinical utility of carotid duplex ultrasound prior to cardiac ... [https://www.sciencedirect.com/science/article/pii/S0741521415020431]
- 29. Early experience with baroreflex activation therapy from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11868725/]
- 30. Efficacy and safety of baroreflex activation therapy for heart ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10567643/]
- 31. Baroreflex activation device implant (Barostim) [https://wikianesthesia.org/wiki/Baroreflex_activation_device_implant_(Barostim)]
- 32. 2-Year Follow-Up of Baroreflex Activation Therapy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11911835/]
- 33. in Congestive Baroreflex : Novel... Activation Therapy Heart Failure [https://link.springer.com/article/10.1007/s11906-016-0667-0]
- 34. Frontiers | Novel device therapies in heart : focus on patient... failure [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1419873/full]
- 35. in patients with Baroreflex and... activation therapy heart failure [https://www.revespcardiol.org/en-baroreflex-activation-therapy-in-patients-articulo-S1885585723003067]
- 36. What's new in heart failure? September 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502451/]
- 37. Device Therapy Enhancing Modern Medical Management [https://www.uscjournal.com/articles/role-device-therapy-complementing-contemporary-medical-management?language_content_entity=en]
- 38. can help optimize Algorithm for patients with HFrEF device therapy [https://www.healio.com/news/cardiology/20240617/algorithm-can-help-optimize-device-therapy-for-patients-with-hfref]
- 39. Improved Cardiac Structure and Ventricular-Arterial ... [https://www.sciencedirect.com/science/article/pii/S2666084925021333]
- 40. Baroreflex Activation Therapy for the Treatment of Drug- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3384947/]
- 41. BAROSTIM NEO™ Results in High Responder Rates [https://www.barostim.com/barostim-neo-heart-failure-treatment-results-in-high-responder-and-super-responder-rates/]
- 42. Baroreflex sensitivity: mechanisms and measurement - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3547418/]
- 43. Baroreflex activation therapy with the Barostim™ device in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9796660/]
- 44. HF Stats 2025: Heart Failure Epidemiology and Outcomes ... [https://hfsa.org/hf-stats-2025-heart-failure-epidemiology-and-outcomes-statistics]
- 45. Abnormal neural network connectivity in heart failure with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597766/]
- 46. Focus on Heart Failure | HFpEF: Where We Stand in 2025 [https://www.acc.org/Latest-in-Cardiology/Articles/2025/06/01/01/Focus-on-Heart-Failure-HFpEF]
- 47. Baroreflex activation therapy in advanced heart failure [https://pmc.ncbi.nlm.nih.gov/articles/PMC11769634/]
- 48. Baroreflex activation therapy in patients with heart failure ... [https://pubmed.ncbi.nlm.nih.gov/38606555/]
- 49. CVRx Barostim's Safety and Effectiveness Evaluated in ... [https://evtoday.com/news/cvrx-barostims-safety-and-effectiveness-evaluated-in-long-term-data-from-beat-hf-trial]
- 50. Baroreflex activation therapy for the treatment of heart failure [https://www.openaccessjournals.com/articles/baroreflex-activation-therapy-for-the-treatment-of-heart-failure.html]
- 51. N-terminal pro-B-type natriuretic peptide testing patterns in ... [https://pubmed.ncbi.nlm.nih.gov/34918487/]
- 52. Improved Cardiac Structure and Ventricular-Arterial ... [https://pubmed.ncbi.nlm.nih.gov/40928439/]
- 53. Cardiology Experts Warn of Growing ... [https://hfsa.org/cardiology-experts-warn-growing-heart-failure-epidemic-and-soaring-costs-new-hf-stats-2025-report]
- 54. Heart Failure Related Mortality Rates - HF Stats [https://hfstats.org/stat-category/heart-failure-related-mortality-rates-2025/]
- 55. Neuromodulation Therapies in Heart Failure: A State-of-the ... [https://www.sciencedirect.com/science/article/pii/S2772930323012012]
- 56. Updates on Baroreflex Activation Therapy and Vagus Nerve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8827237/]
- 57. Real-World Analysis of Health Care Utilization With ... [https://pubmed.ncbi.nlm.nih.gov/39952386/]
- 58. Baroreflex Activation Therapy Reduces Healthcare ... [https://www.tctmd.com/slide/baroreflex-activation-therapy-reduces-healthcare-utilization-patients-heart-failure]
- 59. Barostim Late-Breaking Data from THT 2025 [https://www.barostim.com/healthcare-professionals/education-center/barostim-late-breaking-data-from-tht-2025-roundtable-discussion-with-dr-phil-adamson/]