Advanced Strategies for Water Permeation Prevention in Bioelectronic Encapsulation
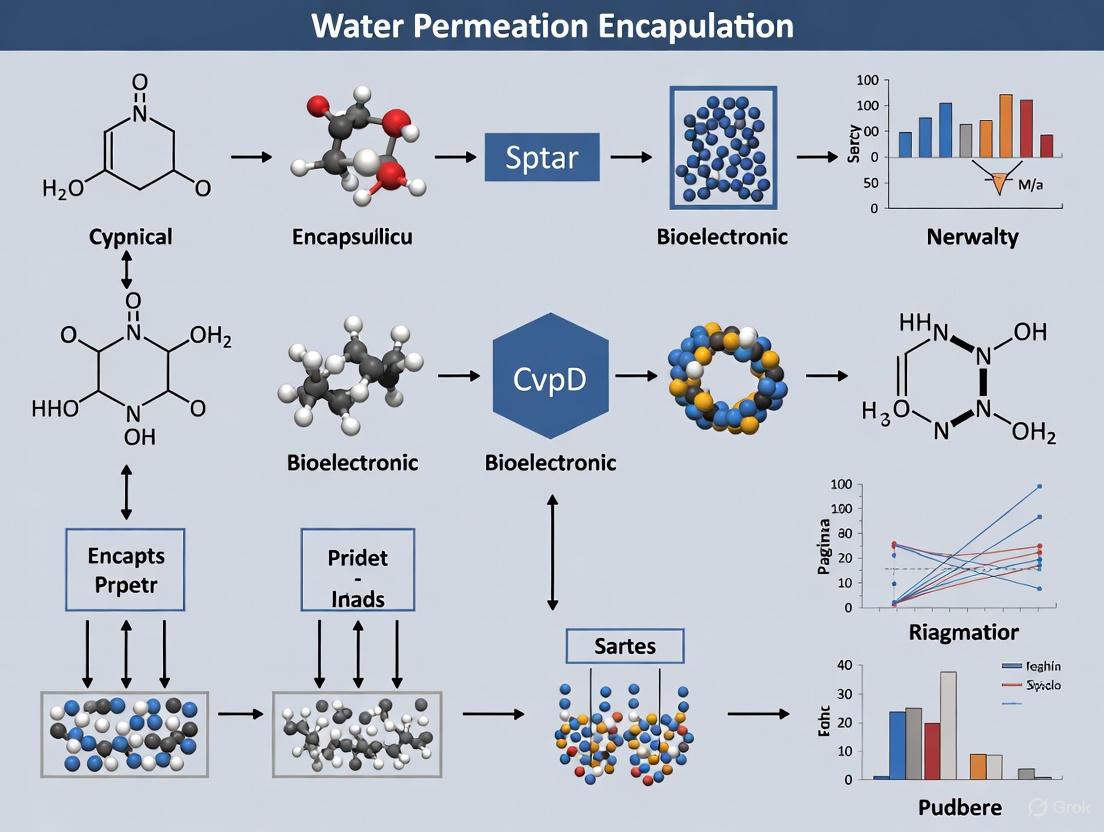
This article provides a comprehensive overview of cutting-edge encapsulation technologies designed to prevent water and ion permeation in implantable and wearable bioelectronics.
Advanced Strategies for Water Permeation Prevention in Bioelectronic Encapsulation
Abstract
This article provides a comprehensive overview of cutting-edge encapsulation technologies designed to prevent water and ion permeation in implantable and wearable bioelectronics. It explores the foundational challenges posed by the body's diverse pH environments and mobile tissues, details innovative material solutions like liquid-based encapsulation, and offers methodological guidance for implementation. Aimed at researchers, scientists, and drug development professionals, the content further covers critical troubleshooting for long-term reliability and outlines rigorous validation frameworks, including in vitro and in vivo benchmarking, to ensure device stability and clinical translation.
The Critical Challenge: Why Water and Ion Permeability Threaten Bioelectronic Longevity
Troubleshooting Guides
Encapsulation Failure in Acidic or Alkaline Environments
Problem: Bioelectronic device failure shortly after implantation in non-neutral pH environments (e.g., stomach, chronic wounds).
- Possible Cause 1: Conventional encapsulation materials like silicone elastomer or Parylene C degrade rapidly in extreme pH.
- Solution: Transition to a liquid-based encapsulation approach using oil-infused elastomers. This provides a superior barrier against H⁺ and OH⁻ ion penetration [1].
- Possible Cause 2: The encapsulation material lacks the necessary mechanical compliance, leading to microcracks in harsh environments.
Loss of Optical Transparency in Optoelectronic Implants
Problem: Encapsulated optoelectronic devices (e.g., LEDs) show dimmed light output or failure.
- Possible Cause: The encapsulation layer has low optical transmittance, scattering or absorbing light.
- Solution: Use materials with high inherent transparency. Oil-infused elastomers have an average optical transmittance of 86.67% across visible wavelengths (380–700 nm), making them suitable for optoelectronics [1].
Mechanical Failure Due to Organ Mobility
Problem: Device encapsulation cracks or delaminates when implanted in mobile organs like the gastrointestinal tract.
- Possible Cause: A mechanical mismatch between stiff encapsulation and soft, dynamic tissues.
- Solution: Select materials with a failure strain close to 100% and a Young's modulus on the order of MPa, which matches the mechanical properties of various biological systems [1].
Table 1: Performance Comparison of Encapsulation Materials in Hostile Environments
| Material | Avg. Optical Transmittance (%) | Failure Strain (%) | Young's Modulus | Performance in Acidic pH (e.g., pH 1.5) |
|---|---|---|---|---|
| Oil-Infused Elastomer | 86.67 | ~100 | ~MPa | Outstanding; functional for nearly 2 years in vitro [1] |
| Silicone Elastomer | 95.33 | ~100 | ~MPa | Fails rapidly [1] |
| Parylene C | 87.43 | <5 | ~GPa | Loses >20% performance within 1.5-19 days [1] |
| Polyimide (PI) | 7.70-71.22 | <5 | ~GPa | Not specified for long-term acidic exposure [1] |
| Liquid Metal | 0.01 | Not specified | Not specified | Susceptible to corrosion under low pH [1] |
Table 2: Quantitative Barrier Performance of Liquid-Based Encapsulation
| Test Environment | Device Type | Encapsulation Method | Result |
|---|---|---|---|
| Extremely Acidic (pH = 1.5, 4.5) | NFC Antenna | Oil-Infused Elastomer | Maintained functionality for ~2 years in vitro [1] |
| Alkaline (pH = 9.0) | Wireless Optoelectronics | Oil-Infused Elastomer | Demonstrated robust encapsulation [1] |
| Physiological (pH = 7.4) | Wireless Optoelectronics | Oil-Infused Elastomer | Year-long performance in vitro; 3 months in vivo in mice [1] |
Frequently Asked Questions (FAQs)
Q1: What makes extreme pH environments so challenging for bioelectronic encapsulation? Biological environments like the gastrointestinal system (pH as low as 1.5) and chronic wounds (pH up to 8.9) contain high concentrations of H⁺ or OH⁻ ions. These ions can penetrate encapsulation materials, leading to current leakage, corrosion of metal components, and eventual device failure. Many flexible materials are only designed for neutral physiological pH (7.4) and fail quickly in these demanding conditions [1].
Q2: How does the liquid-based encapsulation platform work? This bioinspired approach involves creating a roughened polymer elastomer (e.g., PDMS) and infusing it with a hydrophobic oil, such as Krytox (a perfluoropolyether fluid) [1] [2]. The oil fills the micro-scale defects and pores in the polymer matrix, eliminating low-energy pathways for water and ion diffusion. Furthermore, the oil causes water molecules to diffuse as clusters, which dramatically reduces the water permeation rate [2] [3].
Q3: Can this encapsulation method be used for devices requiring wireless communication and power transfer? Yes. Near-Field Communication (NFC) antennas, which are critical for wireless power and data transmission in implants, have been successfully encapsulated with this method. These devices maintained functionality after long-term soaking in acidic environments, proving the compatibility of liquid-based encapsulation with wireless technologies [1] [4].
Q4: Is the oil-infused elastomer biocompatible for long-term implantation? Research demonstrates promising biocompatibility. Immunohistochemistry studies in mice showed that the oil-coated elastomer material is biocompatible. Furthermore, encapsulated wireless optoelectronic devices maintained robust operation and were well-tolerated throughout 3-month implantations in freely moving mice [1].
Q5: The encapsulation seems effective on the top and bottom surfaces. What about the cut edges? The side edges are a potential failure point as they lack the roughened structure to lock in the oil. This can be mitigated by optimizing the laser-cutting parameters during device fabrication. Using a lower cutting speed and specific frequency (e.g., 30 kHz at 100 mm/s) creates a rougher edge surface, which helps retain the protective oil layer and enhances long-term barrier performance [1].
Experimental Protocols
Protocol 1: Fabrication of Oil-Infused Elastomer Encapsulation
This methodology details the preparation of a flexible, transparent, and pH-resistant encapsulation for implantable bioelectronics [1].
Key Reagent Solutions:
- PDMS Elastomer: A silicone-based polymer used as the base substrate.
- Krytox Oil: A synthetic perfluoropolyether (PFPE) fluid with an ultralow water diffusion coefficient, serving as the infused barrier liquid [1].
- Abrasive Paper: Used as a template to create a roughened surface on the PDMS.
Workflow:
- Elastomer Roughening: Create a ~100 µm thick roughened PDMS elastomer film using a molding technique with abrasive paper as a template. The resulting surface should have an arithmetical mean height (Sa) of ~4.7 µm [1].
- Device Sandwiching: Place the implantable bioelectronic device between two layers of the rough elastomer film, with the rough surfaces facing outward.
- Curing: Cure the PDMS-sandwiched device at ambient temperature overnight.
- Laser Cutting: Cut the encapsulated device to the desired shape using a UV laser. Optimize parameters (e.g., 30 kHz frequency, 100 mm/s speed) to create rougher edges for better oil retention [1].
- Oil Infusion: Infuse Krytox oil (to a thickness of ~15 µm) into the rough structures of the elastomer surfaces using a vacuum desiccator.
Protocol 2: In-Vitro Testing in Broad pH Environments
This protocol describes a method to validate the encapsulation's performance across a range of biologically relevant pH conditions [1].
Key Reagent Solutions:
- Buffer Solutions: Prepare solutions at pH 1.5, 4.5, 7.4, and 9.0 to simulate highly acidic, mildly acidic, physiological, and alkaline biological environments.
- NFC Antennas/Wireless Optoelectronics: These are used as model implantable devices for testing.
Workflow:
- Device Preparation: Encapsulate NFC antennas or wireless optoelectronic devices using the oil-infused elastomer method.
- Immersion Test: Soak the encapsulated devices in the different pH buffer solutions. Ensure devices are fully immersed.
- Performance Monitoring: Regularly measure and record device performance metrics. For NFC antennas, this involves monitoring wireless power transfer efficiency and data integrity. For optoelectronics, assess light output stability and device operation.
- Duration: Conduct tests over extended periods (e.g., days to months) to assess long-term durability. Compare the performance with devices encapsulated using conventional materials like plain silicone or Parylene C.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Liquid-Based Encapsulation Research
| Reagent/Material | Function/Description | Key Characteristic |
|---|---|---|
| Krytox Oil | A perfluoropolyether (PFPE) fluid infused into the elastomer to create the primary water/ion barrier [1]. | Ultralow water diffusion coefficient; hydrophobic [1]. |
| PDMS (Polydimethylsiloxane) | A silicone elastomer used as the flexible substrate and structural matrix for the encapsulation [1]. | High optical transparency; stretchable (up to ~100% strain); biocompatible. |
| Abrasive Paper | A template used during the molding process to create a microscopically rough surface on the PDMS film. | The roughness (Sa ~4.7 µm) is critical for mechanically locking the infused oil in place [1]. |
| NFC Antenna | A model implantable device component used for testing encapsulation performance for wireless applications [1] [4]. | Enables wireless power transfer and data communication; sensitive to corrosion. |
| Wireless Optoelectronic Device | A model implantable device (e.g., with LED) used to test encapsulation's optical and functional integrity [1]. | Requires encapsulation with high optical transparency and mechanical flexibility. |
Frequently Asked Questions (FAQs)
1. What are the primary failure modes for bioelectronic encapsulation? The primary failure modes are current leakage, corrosion, and device degradation. These are predominantly initiated by the ingress of water and ions from body fluids, which can lead to electrical shorts, metal corrosion, delamination of encapsulation layers, and a cascade of effects that ultimately result in device malfunction or complete failure [5] [6].
2. Why is encapsulation particularly challenging for implantable bioelectronics? Biological environments are highly dynamic, presenting challenges from broad pH ranges (from pH 1.5 in the stomach to pH 8.9 in chronic wounds), constant mechanical motion, and the presence of corrosive ions. Encapsulation must provide a superior barrier against these factors while remaining mechanically compliant to match the softness of surrounding tissues [1] [7].
3. How can I test the long-term reliability of a new encapsulation material in vitro? Standard methods include soak testing in phosphate-buffered saline (PBS) at 37°C and testing across a spectrum of pH values to simulate different biological environments. Key performance indicators include monitoring changes in electrical impedance, optical transparency (for optoelectronics), and mechanical properties over extended periods [1] [5].
4. What is corrosion-triggered delamination? This is a critical failure mechanism where body fluids diffuse along the interface between a metal (like an electrode or wire) and its polymer encapsulation. This weakens adhesion and promotes corrosion at the metal surface, leading to the progressive delamination of the polymer layer. This process creates pathways for further fluid ingress, accelerating device failure [5].
5. Are rigid or flexible encapsulation materials better for long-term implantation? The field is shifting towards soft and flexible materials. Rigid materials (like epoxy or titanium housings) have a high mechanical mismatch with soft tissues, which can cause inflammation, fibrotic encapsulation, and device failure. Flexible and stretchable materials better match tissue mechanics, promoting better integration and reducing immune responses for more stable long-term performance [7] [6].
Troubleshooting Guide: Identifying and Diagnosing Encapsulation Failure
Symptom: Sudden or Gradual Increase in Device Power Consumption
- Potential Cause: Current leakage through compromised encapsulation.
- Diagnosis:
Symptom: Unstable Electrode Impedance or Loss of Signal Fidelity
- Potential Cause: Corrosion of electrode surfaces or underlying conductive traces.
- Diagnosis:
Symptom: Visible Delamination or Discoloration Under Microscopy
- Potential Cause: Corrosion-triggered delamination or water-induced swelling at material interfaces.
- Diagnosis:
Symptom: Complete Wireless Communication or Power Transfer Failure
- Potential Cause: Catastrophic failure of internal electronics due to water and ion ingress, leading to short circuits or corrosion of antenna elements.
- Diagnosis:
Experimental Data & Material Comparisons
Table 1: Performance of Encapsulation Materials in Harsh Environments
Performance comparison of various encapsulation materials based on recent research.
| Material | Key Characteristic | Failure Timeline (pH 1.5) | Optical Transmittance (%) | Young's Modulus | Key Limitation |
|---|---|---|---|---|---|
| Oil-Infused Elastomer | Liquid perfluoropolyether (Krytox) barrier | >2 years (projected) [1] | ~86.7 [1] | ~MPa range [1] | Potential oil depletion over time |
| Silicone Elastomer (PDMS) | Standard flexible encapsulant | <19 days [1] | ~95.3 [1] | ~MPa range [7] | High water vapor permeability [5] |
| Parylene C | Conformal thin-film coating | <1.5 days [1] | ~87.4 [1] | ~GPa range [1] | Prone to cracking under strain; pin-hole defects [6] |
| Epoxy Resin | Rigid, high-performance seal | N/A (commonly used in GI tract) [1] | Opaque or Low [1] | >GPa [1] | High stiffness causes mechanical mismatch with tissues [1] |
| Liquid Metal | Ultralow water permeability | Susceptible to low pH corrosion [1] | ~0.01 [1] | Liquid | Electrically conductive, not transparent [1] |
Table 2: Common Failure Mechanisms and Diagnostic Signals
A summary of key failure mechanisms, their causes, and how to detect them.
| Failure Mechanism | Root Cause | Observable/Diagnostic Signal |
|---|---|---|
| Current Leakage | Water and ion penetration through encapsulation [5] [6] | Increased power consumption; drop in insulation resistance [8] |
| Corrosion | Electrochemical reactions at metal surfaces exposed to ions and water [5] | Increased electrode impedance; visible pitting or dissolution on metal [5] |
| Corrosion-Triggered Delamination | Diffusion of body fluids into the metal-polymer interface, weakening adhesion [5] | Visible gaps at interfaces; device malfunction without bulk material failure [5] |
| Fibrotic Encapsulation | Chronic immune response to a stiff or bio-incompatible device [7] | Degraded signal-to-noise ratio in recordings; reduced stimulation efficacy over weeks/months [7] [8] |
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function/Benefit |
|---|---|
| Sylgard-184 (PDMS) | A two-part silicone elastomer; the standard for flexible encapsulation research due to its biocompatibility and ease of processing [5]. |
| Krytox Oils | A family of perfluoropolyether (PFPE) fluids; used in liquid-based encapsulation for their ultralow water diffusion coefficient [1]. |
| Parylene C | A vapor-deposited polymer that provides a conformal, pin-hole free coating; often used as a benchmark thin-film barrier [1] [6]. |
| Phosphate-Buffered Saline (PBS) | Standard solution for in vitro soak testing to simulate the ionic environment of the body [1] [5]. |
| Iridium Oxide | A conductive coating applied to electrodes to enhance charge storage capacity and improve stability during electrical stimulation [8]. |
Experimental Protocol: Evaluating Liquid-Based Encapsulation
Objective: To assess the long-term barrier performance of an oil-infused elastomer encapsulation for a wireless bioelectronic device under accelerated aging conditions.
Workflow Overview: The diagram below outlines the key steps in this encapsulation and validation protocol.
Detailed Methodology:
Fabricate Roughened Elastomer:
- Prepare a 100 µm thick layer of PDMS (e.g., Sylgard-184) using a molding technique with abrasive paper as a template. This creates a surface with a high arithmetical mean height (Sa ~4.7 µm) to mechanically lock the infusion liquid [1].
Device Encapsulation:
- Place the bioelectronic device (e.g., a near-field communication antenna or wireless optoelectronic device) between two layers of the rough elastomer film, creating a sandwich structure with rough surfaces facing outward [1].
- Cure the assembly at ambient temperature overnight [1].
- Cut the encapsulated device to the desired shape using an ultraviolet (UV) laser. Optimize parameters (e.g., 30 kHz frequency, 100 mm/s speed) to create a rougher cut edge, which helps minimize the side-edge failure path [1].
- Infuse Krytox oil (a synthetic perfluoropolyether fluid) with a thickness of approximately 15 µm into the rough surface structures of the elastomer using a vacuum desiccator [1].
In Vitro Testing:
- Submerge the encapsulated devices in buffer solutions with pH values representing target biological environments (e.g., pH 1.5 for stomach acid, pH 7.4 for physiological conditions, pH 9.0 for alkaline wounds) [1].
- Maintain the soak tests at 37°C and periodically monitor key device functions. For a wireless optoelectronic device, this includes verifying robust wireless operation and maintaining high optical transparency. For NFC devices, monitor the quality factor or power transfer efficiency [1].
Failure Analysis:
- After testing, use scanning electron microscopy (SEM) to inspect for signs of delamination, corrosion, or cracking, particularly at the critical device edges and metal-polymer interfaces [5].
- Perform electrochemical impedance spectroscopy on electrodes to quantify any degradation caused by exposure [8].
Failure Mechanism Diagram: Corrosion-Triggered Delamination
The following diagram illustrates the key process of corrosion-triggered delamination, a major failure mode at the metal-polymer interface.
Frequently Asked Questions (FAQs)
Q1: Why does our PDMS-encapsulated bioelectronic sensor fail after prolonged exposure to biological fluids?
A: The failure is primarily due to nonspecific adsorption of proteins and absorption of small hydrophobic molecules from the biological fluid into the PDMS matrix [9]. PDMS is inherently hydrophobic, which causes proteins to adhere to its surface, potentially fouling sensors and affecting analyte transport [9]. Furthermore, its porous, absorbent polymer network can sequester small drug-like molecules, altering the local chemical environment and leading to inaccurate readings in drug development applications [9]. While oxygen plasma treatment can temporarily make the surface hydrophilic, PDMS typically undergoes fast hydrophobic recovery within minutes to hours, restoring its fouling characteristics [9].
Q2: Our epoxy-encapsulated implants show reduced performance in humid environments. What is the underlying mechanism?
A: Epoxy resins are susceptible to water absorption, which can lead to several issues [10]. Water molecules diffuse into the polymer matrix, causing:
- Plasticization: Water acts as a plasticizer, reducing the epoxy's stiffness and strength, which can compromise mechanical integrity [10] [11].
- Swelling: The absorbed water induces swelling stresses, potentially leading to microcracks or delamination from the substrate [10].
- Chemical Degradation: In severe cases, especially at elevated temperatures or in alkaline conditions, hydrolysis can occur, breaking the polymer chains and permanently degrading the epoxy [11] [10]. Studies have shown that immersion in alkaline solutions can cause a tensile strength retention of as low as 14% [11].
Q3: We use Parylene C for its excellent barrier properties. In what high-temperature situations might it be unsuitable?
A: While Parylene C offers outstanding barrier performance at room temperature, its properties can degrade at elevated temperatures. Although fluorinated versions like Parylene AF-4 maintain excellent barrier performance after exposure to 300°C, all parylene films have a defined thermal stability window [12]. Exposure to temperatures approaching or exceeding this window during processes like soldering or sterilization can lead to:
- Structural Changes: Increased crystallinity or oxidation, which can alter the mechanical properties of the coating [12].
- Barrier Degradation: A potential increase in the Water Vapor Transmission Rate (WVTR), reducing its effectiveness as a moisture barrier [12]. For the highest temperature applications, Parylene AF-4 is a more robust choice [12].
Q4: Why can't we use silicone (PDMS) for creating a waterproof seal against water vapor?
A: Silicone rubber is an excellent barrier to liquid water but has extremely high permeability to water vapor and many gases [13]. Its polymer matrix has a large "free volume," which allows vapor molecules like oxygen and water vapor to easily migrate through it. Its water vapor permeability can be five to six orders of magnitude higher than that of a material like Teflon, making it unsuitable for applications requiring an effective seal against atmospheric moisture [13].
Troubleshooting Guides
Problem: Rapid Biofouling of PDMS-Based Devices
Symptoms: Signal drift, reduced sensitivity, or clogging of microfluidic channels when used with biological samples.
Root Cause: The hydrophobic nature of PDMS causes rapid, nonspecific protein adsorption [9].
Solutions:
- Surface Hydrophilization: Treat the PDMS surface with oxygen plasma. Note: This is a temporary solution, as hydrophobic recovery occurs quickly [9].
- Permanent Surface Grafting: After plasma activation, graft hydrophilic polymers (e.g., polyethylene glycol) to the surface to create a non-fouling, brush-like layer [9].
- Rigid Coating Application: Apply a thin, rigid coating (e.g., a photo-sensitive thiolene resin) over PDMS structures. This has been shown to reduce deformation by 70% and may limit molecular absorption [9].
Problem: Epoxy Coating Failure in Cyclic Humidity/Temperature Environments
Symptoms: Coating blistering, loss of adhesion to the metal substrate, or hazy/cloudy appearance.
Root Cause: Water absorption leads to plasticization, swelling, and hydrolysis. Thermal cycling creates repeated expansion/contraction stress, causing fatigue failure [14] [10].
Solutions:
- Optimize Curing: Ensure the epoxy is fully cured according to manufacturer specifications, as a higher crosslink density can reduce water absorption [10].
- Environmental Control: Perform installation and curing in controlled conditions (ideally 60-80°F / 15-27°C and relative humidity below 85%) [14].
- Utilize Protective Topcoats: Apply a UV-resistant aliphatic topcoat if UV exposure is a concern, or a specialized sealant for chemical resistance [14].
- Material Selection: For environments with large temperature swings, select more flexible epoxy formulations designed to accommodate thermal movement [14].
Problem: Degradation of Parylene C Barrier in High-Temperature Sterilization
Symptoms: Increased moisture penetration and device failure after autoclaving or other high-temperature sterilization cycles.
Root Cause: Exposure to temperatures beyond the operational limit of Parylene C can degrade its crystalline structure and barrier properties [12].
Solutions:
- Material Upgrade: Switch to a parylene variant with higher thermal stability, such as Parylene AF-4, which demonstrates excellent barrier performance even after 300°C exposure [12].
- Process Validation: Characterize the specific sterilization process's temperature profile and ensure it remains within the safe zone for the chosen parylene type.
- Redundant Sealing: For critical applications, employ a "belt and suspenders" approach where the parylene-coated assembly is housed within a secondary gasketed enclosure [15].
The following tables summarize key performance limitations of the discussed materials, based on experimental data from the literature.
Table 1: Barrier Properties and Thermal Stability of Encapsulation Materials
| Material | Water Vapor Transmission Rate (WVTR) | Helium Transmission Rate (HTR) | Key Thermal Limitations |
|---|---|---|---|
| PDMS (Silicone) | Extremely High [13] | Very High [13] | Swells with organic solvents; properties change with temperature [9] [13] |
| Parylene C | 0.08 (g·mm)/(m²·day) [15] | Data not available in search | Performance degrades at high temperatures; inferior thermal stability vs. AF-4 [12] |
| Parylene AF-4 | 0.22 (g·mm)/(m²·day) at 25µm [15] | 12.18 × 10³ cm³ m⁻² day⁻¹ atm⁻¹ (after 300°C) [12] | Excellent thermal stability; maintains barrier after 300°C exposure [12] |
| Epoxy | ~0.94 (g·mm)/(m²·day) [15] | Data not available in search | Glass transition temperature (Tg) is a key limit; water absorption reduces Tg and mechanical properties [11] [10] |
Table 2: Resistance of Polymer Coatings to Saline Solution (0.9% NaCl)
| Polymer | Coating Method | Layer Thickness (µm) | Time Until Total Breakdown |
|---|---|---|---|
| Parylene C | CVD | 25 | > 30 days [15] |
| Epoxy (ER) | Dip Coating | 100 ± 25 | 6 hours [15] |
| Polyurethane (UR) | Dip Coating | 100 ± 12.5 | 6 hours [15] |
| Silicone (SR) | Dip Coating | 75 ± 12.5 | 58 hours [15] |
Experimental Protocols
Protocol 1: Gravimetric Analysis for Water Absorption in Epoxy
Purpose: To determine the kinetics of water uptake and the equilibrium water content in an epoxy coating sample [10].
Materials:
- Epoxy sample (e.g., 10mm x 10mm x 1mm)
- Analytical balance (±0.1 mg)
- Immersion container with distilled water
- Oven for drying
- Desiccator
Methodology:
- Drying: Dry the epoxy sample in an oven until constant mass (wd) is achieved. Cool in a desiccator [10].
- Immersion: Immerse the sample in distilled water at a constant temperature (e.g., 23°C, 40°C, 60°C) [10].
- Weighing: At regular time intervals, remove the sample, wipe off surface water with filter paper, and weigh immediately (wt) [10].
- Calculation: Calculate the water uptake Mt (%) at each time point using: ( Mt = \frac{wt - wd}{wd} \times 100 ) [10].
- Data Fitting: Plot Mt versus the square root of time. Use models (e.g., Fickian, Carter-Kibler) to analyze the diffusion behavior and determine the diffusion coefficient [10].
Protocol 2: Bubble Point Test for Membrane Integrity
Purpose: To perform a non-destructive test to verify the integrity and pore size of a membrane filter (e.g., Nylon) before and/or after use [16].
Materials:
- Membrane filter
- Bubble point test apparatus (capable of applying air pressure)
- Water to wet the membrane
Methodology:
- Wet the Membrane: Completely saturate the membrane with purified water. Ensure all pores are filled [16].
- Apply Pressure: Place the wetted membrane in the test apparatus and gradually increase the air pressure on the upstream side [16].
- Observe: Monitor the downstream side of the membrane for a continuous stream of air bubbles.
- Record Bubble Point: The pressure at which the first continuous stream of bubbles is observed is the "bubble point" [16].
- Interpretation: Compare the measured bubble point to the manufacturer's specification. A lower-than-expected bubble point indicates damaged or oversized pores, compromising the membrane's retention efficiency [16].
Research Reagent Solutions
Table 3: Essential Materials for Encapsulation and Filtration Research
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Parylene AF-4 Dimer | High-temperature, high-performance conformal coating via CVD [12] | Superior thermal stability and UV resistance; more expensive than Parylene C [12]. |
| Hydrophilic Nylon Membrane (0.45 µm) | Sterile filtration of aqueous and organic solvents in sample preparation [16] | Inherently hydrophilic, high protein binding (~120 µg/cm²), and chemically inert [16]. |
| Oxygen Plasma System | Surface activation of PDMS for temporary hydrophilization or permanent grafting [9] | Parameters (power, time) must be optimized. Hydrophobic recovery begins immediately after treatment [9]. |
| Two-Part Structural Epoxy Adhesive | Bonding and encapsulating components in a humid environment [11] | Susceptible to hygrothermal ageing; verify reduction in Tg and modulus after environmental exposure [11]. |
Experimental Workflow Visualization
Diagram 1: A generalized workflow for identifying and troubleshooting material limitations in encapsulation research.
FAQs on Soft Bioelectronic Encapsulation
1. Why is mechanical compliance so important for implantable bioelectronics?
The human body is composed of soft, dynamic, and continuously moving tissues. Implanted devices made from rigid materials create a mechanical mismatch, which can lead to inflammation, tissue damage, fibrosis (scar tissue formation), and eventual device failure. Soft and flexible encapsulation allows the device to conform and integrate seamlessly with its biological environment, minimizing these adverse responses and ensuring long-term functionality [17].
2. How can I quantitatively monitor water permeation through a flexible thin-film encapsulation in real-time?
A promising method involves using a wireless, battery-free flexible platform that leverages backscatter communication and magnesium (Mg)-based microsensors. Water permeation corrodes the Mg resistive sensor, which shifts the oscillation frequency of the sensing circuit. This frequency shift can be measured wirelessly to provide a real-time, quantitative measure of the Water Transmission Rate (WTR), both in vitro and in living tissue [18].
3. What are the options for encapsulating devices that need to operate in extreme pH environments, such as the stomach?
Conventional encapsulation materials like silicone elastomer or Parylene C often fail quickly in highly acidic or alkaline conditions. A recent development is a liquid-based encapsulation using an oil-infused elastomer. This approach has demonstrated robust protection for implantable wireless devices in environments ranging from pH 1.5 to pH 9, maintaining functionality for extended periods where other materials fail [1].
4. What are the key differences between reliability, stability, and durability in bioelectronic medicine?
These are distinct but interconnected concepts:
- Reliability is the probability a device functions as intended without failure over a specified time.
- Stability is the ability to maintain functional and structural properties over time, resisting degradation from environmental or biological fluctuations.
- Durability refers to physical resilience and the ability to withstand external stresses like mechanical deformation without compromising function [17].
Troubleshooting Guides
Issue 1: Unstable Device Performance Due to Water Ingress
Problem: Gradual degradation or failure of a soft implantable device, suspected to be caused by water vapor and ion permeation through the encapsulation.
Diagnosis and Solution:
| Step | Action | Expected Outcome & Quantitative Metrics |
|---|---|---|
| 1. In-situ Verification | Integrate a wireless Mg-based microsensor into your device encapsulation. Use an external reader to monitor the sensor's oscillation frequency. | A decreasing frequency provides real-time, in-situ confirmation of water permeation and corrosion of the Mg sensor [18]. |
| 2. WTR Quantification | Apply an analytical model to convert the measured frequency shift into a Water Transmission Rate (WTR). | Obtain a quantitative WTR value (e.g., in g/m²/day). Effective encapsulation for bioelectronics requires very low WTR (≤ 10⁻⁴ g/m²/day) [18]. |
| 3. Material Selection | If WTR is too high, consider alternative encapsulation strategies. For extreme pH environments, evaluate an oil-infused elastomer system. | Soaking tests show oil-infused elastomers maintain device performance for nearly 2 years in pH 1.5 and 4.5 solutions, unlike conventional materials which fail within days [1]. |
Experimental Protocol: Fabricating and Testing Mg-based Water Permeation Sensors
- Substrate Preparation: Begin with a flexible 5-µm thick polyimide (PI) substrate.
- Metal Deposition: Deposit a ~20 nm Titanium (Ti) adhesion layer, followed by a ~200 nm thick Mg film via thermal evaporation or DC sputtering.
- Patterning: Use UV photolithography followed by wet or dry etching to pattern the Mg layer into the desired sensor designs (e.g., stripes or serpentines).
- Encapsulation: Apply the thin-film encapsulation (TFE) you wish to test over the sensor.
- In-vitro Testing: Immerse the sensor in phosphate-buffered saline (PBS) at 37°C while monitoring the frequency via a wireless reader. The corrosion of Mg to Mg(OH)₂ will cause a measurable frequency drop [18].
Issue 2: Encapsulation Failure in Extreme pH Environments
Problem: Implantable bioelectronics, such as those for gastrointestinal monitoring, fail rapidly due to corrosion in highly acidic or alkaline conditions.
Diagnosis and Solution:
| Step | Action | Expected Outcome & Quantitative Metrics |
|---|---|---|
| 1. Material Assessment | Test current encapsulation (e.g., silicone elastomer, Parylene C) in the target pH buffer. Monitor device performance (e.g., wireless signal strength). | Conventional materials like silicone may fail completely within 1.5-19 days in pH 1.5 solution [1]. |
| 2. Switch to Liquid Encapsulation | Implement an oil-infused elastomer encapsulation. Sandwich the device between two layers of roughened PDMS (~100 µm), infuse with a 15 µm layer of Krytox oil, and seal the edges with optimized laser cutting. | The encapsulation should maintain high optical transparency (~87% transmittance) and device functionality for up to 2 years in acidic conditions [1]. |
| 3. Biocompatibility & In-vivo Validation | Perform immunohistochemistry studies in an animal model (e.g., mice) to confirm biocompatibility and test the encapsulated device's operation in a freely moving animal. | The encapsulation should show no significant foreign body response and the device should maintain robust wireless operation for at least 3 months post-implantation [1]. |
Workflow for Liquid-based Encapsulation.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function in Research |
|---|---|
| Polyimide (PI) | A common flexible polymer substrate for fabricating thin-film devices and sensors, providing mechanical support and electrical insulation [18]. |
| Magnesium (Mg) Thin Films | Serves as the active material in water permeation sensors. Its corrosion in the presence of water produces a measurable change in electrical resistance or wireless circuit frequency [18]. |
| Parylene C | A common polymer used for conformal coating of bioelectronics. It offers good barrier properties and biocompatibility in neutral pH environments, but can fail in extreme pH [1]. |
| Silicone Elastomer (e.g., PDMS) | A widely used soft and stretchable encapsulation material. It is often the base material for more advanced systems, such as oil-infused elastomers [1]. |
| Krytox Oil (PFPE) | A perfluoropolyether fluid with an ultralow water diffusion coefficient. It is infused into roughened elastomer surfaces to create a slippery, liquid-based barrier against water and ion penetration, even in extreme pH [1]. |
| Epoxy Resin | A rigid encapsulation material often used for implants in harsh environments like the gastrointestinal tract. Its high modulus and thick geometry limit its use in soft bioelectronics [1]. |
Wireless Water Permeation Sensing Principle.
Innovative Encapsulation Solutions: From Liquid Barriers to Conformal Coatings
This technical support center provides essential guidance for researchers working on advanced encapsulation strategies for implantable bioelectronics. The content focuses on liquid-based encapsulation, specifically oil-infused elastomers, which represent a breakthrough in protecting sensitive electronic components from water and ion permeation across challenging pH environments. These materials combine superior barrier performance with the mechanical compliance required for integration with soft, dynamic biological tissues.
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Why is my current encapsulation failing in acidic or alkaline biological environments?
- Answer: Conventional encapsulation materials like silicone elastomer or Parylene C are often designed for near-neutral pH conditions (pH ~7.4) and lack the chemical stability for extended periods in extreme pH. The oil-infused elastomer encapsulation uses a synthetic perfluoropolyether (PFPE) fluid, which provides exceptional stability and barrier performance across a broad pH range (1.5 to 9.0), making it suitable for the gastrointestinal tract (acidic) and chronic wounds (alkaline) [1].
FAQ 2: My encapsulated device has failed at the cut edges. How can I improve edge sealing?
- Answer: The side edges created during cutting are potential failure points as they lack the rough microstructure to retain the oil. To mitigate this:
- Optimize Laser Cutting: Use a UV laser with specific parameters to create a rougher edge surface that better retains the oil. Parameters of 30 kHz frequency and 100 mm/s speed have been shown to be effective without causing excessive burning [1].
- Sandwich Structure: Ensure the bioelectronic device is fully encapsulated between two rough elastomer layers with the infused oil, creating a sealed environment [1].
- Answer: The side edges created during cutting are potential failure points as they lack the rough microstructure to retain the oil. To mitigate this:
FAQ 3: How can I verify the barrier performance of my encapsulation in real-time?
- Answer: You can integrate a wireless, battery-free sensing platform that uses magnesium (Mg) microsensors. As water permeates the encapsulation, the Mg corrodes, changing its electrical resistance. This resistance shift can be wirelessly monitored via a backscatter communication system, providing real-time, quantitative data on water permeation [19].
FAQ 4: I need a transparent encapsulation for my optoelectronic device. Will this method work?
- Answer: Yes. A key advantage of the oil-infused elastomer is its high optical transparency. The combination of a polydimethylsiloxane (PDMS) elastomer and the infused oil maintains an average optical transmittance of 86.67% across the visible wavelength range (380–700 nm), making it highly suitable for optoelectronic implants like wireless stimulators or sensors [1].
FAQ 5: Is the oil-infused elastomer biocompatible for long-term implantation?
- Answer: Yes. In vivo immunohistochemistry studies have demonstrated the biocompatibility of the oil-coated elastomer material. Furthermore, encapsulated wireless optoelectronic devices have maintained robust operation over 3 months of implantation in freely moving mice, confirming both biocompatibility and functional stability [1] [20].
Experimental Protocols & Performance Data
Protocol: Fabrication of Oil-Infused Elastomer Encapsulation
The following workflow details the preparation of a device encapsulated with an oil-infused elastomer.
Quantitative Performance Data
The table below summarizes the key performance metrics of oil-infused elastomer encapsulation compared to other common materials.
Table 1: Performance Comparison of Encapsulation Materials
| Material | Avg. Optical Transmittance (Visible Light) | Failure Strain | Young's Modulus | Longevity in Acidic pH (pH 1.5) |
|---|---|---|---|---|
| Oil-Infused Elastomer | 86.67% [1] | ~100% [1] | ~MPa range [1] | >550 days (NFC antenna) [1] [20] |
| PDMS Elastomer | 95.33% [1] | ~100% [1] | ~MPa range [1] | Failed or lost >20% performance in 1.5-19 days [1] |
| Parylene C | 87.43% [1] | <5% [1] | ~GPa range [1] | Failed or lost >20% performance in 1.5-19 days [1] |
| Liquid Metal | 0.01% [1] | N/A | N/A | Susceptible to corrosion in low pH [1] |
Protocol: Real-Time Monitoring of Water Permeation
For quantitative assessment of encapsulation barrier performance, follow this protocol using magnesium-based sensors.
Principle: Water permeation corrodes a magnesium (Mg) resistive sensor, increasing its resistance. This resistance is part of a circuit that shifts the oscillation frequency of a wireless backscatter tag, allowing for remote monitoring [19].
Steps:
- Fabricate Mg Sensor: Deposit a ~200 nm thick Mg film with a 20 nm Titanium (Ti) adhesion layer onto a flexible polyimide substrate. Pattern the film into a specific geometry (e.g., serpentine) using photolithography and etching [19].
- Integrate with Circuit: Connect the Mg sensor as the resistance (
R_set) in a square-wave oscillator circuit that controls an RF switch connected to a flexible dipole antenna. - Wireless Interrogation: Expose the encapsulated sensor to an aqueous environment (e.g., PBS buffer). Use an external interrogator (reader) to power the tag via radio waves and monitor the frequency of the backscattered signal.
- Data Analysis: Track the decreasing oscillation frequency (
f_osc) over time. Use a pre-calibrated model to correlate the frequency shift with the sensor's resistance change and calculate the Water Transmission Rate (WTR) [19].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials for Oil-Infused Elastomer Encapsulation Research
| Material / Reagent | Function / Role | Specific Example / Properties |
|---|---|---|
| PDMS (Polydimethylsiloxane) | Base elastomer that provides the mechanical scaffold and stretchability. | A soft polymer (Young's modulus in the MPa range) that can be textured to create a rough, micro-structured surface [1]. |
| Krytox Oil | The infused liquid that provides the primary barrier to water and ion penetration. | A synthetic perfluoropolyether (PFPE) fluid characterized by an ultralow water diffusion coefficient [1]. |
| Mg (Magnesium) Thin Film | A sensing element for real-time, wireless monitoring of water permeation through the encapsulation. | ~200 nm thick film; corrodes predictably in the presence of water to Mg(OH)₂, changing its electrical resistance [19]. |
| NFC Antenna | A standard component of implantable bioelectronics for wireless power transfer and data communication, used for testing encapsulation performance. | Used to demonstrate long-term operational stability of the encapsulation under accelerated aging conditions [1]. |
| Titanium (Ti) Adhesion Layer | A thin film layer used to improve the adhesion of Mg to polymer substrates during microfabrication. | Typically ~20 nm thick, deposited via sputtering or thermal evaporation before Mg deposition [19]. |
Frequently Asked Questions (FAQs)
Q1: What makes PFPE-based encapsulation a superior choice for implantable bioelectronics, especially in challenging biological environments?
PFPE fluids exhibit exceptional barrier properties against water and ion permeation, which is critical for the long-term stability of implantable bioelectronics. Their molecular structure provides remarkable chemical inertness, resisting attack even in highly acidic (e.g., pH 1.5, simulating stomach acid) or alkaline (e.g., pH 9.0, simulating chronic wound environments) conditions [21]. Furthermore, when infused into roughened elastomers, they form a slippery, stable layer that significantly reduces water and ion penetration. This liquid-based encapsulation approach has demonstrated functionality in vivo for up to 3 months in freely moving mice and year-long stability in accelerated in vitro soaking tests, outperforming conventional materials like silicone elastomer or Parylene C, which can fail within days under similar acidic conditions [21].
Q2: My current encapsulation (e.g., Parylene C) fails rapidly in extreme pH environments. What key material properties should I prioritize for such applications?
For extreme pH environments, you should prioritize the following material characteristics:
- Chemical Inertness: The encapsulation material must resist hydrolysis and chemical attack from both high concentrations of H⁺ (acidic) and OH⁻ (alkaline) ions. PFPE fluids are renowned for their exceptional chemical stability across a wide pH spectrum [21].
- Ultralow Water Permeability: The primary failure mechanism is often water vapor transmission. Materials with ultralow water diffusion coefficients are essential. PFPE oils, such as Krytox, possess this property [21].
- Mechanical Compliance: The encapsulation must be flexible and stretchable to withstand the dynamic movements of organs and tissues without cracking. A Young's modulus in the MPa range (matching soft biological tissues) is ideal, as opposed to the GPa range of rigid epoxies [21].
- Optical Transparency: For bioelectronics that incorporate optical sensing or stimulation (e.g., optoelectronics), high optical transmittance in the visible wavelength range is necessary. Oil-infused elastomers can maintain an average transmittance of over 85% [21].
Q3: How does the surface roughness of an elastomer contribute to the effectiveness of a liquid-based encapsulation system?
Surface roughness is not a flaw but a design feature in this context. A micro-roughened elastomer surface (with an arithmetical mean height, Sa, of ~4.7 µm) acts as a microscopic network of reservoirs that physically lock the PFPE oil in place via capillary forces and surface interactions [21]. This prevents the lubricating fluid from being squeezed out or de-wetting under mechanical stress, ensuring a continuous and stable barrier layer. Without this roughened structure, the liquid layer would be unstable and prone to failure.
Q4: Are there any biocompatibility concerns with using PFPE fluids and roughened elastomers in chronic implants?
In vivo studies have demonstrated the biocompatibility of the oil-infused elastomer material. Immunohistochemistry studies in mice implanted with devices encapsulated using this strategy showed robust operation over 3 months without significant adverse immune responses, confirming the material's suitability for chronic implantation [21]. As with any implantable material, rigorous sterilization and evaluation according to relevant ISO standards are recommended before clinical translation.
Troubleshooting Common Experimental Challenges
Problem: Inconsistent Encapsulation Performance and Premature Failure at the Edges
- Symptoms: Device failure occurs much earlier than expected, often starting from the cut edges of the encapsulated device. Electrical measurements show a rapid increase in leakage current.
- Root Cause: The side edges, created during the cutting process, lack the micro-roughened structure present on the top and bottom surfaces. This smooth edge offers a pathway for water and ions to wick into the device sandwich structure [21].
- Solution:
- Optimize Laser-Cutting Parameters: The laser-cutting process should be tuned to create a rougher edge surface that can better retain the PFPE fluid.
- Validated Parameter Set: Use a UV laser with a frequency of 30 kHz and a speed of 100 mm/s. Avoid lower frequencies (e.g., 25 kHz) which can cause excessive burning and uneven surfaces [21].
- Post-Cutting Inspection: Use scanning electron microscopy (SEM) to verify the morphology of the cut edges and ensure consistency.
Problem: Delamination of Encapsulation Layers Under Cyclic Mechanical Strain
- Symptoms: The bonded layers of the encapsulation begin to separate after repeated stretching or bending, compromising the barrier.
- Root Cause: Inadequate bonding strength between the elastomer layers that form the "sandwich" around the bioelectronic device.
- Solution:
- Surface Activation: Prior to bonding, treat the smooth inner surfaces of the PDMS elastomer films with oxygen plasma. This creates reactive silanol groups on the surface.
- Bonding Protocol: After plasma treatment, bring the activated surfaces into immediate conformal contact. Cure the assembled structure at ambient temperature overnight to form strong, permanent Si-O-Si bonds [21].
- Mechanical Testing: Perform peel tests on sample sandwiches to validate bond strength before proceeding with functional devices.
Problem: Cloudy Encapsulation Leading to Poor Optical Transmission for Optoelectronic Implants
- Symptoms: The final encapsulated device has reduced optical clarity, hindering the performance of optical components.
- Root Cause: Incomplete infusion of the PFPE oil into the elastomer's rough microstructure, leaving air pockets that scatter light. Alternatively, the oil layer may be too thick.
- Solution:
- Ensure Full Vacuum Infusion: Perform the oil infusion process in a vacuum desiccator. Hold the vacuum for a sufficient duration (e.g., 30-60 minutes) to ensure all air is evacuated from the rough surface and replaced with the PFPE fluid [21].
- Control Oil Thickness: After infusion, wipe the surface with a lint-free cloth to remove excess oil and achieve a thin, uniform layer. The study successfully used an oil thickness of 15 µm [21].
- Material Compatibility: Verify that all materials (elastomer, oil) are optically transparent. PFPE oils and PDMS typically have high inherent transparency.
Experimental Protocol: Fabricating a Liquid-Encapsulated Bioelectronic Device
This protocol details the method for creating an oil-infused elastomer encapsulation for a wireless implantable device, based on the approach validated in the research [21].
The following diagram illustrates the complete fabrication workflow.
Step-by-Step Methodology
Step 1: Preparation of Roughened Elastomer Substrate
- Materials: Polydimethylsiloxane (PDMS) base and cross-linker, abrasive paper (as a molding template).
- Procedure:
- Mix the PDMS precursor at a standard 10:1 base-to-cross-linker ratio.
- Pour the mixture onto the abrasive paper template and spin-coat or doctor-blade to achieve a uniform thickness of 100 µm.
- Cure the PDMS at the manufacturer's recommended temperature (e.g., 70°C for 1-2 hours).
- Peel the cured, roughened PDMS film from the template. Characterize the surface roughness; the target arithmetical mean height (Sa) is approximately 4.7 µm [21].
Step 2: Device Sandwiching and Bonding
- Procedure:
- Place the bioelectronic device (e.g., a near-field communication antenna or wireless optoelectronic device) onto the smooth side of one roughened PDMS film.
- Carefully place a second roughened PDMS film on top, with its smooth side facing the device, creating a sandwich structure.
- Critical Step: Activate the outer smooth surfaces of this sandwich with oxygen plasma to make them hydrophilic and reactive.
- Immediately bring the activated surfaces into conformal contact and apply slight pressure. Cure the assembly at ambient temperature overnight to form an irreversible bond [21].
Step 3: Laser Cutting and Shape Definition
- Equipment: Ultraviolet (UV) laser cutter.
- Procedure:
- Use a UV laser to cut the encapsulated device to its final shape.
- Validated Parameters: Set the laser frequency to 30 kHz and the cutting speed to 100 mm/s. This combination produces a sufficiently rough cut edge without causing excessive burning, which is crucial for edge-sealing [21].
Step 4: PFPE Oil Infusion
- Materials: Krytox GPL series PFPE oil (or equivalent).
- Procedure:
- Place the laser-cut device in a vacuum desiccator.
- Completely cover the device with the PFPE oil.
- Apply a vacuum for 30-60 minutes to evacuate air from the micro-roughness on the elastomer surface.
- Release the vacuum, allowing the oil to be infused into the porous rough structure. The target oil layer thickness is 15 µm [21].
- Wipe away any excess oil from the surface with a lint-free cloth.
Performance Validation and Testing Protocol
After fabrication, validate the encapsulation performance as outlined below.
1. In Vitro Soaking Test:
- Objective: To assess long-term barrier performance under accelerated conditions.
- Method: Immerse the encapsulated device in buffer solutions of varying pH (e.g., pH 1.5, 4.5, 7.4, and 9.0) and maintain at 37°C.
- Measurement: Periodically measure the device's performance, such as the quality factor (Q-factor) of a resonant antenna or wireless link efficiency. A performance drop of more than 20% is typically considered a failure point. The target is to maintain performance for over 1.5 years in acidic conditions and 1 year at physiological pH [21].
2. In Vivo Biocompatibility and Functionality Test:
- Objective: To evaluate biocompatibility and operational stability in a living organism.
- Method: Implant the device subcutaneously in an animal model (e.g., freely moving mice).
- Measurement:
- Biocompatibility: After 3 months, perform immunohistochemistry on the surrounding tissue to assess the immune response (e.g., presence of macrophages, fibrosis).
- Functionality: Continuously or periodically monitor the device's wireless operation throughout the implantation period [21].
Quantitative Data and Material Properties
| Material | Average Optical Transmittance (Visible Spectrum) | Failure Strain | Young's Modulus | Key Characteristics & Performance in Acidic pH |
|---|---|---|---|---|
| Oil-Infused Elastomer | 86.67% | ~100% | A few MPa | Maintains performance for nearly 2 years in pH 1.5 |
| PDMS Elastomer | 95.33% | ~100% | A few MPa | Fails rapidly in extreme pH without oil barrier |
| Parylene C | 87.43% | <5% | A few GPa | Loses >20% performance within 1.5-19 days in pH 1.5 |
| Polyimide (PI) | 7.70% - 71.22% | <5% | A few GPa | Low transparency; stiff and non-stretchable |
| Liquid Metal | ~0.01% | N/A | N/A | Electrically conductive; not transparent |
| Product / Type | Kinematic Viscosity at 20°C (cSt) | Vapor Pressure (torr) @20°C | Continuous Service Temp. Range (°C) | Typical Applications |
|---|---|---|---|---|
| Krytox PFPE Oils (Base for infusion) | Varies by grade (e.g., 150 - 1500) | Ultralow (e.g., ~10⁻¹¹) | -65 to +200+ | Base fluid for vacuum pumps, lubricants, and encapsulation [21] |
| OT 20 Grease | 35 | N/A | -50 to +70 | General purpose, low temperature |
| RT 15 Grease | 1300 | N/A | -20 to +250 | High temperature, low volatility |
| ZLHT Grease | 150 | N/A | -65 to +200 | Wide temperature range |
| AR 555 Grease | 1500 | 3.9 x 10⁻¹¹ | -20 to +250 | Low vapor pressure for high vacuum |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PFPE-Based Encapsulation Research
| Item | Function / Role in Experiment | Specification / Notes |
|---|---|---|
| PDMS | Base elastomer for creating the micro-roughened encapsulation substrate. | Use a standard two-part kit (e.g., Sylgard 184). Aim for a final thickness of 100 µm [21]. |
| Abrasive Paper | Template for molding the microscale rough surface onto the PDMS. | Varying grit sizes can be tested to achieve the target roughness (Sa ~4.7 µm) [21]. |
| Krytox PFPE Oil | The active barrier fluid infused into the rough PDMS surface. | A synthetic perfluoropolyether fluid with an ultralow water diffusion coefficient [21]. |
| Oxygen Plasma System | Activates PDMS surfaces for irreversible bonding of the sandwich structure. | Critical for creating strong bonds without adhesives that could compromise the barrier [21]. |
| UV Laser Cutter | Defines the final shape of the encapsulated device and creates sealed edges. | Must be capable of fine-tuning parameters (30 kHz, 100 mm/s) to create rough, non-burned edges [21]. |
| Vacuum Desiccator | Chamber for degassing and infusing the PFPE oil into the elastomer. | Ensures complete infiltration of oil into the micro-roughness, eliminating air pockets [21]. |
This technical support guide details the fabrication process for developing advanced liquid-encapsulated bioelectronic implants. This method is central to ongoing thesis research on preventing water and ion permeation, a critical challenge for the long-term reliability of implantable devices in the harsh ionic environment of the body [1]. The following sections provide a comprehensive, step-by-step protocol, accompanied by troubleshooting guides and FAQs, to assist researchers in replicating and optimizing this fabrication process.
Experimental Protocol: Core Fabrication Workflow
The following diagram outlines the complete fabrication workflow, from substrate preparation to the final oil infusion step.
Step 1: Molding the Roughened Elastomer Substrate
- Objective: Create a flexible elastomer film with a micro-rough surface to serve as a scaffold for locking the hydrophobic oil in place.
- Detailed Methodology:
- Template Preparation: Use abrasive paper as a template for the molding process. The grit size will determine the surface roughness, which is critical for oil retention [1].
- PDMS Preparation: Mix the PDMS base and curing agent according to the manufacturer's instructions. Degas the mixture in a vacuum desiccator to remove air bubbles.
- Molding and Curing: Pour the PDMS mixture onto the abrasive paper template. Cure at ambient temperature or in an oven according to the polymer's specifications, typically at 70°C for 1-2 hours.
- Demolding: Carefully peel the cured PDMS film from the template. The resulting film should have a thickness of approximately 100 µm and a micro-rough surface with an arithmetical mean height (Sa) of around 4.7 µm [1].
Step 2: Sandwiching the Bioelectronic Device
- Objective: Fully enclose the implantable bioelectronics within a protective elastomer shell.
- Detailed Methodology:
- Device Preparation: Ensure the bioelectronic device (e.g., NFC antenna, wireless optoelectronic device) is clean and functional.
- Assembly: Place the device between two layers of the rough PDMS film, ensuring the rough surfaces are facing outward.
- Bonding: Cure the PDMS "sandwich" at ambient temperature overnight to achieve a strong bond between the layers and fully encapsulate the device [1].
Step 3: Laser Cutting the Encapsulated Device
- Objective: Define the final shape of the implant without compromising the edge seal.
- Detailed Methodology:
- Laser Parameter Optimization: This is a critical step. Use an ultraviolet (UV) laser and optimize parameters to create rough cut edges, which help retain oil and prevent failure pathways [1].
- Recommended Parameters: A frequency of 30 kHz and a speed of 100 mm/s have been shown to create sufficiently rough edges without causing excessive burning [1].
- Cutting Process: Program the laser cutter to trace the desired outline of the device. The laser cutting not only shapes the device but also seals the edges of the PDMS sandwich.
- Laser Parameter Optimization: This is a critical step. Use an ultraviolet (UV) laser and optimize parameters to create rough cut edges, which help retain oil and prevent failure pathways [1].
Step 4: Infusing the Hydrophobic Oil
- Objective: Introduce a permanent liquid barrier that provides ultralow permeability to water and ions.
- Detailed Methodology:
- Oil Selection: Use a synthetic perfluoropolyether (PFPE) fluid such as Krytox oil, which is known for its high stability and ultralow water diffusion coefficient [1] [3].
- Infusion Process: Place the laser-cut device into a vacuum desiccator. Introduce the oil to ensure it fully wets the rough surfaces of the elastomer. The vacuum helps draw the oil into the micro-structured pores of the PDMS.
- Final Preparation: After infusion, a uniform oil layer with a thickness of about 15 µm should be present on the surface [1]. The device is now ready for testing and characterization.
Troubleshooting Guide: Fabrication Challenges and Solutions
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Incomplete or uneven laser cutting [22] | Incorrect laser focus, insufficient power, excessive speed, dirty or misaligned optics. | Verify focal height is correct for material thickness. Clean the focusing lens and mirrors. Perform a ramp test to calibrate focus. Reduce cutting speed or increase laser power in 5% increments [22]. |
| Poor oil retention on elastomer surface | Inadequate surface roughness from molding step, incorrect oil viscosity, contamination on PDMS surface. | Verify the roughness parameters (Sa ~4.7 µm) of the molded PDMS using profilometry. Ensure the PDMS surface is clean and free of dust. Confirm compatibility between the Krytox oil and the elastomer [1]. |
| Device failure during in-vitro testing (early de-lamination) | Weak bonding between PDMS layers during sandwiching, incomplete curing of PDMS, smooth cut edges providing a path for water ingress. | Ensure PDMS layers are fully cured before bonding. Apply even pressure during the sandwiching process. Re-optimize laser parameters to create rougher cut edges that better retain the oil barrier [1]. |
| Optical transparency too low for application | Oil layer too thick, contamination in oil or between layers, use of non-transparent encapsulation materials. | Ensure the PDMS and oil layers are applied uniformly and are free of debris. Note that oil-infused elastomers can achieve an average optical transmittance of 86.67% in the visible spectrum [1]. |
| Laser cut edges are charred or uneven [22] | Laser power is too high, cutting speed is too slow, incorrect frequency setting. | Reduce laser power and/or increase cutting speed. Avoid using a frequency that is too low (e.g., 25 kHz) as it can cause excessive burning. Fine-tune parameters on scrap material first [1] [22]. |
Frequently Asked Questions (FAQs)
Q1: Why is creating a rough edge during laser cutting critical for the long-term performance of the encapsulation?
A1: The side edges created by laser cutting are potential failure points for water permeation, as they lack the micro-rough structure of the top and bottom surfaces. Optimized laser parameters (e.g., 30 kHz, 100 mm/s) create a rougher edge morphology that helps lock in the hydrophobic oil, extending the device's functional lifetime in aqueous environments by blocking this permeation pathway [1].
Q2: How does this liquid-based encapsulation compare to traditional thin-film methods like Parylene C in terms of mechanical properties?
A2: Liquid-based encapsulation offers superior mechanical compliance for interfacing with soft tissues. The oil-infused elastomer has a Young's modulus on the order of a few MPa and can withstand failure strains of up to ~100%. In contrast, Parylene C is much stiffer, with a modulus in the GPa range and a failure strain of <5%, making it less ideal for applications with dynamic movement [1].
Q3: My laser is powered on and moves, but isn't cutting through the material. What should I check first?
A3: This is a common issue. Follow this diagnostic sequence [22] [23]:
- Focus: Confirm the laser beam is correctly focused on the material surface. An out-of-focus beam drastically reduces power density.
- Optics: Inspect and clean the focusing lens and mirrors. Even slight contamination can significantly weaken the output.
- Parameters: Double-check that your software settings for power, speed, and number of passes are appropriate for the material thickness.
- Air Assist: Ensure the air assist is functioning with sufficient pressure (e.g., 10-15 PSI) to clear molten debris and prevent scorching.
Q4: What is the evidence for the biocompatibility and long-term stability of this encapsulation strategy?
A4: Research has demonstrated both in-vitro and in-vivo performance. Immunohistochemistry studies in mice have shown the biocompatibility of the oil-coated elastomer. Furthermore, encapsulated wireless optoelectronic devices have maintained robust operation throughout 3 months of implantation in freely moving animals. In-vitro soaking tests in acidic solutions (pH 1.5) have shown durability for nearly 2 years [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
| Item | Function in the Protocol | Technical Notes |
|---|---|---|
| PDMS (Polydimethylsiloxane) | A flexible, biocompatible silicone elastomer that forms the primary encapsulation structure. | Provides a transparent, stretchable base. The micro-rough surface is key for oil retention [1]. |
| Krytox Oil (PFPE) | A hydrophobic perfluoropolyether fluid that creates the liquid barrier against water and ion permeation. | Selected for its ultralow water diffusion coefficient and chemical stability across a wide pH range [1] [3]. |
| Abrasive Paper | Serves as a molding template to create the micro-rough surface on the PDMS film. | The grit size determines the surface roughness parameters (Sa, Sp), which are critical for oil locking [1]. |
| UV Laser Cutter | Precisely shapes the final device and creates critical rough-edge morphology. | Parameters must be optimized (e.g., 30 kHz, 100 mm/s) to avoid smooth or charred edges [1]. |
| Vacuum Desiccator | Facilitates the infusion of oil into the porous, rough PDMS structure by removing air. | Ensures complete and uniform oil coverage without trapped air bubbles [1]. |
FAQs on Material Performance and Encapsulation
Q: Why is optical transparency important for implantable bioelectronic devices? Optical transparency is crucial for optoelectronic implants, such as those used for optogenetics or light-based therapy and sensing. It allows light to pass through the encapsulation film to interact with both the underlying device components and the biological tissues, enabling device functionality [1].
Q: What are the key mechanical properties an encapsulation layer should possess for use in implantable devices? The encapsulation should be stretchable and mechanically compliant to match the physical properties of surrounding tissues. This ensures the film remains intact during natural movements of body organs, providing long-term reliable protection without compromising structural integrity. A Young's modulus in the range of a few MPa is desirable to conformably integrate with soft tissues [1].
Q: My encapsulated device failed in an acidic environment. What could be the reason? Conventional encapsulation materials like silicone elastomer or Parylene C often lack resistance to extreme pH. They can fail completely or lose significant performance (e.g., >20% performance loss within 1.5-19 days) in highly acidic or alkaline conditions. A liquid-based encapsulation approach has been shown to provide superior barrier performance across a broad pH range (1.5 to 9) [1].
Q: How can I simultaneously achieve high optical transparency, stretchability, and a water barrier in an encapsulation material? Recent research demonstrates that a liquid-based encapsulation strategy using an oil-infused elastomer can meet these combined needs. One study reported an average optical transmittance of 86.67% in the visible wavelength, elastic deformation up to ~100% strain, and outstanding water resistance, maintaining device performance for nearly two years in vitro in acidic environments [1].
Troubleshooting Guides
Problem 1: Device Failure Due to Water and Ion Permeation
| Observation | Investigation Question | Possible Root Cause | Recommended Action |
|---|---|---|---|
| Current leakage, performance degradation, or corrosion in implantable device [1] | Is the encapsulation material an effective barrier against water and ions? | Failure of conventional materials (e.g., PDMS, Parylene C) in challenging pH environments or under mechanical stress [1]. | Implement a liquid-based encapsulation. Adopt an oil-infused elastomer where a perfluoropolyether (PFPE) oil is infused into a roughened PDMS matrix, creating an ultralow water permeability barrier [1] [2]. |
| Device failure in highly acidic (e.g., stomach) or alkaline (e.g., chronic wounds) environments [1] | Was the encapsulation tested and validated for the specific pH of the target biological environment? | Material degradation or accelerated ion penetration (H⁺ or OH⁻) under extreme pH, for which many flexible encapsulations are not designed [1]. | Ensure encapsulation performance is verified across the entire relevant pH range (e.g., from pH 1.5 to 9). Select materials proven stable in these conditions [1]. |
Problem 2: Loss of Optical Transparency or Mechanical Durability
| Observation | Investigation Question | Possible Root Cause | Recommended Action |
|---|---|---|---|
| Diminished light transmission through the encapsulation layer [1] | Does the encapsulation material possess high intrinsic optical transparency? | Use of opaque or low-transparency materials (e.g., liquid metal with ~0.01% transmittance) for applications requiring optical signaling [1]. | Select materials with high optical transparency in the visible spectrum (380–700 nm). Oil-infused elastomers and Parylene C can offer over 85% average transmittance [1]. |
| Cracking or loss of encapsulation integrity during organ movement [1] | Does the mechanical modulus of the encapsulation match that of the surrounding tissue? | Use of materials with high Young's modulus (e.g., Parylene C or Polyimide in the GPa range) and low failure strain (<5%), making them too rigid for mobile organs [1]. | Use elastomeric materials (e.g., specific PDMS formulations) with a compliant Young's modulus (a few MPa) and high failure strain (approaching 100%) to ensure mechanical durability and stretchability [1]. |
Experimental Protocols
Protocol: Fabrication of Oil-Infused Elastomer Encapsulation
This methodology details the creation of a flexible, transparent, and durable encapsulation barrier for implantable bioelectronics [1].
1. Key Research Reagent Solutions
| Item | Function / Rationale |
|---|---|
| PDMS (Polydimethylsiloxane) | A transparent, biocompatible, and stretchable elastomer that forms the polymer matrix of the encapsulation [1]. |
| Abrasive Paper | Serves as a template to create micro-roughness on the PDMS surface, which is essential for locking the infusion oil in place [1]. |
| Krytox Oil (PFPE fluid) | A synthetic perfluoropolyether infusion fluid with an ultralow water diffusion coefficient, forming the core of the liquid barrier against water and ion penetration [1] [2]. |
| UV Laser Cutter | Used to precisely cut the encapsulated device to the desired shape while simultaneously creating controlled roughness on the side edges to minimize potential failure paths [1]. |
2. Step-by-Step Workflow
- Prepare Roughened Elastomer Film: Create a ~100 µm thick PDMS elastomer film using a molding technique with abrasive paper as a template. This process generates a surface with a defined arithmetical mean height (Sa ~4.7 µm) [1].
- Sandwich the Device: Place the implantable bioelectronic device between two layers of the rough elastomer film, ensuring the rough surfaces face outward [1].
- Cure the Assembly: Cure the PDMS-sandwiched device at ambient temperature overnight to bond the layers securely [1].
- Laser Cutting: Cut the encapsulated device to the desired shape using a UV laser. Optimize parameters (e.g., 30 kHz frequency, 100 mm/s speed) to create rougher edge surfaces that help retain the oil and enhance long-term performance [1].
- Oil Infusion: Infuse Krytox oil (to a thickness of ~15 µm) into the rough microstructures of the elastomer surfaces. This is typically done in a vacuum desiccator to ensure the oil penetrates and fills the pores effectively [1].
Protocol: Quantitative Characterization of Encapsulation Performance
1. Optical Transparency Measurement
- Objective: Quantify the light transmission through the encapsulation material.
- Method: Use a spectrophotometer to measure the optical transmission spectra across the visible wavelength range (380–700 nm). Report the average optical transmittance [1].
- Expected Results: As reported, PDMS elastomer (100 µm) can achieve ~95.33% transmittance, while the complete oil-infused elastomer system can maintain ~86.67% transmittance [1].
2. Mechanical Stretchability and Modulus Testing
- Objective: Determine the mechanical compliance and durability of the encapsulation.
- Method: Perform uniaxial tensile tests to obtain stress-strain curves. Measure the failure strain and calculate the Young's modulus from the linear elastic region [1].
- Expected Results: Elastomers like PDMS can show elastic deformation up to ~100% strain, with a Young's modulus in the MPa range, matching soft biological tissues [1].
3. Barrier Performance in pH Environments
- Objective: Validate the encapsulation's resistance to water and ions in biologically relevant pH conditions.
- Method: Soak encapsulated devices (e.g., wireless NFC antennas) in buffer solutions of varying pH (e.g., 1.5, 4.5, 7.4, 9.0) at physiological temperature. Monitor device performance metrics (e.g., quality factor, operational stability) over an extended period [1].
- Expected Results: Liquid-based encapsulation has demonstrated robust operation and high water resistance for periods up to several months or even years in vitro across the pH range of 1.5 to 9.0 [1].
Table 1: Comparative Optical and Mechanical Properties of Encapsulation Materials
| Material | Average Optical Transmittance (Visible Spectrum) | Failure Strain | Young's Modulus |
|---|---|---|---|
| Oil-Infused Elastomer [1] | 86.67% | ~100% | A few MPa |
| PDMS Elastomer [1] | 95.33% | ~100% | A few MPa |
| Parylene C [1] | 87.43% | < 5% | A few GPa |
| Polyimide (PI) [1] | 7.70% - 71.22% | < 5% | A few GPa |
| Liquid Metal [1] | ~0.01% | Not Specified | Not Specified |
Table 2: Barrier Performance of Encapsulation in Acidic Environment (pH = 1.5)
| Encapsulation Strategy | Performance Outcome in Acidic Environment |
|---|---|
| Oil-Infused Elastomer [1] | Maintained device performance for nearly 2 years in vitro. |
| Conventional Silicone Elastomer [1] | Complete failure or >20% performance loss within 1.5-19 days. |
Experimental Workflow and Diagnostics
Oil-Infused Encapsulation Fabrication
Troubleshooting Encapsulation Failure
Ensuring Reliability: Troubleshooting Common Failure Points and Optimizing Performance
FAQs on Edge Protection and Encapsulation
FAQ 1: Why are the edges of a laser-cut encapsulation considered a critical weak point?
The cutting process creates edges that lack the specific protective structures present on the primary surfaces. For example, in advanced liquid-based encapsulation, the top and bottom surfaces may be engineered with rough structures to lock protective oils in place, a feature absent from the cut edges. These edges can provide a potential path for water and ion ingress, leading to device failure [1].
FAQ 2: What laser parameters are critical for optimizing the edge quality of a polymer encapsulation layer?
The key parameters are laser power, cutting speed, and frequency (pulse repetition). Research indicates that using a lower cutting speed and frequency generally creates a rougher edge surface, which can be beneficial for subsequent sealing processes. However, parameters that are too aggressive (e.g., a frequency of 25 kHz in one study) can cause excessive burning and uneven edges, making the process harder to control. An optimized setting (e.g., 30 kHz and 100 mm/s) can produce a controllably rougher edge that improves the effectiveness of the final seal [1].
FAQ 3: How can I quantitatively monitor the success of my encapsulation strategy in real-time?
A novel method involves integrating wireless, battery-free magnesium (Mg) microsensors into the device. When water permeates the encapsulation, it corrodes the Mg sensor, changing its electrical resistance. This resistance shift is wirelessly transmitted as a frequency change in a backscatter signal, allowing for real-time, in-situ quantification of the Water Transmission Rate (WTR) across the thin-film encapsulation [19].
FAQ 4: Besides edge sealing, what other surface optimization techniques improve laser cutting for encapsulation fabrication?
Advanced techniques like waterjet-guided laser cutting can significantly enhance cut quality. This method uses a waterjet to guide the laser, which simultaneously cools the material, reduces the heat-affected zone (HAZ), and minimizes issues like kerf taper, dross adherence, and surface roughness compared to conventional laser cutting [24]. Furthermore, standard optimizations include adjusting the laser's focus position and using appropriate assist gases (e.g., nitrogen for oxide-free cuts) to achieve smoother, cleaner edges [25] [26].
Troubleshooting Guides
Table 1: Troubleshooting Laser-Cut Edge Quality
| Problem | Root Cause | Solution |
|---|---|---|
| Burned or Charred Edges | Excessive heat input from high laser power or slow cutting speed [26]. | Reduce laser power and/or increase the cutting speed [26]. |
| Rough or Jagged Edges | Misaligned laser beam, dirty optical components, or suboptimal laser parameters [26]. | Realign the laser beam and clean the nozzle/lens. Optimize laser frequency and speed for a smoother cut [1] [26]. |
| Oxidized Edges | Use of oxygen as an assist gas, which promotes oxidation of the cut surface [26]. | Switch to an inert assist gas like nitrogen to create clean, oxide-free edges [26]. |
| Slag Adherence (Dross) | Incorrect focal point positioning or insufficient power to fully eject molten material [27]. | Adjust the defocus distance (focal point position) and ensure adequate laser power for the material thickness [27]. |
| Excessive Edge Smoothness | Overly optimized laser cutting that produces a smooth edge with no micro-features for adhesion. | Adjust laser parameters (e.g., lower frequency and speed) to create a controllably rougher surface to improve interlayer adhesion for sealing [1]. |
Table 2: Troubleshooting Encapsulation Failure
| Problem | Root Cause | Solution |
|---|---|---|
| Rapid Device Failure in Acidic pH | Conventional encapsulation materials (e.g., silicone elastomer, Parylene C) are not stable in extreme pH environments [1]. | Employ a liquid-based encapsulation strategy using oil-infused elastomers designed for a broad pH range (1.5-9) [1]. |
| Water Permeation at Edges | The cut edges of the encapsulation lack a functional barrier, allowing water ingress [1]. | Implement a post-cutting edge sealing process, such as applying a compatible sealant or utilizing the edge roughness for enhanced adhesion of a secondary barrier layer [1]. |
| Mechanical Cracking of Encapsulation | Mechanical mismatch between the stiff encapsulation and soft, dynamic biological tissues [7] [28]. | Use soft, flexible nanocomposite matrices like elastomers or hydrogels with a Young's modulus matching the target tissue (kPa to MPa range) [28]. |
| Inability to Quantify Permeation | Lack of integrated sensors to measure water permeation in real-time after implantation [19]. | Integrate wireless, Mg-based microsensors into the device design for real-time monitoring of the encapsulation's barrier performance [19]. |
Experimental Protocols
Protocol 1: Laser Cutting and Edge Sealing of an Oil-Infused Elastomer
This protocol details a method for creating and sealing laser-cut edges of a flexible encapsulation, as derived from research on liquid-based encapsulation for bioelectronics [1].
Key Research Reagent Solutions:
| Item | Function in the Experiment |
|---|---|
| PDMS Elastomer | Forms the primary flexible and stretchable structural matrix of the encapsulation. |
| Abrasive Paper Mold | Used to create a roughened surface topography on the PDMS to lock the oil layer. |
| Krytox Oil (PFPE) | A perfluoropolyether fluid infused into the rough elastomer surface; provides an ultralow water diffusion barrier. |
| UV Laser Cutter | Used for precisely cutting the encapsulated device to the desired shape. |
Methodology:
- Elastomer Preparation: Fabricate a roughened PDMS elastomer layer (e.g., 100 µm thick) using a molding technique with abrasive paper as a template.
- Device Sandwich: Place the bioelectronic device between two layers of the rough elastomer film, with the rough surfaces facing outward. Cure the assembly at ambient temperature overnight.
- Laser Cutting: Cut the encapsulated device to the desired shape using a UV laser. Critical parameters to optimize include:
- Frequency: 30 kHz
- Speed: 100 mm/s
- Adjust parameters to create a controllably rough cut edge without causing excessive burning.
- Oil Infusion: Infuse Krytox oil (e.g., 15 µm thick) into the rough structures of the elastomer surfaces, including the newly cut edges, in a vacuum desiccator. The roughness of the cut edge aids in retaining the oil at this critical weak point.
Protocol 2: Real-Time Monitoring of Water Permeation Using Mg Sensors
This protocol describes how to fabricate and use wireless Mg sensors to monitor the integrity of a thin-film encapsulation [19].
Key Research Reagent Solutions:
| Item | Function in the Experiment |
|---|---|
| Polyimide (PI) Substrate | Serves as the flexible, biocompatible backbone for the sensor. |
| Titanium (Ti) Adhesion Layer | A thin layer (e.g., 20 nm) to ensure the Mg film adheres to the PI substrate. |
| Magnesium (Mg) Film | The active sensing element (~200 nm thick); corrodes predictably upon contact with water, changing resistance. |
| Backscatter Communication Circuit | A wireless, battery-free circuit that converts the resistance of the Mg sensor into a frequency-modulated (FM) backscatter signal. |
Methodology:
- Sensor Fabrication: Microfabricate the Mg sensor on a flexible polyimide substrate. This involves sequential steps of thin-film deposition (DC sputtering, thermal evaporation) and photolithography patterning.
- Deposit a 20 nm Ti adhesion layer onto the PI.
- Deposit a ~200 nm thick Mg film.
- Pattern the Mg into the desired sensor design (e.g., stripes, serpentines) using wet or dry etching.
- Encapsulation & Integration: Apply the Thin-Film Encapsulation (TFE) layer(s) to be tested directly over the Mg sensor. Integrate the sensor with the wireless backscatter circuit.
- Testing & Data Collection: Immerse the encapsulated sensor in a phosphate-buffered saline (PBS) solution or implant it in vivo.
- Monitoring: Use an external reader to wirelessly power the tag and monitor the frequency of the backscattered signal. The corrosion of the Mg sensor causes its resistance (
R_set) to increase, which in turn decreases the oscillation frequency (f_osc) of the circuit. This frequency shift is used to calculate the Water Transmission Rate (WTR) in real-time.
Visualized Workflows
Diagram 1: Encapsulation Failure Pathway
Diagram 2: Laser-Cut Edge Optimization Workflow
Diagram 3: Wireless Permeation Monitoring System
Troubleshooting Guides
FAQ: Addressing Common Interconnect Failure Modes
Q1: What are the primary failure modes for interconnects in flexible bioelectronic implants?
The primary failure modes are delamination and fatigue cracking, largely driven by mechanical mismatch. In flexible implants, rigid inorganic encapsulation layers (like ALD-deposited metal oxides) are often deposited on soft polymer substrates. The high elastic mismatch at this interface creates a significant driving force for mechanical failure under applied loading, leading to delamination. Furthermore, the natural movements of the body apply cyclic stresses to the interconnects, which can lead to metal trace fatigue and cracking over time. [29]
Q2: How does water permeation relate to mechanical failures like delamination?
Mechanical failures create pathways for water and ion permeation, which accelerates device degradation. A failure in the encapsulation barrier, such as a delaminated area or a micro-crack, allows bodily fluids to penetrate the device. This can cause current leakage, corrosion of metal components, and ultimately, device failure. Preventing mechanical delamination is therefore a critical first line of defense against water-induced failure. [1] [29]
Q3: My encapsulated device failed in accelerated aging tests. How can I determine if the failure was mechanical or chemical?
Analysis of the failure site can provide clues. Mechanical failures often present as visible cracks in the encapsulation layer, delamination at material interfaces, or broken electrical traces. Chemical failures due to water permeation often result in corrosion of metal components, such as electrodes or interconnects. Advanced techniques like scanning electron microscopy (SEM) can be used to identify micro-cracks and delamination, while energy-dispersive X-ray spectroscopy (EDS) can detect corrosive products on metal surfaces. [29]
Q4: What strategies can protect the vulnerable sidewalls of microelectrode devices?
Conventional wafer-based fabrication leaves device sidewalls exposed after the final etch, creating a primary path for moisture ingress. A promising strategy is 3D atomic layer infiltration (3D-ALI). This technique involves coating freestanding devices, ensuring that the encapsulation material covers all surfaces, including the vulnerable sidewalls at the electrode vias and device outlines, creating a seamless protective barrier. [29]
Q5: Why is my device experiencing warpage, and how does this stress the interconnects?
Warpage is often caused by thermo-mechanical stress from mismatched Coefficients of Thermal Expansion (CTE) between different materials in the stack (e.g., silicon die, polymer substrate, encapsulation layer). This warpage puts significant stress on the delicate interconnects (like microbumps or hybrid bonds), potentially leading to cracking, open circuits, or delamination. This is a critical consideration in 3D packaging and high-stack architectures. [30] [31]
Troubleshooting Guide: Interconnect Delamination and Fatigue
| Problem Symptom | Possible Root Cause | Diagnostic Experiments | Proposed Solution & Preventive Actions |
|---|---|---|---|
| Electrical opens or intermittent signals | Fatigue cracking of metal interconnects due to cyclic strain from body movement. [7] | - Use coherent laser scanning to detect micro-cracks pre-reflow. [30]- Perform in-situ electrochemical impedance spectroscopy (EIS) during mechanical cycling. | - Redesign layout to place interconnects in the neutral mechanical plane.- Use more ductile metals or liquid metal composites. [7] |
| Delamination of encapsulation layer | High elastic modulus mismatch between rigid encapsulation (e.g., ALD Al₂O₃) and soft polymer substrate. [29] | - Characterize adhesion strength with peel tests.- Use SEM to inspect cross-sections for interface separation. | - Implement a modulus-graded encapsulation (e.g., Atomic Layer Infiltration, ALI) to create an ambiguous, resilient interface. [29] |
| Device warpage leading to interconnect stress | Thermomechanical stress from CTE mismatch in heterogeneous material stack. [30] [31] | - Use surface topography tools to measure warpage at different temperatures. [30]- Simulate stress with finite element analysis (FEA). | - Adopt chip-package co-design to select CTE-compatible materials. [31]- Use underfill materials to redistribute stress. |
| Water ingress and corrosion at edges | Unprotected sidewalls from conventional planar fabrication acting as permeation pathways. [29] | - Soak devices in ionic solution (e.g., pH 7.4 PBS) and monitor leakage current. [1]- Use dye penetration tests to visualize pathways. | - Employ 3D encapsulation strategies (e.g., 3D-ALI or liquid-based encapsulation) that protect all device surfaces. [29] [1] |
| Voids in hybrid bonds or underfill | Particle contamination or organic residue on bonding surfaces preventing proper contact. [30] | - Use high-speed, sub-micron inspection for surface anomalies. [30]- Employ non-contact acoustic metrology to detect sub-1µm voids. | - Implement stringent surface cleaning protocols pre-bonding.- Use analytical software for real-time process control. [30] |
Experimental Protocols for Barrier Performance and Mechanical Integrity
Protocol 1: Accelerated Aging and Electrochemical Failure Analysis
This protocol assesses the long-term stability of encapsulated interconnects under simulated physiological conditions. [29]
Methodology:
- Sample Preparation: Fabricate test devices with interdigitated electrodes (IDEs) and apply the encapsulation strategy under investigation (e.g., ALD, 3D-ALI, liquid-based).
- Solution Immersion: Immerse devices in a phosphate-buffered saline (PBS) solution at a specific pH (e.g., 1.5, 7.4, or 9.0) to simulate different biological environments. [1] Maintain the solution at an elevated temperature (e.g., 87°C) to accelerate aging.
- In-Situ Monitoring: Use electrochemical impedance spectroscopy (EIS) to periodically measure the impedance of the IDEs. A significant drop in impedance indicates a loss of insulation and the formation of a water permeation pathway.
- Failure Analysis: Upon failure (or at set intervals), remove devices for post-mortem analysis using scanning electron microscopy (SEM) to identify the physical failure mechanism, such as delamination or cracking. [29]
Protocol 2: Mechanical Cyclic Strain Testing
This protocol evaluates the fatigue resistance of interconnects under dynamic mechanical loading that mimics implantation in mobile organs. [7]
Methodology:
- Fixture Setup: Mount the flexible bioelectronic device on a custom-built or commercial mechanical tester capable of applying cyclic bending or stretching (e.g., a motorized stage).
- In-Situ Electrical Monitoring: Connect the device's electrical interconnects to a multimeter or source measure unit to continuously monitor for electrical opens or significant resistance changes during testing.
- Apply Cyclic Strain: Subject the device to thousands of cycles of mechanical strain. The strain amplitude and rate should be selected to be biologically relevant (e.g., matching the movement of the heart or gastrointestinal tract).
- Post-Cycling Inspection: After testing, use optical microscopy and SEM to inspect for visible cracks, delamination, or other mechanical damage to the interconnects and encapsulation.
Research Reagent Solutions
Table: Key Materials for Bioelectronic Encapsulation and Interconnect Research
| Reagent / Material | Function / Application | Key Characteristics & Rationale |
|---|---|---|
| Krytox Oil (PFPE) [1] | Liquid-based encapsulation layer. | A perfluoropolyether fluid with an ultralow water diffusion coefficient; forms a slippery, protective surface on roughened elastomers to repel water and ions across a wide pH range. [1] |
| ALD Precursors (e.g., for Al₂O₃, HfO₂) [29] | Depositing thin, conformal inorganic barrier films. | Creates dense, pinhole-free layers that offer superior water and ion barrier properties. Used to encapsulate devices or as part of a multilayer stack. [29] |
| Polyimide (PI) Substrate | Flexible substrate for thin-film devices. | A common polymer with good mechanical and thermal properties for microfabrication; however, it is permeable to water, necessitating high-performance encapsulation. [29] |
| PDMS Elastomer [1] | Soft, flexible encapsulation substrate. | A silicone-based elastomer with a Young's modulus in the MPa range, matching the soft mechanics of biological tissues. Can be roughened to lock in lubricants for liquid-based encapsulation. [1] |
| Atomic Layer Infiltration (ALI) Modifiers [29] | Creating a hybrid polymer-inorganic interface. | By modifying ALD parameters, precursors infiltrate the polymer matrix, forming a gradient modulus that resists interfacial delamination by eliminating a sharp, weak interface. [29] |
Visualizing Encapsulation Strategies and Failure Pathways
Encapsulation Strategy Comparison
Interconnect Failure Pathways
In bioelectronic encapsulation research, preventing water permeation is the primary challenge for ensuring the long-term stability and functionality of implantable devices. Body fluids create a highly demanding environment where humidity and temperature fluctuations can lead to rapid device failure through corrosion, current leakage, and performance degradation [21]. Effective environmental control during manufacturing and operation is therefore not merely a quality check but a fundamental requirement for device success. This technical support center provides targeted guidance to help researchers troubleshoot common environmental stability issues and implement robust testing methodologies aligned with the stringent demands of bioelectronic encapsulation.
Troubleshooting Guides
Guide 1: Resolving Temperature and Humidity Fluctuations in Testing Chambers
Problem: Unstable temperature and/or humidity levels within an environmental test chamber, leading to inconsistent or unreliable experimental data.
Application: This is critical for accelerated aging tests and stability studies for bioelectronic encapsulation materials, where even minor deviations can skew water vapor transmission rate (WVTR) results.
Troubleshooting Steps:
Perform Visual Inspection:
- Check that the chamber door is fully closed and sealed.
- Inspect the door gasket for any signs of wear, cracks, or deformation and clean it if necessary [32].
- Look for any visible obstructions in the air ducts or around the sensors.
- Verify that water reservoirs for humidification are adequately filled and that drain lines are not clogged [33].
Analyze Logged Data:
- Download the chamber's internal data logger to examine the history of temperature and humidity [34] [32].
- Identify if the fluctuations are cyclical (suggesting a compressor or heater issue), constant (suggesting a calibration issue), or sporadic (suggesting human error or external factor influence).
Verify Calibration:
Inspect HVAC System Components:
- Filters: Check and replace air filters if they are dirty, as restricted airflow can disrupt environmental uniformity [32].
- Coils: Inspect evaporator and condenser coils for frost buildup (indicating a refrigeration issue) or excessive dirt (impeding heat transfer) [32].
- Humidification System: For steam-generator systems, check for mineral scale buildup. For atomizing systems, ensure nozzles are not clogged [35].
Guide 2: Investigating and Addressing Chamber Excursions
Problem: A significant excursion outside the predefined temperature and/or humidity tolerances has occurred for a stability study.
Application: Essential for complying with ICH guidelines in pharmaceutical and medical device stability testing, which includes studies for bioelectronic encapsulation materials and drug-device combination products [34] [36].
Troubleshooting Steps:
Immediate Action:
Risk Assessment:
- Gather essential information on the impacted materials, including their inherent stability, known sensitivity to temperature/moisture, and the point in their shelf-life study they had reached [34].
- For temperature-sensitive biologics or complex bioelectronics, even short excursions can be critical, whereas more stable materials may tolerate longer deviations [34].
Scientific Evaluation:
- For Controlled Room Temperature (CRT) chambers, calculate the Mean Kinetic Temperature (MKT) for the excursion period and the previous 30 days. MKT is a calculated, single temperature that reflects the cumulative thermal stress experienced by a product. The excursion may be acceptable if the MKT remains within the specified limit (e.g., not exceeding 25°C or 27°C, depending on the guideline) [34].
- Refer to existing stress study data for the material to understand its degradation profile and identify if the excursion conditions approached a critical phase change temperature (e.g., glass transition temperature) [34].
Corrective and Preventive Action (CAPA):
- Document the root cause analysis, whether it was a power failure, component failure, or human error [34].
- Implement corrective actions, which may include servicing the chamber, retraining staff, or installing a backup power supply.
- Based on the risk assessment, decide on sample disposition: continue the study, pull samples for immediate testing, or initiate a new backup study [34].
Experimental Protocols for Barrier Performance
Protocol 1: Liquid-Based Encapsulation for Extreme pH Environments
This protocol outlines the methodology for creating a robust, liquid-based encapsulation system for implantable bioelectronics that must operate in a broad range of pH conditions (from pH 1.5 to 9.0), such as in the gastrointestinal tract [21].
Workflow:
Materials and Equipment:
- Polydimethylsiloxane (PDMS) elastomer
- Abrasive paper (as a molding template)
- Krytox oil (a perfluoropolyether fluid, PFPE)
- UV laser system
- Vacuum desiccator
- Scanning Electron Microscope (SEM)
- Spectrophotometer
- Mechanical tester
Methodology Details:
- Elastomer Preparation: Create a roughened PDMS elastomer film (100 µm thick) using a molding technique with abrasive paper as a template. The arithmetical mean height (Sa) should be approximately 4.7 µm [21].
- Device Encapsulation: Place the bioelectronic device between two layers of the rough elastomer film, with the rough surfaces facing outward, to form a sandwich structure. Cure this assembly at ambient temperature overnight [21].
- Shaping: Cut the encapsulated device to the desired shape using a UV laser. Optimized parameters (e.g., 30 kHz frequency, 100 mm/s speed) create rougher cut edges that better retain the infusion liquid [21].
- Liquid Infusion: Infuse Krytox oil (15 µm thick) into the rough microstructures of the elastomer surface within a vacuum desiccator. This oil layer creates a slippery barrier with ultralow water permeability [21].
- Characterization:
- Optical: Measure optical transmittance in the visible wavelength range (380–700 nm). The oil-infused elastomer should maintain high transparency (~86.67%) [21].
- Mechanical: Perform stress-strain tests. The encapsulation should withstand up to ~100% strain, matching the compliance of biological tissues [21].
- Barrier Performance: Conduct soaking tests in buffers from pH 1.5 to 9.0, monitoring device performance (e.g., wireless signal strength). This encapsulation has demonstrated functionality for nearly 2 years in acidic conditions, far outperforming conventional materials like silicone or Parylene C [21].
Protocol 2: Measuring Water Transmission Rate (WTR) for Barrier Coatings
While Water Vapor Transmission Rate (WVTR) is a standard metric, the Water Transmission Rate (WTR) is more relevant for implantable devices as it measures permeability against liquid water, simulating direct contact with body fluids [37].
Workflow:
Materials and Equipment:
- Quadrupole Mass Spectrometer (QMS) permeation system
- Constant Conductance Element (CCE) leak for calibration
- Parylene or other barrier coating samples
- Electrolytic detection sensor system (for comparative WVTR via ISO 15106-03) [37]
Methodology Details:
- System Calibration: Calibrate the QMS system using a calibrated CCE leak. This creates a correlation between the ion current measured by the mass spectrometer and the molar flow of water molecules [37].
- Sample Mounting: Mount the barrier coating sample (e.g., a parylene film) in the test cell, separating the supply and detection sides of the apparatus [37].
- Liquid Water Introduction: Introduce liquid water to the supply side of the coating, simulating immersion in body fluid [37].
- Measurement: The QMS detects and quantifies the water molecules that permeate through the coating to the detection side. The system maintains a constant temperature via heaters and thermocouples [37].
- Calculation: Calculate the WTR using the formula:
- WTR = (QH2O × MH2O × 24 × 3600) / A [37]
- Where:
- QH2O is the water flow rate (mol/s) from calibration.
- MH2O is the molar mass of water (18 g/mol).
- A is the membrane area (m²).
- The result is in g m⁻² day⁻¹. Studies show the acceleration factor from WVTR to WTR can range from 4 to 4.8, meaning liquid water permeates 4-5 times faster than vapor [37].
Research Reagent Solutions
The following table details key materials used in advanced encapsulation research and testing.
| Item | Function/Description | Application in Research |
|---|---|---|
| Krytox Oil | A perfluoropolyether (PFPE) fluid with an ultralow water diffusion coefficient, used to create a slippery, liquid-repellent surface [21]. | Serves as the infusion liquid in liquid-based encapsulation, providing a superior barrier against water and ion penetration in extreme pH environments [21]. |
| Parylene C | A chemical vapor deposited polymer coating known for its biocompatibility, flexibility, and barrier properties [37]. | A benchmark material for implantable device encapsulation. Used as a control or base layer in barrier performance studies; reported WTR of 72.5 µm g m⁻² day⁻¹ [37]. |
| Polydimethylsiloxane (PDMS) | A common, biocompatible silicone elastomer. Can be engineered with surface roughness to lock infusion liquids [21]. | Used as the substrate matrix in liquid-based encapsulation systems due to its stretchability and ease of fabrication [21]. |
| Quadrupole Mass Spectrometer (QMS) | A highly sensitive detector that identifies and separates ionized molecules by their mass-to-charge ratio [37]. | The core of advanced permeation systems for accurately measuring the transmission rates of gases and water through thin-film barriers [37]. |
| Constant Conductance Element (CCE) | A calibrated, porous leak made of sintered stainless steel that provides a reference molar flow [37]. | Used for the in-situ calibration of permeation measurement systems like the QMS, ensuring quantitative accuracy [37]. |
Frequently Asked Questions (FAQs)
Q1: What are the ICH guidelines for temperature and humidity in stability chambers?
The ICH Q1A(R2) guideline sets global standards for stability testing conditions [36] [35]:
- Long-term Storage: 25°C ± 2°C / 60% Relative Humidity (RH) ± 5% RH [36]
- Intermediate Testing: 30°C ± 2°C / 65% RH ± 5% RH [36]
- Accelerated Testing: 40°C ± 2°C / 75% RH ± 5% RH [36] Chamber performance must be monitored continuously, and any excursions must be investigated [34].
Q2: Why is controlling humidity so critical for electronic and bioelectronic devices?
Humidity directly threatens electronic components. For every 10°C rise in ambient temperature above 25°C, the life of a battery can be reduced by 50% [38]. Moisture can cause short circuits, corrosion of metal traces, and insulation failure. For bioelectronics encapsulated in polymers, water permeation can lead to delamination, swelling, and ultimately, device failure [21].
Q3: What is the difference between WVTR and WTR, and why does it matter for implants?
- WVTR (Water Vapor Transmission Rate) measures the passage of water vapor through a material [37].
- WTR (Water Transmission Rate) measures the passage of liquid water through a material [37].
WTR is more relevant for implantable bioelectronics because these devices are in direct contact with or immersed in body fluids (a liquid environment). The permeation kinetics differ, with liquid water transmission rates being 4-5 times higher than vapor rates for the same barrier [37].
Q4: How long can a stability chamber excursion be before it impacts my study?
Regulatory guidelines often require investigation for excursions exceeding 24 hours [34]. However, the impact is not based on time alone. A scientific evaluation is necessary, considering:
- The duration and magnitude of the excursion.
- The type of chamber (CRT, accelerated, refrigerated).
- The sensitivity of the material being tested (e.g., biologics are more sensitive) [34]. Tools like Mean Kinetic Temperature (MKT) calculation are used to make this determination scientifically [34].
Q5: What are the key features to look for in a modern humidity chamber for R&D?
Modern chambers should offer:
- Precise Control: Tight ranges (e.g., ±0.5°C for temperature, ±2% RH for humidity) [38] [39].
- Broad Operational Range: Temperature from -70°C to 150°C and humidity from 10% to 98% RH to simulate diverse conditions [38] [33].
- Programmability: Ability to set complex, multi-step temperature and humidity profiles [38] [33].
- Data Logging and Connectivity: Continuous monitoring and data export via USB or Ethernet for compliance and analysis [39] [33].
- Uniformity: Horizontal laminar airflow to ensure consistent conditions across all shelves [35].
Troubleshooting Guide: Common Coating and Encapsulation Failures
How can I diagnose the cause of incomplete surface coverage or uneven coating in my encapsulation layer?
Uneven coating often manifests as visible defects, variable device performance, or inconsistent barrier protection.
| Observed Symptom | Potential Root Cause | Corrective Action |
|---|---|---|
| Incomplete Coverage | Incorrect coating viscosity; Unsuitable surface energy; Improper application technique. | Characterize material viscosity; Implement oxygen plasma treatment to increase surface wettability [1]; Optimize spin-coating or dip-coating parameters. |
| Pinholing/Cratering | Particulate contamination; Substrate outgassing; Rapid, uneven drying. | Filter coating solution prior to use; Ensure substrate is clean and dry; Control ambient humidity during application and curing. |
| Orange Peel Texture | Coating material drying too quickly; Poor flow and leveling. | Adjust solvent composition to slow evaporation rate; Use a leveled surface for curing. |
What are the primary reasons for coating delamination or adhesion failure under physiological conditions?
Adhesion failure occurs when the encapsulation layer separates from the device substrate, leading to immediate barrier compromise.
| Observed Symptom | Potential Root Cause | Corrective Action |
|---|---|---|
| Full Layer Delamination | Inadequate surface pretreatment; Mechanical modulus mismatch; Stresses from swelling. | Employ adhesion promoters (e.g., silanes); Use intermediate modulus layers to grade stiffness from hard electronics to soft coating [7]; Test coating stability in aqueous environments prior to implantation. |
| Edge-Lift Failure | High interfacial stresses at device edges; Weak boundary layer. | Design devices with rounded corners; Ensure laser-cut edges are optimized to retain lubricant [1]; Verify coating conformality over sharp topographical features. |
Why is my encapsulated bioelectronic device failing in acidic or alkaline pH environments?
Conventional encapsulation materials like silicone elastomer (PDMS) or Parylene C can degrade rapidly in non-neutral pH conditions, such as in the gastrointestinal tract (pH ~1.5-4.5) or chronic wounds (pH up to 9) [1].
| Observed Symptom | Potential Root Cause | Corrective Action |
|---|---|---|
| Rapid Performance Drop in Low pH | Material degradation of standard encapsulants in acid. | Implement a liquid-based encapsulation strategy, such as an oil-infused elastomer, designed for broad pH stability [1]. |
| Corrosion of Metal Components | Penetration of H⁺ or OH⁻ ions through the barrier. | Utilize synthetic perfluoropolyether (PFPE) fluids like Krytox oil, which have an ultralow water diffusion coefficient and resist corrosive ions [1]. |
Frequently Asked Questions (FAQs)
Q1: What methods exist for the real-time, in-situ monitoring of water permeation through thin-film encapsulation?
A novel approach uses wireless, battery-free platforms with magnesium (Mg) microsensors. When water permeates the encapsulation, it corrodes the Mg sensor, changing its electrical resistance. This resistance shift is wirelessly transmitted via a backscatter communication system, allowing for real-time quantification of the Water Transmission Rate (WTR) without explanting the device [19]. This method is particularly valuable for chronic implantation studies and predictive failure analysis.
Q2: How can I improve the anti-fouling properties of my encapsulation surface to prevent biofilm and thrombus formation?
Lubricant-Infused Slippery (LIS) surfaces are a promising solution. These are created by infusing a structured elastomer with a biocompatible lubricant like silicone or perfluoropolyether oil. The resulting liquid interface provides a smooth, non-adhesive surface that significantly reduces the adhesion of platelets, proteins, and bacteria, thereby mitigating both thrombosis and biofilm formation [1] [40]. This offers a passive, drug-free strategy for enhancing biocompatibility.
Q3: My encapsulation is flexible but lacks sufficient water barrier properties. What strategies can enhance flexibility while maintaining a high barrier performance?
The key is using hybrid or multilayer strategies. A highly effective method is a liquid-based approach, where a rough, flexible PDMS elastomer is infused with a barrier liquid like Krytox oil. This combination achieves both mechanical compliance (up to ~100% strain) and superior barrier performance, protecting devices for extended periods even in harsh pH environments [1]. Alternatively, multilayer thin-films combining inorganic barriers (e.g., Al₂O₃, SiNₓ) with organic interlayers can also provide excellent flexibility and low Water Transmission Rates (WTR) [19].
Experimental Protocol: Quantifying Barrier Performance with Wireless Mg Sensors
This protocol details a method for in-situ, real-time monitoring of water permeation through thin-film encapsulations using magnesium-based microsensors [19].
Materials Required
- Substrate: Flexible polyimide (PI) film.
- Sensor Metal: High-purity Magnesium (Mg) target for sputtering/evaporation.
- Adhesion Layer: Titanium (Ti).
- Encapsulation Material: The thin-film system under test (e.g., atomic-layer-deposited Al₂O₃, Parylene C).
- Fabrication Tools: Sputter coater or thermal evaporator, UV photolithography setup, wet/dry etching equipment.
- Testing Equipment: Phosphate-Buffered Saline (PBS), environmental chamber, RF spectrum analyzer, custom reader/interrogator.
Step-by-Step Methodology
Sensor Fabrication:
- Deposit a 20 nm Ti adhesion layer onto a clean, cured PI substrate.
- Deposit a ~200 nm thick Mg film via DC sputtering or thermal evaporation.
- Pattern the Mg film into desired geometries (e.g., stripes, serpentines) using photolithography and subsequent wet etching.
Circuit Integration:
- Integrate the patterned Mg sensor as the resistive element (
R_set) in a square-wave oscillator circuit. - Connect the oscillator to an RF switch and a flexible dipole antenna to create a backscatter communication tag.
- Integrate the patterned Mg sensor as the resistive element (
Encapsulation and Calibration:
- Apply the Thin-Film Encapsulation (TFE) of interest to fully cover the Mg sensor.
- Prior to immersion, calibrate the relationship between the sensor's initial resistance and the oscillator's baseline frequency (
f_osc).
In-Vitro Testing and Data Collection:
- Immerse the encapsulated sensor in PBS at a controlled temperature (e.g., 37°C).
- Use an external reader to wirelessly power the tag and record the frequency of the backscattered signal over time.
- Correlate the frequency shift to the increasing resistance of the corroding Mg sensor.
Data Analysis:
- Use an analytical model to convert the time-dependent frequency data into a Water Transmission Rate (WTR) value for the tested encapsulation.
Experimental Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents and Materials
| Material/Reagent | Function in Encapsulation Research |
|---|---|
| Polydimethylsiloxane (PDMS) | A common silicone elastomer used to create flexible, stretchable substrate and encapsulation layers. It is often modified with surface textures or used as a matrix for other materials [1] [40]. |
| Parylene C | A polymer deposited as a conformal, transparent vapor. It provides a good moisture barrier and electrical insulation for neural interfaces and other bioelectronics, though it may be less effective in extreme pH [1] [8]. |
| Krytox Oil (PFPE) | A synthetic perfluoropolyether lubricant with an ultralow water diffusion coefficient. It is infused into textured elastomers to create liquid-based, pH-tolerant slippery surfaces for encapsulation [1]. |
| Magnesium (Mg) Thin Films | Used as a water-sensitive material in permeation microsensors. Its corrosion upon water contact provides a quantifiable, wireless signal to monitor barrier integrity in real-time [19]. |
| Polyimide (PI) | A flexible polymer substrate with high thermal and chemical stability, commonly used as a base for flexible electronics and thin-film encapsulation stacks [19]. |
From Lab to Living Systems: Validating and Benchmarking Encapsulation Performance
Frequently Asked Questions (FAQs)
Q1: Why is testing across a broad pH range (1.5 to 9.0) critical for bioelectronic encapsulation?
Biological tissues and fluids span a wide pH spectrum, from the highly acidic environment of the stomach (as low as pH 1.5) to the alkaline conditions found in some chronic wounds (up to pH 8.9). [1] These varying concentrations of H⁺ and OH⁻ ions can rapidly degrade encapsulation materials that are only designed for neutral, physiological pH (7.4), leading to device failure. Testing across this full range ensures the encapsulation will be robust enough for a variety of clinical applications. [1]
Q2: What are the key performance indicators for an encapsulation material during in vitro soaking tests?
The primary indicators are:
- Barrier Performance: The material's ability to prevent water and ion permeation, which is often quantified by a Water Transmission Rate (WTR). [19] Long-term stability of electrical device performance, such as the consistent operation of a Near-Field Communication (NFC) antenna, is a key functional measure. [1]
- Mechanical Integrity: The material should maintain its flexibility and stretchability without cracking or delaminating, even after prolonged immersion. [1]
- Optical Transparency: For optoelectronic devices, high optical transmittance in the visible wavelength range must be preserved to allow light-based signaling. [1]
Q3: Our encapsulated devices are failing prematurely in acidic soaking tests. What are the most likely causes?
Premature failure often stems from:
- Material Incompatibility: The chosen encapsulation polymer may not be chemically stable in extreme pH, leading to hydrolysis or degradation. [1]
- Inadequate Sealing at Edges: The side edges of the encapsulation, often created by laser cutting, can provide a pathway for fluid ingress if not properly sealed. [1]
- Permeation Through Bulk Material: The material itself may have a high inherent permeability to water vapor and ions, which can be monitored using integrated magnesium (Mg) microsensors. [19]
Q4: How can we monitor water permeation in real-time during a soaking experiment?
You can integrate a wireless, battery-free platform that uses the corrosion of magnesium (Mg) resistive microsensors. [19] When water permeates the encapsulation, it corrodes the Mg sensor, changing its resistance. This resistance shift is wirelessly transmitted via a backscatter communication system, allowing for real-time, in-situ quantification of the Water Transmission Rate (WTR). [19]
Troubleshooting Guides
Problem: Rapid Performance Degradation in Acidic Conditions (pH < 4.5)
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Material lacks chemical resistance to low pH. | Inspect for material swelling, softening, or discoloration. Check literature for material's known pH stability. | Switch to a pH-resistant encapsulation system, such as an oil-infused elastomer, which has demonstrated durability for months in pH 1.5 environments. [1] |
| Fluid ingress through cut edges. | Use microscopy to examine encapsulation edges for gaps or poor adhesion. Use dye penetration tests. | Optimize laser-cutting parameters to create rougher edges that better retain sealing oils or adhesives. [1] |
| Insufficient adhesion between encapsulation layers. | Perform a peel test after soaking. Look for signs of delamination or blistering. | Ensure surfaces are clean and dry before bonding. Use a compatible, stable adhesive and optimize the curing process. |
Problem: Loss of Optical Transparency During Soaking
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Formation of micro-cracks or crazing. | Examine under high-magnification microscope for surface defects. | Use a more flexible and stretchable material to accommodate swelling stresses without cracking. [1] |
| Cloudiness due to material hydrolysis. | Confirm if the haze is uniform, indicating bulk material change. | Select a polymer with higher hydrolytic stability (e.g., specific perfluoropolyethers or silicones). |
| Delamination creating light-scattering interfaces. | Use optical or electron microscopy to inspect cross-sections for gaps between layers. | Improve interfacial adhesion through surface plasma treatment or the use of adhesion promoters. |
Data Presentation: Encapsulation Material Comparison
The following table summarizes key characteristics of various encapsulation materials, based on data from recent research, to aid in material selection for your soaking experiments. [1]
Table 1: Properties of Encapsulation Materials for Bioelectronics
| Material | Avg. Optical Transmittance (Visible Light) | Failure Strain | Young's Modulus | Performance in pH 1.5 Soak |
|---|---|---|---|---|
| Oil-Infused Elastomer | ~86.67% | ~100% | A few MPa | Outstanding; maintains device performance for months to nearly 2 years. [1] |
| Silicone Elastomer (PDMS) | ~95.33% | ~100% | A few MPa | Poor; complete device failure within 1.5-19 days. [1] |
| Parylene C | ~87.43% | < 5% | A few GPa | Poor; rapid performance degradation in acidic environments. [1] |
| Polyimide (PI) | 7.70% - 71.22% | < 5% | A few GPa | Limited to neutral pH; not suitable for broad pH range. [1] |
| Liquid Metal | ~0.01% | N/A - Liquid | N/A - Liquid | Unsuitable for optoelectronics; may corrode in low pH. [1] |
Experimental Protocols
Protocol 1: Long-Term Soaking Test for Barrier Performance
This protocol assesses the long-term durability of encapsulation under extreme pH conditions. [1]
- Sample Preparation: Encapsulate a functional bioelectronic component (e.g., an NFC antenna or a magnesium sensor) using your chosen method. A sandwch structure with the sensitive device between two layers of encapsulation material is recommended. [1]
- Solution Preparation: Prepare buffered soaking solutions at the desired pH values (e.g., 1.5, 4.5, 7.4, 9.0). Phosphate-buffered saline (PBS) is commonly used for neutral pH, while appropriate buffers should be selected for acidic and alkaline conditions.
- Immersion: Immerse the encapsulated devices in the solutions. Maintain a constant temperature (e.g., 37°C) to simulate physiological conditions. Include multiple samples for statistical significance.
- Monitoring:
- Functional Testing: At regular intervals, remove devices and wirelessly test the performance of the encapsulated electronics (e.g., measure the power transfer efficiency of an NFC antenna). [1]
- Real-Time Monitoring: For setups with integrated Mg sensors, continuously monitor the oscillation frequency of the backscatter circuit, which correlates directly with sensor resistance and the extent of water-induced corrosion. [19]
- Endpoint Analysis: After the test period, perform a post-mortem analysis using techniques like scanning electron microscopy (SEM) to inspect for corrosion, cracks, or delamination.
Protocol 2: Real-Time Water Permeation Monitoring with Mg Sensors
This protocol uses a wireless, battery-free platform for in-situ quantification of water permeation. [19]
- Fabricate Mg Sensors: Microfabricate ~200-nm thick Mg film sensors on a flexible polyimide substrate with a thin Titanium (Ti) adhesion layer. Pattern the Mg into designs like stripes or serpentines. [19]
- Integrate and Encapsulate: Integrate the Mg sensor into an oscillator circuit that is connected to a flexible dipole antenna. Fully encapsulate the entire system with the thin-film encapsulation (TFE) you are testing. [19]
- Setup Interrogation System: Place the device in the soaking solution. Use an external RF interrogator (reader) to power the device wirelessly and a spectrum analyzer to measure the frequency of the backscattered signal. [19]
- Data Collection and Analysis: Record the frequency shift over time as the Mg corrodes. Use an analytical model to convert this frequency data into a Water Transmission Rate (WTR) value for the encapsulation. [19]
Experimental Workflow and Failure Analysis
The following diagram illustrates the key steps and decision points in a comprehensive soaking experiment.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Encapsulation Soaking Experiments
| Reagent / Material | Function in Experiment | Key Details / Rationale |
|---|---|---|
| Krytox Oil (PFPE) [1] | Infused into roughened elastomers to create a slippery, impermeable surface barrier. | Synthetic perfluoropolyether fluid with an ultralow water diffusion coefficient, stable across broad pH. [1] |
| Polydimethylsiloxane (PDMS) [1] | A common, stretchable elastomer used as the base substrate for encapsulation. | High optical transparency and mechanical compliance with tissues; requires surface roughening and oil infusion for high barrier performance. [1] |
| Magnesium (Mg) Thin Films [19] | Acts as a corrosive water permeation sensor. Resistance change indicates water ingress. | ~200 nm thick films are microfabricated; corrosion to Mg(OH)₂ is quantifiable and correlates with Water Transmission Rate (WTR). [19] |
| Phosphate-Buffered Saline (PBS) [41] | A standard isotonic soaking solution for simulating physiological (pH 7.4) conditions. | Provides a consistent ionic environment; often used as a baseline for in vitro tests. [41] |
| Polyimide (PI) Substrate [19] | A flexible and mechanically robust substrate for fabricating sensors and devices. | Young's modulus of ~2.5 GPa; provides a stable platform for thin-film devices during soaking. [19] |
This technical support center provides resources for researchers working on bioelectronic encapsulation, with a specific focus on preventing water and ion permeation. The following guides and FAQs offer a comparative analysis of three key encapsulation materials—Silicone Elastomer, Parylene C, and Liquid Metal—based on current research. The information is structured to help you select appropriate materials and troubleshoot common experimental challenges in the development of durable implantable and wearable bioelectronics.
Material Properties at a Glance
The following table summarizes the key properties of the three benchmarked encapsulation materials, providing a baseline for material selection.
| Property | Silicone Elastomer (PDMS) | Parylene C | Liquid Metal (e.g., E-GaInSn) |
|---|---|---|---|
| Primary Material Type | Organic Polymer (Elastomer) | Organic Polymer (Poly(chloro-para-xylylene)) | Metallic Alloy (Gallium-based) |
| Typical Young's Modulus | ~Few MPa (Compliant) [1] | ~Few GPa (Rigid) [1] | Fluid / Defined by composite matrix |
| Failure Strain | ~100% (Stretchable) [1] | <5% (Brittle) [1] | Fluid / Defined by composite matrix |
| Optical Transparency (Visible Spectrum) | High (~95% for 100µm) [1] | High (~87% for 15µm) [1] | Opaque (~0.01% for 15µm) [1] |
| Water Vapor Barrier Performance | Moderate; improved by 3 orders of magnitude with oil-infusion [42] | Good, but limited by defects and inherent permeability over time [43] | Excellent (Hermetic) [1] |
| Performance in Acidic (pH 1.5-4.5) / Alkaline (pH 9) Environments | Excellent when using oil-infused slippery surfaces [1] | Often fails in extreme pH [1] | Susceptible to corrosion in low pH [1] |
| Key Advantage for Bioelectronics | Mechanical compliance and stretchability matching biological tissues [1] | Conformal, pinhole-free coating via chemical vapor deposition (CVD); FDA-approved [44] | Superior thermal conductivity (~30 W m⁻¹ K⁻¹) and hermetic sealing [45] |
| Primary Limitation for Bioelectronics | Permeable to water and ions without advanced modification [42] | Limited stretchability; can delaminate or crack on dynamic surfaces [1] [43] | Opaque, electrically conductive, and can corrode metal components like aluminum [1] [45] |
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: My Parylene C-encapsulated device failed after a few weeks in a saline solution. What could be the cause? A: Failure is often due to water molecule permeation through microscopic defects (pinholes, cracks) or the free volume in the polymer chain itself [43]. This permeation leads to current leakage, corrosion of metal traces, and eventual device failure. Consider using a hybrid barrier, such as a nano-layer of Al₂O₃ deposited via Atomic Layer Deposition (ALD) on top of the Parylene C, to fill defects and significantly extend the device's lifetime [43].
Q2: I need a stretchable encapsulation for a device on a moving organ, but also require a high water barrier. What are my options? A: A recently developed high-performance option is an oil-infused silicone elastomer (PDMS) [1] [42]. This method involves creating a roughened PDMS surface, encapsulating the device, and then infusing a thin layer of a perfluoropolyether (PFPE) oil (e.g., Krytox) into the rough structure in a vacuum. This liquid-based encapsulation provides a water vapor barrier improvement of three orders of magnitude over plain PDMS while maintaining the material's inherent stretchability and optical transparency [42].
Q3: Is liquid metal a suitable hermetic encapsulation for all implantable bioelectronics? A: No, its use cases are specific. While liquid metal provides an ultralow permeability seal [1], it is opaque, blocking light transmission for optoelectronics. It is also electrically conductive, which can short-circuit exposed components. Furthermore, pure gallium-based liquid metals can corrode common metals like aluminum [45]. Its application is best suited for non-optical, thermally conductive encapsulation where its conductivity and opacity are not detrimental.
Troubleshooting Common Experimental Challenges
Problem: Delamination of Parylene C Coating from Substrate
- Potential Cause: Poor adhesion due to low surface energy of the substrate or contamination.
- Solutions:
- Adhesion Promotion: Treat the substrate with an oxygen plasma to activate the surface before deposition [44].
- Silane Coupling Agent: Use a liquid adhesion promoter like A-174 Silane, which forms a durable bond between organic and inorganic materials [44].
- Surface Roughening: Mechanically abrade the substrate to create a topography that the Parylene can better grip [44].
Problem: Liquid Metal Encapsulation Corroding Underlying Metal Components
- Potential Cause: Direct contact between the gallium-based liquid metal and susceptible metals like aluminum, leading to grain boundary penetration and embrittlement [45].
- Solutions:
- Create a Composite: Form a liquid metal-polymer grease by dispersing LM droplets in a matrix like PDMS. The polymer acts as a barrier, isolating the LM from the metal surface and inhibiting corrosion [45].
- Apply a Protective Coating: Anodize the aluminum substrate to create a protective aluminum oxide (AAO) film that prevents direct contact with the liquid metal [45].
Problem: Water Permeation Through Standard Silicone Elastomer (PDMS)
- Potential Cause: PDMS is inherently permeable to water vapor and ions due to its porous molecular structure [42].
- Solution: Implement a Liquid-Based Barrier:
- Fabricate Roughened PDMS: Use a molding technique with abrasive paper as a template to create a micro-rough surface on a ~100 µm PDMS film [1].
- Sandwich the Device: Place your bioelectronic device between two layers of the rough elastomer with the rough surfaces facing outward and cure.
- Infuse with Oil: Place the sandwiched device in a vacuum desiccator with Krytox oil (a PFPE fluid) to infuse the rough structures, creating a stable, slippery surface [1].
Experimental Protocols
Protocol 1: Creating an Oil-Infused Slippery Elastomer for Encapsulation This protocol is adapted from recent research on liquid-based encapsulation for implantable bioelectronics [1].
- Mold the Rough Elastomer: Prepare a ~100 µm thick layer of PDMS using a molding technique with abrasive paper as a template. This creates a surface with a controlled roughness.
- Encapsulate the Device: Sandwich the target bioelectronic device between two layers of the rough PDMS film, ensuring the rough surfaces are facing outward. Cure the assembly at ambient temperature overnight.
- Laser Cutting (Optional): Cut the encapsulated device to the desired shape using a UV laser. Parameters of 30 kHz frequency and 100 mm/s speed can help create rougher edges that better retain the oil [1].
- Oil Infusion: Place the encapsulated device in a vacuum desiccator. Introduce Krytox oil (a PFPE fluid with an ultralow water diffusion coefficient) to infuse the rough surface structures of the elastomer, forming a continuous, slippery layer.
Protocol 2: Enhancing Parylene C Barrier with a Nano-Al₂O₃ Layer (Defect Filling Method) This protocol is based on a defect-filling method to improve the waterproof ability of Parylene C coatings [43].
- Apply Parylene C Coating: First, deposit a conformal layer of Parylene C (e.g., several micrometers thick) onto your device using the standard Chemical Vapor Deposition (CVD) process [44].
- Deposit Al₂O₃ Nano-Layer: Use Atomic Layer Deposition (ALD) to deposit a dense, nanoscale-thick layer of Al₂O₃ directly onto the Parylene C surface. The low-rate ALD process allows Al₂O₃ molecules to fill and repair pinholes and other defects on the polymer surface.
- Cure & Characterize: This micro-nano composite structure creates a hybrid barrier that significantly delays the penetration of water molecules compared to Parylene C alone [43].
Workflow and Material Selection Diagrams
Encapsulation Material Selection Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Research Reagent / Material | Function in Encapsulation Research |
|---|---|
| Krytox Oil (PFPE Fluid) | A synthetic perfluoropolyether oil infused into roughened PDMS to create a slippery surface with exceptional water and ion barrier properties [1] [42]. |
| Parylene C Dimer | The raw powder material used in the Chemical Vapor Deposition (CVD) process to grow a conformal, biocompatible, and waterproof polymer coating [44]. |
| A-174 Silane | A silane coupling agent used as an adhesion promoter to ensure strong bonding between the Parylene C film and the underlying substrate (e.g., metals, silicon) [44]. |
| ALD Al₂O₃ Precursors | Chemicals (e.g., Trimethylaluminum + H₂O) used in Atomic Layer Deposition to create a dense, nanoscale oxide layer that fills defects in Parylene C, enhancing its barrier lifetime [43]. |
| Eutectic Gallium-Indium-Tin (E-GaInSn) | A gallium-based liquid metal alloy with a low melting point, used to create a hermetic, highly thermally conductive seal for specific non-optical applications [45]. |
FAQs: Core Concepts in Implant Stability and Encapsulation
1. What is the primary cause of failure in chronically implanted bioelectronics? Water and ion permeation are the primary causes of failure. Ingress through encapsulation leads to current leakage, corrosion of electronic components, and eventual device failure. Effective encapsulation must provide a superior barrier against this penetration while maintaining flexibility to match surrounding tissues [1] [7] [19].
2. How can we quantitatively monitor water permeation in a live animal model? A wireless, battery-free platform using magnesium (Mg) microsensors can monitor water permeation in real-time. Water permeation corrodes the Mg sensor, changing its resistance. This resistance shift tunes a backscatter circuit, wirelessly transmitting a frequency-modulated signal that correlates directly with the Water Transmission Rate (WTR) [19].
3. Why is flexibility important for implantable bioelectronics? The body comprises soft, dynamic, and continuously moving tissues. Rigid implants cause a mechanical mismatch, leading to inflammation, fibrosis, and device failure. Flexible and stretchable encapsulation materials conform to organs and tissues, reducing immune response and improving long-term stability and signal fidelity [7] [46].
4. My implant shows good short-term biocompatibility but fails long-term. What should I investigate? Focus on the chronic foreign body response and encapsulation durability. Even biocompatible materials can trigger fibrous capsule formation over time, which can isolate the device and degrade performance. Evaluate the integrity of your barrier encapsulation over the intended lifespan and assess the histopathology of the implant-tissue interface at multiple time points [7] [46].
5. Are there encapsulation solutions for extreme biological pH environments? Yes, liquid-based encapsulation strategies have been developed for broad pH environments. For instance, oil-infused elastomers have demonstrated robust performance in vitro in extremely acidic (pH 1.5) and alkaline (pH 9.0) conditions, maintaining functionality where conventional materials like silicone elastomer or Parylene C fail rapidly [1].
Troubleshooting Guides
Problem: Rapid Device Failure in a Dynamic Physiological Environment
Symptoms: Device malfunction or corrosion observed within days or weeks of implantation in mobile organs (e.g., stomach, heart).
Possible Causes and Solutions:
| Cause | Diagnostic Steps | Solution |
|---|---|---|
| Mechanical mismatch | Histopathology to check for excessive fibrotic encapsulation and inflammation at the tissue interface. | Switch to a softer, more compliant encapsulation material with a lower Young's modulus (e.g., PDMS elastomers) to better match the mechanics of the host tissue [7]. |
| Inadequate edge sealing | Inspect device edges post-explanation for pathways of fluid ingress. | Optimize laser-cutting parameters for encapsulation layers to create rougher edges that better retain barrier liquids or sealants [1]. |
| Barrier material failure in extreme pH | Test encapsulation in vitro using buffers that mimic the target biological environment (e.g., pH 1.5 for stomach). | Employ a liquid-based encapsulation designed for harsh pH, such as an oil-infused elastomer, which can provide long-term protection in both acidic and alkaline conditions [1]. |
Problem: Inconsistent or Unreliable Wireless Performance In Vivo
Symptoms: Erratic data transmission or power harvesting from wireless components (e.g., NFC antennas) after implantation.
Possible Causes and Solutions:
| Cause | Diagnostic Steps | Solution |
|---|---|---|
| Corrosion of wireless components | Use a wireless WTR monitoring platform [19] to confirm water ingress. Alternatively, conduct post-explantation analysis of the antenna. | Improve the encapsulation's Water Transmission Rate (WTR). Consider multilayer or liquid-infused barriers with ultralow water permeability [1] [19]. |
| Signal blockage by fibrous capsule | Use medical imaging (e.g., MRI) to observe capsule thickness around the device. | Ensure the outer surface of the encapsulation is biocompatible to minimize fibrous capsule formation. Surface modifications with bioactive coatings can improve integration [47] [46]. |
Experimental Protocols for Key Assessments
Protocol 1: Real-Time, In Vivo Water Permeation Monitoring
This protocol leverages a wireless, battery-free system to quantify the Water Transmission Rate (WTR) of thin-film encapsulations in real-time [19].
1. Sensor Fabrication:
- Substrate: Use a flexible polyimide (PI) substrate (~5 µm thick).
- Sensor Deposition: Deposit a ~200 nm thick Magnesium (Mg) film with a 20 nm Titanium (Ti) adhesion layer via thermal evaporation or DC sputtering. Pattern the Mg into various designs (e.g., stripes, serpentines) using photolithography and etching.
- Encapsulation: Coat the fabricated Mg sensor with the Thin-Film Encapsulation (TFE) you are testing.
2. System Integration:
- Integrate the encapsulated Mg sensor into a flexible, battery-free backscatter communication tag.
- The tag consists of a square-wave oscillator circuit whose frequency (
f_osc) is tuned by the resistance of the Mg sensor (R_set). - A flexible dipole antenna is integrated for wireless communication.
3. In Vivo Implantation and Data Collection:
- Implant the integrated device subdermally or intramuscularly in an anesthetized animal model (e.g., mouse).
- An external interrogator (reader) transmits a radio-frequency (RF) carrier wave to power the tag and receives the backscattered signal.
- As water permeates the TFE, the Mg corrodes, increasing
R_setand decreasingf_osc. - Monitor the frequency shift in the backscattered signal using an RF spectrum analyzer.
4. Data Analysis:
- Use an analytical model to convert the recorded frequency shift over time into a quantitative WTR value for the tested encapsulation.
Protocol 2: Assessing Long-Term Biocompatibility and Tissue Integration
This protocol outlines a standard methodology for evaluating the host tissue response to an implanted material or device over an extended period, as used in studies on nanostructured coatings and magnesium implants [48] [49] [47].
1. Animal Model and Implantation:
- Select an appropriate animal model (e.g., guinea pigs, rats, minipigs) based on the research question and required tissue volume.
- Follow ethical guidelines and obtain necessary approvals.
- Implant the test material and appropriate controls (e.g., inert materials, sham operations) according to standardized surgical procedures.
2. In-Life Monitoring:
- Clinical Observation: Monitor animals daily for signs of pain, distress, or infection.
- Radiological Analysis: Conduct periodic X-ray or MRI scans to observe implant position, surrounding bone structure (for orthopedic implants), and gross tissue changes [48] [49].
- Biochemical Analysis: Collect blood at endpoint (e.g., 26 weeks) to measure key enzymes and metabolites indicating systemic health and organ function (e.g., urea, creatinine, alkaline phosphatase, total protein) [48].
3. Terminal Analysis:
- Histopathological Assessment: After euthanasia, explant the implant with surrounding tissue and vital organs (e.g., heart, liver, spleen, brain).
- Process tissue samples for histological sectioning and staining (e.g., H&E).
- A pathologist, blinded to the experimental groups, should score the tissues for inflammation, fibrosis, necrosis, and other abnormalities, comparing test articles to controls [48] [49].
Real-time Water Permeation Monitoring Workflow
Research Reagent Solutions: Essential Materials for Encapsulation Studies
| Research Reagent | Function / Application | Key Characteristics |
|---|---|---|
| Nanofibrillated Cellulose (NFC) [49] | Biocompatible, plant-based bulking agent or scaffold. | Renewable, does not degrade in vivo (lacks cellulase), supports cell growth, promotes wound healing. |
| Oil-Infused Elastomer [1] | Liquid-based encapsulation for extreme pH environments. | High optical transparency, stretchability, superior water/ion barrier in pH 1.5-9.0. Typically uses Krytox oil infused into roughened PDMS. |
| Magnesium (Mg) Thin Films [19] | Active sensing element for water permeation. | Corrodes predictably in presence of water to Mg(OH)₂; resistance change is wirelessly monitored to calculate WTR. |
| Polydimethylsiloxane (PDMS) [1] | Base elastomer for flexible encapsulation and substrates. | Biocompatible, stretchable, tunable mechanical properties to match soft tissues. |
| Parylene C [1] [19] | Conventional thin-film polymer coating for insulation and moisture barrier. | Good biocompatibility and conformal coating ability, but can fail in extreme pH and is relatively stiff. |
| Polyimide (PI) [1] [19] | Flexible substrate for microfabricated devices and sensors. | High thermal stability, good mechanical strength, and flexibility, suitable for thin-film electronics. |
Implant Failure Modes and Solutions
Frequently Asked Questions (FAQs)
1. What are the key metrics for benchmarking permeability data across different experimental methods? The core metric for quantifying water permeation is the Water Vapor Transmission Rate (WVTR or WTR). It is defined as the mass of water permeated through the barrier per unit area per unit time, typically expressed in g/m²/day. For bioelectronic implants to achieve long-term stability, encapsulation barriers require very low WTR values (≤ 10⁻⁴ g/m²/day) [19].
2. My in silico and in vitro permeability results do not align. What are the first things I should check? Begin by verifying the consistency of your units and experimental conditions. Ensure that the in vitro assay design (e.g., cell culture geometry, temperature, pH) accurately reflects the biological context being modeled in silico. Inconsistencies here are a common source of discrepancy [50].
3. What is the most common cause of failure for flexible thin-film encapsulations in chronic implants? The primary failure mechanism is the permeation of water molecules through the encapsulation. This ingress can lead to device short-circuits, corrosion of metal components, and delamination of the thin films, ultimately causing device failure [19].
4. How can I validate the accuracy of my data pipeline when comparing large permeability datasets? Implement a series of data validation tests. These should include uniqueness checks to ensure no duplicate entries, range checking to verify values fall within plausible limits (e.g., positive permeability values), and consistency checking to confirm logical relationships between related data fields [51] [52].
5. We have a new dataset. What is a quick way to check its basic validity before full benchmarking? Perform data profiling and a smoke test. Data profiling examines the dataset's structure, content, and inter-table relationships for obvious errors. A smoke test involves running your analysis on a small, representative sample of the data to spot easy-to-catch inconsistencies before processing the entire dataset [52].
Troubleshooting Guides
Guide 1: Troubleshooting Discrepancies Between Computational and Experimental Permeability Values
Problem Statement: In silico permeability predictions consistently differ from in vitro experimental measurements.
| Probable Cause | Diagnostic Steps | Resolution |
|---|---|---|
| Incorrect Model Parameters | Verify force field parameters and solute charges used in the simulation against established literature [50]. | Re-run simulations with corrected, community-vetted parameters. |
| Mismatched Experimental Conditions | Audit in vitro conditions (pH, temperature, buffer composition) and ensure they match the physiological state modeled in silico [50]. | Align experimental protocols with in vivo conditions or adjust computational model to match in vitro setup. |
| Limitations of the in vitro Assay | Compare your 2D cell culture model to more complex 3D models or in vivo data to identify system-specific biases [50]. | Use a more physiologically relevant assay or acknowledge the limitation in your benchmarking conclusions. |
Guide 2: Troubleshooting High Variation in Replicated Permeability Measurements
Problem Statement: Measured WTR values show unacceptably high variation across technical or biological replicates.
| Probable Cause | Diagnostic Steps | Resolution |
|---|---|---|
| Inconsistent Sample Preparation | Review fabrication logs for variations in thin-film deposition parameters (e.g., temperature, pressure, deposition rate) [19]. | Establish and adhere to a standardized, documented fabrication protocol. |
| Sensor/Assay Contamination | Inspect sensors under microscopy for surface defects or impurities. Run a control with a known, stable barrier material [19]. | Implement stricter cleanroom protocols and quality control checks post-fabrication. |
| Environmental Fluctuations | Monitor and log laboratory environmental conditions (temperature, humidity) during testing for correlation with WTR results [19]. | Perform experiments in a climate-controlled environmental chamber to stabilize conditions. |
Experimental Protocols & Data
Detailed Methodology: Real-Time WTR Monitoring Using Mg Sensors
This protocol describes a method for in-situ, real-time monitoring of water permeation across thin-film encapsulations using magnesium-based microsensors [19].
Principle: A thin Mg film acts as a resistive sensor. Water permeation through the encapsulation corrodes the Mg, converting it to Mg(OH)₂ and increasing its electrical resistance. This resistance change is wirelessly tracked via a backscatter communication system and correlated to WTR [19].
Workflow Diagram:
Key Materials (Research Reagent Solutions):
| Material/Component | Function in the Experiment |
|---|---|
| Polyimide (PI) Substrate | Serves as the flexible, biocompatible base for building the sensor and encapsulation layers [19]. |
| Magnesium (Mg) Thin Film | Acts as the water-sensitive resistive element. Its corrosion is the core transduction mechanism [19]. |
| Titanium (Ti) Adhesion Layer | A thin layer deposited before Mg to ensure it adheres properly to the PI substrate [19]. |
| Atomic Layer Deposited (ALD) Oxides | (e.g., Al₂O₃). Used as inorganic layers in high-performance hybrid thin-film encapsulations to block water permeation [19]. |
| Phosphate Buffered Saline (PBS) | A standard solution used for in vitro testing to simulate the ionic and pH conditions of the physiological environment [19]. |
| Backscatter Communication Circuit | Enables wireless, battery-free operation by modulating an external RF carrier wave to transmit sensor data [19]. |
Table 1: Comparison of Bioelectronic Encapsulation Barrier Properties
| Barrier Material/Type | Typical Thickness | Target WTR (g/m²/day) | Key Advantages | Key Challenges |
|---|---|---|---|---|
| Atomic Layer Deposited (ALD) Al₂O₃ | < 100 nm | ≤ 10⁻⁴ | Excellent intrinsic barrier properties, conformal coatings. | Can have micro-defects; brittle under strain [19]. |
| Polyimide (PI) | ~5 µm | ~10⁻² - 10⁻¹ | Good flexibility, established microfabrication use. | Relatively high permeability on its own [19]. |
| Parylene C | ~5-20 µm | ~10⁻² | Biocompatible, excellent conformality and dielectric properties. | Moderate barrier property, requires thick layers [19]. |
| Multilayer (Organic/Inorganic Hybrid) | < 5 µm | ≤ 10⁻⁴ | Superior barrier by decoupling defects in layers, good flexibility. | Complex and costly fabrication process [19]. |
Table 2: Data Validation Checks for Permeability Datasets
| Validation Technique | Application in Permeability Benchmarking | Example SQL Test Snippet (Conceptual) |
|---|---|---|
| Range Checking | Ensures WTR values are physically plausible (e.g., positive and within detection limits). | SELECT * FROM permeability_data WHERE wtr_value <= 0; |
| Type Checking | Confirms that data fields contain the expected format (e.g., numeric values, correct date formats). | SELECT * FROM experiment_log WHERE NOT is_date(experiment_date); |
| Uniqueness Checking | Ensures each sample or experiment ID is unique to prevent duplicate data. | SELECT sample_id, COUNT(*) FROM samples GROUP BY sample_id HAVING COUNT(*) > 1; |
| Consistency Checking | Validates relationships between fields (e.g., a higher corrosion rate should correlate with a higher measured WTR). | SELECT * FROM sensor_data WHERE corrosion_rate_high AND wtr_value_low; |
Data Comparison Workflow
The following diagram outlines a systematic process for comparing permeability data from different sources (in silico, in vitro, in vivo) to ensure valid and reliable benchmarking conclusions [50] [19] [52].
Conclusion
The successful prevention of water permeation is the cornerstone of reliable and long-lasting bioelectronic medicine. The shift toward soft, flexible, and liquid-based encapsulation strategies, such as oil-infused elastomers, represents a paradigm shift, enabling robust operation across the body's diverse and challenging environments. These advances in material science, coupled with systematic troubleshooting and rigorous, standardized validation, are paving the way for a new generation of bioelectronics. Future progress hinges on developing even more sophisticated bio-integrated materials, establishing universal benchmarking standards, and accelerating the clinical translation of these durable devices to fulfill their potential in treating chronic neurological, cardiovascular, and metabolic disorders.
References
- 1. Liquid-based encapsulation for implantable bioelectronics ... [https://www.nature.com/articles/s41467-025-55992-x]
- 2. Flexible fluid-based encapsulation platform for water- ... [https://pubmed.ncbi.nlm.nih.gov/37579173/]
- 3. Researchers develop novel encapsulation platform for ... [https://www.perovskite-info.com/researchers-develop-novel-encapsulation-platform-water-sensitive-materials]
- 4. Bioelectronic cell-based device provides a strategy for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9733677/]
- 5. Predicting Corrosion Delamination Failure in Active ... [https://www.mdpi.com/2306-5354/9/1/10]
- 6. Ultra‐Thin Flexible Encapsulating Materials for Soft Bio‐ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9596833/]
- 7. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 8. Overcoming failure: improving acceptance and success of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00168-7]
- 9. Recent advances in nonbiofouling PDMS surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5501164/]
- 10. Water in Epoxy Coatings: Basic Principles of Interaction ... [https://www.mdpi.com/2079-6412/14/1/54]
- 11. Effects of different environmental conditions on the ... [https://www.sciencedirect.com/science/article/pii/S1359836815006666]
- 12. Thermal Analysis of Parylene Thin Films for Barrier Layer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9527014/]
- 13. Silicone rubber and its vapour permeability [https://www.versaperm.com/materials/Silicone%20and%20vapour%20permeability.php]
- 14. How Your Climate Can Affect Your Epoxy Flooring [https://www.perthepoxyflooring.com.au/how-your-climate-can-affect-your-epoxy-flooring-2/]
- 15. Why Aren't All My Electronics Waterproof? [https://vsiparylene.com/resources/parylene-electronics-waterproof/]
- 16. Nylon Membrane Filters, 5.0 Micron, 293mm, 25/Pk [https://www.sterlitech.com/nylon-membrane-filter-ny5029325.html?srsltid=AfmBOornGAKe2G0qd4-J53EZ_42ZXvsxZmtkzxn8M1NmiRhIdsafjtB2]
- 17. Reliability and stability of Bioelectronic Medicine: a critical and... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00179-4]
- 18. Wireless, battery-free, and real-time monitoring of water ... permeation [https://www.nature.com/articles/s41467-024-51247-3?error=cookies_not_supported]
- 19. Wireless, battery-free, and real-time monitoring of water ... [https://www.nature.com/articles/s41467-024-51247-3]
- 20. Liquid-Based Encapsulation for Implantable Bioelectronics ... [https://www.mrs.org/meetings-events/annual-meetings/archive/meeting/presentations/view/2024-fall-meeting/2024-fall-meeting-4152681]
- 21. Liquid-based encapsulation for implantable bioelectronics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11762702/]
- 22. What to Do When Laser Cutter Not Cutting Through? [https://www.1laser.com/blogs/topic/laser-cutter-not-cutting?srsltid=AfmBOooNJPa46YRRFWARjv24Ks1aAd3K3mMhHrKg_eu6rmmSqvZl9zFP]
- 23. Laser Cutting Machine Troubleshooting: A Comprehensive ... [https://www.adhmt.com/laser-cutting-machine-troubleshooting/]
- 24. The Advancement of Waterjet-Guided Laser Cutting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11277706/]
- 25. Surface Optimization Method for Laser Sheet Cutting [https://www.jqlaser.com/surface-optimization-method-for-laser-sheet-cutting/]
- 26. Tips for Improving Edge Quality in Laser Cutting [https://www.vytek.com/blog/news-1/improving-edge-quality-in-laser-cutting-643]
- 27. Best Practice to Cut Carbon Steel with Fiber Laser Cutter [https://www.bodor.com/en/blogs/Optimize-Carbon-Steel-Cutting-Practice.html]
- 28. Integrated implantable bioelectronic system based on ... [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00012-6]
- 29. Failure behavior of polymer microelectrode arrays ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1622927/full]
- 30. The Evolving Role of Interconnect Technologies in HBM [https://ontoinnovation.com/resources/bridging-performance-and-yield-the-evolving-role-of-interconnect-technologies-in-hbm/]
- 31. Thermo-Mechanical Stress On Active Chiplets In A 3D-IC ... [https://semiengineering.com/thermo-mechanical-stress-on-active-chiplets-in-a-3d-ic-heterogeneous-package-assembly/]
- 32. IT Tech | Resolving temperature and humidity issues [https://www.ittech.com.sg/resources/articles/lab-engineering/resolving-temperature-and-humidity-issues]
- 33. – Ensuring Precision in Humidity Testing for... Chamber Environmental [https://www.pacorr.com/blog/humidity-chamber-ensuring-precision-in-environmental-testing-for-industries/]
- 34. How to Investigate Temperature and Humidity Excursions ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/577076-How-to-Investigate-Temperature-and-Humidity-Excursions-of-Stability-Chambers/]
- 35. Considerations, Types, and Applications of Stability Chambers [https://www.iqsdirectory.com/articles/environmental-chamber/stability-chambers.html]
- 36. Stability Chambers: Humidity & Temperature Stability Testing [https://labequipco.com/collections/stability-testing-chambers]
- 37. Development of a Water Transmission Rate (WTR ... [https://www.mdpi.com/2073-4360/15/11/2557]
- 38. The Use of Temperature Humidity in Chamber ... Manufacturing [https://www.testextextile.com/the-use-of-temperature-humidity-chamber-in-manufacturing-product-testing/]
- 39. Environmental Chambers [https://www.fishersci.com/us/en/browse/90088086/environmental-chambers]
- 40. Bioinspired ultra-low fouling coatings on medical devices to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8665144/]
- 41. Protocol to visualize ion channel trafficking in acutely isolated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10783589/]
- 42. Bioinspired Oil-Infused Slippery Surfaces with Water and ... [https://pubmed.ncbi.nlm.nih.gov/34241991/]
- 43. Defect Filling Method of Sensor Encapsulation Based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7915482/]
- 44. What is Parylene Coating and Do You Need It? [https://vsiparylene.com/resources/about-parylene/]
- 45. Softly encapsulated liquid metal grease as high- ... [https://www.sciencedirect.com/science/article/abs/pii/S2468023025009228]
- 46. Implantable bioelectronics toward long-term stability and ... [https://www.sciencedirect.com/science/article/pii/S2590238521000564]
- 47. Long-term in vivo observations show biocompatibility and ... [https://www.sciencedirect.com/science/article/pii/S1742706122007802]
- 48. In Vivo Biocompatibility Study on Functional ... [https://www.mdpi.com/1422-0067/25/8/4249]
- 49. In vivo biocompatibility and long-term durability of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0317859]
- 50. Guidelines for Comparing in Silico, in Vitro, and in Vivo ... [https://pubmed.ncbi.nlm.nih.gov/39823383/]
- 51. 11 Essential Data Validation Techniques [https://www.twilio.com/en-us/resource-center/data-validation-techniques]
- 52. Data Validation Testing: Techniques, Examples, & Tools [https://www.montecarlodata.com/blog-data-validation-testing/]