Computational Models for Neurostimulation Optimization: From Neural Circuits to Personalized Therapies
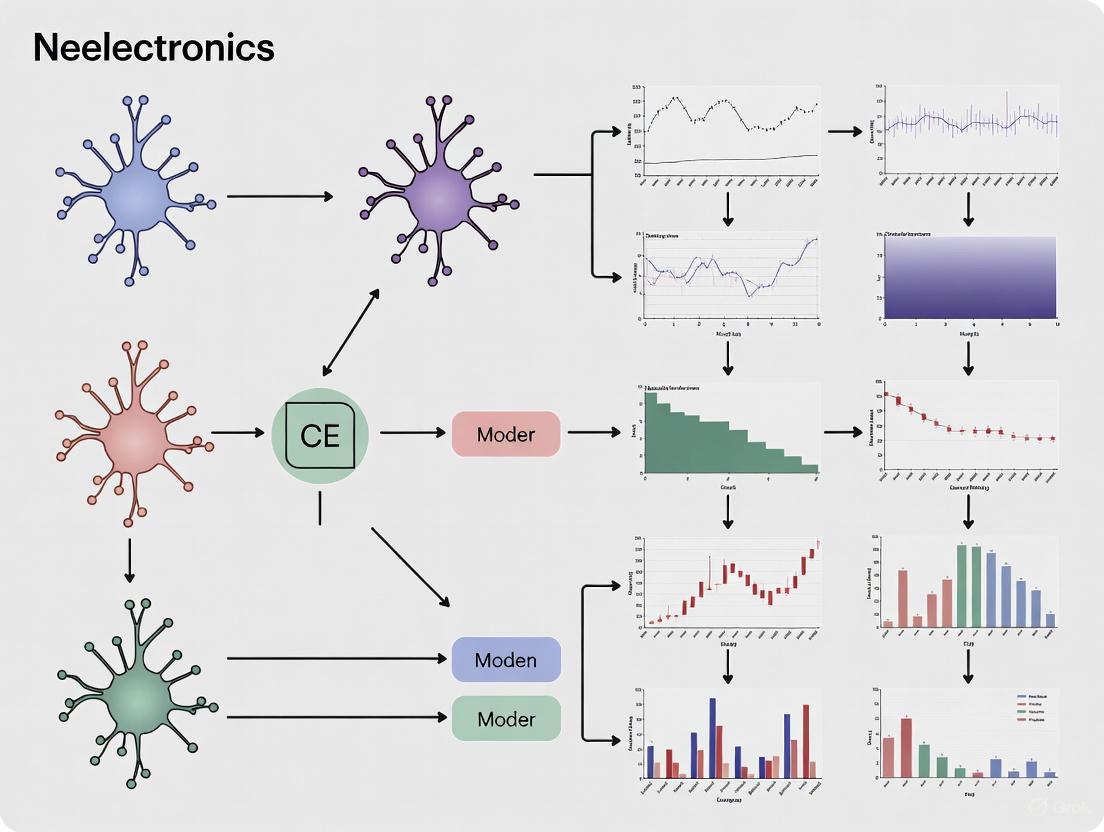
This article explores the transformative role of computational modeling in optimizing neurostimulation for brain disorders.
Computational Models for Neurostimulation Optimization: From Neural Circuits to Personalized Therapies
Abstract
This article explores the transformative role of computational modeling in optimizing neurostimulation for brain disorders. It covers the foundational principles of how models bridge cellular-level processes with disease dynamics, details methodological advances from finite-element analysis to patient-specific virtual platforms, and addresses key challenges in troubleshooting and parameter optimization. A comparative analysis of classical and emerging neuromodulation techniques is provided, highlighting how in silico frameworks accelerate therapeutic discovery and enable closed-loop, AI-driven personalized neuromodulation strategies for conditions ranging from Parkinson's disease to disorders of attention.
Theoretical Foundations: How Computational Models Decode Neurostimulation Mechanisms
Understanding brain diseases requires integrating knowledge across spatial and temporal scales, from the biophysical properties of single neurons to the emergent dynamics of entire brain networks. Computational models are indispensable tools for bridging these scales, providing a framework to formalize hypotheses, incorporate diverse experimental data, and simulate the effects of interventions. A central challenge in the field is that modeling efforts have traditionally occurred in parallel: one class of models focuses on simulating neuronal dynamics (e.g., oscillations, excitability, and connectivity), while another focuses on the biological mechanisms of disease progression (e.g., protein spreading and glial responses) [1]. However, experimental evidence increasingly shows these processes are bidirectionally coupled. Neuronal activity can influence disease progression by, for example, accelerating the transneuronal transport of pathological proteins, while pathology feeds back to disrupt circuit function [1]. This application note outlines integrated computational approaches and detailed protocols to model these interactions, with a particular emphasis on applications in neurostimulation optimization for neurodegenerative diseases and neurological disorders.
Core Computational Frameworks and Their Applications
Modeling Neuronal Dynamics Across Scales
Computational models of neuronal activity during disease aim to simulate and explain functional changes observed via neuroimaging and electrophysiology. These models span from single neurons to whole-brain networks.
Table 1: Computational Models of Neuronal Dynamics in Neurodegeneration
| Model Scale | Core Mathematical Formulation | Key Parameters | Simulated Disease Phenomena | Representative Outputs |
|---|---|---|---|---|
| Single Neuron [1] | ( C\frac{dVi}{dt} = -I{\mathrm{ion}}(Vi, gi) + \sumj w{ij}Sj(t) + I{\mathrm{ext}}(t) ) | Ion channel conductances (( gi )), synaptic weights (( w{ij} )), external drive (( I_{ext} )) | Altered excitability, firing patterns, hyperexcitability | Action potential trains, subthreshold oscillations |
| Neural Mass/Mean-Field [2] [3] | Population firing rate as a function of average membrane potential and input; Kuramoto oscillators for rhythm generation | Synaptic time constants, coupling strength between populations, input from pacemakers (e.g., medial septum) | Theta-gamma phase-amplitude coupling, oscillatory slowing (e.g., reduced alpha/increased theta), hypersynchrony | Local Field Potential (LFP), EEG/MEG spectra, functional connectivity graphs |
| Whole-Brain Network [1] | Coupled neural mass models with inter-regional connectivity defined by the connectome | Structural connectivity matrix, global coupling scaling, transmission delays | Altered functional connectivity (e.g., Default Mode Network disruption), network instability | fMRI BOLD signals, source-localized EEG/MEG dynamics |
Modeling Disease Progression Mechanisms
Beyond neuronal activity, generative models of core disease mechanisms are required to simulate pathology progression.
Table 2: Models of Neurodegenerative Disease Mechanisms
| Modeled Process | Typical Modeling Framework | Key Parameters & Variables | Linked Disease Biology |
|---|---|---|---|
| Prion-like Protein Spreading [1] | Network diffusion models on the connectome; reaction-diffusion equations | Spreading rate, clearance rate, seed location, nodal vulnerability | Accumulation and interneuronal spread of tau, alpha-synuclein, amyloid-beta |
| Glial & Vascular Interactions [1] | Systems of differential equations | Neuroinflammatory signaling, metabolic support, blood flow regulation | Astrocyte dysfunction, microglial activation, neurovascular uncoupling |
| Glymphatic Clearance [1] | Computational fluid dynamics within perivascular spaces | Cerebrospinal fluid flow rate, perivascular space geometry, arterial pulsatility | Impaired clearance of protein waste products, particularly during sleep |
Integrated Frameworks: Bridging Dynamics and Pathology
The most advanced models seek to unify the frameworks described above by creating bidirectional feedback loops between neural activity and disease processes. In such integrated models, neuronal activity can modulate the release and clearance of pathological proteins, while the evolving pathological burden, in turn, alters ion channel function, synaptic efficacy, and cell survival, thereby shaping subsequent neural dynamics [1]. This creates a co-evolutionary process that can capture the progressive nature of neurodegeneration more realistically than unidirectional models.
Detailed Experimental & Simulation Protocols
Protocol 1: Simulating Pathological Theta-Gamma Oscillations and Neurostimulation in a Hippocampal Circuit
Application: This protocol is used to study how neurostimulation affects memory-related oscillations in conditions like Alzheimer's disease and to optimize stimulation parameters [3].
Workflow Diagram: Hippocampal Theta-Gamma Neurostimulation Model
Step-by-Step Methodology:
Model Construction:
- Medial Septum (Pacemaker): Implement a set of abstract Kuramoto oscillators to represent the medial septum. This component generates a dynamical theta rhythm (4-12 Hz) capable of phase reset, as opposed to a simple fixed-frequency input [3].
- Hippocampal Formation (Target): Build a network of biophysically realistic neurons (e.g., using Hodgkin-Huxley formalism) representing key hippocampal subregions. This network should include excitatory and inhibitory populations connected with conductance-based synapses [3].
- Coupling: Connect the Kuramoto oscillator (septal) output to the hippocampal network as an exogenous oscillatory drive.
Model Calibration & Pathological State Induction:
- Healthy Baseline: Adjust the strength of the septal theta drive and the internal synaptic weights within the hippocampal network until the model produces self-sustained theta-nested gamma oscillations, replicating a healthy state [3].
- Inducing Pathology: Weaken the septal theta input or introduce synaptic degradation (e.g., reduce NMDA receptor conductance) to move the network into a "pathological" state. This state is characterized by the absence or severe disruption of theta-gamma oscillations [3].
Neurostimulation Implementation:
- Stimulation Type: Define the stimulation protocol.
- Single-Pulse: A brief, high-amplitude pulse.
- Pulse-Train: A series of pulses delivered at a specific frequency (e.g., theta frequency) [3].
- Stimulation Parameters: Set the amplitude, pulse width, and timing of the stimulation. For closed-loop protocols, define the trigger, such as a specific phase of the ongoing (albeit weak) theta rhythm.
- Stimulation Type: Define the stimulation protocol.
Simulation and Data Analysis:
- Run the simulation and record the local field potential (LFP) and spiking activity from the hippocampal network.
- Quantitative Analysis: Calculate the power spectral density of the LFP to identify dominant rhythms. Use metrics like phase-amplitude coupling (PAC) to quantify the interaction between theta and gamma rhythms. Determine if stimulation successfully restores physiological oscillatory dynamics [3].
Protocol 2: Optimizing Peripheral Nerve Stimulation Using a Surrogate Fiber Model
Application: This protocol accelerates the design and optimization of precise neuromodulation protocols for the vagus nerve (e.g., for epilepsy, depression) and other peripheral nerves (e.g., for chronic pain) [4].
Workflow Diagram: Peripheral Nerve Stimulation Optimization
Step-by-Step Methodology:
Define the Anatomical and Electrical Model:
- Nerve Anatomy: Create a finite element method (FEM) model of the target nerve (e.g., human or pig vagus nerve) including its geometry, fascicles, and surrounding tissue [4].
- Electrode Configuration: Incorporate the geometry and position of the stimulating cuff electrode (e.g., ImThera 6-contact or LivaNova helical cuff) into the FEM model [4].
- Generate Training Data: Use the FEM model to compute the distribution of electric potential within the nerve for a wide range of stimulation parameters (waveform shape, amplitude, pulse width, active contact). Apply these potentials as boundary conditions to a high-fidelity, biophysical nerve fiber model (e.g., the McIntyre-Richardson-Grill (MRG) model in NEURON) to generate a comprehensive dataset of spatiotemporal fiber responses [4].
Develop and Train the Surrogate Model (S-MF):
- Model Architecture: Implement a simplified cable model of a myelinated nerve fiber with trainable parameters. The model should capture the essential nonlinearities of the MRG model but be designed for execution on a GPU [4].
- Training: Use the dataset from Step 1 to train the surrogate model via backpropagation and gradient descent. The goal is for the S-MF to accurately predict the MRG model's responses (e.g., activation threshold, spiking activity) to arbitrary stimulation waveforms [4].
Optimization and Validation:
- Define Objective: State the optimization goal clearly. For example, "activate Fiber Group A while avoiding activation of Fiber Group B within the same nerve."
- Run Optimization: Use the trained S-MF with gradient-based or gradient-free optimization algorithms to search the parameter space (waveform shape, amplitude, contact configuration) for the set that best meets the objective. The computational efficiency of S-MF (providing >2,000x speedup) makes large-scale optimization feasible [4].
- Validate: Test the optimized parameters by running them in the original high-fidelity NEURON model to confirm the predicted outcome [4].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools and Resources
| Tool/Resource Name | Type/Function | Key Application in Multi-Scale Modeling |
|---|---|---|
| NEURON [4] | Environment for detailed single neuron and network simulation | Gold-standard for simulating biophysical neuron models (e.g., MRG fiber); supports extracellular stimulation. |
| Mean-Field / Neural Mass Models [2] [1] | Mathematical framework simulating average activity of neuronal populations | Efficiently simulates EEG/MEG signals and large-scale network dynamics; can be incorporated into whole-brain models. |
| Finite Element Method (FEM) [4] | Numerical technique for solving physical field problems | Calculates the distribution of electric potential in neural tissue during electrical stimulation, crucial for dosing. |
| Kuramoto Oscillators [3] | Mathematical model for describing synchronization in coupled oscillators | Represents pacemaker nuclei (e.g., medial septum) to generate dynamical brain rhythms with phase reset capabilities. |
| AxonML / S-MF Model [4] | GPU-accelerated surrogate model of nerve fibers | Enables rapid, large-scale parameter sweeps and optimization of neurostimulation protocols orders of magnitude faster than NEURON. |
| Patient-Specific Connectomes [5] | Structural connectivity maps of an individual's brain, derived from diffusion MRI | Informs whole-brain network models and prion-like spreading models, allowing for personalized prediction of disease progression and stimulation effects. |
| Duocarmycin SA intermediate-1 | Duocarmycin SA intermediate-1, MF:C30H35IN2O8, MW:678.5 g/mol | Chemical Reagent |
| 2,5-Dimethylpyrazine-d3 | 2,5-Dimethylpyrazine-d3, MF:C6H8N2, MW:111.16 g/mol | Chemical Reagent |
The path to effective neurostimulation therapies for brain diseases lies in embracing the multi-scale, bidirectional complexity of the brain. The integrated computational frameworks and detailed protocols outlined here provide a roadmap for researchers to build models that not only replicate pathological phenotypes but also reveal the mechanistic interplay between neuronal dynamics and disease biology. By leveraging these approaches—from hybrid oscillatory models to highly efficient surrogate fibers—the field can accelerate the rational design of patient-specific neurostimulation protocols that are capable of both restoring function and altering the course of disease progression.
The "informational lesion" concept represents a paradigm shift in understanding deep brain stimulation (DBS), moving beyond simplistic excitation/inhibition models toward a circuit-based framework where high-frequency stimulation masks or disrupts the flow of pathological neural information. This Application Note synthesizes recent advances in DBS mechanisms, focusing on the implications for obsessive-compulsive disorder (OCD) and Parkinson's disease (PD), and provides detailed experimental protocols for investigating these mechanisms. By integrating electrophysiological recordings, computational modeling, and genetically-encoded sensors, researchers can systematically decode how DBS creates informational lesions through differential synaptic depression, antidromic blocking, and network modulation. The protocols outlined herein enable quantitative assessment of presynaptic and postsynaptic dynamics during DBS, facilitating the development of optimized neuromodulation therapies for neurological and psychiatric disorders.
Traditional theories of DBS mechanism oscillated between net excitation and inhibition of neural elements. The "functional lesion" hypothesis suggested DBS inhibits pathological neural activity, similar to ablative procedures but reversibly. This framework has been progressively supplanted by the informational lesion paradigm, which posits that DBS primarily disrupts the transmission of pathological neural signals rather than simply inhibiting or exciting the stimulated nucleus [6] [7].
The informational lesion hypothesis provides a more nuanced explanation for DBS effects, suggesting that high-frequency stimulation prevents neurons from responding to intrinsic oscillations and disrupts pathological network patterns through multiple mechanisms:
- Antidromic blocking: DBS may activate axons antidromically, preventing orthodromic transmission of pathological signals [6]
- Synaptic depression: High-frequency stimulation causes depletion of neurotransmitter release, differentially affecting glutamatergic and GABAergic synapses [8]
- Network resetting: DBS imposes a new, regularized activity pattern that overrides pathological oscillations [6] [9]
This paradigm shift is particularly relevant for psychiatric disorders like OCD, where DBS is thought to disrupt pathological overactivity in cortico-striatal-thalamo-cortical (CSTC) circuits [6]. The informational lesion framework also aligns with the temporal profile of DBS effects in OCD, where immediate improvements in mood and anxiety are followed by more gradual reduction in obsessive-compulsive symptoms, suggesting both immediate neuromodulation and long-term synaptic remodeling [6].
Table 1: Evolution of DBS Mechanism Theories
| Theory | Proposed Mechanism | Key Evidence | Limitations |
|---|---|---|---|
| Functional Lesion | Inhibition of pathological neural activity | Similar effects to ablation; reduced STN output in PD [8] | Cannot explain activation effects; oversimplified |
| Excitation/Inhibition | Net excitation or inhibition of neural elements | Cellular responses to electrical stimulation | Overly simplistic; fails to explain network effects |
| Informational Lesion | Disruption of pathological signal transmission | Antidromic blocking; synaptic depression; network modulation [6] [8] | Complex to measure; multiple simultaneous mechanisms |
| Circuit Modulation | Restoration of natural dynamic communication across brain circuits | Normalization of CSTC hyperactivity in OCD [6] | Circuit interactions not fully characterized |
Quantitative Data Synthesis
Neurophysiological Effects of DBS Across Disorders
Table 2: DBS Outcomes Across Neurological and Psychiatric Disorders
| Disorder | Primary DBS Target | Clinical Efficacy | Cognitive Effects | Mechanistic Insights |
|---|---|---|---|---|
| Parkinson's Disease | STN, GPi | Significant motor improvement [7] | Verbal fluency decline; executive function variably affected [7] | Differential synaptic depression; inhibited STN neurons with activated afferents [8] |
| Obsessive-Compulsive Disorder | Ventral ALIC, NAcc, STN | ~60% response rate; FDA approved under HDE [6] | Cognitively safe; variable across domains [7] | Disruption of pathological CSTC circuit activity [6] |
| Treatment-Resistant Depression | Subcallosal cingulate, MFB | Antidepressant effects, especially MFB target [7] | No decline up to 18 months; mild improvement in memory/attention [7] | Restoration of normative network dynamics |
| Essential Tremor | VIM thalamus | Significant tremor reduction [7] | Occasional verbal fluency decline; other domains largely unaffected [7] | Modulation of cerebello-thalamo-cortical pathways |
| Dystonia | GPi | Significant symptom improvement [7] | Possible decline in processing speed [7] | Suppression of low-frequency (4-12 Hz) GPi oscillations |
Electrophysiological Signatures of Informational Lesions
Table 3: Electrophysiological Markers for DBS Optimization
| Parameter | Measurement Technique | Pathological Signature | DBS Normalization Effect |
|---|---|---|---|
| Beta Oscillations (13-30 Hz) | STN LFP recordings [9] | Elevated beta power in PD [9] | Beta power reduction correlates with motor improvement [9] |
| Low-Frequency Oscillations (4-12 Hz) | GPi LFP recordings [9] | Elevated in dystonia [9] | Suppression correlates with symptom improvement [9] |
| Cortico-Striatal Connectivity | fMRI, EEG/MEG [6] | Overconnectivity in OCD [6] | Reduction correlates with OCD symptom relief [6] |
| Glutamate Release | Fiber photometry with iGluSnFR [8] | Not specified | Profound, intensity-dependent inhibition during DBS [8] |
| GABA Release | Fiber photometry with iGABASnFR [8] | Not specified | Inhibition during DBS, but less than glutamate [8] |
Experimental Protocols
Protocol 1: Assessing Presynaptic and Postsynaptic Dynamics During DBS
Objective: To quantitatively evaluate how DBS differentially affects presynaptic terminal activity versus postsynaptic neuronal activity in target structures.
Background: The informational lesion effect arises from contrasting presynaptic and postsynaptic dynamics. Recent findings show DBS activates afferent axon terminals while inhibiting local neuronal somata, with differential depression of glutamatergic versus GABAergic neurotransmission [8].
Materials:
- Stereotactic surgical apparatus
- Adeno-associated viruses (AAVs) for targeted expression of genetically-encoded indicators
- Hybrid electrode-optical fiber probes for simultaneous stimulation and photometry
- Spectrally-resolved fiber photometry system
- Programmable DBS pulse generator
Methods:
Surgical Preparation and Viral Expression
- Inject AAV9-syn-jGCaMP8f-WPRE into afferent source regions (e.g., M1 cortex for glutamatergic afferents to STN; GPe for GABAergic afferents)
- Inject AAV9-hSyn-DIO-tdTomato into target nucleus (e.g., STN) as fluorescence control
- Allow 3-4 weeks for viral expression and tracer transport
Hybrid Probe Implantation
- Implant custom electrode-optical fiber hybrid probe into target nucleus (e.g., STN)
- Ensure optical fiber tip is placed 0.1-0.2 mm above stimulating electrode tip
- Secure probe with dental acrylic and allow 1-2 weeks recovery
Spectrally-Resolved Fiber Photometry During DBS
- Record baseline fluorescence spectra for 5 minutes pre-stimulation
- Apply DBS using common clinical parameters (130 Hz, 60-μs pulse width, cathodic stimulation)
- Systematically vary stimulation intensity (100, 150, 200 μA) with washout periods between
- Continuously record time-lapsed fluorescence emission spectra throughout stimulation and recovery periods
- Calculate ratio of activity indicator fluorescence (FGCaMP) to control fluorescence (FtdTomato) to control for motion artifacts
Data Analysis
- Compute percent change in F_GCaMP/tdTomato ratio during stimulation versus baseline
- Compare magnitude of effects across stimulation intensities
- Statistically compare presynaptic versus postsynaptic responses
Expected Results: DBS produces sustained activation of presynaptic terminals (increased FGCaMP8f/tdTomato) but inhibition of postsynaptic neuronal activity (decreased FGCaMP6f/tdTomato), with both effects showing intensity-dependence [8].
Protocol 2: Measuring Neurotransmitter-Specific Synaptic Depression
Objective: To quantify DBS-induced changes in glutamate and GABA release in the stimulated nucleus.
Background: The informational lesion effect may involve differential synaptic depression, with greater decrease in glutamate release than GABA release, shifting excitation/inhibition balance toward inhibition [8].
Materials:
- AAV1-hSyn-FLEX-SF-Venus-iGluSnFR.S72A (glutamate sensor)
- AAV1-hSyn-FLEX-iGABASnFR.F102G (GABA sensor)
- AAV9-hSyn-DIO-tdTomato (fluorescence control)
- Hybrid electrode-optical fiber probes
- Spectrally-resolved fiber photometry system
Methods:
Sensor Expression
- Inject AAV1-hSyn-FLEX-SF-Venus-iGluSnFR.S72A and AAV9-hSyn-DIO-tdTomato into target nucleus (e.g., STN) of Vglut2-cre mice for glutamate measurements
- In separate cohort, inject AAV1-hSyn-FLEX-iGABASnFR.F102G and AAV9-hSyn-DIO-tdTomato for GABA measurements
- Allow 3-4 weeks for viral expression
Probe Implantation and Photometry
- Implant hybrid electrode-optical fiber probe into target nucleus
- Record baseline neurotransmitter sensor fluorescence (FVenus-iGluSnFR or FiGABASnFR) and control fluorescence (F_tdTomato)
- Apply DBS at varying intensities (100, 150, 200 μA) with standard parameters
- Continuously monitor fluorescence ratios during stimulation
Quantitative Analysis
- Calculate percent change in F_sensor/tdTomato ratio during DBS
- Compare magnitude of glutamate versus GABA release inhibition
- Determine intensity-dependence of synaptic depression
Expected Results: DBS causes profound, intensity-dependent inhibition of both glutamate and GABA release, with significantly greater depression of glutamatergic transmission, shifting excitation/inhibition balance toward inhibition [8].
Protocol 3: Mapping Circuit-Level Effects of Informational Lesions
Objective: To characterize how DBS creates informational lesions by modulating pathological network activity across distributed brain circuits.
Background: In OCD, DBS is thought to disrupt pathological overactivity in CSTC circuits [6]. Simultaneous electrophysiological recordings across multiple nodes can reveal how DBS creates informational lesions by normalizing network dynamics.
Materials:
- Multi-channel electrophysiology system
- Multi-site electrode arrays or simultaneous EEG/MEG-LFP setups
- Computational tools for connectivity analysis
Methods:
Multi-Site Recording Preparation
- Implant recording electrodes in key nodes of target circuit (e.g., for OCD: OFC, striatum, thalamus; for PD: STN, GPi, cortex)
- For non-invasive components, use high-density EEG or MEG co-registered with structural MRI
- Ensure precise temporal synchronization across all recording modalities
Network Activity Characterization
- Record baseline neural activity across nodes during rest and relevant behavioral tasks
- For OCD studies: measure CSTC circuit activity during symptom provocation
- For PD studies: measure beta oscillations during rest and movement
DBS Application and Network Monitoring
- Apply therapeutic DBS to target nucleus (e.g., ventral ALIC for OCD, STN for PD)
- Simultaneously record network activity across all nodes during stimulation
- Systematically vary DBS parameters (frequency, intensity, pulse width)
Connectivity and Information Flow Analysis
- Compute functional connectivity metrics (coherence, phase-locking value) between nodes
- Measure directionality of information flow (Granger causality, directed transfer function)
- Quantify changes in pathological oscillations (e.g., beta power in PD)
- Assess normalization of network dynamics relative to clinical improvement
Expected Results: Effective DBS normalizes pathological network activity by reducing overconnectivity in hyperactive circuits (e.g., CSTC in OCD), suppressing pathological oscillations (e.g., beta in PD), and restoring more natural information flow patterns [6] [9].
Visualization of Mechanisms and Methodologies
Informational Lesion Mechanisms in DBS
Experimental Workflow for DBS Mechanism Investigation
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for DBS Mechanism Investigations
| Reagent / Tool | Specifications | Research Application | Key Features |
|---|---|---|---|
| Genetically-Encoded Calcium Indicators | AAV9-syn-jGCaMP8f-WPRE; AAV9-hSyn-DIO-GCaMP6f-WPRE | Monitoring neural activity in specific cell populations | High sensitivity; cell-type specific expression; compatible with fiber photometry |
| Neurotransmitter Release Sensors | AAV1-hSyn-FLEX-SF-Venus-iGluSnFR.S72A (glutamate); AAV1-hSyn-FLEX-iGABASnFR.F102G (GABA) | Real-time measurement of neurotransmitter release | Specific to neurotransmitter type; high temporal resolution |
| Fluorescence Control Reporters | AAV9-hSyn-DIO-tdTomato | Control for motion artifacts and non-specific effects | Spectrally distinct from activity sensors; enables ratio-metric measurements |
| Hybrid Stimulation-Recording Probes | Custom electrode-optical fiber assemblies | Simultaneous DBS delivery and optical monitoring | Precise co-localization of stimulation and recording sites; minimal artifact |
| Computational Modeling Platforms | o2S2PARC; Sim4Life.web [10] | In silico testing of DBS parameters and mechanisms | Cloud-native; integrates EM modeling with neuronal dynamics; regulatory-grade |
| Personalized Optimization Algorithms | Bayesian Optimization (pBO) frameworks [11] | Individualized DBS parameter selection | Accounts for anatomical and functional individual differences; efficient parameter space exploration |
| Gamma-6Z-Dodecenolactone-d2 | Gamma-6Z-Dodecenolactone-d2, MF:C12H20O2, MW:198.30 g/mol | Chemical Reagent | Bench Chemicals |
| Fmoc-Gly-Gly-allyl propionate | Fmoc-Gly-Gly-allyl propionate, MF:C25H26N2O7, MW:466.5 g/mol | Chemical Reagent | Bench Chemicals |
The informational lesion paradigm represents a fundamental shift in understanding DBS mechanisms, emphasizing disruption of pathological information flow rather than simple inhibition or excitation. The experimental protocols outlined herein enable researchers to quantitatively investigate these mechanisms across spatial scales - from synaptic-level neurotransmitter dynamics to circuit-level network interactions. As the field advances, computational models that integrate these multi-scale effects will be essential for developing truly personalized DBS therapies that optimize informational lesion creation while minimizing side effects. Future research should focus on closed-loop DBS systems that dynamically adjust stimulation parameters based on real-time biomarkers of pathological information flow, ultimately creating more effective and efficient neuromodulation therapies for neurological and psychiatric disorders.
Mechanistic Modeling for Target Identification in Parkinson's, Epilepsy, and Migraine
The development of effective therapies for complex neurological disorders is often hampered by the intricate and multifactorial nature of their underlying pathophysiology. For Parkinson's disease, epilepsy, and migraine, the precise neural mechanisms triggering symptoms remain incompletely understood, creating a critical bottleneck in therapeutic development. Within this context, computational modeling has emerged as a transformative tool, providing a virtual platform to dissect disease mechanisms, identify critical therapeutic targets, and optimize intervention strategies. These models serve as in-silico testbeds that tame biological complexity, from molecular interactions to large-scale neural network dynamics, offering a principled path toward personalized neuromodulation therapies. This article details specific application notes and experimental protocols for employing mechanistic models in target discovery across these three neurological conditions, framed within a broader research agenda on computational neurostimulation optimization.
Application Notes & Experimental Protocols
Parkinson's Disease: Targeting Basal Ganglia Circuit Dynamics and α-Synuclein Homeostasis
Parkinson's disease (PD) is characterized by the progressive loss of dopaminergic neurons and the pathological accumulation of α-synuclein (αsyn) protein. Computational models provide key insights into both the circuit-level and molecular-level dysfunction driving the disease.
Table 1: Key Computational Insights and Targets in Parkinson's Disease
| Modeling Level | Key Insight | Identified Target/Mechanism | Therapeutic Implication |
|---|---|---|---|
| Circuit Dynamics | Excessive beta-band oscillations arise from cortex-STN-GPe resonance [12] [13] | Cortico-subthalamic hyperdirect pathway; STN-GPe loop | Targets for deep brain stimulation (DBS) to disrupt pathological oscillations [12] [14] |
| Dopamine Signaling | Loss of phasic, not tonic, dopamine drives early motor deficits [12] | Phasic dopamine signaling and its signal-to-noise ratio | Strategies to restore patterned, rather than continuous, dopamine signaling |
| Protein Homeostasis | Positive feedback loops between αsyn aggregation and degraded clearance [15] | Autophagy-lysosome pathway (ALP); Ubiquitin-Proteasome Pathway (UPP) | Small molecule inhibitors of aggregation; enhancers of ALP/UPP activity [15] |
Protocol 1: Developing a Model of α-Synuclein Homeostasis
- Objective: To build a mechanistic model that simulates the interplay between αsyn aggregation and cellular degradation pathways to identify critical control points for intervention.
- Background: The pathological aggregation of αsyn and the impairment of its clearance mechanisms are central to PD. Kinetic models integrate processes like nucleation, elongation, and fragmentation of αsyn aggregates with degradation pathways such as the ubiquitin-proteasome system (UPS) and autophagy-lysosome pathway (ALP) [15].
- Methodology:
- Model Formulation: Use a system of ordinary differential equations (ODEs) to represent the concentrations of different αsyn species (monomer, oligomer, protofibril, fibril). Key reactions include primary nucleation ($v{nuc}$), elongation ($v{elong}$), and fragmentation ($v_{frag}$) [15].
- Incorporate Degradation: Introduce terms for the degradation of each αsyn species via UPS ($v{UPS}$) and ALP ($v{ALP}$). Model the known inhibitory effects of oligomers on proteasomal activity and of fibrils on ALP flux [15].
- Parameter Estimation: Calibrate model parameters (e.g., rate constants) against in vitro kinetic data of αsyn aggregation and clearance from the literature.
- Therapeutic Simulation: Simulate interventions such as: (a) introducing an aggregation inhibitor (reducing $v{elong}$), (b) enhancing ALP activity (increasing $v{ALP}$), and (c) combined strategies. Analyze the effect on steady-state levels of toxic oligomeric species.
- Expected Outcome: The model will identify which intervention, or combination thereof, most effectively reduces the burden of toxic αsyn species, providing a ranked list of promising therapeutic targets.
Diagram 1: α-synuclein aggregation and clearance pathways with intervention points.
Epilepsy: Identifying Seizure Onset and Suppression Targets
In epilepsy, particularly medically refractory forms, computational models help pinpoint the origins of hypersynchrony and guide the development of targeted neurostimulation protocols for seizure suppression.
Table 2: Computational Approaches for Seizure Identification and Control in Epilepsy
| Modeling Approach | Primary Application | Identified Target/Mechanism | Therapeutic Implication |
|---|---|---|---|
| Large-Scale Network Models | Understand hyperexcitability from cell death and altered connectivity [16] | "Hub" neurons with aberrant high connectivity [16] | Focal ablation or silencing of hyper-connected hub cells |
| System Identification (SI) & Control | Reconstruct and mitigate seizures from real patient data [17] | State-space models derived from interictal/ictal EEG/LFP | Customized electrical stimuli for seizure suppression [17] |
| Mean-Field Neural Mass Models | Simulate macroscopic seizure dynamics and bifurcations [18] | Key parameters controlling transition to seizure (e.g., excitatory gain) | Open-loop or closed-loop DBS parameter optimization |
Protocol 2: Data-Driven Seizure Suppression via System Identification and Control
- Objective: To construct a patient-specific model from electrophysiological recordings and design a control input to suppress epileptiform activity.
- Background: System identification (SI) techniques can translate real brain signals (e.g., local field potentials) into mathematical models. These models can be used to design controllers that compute electrical stimuli to drive the brain state from a seizure (ictal) to a non-seizure (interictal) condition [17].
- Methodology:
- Data Acquisition & Preprocessing: Obtain intracranial EEG (iEEG) or local field potential (LFP) recordings from patients, containing both ictal and interictal segments. Filter the data to remove artifacts.
- Model Identification: Fit an Autoregressive (AR) model to the preprocessed signal. The order of the model is determined using criteria like Akaike Information Criterion (AIC). The AR model, which predicts the current signal value based on its past values, is given by: $y(t) = a1 y(t-1) + a2 y(t-2) + ... + ap y(t-p) + e(t)$ where $y(t)$ is the signal, $ai$ are the model coefficients, $p$ is the model order, and $e(t)$ is the error term [17].
- State-Space Conversion: Convert the identified AR model into a state-space representation. This format is essential for control theory applications and allows for the design of observers and controllers.
- Controller Design: Design a state-feedback controller (e.g., a linear-quadratic regulator - LQR). The controller calculates an optimal electrical stimulus $u(t)$ based on the estimated state of the system $x(t)$ to minimize a cost function that penalizes both seizure activity and control effort [17].
- In-Silico Validation: Simulate the closed-loop system (plant + observer + controller) to verify its efficacy in suppressing the simulated epileptiform activity before moving to pre-clinical or clinical testing.
- Expected Outcome: A patient-specific state-space model and an associated control law that can be implemented in a closed-loop neurostimulation device to deliver personalized seizure suppression therapy.
Diagram 2: Workflow for data-driven seizure model identification and control.
Migraine: Uncovering Genetic and Molecular Targets
Migraine is a complex disorder with a strong genetic component. Modern computational approaches integrate large-scale genomic data to pinpoint causal genes and pathways, offering new avenues for drug discovery and repurposing.
Table 3: Multi-Omics Insights for Target Identification in Migraine
| Computational Method | Data Input | Key Finding | Implication for Target Discovery |
|---|---|---|---|
| Machine Learning (ML) on snRNA-seq | snRNA-seq from 43 brain regions; GWAS data [19] | Enrichment in PoN_MG thalamus; calcium signaling pathway (Gene Program 1) | ARID3A transcription factor and calcium-related genes as regulators [19] |
| Integrated GWAS-eQTL-PheWAS | GWAS summary stats; multi-tissue eQTLs; PheWAS [20] | 31 blood and 20 brain migraine-associated genes; 13 druggable genes | Prioritized targets: NR1D1, THRA, NCOR2, CHD4 for drug development [20] |
| Meta-Learning for CGRP Inhibition | Chemical compounds from ChEMBL [21] | High-accuracy prediction of CGRP-inhibiting compounds (MetaCGRP model) | Accelerates screening of natural products and small molecules for migraine [21] |
Protocol 3: An Integrated Multi-Omics Pipeline for Migraine Target Prioritization
- Objective: To systematically identify and prioritize druggable gene targets for migraine by integrating genetic, transcriptomic, and phenomic data.
- Background: Genome-wide association studies (GWAS) identify loci associated with migraine, but linking these to causal genes and druggable targets requires integration with functional genomic data. This protocol uses Summary-data-based Mendelian Randomization (SMR) to test for putative causal genes, followed by rigorous validation [20].
- Methodology:
- Data Integration: Obtain migraine GWAS summary statistics and expression Quantitative Trait Loci (eQTL) data from relevant tissues (e.g., whole blood and multiple brain regions from GTEx, eQTLGen, PsychENCODE) [20].
- Causal Gene Identification: Perform SMR analysis to test for association between the genetic component of gene expression and migraine risk. Follow with HEIDI test to exclude pleiotropy. Genes passing a False Discovery Rate (FDR) < 0.05 and HEIDI p-value > 0.05 are considered putative causal [20].
- Druggability Assessment: Cross-reference the list of putative causal genes with druggable genome databases (e.g., DGIdb). Annotate genes with known drug targets or those belonging to druggable protein families.
- Validation and Prioritization:
- Colocalization Analysis: Assess if the GWAS and eQTL signals share a single causal variant (posterior probability > 0.8).
- Phenome-Wide Association Study (PheWAS): Screen prioritized genes against a wide range of phenotypes to assess potential on-target side effects.
- Protein-Protein Interaction (PPI) Network: Map prioritized genes onto PPI networks to identify hub proteins and explore connections to known migraine pathways.
- Expected Outcome: A shortlist of high-confidence, druggable target genes for migraine (e.g., NR1D1, THRA), along with an assessment of their potential safety profile, ready for experimental validation in cellular or animal models.
Diagram 3: Multi-omics pipeline for migraine target discovery and prioritization.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Computational Tools and Resources for Neurological Target Identification
| Tool/Resource Name | Type | Primary Function | Application Example |
|---|---|---|---|
| NEURON [16] | Simulation Environment | Biophysically detailed simulations of neurons and networks | Modeling microcircuit changes in epileptic dentate gyrus [16] |
| ModelDB [16] [13] | Online Database | Repository of published, peer-reviewed computational models | Accessing and sharing models of Parkinsonian beta oscillations [13] |
| CELLEX [19] | Algorithm | Calculates cell-type-specific expression profiles from snRNA-seq data | Identifying region-specific gene expression in migraine [19] |
| SMR/HEIDI [20] | Statistical Tool | Performs Mendelian Randomization to find putative causal genes | Integrating GWAS and eQTL data for migraine target discovery [20] |
| DGIdb [20] | Database | Information on druggable genes and drug-gene interactions | Filtering candidate genes for druggability potential [20] |
| MetaCGRP [21] | Machine Learning Model | Predicts CGRP-inhibiting compounds from SMILES notation | Virtual screening of natural products for anti-migraine activity [21] |
| GLP-1 receptor agonist 13 | GLP-1 receptor agonist 13, MF:C25H23ClF2N6O, MW:496.9 g/mol | Chemical Reagent | Bench Chemicals |
| TCO-GK-PEG4-NHS ester | TCO-GK-PEG4-NHS ester, MF:C33H52N4O14, MW:728.8 g/mol | Chemical Reagent | Bench Chemicals |
Leveraging Neuroimaging and Connectomics to Inform Anatomically Accurate Models
Computational models are revolutionizing our approach to understanding brain function and developing neuromodulation therapies. However, the predictive power and clinical translatability of these models are fundamentally constrained by their biological accuracy. This protocol details the methodology for leveraging non-invasive neuroimaging and connectomics data to build and constrain anatomically precise computational models of brain dynamics. The framework is designed to integrate individual brain architecture, thereby enabling the in-silico optimization of neurostimulation parameters for personalized therapeutic interventions. This process directly addresses the critical translational gap in neuromodulation by providing a mechanistic bridge between brain structure, function, and stimulation outcome [22] [23].
Application Notes: Core Principles and Rationale
The Role of Computational Modeling in Neurostimulation
Incorporating computational models into neuroimaging analytics provides a mechanistic link between empirically observed neural phenomena and abstract mathematical concepts such as attractor dynamics, multistability, and bifurcations [22]. This is particularly vital for neurostimulation, where understanding the transition between brain states is key. Models allow for a thorough exploration of the parameter space—including stimulation intensity, location, and frequency—that is logistically and ethically intractable to probe comprehensively through experimentation alone [22]. For instance, optimization frameworks have been developed for Spinal Cord Stimulation (SCS) that use computational models to rapidly calculate optimal current amplitudes across electrode contacts, a process that would be prohibitively slow and inefficient in a clinical setting [24].
The Necessity of Anatomical Constraint
A "one-size-fits-all" approach to neurostimulation often leads to inconsistent outcomes because it fails to account for inter-individual variability in brain anatomy and network organization [11]. Individual differences in head size and anatomy significantly influence the amount of current that reaches neural tissue [11]. Computational models that are informed by individual structural data can account for this variability. The integration of structural connectomes, derived from dMRI, ensures that the model's wiring diagram reflects the actual physical architecture of an individual's brain, leading to more accurate predictions of stimulation effects [22].
Experimental Protocols
Protocol 1: Acquiring the Structural and Functional Connectome
Objective: To reconstruct the individual's structural brain network and map intrinsic functional networks to serve as a scaffold for computational modeling.
Materials and Reagents:
- Magnetic Resonance Imaging (MRI) scanner (3T minimum, 7T preferred for higher resolution).
- T1-weighted MPRAGE sequence protocol.
- Diffusion-weighted MRI (dMRI) sequence protocol (multi-shell, high angular resolution preferred).
- Resting-state functional MRI (fMRI) sequence protocol (EPI BOLD).
- MRI-compatible headphones and padding to minimize head motion.
- Electroencephalography (EEG) system (optional, for complementary temporal data).
Procedure:
- Structural Scan: Acquire a high-resolution T1-weighted anatomical scan (e.g., MPRAGE, voxel size ~1mm³). This image will be used for tissue segmentation and as a reference for aligning other scans.
- Diffusion MRI: Acquire dMRI data using a multi-shell diffusion-encoded sequence. A high number of diffusion directions (e.g., 64+ per shell) is recommended for robust fiber orientation modeling.
- Resting-State fMRI: Acquire a 10-15 minute BOLD fMRI scan while the participant is at rest with eyes open, fixating on a crosshair. Instruct the participant to remain awake and still.
- Preprocessing:
- T1 Processing: Perform brain extraction, tissue segmentation (gray matter, white matter, cerebrospinal fluid), and cortical surface reconstruction using tools like FreeSurfer or FSL.
- dMRI Processing: Correct dMRI data for eddy currents, head motion, and susceptibility-induced distortions using tools like FSL's
eddyandtopup. - fMRI Processing: Discard initial volumes for signal equilibrium, apply slice-timing correction, realign volumes for motion correction, and co-register to the T1 image. Perform additional nuisance regression (white matter, CSF signals, motion parameters) and band-pass filtering (typically 0.01-0.1 Hz).
- Tractography and Structural Connectivity (SC):
- Reconstruct the white matter fibers using a tractography algorithm (e.g., probabilistic tractography in FSL's ProbtrackX or deterministic in MRtrix3).
- Parcellate the brain into distinct regions of interest (ROIs) using a standard atlas (e.g., Desikan-Killiany, AAL) warped to the individual's T1 space.
- Generate an SC matrix where each element (i,j) represents the density of reconstructed streamlines between regions i and j.
- Functional Connectivity (FC):
- Extract the mean BOLD time series from each ROI defined in the parcellation.
- Compute the pairwise Pearson correlation coefficients between all regional time series to create a symmetric FC matrix.
Protocol 2: Building and Personalizing the Whole-Brain Model
Objective: To create a biologically realistic, large-scale computational model where the simulated neural dynamics are constrained by the individual's SC and FC.
Materials and Software:
- High-performance computing (HPC) cluster or workstation.
- Computational modeling software (The Virtual Brain, NEST, or custom code in Python/MATLAB).
- Processed SC and FC matrices from Protocol 1.
Procedure:
- Model Selection: Choose a neural mass model (NMM) to represent the dynamics of each brain region. Common choices include the Wilson-Cowan model, the Jansen-Rit model for EEG rhythms, or the reduced Wong-Wang model for fMRI.
- Model Parameterization:
- Set the structural connectivity matrix from dMRI tractography as the coupling weights between network nodes.
- Incorporate a global coupling parameter (G) that scales the entire SC matrix.
- Include other key parameters such as the synaptic excitation-inhibition balance and conduction delays (estimated from inter-regional fiber lengths).
- Model Personalization and Fitting:
- Simulate the model's BOLD signal using a hemodynamic forward model (e.g., Balloon-Windkessel).
- Compare the simulated FC (the matrix of correlations between simulated BOLD signals of all regions) with the empirical FC from resting-state fMRI.
- Use a global optimization algorithm (e.g., Bayesian optimization, genetic algorithm) to fit the model parameters (like G) by maximizing the similarity between the simulated and empirical FC. The Pearson correlation between the upper triangles of the two FC matrices is a common cost function.
Table 1: Key Parameters for Whole-Brain Model Fitting
| Parameter | Description | Fitting Method |
|---|---|---|
| Global Coupling (G) | Scales the overall strength of input from other nodes. | Optimized to match empirical FC. |
| Signal Transmission Speed | Determines inter-regional conduction delays. | Typically derived from fiber length and a fixed velocity. |
| Local Excitatory-Inhibitory Balance | Governs local node dynamics and oscillatory properties. | Can be optimized or set from literature values. |
| Node Noise | Represents unresolved inputs and background activity. | Fixed to a low level or optimized. |
Protocol 3: In-Silico Optimization of Neurostimulation
Objective: To use the personalized model to predict the optimal stimulation parameters for a given individual and cognitive/clinical target.
Materials and Software:
- Personalized whole-brain model from Protocol 2.
- Finite Element Method (FEM) model of the head and brain.
- Optimization toolbox (e.g., SciPy in Python).
Procedure:
- Electric Field Modeling:
- Create an individual-specific head model (including skin, skull, CSF, gray matter, white matter) from the T1 image.
- Position the simulated neurostimulation electrodes (e.g., for tES or TMS) on the scalp according to the desired montage.
- Use FEM software (e.g, SimNIBS, ROAST) to calculate the electric field (E-field) distribution in the brain for a given stimulation intensity.
- Stimulation Input:
- Map the computed E-field onto the brain parcellation to define the region-specific stimulation input. The input to each node in the model is proportional to the average E-field magnitude in that region.
- Define Optimization Goal:
- Formulate a clear objective. For example: "Maximize the functional connectivity between the left dorsolateral prefrontal cortex (dlPFC) and the parietal cortex," or "Shift the whole-brain FC pattern towards a healthy template."
- Run In-Silico Trials:
- Simulate the personalized model under a wide range of stimulation parameters (e.g., intensity from 0.5 mA to 2.0 mA, multiple electrode montages).
- For each parameter set, compute the objective function (e.g., change in target FC strength).
- Parameter Optimization:
- Employ an optimization algorithm, such as Bayesian Optimization (BO), to efficiently navigate the high-dimensional parameter space. BO is ideal for this purpose as it builds a probabilistic model of the objective function and aims to find the global optimum with relatively few simulations [11].
- The output is a set of personalized stimulation parameters predicted to maximize the desired neural effect.
Table 2: In-Silico Optimization Parameters for Transcranial Electrical Stimulation
| Parameter | Role in Optimization | Considerations |
|---|---|---|
| Stimulation Intensity | Primary driver of electric field magnitude. | Follows an inverted U-shape effect; personalized BO can identify the individual "sweet spot" [11]. |
| Electrode Montage | Determines the spatial pattern of the E-field. | Multi-electrode montages create a vast search space, necessitating efficient optimizers [24]. |
| Stimulation Frequency | Targets specific neurophysiological rhythms. | tRNS may benefit lower performers via stochastic resonance [11]. |
| Stimulation Target | The brain region or network to be modulated. | Defined a priori based on the cognitive or clinical target (e.g., dlPFC for attention). |
The following diagram illustrates the integrated workflow from data acquisition to optimized stimulation parameters.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Resources for Connectome-Informed Modeling
| Tool/Resource | Type | Primary Function |
|---|---|---|
| FreeSurfer | Software Suite | Automated cortical surface reconstruction and brain parcellation from T1-weighted MRI. |
| FSL | Software Suite | A comprehensive library for dMRI and fMRI data analysis, including tractography and connectivity mapping. |
| The Virtual Brain (TVB) | Simulation Platform | A open-source platform for constructing and simulating personalized whole-brain network models. |
| SimNIBS | Software Tool | Calculates the electric field distribution in the brain generated by TMS or tES using individual head models. |
| High-Performance Computing (HPC) Cluster | Hardware | Provides the computational power required for running thousands of simulations for model fitting and parameter optimization. |
| Bayesian Optimization Library (e.g., Scikit-Optimize) | Software Library | Implements efficient optimization algorithms for navigating high-dimensional parameter spaces with limited samples. |
| 2'-Deoxycytidine-13C9 | 2'-Deoxycytidine-13C9, MF:C9H13N3O4, MW:236.15 g/mol | Chemical Reagent |
| Taltobulin intermediate-11 | Taltobulin intermediate-11, MF:C17H25NO4, MW:307.4 g/mol | Chemical Reagent |
The following diagram maps the logical relationships and data flow between the key tools in the research pipeline.
Methodologies in Practice: Building and Applying Computational Frameworks
Multi-scale computational modeling has emerged as a transformative approach in neuroscience, bridging microscopic neuronal processes with macroscopic brain network dynamics to advance neurostimulation optimization. This framework integrates diverse computational techniques—from biophysically detailed single-neuron models to population-level approaches—enabling researchers to uncover mechanisms underlying brain function and pathology while accelerating therapeutic development. This application note provides a comprehensive technical resource detailing methodologies, protocols, and tools for implementing multi-scale modeling approaches, with particular emphasis on their application in neurostimulation research. We present structured quantitative comparisons, experimental workflows, and standardized protocols to support researchers in developing clinically relevant computational models for optimizing neuromodulation therapies.
The brain's complex organization spans multiple spatial and temporal scales, from molecular processes within individual neurons to large-scale networks governing cognitive functions and behavior [25]. Multi-scale computational modeling systematically addresses this complexity by integrating representations across hierarchical levels of neural organization, creating bridges between disparate experimental datasets and facilitating mechanistic insights that cannot be derived from any single scale alone [25] [26]. These approaches have become indispensable for understanding how microscopic phenomena (e.g., ion channel dynamics, synaptic transmission) influence macroscopic brain activity and, ultimately, behavior in both health and disease [25].
In neurostimulation research, multi-scale modeling provides a powerful platform for rational therapy design, addressing the critical challenge of how electrical stimulation parameters interact with neural tissue across spatial scales [27] [28]. By incorporating subject-specific anatomical and physiological data, these models enable researchers to predict neural responses to stimulation, optimize targeting strategies, and elucidate mechanisms of action—all in silico before costly clinical trials [29] [28]. The integration of population-level modeling approaches further enhances these capabilities by accounting for biological variability and enabling robust predictions across diverse individuals [29] [30].
Population Models: Capturing Biological Variability
Conceptual Framework and Applications
Population modeling embraces the inherent biological variability in neuronal systems through approaches that systematically explore parameter spaces rather than focusing on single "canonical" models [30]. Traditional single-model approaches often fail to capture the diversity of neural responses observed experimentally, as they typically incorporate average parameter values that may not produce biologically realistic activity [30]. Ensemble modeling, by contrast, identifies multiple parameter combinations (constituting a "solution space") that generate activity within experimentally observed ranges [30]. This approach has revealed that similar network outputs can emerge from substantially different underlying parameter sets, providing crucial insights into the degeneracy and robustness of neural circuits [30].
Population models are particularly valuable in neurostimulation research for predicting inter-subject variability in response to therapy [29]. For example, realistic head models incorporating anatomical differences demonstrate how individual variations in features such as head size, tissue thickness, and gyrification patterns significantly shape electric fields generated by non-invasive brain stimulation techniques [29]. These differences can result in unintended stimulation outcomes that reduce therapeutic efficacy if not properly accounted for in treatment planning.
Table 1: Population Modeling Approaches and Applications
| Approach | Key Features | Primary Applications | Representative Examples |
|---|---|---|---|
| Ensemble Modeling | Identifies multiple parameter sets producing acceptable output; maps "solution spaces" [30] | Understanding degeneracy in neural circuits; predicting variable treatment responses | Stomatogastric ganglion models; cortical network models [30] |
| Virtual Population Cohorts | Multiple realistic head models with anatomical and conductivity variability [29] | Estimating population variability in electric field distributions; stimulation optimization | 100-head model dataset from Human Connectome Project [29] |
| Solution Space Mapping | Systematic exploration of parameter combinations producing target activity [30] | Identifying robust stimulation parameters; understanding parameter interactions | Half-center oscillator parameter analysis [30] |
Technical Implementation and Protocols
Protocol 2.2.1: Developing Virtual Population Head Models for Non-Invasive Brain Stimulation
Purpose: To create a population of realistic head models for estimating inter-subject variability in electric field distributions during non-invasive brain stimulation.
Materials and Software:
- Structural MRI data (T1-weighted and T2-weighted)
- Automated segmentation tools (SimNIBS, FreeSurfer, CAT12)
- Meshing software (GMSH)
- Finite element method solvers
- Programming environment (Python, MATLAB)
Procedure:
- Subject Selection: Select a representative cohort of imaging datasets. For example, the 100-model dataset derived from the Human Connectome Project s1200 release includes 50 males and 50 females (ages 22-35) [29].
- Tissue Segmentation: Process structural MRI scans through automated segmentation pipelines to identify different tissue types (skin, skull, cerebrospinal fluid, gray matter, white matter, eyes) [29].
- Mesh Generation: Convert segmentations into finite-element meshes suitable for electromagnetic simulations. Typical models contain 5-6 million tetrahedral elements [29].
- Quality Assurance: Manually inspect segmentations and meshes for anatomical accuracy and mesh degeneracy. Perform corrections as needed and apply quality metrics to ensure simulation stability [29].
- Conductivity Assignment: Assign tissue-specific conductivity values, incorporating biological variability by sampling from plausible distributions (e.g., Beta(3,3) distribution for scalp, skull, and gray matter conductivities) [29].
- Lead-Field Computation: Generate lead-field matrices for efficient electric field calculations across multiple stimulation configurations [29].
Applications:
- Estimation of population variability in electric field distributions for given stimulation parameters
- Optimization of stimulation protocols for robust targeting across diverse individuals
- Meta-analysis of brain stimulation studies through standardized simulation environments [29]
Protocol 2.2.2: Ensemble Modeling for Neural Circuit Analysis
Purpose: To identify multiple parameter combinations that produce biologically plausible network activity, capturing the degeneracy and variability inherent in neural systems.
Materials and Software:
- Computational models of neurons and networks (e.g., Hodgkin-Huxley type models)
- Parameter sampling algorithms (random sampling, evolutionary algorithms)
- High-performance computing resources
- Activity analysis tools for quantifying output features
Procedure:
- Define Target Ranges: Establish acceptable ranges for network output measures (e.g., burst period, spike frequencies, phase relationships) based on experimental observations [30].
- Select Parameter Space: Identify key parameters to vary (e.g., maximal conductance densities, synaptic strengths) and their plausible ranges [30].
- Sample Parameter Combinations: Systematically explore the parameter space using appropriate sampling strategies (random sampling, Latin hypercube sampling, or more efficient directed searches) [30].
- Simulate and Evaluate: For each parameter combination, run simulations and evaluate whether the resulting activity falls within target ranges [30].
- Analyze Solution Space: Characterize the distribution of acceptable parameter sets and identify correlations between parameters that maintain functional output [30].
Applications:
- Understanding how variable underlying parameters can produce similar functional outputs
- Identifying robust therapeutic targets that remain effective across biological variability
- Predicting which parameter changes might destabilize network function in disease states [30]
Detailed Neuronal Networks: From Single Cells to Microcircuits
Biophysical Detail in Neuronal Modeling
Biophysically detailed neuronal models simulate the morphological and electrophysiological properties of individual neurons and their synaptic connections, providing mechanistic insights into how molecular and cellular processes shape network dynamics [25] [31]. At the microscopic scale, models incorporate the biophysical properties of neurons and synapses, including neurotransmitter dynamics, receptor interactions, and synaptic vesicle release mechanisms [25]. These models often use established frameworks like the Hodgkin-Huxley formalism to simulate ion channel gating kinetics, providing a foundation for understanding action potential propagation and neuronal excitability [25].
The mesoscale level focuses on microcircuits—localized networks of interconnected neurons that perform specialized computational functions [25]. Advances in connectomics and optogenetics have enabled detailed mapping of these circuits, which underlie core cognitive processes such as memory encoding and sensory processing [25]. Network models at this scale often employ graph theory to capture information flow through neural circuits and incorporate additional complexities such as synaptic plasticity and feedback loops [25].
Table 2: Scales of Detail in Neuronal Network Modeling
| Scale | Key Elements | Modeling Approaches | Simulation Tools |
|---|---|---|---|
| Microscopic | Ion channels, synapses, single-neuron morphologies [25] | Hodgkin-Huxley formalism, multi-compartment models [25] | NEURON, NeuroML, Arbor [25] [31] |
| Mesoscopic | Local microcircuits, neuronal ensembles [25] | Network models with detailed connectivity, graph theory [25] | NetPyNE, Brian, EDEN [31] |
| Macroscopic | Large-scale brain networks, systems-level dynamics [25] | Neural mass models, dynamic mean field models [25] | The Virtual Brain, TVB) |
Technical Implementation and Protocols
Protocol 3.2.1: Standardized Model Development Using NeuroML
Purpose: To create standardized, shareable, and reproducible models of neurons and networks using the NeuroML ecosystem.
Materials and Software:
- NeuroML Python libraries
- Supported simulators (NEURON, NetPyNE, Brian, Arbor, EDEN)
- Validation and visualization tools
Procedure:
- Model Component Definition: Define model elements (ion channels, cell morphologies, synapse types) using NeuroML's modular structure [31].
- Dynamics Specification: Formalize mathematical descriptions of component dynamics using LEMS (Low Entropy Modeling Specification) to ensure machine-readable definitions [31].
- Network Construction: Assemble cells into networks by specifying connectivity patterns and synaptic properties [31].
- Simulation Configuration: Define simulation parameters, including duration, time step, and output variables [31].
- Model Validation: Use NeuroML's validation tools to verify model structure and dynamics against experimental data [31].
- Simulation Execution: Run simulations across multiple supported platforms to verify reproducibility [31].
- Model Sharing: Archive and share models in standardized NeuroML format through platforms like Open Source Brain (OSB) and NeuroML Database (NeuroML-DB) [31].
Applications:
- Development of FAIR (Findable, Accessible, Interoperable, Reusable) models
- Collaborative model building across research groups
- Reproducible simulation of neural dynamics across multiple platforms [31]
Protocol 3.2.2: High-Efficiency Surrogate Modeling for Peripheral Nerve Stimulation
Purpose: To develop highly efficient surrogate models of neural fibers that accurately predict responses to electrical stimulation while dramatically reducing computational costs.
Materials and Software:
- GPU computing resources
- AxonML framework
- Training data from biophysically detailed models (e.g., MRG model in NEURON)
- Optimization algorithms
Procedure:
- Training Data Generation: Use established biophysical models (e.g., MRG model in NEURON) to generate comprehensive datasets of neural responses to varied stimulation protocols [4].
- Surrogate Model Architecture: Implement simplified cable models with trainable parameters that capture essential nonlinear dynamics while reducing computational complexity [4].
- Model Training: Train surrogate models using backpropagation and gradient descent to minimize differences between surrogate predictions and detailed model outputs [4].
- Model Validation: Thoroughly validate surrogate model performance across diverse stimulation parameters, fiber diameters, and nerve morphologies [4].
- Optimization Applications: Employ trained surrogate models for rapid parameter optimization in neurostimulation protocols [4].
Performance Metrics: The S-MF (surrogate myelinated fiber) model demonstrates 2,000 to 130,000× speedup over single-core NEURON simulations while maintaining high accuracy (R² = 0.999 for activation thresholds) [4].
Applications:
- Rapid exploration of large parameter spaces for stimulation optimization
- Real-time parameter adjustment in closed-loop stimulation systems
- Patient-specific treatment planning without prohibitive computational costs [4]
Integrated Multi-Scale Approaches
Bridging Scales in Neurostimulation Research
Integrating models across spatial and temporal scales presents significant challenges but offers powerful insights into neurostimulation mechanisms and optimization [25]. Multi-scale approaches enable researchers to trace how molecular-level disruptions (e.g., ion channel mutations) manifest as circuit-wide abnormalities and ultimately affect whole-brain dynamics and behavior [25]. Emerging technologies are helping to bridge these scales by integrating high-resolution molecular data with large-scale neuroimaging, such as mapping transcriptomic profiles from resources like the Allen Brain Atlas onto large-scale connectomic data [25].
Table 3: Multi-Scale Integration Techniques
| Integration Challenge | Approaches | Examples |
|---|---|---|
| Linking Molecular to Cellular Scales | Differentiable neural simulators; integration of transcriptomics and proteomics data [25] | Mapping ion channel mutations to neuronal excitability changes [25] |
| Linking Cellular to Network Scales | Mean-field approximations; simplified neuronal representations; surrogate modeling [4] | S-MF surrogate models for network-level stimulation predictions [4] |
| Linking Network to Systems Scales | Dynamic mean field models; neural mass models; The Virtual Brain platform [26] | Personalizing whole-brain models with individual connectivity data [26] |
| Cross-Species Integration | Comparative anatomy; standardized ontologies; data harmonization [25] | Translation of stimulation parameters from animal models to human applications [25] |
Visualization of Multi-Scale Integration
Multi-Scale Modeling Hierarchy: This diagram illustrates the integration of computational approaches across spatial scales in neuroscience, from molecular to systems levels.
Workflow for Multi-Scale Neurostimulation Optimization
Multi-Scale Neurostimulation Workflow: This diagram outlines an iterative framework for optimizing neurostimulation protocols using multi-scale modeling approaches, incorporating subject-specific data and clinical validation.
Table 4: Research Reagent Solutions for Multi-Scale Modeling
| Resource | Type | Function | Example Applications |
|---|---|---|---|
| NeuroML Ecosystem [31] | Model description standard | Standardized, shareable model development; interoperability across simulators | Creating FAIR models; collaborative modeling; reproducible research [31] |
| SimNIBS [29] | Automated head modeling pipeline | Realistic head model generation from MRI; electric field simulations | Non-invasive brain stimulation optimization; population modeling [29] |
| AxonML/S-MF [4] | Surrogate modeling framework | High-efficiency prediction of neural responses to stimulation | Peripheral nerve stimulation optimization; large parameter sweeps [4] |
| Open Source Brain [31] | Model sharing platform | Collaborative development; model validation; community standards | Sharing and validating models across research groups [31] |
| Virtual Population Datasets [29] | Curated model collections | Population-level analysis; variability assessment; stimulation optimization | Estimating inter-subject variability in electric field distributions [29] |
| Ensemble Modeling Tools [30] | Parameter exploration frameworks | Solution space mapping; robustness analysis; degenerate solutions identification | Understanding parameter interactions in neural circuits [30] |
Multi-scale modeling approaches represent a paradigm shift in computational neuroscience, providing powerful frameworks for understanding complex brain dynamics and optimizing neurostimulation therapies. By integrating across spatial and temporal scales—from ion channels to whole-brain networks—these approaches enable researchers to address fundamental questions about how neural activity emerges from biological components and how it becomes disrupted in disease states. The protocols, tools, and methodologies outlined in this application note provide practical guidance for implementing these approaches in neurostimulation research, with particular emphasis on addressing biological variability through population modeling and capturing mechanistic details through detailed neuronal networks. As these methods continue to evolve and incorporate increasingly sophisticated machine learning techniques and high-performance computing capabilities, they promise to accelerate the development of personalized, effective neuromodulation therapies for a wide range of neurological and psychiatric disorders.
Patient-specific modeling represents a paradigm shift in computational neuroscience and neurostimulation, moving away from standardized approaches to methodologies that incorporate individual anatomical and connectivity profiles. This approach is grounded in the understanding that each human brain possesses a unique neuroanatomical architecture [32] and a distinctive fine-scale connectome structure that is not captured by coarse-scale models [33]. The integration of these individual features enables researchers and clinicians to develop more precise neurostimulation interventions with improved target engagement and reduced variability in outcomes.
The clinical imperative for personalization is particularly evident in neurological disorders such as stroke, where lesions disrupt network dynamics in ways that vary substantially between individuals [34]. Similarly, in neuromodulation therapies, the interaction between stimulation parameters and individual brain anatomy significantly influences the distribution of induced electric fields [35]. This protocol details methodologies for creating and utilizing patient-specific models that integrate individual anatomy and connectivity profiles to optimize neurostimulation parameters, with applications spanning research and clinical domains.
Theoretical Foundation
Individuality of Brain Anatomy and Connectivity
The scientific rationale for patient-specific modeling rests on substantial evidence of inter-individual variation in neuroanatomy and connectivity. Research demonstrates that individual subjects can be accurately identified based solely on their brain anatomical features using standard classification techniques [32]. This individuality emerges from a complex interaction of genetic, non-genetic biological, and environmental influences that shape the brain's morphological characteristics.
At the connectome level, fine-scale structural features exhibit remarkable individuality that is shared across brains but inaccessible to coarse-scale models [33]. These shared fine-scale elements represent a major component of the human connectome that coexists with traditional areal structure. The ability to project individual connectivity data into a common high-dimensional model enables researchers to account for significantly more variance in human connectome organization than previously possible, revealing structure closely related to fine-scale distinctions in information representation.
Impact on Neurostimulation Outcomes
The clinical significance of this inter-individual variation becomes apparent in neurostimulation applications, where anatomical differences substantially influence stimulation dosage and localization. Table 1 summarizes key quantitative evidence supporting the need for patient-specific approaches in neurostimulation.
Table 1: Quantitative Evidence Supporting Patient-Specific Neurostimulation Approaches
| Evidence Type | Standardized Approach Performance | Personalized Approach Performance | Significance |
|---|---|---|---|
| Electric Field Intensity [35] | 0.113 ± 0.028 V/m (mean ± SD) | 0.290 ± 0.005 V/m (mean ± SD) | Personalization reduces variability and improves target engagement |
| Inter-Subject Variability [35] | Levene's test F(1,18)=12.02, p=0.00275 | Significantly reduced variance | Personalized montages produce more consistent outcomes across subjects |
| Surgical Efficiency [36] | Multiple needle insertions (conventional) | Mean 1.2 insertions (personalized) | 3D modeling reduces operative time and improves accuracy |
| Foramen Localization [36] | Extended localization time (conventional) | Mean 0.8 minutes (personalized) | Patient-specific planning streamlines surgical workflow |
Research Reagent Solutions and Computational Tools
Implementing patient-specific modeling requires specialized computational tools and resources. Table 2 catalogs essential research reagents and computational solutions referenced in the literature.
Table 2: Essential Research Reagents and Computational Tools for Patient-Specific Modeling
| Tool/Resource | Type | Primary Function | Application Context |
|---|---|---|---|
| BrainX3 [34] | Neuroinformatics Platform | Visualization, analysis, and simulation of neuroimaging data and brain models | Stroke rehabilitation, lesion identification, whole-brain modeling |
| U-Net Architecture [34] | Convolutional Neural Network | Automated lesion segmentation from multi-modal MRI data | Stroke lesion identification and classification |
| FreeSurfer [32] | Software Suite | Extraction of cortical and subcortical anatomical measures from MRI | Brain feature quantification, cortical thickness, surface area, volume |
| 3D Printed Neurostimulator [35] | Hardware Device | Patient-specific electrode placement for transcranial electrical stimulation | Home-based tES therapy with precise electrode positioning |
| Linear Discriminant Analysis [32] | Statistical Classification | Subject identification based on neuroanatomical features | Quantification of individual neuroanatomical variation |
| Weighted K-Nearest Neighbor [32] | Statistical Classification | Alternative method for subject identification | Comparison with LDA for neuroanatomical individuality assessment |
| MindStim Clinical Trial Platform [35] | Research Infrastructure | Validation of personalized montages through in-silico modeling | Electric field optimization and target engagement assessment |
Application Notes and Experimental Protocols
Protocol 1: Patient-Specific Head Model Creation for Transcranial Electrical Stimulation
Objective: To create individualized head models from structural MRI data for optimizing tES electrode montages and predicting electric field distributions.
Materials and Equipment:
- Structural MRI scans (T1-weighted, minimum 1mm³ resolution)
- Computational resources for finite element method (FEM) modeling
- Software for multi-layer tissue segmentation (e.g., SimNIBS, ROAST)
- 3D printer for creating patient-specific electrode caps (optional)
Methodology:
Image Acquisition and Preprocessing
- Acquire high-resolution T1-weighted MRI scans with whole-head coverage
- Perform image quality assessment and artifact correction
- Align images to standard orientation if needed
Tissue Segmentation
- Automatically segment head tissues into minimum 5 compartments: scalp, skull, cerebrospinal fluid, gray matter, and white matter
- Manually review and correct segmentation errors, particularly at tissue boundaries
- Generate smooth, watertight surface meshes for each tissue type
Electrical Property Assignment
- Assign conductivity values to each tissue compartment based on established literature values
- Account for frequency-dependent conductivity if modeling tACS
- Incorporate anisotropic conductivity in white matter if diffusion tensor imaging data available
Electrode Placement and Montage Optimization
- Define candidate electrode positions based on cap design (minimum 32 positions for optimization flexibility)
- Specify target region of interest and desired electric field intensity (e.g., 0.3 V/m for angular gyrus [35])
- Run optimization algorithm with safety constraints (maximum current per electrode, total current)
- Generate patient-specific cap design for precise electrode positioning
Validation and Model Testing
- Compare predicted electric field distributions with phantom measurements if available
- Perform sensitivity analysis on tissue conductivity parameters
- Document model assumptions and limitations
Workflow Diagram: Patient-Specific Head Model Creation
Protocol 2: Lesion Identification and Whole-Brain Modeling for Stroke Rehabilitation
Objective: To identify stroke lesions automatically and incorporate them into whole-brain models for guiding rehabilitation and neuromodulation strategies.
Materials and Equipment:
- Multi-modal MRI data (T1-weighted, T2-weighted, FLAIR, DWI)
- High-performance computing resources for large-scale neural simulations
- U-Net architecture implementation (Python with TensorFlow/PyTorch)
- Structural connectivity matrices from diffusion MRI (if available)
Methodology:
Lesion Identification and Segmentation
- Preprocess multi-modal MRI data (co-registration, intensity normalization)
- Train U-Net architecture on annotated lesion datasets [34]
- Implement overlap-tile strategy for seamless segmentation of large images
- Generate binary lesion masks and calculate lesion volume/location metrics
Structural Connectivity Mapping
- Reconstruct whole-brain structural connectivity using diffusion MRI tractography
- Apply lesion mask to disconnect affected white matter pathways
- Calculate network metrics (node strength, efficiency, modularity) for affected connectome
Whole-Brain Model Implementation
- Implement dynamic mean-field model of interacting neural populations [34]
- Incorporate patient-specific structural connectivity matrix
- Apply disconnection masks to simulate lesion effects
- Parameterize local excitatory-inhibitory balance for each region
Model Fitting and Personalization
- Adjust local E-I balance parameters to fit empirical functional connectivity
- Compare simulated functional connectivity with empirical resting-state fMRI
- Identify regions with maximal E-I imbalance for targeting neuromodulation
Neuromodulation Target Identification
- Simulate network effects of different stimulation targets
- Identify candidate regions for transcranial ultrasound stimulation (TUS) or other neuromodality
- Predict effects of E-I balance restoration on global network dynamics
Workflow Diagram: Stroke Lesion Modeling and Neuromodulation Targeting
Protocol 3: Surgical Planning for Sacral Neuromodulation Using Patient-Specific 3D Modeling
Objective: To utilize patient-specific 3D anatomical modeling for precise surgical planning in sacral neuromodulation procedures.
Materials and Equipment:
- Sacral-specific CT imaging data
- 3D modeling software (e.g., Mimics)
- 3D printing capability (optional, for physical models)
- Surgical navigation system (optional)
Methodology:
Image Acquisition and Processing
- Acquire high-resolution CT scans of sacral region with appropriate field of view
- Reconstruct 3D images with slice thickness ≤1mm
- Export data in DICOM format for 3D modeling
3D Anatomical Model Generation
- Import CT data into 3D modeling software
- Segment sacrum, S3 foramen, and surrounding tissues
- Generate surface mesh of relevant anatomical structures
- Calculate key surgical parameters:
- Distance between coccyx tip and S3 foramen
- S3 foramen diameter and depth
- Needle insertion angle and trajectory
- Distance from midline to optimal entry point
Surgical Plan Formulation
- Define optimal needle entry point based on 3D model measurements
- Determine insertion angle and depth for S3 foramen access
- Simulate procedure virtually to confirm approach feasibility
- Generate patient-specific measurements for intraoperative guidance
Intraoperative Implementation
- Transfer preoperative measurements to patient in modified prone position
- Mark entry point based on 3D model guidance
- Perform needle insertion without fluoroscopic guidance (initial placement)
- Verify placement with bellows sign and toe reflex stimulation
- Use fluoroscopy confirmation only after optimal response obtained
Outcome Assessment
- Record number of needle insertions required
- Document time to S3 foramen localization
- Measure total operative time
- Assess stimulation parameters and clinical outcomes
Table 3: Quantitative Parameters for Sacral Neuromodulation Surgical Planning [36]
| Parameter | Mean Value | Range | Clinical Significance |
|---|---|---|---|
| Coccyx to S3 Foramen Distance | 70.3 mm | 51.0-85.8 mm | Determines vertical approach dimension |
| Needle Insertion Angle | 61.7° | 60.4-67.7° | Guides trajectory to target |
| S3 Foramen Diameter | 6.1 mm | 4.3-8.9 mm | Indicates anatomical accessibility |
| S3 Foramen Depth | 3.0 mm | 1.4-4.8 mm | Informs lead placement depth |
| Midline to Entry Point Distance | 22.1 mm | 17.7-23.1 mm | Establishes lateral approach dimension |
| Time to S3 Localization | 0.8 min | 0.6-1.0 min | Measures procedural efficiency |
| Number of Needle Insertions | 1.2 | 1-2 | Indicates targeting accuracy |
Data Analysis and Interpretation
Quantitative Assessment of Personalization Benefits
The efficacy of patient-specific modeling approaches can be quantified through multiple performance metrics. For neurostimulation applications, electric field consistency across subjects provides a key validation measure. Research demonstrates that personalized montages reduce inter-subject variability in electric field intensity by approximately 85% compared to standardized approaches [35]. This reduction in variability is statistically significant (F(1,18)=12.02, p=0.00275), indicating substantially more consistent stimulation dosage across different individuals when personalization is implemented.
In surgical applications, patient-specific modeling demonstrates clinically meaningful improvements in procedural efficiency. The use of 3D modeling for sacral neuromodulation surgery reduces the number of needle insertions to a mean of 1.2 compared to multiple attempts typically required with conventional approaches [36]. This improvement in accuracy simultaneously decreases operative time and radiation exposure while potentially improving clinical outcomes through more precise lead placement.
Integration with Clinical Workflows
Successful implementation of patient-specific modeling requires seamless integration with existing clinical and research workflows. The computational pipeline must be designed to accommodate time constraints, particularly in surgical applications where 3D modeling adds approximately 110 minutes to preoperative planning [36]. This time investment must be balanced against intraoperative efficiency gains and improved outcomes.
For non-invasive neuromodulation, the development of patient-specific, 3D-printed caps enables precise electrode positioning that maintains the benefits of personalization across multiple treatment sessions [35]. This approach addresses the critical challenge of implementation fidelity, ensuring that computationally optimized stimulation parameters are accurately translated to actual treatment delivery.
Patient-specific modeling that integrates individual anatomy and connectivity profiles represents a significant advancement in computational neuroscience and neurostimulation optimization. The protocols detailed in this document provide researchers with comprehensive methodologies for implementing these approaches across multiple applications, from non-invasive brain stimulation to surgical planning.
The quantitative evidence demonstrates that personalization yields substantial benefits, including reduced inter-subject variability in stimulation dosage, improved targeting accuracy, and enhanced procedural efficiency. As these methodologies continue to evolve, patient-specific modeling is poised to transform neurostimulation from a standardized intervention to a truly personalized therapeutic approach, ultimately improving outcomes across neurological and psychiatric disorders.
The development of effective neurostimulation therapies faces significant challenges, including inconsistent clinical outcomes and the impracticality of exhaustive physical testing for personalization. In silico testing, which uses computational models and simulations, has emerged as a powerful methodology to overcome these hurdles. This approach enables researchers to virtually prototype electrode designs and optimize stimulation protocols within anatomically detailed and physiologically realistic human models before clinical application. By integrating artificial intelligence (AI) with computational neuroscience, in silico methods facilitate a shift from a "one-size-fits-all" approach to truly personalized neuromodulation therapies, potentially enhancing efficacy and reducing side effects [11] [10].
This Application Note details protocols for leveraging in silico platforms to systematically optimize two critical components of neurostimulation systems: electrode structure and stimulation parameters. The documented methodologies are framed within a broader thesis on computational models for neurostimulation optimization research, providing a reproducible framework for scientists and drug development professionals.
Optimizing Electrode Design Through Computational Modeling
The geometry and configuration of neural electrodes directly influence stimulation efficiency and focality, affecting both therapeutic outcomes and power consumption. The following protocol outlines a integrative computational analysis to guide optimal electrode selection.
Application Protocol: Integrative Electrode Analysis
Objective: To quantitatively assess the impact of electrode shape, size, and configuration on neural activation, with the goal of optimizing for either stimulation efficiency or focality.
Methodology:
Model Construction: Create a 2-D or 3-D finite element method (FEM) model of the electrode and surrounding neural tissue (e.g., gray matter) using a simulation environment like COMSOL Multiphysics.
- Electrode Parameters: Model electrodes as regular polygons, systematically varying the number of edges (e.g., 4, 6, 8, 10) to represent different shapes from rectangular to circular.
- Size Variation: For each shape, define the electrode size by its center-to-vertex distance, testing a range from 50 µm to 1000 µm.
- Configuration: Model both monopolar and bipolar configurations. For bipolar setups, position an identical reference electrode at varying separation distances (e.g., 0.25 mm to 2 mm) from the stimulation electrode [37].
Material and Tissue Properties:
- Assign material properties, such as the electrical conductivity of gold (4.11×10^7 S/m) for the electrode and 0.27 S/m for the gray matter tissue.
- Apply a cathodic stimulation voltage (e.g., -1 V) to the electrode boundary, with the reference potential set to 0 V [37].
Simulation and Metric Calculation:
- Use an electric current solver to compute the spatial distribution of the electric potential (V) and electric field (E).
- Calculate the Activation Function (AF), a key metric predicting neural activation, using the second derivative of the electric potential or the root-mean-square of the first derivative of the electric field components [37].
- Quantitative Metrics:
- Stimulation Efficiency: Defined as the magnitude of the AF.
- Stimulation Focality: Characterized by the Full Area at Half Maximum (FAHM) of the AF, representing the total area where neural activation exceeds the threshold [37].
Expected Outcomes: This analysis will reveal quantitative relationships between design parameters and performance. For instance, sharper, smaller electrodes generally enhance stimulation efficiency. A center-to-vertex distance exceeding 100 µm in bipolar configurations can improve efficiency, and separation distances under 1 mm between electrodes often yield higher efficiency than monopolar configurations. Furthermore, sharper electrodes and most bipolar setups typically achieve more focal neural activation [37].
Research Reagent Solutions: Electrode Modeling
The table below catalogues essential computational tools and concepts for in silico electrode design.
Table 1: Essential Research Reagents for In Silico Electrode Analysis
| Item Name | Function/Description |
|---|---|
| COMSOL Multiphysics | A finite element analysis solver for modeling electrode-electrolyte interfaces and calculating electric field distributions [37]. |
| Finite Element Method (FEM) | A numerical technique for solving partial differential equations, used here to compute electric fields in complex biological tissues. |
| Activation Function (AF) | A mathematical descriptor predicting sites of neural activation based on the second spatial derivative of the extracellular electric potential [37]. |
| o2S2PARC Platform | A cloud-native environment for building, sharing, and executing computational pipelines that couple electromagnetic exposure with neuronal dynamics [10]. |
Workflow Visualization: Electrode Optimization
The following diagram illustrates the logical workflow for the integrative computational analysis of electrode design.
Diagram 1: Workflow for electrode design optimization via in silico modeling.
Personalizing Stimulation Protocols with AI and In Silico Trials
Personalizing stimulation parameters to individual anatomy and baseline physiology is critical for overcoming the inconsistent outcomes seen in clinical neurostimulation. AI-driven optimization and in silico clinical trials provide a robust framework for this personalization.
Application Protocol: AI-Driven Parameter Optimization for Sustained Attention
Objective: To implement a personalized Bayesian Optimization (pBO) algorithm for remotely adjusting neurostimulation parameters to enhance sustained attention in a home-based setting.
Methodology:
System Setup:
- Deploy a home-based neurostimulation system, such as transcranial random noise stimulation (tRNS), targeting brain regions like the dorsolateral prefrontal cortex (dlPFC).
- Participants perform a sustained attention task (e.g., detecting target stimuli) to provide performance feedback (A', a measure of perceptual sensitivity) [11].
Algorithm Implementation:
- Employ a personalized Bayesian Optimization (pBO) algorithm. This AI model uses data from previous sessions and participants to build a probabilistic model of the relationship between stimulation parameters and task performance.
- The pBO algorithm's objective is to identify the "sweet spot" current intensity for each individual, accounting for personal factors such as baseline cognitive performance and head circumference (a proxy for scalp-to-cortex distance) [11].
Validation and Testing:
- Conduct a double-blind, sham-controlled study to validate the optimized protocol.
- Compare the AI-optimized stimulation (pBO-tRNS) against a standard one-size-fits-all tRNS protocol (e.g., fixed at 1.5 mA) and a sham stimulation [11].
Expected Outcomes: Validation studies have demonstrated that pBO-tRNS significantly enhances sustained attention performance, particularly in individuals with lower baseline performance. The algorithm typically identifies an inverted U-shaped relationship between current intensity and performance, confirming the "stochastic resonance" mechanism where an optimal noise level enhances signal detection in neural systems. This approach can maximize efficacy while enabling scalable, personalized therapy [11].
Application Protocol: Conducting an In Silico Clinical Trial (ISCT) for Cardiac Neurostimulation
Objective: To develop and use a computational model as a "digital twin" for in silico testing of neurostimulation therapy for atrial fibrillation (AFib), predicting hemodynamic responses and optimizing dosage.
Methodology:
Model Development:
- Create a closed-loop computational model integrating the human cardiovascular system with the brain's processing centers (e.g., baroreflex control).
- Translate known physiological changes during AFib into mathematical representations within the model [38].
Model Validation:
- Validate the model by ensuring its predictions for heart rate, stroke volume, and blood pressure match clinical data from real AFib patients [38].
Stimulation Testing & Optimization:
- Use the validated model to explore neurostimulation parameters. Test the hemodynamic effects of stimulating different parts of the autonomic nervous system (e.g., the atrioventricular node).
- The model provides real-time feedback on physiological responses, allowing for the identification of optimal stimulation sites and doses without risk to patients [38].
Expected Outcomes: Such models can accurately predict short-term hemodynamic effects of AFib and flag promising stimulation targets. They serve as a low-cost, rapid-testing tool to pre-optimize neurostimulation strategies, forming the basis for a future automated, wearable device that delivers personalized therapy for cardiac arrhythmias [38].
Research Reagent Solutions: Stimulation Protocol Optimization
Table 2: Essential Research Reagents for In Silico Protocol Optimization
| Item Name | Function/Description |
|---|---|
| Personalized Bayesian Optimization (pBO) | An AI algorithm that builds a model of an individual's response to stimulation to find optimal parameters efficiently [11]. |
| Sim4Life Platform | An in silico platform for image-based, regulatory-grade simulations of medical devices within anatomically detailed human body models [10]. |
| Virtual Population (vPOP) | Computer-generated cohorts mimicking the variability of a real patient population, used for in silico clinical trials [39]. |
| Closed-Loop Cardiovascular Model | A computational "digital twin" of the human cardiovascular and control systems for testing neurostimulation for cardiac conditions [38]. |
Workflow Visualization: AI-Driven Stimulation Personalization
The following diagram illustrates the closed-loop process of AI-driven personalization of stimulation protocols.
Diagram 2: AI-driven closed-loop personalization of stimulation protocols.
The integration of in silico testing platforms and AI-driven optimization represents a paradigm shift in neurostimulation research. The protocols detailed herein provide a concrete methodology for researchers to rationally design electrode systems and personalize stimulation protocols with a level of speed, precision, and scale unattainable through traditional experimental approaches alone. By adopting these computational frameworks, the field can accelerate the development of safer, more effective, and truly personalized neuromodulation therapies for a wide range of neurological and psychiatric disorders.
Epidural Spinal Cord Stimulation (eSCS) has undergone a significant paradigm shift, evolving from an open-loop intervention for chronic pain management to a sophisticated, computationally-guided therapy for motor recovery after neurological injury. This transformation is largely driven by the integration of computational models that bridge our understanding of neural circuit interactions from the spinal cord to supraspinal centers. The fundamental mechanistic principle underlying this approach involves eSCS activation of sensory neurons in the dorsal roots, which subsequently transmit synchronized excitatory postsynaptic potentials (EPSPs) to motor neurons and interneurons via mono- or polysynaptic connections [40]. This mechanism not only enhances the functional integration of spinal cord neural circuits but also improves communication between the spinal cord and the brain, significantly promoting the restoration of motor function [40].
Computational models provide the critical framework for optimizing this complex neuromodulation by simulating the effects of various stimulation parameters on neural tissue and predicting outcomes across distributed neural networks. The spatiotemporal specificity of eSCS in motor neuron recruitment means that computational approaches are indispensable for determining optimal electrode placement and stimulation patterns tailored to individual patient anatomy and specific neurological deficits [40]. For improving leg movement, computational models suggest electrode implantation in the lumbosacral thickening area, while for controlling upper limb movement, models guide positioning in the cervical enlargement area [40]. Furthermore, advanced computational techniques now enable the development of closed-loop stimulation systems that dynamically adjust stimulation parameters in real-time based on physiological feedback, representing a significant advancement over traditional open-loop approaches [40].
Quantitative Data in Computational SCS
The application of computational models in SCS relies on quantitative parameters that define the interaction between electrical stimulation and neural tissue. The following tables summarize key quantitative data essential for designing and implementing computational SCS approaches.
Table 1: Key Stimulation Parameters and Their Computational Considerations
| Parameter | Typical Range/Values | Computational Modeling Consideration | Impact on Outcomes |
|---|---|---|---|
| Electrode Placement | Cervical (C3-C7), Lumbosacral (T11-L1) | Finite Element Method (FEM) models electric field spread | Determines upper vs. lower limb motor control [40] |
| Stimulation Frequency | 30-100 Hz (neuromodulatory); Phase-dependent (targeted) | Neural network models of frequency-dependent synaptic facilitation | Continuous vs. gait cycle-specific muscle activation [40] |
| Current Intensity | Individualized based on anatomy and baseline function | Bayesian optimization personalizes intensity based on head size (for brain integration) and spinal anatomy [41] | Inverted U-shaped relationship with performance; avoids under-/over-stimulation [41] |
| Stimulation Mode | Open-loop, Closed-loop (real-time feedback) | Reinforcement learning algorithms for parameter adjustment in closed-loop systems | Closed-loop enables dynamic adjustment for coordinated gait [40] |
Table 2: Computational Techniques and Their Applications in SCS Research
| Computational Technique | Primary Application in SCS | Key Input Variables | Output/Objective |
|---|---|---|---|
| Finite Element Method (FEM) | Models electric field distribution in spinal cord | Electrode configuration, tissue conductivity, anatomy from MRI | Predicts neural activation thresholds and target engagement [40] |
| Bayesian Optimization (BO) | Personalizes stimulation parameters | Baseline performance, anatomical features (e.g., head circumference), previous response data [41] | Identifies patient-specific "sweet spot" intensity (inverted U-shape) [41] |
| Neural Network Modeling | Simulates circuit-level effects of SCS | Stimulation parameters, connectivity maps, neurophysiological data | Predicts effects on proprioceptive feedback and motor pool recruitment [40] |
| Gaussian Process Regression | Models unknown objective functions in closed-loop systems | Sampled data points, noise estimates | Constructs posterior belief about stimulation-response function [41] |
Experimental Protocols for Computational SCS
Protocol 1: Personalized Parameter Optimization Using Bayesian Methods
This protocol outlines a methodology for personalizing SCS parameters using Bayesian optimization, adapted from AI-driven neurostimulation approaches [41].
Objective: To determine patient-specific SCS parameters that maximize motor outcome measures using a computationally efficient Bayesian optimization framework.
Materials and Reagents:
- Clinical-grade SCS system with programmable parameters
- Motion capture system (e.g., 3D infrared cameras with reflective markers)
- Electromyography (EMG) system with multiple surface electrodes
- Computational workstation with Bayesian optimization software package
- Safety monitoring equipment (respiration, cardiovascular monitoring)
Procedure:
- Baseline Assessment: Quantify baseline motor performance using standardized metrics (e.g., Lower Extremity Motor Score, gait velocity, muscle grade scoring). Simultaneously, obtain anatomical measurements (e.g., spinal cord dimensions from MRI, vertebral level distances).
- Algorithm Initialization: Program the Bayesian optimization algorithm with prior distributions for each SCS parameter (intensity, frequency, pulse width, location) based on population data from previous patients with similar characteristics.
- Iterative Testing Sequence: For each iteration (typically 15-20 iterations per session): a. The algorithm selects the next parameter set to evaluate based on the acquisition function (e.g., expected improvement). b. Apply the selected SCS parameters for a standardized duration (5-10 minutes). c. Quantify motor response using motion capture and EMG during standardized motor tasks (e.g., standing, stepping, voluntary leg movements). d. Feed the motor response metric back into the algorithm to update the posterior distribution.
- Convergence Criteria: Continue iterations until performance improvement plateaus (defined as <2% improvement over three consecutive iterations) or maximum iterations are reached.
- Validation: Validate the optimized parameters in a subsequent session by comparing motor performance with optimized parameters versus sham or standard parameters.
Computational Considerations: The algorithm models the relationship between stimulation parameters and motor outcomes as an unknown function to be maximized, balancing exploration of new parameter spaces with exploitation of known effective parameters [41]. For individuals with larger anatomical size (e.g., larger head circumference for brain effects or larger CSF volume for spinal effects), the algorithm typically identifies higher optimal current intensities following an inverted U-shaped function [41].
Protocol 2: Closed-Loop SCS for Gait Restoration
This protocol details the implementation of a closed-loop SCS system that adjusts stimulation parameters in real-time based on gait phase detection.
Objective: To implement a computationally-driven closed-loop SCS system that delivers spatially and temporally targeted stimulation during specific phases of the gait cycle to improve walking function in spinal cord injury patients.
Materials and Reagents:
- Multi-electrode SCS paddle implant with independent current control
- Wearable inertial measurement units (IMUs) placed on feet, shanks, and thighs
- Real-time signal processing unit (FPGA or dedicated DSP)
- EMG system with wireless transmission
- Closed-loop stimulation software with phase detection algorithms
- Treadmill with safety harness system
Procedure:
- System Calibration: a. Place IMUs on lower limb segments and synchronize with SCS system clock. b. Record baseline kinematic and EMG data during assisted stepping to train the gait phase detection algorithm. c. Define stimulation targets for each phase of gait (e.g., quadriceps activation during stance phase, tibialis anterior during swing phase).
- Algorithm Development: a. Implement real-time gait phase detection using kinematic data from IMUs through a hidden Markov model or neural network classifier. b. Program stimulation rules that map specific gait phases to optimal stimulation parameters (electrode configuration, intensity, frequency). c. Implement safety monitoring algorithms to detect abnormal muscle responses or cardiovascular changes.
- Closed-Loop Operation: a. During walking, the system continuously estimates gait phase from IMU data (updated at 100Hz). b. When a gait phase transition is detected, the system selects the corresponding stimulation parameters from the predefined rules. c. Stimulation is delivered with minimal latency (<50ms) from phase detection to parameter adjustment. d. EMG responses are monitored in real-time to assess motor output and adjust parameters if suboptimal response is detected.
- Performance Assessment: Quantify walking function using spatiotemporal gait parameters (velocity, step length, symmetry), kinematics (joint angles), and EMG patterns (muscle activation timing, amplitude). Compare closed-loop stimulation to both open-loop stimulation and no stimulation conditions.
Computational Considerations: This approach requires computational models that understand the relationship between stimulation parameters and their effects on specific spinal circuits controlling different muscle groups during gait. The system uses reinforcement learning to gradually refine stimulation parameters based on continuous performance feedback, optimizing for stable, efficient walking patterns [40].
Signaling Pathways and Neural Circuits in SCS
Computational models of SCS effects must incorporate the complex signaling pathways and neural circuits that mediate its actions from the spinal cord to the brain. The following diagrams visualize these pathways using Graphviz DOT language, with colors selected from the specified palette to ensure optimal contrast and visual clarity.
Diagram 1: Multilevel Neuromodulatory Pathways of SCS. This diagram illustrates the circuit-level mechanisms of SCS, showing how stimulation activates dorsal root ganglion neurons, which then modulate spinal circuits through mono- and polysynaptic connections. The pathways to supraspinal centers demonstrate how SCS influences brainstem, thalamic, and cortical regions, ultimately forming integrated spinal-supraspinal loops for motor control. The closed-loop computational model shows how wearable sensors and optimization algorithms continuously adjust stimulation parameters based on physiological feedback.
The Scientist's Toolkit: Essential Research Reagents and Materials
The implementation of computational SCS models requires specialized tools and methodologies. The following table details essential research reagents and solutions critical for advancing this field.
Table 3: Essential Research Toolkit for Computational SCS Investigations
| Category | Specific Tool/Technology | Research Function | Application in Computational SCS |
|---|---|---|---|
| Stimulation Hardware | Multi-electrode paddle arrays with independent current control | Enables spatially-targeted stimulation | Allows complex electric field shaping guided by computational models [40] |
| Sensing Technologies | High-density EMG systems, Inertial Measurement Units (IMUs) | Captures kinematic and muscle activity data | Provides real-time feedback for closed-loop systems and model validation [40] |
| Computational Modeling | Finite Element Method (FEM) software, Neural network simulators | Models electric field spread and neural activation | Predicts effects of stimulation parameters and optimizes electrode placement [40] |
| Optimization Algorithms | Bayesian Optimization packages, Gaussian Process Regression | Personalizes stimulation parameters | Identifies patient-specific stimulation "sweet spots" using limited data samples [41] |
| Neuroimaging | Functional MRI, Diffusion Weighted Imaging (DWI) | Maps structural and functional connectivity | Informs model initialization with patient-specific anatomy and pathway integrity [42] [40] |
| Electrophysiology | TMS with EMG recording, EEG with ERP analysis | Measures cortical and spinal excitability | Quantifies SCS-induced neuroplasticity in corticospinal pathways [43] [40] |
| Digital Phenotyping | Wearable sensors with continuous monitoring | Captures real-world motor behavior | Provides ecological validation of laboratory findings and long-term outcomes [41] |
| 5-Hydroxy-2-methylpyridine-d6 | 5-Hydroxy-2-methylpyridine-d6, MF:C6H7NO, MW:115.16 g/mol | Chemical Reagent | Bench Chemicals |
| DMT-dA(bz) Phosphoramidite-d9 | DMT-dA(bz) Phosphoramidite-d9, MF:C47H52N7O7P, MW:867.0 g/mol | Chemical Reagent | Bench Chemicals |
The integration of computational models with SCS represents a transformative approach for enhancing motor recovery after neurological injury. Current research demonstrates that computational methods, particularly Bayesian optimization and closed-loop control systems, can significantly improve the precision and efficacy of SCS by accounting for individual neuroanatomy and dynamic physiological states [40] [41]. The future of this field lies in developing increasingly sophisticated multi-scale models that bridge molecular, circuit, and systems-level effects of stimulation, ultimately enabling fully personalized neuromodulation therapies.
Future research directions should focus on several key areas: First, the development of hybrid brain-spine computational models that incorporate both spinal circuit dynamics and supraspinal influences to better predict recovery patterns [40]. Second, the implementation of reinforcement learning algorithms that can adapt stimulation parameters in real-time based on continuous performance metrics [40]. Third, the integration of neurochemical monitoring (e.g., through MRS) with computational models to understand how SCS modulates neurotransmitter systems involved in plasticity and recovery [42]. Finally, addressing the ethical considerations of AI-driven neurostimulation, including ensuring equitable access and establishing safety protocols for autonomous system operation [41].
As computational power increases and our understanding of neural circuit function expands, the synergy between computational modeling and SCS will undoubtedly yield increasingly effective approaches for restoring motor function after injury. The pathway from spine to brain, once considered largely unidirectional, is now revealed as a rich dialogue that computational models can help us understand and therapeutically manipulate for improved patient outcomes.
Computational models for neurostimulation optimization are revolutionizing the treatment of neurological disorders, from chronic pain to motor function restoration [44] [14]. The accuracy of these in-silico frameworks depends critically on precise anatomical inputs, particularly the three-dimensional structure of peripheral nerves. Traditional manual segmentation of nerve histology represents a significant bottleneck—it is labor-intensive, time-consuming, and prone to inter-observer variability [45] [46]. This Application Note details how deep learning-based automated segmentation pipelines can overcome these limitations, providing the high-throughput, reproducible morphological data necessary to build patient-specific neurostimulation models. By translating histological specimens into precise digital models, these techniques enable the creation of more accurate computational phantoms, ultimately guiding the development of targeted and effective neurostimulation therapies.
Performance Comparison of Deep Learning Models for Nerve Segmentation
The selection of an appropriate deep learning architecture is paramount to achieving accurate nerve segmentation. Below is a summary of quantitative performance metrics reported for various models and tissues. Note that performance is highly dependent on specific tasks; a model excelling in one area may not generalize directly to another.
Table 1: Performance Metrics of Segmentation Models for Nerve and Related Tissues
| Model Architecture | Tissue / Nerve Type | Dataset Size | Key Metric | Reported Score | Reference |
|---|---|---|---|---|---|
| 2D/3D nnU-Net | Sciatic Nerve (MRN) | 70 training scans | Dice Similarity Coefficient (DSC) | 0.789 (Test Set) | [45] |
| SegFormer | Nerve Fibers (Histology) | >75,000 images | F1-Score / Dice | 0.91 | [47] |
| VGG-UNet | Nerve Fibers (Histology) | >75,000 images | F1-Score / Dice | ~0.78 (inferred) | [47] |
| Four-Layer U-Net | Median Nerve (Ultrasound) | 500 images/site | Dice Similarity Coefficient (DSC) | 0.971 (Forearm) | [48] |
| Mask R-CNN | Median Nerve (Ultrasound) | 151 images | Dice Similarity Coefficient (DSC) | 0.931 | [48] |
| Custom FCN | Peripheral Nerves (MRN) | 52 subjects | Dice Similarity Coefficient (DSC) | ~0.89 (inferred) | [45] |
Experimental Protocols for Nerve Histology Segmentation
Protocol 1: Sciatic Nerve Segmentation from Magnetic Resonance Neurography (MRN)
This protocol outlines the procedure for automated segmentation of the sciatic nerve and its proximal branches from MRN scans using the nnU-Net framework [45].
- Objective: To achieve fully automated, high-precision segmentation of the sciatic nerve for quantitative feature analysis in neurostimulation research.
- Materials and Reagents:
- MRN Scans: T2-weighted, spectrally fat-saturated images acquired on a 3T scanner (e.g., Siemens Magnetom TIM-TRIO).
- Segmentation Software: ITK-SNAP (v3.8.0) for manual ground truth annotation.
- Computing Framework: Python package
nnU-Net(v1.0). - Hardware: Workstation with high-performance GPUs (e.g., 2x NVIDIA Quadro RTX 8000) and substantial RAM (~380 GB).
- Methodology:
- Data Preparation:
- Format images and manual segmentation labels in the Neuroimaging Informatics Technology Initiative (NIfTI) format.
- Intensity normalization is automatically handled by nnU-Net via z-score normalization (subtraction of mean and division by standard deviation).
- Model Training and Validation:
- Configure nnU-Net for both 2D and 3D full-resolution architectures.
- Train the model using a 5-fold cross-validation scheme on the training dataset (e.g., 70 scans from 35 healthy individuals).
- Set patch size to
512 x 512for 2D and20 x 320 x 256for 3D models. Train the 2D model for 150 epochs and the 3D model for 500 epochs until convergence.
- Inference:
- Apply the trained model to an independent test set of MRN scans.
- Preprocess test images identically to the training set during inference.
- Data Preparation:
- Validation and Analysis:
- Quantify segmentation performance against manual ground truth using the Dice Similarity Coefficient (DSC), Jaccard Index (JI), and Hausdorff Distance (HD).
- Expected baseline performance on a healthy test cohort: DSC ~0.79, JI ~0.67, HD ~2.12 mm [45].
Protocol 2: Nerve Fibre Segmentation in Histological Images Using SegFormer
This protocol describes a comparative analysis for segmenting nerve fibres in haematoxylin and eosin (H&E) stained histological sections using the SegFormer transformer model [47].
- Objective: To leverage an advanced transformer architecture for accurate segmentation of nerve structures in diverse histological images, compensating for morphological variability.
- Materials and Reagents:
- Histological Images: H&E-stained sections from various tissues (e.g., prostate, aorta, myocardium, colon).
- Slide Scanner: Aperio AT2 histological scanner for digitization at 20x magnification.
- Annotation Software: Aperio ImageScope for manual annotation of nerve fibres and ganglia.
- Computational Tools: Python with Albumentations library for data augmentation and SegFormer implementation.
- Methodology:
- Data Preprocessing and Annotation:
- Digitize histological slides and manually annotate nerve fibres and ganglia, saving coordinates in XML files.
- Extract regions containing nerve fibres and tile entire sections into non-overlapping
1024 x 1024pixel patches. - Generate corresponding binary masks where white (1) indicates nerve structures and black (0) denotes background.
- Resize all patches to
224 x 224pixels to optimize computational efficiency while preserving morphological integrity.
- Stain Normalization and Augmentation:
- Apply the Macenko method to standardize stain variation across images.
- Use real-time data augmentation (Albumentations) including random rotations (±15°), horizontal/vertical flips, brightness/contrast adjustments, and elastic deformations.
- Model Training:
- Train SegFormer, VGG-UNet, and FabE-Net models on the curated dataset of >75,000 image-mask pairs.
- Allocate 10% of images for validation during training.
- Data Preprocessing and Annotation:
- Validation and Analysis:
- Evaluate model performance using precision, recall, F1-score (Dice), and accuracy, averaged across assessments from multiple expert pathologists.
- SegFormer typically achieves superior performance (F1-score: 0.91, Precision: 0.84, Recall: 0.99) and faster convergence compared to CNN-based models [47].
Workflow Visualization
The following diagram illustrates the integrated computational pipeline, from raw data acquisition to the final application in neurostimulation modeling.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagents and Computational Tools for Automated Nerve Segmentation
| Item Name | Function / Application | Specifications / Examples |
|---|---|---|
| nnU-Net | A self-configuring framework for biomedical image segmentation; adapts to any dataset. | Automatically determines network architecture, pre-processing, and training parameters. Ideal for MRN and histology data [45]. |
| SegFormer | A transformer-based model for semantic segmentation. | Excels at capturing long-range dependencies in images, effective for variable nerve morphologies in histology [47]. |
| CLAM | A weakly-supervised pipeline for Whole-Slide Image (WSI) analysis. | Uses slide-level labels to classify WSIs and generate tumor/region-of-interest heatmaps without patch-level annotations [49]. |
| ITK-SNAP | Interactive software for manual and semi-automatic image segmentation. | Used for generating ground truth segmentation labels for model training and validation [45]. |
| Aperio ImageScope | Desktop software for viewing and analyzing digital pathology slides. | Enables manual annotation of nerve fibres and ganglia on digitized WSIs [47]. |
| Albumentations | A Python library for fast and flexible image augmentations. | Used for real-time geometric and photometric transformations (rotations, flips, contrast changes) to improve model generalizability [47]. |
| L-Cystine N-carboxyanhydride | L-Cystine N-carboxyanhydride, MF:C8H8N2O6S2, MW:292.3 g/mol | Chemical Reagent |
Overcoming Clinical Hurdles: Troubleshooting Variability and Optimizing Outcomes
Neurostimulation therapies represent a rapidly advancing frontier in treating neurological disorders and enhancing human cognition. However, a persistent and significant challenge hampers the field: the profound variability in treatment efficacy across individual patients. This variability is influenced by a complex interplay of anatomical, physiological, and technical factors. Understanding and addressing these sources of heterogeneity is critical for advancing neurostimulation from a generalized intervention to a precise, personalized therapeutic tool. Computational models have emerged as a powerful methodology to dissect these sources of variability, offering a pathway to optimize stimulation parameters for individual patient profiles. This article explores the core sources of interpatient variability in neurostimulation outcomes and details how computational modeling frameworks are being leveraged to create personalized, and therefore more effective, treatment protocols.
Quantitative Data on Efficacy and Variability
Clinical studies and meta-analyses consistently reveal significant heterogeneity in patient responses to various neurostimulation techniques. The tables below summarize key quantitative findings on efficacy and the factors contributing to variable outcomes.
Table 1: Meta-Analysis Findings for Non-Invasive Brain Stimulation (NIBS) Efficacy [50]
| Condition | Stimulation Technique | Standardized Mean Difference (SMD) vs. Sham | Heterogeneity (I²) |
|---|---|---|---|
| Generalized Anxiety Disorder | TMS | -1.8 (95% CI: -2.6 to -1.0) | Not Significant |
| Substance Use Disorder | tDCS | -0.73 (95% CI: -1.00 to -0.46) | Not Significant |
| Obsessive-Compulsive Disorder | TMS | -0.66 (95% CI: -0.91 to -0.41) | Significant |
| Unipolar Depression | TMS | -0.60 (95% CI: -0.78 to -0.42) | Significant |
| Schizophrenia (Working Memory) | tDCS | -0.38 (95% CI: -0.74 to -0.03) | Not Significant |
Table 2: Documented Sources of Interpatient Variability in Neurostimulation
| Source of Variability | Specific Factors | Impact on Efficacy |
|---|---|---|
| Anatomy | Individual brain/spinal cord anatomy, head size/circumference, electrode-to-nerve distance [51] [11] | Influences electric field distribution and neural target engagement [27]. |
| Pathophysiology | Nature and severity of injury/disease, baseline cognitive performance [11] [52] | Alters underlying excitability and plasticity, affecting response to stimulation. |
| Stimulation Parameters | Electrode configuration, current intensity, pulse width, frequency [51] [53] | Directly determines which neural elements are activated and the mode of activation. |
| Outcome Measurement | Focus on pain intensity vs. multidimensional assessment (IMMPACT criteria) [54] | Inconsistent reporting leads to variable perceived success rates across studies. |
Experimental Protocols for Investigating Variability
Protocol for Patient-Specific Computational Modeling of Peripheral Nerve Stimulation
This protocol is designed to investigate how anatomical differences lead to variable neural recruitment, as demonstrated in pudendal nerve stimulation studies [51].
1. Patient Imaging and Model Reconstruction:
- Imaging: Acquire high-resolution magnetic resonance (MR) images of the target pelvic region from implanted patients. Following implantation, obtain computed tomography (CT) scans to precisely localize the electrode geometry.
- Segmentation: Manually or semi-automatically segment the key anatomical structures from the images, including the pudendal nerve, its branches (genital, perineal, rectal), and the surrounding tissue (fat, muscle, bone).
- Volume Conductor Model: Construct a patient-specific three-dimensional finite element method (FEM) model from the segmented anatomy. Assign electrical conductivity values to each tissue type.
- Neural Models: Incorporate multi-compartment cable models of axons within the pudendal nerve to simulate their response to applied electric fields.
2. Simulation and Analysis:
- Finite Element Analysis (FEA): Solve the FEM model to compute the electric potential field generated in the tissue by specific stimulation configurations (e.g., contact selection, current amplitude).
- Activation Threshold Calculation: Apply the extracellular potential fields along the multi-compartment axon models to calculate the activation threshold for each neural fiber.
- Recruitment Analysis: Determine the relative recruitment of the different nerve branches (genital, perineal, rectal) across multiple patients. Systematically analyze the influence of electrode-to-nerve distance, stimulation configuration, and pulse width on recruitment profiles.
Protocol for AI-Optimized, Home-Based Neurostimulation for Cognitive Enhancement
This protocol outlines a method for personalizing transcranial random noise stimulation (tRNS) for sustained attention, addressing variability from baseline ability and anatomy [11].
1. Participant Characterization:
- Baseline Cognitive Assessment: Administer a sustained attention task (e.g., a continuous performance task) to establish a pre-stimulation performance metric (A' or d-prime).
- Anatomical Measurement: Record head circumference as a proxy for anatomical variability that affects current flow.
2. Personalized Bayesian Optimization (pBO) Algorithm:
- Algorithm Setup: Develop a pBO algorithm that uses baseline performance and head circumference as inputs to its Gaussian Process model.
- Remote Stimulation Sessions: Participants receive neurostimulation at home using a validated, remotely programmable tRNS device.
- Iterative Parameter Search: In each session, the pBO algorithm selects a current intensity (e.g., ranging from 0.5 mA to 2.0 mA). The participant's performance on the attention task during stimulation is fed back to the algorithm.
- Convergence: The algorithm iteratively explores the parameter space, building a patient-specific model of the inverted U-shaped relationship between current intensity and cognitive benefit, ultimately converging on the optimal personalized dose.
3. Validation:
- Control Groups: Compare the pBO-optimized tRNS against a sham stimulation group and a group receiving a fixed, "one-size-fits-all" current intensity (e.g., 1.5 mA) in a double-blind, randomized controlled trial.
- Outcome Analysis: Analyze the differential improvement in sustained attention, with a specific focus on comparing low versus high baseline performers.
Computational Optimization Frameworks
For invasive stimulation, such as Spinal Cord Stimulation (SCS), optimization frameworks can derive patient-specific stimulation parameters. The objective is to find the current fractions (( \alpha_i )) across an electrode array that maximize the activation of a Region of Interest (ROI) while minimizing activation in a Region of Avoidance (ROA) [53].
Single-Objective Optimization Problem: [ \text{maximize:} \quad \max(\mathcal{F}(X)) \quad X \in \text{ROI} ] where ( \mathcal{F}(X) ) is the activating function (e.g., ( d^2V/dr^2 ) for axons) at spatial point ( X ). The field is a linear combination of contributions from individual contacts: ( \mathcal{F}(X, \alpha) = \sum{i=1}^n \alphai fi(X) ), subject to the constraint of balanced currents (( \sum \alphai = 0 ), ( \sum |\alpha_i| = 2 )).
Solution via Smooth Approximation:
- The non-differentiable
maxoperator is approximated using a smooth Log-Sum-Exponent function: [ \text{maxS}(\mathcal{F}(X, \alpha), \beta) = \frac{\sum{i=1}^m \mathcal{F}(Xi, \alpha) \exp(\beta \mathcal{F}(Xi, \alpha))}{\sum{i=1}^m \exp(\beta \mathcal{F}(X_i, \alpha))} ] - The absolute value in the constraint is approximated with a smooth function: ( \text{absS}(\alpha, \gamma) = \alpha \tanh(\gamma \alpha) ).
- This allows the use of efficient analytic optimization methods, such as the method of Lagrange multipliers, to rapidly compute optimal current fractions for a given patient model.
The following diagram illustrates the integrated workflow for addressing variability, from data acquisition to personalized therapy.
Diagram 1: Personalized neurostimulation workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Computational Tools for Neurostimulation Research
| Item/Tool | Function/Description | Application Context |
|---|---|---|
| Finite Element Method (FEM) Software (e.g., COMSOL, Sim4Life) | Creates 3D volume conductor models from medical images to simulate electric field distributions in biological tissues [51] [53]. | Core for building patient-specific models of the brain, spinal cord, or peripheral nerves to predict field spread. |
| Multi-compartment Neuron Models (e.g., NEURON, Brian Simulator) | Biophysical models of axons and neurons that simulate the response to extracellular electrical stimulation, predicting activation thresholds [53]. | Used in conjunction with FEM models to understand which neural elements (e.g., axons, cell bodies) are activated by stimulation. |
| Bayesian Optimization (BO) Libraries (e.g., scikit-optimize, BoTorch) | A machine learning framework for efficiently optimizing expensive black-box functions, requiring minimal evaluations to find a global optimum [11]. | Ideal for personalizing stimulation parameters (e.g., current intensity) by iteratively testing and updating based on patient-specific responses. |
| IMMPACT Criteria Checklist | A standardized set of six core outcome domains for chronic pain trials, including pain intensity, physical and emotional function, and patient satisfaction [54]. | Ensures comprehensive and consistent assessment of therapeutic outcomes in clinical trials, capturing benefits beyond simple pain scores. |
Signaling Pathways in Neurostimulation and Plasticity
The therapeutic effects of neurostimulation are mediated by the activation of specific neural pathways and the induction of synaptic plasticity.
Diagram 2: Key neuroplasticity pathways modulated by stimulation.
Electrical stimulation induces neuronal depolarization, which can modulate synaptic plasticity through several key mechanisms [52]:
- Long-Term Potentiation (LTP): Brief, high-frequency stimulation leads to strong depolarization, relieving the Mg²⺠block of NMDA receptors. The subsequent influx of calcium into the postsynaptic cell triggers intracellular cascades that strengthen the synapse.
- Long-Term Depression (LTD): Prolonged, low-frequency stimulation results in a modest rise in postsynaptic calcium, which activates phosphatases and leads to synaptic weakening.
- Spike-Timing-Dependent Plasticity (STDP): The precise timing of presynaptic and postsynaptic spikes dictates the sign of plasticity. If the presynaptic neuron fires just before the postsynaptic neuron, LTP is induced; the reverse order induces LTD.
Traumatic Brain Injury (TBI) and other neurological conditions can dysregulate these plasticity mechanisms, leading to either hyperexcitability or hypoexcitability [52]. Neurostimulation aims to restore this balance by selectively inducing LTP or LTD to promote functional recovery and alleviate symptoms.
Closed-loop neurostimulation (CLNS) represents a paradigm shift in neuromodulation, moving beyond static, predetermined stimulation parameters to dynamic, responsive systems that adapt to a patient's real-time neural state [55] [56]. This approach is founded on the recognition that neural circuits and pathological states are highly dynamic, meaning the same electrical stimulus can have different effects depending on the underlying physiological context [56]. In contrast to traditional open-loop systems, which deliver stimulation according to a fixed schedule, closed-loop systems continuously monitor physiological biomarkers, process this information through sophisticated algorithms, and dynamically adjust stimulation parameters to optimize therapeutic outcomes [57] [56]. This shift enables unprecedented precision in treating neurological and psychiatric disorders, particularly for conditions like chronic pain where the pathological state is inherently fluctuating and brain-wide [55].
Fundamental Principles and Comparative Advantages
Core Components of a Closed-Loop System
A functional CLNS system integrates several key components:
- Sensing and Monitoring: Continuous recording of physiological signals via modalities like EEG, fMRI, fNIRS, or evoked compound action potentials (ECAPs) [55] [58].
- Signal Processing and Biomarker Detection: Real-time analysis of neural data to detect clinically relevant signatures or states using advanced computational methods [55].
- Control Algorithm: The "brain" of the system that decides when and how to stimulate based on the detected state. This may employ machine learning, reinforcement learning, or predefined rules [55] [56].
- Stimulation Delivery: Adjustable neuromodulation interface that delivers precisely titrated electrical stimulation [56].
Comparative Efficacy: Closed-Loop vs. Open-Loop Systems
Table: Clinical Outcomes of Closed-Loop vs. Open-Loop Neuromodulation
| Outcome Metric | Closed-Loop Systems | Open-Loop Systems |
|---|---|---|
| Pain Reduction | Superior, sustained pain relief [58] | Variable, often inconsistent [55] [58] |
| Therapeutic Precision | High (state-dependent stimulation) [56] | Low (fixed parameters regardless of state) [56] |
| Side Effects | Reduced (minimizes over-stimulation) [58] | More frequent (static settings) [58] |
| Power Consumption | Lower (stimulation only when needed) [56] | Higher (continuous stimulation) |
| Functional Improvement | Significant enhancement in quality of life [58] | Moderate improvement |
Computational Frameworks for State Decoding and Adaptive Control
Multimodal Biomarker Integration
Modern CLNS frameworks leverage complementary neuroimaging modalities to construct comprehensive brain-state representations [55]:
- fMRI: Provides high spatial resolution for identifying network-level modulation, such as enhanced connectivity between anterior cingulate cortex and prefrontal regions during effective stimulation [55].
- EEG: Offers millisecond temporal resolution to capture rapid cortical dynamics, including frontal alpha power increases (reflecting cortical inhibition) and gamma coherence across somatosensory and prefrontal areas [55].
- fNIRS: Delivers ecological validity for monitoring prefrontal oxygenation—a biomarker linked to analgesia—in naturalistic contexts [55].
Machine Learning Approaches for State Decoding
Table: AI-Driven Methods for Neural Decoding in CLNS
| Algorithm Type | Application in CLNS | Key Advantages |
|---|---|---|
| Deep Neural Networks | Feature extraction from high-dimensional fMRI/fNIRS data [55] | Identifies complex spatial patterns in neural activity |
| Convolutional Architectures | Spatial pattern recognition in neuroimaging data [55] | Captures regional activation features (e.g., in prefrontal cortex, insula) |
| Recurrent Models | Analysis of dynamic EEG signals [55] | Models temporal sequences (e.g., gamma synchrony, alpha suppression) |
| Reinforcement Learning | Optimizing stimulation parameters in uncertain environments [55] | Continuously improves control strategy based on therapeutic outcomes |
| Support Vector Machines | Patient stratification (responder vs. non-responder classification) [55] | Informs pre-treatment decisions |
Dynamic Workflow of a Closed-Loop System
Application Notes and Experimental Protocols
Protocol 1: Implementing Closed-Loop TENS for Chronic Pain
Objective: To establish a responsive transcutaneous electrical nerve stimulation (TENS) system that adapts to individual brain-state fluctuations for chronic pain management [55].
Materials and Equipment:
- Multimodal neuroimaging suite (EEG-fNIRS integration)
- Medical-grade TENS device with API for parameter control
- Real-time signal processing platform (e.g., BCI2000, OpenVibe)
- Machine learning framework (Python/TensorFlow or MATLAB)
Procedure:
- Baseline Assessment:
- Collect 10-minute resting-state EEG and fNIRS data
- Identify patient-specific pain biomarkers (e.g., elevated gamma power, reduced prefrontal oxygenation)
- Establish individual pain network connectivity profile via fMRI
System Calibration:
- Define stimulation parameter bounds (amplitude: 2-50mA, frequency: 2-100Hz, pulse width: 50-400μs)
- Map neural features to stimulation parameters using reinforcement learning
- Set safety thresholds and stopping criteria
Closed-Loop Operation:
- Continuously monitor EEG gamma power (30-45Hz) and prefrontal fNIRS oxygenation
- When gamma power exceeds 2 standard deviations above baseline for >5 seconds, trigger stimulation
- Adjust stimulation amplitude proportionally to gamma power deviation
- Modulate frequency based on prefrontal oxygenation levels
- Update control policy every 2 minutes based on analgesic efficacy
Outcome Measures:
- Pain intensity scales (NRS) recorded every 15 minutes
- Neural engagement metrics (target biomarker modulation)
- Stimulation efficiency (energy delivery per therapeutic effect)
Protocol 2: Closed-Loop Spinal Cord Stimulation for Neuropathic Pain
Objective: To implement ECAP-controlled spinal cord stimulation that maintains therapy within an individualized therapeutic window [58].
Materials and Equipment:
- ECAP-capable SCS system (e.g., Evoke system)
- Programming interface with real-time telemetry
- Ambulatory pain and function logging system
Procedure:
- Therapeutic Window Determination:
- Gradually increase stimulation amplitude until perception threshold
- Continue increasing until discomfort threshold
- Define therapeutic window as 60-90% of perceptual range
ECAP Calibration:
- Establish baseline ECAP amplitude-response curve
- Set target ECAP range corresponding to therapeutic window
- Configure recording electrode to capture evoked potentials
Closed-Loop Control:
- Deliver sub-perceptual test pulses interleaved with therapeutic stimulation
- Measure ECAP amplitude after each test pulse
- Adjust stimulation current to maintain ECAP within target range
- Adapt to positional changes (supine, upright, walking)
Outcome Assessment:
- Pain diary completion twice daily
- ODI (Oswestry Disability Index) weekly
- Stimulation usage patterns and consistency reports
Key Research Reagent Solutions
Table: Essential Resources for Closed-Loop Neurostimulation Research
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Neuroimaging Platforms | Simultaneous EEG-fNIRS systems, portable MRI | Multimodal brain-state decoding across spatial and temporal scales [55] |
| Signal Processing Tools | EEGLAB, FieldTrip, MNE-Python | Real-time feature extraction (alpha power, gamma coherence) [55] |
| Machine Learning Libraries | TensorFlow, PyTorch, Scikit-learn | Development of adaptive classification and control algorithms [55] |
| Neuromodulation Devices | ECAP-capable SCS, research TENS with API | Precisely controlled stimulation delivery with parameter modulation [58] |
| Computational Modeling | Brian, NEURON, NEST | Simulation of neural network responses to stimulation parameters |
Signaling Pathways in Closed-Loop Neuromodulation
Quantitative Outcomes and Clinical Validation
Efficacy Metrics Across Neuromodulation Approaches
Table: Performance Benchmarks for Closed-Loop Neuromodulation Systems
| System Type | Clinical Population | Efficacy Outcomes | Superiority vs. Open-Loop |
|---|---|---|---|
| CL-SCS [58] | Chronic low back pain | 70-80% sustained pain reduction | Significant (p<0.01) |
| aDBS [57] | Parkinson's disease | 55-60% improvement in motor symptoms | Equivalent efficacy, reduced side effects |
| Responsive Neurostimulation [57] | Epilepsy | 65-75% seizure reduction | Superior in long-term outcomes |
| CL-TENS [55] | Chronic pain (heterogeneous) | Enhanced analgesia, brain network normalization | Theoretical (under investigation) |
Biomarker Modulation Correlations
Successful closed-loop intervention demonstrates consistent biomarker modulation:
- EEG: Frontal alpha power increase (>2dB from baseline) correlates with analgesic response [55]
- fNIRS: Prefrontal oxygenation elevation (15-20% increase) associated with pain relief [55]
- fMRI: Reduced insula and default mode network hyperactivity, strengthened ACC-prefrontal connectivity [55]
- ECAPs: Maintained amplitude within therapeutic range (60-90% of perceptual threshold) ensures consistent dorsal column recruitment [58]
Implementation Challenges and Future Directions
Despite promising results, CLNS faces several implementation hurdles. Ethical considerations around neural data privacy, algorithmic transparency, and patient autonomy require careful framework development [57]. Technical challenges include optimizing biomarker specificity, managing computational complexity for implantable devices, and establishing standardized validation protocols. Future development will focus on multi-modal biomarker integration, increasingly sophisticated adaptive algorithms capable of long-term learning, and miniaturization of sensing-stimulation systems for broader clinical application [55] [56]. The convergence of artificial intelligence with neurotechnology promises truly personalized neuromodulation therapies that continuously self-optimize based on individual patient responses and changing disease states.
The optimization of neurostimulation therapies through computational modeling is a rapidly advancing field, yet two significant challenges consistently impede progress: the reliable identification of physiological biomarkers and the mitigation of stimulation artifacts that corrupt neural recordings. Overcoming these hurdles is paramount for the development of effective personalized and closed-loop neuromodulation systems. This application note details structured experimental protocols and computational strategies to address these challenges, providing a framework for researchers and scientists engaged in neurostimulation optimization.
Challenge 1: Biomarker Identification for Predicting Treatment Response
A primary obstacle in neuromodulation is the variability in individual patient response. Identifying robust, quantifiable biomarkers that can predict treatment efficacy is thus a critical research focus.
Quantitative Electroencephalography (QEEG) Biomarkers
Electroencephalography (EEG), particularly quantitative EEG (QEEG), serves as a key tool for identifying non-invasive biomarkers due to its high temporal resolution and widespread availability. Research indicates that specific oscillatory patterns in baseline (pre-treatment) EEG can predict response to various neurostimulation techniques.
Table 1: QEEG Biomarkers for Neurostimulation Response Prediction
| Neurostimulation Technique | Condition | Promising Biomarkers | Predicted Outcome |
|---|---|---|---|
| Repetitive Transcranial Magnetic Stimulation (rTMS) [59] | Mild Cognitive Impairment (MCI) | Baseline spectral power in theta (6-8 Hz) and alpha (8-9 Hz) sub-bands | Improved cognitive function post-treatment |
| Transcranial Direct Current Stimulation (tDCS) [60] | Alzheimer's Disease (AD) | Spectral power features at EEG channels FC1, F8, CP5, Oz, and F7 | Cognitive response to tDCS combined with cognitive intervention |
| rTMS [59] | Major Depressive Disorder (MDD) | Frontal theta activity; large spectral power in θ2 (6–8 Hz) and α1 (8–9 Hz) | Positive treatment outcome for depression |
Experimental Protocol: Identifying QEEG Biomarkers for rTMS in MCI
This protocol outlines a method to identify baseline QEEG biomarkers that predict response to rTMS in patients with Mild Cognitive Impairment, based on a published pilot study design [59].
1. Participant Screening and Recruitment:
- Population: Recruit adults aged ≥60 years, diagnosed with MCI according to DSM-V criteria.
- Cognitive Assessment: Administer the Montreal Cognitive Assessment (MoCA) or Mini-Mental State Examination (MMSE) to all participants at baseline.
- Exclusion Criteria: Include standard contraindications for rTMS (e.g., metallic implants, history of seizures) and inability to complete study procedures.
2. Baseline EEG Data Acquisition:
- Equipment: Use a high-density EEG system (e.g., 64-channel or more).
- Procedure: Record resting-state EEG for a minimum of 6 minutes in an eyes-open condition, with participants focusing on a fixed point to minimize ocular artifacts.
- Parameters: Maintain standard sampling rates (e.g., ≥500 Hz) and filter settings.
3. rTMS Intervention:
- Protocol: Administer 10 sessions of high-frequency rTMS over two weeks.
- Target: Locate the left dorsolateral prefrontal cortex (DLPFC) using the EEG 10-20 system or neuronavigation.
- Stimulation Parameters: 20 Hz frequency, 2000 pulses per session.
4. Post-Intervention Assessment and Analysis:
- Outcome Measure: Re-administer the MoCA/MMSE post-treatment.
- Responder Classification: Define responders as those showing a Minimal Clinically Important Difference (MCID) (e.g., an increase of ≥1 point on MoCA or ≥3 points on MMSE).
- QEEG Analysis: Process baseline EEG data to compute power spectral density. Compare spectral power across frequency bands (delta, theta, alpha, beta) between pre-defined responder and non-responder groups using statistical tests (e.g., t-tests, ANOVA). Machine learning classifiers (e.g., Random Forest) can be applied to identify the most predictive EEG features and channels [60].
Challenge 2: Mitigation of Stimulation Artifacts
In closed-loop neuromodulation systems, stimulation artifacts can swamp the low-amplitude neural signals used for feedback, rendering the system ineffective. Computational models provide a powerful method to understand and mitigate these artifacts.
Computational Modeling of Stimulation and Artifact Dynamics
Computational models that integrate detailed 3D nerve anatomies, cuff electrode geometries, and accurate electrophysiological fiber models can simulate the effects of complex stimulation paradigms and the subsequent artifact fields [61]. This allows researchers to:
- Probe Mechanisms: Understand how new stimulation waveforms (e.g., intermittent interferential current stimulation) activate specific neural fibers.
- Optimize Protocols: Test and optimize stimulation parameters in silico before in vivo experiments, saving time and resources.
- Predict Artifacts: Model the spatial and temporal characteristics of the stimulation artifact, informing the design of artifact rejection algorithms.
Table 2: Strategies for Stimulation Artifact Mitigation
| Strategy Category | Specific Method | Principle of Operation | Key Considerations |
|---|---|---|---|
| Stimulation Waveform Design | Interferential Currents (e.g., i2CS) [61] | Uses high-frequency carriers; activation occurs at the interference focus, potentially away from recording contacts. | Requires multi-contact cuff electrodes; computational models are vital for optimization. |
| Recording System Design | Blanking Circuits | Disconnects the amplifier input during the stimulation pulse. | Simple but results in data loss; ineffective for long-lasting artifacts. |
| Signal Processing | Template Subtraction | Models and subtracts the artifact waveform from the recorded signal. | Requires a precise artifact template; performance degrades with non-stationary artifacts. |
Experimental Protocol: Using Computational Models to Optimize Stimulation and Mitigate Artifacts
This protocol describes a workflow for employing computational models to optimize a selective peripheral nerve stimulation paradigm and inform artifact mitigation strategies, as demonstrated in recent bioelectronic medicine research [61].
1. Model Construction:
- Anatomy: Create a realistic 3D model of the target nerve (e.g., vagus nerve). Use histological sections or pre-existing anatomical atlases. For patient-specific approaches, incorporate MRI-based anatomical data [62].
- Electrode: Incorporate the precise geometry of the multi-contact cuff electrode (MCE) into the model.
- Tissue Properties: Assign appropriate electrical conductivity values to the nerve, cuff material, and surrounding tissue.
2. Simulation of Stimulation and Artifacts:
- Stimulation Parameters: Define the stimulation protocol in the model (e.g., i2CS: high-frequency carriers, amplitude modulation, pulse duration).
- Electric Field Solving: Use finite-element method (FEM) solvers (e.g., within platforms like Sim4Life [62]) to compute the electric field distribution.
- Neural Activation: Combine the electric field data with biophysical models of neurons (e.g., Hodgkin-Huxley) to predict action potential generation in different fiber types.
- Artifact Modeling: Simulate the artifact recorded by each contact of the MCE during and after the stimulation pulse.
3. In Vivo Validation:
- Animal Model: Conduct acute experiments (e.g., in pig models) implanting the same MCE used in the model.
- Stimulation & Recording: Apply the simulated stimulation protocols while recording neural signals and physiological readouts (e.g., muscle activation, breathing rate).
- Data Correlation: Compare the model-predicted neural responses and artifact morphology with the empirically recorded data. Iteratively refine the model to improve its accuracy.
4. Protocol Optimization and Closed-Loop Implementation:
- Optimization: Use the validated model to exhaustively test stimulation parameters in silico to maximize target fiber activation and minimize off-target effects.
- Artifact Rejection: Based on the simulated artifact characteristics, develop and test signal processing algorithms (e.g., adaptive filters) to recover neural signals post-stimulation.
- Deployment: Implement the optimized parameters and artifact rejection strategies in a closed-loop system for pre-clinical testing.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Reagents and Tools for Neurostimulation Optimization Research
| Item | Function/Application | Examples & Notes |
|---|---|---|
| Multi-Contact Cuff Electrodes (MCEs) | Enables selective stimulation and recording from peripheral nerves. | Essential for implementing complex waveforms like i2CS [61]. |
| High-Density EEG Systems | Records brain activity with high temporal resolution for biomarker discovery. | Used to capture resting-state or task-based oscillatory activity [59] [60]. |
| Computational Modeling Platforms | Simulates electric fields, neural activation, and artifacts in realistic anatomies. | Sim4Life, NEURON; allows in silico testing and optimization [61] [62]. |
| Transcranial Magnetic Stimulator | Non-invasive brain stimulation for therapeutic intervention. | Used for rTMS protocols in conditions like MCI and depression [59]. |
| tDCS/tRNS Devices | Applies weak electrical currents for neuromodulation. | Can be combined with AI for home-based, personalized protocols [11]. |
| Machine Learning Libraries | Analyzes high-dimensional data (e.g., EEG) to identify predictive features. | Python (scikit-learn), MATLAB; used for classifying responders/non-responders [60]. |
| Real-time fMRI/EEG Setup | Provides brain-state feedback for adaptive closed-loop neuromodulation. | Core component for systems that adjust stimulation based on dynamic biomarkers [63]. |
Brain-based technologies for human augmentation face significant challenges in personalization and real-world translation. This application note details a framework for AI-driven personalized Bayesian optimization that remotely adjusts neurostimulation parameters based on individual baseline ability and head anatomy to enhance sustained attention in home environments. Validated through in silico modeling and double-blind, sham-controlled studies, the approach aligns with MRI-based models and neurobiological theories while maximizing efficacy and enabling scalable, personalized cognitive enhancement. The system represents a significant advancement toward accessible, personalized cognitive enhancement and therapy in real-world settings, addressing critical barriers in the field of computational models for neurostimulation optimization research [11] [64].
Sustained attention—the ability to maintain focus over extended periods—is essential for tasks such as driving, learning, and work-related activities. Deficits in this cognitive domain are linked to various neurological and psychiatric disorders, including schizophrenia, depression, ADHD, Alzheimer's disease, and long COVID [11]. While neurostimulation, particularly transcranial electrical stimulation (tES), has emerged as a promising intervention, outcomes have been inconsistent due to "one-size-fits-all" approaches that neglect individual differences in brain anatomy and baseline performance [11].
The integration of artificial intelligence with neurostimulation creates adaptive systems that overcome two significant barriers: personalization and ecological validity. Traditional personalization methods require resource-intensive procedures like exhaustive parameter testing or MRI-based adjustments, while laboratory settings poorly reflect real-world environments [11]. The system described herein utilizes personalized Bayesian Optimization (pBO) to tailor stimulation parameters remotely, enabling effective home-based deployment while accumulating data across users to refine protocols over time [11].
Experimental Protocols
Protocol 1: Development of Personalized Bayesian Optimization Algorithm
Objective: To develop and train a personalized Bayesian optimization algorithm for adjusting tRNS parameters based on individual baseline attention performance and head anatomy [11].
Materials:
- CE-marked tRNS headgear for home use
- Tablet devices with sustained attention task application
- 103 healthy participants (aged 18-35)
- Head circumference measurement tools
Methodology:
- Baseline Assessment: Participants complete a sustained attention task (A' measure) to establish cognitive performance baseline [11].
- Anatomical Measurement: Record head circumference as a proxy for anatomical variability affecting current intensity requirements [11].
- Algorithm Training: Implement Bayesian optimization to identify optimal stimulation parameters using Gaussian Process surrogate models:
- Model the relationship between current intensity and baseline performance
- Model the relationship between current intensity and head circumference
- Identify inverted U-shaped "sweet spot" for maximum effectiveness
- Determine intensities to avoid that may impair performance [11]
- Data Collection: Conduct 290 home-based sessions to train the algorithm across diverse individual profiles [11].
Output: Personalized Bayesian optimization algorithm capable of recommending optimal tRNS parameters for new individuals based on their baseline attention performance and head circumference.
Protocol 2: In Silico Modeling of Optimization Approaches
Objective: To compare the performance of pBO against alternative optimization methods using computational modeling [11].
Materials:
- Computational modeling environment
- Ackley function for benchmark testing [11]
- Simulation of different noise conditions
Methodology:
- Model Setup: Implement pBO, Random Search, and non-personalized Bayesian Optimization using the Ackley function as a benchmark landscape [11].
- Noise Introduction: Introduce varying levels of noise to simulate real-world measurement variability.
- Performance Evaluation: Compare optimization efficiency across methods by measuring convergence speed and parameter estimation accuracy.
- Noise Impact Analysis: Assess how each method performs under increasing noise conditions, noting where pBO's advantages diminish due to difficulty distinguishing signal from noise [11].
Output: Quantitative comparison of optimization approaches validating pBO's superior performance under realistic noise conditions.
Protocol 3: Double-Blind Validation Study
Objective: To validate pBO-tRNS against one-size-fits-all tRNS and sham tRNS in a new participant sample [11].
Materials:
- 37 new participants (aged 18-35)
- Double-blind study design
- Active and sham tRNS equipment
- Sustained attention task metrics
Methodology:
- Participant Recruitment: Recruit new participants not involved in algorithm development.
- Group Assignment: Implement double-blind conditions with participants receiving:
- pBO-tRNS (personalized parameters)
- One-size-fits-all tRNS (1.5 mA)
- Sham tRNS [11]
- Stratified Analysis: Perform median split of participants based on baseline performance (50th percentile = 0.725 A' score) into low and high baseline performers [11].
- Assessment: Measure sustained attention performance (A') across multiple sessions.
- Statistical Analysis: Employ mixed-effects linear regression with random effects for participant and session.
- Side Effects Monitoring: Record and compare frequency and severity of side effects across conditions [11].
Output: Validation data demonstrating comparative efficacy of pBO-tRNS, particularly for low baseline performers.
Quantitative Results and Data Analysis
Performance Comparison of Optimization Methods
Table 1: In silico performance comparison of optimization methods under varying noise conditions
| Optimization Method | Convergence Speed | Parameter Accuracy | Noise Robustness |
|---|---|---|---|
| Personalized BO | Highest | Highest | Moderate |
| Non-personalized BO | Moderate | Moderate | Moderate |
| Random Search | Lowest | Lowest | Highest |
Source: Experiment 2 results from [11]
Clinical Outcomes by Baseline Performance
Table 2: Effects of different neurostimulation conditions on sustained attention performance
| Participant Group | Stimulation Condition | Performance Improvement (A') | Statistical Significance |
|---|---|---|---|
| Low Baseline | pBO-tRNS | +0.76 | p = 0.015 |
| Low Baseline | One-size-tRNS | Not significant | p = 0.61 |
| Low Baseline | Sham tRNS | Baseline | Reference |
| High Baseline | pBO-tRNS | Not significant | p = 0.58 |
| High Baseline | One-size-tRNS | Not significant | Not significant |
| High Baseline | Sham tRNS | Not significant | Not significant |
Source: Experiment 3 results from [11]
Technical Specifications
Bayesian Optimization Parameters
Table 3: Technical specifications of the Bayesian optimization system
| Component | Specification | Function |
|---|---|---|
| Surrogate Model | Gaussian Process | Models unknown objective function from data |
| Acquisition Function | Not specified (Standard choices: EI, UCB, PI) | Guides selection of next query point |
| Personalization Features | Baseline performance, Head circumference | Individualizes parameter search space |
| Stimulation Parameters | Current intensity (0-2.0 mA) | Directly optimized variable |
| Kernel Function | Not specified (Common: Matern, RBF) | Defines similarity between data points |
| Convergence Criteria | Improvement threshold or iteration limit | Determines when optimization is complete |
Neurostimulation Equipment Specifications
Table 4: Neurostimulation device and component specifications
| Component | Specification | Function |
|---|---|---|
| Stimulation Type | Transcranial Random Noise Stimulation (tRNS) | Modulates neural activity via stochastic resonance |
| Current Range | 0-2.0 mA | Adjustable intensity based on personalization |
| Electrode Placement | Targeting dlPFC | Modulation of sustained attention networks |
| Device Certification | CE-marked | Meets European Union safety standards |
| Application Environment | Home-based | Enables ecological validity and scalable deployment |
Signaling Pathways and Neurobiological Mechanisms
tRNS Mechanism of Action
Diagram 1: tRNS neurobiological mechanisms (57 characters)
Personalized Bayesian Optimization Workflow
Diagram 2: pBO workflow for neurostimulation (45 characters)
Research Reagent Solutions
Table 5: Essential research materials and their applications
| Reagent/Equipment | Function/Application |
|---|---|
| CE-marked tRNS Headgear | Home-based delivery of transcranial random noise stimulation; ensures safety compliance |
| Tablet-based Attention Task | Assessment of sustained attention (A' metric) in ecological home environment |
| Bayesian Optimization Platform | Implements personalized parameter selection using Gaussian Processes |
| Head Circumference Measurement | Proxy for anatomical variability affecting current intensity requirements |
| In Silico Modeling Environment | Validation of optimization approaches using benchmark functions (e.g., Ackley) |
| Double-Blind Control Setup | Ensures rigorous experimental design for sham-controlled conditions |
Discussion and Implementation Guidelines
The implementation of AI-driven personalized neurostimulation represents a paradigm shift in cognitive enhancement technologies. The significant improvement observed in low baseline performers (β = 0.76, SE = 0.29, p = 0.015) demonstrates the potential for reducing cognitive disparities, addressing ethical concerns about neurostimulation widening mental performance gaps [11]. The inverse relationship between baseline performance and stimulation benefit aligns with mechanisms of stochastic resonance, where added noise enhances signal detection in non-linear systems [11].
For research replication, careful attention should be paid to the head circumference measurement protocol, as this critically influences current intensity personalization. The inverted U-shaped relationship between current intensity and both baseline performance and head circumference necessitates sufficient parameter sampling to identify optimal ranges while avoiding detrimental intensities [11].
The home-based deployment model requires robust participant engagement strategies, as monotonous tasks in remote settings present adherence challenges. Future implementations should consider performance-based incentives while addressing associated ethical considerations [11].
This approach advances the United Nations' Sustainable Development Goals, particularly SDG3 (Good Health and Well-Being) and SDG10 (Reduced Inequalities), by developing accessible cognitive enhancement technology while addressing disparities in learning and cognitive function [11].
Computational steering represents a paradigm shift in neurostimulation, using detailed in-silico models to precisely guide electrical currents to therapeutic neural targets while avoiding regions that cause side effects. As neurostimulation technologies evolve with increasingly complex electrode arrays and stimulation paradigms, the parameter space has become too vast for efficient manual exploration [14]. Computational models provide a critical framework to overcome this challenge, enabling the rational design of stimulation protocols that maximize efficacy and minimize adverse effects for therapies such as Deep Brain Stimulation (DBS), Spinal Cord Stimulation (SCS), and Vagus Nerve Stimulation (VNS) [53] [65]. This approach moves clinical programming beyond trial-and-error toward model-informed precision medicine.
Quantitative Comparison of Current Steering Technologies
Performance Metrics in Directional DBS
Current steering technologies distribute current between multiple contacts on segmented electrodes to shape the electrical field. A computational study comparing these technologies using a heterogeneous tissue model revealed significant differences in their performance characteristics [66].
Table 1: Comparison of Current Steering Technologies in Directional Deep Brain Stimulation
| Technology | Steering Laterality | Directional Accuracy | VTA Volume & Shape | Power Consumption |
|---|---|---|---|---|
| Single-Segment Activation (SSA) | Highest laterality | Variable based on placement | Asymmetric, focused | Low (single source) |
| Multiple Independent Current Control (MICC) | Reduced vs. SSA | Directional inaccuracy during radial steering | Larger volume, more spread | No consistent pattern vs. MSS |
| Multi-Stim Set (MSS) | Reduced vs. SSA | More pronounced inaccuracy vs. MICC | Smaller, more compact volume | No consistent pattern vs. MICC |
| Co-activation | Reduced vs. SSA | Greater accuracy at centerline between electrodes | Combined field pattern | Always lower than MICC or MSS |
The study implemented a finite element model (FEM) in Sim4Life v4.0 with the multimodal image-based detailed anatomical (MIDA) model, assigning inhomogeneous tissue properties to all structures using the IT'IS database [66]. A segmented DBS lead was placed in the subthalamic nucleus with a 0.5 mm interelectrode spacing and 0.5-mm thick encapsulation layer. The research distributed 3 mA of current between two electrodes with various splits using a pseudo-biphasic waveform (90 μs pulse width) at 130 Hz [66].
Optimization Outcomes in Spinal Cord Stimulation
An optimization framework for targeted SCS demonstrated how computational approaches can derive novel stimulation configurations that outperform conventional paradigms [53].
Table 2: Optimization Outcomes in Spinal Cord Stimulation
| Stimulation Scenario | Conventional Approach | Computational Optimization Result | Clinical Advantage |
|---|---|---|---|
| Simple ROI | Simple bipolar configuration | Resembled bipolar configuration | Validation of method |
| Multi-Objective (ROI + ROA) | Limited avoidance capability | Non-trivial configurations from Pareto fronts | Selective activation without side effects |
| Dorsal Horn targeting | Non-selective activation | Novel fields targeting DH without DC activation | Potential for improved pain relief |
The optimization framework used the Lagrange multiplier method with smoothing approximations to maximize the field driving polarization of targeted neurons while minimizing activation in regions of avoidance [53]. The approach was tested using a hybrid computational model consisting of finite element method models and multi-compartment models of axons and cells within the spinal cord.
Experimental Protocols
Protocol 1: Comparative Analysis of Current Steering Technologies in DBS
Objective: To quantitatively compare the performance of Multiple Independent Current Control (MICC), Multi-Stim Set (MSS), and co-activation current steering technologies on Volume of Tissue Activated (VTA) and power consumption [66].
Materials:
- Computational Platform: Sim4Life v4.0+ [66]
- Anatomical Model: Multimodal image-based detailed anatomical (MIDA) model [66]
- Tissue Properties: IT'IS database 3.1.1 for heterogeneous electrical properties [66]
- DBS Lead Model: Segmented lead (1-3-3-1 design) with 0.5 mm interelectrode spacing [66]
- Neuronal Models: Multicompartment axons (10 mm length, 5.7 μm diameter) distributed on perpendicular planes [66]
Methodology:
- Model Setup: Implement finite element model (FEM) in Sim4Life with MIDA head model
- Lead Placement: Position segmented DBS lead in subthalamic nucleus (STN) with tip near ventral border
- Encapsulation Layer: Add 0.5-mm thick encapsulation layer around lead
- Mesh Generation: Create rectilinear volumetric mesh grid with 0.1 mm maximum step size near electrode
- Stimulation Parameters: Apply 3 mA total current distributed between two electrodes with current splits from 100%-0% to 50%-50% in 12.5% steps
- Waveform: Use pseudo-biphasic waveform with 90 μs pulse width at 130 Hz
- VTA Calculation: Determine activation sites by interpolating electrical potentials along neurons and identifying action potential initiation sites
- Analysis: Quantify VTA laterality, directional accuracy, volume, shape, and power consumption
Protocol 2: Multi-Objective Optimization for Targeted SCS
Objective: To develop and validate an optimization framework for defining optimal current amplitudes across individual contacts in SCS electrode arrays to selectively target regions of interest (ROI) while avoiding regions of avoidance (ROA) [53].
Materials:
- Computational Framework: Custom optimization algorithms implemented in MATLAB or Python
- Finite Element Model: Realistic volume conductor model of spinal anatomy
- Neuronal Models: Multi-compartment models of axons and dorsal horn neurons
- Optimization Solver: Lagrange multiplier method with smoothing approximations
Methodology:
- Problem Formulation: Define single-objective optimization problem to maximize the maximum of the field (F) driving neuronal polarization in the ROI
- Field Estimation: Calculate F as the second derivative of electric potential (activating function) for axonal excitation
- Smooth Approximation: Replace non-differentiable maximum operator with smooth approximation using scaling parameter β
- Constraint Implementation: Apply current fraction constraints using smooth absolute value approximation with scaling parameter γ
- Multi-Objective Extension: Expand to multi-objective optimization to balance ROI activation against ROA avoidance
- Pareto Front Analysis: Generate and analyze Pareto fronts to identify optimal trade-off configurations
- Validation: Test optimized configurations in hybrid FEM and multi-compartment models to verify selective activation
Protocol 3: Vagus Nerve Stimulation Modeling for Selective Fiber Recruitment
Objective: To create a functionalized VN model for computationally assisted formulation of selective VNS protocols and optimization of electrode designs [65].
Materials:
- Platform: Sim4Life with T-NEURO feature [65]
- Anatomical Model: MIDA head and neck model [65]
- Nerve Model: Detailed VN geometry with fascicular structure
- Electrode Models: Customizable electrode geometries (helical, spiral, etc.)
- Axonal Models: Biophysical models of A-, B-, and C-fibers from NEURON libraries [65]
Methodology:
- VN Geometry Modeling: Create 3D VN model by extruding realistic 2D nerve cross-sections along anatomical trajectories
- Electrode Placement: Position electrode geometries around or within the VN model
- EM Simulation: Set up electro-quasi-static current dominated (EQSCD) solver simulations with Dirichlet boundary conditions for electrode voltages
- Axonal Population: Create and position axonal trajectories within fascicles using splines with defined fiber diameters and biophysical properties
- T-NEURO Simulation: Execute parallel simulations with multiple independent electric sources, each with customizable stimulation waveforms
- Titration Procedure: Identify threshold E-fields for action potential initiation in each axon
- Selectivity Analysis: Generate fiber recruitment curves for different axon populations and optimize stimulation parameters for selective activation
Computational Workflows and Signaling Pathways
Computational Steering Workflow for Neurostimulation Optimization
Multi-Objective Optimization Logic for Selective Stimulation
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Computational Resources for Neurostimulation Steering Research
| Resource Category | Specific Tools/Platforms | Function/Purpose | Key Applications |
|---|---|---|---|
| Computational Platforms | Sim4Life (with T-NEURO) [65], NEURON [65], Brian2 [67] | Multi-physics simulation, neuronal dynamics, network modeling | FEM calculations, axonal response prediction, large-scale network simulations |
| Anatomical Models | MIDA model [66] [65], ViP phantoms [65] | Realistic human anatomy with tissue properties | Electric field modeling in realistic head/body models |
| Tissue Property Databases | IT'IS Database [66] | Dielectric tissue properties for EM simulations | Assigning electrical conductivity and permittivity to tissues |
| Biophysical Neuronal Models | SENN model [65], Sweeney model [65], MOTOR model [65], Hodgkin-Huxley [68] | Predicting neural response to stimulation | Fiber recruitment curves, activation thresholds |
| Optimization Frameworks | Lagrange multiplier method [53], Smoothing approximations [53] | Solving constrained optimization problems | Current fraction optimization, selective activation |
| Experimental Validation | Two-photon calcium imaging [69], Accelerometer measurements [68] | Correlating model predictions with physiological outcomes | Behavioral correlation, neural activity recording |
Discussion and Future Directions
Computational steering represents the frontier of personalized neurostimulation therapy, transforming programming from an empirical art to an engineering science. The integration of heterogeneous tissue properties into these models is crucial, as simplified homogeneous models can misrepresent the steering accuracy and VTA shapes achieved by different current fractionalization technologies [66]. Future developments will likely focus on closed-loop systems that integrate real-time neural signals with computational steering algorithms to dynamically adjust stimulation parameters based on therapeutic needs.
The application of these approaches across different neuromodulation domains—from DBS and SCS to VNS and non-invasive techniques like temporal interference stimulation [68]—demonstrates the universal value of computational steering in improving the precision and efficacy of neurostimulation therapies. As these models continue to incorporate more elements of neural circuitry and their dynamic interactions, they will accelerate the development of next-generation neurostimulation therapies that are both more effective and better tailored to individual patient needs.
Validation and Comparative Analysis: Evaluating Classical and Emerging Techniques
1. Introduction
The field of neuromodulation is rapidly evolving beyond classical "one-size-fits-all" approaches. The integration of computational models is pivotal for optimizing neurostimulation parameters, personalizing therapies, and translating novel techniques from bench to bedside [70] [11] [38]. This document provides application notes and detailed experimental protocols for employing a six-dimensional benchmarking framework to quantitatively compare neuromodulation techniques, enabling data-driven selection and refinement for both basic research and clinical applications.
2. The Six-Dimensional Benchmarking Framework
The following framework facilitates a standardized, multi-faceted comparison of neuromodulation techniques. The table below summarizes the core dimensions and their definitions, synthesizing key considerations for computational and experimental research [70].
Table 1: The Six-Dimensional Framework for Benchmarking Neuromodulation Techniques
| Dimension | Definition | Considerations for Computational Models |
|---|---|---|
| Spatial Resolution | The physical precision of the stimulation focus. | Model the electric field, optical scattering, or ultrasonic wave propagation in anatomically detailed head models [10] [71]. |
| Temporal Resolution | The speed and precision with which neural activity can be controlled. | Simulate the dynamics of neuronal response to pulsed, continuous, or patterned stimulation protocols. |
| Cell-Type Specificity | The ability to target specific neuronal subtypes or glia. | Incorporate genetic and molecular data (e.g., opsin expression for optogenetics) into network models. |
| Stimulation Depth | The effective reach from the stimulation source to the target. | Simulate field attenuation with depth; critical for comparing superficial (TMS) vs. deep (tPBM, DBS) techniques [70] [71]. |
| Biosafety | The risk of tissue damage, heating, or unintended side effects. | Perform thermal and mechanical stress simulations alongside neuronal activation models [10]. |
| Clinical Feasibility | The practicality for human application (invasiveness, cost, portability). | Use model predictions to reduce costly clinical trial iterations; assess feasibility of home-use systems [11]. |
3. Application Note: Computational Modeling for Protocol Optimization
3.1. Background Computational models serve as digital twins of neurostimulation, allowing for the rapid, safe, and cost-effective exploration of parameter spaces. They are indispensable for linking the six-dimensional profile of a technique to its physiological outcomes [10] [38].
3.2. Workflow Diagram The following diagram illustrates a standardized computational workflow for benchmarking and optimizing neuromodulation protocols.
3.3. Key Computational Platforms & Reagents Table 2: Essential Tools for Computational Neuromodulation Research
| Tool / Reagent | Type | Function in Research |
|---|---|---|
| Sim4Life / o2S2PARC [10] | Software Platform | Cloud-native platform for creating, executing, and sharing full computational pipelines, from EM exposure to neuronal dynamics. |
| Personalized Bayesian Optimization (pBO) [11] | AI Algorithm | AI-driven method to personalize stimulation parameters (e.g., current intensity) based on individual baseline performance and anatomy. |
| SPIRIT-iNeurostim [72] | Reporting Guideline | Guidelines for reporting protocols of clinical trials involving implantable neurostimulation devices, ensuring rigor and reproducibility. |
| Cardiovascular-Baroreflex Model [38] | Computational Model | A closed-loop model predicting hemodynamic responses to neurostimulation for conditions like atrial fibrillation. |
4. Experimental Protocol 1: Comparative Efficacy Using Network Meta-Analysis
4.1. Objective To assess the comparative efficacy and acceptability of multiple neuromodulation techniques for a specific condition (e.g., post-stroke spasticity) against control treatments and active comparators.
4.2. Protocol Details This protocol is based on a recent network meta-analysis encompassing 185 randomized controlled trials [73].
- Primary Outcome: Change in spasticity measured by the Modified Ashworth Scale (MAS).
- Secondary Outcomes: Motor function improvement and acceptability (dropout rates).
- Interventions: Include all relevant neuromodulation techniques (e.g., HF-rTMS, LF-rTMS, atDCS, ctDCS, dtDCS) and botulinum toxin (BoNT) as an active control.
- Statistical Analysis:
- Pooling: Use random-effects models to calculate weighted mean differences (WMD) for continuous outcomes and risk ratios (RR) for dichotomous outcomes.
- Ranking: Estimate ranking probabilities for each intervention.
- Clinical Importance: Categorize findings as definite, probable, possible, or not clinically important based on the minimal clinically important difference (MCID).
- Confidence: Assess evidence quality using the CINeMA framework.
4.3. Application of the 6D Framework Interpret the results through the six-dimensional lens. For example, findings that tDCS techniques showed "probable clinical importance" for post-stroke spasticity [73] can be linked to their favorable clinical feasibility (non-invasive, portable) and temporal resolution (capable of modulating cortical excitability for a sustained period post-stimulation).
5. Experimental Protocol 2: Direct Comparison of Techniques via MRI
5.1. Objective To directly compare the effects of two distinct neuromodulation techniques (e.g., TMS and transcranial Photobiomodulation/tPBM) on brain structure and function using MRI.
5.2. Protocol Details This within-subjects pilot protocol is adapted from a study comparing TMS and tPBM [71].
- Design: A counterbalanced, within-subjects design where each participant undergoes four lab visits (Active tPBM, Sham tPBM, Active TMS, Sham TMS).
- Participants: N=8-10 healthy adults with no neurological history.
- Stimulation Parameters:
- tPBM: 1,064 nm wavelength laser, 0.6 W output, 11 min duration, applied at the vertex [71].
- TMS: High-frequency stimulation over the somatomotor cortex (e.g., C3 location), intensity set to individual motor threshold.
- MRI Acquisition: Acquire structural, task-based (e.g., finger-tapping), and resting-state functional MRI immediately before and after each stimulation session.
- Data Analysis:
- Task fMRI: Compare BOLD signal activation during the finger-tapping task post-stimulation vs. pre-stimulation for each condition.
- Connectivity: Analyze changes in functional and structural connectivity between the stimulated region (M1) and connected nodes (e.g., thalamus).
5.3. Application of the 6D Framework This protocol directly benchmarks key dimensions:
- Stimulation Depth: tPBM penetrates ~4 cm, potentially affecting deeper subcortical structures, while TMS is more limited to the cortical surface [71]. Connectivity changes can quantify this.
- Spatial Resolution/Focality: TMS with a figure-8 coil offers high focality, while tPBM has "broad focality" [71]. The spread of BOLD signal changes can be measured.
- Biosafety: Monitor and report any adverse events to compare the safety profiles of the two techniques.
6. Experimental Protocol 3: AI-Optimized Home-Based Neuromodulation
6.1. Objective To validate an AI-driven system for personalizing and optimizing transcranial random noise stimulation (tRNS) for cognitive enhancement in a home-based setting.
6.2. Protocol Details This protocol is derived from a double-blind, sham-controlled study [11].
- Design: Double-blind, sham-controlled trial with three arms: (1) AI-personalized tRNS (pBO-tRNS), (2) one-size-fits-all tRNS (1.5 mA), (3) Sham tRNS.
- Participants: Healthy adults participating remotely from home.
- Personalization Algorithm: Use a Personalized Bayesian Optimization (pBO) algorithm. The algorithm takes individual baseline sustained attention performance (
A') and head circumference as inputs to determine the optimal current intensity [11]. - Stimulation & Task: Participants receive tRNS over the dorsolateral prefrontal cortex (dlPFC) while performing a sustained attention task remotely.
- Outcomes: The primary outcome is the change in sustained attention performance (
A'), analyzed with mixed-effects models. A key analysis involves stratifying results by baseline performance.
6.3. Application of the 6D Framework This protocol exemplifies the optimization of multiple dimensions:
- Clinical Feasibility: The home-based design directly addresses scalability and real-world applicability.
- Spatial Resolution & Specificity: While tRNS itself is not cell-type specific, the AI personalization introduces a new form of functional specificity, optimally targeting individuals based on their baseline neuro-cognitive state.
- Biosafety: The system identifies and avoids current intensities that could impair performance, enhancing safety [11].
The pursuit of precise neural circuit interrogation and therapeutic intervention has yielded a diverse array of neuromodulation technologies, each characterized by a unique spatiotemporal resolution profile. Deep Brain Stimulation (DBS), Transcranial Magnetic Stimulation (TMS), and transcranial Direct Current Stimulation (tDCS) represent established clinical tools, whereas optogenetics and sonogenetics are pioneering techniques emerging from molecular neuroscience research. A core challenge in computational model development for neurostimulation optimization is the accurate mathematical representation of these spatiotemporal trade-offs. Models must integrate the macroscopic electrical field distributions of electromagnetic modalities with the microscopic, cell-type-specific targeting achievable by genetically encoded actuators. This document provides detailed application notes and experimental protocols to standardize the characterization of these parameters, thereby furnishing high-fidelity data for model training and validation, crucial for researchers and drug development professionals engaged in therapeutic targeting and neurological drug discovery.
Quantitative Spatiotemporal Profiles of Neurostimulation Techniques
The efficacy and application scope of a neurostimulation technique are largely defined by its spatial resolution (the minimum volume of tissue that can be selectively targeted) and temporal resolution (the precision with which stimuli can be delivered in time). Computational models for neurostimulation optimization require precise, quantitative inputs of these parameters to accurately predict outcomes. The following table summarizes the characteristic spatiotemporal profiles and primary action mechanisms of the major techniques.
Table 1: Spatiotemporal Characteristics and Mechanisms of Neurostimulation Techniques
| Technique | Spatial Resolution | Temporal Resolution | Mechanism of Action | Penetration Depth |
|---|---|---|---|---|
| DBS | ~1-10 mm [74] | Millisecond to Second | Direct neuronal membrane depolarization via implanted electrodes | Deep brain structures (implant-dependent) |
| TMS | ~1-2 cm | ~100 microseconds | Indirect neuronal depolarization via induced electromagnetic fields | Cortical and superficial subcortical |
| tDCS | ~1-2 cm (diffuse) | Seconds to Minutes | Sub-threshold modulation of neuronal membrane potential | Cortical |
| Optogenetics | ~Single Cell [75] | ~Milliseconds [75] | Genetically encoded ion channels/pumps activated by light [75] | Limited by light scattering (~mm with lasers) |
| Sonogenetics | ~1-3 mm | ~Milliseconds to Seconds | Genetically encoded mechanosensitive channels activated by ultrasound | Entire brain (focused ultrasound) |
A critical trade-off exists between penetration depth and spatial resolution. Electromagnetic techniques like TMS and tDCS offer non-invasive access to deep cortical structures but with diffuse resolution, potentially co-activating multiple neural populations and complicating the interpretation of circuit function. Conversely, optogenetics provides unparalleled cell-type specificity but suffers from limited penetration depth due to light scattering in neural tissue, often requiring invasive fiber optic implants. Sonogenetics represents a promising intermediate, leveraging the deep-penetrating and focusable nature of ultrasound to activate genetically defined cells, though its spatial precision is currently lower than that of optogenetics. For computational neuroscientists, these trade-offs dictate the appropriate model scale: finite-element method (FEM) models are well-suited for simulating the broad electric or acoustic fields of TMS, tDCS, and sonogenetics, whereas compartmental neuron models are essential for simulating the precise, channel-mediated effects of optogenetics and DBS at the cellular level.
Detailed Experimental Protocols for Spatiotemporal Characterization
Protocol: Characterizing Spatial Specificity of Optogenetic Stimulation
This protocol details the steps to quantify the spatial spread of optogenetic activation in vivo, a critical parameter for constraining computational models.
I. Materials and Reagents
- Optogenetic Actuator: AAV-CaMKIIa-ChR2(H134R)-eYFP (for neuronal expression)
- Light Source: Solid-state laser (473 nm) with a fiber optic cannula
- Recording Setup: Multielectrode array or whole-cell patch-clamp rig
- Animal Model: Wild-type mice (C57BL/6)
- Stereotaxic Apparatus
- Anesthesia: Isoflurane vaporizer system
II. Methodology
- Stereotaxic Injection: Anesthetize the mouse and inject the AAV vector into the target brain region (e.g., primary motor cortex, M1). Allow 3-4 weeks for robust opsin expression.
- Implant Integration: Implant a fiber optic cannula above the injection site.
- In Vivo Measurement:
- In an awake, head-fixed mouse, deliver light pulses (473 nm, 1-20 Hz, 5-10 ms pulse width) at varying power densities (1-100 mW/mm²).
- Simultaneously, record neural activity using a multielectrode array positioned at different distances from the fiber tip.
- Data Analysis: Plot the spike probability of recorded neurons against the distance from the light source and the stimulus power. The spatial resolution is defined as the distance at which spike probability drops to 50% of its maximum value. This dose-response-distance data is a direct input for tuning model parameters governing light scattering and opsin conductance.
Protocol: Mapping Electric Field Distribution of tDCS
This protocol describes the empirical validation of computational models predicting the electric field distribution generated by tDCS.
I. Materials and Reagents
- Stimulation Setup: tDCS stimulator with saline-soaked sponge electrodes (e.g., 5x5 cm)
- Phantom Head: A three-dimensional skull model filled with conductive electrolyte solution mimicking brain conductivity.
- Measurement Apparatus: An array of calibrated voltmeters or a current-density imaging system.
- Navigation System: Neuromavigation system co-registered with the phantom.
II. Methodology
- Setup Configuration: Place the tDCS electrodes on the phantom head according to a standard montage (e.g., F3-Fp2 for dorsolateral prefrontal cortex stimulation).
- Field Mapping: Apply a low current (1-2 mA) and measure the voltage difference at multiple pre-defined points within the conductive solution.
- Data Acquisition and Modeling: Calculate the electric field vector (E = -∇V) at each measurement point. Co-register the measured field distribution with a standard MRI brain model. The output is a 3D map of electric field magnitude and direction, which serves as a ground-truth dataset for validating and refining finite-element models of current flow in the head.
Signaling Pathways and Experimental Workflows
The biophysical mechanisms of these techniques engage distinct signaling pathways within neural cells. Understanding these pathways is essential for building biologically realistic computational models.
Optogenetics Signaling Pathway
Diagram 1: Channelrhodopsin Activation Pathway.
The core pathway involves light-sensitive opsins, such as Channelrhodopsin-2 (ChR2), which are genetically encoded in specific cell types [75]. Upon illumination with a specific wavelength of light, the opsin undergoes a conformational change, opening its ion-conducting pore [75]. This allows cations to flow into the cell, leading to a rapid membrane depolarization and the generation of an action potential. This direct, rapid, and reversible control is a key feature for modeling precise causal relationships in neural circuits.
Sonogenetics Signaling Pathway
Diagram 2: Mechanosensitive Channel Activation.
Sonogenetics relies on ultrasound-sensitive ion channels, such as the engineered mechanosensitive channel MscL. The application of low-intensity focused ultrasound exerts a mechanical force on the cell membrane, which is transmitted to the incorporated MscL channel [75]. This mechanical force gates the channel, leading to cation influx and subsequent neuronal depolarization. The spatial precision is determined by the ultrasound focus, and computational models must account for the physics of ultrasound wave propagation and its interaction with the channel.
Comparative Experimental Workflow
Diagram 3: Core Neurostimulation Workflow.
This generalized workflow highlights the divergent starting point based on the choice of technique. The critical distinction is between methods requiring an initial genetic targeting step (Optogenetics, Sonogenetics) and those that rely on physical targeting (DBS, TMS, tDCS). All paths converge on the definition of precise stimulus parameters, the delivery of the stimulus, and the quantitative recording of outcomes. This structured data collection is the prerequisite for feeding information into a computational model to refine predictions or reverse-engineer circuit function.
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of these neurostimulation techniques, particularly the genetically targeted ones, relies on a specific toolkit of reagents and equipment.
Table 2: Essential Research Reagents and Materials for Neurostimulation
| Item Name | Category | Function / Application | Example Specifics |
|---|---|---|---|
| AAV-hSyn-ChR2-eYFP | Viral Vector | Drives expression of the light-sensitive channel Channelrhodopsin-2 in neurons. | Serotype (e.g., AAV5, AAV9) determines tropism and spread. |
| Fiber Optic Cannula | Surgical Implant | Guides light from the laser source to the target brain region for in vivo optogenetics. | Material: Stainless steel or zirconia; Customizable implant length. |
| Multielectrode Array (MEA) | Recording Equipment | Records extracellular action potentials from multiple neurons simultaneously during stimulation. | Can be silicon-based (Neuropixels) or flexible polymer. |
| Focused Ultrasound Transducer | Stimulation Equipment | Generates and focuses ultrasound waves to a specific brain region for sonogenetics. | Center frequency (e.g., 0.5, 1, or 2 MHz) determines focus size. |
| tDCS Stimulator | Stimulation Equipment | Delivers low-intensity, constant direct current to the scalp for neuromodulation. | Features: Constant current output, ramping, impedance monitoring. |
| Sterotaxic Frame | Surgical Equipment | Provides precise 3D positioning for viral injections and implant placements in rodent models. | Digital models integrate with brain atlas software. |
| CLARITY Reagents | Tissue Processing | Renders brain tissue optically transparent for post-hoc validation of opsin expression and electrode placement. | Hydrogel-based chemical solution. |
Computational models have become indispensable in the field of neurostimulation, providing a critical bridge between theoretical concepts and clinical applications. These models serve as virtual testing platforms to study interactions between neuromodulation technologies and the computational structure of the nervous system, thereby accelerating therapy optimization and device design [27]. The synthesis of neuroscientific concepts into in-silico models simultaneously highlights our current understanding of neural systems and identifies areas requiring further experimental research [27]. As the complexity of neurostimulation technologies grows, rigorous validation frameworks that connect model predictions with experimental outcomes become increasingly vital for translating computational insights into clinically viable therapies.
Computational Modeling Approaches in Neurostimulation
Modeling Paradigms and Applications
Computational models in neurostimulation span multiple levels of biological organization, from individual nerve fibers to complex neural circuits. The development of highly efficient surrogate models represents a significant advancement, enabling rapid exploration of parameter spaces that would be prohibitively expensive to investigate using traditional approaches [4]. For example, the Surrogate Myelinated Fiber (S-MF) model accurately predicts neural responses to electrical stimulation while achieving several-orders-of-magnitude improvement in computational efficiency compared to established platforms like NEURON [4]. This computational acceleration is particularly valuable for optimizing stimulation parameters for selective activation of neural pathways in peripheral neuromodulation applications.
Table 1: Computational Modeling Approaches in Neurostimulation
| Model Type | Primary Application | Key Advantages | Validation Status |
|---|---|---|---|
| Finite Element Models [27] | Electric field prediction from implanted electrodes | Predicts spatial distribution of electric fields; Accounts for tissue anisotropy | Extensive validation in DBS and SCS contexts |
| Surrogate Myelinated Fiber (S-MF) [4] | Peripheral nerve stimulation parameter optimization | 2,000-130,000× speedup over NEURON; High predictive accuracy (R² = 0.999) | Validated in pig and human vagus nerve models |
| McIntyre-Richardson-Grill (MRG) Model [4] | Mammalian axon response prediction | Gold standard for predicting fiber responses; Non-linear biophysical properties | Extensive experimental validation across species |
| Patient-Specific Models [27] | Clinical decision support for SCS | Accounts for interpatient variability in anatomy and electrode location | Emerging validation in clinical studies |
Key Quantitative Performance Metrics
Recent advances in computational efficiency have dramatically expanded the feasibility of large-scale parameter optimization. The S-MF model demonstrates remarkable accuracy in predicting activation thresholds across diverse fiber diameters (6-14 µm), nerve morphologies, electrode geometries, and waveform shapes [4]. Performance validation shows a mean absolute percentage error (MAPE) of less than 2.5% across all tested fiber diameters, with superior performance for larger fibers (r = -0.21, p < 0.005) [4]. Threshold errors range from -11.0% to 7.3%, with more than 95% of errors falling within ±5% [4]. This level of accuracy, combined with massive computational acceleration, enables previously infeasible optimization tasks for selective neural stimulation.
Table 2: Performance Metrics of Surrogate Myelinated Fiber (S-MF) Model
| Performance Metric | Result | Testing Conditions |
|---|---|---|
| Threshold Prediction Accuracy (R²) [4] | 0.999 | Across fiber diameters, waveforms, and nerve morphologies |
| Mean Absolute Percentage Error [4] | <2.5% | All fiber diameters (6-14 µm) |
| Computational Speedup [4] | 2,000-130,000× | Compared to single-core NEURON simulations |
| Threshold Error Range [4] | -11.0% to +7.3% | 95% of errors within ±5% |
| Waveform Generalization [4] | Consistent accuracy across 6 waveforms | Trained only on monophasic rectangular pulses |
Experimental Validation Protocols
Preclinical Safety and Efficacy Evaluation
The transition from computational predictions to in vivo application requires rigorous preclinical evaluation to ensure safety and efficacy. Neural stimulators are classified as Class III medical devices by regulatory bodies, necessitating comprehensive testing before clinical trials [76]. The preclinical evaluation pipeline incorporates in vitro studies focused on device reliability, in vivo studies using animal models of disease or injury to assess safety and efficacy, and human cadaver studies to optimize surgical approaches and device form factors [76]. This multifaceted approach provides iterative feedback to refine device design before finalization, potentially reducing the duration and cost associated with commercialization.
Protocol: Validation of Computational Model Predictions In Vivo
Purpose: To quantitatively compare computational model predictions of neural activation thresholds with experimentally measured thresholds in an animal model.
Materials:
- Computational model of target neural structure
- Animal model (e.g., rat, pig)
- Implantable stimulation system with recording capability
- Surgical equipment and stereotaxic apparatus
- Neural recording and stimulation equipment
Procedure:
- Computational Prediction Phase:
- Construct finite element model of electrode placement in target tissue
- Incorporate patient-specific anatomy from medical imaging when available
- Simulate neural responses to stimulation parameters using validated fiber models
- Predict threshold currents for neural activation across parameter space
In Vivo Validation Phase:
- Surgically implant electrode in target neural structure
- Apply stimulation protocols matching computational predictions
- Record neural responses using appropriate methodologies (EMG, EEG, single-unit recording)
- Systematically vary stimulation parameters to determine experimental thresholds
- Blind experimenters to computational predictions during data collection
Data Analysis Phase:
- Compare predicted versus experimental activation thresholds
- Calculate correlation coefficients and absolute error metrics
- Assess selectivity of activation through collateral recording sites
- Perform statistical analysis to determine significance of correlations
Validation Metrics: Mean absolute percentage error (MAPE) between predicted and experimental thresholds, correlation coefficients (R²), spatial accuracy of activated neural populations, and selectivity indices for target versus non-target structures.
Integrated Workflow: From Computational Prediction to Experimental Validation
The validation of computational neurostimulation models requires a systematic approach that integrates in silico, in vitro, and in vivo methodologies. The following workflow illustrates the iterative process of model development, experimental testing, and refinement that ensures predictive accuracy and clinical relevance.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Neurostimulation Validation Studies
| Research Material | Function/Application | Key Considerations |
|---|---|---|
| MRG Fiber Model [4] | Gold standard for mammalian axon response prediction | Incorporates non-linear biophysics; Validated across species |
| NEURON Simulation Environment [4] | Industry-standard platform for neural simulations | Supports extracellular stimulation; CPU-based limitation |
| Finite Element Modeling Software [27] | Predicts electric field distributions from electrodes | Must account for tissue anisotropy and patient anatomy |
| Cuff Electrodes [4] | Peripheral nerve stimulation and recording | Various geometries (e.g., helical, multi-contact) for specific applications |
| Patient-Specific Anatomical Models [27] | Account for interpatient variability in clinical translation | Derived from medical imaging; Critical for accurate prediction |
| GPU Computing Infrastructure [4] | Enables massive parallelization of neural simulations | Essential for surrogate model training and execution |
| Preclinical Animal Models [76] | Safety and efficacy testing before human trials | Species selection based on neural target and disease model |
The integration of computational modeling with rigorous experimental validation represents a paradigm shift in neurostimulation research and development. Computational models, particularly highly efficient surrogate models, enable rapid exploration of complex parameter spaces and optimization of stimulation protocols that would be infeasible through experimental approaches alone [4]. However, the ultimate value of these models depends on their predictive accuracy when translated to biological systems, necessitating comprehensive validation frameworks that bridge the in silico to in vivo divide [27] [76]. As the field advances, the continued refinement of these integrated approaches promises to accelerate the development of more precise and effective neurostimulation therapies while reducing the costs and risks associated with traditional device development pathways.
The development of precise and effective neurostimulation therapies is fundamentally limited by a translational gap between molecular mechanisms and systems-level physiological responses. Traditional approaches, which investigate these domains in isolation, fail to capture the critical interactions that define therapeutic efficacy and side effects. A new, hybrid paradigm is emerging that integrates molecular network analysis with high-fidelity electrophysiological modeling. This integrated framework enables a systems biology approach to neurostimulation optimization, bridging scales from genes and proteins to whole-nerve activation and patient-specific physiological outcomes. By constructing multi-scale models informed by molecular data, researchers can now identify key effector genes and signaling pathways that influence neural excitability and use these insights to personalize computational models for predicting optimal stimulation parameters. This paradigm is crucial for advancing bioelectronic medicine, as it addresses core challenges such as preventing off-target effects and maximizing activation of therapeutically relevant nerve fibers, ultimately accelerating the development of next-generation neurostimulation therapies [77] [78].
Foundational Concepts and Key Rationale
The Critical Need for Hybrid Models in Neurostimulation
The biological response to neurostimulation is a complex, multi-scale phenomenon. A stimulus pulse applied to a nerve triggers a cascade of events, beginning with the opening of voltage-gated ion channels at the molecular level, leading to action potential generation in individual axons, and culminating in the orchestration of organ-level physiological functions. Disconnected analysis of these stages creates significant bottlenecks. For instance, while molecular biology can identify genes and proteins differentially expressed in a disease state, it cannot predict how these changes alter the firing thresholds of different nerve fiber types. Conversely, a purely biophysical nerve model can predict activation thresholds but may lack the biological context of how chronic stimulation or disease modifies the underlying neural tissue. Hybrid models directly address this by creating a continuous in silico pipeline where molecular discoveries can be quantitatively assessed for their functional impact on neural circuitry and therapeutic outcomes [78].
This approach is particularly vital for overcoming the failures of one-size-fits-all neurostimulation protocols. The NECTAR-HF clinical trial for heart failure, for example, highlighted how titration of vagus nerve stimulation (VNS) based on patient tolerance (targeting large-diameter Aα fibers) failed to deliver sufficient current to activate the smaller-diameter B fibers responsible for the therapeutic effect [78]. A hybrid modeling framework, incorporating patient-specific nerve anatomy and the molecular properties of different fiber types, could have preemptively identified this critical dosing gap, demonstrating its power to inform clinical trial design and personalize therapy delivery.
Core Components of the Hybrid Framework
The proposed hybrid framework is built upon two synergistic pillars:
Molecular Network Analysis: This component involves the systems-level interrogation of omics data (e.g., transcriptomics, proteomics) to decode the molecular landscape of the neural tissue targeted for stimulation. Techniques such as differential expression analysis, pathway enrichment, and gene prioritization are used to identify key molecular players. For instance, in a study on cardiac aging and exercise, researchers integrated transcriptomic data from the GTEx project with endurance-exercise-responsive genes from the MoTrPAC dataset. They identified 37 overlapping "effector genes," such as SMPX, which was prioritized for its role in mechano-metabolic coupling and cardiac stress adaptation [77]. In a hybrid model, these molecular insights could be used to parameterize the ion channel densities and metabolic states of computational nerve fiber models, making them more biologically grounded.
Electrophysiological Modeling: This component involves creating biophysically realistic computational models of nerves and their responses to electrical stimulation. The established methodology is a two-step "hybrid modeling" process [78]. First, a field model (often using the finite-element method) calculates the distribution of electrical potentials within the tissue, based on the nerve morphology, electrode geometry, and stimulus waveform. Second, a fiber model uses this extracellular potential to simulate the activation and propagation of action potentials in individual axons using non-linear ionic conductances, such as the well-established McIntyre-Richardson-Grill (MRG) model for myelinated fibers [4]. Recent advances have introduced highly efficient, machine learning-based surrogate models like the S-MF ("smurf"), which can reproduce the spatiotemporal dynamics of the MRG model with several-orders-of-magnitude improvement in computational speed, thereby enabling large-scale parameter exploration and optimization that was previously infeasible [4].
Table 1: Core Analytical Components of the Hybrid Framework
| Component | Primary Function | Key Techniques & Tools | Output |
|---|---|---|---|
| Molecular Network Analysis [77] | Identifies key genes, proteins, and pathways that influence neural function and plasticity. | Transcriptomic integration (e.g., GTEx, MoTrPAC), Pathway enrichment (e.g., Enrichr), Gene prioritization (e.g., FLAMES algorithm). | Prioritized list of effector genes (e.g., SMPX, RYR2); Enriched pathways (e.g., mitochondrial function). |
| Electrophysiological Modeling [4] [78] | Predicts neural activation and block in response to electrical stimuli. | Finite Element Method (FEM) field models, Biophysical fiber models (e.g., MRG model), Surrogate models (e.g., S-MF, AxonML). | Activation thresholds for different fiber types; Prediction of neural recruitment and side effects. |
Application Notes and Detailed Protocols
This section provides a detailed, actionable protocol for implementing the hybrid analysis framework, from data acquisition to model validation.
Protocol 1: Molecular Network Analysis for Target Prioritization
Objective: To identify and prioritize molecular targets (genes, proteins) that modulate neural excitability and can be integrated into electrophysiological models.
Step 1: Data Acquisition and Preprocessing
- Source: Obtain transcriptomic or proteomic datasets relevant to your research context. For human neural pathways, the Genotype-Tissue Expression (GTEx) project provides a foundational resource for baseline gene expression across tissues [77]. For intervention-specific responses (e.g., exercise, disease progression), leverage consortium data like the Molecular Transducers of Physical Activity Consortium (MoTrPAC) or disease-specific omics repositories [77].
- Preprocessing: Perform standard bioinformatic preprocessing, including normalization, batch effect correction, and quality control. For differential expression analysis, use established pipelines (e.g., DESeq2, limma) with stringent statistical thresholds (e.g., adjusted p-value < 0.05, logâ‚‚ fold change > 1 or < -1) [77].
Step 2: Intersectional Analysis and Network Construction
- Intersection: Conduct a Venn-based intersection analysis to identify genes that are differentially expressed in both a relevant disease state and in response to a modulating intervention (e.g., "age-downregulated genes" ∩ "exercise-responsive genes") [77]. This identifies candidate "effector genes" that may bridge pathological decline and therapeutic recovery.
- Pathway Enrichment: Subject the overlapping gene set to pathway enrichment analysis using tools like Enrichr. This maps the gene list to known biological pathways (e.g., KEGG, Reactome), revealing whether the effector genes are collectively involved in processes like mitochondrial dysfunction, sarcomere organization, or lipid metabolism [77].
Step 3: Upstream Regulator and Effector Gene Prioritization
- Upstream Analysis: Use tools like KEA3 (kinase enrichment analysis) and ChEA3 (transcription factor enrichment analysis) to predict upstream regulators (e.g., kinases like PDK family, transcription factors like NKX2-5) of your effector gene set [77].
- Prioritization: Rank the candidate effector genes using a multi-dimensional scoring system. The FLAMES linear scoring algorithm is one method that integrates functional similarity (via ToppGene) and network centrality (via ToppNet) to produce a composite score, highlighting genes like SMPX that are both functionally relevant and central to the molecular network [77].
Step 4: Mapping to Electrophysiological Parameters
- Interpretation: Map the top-ranked effector genes and enriched pathways to parameters in a nerve fiber model. For example:
- A gene involved in potassium channel function could inform the maximal conductance (
gK) in the model. - A pathway related to mitochondrial energy metabolism could inform the ATP-dependent Na+/K+ pump rate, affecting recovery cycles and long-term stability.
- A gene involved in potassium channel function could inform the maximal conductance (
- Interpretation: Map the top-ranked effector genes and enriched pathways to parameters in a nerve fiber model. For example:
Protocol 2: Building and Validating a Hybrid Electrophysiological Model
Objective: To construct a personalizable computational model of a peripheral nerve that incorporates molecular insights and predicts responses to electrical stimulation.
Step 1: Anatomical Model and Field Simulation
- Nerve Reconstruction: Construct a 3D geometric model of the target nerve. This can be derived from:
- Histology: Use automated segmentation tools (e.g., a UNet-based deep neural network) on histological cross-sections to delineate fascicular boundaries and create a realistic nerve topography [79].
- Medical Imaging: Utilize MRI or ultrasound data to inform nerve size and position relative to other tissues.
- Finite Element Model (FEM): Import the geometry into an FEM software (e.g., COMSOL, Sim4Life). Assign electrical conductivity values to different tissues (epineurium, perineurium, endoneurium, surrounding tissue). Define the electrode(s) and their configuration [78].
- Simulation: Solve for the distribution of the electric potential within the model for a given stimulus waveform and amplitude.
- Nerve Reconstruction: Construct a 3D geometric model of the target nerve. This can be derived from:
Step 2: Fiber Population Modeling with Molecular Insights
- Fiber Model Selection: Choose an appropriate biophysical model for the axons. The MRG model is the gold standard for mammalian myelinated fibers [4]. For high-throughput applications, use a GPU-accelerated surrogate model like S-MF [4].
- Population Definition: Define a population of model fibers with realistic distributions of diameter, myelination, and type (Aα, Aβ, B, C). Incorporate the molecular insights from Protocol 1 by adjusting specific parameters (e.g., ion channel densities) in subpopulations of fibers based on the expression levels of your prioritized effector genes.
- Simulation: For each fiber in the population, calculate its response to the extracellular potential field generated in Step 1. Determine the activation threshold (minimum current to elicit an action potential) and whether the stimulus produces conduction block.
Step 3: Model Validation and Optimization
- Validation: Compare model predictions against empirical data. This can include strength-duration curves, recruitment curves of different fiber types, or compound action potential measurements from animal or human studies [78]. The S-MF model, for example, demonstrated high accuracy with a mean absolute percentage error (MAPE) of <2.5% for predicting activation thresholds across various fiber diameters and waveforms [4].
- Optimization: Use the validated model for in silico therapy design. Employ gradient-free or gradient-based optimization algorithms to find the set of stimulation parameters (e.g., waveform shape, amplitude, pulse width, active electrode contact) that maximizes activation of target fascicles/fibers while minimizing off-target recruitment [4]. This process, which is computationally prohibitive with traditional models, becomes feasible with surrogate models like S-MF.
The following workflow diagram illustrates the integration of these two protocols into a cohesive hybrid analysis pipeline.
Table 2: Key Research Reagents and Computational Tools for Hybrid Modeling
| Category | Item / Resource | Function / Application | Example / Source |
|---|---|---|---|
| Data & Biologicals | Human/Murine Transcriptomic Datasets | Provides baseline and intervention-specific gene expression data for molecular network analysis. | GTEx Portal, MoTrPAC Database, dbGaP [77] |
| Peripheral Nerve Histology Sections | Provides ground-truth anatomical data for constructing realistic 3D nerve models. | Human cadaveric samples; UNet-based automated segmentation [79] | |
| Software & Platforms | Bioinformatics Suites | Performs differential expression, pathway enrichment, and gene prioritization. | Enrichr, KEA3, ChEA3, ToppGene Suite [77] |
| Finite Element Modeling Software | Solves for the electric field distribution generated by an electrode in tissue. | COMSOL Multiphysics, Sim4Life, ANSYS | |
| Neural Simulation Environments | Simulates action potential generation and propagation in response to extracellular stimulation. | NEURON, AxonML framework, S-MF Surrogate Model [4] | |
| Optimization Toolboxes | Identifies optimal stimulation parameters to achieve selective neural activation. | Gradient-based (e.g., in PyTorch/TensorFlow) and gradient-free (e.g., Bayesian) methods [4] | |
| Computational Models | MRG Fiber Model | Gold-standard, biophysical model of a mammalian myelinated axon. | Reference implementation in NEURON [4] |
| S-MF Surrogate Model | GPU-accelerated, high-throughput surrogate of the MRG model; enables large-scale optimization. | Implemented in the AxonML framework [4] |
Data Presentation and Visualization
The hybrid framework generates multi-faceted data that must be synthesized to guide research decisions. The tables below summarize key quantitative outputs from the molecular and electrophysiological arms of the analysis.
Table 3: Example Output from Molecular Network Analysis: Top Prioritized Effector Genes [77]
| Rank | Gene Symbol | Functional Relevance | Associated Pathway | Composite Score |
|---|---|---|---|---|
| 1 | SMPX | Mechano-metabolic coupling, redox balance, cardiac stress adaptation. | Sarcomere organization, Striated muscle contraction | 0.95 |
| 2 | KLHL31 | Sarcomeric organization and stability. | Muscle system process, Z-disc | 0.89 |
| 3 | MYPN | Sarcomere assembly and maintenance. | Actin-binding, Structural constituent of muscle | 0.87 |
| 4 | RYR2 | Calcium release from sarcoplasmic reticulum; excitation-contraction coupling. | Calcium signaling pathway, Cardiac muscle contraction | 0.85 |
Table 4: Performance Metrics of the S-MF Surrogate Electrophysiological Model [4]
| Metric | Value | Context / Implication |
|---|---|---|
| Activation Threshold Accuracy (R²) | 0.999 | Near-perfect correlation with the gold-standard NEURON MRG model. |
| Mean Absolute Percentage Error (MAPE) | < 2.5% | High accuracy across fiber diameters (6–14 µm). |
| Computational Speedup | 2,000 to 130,000x | Compared to single-core NEURON simulations; enables large-scale optimization. |
| Waveform Generalization | Accurate for 6 tested waveforms | Trained on monophasic rectangular pulses but generalizes to other shapes (e.g., biphasic). |
The following diagram visualizes the structural hierarchy of the hybrid modeling approach, showing how different components integrate across biological scales.
Conclusion
Computational modeling has emerged as an indispensable tool for advancing neurostimulation, providing a mechanistic bridge from cellular processes to therapeutic outcomes. By enabling patient-specific therapy design, in silico testing and optimization of stimulation protocols, and powering the development of intelligent closed-loop systems, these models are fundamentally reshaping the neurostimulation landscape. Future directions point toward a deeper integration with AI and systems biology, fostering fully integrated, adaptive therapies that can dynamically respond to a patient's unique neurophysiological state. This synergy between computational prediction and clinical application promises not only to enhance efficacy but also to democratize access to precision neuromodulation, ultimately improving care for a broad range of neurological and psychiatric disorders.
References
- 1. Bridging Neuronal Dynamics and Disease Progression [https://arxiv.org/html/2509.05151v1]
- 2. Bridging Single Neuron Dynamics to Global Brain States [https://pmc.ncbi.nlm.nih.gov/articles/PMC6908479/]
- 3. A dynamical computational model of theta generation in ... [https://elifesciences.org/articles/87356]
- 4. Highly efficient modeling and optimization of neural fiber ... [https://www.nature.com/articles/s41467-024-51709-8]
- 5. Computational modeling of neurostimulation in brain ... [https://pubmed.ncbi.nlm.nih.gov/26541382/]
- 6. Mechanisms of DBS: from informational lesions to circuit ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1492744/full]
- 7. Deep Brain Stimulation: Psychological and Neuroethical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566894/]
- 8. Differential synaptic depression mediates the therapeutic ... [https://www.nature.com/articles/s41593-025-02088-w]
- 9. Electrophysiological approaches to informing therapeutic ... [https://www.nature.com/articles/s41531-024-00847-3]
- 10. Advanced Computational Life Science Applications at CNS ... [https://zmt.swiss/news-and-events/news/sim4life/2025/advanced-computational-life-science-applications-at-cns2025/]
- 11. Personalized home based neurostimulation via AI ... [https://www.nature.com/articles/s41746-025-01744-6]
- 12. Insights into Parkinson's disease from computational models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6124639/]
- 13. Computational Models Describing Possible Mechanisms for ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1004609]
- 14. A computational outlook on neurostimulation [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-020-00047-3]
- 15. Mechanistic models of α-synuclein homeostasis for ... [https://www.frontiersin.org/journals/applied-mathematics-and-statistics/articles/10.3389/fams.2022.1060489/full]
- 16. Computational Modeling of Epilepsy - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3201757/]
- 17. Epileptic seizure suppression: A computational approach for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0298762]
- 18. Computational models of epilepsy [https://www.sciencedirect.com/science/article/pii/S1059131112002245]
- 19. Machine learning-driven identification of critical gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11745026/]
- 20. An Integrated GWAS-eQTL-PheWAS Pipeline [https://www.mdpi.com/1420-3049/30/19/3921]
- 21. MetaCGRP is a high-precision meta-model for large-scale ... [https://www.nature.com/articles/s41598-024-75487-x]
- 22. What Can Computational Models Contribute to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6338060/]
- 23. Revisiting the role of computational neuroimaging in ... [https://www.nature.com/articles/s41386-024-01946-8]
- 24. An optimization framework for targeted spinal cord stimulation [https://pubmed.ncbi.nlm.nih.gov/37647885/]
- 25. Multiscale brain modeling: bridging microscopic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11879965/]
- 26. Multiscale modeling of brain dynamics: development ... [https://www.frontiersin.org/research-topics/68003/multiscale-modeling-of-brain-dynamics-development-validation-and-applications-in-artificial-systems-or-clinical-populationsundefined]
- 27. A computational outlook on neurostimulation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7247210/]
- 28. Computational modeling of neurostimulation in brain ... [https://www.sciencedirect.com/science/article/abs/pii/S007961231500103X]
- 29. Human head models and populational framework for ... [https://www.nature.com/articles/s41597-025-04886-0]
- 30. Computational approaches to neuronal network analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2894951/]
- 31. The NeuroML ecosystem for standardized multi-scale ... [https://elifesciences.org/articles/95135]
- 32. Identification of individual subjects on the basis of their ... [https://www.nature.com/articles/s41598-018-23696-6]
- 33. A computational model of shared fine-scale structure in the ... [https://pubmed.ncbi.nlm.nih.gov/29664910/]
- 34. Patient-specific modeling for guided rehabilitation of stroke ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10719856/]
- 35. A patient-specific, 3D printed neurostimulator enabling focal ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-025-01769-8]
- 36. Evaluation of the Effectiveness of Patient-Specific 3D ... [https://www.ics.org/2025/abstract/240]
- 37. Computational analysis of electrode structure and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11208352/]
- 38. Lehigh University team develops computational model to ... [https://www.eurekalert.org/news-releases/1103685]
- 39. Methods to Develop an in silico Clinical Trial [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.741170/full]
- 40. Recent advances in potential mechanisms of epidural ... [https://www.sciencedirect.com/science/article/pii/S0014488625001943]
- 41. Personalized home based neurostimulation via AI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307579/]
- 42. BBI2025, International Neuroscience Conference 2025 ... [https://brainbox-initiative.com/conference/2025]
- 43. A circuit level investigation into the neuromodulatory effect ... [https://pubmed.ncbi.nlm.nih.gov/41265396/]
- 44. A systematic review of computational models for the design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10259770/]
- 45. Automated peripheral nerve segmentation for MR-neurography [https://pmc.ncbi.nlm.nih.gov/articles/PMC11347527/]
- 46. A survey on recent trends in deep learning for nucleus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9987406/]
- 47. A Comparative Analysis of SegFormer, FabE-Net and VGG ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468733/]
- 48. Utilization of a Deep Learning Algorithm for Automated ... [https://www.mdpi.com/2306-5354/12/12/1289]
- 49. mahmoodlab/CLAM: Open source tools for computational ... [https://github.com/mahmoodlab/CLAM]
- 50. Efficacy of neurostimulation across mental disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC8973679/]
- 51. ID: 215134 Interpatient Variability in Neural Recruitment ... [https://www.sciencedirect.com/science/article/pii/S109471592300315X]
- 52. Electrical stimulation methods and protocols for the treatment ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-023-01159-y]
- 53. An optimization framework for targeted spinal cord stimulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC10535048/]
- 54. Randomized Clinical Trials on Neurostimulation for ... [https://www.sciencedirect.com/science/article/abs/pii/S1094715925010323]
- 55. AI-Driven Multimodal Brain-State Decoding for Personalized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467613/]
- 56. Closed-Loop Neuromodulation in Physiological and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6824403/]
- 57. Ethical gaps in closed-loop neurotechnology: a scoping ... [https://www.nature.com/articles/s41746-025-01908-4]
- 58. Closed-Loop Spinal Cord Stimulation in Chronic Pain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12108722/]
- 59. Quantitative Electroencephalographic Biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577763/]
- 60. Identifying biomarkers for tDCS treatment response in ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2023.1234168/full]
- 61. Abstracts from the Sixth Bioelectronic Medicine Summit [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538809/]
- 62. Sim4Life User Workshop @ International Brain Stimulation ... [https://zmt.swiss/news-and-events/events/workshops/sim4life-brainstim-2025/]
- 63. Closing the loop between brain and electrical stimulation [https://www.nature.com/articles/s41398-023-02565-5]
- 64. AI Brain Stimulation Boosts Attention at Home [https://neurosciencenews.com/ai-brain-stimulation-attention-29538/]
- 65. Modeling Vagus Nerve Stimulation » zurich med tech [https://zmt.swiss/applications/modeling-vagus-nerve-stimulation/]
- 66. Comparing Current Steering Technologies for Directional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7318189/]
- 67. Quantitative analyses of how optimally heterogeneous ... [https://www.nature.com/articles/s41598-024-81029-2]
- 68. Quantitative analysis of noninvasive deep temporal ... [https://www.sciencedirect.com/science/article/pii/S2405844024055130]
- 69. Quantitative dynamics of neural uncertainty in sensory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12130215/]
- 70. Emerging techniques for precision neuromodulation [https://www.the-innovation.org/article/doi/10.59717/j.xinn-life.2025.100150]
- 71. Pilot study comparing effects of infrared neuromodulation ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1514087/full]
- 72. SPIRIT 2025 Statement: Defining standard protocol items ... [https://www.equator-network.org/reporting-guidelines/spirit-2013-statement-defining-standard-protocol-items-for-clinical-trials/]
- 73. Comparative efficacy and acceptability of non-invasive ... [https://www.sciencedirect.com/science/article/pii/S2589537024006138]
- 74. Spatiotemporal assessment and trade-offs of multiple ... [https://pubmed.ncbi.nlm.nih.gov/28810509/]
- 75. Optogenetic Approaches for the Spatiotemporal Control of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8157557/]
- 76. The development of neural stimulators: a review of preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6049833/]
- 77. Molecular Network Analysis and Effector Gene ... [https://www.mdpi.com/2073-4425/16/7/814]
- 78. Computational modeling of autonomic nerve stimulation [https://www.sciencedirect.com/science/article/abs/pii/S2468451124000370]
- 79. Building hybrid models of neuromodulation from automatic ... [https://pubmed.ncbi.nlm.nih.gov/40972229/]