Chronic Stability Assessment of Implantable Electrodes: Strategies for Long-Term Reliability in Neural Interfaces
This article provides a comprehensive analysis of the critical factors influencing the long-term stability and performance of implantable electrodes for neural interfaces.
Chronic Stability Assessment of Implantable Electrodes: Strategies for Long-Term Reliability in Neural Interfaces
Abstract
This article provides a comprehensive analysis of the critical factors influencing the long-term stability and performance of implantable electrodes for neural interfaces. Targeting researchers, scientists, and drug development professionals, it explores the biological, material, and mechanical challenges that compromise chronic electrode functionality. The scope spans from foundational mechanisms of foreign body response and glial scarring to advanced methodological approaches for stability assessment, troubleshooting strategies for performance optimization, and comparative validation of emerging technologies. By synthesizing current research and clinical evidence, this review offers a structured framework for developing next-generation bioelectronic implants with enhanced chronic stability for therapeutic and diagnostic applications.
The Biological Battlefield: Understanding Fundamental Stability Challenges in Neural Electrodes
The development of advanced implantable medical devices, particularly neural electrodes, represents a frontier in treating neurological diseases and restoring lost functions. However, a significant biological barrier limits their widespread clinical adoption: the foreign body response (FBR). This inevitable host reaction to implanted materials initiates a cascade of inflammatory and fibrotic processes that severely impair device functionality over time [1] [2]. For implantable electrodes, which require stable, intimate contact with target tissues, the FBR presents a critical challenge to long-term performance [2] [3].
The FBR begins with tissue injury during implantation, triggering acute inflammation characterized by immune cell recruitment [1]. Without successful degradation of the implant, this response transitions to a chronic fibrotic phase marked by dense extracellular matrix deposition and fibrous capsule formation [1] [2]. This capsule functionally isolates the implant from surrounding tissue, disrupting the precise interface necessary for effective signal recording or stimulation [2]. Understanding these mechanisms is paramount for developing next-generation bioelectronic medicines with improved chronic stability.
Molecular and Cellular Mechanisms of FBR
The Cellular Cascade of Foreign Body Reaction
The FBR follows a well-defined temporal sequence of cellular events that begins immediately upon implantation:
Protein Adsorption: Within seconds of implantation, blood-derived proteins (albumin, fibrinogen) non-specifically adsorb to the implant surface, creating a provisional matrix through which cells interact with the foreign material [2] [4]. This protein layer undergoes dynamic changes through the Vroman effect, where smaller proteins are progressively replaced by larger ones [2].
Neutrophil Infiltration: Within minutes, neutrophils migrate to the implantation site as first responders [2]. They adhere to the protein layer and release factors including reactive oxygen species (ROS) and proteolytic enzymes that promote inflammatory progression [2] [5]. This initial wave of neutrophils typically disappears within two days [2].
Monocyte Recruitment and Macrophage Differentiation: Chemical signals from neutrophils, blood clotting, and mast cells attract monocytes to the site [2]. Upon arrival, monocytes differentiate into macrophages that proliferate and populate the lesion [2]. These macrophages mediate the core inflammatory response by releasing pro-inflammatory cytokines including TNFα, IL-1b, IL-6, and IL-8 [2].
Frustrated Phagocytosis: Macrophages adhere to the implant surface through integrins (particularly αMβ2) and attempt to engulf the device [2]. When unable to phagocytose large implants, they enter a state of "frustrated phagocytosis," secreting degrading enzymes and ROS that can damage otherwise stable biomaterials [2] [5].
Fibrotic Encapsulation: If the implant persists, the response transitions to a chronic fibrotic stage characterized by a shift from pro-inflammatory M1 macrophages to anti-inflammatory M2 macrophages [2]. Fibroblasts activate and differentiate into myofibroblasts, secreting collagen that forms a dense, avascular fibrous capsule around the implant [4].
Key Signaling Pathways in Pathological FBR
Recent research has identified RAC2 signaling as a central mediator of pathological FBR. Analysis of human fibrotic capsules from various implant types revealed that severe FBR is characterized by upregulation of this hematopoietic-specific Rho-GTPase, which functions as a mechanical signal transducer [6]. RAC2 guides the expression of genes involved in both cell-activating and inflammatory pathways, driving the pathological FBR independently of implant material properties [6].
The diagram below illustrates the key cellular and molecular events in the foreign body response:
Figure 1: Cellular and Molecular Cascade in Foreign Body Response. The FBR progresses through acute and chronic phases, with RAC2 mechanotransduction signaling identified as a key driver of pathological outcomes.
Impact of FBR on Neural Electrode Performance
Functional Consequences of FBR on Recording Stability
The foreign body response directly impairs neural electrode function through multiple mechanisms that degrade recording quality over time:
Increased Electrode-Tissue Distance: Glial scar formation creates a physical barrier between recording electrodes and target neurons, increasing the effective distance for signal transmission [3]. Since electrodes typically record from neurons within 100 μm, even minimal encapsulation can significantly attenuate signals [3].
Elevated Interface Impedance: The fibrous capsule, composed largely of insulating proteins and cells, increases interfacial impedance at the electrode-tissue boundary [7] [3]. This impedance rise directly reduces the signal-to-noise ratio (SNR) of recorded neuronal activities [3].
Neuronal Loss: Chronic inflammation surrounding implants creates a neurotoxic environment through pro-inflammatory cytokines and free radicals, leading to neuronal death in the immediate vicinity of the probe [3]. This depletes the very signal sources the electrodes are designed to detect.
Microglial Adhesion: Emerging evidence suggests that microglia adhering directly to electrode surfaces, rather than the multicellular scar itself, may be the primary cause of performance deterioration [8]. These surface-adherent microglia can degrade recording quality without full scar formation.
Quantitative Assessment of FBR Impact on Electrode Performance
Table 1: Comparative Performance Metrics of Neural Electrodes Affected by Foreign Body Response
| Electrode Type | Recording Duration | Signal Attenuation | Impedance Change | Key FBR Manifestations |
|---|---|---|---|---|
| Silicon-based Michigan Probes [3] | Months | Progressive decline in single-unit yield | Significant increase over time (~30-50%) | Gliosis, neuronal death, chronic BBB disruption |
| Flexible Polyimide Electrodes [7] | Up to 8 months | More stable than rigid probes | Lower initial rise but still significant | Reduced glial scarring compared to rigid probes |
| NeuroRoots Filament Electrodes [7] | 7 weeks | Maintained signal quality | Minimal change when functional | Distributed design minimizes FBR |
| Utah Arrays [3] | Years in humans | Gradual decline in channel functionality | Progressive increase | Dense fibrous encapsulation, vascular disruption |
| Carbon Fiber Microelectrodes [7] | Several months | Improved chronic stability | Stable low impedance | Reduced mechanical mismatch |
Comparative Analysis of Electrode Design Strategies
Material and Geometrical Optimization for FBR Mitigation
Innovative electrode designs employ various strategies to minimize the foreign body response through material selection and geometrical optimization:
Flexible Materials: Flexible electrodes with low Young's modulus (typically <1 MPa) better match brain tissue mechanics (1-10 kPa), reducing chronic inflammation and mechanical mismatch [7] [9] [3]. The bending stiffness of these devices is typically below 10â»â¹ Nm, compared to >10â»â¶ Nm for rigid devices [9].
Miniaturization: Reducing electrode cross-sectional area to subcellular dimensions minimizes acute injury during implantation and promotes better integration [7]. Nanowire electrodes with cross-sectional areas as small as 10 μm² have demonstrated reduced FBR [7].
Surface Topography: Engineering surface features at micro/nano scales can modulate protein adsorption and immune cell responses [4]. Specific topographies reduce macrophage attachment and foreign body giant cell formation compared to smooth surfaces [4].
Implantation Techniques: The coordination of electrode shape with implantation method significantly affects initial tissue damage [7]. Unified implantation uses a single guidance system for multiple electrodes, while distributed implantation deploys electrodes individually to minimize cross-sectional area [7].
Comparative Performance of Different Electrode Designs
Table 2: Foreign Body Response to Different Neural Electrode Designs and Materials
| Design Strategy | Mechanism of Action | Effect on FBR | Limitations | Recording Stability |
|---|---|---|---|---|
| Flexible Polymer Electrodes (Polyimide, SU-8) [7] [3] | Reduced mechanical mismatch with neural tissue | Significantly reduced glial scarring compared to rigid probes | Require temporary stiffeners for implantation | Months to >1 year with moderate signal decay |
| Ultra-Small Footprint Electrodes (NeuroRoots, nanowires) [7] | Minimal tissue displacement and damage during implantation | Greatly reduced acute and chronic inflammation | Manufacturing complexity, handling challenges | Several weeks to months with stable signals |
| Surface-Modified Electrodes (Biomimetic coatings) [7] [4] | Modulates protein adsorption and immune cell response | Reduced macrophage activation and fibrosis | Long-term coating stability concerns | Improved short-term performance, variable long-term |
| Drug-Eluting Electrodes (Anti-inflammatory releases) [7] | Localized immunosuppression around implant site | Attenuated inflammatory response and glial scar | Finite drug reservoir, potential tissue toxicity | Initial stability may decline after drug depletion |
Experimental Approaches for FBR Investigation
Standardized Methodologies for FBR Assessment
Rigorous assessment of FBR and its impact on electrode performance requires standardized experimental approaches:
Histological Analysis: Post-explantation evaluation of tissue samples using specific markers for glial cells (GFAP for astrocytes, Iba1 for microglia), neurons (NeuN), and inflammatory cells (CD68 for macrophages) [3]. Fibrosis is quantified through collagen staining (Masson's Trichrome, Picrosirius Red) [5] [6].
Electrophysiological Recording: Chronic tracking of signal quality metrics including signal-to-noise ratio, single-unit yield, local field potential power, and electrode impedance [8] [3]. Correlation of these parameters with histological findings establishes structure-function relationships.
Immunohistochemical Workflow:
- Perfusion fixation and brain extraction
- Sectioning and antibody labeling for target proteins
- Confocal microscopy and image analysis
- Quantification of cell densities and distances from implant track
- Statistical correlation with recording performance [3]
In Vivo Functional Testing: For neural interfaces, assessment of decoding performance in brain-machine interface applications provides functional readouts of FBR impact [7]. Deterioration in control accuracy correlates with the extent of FBR.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Foreign Body Response
| Reagent/Category | Specific Examples | Research Application | Function in FBR Investigation |
|---|---|---|---|
| Immune Cell Markers | Iba1 (microglia), CD68 (macrophages), GFAP (astrocytes) | Immunohistochemistry, flow cytometry | Identification and quantification of specific immune cell populations |
| Cytokine Inhibitors | CSF1R inhibitors, RAC2 inhibitors [8] [6] | Pharmacological modulation of FBR | Testing causal relationships between specific pathways and FBR severity |
| Extracellular Matrix Stains | Picrosirius Red, Masson's Trichrome | Histological assessment | Collagen visualization and fibrotic capsule quantification |
| Mechanical Testing Systems | Custom vibrating implants [6] | Application of controlled mechanical forces | Investigation of mechanotransduction in FBR pathogenesis |
| Transgenic Animal Models | RAC2 knockout mice [6] | Genetic manipulation of FBR pathways | Establishing molecular mechanisms of FBR in controlled systems |
| Dehydroeffusol | Effusol | High-Purity Research Compound | Effusol for research applications. This compound is For Research Use Only (RUO). Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
| Spirostan-3-ol | Spirostan-3-ol | High-Purity Steroid Reference Standard | High-purity Spirostan-3-ol for steroid biosynthesis & pharmacology research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
Emerging Strategies and Future Directions
Advanced Approaches for FBR Mitigation
Several innovative strategies show promise for overcoming FBR challenges in next-generation neural interfaces:
Active Anti-inflammatory Approaches: Controlled release systems delivering anti-inflammatory agents (e.g., dexamethasone) directly from the electrode surface [7]. These systems can be engineered for temporal profiles matching the FBR progression.
Biomimetic Surface Modifications: Coating electrodes with bioactive peptides or extracellular matrix components that mimic natural tissue environments [5] [4]. These coatings reduce protein fouling and discourage immune recognition.
Mechanotransduction Modulation: Targeting specific mechanosensitive pathways, particularly RAC2 signaling in myeloid cells, which has been identified as a key mediator of pathological FBR [6]. Pharmacological inhibition of RAC2 shows promise in reducing FBR severity.
Adaptive Electrode Systems: Self-adjusting electrodes that can modify their position or properties in response to tissue changes, maintaining optimal interface despite encapsulation [3].
The relationship between implant properties and FBR severity, along with corresponding mitigation strategies, can be visualized as follows:
Figure 2: Relationship Between Implant Properties and FBR Severity with Corresponding Mitigation Strategies. Key design parameters influence FBR severity, while emerging strategies target these parameters to improve biocompatibility.
The foreign body response remains the fundamental challenge to achieving stable long-term performance in implantable neural electrodes. While traditional approaches focused primarily on material biocompatibility, contemporary research reveals the critical importance of mechanical matching, geometrical optimization, and active immunomodulation. The recognition that RAC2-mediated mechanotransduction drives pathological FBR independently of material chemistry represents a paradigm shift in the field [6].
Future progress will likely involve combinatorial approaches that integrate flexible material platforms with surface modifications, controlled drug delivery, and sophisticated implantation techniques. The ultimate goal is developing truly "bio-integrative" electrodes that become functionally incorporated into neural tissue without provoking destructive immune responses. Achieving this milestone will require continued multidisciplinary collaboration between materials science, immunology, and clinical neurology to translate laboratory innovations into reliable clinical solutions for patients with neurological disorders.
The development of implantable neural electrodes represents a frontier in treating neurological disorders and advancing brain-computer interfaces (BCIs). A central challenge undermining their long-term effectiveness is the profound mechanical mismatch between conventional electrode materials and the neural tissues they interface with. Brain tissue is exceptionally soft, fragile, and dynamic, with a Young's modulus typically ranging from 1 to 10 kPa [10] [11]. In contrast, traditional electrode materials, such as silicon (≈102 GPa) and platinum (≈102 MPa), are several orders of magnitude stiffer [11]. This mechanical disparity creates a significant foreign body reaction, leading to inflammation, scar tissue formation, and eventual electrode failure [7] [12].
This review objectively compares the performance of different neural electrode technologies, focusing on how their mechanical properties influence chronic stability. We summarize experimental data quantifying this mismatch, detail methodologies for assessing interface stability, and provide a toolkit of key reagents and materials. Framed within the broader thesis of chronic stability assessment, this guide serves researchers and scientists in selecting and developing neural interfaces that bridge the stiffness gap for long-term functional integration.
Comparative Analysis of Electrode Properties and Performance
The shift from rigid to soft and flexible bioelectronics is a defining trend in the field, aimed at mitigating mechanical mismatch [9]. The table below provides a quantitative comparison of the core properties of these two electrode classes.
Table 1: Comparative Analysis of Rigid vs. Soft/Flexible Neural Electrodes
| Property | Rigid Bioelectronics | Soft and Flexible Bioelectronics |
|---|---|---|
| Typical Material Types | Silicon, metals, ceramics [9] | Polymers, elastomers, hydrogels, thin-film materials, meshes [9] |
| Young’s Modulus | > 1 GPa [9] | 1 kPa – 1 MPa (typically) [9] |
| Bending Stiffness | > 10–6 Nm [9] | < 10–9 Nm [9] |
| Tissue Integration | Stiffness mismatch causes inflammation and fibrotic encapsulation [9] | Soft, conformal materials match tissue mechanics and reduce immune response [9] |
| Chronic Signal Fidelity | Long-term degradation due to micromotion and scar tissue [9] | Better chronic signal due to more stable tissue contact [9] |
| Implantation Challenge | Mechanically stable but causes significant acute tissue damage [7] | Requires rigid shuttles or stiffness enhancement for implantation [7] |
The performance consequences of these material choices are clear. Flexible electrodes, with their lower bending stiffness, are designed to mimic the softness of brain tissue, which reduces the risk of chronic inflammation and mechanical mismatch [7]. However, their inherent flexibility complicates implantation, often necessitating rigid shuttles or temporary stiffeners [7]. In vivo, the foreign body response to stiff implants involves activated microglia and proliferating astrocytes, which secrete cytokines and extracellular matrix components that ultimately form a compact, insulating glial scar around the electrode [7]. This scar tissue increases the distance between neurons and electrode sites, causing rapid signal attenuation and a sharp rise in impedance, ultimately degrading the electrode's function [7] [12].
Experimental Protocols for Characterizing the Interface
A critical aspect of chronic stability research involves rigorous experimental characterization of the mechanical properties of both the neural tissue and the electrode, as well as the biological response post-implantation.
Characterizing Brain Tissue Mechanics
Accurately measuring the mechanical properties of brain tissue is challenging due to its ultrasoft, fragile, and heterogeneous nature [10]. Both invasive and non-invasive techniques are employed:
- Atomic Force Microscopy (AFM): This technique operates by detecting the contact interaction between an indenter tip and the tissue surface, providing force-displacement curves with piconewton-scale sensitivity. It is ideal for measuring mechanical properties at the micro- and nanoscale, revealing heterogeneity across different brain regions [10].
- Indentation (IND): A versatile platform for probing spatially resolved modulus and time-dependent viscoelastic behaviors of brain tissue [10].
- Magnetic Resonance Elastography (MRE): A non-invasive technique that measures brain tissue mechanical properties in vivo by analyzing the propagation of shear waves through the brain using MRI. It supports population-level studies and longitudinal monitoring within a single individual [10].
Table 2: Techniques for Characterizing Brain Tissue Mechanical Properties
| Technique | Spatial Scale | Measurable Parameters | Key Advantage |
|---|---|---|---|
| Atomic Force Microscopy (AFM) | Cellular / Subcellular | Young's Modulus at micro-scale | High resolution for assessing tissue heterogeneity |
| Indentation (IND) | Mesoscale | Spatially resolved modulus, viscoelastic properties | Versatile; allows testing of time-dependent behavior |
| Magnetic Resonance Elastography (MRE) | Organ (in vivo) | Shear stiffness, storage, and loss moduli | Non-invasive, suitable for longitudinal human studies |
Quantifying Electrode Degradation and Biocompatibility
To assess the long-term stability of electrodes, explant analysis and biological response characterization are essential.
- Scanning Electron Microscopy (SEM) for Explanted Electrodes: A seminal study analyzed 980 explanted microelectrodes from three human participants after 956–2130 days of implantation. Using SEM, researchers quantified physical degradation types (e.g., "cracked" or "pockmarked" surfaces) and correlated these findings with in vivo functional metrics like signal-to-noise ratio (SNR), impedance, and stimulation performance. This method provides a direct link between material integrity and clinical functionality [13].
- Drug-Release Coatings for Biocompatibility: A novel method to improve biocompatibility involves covalent binding of the anti-inflammatory drug dexamethasone onto a polyimide electrode surface. The experimental protocol involves:
- Chemically activating and modifying the polyimide surface.
- Covalently binding dexamethasone to the activated surface.
- Implanting the modified device in vivo.
- Assessing the slow release of the drug over at least two months and quantifying the reduction in immune cell signals and scar tissue formation compared to control implants [14].
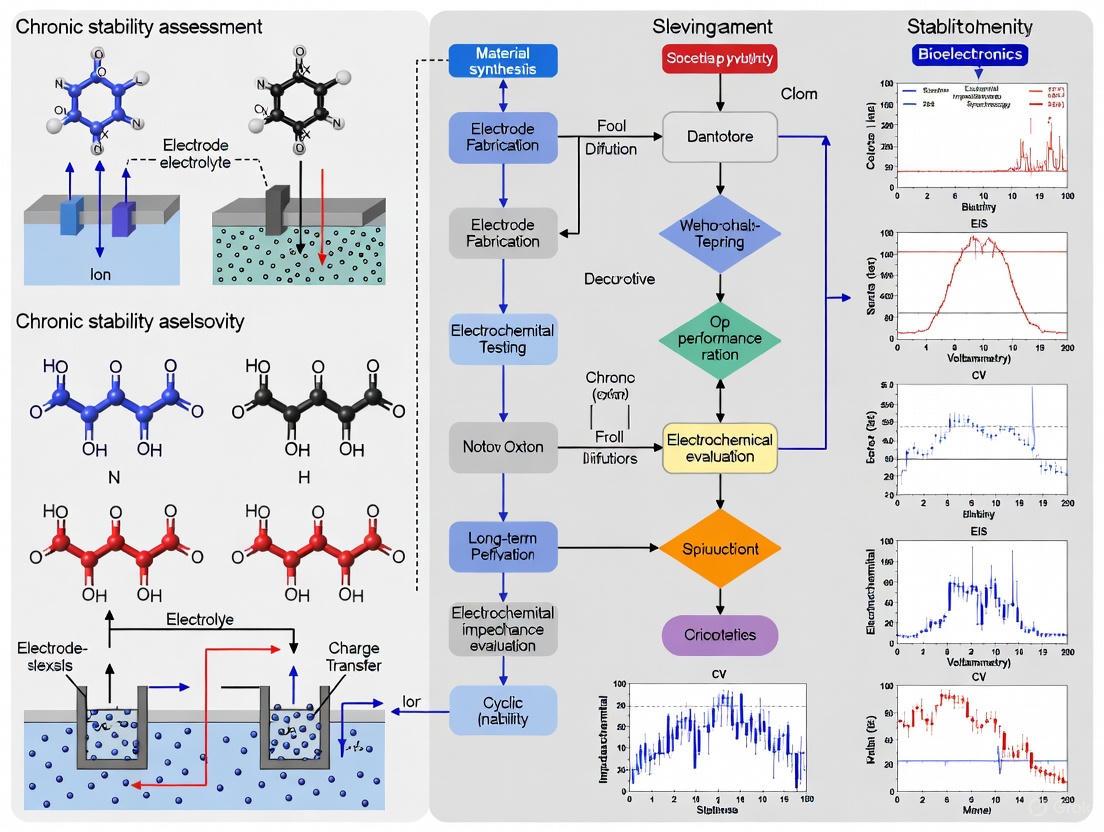
The workflow for a comprehensive chronic stability study, from material characterization to functional validation, can be visualized as follows:
Diagram 1: Chronic Stability Assessment Workflow
The Scientist's Toolkit: Research Reagent Solutions
To conduct the experiments described above, researchers rely on a suite of specialized materials and reagents. The following table details key items essential for working in this field.
Table 3: Essential Research Reagents and Materials for Neural Interface Studies
| Reagent/Material | Function/Application | Experimental Context |
|---|---|---|
| Polyimide | A flexible polymer commonly used as a substrate or insulation for implantable electrodes [7] [14]. | Serves as the base material for flexible neural interfaces; can be surface-modified for drug delivery [14]. |
| Dexamethasone | A potent anti-inflammatory drug used to modulate the immune response at the implant-tissue interface [14]. | Covalently bound to electrode surfaces (e.g., polyimide) to create a localized, slow-release coating that reduces scar formation [14]. |
| Iridium Oxide | A conductive coating applied to electrodes to improve their electrical properties and charge injection capacity [12] [13]. | Used as a coating on electrode sites (e.g., Sputtered Iridium Oxide Film - SIROF) to enhance recording and stimulation performance [13]. |
| Polyethylene Glycol (PEG) | A biocompatible polymer used as a temporary coating or adhesive. | Used as a temporary coating to fix a flexible electrode to a rigid tungsten wire shuttle during implantation; melts upon insertion to release the shuttle [7]. |
| Sputtered Iridium Oxide Film (SIROF) | An advanced electrode coating material with excellent charge transfer capabilities. | Used on electrode tips; studies show SIROF electrodes are twice as likely to record neural activity than platinum despite showing different degradation patterns [13]. |
| 6-Amino-1-hexanol | 6-Amino-1-hexanol | High-Purity Reagent Supplier | 6-Amino-1-hexanol is a bifunctional reagent for organic synthesis & bioconjugation. For Research Use Only. Not for human or veterinary use. |
| Batoprazine | Batoprazine HCl | SERT/NET Inhibitor | For Research | Batoprazine is a potent SERT/NET inhibitor for depression & anxiety research. For Research Use Only. Not for human consumption. |
Overcoming the mechanical mismatch at the neural interface requires a multi-faceted approach. No single strategy is sufficient; instead, integration is key. The path forward involves the synergistic combination of passive and active strategies [7]. Passively, electrodes must be designed with geometries and mechanical properties that minimize initial damage and chronic micromotion, effectively making the device "invisible" to the immune system [7]. Actively, surfaces can be functionalized to biochemically modulate the local environment, such as through the controlled release of anti-inflammatory drugs like dexamethasone to promote tissue repair and integration [14] [7].
The relationship between these integrated strategies and their collective impact on long-term stability is summarized below:
Diagram 2: Integrated Stability Strategies
As quantitative degradation studies in humans demonstrate [13], the clinical success of BCIs depends on overcoming these persistent material challenges. The future of stable implantable electrodes lies in the continued development and intelligent integration of advanced material science, sophisticated engineering, and biological modulation to finally bridge the stiffness gap for the lifetime of the patient.
The successful long-term operation of implantable neural electrodes is a cornerstone of modern neuroscience research and the development of advanced brain-computer interfaces (BCIs). These technologies enable unprecedented access to neural circuits, providing insights into brain function and offering therapeutic pathways for neurological disorders [11]. However, their chronic stability is severely compromised by the brain's inherent biological response to implanted devices, primarily gliosis and glial scar formation [15] [16]. This tissue reaction creates a physical and biological barrier that insulates the electrode from its target neurons, leading to a progressive decline in the quality of recorded neural signals and the efficacy of electrical stimulation over time [3] [11].
The core of the problem lies at the biotic-abiotic interface. Despite the shift from rigid to more flexible electrode materials to improve mechanical compatibility, the implantation of any device inevitably triggers a cascade of immune responses [7]. This begins with an acute inflammatory reaction due to mechanical mismatch and vascular damage during insertion, and evolves into a chronic foreign body reaction (FBR) characterized by the activation of microglia and astrocytes [7] [15]. These reactive glial cells proliferate, migrate toward the injury site, and ultimately form a dense, encapsulating sheath around the implant—the glial scar [7] [3]. This scar tissue, rich in glial fibrillary acidic protein (GFAP) and inhibitory extracellular matrix (ECM) components like chondroitin sulfate proteoglycans (CSPGs), acts as an insulating layer [17] [18]. It increases the distance between neurons and recording sites, causes a sharp rise in electrode impedance, and attenuates signal amplitude, culminating in the functional failure of the neural interface [7] [16]. Understanding and mitigating this gliotic barrier is therefore critical for advancing chronic stability assessment of implantable electrodes.
The Biological Cascade: From Implantation to Insulating Scar
The formation of the gliotic barrier is a dynamic, multi-stage process initiated at the moment of electrode insertion. The following diagram illustrates the key stages and primary cell types involved in this response.
The biological response begins with acute injury during device insertion. The mechanical trauma ruptures blood vessels, disrupting the blood-brain barrier (BBB) and allowing serum proteins like albumin and fibronectin to infiltrate the brain tissue [15]. This breach is a primary trigger for the activation of the brain's resident immune cells, microglia, within hours [7] [17]. Activated microglia adopt an amoeboid morphology, proliferate, and migrate to the implant surface, releasing a storm of pro-inflammatory cytokines, including TNF-α, IL-1β, and IL-6 [3] [19]. These cytokines contribute to a toxic environment for neurons and initiate the activation of astrocytes [15].
Over the following days and weeks, the response transitions to a chronic phase dominated by reactive astrocytes [17]. Driven by signaling from activated microglia and other damage-associated cues, astrocytes undergo reactive astrogliosis—a process characterized by cellular hypertrophy, proliferation, and a marked upregulation of intermediate filaments like GFAP [3] [15]. These reactive astrocytes densely populate the area around the implant, extending elongated processes that progressively form a tight, encapsulating border. As this border matures over weeks, it evolves into a dense glial scar [7] [17]. The scar tissue is not purely cellular; reactive astrocytes and infiltrating fibroblasts deposit inhibitory ECM molecules, most notably CSPGs, which further contribute to the scar's inhibitory properties by physically and chemically blocking axon regeneration [20] [18]. The final result is a compact, insulating sheath that surrounds the chronic implant.
Quantitative Impact: Comparing the Gliotic Barrier's Effect on Electrode Performance
The functional consequences of gliosis and scar formation are quantifiable and critically impact key electrode performance metrics. The following table summarizes the primary effects and their direct impact on signal recording and stimulation.
Table 1: Quantitative Impacts of Gliosis on Neural Electrode Performance Parameters
| Performance Parameter | Impact of Gliosis/Scar Formation | Consequence for Neural Interface |
|---|---|---|
| Electrode Impedance | Sharp increase due to insulating cellular/ECM barrier [16] | Reduced signal-to-noise ratio (SNR) and increased power requirements for stimulation [11] |
| Signal-to-Noise Ratio (SNR) | Progressive decline as scar tissue increases distance to neurons [3] | Loss of single-neuron resolution; inability to isolate action potentials [16] |
| Single-Unit Yield | Gradual decrease over weeks/months post-implantation [3] [16] | Reduced number of detectable and trackable neurons, limiting experimental and BCI throughput [3] |
| Neuronal Density | Significant loss of neurons within 100–150 μm of the electrode interface [3] | Fewer signal sources available for recording, contributing to signal decay [3] |
The most direct electrical impact is a significant rise in electrode impedance at the electrode-tissue interface. The glial scar, comprising cells and ECM proteins, acts as an electrical insulator, impeding the flow of current between the electrode and the brain tissue [16]. This increased impedance detrimentally affects both recording and stimulation. For recording, it leads to a lower SNR, as the tiny electrical signals from neurons are more easily lost in background noise [11]. For stimulation, more power is required to deliver the same amount of current to the neural tissue.
Furthermore, the physical separation caused by the encapsulating scar layer directly translates to signal attenuation. The amplitude of detectable neural signals, particularly action potentials from individual neurons, decays exponentially with distance. Even a scar thickness of tens of micrometers can significantly reduce spike amplitudes, making them undetectable above the noise floor [3]. This effect, combined with the actual death of neurons in the immediate vicinity of the implant due to neuroinflammatory processes and excitotoxicity, leads to a progressive drop in the number of recordable single units (single-unit yield) over time [3] [16]. This loss of stable single-unit recordings is a primary failure mode for chronic neuroscience experiments and clinical BCIs that rely on decoding precise neural spiking activity.
Methodologies for Assessing Gliosis and Scar Formation in Preclinical Models
Rigorous and standardized experimental protocols are essential for quantifying the foreign body response and evaluating new electrode technologies or anti-fibrosis strategies. The following workflow outlines a standard methodology for a correlated, multi-modal assessment.
The standard approach involves a correlative methodology that combines chronic electrical monitoring with post-mortem histological analysis. First, the electrode of interest is implanted into the target brain region (e.g., motor cortex, hippocampus) of an animal model, typically rodents or non-human primates [7]. For chronic electrical assessment, impedance spectroscopy and SNR tracking are performed regularly over the implantation period (e.g., weeks to months). These functional measurements provide a direct, time-lapsed view of device performance degradation [16].
Upon completion of the in vivo study, animals are perfused transcardially with a fixative like 4% paraformaldehyde (PFA) to preserve the tissue architecture. The brain is extracted, and the tissue block containing the implant track is cryo-sectioned or paraffin-embedded and sliced into thin sections (e.g., 10-40 μm thick) for histological analysis [15]. Immunohistochemistry (IHC) is the primary tool for visualizing the cellular components of the FBR. Standard protocols involve blocking with serum, followed by incubation with primary antibodies against key biomarkers:
- Anti-GFAP: To label reactive astrocytes and quantify glial scar thickness and density [3] [15].
- Anti-Iba1: To identify activated microglia and macrophages, assessing their morphology and distribution around the implant [15].
- Anti-NeuN: To label neuronal nuclei and quantify neuronal density and loss in the peri-implant region [3].
Fluorescent or chromogenic detection is used, often with counterstains like DAPI for nuclei. Additional stains, such as antibodies against CSPGs (e.g., CS-56), are used to label the inhibitory ECM of the scar [20] [18]. Finally, high-resolution confocal or fluorescence microscopy is employed to image the tissue sections. Quantitative image analysis software is then used to measure key metrics, including the thickness of the GFAP+ scar capsule, the density of Iba1+ cells, and the number of NeuN+ neurons at various distances from the electrode track [15] [16]. The final, critical step is to correlate these histological endpoints with the chronic electrical recording data to establish a direct link between the degree of gliosis and the decline in electrophysiological performance.
The Scientist's Toolkit: Essential Reagents for Gliosis Assessment
Table 2: Key Research Reagents for Analyzing the Foreign Body Response
| Reagent / Material | Function in Experimental Protocol |
|---|---|
| Anti-GFAP Antibody | Primary antibody for immunohistochemical labeling of reactive astrocytes; essential for quantifying glial scar formation [3] [15]. |
| Anti-Iba1 Antibody | Primary antibody for identifying activated and resting microglia/macrophages in the tissue surrounding the implant [15]. |
| Anti-NeuN Antibody | Primary antibody for staining neuronal nuclei, enabling quantification of neuronal survival and density near the electrode interface [3]. |
| Chondroitin Sulfate Proteoglycan (CSPG) Antibody (e.g., CS-56) | Labels the inhibitory extracellular matrix deposited within the glial scar, a key contributor to its barrier properties [20] [18]. |
| 4% Paraformaldehyde (PFA) | Standard fixative solution for perfusing animals and post-fixing brain tissue to preserve cellular morphology and antigenicity for histology [15]. |
| DAPI (4',6-diamidino-2-phenylindole) | Fluorescent nuclear counterstain that allows for visualization of all cell nuclei in a tissue section, used for cell counting and orientation. |
| Ethyl chrysanthemate | Ethyl Chrysanthemate | High-Purity | For Research |
| epi-Eudesmol | 10-epi-gamma-Eudesmol CAS 15051-81-7 |
Engineering Strategies to Mitigate the Gliotic Barrier
The pursuit of chronic stability has driven innovation in neural interface design, focusing on material properties, device geometry, and active biological modulation to minimize the FBR. A primary strategy involves reducing the mechanical mismatch between the rigid implant and the soft brain tissue (Young's modulus ~1-10 kPa) [11]. This has led to the development of flexible electrodes using polymers like polyimide or Parylene C, and ultrasmall, filamentary designs such as nanoelectronic threads (NETs) [7] [21]. These devices have a lower bending stiffness, which mitigates chronic micromotion-induced inflammation and reduces the strain on surrounding tissue [7] [16].
Complementing this passive approach are active bio-integration strategies. These include surface functionalization of electrodes with bioactive molecules like laminin or polyethylene glycol (PEG) to improve biocompatibility and reduce protein adsorption [7]. A more advanced tactic is the incorporation of controlled-release systems from the electrode itself, designed to locally deliver anti-inflammatory drugs (e.g., dexamethasone) or molecules that inhibit specific signaling pathways involved in astrocyte activation and scar formation [7]. For instance, targeting the IL-20 cytokine pathway with a neutralizing antibody (7E) has been shown in a spinal cord injury model to reduce glial scar formation and improve functional recovery, presenting a potential target for future neural interfaces [19].
Table 3: Comparison of Neural Probe Designs and Their Chronic Performance
| Probe Design/Strategy | Key Characteristics | Reported Impact on Chronic Gliosis & Recording Stability |
|---|---|---|
| Silicon Probes (Michigan, Neuropixels) | Rigid substrate (Silicon), high electrode count, precise geometry [3] [16] | Significant glial scarring and neuronal loss; recording instability over weeks; often requires microdrives for repositioning [3] [16]. |
| Flexible Polymer Probes | Low Young's modulus (e.g., Polyimide, SU-8), better mechanical match to tissue [7] [21] | Reduced chronic inflammation and glial scarring compared to rigid probes; improved long-term signal stability but require stiff temporary shuttles for implantation [7]. |
| Ultrasmall/Filamentary Probes (e.g., NeuroRoots, Carbon Fibers) | Minute cross-sectional area (< 10 μm width/diameter), "invisible" to immune system [7] | Minimal acute damage and chronic FBR; stable recordings reported for months; limited channel count per shank and handling challenges [7]. |
| Drug-Eluting Coatings | Local release of anti-inflammatory agents (e.g., Dexamethasone) from electrode surface [7] | Demonstrated suppression of reactive astrocytes and microglia in vicinity of implant; maintains lower impedance and higher SNR in chronic phase [7]. |
The formation of a gliotic scar represents the most significant biological barrier to the long-term stability and high-fidelity performance of implantable neural electrodes. While the field has made substantial progress in understanding this complex immune response and in developing engineering solutions to mitigate it—such as flexible materials, miniaturized geometries, and bioactive coatings—the challenge is not yet fully solved. The future of chronically stable neural interfaces lies in the continued blurring of the line between living tissue and man-made device [3]. This will likely be achieved through multi-faceted approaches that combine the mechanical stealth of next-generation flexible and injectable electronics [21] with the biological intelligence of immuno-modulatory surface treatments and closed-loop drug delivery systems that actively intervene to prevent scar formation only when necessary. Furthermore, the adoption of advanced assessment techniques, including transcriptomics to map the full molecular landscape of the FBR, will provide deeper insights and new targets for intervention [16]. By systematically addressing the insulating barrier of gliosis, researchers can pave the way for neural interfaces that remain stable and functional for a lifetime, unlocking their full potential for neuroscience and transformative clinical therapies.
Blood-Brain Barrier Disruption and Its Role in Sustaining Neuroinflammation
The blood-brain barrier (BBB) is a highly specialized, semi-permeable interface between the central nervous system (CNS) and the systemic circulation that dynamically regulates the bidirectional exchange of fluids, molecules, and cells [22]. This sophisticated biological barrier protects the brain from harmful substances while maintaining the precise chemical environment necessary for optimal neural function. Histologically, the BBB comprises non-fenestrated endothelial cells that form the capillary walls, supported by pericytes embedded in the basement membrane, and enveloped by astrocyte endfeet that create an intimate interaction with the vascular system [22]. These cellular components collectively form the neurovascular unit (NVU), which includes additional elements such as perivascular macrophages, microglia, and neurons that contribute to BBB function and regulation [23].
At the molecular level, the exceptional impermeability of the BBB arises from complex protein networks that create tight junctions between endothelial cells. These junctions consist of transmembrane proteins including occludin, claudins (particularly claudin-5), and junctional adhesion molecules, which are linked intracellularly to zonula occludens proteins (ZO-1, ZO-2) that anchor the junctional complexes to the actin cytoskeleton [23]. Adherens junctions composed of vascular endothelial cadherin (VE-cadherin) provide additional intercellular adhesion and stability [22]. The cerebral endothelial glycocalyx, a thick layer of proteoglycans, glycoproteins, and glycolipids on the luminal surface, serves as the first physical barrier of the BBB and plays a crucial role in regulating vascular permeability and immune cell adhesion [22].
When the BBB becomes compromised through various pathological mechanisms, its disruption initiates and sustains neuroinflammation through multiple pathways. The breakdown of this critical barrier allows uncontrolled entry of blood-derived components, immune cells, and inflammatory mediators into the CNS, creating a self-perpetuating cycle of inflammation and neuronal damage [22]. This review examines the mechanisms linking BBB disruption to sustained neuroinflammation, with particular emphasis on implications for chronic stability assessment of implantable neural electrodes, highlighting current research methodologies and experimental approaches for investigating these complex interactions.
Mechanisms of BBB Disruption in Neuroinflammation
Molecular Mechanisms of Barrier Breakdown
BBB disruption in neuroinflammatory conditions occurs through multiple interconnected molecular pathways that compromise endothelial integrity. Inflammatory mediators such as cytokines and chemokines play a pivotal role in initiating these changes. Recent research has identified that NLRP3 activation in neutrophils induces BBB disruption via CXCL1/2 secretion and subsequent activation of the CXCL1/2-CXCR2 signaling axis, which directly reduces Claudin-5 expression in brain endothelial cells, increasing paracellular permeability [24]. This pathway represents a crucial mechanism by which innate immune cells directly modulate BBB integrity during neuroinflammation.
The tight junction proteins between endothelial cells undergo significant alterations under inflammatory conditions. Sleep restriction studies in mouse models have demonstrated progressive BBB permeability increases correlated with decreased expression of tight junction proteins claudin-5, occludin, and zonula occludens-1 (ZO-1) [25]. These structural changes are accompanied by pericyte detachment from the capillary wall, further destabilizing the neurovascular unit [25]. Complement system activation, particularly increased levels of the C3 component, contributes to BBB dysfunction by binding to C3aR on endothelial cells and reducing trans-endothelial electric resistance [25].
Recent research has also identified TDP-43 depletion in endothelial cells as a significant mechanism in BBB disruption associated with neurodegenerative diseases. Loss of this RNA-binding protein in endothelial cells leads to reduced nuclear β-catenin and downregulation of β-catenin-dependent genes, coupled with elevated TNF/NF-κB signaling, creating a disease-associated endothelial phenotype that compromises BBB function [26]. This mechanism appears particularly relevant in Alzheimer's disease, amyotrophic lateral sclerosis, and frontotemporal degeneration, suggesting a common pathway in proteinopathic neurodegeneration.
Cellular Senescence and BBB Dysfunction
Cellular senescence has emerged as a critical mechanism linking chronic neuroinflammation to persistent BBB disruption. Sleep restriction studies in young mice have demonstrated progressive increases in senescence markers (β-galactosidase and p21) in cerebral cortex and hippocampus, accompanied by astroglial reactivity and complement activation [25]. These senescent cells exhibit a senescence-associated secretory phenotype (SASP), characterized by secretion of pro-inflammatory cytokines including IL-1α, IL-8, IL-1β, and IL-6, which further perpetuates neuroinflammation and barrier dysfunction [25].
The relationship between cellular senescence and BBB disruption creates a vicious cycle in which neuroinflammation promotes senescence, and senescent cells release inflammatory mediators that further compromise barrier function. This phenomenon has been observed not only in aging but also in response to various stressors, including sleep deprivation, where senescence markers increase progressively alongside BBB hyperpermeability [25]. This mechanism may explain why BBB disruption often persists even after the initial insult has resolved, particularly in conditions such as long COVID-associated cognitive impairment [27].
Table 1: Key Molecular Mechanisms in BBB Disruption
| Mechanism | Key Components | Functional Consequences |
|---|---|---|
| Junctional Disassembly | Reduced claudin-5, occludin, ZO-1 | Increased paracellular permeability |
| Cellular Senescence | β-galactosidase, p21, SASP factors | Chronic low-grade neuroinflammation |
| Inflammatory Signaling | CXCL1/2-CXCR2 axis, TNF/NF-κB | Enhanced leukocyte adhesion & migration |
| Complement Activation | C3 component, C3aR binding | Reduced trans-endothelial resistance |
Consequences of BBB Disruption on Neural Tissue
Neuroinflammatory Cascade and Neuronal Damage
Breakdown of the BBB initiates a neuroinflammatory cascade characterized by activation of glial cells and infiltration of peripheral immune cells. When the barrier becomes compromised, serum proteins, inflammatory mediators, and peripheral immune cells gain access to the CNS parenchyma, triggering microglial activation and astrocyte reactivity [3]. Activated microglia release pro-inflammatory cytokines including IL-1, TNF-α, and IL-6, which further amplify the inflammatory response and contribute to neuronal damage [3]. Reactive astrocytes undergo morphological and functional changes characterized by increased expression of glial fibrillary acidic protein (GFAP) and contribute to inflammatory signaling through production of cytokines and complement components [25].
The sustained neuroinflammation resulting from BBB disruption creates an environment that promotes neuronal dysfunction and ultimately cell death. Pro-inflammatory cytokines and reactive oxygen species generated by activated immune cells exhibit direct neurotoxicity and disrupt normal neuronal signaling [3]. This neuroinflammatory environment has been particularly well-documented in long COVID-associated cognitive impairment, where BBB disruption correlates with significant cognitive deficits, commonly referred to as "brain fog" [27]. The observation that BBB disruption precedes classical Alzheimer's disease pathology and brain atrophy suggests it may be an early driver rather than merely a consequence of neurodegenerative processes [26].
Implications for Neural Interface Technology
The chronic foreign body response to implanted neural electrodes shares remarkable similarities with neuroinflammatory responses to BBB disruption. Conventional rigid neural probes trigger persistent inflammation characterized by gliosis (formation of glial scars) and neuronal death in proximity to the implant [3]. The mechanical mismatch between rigid electrodes and surrounding brain tissue creates ongoing micro-movements that sustain chronic inflammation, activate microglia, and perpetuate BBB disruption [3]. This inflammatory microenvironment leads to the formation of a dense glial scar around implanted electrodes, composed primarily of reactive astrocytes and microglia, which increases the distance between recording electrodes and target neurons, elevates interfacial impedance, and causes progressive signal quality degradation over time [3].
Table 2: Consequences of BBB Disruption on Neural Function
| Consequence | Key Features | Impact on Neural Function |
|---|---|---|
| Gliosis | Reactive astrocytes, glial scar formation | Physical barrier between electrodes and neurons |
| Neuronal Death | Loss of neurons near injury/implant | Reduced signal sources for recording |
| Chronic Inflammation | Persistent cytokine release, oxidative stress | Progressive tissue damage & dysfunction |
| Immune Cell Infiltration | Neutrophils, T-cells, monocytes | Amplification of inflammatory response |
The compromised BBB allows serum proteins and other neurotoxic substances to enter the brain parenchyma, where they exacerbate inflammation and contribute to neuronal injury. In the context of neural interfaces, this phenomenon is particularly detrimental as the barrier disruption permits serum components to leak into the tissue surrounding implants, further accelerating the foreign body response and device failure [3]. Understanding these shared mechanisms provides valuable insights for developing strategies to improve the chronic stability of implantable neural interfaces.
Experimental Models and Assessment Methodologies
In Vivo Assessment Techniques
Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) has emerged as a powerful non-invasive technique for quantifying BBB permeability in living subjects. This methodology has been successfully employed to demonstrate BBB disruption in patients with long COVID-associated cognitive impairment, providing direct clinical evidence of barrier breakdown in humans [27]. The technique involves serial T1-weighted imaging following intravenous administration of gadolinium-based contrast agents, with mathematical modeling of contrast agent kinetics to calculate permeability surface area products and fractional leakage rates.
Evans blue and sodium fluorescein permeability assays represent well-established methodologies for quantifying BBB disruption in animal models. In this protocol, Evans blue (which binds serum albumin) and sodium fluorescein are administered intravenously, followed by a circulation period and subsequent transcardial perfusion to remove intravascular tracer [25]. Brain regions are then dissected, homogenized, and tracer extravasation quantified using fluorescence or spectrophotometric detection. This approach has demonstrated progressive BBB permeability increases following sleep restriction in mice, with significant leakage observed after 3, 5, and 10 days of restriction [25].
Two-photon intravital microscopy (TP-IVM) enables real-time visualization of neurovascular dynamics in living animals. This technique employs fluorescent dextrans of varying molecular weights to assess vascular permeability and immune cell trafficking. In studies of NLRP3 activation, 10-kDa Texas Red-dextran extravasation served as a sensitive indicator of BBB disruption, with intensity outside vessels quantitatively measuring permeability [24]. This methodology allows longitudinal assessment of barrier function and direct observation of neutrophil migration patterns in the cortical vasculature.
Molecular and Cellular Analysis Methods
Western blot analysis of tight junction proteins provides quantitative assessment of molecular correlates of BBB integrity. Standard protocols involve homogenizing brain tissue samples (e.g., cerebral cortex and hippocampus), separating proteins by SDS-PAGE electrophoresis, transferring to PVDF membranes, and probing with antibodies against claudin-5, ZO-1, occludin, and other junctional components [25]. Ponceau red staining typically serves as a loading control for normalization. This technique has confirmed reduced expression of tight junction proteins following sleep restriction in mice [25].
Enzyme-linked immunosorbent assays (ELISA) enable precise quantification of inflammatory mediators in brain tissue and biological fluids. Multiplex Luminex and ProcartaPlex panels permit simultaneous measurement of numerous cytokines (TNF-α, IL-1β, IL-6, IL-4, IL-10), chemokines, growth factors, and markers of endothelial activation in serum, plasma, and brain homogenates [27]. This approach has identified distinct inflammatory profiles in patients with COVID-19-associated neurological symptoms, including elevated S100β, a marker suggestive of BBB dysfunction [27].
Flow cytometry with intravascular staining distinguishes between vascularly confined and parenchymal immune cells in CNS inflammation models. This protocol involves intravenous administration of anti-CD45 antibody several minutes before perfusion, which labels only circulating leukocytes without penetrating the intact BBB [24]. Subsequent flow cytometric analysis of brain homogenates allows precise determination of neutrophil and T-cell infiltration into the CNS parenchyma, providing quantitative data on immune cell trafficking across the disrupted BBB.
Research Reagent Solutions for BBB Studies
Table 3: Essential Research Reagents for BBB Investigation
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| BBB Permeability Tracers | Evans blue, sodium fluorescein, Texas Red-dextran conjugates | Quantitative assessment of barrier integrity in vivo |
| TJ Protein Antibodies | Anti-claudin-5, anti-ZO-1, anti-occludin | Western blot, immunohistochemistry for junctional integrity |
| Cytokine Detection | Multiplex Luminex panels, ELISA kits for TNF-α, IL-1β, IL-6 | Quantification of inflammatory mediators |
| Cell Type Markers | Anti-GFAP (astrocytes), Iba1 (microglia), CD146 (pericytes) | Immunohistochemical cell identification and quantification |
| Molecular Biology | Primers for β-catenin targets, NF-κB pathway genes | qPCR analysis of BBB-relevant signaling pathways |
Signaling Pathways in BBB Disruption
The following diagram illustrates key signaling pathways involved in blood-brain barrier disruption during neuroinflammation, integrating multiple mechanisms identified from recent research:
Schematic of Key BBB Disruption Pathways: This diagram integrates multiple mechanisms identified in recent research, including NLRP3-CXCR2 signaling [24], TDP-43 loss with β-catenin/NF-κB dysregulation [26], and tight junction protein alterations [25] [22].
Implications for Neural Interface Development
The relationship between BBB disruption and sustained neuroinflammation presents significant challenges for chronically implanted neural interfaces. The foreign body response to implanted electrodes shares fundamental mechanisms with neuroinflammatory cascades triggered by BBB breakdown, including persistent activation of microglia and astrocytes, release of pro-inflammatory cytokines, and recruitment of peripheral immune cells [3]. These processes culminate in the formation of glial scars around implants, which electrically isolate electrodes from their target neurons and degrade recording and stimulation performance over time [3].
Advanced electrode design strategies focused on reducing mechanical mismatch with brain tissue show promise for mitigating these inflammatory responses. Flexible neural interfaces with low bending stiffness and Young's modulus comparable to brain tissue (approximately 1-10 kPa) significantly reduce chronic inflammation and glial scarring compared to conventional rigid electrodes [7]. Innovative approaches include ultra-flexible mesh electrodes, filamentous designs with cross-sectional areas at the subcellular level, and bioresorbable supporting structures that provide temporary rigidity during implantation before dissolving to leave only compliant components [7]. These engineering solutions directly address the mechanical factors that contribute to sustained BBB disruption and neuroinflammation around neural implants.
Surface functionalization strategies offer complementary approaches to improve biocompatibility. Anti-inflammatory coatings with controlled drug release systems can actively suppress local immune responses, while biomimetic surface modifications promote integration with neural tissue [7]. The development of neural interfaces that minimize BBB disruption and subsequent neuroinflammation represents a critical frontier in creating stable, long-term brain-computer interfaces for both basic research and clinical applications.
BBB disruption represents a critical mechanism in initiating and sustaining neuroinflammation across diverse neurological conditions, from neurodegenerative diseases to foreign body responses against implanted neural interfaces. The molecular mechanisms underlying this relationship—including tight junction disassembly, cellular senescence, and inflammatory signaling pathways—create self-perpetuating cycles of barrier dysfunction and CNS inflammation. Advanced assessment methodologies, including DCE-MRI, intravital microscopy, and molecular profiling techniques, provide powerful tools for investigating these complex interactions. For neural interface technology, addressing the shared mechanisms of BBB disruption and neuroinflammation through innovative electrode designs and surface modifications offers the most promising path toward achieving stable long-term performance. Future research integrating BBB protection strategies with neural interface development will be essential for creating next-generation devices that maintain signal fidelity over chronic timescales while minimizing tissue damage.
For researchers and drug development professionals working in neurotechnology, the long-term stability of implantable electrodes is a paramount concern. A critical factor determining the success of chronic neural interfaces is the biological response at the electrode-tissue interface, particularly neuronal death. This review objectively compares the performance of different electrode technologies, focusing on how their design and implantation strategies influence neuronal survival and, consequently, the fidelity and longevity of signal acquisition. The chronic stability of an implantable electrode is not merely a function of its electrical properties but is intrinsically linked to its biocompatibility and ability to minimize trauma during and after implantation [7] [28]. The foreign body response, culminating in glial scar formation around the implant, creates a physical barrier that increases the distance between neurons and recording sites. This leads to signal attenuation and a sharp rise in impedance, ultimately compromising the electrode's function [7]. Therefore, understanding and mitigating the causes of neuronal death in the electrode vicinity is a fundamental prerequisite for developing next-generation, high-performance neural interfaces for chronic applications.
Mechanisms of Neuronal Death and Signal Degradation
The process of neuronal degradation and signal loss around implanted electrodes is a complex cascade initiated by the body's immune response. The initial implantation causes acute injury, damaging blood vessels and neuronal tissue, which triggers a release of inflammatory factors [7]. This mechanical mismatch between the electrode and the soft brain tissue (Young's modulus of approximately 1–10 kPa) is a primary source of this trauma [7]. Over time, this acute response can evolve into a chronic inflammatory state. Microglia are activated and release inflammatory cytokines, while astrocytes proliferate and migrate to the injury site, secreting extracellular matrix components [7].
The culmination of this process is the formation of a dense glial scar, which acts as an insulating layer around the electrode [7]. The scar tissue increases the physical distance between viable neurons and the electrode's recording sites, leading to a marked decline in signal quality. This insulation effect results in signal attenuation and a sharp increase in impedance, degrading the electrode's performance for both recording and stimulation purposes [7]. This mode of failure, driven by changes in the biological environment, often occurs in parallel with intrinsic device failures such as corrosion, delamination, or insulation failure of the electrode itself [28]. The diagram below illustrates this sequential relationship between implantation, the immune response, and the final degradation of signal quality.
Comparative Performance of Electrode Technologies
Different electrode technologies interact with neural tissue in distinct ways, leading to varying levels of neuronal death and signal stability. The following table summarizes key performance metrics from chronic studies of three electrode types: flexible deep brain interfaces, peripheral nerve cuff electrodes, and endovascular stent-electrode arrays.
Table 1: Chronic Performance Comparison of Implantable Electrode Technologies
| Electrode Technology | Typical Host Structure | Key Metrics for Chronic Stability | Reported Longevity & Performance Data | Advantages / Disadvantages |
|---|---|---|---|---|
| Flexible Deep Brain Electrode [7] [28] | Brain Parenchyma | Glial scar formation, Immuno-response, Intrinsic device failure | Recording stability: up to 8 months in cortex; Stimulation stability: considerably less [7] [28] | + Lower mechanical mismatch [7]– Challenging implantation; requires rigid shuttle [7] |
| Spiral Nerve Cuff Electrode [29] | Peripheral Nerve | Nerve conduction velocity, Stimulation threshold, Muscle selectivity | Stable thresholds after ~20 weeks; Selective activation maintained for 3 years [29] | + Stable long-term recruitment [29]– Requires surgical access to nerve [29] |
| Endovascular Stent-Electrode (Stentrode) [30] [31] | Superior Sagittal Sinus | Motor signal modulation, Electrode impedance, Resting state band power | Stable movement modulation & impedance over 12 months [30] [31] | + Minimally invasive implantation [30]– Signal source is field potentials, not single units [30] |
A critical experimental finding from studies on spiral nerve cuff electrodes is the timeline for stabilization. In human subjects, the stimulation thresholds for these electrodes were found to stabilize after approximately 20 weeks post-implantation, providing a crucial timeframe for assessing the settling of the acute biological response [29]. Furthermore, the variability in activation over time was found to be no different from that of traditional muscle-based electrodes used in functional electrical stimulation systems, indicating that the nerve-electrode interface can achieve a level of stability suitable for clinical applications [29].
Experimental Protocols for Assessing Electrode Impact and Neuronal Health
To objectively compare electrode technologies and their impact on neuronal health, standardized experimental protocols are essential. The following methodologies are critical for evaluating the chronic performance and biological integration of neural interfaces.
Chronic In Vivo Implantation and Functional Assessment
This protocol is used for long-term evaluation of electrode stability and its functional impact on the surrounding neural tissue, particularly in motor-related applications [29] [30].
- Electrode Implantation: The electrode (e.g., spiral nerve cuff, stentrode, or flexible array) is surgically implanted in the target structure (peripheral nerve, superior sagittal sinus, or brain parenchyma) [29] [30].
- Post-Surgical Recovery & Stabilization: Following implantation, a period of several weeks is allowed for the initial tissue response and electrode encapsulation to stabilize. Shoulders may be immobilized for 3 weeks in the case of peripheral implants [29].
- Exercise Regime: Subjects perform daily exercise sessions to increase the strength and endurance of the target muscles, which also conditions the electrode-tissue interface [29].
- Data Collection Sessions: Data collection begins after the initial stabilization period. Twitch recruitment curves are generated by sending single stimulation pulses and recording the muscle electromyograms (EMG). The activation level is quantified as the area under the rectified EMG response between 5 and 40 ms post-stimulus to eliminate artifact and reflexive contributions [29].
- Long-Term Monitoring: Functional testing occurs over months to years. Metrics include stimulation thresholds, nerve conduction velocity, and for recording electrodes, motor signal modulation (e.g., in high-frequency bands of 30–200 Hz) and electrode impedance [29] [30].
High-Density Multi-Electrode Array (hd-MEA) Analysis of Network Activity
This in vitro protocol uses high-density arrays to monitor the functional effects of interventions, like radiation or toxicological agents, on neuronal networks, providing insights into how similar processes might affect neurons near an implant [32].
- Tissue Preparation: Prefrontal cortex (PFC) or other brain region slices are prepared and maintained in vitro.
- Experimental Intervention: Slices are subjected to the intervention under study (e.g., escalating doses of radiation) using a robotic platform [32].
- hd-MEA Recording: Neural activity is recorded across thousands of channels (e.g., 4,096) to capture extracellular action potentials with high spatial and temporal resolution [32].
- Signal Processing: Voltage deflections (multi-unit spikes) are detected by applying a threshold below the mean voltage. The rate of neural activity at individual channels is computed as the average number of threshold-crossing events per second [32].
- Network Analysis: Key metrics are extracted:
- Firing Rate: The average number of spike events per second across the network.
- Functional Connectivity: Correlations between all pairs of channels on the hd-MEA, with a cut-off (e.g., r = 0.2) applied to reject weak correlations.
- Graph-Theoretic Metrics: Measures such as modularity and global efficiency are calculated to characterize network topology [32].
- Apoptosis Staining: Propidium iodide or other staining is used to quantify a dose-dependent effect on apoptosis, linking functional changes to cell death [32].
The workflow for the hd-MEA protocol, from tissue preparation to data analysis, is visualized below.
Mitigation Strategies for Enhanced Long-Term Stability
The search for chronically stable neural interfaces has led to several innovative strategies focused on mitigating the foreign body response and preventing neuronal death. These can be broadly categorized into passive and active approaches.
Passive Strategies: Material and Design Optimization: The core of this approach is to make the electrode "invisible" to the immune system by minimizing the mechanical mismatch. This involves using flexible materials with a low Young's modulus that closely match that of brain tissue (~1-10 kPa) [7]. Further, optimizing the electrode's geometric shape and implantation cross-sectional area is crucial to reduce acute injury during insertion. Surface functionalization of electrodes with bioactive coatings is another passive strategy to enhance biocompatibility and integration [7].
Active Strategies: Anti-Inflammatory Drug Release: This approach aims to actively modulate the tissue environment post-implantation. It involves integrating drug-controlled release systems into the electrode design [7]. These systems can release anti-inflammatory substances or neurotrophic factors locally to suppress the immune response, promote tissue repair, and support neuronal survival around the implant site [7].
The most advanced solutions likely involve a synergistic combination of these strategies, where the electrode's physical properties are optimized to minimize initial damage, and its surface is engineered to actively maintain a healthy neuronal environment.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and reagents essential for research in neuronal health and electrode performance.
Table 2: Key Reagents and Materials for Neural Interface Research
| Item Name | Function / Application | Key Characteristics |
|---|---|---|
| Spiral Nerve Cuff Electrode [29] | Chronic stimulation and recording from peripheral nerves. | Multi-contact design; spiral shape allows for nerve expansion; used for selective muscle activation. |
| Stentrode (Endovascular Electrode Array) [30] [31] | Minimally invasive recording of motor cortex signals from a blood vessel. | 16-channel stent-electrode array; deployed in superior sagittal sinus. |
| High-Density Multi-Electrode Array (hd-MEA) [32] | High-resolution mapping of network activity in brain slices. | 4,096 recording channels; captures population firing rates and functional connectivity. |
| Activated Caspase-3 (aCasp3) Antibody [33] | Immunohistochemical marker for apoptotic cells. | Early marker of irreversible entry into apoptosis; labels dying neurons. |
| Propidium Iodide [32] | Fluorescent stain for identifying dead cells in a population. | Stains cells with compromised membranes; used to quantify apoptosis. |
| Polyimide-based Flexible Electrode [7] [28] | Substrate for thin-film, flexible neural interfaces. | Biocompatible polymer; provides mechanical flexibility; used as substrate and insulation. |
| Parylene-C [28] | Conformal coating for neural implant insulation. | Biocompatible polymer; provides a moisture barrier and electrical insulation. |
| Ag/AgCl Pseudo Reference Electrode [34] [35] | Provides a stable reference potential in electrochemical setups. | Common in screen-printed and implantable sensors; potential is stable in controlled ionic environments. |
| Cuminaldehyde | Cuminaldehyde, CAS:122-03-2, MF:C10H12O, MW:148.20 g/mol | Chemical Reagent |
| Diisohexyl phthalate | Diisohexyl Phthalate|Plasticizer for Research | Diisohexyl phthalate is a dialkyl phthalate ester used as a plasticizer in polymer research. This product is for research use only and not for human use. |
Assessment Armamentarium: Methodologies for Evaluating Electrode Performance and Stability
For researchers developing chronic implantable electrodes, ensuring long-term electrochemical stability at the neural interface is paramount. Electrochemical Impedance Spectroscopy (EIS) serves as a powerful, non-invasive diagnostic tool for tracking interface degradation and assessing the performance of electrode materials under realistic conditions. This technique probes the electrical properties of the electrode-electrolyte interface, revealing critical information about charge transfer efficiency, corrosion processes, and the onset of material failure that directly impacts device functionality and biological safety [36] [37].
This guide compares the chronic performance of leading electrode material technologies—specifically, thin-film metallization and titanium nitride (TiN) nanostructures—by examining experimental EIS data and complementary electrochemical assessments. We provide structured comparisons and detailed methodologies to inform material selection and testing protocols for next-generation neural interfaces.
Experimental Protocols for EIS in Chronic Stability Assessment
EIS Measurement Methodology
A standard EIS experiment involves applying a small-amplitude sinusoidal alternating current (AC) potential to an electrochemical cell (the electrode in contact with electrolyte or biological tissue) and measuring the resulting current response [38] [39]. The core procedural steps are:
- Signal Application: A potentiostat or frequency response analyzer applies a sinusoidal potential signal, ( E(t) = E0 \sin(\omega t) ), where ( E0 ) is the amplitude (typically 1-10 mV to maintain pseudo-linearity) and ( \omega ) is the radial frequency [38] [39].
- Response Measurement: The resulting current signal, ( I(t) = I0 \sin(\omega t + \phi) ), is measured, where ( I0 ) is the current amplitude and ( \phi ) is the phase shift between potential and current [38].
- Frequency Sweep: The experiment is repeated across a wide frequency range, typically from 100 kHz down to 10 mHz or 1 Hz, with measurements often spaced logarithmically [39].
- Impedance Calculation: The complex impedance ( Z(\omega) ) is calculated at each frequency from the potential and current signals: ( Z(\omega) = \frac{E(t)}{I(t)} = Z0 \frac{\cos(\phi) + j \sin(\phi)} = Z{\text{real}} + j Z_{\text{imag}} ) [38] [39].
Data Presentation and Analysis
Impedance data is commonly presented in two primary formats, each offering distinct analytical advantages:
- Nyquist Plot: Plots the negative imaginary impedance (( -Z{\text{imag}} )) against the real impedance (( Z{\text{real}} )) at each frequency. This representation readily reveals the number of time constants in the system (often appearing as semicircles or depressed semicircles) but does not explicitly show frequency information [38] [39].
- Bode Plot: Displays the impedance magnitude (( |Z| )) and phase angle (( \phi )) each against log frequency. This format clearly shows the frequency dependence of the impedance and is useful for identifying the characteristic frequencies of different electrochemical processes [38] [39].
The resulting data is typically analyzed by fitting to an equivalent circuit model, which uses electrical components like resistors, capacitors, and constant phase elements to represent physical processes at the electrode interface (e.g., solution resistance, charge transfer resistance, double-layer capacitance) [38] [40].
Comparative Performance of Electrode Materials
The long-term stability of implantable electrodes is a complex function of material properties, design, and the biological environment. The following table summarizes key performance metrics for different electrode technologies based on chronic in vivo and accelerated in vitro testing.
Table 1: Chronic Performance Comparison of Neural Electrode Materials
| Material & Design | Study Duration | Key EIS Findings (Impedance Magnitude) | Stability & Charge Injection Performance | Noted Failure Modes |
|---|---|---|---|---|
| Thin-Film Metallization (TIME, Pt) | Up to 6 months (Human) | Initial: 21-100 kΩ (varies by patient); Plateau: ~100 kΩ; Some terminals showed decrease to ~73 kΩ [36]. | Stable within safe limits for up to 22 weeks; enabled precise amplitude modulation [36]. | Adhesion loss mitigated by SiC layer; redesign from rectangular to split ground contact reduced mechanical stress [36]. |
| TiN Thin Films | 1000 CV Cycles (In Vitro) | N/A | ~25% capacitance loss under ambient conditions; ~13% capacitance loss under Ar-saturated conditions [37]. | Performance decay linked to surface oxidation and reduced charge storage capacity over time [37]. |
| TiN Nanowires (NWs) | 1000 CV Cycles (In Vitro) | N/A | ~5% capacitance loss under ambient conditions; ~2% capacitance loss under Ar-saturated conditions [37]. | Superior cycling stability with minimal capacitance decay; enhanced charge injection capability [37]. |
Performance Analysis and Material Selection
The data indicates a clear trend: nanostructured materials like TiN nanowires offer superior electrochemical stability compared to their thin-film counterparts. This is attributed to their significantly increased surface area, which provides more active sites for charge transfer and results in higher capacitance and lower impedance [37]. This makes them exceptionally suitable for miniaturized electrodes that require high charge injection capacity within safe voltage limits.
For chronic human implants, mechanical design and material integrity are as critical as electrochemical properties. The success of thin-film electrodes in human trials for up to six months was achieved through iterative design improvements, such as incorporating adhesion layers and optimizing ground contact geometry to mitigate intrinsic stress and prevent delamination [36].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials and Reagents for Electrode EIS Assessment
| Item | Function in EIS Experiment |
|---|---|
| Potentiostat / Frequency Response Analyzer (FRA) | The core instrument that applies the controlled AC potential and measures the resulting current response from the electrochemical cell [39]. |
| Phosphate Buffered Saline (PBS) (0.1 M) | A standard simulated physiological electrolyte solution used for in vitro testing to approximate the ionic environment of the human body [37]. |
| Reference Electrode (e.g., Ag/AgCl) | Provides a stable, known reference potential against which the potential of the working electrode is measured and controlled [39]. |
| Counter Electrode (Auxiliary Electrode) | Completes the electrical circuit in the three-electrode setup, allowing current to flow through the cell without affecting the measurement of the working electrode [39]. |
| Polyimide-Based Neural Electrodes | A flexible, biocompatible substrate used for chronic implantable electrodes like the TIME, providing mechanical compliance with neural tissue [36]. |
| Titanium Nitride (TiN) Nanowires | A nanostructured electrode coating material characterized by high capacitance and excellent electrochemical stability, enhancing charge transfer and longevity [37]. |
| Ethyl nonadecanoate | Ethyl nonadecanoate, CAS:18281-04-4, MF:C21H42O2, MW:326.6 g/mol |
| Diphenylacetic Acid | Diphenylacetic Acid, CAS:117-34-0, MF:C14H12O2, MW:212.24 g/mol |
Workflow for EIS-Based Degradation Tracking
The following diagram illustrates the logical workflow for using EIS to assess and monitor the stability and degradation of implantable electrodes, from initial material screening to chronic in vivo assessment.
Figure 1: This workflow outlines the process of using EIS for tracking electrode interface degradation. The process begins with in vitro screening of new materials, followed by equivalent circuit modeling to extract key interfacial parameters. Promising candidates then undergo accelerated aging and chronic in vivo EIS tracking to identify degradation signatures. The insights gained from failure mode analysis create a feedback loop for improving material design and enhancing long-term stability.
Electrochemical Impedance Spectroscopy is an indispensable tool for quantifying the stability and predicting the functional lifespan of implantable neural electrodes. The comparative data presented in this guide demonstrates that while standard thin-film electrodes can achieve chronic stability in humans for several months through careful design, emerging nanostructured materials like TiN nanowires exhibit fundamentally superior electrochemical resilience in vitro. For researchers, the integration of robust EIS protocols throughout the development cycle—from accelerated material screening to long-term in vivo validation—is critical for advancing reliable, high-performance bioelectronic therapies. Future progress hinges on the continued correlation of specific EIS signatures, such as impedance drift and capacitance loss, with physical failure mechanisms to enable predictive modeling of electrode longevity.
For researchers developing implantable electrodes, the chronic stability of the device-tissue interface is a paramount concern. The Signal-to-Noise Ratio (SNR) stands as a critical, quantitative metric for assessing the functional quality of neural recordings over time. A decline in SNR directly reflects the deterioration of this interface, often signaling the failure of an experimental device or therapy. This guide objectively compares the performance and stability of different electrode technologies, focusing on the quantitative SNR data and experimental methodologies essential for evaluating long-term viability within chronic implantation research.
Electrode Performance and Stability Comparison
The long-term recording performance of an implantable electrode is fundamentally linked to its material composition and design. The following table synthesizes key findings from chronic studies, with SNR as a central measure of functional stability.
Table 1: Chronic Performance Comparison of Implantable Electrode Technologies
| Electrode Type / Material | Study Duration & Model | Recording Performance (SNR & Stability) | Key Stability Findings |
|---|---|---|---|
| Sputtered Iridium Oxide Film (SIROF) | 956-2130 days (2.6-5.8 years); Human Cortex [13] | â–º Twice as likely to record neural activity than Pt electrodes despite greater physical degradation [13] | â–º 1 kHz impedance correlated with physical damage and performance metrics, serving as a reliable indicator of in vivo degradation [13] |
| Platinum (Pt) | 956-2130 days (2.6-5.8 years); Human Cortex [13] | â–º Lower likelihood of recording neural activity compared to SIROF [13] | â–º Performance degradation observed over the long-term period [13] |
| Case Western Reserve University (CWRU) Spiral Nerve Cuff | Up to 3 years; Human Peripheral Nerve [29] | â–º Stable activation thresholds after ~20 weeks; variability comparable to muscle-based electrodes [29] | â–º No adverse functional effects; nerve conduction velocity remained in clinical range; selective activation maintained for 3 years [29] |
| Polyimide-based Flexible Electrodes | Up to 8 months; Non-Human Primate Cortex [7] | â–º Stable neural signals recorded for cursor control tasks [7] | â–º Glial sheath formation observed two weeks post-implantation, a common challenge for chronic interfaces [7] |
| Dexamethasone-coated Polyimide Electrodes | At least 2 months; Animal Model (Peripheral Nerve) [14] | â–º Functional performance improvement inferred from reduced bio-fouling (Note: Direct SNR requires in vivo validation) [14] | â–º Coating significantly reduces immune response and scar tissue formation; maintains biocompatibility and mechanical integrity [14] |
Experimental Protocols for Chronic Assessment
To generate comparable data on electrode stability, researchers employ standardized experimental workflows. The protocols below detail the key methodologies for quantifying recording quality and linking it to physical degradation.
Protocol 1: Chronic In Vivo Electrophysiology and SNR Quantification
This protocol, adapted from long-term human trials, focuses on the functional assessment of recording quality [29] [13].
1. Electrode Implantation: Surgical implantation of electrode arrays (e.g., multi-contact cuffs for peripheral nerves or micro-arrays for cortex) into the target neural tissue [29]. 2. Chronic Data Collection: Repeated recording sessions over months to years. Neural signals are acquired using biopotential amplifiers. 3. Signal Processing and SNR Calculation: - Raw Signal Acquisition: Wide-band neural data (e.g., 0.1-7.5 kHz) is recorded. - Spike Detection & Alignment: Putative action potentials are detected and aligned. - Noise Estimation: The standard deviation of the background neural noise is calculated from the signal baseline, typically during periods without spiking activity. - SNR Calculation: For each sorted neuron, SNR is computed as the peak-to-peak amplitude of the average spike waveform divided by twice the standard deviation of the noise [13]. 4. Impedance Monitoring: Electrode impedance is regularly measured (e.g., at 1 kHz) to track changes in the electrode-tissue interface [13].
Protocol 2: Post-Explant Physical Degradation Correlation
This protocol establishes a direct link between physical electrode damage and its functional performance, a critical step for device improvement [13].
1. Functional Pre-Characterization: Prior to explant, the recording (SNR, noise, impedance) and stimulation capabilities of each electrode are thoroughly documented in vivo. 2. Explant and Cleaning: After device explantation, the electrode arrays are carefully cleaned to remove biological tissue. 3. High-Resolution Imaging: Scanning Electron Microscopy (SEM) is used to image all electrode sites at high magnification. 4. Quantitative Damage Metrics: Physical degradation (e.g., cracks, pockmarks, delamination) is quantified from the SEM micrographs. 5. Statistical Correlation: A statistical analysis is performed to correlate the quantitative physical damage metrics with the pre-explant functional performance data (e.g., SNR, impedance) [13].
The logical relationship between electrode degradation, the body's immune response, and the resulting decline in recording quality is summarized in the following diagram.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful chronic assessment relies on a suite of specialized materials and reagents designed to ensure device stability and biocompatibility.
Table 2: Key Reagents and Materials for Chronic Neural Interface Research
| Item | Function in Research | Specific Examples / Notes |
|---|---|---|
| SIROF (Sputtered Iridium Oxide Film) | Electrode coating material that provides high charge injection capacity and chronic recording stability, outperforming platinum in long-term human implants [13]. | - |
| Platinum (Pt) Foil/Electrodes | A traditional electrode material used as a benchmark for comparing the performance of new materials like SIROF [13]. | - |
| Polyimide | A flexible polymer used as a substrate and insulation layer for thin-film neural electrodes, offering good mechanical compatibility with soft neural tissues [28] [14]. | - |
| Dexamethasone | A potent anti-inflammatory drug covalently bound to electrode surfaces (e.g., polyimide) for localized, slow release to suppress the immune response and mitigate fibrotic encapsulation [14]. | Covalent binding strategies can extend release to over two months [14]. |
| Parylene-C | A common, conformal polymer used for encapsulating and insulating implantable electrodes, providing a moisture barrier and electrical insulation [28]. | Subject to long-term failure via delamination and water permeation [28]. |
| Liquid Crystal Polymer (LCP) | An emerging encapsulation material with exceptionally low water absorption rates, potentially offering superior long-term stability compared to polyimide and Parylene-C [28]. | - |
| Conductive Polymers (e.g., PEDOT:PSS) | Polymer coatings that can lower electrode impedance and improve charge transfer efficiency, thereby enhancing signal quality [28]. | - |
| Polyethylene Glycol (PEG) | A biocompatible polymer used as a temporary coating to stiffen flexible electrodes for implantation; it dissolves after insertion [7]. | - |
| Feretoside | Feretoside, CAS:27530-67-2, MF:C17H24O11, MW:404.4 g/mol | Chemical Reagent |
| 11-cis-Retinol | 11-cis-Retinol, CAS:22737-96-8, MF:C20H30O, MW:286.5 g/mol | Chemical Reagent |
The quantitative data and methodologies presented here underscore that SNR is more than a performance metric; it is a vital sign of an implantable electrode's health. Direct comparisons reveal that material choice, such as SIROF over platinum, and design innovations, like drug-eluting coatings, are pivotal to achieving chronic stability. As the field moves towards softer, more compliant interfaces, the standardized experimental protocols and rigorous correlation of electrical performance with physical integrity will be indispensable for translating promising laboratory prototypes into reliable clinical solutions.
Scanning Electron Microscopy (SEM) for Post-Explant Physical Damage Analysis
Scanning Electron Microscopy (SEM) has established itself as an indispensable tool in the field of implantable bioelectronics for quantifying physical degradation of explained neural electrodes. As clinical trials for brain-computer interfaces (BCIs) extend over multiple years, understanding the failure mechanisms of chronically implanted devices becomes paramount for improving their functional longevity [41]. SEM provides nanometer-scale resolution imaging capabilities that are crucial for correlating observed physical damage with electrochemical performance metrics recorded in vivo.
The clinical viability of intracortical microelectrode arrays depends on overcoming both biological and material challenges to ensure a long-term stable connection for neural recording and stimulation [13]. SEM-based analysis directly addresses this need by enabling researchers to systematically categorize and quantify damage modes that develop during chronic implantation, from metal corrosion and insulation delamination to silicon substrate degradation [41] [42]. This guide examines the application of SEM for post-explant analysis, comparing its capabilities with alternative imaging modalities, and contextualizing its role within a comprehensive chronic stability assessment framework for implantable electrodes.
Experimental Protocols for SEM Analysis of Explanted Electrodes
Sample Preparation and Imaging Parameters
Standardized protocols for SEM analysis of explanted neural electrodes begin with careful extraction and preservation of the device-tissue interface. Following explantation, arrays are typically fixed in glutaraldehyde or formaldehyde solutions to preserve adherent biological material, then dehydrated using graded ethanol series or critical point drying to minimize structural artifacts [42]. For conductive imaging, samples may be sputter-coated with a thin layer of gold or platinum to reduce charging effects, though uncoated samples can also be imaged using variable pressure SEM modes to examine native surface properties.
Imaging parameters vary depending on the analysis goals. For overview assessment of entire arrays, low magnification (50-500x) provides spatial context about damage distribution across electrode regions. High-magnification imaging (1,000-10,000x) enables detailed inspection of individual electrode tips for micro-scale degradation features such as cracking, pitting, or delamination [41]. Accelerating voltages typically range from 5-20 kV, with lower voltages reducing potential sample damage while providing enhanced surface detail.
Multi-Parameter Damage Rating System
Comprehensive SEM analysis employs standardized rating systems to quantify physical degradation across multiple dimensions. Based on studies of electrodes implanted for 956-2246 days in human participants, the following five metrics are typically assessed by expert raters reviewing electron micrographs [41]:
- Metal loss at electrode tip: Quantified as percentage area reduction of conductive surface
- Separation between silicon shank and tip metal: Measured in micrometers at interface
- Tissue adherence or biomaterial deposition: Categorized as none, mild (<25% coverage), moderate (25-75%), or severe (>75%)
- Damage to shank insulation: Rated based on crack density and delamination extent
- Silicone shaft integrity: Assessed for mechanical deformation or degradation
This multi-parameter approach enables systematic correlation between physical damage and functional performance metrics such as signal-to-noise ratio, impedance, and stimulation capability.
Comparative Performance: SEM Versus Alternative Modalities
Technical Capabilities and Limitations
| Imaging Modality | Resolution Limit | Sample Preparation | Key Strengths | Primary Limitations |
|---|---|---|---|---|
| Scanning Electron Microscopy (SEM) | ~1 nm [43] | Dehydration, conductive coating (often required) | Exceptional surface detail, elemental analysis capability | Vacuum environment, potential sample damage, specialized equipment |
| Digital Image Stacking | ~1 μm [43] | Minimal (no coating required) | Non-destructive, accessible, cost-effective | Lower resolution than SEM, surface analysis only |
| Micro-Computed Tomography (Micro-CT) | ~1 μm [43] | Minimal (may require fixation) | 3D volumetric data, non-destructive | Limited surface detail, lower resolution than SEM |
| Confocal Microscopy | ~200 nm | Fluorescent labeling often required | 3D optical sectioning, live cell compatible | Limited penetration depth, requires transparent samples |
Application-Specific Effectiveness
For post-explant analysis of neural electrodes, SEM demonstrates particular advantages in characterizing nanoscale surface degradation. Studies of Utah arrays explanted from human cortex after multi-year implantation revealed distinctive degradation patterns, including "pockmarked" versus "cracked" electrode morphologies that correlated with stimulation history [41]. These subtle features, often critical for understanding failure mechanisms, frequently fall below the resolution threshold of optical techniques.
Digital image stacking has emerged as a promising alternative for damage assessment, particularly in clinical or resource-limited settings. This technique combines multiple images captured at different focal lengths to create composite images with enhanced depth of field and resolution, capable of detecting microcracks, fissures, and abrasive wear on instrument surfaces [43]. While unable to match SEM's nanometer-scale resolution, this approach provides sufficient detail for many practical assessments without requiring complex sample preparation or expensive specialized equipment.
Signaling Pathways in Electrode Degradation and Analysis
The physical degradation of implanted electrodes occurs through complex biotic-abiotic interactions that SEM analysis helps elucidate. The following diagram illustrates the key pathways linking implantation to functional failure and the role of SEM in characterizing resulting damage:
Pathways of Electrode Degradation and SEM Analysis. Implantation triggers inflammatory responses leading to material degradation and glial scarring, which SEM characterizes through specific damage modes. Diagram highlights how SEM analysis identifies key failure mechanisms.
Quantitative Damage Assessment: SEM Reveals Material-Specific Degradation
Comparative Electrode Performance Metrics
Analysis of 980 microelectrodes from Neuroport arrays explanted from human participants after 956-2246 days of implantation revealed significant differences in degradation patterns between electrode materials [41]:
| Electrode Material | Recording Likelihood (SNR) | Primary Damage Modes | Impedance Correlation | Stimulation Impact |
|---|---|---|---|---|
| Platinum (Pt) | Lower | Metal loss, insulation cracking | Weak correlation with damage | Not significant |
| Sputtered Iridium Oxide (SIROF) | 2x higher than Pt [41] | Pockmarked degradation, silicon erosion | Significant correlation with all damage metrics [41] | New degradation type observed |
Despite showing greater physical degradation, SIROF electrodes maintained significantly better functional performance, being twice as likely to record neural activity than Pt electrodes at the time of explant [41]. For SIROF electrodes, 1 kHz impedance measured in vivo prior to explant significantly correlated with all physical damage metrics, recording quality, and stimulation performance, suggesting impedance serves as a reliable indicator of in vivo degradation for this material [41].
Temporal Progression of Damage
Long-term studies in non-human primates demonstrate progressive material degradation over implantation periods extending to 1051 days [42]. SEM analysis reveals:
- Platinum corrosion begins as surface roughening and progresses to significant metal loss
- Parylene-C insulation develops cracks and delaminates from silicon substrate
- Silicon shanks exhibit erosion, particularly at the metal-silicon interface
- Silicone elastomer encapsulation shows delamination from array edges
This degradation correlates with functional declines, including reduced signal amplitude, increased noise, and diminished viable channels over time [42]. Histological analysis confirms that material defects become more prevalent with extended implantation duration, with substantial tissue encapsulation often growing into defects in both platinum and parylene components.
The Scientist's Toolkit: Essential Reagents and Materials
| Research Reagent/Material | Function in SEM Analysis | Application Notes |
|---|---|---|
| Glutaraldehyde Solution | Tissue fixation for biological adherents | Preserves cellular material on explanted electrodes |
| Critical Point Dryer | Sample dehydration without structural collapse | Alternative to graded ethanol series for delicate samples |
| Gold/Palladium Target | Sputter coating for conductive layers | Reduces charging effects during SEM imaging |
| Conductive Adhesive Tape | Sample mounting for charge dissipation | Ensures proper grounding to prevent image artifacts |
| Standardized Damage Rating Protocol | Quantitative assessment framework | Enables systematic comparison across studies [41] |
| Taxezopidine L | Taxezopidine L, CAS:219749-76-5, MF:C39H46O15, MW:754.8 g/mol | Chemical Reagent |
| Cefetamet | Cefetamet, CAS:65052-63-3, MF:C14H15N5O5S2, MW:397.4 g/mol | Chemical Reagent |
Emerging Innovations and Future Directions
Advanced Surface Modification Strategies
Recent research focuses on developing novel coatings to mitigate degradation mechanisms identified through SEM analysis. One promising approach involves covalent binding of the anti-inflammatory drug dexamethasone to polyimide-based neural implants, creating a slow-release system that maintains therapeutic concentrations at the implant site for at least two months [14]. Biological tests demonstrate that this surface modification reduces inflammation-related signals in immune cells while maintaining material biocompatibility and mechanical integrity.
Animal studies further confirm that dexamethasone-releasing implants significantly reduce immune reactions and scar tissue formation around the device [14]. This innovation directly addresses the biotic component of electrode degradation previously characterized through SEM analysis of explanted devices, offering potential for extended functional lifespan of neural prostheses.
Alternative Assessment Methodologies
While SEM remains the gold standard for high-resolution damage characterization, emerging techniques offer complementary capabilities. Digital image stacking systems leverage high-resolution digital photography and advanced image processing to create composite images with enhanced depth of field [43]. This approach provides a practical, efficient, and objective method for assessing instrument morphology without requiring specialized SEM equipment, though at reduced resolution.
For three-dimensional analysis of internal structures without destructive sectioning, micro-computed tomography (micro-CT) provides volumetric data at approximately 1 μm resolution [43]. This technique is particularly valuable for examining structural integrity beneath surfaces and detecting internal defects not visible with surface-imaging techniques like SEM.
Scanning Electron Microscopy provides unparalleled capability for nanoscale characterization of physical damage in explanted neural electrodes, making it an indispensable tool in chronic stability assessment research. The high-resolution imaging and analytical capabilities of SEM have revealed critical material-specific degradation patterns that directly impact electrode performance, guiding the development of more durable neural interface technologies. While emerging alternatives like digital image stacking offer practical advantages for certain applications, SEM remains the benchmark for comprehensive failure analysis in implantable bioelectronics. As the field progresses toward clinical implementation of brain-computer interfaces spanning decades of patient use, SEM will continue to provide essential insights guiding electrode design, material selection, and surface modification strategies aimed at achieving unprecedented device longevity.
Histological Techniques for Assessing Tissue Integration and Immune Response
The chronic stability of implantable electrodes is a pivotal concern in the development of clinically viable brain-machine interfaces (BMIs) and neuroprosthetics. The functional longevity of these devices is intrinsically linked to the biological response they elicit upon implantation. A complex cascade of tissue integration and immune reactions ultimately determines the electrode's performance and operational lifespan. Consequently, histological techniques for assessing these responses form the cornerstone of chronic stability assessment in neural engineering research. This guide provides a comparative analysis of the key histological methods used to evaluate tissue integration and immune response to implantable electrodes, offering detailed experimental protocols and data interpretation frameworks essential for researchers and drug development professionals.
Core Histological Assessment Modalities for Neural Interfaces
The evaluation of the tissue-electrode interface relies on a multifaceted histological approach, designed to characterize the multifaceted foreign body response. The following table summarizes the primary assessment goals and the corresponding analytical techniques.
Table 1: Core Histological Assessment Modalities for Neural Interfaces
| Assessment Goal | Key Histological & Imaging Techniques | Primary Readouts |
|---|---|---|
| Tissue Architecture & Cellular Density | Hematoxylin & Eosin (H&E) Staining; Nissl Staining | Cortical thickness; neuronal density and distribution; general cytoarchitecture [44] |
| Glial Scar Formation | Immunohistochemistry (IHC) for GFAP; Iba1/Iba1 | Astrocyte activation and hypertrophy (astrogliosis); microglial activation and density [44] [45] |
| Foreign Body Response & Fibrous Encapsulation | Masson's Trichrome Staining; IHC for CD68/ED1 | Collagenous tissue encapsulation; presence of macrophages and foreign body giant cells [44] [45] |
| Neuronal Health & Loss | NeuN Immunohistochemistry; Fluoro-Jade Staining | Neuronal density and nuclear integrity; identification of degenerating neurons [44] |
| Vascular Integrity & Blood-Brain Barrier Disruption | IHC for Laminin or Collagen IV; Evans Blue Extravasation | Vascular density and morphology; assessment of barrier leakage [45] |
The interplay between these assessment modalities can be visualized in the following experimental workflow, which outlines the key steps from implantation to histological analysis.
Comparative Analysis of Key Histological Techniques
A systematic comparison of techniques enables researchers to select the optimal methodological combination. The following table details the applications, advantages, and limitations of each major approach.
Table 2: Comparative Analysis of Key Histological Techniques for Electrode Evaluation
| Technique | Primary Applications | Key Advantages | Inherent Limitations |
|---|---|---|---|
| H&E Staining | General tissue morphology and structure; preliminary assessment of inflammation and damage [44] | Standard, cost-effective; provides overview of cytoarchitecture | Limited specificity; cannot identify specific cell phenotypes |
| Nissl Staining | Identification of neuronal cell bodies; assessment of neuronal density and cortical laminar organization [44] | Highlights all neuronal somata; simple protocol | Does not distinguish neuronal health or subtypes |
| Immuno-histochemistry (IHC) | Cell-specific identification (neurons, astrocytes, microglia); assessment of activation states (e.g., reactive astrocytes) [44] [45] | High specificity and versatility; allows phenotypic characterization | Antibody-dependent variability; requires optimization; semi-quantitative without rigorous controls |
| Masson's Trichrome | Visualization of collagen deposition and fibrous encapsulation around the implant [44] | Clearly distinguishes collagen (blue/green) from muscle/cytoplasm (red) | Does not identify the cellular source of collagen |
| Multiplex Fluorescence IHC | Spatial analysis of multiple cell types and biomarkers simultaneously within the same tissue section | Unravels complex cell-cell interactions; maximizes data from scarce samples | Complex workflow; expensive; requires specialized imaging and analysis |
The foreign body response to an implanted electrode is a dynamic process involving coordinated signaling between various immune and neural cells. The following pathway diagram illustrates the key cellular players and their interactions.
Detailed Experimental Protocols for Key Assays
Protocol for Qualitative and Quantitative Analysis of Glial Scar
This protocol assesses astrocyte and microglial activation, key components of the chronic immune response [44] [45].
- Tissue Preparation: Perfuse-fix the animal with 4% paraformaldehyde (PFA) in 0.1M phosphate buffer. Extract the brain, post-fix for 24 hours in the same fixative, and section the tissue surrounding the implant site coronally at a thickness of 20-40 μm using a vibrating microtome.
- Immunohistochemistry:
- Blocking: Incubate free-floating sections in a blocking solution (e.g., 10% normal goat serum with 0.3% Triton X-100) for 1 hour at room temperature.
- Primary Antibodies: Incubate sections with the following primary antibodies diluted in blocking solution for 24-48 hours at 4°C:
- Anti-GFAP (Rabbit polyclonal, 1:1000) to label astrocytes.
- Anti-Iba1 (Goat polyclonal, 1:500) to label microglia/macrophages.
- Secondary Antibodies: Incubate with species-appropriate fluorescent secondary antibodies (e.g., Alexa Fluor 488, 594) for 2 hours at room temperature.
- Counterstaining and Mounting: Counterstain nuclei with DAPI (1:5000) and mount sections on glass slides.
- Image Acquisition and Analysis:
- Acquire high-resolution images using a confocal or epifluorescence microscope at standardized distances from the electrode track (e.g., 0-50 μm, 50-100 μm, 100-200 μm).
- Quantitative Analysis:
- GFAP+ Area Fraction: Threshold and binarize images to calculate the percentage of area occupied by GFAP+ signal, indicating astrogliosis.
- Iba1+ Cell Density: Count the number of Iba1+ cells per unit area.
- Microglial Morphology: Classify Iba1+ cells as "ramified" (resting) or "amoeboid" (activated) based on process length and cell body roundness.
Protocol for Assessing Neuronal Density and Fibrous Encapsulation
This protocol evaluates the ultimate impact of the implant on neuronal survival and the extent of the fibrotic capsule [44].
- Tissue Processing and Sectioning: Process fixed tissue through a graded ethanol series, clear in xylene, and embed in paraffin wax. Section serially at 5-8 μm thickness and mount on slides.
- Staining Procedures:
- NeuN Immunohistochemistry: Perform IHC as described in Section 4.1 using an anti-NeuN antibody to label mature neuronal nuclei. Use a bright-field secondary detection system (e.g., DAB).
- Masson's Trichrome Staining: Follow standard protocol: stain nuclei with Weigert's iron hematoxylin, cytoplasm with Biebrich scarlet-acid fuchsin, and collagen fibers with aniline blue.
- Quantitative Analysis:
- Neuronal Density: Count NeuN+ neurons within fixed-width radial bins (e.g., 50 μm increments) extending from the electrode track interface outward to 500 μm. Normalize counts to cells/mm² for each bin.
- Fibrous Capsule Thickness: Using Trichrome-stained sections, measure the thickness of the collagen-rich (blue-stained) capsule surrounding the explanted electrode or the implant track at multiple points to calculate an average.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table catalogues critical reagents and their functions for successfully executing the histological assessments described in this guide.
Table 3: Essential Research Reagents for Histological Assessment of Neural Interfaces
| Reagent / Material | Function / Application | Specific Example |
|---|---|---|
| Primary Antibodies | Cell-type specific antigen labeling for IHC | Anti-GFAP (astrocytes), Anti-Iba1 (microglia), Anti-NeuN (neurons), Anti-CD68/ED1 (macrophages) [44] [45] |
| Fluorescent Secondary Antibodies | Detection of primary antibodies for fluorescence microscopy | Alexa Fluor 488, 568, or 647 conjugates for high sensitivity and multiplexing |
| Histological Stains | General and specific tissue component staining | Hematoxylin & Eosin (nuclei/cytoplasm), Masson's Trichrome (collagen) [44] [46] |
| Perfusion & Fixation Solutions | Tissue preservation and structural integrity | 4% Paraformaldehyde (PFA) in 0.1M Phosphate Buffer [44] |
| Tissue Embedding Media | Support for thin-sectioning | Paraffin wax; Optimal Cutting Temperature (O.C.T.) compound for frozen sections |
| Mounting Media | Preserving and mounting coverslips | Aqueous mounting media for fluorescence; permanent mounting media for bright-field |
| Mecoprop-d3 | Mecoprop-d3|Deuterated Herbicide Standard|RUO | Mecoprop-d3 is an internal standard for analytical research of herbicide levels in environmental and agricultural studies. For Research Use Only. Not for human use. |
| Angeloylisogomisin O | Angeloylisogomisin O, CAS:83916-76-1, MF:C23H28O7, MW:416.5 g/mol | Chemical Reagent |
The rigorous histological evaluation of tissue integration and immune response is non-negotiable for advancing the field of chronic implantable electrodes. While H&E and Nissl stains provide a foundational view of tissue architecture, advanced techniques like IHC are indispensable for deconstructing the complex cellular response. The experimental data and protocols compiled in this guide demonstrate that a combinatorial approach—quantifying neuronal loss, glial activation, and fibrous encapsulation—provides the most comprehensive assessment of biocompatibility and chronic stability. As electrode technology evolves towards softer, smaller, and more sophisticated designs, these histological techniques will continue to be the benchmark for validating their safety and efficacy, ultimately accelerating the translation of high-performance neural interfaces from the laboratory to the clinic.
Accelerated Aging Models for Predicting Long-Term Performance
The development of chronically stable implantable neural interfaces represents a frontier in modern bioelectronics, with applications ranging from the treatment of Parkinson's disease and drug-resistant epilepsy to brain-computer interfaces (BCIs) that restore communication and motor control [47] [16]. A paramount challenge in this field is ensuring the long-term performance and functional integrity of these devices over implantation periods that can span years to decades. Unlike acute implants, chronic interfaces face a complex interplay of technological and biological failure modes, including material degradation, mechanical failure, and the foreign body reaction (FBR)—the immune system's response to implanted materials [47] [16].
To preemptively evaluate device longevity without waiting for real-time data over many years, researchers rely on accelerated aging models. These predictive methodologies subject devices to elevated stress conditions, most often increased temperature, to simulate the effects of long-term aging in a drastically reduced timeframe. The data generated is crucial for guiding device design, informing implantation strategies, and establishing provisional shelf-life and functional longevity, ultimately ensuring safety and efficacy for clinical translation [48]. This guide provides a comparative analysis of accelerated aging methodologies employed for implantable electrodes, framing them within the broader research objective of achieving chronic stability.
Accelerated Aging Fundamentals and Protocols
Core Principles and Standardized Protocols
Accelerated aging operates on the fundamental principle that the chemical reactions responsible for material degradation follow the Arrhenius reaction rate theory. This model establishes a quantitative relationship between temperature and the rate of a chemical process, stating that a 10°C increase in temperature typically results in a two-fold increase in the rate of aging [48]. This relationship allows researchers to calculate equivalent aging times.
The most widely recognized standard for this methodology is ASTM F1980. The standard calculation for the accelerated aging time (AAT) is as follows [48]:
AAT = (Real Time Aging Period Desired) / (Accelerated Aging Factor)
Where the Accelerated Aging Factor (Qâ‚â‚€) is calculated as:
Qâ‚â‚€ = e^(ln(AF) / (T_AA - T_RT)/10)
In this equation, T_AA is the accelerated aging temperature, T_RT is the real-time storage temperature, and AF is the aging factor, typically 2.0 [48].
- Key Experimental Protocol (ASTM F1980):
- Objective: To determine the provisional shelf-life of a packaged sterile medical device system.
- Procedure: Samples are subjected to elevated temperatures and controlled relative humidity (typically between 45% and 55% RH) for a calculated period. For a device with a desired shelf life of 5 years stored at 25°C, testing at 55°C would require approximately 3 months to simulate 5 years of real-time aging [48].
- Parallel Real-Time Aging: Regulatory guidelines, such as those from the International Council for Harmonisation (ICH), mandate that accelerated data must be validated with concurrent real-time aging studies conducted at ambient conditions (e.g., 25°C ± 2°C / 60% RH ± 5% RH) [48] [49]. This real-time data ultimately confirms the accuracy of the predictions.
Application-Specific Aging Models for Neural Interfaces
Beyond package shelf-life, accelerated models are critical for assessing the in vivo performance and stability of the electrode-tissue interface itself. These models simulate the hars electrochemical and mechanical environment of the body.
Electrochemical Stability Testing:
- Objective: To evaluate the longevity of electrode materials and their coatings under repeated electrical stimulation.
- Protocol: Electrodes are subjected to continuous electrical pulsing in a simulated physiological environment (e.g., phosphate-buffered saline at 37°C). Parameters such as impedance, charge storage capacity, and charge injection capacity are monitored over millions of cycles. For instance, one study noted that conventional PEDOT:PSS coatings are prone to delamination under such stress, whereas modified PEDOT:PSS-based eutectogels demonstrated superior stability, maintaining over three-fold improvements in impedance and charge injection capacity after testing [50].
Mechanical Fatigue and Micromotion Testing:
- Objective: To assess the ability of flexible electrodes and their interconnects to withstand chronic brain micromotion.
- Protocol: Devices are cyclically flexed or exposed to mechanical agitation for thousands to millions of cycles while monitoring for electrical discontinuities, cracks, or delamination. Finite element analysis (FEA) models, as used to characterize polyimide-based ultrathin electrodes, can complement this by simulating stresses and predicting potential mechanical failure points [51].
The workflow below illustrates how these different accelerated aging protocols are integrated into the development pipeline for implantable electrodes.
Comparative Analysis of Models and Materials
The effectiveness of an accelerated aging model is judged by its correlation with real-world, long-term performance data. The table below summarizes key performance metrics for different electrode technologies and the aging models used to predict their longevity.
Table 1: Comparison of Neural Electrode Technologies and Associated Aging Models
| Electrode Technology / Model | Key Performance Metrics | Aging Model / Stressor Used | Predicted/Observed Long-Term Outcome | Supporting Experimental Data |
|---|---|---|---|---|
| Polyimide-based Flexible Electrodes [51] | Von Mises Strain (ε98), Von Mises Stress (σ98) | Finite Element Analysis (FEA) of insertion & steady-state acceleration | Excellent mechanical stability in vivo; ε98 < 0.3% during acceleration. | FEA simulation showed minimal tissue strain (ε98 < 0.3%) under chronic acceleration forces. |
| PEDOT:PSS/DES Eutectogel [50] | Electrode Impedance, Charge Injection Capacity (CIC) | In vitro electrochemical aging (continuous pulsing) | >3x improvement in CIC and lower impedance vs. conventional PEDOT:PSS. | Thicker (800 nm) coatings enabled by DES; stable performance in acute in vivo rat tests. |
| Conventional PEDOT:PSS [50] | Electrode Impedance, CIC, Coating Delamination | In vitro electrochemical aging and mechanical agitation | Prone to delamination under stress; lower CIC. | Thin films (80-300 nm) are mechanically fragile, limiting long-term stability. |
| Silicon-based Probes [47] [16] | Recording Signal-to-Noise, Single-Unit Yield | Chronic in vivo implantation (real-time) | Gradual performance decay over months/years due to FBR. | Foreign Body Reaction (FBR) leads to glial scarring and neuronal loss. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of accelerated aging studies and the development of robust neural interfaces rely on a suite of specialized reagents and materials. The following table details key items central to this field of research.
Table 2: Key Research Reagents and Materials for Neural Interface Development
| Item Name | Function / Application | Specific Example / Rationale |
|---|---|---|
| PEDOT:PSS/DES Eutectogel [50] | Conductive electrode coating; enhances charge injection and mechanical robustness. | A mixture of PEDOT:PSS with a deep eutectic solvent (ChCl:LAC) and crosslinker (GOPS). Enables thick, stable films for low-impedance interfaces. |
| Polyimide [51] [16] | Flexible substrate and insulation for thin-film neural probes. | Biocompatible polymer with excellent electrical insulation and mechanical flexibility, reducing mismatch with brain tissue. |
| ASTM F1980-Compliant Chamber [48] | Provides controlled, elevated temperature and humidity for accelerated package aging. | Essential for standardized shelf-life validation of the sterile barrier system. |
| Phosphate Buffered Saline (PBS) | Simulated physiological solution for in vitro electrochemical testing. | Provides ionic environment to mimic body fluids for testing electrode stability and performance. |
| Finite Element Analysis (FEA) Software [51] | Models biomechanical interactions to predict tissue strain and potential damage. | Software like ANSYS is used to simulate electrode insertion and chronic micromotion, guiding safe design. |
| Uncarine A | Uncarine A, CAS:6899-73-6, MF:C21H24N2O4, MW:368.4 g/mol | Chemical Reagent |
| Cephalocyclidin A | Cephalocyclidin A, MF:C17H19NO5, MW:317.34 g/mol | Chemical Reagent |
Accelerated aging models, from standardized package testing to sophisticated electrochemical and mechanical simulations, are indispensable tools for de-risking the development of implantable neural electrodes. The comparative data presented in this guide underscores a clear trend: material and mechanical compatibility are paramount for chronic stability. Technologies that minimize the physical mismatch with neural tissue, such as ultra-flexible polyimide probes, and those that enhance the electrochemical interface, like novel PEDOT:PSS eutectogels, consistently demonstrate superior predicted and actual long-term performance in models [51] [50].
The ultimate validation of any accelerated model, however, remains its correlation with real-time aging data, both in vitro and from chronic in vivo studies [48]. As the field advances towards higher-density CMOS-based probes and clinical-grade BCIs, the refinement of these predictive models will be critical. They will enable researchers to efficiently screen next-generation materials and designs, accelerating the translation of safe and effective bioelectronic therapies that can reliably function for a lifetime.
Engineering Resilience: Material and Design Strategies for Enhanced Chronic Stability
The pursuit of stable, long-term neural interfaces represents a central challenge in neurotechnology, with applications ranging from fundamental neuroscience research to therapeutic brain-computer interfaces (BCIs) and treatments for neurological disorders. A primary obstacle to chronic stability is the profound mechanical mismatch that exists between conventional implantable electrodes and the soft, dynamic environment of neural tissue [11] [52]. While biological neural tissues, such as the brain, exhibit a Young's modulus in the range of 1–10 kPa, traditional electrode materials like silicon (~180 GPa) and platinum (~100 GPa) are orders of magnitude stiffer [7] [3]. This mismatch initiates a cascade of biological responses, including chronic inflammation, foreign body response (FBR), glial scar formation, and eventual neuronal death, which collectively degrade signal quality and lead to device failure over time [3] [52].
Flexible and soft materials have emerged as a transformative solution to this challenge. By engineering neural interfaces with mechanical properties that closely mimic those of native neural tissue, researchers aim to minimize tissue damage during implantation, reduce micromotion-induced irritation, and achieve seamless bio-integration [9] [53]. This guide provides a comparative analysis of the primary classes of soft materials used in neural interfaces, evaluates their performance against traditional alternatives, and details the experimental methodologies essential for assessing their efficacy and chronic stability.
Comparative Analysis of Material Strategies
The development of soft neural interfaces relies on two complementary approaches: the use of intrinsically soft materials and innovative structural designs that confer flexibility to otherwise rigid materials. The table below summarizes the key properties and performance metrics of prominent material categories.
Table 1: Comparative Analysis of Materials for Flexible Neural Interfaces
| Material Category | Specific Examples | Young's Modulus | Key Advantages | Documented Limitations | Chronic Performance Evidence |
|---|---|---|---|---|---|
| Polymeric Substrates | Polyimide (PI), SU-8, Parylene-C, PDMS | ~1–3 GPa [52] | Biocompatibility, established microfabrication processes, excellent flexibility [52] | Limited hermeticity, potential for delamination in moist environments [9] | Stable single-unit recordings in rat motor cortex for up to 8 months [7] |
| Conductive Polymers | PEDOT:PSS, PPy, PNAi | kPa – MPa range [53] | Low impedance, mixed ionic-electronic conductivity, can be functionalized [54] [53] | Long-term electrochemical stability under continuous stimulation can be challenging [53] | NeuroGrid arrays recorded single-cell action potentials from rat brain surface for 10 days [52] |
| Hydrogels & Elastomers | Alginate, PEG, hyaluronic acid; Ecoflex | ~1–100 kPa [53] | Tissue-like modulus, high water content, can be bioadhesive and self-healing [53] | Low electrical conductivity, difficult to pattern, may swell [53] | e-dura implants in rat spinal cord showed minimal glial activation after 6 weeks [52] |
| Carbon-Based Nanomaterials | Graphene, Carbon Nanotubes (CNTs) | Flexible and stretchable in composite forms [54] | High electrical conductivity, large surface area, excellent sensitivity for neurochemical sensing [54] | Complex fabrication, potential biocompatibility concerns requiring surface modification [54] [53] | Graphene fiber microelectrodes demonstrated superior dopamine sensitivity and antifouling properties [54] |
| Liquid Metal Composites | EGaIn (Gallium alloys) | Highly deformable [55] | Extreme stretchability (>1200%), maintains conductivity under strain [55] | Patterning resolution and scalability challenges [55] | Balloon catheters with microelectrode arrays provided high-resolution cardiac maps in animal tests [55] |
| Ultrathin Metallic Films | Au, Pt on polymeric supports | Effectively very low bending stiffness [52] | High conductivity, compatible with standard lithography [52] | Susceptible to fatigue and cracking at high strain cycles [9] | Neuron-like Pt electrodes (bending stiffness ~10â»Â¹â¶ N·m²) integrated with minimal FBR [52] |
The relationship between material properties, the body's response, and the ultimate functional outcome of the implant is complex. The following diagram illustrates this critical pathway, from the initial implantation trigger to the final recording stability.
Diagram 1: Pathway from mechanical mismatch to recording failure, and the mitigating role of soft materials.
Experimental Protocols for Assessing Chronic Stability
Evaluating the performance and longevity of flexible neural interfaces requires a multi-faceted approach, integrating functional, biological, and material analyses. The following section details key experimental methodologies cited in recent literature.
Electrochemical Impedance Spectroscopy (EIS)
Objective: To monitor the stability of the electrode-electrolyte interface and detect changes related to material degradation or biological fouling. Protocol:
- Setup: Immerse the fabricated neural probe in a phosphate-buffered saline (PBS) solution at 37°C to simulate physiological conditions [13].
- Measurement: Apply a small AC voltage (typically 10 mV) across a frequency range (e.g., 1 Hz to 100 kHz) using a potentiostat.
- Chronic Tracking: In chronic in vivo studies, measure impedance at a standard frequency (e.g., 1 kHz) at regular intervals post-implantation [13].
- Data Correlation: Correlate impedance changes with post-explant physical analysis of the electrodes. A significant rise in impedance at 1 kHz has been strongly correlated with physical damage to electrode materials like Sputtered Iridium Oxide Film (SIROF) and is a reliable indicator of in vivo degradation [13].
In Vivo Electrophysiological Recording
Objective: To quantify the functional signal quality and stability of the neural interface over time. Protocol:
- Implantation: Surgically implant the flexible electrode array into the target brain region (e.g., motor cortex) of an animal model (e.g., rat, non-human primate) using an appropriate guidance shuttle, such as a temporary tungsten wire or biodegradable polymer [7].
- Signal Acquisition: Record neural signals (both local field potentials and single-unit activity) periodically over weeks to months.
- Signal Analysis: Calculate the Signal-to-Noise Ratio (SNR). This involves isolating the peak-to-peak voltage of neuronal action potentials and dividing it by the root-mean-square of the background noise. A higher SNR indicates better recording quality.
- Performance Metric: Studies have shown that flexible electrodes based on soft materials like polyimide can maintain a stable SNR, enabling the tracking of individual neurons for over eight months [7]. Furthermore, despite greater physical degradation, SIROF electrodes were twice as likely to record neural activity than Platinum (Pt) electrodes, as measured by SNR [13].
Histological and Immunohistochemical Analysis
Objective: To visualize and quantify the biological tissue response, including inflammation and glial scar formation, around the implanted device. Protocol:
- Perfusion and Sectioning: At the endpoint of the study, transcardially perfuse the animal with paraformaldehyde. Extract and section the brain for histological analysis [3].
- Staining: Immunostain the brain sections with specific antibodies:
- Glial Fibrillary Acidic Protein (GFAP): To label reactive astrocytes forming the glial scar [3].
- Ionized Calcium-Binding Adapter Molecule 1 (Iba1): To identify activated microglia, the primary immune cells of the central nervous system [3].
- Neuronal Nuclei (NeuN): To quantify neuronal density and survival in the vicinity of the implant.
- Quantification: Use fluorescence microscopy and image analysis software to measure the intensity and thickness of the GFAP-positive scar barrier and the density of neurons within a defined radius (e.g., 100 µm) from the implant track. Reduced glial scarring and higher neuronal survival are hallmarks of improved biocompatibility with soft materials [3] [52].
Post-Explant Material Characterization
Objective: To directly inspect and quantify physical degradation of the explanted electrodes. Protocol:
- Explantation: Carefully remove the neural electrode array after long-term implantation (in humans, studies have analyzed devices implanted for 956–2130 days) [13].
- Imaging: Use Scanning Electron Microscopy (SEM) to image the electrode surfaces at high resolution.
- Damage Quantification: Systematically categorize and quantify physical damage, such as cracks, delamination, pockmarks, or erosion of the electrode material and its encapsulation [13].
- Functional Correlation: Correlate the physical degradation metrics with the in vivo performance data (impedance, SNR, stimulation capability) obtained prior to explant. This provides a direct link between material integrity and device functionality [13].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research and development in this field depend on a suite of specialized materials and reagents. The following table details key components for fabricating and testing flexible neural interfaces.
Table 2: Essential Research Reagents and Materials for Flexible Neural Interface Development
| Item Name | Function/Application | Specific Examples & Notes |
|---|---|---|
| Soft Substrate Materials | Provides the structural backbone of the flexible device. | Polyimide [7], SU-8 [52], Polydimethylsiloxane (PDMS) [53] [52]; Chosen for flexibility and biocompatibility. |
| Conductive Materials | Forms the electrodes and interconnects for signal transduction. | PEDOT:PSS [53] [52], Liquid Metals (e.g., EGaIn) [55], Carbon Nanotubes/Graphene [54] [53]; Selected for conductivity and mechanical compliance. |
| Biodegradable Polymers | For transient electronics or temporary implantation shuttles. | Polycaprolactone (PCL), Polylactic-glycolic acid (PLGA) [53]; Degradation rate must match the application's timeframe. |
| Rigid Implantation Shuttles | Provides temporary stiffness for precise surgical insertion of flexible probes. | Tungsten wires [7], SU-8 shanks [7], biodegradable silk [3]; Critical for deploying ultra-soft devices. |
| Immunostaining Antibodies | To label and quantify the tissue's immune response to the implant. | Anti-GFAP (astrocytes) [3], Anti-Iba1 (microglia) [3], Anti-NeuN (neurons); Essential for histology protocols. |
| Electrochemical Cell Setup | For in vitro characterization of electrode performance. | Potentiostat, Phosphate-Buffered Saline (PBS) or artificial cerebrospinal fluid (aCSF) [13]; Used for EIS and cyclic voltammetry. |
| Biotin sodium | Biotin sodium, MF:C10H15N2NaO3S, MW:266.29 g/mol | Chemical Reagent |
The development of a high-performance, chronically stable neural interface is an iterative process that relies on the integration of material design, fabrication, and rigorous validation. The workflow below outlines the key stages from concept to functional assessment.
Diagram 2: Integrated experimental workflow for developing and validating flexible neural interfaces.
The strategic application of flexible and soft materials is paramount for advancing the field of chronically stable implantable neural electrodes. By mitigating the mechanical mismatch at the tissue-device interface, these materials directly address the root cause of the foreign body response and glial scarring that plague traditional rigid implants. As evidenced by comparative data, materials such as conductive polymers, hydrogels, and ultrathin geometries have demonstrated superior ability to maintain high signal quality and biocompatibility over extended periods. Future progress hinges on the continued refinement of these material systems, the development of more robust and scalable fabrication techniques, and the deep integration of biological cues to create truly bio-integrative and "living" neural interfaces [52]. The experimental frameworks and comparative data provided in this guide serve as a foundation for researchers to objectively evaluate new material strategies and drive the development of next-generation, clinically viable neurotechnologies.
Surface Functionalization and Anti-inflammatory Drug Coatings for Controlled Release
The long-term success of implantable medical devices, from neural electrodes to orthopedic implants, is critically limited by the foreign body reaction (FBR), a complex immune response that often leads to fibrotic encapsulation and device failure [56] [7]. This FBR initiates with non-specific protein adsorption onto the implant surface, followed by an acute inflammatory phase characterized by the infiltration of immune cells, primarily monocytes, which differentiate into macrophages on the device surface [56]. Controlling this post-implantation inflammatory phase is paramount to mitigating the FBR and promoting successful device integration [56].
Surface functionalization with anti-inflammatory drug coatings represents a powerful strategy to modulate the host immune response locally at the implant-tissue interface. Unlike systemic drug administration, which may not achieve therapeutic local concentrations and can cause side effects, controlled release systems integrated into the implant surface deliver therapeutic agents precisely where needed [56] [57]. This approach is particularly crucial for chronic implants, such as neural interfaces, where long-term stability is essential for consistent performance [7] [28]. This guide provides a comparative analysis of leading coating technologies, their experimental assessment, and their role in enhancing the chronic stability of implantable systems.
Comparative Analysis of Coating Strategies
Various coating strategies have been developed to confer anti-inflammatory properties to implant surfaces. The following table compares the key characteristics of prominent approaches.
Table 1: Comparison of Anti-Inflammatory Coating Strategies for Implants
| Coating Strategy | Key Components/Agents | Mechanism of Action | Stability & Release Profile | Key Advantages | Reported Limitations |
|---|---|---|---|---|---|
| Zwitterionic Polymers [56] | MPC (2-methacryloyloxyethyl phosphorylcholine), SBMA ([2-(methacryloyloxy)ethyl]dimethyl-(3-sulfopropyl)ammonium hydroxide) | Creates a biomimetic, ultra-low fouling surface that resists protein adsorption; modulates macrophage phenotype to reduce pro-inflammatory cytokine release (IL-1β, IL-6, TNF-α) [56]. | Highly stable for up to 8 weeks in simulated physiological conditions; sustained anti-inflammatory effect [56]. | Superior stability, excellent biocompatibility, reduced risk of immune rejection, non-fouling [56]. | Chemical stability of PEEK makes surface modification challenging, often requires polydopamine adhesive layer [56]. |
| Polymer Films for Drug Delivery [57] | Biodegradable (e.g., PLGA, PCL) and non-biodegradable (e.g., PEG) polymers loaded with anti-inflammatory drugs (e.g., steroids, NSAIDs). | Provides a controlled release of encapsulated anti-inflammatory agents directly at the implant-tissue interface to suppress local inflammation [57]. | Tunable from days to months based on polymer composition, thickness, and degradation rate; potential for burst release [57]. | Versatile platform, tunable release kinetics, can be applied to various implant geometries using dip/spray coating [57]. | Potential for burst release, polymer degradation may affect mechanical properties, long-term effects of localized release require more study [57]. |
| Hybrid/Bioactive Coatings [58] | Polydopamine (PDA) base with integrated bioactive compounds (e.g., Vancomycin, Zoledronate). | Combultiple bioactivities: anti-inflammatory, antibacterial, and osteoinductive in a single coating [58]. | Demonstrated increased corrosion resistance (7x) for Mg alloys; sustained bioactive effect [58]. | Multifunctional, optimal wettability for cell adhesion, combines therapy with enhanced implant performance [58]. | Complex fabrication process; long-term stability in vivo requires further validation [58]. |
| Nanoparticle-based Systems [59] | Organic/Inorganic NPs (e.g., Liposomes, Gold, Silica) loaded with anti-inflammatory drugs (e.g., IL-1β inhibitors). | Utilizes enhanced permeability for targeted delivery; can be engineered for stimuli-responsive release (e.g., to pH, ROS) in inflammatory microenvironments [59]. | Improved drug encapsulation and sustained release, reducing premature degradation [59]. | High targeting potential, can navigate complex inflammatory environments, reduced systemic toxicity [59]. | Challenges in precise targeting, manufacturing scalability, and long-term biosafety remain [59]. |
Performance Data for Zwitterionic Coatings
Recent research directly comparing zwitterionic coatings on polyether-ether-ketone (PEEK) surfaces provides quantitative insights into their anti-inflammatory performance. The following data, derived from in vitro studies with M1 macrophages, highlights the efficacy of these coatings.
Table 2: Experimental Anti-inflammatory Performance of Zwitterionic Coatings on PEEK [56]
| Coating Type | Substrate Roughness | Effect on Macrophage Viability | Reduction in Pro-inflammatory Cytokines | Inhibition of Nitric Oxide Release |
|---|---|---|---|---|
| MPC-based | Smooth (Sa: 1.4 μm ± 0.3 μm) | Significantly supported viability | Significant reduction in IL-1β, IL-6, and TNF-α | Significant inhibition |
| SBMA-based | Smooth (Sa: 1.4 μm ± 0.3 μm) | Moderate effect | Moderate reduction | Less effective than MPC |
| MPC-based | Rough (Sa: 7 μm ± 4 μm) | Less effective than on smooth surface | Less effective than on smooth surface | Less effective than on smooth surface |
| Uncoated PEEK | N/A | Baseline | Baseline (High release) | Baseline (High release) |
The data demonstrates that the MPC-based coating on a smooth PEEK surface delivered the most remarkable anti-inflammatory effects, suggesting a superior capability to modulate the immune response [56]. The results also underscore the significant influence of substrate topography on coating performance.
Experimental Protocols for Coating Development and Assessment
To ensure the reliability and comparability of data in this field, standardized experimental protocols are essential. This section outlines key methodologies for fabricating, applying, and evaluating anti-inflammatory coatings.
Coating Fabrication and Application
Protocol 1: Zwitterionic Coating on PEEK via Polydopamine Adhesive Layer [56]
- Surface Preparation: PEEK substrates (e.g., smooth, Sa ~1.4 μm; rough, Sa ~7 μm) are cleaned and sterilized.
- Polydopamine Priming: Submerge PEEK samples in an aqueous dopamine solution (e.g., 2 mg/mL in 10 mM Tris-HCl buffer, pH 8.5) for 24 hours under constant agitation. This forms a strong adhesive primer layer.
- Zwitterionic Grafting: Immerse the polydopamine-coated PEEK into a solution containing the zwitterionic monomer (MPC or SBMA) and a stabilizer co-monomer (e.g., N-[3-(dimethylamino)propyl]acrylamide). Polymerization is initiated to graft the zwitterionic copolymer onto the primed surface.
- Post-processing & Sterilization: Rinse coated samples thoroughly with deionized water to remove unreacted monomers and sterilize via gamma irradiation or ethylene oxide before in vitro/in vivo testing.
Protocol 2: Dip Coating of Polymer Films for Drug Delivery [57]
- Polymer Solution Preparation: Dissolve a biodegradable polymer (e.g., PLGA) and the selected anti-inflammatory drug (e.g., Dexamethasone) in an organic solvent (e.g., dichloromethane) to form a homogeneous solution.
- Coating Process: Immerse the implantable device (e.g., a neural electrode or stent) into the polymer-drug solution.
- Controlled Withdrawal: Withdraw the device at a controlled, slow speed to ensure a uniform coating layer. The speed directly influences the final coating thickness.
- Solvent Evaporation: Allow the solvent to evaporate completely in a controlled environment (e.g., under vacuum), leaving a solid polymer film with entrapped drug on the device surface.
- Curing: Further cure the coating, if necessary, at an elevated temperature to ensure stability.
Coating Characterization and Anti-inflammatory Efficacy
Protocol 3: In Vitro Assessment of Anti-inflammatory Effects [56]
- Cell Culture: Use a macrophage cell line (e.g., RAW 264.7) or primary macrophages. Differentiate monocytes into M1 (pro-inflammatory) macrophages using interferon-gamma (IFN-γ) and lipopolysaccharide (LPS).
- Sample Exposure: Culture the activated M1 macrophages on coated and uncoated (control) material samples for a set period (e.g., 24-72 hours).
- Viability Assay: Quantify macrophage viability using a standard assay like MTT or live/dead staining.
- Cytokine Analysis: Collect the cell culture supernatant. Quantify the concentration of key pro-inflammatory cytokines (e.g., IL-1β, IL-6, TNF-α) using Enzyme-Linked Immunosorbent Assay (ELISA) kits.
- Nitric Oxide Measurement: Assess the concentration of nitric oxide, a key inflammatory mediator, in the culture supernatant using the Griess reagent assay.
Protocol 4: Stability and Chemical Characterization [56]
- Stability Study: Incubate coated samples in phosphate-buffered saline (PBS) or simulated body fluid at 37°C for extended periods (e.g., up to 8 weeks).
- Surface Analysis (Pre/Post Incubation):
- X-ray Photoelectron Spectroscopy (XPS): Analyze the elemental composition and chemical states on the coating surface to detect changes over time.
- Water Contact Angle (WCA): Measure the hydrophilicity/hydrophobicity of the surface. Stable zwitterionic coatings will maintain a low WCA, indicating preserved hydrophilicity.
- Coating Thickness: Qualitatively confirm the presence and uniformity of the coating layer using Focused Ion Beam-Scanning Electron Microscopy (FIB-SEM).
Visualizing Coating Function and Macrophage Polarization
The following diagrams illustrate the core concepts of how anti-inflammatory coatings function and their effect on the key immune cells involved in the foreign body reaction.
Anti-inflammatory Coating Mechanisms
Macrophage Signaling and Cytokine Release
The Scientist's Toolkit: Essential Research Reagents
This table lists key materials and reagents used in the development and testing of anti-inflammatory coatings, as cited in the referenced studies.
Table 3: Essential Reagents for Coating Development and Evaluation
| Reagent / Material | Function / Application | Specific Examples / Targets |
|---|---|---|
| Zwitterionic Monomers [56] | Formulate non-fouling, biomimetic coating surfaces that resist protein adsorption and modulate macrophage activity. | MPC (2-methacryloyloxyethyl phosphorylcholine), SBMA ([2-(methacryloyloxy)ethyl]dimethyl-(3-sulfopropyl)ammonium hydroxide) |
| Polydopamine [56] | Serves as a universal, strong adhesive primer layer on diverse substrates (e.g., PEEK, metals) to enable subsequent functionalization. | Aqueous dopamine solution (2 mg/mL in Tris-HCl buffer, pH 8.5) |
| Biodegradable Polymers [57] | Act as a reservoir matrix for the controlled release of encapsulated anti-inflammatory drugs from the implant surface. | PLGA (Polylactic-co-glycolic acid), PCL (Poly(ε-caprolactone)), Chitosan |
| Pro-inflammatory Cytokines [56] [59] | Key biomarkers measured in vitro and in vivo to quantify the anti-inflammatory efficacy of coatings. | IL-1β (Interleukin-1 beta), IL-6 (Interleukin-6), TNF-α (Tumor Necrosis Factor-alpha) |
| Macrophage Polarization Agents [56] [59] | Used in cell culture to differentiate monocytes/macrophages into the pro-inflammatory M1 phenotype for testing. | LPS (Lipopolysaccharide), IFN-γ (Interferon-gamma) |
| ELISA Kits [56] | Standard tool for the quantitative measurement of specific cytokine concentrations in cell culture supernatants or tissue lysates. | Commercial kits for IL-1β, IL-6, TNF-α |
| Characterization Equipment [56] | Essential for analyzing coating chemistry, stability, thickness, and morphology. | XPS (X-ray Photoelectron Spectroscopy), FIB-SEM (Focused Ion Beam-Scanning Electron Microscopy), Water Contact Angle Goniometer |
The strategic functionalization of implant surfaces with anti-inflammatory coatings is a cornerstone for achieving chronic stability in implantable devices. Direct comparisons reveal that while zwitterionic MPC-based coatings on smooth substrates show exceptional promise for passively modulating the immune response, active drug delivery systems using biodegradable polymers offer a versatile and tunable alternative. The choice of strategy must be informed by the specific implant application, desired release profile, and the nature of the inflammatory challenge. The ongoing integration of these approaches—such as combining non-fouling zwitterionic surfaces with targeted, controlled release of anti-inflammatory biologics—represents the future frontier. This synergistic path holds the greatest potential to create truly "invisible" implants that seamlessly integrate with host tissue, thereby ensuring long-term functional stability and revolutionizing patient care.
The long-term performance of implantable electrodes is a pivotal challenge in modern neuroengineering and medical prosthetics. The core thesis of this field posits that the chronic stability of an implant is not a function of a single parameter but is instead determined by a complex interplay between its geometric design, the surgical implantation protocol, and the ensuing biological response. Achieving minimal tissue disturbance while maintaining high-fidelity signal acquisition or stimulation over months and years requires a deliberate optimization of the implant's physical form and its integration strategy. Geometric optimization, encompassing both the miniaturization of devices and the strategic use of shape-specific designs, has emerged as a critical pathway to mitigate the foreign body response, enhance biocompatibility, and ensure the long-term functional viability of neural interfaces [3] [60].
The fundamental biological challenge driving this optimization is the chronic foreign body reaction. When a device is implanted, the mechanical mismatch between the typically rigid, large probe and the soft, dynamic brain tissue triggers a cascade of adverse events. This includes the activation of microglia, chronic blood-brain barrier disruption, and the eventual formation of a dense glial scar composed of reactive astrocytes. This scar tissue insulates the electrode from its target neurons, increasing interfacial impedance and leading to a progressive decline in the signal-to-noise ratio (SNR) of recorded neuronal activities. Concurrently, neurotoxic inflammatory cytokines and oxidative stress can lead to neuronal death in the immediate vicinity of the implant, resulting in a permanent loss of signal sources [3]. Therefore, the overarching goal of geometric optimization is to design devices that blur the distinction between man-made implants and natural-born tissues, thereby promoting seamless integration and long-term stability.
Comparative Analysis of Geometric Design and Performance
The following section provides a detailed, data-driven comparison of how different geometric parameters—including shape, size, and density—influence the key performance metrics of implantable electrodes.
Table 1: Influence of Implant Shape and Surgical Protocol on Primary Stability
This table synthesizes experimental data on how the geometric shape of an implant and the precision of bone preparation surgical technique affect its initial mechanical stability, a precursor to long-term osseointegration [61].
| Implant Shape | Bone Preparation Protocol | Bone Quality Model | Implant Stability Quotient (ISQ) ± SD | Key Finding |
|---|---|---|---|---|
| Straight-Screw | Standard Preparation | Type II (Good) | 73.30 ± 6.21 | Primary stability is not significantly affected by preparation depth for straight-screw designs [61]. |
| Straight-Screw | 1 mm Under-Preparation | Type II (Good) | 72.23 ± 8.72 | |
| Straight-Screw | 1 mm Over-Preparation | Type II (Good) | 73.20 ± 6.40 | |
| Tapered-Screw | Standard Preparation | Type II (Good) | 74.27 ± 5.32 | Tapered designs are highly sensitive to surgical technique; under-preparation significantly boosts stability [61]. |
| Tapered-Screw | 1 mm Under-Preparation | Type II (Good) | 76.83 ± 4.69 | |
| Tapered-Screw | 1 mm Over-Preparation | Type II (Good) | 66.60 ± 5.72 | |
| Straight-Screw | Standard Preparation | Type IV (Poor) | 63.37 ± 5.59 | Bone density has a prevailing effect, but shape-specific advantages persist in poor quality bone [61]. |
| Straight-Screw | 1 mm Under-Preparation | Type IV (Poor) | 61.40 ± 7.09 | |
| Tapered-Screw | 1 mm Under-Preparation | Type IV (Poor) | 66.37 ± 6.54 |
Table 2: Impact of Electrode Density and Miniaturization on Neural Decoding Performance
This table compares the performance of standard versus high-density microelectrode arrays in decoding neural signals for brain-computer interface (BCI) applications, highlighting the advantages of miniaturization and increased spatial resolution [62].
| Electrode Grid Type | Electrode Diameter / Spacing | Decoding Task | Average Best Decoding Error | Key Finding |
|---|---|---|---|---|
| Standard ECoG Grid | 4 mm / 10 mm | State Decoder (Movement vs. Idle) | 8.5% | Standard grids are inadequate for resolving multi-degree-of-freedom arm movements due to limited spatial resolution [62]. |
| High-Density (HD) ECoG Grid | 2 mm / 4 mm | State Decoder (Movement vs. Idle) | 2.6% | HD grids offer superior signal quality and resolution, enabling highly accurate detection of movement onset [62]. |
| Standard ECoG Grid | 4 mm / 10 mm | Movement Decoder (6-Class) | 33.1% | Low electrode density leads to significant confusion between different arm movements (e.g., grasp vs. wrist movement) [62]. |
| High-Density (HD) ECoG Grid | 2 mm / 4 mm | Movement Decoder (6-Class) | 11.9% | Increased electrode density better resolves functional representations, drastically improving classification of elementary movements [62]. |
Table 3: Long-Term Clinical Outcomes of Wedge-Shaped vs. Conventional Cylindrical Implants
This table presents long-term clinical data for an unconventional wedge-shaped dental implant design, demonstrating how shape-specific strategies can address anatomical constraints [63].
| Implant Characteristic | Wedge-Shaped Implant (Rex TL) | Conventional Narrow-Diameter Implant (Typical Profile) |
|---|---|---|
| Geometric Design | Bucco-lingual width: 1.8 mm; Flat lateral surfaces with macro-grooves | Cylindrical or tapered screw; Diameter typically >3.0 mm |
| Target Application | Horizontally atrophic alveolar ridges (mean thickness ~3.73 mm) | Ridges with sufficient bone volume for standard implant placement |
| Engagement Strategy | Designed to engage both buccal and lingual cortices | Relies on bone in-growth and engagement along the entire bone wall |
| 7-Year Survival Rate | 95.5% | (Context-dependent; study demonstrates wedge-shaped is viable) |
| Marginal Bone Loss (MBL) | 1.45 ± 1.41 mm (after 7 years) | Varies, but design aims to minimize MBL |
| Key Advantage | Avoids the need for invasive bone augmentation procedures in narrow ridges | Established, well-understood surgical and prosthetic protocols |
Experimental Protocols for Assessing Geometry and Stability
To generate the comparative data presented in this guide, researchers employ a suite of standardized experimental protocols. These methodologies are crucial for objectively evaluating the impact of geometric variables on implant performance.
Resonance Frequency Analysis (RFA) for Primary Stability
Objective: To quantitatively measure the initial mechanical stability of an implant immediately following insertion [61]. Protocol:
- Model Preparation: Use fresh bovine rib blocks as bone models. To simulate different bone densities, cortical bone can be left intact (Type II model) or removed and the trabecular bone partially decalcified with acetic acid (Type IV model).
- Surgical Implantation: Implant fixtures (e.g., straight-screw vs. tapered-screw) are inserted into prepared osteotomies. The bone preparation depth is systematically varied (e.g., 1 mm under-preparation, standard, 1 mm over-preparation) while ensuring the implant platform height remains consistent.
- Measurement: Immediately after insertion, a smartpeg is attached to the implant fixture. A resonance frequency analyzer (e.g., Osstell) is used to measure the Implant Stability Quotient (ISQ). The measurement is repeated three times, and the average value is recorded for analysis [61]. Relevance: This protocol directly tests the hypothesis that tapered implants achieve higher primary stability than straight-walled implants in under-prepared osteotomies, a key geometric-surgical interaction.
Chronic In-Vivo Neural Recording and Histological Correlation
Objective: To evaluate the long-term recording performance and biological integration of neural microelectrodes with different geometries and material properties [3] [60]. Protocol:
- Implantation: Neural probes (e.g., Michigan-style shanks, Neuropixels, or flexible polymer-based probes) are implanted into the target brain region (e.g., motor cortex) of animal models.
- Chronic Signal Monitoring: Neural signals (spikes and local field potentials) are recorded regularly over a period of months. Key metrics such as Signal-to-Noise Ratio (SNR), single-unit yield, and amplitude of recorded action potentials are tracked over time.
- Histological Analysis: Upon termination of the experiment, brain tissue is perfused, fixed, and sectioned. Immunohistochemical staining is performed for specific biomarkers:
- Glial Fibrillary Acidic Protein (GFAP): To label reactive astrocytes and quantify glial scar thickness.
- Ionized Calcium-Binding Adapter Molecule 1 (Iba1): To identify activated microglia and macrophages.
- NeuN: To label neuronal nuclei and quantify neuronal density around the implant track [3].
- Correlation: The chronic electrophysiology data is directly correlated with the post-mortem histological findings to establish a causal link between probe geometry, the foreign body response, and the decay in recording performance.
High-Density Electrocorticography (ECoG) Decoding Workflow
Objective: To compare the ability of standard and high-density ECoG grids to decode complex motor commands [62]. Protocol:
- Subject Implantation: Patients undergoing epilepsy monitoring are implanted with either standard (4mm diameter, 10mm spacing) or high-density (2mm diameter, 4mm spacing) subdural electrode grids that cover the primary motor cortex.
- Task Performance: Subjects perform a series of repetitive, elementary arm movements (e.g., pincer grasp, wrist flexion/extension, elbow flexion/extension) while ECoG signals and movement kinematics are recorded synchronously.
- Signal Processing: ECoG signals are filtered into standard frequency bands (μ: 8-13 Hz, β: 13-30 Hz, low-γ: 30-50 Hz, high-γ: 80-160 Hz). The power in these bands is used as the primary feature for decoding.
- Decoder Training and Validation: Machine learning classifiers (e.g., a binary state decoder for movement/idling and a multi-class movement decoder) are trained on the ECoG features. Performance is rigorously evaluated using cross-validation, and decoding errors are calculated to compare the resolution of the two grid types [62].
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key materials and reagents essential for conducting research in geometric optimization of implantable electrodes.
Table 4: Research Reagent Solutions for Electrode Development and Testing
| Item Name | Function/Application | Relevance to Geometric Optimization |
|---|---|---|
| Titanium Alloys (e.g., Ti6Al4V) | Biocompatible substrate for bone and neural implants; can be machined or 3D-printed into various shapes. | Used for creating tapered-screw, straight-screw, and wedge-shaped implant bodies. Its mechanical properties allow for miniaturization [61] [63]. |
| Platinum (Pt) and Iridium (Ir) | Conductive metals used for electrode sites and interconnects due to excellent charge injection capacity and corrosion resistance. | Essential for fabricating micro-scale electrode sites on high-density arrays. Often electroplated as Pt Black to increase surface area and reduce impedance at small geometries [60]. |
| Conductive Polymers (e.g., PEDOT:PSS) | Electrodeposited coating for electrode sites to significantly lower interfacial impedance and improve biocompatibility. | Used to modify the surface of miniaturized electrodes, counteracting the impedance increase that comes with reduced geometric surface area [60]. |
| Polyimide | Flexible, biocompatible polymer used as an insulation and substrate material for thin-film neural probes. | Enables the fabrication of flexible, miniaturized shanks that reduce mechanical mismatch with brain tissue, a key strategy for improving chronic stability [3]. |
| SLActive Hydrophilic Surface | Chemically modified, high-surface-energy titanium implant surface (Straumann). | While a surface treatment, it works synergistically with implant geometry by accelerating osseointegration, which is crucial for the stability of non-cylindrical designs like wedge implants [64]. |
| Piezoelectric Surgical Instrument | Device for precise, vibration-based bone cutting with minimal tissue damage. | Critical for executing shape-specific implantation protocols, such as preparing the precise osteotomy for a press-fit wedge-shaped implant without causing microfractures [63]. |
Signaling Pathways and the Foreign Body Response
The long-term failure of implantable electrodes is mediated by well-defined biological signaling pathways. The following diagram illustrates the key mechanistic relationship between implant geometry, the resulting biological response, and the ultimate functional outcome.
Diagram: Implant Geometry Triggers a Signaling Cascade Affecting Chronic Performance
The development of implantable electrodes represents a frontier in modern medicine, enabling breakthroughs in treating neurological disorders, restoring sensory functions, and facilitating brain-computer interfaces. However, the long-term efficacy of these devices is fundamentally constrained by the biological-tissue integration challenge. While traditional rigid electrodes from materials like silicon and metals provide excellent electrical properties, their mechanical mismatch with soft neural tissue (GPa vs. kPa modulus range) triggers chronic inflammatory responses, glial scarring, and eventual signal degradation [7] [65].
This comparative guide examines the landscape of novel conductive materials and coating strategies that aim to resolve this conflict by balancing electrical conductivity with biocompatibility. The ultimate goal is achieving "invisibility" to the immune system while maintaining stable electrical performance over implantation periods lasting years. We evaluate these technologies through the critical lens of chronic stability assessment, providing researchers with experimental data and methodologies to inform material selection for next-generation neural interfaces.
Material Comparisons: Performance Metrics and Trade-offs
Conductive Coating Materials for Neural Interfaces
Table 1: Comparison of Conductive Coating Materials for Neural Interfaces
| Material Category | Representative Materials | Conductivity Range | Key Advantages | Chronic Stability Challenges | Primary Applications |
|---|---|---|---|---|---|
| Conductive Polymers | Polypyrrole (PPy), PEDOT:PSS | 10-1000 S/cm [66] | Mechanical flexibility, biocompatibility, surface modification capability | Potential delamination, oxidative degradation under electrical stimulation | Neural recording electrodes, nerve guidance conduits [66] |
| Carbon-Based Materials | Graphene, Carbon Nanotubes (CNTs) | 100-10,000 S/cm (varying by structure) [66] | High surface area, chemical stability, excellent charge injection capacity | Potential particle shedding, inflammatory response to certain morphologies | Composite coatings, neural stimulation electrodes [66] |
| Metallic Coatings | Platinum Black (PtB), Gold | 10â´-10ⶠS/cm (bulk) [65] | Excellent conductivity, established clinical history | Mechanical stiffness, corrosion under stimulation | High-density microelectrodes, stimulation interfaces [65] |
| Biomimetic Coatings | Catechol-based polymers, RGD peptide-modified | Variable (often composite) [67] | Enhanced tissue integration, reduced foreign body response | Conductivity often dependent on composite materials | Bioadhesive interfaces, tissue-integrating electrodes [67] |
Quantitative Performance Comparison in Biological Environments
Table 2: Experimental Performance Metrics of Conductive Coatings in Neural Applications
| Material System | Impedance at 1kHz (kΩ) | Charge Injection Limit (mC/cm²) | Recording SNR (dB) | In Vivo Stability Duration | Glial Scar Thickness vs. Controls |
|---|---|---|---|---|---|
| PEDOT:PSS Coating | 2-5 [65] | 1.5-3.0 [65] | 12-15 [65] | 6-8 months [7] | 40-60% reduction [7] |
| PtB Electrodes | 0.5-2 [65] | 5.0-8.0 (varies with roughness) [65] | 15-20 [65] | >12 months [65] | Comparable to rigid controls [65] |
| CNT-Polymer Composite | 10-20 [66] | 2.0-4.0 [66] | 8-12 [66] | 3-6 months (mechanical integrity) [66] | 50-70% reduction [66] |
| Graphene-PCL Nerve Conduit | N/A (conductive scaffold) | N/A | N/A | 12+ months (degradable) [66] | Promotes axonal regeneration [66] |
Experimental Protocols for Chronic Stability Assessment
Electrochemical Impedance Spectroscopy (EIS) for Interface Stability
Protocol Objective: Quantify the stability of the electrode-tissue interface through periodic impedance measurements.
Materials and Equipment:
- Potentiostat/Galvanostat with EIS capability
- Standard three-electrode cell (working, counter, reference electrodes)
- Phosphate-buffered saline (PBS) or artificial cerebrospinal fluid (aCSF) at 37°C
- Data acquisition software
Methodology:
- Baseline Measurement: Perform EIS sweep from 100 Hz to 100 kHz at amplitude of 10 mV before implantation
- In Vivo Monitoring: For chronic studies, conduct weekly EIS measurements post-implantation
- Data Analysis: Track changes in impedance magnitude at 1 kHz, which correlates with glial scar formation
- Equivalent Circuit Modeling: Fit data to Randles circuit to isolate interface component changes
Key Metrics: Impedance at 1 kHz, phase angle, and solution resistance changes over time indicate encapsulation tissue formation and interface stability [7] [65].
Immunohistological Analysis of Foreign Body Response
Protocol Objective: Quantitatively assess inflammatory response and tissue integration following explantation.
Materials and Equipment:
- Tissue fixation (4% paraformaldehyde)
- Cryostat or microtome
- Primary antibodies: Anti-GFAP (astrocytes), Anti-IBA1 (microglia), Anti-CD68 (macrophages)
- Fluorescently tagged secondary antibodies
- Confocal microscope with image analysis software
Methodology:
- Tissue Processing: Perfuse and fix brain tissue with implanted electrodes at study endpoint
- Sectioning: Prepare 20-40 μm thick sections containing electrode track
- Immunostaining: Incubate with primary antibodies (24h, 4°C) followed by secondary antibodies (2h, RT)
- Imaging and Quantification: Capture high-resolution images of interface region and quantify:
- Glial scar thickness (GFAP+ area)
- Microglial activation (IBA1+ cell density and morphology)
- Macrophage infiltration (CD68+ cell count)
Chronic Stability Indicators: Reduced glial scar thickness (<50 μm), ramified (resting) microglia morphology, and minimal macrophage presence indicate improved biocompatibility [7] [67].
Diagram 1: Foreign Body Response and Biocompatibility Strategy Pathway. This workflow illustrates the cascade of inflammatory events following electrode implantation and corresponding strategies to mitigate these effects for enhanced chronic stability.
Emerging Coating Technologies and Their Mechanisms
Biomimetic Surface Engineering
Nature-inspired coating strategies represent a paradigm shift in addressing the biocompatibility challenge. These approaches mimic biological structures and mechanisms to create surfaces that actively resist fouling or promote specific cellular interactions:
- Gecko-Inspired Adhesives: Micro- and nanoscale pillar structures create high surface area for stable tissue integration without chemical adhesion [67]
- Mussel-Inspired Chemistry: Polydopamine and other catechol-based coatings provide universal surface modification capabilities and robust adhesion in wet environments [67]
- Shark Skin-Inspired Antifouling: Micro-ridge patterns physically disrupt bacterial adhesion and biofilm formation without chemical antimicrobials [67]
- Lotus Leaf-Inspired Superhydrophobicity: Hierarchical structures create self-cleaning surfaces that minimize protein adsorption and cell adhesion [67]
These biomimetic approaches can be combined with conductive materials to create multifunctional surfaces that address both electrical and biological requirements.
Conductive Hydrogels for Tissue Integration
Conductive hydrogels represent an emerging class of materials that bridge the mechanical property gap while providing electrical functionality. These systems typically combine conductive polymers (PPy, PEDOT) or carbon nanomaterials with hydrogels based on natural (alginate, chitosan) or synthetic (PEG, PVA) polymers. The resulting composites exhibit Young's moduli in the kPa range, closely matching neural tissue, while maintaining conductivities sufficient for recording and stimulation applications [66].
Experimental data from peripheral nerve regeneration studies demonstrate that conductive hydrogels supporting electrical stimulation (1-100 mV/mm) enhance neurite extension by 25-40% compared to non-conductive controls through mechanisms including enhanced Schwann cell migration and neurotrophic factor secretion [66].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Conductive Biomaterials Development
| Reagent/Material | Supplier Examples | Function in Research | Application Notes |
|---|---|---|---|
| PEDOT:PSS Dispersion | Heraeus, Sigma-Aldrich | Conductive polymer coating for electrode surfaces | Often requires additives (DMSO, surfactants) for stability; biocompatibility varies by formulation |
| Polydopamine HCl | Sigma-Aldrich, StemCell Technologies | Universal surface primer for subsequent functionalization | Polymerization time (2-24h) controls thickness; can be combined with conductive materials |
| RGD Peptide | Tocris, MedChemExpress | Promotes cell adhesion through integrin binding | Typically used at 0.1-1.0 mM concentration; can be conjugated to various surfaces |
| Carbon Nanotubes | NanoLab, Sigma-Aldrich | Conductive filler for composite materials | Functionalization (COOH, NHâ‚‚) often needed for dispersion and biocompatibility |
| Polycaprolactone (PCL) | Sigma-Aldrich, Corbion | Biodegradable polymer for nerve guidance conduits | Often combined with conductive fillers; compatible with 3D printing [66] |
| Platinum Black Electroplating Solution | Metrohm, BASi | Creates high-surface-area coatings for stimulation electrodes | Electroplating parameters critically control morphology and stability [65] |
Diagram 2: Experimental Workflow for Chronic Stability Assessment. This workflow outlines the key stages in developing and evaluating conductive coatings for neural interfaces, from material selection through comprehensive in vivo assessment.
The ideal conductive coating for chronic neural interfaces remains elusive, as evidenced by the performance trade-offs quantified in this guide. No single material system currently leads across all metrics—conductive polymers offer excellent mechanical matching but limited stability, metallic coatings provide superior electrical performance but trigger foreign body responses, and biomimetic strategies enhance biocompatibility while often compromising conductivity.
The most promising path forward appears to lie in multimaterial systems that strategically combine components to address specific aspects of the stability challenge. Examples include PEDOT:PSS coatings on flexible substrates with surface-immobilized anti-inflammatory molecules, or carbon nanotube composites in biodegradable polymers with tuned release kinetics. Furthermore, the emergence of "living electrodes" incorporating biological components represents a paradigm shift toward truly integrated neural interfaces.
For researchers navigating this complex landscape, systematic evaluation using the standardized protocols and metrics outlined in this guide will enable direct comparison between emerging technologies. The chronic stability assessment framework—encompassing electrochemical, functional, and histological endpoints—provides a comprehensive approach to identifying materials capable of supporting the next generation of durable neural interfaces.
Active Modulation of the Immune Response Through Bioactive Interfaces
For researchers and drug development professionals working on chronic neural implants, the foreign body response (FBR) presents a fundamental barrier to long-term device stability and function. The FBR is a complex neuroinflammatory reaction to implanted electrodes, initiating upon device insertion and evolving into a chronic state that ultimately compromises signal fidelity and therapeutic efficacy [68]. This response begins with acute trauma from implantation, where electrodes disrupt vasculature, damage the blood-brain barrier, and cause mechanical injury to cells and extracellular matrix [45] [68]. Within hours, microglia activate and migrate to the injury site, followed by astrocytes transitioning to a reactive state over subsequent days [45]. These activated glial cells release pro-inflammatory cytokines, reactive oxygen species, and cytotoxic factors that create a neurotoxic microenvironment [68]. Over weeks, a dense glial scar forms around the implant, consisting of reactive astrocytes, connective tissue, and extracellular matrix components [7] [68]. This scar tissue physically isolates the electrode from nearby neurons and significantly increases electrical impedance, leading to progressive signal degradation and eventual device failure [7] [45].
While traditional approaches have focused on passive strategies to minimize initial tissue damage, active modulation of the immune response represents a paradigm shift in neural interface design. This proactive approach seeks to directly intervene in the inflammatory cascade using bioactive components that deliver therapeutic agents, present biological cues, or integrate living cellular elements. By actively shaping the host immune response rather than merely resisting it, these advanced interfaces offer promising pathways to extend functional electrode lifetimes from months to years, a critical requirement for viable clinical applications of brain-computer interfaces and chronic neuromodulation therapies.
Comparative Analysis of Bioactive Strategies
This section provides a systematic comparison of three principal approaches for active immune modulation, summarizing their mechanisms, experimental implementations, and quantitative outcomes.
Table 1: Comparison of Bioactive Interface Strategies for Immune Modulation
| Strategy | Mechanism of Action | Key Materials/Components | Experimental Outcomes | Limitations |
|---|---|---|---|---|
| Drug Delivery Systems | Controlled release of anti-inflammatory compounds to modulate local cellular response [7] [69]. | Dexamethasone (DEX), anti-inflammatory cytokines; carrier matrices: alginate hydrogels, PLGA nanofibers [69]. | ~50% slower drug release with alginate coatings; reduced glial scarring and neuronal density loss in rodent models [69]. | Finite drug reservoir; potential for burst release; long-term stability of polymer carriers. |
| Bioactive Coatings & Surface Functionalization | Presentation of biomolecular cues to promote neuronal integration and suppress glial activation [7] [69]. | Laminin, chitosan, IKVAV peptides, silk fibroin, marine polysaccharides (ulvan) [69]. | Enhanced hippocampal neuron proliferation; reduced astrocyte adhesion by ~40% with NM-based coatings; improved neurite outgrowth [69]. | Coating stability and durability under chronic implantation; potential delamination. |
| Living Cell Interfaces | Creation of a biologically active layer that integrates with host tissue, providing natural synaptic modulation [68]. | Pre-formed neural micro-tissues, axonal tracts within biomaterial micro-columns ("living electrodes") [68]. | Improved host-implant integration in preclinical models; synaptic-based modulation of host circuitry; reduced chronic FBR [68]. | High complexity of fabrication and implantation; long-term viability of cellular components; regulatory challenges. |
Drug Delivery Systems
Drug-eluting systems represent one of the most direct approaches for active immunomodulation. These systems integrate controlled-release mechanisms to deliver anti-inflammatory agents locally to the tissue surrounding the implant. A prominent example involves coatings made from alginate hydrogels loaded with dexamethasone (DEX), a potent corticosteroid [69]. In one experimental protocol, researchers first encapsulated DEX within poly(lactic-co-glycolic acid) (PLGA) nanofibers electrospun onto the electrode surface. This drug-loaded scaffold was then coated with an alginate hydrogel layer, which served a dual purpose: it acted as a diffusion barrier to prolong drug release and provided a substrate for the subsequent electrochemical deposition of the conducting polymer PEDOT to enhance electrical performance [69]. This configuration demonstrated a significant reduction in drug release kinetics, slowing DEX diffusion by approximately 50% compared to uncoated electrodes, thereby extending the therapeutic window [69].
The efficacy of such systems is typically validated in rodent models. Histological analyses at chronic time points (e.g., 6-16 weeks post-implantation) quantify key metrics such as the thickness of the glial scar (identified by GFAP immunostaining), the density of activated microglia (using IBA-1 or ED1 markers), and neuronal survival in the vicinity of the implant. Studies have shown that electrodes with sustained anti-inflammatory drug release maintain significantly lower impedance over time and record neural signals with higher signal-to-noise ratios compared to passive control electrodes [7] [69].
Bioactive Coatings and Surface Functionalization
This strategy moves beyond drug delivery to create a surface biochemical environment that actively promotes beneficial cellular interactions. Using techniques like layer-by-layer (LbL) assembly, researchers can fabricate nanostructured coatings with precise control over thickness, stiffness, and bioactivity [69]. For instance, coatings incorporating chitosan (a crustacean-derived polysaccharide) and ulvan (from green algae) have been shown to create an extracellular matrix (ECM)-like environment that is favorable for neural cells [69]. Experimental results demonstrate that these nature-derived material (NM) based coatings significantly enhance hippocampal neuron proliferation while reducing astrocyte adhesion by approximately 40%, effectively steering the cellular response toward integration rather than isolation [69].
Another approach involves functionalizing polyimide electrode surfaces with IKVAV peptides, which are sequences derived from laminin that promote neurite outgrowth. In vitro experiments with PC12 cells (a neuronal cell model) on such modified surfaces show enhanced cell adhesion and extensive neurite extension compared to unmodified polyimide [69]. The experimental workflow for evaluating these coatings involves: (1) surface characterization (e.g., atomic force microscopy for roughness, spectroscopy for chemical composition), (2) in vitro cytocompatibility and specificity assays with co-cultures of neurons and glial cells, and (3) in vivo implantation with subsequent histological analysis to quantify neuronal density and glial scarring at the interface.
Living Cell Interfaces
As a frontier approach, biohybrid interfaces incorporate living cellular components to create a truly biologically active interface. Our lab has developed "living electrodes" consisting of pre-formed neural micro-tissues featuring long axonal tracts encased within biocompatible, micromachined biomaterial columns [68]. These constructs are designed to establish natural, synaptic-based connections with host neural circuitry while remaining under external control via integrated electronics.
The fabrication protocol involves: (1) creating a tailored biomaterial scaffold (e.g., using collagen or agarose) with mechanical properties matching the brain (Young's modulus ~1-10 kPa); (2) seeding and cultivating neural cells within this scaffold to form organized, axon-rich micro-tissues; and (3) integrating this living system with a miniature electrode array for recording and stimulation [68]. Upon implantation, these living electrodes are designed to interact synaptically with host neurons, potentially bypassing the foreign body response that typically isolates conventional electrodes. In vivo characterization in rodent models includes electrophysiological recording of synaptic activity between the implant and host, immunohistochemical analysis of inflammatory markers, and tracing of axonal projections between the living electrode and host brain to assess functional integration [68].
Table 2: Quantitative Performance Metrics of Bioactive Interfaces
| Performance Metric | Drug Delivery Systems | Bioactive Coatings | Living Cell Interfaces |
|---|---|---|---|
| Reduction in Glial Scar Thickness | 40-60% reduction (vs. controls) with sustained DEX release [69]. | 30-50% reduction with ECM-mimetic coatings [69]. | Qualitative improvements in integration; quantitative metrics emerging [68]. |
| Impact on Electrode Impedance | Maintains stable lower impedance during drug release phase [7]. | Initial reduction, but long-term stability depends on coating integrity [69]. | Not fully characterized; potential for stable long-term impedance via integration. |
| Neuronal Density at Interface | Improved preservation within 100 µm of electrode surface [68] [69]. | Up to 40% increase with peptide-functionalized surfaces [69]. | Promotes direct synaptic integration with host neurons [68]. |
| Functional Recording Lifetime | Extension to several months in rodent models [7]. | Moderate improvements; highly dependent on coating stability [69]. | Potential for very long-term stability; currently under investigation [68]. |
Diagram Title: Foreign Body Response and Bioactive Intervention Pathways
The Scientist's Toolkit: Essential Reagents and Materials
Successfully implementing the strategies described above requires specific research reagents and materials. The following table catalogues key solutions for developing bioactive neural interfaces.
Table 3: Essential Research Reagents for Bioactive Neural Interface Development
| Reagent/Material | Function | Experimental Application Notes |
|---|---|---|
| Dexamethasone (DEX) | Potent anti-inflammatory corticosteroid for local immune suppression [69]. | Typically loaded into PLGA nanofibers or alginate hydrogels for sustained release; effective in reducing acute inflammation. |
| Alginate Hydrogel | Nature-derived polysaccharide for drug encapsulation and controlled release [69]. | Serves as diffusion barrier to extend drug release profile; also used as substrate for conducting polymer deposition. |
| Chitosan | Marine-derived polysaccharide for creating biocompatible, ECM-mimetic coatings [69]. | Used in layer-by-layer assembly with other polymers; promotes neuronal attachment while reducing glial adhesion. |
| IKVAV Peptide | Laminin-derived bioactive peptide sequence that promotes neurite outgrowth [69]. | Functionalized onto polyimide electrode surfaces to enhance neuronal integration at the tissue-device interface. |
| Silk Fibroin | Biocompatible protein polymer with excellent mechanical properties for flexible interfaces [69]. | Used as dissolvable sacrificial layer for device implantation or as biocompatible coating material. |
| Laminin | Extracellular matrix protein that promotes neuronal attachment and axon guidance [69]. | Incorporated into multilayer coatings via layer-by-layer assembly to create bioactive interfaces. |
Diagram Title: Experimental Workflow for Bioactive Interface Development
The active modulation of immune responses through bioactive interfaces marks a significant evolution in neural interface technology, shifting the paradigm from passive tissue compatibility to dynamic biological integration. The comparative analysis presented here demonstrates that while drug delivery systems offer potent, short-term control over inflammation and bioactive coatings provide excellent biomimetic surfaces for neuronal integration, the emerging frontier of living cell interfaces holds unique potential for achieving truly seamless neural integration through synaptic connectivity. Each approach presents a distinct set of advantages and implementation challenges, suggesting that hybrid strategies may ultimately prove most effective.
For the field to advance, future research must prioritize the development of standardized preclinical models for evaluating long-term interface stability, the creation of novel biomaterials with dynamically responsive properties, and the refinement of fabrication techniques that enable scalable production of these complex bioactive systems. As these technologies mature, active immunomodulation strategies will substantially contribute to the overarching thesis in chronic stability assessment—that the next generation of implantable electrodes must not merely exist within the neural environment, but must actively engage with it to achieve lasting functional integration.
Bench to Bedside: Validating Performance Across Preclinical and Clinical Settings
The clinical success of next-generation bioelectronic medicine, from brain-computer interfaces (BCIs) to neuromodulation therapies, depends critically on the long-term stability of implantable electrodes [13] [12]. These devices must maintain a stable, high-fidelity connection with neural tissue for years or even decades to reliably record neural activity or deliver therapeutic stimulation. However, a major challenge hindering their widespread adoption is performance degradation over time, ultimately leading to device failure [60] [12].
Understanding this decline requires moving beyond isolated assessments. Correlative studies that explicitly link quantitative measurements of an electrode's physical condition to its functional performance metrics are essential to unravel the complex failure mechanisms [13] [70]. Such studies provide the critical insights needed to develop novel electrode designs and materials capable of stable performance throughout a patient's lifetime [13]. This guide objectively compares current findings and methodologies in this vital field of chronic stability assessment for implantable electrodes.
Quantitative Comparison of Electrode Degradation and Performance
Research directly comparing different electrode materials and designs reveals how physical degradation impacts function. The table below summarizes key findings from recent correlative studies.
Table 1: Correlating Physical Electrode Degradation with Functional Performance
| Electrode Type / Study | Implantation Duration & Model | Key Physical Degradation Metrics | Key Functional Performance Metrics | Correlation Findings |
|---|---|---|---|---|
| SIROF vs. Platinum (Pt) [13] [70] | 956-2130 days (Humans with tetraplegia) | - "Pockmarked" vs. "Cracked" surface degradation- Silicon shank erosion- Metal coating damage | - Signal-to-Noise Ratio (SNR)- Impedance at 1 kHz- Stimulation ability | - Despite greater physical degradation, SIROF electrodes were twice as likely to record neural activity than Pt [13] [70].- For SIROF, 1 kHz impedance significantly correlated with all physical damage metrics and functional performance, suggesting it is a reliable indicator of in vivo degradation [13]. |
| Platinum Cochlear Implants [71] | ~120 min to 8 weeks (Guinea pigs) | - Electrode polarisation- Protein fouling- Fibrous tissue formation | - Charge Storage Capacity (CSC)- Electrochemical Impedance Spectroscopy (EIS)- Charge density | - Initial in vitro measurements were poor predictors of subsequent in vivo performance [71].- Impedance at 1 kHz was a very poor predictor of overall electrode performance; lower frequencies were more informative [71].- Tissue encapsulation had minimal impact compared to electrode activation/polarisation [71]. |
| Utah Arrays (Pt & Iridium Oxide) [72] | 594-2680 days (Non-human primates) | - Metal coating cracks- Silicon tip breakage- Parylene C delamination/cracks- Shank fracture- Biological debris | - Recording quality and stability | - No statistically significant difference in physical damage was found between electrodes used for electrolytic lesioning and those that were not [72].- Outer-edge electrodes showed more severe damage than inner electrodes [72]. |
Experimental Protocols for Correlative Analysis
To generate the data for comparative studies, standardized yet versatile experimental workflows are employed. The following section details the key methodologies cited.
Chronic In Vivo Functional Testing
The cornerstone of correlative studies is the longitudinal measurement of functional performance in vivo prior to explantation.
- Neural Recording Assessment: The quality of recorded neural signals is typically quantified by the Signal-to-Noise Ratio (SNR), calculated as ( \frac{V{max} - V{min}}{2 \cdot RMS} ), where ( V{max} ) and ( V{min} ) are the peak-to-peak voltage of the spike signal and ( RMS ) is the root mean square of the background noise [60]. A higher SNR indicates better recording fidelity.
- Electrochemical Impedance Spectroscopy (EIS): This is a standard method to characterize the electrode-tissue interface [71]. It involves applying a small AC voltage amplitude (e.g., 10 mV) over a wide frequency range (e.g., 0.1 Hz to 100,000 Hz) and measuring the impedance. While 1 kHz is commonly reported, studies note that lower frequencies can be more sensitive to changes at the interface [71].
- Stimulation Performance Testing: For stimulating electrodes, the ability to evoke a physiological response (e.g., a somatosensory percept or muscle twitch) is assessed. The charge injection capacity and the efficacy of the stimulation at safe charge density limits are critical metrics [13] [12].
- Cyclic Voltammetry (CV): Used to evaluate the charge storage capacity (CSC) of an electrode, which is crucial for stimulation. A slow scan rate (e.g., 20-50 mV/s) between set potential limits (e.g., -0.6 V to 0.8 V vs. a reference) is applied, and the resulting current is measured [71].
Post-Explant Physical Characterization
After explantation, electrodes undergo rigorous physical analysis to quantify degradation.
- Scanning Electron Microscopy (SEM): This is the primary technique for high-resolution imaging of explanted electrodes [13] [72]. It allows for qualitative and quantitative assessment of damage categories such as:
- Metal coating cracks (in Pt or IrOx)
- "Pockmarked" or cratered surfaces
- Delamination or cracking of the insulation layer (e.g., Parylene C)
- Fracture of the substrate (e.g., silicon shank)
- Buildup of biological debris [72]
- Damage Scoring Systems: To standardize analysis, electrodes are systematically scored across multiple pre-defined damage categories. For example, each electrode on an array can be scored for the presence and severity of cracks, delamination, and debris, allowing for statistical comparison across electrode types, locations, and functions [72].
Data Correlation and Analysis
The final, crucial step is to statistically correlate the quantitative physical damage scores with the chronic functional performance data collected in vivo. This can reveal which types of physical damage (e.g., insulation delamination vs. metal cracking) have the most significant impact on specific performance metrics (e.g., increased noise vs. reduced charge injection) [13] [70].
The Scientist's Toolkit: Essential Research Reagents and Materials
This table details key materials and instruments central to conducting correlative studies of implantable electrodes.
Table 2: Essential Research Reagents and Materials for Correlative Electrode Studies
| Item Name | Function/Application | Specific Examples & Notes |
|---|---|---|
| Neuroport Arrays | A common intracortical microelectrode array platform used for long-term BCI studies in humans and NHPs. | - Utah array design with Pt or sputtered iridium oxide film (SIROF) tips [13] [72]. |
| Platinum (Pt) & Sputtered Iridium Oxide Film (SIROF) | Conductive electrode tip materials compared for long-term stability. | - SIROF showed superior functional performance despite greater physical degradation in one long-term human study [13]. |
| Poly(3,4-ethylenedioxythiophene) (PEDOT) | A conductive polymer used to coat electrode sites. | - Lowers impedance and increases charge storage capacity [73].- Can be doped with nanoparticles for electrically-controlled drug delivery [73]. |
| Parylene C | A biocompatible polymer used as a flexible substrate and insulation layer for neural probes. | - Provides flexibility and a moisture barrier [73].- Subject to delamination and cracking, a key degradation metric [72]. |
| Scanning Electron Microscope (SEM) | High-resolution imaging of explanted electrodes to quantify physical degradation. | - Essential for visualizing cracks, delamination, and biological debris [13] [72].- Often used in low-vacuum mode for samples with organic material [72]. |
| Potentiostat / Impedance Analyzer | Instrument for performing EIS and CV to characterize the electrochemical properties of electrodes. | - Measures impedance spectrum and charge storage capacity in vitro and in vivo [71]. |
| Tungsten Wire & Polyethylene Glycol (PEG) | A temporary rigid shuttle and adhesive for implanting flexible polymer-based electrodes. | - The tungsten wire provides stiffness for insertion; PEG dissolves after implantation, allowing the wire to be retracted [7] [73]. |
Correlative studies that systematically link physical degradation to functional performance are indispensable for advancing the field of chronic neural interfaces. The experimental data clearly show that the relationship between physical integrity and function is not always straightforward, as demonstrated by the superior recording capability of SIROF despite its greater degradation [13] [70]. Furthermore, common simplified metrics like impedance at 1 kHz can be misleading, underscoring the need for comprehensive electrochemical characterization [71].
The future of stable bioelectronics is leaning towards soft, flexible materials that minimize mechanical mismatch with tissue [7] [9] [73]. The standardized methodologies and comparative data presented in this guide provide a framework for researchers to rigorously evaluate these next-generation designs, with the ultimate goal of creating implantable electrodes that remain functional and reliable for decades.
Implantable electrodes are critical components of modern bioelectronic medicine, enabling treatments for neurological disorders and facilitating brain-computer interfaces. The chronic stability of these electrodes directly determines their clinical viability and long-term performance. Among the various materials used, platinum (Pt) and iridium oxide (IrOx) films represent two of the most extensively investigated options, each with distinct electrochemical characteristics and stability profiles. This comparative guide provides an objective analysis of their performance within the broader context of chronic stability assessment for implantable electrodes, synthesizing current research findings to inform material selection for specific applications. The electrochemical interface must maintain stability under demanding biological conditions while ensuring efficient charge transfer, making material properties a paramount consideration for researchers and developers in the field [74] [9].
Performance Comparison: Quantitative Data
The following tables summarize key electrochemical properties and stability metrics for platinum and iridium oxide films, compiled from recent experimental studies.
Table 1: Electrochemical Performance Characteristics
| Performance Parameter | Platinum (Pt) Films | Iridium Oxide (IrOx) Films |
|---|---|---|
| Charge Storage Capacity (CSC) | ~330 mC/cm² (on hierarchical substrates) [75] | >330 mC/cm² (on hierarchical substrates) [75] |
| Impedance at 1 kHz | Reduces substrate impedance by >1 order of magnitude [74] | Reduces substrate impedance by >1 order of magnitude [74] |
| Charge Injection Capacity | Limited, hinders extended applications [74] [75] | High, superior to Pt; suitable for higher charge demands [74] |
| Long-Term Recording Function | Lower likelihood compared to SIROF (Sputtered IrOx) after chronic implantation [70] | Twice as likely to record neural activity than Pt after years of implantation [70] |
Table 2: Chronic Stability and Biocompatibility Assessment
| Stability & Biocompatibility Factor | Platinum (Pt) Films | Iridium Oxide (IrOx) Films |
|---|---|---|
| Adhesion to Smooth Pt-Ir | Cracking after ultrasonic and stability testing [75] | Some shedding after 1-hour sonication; stable in agarose gel and CV tests [75] |
| Adhesion to Hierarchical Pt-Ir | Reduced cracking; significantly enhanced stability [75] | Good stability in agarose gel and CV tests [75] |
| Primary Degradation Mode | Physical damage (cracking) [70] | Diverse degradation; "pockmarked" or "cracked" surfaces [70] |
| Stability in Sensitive Environments | Generally chemically inert | Accelerated dissolution in presence of organic compounds (e.g., ethanol) [76] |
| Stimulation Stability | N/A | AIROF electrodes maintained stable voltage transients during 24-day pulsing in saline and 24-hour in vivo testing [77] |
Experimental Protocols for Stability Assessment
Standardized experimental protocols are essential for obtaining comparable data on electrode material stability. The following section details key methodologies cited in recent literature.
Electrodeposition Protocol
The electrodeposition process is a common method for applying Pt and IrOx coatings onto electrode substrates, often using a standard three-electrode setup (working electrode, reference electrode, and counter electrode) [75].
- NanoPt Deposition: Conducted from an aqueous solution of 5 mM H₂PtCl₆. The process uses cyclic voltammetry (CV) scanned between -0.3 V and 0.3 V (vs. Ag/AgCl) at a rate of 120 mV/s for 180 to 720 cycles [75].
- IrOx Deposition: Performed in an electrolyte containing 4 mM IrClâ‚„, 1 wt% Hâ‚‚Oâ‚‚, and 40 mM oxalic acid, with pH adjusted to approximately 10.5. A constant potential of 0.55 V vs. Ag/AgCl is applied for 15 to 60 minutes [75].
Mechanical Stability Testing
Assessing the adhesion strength of coatings is critical for predicting long-term performance in implantable devices.
- Ultrasonic Testing: Electrodes are submerged in water and subjected to an ultrasonic bath (e.g., 150 W) for up to 60 minutes. Coating integrity is evaluated via optical microscopy and SEM at intervals (e.g., 0, 15, 30, 60 min), with concurrent CV and EIS measurements to track performance changes [75].
- Agarose Gel Test: Electrodes are repeatedly inserted into a soft agarose gel at different positions. This simulates mechanical stress during surgical implantation and evaluates a coating's resistance to shear forces and delamination [75].
Electrochemical and Chronic Stability Testing
- Accelerated Pulsing in Saline: Electrodes are subjected to continuous current pulsing in phosphate-buffered saline (PBS) for extended periods. For instance, Activated Iridium Oxide Film (AIROF) electrodes were pulsed at 80 μA (16 nC/phase) for 24 days. Stability is monitored by tracking the voltage transient (VT) response to ensure electrode polarization remains within safe limits [77].
- In Vivo Stimulation Testing: Following implantation, electrodes are pulsed at various current levels for a defined period. VT responses are recorded via reverse telemetry to monitor changes in the electrode-tissue interface under realistic biological conditions [77].
- Long-Term Human Implantation Analysis: Explanted microelectrode arrays from long-term clinical trials are analyzed using Scanning Electron Microscopy (SEM). This allows for direct quantification of physical degradation (e.g., cracking, pockmarks) and correlation with in vivo functional performance metrics like signal-to-noise ratio and impedance [70].
Failure Analysis and Degradation Pathways
Understanding the failure modes of electrode materials is essential for improving chronic stability.
The diagram above illustrates the distinct degradation pathways for platinum and iridium oxide films. For IrOx, the Lattice Oxygen Mechanism (LOM), predominant in its amorphous form, creates oxygen vacancies that weaken the oxide matrix, making it susceptible to dissolution. This process is dramatically accelerated by the presence of organic compounds like ethanol, which can oxidize on the surface, further destabilizing the lattice [76]. In contrast, Pt films are more susceptible to mechanical failure through cracking, a process influenced by physical stress and cyclic loading [70].
The Scientist's Toolkit: Essential Research Materials
Table 3: Key Reagents and Materials for Electrode Development and Testing
| Material / Reagent | Function / Application | Research Context |
|---|---|---|
| Hexachloroplatinic Acid (H₂PtCl₆) | Precursor salt for electrodeposition of nanostructured platinum (nanoPt) coatings [75]. | Essential for creating high-surface-area Pt films to enhance charge storage capacity [74] [75]. |
| Iridium Tetrachloride (IrClâ‚„) | Primary precursor for the electrodeposition of iridium oxide (IrOx) films [75]. | Used in electrolytes for creating IrOx coatings with high charge injection capacity [75]. |
| Femtosecond Laser | Tool for creating hierarchical micro-nanostructures on Pt-Ir alloy substrates [75]. | Surface structuring drastically improves electrochemical performance and mechanical anchoring of coatings, enhancing adhesion stability [75]. |
| Agarose Gel | Medium for simulating mechanical stresses during electrode implantation [75]. | Used in standardized agarose gel testing to evaluate coating adhesion and resistance to shear forces ex vivo [75]. |
| Phosphate Buffered Saline (PBS) | Standard electrolyte solution for in vitro electrochemical testing (e.g., CV, EIS) [75]. | Provides a consistent and physiologically relevant ionic environment for initial performance and stability characterization [75] [77]. |
The choice between platinum and iridium oxide films involves a critical trade-off between mechanical integrity and electrochemical performance. Platinum films offer robust mechanical stability, particularly on structured substrates, but are limited by lower charge injection capacity and a higher likelihood of signal loss in chronic recordings. Iridium oxide films provide superior charge injection and are more likely to maintain long-term recording functionality, but their stability is highly dependent on crystallinity and can be severely compromised by electrochemical dissolution in specific biological environments. Future research directions include developing composite coatings, optimizing nanostructured substrates for enhanced adhesion, and engineering crystalline IrOx phases that balance high activity with long-term durability. This comparative analysis underscores that material selection must be application-specific, weighing the demands for stimulation efficiency, recording fidelity, and intended functional lifespan within the biological environment.
The clinical success of Brain-Computer Interfaces (BCIs) and neurostimulation therapies hinges on the long-term stability and reliability of implanted electrodes. Chronic implantation presents a significant challenge, as devices must maintain functionality for years within the dynamic and hostile environment of the human body. The foreign body response—a biological reaction to implanted materials—often leads to the formation of an insulating glial scar around the electrode. This scar tissue increases the distance between neurons and recording sites, causing rapid signal attenuation and a sharp rise in impedance, which can ultimately lead to device failure [7]. Furthermore, the electrodes themselves can undergo physical degradation over time, compromising both recording and stimulation capabilities [13]. This review synthesizes evidence from multi-year human clinical trials, objectively comparing the performance, longevity, and stability of various implantable electrode technologies. By examining quantitative data on signal fidelity, electrode longevity, and physical degradation, this guide provides researchers and clinicians with a evidence-based framework for selecting and developing neural interfaces for chronic applications.
Performance Comparison of Major Electrode Platforms
Long-term clinical data from human trials provides critical insights into the real-world performance of different electrode technologies. The table below summarizes key findings from major clinical studies and commercial devices, highlighting the comparative advantages and limitations of each platform.
Table 1: Performance Comparison of Electrodes in Long-Term Human Clinical Trials
| Electrode Type / Study | Implantation Duration | Key Performance Metrics | Stability Findings | Primary Applications |
|---|---|---|---|---|
| Utah Array (BrainGate Trial) [78] | Up to 7.6 years (Mean: 2.8 years) | - 35.6% of electrodes recorded neural spikes- Only 7% signal decline over enrollment- Peak dSNR > 4.5 (approaching able-bodied control of 6.29) | - 11 of 14 arrays provided meaningful movement decoding throughout study- Longevity better than in nonhuman primate studies | BCI for paralysis (computer control, communication) |
| Pt vs. SIROF Electrodes [13] | 956–2130 days (2.6–5.8 years) | - SIROF electrodes twice as likely to record neural activity than Pt (measured by SNR)- 1 kHz impedance correlated with physical damage | - Different degradation patterns: "pockmarked" vs. "cracked" surfaces- Erosion of silicon shank accelerates metal tip damage | Intracortical recording and stimulation |
| Paradromics BCI [79] | Clinical trials starting 2025 | - Targets speech restoration via motor cortex recording- Converts neural patterns to text/synthetic voice | - Initial focus on safety and communication restoration | Speech restoration for severe motor impairments |
| Flexible Deep Brain Electrodes [7] | Research stage (animal studies up to 8 months) | - Reduced glial sheath formation compared to rigid electrodes | - Chronic inflammatory response significantly mitigated- Challenges remain in implantation techniques and long-term signal stability | Neural signal detection, neurological disease treatment |
The data reveals a trade-off between signal quality and biocompatibility. While rigid Utah arrays demonstrate impressive multi-year performance in human trials [78], flexible electrodes show superior biocompatibility and reduced immune response in research settings, though their long-term human clinical data is still emerging [7]. Material choice significantly impacts performance, with sputtered iridium oxide film (SIROF) electrodes outperforming platinum (Pt) in chronic recording applications despite showing greater physical degradation [13].
Table 2: Electrode Material and Design Trade-offs in Chronic Implantation
| Attribute | Rigid Electrodes (e.g., Utah Array) | Flexible Electrodes | SIROF Coating | Platinum Electrodes |
|---|---|---|---|---|
| Signal Quality | High single-neuron resolution maintained for years [78] | Improved chronic signal due to stable tissue contact [7] | Superior recording capability despite physical degradation [13] | Lower signal-to-noise ratio over time [13] |
| Immune Response | Significant glial scarring and chronic inflammation [7] | Reduced inflammation and mechanical mismatch [7] | Not applicable | Not applicable |
| Physical Degradation | Progressive erosion of silicon shank damages tip metal [13] | Mechanical fatigue at interconnects [7] | "Pockmarked" degradation pattern [13] | "Cracked" degradation pattern [13] |
| Implantation Challenges | Standardized surgical procedures | Requires rigid shuttles or stiffness enhancement [7] | Not applicable | Not applicable |
Experimental Protocols for Assessing Chronic Stability
Long-Term Electrophysiological Monitoring
The comprehensive BrainGate trial analysis employed rigorous methodologies to assess array performance across 2,319 recording sessions from 20 arrays in 14 participants [78]. The protocol involved:
- Regular Recording Sessions: Neural data was collected during structured tasks and at rest periods to assess both evoked and spontaneous neural activity.
- Signal Quality Metrics: Electrodes were quantitatively assessed for the presence of neural spiking activity, signal-to-noise ratio (SNR), and impedance measurements.
- Decoding Performance Assessment: Researchers developed a "decoding signal-to-noise ratio" (dSNR) metric to objectively quantify how well neural signals could be translated into control commands for computer cursors or prosthetic devices. This dSNR metric allowed for direct comparison of performance across different arrays and participants [78].
- Longitudinal Tracking: Performance metrics were tracked over time, with some participants contributing data for up to 7.6 years, enabling analysis of performance degradation rates.
The finding that arrays showed only a 7% decline in recording performance over the study enrollment period provides compelling evidence for the long-term viability of properly implanted Utah arrays [78].
Post-Explantation Material Analysis
A critical methodology for understanding failure mechanisms involves detailed analysis of explanted electrodes. A comprehensive study examined 980 electrodes from 11 arrays explanted from three human participants after 956–2130 days of implantation [13]. The protocol included:
- Scanning Electron Microscopy (SEM): High-resolution imaging of explanted electrodes to quantify physical damage patterns, including both "pockmarked" and "cracked" degradation types.
- Correlation with Functional Metrics: Physical damage metrics were systematically correlated with pre-explantation functional performance, including recording quality (SNR, noise characteristics, impedance) and stimulation capability.
- Material Comparison: Parallel analysis of platinum (Pt, n=8 arrays) and sputtered iridium oxide film (SIROF, n=3 arrays) electrodes under identical implantation conditions and durations.
- Damage Localization: Specific attention was paid to damage at the electrode-tissue interface and erosion of the silicon shank, which was hypothesized to accelerate tip metal damage [13].
This multi-modal approach revealed that despite greater physical degradation, SIROF electrodes were twice as likely to record neural activity than Pt electrodes, highlighting the complex relationship between physical integrity and functional performance [13].
Intraoperative Optimization Techniques
Advanced surgical planning and intraoperative monitoring techniques contribute significantly to long-term stability. The "stimulation maps" approach developed for Deep Brain Stimulation (DBS) electrode placement represents a sophisticated methodology for optimizing initial positioning [80]. This technique integrates:
- Patient-Specific Anatomical Modeling: Pre-operative T1 MRI and white-matter attenuation inversion recovery (WAIR) sequences are used to create detailed 3D models of thalamic nuclei and basal ganglia structures.
- Quantitative Symptom Evaluation: Accelerometers attached to the patient's wrist provide quantitative, real-time assessment of tremor improvement during stimulation tests, moving beyond subjective clinical scales.
- Electric Field Simulation: Patient-specific finite element method (FEM) modeling simulates the spatial distribution of the electric field for different stimulation parameters and electrode positions.
- Data Integration and Visualization: The integration of anatomical outlines, quantitative symptom evaluation, and electric field simulations generates "stimulation maps" that divide the stimulation region into areas with different improvement levels, visually guiding optimal lead placement [80].
This methodology demonstrates how intraoperative data collection and computational modeling can be combined to maximize therapeutic effect while minimizing side effects, potentially extending the functional lifespan of the implant.
Visualization of Chronic Stability Assessment Workflow
The following diagram illustrates the integrated experimental workflow for assessing long-term stability of implantable electrodes, from initial implantation to final analysis:
Chronic Electrode Assessment Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful long-term implantation studies require specialized materials and assessment tools. The following table details key resources mentioned in clinical studies and their functional significance for chronic stability research.
Table 3: Essential Research Materials for Chronic Electrode Studies
| Material/Reagent | Function/Application | Significance in Chronic Studies |
|---|---|---|
| Sputtered Iridium Oxide Film (SIROF) | Electrode coating material for recording and stimulation | Demonstrates superior recording capability despite physical degradation; twice as likely to record neural signals vs. platinum [13] |
| Platinum (Pt) Electrodes | Traditional electrode material for neural interfaces | Baseline for comparison; shows different degradation patterns ("cracked" vs. "pockmarked") [13] |
| Polyimide-based Flexible Electrodes | Substrate for flexible neural interfaces | Reduces mechanical mismatch with brain tissue (Young's modulus ~1-10 kPa); mitigates chronic inflammatory response [7] |
| Tungsten Guidance Wires | Implantation shuttle for flexible electrodes | Enables precise placement of flexible electrodes without compromising design integrity [7] |
| Scanning Electron Microscopy (SEM) | High-resolution imaging of explanted electrodes | Quantifies physical degradation patterns and correlates with functional performance [13] |
| Accelerometers | Quantitative tremor assessment during DBS surgery | Provides objective measurement of symptom improvement for optimal electrode positioning [80] |
| Patient-Specific Brain Models | Computational models for surgical planning and simulation | Enables personalized electrode placement and electric field simulation [80] |
| NeuroPort Arrays | Commercial microelectrode arrays for chronic implantation | Platform for long-term human studies (956-2130 days); provides standardized comparison baseline [13] |
The evidence from multi-year human clinical trials demonstrates substantial progress in achieving chronic stability for implantable electrodes. Utah arrays have shown reliable recording capability for up to 7.6 years in human participants, with only minimal degradation in signal quality [78]. Material advancements, particularly SIROF coatings, provide enhanced recording capabilities despite physical degradation [13]. The field is increasingly moving toward flexible electrodes that better match the mechanical properties of neural tissue, reducing chronic immune responses [7]. However, challenges remain in standardizing implantation techniques for flexible devices and understanding the complex relationship between physical degradation and functional performance. As research continues, the integration of advanced materials, sophisticated surgical planning, and comprehensive post-explantation analysis will be crucial for developing neural interfaces that maintain functionality for decades, ultimately enabling lifelong restoration of neurological function for people with disabilities.
Performance Benchmarking Across Different Neural Interface Platforms
Benchmarking the performance of neural interfaces is a critical endeavor for advancing both neuroscience research and clinical neurotechnology. For implantable electrodes, performance is not a single metric but a complex interplay of information transfer capacity, long-term chronic stability, and biocompatibility. The field has historically been challenged by a lack of standardized, application-agnostic benchmarks, making direct comparisons between different technological platforms difficult [81]. Recent initiatives, such as the introduction of the SONIC (Standard for Optimizing Neural Interface Capacity) benchmark, aim to establish rigorous, transparent frameworks for evaluating brain-computer interface (BCI) performance in a holistic manner, accounting for both throughput and latency [81]. This guide provides an objective comparison of contemporary neural interface platforms, focusing on quantitative performance data and the experimental methodologies used to obtain it, all within the critical context of chronic stability for implantable electrodes.
Performance Metrics and Comparative Data
The performance of neural interfaces can be quantified using several key engineering and biological metrics. These metrics collectively define the fidelity, capacity, and longevity of the interface.
Key Performance Metrics
- Information Transfer Rate (ITR): Measured in bits per second (bps), this is a measure of the speed of communication between the brain and an external device. A higher ITR enables more complex and rapid control, which is crucial for applications like conversational speech prostheses [81].
- Latency: The delay between a neural event and the corresponding output from the BCI system, typically measured in milliseconds (ms). Low latency is essential for real-time, closed-loop control, as high delays can make systems clumsy or unusable [81].
- Chronic Stability: The ability of an interface to maintain stable performance over long periods (months to years) after implantation. This is primarily hindered by the foreign body response, which leads to glial scar formation, signal attenuation, and a rise in impedance [7] [82].
- Spatial and Temporal Resolution: Spatial resolution refers to the smallest distinguishable spatial detail in neural activity, while temporal resolution refers to the ability to track rapid changes in neural signals over time. Invasive interfaces generally offer superior resolution on both fronts [83].
- Biocompatibility: The extent to which an implant minimizes the immune response. This is influenced by the material's mechanical properties (e.g., Young's modulus), geometry, and surface functionalization [7] [82].
Comparative Performance of Neural Interface Platforms
The table below summarizes the performance characteristics of various neural interface platforms based on recent public data and scientific literature.
Table 1: Performance Benchmarking of Select Neural Interface Platforms
| Platform / Company | Interface Type | Key Performance Metrics (ITR, Latency) | Reported Chronic Stability & Notes |
|---|---|---|---|
| Paradromics Connexus | Invasive (Intracortical) | >200 bps with 56ms latency; >100 bps with 11ms latency [81] | Preclinical data from sheep; ITR exceeds transcribed human speech (~40 bps) [81] |
| Neuropixels | Invasive (Intracortical) | High channel count (up to 1000+ sites); exceptional spatial resolution [84] | Primarily for acute research; silicon-based probes face chronic stability challenges due to immune response [82] [84] |
| Neuralink | Invasive (Intracortical) | Representative performance for alphabet task is <10 bps (as benchmarked by others) [81] | Utilizes thin-film polymer threads and robotic insertion to minimize acute damage and vasculature [82] |
| Utah Array (Blackrock Neurotech) | Invasive (Intracortical) | Established clinical use; performance lower than newer platforms [83] | The first FDA-approved intracortical array; chronic recording limited by immune response and glial scarring [82] |
| Synchron | Minimally Invasive (Endovascular) | Low information transfer rate (~1 bps as benchmarked by others) [81] | Stent-based electrode array; avoids open-brain surgery, potentially improving safety and reducing acute immune response [83] |
| High-Density Flexible Arrays | Invasive (Intracortical) | High-quality single-unit recordings [7] | Mesh electronics have shown stable recordings for ~4 months in rodents with reduced chronic inflammation [7] [84] |
Experimental Protocols for Benchmarking and Stability Assessment
To ensure objective comparisons, a clear understanding of the experimental protocols used to generate performance data is essential.
The SONIC Benchmarking Protocol
Paradromics developed the SONIC benchmark to provide an application-agnostic measure of a BCI system's core engineering performance. The methodology is as follows [81]:
- Objective: To measure the mutual information between a presented stimulus and the BCI's decoded output.
- Model System: Preclinical experiments in sheep.
- Stimulus Presentation: Controlled sequences of sounds (five-note musical tones) are played to the animal. Each unique five-tone sequence is mapped to a specific character, creating a "dictionary."
- Neural Recording: The fully implanted BCI system records neural activity from the auditory cortex during stimulus presentation.
- Decoding and Analysis: The recorded neural signals are used to predict which sounds were presented. The mutual information between the presented and predicted sounds is calculated, yielding the ITR in bits per second. This protocol explicitly accounts for system latency.
Assessing Chronic Stability and Biocompatibility
Evaluating the long-term stability of neural interfaces involves histological and functional assessments to quantify the foreign body response. Key methodologies include [7]:
- Histological Analysis: Post-implantation, brain tissue is sectioned and stained to identify specific cell types.
- Immunostaining for Microglia and Astrocytes: markers like Iba1 (for microglia) and GFAP (for astrocytes) are used to visualize and quantify the activation of these glial cells around the implant.
- Neuronal Density Staining: markers like NeuN are used to count neuronal nuclei in the vicinity of the implant. A higher neuronal density near the interface indicates better biocompatibility.
- Functional Electrophysiology: The quality of neural signals is tracked over time.
- Signal-to-Noise Ratio (SNR): A decline in SNR can indicate tissue encapsulation.
- Electrode Impedance: A sustained increase in impedance is a classic sign of glial scar formation around the electrode site.
- Single-Unit Yield: The number of detectable single neurons over time is a direct measure of functional stability.
Workflow for Neural Interface Benchmarking
The following diagram illustrates the integrated workflow for benchmarking both the engineering performance and chronic stability of a neural interface, synthesizing the protocols described above.
The Scientist's Toolkit: Research Reagents and Materials
The development and evaluation of high-performance neural interfaces rely on a suite of specialized materials and reagents. The table below details key items central to this field.
Table 2: Essential Research Toolkit for Neural Interface Development & Assessment
| Category / Item | Specific Examples | Function & Rationale |
|---|---|---|
| Electrode Materials | Polyimide, Parylene-C, SU-8 [7] | Flexible polymer substrates used to create soft neural probes that reduce mechanical mismatch with brain tissue, thereby mitigating chronic inflammation. |
| Conductive Materials | Platinum, Iridium Oxide, Gold, Carbon Nanotubes [82] | Form the electrode sites for recording and stimulation. Materials like IrOx offer high charge injection capacity crucial for safe and effective stimulation. |
| Barrier/Packaging | Silicon Dioxide (SiO₂), Silicon Nitride (Si₃N₄) [82] | Inorganic barrier layers critical for protecting implantable electronics from the corrosive in vivo environment (water, ions) to ensure long-term device functionality. |
| Histological Stains | Antibodies for Iba1, GFAP, NeuN [7] | Immunohistochemical markers used to identify and quantify microglia (Iba1), astrocytes (GFAP), and neurons (NeuN) to assess the foreign body response and biocompatibility. |
| Functional Probes | Genetically Encoded Calcium Indicators (e.g., GCaMP) [84] | Fluorescent sensors that report neural activity via changes in intracellular calcium levels, enabling optical recording complementary to electrophysiology. |
The landscape of neural interface platforms is diverse, with technologies ranging from minimally invasive endovascular stents to high-channel-count intracortical arrays, each offering distinct trade-offs between performance, invasiveness, and long-term stability. The emergence of standardized benchmarking protocols like SONIC is a significant step toward transparent and objective performance comparisons, highlighting the critical importance of both information transfer rate and latency [81]. Ultimately, the choice of a neural interface platform is dictated by the specific research or clinical application. However, the overarching challenge across all invasive technologies remains the achievement of chronic stability. Future progress hinges on the continued development of "stealth" interfaces through material science innovations that minimize the foreign body response, coupled with robust engineering benchmarks that ensure these devices can deliver high-fidelity performance not just for weeks, but for decades [7] [82].
Reliability Assessment of Integrated System Components Beyond the Electrode-Tissue Interface
In the field of implantable bioelectronic medicines, research has historically focused on the critical electrode-tissue interface, where issues like the foreign body response and glial scarring can degrade signal quality over time [11] [60]. However, for devices intended for chronic, long-term implantation—ranging from deep brain stimulators (DBS) to neuromusculoskeletal prostheses—the reliability of the entire integrated system is paramount for clinical success [9] [85]. System failures often originate not at the interface, but from the physical degradation of other components, including the electrode wires, interconnects, and encapsulation, which are continuously subjected to a harsh biomechanical and chemical environment [85] [13]. This review moves beyond the tissue interface to objectively compare the failure modes and reliability of these integrated system components, providing a synthesized analysis of quantitative performance data and the standardized experimental protocols required to assess them.
Comparative Analysis of Component Reliability and Failure Modes
The chronic stability of an implantable system is compromised by the synergistic effect of multiple failure modes. The table below summarizes the primary abiotic (non-biological) failure mechanisms affecting system components, based on long-term implantation studies and accelerated reliability testing.
Table 1: Key Failure Modes of Integrated System Components in Chronic Implants
| System Component | Primary Failure Modes | Impact on Function | Supporting Experimental Evidence |
|---|---|---|---|
| Electrode Wires/Leads | Fatigue fracture from cyclic mechanical stress (bending, twisting, stretching) [85]. | Intermittent or permanent loss of signal recording/stimulation capability [85]. | Analysis of DBS electrode wires shows fractures from neck movement-induced stress [85]. |
| Electrode Metallization | Corrosion and dissolution of metal coatings (e.g., Platinum, SIROF) in saline environment [13] [60]. | Increased electrode impedance, reduced charge injection capacity, and signal-to-noise ratio (SNR) degradation [13]. | SEM of human-explanted arrays (956-2130 days) shows "cracked" and "pockmarked" degradation on Pt and SIROF surfaces [13]. |
| Insulation/Encapsulation | Delamination (e.g., of Parylene C), cracking, and water permeation [9] [72]. | Current leakage, short circuits, and failure of microelectronics [9]. | SEM scoring of Utah arrays post-explant identified Parylene C delamination and cracks as common damage categories [72]. |
| Microelectrode Shank | Erosion and fracture of the silicon substrate [13]. | Mechanical failure of the electrode structure, potentially leading to complete channel failure [13]. | Long-term human study hypothesizes biotic processes erode the silicon core after metal tip damage is initiated [13]. |
Quantitative data from explant studies provides direct evidence of these degradation processes. A systematic analysis of 980 microelectrodes explanted from humans after 956-2,130 days of service revealed distinct material damage. Platinum (Pt)-coated electrodes exhibited physical degradation, but Sputtered Iridium Oxide Film (SIROF) electrodes were twice as likely to record neural activity despite showing greater physical degradation, as measured by Signal-to-Noise Ratio (SNR) [13]. Furthermore, a study of eleven explanted Utah arrays found that damage was more severe on outer-edge electrodes than on inner electrodes, highlighting the role of spatial location in mechanical stress [72].
Standardized Experimental Protocols for Reliability Assessment
To predict and improve the long-term performance of implants, standardized in vitro reliability tests that simulate the harsh in vivo environment are essential.
Mechanical Fatigue Testing
Mechanical forces, particularly from body movements, are a major cause of lead fracture. A tailored testing scheme for DBS electrode wires incorporates three key tests to simulate these stresses [85].
Table 2: Protocols for Mechanical Fatigue Testing of Electrode Wires
| Test Type | Protocol Summary | Simulated In-Vivo Condition |
|---|---|---|
| Bending Fatigue Test | - Vertically mount wire section on apparatus.- Apply cyclic vertical swing at ±45° angle.- Frequency: 2 Hz.- Monitor for morphological changes [85]. | Neck bending motions [85]. |
| Twisting Fatigue Test | - Vertically mount wire section on torsion apparatus.- Apply cyclic horizontal swing at ±45°.- Frequency: 2 Hz.- Record twisting angle and stress [85]. | Neck twisting motions [85]. |
| Tensile Fatigue Test | - Horizontally secure one end of wire.- Apply cyclic tensile force to the other end.- Frequency: 2 Hz.- Measure tensile deformation and stress [85]. | Muscle tissue activity and stretching [85]. |
Accelerated Aging in Simulated Biological Environment
The body's saline environment and core temperature of 37°C create conditions that accelerate material corrosion and polymer degradation. An accelerated test protocol combines high temperature and saline exposure to mimic long-term aging in a shorter timeframe [85].
Procedure:
- Condition Setting: Place the electrode wire test section in a high-temperature environment of 65°C.
- Saline Immersion: Submerge the test section in a 0.9 g/L physiological saline solution.
- Aging Duration: Allow continuous aging for several hours. The duration is calculated using the Arrhenius model to achieve a predetermined acceleration factor, correlating high-temperature aging rates with those at body temperature [85].
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key materials and their functions as derived from the cited experimental research, providing a resource for replicating studies or developing new prototypes.
Table 3: Research Reagent Solutions and Materials for Reliability Testing
| Item Name | Function in Research/Testing | Experimental Context |
|---|---|---|
| Physiological Saline (0.9 g/L) | Simulates the ionic composition and corrosivity of body fluids in accelerated aging tests [85]. | Used in high-temperature accelerated tests to replicate the bodily fluid environment [85]. |
| Platinum (Pt) & Iridium Oxide (SIROF) | Metallization materials for electrode tips, enabling electrical contact. Compared for long-term durability [13]. | SEM analysis compared degradation of Pt and SIROF on explanted arrays from humans [13]. |
| Parylene C | A biocompatible polymer used for insulating and encapsulating electrodes and circuits [9] [72]. | Its delamination and cracking were identified as key failure modes in explanted Utah arrays [72]. |
| Scanning Electron Microscopy (SEM) | A critical imaging technique for post-mortem analysis of explanted devices to quantify physical degradation [13] [72]. | Used to score damage on 980 electrodes from human studies, correlating physical state with performance [13] [72]. |
| Platinum-Iridium (Pt90/Ir10) & Stainless Steel 316 LVM | Materials for implantable electrode contacts (Epimysial) and wires (Intramuscular) [86]. | Used in a comparative study of epimysial and intramuscular electrodes for prosthetic control [86]. |
Visualizing Reliability Assessment Workflows
The following diagram illustrates the integrated logical workflow for assessing the reliability of implantable system components, from in vitro testing to in vivo performance analysis and design improvement.
Diagram 1: Integrated Workflow for Implantable System Component Reliability Assessment. This workflow shows how standardized in vitro tests simulate the in vivo environment, and how data from explanted devices is used to close the loop for iterative design improvements.
The failure mechanisms identified through the above workflow are complex and interrelated. The following diagram maps the causal pathways leading to the ultimate failure of the neural interface.
Diagram 2: Failure Mechanism Pathways in Implantable Bioelectronic Systems. This causal map illustrates how the body's mechanical and chemical environment drives specific failure modes in system components, ultimately leading to the loss of device function.
Conclusion
The pursuit of chronically stable implantable electrodes requires a multifaceted approach that addresses the complex interplay between biological responses and engineering solutions. Key takeaways include the critical importance of minimizing the foreign body response through mechanical compatibility, the value of active anti-inflammatory strategies through drug-eluting coatings, and the necessity of robust assessment methodologies that correlate physical degradation with functional performance. Future directions should focus on the development of smart, adaptive interfaces that can actively modulate their local environment, the integration of AI for real-time performance monitoring, and the creation of standardized validation frameworks that bridge preclinical testing and clinical outcomes. As these technologies evolve, they promise to unlock new frontiers in bioelectronic medicine, enabling lifelong neural interfaces that maintain stable performance for treating neurological disorders and restoring neural functions.
References
- 1. Molecular Signaling in Biomaterial-induced Foreign Body ... [https://pubmed.ncbi.nlm.nih.gov/40981767/]
- 2. Foreign Body Reaction to Implanted Biomaterials and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8081831/]
- 3. Material and design strategies for chronically-implantable ... [https://www.nature.com/articles/s41427-025-00613-8]
- 4. Advanced strategies to thwart foreign body response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9472022/]
- 5. Biomimetic optimization of silicone breast implant integration [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1668930/full]
- 6. Allometrically scaling tissue forces drive pathological ... [https://www.nature.com/articles/s41551-023-01091-5]
- 7. Long-term stability strategies of deep brain flexible neural ... [https://www.nature.com/articles/s41528-025-00410-x]
- 8. Significantly reduced inflammatory foreign-body-response ... [https://www.sciencedirect.com/science/article/pii/S1742706123000065]
- 9. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 10. Mechanical Characterization of Brain Tissue - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12045392/]
- 11. Revolutionizing brain‒computer interfaces - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243264/]
- 12. Overcoming failure: improving acceptance and success of ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00168-7]
- 13. Quantifying physical degradation alongside recording and ... [https://www.sciencedirect.com/science/article/pii/S1742706125001151]
- 14. Novel method to improve the biocompatibility and chronic ... [https://www.news-medical.net/news/20250630/Novel-method-to-improve-the-biocompatibility-and-chronic-stability-of-neural-electrode-implants.aspx]
- 15. Glial responses to implanted electrodes in the brain - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6261524/]
- 16. Advancing the interfacing performances of chronically ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1275908/full]
- 17. Dissecting the Dual Role of the Glial Scar and ... [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2020.00078/full]
- 18. Function of GSK‑3 signaling in spinal cord injury (Review) [https://www.spandidos-publications.com/10.3892/etm.2023.12240]
- 19. Anti-IL-20 antibody improved motor function and reduced glial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7227062/]
- 20. Spinal Cord Injury Scarring and Inflammation [https://www.sciencedirect.com/science/article/pii/S1878747923010437]
- 21. Engineering aspects and materials for next generation ... [https://www.sciencedirect.com/science/article/pii/S1877117325001279]
- 22. Blood-brain barrier disruption: a culprit of cognitive decline? [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-024-00563-3]
- 23. Blood–Brain Barrier Breakdown in Neuroinflammation [https://www.mdpi.com/1422-0067/24/16/12699]
- 24. NLRP3 activation induces BBB disruption and neutrophil ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-025-03468-6]
- 25. Progressive Blood–Brain Barrier Disruption in Sleep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361337/]
- 26. Endothelial TDP-43 depletion disrupts core blood–brain ... [https://www.nature.com/articles/s41593-025-01914-5]
- 27. Blood–brain barrier disruption and sustained systemic ... [https://www.nature.com/articles/s41593-024-01576-9]
- 28. Achieving long-term stability of thin-film electrodes for ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706121003056]
- 29. Stimulation Stability and Selectivity of Chronically Implanted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2927980/]
- 30. Signal properties and stability of a chronically implanted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12486012/]
- 31. Signal properties and stability of a chronically implanted ... [https://www.medrxiv.org/content/10.1101/2025.09.19.25335897v1]
- 32. A high-density multi-electrode platform examining the ... [https://www.nature.com/articles/s41598-024-71038-6]
- 33. Electrical activity controls area-specific expression of neuronal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5582867/]
- 34. Pseudo vs. True Reference Electrodes: An Electrochemist's ... [https://www.zimmerpeacock.com/2025/10/14/pseudo-vs-true-reference-electrodes-an-electrochemists-guide/]
- 35. How to select the right reference electrode? [https://www.biologic.net/topics/how-to-select-the-right-reference-electrode/]
- 36. Bringing sensation to prosthetic hands—chronic ... [https://www.nature.com/articles/s41528-023-00284-x]
- 37. A comparative study of electrochemical stability and ... [https://www.sciencedirect.com/science/article/abs/pii/S0013468624007679]
- 38. Basics of Electrochemical Impedance Spectroscopy [https://www.gamry.com/application-notes/EIS/basics-of-electrochemical-impedance-spectroscopy/]
- 39. Electrochemical Impedance Spectroscopy (EIS) Basics [https://pineresearch.com/support-article/eis-basics/]
- 40. Robust interpretation of electrochemical impedance ... [https://arxiv.org/html/2510.17835v1]
- 41. Quantifying physical degradation alongside recording and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11419230/]
- 42. Scanning electron microscopy of chronically implanted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4854331/]
- 43. Innovative Damage Assessment of Endodontic Instruments ... [https://www.mdpi.com/2039-7283/15/1/3]
- 44. Histological Evaluation of a Chronically-implanted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4993459/]
- 45. Chronically Implanted Intracranial Electrodes: Tissue ... [https://www.mdpi.com/2072-666X/9/9/430]
- 46. Comparative evaluation of different histoprocessing methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC5426407/]
- 47. Overcoming failure: improving acceptance and success of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11907899/]
- 48. Accelerated and Real-Time Aging Services [https://www.steris-ast.com/solutions/testing-and-validation/packaging-testing/accelerated-and-real-time-aging]
- 49. ICH versus Accelerated Predictive Stability Studies [https://pmc.ncbi.nlm.nih.gov/articles/PMC9693625/]
- 50. PEDOT:PSS conducting eutectogel for enhanced electrical ... [https://pubs.rsc.org/en/content/articlehtml/2025/tc/d5tc03054d?page=search]
- 51. Biomechanics characterization of an implantable ultrathin ... [https://www.nature.com/articles/s41598-025-04737-3]
- 52. Bio-inspired electronics: Soft, biohybrid, and “living†neural ... [https://www.nature.com/articles/s41467-025-57016-0]
- 53. Recent Progress of Soft and Bioactive Materials in Flexible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12038164/]
- 54. Recent Advances in Flexible Sensors for Neural Interfaces [https://www.mdpi.com/2079-6374/15/7/424]
- 55. Medical Electronics that Match the Stretchability of Human ... [https://viterbischool.usc.edu/news/2025/09/medical-electronics-that-match-the-stretchability-of-human-tissue/]
- 56. Comparison between SBMA and MPC coatings on PEEK ... [https://www.nature.com/articles/s41598-025-25082-5]
- 57. Functionalization of Implantable Systems for Controlled ... [https://link.springer.com/article/10.1007/s40883-025-00401-4]
- 58. Hybrid surface layers with antibacterial and anti- ... [https://www.sciencedirect.com/science/article/pii/S221395672500146X]
- 59. Nanoparticle-based drug delivery systems targeting ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1657300/full]
- 60. Implantable intracortical microelectrodes: reviewing the ... [https://www.nature.com/articles/s41378-022-00451-6]
- 61. The effect of implant shape and bone preparation on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2967812/]
- 62. Comparison of decoding resolution of standard and high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6508958/]
- 63. Long-Term Clinical Outcomes of Wedge-Shaped Implants ... [https://www.mdpi.com/2077-0383/14/17/6299]
- 64. A systematic assessment of the stability of SLA® vs. ... [https://www.nature.com/articles/s41432-024-01097-1]
- 65. Advances in bioelectronics for neural interfacing [https://link.springer.com/article/10.1557/s43579-025-00822-w]
- 66. Advanced development of conductive biomaterials for ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra01107h]
- 67. Nature-inspired surface modification strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11925587/]
- 68. Bioactive Neuroelectronic Interfaces [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2019.00269/full]
- 69. Progress and challenges of implantable neural interfaces ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-021-00067-7]
- 70. Quantifying physical degradation alongside recording and ... [https://pubmed.ncbi.nlm.nih.gov/40037510/]
- 71. Comparison of the In Vitro and In Vivo Electrochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8779563/]
- 72. Material Damage to Multielectrode Arrays after Electrolytic ... [https://elifesciences.org/reviewed-preprints/106452]
- 73. Fully flexible implantable neural probes for ... [https://www.nature.com/articles/s41378-024-00685-6]
- 74. Electrodeposited coatings for neural electrodes: A review [https://www.sciencedirect.com/science/article/abs/pii/S0956566325003665]
- 75. A Comparative Study on the Effect of Substrate Structure ... [https://www.mdpi.com/2072-666X/15/1/70]
- 76. Accelerated dissolution of iridium anode in the presence of ... [https://www.nature.com/articles/s41467-025-63992-0]
- 77. Chronic stability of activated iridium oxide film voltage ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9393423/]
- 78. Long-term performance of intracortical microelectrode ... [https://www.medrxiv.org/content/10.1101/2025.07.02.25330310v1]
- 79. A brain implant that could rival Neuralink's enters clinical ... [https://www.nature.com/articles/d41586-025-03849-0]
- 80. Stimulation maps: visualization of results of quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7156362/]
- 81. Think Fast | Setting new standards and new records for ... [https://www.paradromics.com/blog/bci-benchmarking]
- 82. Recent advances in neural interfaces—Materials chemistry to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8536148/]
- 83. Brain Computer Interfaces 2025-2045: Technologies, ... [https://www.idtechex.com/tw/research-report/brain-computer-interfaces/1024]
- 84. Neuron devices: emerging prospects in neural interfaces ... [https://www.nature.com/articles/s41378-022-00453-4]
- 85. Design of reliability test for nerve electrode wires of deep ... [https://www.spiedigitallibrary.org/conference-proceedings-of-spie/13513/1351322/Design-of-reliability-test-for-nerve-electrode-wires-of-deep/10.1117/12.3045622.full]
- 86. Comparing implantable epimysial and intramuscular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12206804/]