Strategies for Preventing Inflammation from Bioelectronic Implants: From Material Design to Clinical Management
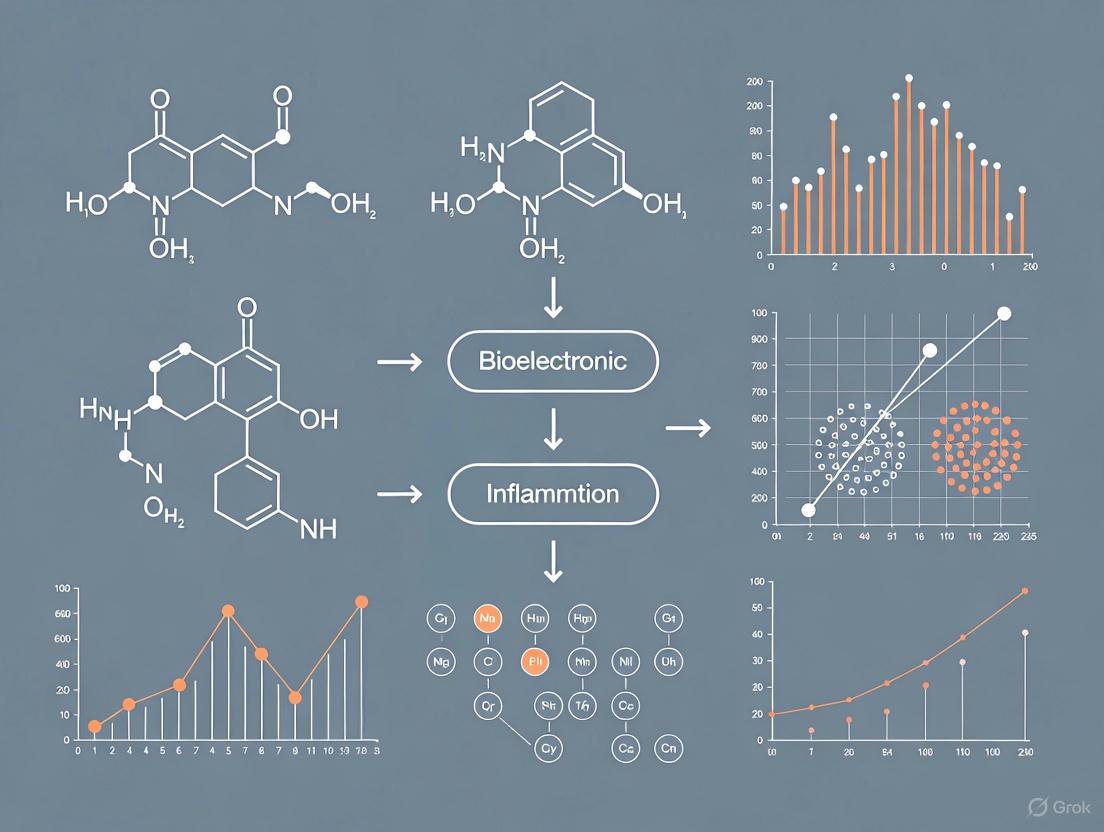
This article provides a comprehensive analysis of strategies to prevent inflammatory responses to bioelectronic implants, a critical challenge limiting their long-term reliability and clinical adoption.
Strategies for Preventing Inflammation from Bioelectronic Implants: From Material Design to Clinical Management
Abstract
This article provides a comprehensive analysis of strategies to prevent inflammatory responses to bioelectronic implants, a critical challenge limiting their long-term reliability and clinical adoption. Targeting researchers, scientists, and drug development professionals, it explores the foundational biology of the Foreign Body Response (FBR), methodological advances in soft materials and device design, troubleshooting for existing failure modes, and validation through preclinical and clinical evidence. The scope spans from fundamental mechanisms and emerging material science—including soft electronics, bioactive interfaces, and novel paradigms like 'Circulatronics'—to practical optimization of implant systems and a forward-looking perspective on closed-loop, intelligent therapeutic platforms.
Understanding the Inflammatory Foe: The Biological Basis of the Foreign Body Response to Implants
The Foreign Body Response (FBR) is a universal immunological process that mammalian hosts initiate against implanted biomaterials, leading to the biological encapsulation of the implant [1]. This reaction presents a fundamental challenge in biomedical research, particularly for the performance and durability of implantable devices such as bioelectronic medicines [2]. When an object is implanted, the body's immune system does not recognize it as "self," activating complex signaling cascades designed to wall off and isolate the foreign material [1] [3]. This process can compromise device function by forming a thick fibrotic capsule that disrupts biosensing functions, causes patient discomfort, cuts off nourishment for cell-based implants, and ultimately leads to device failure [2]. Understanding and mitigating the FBR is therefore critical for advancing bioelectronic implants and other medical technologies.
The FBR Cascade: A Step-by-Step Breakdown
The Foreign Body Response is a coordinated sequence of immune events. The table below summarizes the key phases, their timelines, and the primary cellular players involved.
Table 1: The Temporal Progression of the Foreign Body Response
| Phase | Time Post-Implantation | Key Cells Involved | Major Events |
|---|---|---|---|
| Protein Adsorption | Seconds to Minutes | Plasma Proteins (Fibrinogen, Fibronectin) | Non-specific protein adsorption on the implant surface [2] |
| Acute Inflammation | Hours to Days | Neutrophils, Monocytes/Macrophages | Neutrophil infiltration and degranulation; Monocyte recruitment and differentiation into macrophages [2] [4] |
| Chronic Inflammation & FBGC Formation | Days to Weeks | Macrophages, Foreign Body Giant Cells (FBGC) | Macrophage fusion into FBGCs; Secretion of pro-inflammatory cytokines (TNF-α, IL-1β) [2] [4] |
| Fibrosis & Encapsulation | Weeks to Months | Fibroblasts, Myofibroblasts | Collagen deposition; Formation of a fibrous capsule walling off the implant [2] [4] [3] |
Initial Protein Adsorption and Acute Inflammation
Immediately following implantation, non-specific protein adsorption occurs on the material's surface [2]. The composition of this protein layer is influenced by the biomaterial's properties and dictates subsequent immune recognition [2]. Fibrinogen is a prominently adsorbed protein that promotes inflammation by interacting with Mac-1 integrin on immune cells [2]. Within hours, the body mobilizes neutrophils, which are the primary cell type at the site for the first two days [2]. Neutrophils attempt to phagocytose the implant and release reactive oxygen species and proteolytic enzymes, which can cause damage to the implant itself [2].
Chronic Inflammation and Foreign Body Giant Cell Formation
As the response progresses, monocytes infiltrate the site and differentiate into macrophages [2]. These activated macrophages attempt to engulf the foreign material. When they cannot eliminate the large object, they fuse together to form Foreign Body Giant Cells (FBGCs), which can contain dozens of nuclei [2]. This chronic phase is characterized by high concentrations of pro-inflammatory cytokines, including Tumor Necrosis Factor-alpha (TNF-α) and Interleukin-1 beta (IL-1β), which perpetuate the inflammatory state and initiate downstream signaling pathways such as NF-κB and JNK [2] [4]. Single-cell RNA sequencing has identified specific FBR-enriched macrophage subclusters that highly express these pro-fibrotic and pro-inflammatory mediators [3].
Fibrous Capsule Formation
The final and most detrimental stage for device functionality is fibrosis. Starting around day 7-14 post-implantation, fibroblasts appear in significant numbers and are activated to become myofibroblasts [2] [4]. These cells deposit dense collagen and other extracellular matrix components, eventually forming a avascular, fibrous capsule that completely walls off the implant from the surrounding tissue [2] [4] [3]. In studies, this capsule becomes clearly visible by day 14, with collagen deposition peaking and remaining substantial until at least day 90 [4]. Single-cell analyses have identified specific subpopulations of fibroblasts, such as Pi16+ and Mmp3+ fibroblasts, that are enriched in FBR conditions and demonstrate significant activity in the pro-fibrotic TGF-β signaling pathway [3].
The following diagram illustrates the key cellular events and signaling pathways in the FBR cascade:
Troubleshooting Common FBR Experimental Issues
Frequently Asked Questions
Q: What are the primary immune cell types I should focus on when analyzing the FBR?
- A: Macrophages and fibroblasts are the two predominant cell types driving the response [3]. Macrophages are key for chronic inflammation and FBGC formation, while fibroblasts are responsible for the final fibrous encapsulation [2]. Single-cell RNA sequencing has further refined this, identifying specific pro-fibrotic subpopulations of both cell types [3].
Q: Why is my implant failing despite using a biocompatible material?
- A: The FBR is a universal process that occurs even to materials considered "biocompatible." The key is not necessarily to prevent the response entirely, but to modulate its intensity and outcome [1] [2]. The formation of a thick, avascular fibrous capsule is often the root cause of device failure, as it isolates the implant and can disrupt its function [2].
Q: How can I experimentally reduce the fibrotic capsule around my implant?
- A: Research indicates that targeting macrophage recruitment and activation is highly effective. Studies show that macrophage depletion can almost entirely prevent fibrosis [2]. Furthermore, disrupting specific pathways like Mac-1 integrin (which binds to adsorbed fibrinogen) or using anti-fouling polymers to minimize protein adsorption can significantly reduce capsule thickness [1] [2].
Q: I am working with a biodegradable polymer. How does degradation affect the FBR?
- A: The erosion and degradation behavior of polymers profoundly influences the FBR [1]. Degradation byproducts can create a sustained inflammatory stimulus, potentially leading to a more severe and prolonged FBR compared to non-degradable materials. It is critical to design polymers with degradation kinetics that do not overwhelm the local tissue's ability to clear the byproducts.
Advanced Experimental Guide: Utilizing Single-Cell RNA Sequencing
Modern techniques like single-cell RNA sequencing (scRNA-seq) allow for unprecedented resolution in dissecting the FBR. The following workflow is based on a recent meta-analysis of mouse FBR studies [3].
Table 2: Key Research Reagents for scRNA-seq Analysis of FBR
| Reagent/Resource | Function/Description | Example from Literature |
|---|---|---|
| Droplet-based scRNA-seq Platform | High-throughput single-cell capture and RNA barcoding. | 10X Genomics Chromium [3] |
| Bioinformatic Integration Tool | Harmonizes multiple datasets to identify universal signatures. | Seurat v5 with Harmony [3] |
| Cell-Cell Communication Analysis | Infers signaling interactions between cell subpopulations. | CellChat [3] |
| FBR Model | In vivo system to generate foreign body reaction tissue. | Subcutaneous silicone implant; Intra-abdominal silk sponge [3] |
Experimental Workflow:
- Model Establishment: Implant your biomaterial of interest in an appropriate animal model (e.g., subcutaneous pocket in mice) [3].
- Tissue Harvest: At predetermined time points (e.g., POD 5, 1 week, 2 weeks, 4 weeks, 6 weeks), explant the FBR tissue, including the implant and the surrounding capsule [3].
- Cell Processing: Dissociate the harvested tissue into a single-cell suspension. It is crucial to optimize the dissociation protocol to maintain cell viability and minimize stress-induced gene expression changes.
- scRNA-seq Library Preparation & Sequencing: Use a platform like 10X Genomics to prepare libraries and sequence them. The meta-analysis by Stanford researchers included data from 27 such mouse samples, totaling 108,826 cells [3].
- Bioinformatic Data Integration and Analysis:
- Integration: Use tools like Seurat to merge and harmonize data from different samples or studies. This corrects for technical batch effects and allows for cross-study comparison [3].
- Clustering & Annotation: Identify distinct cell populations (e.g., macrophages, fibroblasts, T cells) and then perform subcluster analysis to find unique subpopulations within these groups [3].
- Differential Expression: Identify genes that are significantly upregulated in FBR conditions compared to control tissues (e.g., "Surgery Control" or "Tissue Control") [3].
- Pathway & Interaction Analysis: Use gene ontology analysis and tools like CellChat to identify activated signaling pathways (e.g., TGF-β, TNF) and predict key cellular communication networks driving the FBR [3].
The following diagram visualizes this integrated analytical workflow:
Emerging Strategies to Modulate the FBR for Bioelectronic Implants
The ultimate goal in bioelectronics is to achieve seamless integration of the device with neural tissue. The following table summarizes key strategies informed by the FBR cascade.
Table 3: Strategic Approaches to Mitigate the Foreign Body Response
| Strategic Approach | Mechanism of Action | Example in Research |
|---|---|---|
| Material Surface Modification | Minimize initial protein adsorption, the first step of FBR. | Hydrophilic hydrogels in catheters reduce protein adhesion and clotting [5]. |
| Immunomodulatory Design | Actively steer the immune response toward a healing/tolerant phenotype. | Targeting Mac-1 integrin or using anti-fouling polymers to disrupt macrophage adhesion [1] [2]. |
| Mechanical Compliance | Reduce mechanical mismatch between device and tissue to minimize chronic inflammation. | Shift from rigid silicon/metal implants to soft, flexible electronics made from polymers and elastomers [6]. |
| Novel Implantation Techniques | Avoid major surgical trauma and preserve protective biological barriers. | "Circulatronics": microscopic, wireless, cell-guided electronics that self-implant via the bloodstream, crossing the blood-brain barrier without invasive surgery [7]. |
The Shift to Soft Bioelectronics
A major trend is the move away from rigid implants, which cause a significant mechanical mismatch with soft, dynamic tissues, leading to inflammation and fibrosis [6]. Next-generation devices are being fabricated from soft polymers, elastomers, and hydrogels with Young's moduli closer to biological tissues (1 kPa – 1 MPa) and bending stiffness below 10â»â¹ Nm [6]. These materials allow for better conformal contact with tissues, reducing micromotion and the ensuing chronic inflammatory stimulus [6].
Frontier Technology: Self-Implanting Bioelectronics
A revolutionary approach to bypassing the surgical FBR is "circulatronics." Researchers have developed microscopic, wireless electronic devices that are fused with living cells (e.g., monocytes) and injected into the bloodstream [7]. These cell-electronics hybrids use the cells' natural homing capabilities to cross the intact blood-brain barrier and autonomously implant in a target brain region, where they can provide electrical stimulation [7]. Because the electronics are camouflaged by living cells, they evade immune detection and do not trigger a significant FBR, offering a potential future where brain implants do not require invasive surgery [7].
Frequently Asked Questions (FAQs)
Q1: What is fibrotic encapsulation and why is it a major problem for bioelectronic implants? Fibrotic encapsulation is a foreign body reaction where the immune system forms a dense, collagenous scar tissue layer around an implanted device. This capsule acts as an electrical and chemical barrier, physically isolating the implant from the target neural tissue [8]. The consequences are significant: for recording electrodes, it causes signal degradation and a decreasing signal-to-noise ratio over time. For stimulating electrodes, it increases impedance and requires higher currents for effective stimulation, which can lead to tissue damage and reduced device longevity [9] [10].
Q2: What are the primary biological drivers behind this process? The process is driven by a complex immune response. Key players include:
- Macrophages: Immune cells that coordinate the response. Pro-inflammatory (M1) and pro-fibrotic (M2) subtypes are involved [11].
- Myofibroblasts: Activated fibroblasts that deposit excessive collagen, forming the fibrous capsule. Their activation is heavily influenced by mechanical forces and the cytokine TGF-β1 [12] [11].
- TGF-β1 (Transforming Growth Factor Beta 1): A pivotal pro-fibrotic cytokine. Its activation from a latent to an active state is often mechanically triggered by the stiffness mismatch between a rigid implant and soft tissue [12].
Q3: Besides biological factors, what other aspects of an implant can trigger fibrosis? The material and mechanical properties of the implant itself are critical triggers:
- Mechanical Mismatch: A large stiffness difference between a rigid implant (GPa) and soft neural tissue (kPa) generates chronic mechanical stress at the interface, promoting inflammation and fibroblast activation [10] [12].
- Implant-Tissue Interface: Non-adhesive implants that do not form a conformal bond with the tissue create micro-movements and spaces that allow for the infiltration of inflammatory cells, initiating the fibrotic cascade [8] [13].
Q4: What are the most promising new strategies to prevent fibrotic encapsulation? Recent research focuses on addressing the root causes:
- Adhesive Interfaces: Creating implants that form a tight, conformal bond with tissue, which prevents inflammatory cell infiltration and has been shown to prevent observable fibrosis for up to 12 weeks in animal models [8].
- Surface Softening: Using soft materials (∼2 kPa) at the tissue interface to reduce mechanical mismatch and the subsequent force-mediated activation of TGF-β1 and myofibroblasts [12].
- Advanced Encapsulation: Developing 3D barrier coatings, such as Atomic Layer Infiltration (ALI), to protect vulnerable parts of flexible microelectrodes from moisture and ion permeation, thereby delaying device failure [14].
Troubleshooting Guide: Diagnosing and Mitigating Failure Modes
Problem 1: Gradual Degradation of Neural Recording Signal Quality
| Observation | Potential Cause | Diagnostic Experiments | Solution & Prevention |
|---|---|---|---|
| Decreasing signal-to-noise ratio (SNR) over weeks/months. | Fibrotic capsule formation increasing distance between electrodes and neurons [10]. | Histology: Explain tissue to quantify capsule thickness (e.g., Masson's Trichrome stain for collagen). Impedance Spectroscopy: Monitor increases in electrode impedance at low frequencies [9]. | Utilize softer, flexible materials (e.g., polyimide) to minimize mechanical mismatch [10]. Implement adhesive anti-fibrotic interfaces [8]. |
| Complete loss of signal from specific channels. | Individual electrode or interconnect failure due to moisture-induced corrosion [14]. | Leakage Current Testing: Measure under accelerated aging conditions (e.g., 87°C PBS). Visual Inspection: Use microscopy to identify delamination or cracks in encapsulation [14]. | Employ robust sidewall encapsulation strategies like 3D-Atomic Layer Infiltration (3D-ALI) to protect vulnerable areas [14]. |
Problem 2: Rising Impedance and Loss of Stimulation Efficacy
| Observation | Potential Cause | Diagnostic Experiments | Solution & Prevention |
|---|---|---|---|
| Higher voltages required to achieve same therapeutic effect. | Fibrous capsule acting as an insulating layer [9] [8]. | Voltage Transient Measurement: Analyze changes in voltage waveforms during stimulation. Cyclic Voltammetry: Assess charge injection capacity of electrodes [9]. | Apply anti-fibrotic coatings (e.g., drug-eluting with TGF-β inhibitors) [12]. Design devices with smaller footprints and softer mechanics to reduce immune response [10]. |
| Inconsistent stimulation output. | Corrosion or delamination of stimulating electrode or leads [9]. | Continuous Impedance Monitoring: Track changes over time. Electrochemical Impedance Spectroscopy (EIS): Characterize the electrode-tissue interface [14]. | Select stable electrode materials like PtIr or IrOx. Ensure hermetic packaging and feedthroughs for the pulse generator [9]. |
Problem 3: Physical Device Failure or Damage
| Observation | Potential Cause | Diagnostic Experiments | Solution & Prevention |
|---|---|---|---|
| Broken lead wires or interconnects. | Mechanical fatigue from repetitive stress or strain due to body movement [9]. | Micro-CT Scan: Non-destructively inspect for fractures. Failure Analysis: Use SEM/EDS on explanted devices to examine fracture surfaces [9]. | Use stretchable or flexible conductive composites. Design strain-relief features in lead routing. Utilize elastic substrates like silicone [6]. |
| Delamination of thin-film layers. | Poor adhesion between dissimilar materials in a humid environment [14]. | Accelerated Aging Tests: Submerge in saline at elevated temperatures and monitor performance. Interface Toughness Measurement: Use standardized mechanical tests like peel tests [14]. | Implement gradient modulus interfaces like Atomic Layer Infiltration (ALI) to improve adhesion and resist delamination [14]. |
Experimental Protocols for Key Analyses
Protocol 1: Quantifying Fibrotic Capsule Thickness
Objective: To histologically measure the extent of collagenous encapsulation around an explanted device.
Materials:
- Explanted device with surrounding tissue
- 10% Neutral Buffered Formalin
- Paraffin embedding station and microtome
- Masson's Trichrome stain kit
Methodology:
- Fixation: Fix explanted tissue-device construct in formalin for 48 hours.
- Processing & Sectioning: Process tissue through a graded ethanol series, embed in paraffin, and section at 5-10 µm thickness.
- Staining: Perform Masson's Trichrome staining following kit protocol. This stains collagen blue, cytoplasm red, and nuclei dark brown/black.
- Imaging & Analysis: Image sections under a light microscope. Use image analysis software (e.g., ImageJ) to measure the thickness of the blue collagenous capsule at multiple, random locations around the implant interface. Calculate average and standard deviation [8].
Protocol 2: Accelerated Aging Test for Device Encapsulation
Objective: To rapidly assess the long-term reliability of a device's moisture barrier in vitro.
Materials:
- Device Under Test (DUT)
- Phosphate Buffered Saline (PBS), pH 7.4
- Laboratory oven capable of maintaining 87°C
- Electrochemical impedance spectrometer or high-resistance meter
Methodology:
- Baseline Measurement: Record the initial electrical characteristics (e.g., impedance or leakage current) of the DUT.
- Submersion: Submerge multiple DUTs in PBS solution within sealed containers.
- Accelerated Aging: Place containers in an oven at 87°C. This elevated temperature accelerates failure mechanisms, simulating months of implantation in a matter of weeks.
- Monitoring: Periodically remove DUTs, rinse with DI water, dry, and re-measure electrical characteristics. Plot parameters like impedance magnitude versus aging time to identify failure points [14].
Key Signaling Pathways in Fibrosis
This diagram illustrates the core signaling pathways involved in the foreign body response and fibrotic encapsulation, highlighting the critical role of mechanical forces.
Fibrosis Signaling Pathway
Experimental Workflow for Implant Evaluation
The following diagram outlines a comprehensive workflow for evaluating the performance and failure modes of a bioelectronic implant, from in vitro testing to in vivo validation and post-analysis.
Implant Evaluation Workflow
Research Reagent Solutions
The following table details key materials and reagents used in the development and testing of advanced bioelectronic implants, as featured in recent research.
| Reagent/Material | Function/Benefit | Key Application Notes |
|---|---|---|
| Poly(vinyl alcohol)-based Adhesive | Forms a conformal, anti-fibrotic interface that prevents inflammatory cell infiltration and collagen deposition [8]. | Provides stable, long-term adhesion to wet tissues. Compared to commercial adhesives (Coseal, Tisseel), it shows superior prevention of fibrous capsule formation over 12 weeks [8]. |
| Soft Silicone (∼2 kPa) | Surface-modifying layer that reduces mechanical mismatch with soft tissue (∼1 kPa), minimizing pro-fibrotic TGF-β1 activation [12]. | Can be coated onto conventionally stiff silicones (~2 MPa) to significantly reduce collagen deposition and myofibroblast activation without affecting macrophage counts [12]. |
| Atomic Layer Infiltration (ALI) | Creates a gradient modulus hybrid material at the polymer-ceramic interface, resisting delamination and improving encapsulation reliability [14]. | Modifies standard ALD parameters to allow precursors to infiltrate the porous polymer matrix. Key for 3D sidewall encapsulation of freestanding microelectrodes [14]. |
| CWHM-12 Small Molecule Inhibitor | Antagonizes αv integrin binding to the LAP complex, suppressing the mechanical activation of TGF-β1 [12]. | A pharmacological strategy to prevent fibrosis around stiff implants when material softening is not feasible. Effective in murine subcutaneous implant models [12]. |
| In Silico FBR Model | A computational tool using standardized ODEs to predict fibrotic outcomes based on implant properties (stiffness, immunogenicity) [11]. | Bridges in vitro and in vivo studies. Useful for screening implant designs and materials in early R&D, potentially reducing animal testing. Validated against experimental anti-fibrotic interventions [11]. |
Frequently Asked Questions (FAQs)
Q1: What is the "Mechanical Mismatch Problem" in bioelectronic implants? The mechanical mismatch problem refers to the detrimental effects caused by the significant difference in stiffness between traditional, rigid implant materials (like silicon and metals) and the soft, dynamic tissue of the brain. This stiffness discrepancy leads to continuous micromotion at the tissue-implant interface, which can provoke chronic neuroinflammation, scar tissue formation (gliosis), and instability of the blood-brain barrier, ultimately compromising the long-term performance and reliability of the device [15] [16].
Q2: What are the primary biological consequences of this mismatch? The primary consequences are a sustained neuroinflammatory response and instability of the blood-brain barrier. Research shows that stiff implants trigger a significant increase in the presence of activated immune cells (like microglia and astrocytes) around the implant site. Furthermore, the constant mechanical agitation can disrupt the delicate endothelial cells that form the blood-brain barrier, leading to increased permeability and potential further damage to neural tissue [15].
Q3: Are there innovative material strategies to overcome this problem? Yes, two prominent advanced strategies are:
- Mechanically-Adaptive Materials: These materials are rigid during surgical implantation for ease of handling but become soft and compliant after being exposed to the physiological conditions of the body, thereby minimizing the mechanical mismatch [15].
- Ultra-Soft & Flexible Bioelectronics: This approach involves using inherently soft, flexible, and stretchable materials from the outset. Recent developments include subcellular-sized, wireless electronic devices that can be non-surgically delivered, often integrated with living cells to create compliant hybrids that seamlessly interface with neural tissue [7] [16] [17].
Q4: How can I quantitatively evaluate the success of a compliant implant in my experiment? Success is evaluated through a combination of quantitative histological analysis and functional testing. Key metrics include quantifying the density of immune cells (e.g., microglia and astrocytes) at the implant interface, assessing blood-brain barrier integrity, and measuring the electrical impedance of the implant-tissue interface over time. Compliant implants should show a statistically significant reduction in these inflammatory markers and more stable electrical properties compared to stiff controls [15].
Troubleshooting Guides
Problem: Chronic Neuroinflammatory Response Observed Around Implant
Potential Cause: The mechanical stiffness (Young's modulus) of your implant is too high compared to the surrounding brain tissue, causing persistent micromotion and tissue strain.
Solutions:
- Action 1: Switch to a compliant material system. Consider using mechanically-adaptive polymers or soft elastomers that closely match the brain's modulus (in the kilopascal range).
- Action 2: Implement a flexible form factor. Design implants with ultra-thin and porous geometries that can bend and flex with the brain tissue.
- Action 3: Validate with long-term studies. Ensure that your material remains compliant and stable over the entire planned duration of your experiment, as some materials may degrade or stiffen.
Problem: Unstable Electrical Recordings or Stimulation Efficacy Over Time
Potential Cause: The inflammatory response and subsequent formation of an insulating glial scar around a rigid implant increases the distance between the electrode and viable neurons, raising impedance and reducing signal quality.
Solutions:
- Action 1: Characterize the interface impedance. Regularly measure electrochemical impedance spectroscopy (EIS) to monitor the health of the electrode-tissue interface.
- Action 2: Prioritize biocompatibility and compliance. Use materials that minimize the foreign body response. Softer implants have been shown to develop a much thinner and less dense glial scar, preserving signal fidelity [15] [16].
- Action 3: Consider a non-surgical approach. For specific applications, novel methods like "Circulatronics"—where cell-borne electronic devices are injected and travel to the target site—can eliminate surgical trauma and the associated inflammatory cascade entirely [7] [17].
Key Experimental Data & Protocols
The table below summarizes key experimental data demonstrating the impact of implant stiffness on biological responses.
Table 1: Comparative Effects of Stiff vs. Compliant Intracortical Implants
| Parameter | Stiff Implants | Compliant Implants | Significance & Notes |
|---|---|---|---|
| Neuroinflammatory Response (Chronic) | Significantly Increased [15] | Significantly Reduced [15] | Measured at 2, 8, and 16 weeks post-implantation. |
| Blood-Brain Barrier (BBB) Stability | Unstable [15] | More Stable [15] | Critical for preventing further neural damage. |
| Tissue Strain & Micromotion | High [16] | Low [16] | Driven by mechanical mismatch with soft brain tissue. |
| Typical Material Stiffness | GPa range (e.g., Silicon) [16] | kPa-MPa range (e.g., adaptive polymers) [15] [16] | Brain tissue stiffness is in the kPa range. |
| Long-term Recording/Stimulation Stability | Often Degrades [16] | Improved [15] [16] | Linked to reduced glial scarring. |
Experimental Protocol: Evaluating the Neuroinflammatory Response to Implants
Objective: To quantitatively assess the chronic neuroinflammatory response to an intracortical implant with different mechanical properties.
Materials:
- Test implants (stiff control vs. compliant material).
- Animal model (e.g., rat cortex).
- Perfusion and fixation equipment.
- Primary antibodies: Anti-Iba1 (for microglia), Anti-GFAP (for astrocytes).
- Fluorescently-labeled secondary antibodies.
- Confocal microscope.
Method:
- Implantation: Surgically implant the stiff and compliant devices into the target brain region (e.g., rat cortex) following sterile procedures and approved animal protocols.
- Survival Time: Allow animals to survive for the desired chronic time points (e.g., 2 weeks, 8 weeks, 16 weeks) to observe long-term tissue responses [15].
- Perfusion and Tissue Sectioning: At the endpoint, transcardially perfuse the animals with paraformaldehyde. Extract the brains, post-fix, and section them into coronal slices containing the implant site.
- Immunohistochemistry: Label the tissue sections using standard IHC protocols. Incubate slices with primary antibodies (Iba1, GFAP) overnight, followed by appropriate secondary antibodies.
- Imaging and Quantification: Capture high-resolution images of the tissue surrounding the implant using a confocal microscope. Quantify the inflammatory response by measuring:
- The density of Iba1-positive microglia within a defined radius (e.g., 100 µm) from the implant interface.
- The intensity and extent of GFAP-positive astrocytic scarring.
- Statistical Analysis: Perform statistical tests (e.g., t-test, ANOVA) to compare the quantified metrics between the stiff and compliant implant groups. A successful compliant implant will show a statistically significant reduction in both microglial activation and astrocytic scarring.
The Inflammatory Cascade Caused by Mechanical Mismatch
The following diagram illustrates the key signaling pathway and biological sequence of events triggered by a rigid implant.
Mechanism of Implant-Induced Inflammation
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Investigating Compliant Neural Implants
| Reagent / Material | Function / Description | Key Consideration |
|---|---|---|
| Mechanically-Adaptive Polymers | Initially rigid for implantation, become compliant in vivo to reduce mismatch [15]. | Verify the activation time and final modulus match your experimental needs. |
| Soft Elastomers (e.g., PDMS) | Model compliant materials with tunable Young's modulus for in vitro and in vivo testing. | Biocompatibility grades and surface modifications are crucial for integration. |
| Recombinant Human Collagen (rhCol) | Bioactive coating to enhance cell adhesion and integration on synthetic polymer scaffolds [18]. | Xeno-free and avoids immune reactions associated with animal-derived collagen. |
| Primary Antibodies (Iba1, GFAP) | Key immunohistochemical markers for quantifying microglial and astrocytic response. | Optimize dilution and staining protocols for your specific tissue model. |
| Subcellular-Sized Wireless Electronic Devices (SWEDs) | Enable non-surgical implantation and ultra-focal neuromodulation, bypassing surgical trauma [17]. | Requires development of cell-hybrid systems for targeting and wireless powering. |
| NS2 (114-121), Influenza | NS2 (114-121), Influenza, MF:C48H74N12O12, MW:1011.2 g/mol | Chemical Reagent |
| Fmoc-Ser(PO(NHPr)2)-OH | Fmoc-Ser(PO(NHPr)2)-OH, MF:C24H32N3O6P, MW:489.5 g/mol | Chemical Reagent |
Frequently Asked Questions (FAQs)
Q1: What are the primary biological challenges causing bioelectronic implant failure? The primary challenges are biofouling, the Foreign Body Response (FBR), and microbial colonization. Biofouling is the spontaneous accumulation of proteins, cells, and bacteria on the implant surface [19]. This triggers the FBR, a complex immune response that often results in the formation of a fibrous capsule, isolating the device and leading to failure [20] [19]. Microbial colonization can lead to biofilm formation, where communities of bacteria become highly resistant to antibiotics and the host immune system, causing persistent infections [21].
Q2: Why are biofilms on medical devices particularly problematic? Bacteria in a biofilm state can be 500 to 5,000 times more resistant to antibiotics than their free-floating counterparts [21]. The biofilm matrix acts as a physical barrier that prevents antibiotics from reaching the bacterial cells and facilitates the exchange of antimicrobial-resistant genes [21]. This leads to recalcitrant, chronic infections that are very difficult to eradicate without removing the device.
Q3: How does the surface property of an implant influence biofilm formation? The chemical composition and physical morphology of an implant's surface play a crucial role in bacterial adhesion and biofilm formation [21]. A conditioning film of host proteins and other organic molecules forms almost immediately on the implant after placement, which bacteria use as a nutrient source for initial attachment and growth [21].
Q4: What is the difference between reliability and stability in bioelectronic implants?
- Reliability is the probability that a device will function as intended without failure over a specified period. It is measured by metrics like mean time between failures (MTBF) [16] [6].
- Stability refers to the device's ability to maintain its functional and structural properties over time, with minimal drift in performance, despite environmental and biological fluctuations [16] [6].
Troubleshooting Guide: Common Experimental Challenges
Problem 1: Rapid Signal Degradation in Chronic Animal Studies
Potential Cause: Fibrous encapsulation of the implant due to the Foreign Body Response (FBR), blocking analyte diffusion or altering electrical properties [19]. Solutions:
- Consider Soft Materials: Shift from rigid (silicon, metal) to soft, flexible materials (polymers, elastomers) that better match tissue mechanics and reduce inflammatory response [16] [6].
- Apply Anti-fouling Coatings: Use coatings such as zwitterionic polymers, polyethylene glycol (PEG), or biomimetic slippery liquid-infused porous surfaces (SLIPS) to prevent protein and cell adhesion [19] [22] [23].
Problem 2: Bacterial Contamination and Biofilm Formation on Explanted Devices
Potential Cause: Ineffective anti-biofouling strategy or surface defects that act as nucleation sites for bacterial attachment [21] [22]. Solutions:
- Implement Nature-Inspired Coatings: Develop surfaces with nanoscale topographies inspired by cicada wings (bactericidal) or shark skin (anti-adhesive) to physically prevent colonization [23].
- Use Biocidal Release Coatings: Incorporate and test coatings that elute antibiotics or silver ions; however, be aware of finite reservoir life and potential for antibiotic resistance [21] [19].
Problem 3: Inconsistent In Vitro to In Vivo Translation of Anti-fouling Strategies
Potential Cause: Static in vitro tests may not replicate the dynamic, complex immune and microbial environment in a living organism [21] [19]. Solutions:
- Refine In Vitro Models: Incorporate dynamic flow conditions and complex protein solutions to better simulate the in vivo environment [21].
- Conduct Early Pilot In Vivo Studies: Perform short-term animal studies to quickly assess the host response and coating stability before committing to long-term chronic studies [22].
Key Experimental Protocols
Protocol 1: Evaluating Anti-biofouling Coatings Using an In Vitro Bacterial Adhesion Assay
Objective: To quantitatively compare the ability of different surface modifications to resist bacterial colonization. Materials:
- Coated and uncoated implant material samples.
- Bacterial culture (e.g., Staphylococcus aureus or S. epidermidis).
- Standard growth broth and agar plates.
- Phosphate Buffered Saline (PBS).
- Fluorescence microscope and DNA-binding stain (e.g., SYTO 9).
Methodology:
- Sample Preparation: Sterilize all test samples (e.g., via UV irradiation or ethanol wash).
- Bacterial Inoculation: Immerse samples in a bacterial suspension of a standardized concentration (e.g., 10^7 CFU/mL) and incubate under gentle agitation for a set period (e.g., 2-24 hours).
- Rinsing: Gently rinse samples with PBS to remove non-adhered planktonic bacteria.
- Fixation and Staining: Fix adhered bacteria and stain with a fluorescent DNA dye.
- Quantification: Image multiple fields of view per sample using fluorescence microscopy and use image analysis software to count the number of adhered bacteria per unit area. Alternatively, detach bacteria by sonication and perform serial dilution plating to determine Colony Forming Units (CFU).
Protocol 2: Assessing the Foreign Body Response (FBR) and Biofilm Formation In Vivo
Objective: To evaluate the long-term biocompatibility and infection resistance of an implant coating in a rodent model. Materials:
- Test and control implant materials.
- Animal model (e.g., mouse or rat).
- Surgical equipment and anesthetic.
- Histology reagents: formalin, paraffin, Hematoxylin and Eosin (H&E) stain, Masson's Trichrome stain.
- Equipment for bacterial quantification: homogenizer, agar plates.
Methodology:
- Implantation: Surgically implant material samples subcutaneously or at the relevant anatomical site under aseptic conditions. For infection challenge models, introduce a known quantity of bacteria at the time of implantation.
- Explanation: After a predetermined period (e.g., 1, 4, or 12 weeks), euthanize the animals and explant the devices with surrounding tissue.
- Analysis:
- Microbial Load: Homogenize the explanted device and a portion of the surrounding tissue. Plate the homogenate on agar to quantify viable bacteria (CFU).
- Histological Analysis: Fix the tissue in formalin, embed in paraffin, section, and stain.
- H&E Staining: Assess general tissue architecture and inflammatory cell infiltration.
- Masson's Trichrome Staining: Visualize collagen deposition and quantify the thickness of the fibrous capsule forming around the implant.
Table 1: Comparison of Advanced Anti-Biofouling and Anti-Biofilm Surface Strategies
| Strategy | Mechanism of Action | Key Advantages | Potential Limitations |
|---|---|---|---|
| SLIPS (Slippery Liquid-Infused Porous Surfaces) [22] | Creates a dynamic, immobilized liquid interface that prevents bacterial adhesion and is self-healing. | Broad-spectrum anti-adhesion; protects against a wide range of contaminants and bacteria. | Long-term stability of the lubricant layer in vivo; requires a compatible porous substrate. |
| Biomimetic Nanotopographies [23] | Physically ruptures bacterial membranes using nanoscale sharp features inspired by insect wings. | Non-chemical, avoids antibiotic resistance; long-lasting physical effect. | Complex fabrication; potential for clogging or damage to nanostructures. |
| Zwitterionic & Hydrophilic Polymer Brushes [19] [23] | Forms a hydration layer via strong electrostatic interactions, creating a physical and energetic barrier to protein adsorption. | Highly effective against non-specific protein fouling; can be chemically tuned. | Long-term stability and susceptibility to oxidative degradation in vivo. |
| Controlled Biocidal Release [21] [19] | Locally elutes antibiotics or antimicrobial agents (e.g., silver ions) to kill approaching bacteria. | Highly effective in the short term. | Finite reservoir leads to limited functional lifetime; promotes antimicrobial resistance. |
| Electroceutical Therapy [24] | Uses programmable electrical stimulation to disrupt bacterial communication (quorum sensing) and prevent biofilm formation. | Drug-free approach; can be tailored and activated on demand. | Emerging technology; long-term effects and optimal parameters still under investigation. |
Table 2: Quantitative Results from Key Anti-Biofouling Studies
| Study & Strategy | Experimental Model | Key Quantitative Outcome | Reference |
|---|---|---|---|
| SLIPS-coated ePTFE | In vivo rodent model challenged with S. aureus | ~85% reduction in bacterial colonization on explanted devices compared to controls. | [22] |
| Electroceutical Patch | Preclinical test on pig skin | Achieved nearly a tenfold (10x) reduction in bacterial colonization. | [24] |
| Computational Model of Biocide-Releasing Surface | In silico simulation of marine biofilm formation | Predicted that the time to biofilm establishment depends exponentially on the surface biocide concentration and the arrival rate of resistant organisms. | [25] |
Visualization of Key Concepts
Biofilm Development Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Investigating the Tissue-Device Interface
| Reagent / Material | Function in Research | Specific Example / Note |
|---|---|---|
| Zwitterionic Polymers | Create highly hydrophilic, anti-fouling surfaces that resist non-specific protein adsorption [19]. | e.g., Poly(sulfobetaine methacrylate) (PSBMA). Used as a coating to minimize the initial conditioning film. |
| Fluorinated Lubricants | Key component for creating SLIPS coatings; provides the dynamic, anti-adhesive liquid layer [22]. | e.g., Perfluoropolyether (PFPE), Perfluoroperhydrophenanthrene (PFPH). Must have high chemical affinity for the substrate. |
| Catechol-Based Polymers | Provide strong, versatile adhesion to various substrates in wet environments, inspired by mussel adhesives [23]. | e.g., Polydopamine. Often used as a primer layer for subsequent functionalization with biomolecules or other polymers. |
| RGD Peptide Sequences | Promote specific cell adhesion and tissue integration by mimicking the extracellular matrix (ECM) [23]. | Coated on implants to improve biocompatibility and reduce the FBR by encouraging host tissue acceptance. |
| Fluorescent DNA Stains | Enable visualization and quantification of adhered bacteria and biofilms on explanted devices or in vitro samples. | e.g., SYTO 9 (for live cells). Critical for confocal microscopy analysis of biofilm structure and biomass. |
| Triamcinolone acetonide-d7-1 | Triamcinolone acetonide-d7-1, MF:C24H31FO6, MW:441.5 g/mol | Chemical Reagent |
| N-Octanoyl-D15-glycine | N-Octanoyl-D15-glycine, MF:C10H19NO3, MW:216.35 g/mol | Chemical Reagent |
Engineering Solutions: Material Innovations and Design Strategies for Bio-integrative Implants
Core Concepts: Why Soft Bioelectronics?
FAQ: Why is the mechanical mismatch between implants and tissue a significant problem?
Traditional bioelectronics are fabricated from rigid materials like metals and silicon. When implanted into soft, dynamic biological tissues, this stiffness difference creates a mechanical mismatch. The body recognizes this rigid interface as a foreign body, initiating a chronic immune response. This typically results in the formation of a fibrotic scar tissue capsule that walls off the device. This encapsulation electrically insulates the implant, severely degrading signal quality and often leading to device failure over time [6] [26].
FAQ: How do soft and flexible materials mitigate the immune response?
Soft bioelectronics, made from polymers, elastomers, and hydrogels, have a Young's modulus much closer to that of natural tissue (typically in the kPa to MPa range). This mechanical compatibility minimizes chronic irritation and micromotion damage as the body moves. Consequently, the foreign body response is significantly reduced, leading to better tissue integration, less fibrotic encapsulation, and more stable long-term performance [6] [16].
Table 1: Quantitative Comparison of Rigid vs. Soft Bioelectronics
| Property | Rigid Bioelectronics | Soft & Flexible Bioelectronics |
|---|---|---|
| Typical Material Types | Silicon, metals, ceramics | Polymers, elastomers, hydrogels, thin-film materials [6] |
| Young's Modulus | > 1 GPa | 1 kPa – 1 MPa [6] |
| Bending Stiffness | > 10â»â¶ N·m | < 10â»â¹ N·m [6] |
| Tissue Integration | Poor; stiffness mismatch causes inflammation and fibrotic encapsulation | Excellent; soft, conformal materials match tissue mechanics and reduce immune response [6] |
| Signal Fidelity | Strong short-term signal quality, but long-term degradation due to scar tissue | Better chronic signal stability due to stable tissue-contact interface [6] |
Troubleshooting Common Experimental Challenges
FAQ: My soft device is delaminating in aqueous biological environments. What are potential solutions?
Delamination is a common failure mode for multilayer soft devices due to water permeation and weak interfacial adhesion.
- Solution A (Encapsulation): Implement advanced encapsulation strategies using ultrathin, flexible barrier layers (e.g., parylene, silicon carbide, or novel polymers) that protect internal components while maintaining overall device flexibility [6] [27].
- Solution B (Material Innovation): Shift towards monolithic devices or use materials with inherent adhesion. For example, conductive hydrogels can be designed to have interpenetrating polymer networks that create a more unified structure, significantly reducing delamination risk [26].
FAQ: I am observing a decline in the conductivity of my flexible conductive traces under repeated strain. How can I address this?
Conductive materials on soft substrates can suffer from microcracking and fatigue.
- Solution A (Geometric Engineering): Use serpentine or fractal "kirigami/origami" designs for metal traces. These geometries allow the material to stretch and bend without subjecting the conductive metal to excessive tensile strain, thus preventing crack formation [6].
- Solution B (Alternative Conductors): Replace traditional metal films with conductive composites or liquid metals. PEDOT:PSS-based conductive hydrogels or gallium-indium alloys maintain conductivity even under deformation and are a focus of current research [26].
FAQ: My in vivo experiment shows unexpected inflammation despite using a soft substrate. What could be the cause?
While softness reduces the primary mechanical trigger for inflammation, other factors can be at play.
- Diagnostic Steps:
- Check Edge Sharpness: Even a soft device can have microscopically sharp edges that aggravate local tissue.
- Verify Material Purity: Ensure no leachable toxic compounds (e.g., residual solvents or unreacted monomers) are present in your polymer or hydrogel.
- Assess Device Size and Tethering: A very large device or one that is tightly tethered can still cause macro-motion irritation, provoking a response [9].
Experimental Protocols & Characterization
Standardized Protocol for In Vivo Biocompatibility and Stability Assessment
Objective: To quantitatively evaluate the chronic immune response and functional stability of a novel soft bioelectronic implant.
- Implantation: Aseptically implant the device in the target tissue (e.g., subcutaneous, neural) of an animal model. Ensure surgical controls are identical.
- Chronic Monitoring:
- Functional Electrochemistry: Perform electrochemical impedance spectroscopy (EIS) and cyclic voltammetry (CV) weekly at the electrode-tissue interface. A stable or slowly increasing impedance indicates minimal fibrotic growth.
- Biological Sampling: Collect blood serum at predefined intervals (e.g., 1, 4, and 12 weeks) to quantify systemic inflammatory biomarkers (e.g., TNF-α, IL-1β, IL-6) via ELISA.
- Endpoint Analysis:
- Histology: Explain the device and surrounding tissue. Process for H&E staining and immunohistochemistry for specific cell markers (e.g., CD68 for macrophages, α-SMA for fibroblasts).
- Fibrosis Quantification: Measure the thickness of the collagen-rich fibrotic capsule (stained with Masson's Trichrome or Picrosirius Red) using image analysis software. A thinner capsule signifies a superior biocompatible response [9].
Workflow Diagram: From Problem to Solution in Bioelectronics
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials for Developing Soft Bioelectronic Implants
| Material/Reagent | Function | Key Characteristics & Examples |
|---|---|---|
| Conductive Hydrogels (e.g., PEDOT:PSS-based) | Serves as the soft, conductive interface for stimulation/recording. Mimics tissue modulus and supports electronic properties [26]. | Nontoxic additives can be used to dope and enhance performance. Key for fabricating soft microelectronics. |
| Elastomeric Substrates (e.g., PDMS, SEBS) | Provides the flexible and stretchable structural backbone for the device. | Offers low Young's modulus and high stretchability, allowing devices to conform to dynamic tissues. |
| Electrospun Polymer Nanofibers | Creates porous, high-surface-area scaffolds for sensing or tissue integration. | Enables convenient microstructure generation and improved functionalization at low cost [28]. |
| Flexible Encapsulants (e.g., Parylene, Silicone) | Forms a barrier to protect electronic components from ionic body fluid ingress. | Must be thin, flexible, and possess low water vapor transmission rates to ensure long-term stability [6] [27]. |
| Soft Adhesives (e.g., Bio-adhesive Hydrogels) | Allows the device to securely attach to wet, moving tissue surfaces without sutures. | Provides strong, biocomhesive interface while maintaining softness and compliance. |
| 2-Methylthio-AMP diTEA | 2-Methylthio-AMP diTEA, MF:C23H46N7O7PS, MW:595.7 g/mol | Chemical Reagent |
| Curcumin monoglucuronide | Curcumin monoglucuronide, MF:C27H28O12, MW:544.5 g/mol | Chemical Reagent |
Troubleshooting Guides and FAQs
This technical support resource addresses common experimental challenges in developing bioelectronic implants, with a focus on mitigating inflammation through advanced material science.
Conducting Polymers (CPs)
Q1: My PEDOT:PSS film has low conductivity and poor adhesion to the flexible substrate. What can I do?
- Problem: A common issue is the inability to balance high electrical performance with robust mechanical integration.
- Solution: Implement a solvent-mediated solid-liquid interface (SLI) doping strategy to engineer a vertically phase-separated (VPS) structure.
- Protocol:
- Blade Coating: Apply commercial PEDOT:PSS ink onto your substrate to form a pre-oriented pristine film.
- SLI Doping: Shear a metastable liquid-liquid contact (MLLC) doping dispersion (an ethylene glycol-diluted PEDOT:PSS formulation with a reduced PSS/PEDOT ratio) onto the surface of the pristine film.
- Annealing: Anneal the film. This process encourages PSS (hydrophilic) to migrate to the surface, improving adhesion to biological tissues, while PEDOT-rich domains aggregate at the bottom, enhancing crystallinity and conductivity. This VPS structure can achieve conductivities up to ~8800 S cmâ»Â¹ [29].
- Prevention: Precisely control coating speed and solvent evaporation during the SLI process to optimize polymer alignment and phase separation.
Q2: How can I improve the chronic stability of my neural electrode coated with a conductive polymer?
- Problem: The charge-transfer efficiency of the electrode degrades over time, often due to fibrotic encapsulation (gliosis) and mechanical mismatch.
- Solution: Use softer, electrodeposited CP composites that mimic tissue mechanics and can be biofunctionalized.
- Protocol (for Electrodeposited PEDOT/HAp Coatings):
- Solution Preparation: Prepare an aqueous solution containing 0.1 M EDOT monomer and a bioactive dopant, such as 0.5% (w/v) hyaluronic acid (HAp).
- Electrodeposition: Use a standard three-electrode system. Apply a constant current density (e.g., 0.5 mA/cm²) for 100-200 seconds to deposit the PEDOT/HAp film directly onto your metal electrode (working electrode) [30] [31].
- Characterization: Use cyclic voltammetry and electrochemical impedance spectroscopy to verify a lower impedance and higher charge storage capacity compared to bare metal electrodes.
- Rationale: CPs like PEDOT facilitate efficient ionic-electronic charge transfer. Incorporating a bioactive dopant like HAp can improve biocompatibility, reduce the foreign body response, and enhance integration [31].
Hydrogels and Conductive Hydrogels (CHs)
Q3: My conductive hydrogel is too mechanically weak for handling or implantation.
- Problem: Achieving high electrical conductivity often compromises mechanical robustness and processability.
- Solution: Form a dual-network hydrogel with tunable mechanical properties.
- Protocol (for PVA/Gelatin Dual-Network Hydrogel):
- Preparation: Dissolve Polyvinyl Alcohol (PVA) in a binary solvent of glycerol and water. Add gelatin to the mixture.
- Gelation: Inject the solution into a mold and freeze at -20°C for several hours. Subsequently, thaw at 25°C for 2 hours. Repeat this freeze-thaw cycle to form a stable microcrystalline PVA network.
- Tuning: Adjust the glycerol content (e.g., a 40% ratio was found optimal in one study) to balance elasticity and flexibility. The glycerol forms strong hydrogen bonds with PVA, increasing tensile strength [32].
- Alternative: For conductive hydrogels, incorporate Fe³⺠ions as dynamic cross-linkers into a gelatin/poly(acrylic acid-co-acrylamide) network. The Fe³⺠concentration can tune both mechanical toughness (up to 569% elongation at break) and electrical conductivity [32].
Q4: How can I fabricate a microelectrode array on a soft hydrogel substrate?
- Problem: Standard microfabrication techniques are not compatible with soft, water-swollen hydrogels.
- Solution: Utilize laser processing to pattern high-fidelity circuits on conductive polymer films, which can be integrated with hydrogel systems.
- Protocol:
- Film Preparation: First, create a highly conductive and patternable film, such as the VPS PEDOT:PSS film described in Q1 [29].
- Laser Patterning: Use a laser ablation system to directly write and pattern the desired microelectrode array design onto the film.
- Integration: The laser-patterned film can serve as a conformable electrode layer in contact with or laminated to a softer hydrogel layer for final device assembly [29].
Bioresorbable Composites
Q5: The degradation rate of my bioresorbable nerve guide is too fast, losing mechanical strength before tissue healing is complete.
- Problem: Rapid degradation leads to premature loss of mechanical support and potential inflammatory responses.
- Solution: Use composite materials to finely tune the degradation profile and mechanical properties.
- Protocol (for β-Tricalcium Phosphate (β-TCP) Polymer Composite):
- Material Selection: Select a biodegradable polymer matrix (e.g., PLGA) and blend it with β-TCP ceramic particles.
- Fabrication: Fabricate the scaffold using methods like solvent casting, compression molding, or 3D printing, ensuring a homogeneous distribution of β-TCP.
- Rationale: β-TCP has a chemical composition similar to bone mineral, is osteoconductive, and degrades slower than some fast-resorbing polymers. Its incorporation buffers the local pH during polymer degradation, mitigating inflammatory reactions and providing a more controlled resorption timeline (typically from 10 months to 2 years in bone models) [33].
Q6: What are the key scaffold design factors to minimize inflammation in tissue engineering?
- Problem: Scaffold design triggers a foreign body response, leading to fibrotic encapsulation and implant failure.
- Solution: Optimize scaffold characteristics to promote integration and minimize mechanical mismatch.
- Guidelines:
- Porosity: Ensure a minimum pore size of 100 µm for nutrient diffusion, with ideal pore sizes of 200-350 µm for bone tissue in-growth [33].
- Mechanical Properties: Tailor the elastic modulus to match the target tissue (1 kPa - 1 MPa for soft tissues) to reduce shear stress and chronic inflammation [34].
- Surface Chemistry: Use bioactive materials (e.g., HAp, specific peptides) that support normal cellular activity and osteoconduction [33].
Experimental Data and Material Properties
Table 1: Key Properties of Conducting Polymers for Neural Interfaces
| Polymer | Typical Conductivity Range | Key Advantages | Reported High Performance |
|---|---|---|---|
| PEDOT:PSS | 1 - 10â´ S cmâ»Â¹ [29] | Tunable conductivity, commercial availability, biocompatibility. | ~8800 S cmâ»Â¹ with VPS structure [29]. |
| Polypyrrole (PPy) | Widely investigated [31] | Excellent aqueous processability, good cytocompatibility. | Often used with bioactive dopants (e.g., laminin) for neural growth [31]. |
| Poly(3-hexylthiophene) (P3HT) | Used in photovoltaics [17] | Organic semiconductor, tunable for specific optical wavelengths. | VOC = 0.2 V, ISC = 12.8 nA (10 µm device at 10 mW mmâ»Â²) [17]. |
Table 2: Mechanical and Electrical Properties of Hydrogel-Based Materials
| Material Type | Elastic Modulus | Stretchability | Electrical Conductivity | Key Function |
|---|---|---|---|---|
| Biological Tissues | 1 Pa - 100 kPa [32] | High | Ionic | Target for mechanical matching. |
| Conventional Electronics | 10 - 200 GPa [32] | < 1% (brittle) | High (electronic) | Source of mechanical mismatch. |
| Hydrogels | 1 kPa - 1 MPa [34] | ~20-75% [34] | N/A (Insulating) | Biocompatible, tissue-like scaffold. |
| Conductive Hydrogels (CHs) | < 100 kPa [34] | > 100% strain [34] | 10â»â´ - 10² S/m [34] | Enable ionic-electronic charge transfer at the interface. |
Table 3: Research Reagent Solutions
| Reagent / Material | Function | Application Example |
|---|---|---|
| PEDOT:PSS | Intrinsically conductive polymer. | Core material for neural electrodes and wearable sensors [29] [31]. |
| Poly(3-hexylthiophene) (P3HT) | Organic semiconducting polymer (donor material). | Active layer in subcellular-sized, wireless photovoltaic devices for neuromodulation [17]. |
| β-Tricalcium Phosphate (β-TCP) | Bioresorbable, osteoconductive ceramic. | Composite filler in bone grafts to control degradation and support remodeling [33]. |
| Hyaluronic Acid (HAp) | Bioactive glycosaminoglycan and dopant. | Incorporated into PEDOT as a dopant to improve biocompatibility and reduce inflammation [31]. |
| Polyvinyl Alcohol (PVA) | Hydrogel-forming polymer. | Base for dual-network hydrogels to create tough, tunable mechanical substrates [32]. |
| Fe³⺠Ions | Dynamic cross-linker and conductive additive. | Used to tune the mechanical toughness and electrical conductivity of gelatin-based hydrogels [32]. |
Experimental Workflow Visualizations
Conductive Polymer Electrode Fabrication
Hydrogel-Based Implant Development
Troubleshooting Guide & FAQs
FAQ 1: How can I improve the long-term stability and signal fidelity of my neural implant?
Answer: The most common cause of signal degradation over time is the foreign body response (FBR), which leads to inflammation and glial scar formation. This is often triggered by a mechanical mismatch between the implant and the native tissue.
- Problem: Conventional rigid implants (made from silicon or metals) have a Young's modulus in the GPa range, while brain tissue is in the kPa range. This stiffness mismatch causes chronic inflammation and eventual signal loss [10] [35].
- Solution: Transition to soft, flexible materials that mechanically mimic neural tissue.
- Material Choices: Use polymers like polydimethylsiloxane (PDMS), polyimide (PI), or parylene-C as substrates and encapsulants [35].
- Design Strategies: Implement ultra-thin films (<10 µm), mesh geometries, or serpentine structures to reduce flexural rigidity and improve conformability with tissue [35]. These designs minimize micromotion-induced damage and dampen the FBR, leading to more stable long-term recordings [35] [9].
FAQ 2: What are the key failure points I should monitor in a chronic implantation study?
Answer: Failures can be abiotic (technical/mechanical) or biotic (biological). A systematic checklist is provided below for key components [9].
Table: Chronic Implant Failure Mode Checklist
| Component | Common Failure Modes | Diagnostic & Mitigation Strategies |
|---|---|---|
| Electrodes | Corrosion, delamination, increased impedance [9]. | Use stable coatings (e.g., Iridium Oxide); perform regular electrochemical impedance spectroscopy [9]. |
| Lead Wires/Interconnects | Fatigue fracture from repeated movement [9]. | Use flexible polymers (e.g., silicone) for insulation; inspect with micro-CT scanning [9]. |
| Packaging | Loss of hermeticity, moisture ingress [9]. | Use robust housing (e.g., titanium); conduct accelerated aging tests [9]. |
| Tissue Interface | Glial scarring, neuronal loss, chronic inflammation [10] [35]. | Use soft materials; perform post-mortem histology for astrocytes (GFAP) and microglia (Iba1) markers [35]. |
FAQ 3: My goal is to achieve intracellular recording from a network of neurons. What high-density array technologies should I consider?
Answer: Recent advances in CMOS-based platforms now enable parallel intracellular recording and stimulation, bridging the gap between traditional patch-clamp and large-scale extracellular electrophysiology [10].
- Technology: CMOS-integrated circuits with vertical nanoelectrodes or microhole arrays.
- Key Specifications:
- Electrode Density: Platforms with 4,096 electrodes are available, capable of mapping over ~70,000 synaptic connections among thousands of neurons [10].
- Electrode Design: Nanoelectrodes (~2 µm diameter) or microholes (~2 µm diameter) allow neurons to seal over the electrodes, enabling stable recording of subthreshold membrane potentials [10].
- Material: Platinum-black (PtB) is often used to enhance surface area, reduce impedance, and increase charge injection capacity for stimulation [10].
FAQ 4: Are there non-surgical alternatives for deploying neural interfaces in deep brain regions?
Answer: Yes, an emerging paradigm called "Circulatronics" offers a non-surgical approach for deep brain neuromodulation [7] [17].
- Principle: Subcellular-sized, wireless electronic devices (SWEDs) are fused with living immune cells (e.g., monocytes) to create cell-electronics hybrids.
- Workflow: These hybrids are injected intravenously. The living cells camouflage the electronics, enabling them to cross the intact blood-brain barrier and autonomously traffic to sites of inflammation in the brain. Once there, they can be wirelessly powered to provide focal electrical stimulation [17].
- Key Advantage: This method eliminates the need for invasive intracranial surgery and its associated risks, providing a platform for highly precise neuromodulation [7].
Experimental Protocols
Protocol 1: Fabrication and In Vitro Validation of "Living Electrodes" (μTENNs)
This protocol details the creation of Microtissue Engineered Neural Networks (μTENNs) as a biological interface for optobiological monitoring and modulation [36].
1. Aim: To biofabricate implantable, optically controlled living electrodes that can synaptically integrate with host neural circuitry, providing a more specific and stable neural interface.
2. Materials
- Hydrogel: Agarose (3% w/v in DPBS)
- Cells: Primary cortical neurons isolated from embryonic day 18 rats
- Culture Media: Serum-free neuronal culture media (Neurobasal + B27 + Glutamax)
- Mold: Custom-designed acrylic mold and acupuncture needles for microcolumn fabrication
- Aggregation Device: PDMS wells with inverted pyramidal shapes
3. Step-by-Step Procedure
- Fabricate Agarose Microcolumns:
- Insert acupuncture needles into the custom acrylic mold channels.
- Pour molten agarose into the assembly and allow it to cool and solidify.
- Remove the needles and disassemble the mold to yield hollow agarose microcolumns (e.g., 398 µm OD, 180 µm ID). Cut to the desired length [36].
- Prepare Neuronal Aggregates:
- Dissociate cortical tissue and suspend neurons in culture media at 1.0-2.0 million cells/ml.
- Transfer the cell suspension to the pyramidal PDMS wells.
- Centrifuge at 200g for 5 min to force aggregate formation.
- Incubate overnight at 37°C, 5% CO2 [36].
- Seed Microcolumns to Create μTENNs:
- Remove microcolumns from DPBS and clear fluid from the channels.
- Pipette a single neuronal aggregate into one or both ends of the microcolumn to create unidirectional or bidirectional μTENNs, respectively.
- Culture the constructs, allowing axons to grow through the microcolumn, forming a long, protected axonal tract [36].
- Optogenetic Transduction & In Vitro Validation:
- Transduce μTENN neurons to express optogenetic proteins (e.g., Channelrhodopsin-2) before or during culture.
- Validate functionality using simultaneous optical stimulation and recording (e.g., calcium imaging or electrophysiology) to confirm network activity and control [36].
Diagram Title: Living Electrode (μTENN) Fabrication Workflow
Protocol 2: Establishing a "Circulatronics" System for Non-Surgical Brain Implantation
This protocol outlines the creation and in vivo application of cell-SWED hybrids for non-surgical, focal neuromodulation [17].
1. Aim: To develop and administer subcellular-sized wireless electronic devices (SWEDs) fused with immune cells that can autonomously implant in a target brain region after intravenous injection.
2. Materials
- SWEDs: Fabricated organic photovoltaic devices (e.g., ~10 µm diameter, ~200 nm thick).
- Cells: Primary monocytes (diameter 12-18 µm).
- Fabrication Substrate: Silicon wafer with sacrificial aluminum layer.
- Release Agent: Tetramethylammonium hydroxide (TMAH).
- In Vivo Model: Mice with localized brain inflammation.
3. Step-by-Step Procedure
- Fabricate and Release SWEDs:
- Mass-fabricate SWEDs on a 4-inch silicon wafer using CMOS-compatible processes. The structure is typically anode/organic semiconductor blend/cathode.
- Release the SWEDs from the substrate by etching the sacrificial aluminum layer with TMAH.
- Collect the free-floating SWEDs and confirm their power conversion efficiency remains functional [17].
- Create Cell-SWED Hybrids:
- Isolate primary monocytes.
- Use a covalent chemical reaction to fuse the SWEDs to the monocytes, creating stable hybrids. The living cells act as a biological camouflage and targeting system [17].
- Intravenous Administration and Implantation:
- Inject the cell-SWED hybrids intravenously into the animal model.
- The monocytes naturally traffic to sites of inflammation in the brain, carrying the SWEDs across the intact blood-brain barrier.
- The hybrids autonomously implant in the inflamed target region [17].
- Wireless Neuromodulation:
- Apply near-infrared (NIR) light transcranially to power the implanted SWEDs photovoltaically.
- The SWEDs convert optical energy to electrical potentials, enabling focal electrical stimulation of the surrounding neural tissue with high spatial precision (~30 µm) [17].
Diagram Title: Circulatronics Implantation and Stimulation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Novel Neural Interface Research
| Research Reagent / Material | Function / Application | Key Characteristics & Rationale |
|---|---|---|
| Soft Polymer Substrates (PDMS, Polyimide, Parylene-C) [35] | Insulating substrate and encapsulation for flexible neural probes. | Biocompatible, mechanically compliant (low Young's modulus), and processible with conventional lithography. Reduces FBR. |
| Conductive Polymers (PEDOT:PSS) [35] | Electrode coating or free-standing electrode material. | Enhances conductivity, reduces electrode impedance, and improves signal-to-noise ratio in recording and stimulation. |
| Agarose Hydrogel [36] | Scaffold for "Living Electrodes" (μTENNs). | Forms biocompatible microcolumns that protect and guide axonal growth in 3D engineered neural tissue. |
| Primary Cortical Neurons [36] | Cellular component for μTENN biofabrication. | Forms the functional, synaptically active core of the living electrode, enabling integration with host circuitry. |
| Primary Monocytes [17] | Cellular carrier for Circulatronics devices. | Naturally targets sites of inflammation, enabling blood-brain barrier crossing and precise self-implantation of SWEDs. |
| Organic Photovoltaic Polymers (e.g., P3HT, PCPDTBT) [17] | Active layer material for Subcellular-sized Wireless Electronic Devices (SWEDs). | Enables wireless powering via near-infrared light; biocompatible and tunable for different optical wavelengths. |
| Platinum-black (PtB) [10] | Coating for high-density microelectrodes. | High surface area reduces impedance and increases charge injection capacity, crucial for intracellular recording/stimulation. |
| GABAA receptor agent 6 | GABAA Receptor Agent 6 | GABAA receptor agent 6 is a high-purity chemical for neuroscientific research. This product is For Research Use Only and not for human or veterinary diagnosis or therapy. |
| Ivabradine impurity 7-d6 | Ivabradine impurity 7-d6, MF:C27H34N2O6, MW:488.6 g/mol | Chemical Reagent |
FAQs: Immune Response to Bioelectronic Implants
1. What are the primary immune challenges faced after bioelectronic implant insertion? The initial immune response to an implant begins with an acute inflammatory reaction to the injury and the innate recognition of the foreign material itself. This is characterized by protein deposition on the biomaterial, activation of complement proteins, and the recruitment of polymorphonuclear neutrophils (PMNs) and monocytes to the injury site [37]. These cells release reactive oxygen species (ROS) and pro-inflammatory cytokines like IL-1β and TNF-α, which can cause secondary tissue damage and hinder device integration [37]. This can transition to a chronic phase involving lymphocytes, potentially leading to fibrosis (scar tissue formation) around the implant, which can isolate the device and compromise its long-term function [37].
2. How can surface engineering directly influence the immune response? Surface engineering aims to create biocompatible interfaces with properties designed to enhance the biological response and reduce polymicrobial accumulation, which can trigger inflammation [38]. This can be achieved by:
- Modifying Physicochemical Properties: Altering surface topography, chemistry, and energy to make the surface less recognizable as foreign, thereby dampening the foreign body reaction [37].
- Incorporating Active Agents: Developing antimicrobial or immunomodulatory coatings that utilize a range of compounds for contact-killing or as localized drug-delivery systems to manage the immune environment actively [38].
3. What surface topographies are known to promote a favorable (M2) macrophage phenotype? While specific topographies are not detailed in the provided search results, the principle is that the physical and mechanical properties of the implant surface are largely responsible for the foreign body reaction propagated by infiltrating immune cells [37]. Research in biomedical engineering focuses on creating specific surface architectures that can direct immune cell polarization toward the regenerative/anti-inflammatory (M2) macrophage phenotype, which is associated with tissue healing and repair, rather than the inflammatory (M1) phenotype [37].
4. My in vivo experiments show unexpected fibrosis. What surface properties should I re-evaluate? Unexpected fibrosis is a sign of a persistent chronic inflammatory response. You should systematically investigate the following surface properties:
- Surface Chemistry: Assess whether degradation products from your coating or base material are pro-inflammatory [37].
- Topography and Roughness: Re-evaluate the micro- and nano-scale features of your surface, as these directly influence how immune cells like macrophages and fibroblasts adhere and behave [37].
- Coating Stability: Verify the integrity and adhesion of any functional coatings under physiological conditions. Delamination or inconsistent coating can expose underlying materials, triggering a stronger immune reaction [39].
5. How do I accurately characterize the mechanical properties of a thin functional coating? Characterizing the mechanical properties of engineered surfaces at the appropriate length scale is key to understanding performance [39]. Key methods include:
- Nanoindentation: Used to measure hardness and elastic modulus, with advanced versions capable of operating at high temperatures to simulate demanding environments [39].
- Micro-Scratch Testing: Conducted with apparatus designed to measure coating durability and adhesion, often while observed in an electron microscope to understand failure mechanisms [39].
- Focused Ion Beam (FIB) Milling: Used to create micro-pillars or cantilevers from the coating, whose mechanical properties can then be measured under an electron microscope [39].
Troubleshooting Guides
Issue 1: Persistent Inflammation and Fibrosis Around the Implant
| Possible Cause | Diagnostic Experiments | Potential Surface Engineering Solution |
|---|---|---|
| Pro-inflammatory surface chemistry | - Perform surface analysis (XPS, FTIR) to confirm coating composition. - Test in vitro for macrophage activation (M1 cytokine secretion: IL-1β, TNF-α) [37]. | Apply a bio-inert coating or a coating that releases anti-inflammatory cytokines (e.g., IL-4, IL-10) to promote M2 macrophage polarization [37]. |
| Incorrect surface topography | - Use SEM to characterize surface topography at multiple scales. - Correlate specific topographical features with fibroblast activation in vitro. | Re-engineer the surface topography to feature structures known to discourage fibroblast proliferation and collagen deposition, promoting a more regenerative interface. |
| Unstable or degrading coating | - Use adhesion tests (e.g., tape test, scratch test) post-implantation [39]. - Analyze explanted surfaces for signs of delamination or wear. | Optimize the coating deposition method to improve adhesion and stability. Consider using functionally graded coatings (FGCs) for better integration and mechanical performance [40]. |
Issue 2: Poor Bio-Integration and Device Failure
| Possible Cause | Diagnostic Experiments | Potential Surface Engineering Solution |
|---|---|---|
| Robust foreign body reaction | - Histological analysis of the implant-tissue interface for presence of giant cells and a thick fibrous capsule [37]. | Modify surface energy and wettability to reduce non-specific protein adsorption, which is the first step in the foreign body reaction [37]. |
| Lack of tissue-specific cues | - Immunostaining for key extracellular matrix (ECM) proteins and integrins at the interface. | Functionalize the surface with bioactive peptides (e.g., RGD) derived from ECM proteins to promote specific cell adhesion and signaling, encouraging integration over isolation [37]. |
| Bacterial colonization & infection | - Use microbial culture or DNA sequencing on explanted devices. - Perform in vitro antimicrobial adhesion assays. | Implement an antimicrobial coating strategy, either by incorporating contact-killing agents (e.g., silver nanoparticles) or a drug-delivery system for controlled release of antibiotics [38]. |
Issue 3: Inconsistent Coating Performance Across Batches
| Possible Cause | Diagnostic Experiments | Potential Surface Engineering Solution |
|---|---|---|
| Uncontrolled coating deposition parameters | - Review process logs for variability in temperature, pressure, or deposition rate. - Use spectroscopic ellipsometry to measure coating thickness uniformity. | Establish and adhere to a strict Standard Operating Procedure (SOP) with real-time monitoring of key deposition parameters. |
| Substrate surface contamination | - Perform surface analysis (XPS, AES) before coating to detect organic or inorganic contaminants. | Implement a rigorous and validated substrate cleaning protocol (e.g., plasma cleaning, solvent cleaning) prior to coating deposition. |
| Inadequate quality control metrics | - Statistically analyze coating performance data (e.g., adhesion, composition) against in vivo outcomes. | Introduce additional characterization checkpoints, such as consistent measurement of coating thickness, adhesion, and chemical composition before proceeding to in vivo testing [39]. |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Implant Surface and Immune Modulation Research
| Item | Function in Research |
|---|---|
| Protein NPs (e.g., eOD-GT8 60mer) | These protein nanoparticles, with a size optimized for lymphatic uptake, can be used as a platform to deliver immunomodulatory signals (e.g., antigens) directly to lymph nodes to steer the adaptive immune response [41]. |
| Amphiphilic Conjugates (Amph-vaccines) | Conjugates consisting of peptides or oligonucleotides linked to an albumin-binding lipid tail. They bind to endogenous albumin in vivo, improving targeting and exposure to lymphoid tissues for enhanced immunomodulation [41]. |
| Lipid Nanoparticles (LNPs) | A versatile delivery system that can encapsulate a wide range of immunomodulatory payloads, such as mRNA encoding for cytokines (e.g., IL-12) or other signaling proteins, for localized delivery to specific immune cells [41]. |
| Poly(lactic-co-glycolic acid) (PLGA) NPs | Biodegradable and biocompatible polymer nanoparticles used as vehicles for the controlled release of antigens or immune adjuvants, allowing for sustained modulation of the local immune environment [41]. |
| Toll-like Receptor (TLR) Agonists (e.g., CpG oligonucleotides) | Molecules that activate specific pattern recognition receptors on immune cells. They can be incorporated into coatings or delivery systems to deliberately trigger or enhance specific immune pathways [41]. |
| Self-assembling Saponin/Lipid NPs (ISCOMs) | Cage-like nanoparticles (~40 nm) that are potent vaccine adjuvants and have an ideal size for trafficking to lymph nodes, useful for studying systemic immune induction [41]. |
| Functionalized Polymer Scaffolds | Porous scaffolds that can be loaded with a combination of signals (e.g., GM-CSF, CpG) and implanted to create a localized niche for recruiting and programming immune cells in situ [41]. |
| Vitamin K1 2,3-epoxide-d7 | Vitamin K1 2,3-epoxide-d7 Stable Isotope|VK1O-d7 |
| Cap-dependent endonuclease-IN-25 | Cap-dependent endonuclease-IN-25|CEN Inhibitor |
Experimental Protocols
Protocol 1: Evaluating Macrophage Polarization on Engineered SurfacesIn Vitro
Objective: To assess how a novel surface topography or coating influences the polarization of macrophages toward pro-inflammatory (M1) or regenerative (M2) phenotypes.
Materials:
- Test substrates (e.g., coated implant discs)
- Cell culture plate (e.g., 24-well)
- Primary human monocyte-derived macrophages or a macrophage cell line (e.g., RAW 264.7)
- Cell culture media and supplements
- Lipopolysaccharide (LPS) & Interleukin-4 (IL-4) for positive controls
- RNA extraction kit
- qPCR reagents
- ELISA kits for TNF-α, IL-1β (M1 markers), and IL-10, TGF-β (M2 markers)
Method:
- Substrate Preparation: Sterilize all test substrates (e.g., via UV irradiation or ethanol wash) and place them securely into the wells of a culture plate.
- Cell Seeding: Seed macrophages onto the test substrates at a standardized density (e.g., 100,000 cells/cm²) in complete growth medium. Include control wells with cells on standard tissue culture plastic.
- Stimulation and Incubation: After cell attachment, replace the medium. For positive controls, add LPS (e.g., 100 ng/mL) to induce M1 polarization or IL-4 (e.g., 20 ng/mL) to induce M2 polarization. Leave test substrate groups in base media. Incubate for 24-48 hours.
- Analysis:
- Gene Expression (qPCR): Harvest cells and extract RNA. Perform qPCR for M1 markers (e.g., iNOS, CD80) and M2 markers (e.g., ARG1, CD206).
- Protein Secretion (ELISA): Collect cell culture supernatants. Use ELISA to quantify the secretion of M1-associated cytokines (TNF-α, IL-1β) and M2-associated cytokines (IL-10, TGF-β) [37].
- Cell Morphology: Use fluorescence microscopy (after staining for F-actin) to observe cell morphology; M1 macrophages tend to be spread and flattened, while M2 macrophages are often more elongated.
Protocol 2: Assessing Coating Adhesion and Durability
Objective: To determine the mechanical stability and adhesion strength of a functional coating on an implant substrate, simulating physiological stresses.
Materials:
- Coated test substrates
- Micro-scratch tester or nanoindenter with a scratch module
- Optical microscope or SEM
- Tape adhesion test kit (e.g., ASTM D3359)
Method:
- Macro-Scale Adhesion (Tape Test):
- Make a cross-hatch pattern of cuts through the coating down to the substrate using a calibrated blade.
- Apply and firmly rub a specialized pressure-sensitive tape over the grid.
- Rapidly remove the tape at a 180° angle.
- Examine the grid area under a microscope and rate the adhesion based on the percentage of coating removed (per ASTM D3359) [39].
- Micro-Scale Adhesion (Scratch Test):
- Mount the coated sample on the stage of a micro-scratch tester.
- Use a stylus (e.g., Rockwell diamond indenter) to make a scratch across the surface under a progressively increasing normal load.
- Simultaneously, use an acoustic emission sensor or friction force measurement to detect coating failure events.
- Observe the scratch path under an optical microscope or SEM to identify the critical load (Lc) at which cohesive or adhesive failure occurs (e.g., cracking, chipping, delamination) [39].
Signaling Pathways and Experimental Workflows
Diagram: Immune Response to Implanted Biomaterials
Diagram Title: Immune Response Pathway Following Implant Insertion
Diagram: Surface Engineering Development Workflow
Diagram Title: Surface Engineering Development and Testing Workflow
Overcoming Failure Modes: Diagnosing, Mitigating, and Optimizing Implant Performance
Troubleshooting Guides
Mechanical Fatigue of Implanted Electrodes
Q: Why do my planar silicon electrode arrays show degraded recording performance and physical damage after several months of chronic implantation?
A: Chronic mechanical fatigue, driven by material mismatch and micro-motion, is a primary cause. Finite Element Model (FEM) simulations show that mechanical mismatch between materials like iridium and silicon leads to concentrated strain, particularly at protrusions such as electrical traces. This strain is further amplified by small, repeated movements (micromotion) of the brain relative to the implant, leading to material failure over time [42].
Table 1: Material Properties and Failure Strains of Common Intracortical Electrode Components [42]
| Material | Fracture Strength (MPa) | Young's Modulus (GPa) | Key Failure Modes in Chronic Implants |
|---|---|---|---|
| Silicon (substrate) | 1,800 | 200 | Brittle fracture; cracking |
| Polycrystalline Silicon (trace) | 1,200 | ~160 (estimated) | Crack formation and propagation |
| Silicon Oxide (insulation) | 360 | ~70 (estimated) | Delamination, cracking |
| Iridium (recording site) | 500–740 | 528 | Strain concentration at material borders |
Diagnosis and Analysis Protocol:
- Pre-implant Simulation: Conduct a 3D Finite Element Model (FEM) to analyze the von Mises Equivalent Elastic Strain on your electrode design, focusing on interfaces between different materials and small protrusions [42].
- Post-explant Inspection: Use Scanning Electron Microscopy (SEM) to visually identify cracks, delamination, or other physical damage on explanted devices, particularly around recording sites and traces [42].
- Chronic Performance Correlation: Correlate the physical damage observed via SEM with longitudinal performance metrics, including single-unit electrophysiology recordings and electrochemical impedance spectroscopy [42].
Solutions:
- Design: Minimize material mismatches and protrusions in new electrode designs. Transition towards soft, flexible materials that better match the mechanical properties of neural tissue [6] [9].
- Materials: Consider using more ductile materials or composites for traces and interconnects to better withstand repeated strain [6].
Corrosion of Bioelectronic Implants
Q: What causes the corrosion of implant metals, and how can it be mitigated in the physiological environment?
A: Corrosion is an electrochemical process accelerated in the saline, protein-rich physiological environment. It can lead to the release of toxic ions, degradation of structural integrity, and failure of electronic components. The problem is exacerbated for materials like magnesium alloys, which are designed to be bioresorbable, and for all implants subjected to mechanical stress (corrosion-fatigue) [43] [44].
Table 2: Corrosion and Corrosion-Fatigue Behavior of Implant Metals [43]
| Material Class | Key Corrosion Challenge | Factors Influencing Failure | Potential Mitigation Strategy |
|---|---|---|---|
| Magnesium-based Biocomposites | High degradation rate in physiological environment compromises mechanical integrity. | Fluctuating load (fatigue), chloride ions, local pH changes. | Alloying, surface coatings, and control of microstructure. |
| Platinum & Platinum-Iridium | Generally high corrosion resistance, but can be susceptible at high stimulation charges or in flawed designs. | Electrical stimulation parameters, presence of impurities, mechanical cracks in insulation. | Use of charge-balanced stimulation waveforms, robust encapsulation. |
Diagnosis and Analysis Protocol:
- Accelerated Aging Tests: Perform in vitro tests in simulated body fluid (SBF) at 37°C to assess corrosion rates and products.
- Surface Analysis: Use techniques like energy-dispersive X-ray spectroscopy (EDS) on explanted devices to identify corrosive products and elemental composition changes.
- Electrochemical Characterization: Perform electrochemical impedance spectroscopy (EIS) and cyclic voltammetry to monitor the stability of electrode materials and coatings over time.
Solutions:
- Coatings: Apply stable, biocompatible coatings (e.g., iridium oxide, silicon carbide) to act as a barrier [9].
- Material Selection: Use highly corrosion-resistant alloys (e.g., Pt-Ir) for stimulating electrodes [9].
- Hermetic Packaging: Ensure a complete hermetic seal around all active electronics using titanium housings or advanced thin-film barriers to prevent moisture ingress [9].
Foreign Body Response and Encapsulation Failure
Q: How does the chronic foreign body response lead to the encapsulation of neural implants and degradation of signal quality?
A: The immune system recognizes the implant as a foreign body, triggering an acute inflammatory response that can evolve into a chronic state. This ultimately results in the formation of a dense, fibrotic capsule of glial cells and collagen around the implant. This encapsulation physically isolates the electrode from nearby neurons and increases impedance, leading to signal attenuation or loss [9] [44].
Diagnosis and Analysis Protocol:
- Histological Analysis: Post-mortem, section the implanted tissue and stain for specific cell types (e.g., Iba1 for microglia, GFAP for astrocytes, CD68 for macrophages) and collagen to quantify the extent of glial scarring and fibrotic encapsulation [42] [9].
- In Vivo Monitoring: Track impedance trends over time; a steady increase can indicate progressive encapsulation and tissue reaction [42].
- Imaging: Utilize non-invasive imaging like MRI to monitor tissue changes and inflammation around the implant chamberically [42] [44].
Solutions:
- Mechanical Compliance: Use soft, flexible materials with low bending stiffness (e.g., < 10â»â¹ Nm) that mimic the Young's modulus of brain tissue (~1 kPa) to reduce micromotion-induced inflammation [6].
- Surface Modifications: Develop bioactive coatings with anti-inflammatory drugs (e.g., dexamethasone) or neurotrophic factors to modulate the local immune response [9].
- Device Geometry: Minimize the cross-sectional footprint of implant shanks to reduce tissue displacement and damage during insertion and chronic implantation [42].
Frequently Asked Questions (FAQs)
Q: What are the key differences in failure modes between rigid (e.g., silicon) and soft, flexible implants? A: Rigid implants primarily fail due to mechanical mismatch with tissue, causing inflammation, strain concentration on brittle materials, and eventual fracture. Soft, flexible implants better match tissue mechanics, reducing the chronic immune response. However, their failure modes often involve mechanical fatigue at interconnects, delamination of thin films in wet environments, and long-term degradation of polymer substrates [6].
Q: Beyond the electrode itself, what other components of a full implant system are prone to failure? A: A complete neural interface system has multiple critical points of failure [9]:
- Lead Wires: Insulation failure (cracking of polyimide or parylene) and conductor breakage due to repeated flexing.
- Hermetic Packaging: Failure of the seal (e.g., at feedthroughs) allows moisture ingress, corroding internal electronics.
- Interconnects: Mechanical and electrochemical degradation at junctions between different materials (e.g., wire bonds).
- Pulse Generator / Housing: Can cause pressure sores or skin erosion, and the battery has a finite lifespan [9].
Q: Are there standardized methods for long-term biocompatibility assessment of new implant designs? A: Yes, foundational guidelines like ISO 10993 provide a framework for testing cytotoxicity, sensitization, and chronic implantation. However, these standards are often insufficient for capturing complex, long-term dynamic responses. The field is moving towards multimodal, longitudinal assessments combining advanced in vitro models (e.g., organ-on-chip), real-world evidence, and non-invasive imaging (MRI, PET) to better predict clinical performance [44].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for Chronic Implant Research and Development
| Item / Reagent | Function / Application | Technical Notes |
|---|---|---|
| Finite Element Modeling (FEM) Software (e.g., ANSYS) | To simulate mechanical strain and identify high-risk areas in electrode designs prior to fabrication [42]. | Critical for analyzing von Mises strain at material interfaces. |
| Parylene-C | A common polymer used for flexible insulation of electrodes and lead wires [9]. | Susceptible to cracking and delamination under chronic strain; barrier properties can degrade. |
| Iridium Oxide | A conductive coating for electrode sites to lower impedance and increase charge injection capacity [9]. | Improves interface stability under electrical stimulation. |
| Platinum-Iridium Alloy | A standard material for stimulating and recording electrodes due to its excellent corrosion resistance and durability [9]. | Typically used in ratios like 90%/10% (Pt/Ir). |
| Silicon-on-Insulator Wafers | The substrate for microfabricating planar silicon (Michigan) electrodes [42]. | Allows for precise etching of shanks and recording sites. |
| Simulated Body Fluid (SBF) | An in vitro solution for accelerated aging tests to study corrosion and material degradation [43]. | Mimics the ionic composition of human blood plasma. |
| Anti-inflammatory Drug (e.g., Dexamethasone) | Used in local drug delivery systems from coated implants to suppress the acute foreign body response [9]. | Can be incorporated into biodegradable polymer coatings. |
| S-Sulfo-DL-cysteine-2,3,3-d3 | S-Sulfo-DL-cysteine-2,3,3-d3, MF:C3H7NO5S2, MW:204.2 g/mol | Chemical Reagent |
| Hydroxy Pioglitazone (M-II)-d4 | Hydroxy Pioglitazone (M-II)-d4, MF:C19H20N2O4S, MW:376.5 g/mol | Chemical Reagent |
Experimental Workflows & Signaling Pathways
Diagram: Chronic In Vivo Failure Analysis Workflow
Diagram: Foreign Body Response & Encapsulation Signaling Pathway
For researchers developing bioelectronic implants, achieving stable power and data transmission without triggering detrimental immune responses is a significant hurdle. The very act of installing a functional device within the body initiates a complex biological reaction—the Foreign Body Response (FBR). This response can severely compromise the device's performance by increasing impedance at the tissue-device interface, leading to signal loss and eventual functional failure [9] [45]. This guide provides targeted troubleshooting advice to help you navigate these challenges and design experiments that effectively balance electronic performance with biological integration.
Troubleshooting Guides
Problem 1: Rising Impedance and Signal Loss Over Time
Symptoms: Gradual degradation of recorded neural signal quality or increased power requirements for effective stimulation in chronic experiments.
Underlying Cause: The foreign body response leads to the formation of a fibrotic collagen capsule, which acts as an insulating layer between the electrode and the target tissue [9] [45].
Solutions:
- Material Selection: Move from traditional rigid materials (silicon, metals) to soft, flexible electronics. Devices with a Young's modulus below 1 MPa and a bending stiffness under 10â»â¹ N·m significantly reduce the mechanical mismatch with soft tissues, thereby dampening the immune response and improving chronic signal fidelity [6].
- Surface Engineering: Implement novel semiconducting polymers with intrinsic immunomodulatory properties. Research shows that incorporating selenophene into the polymer backbone can suppress macrophage activation, reducing collagen density by approximately 50% compared to standard materials. Further functionalizing side chains with groups like triazole-thiomorpholine 1,1-dioxide (TMO) can reduce collagen deposition by up to 68% [45].
- Mechanical Design: Utilize ultra-thin (< 100 µm) and injectable mesh electronics. These designs conform to tissue surfaces, minimize micromotion-induced damage, and promote better integration with the surrounding biological environment [6].
Problem 2: Wireless Power and Data Transfer Inefficiency
Symptoms: Inconsistent device operation, insufficient power for stimulation/sensing, or unreliable data uplink, often exacerbated by device depth or movement.
Underlying Cause: Power transfer via inductive RF coils is highly sensitive to coil alignment and the thickness of intervening tissue. Safety limits restrict power density to < 80 mW/cm² to prevent tissue heating [9].
Solutions:
- Coil Design and Placement: For implanted devices requiring inductive coupling, ensure the external and internal RF coils are designed for maximum overlap and are separated by the thinnest possible layer of tissue. This optimizes coupling efficiency [9].
- Alternative Power Transfer Technologies: Investigate emerging methods like magnetoelectric power transfer. This technology enables the creation of miniature, battery-free implants that can be wirelessly powered, which is particularly useful for deep-seated targets and eliminates the failure modes associated with batteries [46].
- Power Management Circuitry: Design electronics with high power conversion efficiency. This is critical for devices powered wirelessly deep within the body, as it allows them to operate effectively with less harvested energy [7].
Problem 3: Device Failure Due to Biocompatibility Issues
Symptoms: Device encapsulation, inflammation in surrounding tissue, or complete functional failure requiring explantation.
Underlying Cause: A persistent immune reaction, initiated by both the physical presence of the device and potentially the materials used, leading to chronic inflammation and fibrosis [20] [9] [45].
Solutions:
- Rigorous Biocompatibility Testing: Adhere to the updated ISO 10993-1:2025 standard, which fully integrates a biological risk management process. This includes considering "reasonably foreseeable misuse," such as longer implantation times than initially intended, and assessing the potential for bioaccumulation of leached chemicals [47].
- Advanced Material Integration: Explore "circulatronics" approaches. Fusing microscopic electronic devices with living cells (e.g., monocytes) before injection can camouflage the device from the immune system, allowing it to cross the blood-brain barrier intact and self-implant without triggering a significant inflammatory reaction [7].
- Hermetic Packaging: Ensure all active electronics are protected with a hermetic seal, typically using titanium housing or advanced thin-film barriers, to prevent moisture ingress and ion diffusion that can damage electronics or leach harmful substances into tissue [9].
Frequently Asked Questions (FAQs)
Q1: What are the key material properties to consider for minimizing the Foreign Body Response? The key properties are mechanical softness and surface chemistry. Aim for materials with a low Young's modulus (closer to 1 kPa than 1 GPa) to match tissue mechanics. Chemically, incorporate immunomodulatory groups like selenophene or TMO into semiconducting polymers to actively suppress macrophage activation and collagen deposition [6] [45].
Q2: How can I power an implant without a bulky battery? Several strategies are available:
- Wireless Power Transfer: Use inductive (RF) or magnetoelectric coupling for devices that require continuous operation [46] [9].
- Energy Harvesting: Investigate technologies that convert body motion, thermal gradients, or biochemical energy (e.g., glucose fuel cells) into electrical power [6].
- Battery-Free Designs: For miniaturized implants, magnetoelectric power transfer can enable fully battery-free operation, as demonstrated by startups like Motif Neurotech [46].
Q3: Our implant works well acutely but fails after a few weeks. What should we investigate? Focus on the chronic foreign body response. Perform histology on explanted tissue to quantify fibrotic capsule thickness and immune cell markers (e.g., CD68 for macrophages, α-SMA for myofibroblasts). This will confirm if fibrosis or chronic inflammation is the root cause. Then, re-evaluate your material's long-term stability and mechanical compliance in vivo [9] [45].
Q4: The new ISO 10993-1:2025 standard mentions "foreseeable misuse." How does this affect my biological evaluation? Your biological evaluation plan must now consider scenarios where the device might be used outside its intended instructions. A common example is use for a longer duration than specified. This could potentially re-categorize a device from "prolonged" to "long-term" use, requiring a more extensive biological safety evaluation [47].
Experimental Protocols & Methodologies
Protocol 1: In Vivo Quantification of Foreign Body Response
Objective: To quantitatively assess the extent of fibrotic encapsulation and immune activation around an implanted material.
Materials: Test material films, control material films, SEBS substrate, animal model, equipment for histology and RNA analysis.
Methodology:
- Implantation: Implant thin films of the test and control polymers subcutaneously in an animal model (e.g., mouse dorsal region).
- Explanation: Sacrifice animals and explant the material-tissue interface at defined endpoints (e.g., 1 week for acute response, 4 weeks for chronic fibrosis).
- Histological Analysis:
- Process tissue for Masson's Trichrome (MT) staining to visualize collagen.
- Use image analysis software to calculate collagen density as the percentage of blue-stained area in the tissue immediately surrounding the implant.
- Immunofluorescence Staining:
- Stain tissue sections for macrophages (anti-CD68 antibody) and myofibroblasts (anti-α-SMA antibody).
- Quantify immune cell density around the implant.
- Gene Expression Analysis:
- Isolve mRNA from the peri-implant tissue.
- Perform quantitative PCR (qPCR) to measure expression levels of collagen type I and III, and key inflammatory biomarkers (e.g., IL-6, IL-1β, IL-10) [45].
Protocol 2: Evaluating a Novel Wireless Power Transfer System
Objective: To measure the efficiency and safety of a wireless power link for an implantable device.
Materials: External transmitter coil, implanted receiver coil, test implant device, tissue phantom or animal model, thermal camera, power meter.
Methodology:
- Setup: Position the external transmitter and implanted receiver coils with a known thickness of tissue or tissue-equivalent phantom between them.
- Power Transfer Efficiency:
- Deliver a known input power to the transmitter.
- Measure the power received at the implant's load.
- Calculate efficiency as (Power
*out*/ Power*in*).
- Stability Testing: Measure how power transfer efficiency varies with coil misalignment (lateral and angular) and over time with simulated movement.
- Thermal Safety:
- Use a thermal camera to monitor the temperature at the tissue-coil interface during operation.
- Ensure the power density remains below the safety threshold of 80 mW/cm² to prevent tissue damage from heating [9].
Table 1: Impact of Material Properties on Device-Tissue Interface
| Property | Rigid Bioelectronics | Soft/Flexible Bioelectronics | Effect on Tissue Interface |
|---|---|---|---|
| Young's Modulus | > 1 GPa | 1 kPa – 1 MPa | Softer materials reduce mechanical mismatch and inflammation. |
| Bending Stiffness | > 10â»â¶ N·m | < 10â»â¹ N·m | Ultra-low stiffness prevents tissue damage from micromotion. |
| Device Thickness | > 100 µm | < 100 µm | Thinner devices are more compliant and less invasive. |
| Signal Fidelity (Long-term) | Degrades due to scar tissue | More stable due to better tissue integration | Improved chronic performance [6]. |
Table 2: Efficacy of Immune-Compatible Polymer Designs
| Polymer Design | Collagen Density (%) | Reduction vs. Control | Macrophage Population Reduction | Key Feature |
|---|---|---|---|---|
| Control p(g2T-T) | ~25% | Baseline | Baseline | Standard conjugated polymer. |
| p(g2T-Se) | ~13% | ~50% | ~40% | Selenophene backbone suppresses macrophage activation. |
| p(g2T-Se)-TMO | ~8% | ~68% | ~68% | Side-chain with TMO group further downregulates inflammation [45]. |
Research Reagent Solutions
Table 3: Essential Materials for Bioelectronic Interface Research
| Research Reagent | Function / Application | Key Consideration |
|---|---|---|
| Selenophene-based Semiconducting Polymers | Active layer for electrodes/transistors; suppresses FBR. | Charge-carrier mobility can be maintained at ~1 cm²Vâ»Â¹sâ»Â¹ while reducing collagen deposition [45]. |
| Platinum / Platinum-Iridium Alloys | Traditional electrode material for stimulation/recording. | Excellent electrochemical stability but prone to fibrotic encapsulation without surface modification [9]. |
| Iridium Oxide Coatings | Electrode coating to increase charge injection capacity. | Improves stimulation efficiency but long-term stability under chronic FBR needs evaluation [9]. |
| Soft Elastomers (e.g., SEBS) | Substrate for flexible electronics. | Provides tissue-like mechanical properties to host electronic components [45]. |
| Monocytes (for Cell-Electronics Hybrids) | Living component for "circulatronics" devices. | Camouflages electronics for immune evasion and targeted self-implantation [7]. |
Visual Guide: Signaling Pathways and Workflows
The following diagrams illustrate the core biological challenge and the strategic solutions discussed in this guide.
Foreign Body Response Signaling Pathway
Material Design Strategy to Suppress FBR
Experimental Workflow for In Vivo FBR Evaluation
Strategies for Robust Encapsulation and Hermetic Sealing in Miniaturized Devices
Troubleshooting Guides
Guide 1: Troubleshooting Moisture Ingress in Implantable Medical Devices
Problem: Failure of a miniaturized bioelectronic implant due to internal moisture condensation, leading to circuit corrosion and malfunction.
| Observation/ Symptom | Potential Root Cause | Diagnostic Method | Corrective Action |
|---|---|---|---|
| Condensation inside device package | Internal water vapor content too high (exceeding ~5000 ppm) [48] | Mass spectrometer or pressure-decay leak test to measure internal moisture [48] [49] | Implement stricter bake-out procedures for internal components before final sealing [48]. |
| Corrosion on sensitive components | Direct leak path in primary hermetic seal [48] | Helium mass spectrometer leak testing; fine leak test with rates < 10â»â¸ He/cm³/sec [48] | Review and optimize sealing process (e.g., laser welding parameters); inspect for micro-cracks [48] [49]. |
| Gradual increase in moisture levels over time | Bulk permeation through non-hermetic polymer materials [48] | Accelerated aging tests (e.g., 85°C/85%RH) while monitoring internal moisture [50] [48] | Replace permeable polymers with impermeable barrier materials like ceramics, metals, or specialized glass [51] [48]. |
| Device failure after thermal cycling | Mechanical stress fracturing a glass-to-metal feedthrough seal [48] | Dye-penetrant or bubble-emission test to locate leak path; thermal cycle testing [48] [49] | Switch from a compression seal to a matched coefficient of thermal expansion (CTE) seal to reduce stress [48]. |
Guide 2: Addressing EMI Shielding and Sealing in Miniaturized Wearables
Problem: A wearable medical device experiences electromagnetic interference (EMI) and fails its IP68 rating for water resistance after miniaturization.
| Observation/ Symptom | Potential Root Cause | Diagnostic Method | Corrective Action |
|---|---|---|---|
| Erratic sensor readings in electrically noisy environments | Inadequate EMI shielding in compact form factor [50] [52] | Test Shielding Effectiveness (SE) across 30 MHz to 6 GHz range; target 40-80 dB attenuation [50] | Use custom conductive gaskets with form-in-place (FIP) technology for maximal coverage in limited space [50]. |
| Loss of environmental sealing (IP rating) | Conductive gasket loses compression or degrades from perspiration [50] | Mechanical durability testing (compression set evaluation); chemical resistance testing in saline [50] | Select gasket materials with USP Class VI biocompatibility and resistance to bodily fluids [50]. |
| Shielding performance drops after repeated flexing | Traditional gasket material cannot withstand dynamic bending in body-worn devices [50] | Flex testing combined with real-time EMI performance monitoring [50] | Adopt advanced, flexible conductive gasket materials like silicone filled with silver-coated glass spheres [50]. |
| Device overheating during operation | Gasket and enclosure impede heat dissipation in a compact assembly [50] | Thermal imaging under operating load; measure performance at elevated temperatures (e.g., 37°C body temp) [50] | Integrate thermal management into design, using gaskets that provide both EMI shielding and a thermal conduction path [50]. |
Frequently Asked Questions (FAQs)
Q1: What is the fundamental definition of a "hermetic seal" in the context of medical implants? A hermetic seal is an advanced, airtight seal designed to be impervious to the passage of gases and moisture down to the molecular level. For medical implants, the goal is to keep the internal moisture content low enough to prevent droplet condensation—typically below 5000 ppm—throughout the device's operational life, thereby protecting sensitive electronics from the harsh biological environment [48] [49].
Q2: What is the most critical factor for ensuring the long-term reliability of an implant's hermetic package? Long-term reliability is a function of both material selection and sealing process control. The bulk material (e.g., titanium, ceramic, specific glasses) must have inherently low permeability, while the sealing process (e.g., laser welding, glass frit sealing) must create a joint free of physical leak paths like cracks or pores. Controlling internal outgassing from epoxies and other materials inside the package is equally critical [48].
Q3: Our miniaturized device requires both EMI shielding and environmental sealing. Is there a single component that can achieve both? Yes, conductive gaskets are specifically engineered for this dual purpose. In miniaturized devices, they must simultaneously provide EMI shielding (40-80 dB attenuation) and environmental protection (e.g., IP68 rating). The key challenge is selecting a material that maintains both functionalities under mechanical stress, thermal cycling, and exposure to bodily fluids [50].
Q4: What are the key differences between reliability and stability for a bioelectronic implant? These are distinct but interconnected concepts crucial for clinical adoption:
- Reliability: The probability that a device functions as intended without failure over a specified time and under defined conditions. It is quantified by metrics like Mean Time Between Failures (MTBF) [16].
- Stability: The ability of a device to maintain its functional and structural properties (electrical, chemical, mechanical) over time, resisting degradation from environmental and biological fluctuations [16]. A device can be stable (consistent performance) but unreliable (fails intermittently), or reliable (doesn't fail often) but lack stability (its performance drifts over time) [16].
Q5: What are the standard testing methods for verifying the hermeticity of a final device? A combination of methods is used, ranging from gross to fine leak detection:
- Gross Leak: Pressure-decay, bubble-emission, or dye-penetrant tests [48] [49].
- Fine Leak: Helium mass spectrometer testing is the gold standard for detecting very low leak rates (e.g., < 10â»â¸ He/cm³/sec) required for high-reliability implants [48] [49].
Quantitative Data for Design and Validation
Table 1: Critical Internal Moisture Specifications
| Parameter | Target Value | Rationale | Test Standard/Method |
|---|---|---|---|
| Maximum Internal Water Vapor Content | ≤ 5000 ppm | Prevents liquid droplet condensation at 1.0 atm and 0°C (dew point) [48] | Mass spectrometry of package atmosphere |
| Acceptable Helium Leak Rate | < 10â»â¸ He/cm³/sec | Ensures long-term exclusion of moisture and contaminants for high-reliability systems [48] | Helium mass spectrometer fine leak test |
Table 2: Performance Requirements for Conductive Gaskets in Miniaturized Wearables
| Parameter | Typical Requirement | Challenge in Miniaturization |
|---|---|---|
| EMI Shielding Effectiveness | 40-80 dB attenuation | Maintaining performance with reduced contact area and ground plane [50] |
| Environmental Sealing | IP67 or IP68 rating | Achieving seal integrity with reduced compression force and gasket size [50] |
| Operating Temperature | -10°C to 60°C | Managing thermal expansion mismatches in tight tolerances [50] |
| Biocompatibility | USP Class VI or ISO 10993 | Finding materials that are conductive, flexible, and biocompatible [50] |
Experimental Protocols
Protocol 1: Accelerated Aging for Long-Term Hermeticity Validation
Objective: To predict the long-term reliability of a hermetic seal in a bio-implantable environment within a condensed timeframe. Background: This test subjects the device to elevated temperatures and humidity to accelerate failure mechanisms like moisture permeation and corrosion [50] [48]. Materials:
- Device Under Test (DUT) with internal moisture sensor (if possible)
- Environmental chamber capable of controlling temperature and humidity
- Helium mass spectrometer leak tester Methodology:
- Pre-conditioning: Measure and record the initial internal moisture content and leak rate of each DUT.
- Test Setup: Place the DUTs in the environmental chamber.
- Accelerated Aging: Expose the DUTs to conditions of 85°C and 85% relative humidity for a predefined period (e.g., 500-1000 hours) [50].
- Intermediate Monitoring: At regular intervals (e.g., 250, 500, 750 hours), remove a sample of DUTs.
- Post-Test Analysis: For each sampled DUT:
- Measure the final internal moisture content.
- Perform a final helium leak test.
- Perform functional electrical testing.
- Optionally, perform destructive physical analysis to inspect for corrosion. Data Analysis: Plot internal moisture content and leak rate versus aging time. A stable, flat curve indicates a robust seal. A rising curve indicates a failing seal.
Protocol 2: In-Vitro Biocompatibility and Chemical Resistance Testing for Seals
Objective: To evaluate the stability and durability of sealing materials and gaskets when exposed to simulated bodily fluids. Background: Seals must resist degradation from perspiration, saline, and other chemicals in the body to maintain long-term performance [50]. Materials:
- Samples of the gasket or sealing material
- Artificial sweat and saline solutions
- Controlled temperature bath (maintained at 37°C)
- Tensile testing machine or durometer
- EMI shielding effectiveness test chamber Methodology:
- Baseline Measurement: Measure and record the baseline mechanical (e.g., hardness, compression set) and electrical (e.g., shielding effectiveness) properties of the samples.
- Immersion: Immerse the samples in the test solutions (artificial sweat, saline) in containers placed in the 37°C bath.
- Aging: Maintain the immersion for a prolonged period (e.g., 30-90 days).
- Post-Test Analysis: Remove samples, clean, and dry.
- Re-measure mechanical properties and compare to baseline.
- Re-measure EMI shielding effectiveness and compare to baseline.
- Visually inspect for signs of corrosion, swelling, or cracking. Data Analysis: Quantify the percentage degradation of key properties. Materials showing minimal change (<10% recommended) are suitable for long-term implantation.
Visual Workflows and Logical Diagrams
Diagram 1: Hermetic sealing development and failure analysis workflow.
Diagram 2: Logical pathway from device failure to clinical outcome.
The Scientist's Toolkit: Essential Materials and Reagents
Table 3: Research Reagent Solutions for Hermetic Seal Development
| Item | Function/Application | Key Considerations |
|---|---|---|
| Helium Mass Spectrometer | Gold standard for fine leak detection of final sealed packages [48] [49] | Capable of detecting leak rates as low as 10â»Â¹â° atm·cc/sec; requires calibration standards. |
| Artificial Sweat & Saline Solutions | In-vitro chemical resistance testing of gaskets and seals [50] | Formulations should comply with standards like ISO 3160-2 for biocompatibility pre-screening. |
| Conductive Silicone Elastomers (Ag-filled) | Fabrication of form-in-place (FIP) gaskets for combined EMI shielding and environmental sealing [50] | Ensure filler loading provides sufficient conductivity without compromising mechanical flexibility or biocompatibility. |
| Laser Welding System | High-precision method for creating permanent hermetic seals on metal enclosures [49] | Allows welding of thin housings (~0.1mm) near temp-sensitive components; achieves leak rates < 10â»â¹ mbar·L/s [49]. |
| Glass Frit Preforms | Creating matched CTE glass-to-metal seals for ceramic or metal feedthroughs [48] | Critical to have a matched coefficient of thermal expansion (CTE) between glass, metal pin, and housing to prevent stress cracks [48]. |
Troubleshooting Common Experimental Challenges
Q1: Our in vitro microcurrent setup is failing to produce a significant anti-biofilm effect. What could be going wrong?
- A: This is a common issue often traced to incorrect electrical parameters or biofilm maturity.
- Check Current Parameters: Ensure you are using true microcurrent levels (typically 10-999 µA). Effects are highly dependent on specific current, voltage, and waveform (square, sinusoidal) [53]. Verify your equipment's output with a calibrated multimeter.
- Confirm Biofilm Maturity: Microcurrents are most effective against mature biofilms that have developed their full extracellular polymeric substance (EPS) structure. Standardize your biofilm growth time (e.g., 48-72 hours) and validate maturity using methods like confocal microscopy or crystal violet staining [54].
- Control the Microenvironment: The biofilm's local environment, including pH and ion concentration, can influence current flow. Use a well-defined electrolyte solution to ensure consistent conductivity in your experimental setup [55].
Q2: We are observing inconsistent anti-inflammatory results in our animal models. How can we improve reproducibility?
- A: Inconsistency often stems from variability in stimulus application or animal model status.
- Standardize Application: Ensure consistent electrode placement, contact, and duration for each treatment session. The use of custom-fitted cuffs or implants can improve reproducibility [56].
- Monitor Baseline Inflammation: The level of pre-existing inflammation can affect outcomes. Use biomarkers (e.g., cytokine levels from blood or tissue samples) to stratify subjects before starting the experiment.
- Verify Device Output: Regularly check that your microcurrent device is delivering the specified dose. Battery degradation or electrode corrosion in chronic studies can lead to a drop in delivered current.
Q3: Our laboratory-made electrodes are causing tissue irritation in animal studies. How can this be mitigated?
- A: Tissue irritation indicates a problem with biocompatibility or the foreign body reaction (FBR).
- Consider Electrode Material: Traditional stiff metal electrodes can exacerbate FBR. Transition to more flexible, soft electrodes made from conductive polymers (e.g., PEDOT:PSS) or advanced materials like graphene, which better match the mechanical properties of biological tissue and improve biocompatibility [56].
- Optimize Encapsulation: The interface between the "wet" electrode and "dry" electronics must be perfectly sealed. Use advanced, hermetic encapsulation materials designed for chronic implants to prevent leakage and tissue damage [56].
Q4: How can we distinguish the direct anti-biofilm effect of microcurrents from secondary anti-inflammatory effects in our data analysis?
- A: Disentangling these mechanisms requires a carefully designed experimental workflow.
- Employ Separate Assays:
- For Direct Anti-biofilm: Use in vitro models with single-species biofilms and quantify bacterial viability (e.g., CFU counts) and biofilm biomass. A significant reduction here points to a direct effect [55].
- For Anti-inflammatory: In cell culture or animal models, measure specific inflammatory cytokines (e.g., TNF-α, IL-6) and immune cell infiltration after microcurrent application in the absence of a biofilm [53].
- Use a Staged Approach: In a complex wound model, apply microcurrents and measure biofilm reduction and inflammation markers at different time points. A rapid drop in bacterial load followed by a later decrease in inflammation suggests a primary anti-biofilm effect.
- Employ Separate Assays:
The following tables summarize key quantitative findings from recent research on the bioelectric effect, providing a reference for expected outcomes.
Table 1: Clinical Efficacy of a Bioelectric Effect Toothbrush on Dental Implants Data derived from a clinical trial on patients with dental implants (N=36), showing percentage reduction after 4 weeks of use [55].
| Assessment Index | Surfaces Evaluated | Reduction with BE Toothbrush | Reduction with Non-BE Toothbrush |
|---|---|---|---|
| Modified Plaque Index (mPI) | All Surfaces | 67% (Significant, P < 0.05) | Not Significant |
| Modified Sulcus Bleeding Index (mSBI) | All Surfaces | 59% (Significant, P < 0.05) | Not Significant |
| mPI & mSBI | Interproximal & Lingual Surfaces | Most Significant Reduction | No Significant Change |
Table 2: Categorization and Parameters of Electrical Stimulation Therapies Adapted from scientific literature comparing different electrical stimulation modalities [53].
| Categorization | Primary Purpose | Typical Intensity Range | Key Controllable Parameters |
|---|---|---|---|
| Microcurrent Stimulation (MCS) | Tissue repair, pain management, enhancing cellular function | 10 - 999 µA (sub-sensory) | Intensity (µA), Frequency (0.1-1000 Hz), Pulse Shape |
| Transcutaneous Electrical Nerve Stimulation (TENS) | Pain relief | Adjustable in mA range | Intensity (mA), Frequency (1-200 Hz), Pulse Width (ms) |
| Electrical Muscle Stimulation (EMS) | Muscle strengthening & rehabilitation | Adjustable in mA range | Intensity (mA), Frequency (1-100 Hz), Pulse Width (µs) |
| Functional Electrical Stimulation (FES) | Facilitating functional movements | Adjustable in mA range | Intensity (mA), Frequency (20-100 Hz), Stimulation Timing |
Detailed Experimental Protocols
Protocol 1: In Vitro Assessment of Microcurrent Anti-Biofilm Efficacy
Objective: To quantify the effectiveness of microcurrents in disrupting pre-established bacterial biofilms.
Materials:
- Bacterial Strains: Porphyromonas gingivalis (for oral/dental models) or Pseudomonas aeruginosa (for general wound models) are commonly used [55].
- Growth Medium: Appropriate broth and agar (e.g., Tryptic Soy Broth for P. aeruginosa, Brain Heart Infusion for P. gingivalis).
- Biofilm Setup: 96-well polystyrene plates or a flow cell system for mature biofilm growth.
- Microcurrent Device: A function generator or a dedicated microcurrent system with calibrated output.
- Electrodes: Sterile, non-corrosive electrodes (e.g., platinum or Ag/AgCl).
- Electrolyte Solution: Phosphate-buffered saline (PBS) or a defined minimal salts medium.
- Viability Assay: Equipment for Colony Forming Unit (CFU) counts or a metabolic assay like MTT.
Methodology:
- Biofilm Growth: Inoculate wells with a standardized bacterial suspension and incubate under optimal conditions for 48-72 hours to form mature biofilms. Replace medium every 24 hours.
- Experimental Groups: Establish groups: (1) Test: Biofilm + Microcurrent, (2) Sham Control: Biofilm + Electrodes (no current), (3) Media Control: Media only.
- Microcurrent Application: Submerge the electrodes in the electrolyte solution above the biofilm. Apply the selected microcurrent waveform. A referenced parameter is a 1000 µA direct current (DC) for specified durations [55].
- Post-Treatment Analysis:
- Viability: Gently wash the biofilm to remove planktonic cells. Disrupt the biofilm by sonication/vortexing, perform serial dilution, and plate for CFU counts.
- Biomass: Use crystal violet staining to quantify total adhered biofilm biomass.
- Visualization: Use Scanning Electron Microscopy (SEM) or Confocal Laser Scanning Microscopy (CLSM) to observe structural disintegration of the biofilm.
Protocol 2: Evaluating Anti-inflammatory Effects in a Cell Culture Model
Objective: To assess the modulation of inflammatory responses in mammalian cells using microcurrent stimulation.
Materials:
- Cell Line: Macrophage cell lines (e.g., RAW 264.7) or primary human macrophages.
- Stimulation Agent: Lipopolysaccharide (LPS) to induce inflammation.
- Cell Culture Equipment: Standard tissue culture flasks, multi-well plates, COâ‚‚ incubator.
- Microcurrent Device & Electrodes: As in Protocol 1, with sterile, cell-compatible electrodes.
- Analysis Tools: ELISA kits for cytokines (TNF-α, IL-6, IL-10) and equipment for RNA extraction and qPCR.
Methodology:
- Cell Preparation: Seed macrophages in multi-well plates and allow to adhere overnight.
- Inflammation Induction: Stimulate cells with a predetermined concentration of LPS (e.g., 100 ng/mL) for 1-2 hours.
- Microcurrent Treatment: Apply microcurrent to the test groups. A typical MCS frequency may be in the sub-sensory range, around 0.1 to 1000 Hz [53]. The sham control receives LPS but no current.
- Post-Incubation: Continue incubating the cells for 6-24 hours to allow for cytokine production.
- Sample Collection & Analysis:
- Protein Level: Collect cell culture supernatant and analyze pro-inflammatory (TNF-α, IL-6) and anti-inflammatory (IL-10) cytokine levels via ELISA.
- Gene Expression: Extract total RNA from cells and perform qPCR to measure the expression of genes related to inflammation (e.g., iNOS for M1 phenotype) and repair (e.g., Arg1 for M2 phenotype) [53] [57].
Signaling Pathways and Experimental Workflows
Diagram Title: Proposed Mechanisms of Microcurrent Anti-biofilm and Anti-inflammatory Action
Diagram Title: Experimental Workflow for Microcurrent Therapy Development
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Microcurrent and Biofilm Research
| Item | Function & Rationale | Example / Specification |
|---|---|---|
| Programmable Microcurrent Generator | To deliver precise, low-level electrical currents (µA range). Essential for defining the therapeutic "dose" [53]. | Equipment with adjustable waveform, frequency (0.1-1000 Hz), and intensity (1-1000 µA). |
| Bio-compatible Electrodes | To interface the electrical signal with biological tissue or culture. Material choice minimizes foreign body reaction [56]. | Platinum-iridium, Ag/AgCl, or conductive polymers (PEDOT:PSS). |
| Biofilm Reactor / Flow Cell System | To grow standardized, mature biofilms that closely mimic in vivo conditions for consistent testing [54]. | 96-well plates for screening; CDC biofilm reactors or flow cells for complex models. |
| Confocal Laser Scanning Microscope (CLSM) | To visualize the 3D structure of biofilms and quantify live/dead bacteria and EPS matrix before and after treatment. | Used with fluorescent stains (e.g., SYTO9, propidium iodide, ConA). |
| Cytokine ELISA Kits | To quantitatively measure key inflammatory markers (e.g., TNF-α, IL-6, IL-10) in cell supernatant or tissue homogenates. | Validated kits for specific model species (human, mouse, rat). |
| Conductive Polymer Coating | Advanced electrode coating that improves signal transduction and biocompatibility by bridging ionic (biology) and electronic (device) conduction [56]. | Poly(3,4-ethylenedioxythiophene) polystyrene sulfonate (PEDOT:PSS). |
From Bench to Bedside: Validating Anti-Inflammatory Efficacy in Preclinical and Clinical Settings
FAQs: Core Principles and Biological Responses
FAQ 1: What is the primary biological driver of Foreign Body Response (FBR) against bioelectronic implants, and how do rigid and soft devices differ in their impact?
The primary driver of FBR is the mechanical mismatch between the implant and the native tissue. The body recognizes this mismatch as a foreign entity, triggering an inflammatory cascade that leads to the formation of a fibrotic capsule, isolating the device and degrading its performance [6] [58].
- Rigid Bioelectronics: Traditional devices made from silicon or metals have a Young's modulus > 1 GPa, which is orders of magnitude stiffer than soft, dynamic tissues (e.g., brain tissue has a modulus of < 1 kPa) [6] [59]. This significant stiffness mismatch causes chronic micromotion, inflammation, and substantial fibrotic encapsulation, with reported capsule thicknesses around 85.2 ± 12.7 μm for conventional materials like platinum [59].
- Soft/Flexible Bioelectronics: Devices fabricated from polymers, elastomers, and hydrogels can achieve a tissue-like modulus (1 kPa – 1 MPa) and ultra-low bending stiffness (< 10â»â¹ Nm) [6]. This mechanical compliance minimizes tissue trauma and immune activation. Advanced soft devices have demonstrated a reduction in fibrous capsule thickness to 28.6 ± 5.4 μm, about one-third that of rigid interfaces [59].
FAQ 2: How does device flexibility influence long-term signal fidelity and stimulation performance?
Long-term performance is critically dependent on stable tissue integration, which is directly compromised by FBR.
- Rigid Devices: While they may offer strong short-term signal quality, their long-term performance degrades due to micromotion and the formation of an insulating scar tissue layer. This fibrotic capsule increases the interface impedance and dampens signal transmission [6].
- Soft/Flexible Devices: Their ability to form conformal, stable interfaces with tissues results in better chronic signal acquisition. For instance, soft bioelectronic interfaces have demonstrated stable electrophysiological signal acquisition over 30 days, achieving a high signal-to-noise ratio (SNR) of 37 dB, compared to only 15 dB for conventional Pt electrodes [59].
FAQ 3: What are the key material and design strategies for developing bioelectronics that minimize FBR?
Research focuses on material chemistry and structural design to bridge the biotic-abiotic interface seamlessly.
- Material Innovation: Using conductive hydrogels crosslinked with dynamic bonds allows for self-healing properties and ultra-high toughness. Integrating bioactive coatings, such as MXene-silk fibroin composites, can actively suppress immune responses by scavenging reactive oxygen species (ROS) [59].
- Design Innovation: Moving beyond flat geometries, fiber-based electronic devices (FEDs) and open-mesh, closed-mesh, or island-bridge electrode designs enhance conformability and strain tolerance [60] [61]. The "living electrode" concept, which integrates a functional cell layer with the electronic device, represents a frontier in minimizing the biotic/abiotic mismatch [58].
Troubleshooting Guides for Common Experimental Challenges
Problem: Inconsistent Electrical Performance in Flexible Electrodes During Cyclic Loading
- Symptoms: Fluctuating impedance, signal drift, or complete failure during stretching or bending tests.
- Root Cause: Mechanical fatigue of conductive materials, delamination of functional layers, or strain concentration at design interfaces.
- Solution:
- Geometry Optimization: Adopt strain-resilient designs. A comparative study showed that an island-bridge design exhibited the lowest resistance variation (±1.61%) under strain, while a closed-mesh design provided a balanced performance with high signal-to-noise ratios (up to 14.83 dB) in EMG tests [60].
- Material Selection: Use intrinsically stretchable conductors like liquid metals or conductive polymer composites. Ensure strong interfacial adhesion by employing appropriate adhesion layers (e.g., Chromium for gold on polyimide) [6] [60].
- Protocol Verification: Standardize testing parameters (e.g., strain rate, number of cycles) and implement real-time monitoring of resistance during deformation to identify failure points.
Problem: Uncontrolled Foreign Body Response in Animal Implantation Models
- Symptoms: Thick fibrous encapsulation, degradation of signal quality over time, and histological markers of chronic inflammation.
- Root Cause: Excessive mechanical mismatch and/or lack of bioactive surface properties to modulate the immune response.
- Solution:
- Modulus Matching: Select substrate materials with Young's modulus close to the target tissue. For neural interfaces, use soft materials like polyurethane elastomers with a modulus < 1 kPa [59].
- Biofunctionalization: Implement bioactive coatings that release anti-inflammatory signals or actively modulate macrophage polarization. A mussel-inspired, self-healing bioadhesive interface has been shown to reduce fibrous capsule thickness significantly [59].
- Histological Analysis: Follow a standardized protocol for explant analysis. Perfuse the animal, explant the device with surrounding tissue, and section for staining (e.g., H&E for capsule thickness, immunofluorescence for immune cell markers like CD68 for macrophages).
Experimental Protocol: Histological Evaluation of FBR
This protocol outlines the key steps for assessing Foreign Body Response (FBR) to an implanted device in a rodent model.
Problem: Delamination of Conductive Coatings in Humid or Aqueous Environments
- Symptoms: Gradual or sudden increase in electrical impedance, visual peeling or cracking of the conductive layer.
- Root Cause: Poor adhesion between the functional coating and the substrate, often exacerbated by cyclic strain or hydrolytic degradation.
- Solution:
- Surface Pretreatment: Use oxygen plasma or chemical etching to improve surface energy and adhesion.
- Adhesion Layers: Employ thin adhesion layers like Chromium (Cr) or Titanium (Ti) when sputtering metals onto polymer substrates [60].
- Advanced Encapsulation: Develop multilayer encapsulants or use self-healing materials that can recover barrier properties. Note that some soft materials may show a 23% conductivity decay after 28 days of biofluid immersion, highlighting the need for robust encapsulation [59].
Quantitative Data Comparison
The following tables summarize key performance differences between rigid and soft/flexible bioelectronics.
Table 1: Mechanical and Electrical Properties Comparison
| Property | Rigid Bioelectronics | Soft/Flexible Bioelectronics |
|---|---|---|
| Young's Modulus | > 1 GPa [6] | 1 kPa – 1 MPa [6] |
| Bending Stiffness | > 10â»â¶ Nm [6] | < 10â»â¹ Nm [6] |
| Stretchability | < 1% (brittle) [6] | > 10% (can exceed 100%) [6] |
| Typical Materials | Silicon, Metals, Ceramics [6] | Polymers, Elastomers, Hydrogels, Liquid Metals [6] |
| Signal-to-Noise Ratio (SNR) | ~15 dB (Conventional Pt electrodes) [59] | ~37 dB (Advanced soft interfaces) [59] |
Table 2: Foreign Body Response and Reliability Metrics
| Metric | Rigid Bioelectronics | Soft/Flexible Bioelectronics |
|---|---|---|
| Fibrous Capsule Thickness | ~85.2 ± 12.7 µm [59] | ~28.6 ± 5.4 µm [59] |
| Chronic Signal Stability | Degrades due to micromotion and scar tissue [6] | Stable acquisition over 30 days demonstrated [59] |
| Impedance Change after 10,000 cycles | N/A | ~8.7% increase (Self-healing hydrogel) [59] |
| Resistance Variation under Strain | N/A | ±1.61% (Island-bridge design) [60] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions
| Item | Function/Benefit | Example Application |
|---|---|---|
| Polyimide Film | A common flexible substrate with good thermal and chemical stability. | Fabrication of flexible electrode arrays for neural recording [60]. |
| PDMS (Polydimethylsiloxane) | A soft, stretchable elastomer used as a substrate or an adhesive layer. | Spin-coating as a reversible adhesive to bond flexible films to rigid supports during fabrication [60]. |
| Conductive Hydrogels | Provide mixed ionic/electronic conductivity and mechanical compliance with tissues. | Used as a soft interface layer for stimulation and recording, with self-healing capabilities [59]. |
| PEDOT:PSS | A conductive polymer with excellent biocompatibility and stable electrochemical properties. | Coating on electrodes to lower impedance and improve charge injection capacity [17]. |
| Chromium (Cr) Adhesion Layer | A thin layer to promote adhesion between gold and polymer substrates. | Sputtering a 5 nm layer before gold deposition on polyimide to prevent delamination [60]. |
| MXene-Silk Fibroin Composite | A bioactive coating that scavenges reactive oxygen species to suppress inflammation. | Coating on neural implants to reduce FBR by modulating macrophage activity [59]. |
Advanced Experimental Workflow: Developing a Soft Bioelectronic Interface
The following diagram outlines a comprehensive research and development workflow for creating and validating a soft, bioactive bioelectronic device.
Frequently Asked Questions (FAQs)
Q1: What are the primary biological mechanisms causing inflammation around bioelectronic implants? The primary mechanism is the body's immune response to a foreign object. This often results in fibrotic encapsulation, where the body walls off the implant with scar tissue. This process is driven by chronic inflammation at the implant-tissue interface, which can be exacerbated by mechanical mismatch (e.g., a rigid implant in soft tissue) and leads to the degradation of recording or stimulation fidelity over time [6] [10].
Q2: What clinical metrics are used to quantify implant-induced inflammation? Metrics are specific to the implant site. In dental implants, the modified Plaque Index (mPI) quantifies biofilm accumulation and the modified Sulcus Bleeding Index (mSBI) measures gingival bleeding as a direct sign of inflammation [55]. For neural and other implants, inflammation is often assessed indirectly through signal-to-noise ratio (SNR) degradation in recorded signals and histopathological analysis of fibrotic tissue post-explantation [10].
Q3: What is the bioelectric effect (BE) and how is it applied? The bioelectric effect (BE) uses low-level electrical currents—below 0.82 V to prevent electrolysis—to disrupt biofilm formation and enhance biofilm removal. This technology has been integrated into devices like toothbrushes to manage peri-implant inflammation in dentistry by enabling current to propagate through saliva to reach areas unreachable by bristles [55].
Q4: How do 'circulatronics' devices minimize inflammatory responses? Circulatronics are microscopic, wireless electronic devices that can travel through the bloodstream and self-implant in target regions. They are fused with living cells (e.g., monocytes) before injection, which camouflages them from the immune system. This allows them to cross the blood-brain barrier intact without causing a significant inflammatory reaction and to integrate biocompatibly among neurons [7].
Q5: What are the advantages of soft, flexible bioelectronics over rigid implants? Flexible bioelectronics, made from polymers and elastomers with a Young's modulus matching biological tissues (kPa range), significantly reduce mechanical mismatch. This minimizes chronic inflammation, glial scarring in neural applications, and device failure, enabling more stable long-term integration and signal fidelity [6] [10].
Troubleshooting Common Experimental Issues
Issue 1: Chronic Degradation of Neural Signal Quality
- Problem: Signal-to-noise ratio (SNR) decreases over weeks or months following implantation.
- Potential Cause & Solution: The leading cause is inflammatory tissue response and fibrotic encapsulation due to mechanical mismatch.
- Solution: Utilize flexible neural probes made from soft polymers. These devices have a lower bending stiffness (< 10â»â¹ Nm) and Young's modulus (1 kPa – 1 MPa) that closely match brain tissue, reducing immune response and maintaining stable chronic recordings [10].
Issue 2: Rapid Biofilm Formation on Dental Implant Surfaces
- Problem: Plaque (biofilm) accumulates on implant structures, leading to peri-implant mucositis and bleeding.
- Potential Cause & Solution: Biofilms can form within 8 hours and are difficult to remove from deep pockets.
- Solution: Integrate the bioelectric effect (BE) into cleaning protocols. Clinical trials show that using a BE-integrated toothbrush for 4 weeks significantly reduced the modified Plaque Index (mPI) by 67% and the modified Sulcus Bleeding Index (mSBI) by 59% on implant surfaces [55].
Issue 3: Invasive Surgery for Deep Brain Implants Causes Trauma
- Problem: Traditional implantation of brain devices requires invasive surgery, which can trigger significant inflammation and involves high risk and cost.
- Potential Cause & Solution: The size and delivery method of the implant are traumatic.
- Solution: Employ novel delivery platforms like "circulatronics." These injectable, cell-based hybrid devices can navigate the vasculature to self-implant in precise brain regions, eliminating the need for major surgery and its associated inflammatory response [7].
The tables below summarize key quantitative findings from clinical and experimental studies on inflammatory outcomes.
Table 1: Clinical Outcomes of Bioelectric Effect on Dental Implants
Data from a 4-week clinical trial on patients with dental implants (N=36) comparing a Bioelectric Effect (BE) toothbrush with a non-BE control [55].
| Metric | Surface Type | Baseline Value | 4-Week Value (BE) | Reduction with BE | P-value |
|---|---|---|---|---|---|
| Modified Plaque Index (mPI) | All Surfaces | 1.21 | 0.40 | 67% | < 0.05 |
| Interproximal Surfaces | 1.45 | 0.48 | 67% | < 0.05 | |
| Modified Sulcus Bleeding Index (mSBI) | All Surfaces | 1.32 | 0.54 | 59% | < 0.05 |
| Lingual Surfaces | 1.28 | 0.52 | 59% | < 0.05 |
Table 2: Material Properties and Inflammatory Response of Bioelectronics
Comparison of key properties between traditional rigid and advanced soft/flexible bioelectronic implants [6] [10].
| Property | Rigid Bioelectronics | Soft/Flexible Bioelectronics | Impact on Inflammation |
|---|---|---|---|
| Young's Modulus | > 1 GPa | 1 kPa – 1 MPa | Minimizes mechanical mismatch and tissue irritation. |
| Bending Stiffness | > 10â»â¶ Nm | < 10â»â¹ Nm | Allows conformal contact, reducing micromotion and chronic inflammation. |
| Typical Materials | Silicon, Metals | Polymers, Elastomers, Hydrogels | Improved biocompatibility and reduced foreign body response. |
| Long-Term Signal Fidelity | Degrades due to scar tissue | Stable due to better tissue integration | Maintains functionality for chronic applications. |
Detailed Experimental Protocols
Protocol 1: Evaluating the Bioelectric Effect on Peri-Implant Inflammation
This protocol is based on a clinical study for assessing the efficacy of a bioelectric device in managing inflammation around dental implants [55].
- Objective: To quantify the reduction in plaque accumulation (mPI) and gingival bleeding (mSBI) around dental implants using a BE-integrated toothbrush over a 4-week period.
- Materials:
- BE-integrated toothbrush and an identical non-BE toothbrush (control).
- 36 participants with dental implants (e.g., Osstem implant system).
- Standard dental examination tools for measuring mPI and mSBI.
- Methodology:
- Study Design: Conduct a blind, controlled trial. Randomize participants into two groups: one using the BE toothbrush and the other using the non-BE toothbrush.
- Baseline Measurement: Before the intervention, record the mPI and mSBI for each implant at four locations: facial, mesiofacial, distofacial, and lingual.
- Intervention: Instruct participants to use the assigned toothbrush for a recommended brushing time (e.g., 2.5 minutes) twice daily for 4 weeks.
- Post-Intervention Measurement: After 4 weeks, re-measure the mPI and mSBI indices for all surfaces.
- Data Analysis: Perform statistical analysis (e.g., ANOVA, Chi-square test) to compare the within-group (pre vs. post) and between-group (BE vs. non-BE) differences in mPI and mSBI scores. A P-value of < 0.05 is considered statistically significant.
Protocol 2: Assessing Biocompatibility of Flexible Neural Probes In Vivo
This protocol outlines the evaluation of chronic inflammatory response to flexible neural implants [10].
- Objective: To determine the long-term biocompatibility and inflammatory tissue response to a flexible neural interface compared to a traditional rigid probe.
- Materials:
- Flexible neural probe (e.g., polymer-based).
- Traditional rigid control probe (e.g., silicon Michigan-style probe).
- Animal model (e.g., rodent).
- Histological staining equipment (e.g., for H&E, GFAP, Iba1).
- Electrophysiology recording system.
- Methodology:
- Implantation: Surgically implant both the flexible and rigid probes into the target brain region.
- Chronic Monitoring: Regularly record neural signals (e.g., spikes, local field potentials) over several weeks to months to track signal quality and SNR.
- Histological Analysis: After a predetermined period (e.g., 12 weeks), perfuse the animal and extract the brain.
- Section the brain tissue containing the implant tract.
- Stain sections to visualize neuronal nuclei (NeuN), astrocytes (GFAP), and microglia (Iba1).
- Quantification:
- Signal Fidelity: Calculate the SNR of recorded signals over time and compare the rate of degradation between probe types.
- Immune Response: Quantify the thickness of the glial scar (GFAP+ area) and the density of activated microglia (Iba1+ area) around the implant site.
- Data Analysis: Use statistical tests (e.g., t-test, repeated measures ANOVA) to confirm that flexible probes elicit a significantly reduced inflammatory response and maintain superior signal stability.
Signaling Pathways and Workflow Diagrams
Inflammation Pathway and Interventions
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Inflammation Management in Implant Research
A list of key reagents, technologies, and materials for developing and testing anti-inflammatory strategies for bioelectronic implants.
| Item | Function/Description | Example Use Case |
|---|---|---|
| BE-Integrated Toothbrush | A device that applies a microcurrent (< 0.82 V) to disrupt oral biofilms via the bioelectric effect [55]. | Clinical and pre-clinical management of peri-implant mucositis and inflammation. |
| Flexible Polymer Substrates | Soft materials (e.g., polyimide, PDMS) with low Young's modulus to fabricate neural probes that minimize mechanical mismatch [10]. | Manufacturing chronic neural interfaces that reduce glial scarring and signal loss. |
| Cell-Electronics Hybrids | Living cells (e.g., monocytes) chemically bonded to microscopic electronic devices to create biocompatible, injectable implants [7]. | Creating "circulatronics" for non-surgical, targeted implantation with reduced immune rejection. |
| Piezoelectric Nanogenerators (PENGs) | Self-powered devices that harvest biomechanical energy to provide electrical stimulation, which can support tissue repair and modulate inflammation [62]. | Powering implantable sensors and stimulators for regenerative bioelectronics. |
| High-Density Microelectrode Arrays | CMOS-based neural probes with thousands of electrodes for large-scale, high-resolution recording of neural activity and inflammatory degradation [10]. | Pre-clinical evaluation of inflammatory impacts on neural signal fidelity over time. |
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of a closed-loop system over traditional open-loop bioelectronic therapy? Closed-loop systems continuously monitor physiological states and dynamically adjust therapy in real-time. This allows for personalized, adaptive treatment that can respond to the patient's changing needs. For instance, in epilepsy treatment, responsive neurostimulation delivers therapy only when neural signatures predict a seizure, achieving over 40% seizure reduction while minimizing side effects, unlike continuous stimulation [63].
Q2: Our research team is observing a decline in neural signal quality over time in our chronic implant studies. What are the common causes? Signal degradation is a common challenge often linked to the biological foreign body response. After implantation, the device can trigger inflammation, leading to fibrotic encapsulation (scar tissue formation) that insulates the electrode from the target neural tissue [9]. This is compounded by mechanical mismatch between rigid implant materials and soft, dynamic biological tissues, which can cause chronic inflammation and micromotion that damages the interface [6] [9].
Q3: How can Machine Learning (ML) help manage inflammation in bioelectronic implants? ML can be integrated into the closed-loop system to proactively manage inflammation. The system can use ML models to diagnose the state of the tissue (e.g., from captured wound images) and prescribe a personalized anti-inflammatory therapy, such as a specific electric field strength or drug dosage [64]. This creates an adaptive cycle: measure, diagnose, treat, and re-assess.
Q4: What are the key points of failure we should consider when validating a new implantable closed-loop device? Implanted neural interfaces are complex systems with multiple potential failure points [9]:
- Biological: Acute and chronic immune response (fibrosis, inflammation).
- Mechanical: Lead wire breakage, electrode delamination, macro/micro movements of the device.
- Technical: Battery depletion, electronic component failure in the pulse generator, loss of wireless connectivity, and moisture breach of the hermetic packaging.
Q5: Our team is developing a soft, flexible implant. What are its main advantages and new validation challenges? Advantages: Soft, flexible bioelectronics have a Young's modulus closer to biological tissues (typically 1 kPa – 1 MPa), which significantly reduces mechanical mismatch, minimizes inflammation, and improves long-term signal fidelity and stability [6]. New Challenges: These devices may be more prone to mechanical fatigue at interconnects, delamination in moist environments, and their fabrication can be more complex with lower production yields compared to rigid electronics [6].
Troubleshooting Common Experimental Issues
Table 1: Troubleshooting Common Issues in Closed-Loop Bioelectronic Research
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Biological Response | Excessive fibrotic encapsulation around implant [9] | Body's foreign body response to device material and/or mechanical mismatch. | Explore soft, flexible materials (polymers, elastomers) with a lower Young's modulus to improve biocompatibility [6] [65]. |
| Chronic inflammation at implant site [55] | Biofilm formation on device surface; persistent immune activation. | Integrate anti-biofilm technologies (e.g., bioelectric effect using low-level microcurrents) into the device design [55]. | |
| Technical Performance | Unstable or drifting electrochemical readings [9] | Electrode fouling, degradation of conductive coatings, or failing hermetic seal allowing moisture ingress. | Use stable electrode coatings like Iridium Oxide; perform pre-implantation leak testing of device packaging [9]. |
| Poor signal-to-noise ratio (SNR) in recorded neural data [66] | Signal corruption from noise (e.g., motion artifacts, electromagnetic interference), low-amplitude signals. | Employ machine learning techniques like Transfer Learning (TL) or Convolutional Neural Networks (CNNs) for advanced signal processing and feature extraction [66]. | |
| Data & ML Model | ML model fails to generalize to new subjects [66] | High variability in neural signals between individuals; model overfitted to a small training dataset. | Implement Transfer Learning (TL) to fine-tune pre-trained models for new subjects, reducing the need for long calibration sessions [66]. |
| ML Physician prescribes ineffective therapy [64] | Poor reward function design in the DRL algorithm; inaccurate state representation of the wound. | Redesign the reward function to better reflect therapeutic goals (e.g., use Euclidean distance to an optimal healing trajectory) [64]. |
Experimental Protocols for Key Validation Experiments
Protocol 1: Validating a Closed-Loop Anti-Inflammatory Intervention In Vivo
This protocol outlines the steps to validate an adaptive closed-loop system designed to manage inflammation, based on platforms like the a-Heal system [64].
1. Objective: To demonstrate that a closed-loop system can automatically diagnose a pro-inflammatory state and deliver a bioelectronic therapy (e.g., electric field) to effectively reduce inflammation metrics.
2. Experimental Setup and Materials:
- Animal Model: A large animal model (e.g., porcine) with induced inflammation or a humanized immune-response model [67].
- Closed-Loop Platform: A integrated system consisting of:
- Sensing Module: A real-time biomarker sensor (e.g., cytokine sensor [65] or imaging camera [64]).
- ML Physician: A computer running the diagnostic and control algorithm (e.g., a Deep Reinforcement Learning controller) [64].
- Therapy Delivery Module: A bioelectronic actuator capable of delivering a defined electric field [64].
3. Procedure:
- Step 1: System Calibration. Calibrate the sensor readings against gold-standard measures of inflammation (e.g., ELISA for cytokine levels).
- Step 2: Baseline Data Acquisition. Induce a localized inflammatory response. Collect baseline sensor data and tissue samples for histology.
- Step 3: Closed-Loop Operation. a. The sensor continuously monitors predefined inflammatory biomarkers. b. Sensor data is transmitted to the ML Physician. c. The ML Physician analyzes the data. If biomarker levels exceed a learned threshold, it diagnoses a "high-inflammation" state. d. The ML Physician calculates and prescribes an optimal bioelectric therapy parameters (e.g., 200 µA DC for 15 minutes). e. The prescription is sent to the bioelectronic actuator, which delivers the therapy.
- Step 4: Post-Intervention Assessment. After the therapy cycle, the sensor re-measures biomarkers. This data is fed back to the ML Physician to assess efficacy.
- Step 5: Endpoint Analysis. At the end of the study, collect tissue from the implant site for histological analysis of inflammation and fibrosis, comparing to control groups.
4. Key Measurements:
- Primary: Reduction in target inflammatory biomarkers (e.g., cytokine levels) measured by the integrated sensor.
- Secondary: Histological scores of inflammation and fibrosis; time to resolution of inflammatory state.
Protocol 2: Chronic Biocompatibility and Signal Stability Testing for Soft Implants
1. Objective: To evaluate the long-term reliability and tissue integration of a soft, flexible bioelectronic implant and its impact on signal fidelity.
2. Experimental Setup and Materials:
- Implant Device: A soft, flexible neural electrode array (e.g., made from polymers or ultrathin meshes) with a low bending stiffness (< 10â»â¹ Nm) [6].
- Control Device: A traditional rigid implant (e.g., silicon-based).
- Animal Model: A genetically engineered or humanized animal model appropriate for chronic studies [67].
- Validation Tools: Histology, micro-CT, continuous electrical impedance monitoring.
3. Procedure:
- Step 1: Implantation. Surgically implant both the test and control devices in the target tissue (e.g., brain, peripheral nerve).
- Step 2: In-Life Monitoring. Regularly monitor the following over a period of months: a. Electrical Impedance: Track electrode-tissue interface stability. b. Signal Quality: Record neural signals (if a recorder) to assess signal-to-noise ratio (SNR) and single-unit yield. c. Clinical Observation: Monitor for signs of infection or discomfort.
- Step 3: Terminal Endpoint. a. Perform a final in vivo functional readout. b. Euthanize the animal and perfuse-fix the tissue. c. Explain the devices and surrounding tissue.
4. Key Measurements:
- Primary: Histological quantification of fibrotic capsule thickness and immune cell presence (e.g., macrophages) around the explanted device.
- Secondary: Rate of decline in signal quality/SNR over time; electrode impedance trends; mechanical integrity of the explanted device.
System Workflow and Signaling Pathways
Diagram: Closed-Loop Adaptive Therapy Workflow
Diagram: Key Signaling Pathways in Inflammation and Bioelectric Intervention
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Closed-Loop Bioelectronics Research
| Item Name | Function / Application | Specific Examples / Notes |
|---|---|---|
| Soft Implantable Electrodes | Interfaces with neural or inflamed tissue for stimulation/recording; reduces fibrotic response. | Materials: Polymers, elastomers, hydrogels. Designs: Ultrathin films, flexible meshes, injectable electronics [6] [65]. |
| ML-Algorithm Training Suites | For developing the "ML Physician" for diagnosis and control. | Techniques: Deep Reinforcement Learning (DRL), Autoencoders, Convolutional Neural Networks (CNNs), Transfer Learning (TL) [66] [64]. |
| Genetically Engineered Animal Models (gEAMs) | Preclinical validation in a human-relevant physiological and immune environment. | Types: Immune-humanized mice, humanized porcine models for cardiac implants, osteoporotic rat models [67]. |
| Real-Time Biomarker Sensors | Continuous monitoring of inflammatory state for closed-loop feedback. | Examples: Implantable cytokine sensors [65], wound imaging cameras for visual diagnosis of state [64]. |
| Bioelectronic Actuators | Deliver the prescribed therapeutic intervention (electrical or pharmaceutical). | Examples: Iontophoretic pumps for drug delivery [64], electrodes for applying controlled electric fields (e.g., for Bioelectric Effect) [55]. |
| Stable Electrode Coatings | Improve charge injection and longevity of the electrode-tissue interface. | Materials: Iridium Oxide (IrOx), Platinum-Iridium alloys [9]. |
| Hermetic Packaging Materials | Protect internal electronics from corrosive bodily fluids for long-term stability. | Materials: Titanium housing, ceramic or fused silica feedthroughs [9]. |
FAQ & Troubleshooting Guide
Material Biocompatibility and the Foreign Body Response
Q: What are the key quantitative metrics for assessing Foreign Body Response (FBR) to implantable semiconductors in vivo?
A: A comprehensive FBR assessment requires a multi-fetric approach quantifying both the final fibrotic capsule and underlying immune cell activity. Key metrics and their measurement techniques are summarized in the table below.
Table 1: Key Quantitative Metrics for Assessing Foreign Body Response (FBR)
| Metric Category | Specific Metric | Measurement Technique | Typical Experimental Output |
|---|---|---|---|
| Fibrotic Encapsulation | Collagen Density | Masson's Trichrome Staining & pixel density analysis | ~50% decrease with selenophene backbone; ~68% total decrease with combined backbone/side-chain designs [45] |
| mRNA Expression of Collagen Types | Quantitative PCR (qPCR) | ~20-40% decrease in Collagen I/III (backbone engineering); ~50-70% decrease (combined designs) [45] | |
| Immune Cell Recruitment | Macrophage Population | Immunofluorescence (e.g., CD68 marker) | ~68% decrease in macrophage density [45] |
| Myofibroblast Population | Immunofluorescence (e.g., α-SMA marker) | ~79% decrease in myofibroblast density [45] | |
| Inflammatory Signaling | Pro-inflammatory Biomarkers | Cytokine Assay / PCR (e.g., TNF-α, IFN-γ, IL-6, IL-1β) | Significant downregulation of pro-inflammatory markers [45] |
| Anti-inflammatory Biomarkers | Cytokine Assay / PCR (e.g., IL-10, IL-4) | Upregulation of anti-inflammatory markers [45] |
Experimental Protocol: Evaluating FBR to Polymer Films In Vivo
- Sample Preparation: Fabricate semiconducting polymer thin films on biocompatible substrates (e.g., SEBS).
- Implantation: Implant samples subcutaneously in an animal model (e.g., mouse dorsal region).
- Explanation and Analysis: After predetermined periods (e.g., 1 week, 4 weeks), explant the samples with surrounding tissue.
- Histological Staining: Process tissue for Masson's Trichrome staining to visualize and quantify collagen deposition.
- Immunofluorescence Imaging: Stain tissue sections for specific cell markers (CD68 for macrophages, α-SMA for myofibroblasts) and quantify cell density.
- Genetic and Protein Analysis: Use qPCR to quantify mRNA expression levels of collagen types and key inflammatory cytokines from the tissue surrounding the implant [45].
Q: How can molecular design of semiconducting polymers intrinsically mitigate FBR?
A: Intrinsic immunomodulatory properties can be engineered into semiconducting polymers without sacrificing electronic performance, avoiding the need for coatings that can increase impedance or have limited efficacy [45].
- Backbone Engineering: Incorporating selenophene (replacing thiophene) into the polymer backbone can suppress macrophage activation, potentially via antioxidant effects that scavenge reactive oxygen species (ROS). This single modification reduced collagen density by approximately 50% [45].
- Side-Chain Functionalization: Attaching immunomodulatory groups like triazole-tetrahydropyran (THP) or triazole-thiomorpholine 1,1-dioxide (TMO) to the polymer side chains further downregulates inflammatory biomarkers. When combined with a selenophene backbone, this approach reduced FBR by up to 68% (based on collagen density) while maintaining a charge-carrier mobility of ~1 cm²Vâ»Â¹sâ»Â¹ [45].
Diagram 1: Foreign Body Response (FBR) Cascade to Implanted Materials.
Electrical Performance and Long-Term Stability
Q: What are the primary causes of chronic recording instability in implantable neural probes, and how are they quantified?
A: The gradual degradation of signal quality over time is primarily driven by the biological response to the implant and mechanical mismatch [68].
Biological Failure Modes:
- Gliosis (Glial Scarring): The formation of a dense layer of reactive astrocytes and microglia around the implant. This scar increases the distance between electrodes and neurons and elevates interfacial impedance, leading to a decay in the signal-to-noise ratio (SNR) [68].
- Neuronal Loss: The death of neurons in the immediate vicinity (<100 µm) of the probe, directly reducing detectable signals. This is often caused by chronic inflammation and the neurotoxicity of pro-inflammatory cytokines (e.g., IL-1, TNF-α, IL-6) and free radicals [68].
Key Quantitative Metrics:
- Signal-to-Noise Ratio (SNR): Tracked over weeks and months to monitor signal quality decay.
- Electrode Impedance: Measured regularly; a steady increase often indicates build-up of insulating fibrotic tissue.
- Neuron Count/Sorting Yield: The number of single units (distinct neurons) that can be identified over time [9].
- Immunohistochemical Analysis: Post-explant, tissue is analyzed for biomarkers like GFAP (for astrocytes), Iba1 (for microglia), and NeuN (for neurons) to quantify glial scarring and neuronal density [68].
Q: Our flexible device's electrical performance degrades in the humid biological environment. What are the critical failure modes and tests for encapsulation?
A: Fluid permeation is a major cause of failure for flexible bioelectronics. Effective encapsulation is critical for maintaining long-term functionality [6] [69].
Critical Failure Modes:
- Water Vapor Transmission: Even minute amounts of moisture can corrode thin metal traces and degrade organic semiconductors.
- Delamination: Poor adhesion between different material layers (e.g., conductor-polymer substrate) allows fluid ingress.
- Mechanical Fatigue: Repeated strain from body movement can cause microcracks in encapsulation layers.
Testing and Validation Protocols:
- Accelerated Aging Tests: Devices are incubated in phosphate-buffered saline (PBS) at elevated temperatures (e.g., 57°C, 67°C) to simulate long-term implantation in an accelerated manner. Electrical performance (impedance, functionality) is monitored periodically [69].
- Lifetime Modeling: Data from accelerated aging is used to extrapolate and predict functional lifetime under normal physiological conditions (37°C) using established models like the Arrhenius equation [69].
- Cyclic Mechanical Testing: Devices are subjected to repeated bending or stretching cycles while immersed in saline to test the robustness of the encapsulation and conductors under simulated physiological motion.
Mechanical Stability and Device-Tissue Integration
Q: How does mechanical mismatch between a rigid probe and soft brain tissue contribute to failure?
A: The brain is soft (~kPa), while conventional silicon or metal probes are rigid (GPa). This significant mechanical mismatch causes continuous micro-motion at the tissue-device interface, which [68] [10]:
- Activates Microglia: The primary immune cells of the central nervous system, leading to chronic inflammation [68].
- Disrupts the Blood-Brain Barrier (BBB): Causes leakage of neurotoxic serum proteins and pro-inflammatory factors into the surrounding tissue [68].
- Exacerbates Gliosis and Neuronal Loss: The chronic inflammation and toxicity lead to glial scar formation and neuronal death, which are direct causes of signal degradation [68].
Table 2: Comparison of Rigid vs. Soft/Flexible Bioelectronics
| Property | Rigid Bioelectronics | Soft & Flexible Bioelectronics |
|---|---|---|
| Typical Materials | Silicon, metals, ceramics | Polymers, elastomers, hydrogels, thin-film metals |
| Young's Modulus | > 1 GPa | 1 kPa – 1 MPa |
| Bending Stiffness | > 10â»â¶ Nm | < 10â»â¹ Nm |
| Tissue Integration | Poor; stiffness mismatch causes inflammation and fibrotic encapsulation | Excellent; conformal contact reduces immune response |
| Chronic Signal Fidelity | Degrades over time due to scar tissue | More stable due to reduced scarring and micromotion |
| Key Challenge | Inherent property of classic electronic materials | Prone to mechanical fatigue; complex fabrication [6] |
Q: What design strategies improve the mechanical integration of devices with neural tissue?
A: The field is shifting towards "soft bioelectronics" to blur the distinction between man-made devices and natural tissues [68].
- Ultra-flexible and Ultra-thin Probes: Reducing the device thickness to below 10 µm dramatically decreases bending stiffness, allowing the probe to move with the tissue rather than against it, thereby minimizing micromotion-induced damage [68].
- Mesh and Net-like Designs: Injectable mesh electronics can interpenetrate with the neural tissue, promoting intermingling of neurons and supporting cells with the device structure, which significantly improves integration and stability [68].
- Neutral Mechanical Plane Design: For wearable patch-type devices, placing stiff electronic components (e.g., IC chips) along the neutral mechanical plane of the flexible substrate minimizes strain on these components during bending, enhancing mechanical durability [70].
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents and Materials for Bioelectronic Compatibility Research
| Reagent / Material | Function / Application | Key Characteristics / Rationale |
|---|---|---|
| p(g2T-T) & p(g2T-Se) Polymers | Base semiconducting polymers for organic electrochemical transistors (OECTs) and FBR studies. | p(g2T-Se) incorporates selenophene in the backbone, providing intrinsic immunomodulatory properties and suppressing FBR [45]. |
| THP & TMO Groups | Immunomodulatory side chains for polymer functionalization. | When attached to polymer side chains, these groups downregulate inflammatory biomarkers, further suppressing FBR [45]. |
| Masson's Trichrome Stain | Histological stain for visualizing collagen fibers. | Allows quantification of fibrotic capsule density around explanted devices [45]. |
| CD68 & α-SMA Antibodies | Immunofluorescence markers for macrophages and myofibroblasts, respectively. | Enable quantification of key immune cell populations involved in the FBR cascade [45]. |
| PEDOT:PSS | Conducting polymer for electrodes and OECT channels. | Mixed ionic-electronic conductivity, good biocompatibility, and mechanical flexibility ideal for soft bioelectronics [70]. |
| Parylene-C | A biocompatible polymer used as a thin-film substrate and encapsulation layer. | Provides excellent barrier properties, electrical insulation, and conformality for flexible implants [70]. |
| Neuropixels Probes | High-density silicon-based neural probes for large-scale electrophysiology. | Enable recording from thousands of neurons simultaneously; a benchmark technology for studying recording stability [68] [10]. |
Diagram 2: Experimental Workflow for Implant Evaluation.
Conclusion
Preventing inflammation from bioelectronic implants requires a multifaceted strategy that converges advanced materials science, sophisticated device engineering, and a deep understanding of immunology. The key takeaways affirm that mitigating the Foreign Body Response is paramount for long-term device reliability and can be achieved through mechanical compliance using soft, flexible materials; innovative interfacial designs like 'living electrodes'; and robust, failure-resistant system engineering. Future progress hinges on the development of intelligent, closed-loop systems that dynamically adapt to the biological environment, the clinical translation of minimally invasive or non-surgical implantation techniques, and the creation of novel bioactive materials that actively promote tissue integration rather than passive tolerance. These advancements will not only enhance the safety and efficacy of existing bioelectronic therapies but also unlock new frontiers in personalized, adaptive medicine for chronic neurological, metabolic, and inflammatory diseases.
References
- 1. The Foreign Demystified Body Response [https://pubmed.ncbi.nlm.nih.gov/33405858/]
- 2. Domesticating the Foreign Body Response: Recent Advances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6774350/]
- 3. Understanding the Foreign Body Response via Single-Cell ... [https://www.mdpi.com/2079-7737/13/7/540]
- 4. induced by tissue expander implantation Foreign body response [https://www.spandidos-publications.com/mmr/9/3/872]
- 5. Foreign Body Response to Intravenous Catheter Materials [https://www.accessvascularinc.com/take-action/foreign-body-response-materials]
- 6. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 7. New therapeutic brain implants could defy the need for ... [https://news.mit.edu/2025/new-therapeutic-brain-implants-defy-surgery-need-1105]
- 8. Adhesive anti-fibrotic interfaces on diverse organs [https://www.nature.com/articles/s41586-024-07426-9]
- 9. Overcoming failure: improving acceptance and success of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00168-7]
- 10. Advances in bioelectronics for neural interfacing [https://link.springer.com/article/10.1557/s43579-025-00822-w]
- 11. Towards predicting implant-induced fibrosis: A standardized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312070/]
- 12. Suppression of the fibrotic of silicone encapsulation by... implants [https://www.nature.com/articles/s41551-021-00722-z?error=cookies_not_supported&code=ccaf58e7-18b3-4272-b8bd-11b8153fd3b7]
- 13. Adhesive implant interfaces prevent fibrosis by disrupting... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12157482/]
- 14. Frontiers | Failure behavior of polymer microelectrode arrays... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1622927/full]
- 15. -compliant intracortical Mechanically reduce the... implants [https://pubmed.ncbi.nlm.nih.gov/25125443/]
- 16. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00179-4]
- 17. A nonsurgical brain implant enabled through a cell ... [https://www.nature.com/articles/s41587-025-02809-3]
- 18. The Importance of Controlled Mismatch of Biomechanical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6287196/]
- 19. Anti-Biofouling Strategies for Long-Term Continuous Use ... [https://www.mdpi.com/2227-9040/8/3/66]
- 20. Clinical challenges and opportunities related to the ... [https://www.sciencedirect.com/science/article/pii/S1742706124007566]
- 21. Medical Device-Associated Infections Caused by Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274200/]
- 22. An immobilized liquid interface prevents device associated ... [https://www.sciencedirect.com/science/article/abs/pii/S014296121630535X]
- 23. Nature-inspired surface modification strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11925587/]
- 24. Innovative Bioelectronic Device Offers New Hope in the Fight ... [https://today.ucsd.edu/story/innovative-bioelectronic-device-offers-new-hope-in-the-fight-against-bacterial-infections]
- 25. A computational model for microbial colonization of an ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.920014/full]
- 26. Summer 2025: Soft, Stretchable Hydrogel Bioelectronics for ... [https://aggieresearch.tamu.edu/summer-2025-soft-stretchable-hydrogel-bioelectronics-for-neural-interfacing/]
- 27. Recent Progress in Materials Chemistry to Advance Flexible... [https://pubmed.ncbi.nlm.nih.gov/34751987/]
- 28. Functional electrospun polymeric materials for bioelectronic ... devices [https://pubs.rsc.org/en/content/articlelanding/2022/ma/d1ma01114f]
- 29. Highly conductive polymer with vertical phase separation ... [https://www.nature.com/articles/s41528-025-00441-4]
- 30. Electrically conducting polymers for bio-interfacing ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566320306102]
- 31. Conducting Polymers for Neural Prosthetic ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4681501/]
- 32. Emerging roles of hydrogels, organogels, and their hybrids ... [https://www.nature.com/articles/s44328-025-00055-w]
- 33. Biodegradable Materials and Metallic Implants—A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC5748551/]
- 34. Hydrogels and conductive hydrogels for implantable ... [https://link.springer.com/article/10.1557/s43577-023-00536-1]
- 35. Bio-inspired electronics: Soft, biohybrid, and “living†neural ... [https://www.nature.com/articles/s41467-025-57016-0]
- 36. Development of optically controlled “living electrodes†with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10670819/]
- 37. Tissue engineering tools for modulation of the immune response [https://pmc.ncbi.nlm.nih.gov/articles/PMC3526814/]
- 38. Engineered surface strategies to manage dental implant- ... [https://pubmed.ncbi.nlm.nih.gov/40626507/]
- 39. Surface engineering and advanced coatings [https://www.npl.co.uk/research/advanced-materials/surface-engineering]
- 40. A comprehensive review of functionally graded coatings for ... [https://www.sciencedirect.com/science/article/pii/S2666845925000960]
- 41. Targeted modulation of immune cells and tissues using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10538251/]
- 42. Mechanical failure modes of chronically implanted planar ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4312222/]
- 43. Corrosion and corrosion-fatigue behavior of magnesium ... [https://www.sciencedirect.com/science/article/pii/S2213956723000889]
- 44. Long-term Biocompatibility Assessment of Implantable ... [https://www.hilarispublisher.com/open-access/longterm-biocompatibility-assessment-of-implantable-devices-challenges-and-standards-115351.html]
- 45. Immune-compatible designs of semiconducting polymers for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355568/]
- 46. Top 5 Implantable Bioelectronic Devices Startups to Watch in 2025 [https://www.greyb.com/blog/implantable-bioelectronic-devices/]
- 47. ISO 10993-1:2025 Updates —Top 10 Biological Evaluation ... [https://namsa.com/resources/blog/iso-10993-12025top-10-biological-evaluation-essentials-in-the-update/]
- 48. Issues in Hermetic Sealing of Medical Products [https://www.mddionline.com/product-development/issues-in-hermetic-sealing-of-medical-products]
- 49. Hermetic Seal Definition: Complete Manufacturing Guide [https://amsmachinesinc.com/what-is-hermetic-seal-definition-guide/]
- 50. Conductive Gaskets in Wearable Medical Devices [https://www.modusadvanced.com/resources/blog/conductive-gaskets-in-wearable-medical-devices-miniaturization-challenges]
- 51. Hermetic Packaging Material in the Real World: 5 Uses ... [https://www.linkedin.com/pulse/hermetic-packaging-material-real-world-5-uses-oe2ac/]
- 52. Electrical Enclosure Modern Solutions [https://pti.tech/2025/09/19/conductive-shielded-and-high-performance-plastics-for-electrical-enclosures/]
- 53. Bioelectric medicine: unveiling the therapeutic potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11026362/]
- 54. Nanomaterial-enabled anti-biofilm strategies - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d4nr04774e]
- 55. Bioelectric device for effective biofilm inflammation ... [https://www.nature.com/articles/s41598-023-48205-2]
- 56. The rise of bioelectronic medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11337583/]
- 57. Biofilm microenvironment triggered self-enhancing ... [https://www.nature.com/articles/s41467-023-43067-8]
- 58. The rise of bioelectronic medicine - BioMed Central [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-024-00151-8]
- 59. Recent progress of soft and bioactive materials in flexible ... [https://www.eurekalert.org/news-releases/1103092]
- 60. A comparative study of flexible electrode design on the ... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1632279/full]
- 61. Advances and perspectives in fiber-based electronic ... [https://www.nature.com/articles/s41528-025-00465-w]
- 62. Piezo-electronics: A paradigm for self-powered bioelectronics [https://www.sciencedirect.com/science/article/abs/pii/S0142961225000377]
- 63. How Closed-Loop Systems Will Redefine Cognitive Care [https://vibesbiowear.ai/adaptive-brain-health-how-closed-loop-systems-will-redefine-cognitive-care]
- 64. Towards adaptive bioelectronic wound therapy with ... [https://www.nature.com/articles/s44385-025-00038-6]
- 65. Biohybrid Systems for Better Living | Magazine [https://www.mccormick.northwestern.edu/magazine/spring-2025/biohybrid-systems-for-better-living/]
- 66. Advancing Brain-Computer Interface Closed-Loop Systems for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12588595/]
- 67. Personalized and genetically engineered animal models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577965/]
- 68. Material and design strategies for chronically-implantable ... [https://www.nature.com/articles/s41427-025-00613-8]
- 69. Enhancing Durability of Bioelectronic Implants: Innovations ... [https://www.frontiersin.org/research-topics/63927/enhancing-durability-of-bioelectronic-implants-innovations-in-encapsulation-materials-and-methods]
- 70. Materials strategy and device fabrication for stable closed ... [https://www.nature.com/articles/s44328-025-00045-y]