Biocompatibility in Organic Bioelectronics: Materials, Mechanisms, and Clinical Translation
This article provides a comprehensive overview of biocompatibility in organic bioelectronics, a field poised to revolutionize medical implants and wearable devices.
Biocompatibility in Organic Bioelectronics: Materials, Mechanisms, and Clinical Translation
Abstract
This article provides a comprehensive overview of biocompatibility in organic bioelectronics, a field poised to revolutionize medical implants and wearable devices. Tailored for researchers and drug development professionals, it explores the foundational principles of designing soft, conformable electronic materials that interface seamlessly with biological tissues. The scope spans from core material properties and underlying mechanisms to advanced fabrication techniques for implantable sensors and drug delivery systems. It critically addresses persistent challenges in long-term stability and immune response, while also presenting rigorous in vitro and in vivo validation frameworks. By synthesizing current research and emerging trends, this review serves as a strategic guide for developing the next generation of safe, effective, and clinically viable bioelectronic therapeutics.
The Foundations of Biocompatibility: Why Organic Electronics Uniquely Interface with Biology
The emergence of implantable bioelectronics represents a paradigm shift in therapeutic interventions, offering novel treatments for conditions ranging from neurological disorders to chronic inflammatory diseases. These advanced medical devices interface directly with the body's electrically active tissues to modulate neural activity, monitor physiological signals, and deliver targeted therapies. Unlike traditional pharmaceuticals, bioelectronic medicine operates through precise electrical modulation of specific neural pathways, potentially offering higher specificity and fewer systemic side effects [1]. The fundamental requirement for the successful integration and long-term function of these devices is biocompatibility – the ability of a medical device or material to perform with an appropriate host response in a specific application [2]. For implantable bioelectronics, this extends beyond traditional material safety to encompass seamless integration with biological tissues without provoking adverse immune responses, maintaining stable electrical performance in physiological environments, and ensuring long-term reliability despite continuous mechanical stress from dynamic biological surroundings.
The field of organic bioelectronics has significantly advanced this frontier by developing carbon-based semiconducting materials that uniquely match the mechanical and conduction properties of biological tissues [3]. These materials demonstrate inherent flexibility, biocompatibility, and the capacity to carry both electrical and ionic impulses, making them ideal for interfacing human tissue with electronic technology [4]. This review examines the evolving framework for defining, evaluating, and ensuring biocompatibility for implantable bioelectronics, spanning international standards, material innovation, testing methodologies, and clinical translation challenges.
Regulatory Framework and ISO 10993-1:2025 Updates
The Risk-Based Approach to Biological Evaluation
The International Standard ISO 10993-1 serves as the cornerstone for biological evaluation of medical devices, defining principles and requirements for assessing biological safety within a risk management framework [5]. The 2025 edition represents a significant evolution, creating a tighter integration with the risk management process outlined in ISO 14971. Biological evaluation is now formally positioned as an integral component of the overall risk management process, requiring identification of biological hazards, definition of biologically hazardous situations, and establishment of potential biological harms [6].
This updated framework introduces a structured biological evaluation process that mirrors ISO 14971's lifecycle approach, ensuring biological safety is assessed from initial design through post-market surveillance [6]. The standard now explicitly requires biological risk estimation based on severity and probability of harm, followed by biological risk control measures to mitigate unacceptable risks. This paradigm shift means one cannot effectively implement ISO 10993-1:2025 without simultaneously applying the risk management principles of ISO 14971 [6].
Key Updates in the 2025 Revision
Integration of Foreseeable Misuse: The standard now requires consideration of reasonably foreseeable misuse during biological risk assessment. For example, using a device longer than intended by the manufacturer, resulting in longer exposure duration, must be evaluated. This assessment should leverage post-market surveillance data and clinical literature to identify systematic misuse patterns [6].
Refined Exposure Assessment: The standard provides clearer definitions for determining contact duration, introducing concepts of "total exposure period" (number of contact days between first and last use), "contact day" (any contact within a 24-hour period), and distinctions between "daily contact" and "intermittent contact" [6]. The term "transitory" has been removed while "very brief contact" (less than one minute) remains with the understanding that such exposure typically presents negligible risk of biological harm [6].
Bioaccumulation Considerations: Manufacturers must now assess whether chemicals present in devices are known to bioaccumulate. When bioaccumulation is expected, the contact duration must be classified as long-term (>30 days) unless otherwise justified, requiring deeper material characterization and risk assessment [6].
FDA Guidance and Regulatory Alignment
The U.S. Food and Drug Administration recognizes the ISO 10993 series as Consensus Standards and has published detailed guidance documents specifically addressing the use of ISO 10993-1 for premarket applications [7]. The FDA's guidance incorporates several additional considerations, including risk-based approaches to determine if biocompatibility testing is needed, chemical assessment recommendations, and special considerations for devices with submicron or nanotechnology components or in situ polymerizing materials [7]. Recent updates also emphasize the "3Rs approach" (reduction, refinement, and replacement of animal testing) and provide more detailed requirements for chemical characterization per ISO 10993-18 [2].
Table 1: Key Biological Safety Endpoints per ISO 10993-1
| Endpoint | Description | Examples of Assessment Methods |
|---|---|---|
| Cytotoxicity | Cell damage or death | Direct contact, agar diffusion, extract dilution |
| Sensitization | Allergic reaction | Guinea pig maximization test, local lymph node assay |
| Irritation | Localized inflammatory response | Intracutaneous reactivity, skin irritation tests |
| Systemic Toxicity | Effects on entire organism | Acute, subacute, subchronic toxicity studies |
| Genotoxicity | Damage to genetic material | Ames test, chromosomal aberration assay |
| Carcinogenicity | Cancer-causing potential | Long-term rodent studies, cell transformation |
| Implantation Effects | Local effects after implantation | Histopathological evaluation of implant sites |
Material Considerations for Implantable Bioelectronics
The Shift to Soft and Flexible Materials
Traditional implantable electronics utilizing rigid materials like silicon and metals create mechanical mismatch with soft biological tissues, leading to complications such as microinjury, inflammation, fibrosis, and eventual device failure [1]. This mechanical disparity triggers a foreign body response, where the immune system recognizes the implant as a foreign object, resulting in fibrous encapsulation that isolates the device from target tissue and compromises signal integrity [4]. The field has consequently shifted toward soft, flexible bioelectronic devices that match the mechanical properties of biological tissues.
Table 2: Mechanical Properties Comparison: Traditional vs. Advanced Materials
| Material Category | Example Materials | Young's Modulus | Advantages | Disadvantages |
|---|---|---|---|---|
| Traditional Rigid Electronics | Silicon, Gold, Polyimide | >1 GPa | Established fabrication, stable performance | Mechanical mismatch causes inflammation |
| Medical Grade Elastomers | BIIR, PDMS, Polyurethane | 1 kPa - 1 MPa | Excellent biocompatibility, shock absorption | May require specialized processing |
| Conducting Polymers | PEDOT:PSS, PANI | 20 kPa - 3 GPa | Mixed ionic-electronic conduction | Potential long-term stability challenges |
| Hydrogels | Alginate, Hyaluronic acid-based | ~10 kPa | Similar modulus to excitable tissues | Limited semiconductor capabilities |
Recent breakthroughs demonstrate this principle through elastomeric organic field-effect transistors made from blends of semiconducting nanofibers and biocompatible elastomers. These composites exhibit mechanical stretchability with similar Young's modulus to human tissues while maintaining stable electrical performance under strain up to 50% [8]. Specifically, devices utilizing bromo isobutyl–isoprene rubber (BIIR) – a medical-grade elastomer meeting stringent biocompatibility standards – combined with semiconducting polymers have demonstrated stable operation in logic circuits under physiological conditions with minimal inflammatory response in vivo [8].
Organic Electronic Materials
Organic electronic materials provide unique advantages for bioelectronic interfaces due to their mechanical compatibility and mixed conduction capabilities. These carbon-based semiconducting materials can be engineered to be flexible, elastic, biodegradable, or biocompatible, enabling seamless integration with biological systems [3]. Their fundamental advantage lies in capacity for mixed conduction – facilitating transport of both electrons and ions – which is crucial for interfacing with biological systems where communication typically occurs through ionic mechanisms [4].
Conductive polymers like Poly(3,4-ethylenedioxythiophene) polystyrene sulfonate (PEDOT:PSS) have demonstrated particular promise, creating nerve interfaces that remained stable for over 7 months in vivo [4]. These materials can be processed using low-cost techniques like inkjet printing, spray coating, and spin coating, enabling fabrication of ultra-thin, lightweight devices that can be seamlessly integrated with biological tissues [3].
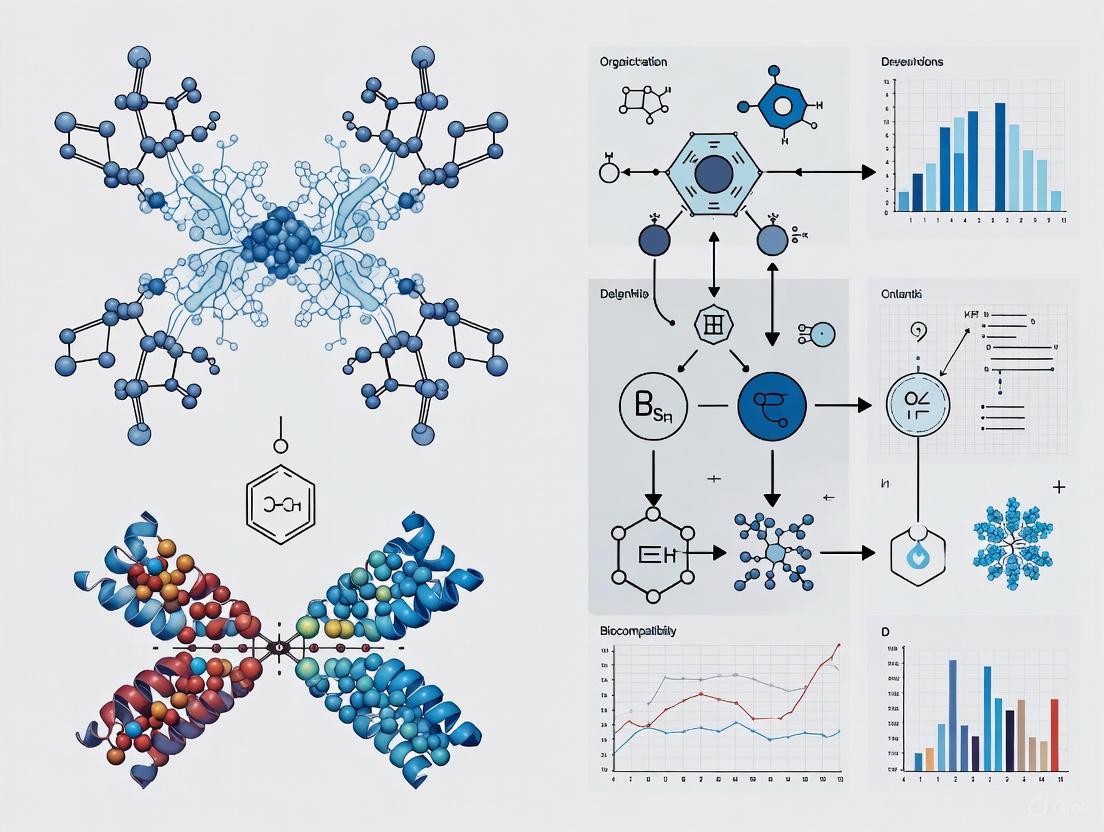
Figure 1: Property-to-Function Relationship in Organic Bioelectronic Materials
Testing Methodologies and Experimental Protocols
ISO 10993 Biocompatibility Testing Framework
The biological evaluation of medical devices follows a structured approach outlined in ISO 10993, requiring different tests based on the nature and duration of body contact. For implantable bioelectronics, which typically fall under "externally communicating" or "implant" devices with prolonged or long-term contact duration, a comprehensive testing strategy is essential [2].
The evaluation process begins with chemical characterization per ISO 10993-18, which identifies and quantifies constituent materials and extractable substances. This is followed by a battery of tests assessing various biological endpoints:
In vitro cytotoxicity tests (ISO 10993-5): Determine if device materials contain harmful extractables that cause cell death or damage. Common assays include mitochondrial dehydrogenase performance measurement (MTT assay), XTT cell proliferation assay, and neutral red uptake cytotoxic assay [4].
Sensitization and irritation tests (ISO 10993-10): Evaluate potential for allergic contact dermatitis and localized inflammatory responses.
Systemic toxicity assays (ISO 10993-11): Assess effects on entire organism through acute, subacute, subchronic, and chronic toxicity studies.
Genotoxicity tests (ISO 10993-3): Screen for damage to genetic material using bacterial reverse mutation tests (Ames test) and mammalian cell chromosomal aberration assays.
Implantation studies (ISO 10993-6): Evaluate local effects after implantation in living tissue, typically assessed through histopathological evaluation of implant sites after explanation.
Figure 2: Biological Evaluation Workflow for Implantable Bioelectronics
Advanced Testing Protocols for Bioelectronics
Beyond standard ISO testing, implantable bioelectronics require specialized evaluations addressing their unique functional requirements:
Electrical Performance in Physiological Environments: Assessing maintained functionality during continuous exposure to biofluids. This includes evaluating insulation resistance, electrode impedance, and stimulus efficacy after accelerated aging in simulated physiological solutions [1].
Mechanical Reliability Under Dynamic Strain: Testing operational stability during repeated mechanical deformation mimicking body movements. For neural interfaces, this includes assessing signal fidelity during cyclic bending and stretching [8].
Long-term Biostability: Evaluating material degradation and foreign body response over extended implantation periods. Advanced protocols include multimodal characterization of explanted devices using electron microscopy, spectroscopic analysis, and electrochemical impedance spectroscopy [4].
Functional Integration with Neural Tissue: Assessing device-tissue integration through immunohistochemical analysis of neuronal and glial markers at the interface, quantifying neuronal density, astrocyte activation, and microglial response [4].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Bioelectronics Biocompatibility Research
| Reagent/Material | Function | Application Examples |
|---|---|---|
| BIIR (Bromo Isobutyl–Isoprene Rubber) | Medical-grade elastomer matrix | Provides biocompatibility and mechanical flexibility in semiconductor blends [8] |
| PEDOT:PSS | Conductive polymer with mixed conduction | Neural interface electrodes, transistor channels [4] |
| DPPT-TT Semiconductor | Donor-acceptor semiconducting polymer | Creates stretchable semiconducting nanofiber networks [8] |
| Poly-l-lysine | Positively charged adhesion promoter | Enhances cell adhesion to hydrophobic semiconductor surfaces [4] |
| Sulfur Vulcanization System | Chemical crosslinking of elastomers | Enhances mechanical properties of rubber-based semiconductors [8] |
| Dual-layer Ag/Au Metallization | Stretchable, corrosion-resistant electrodes | Maintains conductivity in biofluid environments [8] |
| JTE-952 | JTE-952, MF:C30H34N2O6, MW:518.6 g/mol | Chemical Reagent |
| Enpp-1-IN-26 | Enpp-1-IN-26, MF:C16H12FN5O2S, MW:357.4 g/mol | Chemical Reagent |
Emerging Technologies and Clinical Translation
Innovative Bioelectronic Platforms
Recent technological advances have produced increasingly sophisticated bioelectronic platforms with enhanced biocompatibility:
Circulatronics: MIT researchers have developed microscopic wireless electronic devices that travel through blood vessels and autonomously self-implant in target brain regions. These cell-electronics hybrids fuse the versatility of electronics with biological transport capabilities of living cells, enabling implantation without invasive surgery and without triggering immune rejection [9].
Soft, Injectable Electronics: Ultra-flexible mesh electronics capable of injection into target tissues with minimal damage, creating stable long-term interfaces with neurons without chronic immune response [1].
Bioresorbable Electronics: Temporary devices that dissolve after a prescribed operational period, eliminating need for surgical extraction. These systems maintain functionality during treatment timelines then safely resorb [1].
Clinical Outcomes and Performance Metrics
The ultimate validation of biocompatibility comes from clinical performance. Successful implantable bioelectronics demonstrate:
Stable Long-term Function: Devices like poly(3,4-ethylenedioxythiophene) (PEDOT) neural interfaces have maintained functionality for over 7 months in vivo without significant signal degradation [4].
Minimal Foreign Body Response: Advanced materials showing reduced fibrotic encapsulation, with histopathological analysis revealing integration within neural tissue without significant glial scarring [8].
Preserved Tissue Integrity: Biocompatible elastomeric transistors show no adverse effects on cell viability, proliferation, or migration in vitro, and no major inflammatory response or tissue damage in vivo [8].
Challenges in Reliability and Stability
Despite significant advances, long-term reliability of implantable bioelectronics remains challenging. Key failure modes include:
Water Permeation and Encapsulation Failure: Degradation of barrier layers allowing biofluid penetration and device corrosion [1].
Mechanical Fatigue at Interconnects: Stress concentration points between materials with different mechanical properties leading to circuit failure [1].
Biofouling and Impedance Changes: Protein adsorption and cellular attachment on electrode surfaces altering interface properties and signal fidelity [4].
Foreign Body Response Evolution: Chronic inflammatory response continuing beyond initial implantation phase, leading to progressive signal degradation [1].
Defining biocompatibility for implantable bioelectronics requires a multidimensional approach spanning regulatory standards, material science, biological testing, and clinical validation. The evolving ISO 10993-1:2025 framework emphasizes integration with risk management processes throughout the device lifecycle, while advances in organic bioelectronic materials enable increasingly seamless tissue-device interfaces. The field continues to progress toward softer, more compliant materials that minimize mechanical mismatch, sophisticated surface modifications that direct favorable biological responses, and comprehensive testing strategies that predict long-term performance. As these technologies advance toward broader clinical adoption, maintaining focus on fundamental biocompatibility principles will ensure new bioelectronic therapies achieve their potential to transform treatment of neurological disorders, chronic diseases, and other challenging conditions while ensuring patient safety and device efficacy.
The development of advanced bioelectronic interfaces for healthcare monitoring, diagnostics, and therapeutics represents one of the most promising frontiers in medical science. However, a fundamental challenge persists: the significant mechanical mismatch between conventional electronic materials and the soft, dynamic tissues of the human body. This disparity in mechanical properties—particularly Young's modulus, which quantifies material stiffness—creates substantial barriers to effective biointegration. Traditional inorganic electronic materials, such as silicon and metals, possess moduli in the gigapascal (GPa) range, making them orders of magnitude stiffer than biological tissues, which typically exhibit moduli in the kilopascal (kPa) range [10] [3]. This mechanical incompatibility leads to interfacial stress, tissue damage, chronic inflammation, and ultimately device failure [8] [1].
The field has consequently pivoted toward soft organic materials—including conductive polymers, elastomers, and hydrogels—that can closely mimic the mechanical properties of biological tissues. These materials form the foundation of organic bioelectronics, an interdisciplinary field leveraging carbon-based semiconductors to create seamless interfaces with biological systems [11] [3]. This technical analysis examines the core of the mechanical mismatch problem, contrasting the properties and biological impacts of rigid inorganic versus soft organic materials within the context of biocompatibility research. By synthesizing recent advances in materials science and device engineering, this review provides a framework for developing next-generation bioelectronic systems that achieve mechanical harmony with living tissues.
Quantitative Analysis of Material Properties
The mechanical mismatch between bioelectronic interfaces and biological tissues can be quantitatively assessed through several key parameters, with Young's modulus being the most critical for predicting biocompatibility and long-term integration.
Table 1: Mechanical Properties of Biological Tissues and Electronic Materials
| Material Category | Example Materials | Young's Modulus | Tensile Strain (%) | Key Characteristics |
|---|---|---|---|---|
| Biological Tissues | Brain Tissue | 1 - 4 kPa [12] | N/A | Soft, viscoelastic, aqueous |
| Myocardial Tissue | 10 - 15 kPa [10] | N/A | Dynamic, continuously moving | |
| Skin | 100 kPa - 1 MPa [13] [3] | N/A | Multilayered, protective | |
| Rigid Inorganic Materials | Silicon (Bulk) | ~100 GPa [10] | <1% [1] | Brittle, high processing temperature |
| Gold (Au) | 20 - 80 GPa [3] | <5% [1] | Ductile but stiff, corrosion-resistant | |
| Silicon Dioxide (SiOâ‚‚) | ~70 GPa [10] | <1% | Excellent insulator, chemically stable | |
| Soft Organic Materials | PEDOT:PSS (Pure Film) | 1 - 2 GPa [12] | ~2% [12] | Conductivity-mechanical trade-off |
| PEDOT:PSS Hydrogels | 0.1 - 1 MPa [13] | >20% | Tissue-like, mixed ionic-electronic conduction | |
| Biocompatible Elastomers (e.g., BIIR) | ~100 kPa [8] | Up to 100% [8] | Medical-grade, high elasticity | |
| Conductive Hydrogels (PEDOT:DBSA) | <1 MPa [13] | Tunable | High water content, excellent biocompatibility |
Table 2: Performance Comparison of Rigid vs. Soft Bioelectronics
| Property | Rigid Bioelectronics | Soft and Flexible Bioelectronics |
|---|---|---|
| Typical Material Types | Silicon, metals, ceramics | Polymers, elastomers, hydrogels |
| Young's Modulus Range | >1 GPa [1] | 1 kPa - 1 MPa [1] |
| Bending Stiffness | >10â»â¶ Nm [1] | <10â»â¹ Nm [1] |
| Stretchability | <1% (brittle) [1] | >10% (>100% for ultra-soft) [1] |
| Tissue Integration | Stiffness mismatch causes inflammation and fibrotic encapsulation [1] | Matches tissue mechanics, reduces immune response [1] |
| Signal Fidelity | Strong short-term signal quality [1] | Better chronic signal due to stable tissue contact [1] |
| Long-term Stability | Long-term degradation due to micromotion and scar tissue [1] | Can degrade due to soft substrate fatigue [1] |
The quantitative data reveals the profound mechanical disparity that exists at the bioelectronic interface. The modulus of silicon is approximately 10 million times stiffer than that of brain tissue, creating a significant mechanical gradient that the body perceives as a foreign object [12]. This mismatch triggers a cascade of biological responses, beginning with protein adsorption and culminating in the formation of a fibrotic capsule around the implant, which electrically isolates the device and degrades its performance over time [10].
In contrast, soft organic materials bridge this mechanical divide. Advanced material systems, such as the vulcanized blend of DPPT-TT and bromo isobutyl-isoprene rubber (BIIR) reported by [8], achieve both semiconducting functionality and mechanical compatibility. This particular composite exhibits a Young's modulus similar to human tissues and maintains stable electrical performance even under 50% strain, representing a significant advancement toward truly biocompatible electronics [8].
The Biological Impact of Mechanical Mismatch
Foreign Body Response and Fibrotic Encapsulation
The implantation of any medical device triggers a complex biological sequence known as the foreign body response (FBR). While this process is inevitable, its severity is directly influenced by the mechanical properties of the implanted material. Rigid implants with high modulus mismatch cause sustained mechanical irritation at the tissue interface, amplifying the FBR and leading to the formation of a dense collagenous capsule that can be hundreds of micrometers thick [10] [1]. This fibrotic tissue acts as an electrical insulator, diminishing signal quality in recording applications and increasing impedance in stimulation devices. Studies have shown that the chronic inflammatory response to stiff implants can persist for the entire duration of implantation, continuously degrading the interface and ultimately leading to device failure [10].
Tissue Damage and Signal Integrity
Beyond chronic inflammation, the acute mechanical mismatch between rigid devices and soft tissues can cause direct physical damage during implantation and normal physiological motion. The brain, for instance, exhibits micromotion due to cardiovascular and respiratory cycles, creating repeated shear forces at the interface with rigid implants [12]. This results in progressive tissue damage, neuronal death, and glial scarring, which compromises the very cellular populations that neural interfaces aim to monitor or stimulate. The resulting signal degradation manifests as decreased signal-to-noise ratio, increased instability, and eventual loss of functional recording or stimulation capability [1] [12].
Organic Materials as a Solution to Mechanical Mismatch
Conductive Polymers and Their Composites
Poly(3,4-ethylenedioxythiophene):polystyrenesulfonate (PEDOT:PSS) has emerged as a cornerstone material in organic bioelectronics due to its combination of high electrical conductivity, environmental stability, and tunable mechanical properties [12]. When processed as a pure film, PEDOT:PSS still exhibits a relatively high modulus (~1-2 GPa), but through various formulation strategies—including the addition of plasticizers, secondary dopants, and blending with elastomers—its mechanical properties can be engineered to better match biological tissues [12].
Recent innovations have produced PEDOT:PSS-based hydrogels that achieve conductivities up to 5 × 10³ S/m while maintaining moduli in the MPa range, significantly closer to tissue values [13] [12]. Alternative formulations, such as PEDOT:DBSA hydrogels, offer improved biocompatibility by eliminating the potentially cytotoxic PSS component while maintaining tissue-like mechanical properties (Young's modulus <1 MPa) and sufficient conductivity for bioelectronic applications [13].
Elastomer-Semiconductor Composites for Intrinsic Stretchability
Beyond conductivity matching, the next frontier in biocompatible interfaces involves creating devices with intrinsic stretchability to accommodate tissue dynamics. Pioneering work by [8] demonstrates a biocompatible elastomeric organic transistor using a blend of semiconducting nanofibers (DPPT-TT) and a medical-grade elastomer (BIIR). This composite system exhibits several critical advantages:
- High mechanical stretchability (up to 100% strain without cracking)
- Biocompatibility confirmed through in vitro and in vivo studies
- Stable electrical performance under physiological conditions
- Similar Young's modulus to human tissues [8]
The vulcanization process used in fabricating these devices selectively crosslinks the elastomer matrix while preserving the conjugated structure of the semiconductor, enabling both mechanical robustness and electronic functionality [8]. This approach represents a significant advancement over earlier stretchable electronics that used non-biocompatible elastomers like PDMS, which could induce chronic foreign body reactions despite their favorable mechanical properties [8].
Experimental Protocols for Assessing Mechanical Compatibility
In Vitro Biocompatibility Testing
Rigorous assessment of new bioelectronic materials requires standardized in vitro protocols to evaluate cellular responses prior to in vivo implantation.
Table 3: Research Reagent Solutions for Biocompatibility Testing
| Reagent/Material | Function/Application | Experimental Context |
|---|---|---|
| Human Dermal Fibroblasts | Model cell type for assessing cytotoxicity | In vitro biocompatibility testing [8] |
| Macrophages | Model immune response to implants | In vitro inflammatory response assessment [8] |
| Cell Viability Assays | Quantify live/dead cell ratios | Determine material cytotoxicity [8] |
| Proliferation/Migration Assays | Assess impact on cellular function | Evaluate long-term biocompatibility [8] |
| Murine Endothelial Cells | Model vascular interface compatibility | Test blood-contacting devices [13] |
Protocol: Cytocompatibility Assessment of Conductive Hydrogels
Material Preparation: Formulate hydrogel samples under sterile conditions. For PEDOT:DBSA hydrogels, this involves mixing the polymer dispersion with DBSA (3-10 v/v%) at room temperature until homogenized, followed by centrifugation to separate microgels [13].
Cell Seeding: Plate relevant cell types (e.g., human dermal fibroblasts, murine endothelial cells) in standard culture plates at appropriate densities (typically 10,000-50,000 cells/cm²).
Material Exposure: Apply sterile material extracts or place direct material contacts onto established cell monolayers. For direct contact tests, use material discs with standardized surface area-to-volume ratios.
Viability Assessment: After 24-72 hours of exposure, perform viability assays (e.g., Live/Dead staining, MTT, Alamar Blue) according to manufacturer protocols. Calculate viability percentages relative to negative controls.
Proliferation and Migration Analysis: Quantify cell proliferation rates over 3-7 days using DNA content assays or direct cell counting. Assess migration through scratch/wound healing assays, measuring closure rates over 24-48 hours [8] [13].
In Vivo Implantation Studies
Long-term biocompatibility and mechanical integration must be evaluated in living organisms to account for the full complexity of the foreign body response.
Protocol: In Vivo Evaluation of Soft Bioelectronic Implants
Device Fabrication: Fabricate test devices using the target material system. For elastomeric transistors, this involves creating blend films of semiconductor and elastomer (e.g., DPPT-TT:BIIR at 3:7 ratio), followed by vulcanization with sulfur-based crosslinkers [8].
Surgical Implantation: Under approved animal protocol guidelines, implant devices in target tissues (e.g., subcutaneous, neural, or cardiac) using aseptic surgical techniques. Include appropriate controls (sham surgery, commercially available materials).
Histological Analysis: After predetermined intervals (e.g., 2, 4, 12 weeks), euthanize animals and harvest implant sites with surrounding tissues. Process for histological sectioning and staining (H&E for general morphology, Masson's Trichrome for collagen deposition, immunohistochemistry for specific cell types).
Inflammatory Response Quantification: Score histological sections for key indicators of the foreign body response: inflammatory cell density (neutrophils, macrophages), fibrotic capsule thickness, and tissue integration quality. Compare experimental groups to controls [8].
Functional Stability Assessment: For active electronic devices, monitor electrical performance (impedance, signal-to-noise ratio, stimulation efficacy) throughout the implantation period to correlate mechanical integration with functional stability [8] [12].
Diagram 1: Experimental workflow for evaluating mechanical compatibility of bioelectronic materials, integrating both in vitro and in vivo assessments to ensure comprehensive biocompatibility validation.
Emerging Strategies and Future Directions
Multimodal Integration and Closed-Loop Systems
The convergence of soft bioelectronics with artificial intelligence is enabling a new generation of closed-loop bioelectronic systems that can adaptively respond to physiological states. These systems leverage conformable interfaces to acquire high-fidelity signals, process them using machine learning algorithms, and deliver precise therapeutic interventions—all while maintaining mechanical harmony with tissues [14] [15]. Such integrated platforms represent the future of bioelectronic medicine, transitioning from static implants to dynamic systems that can evolve with patient needs.
Advanced Manufacturing and Minimally Invasive Deployment
Sophisticated fabrication techniques are critical for realizing the full potential of soft bioelectronic materials. 3D printing technologies enable the creation of complex, customized architectures from conductive polymer hydrogels, allowing for patient-specific interface designs [12]. Simultaneously, the development of injectable bioelectronics—including flexible mesh electrodes and hydrogel-based devices that can be delivered through syringe injection—promises to minimize surgical trauma and improve patient outcomes [10] [1] [15]. These deployment strategies are particularly valuable for interfacing with delicate tissues like the brain, where minimizing insertion damage is paramount for long-term functionality.
The mechanical mismatch between traditional rigid electronics and soft biological tissues represents a fundamental barrier in bioelectronic medicine. Through the strategic development and implementation of soft organic materials—including conductive polymers, elastomeric composites, and hydrogels—the field is making significant progress toward seamless bioelectronic interfaces. These advanced materials systems demonstrate that achieving mechanical harmony with biological tissues is not merely a desirable feature but an essential requirement for chronic device functionality and biocompatibility.
As research progresses, the integration of these soft materials with sophisticated manufacturing techniques and intelligent control systems will enable a new paradigm in bioelectronic medicine. The future of the field lies in creating devices that not only match the mechanical properties of tissues but also adapt to their dynamic nature, ultimately forming stable, long-lasting interfaces that can transform our approach to diagnosing and treating disease.
The emergence of organic bioelectronics represents a paradigm shift in the development of medical devices, enabling seamless integration of electronic components with biological systems. This field leverages the unique properties of organic electronic materials to create devices that can successfully interface with the electrically active tissues of the human body [16]. The fundamental challenge in bioelectronic medicine has been the mechanical and chemical mismatch between conventional rigid electronic components and soft, dynamic biological tissues, which often leads to tissue damage, inflammation, and device failure over time [8] [17]. Overcoming this challenge requires the strategic engineering of three core material properties: biocompatibility to ensure safe biological interactions, stretchability to achieve mechanical compatibility with soft tissues, and mixed ionic-electronic conduction to facilitate seamless communication between electronic devices and ionic biological systems [16] [18]. This whitepaper provides an in-depth technical examination of these key properties, their interrelationships, measurement methodologies, and their critical role in advancing organic bioelectronics for therapeutic applications, framed within the context of biocompatibility research for next-generation medical devices.
Fundamental Properties in Organic Bioelectronics
Biocompatibility
Biocompatibility extends beyond simple non-toxicity to encompass the ability of a material to perform with an appropriate host response in a specific application [17]. For implantable bioelectronic devices, this property is paramount as it determines the long-term viability and safety of the device-tissue interface. The biocompatibility of organic electronic materials derives from their molecular structure, surface chemistry, and mechanical properties, which collectively influence protein adsorption, cellular adhesion, and immune responses [16].
Recent advances have demonstrated that medical-grade elastomers such as bromo isobutyl–isoprene rubber (BIIR) meet stringent biocompatibility standards set by regulatory bodies (ISO 10993, European Pharmacopoeia) and exhibit excellent mechanical properties including shock absorption, aging resistance, and high physical strength [8]. These materials show minimal adverse effects on cell viability, proliferation, and migration in vitro, and elicit no major inflammatory response or tissue damage in vivo, as confirmed by implantation studies in animal models [8].
Table 1: Biocompatibility Assessment Parameters and Methods
| Assessment Parameter | Experimental Methodology | Key Metrics |
|---|---|---|
| Cellular Response | In vitro co-culture with human dermal fibroblasts and macrophages | Cell viability, proliferation rates, migration patterns |
| Immune Response | In vivo implantation studies (e.g., mouse model) | Inflammatory markers, fibrosis, tissue damage assessment |
| Long-term Stability | Accelerated aging tests in simulated physiological conditions | Material degradation rates, leachable compounds analysis |
| Systemic Toxicity | ISO 10993 standard testing | Hematological parameters, organ histopathology |
Stretchability
Stretchability refers to a material's ability to undergo mechanical deformation (bending, twisting, stretching) while maintaining its structural integrity and electronic functionality [16]. This property is crucial for bioelectronic devices that need to conform to dynamic biological surfaces such as beating hearts, contracting muscles, or moving joints [8]. The mechanical mismatch between conventional rigid electronics (Young's modulus in GPa range) and soft biological tissues (Young's modulus in kPa to MPa range) can lead to tissue damage, inflammation, and device failure [16] [8].
Advanced material designs have achieved remarkable stretchability through innovative approaches such as semiconducting nanofiber networks embedded within elastomer matrices. For instance, composite films of poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] (DPPT-TT) and BIIR can sustain up to 100% strain without mechanical damage and maintain stable electrical performance under 50% strain [8]. These stretchable organic field-effect transistors (sOFETs) demonstrate stable operation in logic circuits (inverters, NOR gates, NAND gates) even under physiological conditions, making them suitable for implantable applications [8].
Table 2: Mechanical Properties of Bioelectronic Materials vs. Biological Tissues
| Material/Tissue | Young's Modulus | Key Characteristics |
|---|---|---|
| Traditional Silicon | 100-200 GPa | Rigid, brittle, significant mechanical mismatch |
| Gold Electrodes | 50-80 GPa | High conductivity but stiff |
| Polyimide (PI) | 2-3 GPa | Flexible but relatively high modulus |
| Conducting Polymers (PEDOT:PSS) | 1 MPa - 2 GPa | Tunable mechanical properties |
| Elastomers (PDMS, PU) | 0.1-3 MPa | Soft, stretchable, tissue-compatible |
| Human Tissues (Brain, Heart, PNS) | 0.1-100 kPa | Soft, hydrated, viscoelastic |
Mixed Ionic-Electronic Conduction
Organic mixed ionic-electronic conductors (OMIECs) represent a specialized class of materials capable of transporting both electronic charge carriers (electrons and holes) and ionic species (Na+, K+, Cl-, etc.) simultaneously [18]. This dual conduction mechanism is particularly advantageous for bioelectronics applications where efficient translation between electronic signals in devices and ionic signals in biological systems is required [16] [18]. The performance and operational stability of OMIECs in aqueous environments are influenced by dynamic interactions between polymer functionalities and electrolyte species [18].
Key OMIECs such as poly(3,4-ethylenedioxythiophene) polystyrene sulfonate (PEDOT:PSS) and various polyaniline (PANI) derivatives demonstrate excellent mixed conduction properties, making them ideal for organic electrochemical transistors (OECTs) [16]. The molecular design of these materials, particularly sidechain engineering, significantly impacts ion transport, hydration, swelling behavior, and mixed conduction properties [18]. For instance, ethylene glycol-based sidechains and emerging hybrid designs incorporating ionic moieties can tune material-electrolyte interactions, affecting doping mechanisms and structural stability [18].
Interrelationship of Key Properties
The three core properties—biocompatibility, stretchability, and mixed ionic-electronic conduction—are not independent but exhibit strong interdependencies that must be considered in material design. The relationship between these properties forms the foundation for high-performance bioelectronic devices.
Diagram 1: Property Interrelationships in Bioelectronic Materials
The interconnected nature of these properties creates both challenges and opportunities in material design. For instance, achieving mixed ionic-electronic conduction often requires hydrophilic components that facilitate ion transport, but these same components may swell excessively in physiological environments, compromising mechanical stability and potentially triggering adverse biological responses [18]. Similarly, enhancing stretchability through elastomeric blending must be balanced against potential impacts on electrical performance and biocompatibility [8]. Understanding these complex interrelationships enables the rational design of materials optimized for specific bioelectronic applications.
Experimental Protocols and Characterization Methods
Synthesis of Stretchable Biocompatible Semiconductors
The development of high-performance stretchable semiconductors employs sophisticated material processing techniques. A representative protocol for creating biocompatible stretchable transistors involves:
Material Preparation: Prepare a blend solution of semiconducting polymer (e.g., DPPT-TT) and medical-grade elastomer (e.g., BIIR) in appropriate organic solvents. Optimal electrical and mechanical properties are typically achieved at a 3:7 weight ratio of DPPT-TT to BIIR [8].
Vulcanization Process: Add vulcanizing agents including sulfur (crosslinker), dipentamethylenethiuram tetrasulfide (DPTT, accelerator), and stearic acid (initiator) to the blend solution. The vulcanization process involves three stages: initiation for radical formation, propagation for crosslinking BIIR with sulfur, and termination for reaction completion [8].
Film Fabrication: Deposit the vulcanized blend solution onto substrates using spin-coating, blade-coating, or printing techniques. Achieve uniform film thickness between 100-500 nm for optimal electronic and mechanical performance.
Characterization: Validate successful vulcanization through Fourier transform infrared spectroscopy (FTIR) by monitoring reduction in C–Br peaks (667 cm−1) and C=C peaks (1,538 cm−1) in neat BIIR post-vulcanization [8].
This protocol yields a composite film with semiconducting nanofiber networks embedded within an elastomer matrix, exhibiting high mechanical stretchability (up to 100% strain), biocompatibility, and stable electrical performance under deformation [8].
Biocompatibility Assessment Workflow
Rigorous biocompatibility assessment follows a structured workflow to evaluate material safety for biomedical applications.
Diagram 2: Biocompatibility Assessment Workflow
This comprehensive assessment approach ensures that bioelectronic materials meet the stringent safety requirements for clinical applications. The in vitro phase typically involves co-culture studies with relevant cell lines (e.g., human dermal fibroblasts and macrophages) to assess cytotoxicity, while in vivo studies evaluate the host response to implanted materials over extended periods [8]. Materials showing favorable performance in these assessments can proceed to regulatory validation following established standards such as ISO 10993 [8].
Electrical Performance Under Strain
Characterizing the electrical properties of bioelectronic materials under mechanical deformation requires specialized measurement techniques:
Strain-Dependent Electrical Measurements: Mount stretchable semiconductor films on custom strain jigs capable of applying precise mechanical deformation (0-100% strain). Measure field-effect mobility, ON/OFF ratio, and threshold voltage at various strain levels using semiconductor parameter analyzers [8].
Cyclic Stretch Testing: Subject devices to repeated stretching cycles (e.g., 1,000 cycles at 100% strain) to evaluate mechanical durability and electrical stability under physiological-like conditions [8].
Operando Characterization: Employ advanced operando techniques including conductive atomic force microscopy (C-AFM) to monitor nanoscale morphological changes and charge transport under applied strain. This reveals the alignment of semiconducting nanofibers along the strain direction, which provides strain-insensitive conductive pathways [8].
These methodologies demonstrate that optimized stretchable semiconductors can maintain stable field-effect mobility (>1 cm²/V·s) even under 50% strain and after thousands of stretching cycles, satisfying the requirements for implantable bioelectronic applications [8].
The Scientist's Toolkit: Research Reagent Solutions
Advancing research in organic bioelectronics requires access to specialized materials and characterization tools. The following table outlines essential components of the research toolkit for investigating biocompatibility, stretchability, and mixed conduction.
Table 3: Essential Research Reagents and Materials for Organic Bioelectronics
| Material/Reagent | Function and Application | Key Characteristics |
|---|---|---|
| PEDOT:PSS | Benchmark organic mixed conductor for OECTs and electrodes | High conductivity, tunable mechanical properties, commercial availability |
| DPPT-TT Semiconductor | High-performance semiconducting polymer for stretchable OFETs | Donor-acceptor structure, field-effect mobility, processability |
| BIIR Elastomer | Biocompatible elastomer matrix for medical devices | ISO 10993 certification, mechanical robustness, chemical resistance |
| Medical-Grade PDMS | Flexible substrate and encapsulation material | Transparency, biocompatibility, tunable modulus |
| Ag/Au Dual-Layer Metallization | Stretchable, corrosion-resistant electrodes for implants | Ag for conductivity, Au for biofluid resistance, stretchable design |
| Vulcanization Agents | Crosslinking system for enhancing mechanical properties | Sulfur (crosslinker), DPTT (accelerator), stearic acid (initiator) |
| Ferolin | Ferolin, MF:C22H30O4, MW:358.5 g/mol | Chemical Reagent |
| Luteolin 7-O-glucuronide | Luteolin 7-O-glucuronide, MF:C21H17O12-, MW:461.4 g/mol | Chemical Reagent |
This toolkit provides the foundation for developing and characterizing advanced bioelectronic materials. The selection of appropriate materials must consider the specific application requirements, including the intended implantation site, duration of use, and necessary signal transduction mechanisms.
The convergence of biocompatibility, stretchability, and mixed ionic-electronic conduction represents the cornerstone of next-generation organic bioelectronics. These interdependent properties enable the creation of devices that can seamlessly integrate with biological systems, providing stable long-term interfaces for monitoring and modulating physiological activity. Advances in material design, particularly the development of nanostructured composites and sophisticated molecular engineering approaches, have yielded significant progress in achieving this combination of properties in functional devices. The ongoing refinement of characterization methodologies and the establishment of comprehensive biocompatibility assessment protocols continue to drive the field toward clinical translation. As research in this area advances, the strategic integration of these three fundamental properties will unlock new possibilities in personalized medicine, neural interfaces, and implantable therapeutic devices, ultimately transforming the landscape of healthcare and human-machine integration.
Organic bioelectronics represents a transformative frontier in medical science, enabling the development of devices that seamlessly integrate with biological systems for monitoring, diagnostics, and therapeutics. This field leverages carbon-based semiconductors and elastomeric polymers to create interfaces that overcome the limitations of traditional rigid electronics, particularly the mechanical mismatch with soft biological tissues. The convergence of these materials has catalyzed advancements in implantable sensors, neural interfaces, and wearable health monitors.
This whitepaper provides a comprehensive technical analysis of three pivotal materials in organic bioelectronics: the conducting polymer PEDOT:PSS, the semiconducting polymer DPPT-TT, and the medical-grade elastomer bromo isobutyl-isoprene rubber (BIIR). We examine their fundamental properties, processing techniques, and performance characteristics within the critical framework of biocompatibility research, addressing both current applications and future potential for clinical translation.
Material Properties and Characteristics
PEDOT:PSS (Poly(3,4-ethylenedioxythiophene):Poly(Styrene Sulfonate))
PEDOT:PSS is a conductive polymer complex consisting of a conjugated, positively-charged PEDOT backbone and an insulating, negatively-charged PSS polyelectrolyte. This structure forms a colloidal dispersion in water, where PSS stabilizes the otherwise insoluble PEDOT through electrostatic interactions [19] [12]. The material is commercially available as an aqueous dispersion or powder from suppliers such as Heraeus Holding GmbH (Clevios) and Agfa-Gevaert N.V. (Orgacon) [19].
Table 1: Key Properties of PEDOT:PSS
| Property | Typical Range/Value | Notes and Influencing Factors |
|---|---|---|
| Conductivity | < 1 to ~300 S/cm [19] [12] | Highly tunable; pristine form is at lower end, can be enhanced with secondary doping [12] |
| Mechanical Properties | Young's Modulus: 1-2 GPa [12] | Relatively rigid in pure form; can be plasticized or formulated into hydrogels for softness |
| Stretchability | ~2% elastic strain (pristine) [12] | |
| Optical Transparency | High in thin films [19] | Suitable for transparent electrode applications |
| Biocompatibility | Good [19] [12] | Considered biocompatible; essential for bioelectronic interfaces |
| Primary Bioelectronic Use | Electrodes, sensors, OECTs [19] [12] | Used as thin films, coatings, or scaffolds |
DPPT-TT (Poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)])
DPPT-TT is a donor-acceptor (D-A) type semiconducting polymer known for its high charge-carrier mobility. Its structure features electron-deficient diketopyrrolopyrrole (DPP) and electron-rich dithiophene (TT) units, which promote strong π-π stacking and efficient charge transport [8] [20]. It is typically processed from organic solvents and forms semi-crystalline films.
Table 2: Key Properties of DPPT-TT
| Property | Typical Range/Value | Notes and Influencing Factors |
|---|---|---|
| Field-Effect Mobility | High performance in OFETs | Maintains performance when blended with elastomers like BIIR [8] |
| Mechanical Properties | Intrinsically rigid/semi-crystalline | Becomes stretchable when blended into an elastomer matrix (e.g., BIIR) [8] |
| Stretchability | Low in neat form; >100% strain when blended with BIIR (3:7 ratio) [8] | The nanofiber network within the elastomer allows for stretchability without electrical failure |
| Optical Properties | Opaque | Characteristic absorption in the visible to near-infrared region |
| Biocompatibility | Requires encapsulation or blending | Not intrinsically biocompatible; made biocompatible through integration with medical-grade matrices [8] |
| Primary Bioelectronic Use | Active channel in stretchable OFETs [8] [20] | For logic circuits and signal processing in implantable devices |
Medical-Grade BIIR (Bromo Isobutyl-Isoprene Rubber)
BIIR is a medical-grade elastomer that meets stringent ISO 10993 biocompatibility standards, making it suitable for long-term implantation [8]. It can be cross-linked through a vulcanization process, which enhances its mechanical properties and stability. Its primary role in bioelectronics is to serve as a compliant, biocompatible matrix for semiconducting polymers.
Table 3: Key Properties of Medical-Grade BIIR
| Property | Typical Range/Value | Notes and Influencing Factors |
|---|---|---|
| Young's Modulus | ~10^7.7 to 10^8.8 Pa [8] | Similar to human tissues, minimizing mechanical mismatch |
| Biocompatibility | High; certified to ISO 10993 [8] | Shows no adverse effects on cell viability, proliferation, or migration in vitro [8] |
| Key Features | Aging resistance, high physical strength, low permeability, chemical resistance [8] | Ideal for chronic implants |
| Primary Bioelectronic Use | Elastomer matrix in stretchable semiconductor composites [8] | Provides mechanical stretchability and biocompatibility to otherwise rigid semiconductors |
Fabrication and Processing Methodologies
Processing Techniques for PEDOT:PSS
The water dispersibility of PEDOT:PSS allows for a variety of solution-processing techniques, which are crucial for fabricating thin films and patterns on diverse substrates.
- Spin-Coating: This method produces uniform, nanoscale thin films ideal for research and small-scale applications. The process involves depositing a droplet of PEDOT:PSS dispersion onto a substrate, which is then rotated at high speed. The centrifugal force spreads the solution into a homogeneous film, with thickness controlled by spin speed and solution viscosity. A key drawback is significant material waste [19].
- Printing Techniques: Inkjet printing and screen printing are direct-write technologies that enable patterned deposition. Inkjet printing precisely dispenses microdroplets through fine nozzles, while screen printing forces ink through a stencil onto a predefined pattern. These techniques are scalable and minimize ink wastage, making them attractive for large-area, patterned electrode fabrication [19].
- Spray Coating: This cost-effective technique is suitable for coating large or irregular surfaces. The PEDOT:PSS solution is aerosolized and sprayed onto a substrate from a nozzle. It results in smooth coatings, though surface wettability and adhesion can be challenges common to all coating methods [19].
- Post-Processing/Annealing: Control over the solvent evaporation rate via annealing (temperature, time, humidity) is critical for forming a homogeneous film from the randomly oriented PEDOT crystals and PSS chains in the dispersion [19].
Creating Stretchable Semiconductors with DPPT-TT and BIIR
The integration of a rigid semiconductor like DPPT-TT with an elastomer like BIIR requires specific processing to achieve a stretchable, electrically functional composite.
- Solution Blending: DPPT-TT and BIIR are co-dissolved in a common organic solvent. The weight ratio is critical; a ratio of 3:7 (DPPT-TT:BIIR) has been optimized to balance electrical performance and mechanical stretchability. At this ratio, the composite film can withstand up to 100% strain without cracking [8].
- Film Formation: The blended solution is deposited onto a substrate via techniques such as spin-coating or blade-coating.
- Vulcanization (Chemical Cross-linking): The deposited film undergoes vulcanization. This process uses sulfur as a crosslinker, dipentamethylenethiuram tetrasulfide (DPTT) as an accelerator, and stearic acid as an initiator [8].
- Initiation: The process begins with radical formation, facilitated by the reduction of C–Br bonds in the BIIR, as confirmed by Fourier-transform infrared (FTIR) spectroscopy [8].
- Propagation and Termination: Sulfur crosslinks the BIIR chains, forming a robust, elastic network. FTIR analysis shows a reduction in C=C peaks in neat BIIR, confirming crosslinking. Notably, the C=C conjugated structure of DPPT-TT remains unchanged, preserving its semiconducting capability [8].
This process results in a phase-separated morphology where a percolating network of DPPT-TT nanofibers is embedded within the elastic BIIR matrix. This structure provides a continuous pathway for charge transport while allowing the material to stretch extensively.
Experimental Protocols for Performance and Biocompatibility Evaluation
Electrical Characterization of Stretchable Transistors
The electrical performance of devices like DPPT-TT:BIIR-based stretchable organic field-effect transistors (sOFETs) is characterized using a semiconductor parameter analyzer (e.g., Keysight B1500) [20].
- Transfer Characteristic Measurement: This measures the drain current (ID) as a function of gate voltage (VG) at a constant drain voltage (VD). From this curve, key parameters are extracted:
- Field-Effect Mobility (μ): Calculated in the saturation regime using the equation: ( ID = (W/2L) \mu Ci (VG - V{th})^2 ), where W and L are channel width and length, and Ci is gate dielectric capacitance per unit area.
- Threshold Voltage (V_th): The gate voltage at which the channel begins to conduct.
- Subthreshold Swing (SS): Indicates how sharply the transistor switches on.
- ON/OFF Current Ratio: The ratio between the maximum and minimum drain current.
- Output Characteristic Measurement: This measures ID as a function of VD at different, fixed VG values. The linearity of the curves at low VD is used to extract the on-state resistance (R_on).
- Performance under Strain: These measurements (transfer and output characteristics) are repeated while the transistor is subjected to controlled uniaxial strain (e.g., 0% to 50% or 100%). The stability of mobility and other parameters under strain demonstrates the efficacy of the composite design [8].
Biocompatibility Assessment
Adherence to international standards is paramount for bioelectronic materials. The ISO 10993 series provides a framework for the biological evaluation of medical devices within a risk management process [6].
- In Vitro Cytotoxicity Testing (ISO 10993-5): This is a first-line test to assess the potential for cell death. The protocol involves:
- Sample Preparation: Extracting the material (or a finished device) using both polar and non-polar solvents to simulate the release of leachable chemicals.
- Cell Culture: Exposing mammalian cell lines (e.g., L-929 mouse fibroblasts) to the extracts.
- Viability Assessment: Using a quantitative assay like MTT, which measures mitochondrial activity. A reduction in cell viability by more than 30% is considered a potential cytotoxic effect.
- For the DPPT-TT:BIIR blend, in vitro assessments with human dermal fibroblasts and macrophages showed no adverse effects on cell viability, proliferation, or migration [8].
- In Vivo Implantation Studies: For implantable materials, long-term in vivo studies are essential.
- Animal Model: Devices are implanted in a relevant animal model (e.g., mice or rats).
- Histopathological Analysis: After a predetermined period (e.g., 4, 12, or 26 weeks), the implant site and surrounding tissues are explanted.
- Tissue Staining: The tissue sections are stained (e.g., with Hematoxylin and Eosin) and examined under a microscope for signs of inflammation, fibrosis, and tissue damage.
- For the DPPT-TT:BIIR blend, in vivo implantation studies in mice showed no major inflammatory response or tissue damage [8].
The overall biological evaluation is an iterative process integrated with the device's risk management, as outlined in the updated ISO 10993-1:2025 standard [6] [21].
Visualizing Material Integration and Testing Workflows
The following diagrams illustrate the key concepts of composite material structure and the biocompatibility testing workflow.
Diagram 1: Material integration for bioelectronic interfaces. The diagram shows how PEDOT and PSS form a complex via electrostatic bonding, and how DPPT-TT and BIIR are blended and vulcanized to form a stretchable composite. Both systems converge to create a functional bioelectronic interface.
Diagram 2: Biocompatibility testing workflow. The diagram outlines the key stages of evaluating material safety, starting with a risk management plan, progressing through in vitro cytotoxicity tests, and, if passed, moving to in vivo implantation studies. All data is consolidated into a final biological evaluation report.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for Bioelectronic Device Fabrication
| Item Name | Function/Application | Technical Notes |
|---|---|---|
| PEDOT:PSS Dispersion | Conductive ink for electrodes, sensors, and OECTs. | Available from Heraeus (Clevios) or Agfa (Orgacon); often requires secondary doping or additive modification for enhanced performance [19] [12]. |
| DPPT-TT Polymer | High-mobility p-type semiconductor for OFETs. | Used as the active channel material; typically blended with elastomers like BIIR for stretchable devices [8] [20]. |
| Medical-Grade BIIR | Biocompatible elastomer matrix. | Provides mechanical compliance and stretchability; crosslinked via vulcanization for enhanced durability [8]. |
| Sulfur & Vulcanization Kit | Crosslinking agents for BIIR. | Includes sulfur (crosslinker), DPTT (accelerator), and stearic acid (initiator) to create a robust elastic network [8]. |
| Dual-Layer Ag/Au Metallization | Biocompatible and corrosion-resistant stretchable electrodes. | Ag provides excellent electrical contact, while an outer Au layer protects against biofluid corrosion [8]. |
| ISO 10993-5 Test Kit | For in vitro cytotoxicity testing. | Includes reagents (e.g., MTT), standardized cell lines (e.g., L-929 fibroblasts), and materials for extract preparation [6] [21]. |
| XEN103 | XEN103, MF:C22H23F4N5O2, MW:465.4 g/mol | Chemical Reagent |
| THP104c | THP104c, MF:C20H16N4O2S, MW:376.4 g/mol | Chemical Reagent |
Natural polymers represent a cornerstone of modern bioelectronic and biomedical research, offering unparalleled biocompatibility, tunable mechanical properties, and sustainable sourcing. This technical review comprehensively examines three pivotal natural polymers—cellulose, chitosan, and silk fibroin—focusing on their fundamental properties, biocompatibility mechanisms, and applications in advanced bioelectronics and therapeutic platforms. Within the context of organic bioelectronics, we analyze how these materials address the critical challenge of mechanical mismatch between conventional electronic components and soft biological tissues. The review provides detailed experimental protocols for material processing and characterization, visualizes key structure-function relationships through specially formulated diagrams, and presents a curated toolkit of research reagents to facilitate further innovation in this rapidly evolving field.
The integration of biological systems with electronic devices necessitates materials that can seamlessly interface with living tissue without provoking adverse immune responses. Natural polymers have emerged as ideal candidates for this purpose due to their inherent biocompatibility, biodegradability, and structural similarity to native extracellular matrix components. The global market for natural biocompatible polymers is experiencing robust growth, projected to reach $1097.5 million in 2025 with a Compound Annual Growth Rate (CAGR) of 6.8% from 2025 to 2033, reflecting their expanding role in medical technologies [22].
Within the specialized domain of organic bioelectronics, these materials facilitate the development of next-generation implantable devices that overcome the limitations of traditional rigid electronics. This review focuses specifically on cellulose, chitosan, and silk fibroin—three natural polymers with distinct structural and functional properties that make them particularly valuable for biointerfacing applications. We examine their molecular characteristics, biocompatibility metrics, processing methodologies, and implementation in bioelectronic platforms, with particular emphasis on their roles in creating mechanically compliant, physiologically stable interfaces.
Fundamental Properties and Biocompatibility Profiles
Structural Characteristics and Native Properties
Cellulose, the most abundant natural polymer, is a complex carbohydrate consisting of long chains of glucose molecules forming a rigid framework that provides structural support in plants [23]. Its semi-crystalline structure, high tensile strength, biodegradability, and chemical reactivity make it incredibly versatile for biomedical applications. Cellulose is insoluble in water but can be processed into various forms including regenerated cellulose fibers, films, and hydrogels through dissolution and reconstitution methods [24]. The transformation of cellulose chain conformation from cellulose I to cellulose II during regeneration creates structures with more amorphous regions and enhanced crystallinity, facilitating extensive modifications for specific applications [24].
Chitosan, a cationic natural polymer composed of glucosamine and N-acetylglucosamine residues connected by glycosidic bonds, is typically extracted from shrimp and crab shells through demineralization, deproteinization, and deacetylation processes [25]. Its excellent physicochemical properties include stability in natural environments, metal ion chelation, high sorption capacity, and solubility in acidic solutions. Chitosan's chemical structure facilitates remarkable biocompatibility and biodegradability, while its protonated amino groups under acidic conditions confer mucoadhesive properties that promote prolonged contact with biological surfaces and enhanced drug absorption [25].
Silk fibroin (SF), a macromolecular fibrous protein, exhibits irreplaceable value in biomedical applications due to its exceptional mechanical properties, controllable degradability, and unique structure regulation ability [26]. The incorporation of SF into composite materials significantly enhances compressive strength, toughness, and structural stability through the formation of β-sheet crystal structures and intermolecular interactions [26]. This unique structural organization allows SF to address application limitations of traditional biomaterials in tissue engineering, particularly for load-bearing applications.
Biocompatibility and Biological Interactions
Table 1: Biocompatibility Profiles of Natural Polymers
| Polymer | Cytocompatibility Evidence | Immunogenic Response | Regulatory Status | Degradation Profile |
|---|---|---|---|---|
| Cellulose | Excellent biocompatibility with minimal allergic reactions; promotes cell adhesion in tissue scaffolds [24] | Minimal immune activation; suitable for long-term implantation | FDA approved for various medical applications including wound care and tissue engineering [24] | Highly biodegradable through enzymatic action; degradation rate varies by crystallinity and functionalization [23] |
| Chitosan | Cell viability >90% even at high concentrations; supports epithelial cells, fibroblasts, osteoblasts, and chondrocytes [25] | Non-immunogenic; mucoadhesive properties reduce irritation | FDA GRAS (Generally Recognized as Safe) status; FDA approved as primary wound healing material (August 2023) [25] | Enzymatic hydrolysis by lysozymes; degradation rate depends on degree deacetylation and molecular weight [25] |
| Silk Fibroin | Promotes adhesion, proliferation, and differentiation of mesenchymal stem cells; upregulates osteogenic markers [26] | Minimal inflammatory response; compatible with various tissues | Used in FDA-approved medical devices; extensive clinical history in sutures [27] | Controllable proteolytic degradation; rate tunable via cross-linking and processing [26] |
Quantitative Material Properties Comparison
Table 2: Comparative Physicochemical Properties for Bioelectronic Applications
| Property | Cellulose | Chitosan | Silk Fibroin | Test Method |
|---|---|---|---|---|
| Tensile Strength (MPa) | Up to 1000 (crystal) | 20-50 (films) | 100-740 (fibers) | ASTM D638 |
| Young's Modulus (GPa) | 100-140 (crystal) | 2-7 | 5-17 | ASTM E111 |
| Degradation Time | Weeks to months | 2-12 weeks | 2 months to years | Enzymatic assay |
| Biocompatibility Score | Excellent | Excellent | Excellent | ISO 10993 |
| Surface Charge | Negative | Positive (pH-dependent) | Negative | Zeta potential |
| Water Absorption (%) | 60-1000 (hydrogels) | 100-600 | 100-300 | Gravimetric analysis |
Processing and Functionalization Methodologies
Material Processing and Scaffold Fabrication
Cellulose Processing: Regenerated cellulose fibers are produced through dissolution of natural cellulose sources (typically wood pulp or cotton linters) and reconstitution into fiber form. The viscose process—the most common method—involves steeping cellulose in sodium hydroxide, reaction with carbon disulfide to form cellulose xanthate, dissolution in dilute alkali to create viscose dope, and finally extrusion into an acidic coagulation bath to regenerate cellulose [24]. More recent environmentally friendly processes include the Lyocell process, which uses N-methylmorpholine N-oxide (NMMO) as a direct solvent in a closed-loop system that minimizes environmental impact [24].
Chitosan Nanoparticle Synthesis: Ionic gelation method represents the most prevalent technique for producing chitosan nanoparticles for drug delivery applications. The process involves dissolving chitosan in aqueous acidic solution (typically 1% acetic acid) to protonate amino groups, followed by dropwise addition of cross-linking agent (most commonly tripolyphosphate - TPP) under constant magnetic stirring at room temperature. The resulting nanoparticles are collected by ultracentrifugation (10,000-15,000 rpm for 30-60 minutes) and washed repeatedly with deionized water [25]. Critical parameters affecting nanoparticle characteristics include chitosan molecular weight and degree of deacetylation, chitosan-to-TPP ratio, pH, stirring speed, and temperature.
Silk Fibroin Processing: Silk fibroin is typically extracted from Bombyx mori cocoons through a multi-step purification process. Cocoons are boiled in 0.02M sodium carbonate solution for 30-60 minutes to remove sericin, the glue-like protein. The extracted fibroin fibers are then dissolved in 9.3M LiBr solution at 60°C for 4 hours, followed by dialysis against deionized water using cellulose tubular membranes (MWCO 3.5-14 kDa) for 48-72 hours to remove salt. The resulting aqueous silk fibroin solution can be processed into various material formats including films, hydrogels, sponges, and fibers through techniques like solvent casting, electrospinning, or freeze-drying [26].
Biofunctionalization Strategies
Surface modification of natural polymers enhances their functionality for specific bioelectronic applications. Chitosan's chemical versatility allows modification through primary amino groups at C2 and hydroxyl groups at C3 and C6 positions, enabling graft copolymerization, cross-linking, and polyelectrolyte complex formation to tailor stability, hydrophobicity, pharmacokinetics, solubility, durability, and biocompatibility [25]. Cellulose can be functionalized with antimicrobial agents (e.g., silver nanoparticles, iodine) for advanced wound care applications or with conductive polymers (e.g., PEDOT:PSS) for bioelectronic interfaces [24]. Silk fibroin's surface can be modified with cell-adhesive peptides (e.g., RGD sequences) to enhance cellular interaction or with inorganic nanoparticles (e.g., hydroxyapatite) to improve osteoconductivity for bone tissue engineering applications [26].
Applications in Bioelectronics and Therapeutic Platforms
Bioelectronic Interfaces and Implantable Devices
The mechanical mismatch between conventional electronic components and soft biological tissue represents a significant challenge in implantable bioelectronics, often leading to tissue damage, inflammation, and device failure [8]. Natural polymers address this limitation through their tunable mechanical properties and inherent biocompatibility. Recent research has demonstrated the development of fully elastomeric organic field-effect transistors made from blends of semiconducting nanofibers and biocompatible elastomers, exhibiting Young's modulus similar to human tissues and stable electrical performance under 50% strain [8]. These devices maintain functionality in logic circuits (including inverters, NOR gates, and NAND gates) under physiological conditions, with in vivo implantation studies in mice showing no major inflammatory response or tissue damage [8].
Cellulose-based substrates have been employed as flexible, biodegradable platforms for transient electronics, with tunable degradation rates matching specific clinical timeframes. Regenerated cellulose fibers demonstrate exceptional biocompatibility and moisture management capabilities, making them ideal for biointegrated sensing applications [24]. Their moderate cost, excellent biocompatibility, and ability to be sterilized via autoclaving or gamma radiation without losing structural integrity make them particularly suitable for clinical translation [24].
Drug Delivery Systems
Chitosan-based formulations exemplify the potential of natural polymers in advanced drug delivery applications. The unique mucoadhesive properties of chitosan, derived from its cationic nature, facilitate prolonged contact with mucosal surfaces, enhancing drug absorption and bioavailability [25]. Nanoparticles and microparticles fabricated from chitosan and its derivatives enable controlled release kinetics, with sustained drug release profiles lasting more than 72 hours [25]. The release mechanisms include diffusion from the carrier surface, diffusion through the matrix, and release due to erosion and/or degradation of the polymer, typically occurring in combination rather than isolation [25].
Table 3: Research Reagent Solutions for Natural Polymer Experimentation
| Reagent/Material | Function | Application Context |
|---|---|---|
| Tripolyphosphate (TPP) | Ionic cross-linker for chitosan nanoparticles | Forms polyelectrolyte complexes with cationic chitosan; creates stable nanoparticles for drug encapsulation [25] |
| Lysozyme | Enzymatic degradation studies | Hydrolyzes glycosidic bonds in chitosan; used to simulate and study biodegradation profiles [25] |
| N-Methylmorpholine N-oxide (NMMO) | Direct cellulose solvent | Lyocell process for regenerated cellulose fibers; closed-loop environmentally friendly processing [24] |
| Lithium Bromide (LiBr) | Silk fibroin solvent | Dissolves degummed silk fibers to create aqueous silk solutions for biomaterial fabrication [26] |
| Glycerol | Plasticizing agent | Enhances flexibility and processability of natural polymer films; reduces brittleness [28] |
| Genipin | Natural cross-linker | Alternative to glutaraldehyde; crosslinks chitosan and other natural polymers with reduced cytotoxicity [25] |
Tissue Engineering Scaffolds
Silk fibroin has demonstrated exceptional utility in tissue engineering, particularly for bone regeneration where mechanical strength and osteoconductivity are critical requirements. The incorporation of SF into composite materials significantly enhances compressive strength, toughness, and structural stability through the formation of β-sheet crystal structures and intermolecular interactions [26]. SF promotes the adhesion, proliferation, and differentiation of mesenchymal stem cells, upregulating the expression of key osteogenic markers such as alkaline phosphatase and osteocalcin through participation in signaling pathways [26]. When combined with ceramics or metal implants, SF-based composites demonstrate excellent osteogenic ability, providing a theoretical framework for creating composite bone repair materials with precise mechanical matching and efficient osteogenic induction functions [26].
Plant-based polymers, including cellulose and chitosan, offer sustainable alternatives for tissue engineering scaffolds, with inherent biocompatibility and adjustable physicochemical characteristics that support cell adhesion, proliferation, and extracellular matrix deposition [28]. These biomaterials provide distinct advantages over synthetic polymers, including reduced inflammatory responses and inherent bioactivity, though challenges remain in achieving sufficient mechanical strength for load-bearing applications without additional reinforcement strategies [28].
Experimental Protocols and Characterization
Biocompatibility Assessment Protocol
Comprehensive biocompatibility evaluation follows ISO 10993 standards and involves multiple assessment techniques:
Cell Viability Assay (MTT Assay): Seed cells (e.g., human dermal fibroblasts) in 96-well plates at density of 1×10ⴠcells/well and culture for 24 hours. Prepare polymer extracts by incubating sterile material samples in complete cell culture medium at 37°C for 24 hours at surface area-to-volume ratio of 3 cm²/mL. Replace cell culture medium with material extracts and incubate for 24-72 hours. Add MTT solution (0.5 mg/mL) and incubate for 4 hours. Dissolve formed formazan crystals with DMSO and measure absorbance at 570 nm with reference at 630 nm [25].
Hemocompatibility Testing: Collect fresh human whole blood with anticoagulant. Incubate polymer samples with diluted blood (1:10 in PBS) at 37°C for 1 hour with gentle mixing. Centrifuge and measure hemoglobin release at 540 nm. Calculate hemolysis percentage relative to positive (water) and negative (PBS) controls. Values below 5% indicate acceptable blood compatibility [29].
Cytokine Expression Profiling: Culture macrophages (e.g., THP-1 cells) with material samples for 24 hours. Collect supernatant and analyze pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) using ELISA kits according to manufacturer protocols. Compare to positive (lipopolysaccharide) and negative (culture medium) controls [8].
In Vivo Implantation Protocol
Animal Model Preparation: Utilize appropriate animal model (typically mice or rats) with approval from institutional animal care and use committee. Anesthetize animals using isoflurane (3-5% for induction, 1-3% for maintenance) or ketamine/xylazine cocktail (80/10 mg/kg intraperitoneal).
Surgical Implantation: Aseptically prepare surgical site. Create subcutaneous pocket via 1-2 cm incision through skin. Implant sterile polymer samples (typically 5×5 mm) into pocket. Close incision with sutures or wound clips. Administer postoperative analgesia as required.
Histological Analysis: Euthanize animals at predetermined timepoints (e.g., 1, 4, 12 weeks). Excise implant with surrounding tissue. Fix in 10% neutral buffered formalin for 24-48 hours. Process through graded ethanol series, embed in paraffin, section at 5 µm thickness, and stain with Hematoxylin and Eosin (H&E) for general morphology or Masson's Trichrome for collagen deposition. Evaluate inflammatory response, fibrosis, and tissue integration using standardized scoring systems [8].
Structural and Functional Relationships
The biocompatibility of natural polymers is intrinsically linked to their molecular structures and interactions with biological systems. The following diagram illustrates the key structure-function relationships that dictate the biological performance of cellulose, chitosan, and silk fibroin:
Natural polymers—cellulose, chitosan, and silk fibroin—offer unparalleled opportunities for advancing bioelectronic and biomedical technologies through their inherent biocompatibility, tunable mechanical properties, and sustainable sourcing profiles. Their unique structural characteristics enable the development of advanced biointerfaces that mitigate foreign body responses and promote seamless integration with biological tissues. As research continues to refine processing methodologies and functionalization strategies, these materials are poised to play increasingly critical roles in next-generation implantable devices, targeted therapeutic systems, and engineered tissue constructs. The ongoing challenge of balancing mechanical performance with biological functionality continues to drive innovation in material design and processing techniques, promising continued advancement in organic bioelectronics and regenerative medicine applications.
Engineering and Applying Biocompatible Devices: From Fabrication to Clinical Implementation
The emerging field of organic bioelectronics critically depends on advanced fabrication techniques to create devices that seamlessly integrate with biological systems. The core challenge lies in manufacturing electronic components that are not only functionally sophisticated but also mechanically compliant and biocompatible. This whitepaper provides an in-depth technical analysis of three pivotal fabrication methodologies—inkjet printing, vapor deposition, and vulcanization—that enable the scalable production of such devices. By detailing their operational principles, experimental protocols, and specific applications in biocompatible electronics, this guide serves as an essential resource for researchers and drug development professionals working at the intersection of materials science and biomedical engineering.
Core Fabrication Techniques
Inkjet Printing of Conductive Nanomaterials
Inkjet printing has emerged as a transformative digital fabrication technology for depositing functional electronic materials onto flexible and unconventional substrates, including textiles and biological tissues [30]. This non-contact, additive manufacturing method enables the precise patterning of conductive inks with complex geometries, offering significant advantages for customizable bioelectronic device fabrication.
Experimental Protocol for Inkjet Printing on Textiles:
- Ink Formulation: Prepare conductive ink by synthesizing or procuring stable dispersions of conductive nanomaterials. Common formulations include:
- Silver nanoparticles (AgNPs): Typically 20-40 nm particles dispersed in a mixture of diethylene glycol and water (e.g., 20:80 ratio) with surfactant (e.g., 0.1% w/w Polyvinylpyrrolidone) to prevent aggregation.
- Conductive polymers: Poly(3,4-ethylenedioxythiophene) polystyrene sulfonate (PEDOT:PSS) formulations with 5-10% ethylene glycol to enhance conductivity and dimethyl sulfoxide (1-5%) to improve jetting stability.
- Carbon-based materials: Graphene oxide or single-walled carbon nanotubes dispersed in aqueous solutions with biocompatible surfactants.
Substrate Preparation: Clean textile substrates (e.g., polyester, cotton-polyester blends) sequentially in acetone, isopropyl alcohol, and deionized water via ultrasonic bath for 15 minutes each. Plasma treat substrates (Oâ‚‚ plasma, 100 W, 2 minutes) to enhance surface energy and ink wettability.
Printing Parameters Optimization:
- Determine optimal droplet velocity (typically 2-8 m/s) and volume (1-10 pL) using drop-watch camera systems.
- Calibrate jetting waveform parameters (voltage pulse amplitude, duration, and shape) for specific ink rheology.
- Set substrate temperature to 40-60°C to promote controlled solvent evaporation without clogging printhead nozzles.
Post-Processing: Thermally anneal printed patterns in a convection oven using a stepped profile: ramp to 120°C at 5°C/min, hold for 30 minutes; then ramp to 180°C at 3°C/min, hold for 60 minutes to achieve optimal conductivity and adhesion.
Table 1: Performance Metrics of Inkjet-Printed Conductive Inks on Flexible Substrates
| Ink Material | Typical Viscosity (mPa·s) | Conductivity (S/cm) | Resolution (µm) | Curing Temperature (°C) | Biocompatibility |
|---|---|---|---|---|---|
| Silver Nanoparticles | 8-15 | 1×10ⵠ- 6×10ⵠ| 20-50 | 120-180 | Moderate |
| PEDOT:PSS | 10-20 | 50-1000 | 30-100 | 100-140 | High |
| Graphene | 5-12 | 100-1000 | 25-75 | 130-200 | High |
| Carbon Nanotubes | 6-15 | 100-5000 | 30-80 | 120-180 | Moderate |
The inkjet printing process for creating wearable bioelectronics involves multiple interconnected stages, from material preparation to final performance validation, as illustrated below:
Vapor Deposition Techniques
Vapor deposition encompasses several high-precision coating technologies that create thin, functional films on substrate surfaces. These techniques are particularly valuable for biomedical implants where conformal, pinhole-free coatings are essential for biocompatibility and functionality.
Chemical Vapor Deposition (CVD) Protocol for Biomedical Implants:
- Substrate Preparation: Polish titanium implant substrates with successive silicon carbide papers (P400-P4000 grit). Clean in ultrasonic bath with acetone, ethanol, and deionized water (15 minutes each). Dry under nitrogen stream.
Reactor Loading and Evacuation: Load substrates into CVD chamber. Evacuate to base pressure of 10â»Â³ to 10â»â¶ Torr using turbomolecular pumping system.
Precursor Introduction and Deposition:
- Heat substrate to deposition temperature (typically 400-900°C for inorganic coatings).
- Introduce precursor gases (e.g., hydrocarbon source like CHâ‚„ for DLC coatings at 10-100 sccm flow rate).
- Maintain deposition pressure of 0.1-10 Torr with carrier gas (Ar or Hâ‚‚).
- Apply RF plasma (13.56 MHz, 50-300 W) to activate gas phase reactions for plasma-enhanced CVD (PECVD).
Film Characterization: Measure coating thickness using spectroscopic ellipsometry or profilometry. Evaluate adhesion via scratch test (critical load >20N). Assess corrosion resistance in simulated body fluid (SBF) using potentiostatic measurements.
Physical Vapor Deposition (PVD) Market and Technical Outlook: The PVD market is experiencing rapid growth, projected to expand significantly through 2032, driven by demand across aerospace, automotive, electronics, and medical sectors [31]. This expansion reflects the critical role of vapor deposition in creating advanced coatings that enhance performance, durability, and sustainability of biomedical devices.
Table 2: Comparative Analysis of Vapor Deposition Techniques for Biomedical Applications
| Parameter | Plasma Electrolytic Oxidation (PEO) | Chemical Vapor Deposition (CVD) | Physical Vapor Deposition (PVD) |
|---|---|---|---|
| Coating Thickness | 5-100 µm | 0.01-10 µm | 0.1-5 µm |
| Adhesion Strength | Excellent (metallurgical bond) | Very Good | Good to Very Good |
| Deposition Temperature | Ambient-70°C | 400-900°C | 150-500°C |
| Coating Structure | Porous, fractal | Dense, conformal | Dense, columnar |
| Biocompatibility Enhancement | High (biomimetic surface) | Moderate to High | Moderate to High |
| Corrosion Protection | Excellent | Excellent | Excellent |
| Typical Coating Materials | Ca-, P-containing bioactive phases | Diamond-like carbon, TiN, SiOâ‚‚ | TiN, CrN, HA, Ag |
| Coating Rate | 1-3 µm/min | 0.01-1 µm/min | 0.1-5 µm/min |
Vulcanization Techniques
Vulcanization represents a critical chemical process for enhancing the mechanical properties and stability of elastomeric materials used in bioelectronics. Recent advances have enabled the development of biocompatible, stretchable semiconductors essential for next-generation implantable devices.
Experimental Protocol for Biocompatible Elastomeric Transistors:
- Material Preparation:
- Prepare polymer semiconductor solution: Dissolve poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] (DPPT-TT) in chlorobenzene (5-10 mg/mL).
- Prepare elastomer matrix: Dissolve bromo isobutyl-isoprene rubber (BIIR) in toluene (50-100 mg/mL).
- Prepare vulcanizing agent mixture: Combine sulfur (crosslinker), dipentamethylenethiuram tetrasulfide (DPTT, accelerator), and stearic acid (initiator) in 1:0.5:1 weight ratio.
Solution Blending and Film Formation:
- Mix DPPT-TT and BIIR solutions at optimized 3:7 weight ratio.
- Add vulcanizing agent mixture at 5-10% w/w of total polymer content.
- Stir solution for 2-4 hours at 50°C until homogeneous.
- Deposit blend via spin-coating (500-2000 rpm, 60 s) or blade-coating onto substrate.
- Pre-bake at 70°C for 5 minutes to remove residual solvent.
Vulcanization Process:
- Cure film at 140-160°C for 20-60 minutes in nitrogen atmosphere.
- Control crosslinking density by varying temperature and time.
- Confirm vulcanization completion via Fourier transform infrared spectroscopy (disappearance of C–Br peak at 667 cmâ»Â¹).
Device Fabrication and Characterization:
- Pattern electrodes using biocompatible dual-layer Ag/Au metallization.
- Encapsulate devices with medical-grade silicone layer.
- Perform mechanical testing (cyclic stretching to 100% strain).
- Evaluate electrical performance (field-effect mobility, ON/OFF ratio) under strain.
Molecular Dynamics Simulation of Vulcanization: Advanced computational approaches provide atomic-scale insights into vulcanization mechanisms. Molecular dynamics simulations using GROMACS with GAFF2 force field can model interfacial adhesion energy, diffusion coefficients, and chain entanglements in vulcanized blends [32]. These simulations reveal how different dynamic vulcanization strategies (using diisocyanates, peroxides, or epoxy oligomers) affect mechanical properties through distinct crosslinking topologies.
The relationship between molecular structure, fabrication process, and final device performance in vulcanized bioelectronics involves multiple interconnected factors:
Table 3: Vulcanization Parameters and Performance Outcomes in Biocompatible Electronics
| Vulcanization Parameter | DPPT-TT:BIIR (3:7) Blend | Inverse Vulcanized Polymers | Traditional Vulcanized Rubber |
|---|---|---|---|
| Crosslinking Mechanism | Sulfur vulcanization | Inverse vulcanization (sulfur as major component) | Sulfur vulcanization |
| Young's Modulus | 10â·.â·-10â¸.⸠Pa | 10â¸-10â¹ Pa | 10â·-10â¹ Pa |
| Crack-Onset Strain | >100% | 10-50% | 100-500% |
| Charge Carrier Mobility | 0.1-1 cm²/V·s | Not Applicable | Not Applicable |
| Biocompatibility Standard | ISO 10993 | Under Investigation | Variable |
| Key Applications | Implantable transistors, stretchable circuits | Energy storage, environmental remediation | Tires, seals, gaskets |
| Stability in Physiological Conditions | >30 days | Variable | Not Applicable |
Advanced Applications in Bioelectronics
Biocompatible and Implantable Electronics
The convergence of these fabrication techniques enables revolutionary advances in biocompatible electronics. For instance, vulcanized blend films incorporating semiconducting nanofibers within a medical-grade elastomer matrix have demonstrated exceptional compatibility with biological systems while maintaining electrical functionality under mechanical deformation [8]. These devices exhibit stable operation in logic circuits (inverters, NOR gates, and NAND gates) under physiological conditions, opening possibilities for fully implantable bioelectronic systems.
In Vitro and In Vivo Validation Protocols:
- Cytocompatibility Assessment: Culture human dermal fibroblasts and macrophages on device surfaces for 24-72 hours. Evaluate cell viability using MTT assay (≥90% viability required for biocompatibility). Assess cell proliferation via fluorescence microscopy of stained nuclei and cytoskeleton.
- Inflammatory Response Evaluation: Implant devices subcutaneously in mouse models for 4-12 weeks. Histologically analyze tissue samples for inflammatory markers, fibrosis, and necrosis. Compare with negative (sham surgery) and positive (toxic material) controls.
- Functional Stability Testing: Operate devices in simulated body fluid (SBF) at 37°C for extended periods (30+ days). Monitor electrical performance (mobility, threshold voltage shift, ON/OFF ratio) and structural integrity.
Sustainable Material Considerations
The environmental impact of electronic devices has prompted research into sustainable alternatives. Inverse vulcanized polymers utilizing waste sulfur from fossil fuel refinement represent a promising approach to valorizing industrial byproducts [33]. These materials can contribute to multiple UN Sustainability Goals, including clean water (wastewater remediation), affordable clean energy (better energy storage), industry innovation (construction materials), and responsible consumption (economic symbiosis).
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Bioelectronic Fabrication
| Reagent/Material | Function | Example Specifications | Biocompatibility Considerations |
|---|---|---|---|
| DPPT-TT Semiconductor | Charge transport in organic transistors | Mw: 50-100 kDa, Hole mobility: 0.1-1 cm²/V·s | Requires encapsulation for long-term implantation |
| Bromo Isobutyl–Isoprene Rubber (BIIR) | Biocompatible elastomer matrix | Medical grade, ISO 10993 certified, Young's modulus: 10â·-10⸠Pa | Excellent biocompatibility with minimal inflammatory response |
| PEDOT:PSS | Conductive polymer for printed electrodes | 1-1.3% dispersion in water, Conductivity: 1-1000 S/cm (after treatment) | Good cytocompatibility, stable in physiological environments |
| Silver Nanoparticles | Conductive ink for printed interconnects | 20-40 nm diameter, ≥99.5% metal basis | Potential cytotoxicity requires complete encapsulation |
| Sulfur Vulcanizing System | Crosslinking agent for elastomers | Sulfur (crosslinker), DPTT (accelerator), stearic acid (activator) | Ensure complete reaction to prevent leaching |
| Phosphate Buffered Saline (PBS) | Biocompatibility testing medium | 1X, pH 7.4, without calcium and magnesium | Standard medium for in vitro biocompatibility screening |
| Simulated Body Fluid (SBF) | Corrosion testing electrolyte | Ion concentrations nearly equal to human blood plasma | Accelerated testing of implant degradation |
| N-cyclohexanecarbonylpentadecylamine | N-cyclohexanecarbonylpentadecylamine, MF:C22H43NO, MW:337.6 g/mol | Chemical Reagent | Bench Chemicals |
| Tiprelestat | Tiprelestat, CAS:820211-82-3, MF:C254H416N72O75S10, MW:5999 g/mol | Chemical Reagent | Bench Chemicals |
The strategic integration of inkjet printing, vapor deposition, and vulcanization techniques provides a powerful fabrication toolkit for advancing organic bioelectronics. These methodologies enable the creation of devices with tailored mechanical, electrical, and biological properties essential for seamless integration with living systems. As research continues to refine these processes and address remaining challenges in stability and scalable manufacturing, these advanced fabrication techniques will play an increasingly vital role in realizing the full potential of bioelectronic medicine. The ongoing innovation in these areas promises to accelerate the development of next-generation biomedical devices that can monitor, stimulate, and support biological functions with unprecedented precision and biocompatibility.
The field of implantable neural interfaces is undergoing a transformative shift from rigid to soft, tissue-like electronics, driven by the critical need for improved biocompatibility. Traditional neural implants, constructed from rigid materials like silicon, platinum, and gold, exhibit a significant mechanical mismatch with brain tissue (approximately 180 GPa vs. 1–30 kPa), leading to foreign body responses, inflammation, glial scar formation, and eventual device failure [34] [35]. Organic bioelectronics addresses this fundamental challenge by using carbon-based semiconducting materials that offer intrinsic flexibility, biocompatibility, and the ability to transport both electronic and ionic signals, enabling seamless integration with biological systems [3].
The core thesis of modern biocompatibility research in this domain extends beyond mere inertness; it aims for seamless structural and functional integration. This involves creating devices that are not only soft and flexible but also bioactive or "living," capable of interacting with the nervous system in a truly symbiotic manner [35]. This whitepaper provides an in-depth technical guide to the materials, device architectures, experimental methodologies, and clinical applications of soft, transistor-based neural interfaces, framing them within the broader context of biocompatibility research in organic bioelectronics.
Materials Design for Biocompatible Soft Transistors
Key Material Classes and Their Properties
The pursuit of biocompatibility has driven innovation in several classes of soft electronic materials. The following table summarizes the key materials, their compositions, and their primary characteristics relevant to neural interfacing.
Table 1: Key Materials for Soft, Biocompatible Neural Interfaces
| Material Class | Example Materials | Key Properties | Role in Device |
|---|---|---|---|
| Conductive Polymers | PEDOT:PSS, Polyaniline (PANI) [3] | Mixed ionic-electronic conduction, flexibility, reduced impedance [35] [3] | Electrodes, channel material in OECTs |
| Semiconducting Polymers | DPPT-TT, P3HT, PCPDTBT [8] [36] | Tunable electronic properties, optical absorption for photovoltaics [36] | Active layer in OFETs and photovoltaic devices |
| Biocompatible Elastomers | Bromo isobutyl–isoprene rubber (BIIR), Medical-grade PDMS [8] [35] | Young's modulus matching neural tissue (<100 kPa), ISO 10993 biocompatibility [8] | Matrix for stretchable semiconductors, substrate |
| Hydrogels | Various biopolymer-based gels [35] | High water content, tissue-like mechanical properties [35] | Conformal coating, substrate |
A pivotal advancement is the development of elastomeric organic field-effect transistors (OFETs). One breakthrough involves a vulcanized blend of the semiconducting polymer poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] (DPPT-TT) and the medical-grade elastomer bromo isobutyl–isoprene rubber (BIIR) [8]. This composite forms a semiconducting nanofiber network embedded within an elastic matrix, achieving a Young's modulus similar to human tissues and maintaining stable electrical performance under 50% strain [8]. The vulcanization process, using sulfur-based crosslinkers, enhances mechanical elasticity without disrupting the conjugated structure of the semiconductor, which is crucial for preserving electrical functionality [8].
Addressing the Biointerface with Conformal and Living Electronics
Beyond bulk material properties, the biointerface is critical. To ensure stable and corrosion-resistant contact, researchers have implemented dual-layer metallization using silver (Ag) for excellent electrical contact and gold (Au) for biofluid-corrosion resistance [8]. The ultimate form of biointegration is the creation of "biohybrid" and "all-living" interfaces. A groundbreaking example is "Circulatronics," which uses immune cell–electronics hybrids [36]. Subcellular-sized, wireless, photovoltaic electronic devices (SWEDs) are covalently attached to monocytes and administered intravenously. These hybrids autonomously traffic to inflamed brain regions, implant themselves, and enable focal neuromodulation, completely circumventing the need for surgery [36].
Table 2: Quantitative Performance of Featured Soft Transistors
| Device Parameter | Elastomeric OFET [8] | Circulatronics SWED [36] |
|---|---|---|
| Material System | DPPT-TT:BIIR (3:7 blend) | P3HT:PCBM or PCPDTBT:PCBM |
| Young's Modulus | ~107.7 - 108.8 Pa | Subcellular, free-floating |
| Mechanical Robustness | Stable performance under 50% strain; survives 1000 cycles at 100% strain | Designed for circulation in vasculature |
| Electrical Output | Stable field-effect mobility | VOC = 0.2 V, ISC = 12.8 nA (P3HT, at 10 mW mmâ»Â²) |
| Biocompatibility Evidence | In vitro (human cells) & in vivo (mice): no adverse effects on viability, no major inflammatory response | In vivo (mice): focal implantation in inflamed brain regions |
Experimental Protocols for Biocompatibility and Functionality
Rigorous experimental protocols are essential for validating the performance and biocompatibility of soft neural interfaces. The following workflow and detailed methodologies outline key experiments.
Protocol 1: Fabrication and Characterization of Elastomeric OFETs
Objective: To create and characterize a stretchable, biocompatible OFET based on a semiconducting polymer-elastomer blend [8].
- Solution Preparation: Prepare a blend of the semiconducting polymer (e.g., DPPT-TT) and the medical-grade elastomer (e.g., BIIR) in a suitable solvent. An optimized weight ratio of 3:7 (DPPT-TT:BIIR) is recommended to balance electrical and mechanical properties [8].
- Vulcanization: Add a vulcanization package to the blend, typically comprising sulfur (crosslinker), dipentamethylenethiuram tetrasulfide (DPTT, accelerator), and stearic acid (initiator). This chemically crosslinks the elastomer matrix.
- Film Formation & Characterization:
- Spin-coat or drop-cast the solution onto a substrate.
- Use Fourier Transform Infrared (FTIR) Spectroscopy to confirm successful vulcanization by monitoring the reduction of C–Br peaks (e.g., at 667 cmâ»Â¹) [8].
- Use Atomic Force Microscopy (AFM) and Conductive-AFM (C-AFM) to verify the formation of an interconnected semiconducting nanofiber network and to map its electronic properties [8].
- Device Completion: Pattern source and drain electrodes using a biocompatible, stretchable conductor (e.g., dual-layer Ag/Au metallization) to complete the transistor structure [8].
- Electrical Testing under Strain: Mount the device on a tensile stage and measure transfer and output characteristics (field-effect mobility, ON/OFF ratio) at applied strains from 0% to 50% and over repeated stretching cycles (e.g., 1000 cycles) to assess electromechanical stability [8].
Protocol 2: In Vitro Biocompatibility Assessment
Objective: To evaluate the cytotoxicity and biocompatibility of the device materials.
- Cell Culture: Use relevant cell lines, such as human dermal fibroblasts and macrophages, cultured according to standard protocols.
- Extract Preparation: Incubate sterile device materials or their extracts in cell culture medium.
- Viability and Proliferation Assays:
- Cell Viability: Perform live/dead staining assays after 24-72 hours of exposure to material extracts. Quantify the percentage of live versus dead cells.
- Cell Proliferation: Use metabolic assays like MTT or Alamar Blue to assess cell proliferation over several days. Compare results to cells cultured on standard tissue culture plastic [8].
- Cell Migration Assay: Perform a scratch wound healing assay to determine if the materials or their leachates inhibit normal cell migration [8].
Protocol 3: In Vivo Implantation and Functional Validation
Objective: To assess long-term tissue integration, foreign body response, and device functionality in a living animal model.
- Animal Model and Implantation: Perform sterile implantation of the device into the target region (e.g., cortex, specific nucleus) of an animal model (e.g., mouse) following approved ethical guidelines. For Circulatronics, intravenously inject the monocyte-SWED hybrids [36].
- Histological Analysis (after weeks/months):
- Perfuse and fix the animal's brain at predetermined time points.
- Section the tissue and perform immunohistochemical staining for key biomarkers.
- Gliosis: Stain for glial fibrillary acidic protein (GFAP) to label astrocytes. A minimal increase in GFAP signal around the implant indicates a mild FBR.
- Microglial Activation: Stain for ionized calcium-binding adapter molecule 1 (Iba1) to identify activated microglia.
- Neuronal Survival: Stain for neuronal nuclei (NeuN) to quantify neuronal density near the implant interface compared to distal regions [8] [34].
- Functional Neuromodulation: For active devices, demonstrate the capability to record neural signals or, as with Circulatronics, wirelessly stimulate neural activity. For stimulation, apply the triggering input (e.g., specific wavelength of light for photovoltaic SWEDs) and measure evoked neural responses or behavioral changes, confirming focal modulation with ~30-µm precision [36].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Soft Neural Interface Development
| Reagent/Material | Function in Research | Example Use Case |
|---|---|---|
| DPPT-TT Semiconductor | Provides high charge-carrier mobility in a polymer backbone. | Forms the conductive nanofiber network in elastomeric OFETs [8]. |
| BIIR (Bromo Isobutyl–Isoprene Rubber) | Medical-grade elastomer that provides a biocompatible, stretchable matrix. | Blended with DPPT-TT to create a soft, vulcanizable semiconductor film [8]. |
| PEDOT:PSS | Conductive polymer for low-impedance charge injection and ion-to-electron transduction. | Used as a coating for neural electrodes or as a stand-alone electrode in devices like NeuroGrid [35] [3]. |
| Sulfur Vulcanization Package | Enables chemical crosslinking of the elastomer, enhancing mechanical integrity. | Used to vulcanize BIIR, improving the elasticity and stability of the blend film [8]. |
| Subcellular-sized Wireless Electronic Devices (SWEDs) | Act as free-floating, wirelessly powered stimulators for non-surgical implantation. | Covalently attached to monocytes for targeted delivery to inflamed brain regions (Circulatronics) [36]. |
| ER-000444793 | ER-000444793, MF:C23H18N2O2, MW:354.4 g/mol | Chemical Reagent |
| NHI-2 | NHI-2, MF:C17H12F3NO3, MW:335.28 g/mol | Chemical Reagent |
Clinical Translation and Future Perspectives
The field is rapidly moving from laboratory research to clinical application. Closed-loop, sensing-enabled deep brain stimulation (DBS) systems, such as Medtronic's BrainSense technology, represent a significant milestone. This system, recently approved by the FDA, can record brain signals and adapt stimulation in real-time for Parkinson's disease, marking the largest commercial launch of therapeutic brain-computer interface technology to date [37]. Furthermore, ultra-thin micro-electrocorticography (μECoG) grids from companies like Precision Neuroscience are advancing through clinical trials, aiming for minimally invasive cortical mapping [35].
Future research directions will focus on further enhancing biocompatibility through "living" electrodes that actively promote tissue repair, developing fully bioresorbable devices to eliminate the need for explantation surgery, and refining non-surgical delivery methods like Circulatronics for a wider range of neurological applications [35] [36]. The convergence of organic bioelectronics with immunology and cell biology will continue to blur the lines between electronic implants and biological tissue, ultimately realizing the promise of seamless, lifelong neural interfaces for treating and understanding brain disorders.
Chronic wounds, including diabetic foot ulcers, venous leg ulcers, and pressure ulcers, represent a significant global health challenge characterized by prolonged inflammation, high infection risk, and impaired tissue regeneration. These non-healing wounds affect millions of patients worldwide, with treatment costs in the United States alone exceeding $25 billion annually [38] [39]. Traditional wound dressings operate passively, primarily providing coverage and moisture control without actively monitoring or responding to the dynamic wound microenvironment [39]. This limitation has spurred the development of intelligent wound dressings that integrate sensing capabilities with active therapeutic interventions to promote healing.
Smart bandages represent a paradigm shift in wound care, moving beyond passive protection to active wound management. These advanced systems incorporate flexible electronics, microfluidics, and stimuli-responsive biomaterials to continuously monitor wound status and deliver targeted therapies in response to pathological changes [38]. By combining real-time diagnostic capabilities with automated treatment modalities, smart bandages aim to address the complex challenges of chronic wound management, including persistent infection, prolonged inflammation, and inadequate healing signals [39]. The evolution of these technologies marks a convergence of bioengineering, materials science, and digital health, offering the potential for personalized wound therapy that adapts to the changing wound environment.
The integration of organic bioelectronics has been particularly transformative for smart bandage development, as these materials offer superior biocompatibility, mechanical flexibility, and chemical functionality compared to conventional inorganic electronics. This technical guide explores the core components, operating principles, and experimental methodologies underlying modern smart bandage technologies, with particular emphasis on their applications within organic bioelectronics biocompatibility research.
Core Components and Operating Principles
Integrated Sensing Systems
Smart bandages incorporate multiple sensing modalities to monitor the complex wound microenvironment. These sensors track biochemical and physical parameters that serve as critical indicators of healing status and infection presence. The most advanced systems employ multiplexed sensing approaches to provide a comprehensive assessment of wound conditions.
Table 1: Key Biomarkers Monitored by Smart Bandage Sensors
| Biomarker | Significance in Wound Healing | Detection Methods | Normal Range | Pathological Indication |
|---|---|---|---|---|
| pH | Indicates infection and healing status [38] | Potentiometric sensors, colorimetric dyes [40] [39] | 4.5-6.5 (healthy skin) [39] | Alkaline shift (7.0-9.0) suggests infection [39] |
| Temperature | Marker of inflammation and infection [38] | Thermal sensors, thermistors [38] | Varies by body location | Elevated temperature indicates inflammatory response |
| Oxygen | Indicator of tissue perfusion and angiogenesis [38] | Electrochemical sensors, optical probes [38] | Tissue-dependent | Hypoxia impairs healing [38] |
| Nitric Oxide | Inflammatory marker [41] [42] | Electrochemical sensors [41] | Baseline level elevation | Persistent elevation indicates chronic inflammation [41] |
| Hydrogen Peroxide | Infection biomarker [41] [42] | Enzymatic and non-enzymatic sensors [41] | Minimal in healthy wounds | Elevated levels signal bacterial presence [41] |
| Moisture | Affects re-epithelialization and inflammation [38] | Impedance sensors, capacitive measurement [38] | Balanced moisture | Excess fluid promotes bacterial growth [38] |
Recent advances in sensing technologies have enabled the development of sophisticated monitoring systems. The iCares smart bandage, for instance, incorporates a nanoengineered biomarker sensor array that detects reactive oxygen and nitrogen species, pH, and temperature simultaneously [41] [42]. This multi-parameter approach allows for comprehensive wound assessment and early detection of complications. Similarly, liquid diode-based bandages integrate ultrasensitive 3D polyaniline mesh (M-PANI) biosensors with unidirectional fluid drainage capabilities, enabling dynamic pH monitoring while managing wound exudate [40]. These systems demonstrate the trend toward integrated sensing platforms that provide real-time, multidimensional data on wound status.
Drug Delivery Mechanisms
Smart bandages employ various controlled release mechanisms to deliver therapeutic agents in response to wound conditions. These systems represent a significant advancement over conventional dressings that release drugs passively without regard to actual wound needs.
Stimuli-Responsive Release Systems utilize materials that change their properties in response to specific wound biomarkers. pH-responsive hydrogels, for instance, can swell or shrink in response to pH changes, releasing antimicrobials or growth factors when the wound environment becomes alkaline, indicating infection [39]. Similarly, temperature-sensitive polymers can release therapeutic payloads in response to localized fever at the wound site [39]. These materials form the basis of autonomous wound management systems that require no external intervention.
Microfluidic Delivery Platforms represent another approach to controlled drug release. The iCares bandage employs a triad of microfluidic modules: a membrane that draws wound fluid from the wound surface, a bioinspired component that transports the fluid to the sensor array, and a micropillar module that carries the sampled fluid away from the bandage [41]. This system not only manages exudate but can also be integrated with drug reservoirs for targeted therapy delivery in response to sensor readings.
Electrically-Controlled Release Systems use applied electrical fields to trigger drug release from conductive polymers or hydrogel matrices. These systems enable precise temporal control over drug delivery and can be coordinated with sensor readings to provide on-demand therapy [41]. The ability to apply electrical stimulation directly to the wound bed also promotes healing through enhanced cell migration and proliferation [39].
Table 2: Drug Delivery Mechanisms in Smart Bandages
| Delivery Mechanism | Triggering Signal | Therapeutic Agents | Control Modality | Advantages |
|---|---|---|---|---|
| Stimuli-Responsive Hydrogels | pH, temperature, enzyme levels [39] | Antibiotics, growth factors, anti-inflammatories [38] | Autonomous | Self-regulated, no external power needed |
| Microfluidic Systems | Sensor input or predefined schedule [41] | Liquid formulations, biologics [41] | Active (pump-based) | Precise volume control, multi-drug delivery |
| Conductive Polymer Films | Electrical stimulation [39] | Ions, small molecules [39] | Externally controlled | Precise temporal control, on-demand release |
| Nanofiber Membranes | Diffusion-based or material degradation [43] | Antimicrobial nanoparticles, growth factors [43] | Passive or enzyme-triggered | High surface area, tunable release kinetics |
Experimental Protocols and Methodologies
Sensor Performance Validation
Robust validation of sensor performance is essential for reliable wound monitoring. The following protocol outlines standard methodologies for characterizing pH sensors in smart bandages, based on recent studies [40].
Electrochemical Characterization of pH Sensors: Prepare standard pH buffer solutions ranging from 4.0 to 9.0, covering the physiologically relevant range for wounds. Using a three-electrode system (working electrode, reference electrode, counter electrode), measure the open-circuit potential of the pH sensor at each pH value. Plot the potential against pH to determine sensor sensitivity (mV/pH) through linear regression. The M-PANI-based pH biosensor demonstrated a sensitivity of 61.5 mV/pH across this range, indicating excellent performance [40].
Stability and Reproducibility Testing: For stability assessment, continuously monitor the sensor response in a controlled pH environment over 48 hours, recording signal variation. To evaluate reproducibility, test multiple sensors (n ≥ 5) from different production batches in the same pH conditions and calculate the relative standard deviation (RSD). The liquid diode-based smart bandage exhibited only 4.8% signal decline after 48 hours of dynamic testing and a device-to-device RSD of 3.1%, confirming high stability and repeatability [40].
Selectivity Testing: Expose the sensor to potential interferents present in wound exudate, including uric acid, glucose, and lactate, at physiologically relevant concentrations. Measure the sensor response in the presence of these compounds to confirm that pH measurements remain unaffected.
In Vivo Efficacy Evaluation
Animal studies provide critical data on smart bandage performance in biologically relevant environments. The following protocol is adapted from recent smart bandage evaluations [41] [40].
Animal Model Establishment: Utilize diabetic or immunocompromised rodent models to mimic impaired healing conditions. For the iCares bandage evaluation, researchers employed a mouse model of diabetes to replicate the challenging healing environment of diabetic foot ulcers [41]. Create standardized full-thickness wounds on the dorsal surface using biopsy punches.
Experimental Groups: Include multiple experimental groups: (1) smart bandage with active sensing and treatment capabilities, (2) passive advanced dressing control, (3) conventional gauze control, and (4) untreated wounds. Assign animals randomly to groups and ensure blinded assessment of outcomes.
Monitoring and Analysis: Apply smart bandages and monitor sensor readings continuously throughout the healing process. For the iCares system, researchers collected data on nitric oxide, hydrogen peroxide, pH, and temperature, identifying early changes consistent with infection before visible symptoms appeared [41]. Assess wound closure rates through regular photographic documentation and planimetric analysis. At predetermined endpoints, harvest tissue for histological evaluation of re-epithelialization, granulation tissue formation, and inflammatory response.
Clinical Validation in Human Subjects
Translation to human clinical studies represents the final stage of smart bandage validation. Recent research has demonstrated the feasibility of smart bandages in patient care settings [41].
Patient Recruitment and Selection: Enroll patients with chronic wounds, including diabetic foot ulcers and venous leg ulcers, that have failed to heal through conventional therapies. The iCares study included 20 human patients with chronic wounds that were not healing due to diabetes or poor blood circulation [41]. Obtain informed consent and ethical approval following institutional guidelines.
Bandage Application and Monitoring: Apply smart bandages to wounds according to standardized protocols. For the iCares bandage, researchers utilized a flexible, biocompatible polymer strip that could be 3D printed at low cost, incorporating a disposable sensor array and reusable electronics for signal processing [41]. Monitor patients for the duration of the study, collecting sensor data continuously.
Data Analysis and Algorithm Development: Process sensor data to extract meaningful patterns related to wound status. In the iCares clinical study, researchers developed a machine-learning algorithm that successfully classified patients' wounds and predicted healing time with accuracy comparable to an expert clinician [41]. This approach demonstrates the potential for data-driven wound assessment and personalized treatment planning.
Safety and Comfort Evaluation: Document any adverse events, skin reactions, or patient discomfort associated with smart bandage use. Assess ease of application and removal, as well as wearability during daily activities.
Wound Healing Signaling Pathways
Understanding the molecular pathways involved in wound healing is essential for developing targeted interventions in smart bandage systems. Chronic wounds are characterized by dysregulation of these pathways, particularly in diabetic and immunocompromised patients.
The normal wound healing process progresses through coordinated phases of hemostasis, inflammation, proliferation, and remodeling [38]. In chronic wounds, this process becomes disrupted, with the inflammatory phase persisting for months or even years [38]. Key abnormalities include persistent neutrophil activation leading to elevated protease levels (matrix metalloproteinases), which degrade extracellular matrix proteins and growth factors essential for healing [38] [39]. Simultaneously, macrophage dysfunction impairs the transition from inflammatory to proliferative phase, resulting in inadequate angiogenesis and tissue formation [39].
Smart bandages target these dysregulated pathways through multiple mechanisms. Sensing of inflammatory biomarkers like nitric oxide and hydrogen peroxide allows for early detection of persistent inflammation [41]. Controlled release of anti-inflammatory compounds, antimicrobial agents, or growth factors can then intervene at the molecular level to restore balanced healing responses. Electrical stimulation modalities can enhance cell migration and angiogenesis, addressing the impaired proliferation characteristic of chronic wounds [39].
Research Reagent Solutions
The development and implementation of smart bandage technologies require specialized materials and reagents that enable sensing, drug delivery, and biocompatibility.
Table 3: Essential Research Reagents for Smart Bandage Development
| Reagent Category | Specific Examples | Function in Smart Bandages | Key Characteristics |
|---|---|---|---|
| Flexible Substrate Materials | Poly(ethylene terephthalate) (PET), Polyether sulfone (PES), Thermoplastic polyurethane (TPU) [40] | Base material for sensors and electronics | Biocompatibility, mechanical flexibility, gas permeability |
| Conductive Polymers | Polyaniline (PANI), Poly(3,4-ethylenedioxythiophene) (PEDOT) [40] | Sensor electrodes, electrically-controlled drug release | Conductivity, electrochemical stability, biocompatibility |
| Stimuli-Responsive Hydrogels | pH-sensitive polyacrylates, temperature-sensitive poly(N-isopropylacrylamide) | Controlled drug delivery, wound interface layer | Responsive swelling/deswelling, biocompatibility |
| Microfluidic Components | PDMS channels, membrane pumps, microvalves [41] | Fluid management, sample transport to sensors | Precise fluid control, miniaturization, reliability |
| Biosensing Elements | Enzyme-based sensors (glucose oxidase, urease), nanoparticle-based sensors | Specific biomarker detection | Sensitivity, selectivity, stability in wound environment |
| Antimicrobial Agents | Silver nanoparticles, iodine complexes, antibiotics [38] | Infection control in infected wounds | Broad-spectrum activity, controlled release profile |
| Growth Factors | VEGF, PDGF, EGF [38] | Promotion of angiogenesis and tissue regeneration | Stability, bioactivity, appropriate release kinetics |
The selection of appropriate reagents is critical for ensuring smart bandage functionality and biocompatibility. For instance, the liquid diode-based smart bandage utilizes an ultrahydrophilic PES membrane combined with a hydrophobic TPU layer to achieve unidirectional fluid transport [40]. This asymmetric wettability enables continuous drainage of wound exudate while preventing backflow of contaminants. Similarly, the integration of 3D polyaniline mesh (M-PANI) as a pH sensing interface provides excellent sensitivity (61.5 mV/pH) across the physiologically relevant range while maintaining stability during extended use [40].
Organic bioelectronic materials play a particularly important role in advancing smart bandage technology. These materials offer unique advantages including mechanical compatibility with soft tissues, efficient ionic conductivity, and mixed ionic-electronic conduction capabilities that enable seamless interfacing with biological systems. The development of novel organic electronic materials continues to expand the functionality and biocompatibility of smart wound care devices.
Smart bandages represent a transformative approach to wound care, integrating sensing capabilities with active treatment modalities to address the complex challenges of chronic wounds. Recent advances in flexible electronics, microfluidics, and stimuli-responsive materials have enabled the development of sophisticated systems that can monitor multiple wound biomarkers simultaneously and respond with appropriate therapeutic interventions. Technologies like the iCares bandage and liquid diode-based dressings demonstrate the potential for real-time wound assessment and personalized treatment, with clinical studies showing promising results in human patients [41] [40].
Despite these advances, significant challenges remain in the widespread clinical adoption of smart bandage technologies. Ensuring long-term stability and reliability in the harsh wound environment requires continued materials development. Manufacturing scalability and cost-effectiveness must be addressed to make these technologies accessible to diverse patient populations [43] [39]. Additionally, navigating regulatory pathways for complex combination products presents hurdles that must be overcome through rigorous validation and standardization.
Future research directions will likely focus on enhancing the intelligence of these systems through more sophisticated algorithms and decision-making capabilities. Integration with telemedicine platforms could enable remote wound monitoring, expanding access to expert care beyond clinical settings. The development of closed-loop systems that autonomously adjust therapy based on sensor readings represents the ultimate goal for smart wound management. As organic bioelectronics continue to advance, smart bandages will become increasingly sophisticated in their ability to interface with biological systems, ultimately transforming the standard of care for patients with chronic wounds.
The field of implantable bioelectronics is undergoing a transformative shift from rigid, passive devices toward soft, intelligent systems capable of seamless integration with biological tissues. Stretchable active-matrix transistors represent a cornerstone technology in this evolution, enabling the development of complex logic circuits on substrates that mimic the mechanical properties of human tissue. Traditional biomedical implants, constructed from rigid inorganic materials like silicon, exhibit a significant mechanical mismatch with soft biological tissues, often leading to complications such as microinjury, inflammation, and fibrosis over time [8]. This mechanical disparity compromises both device functionality and long-term biocompatibility.
Organic bioelectronics has emerged as a promising solution to this challenge by leveraging carbon-based semiconducting materials that demonstrate inherent flexibility, biocompatibility, and the capacity to carry both electrical and ionic impulses [44] [3]. The unique value proposition of stretchable active-matrix transistors lies in their ability to maintain stable electrical performance under mechanical deformation while interfacing directly with biological systems without eliciting significant immune responses. These devices form the fundamental building blocks for sophisticated bioelectronic circuits capable of processing physiological signals in situ, enabling applications from continuous health monitoring to closed-loop therapeutic interventions [8].
The integration of complex logic functionality onto biocompatible substrates represents a significant advancement over first-generation bioelectronic devices. Where early implants primarily recorded or stimulated tissue activity, modern stretchable active-matrix systems can perform local signal processing, decision-making, and multiplexed operations at the biotic-abiotic interface [3]. This capability is particularly crucial for managing the vast amounts of data generated by high-density electrode arrays and for implementing intelligent stimulation protocols that respond to physiological states in real-time. The development of such systems requires careful co-optimization of electrical performance, mechanical properties, and biological compatibility—a multidisciplinary challenge at the frontiers of materials science, electrical engineering, and biology.
Material Design Strategies for Biocompatible Stretchable Transistors
Semiconductor-Elastomer Composites
The core innovation enabling stretchable transistor technology involves creating semiconductor-elastomer composites that balance electrical and mechanical properties. Recent breakthroughs have utilized blends of semiconducting polymers with medical-grade elastomers, particularly through the development of a vulcanized blend film of bromo isobutyl–isoprene rubber (BIIR) and poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] (DPPT-TT) [8]. In this composite architecture, DPPT-TT forms an interconnected nanofibre network within the elastic BIIR matrix, imparting both stretchability and semiconducting functionality. The phase separation that forms this nanofibre network results from the surface energy disparity between the semiconductor and elastomer, creating percolation pathways for charge transport that remain stable under mechanical deformation [8].
The vulcanization process represents a critical fabrication step that enhances the mechanical properties of the composite through chemical crosslinking. This process employs sulfur as a crosslinker, dipentamethylenethiuram tetrasulfide (DPTT) as an accelerator, and stearic acid as an initiator [8]. Fourier transform infrared spectroscopy analysis confirms successful vulcanization through the reduction of C–Br peaks (at 667 cm−1) and C=C peaks (at 1,538 cm−1) in the BIIR component, while the conjugated structure of DPPT-TT remains preserved, as evidenced by unchanged UV-visible absorption spectra [8]. This selective crosslinking enhances elasticity while maintaining electrical functionality, with vulcanized blend films demonstrating higher field-effect mobility and ON/OFF ratios compared to non-vulcanized counterparts.
Table 1: Key Material Properties of Semiconductor-Elastomer Composites
| Material Component | Function | Key Properties | Optimized Parameters |
|---|---|---|---|
| DPPT-TT | Semiconductor | Forms interconnected nanofibre network for charge transport | High charge carrier mobility maintained under strain |
| BIIR (Bromo Isobutyl–Isoprene Rubber) | Elastomer Matrix | Medical-grade, biocompatible, provides stretchability | Young's modulus similar to human tissue (~10⸠Pa) |
| Sulfur-based Vulcanization System | Crosslinking | Enhances mechanical properties through chemical bonds | Maintains electrical performance up to 100% strain |
| Dual-layer Ag/Au Electrodes | Conductors | Provide robust, stretchable, corrosion-resistant contacts | Biocompatible interface resistant to biofluid corrosion |
Biocompatibility Considerations for Implantable Electronics
Biocompatibility in implantable electronics extends beyond mere non-toxicity to encompass comprehensive biological integration. According to ISO 10993 standards for biological evaluation of medical devices, biocompatibility assessment must consider the specific application environment and contact duration [44]. Materials can interact with tissues in four primary ways: toxic (causing adverse effects), bioinert (minimal interaction), bioactive (forming intimate connections), or bioresorbable (dissolving over time) [44]. For long-term implantable transistors, a bioinert or bioactive response is typically desired to maintain device functionality while minimizing foreign body reactions.
The mechanical properties of electronic materials play a crucial role in biocompatibility. Biological tissues typically exhibit Young's moduli in the kPa range (e.g., brain ~1 kPa, skin ~100 kPa), while conventional electronic materials like silicon have moduli of ~100 GPa [44] [3]. This dramatic mechanical mismatch can cause chronic inflammation, fibrosis, and device encapsulation. Organic semiconductors address this challenge with tunable mechanical properties—conducting polymers exhibit moduli from 20 kPa to 3 GPa (or 20 kPa–2 MPa as gels), much closer to biological tissues [44]. The vulcanized DPPT-TT:BIIR blend previously discussed achieves a Derjaguin–Muller–Toporov (DMT) modulus ranging from approximately 10â·.â· Pa to 10â¸.⸠Pa, closely matching human tissues and reducing mechanical mismatch [8].
In vitro biocompatibility assessments for organic electronic materials typically employ direct contact cytotoxicity tests, including mitochondrial dehydrogenase performance measurement (MTT assay), XTT cell proliferation assay, neutral red uptake cytotoxic assay, and colony formation assays [44]. For the DPPT-TT:BIIR blend transistors, in vitro assessments with human dermal fibroblasts and macrophages showed no adverse effects on cell viability, proliferation, or migration [8]. Furthermore, in vivo implantation studies in mice demonstrated no major inflammatory response or tissue damage, confirming the long-term integration potential of these devices [8].
Fabrication and Manufacturing Approaches
Advanced Fabrication Protocols for Stretchable Transistors
The fabrication of high-performance stretchable transistors requires specialized methodologies that accommodate both electrical performance and mechanical deformability. A representative protocol for creating biocompatible stretchable organic field-effect transistors (sOFETs) involves multiple carefully optimized steps [8]:
Substrate Preparation and Electrode Patterning: The process begins with the selection of an appropriate elastomeric substrate, typically medical-grade BIIR or similar biocompatible elastomer. The substrate is cleaned and prepared for electrode deposition. For creating stretchable and biocompatible electrodes, a dual-layer metallization approach is employed, sequentially depositing silver (Ag) for excellent electrical contact properties, followed by gold (Au) for robust protection against biofluid-induced corrosion. X-ray photoelectron spectroscopy (XPS) depth profiling confirms the uniform distribution of these metal layers, ensuring consistent performance [8].
Semiconductor Composite Preparation and Deposition: The semiconductor composite is prepared by blending DPPT-TT and BIIR in an optimized 3:7 weight ratio using a solution-processing technique. This specific ratio has been demonstrated to provide the optimal balance between field-effect mobility and crack-onset strain, sustaining up to 100% strain without mechanical damage [8]. The blend is dissolved in an appropriate solvent system and deposited onto the substrate through spin-coating or printing techniques to form a uniform thin film.
Vulcanization Process: The deposited semiconductor film undergoes vulcanization to enhance its mechanical properties. The process involves heating the film to a specific temperature (optimized based on the elastomer system) in the presence of the sulfur-based crosslinking system. The vulcanization procedure serves dual purposes: it crosslinks the BIIR elastomer chains to improve elasticity while simultaneously acting as a thermal annealing process that optimizes the morphology of the semiconducting polymer film [8].
Encapsulation and Device Integration: For implantable applications, appropriate encapsulation is critical to protect the device from biofluids while maintaining mechanical flexibility. Thin, permeable encapsulation layers that allow certain molecular exchanges while protecting electronic components are typically employed. Finally, multiple transistors are interconnected to form functional circuits, with careful attention to maintaining stretchability throughout the entire system.
Manufacturing Techniques for Scalable Production
Unlike conventional silicon electronics that require production in expensive multi-billion-dollar foundries, organic electronics are characterized by compatibility with low-cost manufacturing techniques [3]. Solution-processable organic semiconductors can be formulated into functional inks and processed at ambient temperatures, enabling techniques such as inkjet printing, screen printing, spin-coating, spray-coating, and vacuum evaporation [3]. These methods facilitate cost-effective, high-volume fabrication of electronics on lightweight, adaptable polymer substrates.
Printing processes have shown particular promise for scalable production of stretchable electronics. Screen printing, as a stencil printing process using an emulsion screen template, enables mass production of highly reproducible electrodes and circuits [45]. Inkjet printing offers digital patterning capabilities without the need for physical masks, allowing for rapid prototyping and customization [45]. For carbon-based materials, pattern transferring processes, spray coating, and layer-by-layer assembly have been successfully employed, though each method presents specific challenges such as residual polymers in transfer processes or adhesion stability in spray coating [45].
Electrical Performance and Logic Circuit Integration
Electrical Characterization Under Mechanical Deformation
The electrical performance of stretchable transistors must remain stable under various mechanical deformations encountered during implantation and use. Comprehensive characterization involves evaluating key parameters across different strain conditions:
Strain-Dependent Electrical Properties: For the vulcanized DPPT-TT:BIIR blend transistors, electrical performance remains remarkably stable under mechanical strain. These devices exhibit negligible changes in mobility under strains from 0% to 100% on rigid substrates [8]. The interconnected DPPT-TT nanofibre network aligns along the strain direction without mechanical cracking, as evidenced by the linear increase in dichroic ratio with applied strain (0%–50%) [8]. Atomic force microscopy (AFM) and conductive AFM (C-AFM) images confirm this alignment, showing a strain-insensitive conductive path maintained through the nanofibre network [8].
Durability and Cycling Performance: For practical implantable applications, devices must maintain functionality through repeated mechanical stress. The mobility of the DPPT-TT:BIIR blend film remains consistent after 1,000 stretching cycles at 100% strain, demonstrating excellent mechanical durability [8]. This endurance is critical for applications in dynamic biological environments such as moving muscle tissue or pulsating blood vessels.
Stability in Physiological Environments: Operation in biological environments presents additional challenges including exposure to ions, proteins, and varying pH levels. The dual-layer Ag/Au metallization provides robust protection against biofluid corrosion, maintaining electrode integrity in physiological conditions [8]. Additionally, transistors exhibit stable operation in logic circuits (including inverters, NOR gates, and NAND gates) under physiological conditions, enabling complex signal processing at the biotic-abiotic interface [8].
Table 2: Electrical Performance Metrics of Stretchable Transistors Under Deformation
| Performance Parameter | Initial Value (0% Strain) | Value at 50% Strain | Value at 100% Strain | After 1000 Cycles (100% Strain) |
|---|---|---|---|---|
| Field-Effect Mobility | High (Material Dependent) | Negligible Change | Negligible Change | Consistent with Initial |
| ON/OFF Current Ratio | >10³ | Maintained | Maintained | Maintained |
| Contact Resistance | Low | Minimal Increase | Minimal Increase | Slight Increase |
| Circuit Functionality | Full Operation | Maintained | Maintained | Maintained with Minor Degradation |
Complex Logic Circuit Implementation
The integration of individual stretchable transistors into complex logic circuits represents a significant milestone toward sophisticated bioelectronic systems. Recent demonstrations have successfully implemented fundamental logic gates including inverters, NOR gates, and NAND gates using stretchable organic field-effect transistors (sOFETs) on biocompatible substrates [8]. These logic families provide the foundation for more complex computational capabilities directly at the tissue-device interface.
The transition from discrete transistors to functional circuits requires careful design considerations to maintain performance under mechanical deformation. Interconnects between devices must exhibit similar stretchability to the transistors themselves, necessitating specialized routing strategies and materials. The use of meander-shaped or serpentine interconnects can accommodate significant strain while maintaining electrical continuity. Additionally, circuit design must account for potential variations in transistor parameters under strain, employing robust architectures that tolerate parameter fluctuations.
For bioelectronic applications, these logic circuits enable critical functions such as signal preprocessing, multiplexing, and closed-loop control. For example, active-matrix arrays for neural recording can incorporate local amplification and filtering at each electrode site, significantly improving signal quality before transmission [3]. Similarly, intelligent stimulation systems can implement safety limits and adaptive protocols directly on the implant, reducing the computational burden on external systems and enhancing response times.
Experimental Characterization Protocols
Mechanical and Electrical Testing Methodology
Rigorous experimental characterization is essential to validate the performance of stretchable transistors for implantable applications. Standardized testing protocols enable meaningful comparison between different material systems and device architectures:
Mechanical Testing Protocol:
- Uniaxial Strain Testing: Devices are mounted on a programmable strain stage capable of applying precise uniaxial deformation. Strain is applied in incremental steps (typically 10% increments) up to the maximum specified strain (e.g., 100%). At each strain level, optical microscopy images are captured to monitor for crack formation or delamination [8].
- Cyclic Fatigue Testing: For durability assessment, samples undergo repeated stretching cycles (e.g., 1,000 cycles at 100% strain) while monitoring electrical parameters at regular intervals. The testing frequency is typically set to 0.1-1 Hz to simulate physiological motion [8].
- Modulus Measurement: Atomic force microscopy (AFM) in force spectroscopy mode is employed to map the Derjaguin–Muller–Toporov (DMT) modulus across the semiconductor film, confirming mechanical compatibility with biological tissues [8].
Electrical Characterization Protocol:
- Transfer and Output Characteristics: Standard field-effect transistor characterization is performed using a semiconductor parameter analyzer. Transfer characteristics (drain current vs. gate voltage) are measured at constant drain voltage, while output characteristics (drain current vs. drain voltage) are measured at various gate voltages. These measurements are repeated at different strain levels to quantify performance stability [8].
- Mobility Extraction: Field-effect mobility is calculated from the transfer characteristics in the linear regime using standard MOSFET equations. The stability of this parameter under strain is a key performance metric [8].
- Gate Bias Stress Testing: To evaluate operational stability, devices are subjected to continuous gate bias stress while monitoring threshold voltage shifts over time. This testing is particularly important for assessing longevity in continuous monitoring applications [8].
Biocompatibility Assessment Procedures
Biocompatibility evaluation follows standardized ISO 10993 protocols, adapted for organic electronic materials:
In Vitro Cytotoxicity Assessment:
- Direct Contact Test: Devices or material samples are placed in direct contact with cultured cells (typically human dermal fibroblasts and macrophages for initial screening). Cell viability is assessed after 24-72 hours using MTT assay, which measures mitochondrial dehydrogenase activity as an indicator of metabolic health [8] [44].
- Extract Testing: Material extracts are prepared by incubating devices in cell culture media at 37°C for 24 hours. This extract is then applied to cell cultures, and viability is assessed after 24-48 hours [44].
- Cell Proliferation and Migration Assays: Beyond basic cytotoxicity, effects on cell proliferation (using BrdU incorporation or similar methods) and migration (using scratch wound assays) are evaluated to ensure normal cellular function in the presence of the material [8].
In Vivo Biocompatibility Assessment:
- Subcutaneous Implantation: Devices are implanted subcutaneously in animal models (typically mice or rats) for specified durations (e.g., 4, 12, and 24 weeks). The implantation site is subsequently examined for inflammatory responses, fibrosis, and tissue integration [8].
- Histological Analysis: Explanted tissue surrounding the device is sectioned and stained (e.g., with H&E for general morphology, Masson's trichrome for collagen deposition) to evaluate tissue response and fibrous capsule formation [8] [44].
- Immunohistochemistry: Staining for specific immune markers (e.g., CD68 for macrophages, CD3 for T-cells) provides detailed information about the immune response to the implanted material [44].
The Scientist's Toolkit: Essential Materials and Methods
Table 3: Research Reagent Solutions for Stretchable Bioelectronic Devices
| Material/Reagent | Function | Key Characteristics | Application Notes |
|---|---|---|---|
| DPPT-TT Semiconductor | Charge Transport | High mobility, forms nanofibre networks | Optimized at 30% weight fraction in BIIR blend |
| BIIR Elastomer | Stretchable Matrix | Medical-grade, biocompatible, crosslinkable | Meets ISO 10993 standards; enables tissue-like mechanics |
| Sulfur Vulcanization System | Crosslinking | Enhances mechanical properties | Includes sulfur, DPTT accelerator, stearic acid initiator |
| Dual-Layer Ag/Au Electrodes | Conductive Interconnects | Biofluid-resistant, stretchable | Ag for conductivity, Au for corrosion protection |
| PEDOT:PSS | Alternative Conductive Polymer | Mixed ionic-electronic conduction | Suitable for electrochemical transistors; requires stability enhancements |
| Cell Culture Assays | Biocompatibility Screening | MTT, XTT, neutral red uptake | Required for ISO 10993 compliance |
| AFM with Conductive Mode | Material Characterization | Maps modulus and conductivity simultaneously | Critical for structure-property relationships |
| (R)-Clevidipine-13C,d3 | (R)-Clevidipine-13C,d3, MF:C21H23Cl2NO6, MW:460.3 g/mol | Chemical Reagent | Bench Chemicals |
| CVI-LM001 | CVI-LM001, MF:C25H25NO5S, MW:451.5 g/mol | Chemical Reagent | Bench Chemicals |
Stretchable active-matrix transistors represent a foundational technology for the next generation of bioelectronic implants, enabling complex logic circuits on substrates that mechanically match biological tissues. The development of semiconductor-elastomer composites, particularly vulcanized blends of DPPT-TT and BIIR, has demonstrated the feasibility of creating devices that maintain electrical functionality under significant mechanical deformation while exhibiting excellent biocompatibility. These advances address the critical challenge of mechanical mismatch that has plagued traditional rigid implants, potentially enabling new paradigms in chronic bioelectronic interfaces.
Looking forward, several emerging research directions promise to further advance the field. The development of stretchable synaptic transistors that mimic the function and structure of biological synapses could enable neuromorphic computing directly at the tissue interface, potentially facilitating more natural communication with neural systems [46]. Similarly, the integration of AMOLED technology with biostimulatory devices opens possibilities for optoelectronic interfaces that combine electrical recording and optical stimulation in compact, flexible formats [47]. As these technologies mature, we anticipate a convergence of sensing, processing, and actuation capabilities in truly intelligent bioelectronic systems that autonomously adapt to physiological states.
Despite significant progress, challenges remain in scaling up production, ensuring long-term stability in physiological environments, and further improving the density and complexity of integrable circuits. Addressing these challenges will require continued multidisciplinary collaboration across materials science, electrical engineering, and biology. The successful development of these technologies holds tremendous potential to transform healthcare through advanced diagnostic capabilities, closed-loop therapeutic interventions, and ultimately, seamless integration of electronic systems with the human body.
Closed-loop therapeutic systems represent a paradigm shift in medical treatment, transitioning from static, pre-programmed interventions to dynamic, adaptive therapies that respond in real-time to a patient's physiological state. These sophisticated systems autonomously monitor specific physiological biomarkers or signals via integrated biosensors, process this information, and subsequently trigger a therapeutic action—such as drug release or electrical stimulation—to maintain optimal health outcomes [48]. This self-regulating approach is particularly transformative for managing chronic conditions like diabetes, neurological disorders, and cardiovascular diseases, where maintaining physiological parameters within a narrow therapeutic window is crucial for long-term health [48]. The core innovation lies in the seamless integration of biosensing mechanisms, data processing units, and therapeutic actuators into a single, autonomous system capable of achieving therapeutic outcomes previously unattainable with conventional treatments.
The operational foundation of these systems is built upon continuous, real-time data acquisition. Unlike traditional monitoring that provides intermittent snapshots, closed-loop systems offer a constant stream of physiological data, enabling immediate detection of aberrant states (e.g., a hypoglycemic event or an oncoming seizure) and preemptive therapeutic intervention [48]. This capability enhances the patient-specificity of medical interventions, an essential aspect of personalized healthcare, and reduces the burden on patients and healthcare providers. The integration of these systems is largely driven by advancements in organic bioelectronics, which provide the material basis for creating devices that are mechanically and biologically compatible with human tissues [3]. By embedding biosensors into advanced systems, closed-loop devices can achieve dynamic, patient-centered solutions that continuously adapt to the individual's physiological state, revolutionizing disease management and treatment personalization [48].
The Foundation: Biocompatibility in Organic Bioelectronics
The successful implementation of implantable closed-loop systems hinges on the principle of biocompatibility—the ability of electronic materials to interact with biological systems without causing harm, irritation, or inflammatory responses [3]. Traditional implantable electronics, based on rigid inorganic materials like silicon and metals, exhibit a significant mechanical mismatch with soft, dynamic biological tissues. This mismatch often leads to micro-injuries, chronic inflammation, fibrosis, and ultimately, device failure [8]. Organic bioelectronics addresses this critical challenge by utilizing carbon-based semiconducting materials that offer inherent flexibility, softness, and compatibility with biological environments.
A key property of these organic materials is their mechanical compatibility. As illustrated in Table 1, the Young's modulus of organic materials can be engineered to closely match that of various biological tissues, enabling the creation of interfaces that minimize foreign body response and ensure long-term signal integrity [3].
Table 1: Mechanical Properties of Biological Tissues and Electronic Materials
| Material or Tissue Type | Young's Modulus (Approximate) | Implication for Biointegration |
|---|---|---|
| Brain, Heart, Peripheral Nerves | ~1 kPa | Requires very soft, compliant interfaces |
| Hydrogels & Soft Elastomers | 1 kPa - 1 MPa | Ideal for interfacing with excitable tissues |
| Conducting Polymers (e.g., PEDOT:PSS) | 1 MPa - 1 GPa | Suitable for a range of soft tissues |
| Conventional Elastomers (e.g., PDMS, PU) | 1 MPa - 1 GPa | Commonly used, but can be optimized for better compatibility |
| Silicon, Gold, Polyimide | ~100 GPa - 1 TPa | Significant mechanical mismatch, causes inflammation |
Beyond flexibility, organic semiconductors often function as mixed conductors, capable of transporting both electronic and ionic charges [3]. This dual capability is fundamental for seamless communication with biological systems, where signaling occurs primarily through ion flows. A relevant example is a recently developed elastomeric organic field-effect transistor designed for implantable electronics [8]. This device uses a blend of a semiconducting polymer (DPPT-TT) and a medical-grade, biocompatible elastomer (bromo isobutyl–isoprene rubber, BIIR) to create a composite film with a Young's modulus similar to human tissues. The film maintains stable electrical performance under 50% strain and demonstrates high biocompatibility, with in vitro assessments showing no adverse effects on human dermal fibroblasts and macrophages, and in vivo studies in mice showing no major inflammatory response or tissue damage [8]. This exemplifies the progress towards creating truly compatible implantable electronic circuits.
Biosensing Mechanisms for Physiological Monitoring
The sensor is the "input" module of a closed-loop system, responsible for accurately detecting and quantifying relevant physiological parameters. Biosensing strategies can be broadly categorized into chemical, physical, and electrophysiological sensing, each with distinct mechanisms and applications [48].
Table 2: Biosensing Strategies in Closed-Loop Systems
| Sensor Type | Core Mechanism | Key Characteristics | Application in Closed-Loop Systems |
|---|---|---|---|
| Chemical Sensors | Redox-based, impedance-based, transistor-based | Detect biomarkers and metabolic parameters; high specificity and sensitivity | Real-time monitoring of biomarkers (e.g., glucose, lactate) for adaptive drug delivery |
| Physical Sensors | Capacitive, piezoelectric, thermal resistive | Measure pressure, temperature; high sensitivity, flexibility, rapid response | Monitoring vital signs such as blood pressure, intraocular pressure, and body temperature |
| Electrophysiological Sensors | Invasive and surface electrodes | Capture bioelectrical activities from brain, heart, muscles; require high signal-to-noise ratio | Monitoring neural activities for seizure detection, managing heart rhythms, providing sensory feedback |
Chemical Sensing
Chemical sensing focuses on the detection of specific biomarkers in biofluids. Redox-based biosensors are a prominent example, often relying on enzymes for specificity. For instance, an amperometric glucose sensor uses the enzyme glucose oxidase (GOx) immobilized on a working electrode. GOx catalyzes the oxidation of glucose to gluconic acid, generating hydrogen peroxide, which is then electrochemically oxidized to produce a current proportional to glucose concentration [48]. This precise, continuous quantification is the cornerstone of closed-loop glycemic control systems, often called an "artificial pancreas." Similar principles apply to lactate sensors using lactate oxidase (LOx) for monitoring metabolic stress [48]. Recent innovations include wearable sensor arrays that can simultaneously quantify multiple metabolites (e.g., glucose, lactate), electrolytes (e.g., Na+, K+), and skin temperature, providing a comprehensive metabolic picture [48].
Physical and Electrophysiological Sensing
Physical sensors provide critical information on physiological conditions. Pressure sensors can monitor intraocular pressure for glaucoma or intracranial pressure following trauma, while temperature sensors can track core body temperature or local inflammation [48]. Electrophysiological sensors are vital for neural and cardiac applications. Surface electrodes in wearable patches can capture electrocardiogram (ECG) or electromyogram (EMG) signals, while invasive, high-density electrode arrays can record neural activity with high spatial and temporal resolution from the brain or peripheral nerves [48]. These signals can be used to detect the onset of arrhythmias or epileptic seizures, triggering immediate therapeutic intervention.
Therapeutic Intervention: Drug Delivery and Electrical Stimulation
The "output" modules of closed-loop systems are the therapeutic actuators that deliver treatment based on sensor input. The two primary modalities are drug delivery and electrical stimulation.
Drug Delivery Systems
Smart drug delivery systems use biosensor data to control the release of therapeutic agents in real-time. A canonical example is the glucose-responsive insulin delivery system. These systems often use microneedle patches containing insulin reservoirs and a glucose-sensing mechanism [48]. Upon detecting elevated glucose levels, the material properties of the system change (e.g., a hydrogel swells or a membrane degrades), leading to the controlled release of insulin. This mimics the natural glucose regulation of a healthy pancreas and significantly improves glycemic control compared to manual insulin injections [48]. Similar principles are being applied to neurological conditions, where implantable devices can release anticonvulsant medication upon detecting specific bioelectrical signals indicative of a seizure, providing immediate intervention [48].
Electrical Stimulation Devices
Electrical stimulation applies controlled electrical currents to tissues to modulate their activity. When enhanced by biosensing, these devices offer targeted therapeutic effects. For example, in a closed-loop neuromodulation system for Parkinson's disease, sensors monitor neural signals for tremors or dyskinesias. When abnormal activity is detected, the system delivers precisely timed electrical pulses to specific brain regions (e.g., the subthalamic nucleus) to suppress symptoms [48]. Another innovative application is the self-powered electronic bandage, which accelerates wound healing. Such a device might monitor biomarkers of inflammation or infection at the wound site and, in response, deliver mild electrical stimulation to promote blood flow and tissue regeneration [48].
Integration and Experimental Workflow in Closed-Loop Systems
The creation of a functional closed-loop system requires the meticulous integration of sensing and therapeutic components, often within a single, miniaturized device. The experimental workflow involves material synthesis, device fabrication, in vitro and in vivo testing, and system validation.
The following diagram illustrates the core logical workflow of a generic closed-loop therapeutic system:
For researchers, a critical step is the fabrication of biocompatible, stretchable electronic components. The protocol below details the creation of a vulcanized semiconducting blend film, a key material for implantable transistors [8].
Experimental Protocol: Fabrication of a Vulcanized Biocompatible Semiconducting Film [8]
- Objective: To create a highly stretchable and biocompatible semiconducting composite film for use in implantable organic field-effect transistors (sOFETs).
- Materials:
- Semiconducting Polymer: Poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] (DPPT-TT).
- Elastomer Matrix: Bromo isobutyl–isoprene rubber (BIIR), a medical-grade biocompatible elastomer.
- Vulcanization Additives: Sulfur (crosslinker), dipentamethylenethiuram tetrasulfide (DPTT, accelerator), and stearic acid (initiator).
- Solvent: A suitable organic solvent like chlorobenzene or toluene.
- Procedure:
- Solution Preparation: Prepare separate solutions of DPPT-TT and BIIR in the solvent. Blend them at an optimized weight ratio of 3:7 (DPPT-TT:BIIR) to achieve a balance between electrical performance and mechanical stretchability.
- Additive Mixing: Add the vulcanization additives (sulfur, DPTT, stearic acid) to the blended polymer solution and mix thoroughly.
- Film Casting: Deposit the final mixture onto a clean substrate (e.g., glass or plastic) via spin-coating or blade-coating to form a thin, uniform wet film.
- Vulcanization: Thermally anneal the film at an elevated temperature (e.g., 100-150°C) for a specified time. This heat treatment initiates the vulcanization process, which:
- Crosslinks the BIIR chains via radical formation (evidenced by reduction of C-Br FTIR peak at 667 cmâ»Â¹) and propagation (reduction of C=C peak in neat BIIR).
- Preserves the conjugated structure of DPPT-TT (confirmed by unchanged UV-Vis absorption spectra).
- Enhances the film's elasticity and mechanical durability (confirmed by increased Derjaguin-Muller-Toporov modulus).
- Validation:
- Mechanical Testing: The resulting film should sustain up to 100% strain without mechanical cracking and maintain stable electrical performance after 1,000 stretching cycles at 100% strain.
- Electrical Characterization: Transistors made with the vulcanized film should exhibit higher field-effect mobility and ON/OFF ratio compared to non-vulcanized blends.
- Biocompatibility Assessment: Perform in vitro cell viability, proliferation, and migration assays with human dermal fibroblasts and macrophages. Conduct in vivo implantation studies in animal models (e.g., mice) to confirm the absence of a major inflammatory response or tissue damage.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Organic Bioelectronics
| Material/Reagent | Function/Description | Application in Research |
|---|---|---|
| Conductive Polymers (e.g., PEDOT:PSS) | Mixed ionic-electronic conductor; high biocompatibility and flexibility. | Used for electrodes, channels in transistors, and neural interfaces to improve signal fidelity [3]. |
| Medical-Grade Elastomers (e.g., BIIR) | Biocompatible rubber matrix; provides mechanical stretchability and shock absorption. | Serves as the elastic host for semiconducting nanofibers to create stretchable, implantable electronics [8]. |
| DPPT-TT Semiconducting Polymer | Donor-acceptor polymer; forms semiconducting nanofibers within an elastomer matrix. | The active material in stretchable organic field-effect transistors (sOFETs) for signal processing [8]. |
| Enzymes (e.g., Glucose Oxidase, Lactate Oxidase) | Biological recognition element; provides high specificity to target analytes. | Immobilized on electrodes in amperometric sensors for continuous biomarker monitoring (e.g., in closed-loop diabetes management) [48]. |
| Vulcanization Additives (Sulfur, DPTT, Stearic Acid) | Chemical crosslinkers; form covalent bonds between polymer chains. | Used to enhance the mechanical properties, elasticity, and durability of elastomeric semiconductors [8]. |
| Dual-Layer Metallization (Ag/Au) | Provides conductive, stretchable, and corrosion-resistant electrodes. | Ag ensures excellent electrical contact, while a top layer of Au provides robust protection against biofluid corrosion [8]. |
| Dphpc | Dphpc, MF:C48H96NO8P, MW:846.3 g/mol | Chemical Reagent |
| ZK824859 | ZK824859, MF:C23H22F2N2O4, MW:428.4 g/mol | Chemical Reagent |
Closed-loop therapeutic systems, underpinned by the advances in organic bioelectronics, are poised to redefine personalized medicine. By seamlessly integrating biosensing with real-time therapeutic intervention, these systems offer a dynamic and adaptive approach to managing complex chronic diseases. The ongoing research focused on enhancing biocompatibility, ensuring long-term stability in vivo, and developing more sophisticated sensing and actuation technologies will continue to push the boundaries of what is possible. As these technologies mature, they hold the immense potential to transform patient care from a reactive to a proactive, continuous, and highly personalized paradigm.
Overcoming Biocompatibility Challenges: Ensuring Long-Term Reliability and Stability
Addressing Chronic Foreign Body Response and Fibrotic Encapsulation
The integration of organic bioelectronic devices with biological systems presents a formidable challenge: the chronic foreign body response (FBR) and subsequent fibrotic encapsulation. This universal host reaction to implanted biomaterials remains a significant barrier to the long-term performance and biocompatibility of medical devices, including neural interfaces, biosensors, and drug delivery systems [49]. The FBR is a complex, multi-stage immunological process that begins immediately upon implantation and culminates in the formation of a dense, collagenous fibrous capsule that isolates the device from surrounding tissue [50] [51]. This fibrotic encapsulation disrupts critical device-tissue communication, impedes analyte diffusion for sensors, reduces electrical signal fidelity in electrodes, and compromises drug release kinetics from delivery systems [49] [52]. Within the context of organic bioelectronics biocompatibility research, understanding and mitigating the FBR is paramount for developing next-generation implants that maintain stable, functional interfaces with host tissues over clinical timescales. This whitepaper provides a comprehensive technical analysis of FBR mechanisms, current intervention strategies, and advanced methodological approaches to address this persistent challenge in implantable medical devices.
Molecular and Cellular Mechanisms of FBR
The foreign body response unfolds through a highly orchestrated sequence of cellular events mediated by distinct molecular signaling pathways. Understanding these mechanisms is fundamental to developing effective anti-fibrotic strategies for organic bioelectronic interfaces.
Progressive Stages of Foreign Body Response
Protein Adsorption: Within seconds of implantation, blood plasma proteins (primarily albumin, fibrinogen, fibronectin, and vitronectin) spontaneously adsorb to the biomaterial surface, forming a provisional matrix [50] [51]. This protein layer establishes a "molecular fingerprint" that dictates subsequent cellular interactions [53]. The dynamic exchange of proteins at the surface, known as the Vroman effect, further modulates the inflammatory response [50].
Acute Inflammation: The injury from surgical implantation triggers neutrophil infiltration within minutes to hours [54]. These polymorphonuclear leukocytes (PMNs) attempt to phagocytose the foreign material and secrete pro-inflammatory mediators, including cysteinyl leukotrienes (CysLTs) that regulate their own recruitment and survival while stimulating fibroblast migration [51]. This acute phase typically resolves within one week in the absence of a persistent foreign body [50].
Chronic Inflammation and Macrophage Activation: If the implant remains, acute inflammation transitions to chronic inflammation characterized by monocyte infiltration and differentiation into macrophages [50] [51]. These macrophages attempt to engulf the device through "frustrated phagocytosis," releasing reactive oxygen species (ROS) and matrix metalloproteinases (MMPs) in an attempt to degrade the material [49] [54]. Macrophages exhibit phenotypic plasticity, with pro-inflammatory M1 subtypes dominating initially and later shifting toward pro-fibrotic M2 phenotypes that upregulate tissue remodeling pathways [49] [53].
Foreign Body Giant Cell Formation: The inability to eliminate large implants leads macrophages to fuse into multinucleated foreign body giant cells (FBGCs) [50] [51]. These persistent cells continue to secrete inflammatory cytokines and degradative enzymes, contributing to the chronic inflammatory state and potential device degradation [49].
Fibrous Encapsulation: The culmination of FBR is the formation of a dense, avascular collagenous capsule that isolates the implant from surrounding tissue [51]. This process is driven by fibroblast recruitment and differentiation into α-smooth muscle actin (α-SMA)-expressing myofibroblasts, which deposit excessive extracellular matrix (ECM) components, primarily collagen types I and III [55] [51]. The resulting fibrous capsule can impede device function by creating a diffusion barrier and physically separating the implant from its target tissue [49].
Key Signaling Pathways in Fibrosis
The following diagram illustrates the primary molecular pathways driving fibrotic encapsulation:
The molecular signaling network driving fibrosis centers on several key pathways. Transforming growth factor-beta (TGF-β) serves as a master regulator, activating both Smad-dependent and Smad-independent pathways (including Rho/ROCK) that drive fibroblast-to-myofibroblast differentiation and collagen production [51]. Interleukins IL-4 and IL-13 promote macrophage fusion into FBGCs and stimulate alternative macrophage activation [50]. Recently, S100A8/A9 alarmins have been identified as critical mediators, with inhibition or knockout experiments demonstrating substantial attenuation of fibrosis in murine models [56]. The equilibrium between matrix metalloproteinases (MMPs) and their inhibitors (TIMPs) ultimately determines collagen deposition and extracellular matrix composition [51].
Quantitative Analysis of FBR and Intervention Efficacy
Fibrous Capsule Thickness Across Biomaterials
Table 1: Comparative analysis of fibrous capsule thickness following subcutaneous implantation in rodent models
| Material/Intervention | Implantation Duration | Capsule Thickness (μm) | Reference Model |
|---|---|---|---|
| EVADE Elastomer (H90) | 1 month | 10-40 | [56] |
| Polydimethylsiloxane (PDMS) | 1 month | 45-135 | [56] |
| Thermoplastic Polyurethane (TPU) | 1 month | 35-160 | [56] |
| pHEMA (34μm porosity) | 3 weeks | Significant reduction vs. non-porous | [49] |
| Polycrystalline Diamond Ti | 4 weeks | Similar to uncoated Ti | [49] |
| Electrospun PTFE | Not specified | Reduced vs. flat/expanded PTFE | [49] |
The data demonstrate that material composition significantly influences the extent of fibrotic encapsulation. EVADE elastomers (particularly H90 formulation) exhibit superior performance with capsule thickness approximately 3-4 times lower than conventional PDMS [56]. Surface topography also plays a crucial role, with optimized porosity (34μm in pHEMA) and nanoscale features (electrospun PTFE) reducing capsule formation compared to smooth surfaces [49].
Anti-Fibrotic Coating Strategies and Efficacy
Table 2: Experimentally validated anti-fibrotic coating approaches and their outcomes
| Coating Strategy | Mechanism of Action | Experimental Model | Key Efficacy Findings | |
|---|---|---|---|---|
| THPT-derived Coating | Anti-FBR surface modification | PDMS devices, silicone prosthesis | Reduced capsule formation | [56] |
| Zwitterionic Polymer | Anti-fouling, reduces protein adsorption | Various implant surfaces | Decreased macrophage adhesion | [49] |
| Drug-eluting (Dexamethasone) | Localized anti-inflammatory delivery | Neural interfaces, biosensors | Transient suppression of inflammation | [49] |
| Bioadhesive Interfaces | Prevents micromotion, reduces immune cell infiltration | Peripheral nerve bioelectronics | Minimal fibrosis at 12 weeks | [57] |
| Acellular Dermal Matrix | Provides natural ECM scaffold, modulates immune response | Silicone breast implants | Reduced capsular contracture | [51] |
Anti-fibrotic coatings represent a promising approach to mitigate FBR, with mechanisms ranging from preventing initial protein adsorption to modulating downstream immune activation. The bioadhesive strategy inspired by traditional acupuncture demonstrates particularly impressive results, maintaining minimal fibrosis on peripheral nerves for up to 12 weeks with continuous stimulation [57].
Experimental Methodologies for FBR Characterization
In Vivo Implantation and Histological Analysis
Animal Models and Surgical Implantation:
- Utilize C57BL/6 mice or Sprague-Dawley rats (8-12 weeks old) for subcutaneous implantation studies [56]
- Implant material discs (typically 5-10mm diameter, 0.5-1mm thickness) in dorsal subcutaneous pockets under isofluorane anesthesia [56]
- Include positive controls (PDMS, TPU) and negative controls (sham surgery) for comparative analysis
- For non-human primate studies, cynomolgus monkeys provide translational models that closely mimic human FBR [56]
Histological Processing and Staining:
- Explant implants with surrounding tissue at predetermined endpoints (e.g., 2 weeks, 1 month, 3 months, 1 year) [56]
- Fix tissue in 4% paraformaldehyde, embed in paraffin, and section at 5μm thickness
- Employ Masson's trichrome staining for collagen visualization and fibrous capsule thickness measurement [56]
- Use hematoxylin and eosin (H&E) staining for general tissue architecture and cellular infiltration assessment [56]
- Perform immunohistochemistry for inflammatory markers (CCR-7, TNF-α, IL-6) and anti-inflammatory markers (IL-10) [56]
Capsule Thickness Quantification:
- Measure capsule thickness at multiple random locations around the implant circumference using image analysis software (e.g., ImageJ)
- Report mean thickness ± standard deviation with statistical analysis (typically one-way ANOVA with post-hoc testing) [56]
Proteomic Analysis of FBR Molecular Signatures
The following workflow illustrates the comprehensive proteomic approach for characterizing the foreign body response:
Sample Collection Protocol:
- Collect wound bed fluid from implant sites during the first 5 days post-implantation using sterile techniques [55]
- Harvest implant-adhered proteome after 6-8 months of implantation through surface stripping [55]
- Obtain simultaneous plasma samples as reference for differential protein expression analysis [55]
Quantitative Proteomic Profiling:
- Apply TMT (Tandem Mass Tag) liquid chromatography-tandem mass spectrometry (LC-MS/MS) for relative protein quantitation in acute wound fluid [55]
- Utilize label-free LC-MS/MS approaches for characterizing long-term implant-adhered proteomes [55]
- Identify differentially expressed proteins (DEPs) through statistical analysis of spectral counts [55]
Functional Bioinformatics Analysis:
- Perform functional enrichment analysis of DEPs using databases such as Gene Ontology (GO) and KEGG pathways [55]
- Identify dysregulated signaling pathways, particularly those involved in immediate inflammatory response and ECM turnover [55]
- Develop biomarker panels for early detection of excessive fibrosis based on consistently upregulated proteins in progressive FBR [55]
In Vitro Macrophage Response Assays
Macrophage Culture and Polarization:
- Utilize human THP-1 monocyte cell line or primary human monocyte-derived macrophages
- Differentiate monocytes into macrophages using phorbol 12-myristate 13-acetate (PMA) or macrophage colony-stimulating factor (M-CSF)
- Polarize macrophages toward M1 phenotype with LPS and IFN-γ, or toward M2 phenotype with IL-4 and IL-13 [49]
Material-Macrophage Interaction Studies:
- Culture macrophages on material surfaces with different topographies, stiffness, and chemical compositions
- Assess macrophage adhesion and spreading through fluorescence microscopy (F-actin staining)
- Quantify FBGC formation by counting multinucleated cells (>3 nuclei) after 5-7 days of culture
- Analyze cytokine secretion profiles using ELISA or multiplex assays (TNF-α, IL-1β, IL-6, IL-10 for M1/M2 balance) [49]
Research Reagent Solutions for FBR Studies
Table 3: Essential research reagents and materials for investigating foreign body response
| Reagent/Material Category | Specific Examples | Research Application | Key Function | |
|---|---|---|---|---|
| Polymer Elastomers | PDMS, TPU, EVADE (HPEMA/ODA copolymers) | Implant substrate studies | Material-tissue interaction analysis | [56] |
| Surface Modification Reagents | Zwitterionic monomers, THPT derivatives, methacryloyloxyethyl phosphorylcholine (MPC) | Anti-fouling surface development | Reduce protein adsorption and macrophage adhesion | [49] [56] |
| Pharmacological Inhibitors | Tranilast, Triamcinolone acetonide (TA), S100A8/A9 inhibitors | Anti-fibrotic drug screening | Target specific pathways in fibrosis development | [51] [56] |
| Proteomic Analysis Kits | TMT labeling kits, Protein extraction buffers | Molecular signature characterization | Quantitative analysis of protein expression in FBR | [55] |
| Immunohistochemistry Antibodies | Anti-CCR7, Anti-TNF-α, Anti-IL-6, Anti-α-SMA | Inflammatory and fibrotic marker detection | Identify specific cell types and activation states in tissue | [56] |
| Cell Culture Assays THP-1 cell line, M-CSF, Polarizing cytokines (IL-4, IL-13, LPS, IFN-γ) | In vitro macrophage response studies | Standardized assessment of material immunocompatibility | [49] |
The research reagents outlined in Table 3 represent essential tools for investigating FBR mechanisms and developing intervention strategies. EVADE elastomers (HPEMA/ODA copolymers) have emerged as particularly promising materials, demonstrating negligible inflammation and minimal capsule formation in both rodent and non-human primate models for extended periods up to one year [56]. The identification of S100A8/A9 as a key regulatory target in fibrosis provides new opportunities for specific pharmacological intervention [56].
The chronic foreign body response and subsequent fibrotic encapsulation present formidable challenges to the long-term success of organic bioelectronic devices. Through comprehensive understanding of the cellular and molecular mechanisms driving FBR—from initial protein adsorption to mature collagenous capsule formation—researchers can develop targeted strategies to mitigate this response. Current approaches including advanced material engineering (EVADE elastomers), surface topography optimization, bioadhesive interfaces, and localized pharmacological delivery show significant promise in reducing fibrous encapsulation. The integration of sophisticated characterization methodologies, particularly quantitative proteomics and standardized in vivo implantation models, provides robust frameworks for evaluating novel anti-fibrotic strategies. As organic bioelectronics continue to evolve toward more sophisticated and minimally invasive interfaces, overcoming the biological challenge of FBR will be essential for achieving seamless integration between electronic and biological systems. The experimental tools and analytical approaches detailed in this technical guide provide a foundation for advancing this critical frontier in biocompatibility research.
The integration of electronic devices with biological systems represents a frontier in medical science, enabling advanced therapies and monitoring capabilities. However, the physiological environment presents a significant challenge to the long-term stability of implanted electronics. Biofluids constitute a corrosive electrolyte rich in ions such as Na+, K+, and Cl-, which can initiate multiple degradation pathways in electronic materials, including electrochemical corrosion, ion penetration, and delamination. These processes compromise device functionality and biocompatibility, potentially leading to device failure and inflammatory tissue responses. This technical guide examines two cornerstone strategies for achieving biofluid corrosion resistance—dual-layer metallization and encapsulation—within the broader context of enhancing the biocompatibility and chronic stability of organic bioelectronic implants. By exploring material selections, protection mechanisms, and experimental validation protocols, this review provides a framework for developing next-generation bioelectronic devices capable of reliable long-term operation in physiological environments.
Dual-Layer Metallization for Corrosion-Resistant Electrodes
Principle and Material Selection
Dual-layer metallization is an advanced strategy for creating robust, stretchable, and biofluid-corrosion-resistant electrodes, which are critical components of implantable organic field-effect transistors (OFETs). This approach leverages the synergistic properties of two distinct metals to overcome the limitations of single-material electrodes. The underlying principle involves combining an inner layer selected for its superior electrical and mechanical contact properties with an outer layer chosen for its high chemical inertness and resistance to biofluid corrosion. This configuration ensures that the electrode maintains high conductivity and stable interfacial contact with the semiconductor while being effectively shielded from the aggressive ionic environment of the body.
Recent research has demonstrated the effectiveness of a dual-layer architecture using silver (Ag) as the inner contact layer and gold (Au) as the outer protective layer [8]. Silver provides excellent electrical conductivity and forms a favorable electrical contact with the organic semiconductor channel. However, silver is susceptible to corrosion and sulfide formation in biological environments. Gold, while less conductive than silver, is highly inert and resistant to corrosion and oxidation, making it an ideal barrier material. The outer gold layer thus acts as a dense, impermeable shield, preventing biofluids from reaching the underlying silver and ensuring the long-term integrity of the conductive path [8].
Table 1: Key Properties of Metals in Dual-Layer Metallization
| Metal | Role in Stack | Key Advantages | Potential Limitations |
|---|---|---|---|
| Silver (Ag) | Inner Layer | High electrical conductivity, excellent contact properties with organic semiconductors | Susceptible to corrosion and sulfide tarnishing in biofluids |
| Gold (Au) | Outer Layer | High biofluid corrosion resistance, chemical inertness, biocompatibility | Higher material cost, lower conductivity than Ag |
Experimental Protocol and Validation
Fabrication Methodology: The fabrication of dual-layer Ag/Au electrodes typically involves sequential deposition processes such as thermal evaporation or sputtering through a shadow mask to define the electrode pattern. The silver layer is deposited first onto the substrate, directly interfacing with the organic semiconductor, followed by the deposition of the gold layer. Precise control over the thickness of each layer is critical; the gold layer must be sufficiently thick and continuous to form a pinhole-free barrier, yet the overall stack must remain compliant for use in stretchable devices [8].
Performance Characterization: The efficacy of the dual-layer metallization is validated through a combination of electrical, electrochemical, and material tests.
- Electrical Performance: The field-effect mobility and ON/OFF ratio of transistors incorporating the dual-layer electrodes are measured and compared to devices with single-layer electrodes. Stability is assessed by monitoring these parameters during continuous operation in a physiological saline solution or simulated body fluid (SBF).
- Corrosion Resistance: Electrochemical impedance spectroscopy (EIS) and cyclic voltammetry (CV) are used to evaluate the corrosion resistance of the electrodes. A higher charge-transfer resistance and a lower corrosion current density, as derived from Tafel plot analysis, indicate superior barrier performance.
- Material Analysis: X-ray photoelectron spectroscopy (XPS) depth profiling is employed to confirm the uniform distribution of elements and the integrity of the interface between the Ag and Au layers after prolonged exposure to biofluids. This technique verifies that the gold layer successfully prevents the diffusion of corrosive ions to the silver layer [8].
Figure 1: Experimental workflow for developing and validating dual-layer metallization for biofluid corrosion resistance.
Encapsulation Strategies for Hermeticity and Biocompatibility
Material Systems and Protection Mechanisms
While dual-layer metallization protects the electrodes, a comprehensive strategy requires the protection of the entire integrated circuit (IC). Encapsulation involves applying a continuous, protective coating that acts as a barrier against moisture and ions. The ideal encapsulant must combine excellent barrier properties with biocompatibility and mechanical compliance to minimize the foreign body response.
Medical-Grade Elastomers: Bromo isobutyl–isoprene rubber (BIIR), a medical-grade elastomer, has been successfully integrated into the semiconductor layer itself to create intrinsically biocompatible and stretchable OFETs [8]. BIIR meets stringent ISO 10993 biocompatibility standards and, when vulcanized and blended with a semiconductor polymer like DPPT-TT, forms a composite film that is both electrically functional and mechanically compatible with human tissue (Young's modulus of ~10^8 Pa) [8].
Silicone Elastomers: Polydimethylsiloxane (PDMS) is another widely used encapsulant due to its proven long-term biocompatibility, biostability, and low Young's modulus [58]. A critical insight from recent studies is that PDMS itself is permeable to water vapor. Its protective mechanism is not to provide a hermetic moisture barrier but to create a benign environment where the encapsulated IC operates at 100% relative humidity, shielded from direct contact with ionic liquids and organic species present in biofluids [58]. This protection relies on the inherent hermeticity of the IC's native passivation layers (e.g., SiNX/SiOX). For this approach to succeed, strong interfacial adhesion between the PDMS and the IC is essential to prevent the formation of leakage paths, particularly at wire-bond sites [58].
Advanced Coatings: Beyond bulk encapsulation, superhydrophobic (SHB) coatings are being developed to create biofluid-repellent surfaces. For instance, a nanograss alumina coating functionalized with a fluorinated silane can be applied conformally to the inner surfaces of glass capillaries, making them highly repellent to proteins and blood [59]. This "lotus effect" minimizes the contact area between the biofluid and the solid surface, thereby reducing hydraulic resistance, protein adsorption, and subsequent biofilm formation [59].
Table 2: Comparison of Encapsulation and Coating Materials
| Material | Protection Mechanism | Key Advantages | Validated Performance |
|---|---|---|---|
| BIIR Elastomer | Intrinsic biocompatibility; Integration into active layer | ISO 10993 certified; Similar Young's modulus to tissue | No adverse effects on cell viability; No major inflammatory response in vivo [8] |
| PDMS | Shields IC from direct ionic contact; Relies on IC's inherent hermeticity | Proven biocompatibility; Low Young's modulus; Easy processing | Limited IC degradation after 12 months in vivo vs. bare-die [58] |
| SHB Nanograss Alumina | Air plastron minimizes solid-liquid contact; Biofluid repellence | Reduces protein adsorption and hydraulic resistance | 83% reduction in blood adhesion; 0-50% reduction in hydraulic resistance for protein solutions [59] |
Experimental Protocol for Long-Term Validation
Accelerated Aging Studies: To predict long-term stability, encapsulated ICs are subjected to accelerated in vitro aging. A standard protocol involves submerging devices in phosphate-buffered saline (PBS) at an elevated temperature (e.g., 67°C) while under electrical bias (e.g., up to 15V) [58]. The devices are periodically monitored for changes in electrical performance, such as shifts in threshold voltage, mobility, or the onset of leakage currents.
In Vivo Implantation Studies: Long-term biocompatibility and stability are ultimately validated through in vivo models. Devices are implanted in animal models (e.g., rats or mice) for extended periods (e.g., one year) [8] [58]. Post-explantation analysis includes:
- Electrical Testing: Final electrical performance is measured and compared to pre-implantation baselines.
- Material Analysis: Techniques like time-of-flight secondary ion mass spectrometry (ToF-SIMS) are used at the nanometer scale to identify ion ingress (e.g., Na+, K+) and material degradation in the IC's passivation layers.
- Histological Evaluation: The implant site is examined for inflammatory responses, fibrosis, and tissue damage to confirm biocompatibility [8].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Biofluid-Resistant Bioelectronics
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| DPPT-TT Semiconductor | Provides p-type semiconducting channel | Blended with BIIR elastomer for stretchable OFETs [8] |
| BIIR Elastomer | Biocompatible matrix for semiconductor blend | Creates soft, tissue-like electronic film [8] |
| Ag/Au Evaporation Targets | Forms conductive, corrosion-resistant electrodes | Dual-layer metallization for stretchable interconnects [8] |
| Medical-Grade PDMS | Soft encapsulant for integrated circuits | Protects ICs from direct biofluid contact in chronic implants [58] |
| TPFS Silane | Low-surface-energy coating agent | Functionalizes nanograss alumina for superhydrophobic tubes [59] |
| Simulated Body Fluid (SBF) | In vitro corrosion testing medium | Accelerated aging studies of materials and devices [60] |
| (Rac)-RK-682 | (Rac)-RK-682, MF:C21H36O5, MW:368.5 g/mol | Chemical Reagent |
Figure 2: Logical framework of corrosion resistance strategies for organic bioelectronics.
The seamless integration of bioelectronic devices with living tissues is paramount for advancing personalized medicine and regenerative therapies. The strategies of dual-layer metallization and advanced encapsulation, as detailed in this guide, provide a robust technical foundation for overcoming the significant challenge of biofluid-induced corrosion. The dual-layer Ag/Au approach ensures that conductive elements remain electrochemically stable, while encapsulation with materials like BIIR and PDMS protects the entire device architecture. The experimental protocols and material toolkit outlined herein offer researchers a clear pathway for validating new materials and protection strategies. As the field progresses, the synergy between intrinsically stable materials, innovative barrier designs, and bio-repellent surfaces will undoubtedly yield a new generation of chronic bioelectronic implants with enhanced reliability and biocompatibility, ultimately closing the loop between diagnostic sensing and therapeutic intervention.
The advancement of organic bioelectronics promises a new era of medical implants and diagnostic tools that can seamlessly integrate with biological systems for continuous health monitoring and therapy. A core thesis in this field posits that true biocompatibility extends beyond biological inertness; it requires a holistic integration at the mechanical, chemical, and physical levels to ensure long-term device functionality and tissue safety. A significant obstacle to this goal is device failure stemming from the harsh physiological environment. Mechanical fatigue from constant bodily movements, delamination at material interfaces due to thermal and hygroscopic stresses, and water permeation leading to corrosion and swelling collectively threaten the operational lifetime of implantable devices [8] [61]. This technical guide examines the fundamental mechanisms behind these failure modes and details the latest material strategies and experimental protocols designed to mitigate them, thereby supporting the development of robust and reliable bioelectronic systems.
Material Strategies for Enhanced Device Durability
The selection and engineering of materials are foundational to overcoming failure modes in bioelectronics. The following table summarizes key material solutions and their specific functions in mitigating device failure.
Table 1: Research Reagent Solutions for Mitigating Bioelectronic Device Failure
| Material/Strategy | Function in Mitigating Failure |
|---|---|
| DPPT-TT/BIIR Blend Film [8] | A semiconductor (DPPT-TT) and medical-grade elastomer (BIIR) blend that creates a stretchable composite with a Young's modulus similar to human tissue, mitigating mechanical mismatch. |
| Chemical Vulcanization [8] | A crosslinking process using sulfur-based compounds that enhances the elastic modulus and mechanical integrity of the elastomer matrix without disrupting the semiconductor. |
| Dual-Layer Ag/Au Metallization [8] | Provides highly conductive, stretchable, and biofluid-corrosion-resistant electrodes, where Ag ensures electrical contact and Au acts as a protective layer. |
| Block Copolymers & Self-Healing Polymers [61] | Emerging materials that can improve a device's moisture resistance and autonomously repair cracks and delamination damage, thereby extending service life. |
| RDL Structure Modification [61] | A structural redesign of the Redistribution Layer to improve the thermal stress state and moisture resistance at critical interfaces within a packaged device. |
Analyzing Primary Failure Mechanisms and Experimental Data
Understanding the quantitative impact of these strategies is crucial. The data from accelerated testing and in vivo studies provide a basis for evaluating their effectiveness.
Table 2: Quantitative Performance of Mitigation Strategies
| Failure Mechanism | Mitigation Strategy | Experimental Performance Data | Testing Conditions |
|---|---|---|---|
| Mechanical Fatigue | DPPT-TT/BIIR Blend Film [8] | Stable field-effect mobility under 50% strain; negligible change after 1,000 stretching cycles at 100% strain. | In vitro on rigid substrate. |
| Delamination (Thermal Stress) | RDL Structure Modification [61] | Significant improvement in the thermal stress state of encapsulated devices, reducing interfacial failure. | Finite Element Analysis (FEA) simulation. |
| Water Permeation | Dual-Layer Ag/Au Electrodes [8] | Robust performance and resistance to corrosion in biofluid environments. | In vitro physiological conditions. |
Mechanical Fatigue
The mechanical mismatch between rigid electronic components and soft tissue is a primary source of failure. Implantable devices are subjected to continuous deformation (e.g., from muscle movement or pulsatile blood flow), leading to mechanical fatigue. A promising solution is the development of intrinsically stretchable semiconductors. For instance, a vulcanized blend of the semiconducting polymer DPPT-TT and the medical-grade elastomer bromo isobutyl–isoprene rubber (BIIR) creates a composite film where a nanofibre network of the semiconductor is embedded within an elastic matrix [8]. This structure maintains electrical conductivity even under significant mechanical deformation. The vulcanization process, using additives like sulfur (crosslinker) and dipentamethylenethiuram tetrasulfide (accelerator), chemically crosslinks the BIIR chains, enhancing the film's elasticity and mechanical durability [8].
Delamination
Delamination is a low-cycle fatigue failure at the interfaces between different material layers, often triggered by thermal cycling and moisture absorption during device operation [61]. The differing coefficients of thermal expansion (CTE) of adjacent materials generate cyclic shear stresses at their interface, leading to crack initiation and propagation. Furthermore, moisture that has permeated into the device can vaporize at high temperatures (e.g., during operation), creating pressure that exacerbates delamination, a phenomenon known as the "popcorn" effect [61]. Mitigation strategies focus on improving interfacial adhesion and managing stress. Redesigning the Redistribution Layer (RDL) structure and incorporating functional fillers into polymer matrices can significantly improve the thermal stress state and moisture resistance of the package [61].
Water Permeation
Physiological environments are aqueous, making water permeation a critical failure mode. Water diffusion into organic materials can cause swelling, degradation of electrical insulation, and corrosion of metallic components. Polar water molecules can form hydrogen bonds with polymer chains, leading to the formation of "bound water" and "adsorbed water," which plasticizes the material and alters its mechanical and electrical properties [61]. To protect critical components, a dual-layer metallization of silver and gold can be employed for electrodes. Silver provides excellent electrical conductivity and contact, while a top layer of gold offers a robust, bio-inert barrier that resists corrosion in biofluids [8].
Experimental Protocols for Failure Analysis
To develop and validate mitigation strategies, standardized experimental protocols are essential.
Protocol: Evaluating Mechanical Durability of Stretchable Semiconductors
Objective: To determine the electromechanical stability of a stretchable semiconductor film under cyclic strain. Materials: Stretchable substrate (e.g., PDMS), semiconductor blend film (e.g., DPPT-TT/BIIR), source-meter unit, mechanical stretcher. Methodology:
- Fabricate organic field-effect transistors (OFETs) on the stretchable substrate.
- Mount the device on a calibrated mechanical stretcher.
- Apply uniaxial tensile strain (e.g., 0% to 50%) while monitoring key electrical parameters (field-effect mobility, ON/OFF current ratio).
- For fatigue testing, subject the device to a fixed number of stretching cycles (e.g., 1,000 cycles at 100% strain) and measure the mobility retention at regular intervals. Validation: Devices incorporating the vulcanized DPPT-TT/BIIR blend have demonstrated negligible changes in mobility after 1,000 stretching cycles, confirming excellent mechanical durability [8].
Protocol: Characterizing Moisture Diffusion using FEA
Objective: To model and analyze the moisture diffusion process within a polymer-based encapsulated device.
Materials: Finite Element Analysis (FEA) software (e.g., ANSYS, ABAQUS), material properties (saturated moisture concentration C_sat, diffusion coefficient D).
Methodology:
- Construct a detailed 3D model of the device geometry and material layers.
- Apply a normalized wet concentration
W(ratio of wet concentration to saturated wet concentration) to handle material discontinuity at interfaces [61]. - Input the governing diffusion equation, which may need to account for temperature dependence above the glass transition temperature (Tg):
C_sat(T) = C_sat,ref * exp( -ΔH_abs / R * (1/T - 1/T_ref) )[61] - Simulate moisture ingress under defined temperature and humidity conditions over time. Validation: This "endogenous technique" allows for the compensation of temperature term omissions in FEA and helps predict areas within the device package most susceptible to moisture-induced failure, such as delamination [61].
Visualizing Failure Analysis and Mitigation Workflows
The following diagrams map the logical flow of failure mechanisms and the experimental process for validating key material properties.
Diagram 1: Bioelectronics Device Failure Pathways. This map illustrates how environmental stresses in the body lead to specific failure mechanisms and ultimately result in device failure.
Diagram 2: Validating a Stretchable Semiconductor. This workflow outlines the key steps for creating and testing a stretchable semiconductor, from material synthesis to biological safety assessments.
The path toward durable and reliable organic bioelectronics hinges on a fundamental understanding of mechanical fatigue, delamination, and water permeation. By adopting advanced material solutions such as vulcanized biocompatible elastomers, corrosion-resistant metallization, and novel self-healing polymers, researchers can directly address these failure points. Coupling these innovations with robust experimental protocols for accelerated testing and finite element modeling enables the predictive design of devices that can withstand the dynamic conditions of the human body. As the field progresses, the integration of these mitigation strategies will be paramount in fulfilling the promise of long-term, implantable bioelectronic systems that are both functionally stable and truly biocompatible.
The integration of electronic systems with biological tissues represents a frontier in modern bioelectronics, with applications spanning from continuous health monitoring to closed-loop therapeutic interventions. A significant impediment to the chronic stability and biocompatibility of these interfaces is the mechanical and chemical mismatch caused by conventional power sources and data transmitters. This whitepaper examines the core challenges associated with power and data transfer for implantable and wearable bioelectronic devices. It explores the evolution of innovative battery-free and wireless systems, with a specific focus on material choices and engineering strategies that enhance biocompatibility and functional longevity within the context of organic bioelectronics. The synthesis of emerging energy harvesting techniques, novel communication protocols, and biocompatible materials is poised to enable a new generation of seamlessly integrated bioelectronic interfaces.
The vision of seamless integration between electronics and the human body is a central pursuit in organic bioelectronics. Traditional bioelectronic implants, such as pacemakers and neurostimulators, rely on rigid, bulky batteries and wired connections for power and data. These elements create a fundamental mechanical mismatch with soft, dynamic biological tissues, often leading to foreign body responses, inflammation, fibrosis, and eventual device failure [8]. The need for repeated surgical interventions to replace batteries further introduces risk and patient discomfort, limiting the long-term viability of these devices.
Within the broader thesis on organic bioelectronics biocompatibility research, the hurdles of power and data transfer are not merely operational but fundamentally biological. The goal is to develop systems that are not only technically efficient but also mechanically compliant and biologically inert. This requires a multidisciplinary approach, drawing from materials science, electrical engineering, and biology to create devices that can operate continuously and autonomously within or on the body. The emergence of wireless, battery-free platforms represents a paradigm shift, potentially eliminating the most problematic components of current implants and wearables. These platforms rely on two key technological pillars: advanced methods for wireless power transfer (WPT) and ultra-low-power communication protocols, both of which must be engineered with biocompatibility as a primary design constraint [62].
Core Technical Hurdles in Power and Data Transfer
Developing effective wireless and battery-free systems for biointegration requires overcoming significant technical challenges. These hurdles dictate the performance, reliability, and ultimately, the safety of the device within a biological environment.
The primary challenge in power transfer is achieving efficient and sufficient energy delivery while minimizing the physical footprint of the harvesting unit. For implants, the body itself presents a significant barrier; tissues attenuate electromagnetic waves, limiting the depth from which energy can be effectively harvested. Furthermore, the efficiency of energy harvesters (e.g., RF antennas, piezoelectric transducers) is often low, requiring sophisticated power management circuits to store and regulate the harvested energy for stable device operation [62]. The use of supercapacitors instead of batteries is a common strategy to mitigate the longevity and toxicity concerns associated with batteries, but they offer limited energy storage capacity, necessitating duty cycling of the device functions [63].
For data communication, the central hurdle is the conflict between power consumption and bandwidth. High-data-rate transmission, such as that required for neural recording or high-resolution imaging, is traditionally power-intensive. However, the power budget for a battery-free device is constrained by what can be harvested from the ambient environment or beamed in from an external source. This necessitates the development of communication schemes that are exceptionally power-frugal. While established protocols like Near Field Communication (NFC) offer a good balance of power and data rate for near-surface applications, they are unsuitable for deep-tissue implants or high-bandwidth applications [64] [62]. Alternatives like acoustic backscatter have been demonstrated for underwater imaging, consuming as little as 59 μW for data transmission, but they face challenges with bandwidth and signal interference [63].
Table 1: Key Challenges in Wireless, Battery-Free System Design
| Domain | Specific Challenge | Impact on Biocompatibility & Function |
|---|---|---|
| Power Transfer | Limited energy harvesting efficiency | Restricts device functionality, requires larger harvesters, increasing device size and stiffness. |
| Power Transfer | Attenuation of energy through biological tissue | Limits implantation depth, may require higher external transmission power. |
| Power Transfer | Energy storage capacity of miniaturized supercapacitors | Necessitates intermittent operation (duty cycling), potentially missing critical biosignals. |
| Data Communication | High power consumption of conventional transceivers | Depletes limited energy budget, generates heat, can cause tissue damage. |
| Data Communication | Limited bandwidth of low-power protocols (e.g., backscatter) | Constrains data throughput, limiting application in high-resolution sensing or imaging. |
| System Integration | Corrosion of metal components in biofluids | Releases toxic ions, causes device failure, triggers inflammatory response. |
| System Integration | Mechanical mismatch between device and tissue | Causes micro-injuries, inflammation, fibrosis, and reduces signal fidelity [8]. |
Innovations in Battery-Free Power Solutions
To overcome the power hurdle, research has focused on two main approaches: power casting (directed external energy) and ambient energy harvesting. The choice of strategy is critical as it directly influences the device's form factor, operational lifetime, and application scope.
Power Casting Techniques
Power casting involves the directed transmission of energy from an external source to the implanted or wearable device. This method provides a reliable and controllable power source, which is ideal for applications with predictable and consistent power demands.
Near-Field Magnetic Resonant Coupling (MRC): This is one of the most prevalent methods, operating in the non-radiative near-field regime (typically at 13.56 MHz, the NFC standard). An external primary coil generates an alternating magnetic field, which is captured by a secondary coil antenna on the implant. The captured AC energy is then rectified and regulated to power the electronics. MRC is highly efficient over short distances (less than the diameter of the transmitter coil) and allows for simultaneous data communication via load modulation. Recent innovations include the development of wearable "smart" clothing with embroidered conductive threads that act as relay coils, extending the powering range over the body [62]. This technology is well-suited for powering subcutaneous devices and thin, wearable sensors [64].
Radio Frequency (RF) Energy Harvesting: RF energy harvesting captures radiated electromagnetic waves from ambient sources (e.g., Wi-Fi, cellular) or dedicated transmitters. While it offers the potential for longer-range power delivery compared to MRC, its efficiency is lower due to radiative losses and significant attenuation by biological tissues. Nevertheless, companies like Energous and Powercast are developing RF-based platforms for asset tracking and sensors, achieving power delivery over distances of several feet [65] [66]. For biomedical applications, RF is more suitable for wearable devices rather than deep implants.
Acoustic Energy Harvesting: Particularly useful in underwater environments or where electromagnetic waves are ineffective, this method uses ultrasonic transducers to convert sound waves into electrical energy. It has been successfully demonstrated to power a fully submerged battery-free camera system, with harvested energy stored in a supercapacitor to support imaging cycles [63]. Acoustic waves propagate well through water and soft tissues, making this a promising approach for certain implantable applications.
Ambient Energy Harvesting
This approach leverages the patient's own biological or environmental energy, enabling truly self-powered and autonomous operation without the need for an external transmitter.
Piezoelectric/Triboelectric Harvesting: These generators convert mechanical energy from body movements, muscle stretches, or even heartbeats into electricity. Piezoelectric materials generate a charge in response to applied mechanical stress, while triboelectric effects harness contact electrification [62].
Thermoelectric Harvesting: This technique exploits the temperature gradient between the body's core and the external environment to generate a small but continuous flow of power, suitable for ultra-low-power sensors [62].
Table 2: Comparison of Wireless Power Transfer Methods for Bioelectronics
| Method | Operating Principle | Typical Power Output | Advantages | Disadvantages | Suitable Bio-applications |
|---|---|---|---|---|---|
| MRC / NFC | Magnetic inductive coupling | Up to 500 mW [62] | High efficiency, bidirectional data, well-established standard. | Very short range, sensitive to coil alignment. | Subcutaneous implants, skin-mounted sensors [64]. |
| RF Harvesting | Capture of radiated EM waves | Microwatts to milliwatts | Longer operational range, leverages ambient sources. | Low efficiency, tissue heating concerns, large antenna size. | Wearable patches, smart textiles. |
| Acoustic Harvesting | Conversion of sound pressure waves | ~276 μW (for imaging) [63] | Good tissue penetration, efficient in fluids. | Limited bandwidth for data, potential for cavitation. | Underwater monitors, deep-tissue implants. |
| Piezoelectric | Mechanical stress on active material | Variable (μW to mW) | Self-powered, no external source needed. | Intermittent power, dependent on patient activity. | Pacemakers, joint motion sensors. |
| Thermoelectric | Body-environment temperatureå·® | Tens of microwatts | Continuous, low-power source. | Very low power output, requires significant gradient. | Continuous low-power monitoring (e.g., temperature). |
Breakthroughs in Ultra-Low-Power Data Communication
Once power is secured, transmitting data without depleting the energy budget is the next critical challenge. The trend is moving away from traditional, power-hungry active radios toward reflective communication and efficient standards.
Backscatter Communication is a cornerstone technology for battery-free systems. Instead of generating a new radio wave, backscatter devices modulate and reflect an existing incoming RF or acoustic wave. This process consumes orders of magnitude less power than active transmission. A seminal example is the underwater battery-free camera, which uses piezo-acoustic backscatter. The camera modulates the reflection coefficient of its piezoelectric transducer by switching connected electrical loads (inductors), encoding data in the reflected acoustic pattern with a power consumption of only 24 nanowatts for the switching operation and 59 μW for the entire communication process [63]. This net-zero-power approach enables real-time data telemetry from a device powered entirely by harvested acoustic energy.
Near Field Communication (NFC) remains a widely adopted standard for short-range, bidirectional data exchange. It is often integrated with MRC power transfer, creating a unified platform for power and data. Its key advantage is its ultra-low-power design and integration into many consumer smart devices (e.g., smartphones, tablets), which can act as convenient readers. This makes it ideal for wearable, skin-mountable sensors that monitor parameters like pressure, shear stress, and temperature, as demonstrated by a multi-axial sensor for augmented reality-assisted healthcare monitoring [64].
The following diagram illustrates the typical signal and data workflow in a wireless, battery-free sensing system, integrating both power casting and data backscattering.
Experimental Protocols and Material Foundations
The reliability of data from wireless, battery-free bioelectronic devices hinges on robust experimental methodologies and the use of materials that ensure both electrical performance and biocompatibility.
Protocol: In Vivo Biocompatibility Testing of an Implantable Transistor
This protocol is based on the pioneering work detailed in [8], which reported a biocompatible and stretchable organic field-effect transistor (OFET).
Device Fabrication:
- Material Synthesis: Prepare a semiconducting blend film by combining a conjugated polymer (e.g., poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] or DPPT-TT) with a medical-grade bromo isobutyl–isoprene rubber (BIIR) elastomer at an optimized weight ratio (e.g., 3:7 DPPT-TT:BIIR).
- Vulcanization: Chemically crosslink the blend film using a sulfur-based vulcanization process with additives (e.g., stearic acid as an initiator) to enhance mechanical elasticity and stability.
- Electrode Fabrication: Use a dual-layer metallization of silver and gold to create stretchable, corrosion-resistant electrodes. The gold layer provides a biocompatible and biofluid-resistant outer surface.
- Encapsulation: Fully encapsulate the device in a medical-grade elastomer (e.g., BIIR or PDMS) to isolate it from the biological environment.
In Vitro Biocompatibility Assessment:
- Cell Culture: Culture relevant cell lines, such as human dermal fibroblasts and macrophages.
- Viability Assay: Expose cells to the device or its material extracts for a predetermined period (e.g., 24-72 hours). Perform assays like MTT or Live/Dead staining to quantify cell viability relative to a control.
- Proliferation & Migration Assays: Assess potential impact on cell proliferation (e.g., via BrdU assay) and migration (e.g., via scratch assay) to ensure the device does not inhibit normal cellular functions.
In Vivo Implantation and Evaluation:
- Animal Model: Implant the fabricated transistor subcutaneously in a mouse model, following approved ethical and surgical guidelines.
- Histological Analysis: After a set period (e.g., 2-4 weeks), explant the device and the surrounding tissue. Process the tissue for histological sectioning and staining (e.g., H&E for general morphology, Masson's trichrome for collagen deposition/fibrosis).
- Evaluation Criteria: Analyze the tissue slides for key indicators of biocompatibility: the absence of a major inflammatory response (minimal immune cell infiltration), no signs of necrosis, and minimal fibrous capsule formation around the implant.
The Scientist's Toolkit: Essential Materials for Biocompatible Wireless Electronics
Table 3: Key Research Reagents and Materials for Device Fabrication
| Material / Component | Function | Biocompatibility & Research Rationale |
|---|---|---|
| BIIR (Bromo Isobutyl–Isoprene Rubber) | Medical-grade elastomer matrix for semiconductors and encapsulation. | Meets ISO 10993 standards; offers high biocompatibility, aging resistance, and a Young's modulus similar to human tissue, minimizing mechanical mismatch [8]. |
| DPPT-TT Semiconducting Polymer | Provides charge transport pathway in organic transistors. | Enables the creation of a stretchable semiconducting nanofibre network when blended with BIIR, allowing for high electrical performance under strain [8]. |
| Ag/Au Dual-Layer Electrodes | Conductive interconnects and contact pads. | Silver offers excellent conductivity, while a gold outer layer provides robust corrosion resistance against biofluids, preventing toxic ion release [8]. |
| NFC System-on-Chip (SoC) | Integrated circuit for power harvesting and data communication. | Enables battery-free operation via harvested RF energy and facilitates bidirectional data transmission using an established, low-power standard (ISO 15963) [64]. |
| Piezoelectric Transducer | Converts acoustic energy to electricity and enables acoustic backscatter. | Serves a dual purpose: as an energy harvester in relevant environments (e.g., underwater) and as an ultra-low-power communication element via impedance modulation [63]. |
| Polydimethylsiloxane (PDMS) | Flexible and stretchable encapsulation material. | Provides a moisture barrier and electrical insulation while maintaining device flexibility. Its biocompatibility makes it a widely used material in biomedical devices [64]. |
The architecture of a compliant implantable device relies on the strategic integration of these materials, as visualized in the following diagram of a biocompatible transistor.
Implementation in Research and Clinical Applications
The convergence of these technologies is enabling sophisticated applications that were previously impractical. Two examples highlight this transition from concept to functional system.
1. Implantable, Biocompatible Organic Transistors for Electrophysiology: As detailed in [8], the development of a stretchable OFET using a DPPT-TT:BIIR blend represents a significant milestone. This device overcomes the critical limitation of mechanical mismatch by possessing a Young's modulus similar to human tissue. It maintains stable electrical performance under 50% strain and showed no adverse effects on cell viability or major inflammatory responses in vivo. This technology paves the way for chronically stable implants that can seamlessly interface with nerves, muscles, or the brain for continuous signal monitoring and modulation, forming a core component of advanced organic bioelectronic interfaces.
2. Wireless, Battery-Free Multi-Axial Sensor for AR-Assisted Healthcare: This system, described in [64], integrates an NFC-powered, skin-mountable sensor with an augmented reality platform. The sensor, which measures pressure, shear stress, and temperature at the skin interface, is thin, small, and battery-free, ensuring patient comfort and long-term monitoring capability. The data is wirelessly transmitted to a laptop, processed via machine learning to determine force magnitude and direction, and then visualized through AR glasses or a smartphone. This application demonstrates a practical use case in preventing pressure injuries and monitoring posture, providing medical staff with an intuitive, real-time view of biomechanical data directly overlaid on the patient.
The field of wireless, battery-free systems is rapidly evolving, directly addressing the core power and data transfer hurdles that have long impeded the progress of chronic bioelectronic implants and wearables. The strategic shift from rigid batteries to flexible energy harvesters, and from power-hungry radios to ultra-low-power backscatter communication, is foundational to creating devices that are both functionally robust and biologically compliant. The emphasis on medical-grade, stretchable materials like BIIR is a critical step in ensuring that these devices can coexist harmoniously with biological tissues without eliciting a detrimental immune response.
Looking forward, the integration of these platforms with artificial intelligence and edge computing will unlock new capabilities in predictive analytics and personalized therapy. Furthermore, the ongoing development of advanced nanomaterials, such as graphene, and the advent of future communication protocols like 6G, promise to enhance energy harvesting efficiency and data transmission bandwidth [67]. As these innovations mature, the vision of a seamlessly integrated bioelectronic system, capable of long-term, high-fidelity interaction with the human body for advanced diagnostics and therapeutics, is steadily moving toward reality.
Optimizing Material Degradation Profiles for Bioresorbable and Transient Electronics
The emergence of bioresorbable and transient electronics represents a paradigm shift in bioelectronics, moving from devices designed for permanent persistence to those that operate for a defined period before physically disappearing [68]. This technology, framed within the broader context of organic bioelectronics biocompatibility research, offers transformative potential for implantable medical devices that provide temporary diagnostic or therapeutic functions and then safely dissolve, eliminating the need for secondary extraction surgery [68] [69]. The core challenge lies in precisely controlling material degradation profiles to ensure device functionality throughout the required operational lifetime while guaranteeing complete, benign resorption thereafter [68]. This technical guide examines the current state of material systems, degradation mechanisms, characterization methodologies, and optimization strategies essential for advancing this rapidly evolving field, with particular emphasis on balancing electronic performance with biocompatibility and predictable degradation behavior.
Material Systems and Their Degradation Kinetics
Inorganic Semiconductors and Metals
Bioresorbable electronics utilize a carefully selected palette of inorganic materials with well-characterized dissolution profiles in physiological environments. Silicon, in various structural forms, serves as a foundational material, with its degradation occurring via hydrolysis: Si + 4H₂O → Si(OH)₄(aq) + 2H₂ [69]. The degradation rate is highly dependent on crystallinity and doping, with amorphous silicon degrading fastest, followed by polycrystalline and single-crystalline forms [68] [69].
Table 1: Degradation Rates of Key Inorganic Semiconductor Materials
| Material | Form/Description | Degradation Conditions | Degradation Rate | Key Influencing Factors |
|---|---|---|---|---|
| Silicon | Single-crystalline (B-doped 10¹ⶠcmâ»Â³, 100nm) | 1M PBS, pH 7.4, 37°C | ~100 nm/day | Dopant type & concentration, temperature, pH [69] |
| Silicon | Single-crystalline (highly doped) | PBS, pH 7.4, 37°C | 0.3-0.8 nm/day | Higher dopant concentration slows degradation [69] |
| Germanium | Nanomembranes | Aqueous solutions | Faster than Si | Crystallinity, pH, temperature [68] [69] |
| IGZO (Indium-Gallium-Zinc Oxide) | Amorphous oxide semiconductor | Aqueous solutions | Tunable rates | Composition, structure, thickness [68] |
Bioresorbable metals function as essential components for interconnects, electrodes, and structural elements. Their degradation occurs through electrochemical processes that are strongly influenced by local environmental conditions.
Table 2: Degradation Profiles of Bioresorbable Metals
| Metal | Degradation Conditions | Degradation Rate | Applications | Considerations |
|---|---|---|---|---|
| Magnesium | Simulated Body Fluid (SBF), pH 7.4, 37°C | 1.2-12 µm/day | Electrodes, interconnects, structural components [68] | Rapid degradation may limit functional lifetime; alloying can modulate rates [68] |
| Zinc | Phosphate Buffered Saline (PBS), pH 7.4, 37°C | ~3.5 µm/day [68] | Electrodes for bioresorbable batteries [70] | More stable than Mg; suitable for medium-duration implants |
| Tungsten | SBF, pH 7.4, room temperature | 0.48-1.44 µm/day [68] | Interconnects, substrates | Slow degradation suitable for longer-term applications |
| Molybdenum | pH 7 buffer, room temperature | ~0.001 µm/day [68] | Interconnects, substrates | Very slow degradation; potential for very long-term devices |
Organic and Polymeric Materials
Organic materials provide flexibility, functionality, and tunable degradation profiles in transient electronic systems. Their degradation typically occurs through hydrolysis (enzymatic or non-enzymatic) or enzymatic cleavage, with rates dependent on chemical structure, molecular weight, and crystallinity.
Table 3: Organic and Polymeric Materials in Transient Electronics
| Material | Type | Degradation Mechanism | Applications | Degradation Byproducts |
|---|---|---|---|---|
| Silk Fibroin | Protein polymer | Proteolytic enzymatic degradation [68] | Substrates, encapsulation [71] [70] | Amino acids, peptides (potential copper complexes) [71] |
| Poly(lactic-co-glycolic acid) (PLGA) | Synthetic polyester | Hydrolysis of ester bonds | Substrates, encapsulation | Lactic acid, glycolic acid |
| Poly(ethylene oxide) (PEO) | Synthetic polymer | Hydrolysis, oxidation | Sensing layers, matrices [71] | Oligomers, ethylene glycol [71] |
| Cellulose Acetate | Modified natural polymer | Deacetylation, hydrolysis | Substrates [71] | Acetic acid, cellulose (dependent on degree of substitution) [71] |
| Poly(3,4-ethylenedioxythiophene): Polystyrene sulfonate (PEDOT:PSS) | Conductive polymer | Hydrolysis, potentially incomplete | Electrodes [71] | Potential polystyrene derivatives/microplastics [71] |
Degradation Mechanisms and Pathways
The dissolution of bioresorbable materials follows distinct chemical pathways that can be modulated through material selection, processing, and environmental control. Understanding these mechanisms at a fundamental level is essential for predicting and optimizing device lifetime.
Material Degradation Pathways: This diagram illustrates the primary mechanisms through which different classes of bioresorbable materials degrade when exposed to environmental stimuli, and how their byproducts necessitate thorough biocompatibility assessment.
Experimental Characterization Methodologies
In Vitro Degradation Testing
Standardized in vitro testing provides controlled conditions for initial screening of material degradation behavior and kinetics. The following protocol outlines a comprehensive approach:
Protocol: Hydrolytic Degradation Analysis
Sample Preparation: Fabricate material samples with standardized dimensions (e.g., 1×1 cm²). For thin films, use consistent thicknesses (typically 100-500 nm). Measure and record initial mass (M₀), thickness, and functional properties (electrical conductivity, optical transmittance, etc.).
Solution Preparation: Prepare degradation media simulating physiological conditions:
- Phosphate Buffered Saline (PBS), pH 7.4, for general screening
- Simulated Body Fluid (SBF) for biomedically targeted materials
- Solutions with varying pH (3-10) to assess pH dependence
- Add enzymes (e.g., proteases for protein-based materials) for enzymatic degradation studies
Incubation Conditions: Maintain samples in media at 37°C with constant agitation. Use a sufficient volume of solution to ensure sink conditions (typically 20:1 volume-to-sample surface area ratio). Sterilize samples if testing for biomedical applications.
Time-Point Analysis: Remove samples at predetermined intervals (e.g., 1, 3, 7, 14, 28 days). Rinse with deionized water and dry thoroughly before analysis. Include triplicate samples for statistical significance.
Characterization Techniques:
- Mass Loss: Measure dry mass (Mₜ) at each time point and calculate percentage mass loss: [(M₀ - Mₜ)/M₀] × 100
- Thickness Change: Use profilometry or microscopy to track dimensional changes
- Surface Morphology: Employ scanning electron microscopy (SEM) to observe surface degradation features
- Chemical Analysis: Utilize Fourier-transform infrared spectroscopy (FTIR) and X-ray photoelectron spectroscopy (XPS) to track chemical changes
- Byproduct Identification: Implement liquid chromatography-mass spectrometry (LC-MS) for comprehensive analysis of degradation fragments [71]
Functional Assessment: For electronic materials, monitor electrical properties (conductivity, capacitance) throughout degradation process.
Byproduct Analysis and Environmental Impact Assessment
The environmental safety of transient electronics depends not only on material disappearance but also on the nature of degradation byproducts. As highlighted by recent research, "degradability or biodegradability of electronic devices alone is insufficient to ascertain environmental safety" [71]. The following workflow outlines a systematic approach to byproduct characterization:
Protocol: Degradation Byproduct Analysis Using LC-MS
Sample Collection: Collect degradation media at multiple time points throughout the degradation process. Include early, middle, and late stages to capture evolving byproduct profiles.
Sample Preparation:
- Filter solutions through 0.22 µm filters to remove particulate matter
- Concentrate samples if necessary using lyophilization or solid-phase extraction
- Derivatize if needed to enhance detection of specific compound classes
Liquid Chromatography Separation:
- Column: C18 reverse-phase column (e.g., 2.1 × 100 mm, 1.7 µm)
- Mobile phase: Gradient from aqueous to organic solvent (e.g., water to acetonitrile)
- Flow rate: 0.2-0.4 mL/min
- Injection volume: 1-10 µL
Mass Spectrometry Analysis:
- Ionization: Electrospray ionization (ESI) in positive and negative modes
- Mass range: m/z 50-2000 for comprehensive coverage
- Resolution: High resolution (>20,000) for accurate mass determination
- Data acquisition: Full scan mode for untargeted analysis, followed by MS/MS for structural elucidation
Data Interpretation:
- Identify potential degradation fragments based on accurate mass and fragmentation patterns
- Compare against databases of known biological compounds and potential toxins
- Track evolution of byproducts over time to understand degradation pathways
- Pay special attention to coordination complexes with metal ions (e.g., copper complexes with silk fibroin fragments) [71]
Toxicity Assessment:
- Conduct cell viability assays (e.g., MTT assay) with byproduct mixtures
- Perform environmental toxicity tests if devices are designed for environmental disposal
- Assess potential for bioaccumulation of persistent fragments
Strategies for Degradation Profile Optimization
Material Selection and Engineering
Optimizing degradation profiles requires a multi-faceted approach beginning with strategic material selection and modification:
Composite Material Design: Combining materials with complementary properties can yield optimized degradation profiles. For example, incorporating ZnFeâ‚‚Oâ‚„ or MgFeâ‚‚Oâ‚„ nanoparticles into PLA matrices has been shown to enhance both triboelectric performance and modify degradation behavior in energy harvesting applications [72].
Alloying and Doping: Metallic and semiconductor dissolution rates can be precisely tuned through compositional modification. Silicon degradation slows with increasing dopant concentration, while magnesium-zinc alloys offer intermediate degradation rates between pure components [68] [69].
Structural Engineering: Nanostructuring and controlling crystallinity significantly impact degradation kinetics. Amorphous silicon degrades faster than crystalline forms, while porous structures accelerate dissolution through increased surface area [68].
Cross-Link Density Control: For polymeric systems, degradation rates correlate with cross-link density. Reducing cross-links in hydrogels and elastomers generally accelerates degradation, while increased cross-linking extends functional lifetime [72].
Encapsulation and Lifetime Control
Encapsulation strategies provide the most direct method for controlling functional device lifetime by modulating environmental exposure:
Encapsulation Control Strategies: This diagram categorizes the primary approaches for controlling device lifetime through encapsulation technologies, from passive barrier methods to actively triggered dissolution mechanisms.
Barrier Layer Thickness Optimization: The operational lifetime of bioresorbable devices correlates directly with encapsulation thickness. Silicon oxide and silicon nitride layers provide effective moisture barriers, with degradation rates of approximately 0.1-10 nm/day depending on structure and density [69]. By stacking layers with different dissolution profiles, sequential degradation and multi-stage functional changes can be achieved.
Stimuli-Responsive Materials: Materials that degrade in response to specific triggers (temperature, pH, light, magnetic fields) enable external control over device lifetime. Shape-memory polymers that dissolve upon heating or pH-sensitive hydrogels that swell under specific conditions offer pathways for on-demand dissolution [68].
Geometric Design Considerations: Device architecture significantly influences degradation profiles. Patterned structures with varying thicknesses across different components can create sequential failure modes, maintaining critical functions while allowing non-essential components to degrade first.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Bioresorbable Electronics Development
| Category | Specific Materials | Function in Research | Key Considerations |
|---|---|---|---|
| Semiconductors | Silicon nanomembranes (single crystal, polycrystalline, amorphous) | Active device components, sensors | Tunable degradation via crystallinity and doping [68] [69] |
| Germanium, IGZO, ZnO | Alternative semiconductors | Different bandgaps, degradation rates [68] | |
| Conductive Materials | Magnesium, Zinc foils | Electrodes, interconnects | Biocompatible, degradable, different dissolution rates [68] [70] |
| Tungsten, Molybdenum | Long-lifetime interconnects | Slow dissolution for extended functionality [68] | |
| Polymer Substrates | Silk fibroin | Biocompatible substrate, encapsulation | Tunable degradation via processing, excellent biocompatibility [71] [70] |
| Poly(lactic-co-glycolic acid) (PLGA) | Structural support, encapsulation | Predictable hydrolysis, FDA-approved for many applications | |
| Cellulose acetate | Flexible substrates | Biodegradable, optical transparency [71] | |
| Hydrogel Electrolytes | Guar gum/gelatin/Zn²⺠(GG-Zn) | Quasi-solid electrolytes for batteries | High ionic conductivity (16.1 mS cmâ»Â¹), biocompatible [70] |
| Encapsulation Materials | Silicon oxide, Silicon nitride | Diffusion barriers | Control device lifetime, tunable dissolution rates [69] |
| Characterization Reagents | Phosphate Buffered Saline (PBS) | In vitro degradation studies | Simulates physiological ionic environment [69] |
| Simulated Body Fluid (SBF) | Bio-relevant degradation testing | Closer mimic of physiological conditions than PBS | |
| Proteases, esterases | Enzymatic degradation studies | Accelerated testing for biodegradable polymers |
Optimizing degradation profiles in bioresorbable and transient electronics requires a multidisciplinary approach integrating materials science, chemistry, electronics, and biology. The field has progressed from fundamental material discoveries to functional system-level demonstrations, yet challenges remain in achieving precise lifetime control, expanding material options, and ensuring complete environmental compatibility of degradation byproducts.
Future research directions should focus on developing dynamic encapsulation systems capable of responsive degradation control, expanding the library of bioresorbable semiconductors with diverse electronic properties, and establishing standardized protocols for assessing environmental impact of degradation products. As these technologies advance toward clinical translation, comprehensive biocompatibility assessment and manufacturing scalability will become increasingly critical. The continued convergence of organic bioelectronics with bioresorbable materials promises to enable truly transient medical implants that provide critical diagnostic and therapeutic functions before safely disappearing, ultimately improving patient outcomes while addressing the growing challenge of electronic waste.
Validating Safety and Efficacy: In Vitro, In Vivo, and Comparative Analysis Frameworks
Biocompatibility testing is a pivotal element within the medical device development and regulatory approval processes, ensuring safety and compatibility when interacting with biological systems [73]. For organic bioelectronics—a field creating seamless interfaces between carbon-based electronic devices and biological tissues—demonstrating biocompatibility is fundamental to their function and acceptance [16]. Central to this safety assessment are the "Big Three" tests: cytotoxicity, sensitization, and irritation evaluation [73] [74]. These tests are mandatory for almost all medical devices being introduced to the market and serve as the cornerstone of the biocompatibility assessment, upon which additional, more specific testing may be built [73].
The ISO 10993 series of standards, particularly ISO 10993-1, provides the globally harmonized framework for evaluating the biological safety of medical devices within a risk management process [75] [76]. This standard classifies devices based on the nature and duration of body contact to determine the necessary biological evaluations [75]. As the field of organic bioelectronics advances, creating devices with inherent stretchability and biocompatibility, the rigorous application of these standardized tests provides the critical data needed to validate new materials and ensure patient safety [8] [16].
Regulatory Framework and Testing Strategy
The ISO 10993 Standard Series
The ISO 10993 set entails a series of standards for evaluating the biocompatibility of medical devices to manage biological risk [75]. Its core principle is that biocompatibility is not an intrinsic property of a material but is contingent upon the device's specific application and the nature and duration of its contact with the body [75] [77]. The evaluation is intended to be a structured process within a risk management framework, as outlined in ISO 10993-1:2018, "Evaluation and testing within a risk management process" [75] [76]. This process begins with a thorough assessment of the device, including its material components, manufacturing processes, and clinical use, including the intended anatomical location and the frequency and duration of exposure [77].
The U.S. Food and Drug Administration (FDA) requires biocompatibility assessments for medical devices that have direct or indirect contact with the human body and provides a specific guidance document clarifying its interpretation of the ISO 10993-1 standard [75] [77]. The FDA emphasizes that the assessment should be performed on the medical device in its final finished form, including the effects of sterilization, as this is the form in which the device will be used on patients [77].
Device Categorization and Endpoint Selection
ISO 10993-1 uses a matrix based on the nature of body contact and the contact duration to recommend which biological endpoints require evaluation for a given device [75]. The "Big Three" tests—cytotoxicity, sensitization, and irritation—are required for most medical device categories, making them the most frequently performed biocompatibility assessments [73]. The table below summarizes the testing considerations based on device categorization.
Table 1: ISO 10993-1 Endpoint Considerations Based on Device Categorization (Adapted from FDA-modified matrix) [75]
| Nature of Body Contact | Contact Duration | Cytotoxicity | Sensitization | Irritation | |
|---|---|---|---|---|---|
| Surface Device | Intact Skin | A (≤24 h) | X | X | X |
| B (>24 h to 30 d) | X | X | X | ||
| C (>30 d) | X | X | X | ||
| Mucosal Membrane | A | X | X | X | |
| B | X | X | X | ||
| C | X | X | X | ||
| External Communicating Device | Blood Path, Indirect | A | X | X | X |
| B | X | X | X | ||
| C | X | X | O | ||
| Implant Device | Tissue/Bone | A | X | X | X |
| B | X | X | X | ||
| C | X | X | X | ||
| Legend: X = ISO 10993-1 recommended endpoint for consideration; O = Additional FDA recommended endpoint for consideration. |
The following diagram illustrates the logical decision-making process for initiating a biocompatibility evaluation and selecting the necessary tests per ISO 10993-1.
Detailed Analysis of the "Big Three" Assays
Cytotoxicity Testing (ISO 10993-5)
Cytotoxicity testing evaluates whether a medical device or its materials release substances that are toxic to living cells, causing cell damage or death [78]. This test serves as an excellent initial screen for the potential toxicity of device materials [79].
- Purpose and Importance: The primary purpose is to assess the potential for cell damage, a crucial step in identifying any toxic effects the device materials might have on the body [74]. It is a sensitive and rapid in vitro method that can detect the presence of biologically harmful leachables [78] [79].
- Mechanism of Action: Cytotoxicity occurs when leachable chemicals from a device diffuse into the culture medium and contact a layer of cultured mammalian cells. These chemicals can disrupt essential cellular functions, leading to effects such as:
- Experimental Protocols: Testing is governed by ISO 10993-5:2009, "Tests for in vitro cytotoxicity" [75] [78]. The following table summarizes the key methodological approaches.
Table 2: Standardized Methods for Cytotoxicity Testing (ISO 10993-5) [78] [79] [73]
| Method | Principle | Sample Type | Key Procedural Steps | Endpoint Measurement |
|---|---|---|---|---|
| Direct Contact | Test material is placed directly onto cells. | Low-density materials (e.g., polymer films). | 1. Grow cells to near-confluency. 2. Place test material directly on cell layer. 3. Incubate (e.g., 24 h). | Microscopic evaluation of zone of malformation, degeneration, or lysis around test material. |
| Agar Diffusion | A nutrient-supplemented agar layer is placed between cells and test material. | High-density materials (e.g., elastomers). | 1. Grow cells to confluency. 2. Overlay with agar. 3. Place test material on agar surface. 4. Incubate. | Microscopic evaluation of zone of malformed or lysed cells under and around test material. |
| MEM Elution | Extracts of the test material are prepared and applied to cells. | Applicable to most devices, allows for extraction condition tailoring. | 1. Prepare extracts using various media (e.g., saline, serum). 2. Apply extract onto cell layer. 3. Incubate. | Microscopic evaluation of cell layer for malformation, degeneration, and lysis. Can be semi-quantitative. |
| Quantitative (MTT) Assay | Measures reduction of yellow MTT to purple formazan by mitochondrial enzymes in living cells. | Extracts or direct contact; preferred for quantitative data. | 1. Expose cells to extract or test material. 2. Add MTT reagent and incubate. 3. Solubilize formazan crystals. 4. Measure absorbance with a plate reader. | Cell viability calculated as a percentage of the negative control. <70% cell viability is often a cause for investigation [73]. |
Sensitization Testing (ISO 10993-10)
Sensitization testing assesses the potential of a device or its materials to cause an allergic reaction, specifically a delayed-type (Type IV) hypersensitivity response [78]. This is critical for patient safety, as allergic reactions can range from mild irritation to severe systemic responses [78].
- Purpose and Importance: The test evaluates whether repeated or prolonged exposure to device materials can trigger the immune system to become overreactive, leading to persistent allergic symptoms upon subsequent contact [78] [79]. It is recommended for all classes of medical devices [79].
- Mechanism of Action: Sensitization involves immunologic mechanisms. During an induction phase, a hapten (a small molecule that can elicit an immune response only when attached to a large carrier) from the device material is taken up by antigen-presenting cells in the skin, which then migrate to the draining lymph nodes and activate T-lymphocytes. Upon a subsequent challenge (re-exposure), these primed T-cells proliferate rapidly and initiate a localized inflammatory response, manifesting as redness, swelling, and itching [78] [79].
- Experimental Protocols: Testing is guided by ISO 10993-10 (now partly superseded by ISO 10993-23) and typically uses animal models [75] [78]. The following table compares the common assays.
Table 3: Standardized Methods for Sensitization Testing [78] [79]
| Method | Principle | Animal Model | Key Procedural Steps | Endpoint Measurement |
|---|---|---|---|---|
| Guinea Pig Maximization Test (GPMT) | Maximizes sensitization potential by injecting test material with an adjuvant. | Guinea Pig | 1. Induction: Intradermal injections with/without adjuvant. 2. Rest period. 3. Challenge: Topical application. | Visual scoring of erythema and edema at challenge sites compared to controls. |
| Buehler Test (Closed Patch) | A less invasive method using repeated topical application. | Guinea Pig | 1. Induction: Repeated topical application of test material to shaved skin. 2. Rest period. 3. Challenge: Topical application to a new site. | Visual scoring of skin reactions (redness and swelling) at the challenge site. |
| Murine Local Lymph Node Assay (LLNA) | Quantifies lymphocyte proliferation in lymph nodes draining the application site. | Mouse | 1. Induction: Topical application of extract or material to ears for 3 consecutive days. 2. Pulse: Inject radioactive isotope. 3. Harvest: Drain auricular lymph nodes. | Measure lymphocyte proliferation via radioactive incorporation or other markers. A stimulation index is calculated. |
Irritation Testing (ISO 10993-10 / -23)
Irritation testing estimates the potential of a device, its materials, or extracts to cause localized, non-immunological inflammation or discomfort at the site of contact [78]. Unlike sensitization, irritation does not involve a learned immune response and typically occurs immediately after exposure [78].
- Purpose and Importance: This test ensures that devices do not cause pain, redness, or inflammation during use, which is crucial for patient comfort and compliance [78]. It is critical for devices like wound dressings, surgical drapes, and catheters that remain in contact with skin or mucous membranes [78].
- Mechanism of Action: Irritation is a localized inflammatory response triggered by the direct chemical action of a leachable substance on tissues. It involves the release of inflammatory mediators such as histamines and cytokines, leading to vasodilation (causing redness and warmth), increased vascular permeability (causing swelling or edema), and potential damage to tissue at the contact site [78] [79].
- Experimental Protocols: Guidance is provided in ISO 10993-10 and ISO 10993-23 [75]. The route of exposure should simulate the anticipated clinical use.
Table 4: Standardized Methods for Irritation Testing [78] [79]
| Method | Principle | Application / Model | Key Procedural Steps | Endpoint Measurement |
|---|---|---|---|---|
| Intracutaneous Reactivity Test | Injects device extracts intradermally to assess localized inflammation. | Recommended for devices with internal contact. | 1. Prepare extracts in polar and non-polar solvents. 2. Inject intracutaneously into the shaved skin of rabbits. 3. Use blank extracts as controls. | Score injection sites for erythema (redness) and edema (swelling) at 24, 48, and 72 hours post-injection. |
| Primary Skin Irritation Test | Applies the test material or extract directly to intact and abraded skin. | Recommended for topical devices with external contact. | 1. Apply test material to intact and abraded skin sites on rabbits. 2. Cover and restrain for 24 hours. 3. Remove material and score sites. | Score sites for erythema and edema immediately after removal and at 24, 48, and 72 hours. |
| Mucous Membrane Irritation Test | Assesses irritation potential on sensitive mucous membranes. | For devices contacting natural channels (e.g., oral, vaginal, ocular). | Varies by tissue (e.g., vaginal, cheek pouch, eye irritation studies). Often uses extracts. | Specific to the tissue; e.g., the eye test scores corneal opacity, iris hyperemia, and conjunctival redness/swelling. |
Application in Organic Bioelectronics Research
The field of organic bioelectronics aims to create seamless, adaptable, and intelligent interfaces between electronic devices and biological systems [16]. For these devices—which include implantable neural interfaces, wearable health monitors, and tissue engineering scaffolds—biocompatibility is not just a regulatory hurdle but a fundamental prerequisite for functionality [8] [16].
Unique Material Challenges and Testing Adaptations
Traditional rigid electronic materials like silicon and gold exhibit a significant mechanical mismatch with soft biological tissues, often leading to inflammation and device failure [16]. Organic bioelectronics employs soft, conductive materials such as conjugated polymers (e.g., PEDOT:PSS) and biocompatible elastomers (e.g., Bromo Isobutyl–Isoprene Rubber, BIIR) to create devices with a Young's modulus similar to human tissues [8] [16]. This inherent mechanocompatibility is a key advantage, but these novel composite materials still require rigorous chemical biocompatibility testing as per ISO 10993 [8].
A recent pioneering example is the development of a fully elastomeric organic field-effect transistor (OFET) for implantable electronics. The device was fabricated using a vulcanized blend of a semiconducting polymer (DPPT-TT) and BIIR, a medical-grade elastomer [8]. This material combination was specifically chosen for its potential to meet stringent biocompatibility standards like ISO 10993 [8].
- In Vitro Validation: The researchers performed in vitro cytotoxicity assessments consistent with ISO 10993-5, culturing human dermal fibroblasts and macrophages with their transistor materials. Results showed no adverse effects on cell viability, proliferation, or migration, successfully passing this critical "Big Three" endpoint [8].
- In Vivo Correlation: The study also included in vivo implantation in mice, a test aligned with ISO 10993-6:2016, "Tests for local effects after implantation". The findings showed no major inflammatory response or tissue damage, confirming the biocompatibility predicted by the in vitro tests and demonstrating the material's suitability for long-term integration [8].
This case demonstrates a complete testing workflow: from material design with biocompatibility in mind (using medical-grade BIIR), through standardized in vitro cytotoxicity screening, and final validation with an in vivo implantation study.
The Scientist's Toolkit: Essential Reagents and Materials
Table 5: Key Research Reagent Solutions for "Big Three" Testing
| Reagent / Material | Function in Biocompatibility Testing | Example Application in Bioelectronics |
|---|---|---|
| Mammalian Cell Lines (e.g., L929, Balb/3T3 fibroblasts) | Used as the biological substrate for in vitro cytotoxicity testing (ISO 10993-5). | Assessing the toxic leachables from novel conductive polymers or elastomers. |
| Extraction Solvents (e.g., Physiological Saline, Vegetable Oil, MEM) | Used to prepare extracts of device materials, simulating the elution of chemicals in different biological milieus (ISO 10993-12). | Testing organic electronic components by extracting them in simulated body fluids. |
| MTT Reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide) | A colorimetric agent for quantitative cytotoxicity assays; measures mitochondrial activity as a marker of cell viability. | Providing a quantitative dose-response curve for the cytotoxicity of a material extract. |
| Complete Freund's Adjuvant (CFA) | An immunopotentiator used in the Guinea Pig Maximization Test to enhance the immune response during the induction phase. | Maximizing sensitivity to detect the potential for delayed hypersensitivity to polymer residues. |
| Medical-Grade Elastomers (e.g., BIIR, Polyurethane) | Used as the matrix or substrate in stretchable bioelectronics to provide mechanical compliance and inherent biocompatibility. | Serving as the foundational, biocompatible material in implantable stretchable transistors [8]. |
| Dual-Layer Metallization (e.g., Ag/Au) | Used to create robust, stretchable, and biofluid-corrosion-resistant electrodes for implantable devices. | Ensuring electrical functionality and biocompatibility of interconnects in physiological environments [8]. |
The following diagram illustrates the integrated experimental workflow from material synthesis to biological safety validation, as demonstrated in advanced bioelectronics research.
The "Big Three" biocompatibility tests—cytotoxicity, sensitization, and irritation—form the indispensable foundation for ensuring the safety of all medical devices, including the emerging and revolutionary class of organic bioelectronics [73] [74]. The standardized methodologies outlined in the ISO 10993 series provide a rigorous and globally recognized framework for conducting these assessments within a risk management process [75] [76].
For researchers in organic bioelectronics, adhering to these standards is not merely about regulatory compliance. It is a critical component of the design and validation process that enables the translation of laboratory innovations into safe and effective clinical applications [8]. By integrating biocompatibility testing early in the development pipeline—from the initial selection of medical-grade elastomers and conductive polymers to the final in vivo validation of a functioning device—scientists can de-risk the development process and build a robust safety profile for their technologies [8]. As the field progresses towards more complex and integrated bioelectronic systems, the principles of ISO 10993 and the diligent application of the "Big Three" tests will continue to be paramount in bridging the gap between electronic technology and human biology safely and effectively.
In vitro assessment of cellular behaviors is a cornerstone of biomedical research, providing critical insights into the biological performance of novel therapeutic agents and materials. Within the rapidly advancing field of organic bioelectronics, where devices interface directly with biological systems, rigorous biocompatibility evaluation using human cell lines is paramount. These assessments ensure that innovative technologies such as implantable organic field-effect transistors (OFETs) and therapeutic extracellular vesicles (EVs) can safely and effectively modulate cellular functions without provoking adverse responses [8] [80]. This guide details established methodologies for quantifying fundamental cellular parameters—viability, proliferation, and migration—framed within the context of organic bioelectronics research. The protocols and data presentation standards herein are designed to help researchers reliably evaluate how organic electronic materials, with their unique properties of flexibility, mixed ionic-electronic conduction, and engineered biocompatibility, influence cellular behavior in controlled laboratory environments [16].
Core Cellular Assessments: Principles and Protocols
Cell Viability and Cytotoxicity Assessment
Cell viability assays determine the proportion of living cells within a population after exposure to test materials or compounds, providing a crucial first measure of biocompatibility or therapeutic efficacy.
Detailed MTT Assay Protocol:
- Cell Seeding and Culture: Plate cells (e.g., U-87 MG glioblastoma or HDFa fibroblast lines) in 96-well plates at a density of 5–7 × 10³ cells per well in complete medium. Allow cells to adhere for 24 hours under standard culture conditions (37°C, 5% CO₂) [81].
- Treatment Application: Apply the test intervention. For bioelectronics, this could involve conditioning media with material extracts or particles. For biochemical studies, transfert with siRNA (e.g., 100 nM siPFKFB4 or siHMOX1 using Lipofectamine RNAiMAX) or add chemotherapeutic agents like doxorubicin (DOX) across a concentration range (e.g., 0.025–12.5 µM) [81].
- MTT Incubation: After the treatment period (e.g., 72 hours), add MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) to each well. Incubate for 2–4 hours to allow formazan crystal formation by metabolically active cells [81].
- Solubilization and Measurement: Carefully remove the medium and dissolve the formed formazan crystals in a suitable solvent (e.g., DMSO). Measure the absorbance of the solution at 570 nm using a microplate reader [81].
- Data Analysis: Calculate cell viability as a percentage relative to untreated control wells. Determine half-maximal inhibitory concentration (ICâ‚…â‚€) values using non-linear regression analysis in software such as GraphPad Prism [81].
Key Applications in Bioelectronics: This assay can validate that novel elastomeric organic transistors or materials like vulcanized blends of DPPT-TT and BIIR do not release cytotoxic compounds, ensuring they meet biocompatibility standards for implantable devices [8].
Cell Proliferation Measurement
Proliferation assays track population expansion over time, distinguishing between increased cell division and mere survival.
Trypan Blue Exclusion Method Protocol:
- Cell Harvesting: At designated time points, detach adherent cells using a standard trypsin/EDTA solution.
- Staining: Mix the cell suspension 1:1 with a trypan blue solution.
- Counting: Load a small volume of the mixture onto a hemocytometer. Count unstained (viable) and blue-stained (non-viable) cells under a microscope. Cell viability is calculated as the percentage of viable cells relative to the total cell count [81].
This method is often used to establish baseline health and growth rates of cell lines before more complex assays, ensuring that any observed effects in migration or gene expression studies are interpreted in the context of a stable proliferating population [80].
Cell Migration and Invasion Evaluation
The ability of cells to migrate is a critical functional output, relevant for evaluating anti-metastatic cancer therapies and ensuring that bioelectronic implants do not inadvertently promote undesirable cell movement.
Detailed Wound Healing (Scratch) Assay Protocol:
- Cell Seeding: Seed cells in a culture vessel (e.g., 6-well plate) at a high density to form a confluent monolayer.
- Wound Creation: Use a sterile pipette tip to scratch a straight line through the monolayer, creating a "wound."
- Wash and Imaging: Gently wash away dislodged cells and add fresh medium. Capture images of the wound at regular intervals (e.g., 0, 24, 48 hours) using a microscope.
- Quantification: Measure the change in the width of the cell-free area over time using image analysis software (e.g., ImageJ). Express migration as percentage wound closure relative to the initial wound area [82] [81] [80].
Key Findings: Studies using this method have shown that exercise-induced extracellular vesicles (HIIE-EVs) can reduce HT-29 colon cancer cell migration by 39%, and siPFKFB4/DOX combination therapy can inhibit U-87 MG glioblastoma cell migration by 65% [82] [81].
Table 1: Summary of Cytotoxic and Anti-Migratory Effects from Recent Studies
| Cell Line | Intervention | Key Outcome on Viability/Proliferation | Key Outcome on Migration | Source |
|---|---|---|---|---|
| HT-29 Colon Cancer | PRE Serum EVs | 35% reduction in viability vs. PBS | 27% reduction in migration | [82] |
| HT-29 Colon Cancer | HIIE Serum EVs | 47% reduction in viability vs. PBS | 39% reduction in migration | [82] |
| U-87 MG Glioblastoma | siPFKFB4 + DOX | 6-fold reduction in DOX ICâ‚…â‚€ | 65% reduction in migration | [81] |
| U-87 MG Glioblastoma | siHMOX1 + DOX | 2-fold reduction in DOX ICâ‚…â‚€ | 75% reduction in migration | [81] |
| 8505C ATC | hDPSC-EVs | No impact on proliferation | Selective inhibition of migration | [80] |
Table 2: Apoptotic Markers Modulated by Experimental Treatments
| Treatment | Cell Line | Upregulated Markers | Downregulated Markers | Source |
|---|---|---|---|---|
| HIIE-EVs | HT-29 | Bax/Bcl-2 ratio (+56%), Caspase-3 (+30%) | - | [82] |
| siPFKFB4 + DOX | U-87 MG | DPYSL4 | BCL-2, PARP2 | [81] |
| siHMOX1 + DOX | U-87 MG | CYLD, FAS, CASP3 | - | [81] |
| hDPSC-EVs | 8505C ATC | 16 genes (e.g., immune-related) | 8 genes (e.g., FN1) | [80] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for In Vitro Assessment
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| MTT Assay Kit | Measures cell metabolic activity as a proxy for viability. | Quantifying cytotoxicity of chemotherapeutics or material extracts [81]. |
| Lipofectamine RNAiMAX | Transfection reagent for introducing siRNA into cells. | Silencing specific genes (e.g., PFKFB4, HMOX1) to study their function [81]. |
| Small Interfering RNA (siRNA) | Selectively knocks down expression of a target gene. | Investigating the role of specific genes in proliferation and migration [81]. |
| Extracellular Vesicles (EVs) | Natural nanocarriers for intercellular communication. | Studying the effects of exercise or stem cell paracrine signaling on cancer cells [82] [80]. |
| Doxorubicin (DOX) | A broad-spectrum chemotherapeutic agent. | Used as a standard cytotoxic agent in combination therapy studies [81]. |
| Temozolomide (TMZ) | An alkylating chemotherapeutic agent. | Standard of care for glioblastoma; used to test for chemosensitization [81]. |
| Biocompatible Elastomers (e.g., BIIR) | Flexible, stretchable substrate for implantable electronics. | Creating bioelectronic devices with mechanical properties matching human tissue [8]. |
Visualizing Experimental Workflows and Signaling Pathways
In Vitro Assessment Workflow
Apoptotic Signaling Pathway
Integration with Organic Bioelectronics Biocompatibility Research
The in vitro methodologies detailed above form the foundation of the safety and efficacy evaluation pipeline for organic bioelectronic devices. For instance, before implantable elastomeric OFETs—fabricated from blends like DPPT-TT and the medical-grade rubber BIIR—can progress to in vivo models, they must be rigorously assessed using these very techniques [8]. The core principle is biocompatibility, defined as the ability of a material to perform with an appropriate host response in a specific application. In vitro assessments directly test this by evaluating whether device materials or their leachates adversely affect cell viability, provoke uncontrolled proliferation, or stimulate aberrant migration.
Advanced bioelectronic systems aim to seamlessly integrate with human tissue, requiring not only electrical functionality but also mechanical compatibility, with Young's moduli matching those of biological tissues like the brain and skin [16]. Furthermore, the emergence of extracellular vesicles as therapeutic agents and communication vectors highlights a parallel frontier in bioelectronic integration, where EV-based signaling could be harnessed to direct tissue responses around implanted devices [82] [80]. By applying standardized, quantitative in vitro assessments, researchers can deconstruct these complex bio-interactions, laying a robust preclinical foundation for the next generation of biointegrated technologies.
The long-term functional stability of implantable bioelectronic devices is predominantly governed by the host organism's immune response following implantation. The foreign body response (FBR), a immune-mediated reaction to synthetic materials, poses the most significant challenge, often leading to the encapsulation of implants in dense collagenous tissue, increased interface impedance, and ultimate device failure [83]. Within the broader context of organic bioelectronics biocompatibility research, achieving seamless integration requires electronic materials that conform mechanically and interact benignly with the immune system. This guide details recent advances in the design and evaluation of immune-compatible semiconducting polymers, providing a technical roadmap for assessing their in vivo performance and histological outcomes through rigorous long-term implantation studies.
Molecular Design Strategies for Immune Compatibility
The core hypothesis driving recent material design is that incorporating specific immunomodulatory moieties directly into the molecular structure of semiconducting polymers can intrinsically mitigate the FBR.
Backbone Engineering with Selenophene
Replacing a thiophene unit in a high-performance polymer backbone with selenophene serves a dual purpose. Drawing from immunology studies, the selenium-containing structure possesses antioxidant properties, potentially scavenging reactive oxygen species (ROS) that contribute to macrophage activation and inflammation. From an electronics perspective, this substitution maintains, or can even enhance, charge transport capabilities, making it an ideal strategy for bioelectronic applications [83].
Side-Chain Functionalization with Immunomodulatory Groups
Side chains offer a versatile platform for introducing sophisticated immunomodulatory chemical groups without disrupting the conjugated backbone responsible for electrical conduction. Two groups have shown significant efficacy:
- Triazole-tetrahydropyran (THP)
- Triazole-thiomorpholine 1,1-dioxide (TMO)
These groups are incorporated at the terminus of the polymer's side chains using efficient conjugation chemistry, such as the "click-to-polymer" (CLIP) method, achieving near-quantitative attachment ratios [83].
Base Polymer and Model System
These design strategies are effectively demonstrated using a base polymer structure of poly(3,3’-bis(2-(2-(2-methoxyethoxy)ethoxy)ethoxy)-2,2’:5’,2â€-terthiophene) (p(g2T-T)), a material known for its state-of-the-art performance in organic electrochemical transistors (OECTs). The resulting engineered polymers are p(g2T-Se) (selenophene backbone), and its side-chain functionalized derivatives, p(g2T-Se)-THP and p(g2T-Se)-TMO [83].
Figure 1: Foreign Body Response Cascade and Immunomodulatory Intervention Points. The native FBR progression (red) leads to device failure. Molecular design strategies (blue) intervene to suppress key inflammatory stages, improving outcomes (green).
Experimental Protocols for In Vivo Evaluation
A comprehensive assessment of immune compatibility requires a multi-faceted experimental approach, combining in vivo implantation with ex vivo histological and molecular analyses.
In Vivo Implantation Model
- Animal Model: Female C57BL/6J mice (8-10 weeks old).
- Implantation Procedure: Polymer films (e.g., p(g2T-T), p(g2T-Se), p(g2T-Se)-THP, p(g2T-Se)-TMO) are fabricated as thin films supported by thin circular SEBS substrates and implanted subcutaneously in the dorsal region.
- Study Duration: Implants are explained after two key endpoints: 1 week (for acute inflammatory response) and 4 weeks (for chronic FBR and fully developed fibrotic capsule formation) [83].
Histological and Immunofluorescence Analysis
- Masson’s Trichrome (MT) Staining: Used to visualize and quantify collagen deposition (fibrosis) around the explanted polymer films. The collagen density is quantified as the percentage of blue pixels in the tissue area immediately surrounding the implant.
- Immunofluorescence Staining: Enables specific cell population quantification.
- Macrophages: Stained with anti-CD68 antibodies.
- Myofibroblasts: Stained with anti-α-smooth muscle actin (α-SMA) antibodies.
- Cell populations are quantified from multiple high-power fields per sample [83].
Molecular Biology Techniques
- Quantitative Polymerase Chain Reaction (qPCR): Performed on RNA extracted from the peri-implant tissue to quantify mRNA expression levels of:
- Collagen Type I and III: Key structural components of the fibrotic capsule.
- Inflammatory Biomarkers: A panel of pro- and anti-inflammatory cytokines and chemokines (e.g., CCR7, IFN-γ, GM-CSF, MCP-1, IL-6, IL-1β, IL-10, IL-4) [83].
- Cytokine Assays: Multiplex immunoassays (e.g., Luminex) quantify protein levels of key inflammatory mediators in the tissue homogenates.
Figure 2: Experimental Workflow for Evaluating Polymer Biocompatibility. The process spans from material preparation through in vivo implantation to multi-modal post-explantation analysis.
Quantitative Results and Data Analysis
Rigorous quantification is critical for evaluating the efficacy of immune-compatible designs. The data below summarize key findings from a four-week implantation study.
Table 1: Quantification of Fibrotic Encapsulation and Key Cell Populations After 4-Week Implantation
| Polymer | Collagen Density (%) | Reduction vs. Control | Macrophages (CD68+) | Myofibroblasts (α-SMA+) |
|---|---|---|---|---|
| p(g2T-T) (Control) | ~25% | — | Baseline | Baseline |
| p(g2T-Se) | ~13% | ~50% | Reduced | Reduced |
| p(g2T-Se)-THP | ~8.5% | ~65% | Significantly Reduced | Significantly Reduced |
| p(g2T-Se)-TMO | ~8.0% | ~68% | ~68% Reduction | ~79% Reduction |
Source: Adapted from [83]. Collagen density measured via Masson's Trichrome staining; cell populations quantified via immunofluorescence.
Table 2: Expression Levels of Inflammatory Biomarkers in Peri-Implant Tissue
| Biomarker | Function | p(g2T-T) (Control) | p(g2T-Se) | p(g2T-Se)-TMO |
|---|---|---|---|---|
| CCR7 | Pro-inflammatory, M1 macrophage | Baseline | Downregulated | Strongly Downregulated |
| IFN-γ | Pro-inflammatory cytokine | Baseline | Downregulated | Strongly Downregulated |
| GM-CSF | Myeloid cell activation | Baseline | Downregulated | Strongly Downregulated |
| MCP-1 | Monocyte recruitment | Baseline | Downregulated | Strongly Downregulated |
| IL-6, IL-1β | Pro-inflammatory cytokines | Baseline | Downregulated | Strongly Downregulated |
| IL-10 | Anti-inflammatory cytokine | Baseline | Upregulated | Upregulated |
| IL-4 | Anti-inflammatory, M2 macrophage | Baseline | Upregulated | Upregulated |
Source: Adapted from [83]. Data based on qPCR and cytokine protein assays. "Downregulated/Upregulated" indicates a statistically significant change relative to the control polymer.
The data demonstrate a clear trend: both backbone and side-chain engineering contribute significantly to suppressing the FBR. The most effective polymer, p(g2T-Se)-TMO, achieved a remarkable ~68% reduction in collagen density and a ~79% reduction in myofibroblast population compared to the control. Molecular analysis confirms a shift in the immune response from a pro-inflammatory (M1) to a more pro-healing, anti-inflammatory (M2) state [83].
The Scientist's Toolkit: Essential Research Reagents and Materials
This section catalogs the key materials and reagents central to conducting this research, as identified in the cited studies.
Table 3: Key Research Reagents and Materials for Immune-Compatible Organic Bioelectronics
| Item | Function / Description | Example / Specification |
|---|---|---|
| Base Semiconducting Polymer | High-performance OECT material; serves as the scaffold for modification. | p(g2T-T) [83] |
| Selenophene Monomer | Backbone immunomodulatory unit; replaces thiophene to confer antioxidant properties. | N/A [83] |
| Immunomodulatory Side Chains | Chemical groups attached to side chains to downregulate inflammatory biomarkers. | THP (Triazole-tetrahydropyran) and TMO (Triazole-thiomorpholine 1,1-dioxide) [83] |
| Biocompatible Elastomer | Medical-grade rubber matrix for creating soft, stretchable semiconductor composites. | Bromo isobutyl–isoprene rubber (BIIR) [8] |
| Semiconductor for Stretchable Blends | Donor-acceptor polymer for imparting electrical properties to elastomer blends. | DPPT-TT [8] |
| Substrate Material | Support for polymer films during in vivo testing. | SEBS (Styrene-ethylene-butylene-styrene) [83] |
| Primary Antibodies (IF) | For identifying specific cell types in tissue sections. | Anti-CD68 (macrophages), Anti-α-SMA (myofibroblasts) [83] |
| qPCR Assays | For quantifying gene expression of collagen and cytokines. | Assays for Collagen I, Collagen III, CCR7, IFN-γ, IL-6, IL-10, etc. [83] |
The integration of immunomodulatory molecular design represents a paradigm shift in the development of organic bioelectronics. Moving beyond inertness, these materials actively engage with the biological environment to promote tolerance. The presented data unequivocally show that rational design—incorporating selenophene in the backbone and THP/TMO groups on the side chains—can suppress the FBR by up to 68% while preserving electrical performance (charge-carrier mobility ~1 cm²Vâ»Â¹sâ»Â¹) [83].
These findings must be viewed within the broader thesis of biocompatibility research, which also encompasses the use of intrinsically biocompatible elastomers like BIIR to achieve mechanical compatibility with tissues, further minimizing inflammatory responses [8]. The convergence of immune-compatible molecular design and tissue-like mechanical properties is the cornerstone for the next generation of chronically stable, implantable bioelectronic devices for neural interfaces, wearable monitors, and advanced drug delivery systems. Future work will focus on expanding the library of immunomodulatory motifs, understanding long-term degradation products, and translating these material design principles into complex, multifunctional bioelectronic implants.
The advancement of organic bioelectronics is intrinsically linked to the development of polymer-based devices, where the critical choice between rigid and soft or synthetic and natural materials directly dictates performance and biocompatibility. This review provides a structured, technical analysis of these material classes, framing them within the context of implantable and wearable bioelectronic applications. A fundamental challenge in bioelectronics is the mechanical mismatch at the tissue-device interface; traditional rigid electronics can cause inflammation and tissue damage, while emerging soft electronics aim to replicate the mechanical properties of biological tissues for seamless integration [8] [16]. This analysis quantitatively compares the performance benchmarks of these divergent material strategies, providing researchers and drug development professionals with clear protocols and data to guide the selection and development of polymers for next-generation biomedical devices.
Material Properties and Performance Benchmarks
The performance of polymer devices in bioelectronic applications is governed by a set of key physical, electrical, and biological properties. The selection between rigid and soft, or synthetic and natural polymers, involves trade-offs between mechanical strength, electrical performance, and biocompatibility.
Quantitative Comparison of Rigid vs. Soft Polymers
Table 1: Performance Benchmarks of Rigid vs. Soft Polymers for Bioelectronics
| Performance Characteristic | Rigid Polymers (e.g., PEEK, PS, PMMA) | Soft/Elastomeric Polymers (e.g., BIIR, PDMS, PU) | Test Method / Context |
|---|---|---|---|
| Young's Modulus | GPa range (several orders higher than tissue) [16] | ~107.7 to 108.8 Pa (similar to skin tissue) [8] | Atomic Force Microscopy (AFM), DMT Modulus mapping [8] |
| Strain at Failure | Low (< 5%), prone to cracking [8] | High (up to 100% strain without cracking) [8] | Uniaxial tensile testing, optical microscopy under strain [8] |
| Field-Effect Mobility | Generally high on rigid substrates | Retained performance under strain (e.g., stable operation at 50-100% strain) [8] | Field-effect transistor characterization [8] |
| Biocompatibility (Foreign Body Response) | Higher risk of inflammation, tissue damage, fibrotic encapsulation [8] [16] | Significantly reduced inflammatory response; "no major inflammatory response or tissue damage" in vivo [8] | In vitro cell viability/proliferation assays; in vivo implantation studies (e.g., in mice) [8] |
| Primary Application in Bioelectronics | Structural implants, non-degradable devices [84] | Skin-like implants, wearable sensors, neural interfaces [8] [16] |
Quantitative Comparison of Synthetic vs. Natural Polymers
Table 2: Performance Benchmarks of Synthetic vs. Natural Polymers for Bioelectronics and Biomaterials
| Performance Characteristic | Synthetic Polymers (e.g., PVC, PTFE, PEEK, PLGA) | Natural Polymers (e.g., Collagen, Chitosan, Alginate) | Test Method / Context |
|---|---|---|---|
| Tensile Strength | High (e.g., for medical devices and implants) [84] | Superior in certain natural polymers (e.g., for packaging) [85] | Universal tensile testing machine |
| Elongation at Break | Significant advantages (e.g., for packaging) [85] | Lower compared to synthetics [85] | Universal tensile testing machine |
| Oxygen Barrier Properties | Variable | Superior in certain natural polymers (e.g., for packaging) [85] | Permeability analysis |
| Biodegradability | Typically non-biodegradable (exceptions: PLGA, PCL) [86] | High biodegradability and composability [85] | Enzymatic or soil burial tests; according to standards like EN 17033 [85] |
| Toxicity & Biocompatibility | Risk of chronic foreign body reactions; may leach toxic byproducts [8] [85] | Generally low toxicity and high biocompatibility [84] | ISO 10993 biocompatibility standards; in vitro and in vivo assessments [8] |
| Primary Application in Biomedicine | Medical devices, drug delivery systems, surgical implants [84] | Regenerative medicine, tissue engineering, wound healing [84] [86] | |
| Production Scalability & Cost | Mature technology, cost-effective mass production [85] | Challenges in production scalability and higher costs [85] |
Experimental Protocols for Key Methodologies
To ensure the reproducibility of performance benchmarks, detailed protocols for key experiments are provided below. These methodologies are critical for characterizing the properties outlined in the previous section.
Protocol for Fabricating a Biocompatible, Stretchable Organic Field-Effect Transistor (sOFET)
This protocol is adapted from the seminal work published in Nature Electronics [8], which reported an elastomeric OFET with stable performance under 50% strain and minimal inflammatory response in vivo.
Material Synthesis and Formulation:
- Prepare a blend solution of the semiconducting polymer and the medical-grade elastomer. The cited study used a weight ratio of 3:7 of DPPT-TT (a conjugated polymer) to Bromo Isobutyl–Isoprene Rubber (BIIR).
- Add vulcanizing agents to the solution: sulfur acts as a crosslinker, Dipentamethylenethiuram Tetrasulfide (DPTT) as an accelerator, and stearic acid as an initiator.
Film Vulcanization and Cross-linking:
- Deposit the blend solution onto a substrate via spin-coating or a similar technique to form a thin film.
- Initiate the vulcanization process by heating the film. This process chemically crosslinks the BIIR elastomer matrix, enhancing its mechanical elasticity. The reaction proceeds through:
- Initiation: Radical formation facilitated by the breakdown of C–Br bonds in BIIR, confirmed via Fourier Transform Infrared (FTIR) spectroscopy by monitoring the reduction of the C–Br peak at 667 cmâ»Â¹.
- Propagation: Crosslinking of BIIR chains with sulfur, indicated by a reduction in the C=C peak (at 1538 cmâ»Â¹) in neat BIIR via FTIR.
- Termination: The reaction concludes, resulting in a robust, elastic network. The vulcanization process should preserve the conjugated structure of the semiconductor, as verified by unchanged UV-visible absorption spectra.
Morphological and Mechanical Verification:
- Use Atomic Force Microscopy (AFM) and Conductive-AFM (C-AFM) to confirm the formation of an interconnected semiconducting nanofibre network within the elastomer matrix.
- Perform DMT modulus mapping to verify the increased modulus and uniformity post-vulcanization. The Young's modulus should match that of human tissues (in the range of ~10⸠Pa).
Electrode Patterning for Biostability:
- Pattern stretchable electrodes using a dual-layer metallization technique. First, deposit a layer of Silver (Ag) for excellent electrical contact. Then, deposit a top layer of Gold (Au) to provide a robust, corrosion-resistant barrier against biofluids. X-ray Photoelectron Spectroscopy (XPS) depth profiling can confirm the layered structure and integrity.
Electrical Characterization Under Strain:
- Fabricate transistors and logic circuits (e.g., inverters, NOR, NAND gates) on a stretchable substrate.
- Use a custom or commercial strain stage to measure key electrical parameters (field-effect mobility, ON/OFF current ratio, threshold voltage) while applying uniaxial strain from 0% to 100%.
- Perform cyclic stretching tests (e.g., 1,000 cycles at 100% strain) to assess mechanical durability and electrical performance stability.
Protocol for Assessing Biocompatibility of Polymer Films
This protocol outlines the standard in vitro and in vivo assessments used to evaluate polymer biocompatibility, as critical for regulatory approval (e.g., ISO 10993) [8] [86].
In Vitro Cell Viability and Proliferation Assay:
- Cell Culture: Seed relevant cell lines, such as Human Dermal Fibroblasts (HDFs) and macrophages, onto sterilized samples of the polymer film. Include a control group cultured on a standard tissue culture plate.
- Viability Assay: After a predetermined incubation period (e.g., 24-72 hours), expose the cells to a viability indicator like AlamarBlue or MTT. These assays measure metabolic activity, which is a proxy for cell health and proliferation.
- Data Analysis: Quantify fluorescence or absorbance and compare to the control. A biocompatible film will show no significant adverse effect on cell viability or proliferation. Furthermore, use microscopy to inspect cell morphology and adhesion on the film surface.
In Vitro Cell Migration Assay:
- Perform a scratch assay or use a transwell migration chamber with the polymer film extract or the film itself placed in the migration path.
- Monitor the rate at which cells migrate into the wounded area or through the membrane. A biocompatible material should not inhibit normal cell migration processes.
In Vivo Implantation and Histological Analysis:
- Implantation: Surgically implant the sterilized polymer device (e.g., a transistor film) into an animal model, such as a mouse, typically in a subcutaneous pocket.
- Explanation and Fixation: After a set period (e.g., several weeks), euthanize the animal and excise the implant along with the surrounding tissue.
- Tissue Processing and Staining: Fix the tissue, embed it in paraffin, section it into thin slices, and mount them on slides. Stain the sections with Hematoxylin and Eosin (H&E) to visualize general tissue structure and inflammation. Staining for specific immune markers (e.g., via immunohistochemistry for CD68 to identify macrophages) can provide a more detailed analysis of the immune response.
- Histopathological Evaluation: A pathologist should examine the stained tissue sections under a microscope for key indicators of the foreign body response, including:
- Degree of inflammatory cell infiltration (neutrophils, lymphocytes, macrophages).
- Presence of giant cells.
- Thickness of fibrous capsule formation around the implant.
- A highly biocompatible material, like the BIIR-based sOFET, will show "no major inflammatory response or tissue damage" compared to control [8].
Visualization of Experimental Workflows and Material Properties
To elucidate the logical relationships and workflows described in the experimental protocols and material comparisons, the following diagrams were generated using Graphviz DOT language.
Diagram 1: This workflow outlines the key steps for fabricating and validating a stretchable, biocompatible organic field-effect transistor (sOFET), from material preparation to final performance evaluation.
Diagram 2: This decision tree provides a logical framework for selecting the appropriate polymer class based on the key requirements of a specific bioelectronic application.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Bioelectronic Polymer Development
| Reagent / Material | Function / Role in Research | Example Use-Case / Rationale |
|---|---|---|
| BIIR (Bromo Isobutyl–Isoprene Rubber) | A medical-grade, biocompatible elastomer used as the matrix for stretchable semiconductors. | Primary elastomer in the cited sOFET [8]; provides intrinsic stretchability and meets ISO 10993 biocompatibility standards. |
| DPPT-TT (Conjugated Polymer) | A high-performance semiconducting polymer providing the charge transport pathway. | Forms an interconnected nanofibre network within the BIIR matrix, enabling high field-effect mobility even under strain [8]. |
| Vulcanization Kit (S, DPTTT, Stearic Acid) | A chemical package to crosslink the elastomer matrix, enhancing mechanical robustness and elasticity. | Critical for creating the durable, stretchable network in BIIR-based devices without disrupting the semiconductor's conjugation [8]. |
| Ag/Au Dual-Layer Metallization | A strategy for creating stretchable and biofluid-corrosion-resistant electrodes. | Ag provides excellent conductivity, while Au offers a bio-inert, corrosion-resistant outer layer, ensuring stable electrode performance in physiological environments [8]. |
| PEDOT:PSS | A conductive polymer with mixed ionic-electronic conduction, ideal for interfacing with biological systems. | Commonly used in Organic Electrochemical Transistors (OECTs) for sensitive biosensing and neural interfacing due to its biocompatibility and efficient ion-to-electron transduction [16]. |
| PEEK (Polyetheretherketone) | A high-strength, rigid synthetic polymer for load-bearing implants. | Used in orthopedic and spinal implants due to its excellent mechanical strength, chemical resistance, and biostability [84]. |
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable synthetic polymer for temporary implants and drug delivery. | Serves as a resorbable scaffold in tissue engineering and a controlled-release vehicle for pharmaceuticals, hydrolyzing into metabolizable acids [86]. |
| Chitosan | A natural biopolymer derived from chitin, known for its biocompatibility and biodegradability. | Applied in wound healing, tissue engineering scaffolds, and drug delivery systems due to its low toxicity, antimicrobial properties, and ability to form gels and films [84] [85]. |
The comparative analysis presented herein underscores that the dichotomy between rigid and soft polymers is not a simple question of superiority but one of application-specific suitability. The quantitative data and protocols confirm that soft, elastomeric materials like BIIR are unparalleled for creating mechanically compliant interfaces with biological tissues, a critical factor for long-term implantable bioelectronics such as neural interfaces and continuous health monitors. Conversely, rigid polymers like PEEK remain indispensable where high structural integrity and durability are paramount. Similarly, the choice between synthetic and natural polymers involves a fundamental trade-off between the robust, tunable mechanical properties and scalable manufacturing of synthetics, and the superior biocompatibility, biodegradability, and low environmental impact of natural polymers. The future of organic bioelectronics lies in the continued refinement of these material classes and, more importantly, in the development of sophisticated hybrid and block-copolymerized systems that strategically combine the advantages of each to overcome the inherent limitations of individual components. This will pave the way for a new generation of smart, adaptive, and fully integrated bioelectronic devices for advanced healthcare.
The evolution of organic bioelectronics is paving the way for a new generation of medical devices that seamlessly integrate with biological systems for long-term diagnostics and therapeutics. Unlike traditional rigid implants, these devices leverage carbon-based semiconducting materials, such as conductive polymers, which offer inherent flexibility, biocompatibility, and the capacity to carry both ionic and electronic impulses [3]. The core value proposition of these technologies—continuous, real-time physiological monitoring and modulation—is entirely dependent on their ability to maintain stable performance over weeks or months of uninterrupted operation. This chronic stability rests on two interdependent pillars: signal fidelity, the consistent and accurate acquisition of high-quality biological signals, and functional longevity, the reliable operation of the device itself within the dynamic and demanding environment of the body [87]. The mechanical mismatch between conventional electronics and soft tissues can lead to inflammation, fibrosis, and device failure, ultimately degrading signal quality over time [1] [8]. Therefore, within the context of biocompatibility research, evaluating these metrics is not merely about device durability but about ensuring the efficacy and safety of the biointerface throughout its intended operational lifespan. This guide details the critical metrics and methodologies for quantifying the performance and longevity of organic bioelectronic devices destined for chronic use.
Core Metrics for Performance Evaluation
The evaluation of chronic device performance requires a multi-faceted approach, assessing electrical, mechanical, and biological domains. The following metrics are essential for a comprehensive understanding of device behavior under physiological conditions.
Signal Fidelity Metrics
Signal fidelity pertains to the quality and reliability of the data acquired from the biological system.
- Signal-to-Noise Ratio (SNR): A fundamental metric for the clarity of the recorded signal. For neural applications, a high SNR is critical for resolving low-amplitude action potentials (typically tens to hundreds of microvolts) from background noise [88]. Amplification techniques, such as those using Organic Electrochemical Transistors (OECTs), have been shown to improve SNR by amplifying weak bioelectronic signals while reducing background noise [89].
- Stability of Electrical Performance: This involves monitoring key electrical parameters over time and under strain. For transistors, this includes field-effect mobility and ON/OFF ratio. Research on elastomeric organic field-effect transistors has demonstrated stable field-effect mobility with negligible changes even under 50% strain and after 1,000 stretching cycles at 100% strain, which is crucial for implantable applications [8].
- Temporal Signal Stability: The consistency of signal acquisition over extended periods, which can be compromised by factors such as biofilm formation, material degradation, or fibrotic encapsulation [1].
- Spatial Resolution: The ability to distinguish signals from neighboring sources. High-density microelectrode arrays with thousands of channels place significant demands on data handling but offer superior spatial resolution for mapping neural activity [88].
Functional Longevity Metrics
Functional longevity assesses the physical and operational durability of the device itself.
- Device Lifespan: The total operational time under physiological conditions. The goal for next-generation wearables and implants is continuous operation over weeks or months, a target limited by power supply, material durability, and biofouling [87].
- Mechanical Durability: The ability to withstand repeated mechanical stress. This is quantified by performance retention after thousands of cycles of bending, stretching, or twisting. Fiber-based electronic devices (FEDs), for instance, must endure cyclic tensile, compressive, or bending strains without developing microcracks that lead to electrical failure [90].
- Biocompatibility and Foreign Body Response (FBR): A critical biological metric. A successful device minimizes chronic inflammation, fibrosis, and tissue damage. In vivo implantation studies are essential, with outcomes assessed through histology to evaluate inflammatory response and tissue integration [8]. The Young's modulus of the device material should match that of the target tissue (e.g., kPa range for brain and peripheral nerves) to reduce mechanical mismatch [3].
- Power Efficiency and Operational Stability: For chronically implanted devices, power management is paramount. This includes both low-power operation and stable performance under the device's power budget, which is often restricted in wireless implants [88].
Table 1: Key Metrics for Evaluating Chronic Device Performance
| Domain | Metric | Definition | Target Value/Observation |
|---|---|---|---|
| Signal Fidelity | Signal-to-Noise Ratio (SNR) | Ratio of desired signal power to background noise power | High enough to resolve low-amplitude signals (e.g., neural spikes) [88]. |
| \hspace{20pt} Electrical Performance | Stability of key parameters (e.g., mobility, ON/OFF ratio) | Negligible change in mobility under 50% strain and after 1,000 stretch cycles [8]. | |
| \hspace{20pt} Temporal Stability | Consistency of signal acquisition over time | Uninterrupted, high-fidelity data streams over weeks [87]. | |
| Functional Longevity | Device Lifespan | Total operational time in physiological conditions | Weeks to months of continuous operation [87]. |
| \hspace{20pt} Mechanical Durability | Performance retention after repeated mechanical stress | Stable electrical function after 1,000+ deformation cycles [8] [90]. | |
| \hspace{20pt} Biocompatibility (FBR) | Level of chronic inflammatory or fibrotic response | No major inflammatory response or tissue damage in vivo [8]. | |
| \hspace{20pt} Power Efficiency | Power consumption during operation | Low-power operation suitable for wireless, battery-powered implants [88]. |
Advanced Data Handling Metrics
For high-density devices, data management itself becomes a critical component of system performance.
- Data Compression Ratio: The efficiency of on-implant algorithms in reducing data volume before transmission. This is vital for managing the massive data streams from high-channel-count neural interfaces to overcome wireless bandwidth limitations [88].
- Computational Efficiency: The power and hardware resources required for on-device signal processing. Techniques must be low-complexity to be implemented within the strict power and size constraints of an implant [88].
- On-Device vs. Cloud-Based Analysis Trade-off: The choice between local processing (low power, limited complexity) and cloud transmission (high computational power, higher data rate needs) impacts system architecture and power budget [87].
Table 2: Data Handling and Communication Metrics for High-Density Implants
| Parameter | Challenge | Considerations & Technologies |
|---|---|---|
| Data Volume | Handling massive data from high-density arrays (e.g., >1000 channels) [88] | On-implant signal processing (spike detection, compression) is essential to reduce telemetry load [88]. |
| Wireless Data Telemetry | Limited bandwidth and power for data transmission [88] | RF, UWB, and ultrasonic links offer different trade-offs in bit rate and communication range [88]. |
| Communication Protocols (Wearables) | Balancing data rate, range, and power [87] | BLE: High data rate (~1.3 Mbps) but proximity-dependent. LoRa: Long-range, very low power, but low data rate (0.3-100 kbps) [87]. |
Experimental Protocols for Metric Validation
Rigorous and standardized experimental protocols are required to reliably quantify the metrics defined above.
In Vitro Characterization of Electrical and Mechanical Stability
Objective: To evaluate the baseline electrical performance and resilience of a device to mechanical deformation. Methodology:
- Electrical Characterization: Using a semiconductor parameter analyzer, measure transfer and output characteristics to extract field-effect mobility, threshold voltage, and ON/OFF ratio in a physiological solution (e.g., phosphate-buffered saline) at 37°C [8].
- Mechanical Strain Testing: Mount the device on a programmable tensile stage. Measure electrical parameters (e.g., mobility, conductivity) in situ while applying uniaxial strain. The strain should be increased incrementally (e.g., to 50%) to determine the crack-onset point [8].
- Cyclic Fatigue Testing: Subject the device to thousands of cycles of repetitive stretching (e.g., at 100% strain). Monitor electrical performance at regular intervals to track degradation and identify failure mechanisms [8] [90].
- Stability in Biofluids: Immerse the device in a simulated biological fluid at 37°C while continuously or intermittently monitoring key electrical parameters over days or weeks to assess long-term stability and corrosion resistance [8].
Biocompatibility and In Vivo Integration Assessment
Objective: To determine the biological safety of the device and the quality of the tissue-device interface over time. Methodology:
- In Vitro Biocompatibility: Following ISO 10993 standards, culture relevant cells (e.g., human dermal fibroblasts, macrophages) with device materials or extracts. Assess cell viability, proliferation, and migration to ensure no adverse effects [8].
- In Vivo Implantation: Surgically implant the device in an appropriate animal model (e.g., mice, rats). Include a control group with a sham surgery [8].
- Functional Monitoring: For the implant duration, periodically measure the device's signal fidelity (e.g., SNR, signal amplitude) to correlate performance with the biological response [1].
- Histological Analysis: After a predetermined period (e.g., 4, 12 weeks), euthanize the animal and harvest the implant site. Process the tissue for histological sectioning and staining (e.g., H&E for general morphology, antibodies for immune cell markers). Quantify the thickness of the fibrotic capsule and the density of inflammatory cells at the interface compared to controls [8].
Protocol for On-Implant Neural Signal Processing
Objective: To validate the efficiency and accuracy of data reduction algorithms for high-density neural recording. Methodology:
- Signal Acquisition: Record neural data using the implantable device, typically bandpass-filtered (e.g., 300 Hz - 6 kHz for spikes) and sampled at a high rate (e.g., 20-30 kSps) [88].
- Algorithm Implementation: Implement signal processing algorithms (e.g., spike detection, compression, spike sorting) on the implant's hardware or a hardware-emulated environment.
- Performance Benchmarking:
- Spike Detection: Compare the algorithm's detected spikes against a manually curated ground truth to calculate accuracy, precision, and recall.
- Data Compression: Calculate the compression ratio and then reconstruct the signal off-implant. Compare the reconstructed signal to the original using a metric like normalized root-mean-square error to quantify information loss [88].
- Spike Sorting: Assess the clustering accuracy to ensure different neurons can be reliably distinguished post-processing [88].
- Hardware Efficiency: Measure the power consumption and computational latency of the algorithm during operation to ensure it meets the implant's strict constraints [88].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and testing of chronic organic bioelectronics rely on a specific set of materials and functional components.
Table 3: Essential Research Materials for Organic Bioelectronics
| Category | Material/Component | Function & Rationale |
|---|---|---|
| Semiconducting Polymers | Poly[(dithiophene)-alt-(2,5-bis(2-octyldodecyl)-3,6-bis(thienyl)-diketopyrrolopyrrole)] (DPPT-TT) | Acts as the active semiconducting material in stretchable transistors, forming a nanofibre network for charge transport [8]. |
| \hspace{20pt} Conductive Polymers | PEDOT:PSS, Polyaniline (PANI) | Used for electrodes and interfaces; offer mixed ionic-electronic conduction, flexibility, and biocompatibility for seamless biointegration [3]. |
| Biocompatible Elastomers | Bromo Isobutyl–Isoprene Rubber (BIIR) | A medical-grade elastomer used as a matrix to impart stretchability and biocompatibility, meeting ISO 10993 standards [8]. |
| \hspace{20pt} Other Elastomers | Polydimethylsiloxane (PDMS), Polyurethane (PU) | Common soft substrates and encapsulation materials with tunable mechanical properties [3]. |
| Stretchable Conductors | Silver (Ag) / Gold (Au) dual-layer metallization | Provides conductive, stretchable, and corrosion-resistant interconnects and electrodes for stable operation in biofluids [8]. |
| Signal Processing Cores | Low-power Microcontrollers (MCUs) / Application-Specific Integrated Circuits (ASICs) | Hardware for implementing on-implant data reduction algorithms (spike detection, compression) to manage data from high-density arrays [88]. |
| Biofunctional Elements | Enzymes (e.g., Glucose Dehydrogenase) / Engineered Microbes (e.g., E. coli) | Used in biofuel cells and biosensors to transduce the presence of a specific analyte (e.g., glucose, arsenite) into an electrical signal [89]. |
The successful development of organic bioelectronic devices for chronic use hinges on a rigorous, multi-dimensional evaluation framework. As this guide has detailed, metrics for signal fidelity and functional longevity are deeply intertwined with the fundamental principles of biocompatibility. The mechanical and chemical harmony between device and tissue, exemplified by matching Young's modulus and using biocompatible elastomers, is a prerequisite for achieving stable electrical performance over the long term. Furthermore, the escalating data demands of high-density interfaces necessitate sophisticated on-implant signal processing to ensure system viability. By adopting the standardized metrics, experimental protocols, and material strategies outlined herein, researchers can systematically advance the field towards the creation of robust, reliable, and clinically impactful bioelectronic therapies that maintain their performance not for days, but for years.
Conclusion
The successful integration of organic bioelectronics into clinical practice hinges on a deep and multifaceted understanding of biocompatibility. As summarized, this requires a concerted effort across disciplines—from designing materials with innate tissue-like properties to developing robust, stable devices and validating their safety through rigorous standards. The future of the field points toward increasingly intelligent, closed-loop systems that leverage AI for adaptive therapy, multifunctional materials for combined sensing and treatment, and a stronger emphasis on biodegradable platforms to eliminate the need for surgical removal. For researchers and drug development professionals, these advances open new frontiers in personalized medicine, offering the potential for bioelectronic devices that not only treat disease but also heal and integrate with the body seamlessly, ultimately transforming standards of patient care.
References
- 1. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255127/]
- 2. Biocompatibility - Biological Safety - ISO 10993 [https://blog.johner-institute.com/tag/biocompatibility-iso-10993/]
- 3. Organic Bioelectronics: Diversity of Electronics Along with ... [https://www.mdpi.com/2079-6374/15/9/587]
- 4. Organic Bioelectronics: Materials and Biocompatibility [https://www.mdpi.com/1422-0067/19/8/2382]
- 5. ISO 10993-1:2025 - Biological evaluation of medical devices [https://www.iso.org/standard/10993-1]
- 6. ISO 10993-1:2025 Updates —Top 10 Biological Evaluation ... [https://namsa.com/resources/blog/iso-10993-12025top-10-biological-evaluation-essentials-in-the-update/]
- 7. Use of International Standard ISO 10993-1, "Biological ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/use-international-standard-iso-10993-1-biological-evaluation-medical-devices-part-1-evaluation-and]
- 8. A biocompatible elastomeric organic transistor for ... [https://www.nature.com/articles/s41928-025-01444-9]
- 9. New therapeutic brain implants could defy the need for ... [https://news.mit.edu/2025/new-therapeutic-brain-implants-defy-surgery-need-1105]
- 10. Recent Progress of Soft and Bioactive Materials in Flexible Bioelectronics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12038164/]
- 11. Organic semiconductors based wearable bioelectronics [https://www.sciencedirect.com/science/article/pii/S2950235725000034]
- 12. PEDOT:PSS-based bioelectronics for brain monitoring and ... [https://www.nature.com/articles/s41378-025-00948-w]
- 13. Novel conductive PEDOT:DBSA hydrogels with tuneable ... [https://pubs.rsc.org/en/content/articlehtml/2025/ma/d4ma00987h]
- 14. Materials design and integration strategies for soft bioelectronics in digital healthcare | Nature Reviews Materials [https://www.nature.com/articles/s41578-025-00819-w]
- 15. Materials strategy and device fabrication for stable closed-loop bioelectronics | npj Biosensing [https://www.nature.com/articles/s44328-025-00045-y]
- 16. Organic Bioelectronics: Diversity of Electronics Along with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467551/]
- 17. Reliability and stability of Bioelectronic Medicine: a critical and ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00179-4]
- 18. Organic Mixed Ionic-Electronic Conductors for ... [https://pubmed.ncbi.nlm.nih.gov/41016730/]
- 19. Review Advancements in tailoring PEDOT: PSS properties ... [https://www.sciencedirect.com/science/article/abs/pii/S2772950823003783]
- 20. Experimental Investigation on the Electrical Properties of ... [https://www.mdpi.com/2073-4360/17/3/289]
- 21. Biocompatibility and Toxicology Program: Research on ... [https://www.fda.gov/medical-devices/medical-device-regulatory-science-research-programs-conducted-osel/biocompatibility-and-toxicology-program-research-medical-devices-biocompatibility-and-toxicology]
- 22. Natural Biocompatible Polymers Market's Evolutionary ... [https://www.datainsightsmarket.com/reports/natural-biocompatible-polymers-1827614]
- 23. Cellulose: A comprehensive review of its properties and ... [https://www.sciencedirect.com/science/article/pii/S2949839225000781]
- 24. Properties, Production, and Recycling of Regenerated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11595832/]
- 25. Chitosan-based formulations for therapeutic applications. A ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-025-01161-7]
- 26. Effects of silk fibroin incorporation on the mechanical ... [https://www.sciencedirect.com/science/article/pii/S2590093525000505]
- 27. Recent advances in silk fibroin-based biomaterials for ... [https://pubmed.ncbi.nlm.nih.gov/40803475/]
- 28. Plant-based Biodegradable and Biocompatible Polymers ... [https://www.sciencedirect.com/science/article/abs/pii/S0008621525003258]
- 29. Advanced Biocompatible and Biodegradable Polymers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12611034/]
- 30. Inkjet printing of conductive nanomaterials on textiles for ... [https://www.sciencedirect.com/science/article/pii/S2590049825000748]
- 31. Physical Vapor Deposition Market Outlook Report 2025: [https://www.globenewswire.com/news-release/2025/09/16/3151014/28124/en/Physical-Vapor-Deposition-Market-Outlook-Report-2025-Industry-Size-Market-Shares-Data-Insights-Growth-Trends-Opportunities-Competition-2024-2032.html]
- 32. Comparative study of dynamic vulcanization strategies for ... [https://www.sciencedirect.com/science/article/abs/pii/S0032386125011620]
- 33. A critical review on the sustainability of inverse vulcanised ... [https://pubs.rsc.org/en/content/articlehtml/2025/su/d5su00387c]
- 34. Revolutionizing brain‒computer interfaces [https://pubmed.ncbi.nlm.nih.gov/40640801/]
- 35. Bio-inspired electronics: Soft, biohybrid, and “living†neural ... [https://www.nature.com/articles/s41467-025-57016-0]
- 36. A nonsurgical brain implant enabled through a cell ... [https://www.nature.com/articles/s41587-025-02809-3]
- 37. Medtronic BrainSenseâ„¢ Adaptive Deep Brain Stimulation ... [https://news.medtronic.com/2025-10-09-Medtronic-BrainSense-TM-Adaptive-Deep-Brain-Stimulation-named-a-2025-TIME-Best-Inventions]
- 38. Smart bandages: The future of wound care - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6511580/]
- 39. Smart Biomaterials in Wound Healing: Advances, ... [https://www.mdpi.com/2306-5354/12/11/1178]
- 40. a liquid diode-based smart bandage with ultrasensitive pH ... [https://www.nature.com/articles/s41378-024-00801-6]
- 41. Smart Bandage Clears New Hurdle: Monitors Chronic ... [https://www.caltech.edu/about/news/smart-bandage-clears-new-hurdle-monitors-chronic-wounds-in-human-patients]
- 42. “Lab on Skin†Smart Bandage Predicts Wound Healing [https://www.insideprecisionmedicine.com/topics/precision-medicine/lab-on-skin-smart-bandage-predicts-wound-healing/]
- 43. Advancements in smart wearable patch systems for ... [https://www.japtronline.com/index.php/joapr/article/view/667]
- 44. Organic Bioelectronics: Materials and Biocompatibility - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6121695/]
- 45. and Textile-Based Wearable Sensors for Health Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412463/]
- 46. Manufacturing Strategies for Stretchable Synaptic Transistors [http://www.sciencedirect.com/science/article/pii/S2950235725000174]
- 47. How AMOLED impacts biostimulatory device effectiveness? [https://eureka.patsnap.com/report-how-amoled-impacts-biostimulatory-device-effectiveness]
- 48. Wearable and implantable biosensors: mechanisms and applications in closed-loop therapeutic systems - Journal of Materials Chemistry B (RSC Publishing) DOI:10.1039/D4TB00782D [https://pubs.rsc.org/en/content/articlehtml/2024/tb/d4tb00782d]
- 49. Advanced strategies to thwart foreign body response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9472022/]
- 50. FOREIGN BODY REACTION TO BIOMATERIALS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2327202/]
- 51. Decoding Fibrotic Encapsulation in Plastic Surgery implants [https://www.sciencedirect.com/science/article/abs/pii/S0927776525006988]
- 52. The effect of the foreign body response on drug elution ... [https://www.sciencedirect.com/science/article/pii/S0142961225000298]
- 53. Biomimetic optimization of silicone breast implant integration [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1668930/full]
- 54. Foreign Body Reaction to Implanted Biomaterials and Its ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.622524/full]
- 55. Quantitative Proteomic Characterization of Foreign Body ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9953687/]
- 56. Immunocompatible elastomer with increased resistance to ... [https://www.nature.com/articles/s41467-024-52023-z]
- 57. In the News - MIT Department of Mechanical Engineering [https://meche.mit.edu/news-media/new-bioadhesive-strategy-can-prevent-fibrous-encapsulation-around-device-implants]
- 58. On the longevity and inherent hermeticity of silicon-ICs [https://pmc.ncbi.nlm.nih.gov/articles/PMC11697292/]
- 59. A biofluid-repellent nanograss coating enhances flow of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593835/]
- 60. Bio-corrosion Behavior of Direct Metal Laser Sintering- ... [https://ui.adsabs.harvard.edu/abs/2025MMTA...56.4702G/abstract]
- 61. Delamination of Plasticized Devices in Dynamic Service ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10972266/]
- 62. Wireless, Battery-free Platforms for Collection of Biosignals [https://pmc.ncbi.nlm.nih.gov/articles/PMC8112193/]
- 63. Battery-free wireless imaging of underwater environments [https://www.nature.com/articles/s41467-022-33223-x]
- 64. Wireless, battery-free multi-axial sensor for augmented ... [https://www.nature.com/articles/s41528-025-00479-4]
- 65. Sustainable Wireless Power Solutions Combat IoT Battery ... [https://www.powercastco.com/news/sustainable-wireless-power-solutions-combat-iot-battery-waste]
- 66. Energous Introduces Battery-Free e-Sense Tag, ... [https://energous.com/company/newsroom/news/energous-introduces-battery-free-e-sense-tag-establishing-first-end-to-end-wireless-power-platform-for-the-ambient-iot/]
- 67. Battery-Free Sensors Market Size & Trends 2025-2035 [https://www.futuremarketinsights.com/reports/battery-free-sensors-market]
- 68. Transient electronics for sustainability: Emerging technologies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12415906/]
- 69. Bioresorbable Materials on the Rise [https://pmc.ncbi.nlm.nih.gov/articles/PMC7029671/]
- 70. Bioimplantable and bioresorbable zinc-ion batteries based ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725057638]
- 71. End-of-Life usefulness of degradation by products from ... [https://www.nature.com/articles/s41528-025-00411-w]
- 72. Biodegradable electronic materials for promoting ... [https://link.springer.com/article/10.1007/s43939-025-00381-w]
- 73. The “Big Three†in biocompatibility testing of medical devices [https://pmc.ncbi.nlm.nih.gov/articles/PMC10800850/]
- 74. The Big Three: Cytotoxicity, Sensitization & Irritation Testing [https://academy.soterahealth.com/courses/the-big-three-cytotoxicity-sensitization-irritation-testing/]
- 75. ISO 10993 - Wikipedia [https://en.wikipedia.org/wiki/ISO_10993]
- 76. ISO 10993-1:2018 - Biological evaluation of medical devices — Part 1: Evaluation and testing within a risk management process [https://www.iso.org/standard/68936.html]
- 77. Basics of Biocompatibility: Information Needed for ... [https://www.fda.gov/medical-devices/biocompatibility-assessment-resource-center/basics-biocompatibility-information-needed-assessment-fda]
- 78. Cytotoxicity, Sensitization & Irritation Testing Explained [https://nabi.bio/cytotoxicity-sensitization-and-irritation-testing-what-do-they-involve/]
- 79. Biocompatibility Test Methods [https://pacificbiolabs.com/biocompatibility-test-methods/]
- 80. Preclinical In Vitro Evaluation of Extracellular Vesicles from ... [https://www.mdpi.com/1422-0067/26/13/6443]
- 81. Targeting the proliferation of glioblastoma cells and ... [https://www.nature.com/articles/s41598-025-97192-z]
- 82. Exercise-induced extracellular vesicles mediate apoptosis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479696/]
- 83. Immune-compatible designs of semiconducting polymers for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355568/]
- 84. Biocompatible Polymers Market Size & Trends 2025 to 2035 [https://www.futuremarketinsights.com/reports/biocompatible-polymers-market]
- 85. Natural polymer-based food packaging: paving the way to a ... [https://pubs.rsc.org/en/content/articlehtml/2025/fb/d5fb00021a]
- 86. Polymer Biomaterial Global Market Report 2025 [https://www.thebusinessresearchcompany.com/report/polymer-biomaterial-global-market-report]
- 87. Continuous biosignal acquisition beyond the limit of epidermal ... [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d5mh00758e]
- 88. Real-time, neural signal processing for high-density brain ... [https://bioelecmed.biomedcentral.com/articles/10.1186/s42234-025-00177-6]
- 89. New method developed to dramatically enhance bioelectronic ... [https://news.rice.edu/news/2025/new-method-developed-dramatically-enhance-bioelectronic-sensors]
- 90. Advances and perspectives in fiber-based electronic ... [https://www.nature.com/articles/s41528-025-00465-w]