Advancing Long-Term Neural Signal Fidelity: Materials, Methods, and Mitigation Strategies for Next-Generation Brain Interfaces
This article synthesizes the latest advancements and persistent challenges in achieving high-fidelity long-term neural recordings, a cornerstone for progress in neuroscience research, drug development, and clinical brain-computer interfaces.
Advancing Long-Term Neural Signal Fidelity: Materials, Methods, and Mitigation Strategies for Next-Generation Brain Interfaces
Abstract
This article synthesizes the latest advancements and persistent challenges in achieving high-fidelity long-term neural recordings, a cornerstone for progress in neuroscience research, drug development, and clinical brain-computer interfaces. We explore the fundamental obstacles of signal degradation, from foreign body reactions to technological bottlenecks in data transmission. The content details innovative methodological breakthroughs in flexible electrodes, bioadaptive coatings, and on-implant processing. Furthermore, it provides a critical analysis of troubleshooting strategies for issues like crosstalk and mechanical mismatch, and offers a comparative validation of emerging technologies, equipping researchers and professionals with a comprehensive overview of the field's current state and future trajectory.
The Core Hurdles: Understanding the Biological and Technical Barriers to Stable Neural Recordings
The long-term stability of intracortical neural interfaces is fundamentally constrained by the brain's biological response to implanted devices. This foreign body reaction (FBR) is a complex, multi-stage process that begins with acute injury and can culminate in the formation of an insulating glial scar at the tissue-electrode interface [1] [2]. For researchers and drug development professionals, understanding this cascade is critical, as the ensuing chronic inflammation and scarring are major contributors to signal degradation over time, ultimately limiting the efficacy of chronic neural recording and stimulation technologies [3] [2]. This guide objectively compares the key biological stages and their impact on signal fidelity, supported by experimental data and methodologies central to the field. The overarching thesis is that signal longevity depends not merely on the initial electrode performance but on mitigating the dynamic and persistent tissue response.
The Biological Cascade: From Implantation to Chronic Scarring
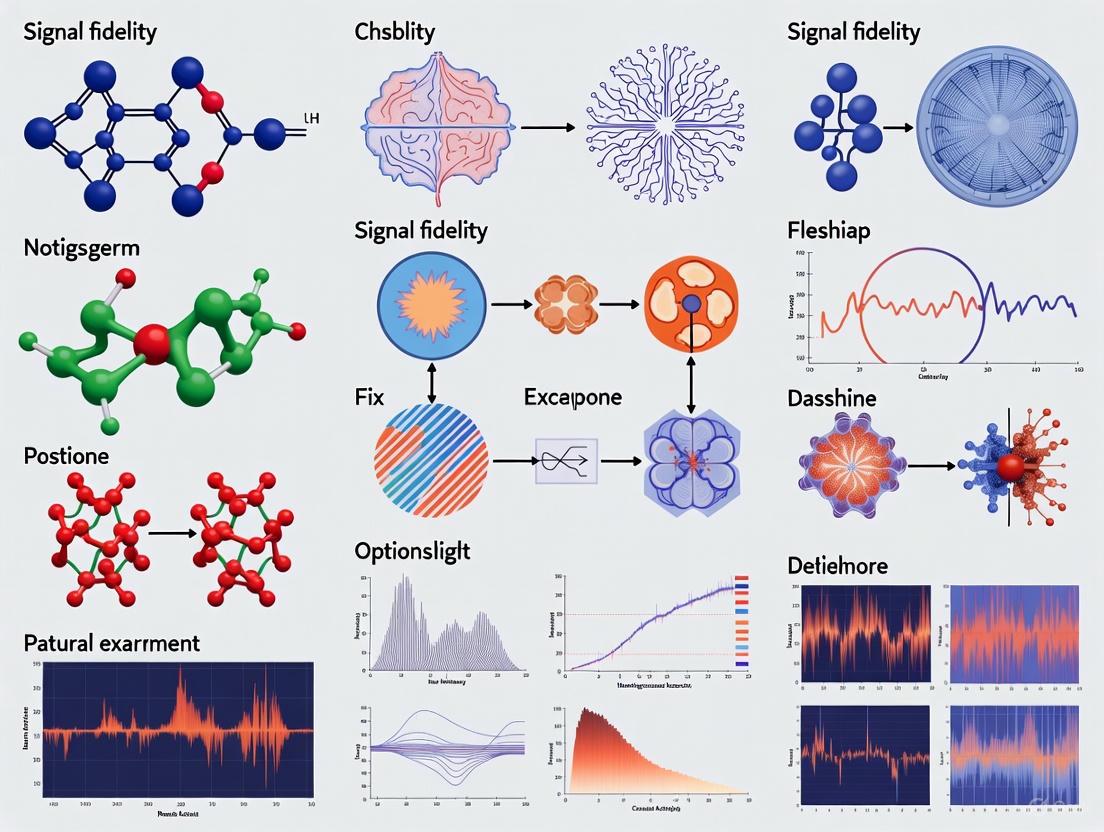
The tissue response to an implanted neural probe is a timed sequence of events, progressing from immediate injury to a chronic foreign body reaction. The following diagram illustrates the key stages and their interrelationships.
Diagram 1: The sequential progression of the foreign body reaction following neural probe implantation, culminating in glial scarring and signal degradation.
Stage 1: Acute Injury and Inflammation
The initial implantation trauma severs blood vessels and neural processes, causing bleeding and the release of blood plasma contents into the brain tissue [2]. This triggers an acute inflammatory response characterized by the recruitment of neutrophils and the activation of microglia, the brain's resident immune cells [1] [2]. A critical early event is the instantaneous adsorption of blood proteins (e.g., fibrinogen, albumin, complement) onto the probe surface, forming a "provisional matrix" that dictates subsequent cellular interactions [1].
Stage 2: Chronic Inflammation and Foreign Body Reaction
Within days, the acute response transitions to a chronic inflammatory phase dominated by monocytes and lymphocytes [1]. Blood-derived macrophages and activated microglia congregate at the implant interface [2]. A hallmark of the chronic FBR is the fusion of macrophages to form foreign body giant cells (FBGCs), which persist at the interface for the device's lifetime and participate in the chronic inflammatory response [1].
Stage 3: Gliosis and Glial Scar Formation
The persistent presence of the implant and the inflammatory milieu lead to reactive astrogliosis, where astrocytes undergo hypertrophy, proliferate, and upregulate expression of glial fibrillary acidic protein (GFAP) [2]. Along with activated microglia, these reactive astrocytes form a dense, insulating barrier around the implant known as the glial scar [3] [4]. While this scar tissue can functionally insulate the electrode, its effect on signal quality is complex and influenced by multiple factors, as detailed in the following sections.
Comparative Analysis of Factors Influencing the FBR and Signal Quality
The extent of the FBR and its impact on recording stability are modulated by several probe-related factors. The table below synthesizes experimental findings on how key properties influence tissue response and signal outcomes.
Table 1: Comparison of Neural Probe Properties and Their Impact on the Foreign Body Reaction
| Probe Property | Experimental Findings & Impact on FBR | Effect on Recording Signal |
|---|---|---|
| Probe Density [4] | High-density probes (e.g., platinum, 21.45 g/cm³) cause significantly larger astrocytic scars (GFAP intensity) than low-density probes (~1.35 g/cm³), despite similar size/shape/surface. Inertial forces from density mismatch drive scarring. | Not directly measured, but a larger astrocytic scar is hypothesized to increase functional insulation of the electrode. |
| Probe Size/Cross-section [3] | Smaller probes displace less tissue, disrupt fewer capillaries, and reduce biomolecule adsorption. This minimizes the initial injury and subsequent perfusion deficits, supporting neuronal health near the interface. | Directly linked to improved long-term stability. Smaller, slender probes allow for nearly "seamless" integration and sustained high-quality recordings [3]. |
| Probe Flexibility [3] | Flexible probes mitigate micro-motions caused by brain pulsations, reducing secondary trauma and chronic irritation. Stiff, tethered probes translate skull-brain movements into tissue damage. | Reduces chronic inflammation and gliosis, promoting a stable interface and consistent signal quality over time. |
| Biofouling & Interface Resistivity [5] | A thin, non-cellular interface layer of adsorbed proteins (biofouling) on the electrode tip is a primary driver of increased impedance. Glial scarring alone may not fully explain electrical changes. | A biofouling-induced increase in interface resistivity raises impedance but may not significantly affect recorded spike amplitude unless neurons are displaced [5]. |
Experimental Protocols for Characterizing the FBR
Research in this field relies on a combination of in vivo electrophysiology, histology, and computational modeling to dissect the components of the FBR.
In Vivo Electrophysiology and Impedance Tracking
Objective: To chronically monitor the electrical performance of implanted electrodes and correlate changes with the biological response.
Methodology:
- Implantation: Microelectrode arrays (e.g., Utah Array, Michigan probes) are surgically implanted into the target brain region of animal models (e.g., non-human primates, rats) [5].
- Recording: Neural signals (single-unit and multi-unit activity) and electrode impedance are tracked regularly over weeks to months. Key metrics include signal-to-noise ratio (SNR), spike amplitude, and impedance at 1 kHz [5].
- Data Analysis: Trends are analyzed, such as an initial increase in impedance and amplitude followed by stabilization or decline, which are then correlated with histological endpoints.
Histopathological Analysis and Immunohistochemistry
Objective: To quantitatively assess the cellular components of the FBR post-mortem.
Methodology:
- Perfusion and Sectioning: After a predetermined period, animals are perfused, and brain tissue is sectioned for analysis. In some protocols, probes are explanted to examine cells adhering to the implant surface [4].
- Staining: Tissue sections are stained with specific antibodies to identify key cell types:
- Anti-GFAP: Labels reactive astrocytes to quantify astrogliosis and glial scar thickness [2] [4].
- Anti-CD68 (ED1): Labels activated microglia and macrophages to assess the innate immune response [2] [4].
- Anti-NeuN: Labels neuronal nuclei to quantify neuronal density and loss around the implant site [4].
- Quantification: Staining intensity and cell density are measured at defined distances from the implant track (e.g., 0-50 μm, 50-100 μm) to create a quantitative profile of the FBR [4].
Data-Driven Computational Modeling
Objective: To isolate the individual contributions of glial scarring and biofouling to electrical changes.
Methodology:
- Model Construction: A finite-element model of the electrode in tissue is coupled with a multi-compartmental neuron model [5].
- Parameter Variation: The model incorporates variables such as encapsulation layer thickness (simulating glial scar), encapsulation resistivity, and interface resistivity (simulating biofouling) [5].
- Validation: Model outputs (impedance, signal amplitude) are reconciled with longitudinal in vivo data and histology to determine which biological factors best explain the observed electrical changes [5]. This approach demonstrated that a thin, high-resistance interface layer, rather than the glial scar itself, was the primary cause of rising impedance.
The workflow for integrating these methodologies is summarized below.
Diagram 2: The integrated experimental workflow for investigating the foreign body reaction, combining in vivo data, histology, and computational modeling.
The Scientist's Toolkit: Key Reagents and Materials
Table 2: Essential Research Reagents and Tools for FBR Studies
| Item | Function/Application |
|---|---|
| Microelectrode Arrays (e.g., Utah Array, Michigan Probe) | The implanted device for chronic neural recording and stimulation; the subject of the FBR [2] [5]. |
| Anti-GFAP Antibody | Primary antibody for immunohistochemical labeling of reactive astrocytes, enabling quantification of astrogliosis [2] [4]. |
| Anti-CD68 (ED1) Antibody | Primary antibody for immunohistochemical labeling of activated microglia and infiltrating macrophages [2] [4]. |
| Anti-NeuN Antibody | Primary antibody for labeling neuronal nuclei to assess neuronal density and viability near the implant [4]. |
| Parylene C | A common, biocompatible polymer used as an insulating coating for neural probes to isolate the effect of underlying material properties [4]. |
| Finite-Element Modeling Software (e.g., COMSOL) | Platform for building computational models to simulate the electrical properties of the electrode-tissue interface and deconstruct contributing factors [5]. |
| D-Biopterin | 2-amino-6-(1,2-dihydroxypropyl)-3H-pteridin-4-one (Biopterin) |
| Indolelactic acid | Indole-3-lactic Acid|High-Purity ILA Reagent |
The journey from acute inflammation to chronic glial scarring represents the central challenge to achieving stable, long-term neural recordings. The foreign body reaction is not a single entity but a multifaceted process driven by initial injury, mechanical forces (from density and stiffness mismatches), and persistent immune activation. A critical insight from recent research is that the glial scar itself may not be the primary electrical barrier to signal quality; instead, a thin biofouling layer at the electrode interface may be a more significant factor in impedance increases [5]. This paradigm shift suggests that future engineering strategies must move beyond a singular focus on eliminating gliosis and instead pursue integrated solutions that address probe biomechanics (miniaturization, flexibility, density), surface chemistry (to minimize biofouling), and the underlying inflammatory cascade. For the field to advance, the continued development and application of the sophisticated experimental protocols and reagents detailed herein will be essential for disentangling this complex biological puzzle. :::
The evolution of brain-implantable microsystems has entered a critical phase where engineering advancements in microelectrode array fabrication have dramatically outpaced capabilities for handling the resulting neural data. High-density microelectrode arrays (HD-MEAs) with thousands of recording channels represent the frontier of neural interfacing technology, enabling unprecedented access to brain activity with exceptional spatial and temporal resolution [6] [7]. However, this remarkable recording capability has created a fundamental engineering constraint: the wireless transmission bottleneck. As channel counts escalate to 10,000+ electrodes, the massive data volumes generated threaten to overwhelm both the power budgets and transmission bandwidth of implantable systems [6] [8]. This comparative analysis examines the core technical challenges and emerging solutions for maintaining signal fidelity while overcoming data transmission constraints in next-generation neural interfaces.
The central dilemma is straightforward yet formidable. While microfabrication technologies now enable creating microelectrode arrays with extreme channel densities (>3000 electrodes per mm²), simultaneously streaming raw data from all these channels would require wireless data rates that are physiologically and technically implausible for implantable devices [6]. For instance, a 1,024-channel system sampling at 30 kHz with 10-bit resolution would generate a continuous data stream of approximately 307 Mbps before accounting for overhead—far exceeding practical limits for implanted transmitters operating under strict power constraints [8]. This review systematically compares the predominant strategies being developed to resolve this critical bottleneck while preserving the neural information essential for both basic neuroscience and clinical applications.
Technical Challenges in High-Density Neural Data Transmission
The Scaling Problem: Data Volume Versus Transmission Capacity
The fundamental challenge stems from an exponential growth in data generation that linearly outpaces improvements in transmission efficiency. Contemporary HD-MEAs now accommodate up to 236,880 electrodes with simultaneous readout from 33,840 channels at 70 kHz sampling rates [7]. The raw data output from such systems would approach several gigabits per second—far beyond the capabilities of any existing implantable wireless technology under power constraints suitable for safe human implantation [6].
Table 1: Microelectrode Array Scaling Trends and Data Generation
| Parameter | Traditional Arrays | Current HD-MEAs | Next-Generation HD-MEAs |
|---|---|---|---|
| Channel Count | 10-100 electrodes | 1,000-10,000 electrodes | 10,000-100,000 electrodes |
| Electrode Density | 10-100/mm² | 100-1,000/mm² | >1,000/mm² |
| Raw Data Rate | 1-10 Mbps | 100 Mbps - 1 Gbps | >1 Gbps |
| Spatial Resolution | Network-level activity | Multi-unit activity | Single-unit, subcellular |
| Primary Limitation | Signal quality | Data transmission | Power efficiency & heat dissipation |
The wireless telemetry technologies currently available for brain implants present severe limitations for high-density data transmission. Radio frequency (RF) links, commonly used in medical implants, typically offer bit rates below 100 Mbps with communication ranges of a few centimeters [6]. While ultra-wideband (UWB) and optical links can provide higher data rates, they face challenges with tissue penetration and power efficiency. As illustrated in Figure 5 of the search results, even the most advanced wireless technologies struggle to support the multi-gigabit per second requirements of uncompressed full-bandwidth data from next-generation HD-MEAs [6].
Power and Thermal Constraints
Beyond pure data rate limitations, implantable systems operate under exceptionally strict power budgets—typically sub-milliwatt per channel—to prevent tissue heating and damage [6] [8]. The power consumption of wireless transmitters increases super-linearly with data rate, making raw data transmission prohibitively expensive from a power perspective. Additionally, heat dissipation becomes a critical safety concern when processing and transmitting massive data volumes within confined implant packages [7]. These constraints fundamentally necessitate a paradigm shift from "transmit everything" to "process intelligently and transmit selectively."
Comparative Analysis of Data Reduction Strategies
On-Implant Signal Processing Techniques
The most promising approach to overcoming the transmission bottleneck involves performing sophisticated signal processing directly on the implant to reduce data volume before transmission. These techniques can be broadly categorized into temporal compression, spatial compression, and feature extraction methods, each with distinct trade-offs between compression efficiency, computational complexity, and signal fidelity preservation [6].
Table 2: Comparison of On-Implant Data Reduction Techniques
| Technique | Compression Principle | Compression Ratio | Hardware Efficiency | Information Preservation |
|---|---|---|---|---|
| Spike Detection & Extraction | Discards inter-spike data | 10-100x (dependent on firing rate) | Very High | Only preserves action potentials |
| Salient Sample Compression | Transmits key spike features | 2000x+ (at 8 spikes/s) | High | Reconstructs spike waveforms |
| Transform-Based Methods | Projects signals to compact domain | 10-50x | Moderate | Near-lossless reconstruction |
| Spatial Compression | Exploits channel correlation | 5-20x | Moderate | Preserves spatial relationships |
| Compressive Sensing | Sub-Nyquist sampling | 4-16x | Low-Moderate | Theoretical perfect reconstruction |
Spike detection and extraction represents the most established approach, where only the action potential waveforms are preserved while discarding background neural data between spikes [6] [8]. This method achieves compression ratios of 10-100x, depending on neuronal firing rates, with minimal computational overhead. However, it irrevocably discards local field potential (LFP) information and requires careful spike detection thresholds to avoid losing valuable neural events [6].
Advanced Compression Methodologies
Salient Sample Extraction and Curve Fitting
A particularly innovative approach recently demonstrated achieves remarkable compression ratios exceeding 2000x through a method called salient sample extraction and curve fitting [8]. This technique identifies critical points in spike waveforms (start/end points and extremum points) and transmits only these features rather than complete waveforms. On the external side, predefined smooth curves are fit to these points to reconstruct spike shapes.
The experimental protocol for this method involves:
- Spike detection using amplitude thresholding or more sophisticated algorithms
- Salient point identification through analysis of triplets of consecutive samples to detect slope sign changes
- Feature encoding of salient point timing and amplitudes
- Wireless transmission of compressed feature set
- Waveform reconstruction on external equipment using polynomial fitting functions
This approach achieves unprecedented compression while maintaining signal fidelity, with the added benefit of inherent noise reduction through the curve-fitting process [8]. Hardware implementation in 130-nm CMOS technology consumes only 0.164 µW per channel at 1V supply—well within the strict power constraints of implantable devices [8].
Transform-Based and Spatial Compression
Transform-based methods including discrete wavelet transform (DWT), discrete cosine transform (DCT), and Walsh-Hadamard transform (WHT) project neural signals into alternative domains where they can be represented more compactly [6] [8]. These techniques typically achieve moderate compression ratios (10-50x) with better preservation of original signal morphology compared to spike-only approaches.
Spatial compression techniques exploit the inherent correlation between adjacent recording channels to reduce redundancy in multi-channel neural data [8]. Methods such as the whitening transform and MBED technique have demonstrated effectiveness, particularly as electrode densities increase and the spatial correlation between channels becomes more pronounced [8].
Signal Fidelity Considerations in Long-Term Neural Recording
The Fidelity-Compression Tradeoff
A central tension in neural data compression lies in balancing compression efficiency against signal fidelity preservation. Different neural applications require different aspects of signal fidelity—for motor decoding applications, precise spike timing may be paramount, while for neurological disorder monitoring, specific LFP frequency bands might carry critical information [6] [9].
The non-linear modeling of complete neural recording systems has revealed that different components contribute unequally to overall signal degradation [9]. Specifically, analog-to-digital converter (ADC) non-linearity has a greater impact on system performance than front-end amplifier non-linearity, providing crucial guidance for optimizing system design when balancing performance against power and area constraints [9].
Long-Term Stability Challenges
Maintaining signal fidelity over extended implantation periods presents additional challenges related to foreign body response, biofouling, and electrode impedance changes [10]. Recent advances in bioadaptive interfaces have demonstrated promising approaches for sustained high-quality recording. The TAB (targeting-specific interaction and blocking nonspecific adhesion) coating strategy combines brain-derived neurotrophic factor (BDNF) conjugation with a lubricant-infused surface to promote positive neural interactions while minimizing inflammatory response [10].
Experimental results with TAB-coated fibers demonstrated high-quality single-unit neural signals maintained for over 12 months post-implantation, representing a significant advancement for long-term neural interfaces [10]. This sustained performance is crucial for clinical applications where stable decoding performance over years is required.
Experimental Protocols for Method Validation
Protocol 1: Evaluating Compression Efficacy
To objectively compare compression techniques, researchers should implement the following standardized protocol:
- Data Acquisition: Record neural data using HD-MEAs from appropriate models (in vitro cultures, animal models, or human intraoperative recordings)
- Ground Truth Establishment: Manually curate a subset of data with expert-labeled spikes and LFPs
- Algorithm Application: Apply each compression technique to the same dataset
- Performance Metrics Calculation:
- Compression Ratio: Original size / compressed size
- Spike Detection Accuracy: Precision, recall, F1-score compared to ground truth
- Waveform Reconstruction Error: Mean squared error between original and reconstructed spikes
- Decoding Performance: Comparison of information transfer rates in brain-computer interface tasks
- Hardware Efficiency Assessment: Measure power consumption, silicon area, and processing latency for implant implementation
Protocol 2: Long-Term Signal Stability Assessment
For evaluating sustained performance in chronic implants:
- Surgical Implantation: Precisely place HD-MEAs using minimally invasive techniques [11]
- Longitudinal Monitoring: Regularly acquire neural data over weeks to months
- Signal Quality Metrics: Track signal-to-noise ratio, unit yield, and amplitude stability over time
- Histological Correlation: Upon endpoint, examine tissue response and electrode encapsulation
The cranial micro-slit technique described in recent literature enables minimally invasive implantation of high-density arrays while minimizing tissue damage [11]. This procedure uses 500-900μm wide incisions for subdural insertion of thin-film arrays without requiring full craniotomy, significantly improving recovery and long-term viability [11].
Research Reagent Solutions for Neural Interface Studies
Table 3: Essential Research Materials and Experimental Tools
| Reagent/Technology | Function/Application | Key Characteristics |
|---|---|---|
| CMOS HD-MEA Chips | Neural signal acquisition | High electrode density, integrated electronics, scalable manufacturing [7] |
| Flexible Thin-Film Arrays | Cortical surface recording | Conformable to brain surface, minimal mechanical mismatch [11] |
| TAB Coating | Surface modification for long-term stability | BDNF conjugation + lubricant infusion reduces fouling [10] |
| Salient Sample Compression ASICs | On-implant data reduction | Custom CMOS implementation, ultra-low power operation [8] |
| Bioadaptive Polymer Substrates | Neural probe fabrication | Mechanical compliance matching neural tissue [10] |
| Wireless Telemetry Systems | Data transmission from implant | UWB, RF, or infrared based on application requirements [6] |
Emerging Directions and Future Prospects
The field of neural interface data handling is rapidly evolving toward more intelligent, adaptive approaches. Machine learning-based compression techniques show promise for dynamically optimizing compression strategies based on neural content and application requirements [12]. Additionally, hierarchical processing approaches that combine multiple compression techniques adaptively may further push the boundaries of what is achievable within strict implant power budgets.
Future systems will likely incorporate closed-loop operation where neural recording, processing, and stimulation are tightly integrated [6] [7]. In such systems, efficient data handling becomes even more critical as computational resources must be shared between decoding algorithms and stimulus optimization routines.
The continuing progression toward higher channel counts necessitates a fundamental rethinking of neural data paradigms. Rather than attempting to transmit increasingly massive raw data streams, the field is shifting toward on-implant feature extraction where only behaviorally or clinically relevant information is communicated externally [6] [8]. This approach aligns with both technical constraints and the fundamental goal of neural interfaces—to extract meaningful information about brain function and dysfunction.
The data transmission bottleneck in high-density neural interfaces represents both a formidable challenge and a catalyst for innovation in neural engineering. Through comparative analysis of current approaches, it is evident that no single solution optimally addresses all requirements for compression efficiency, computational complexity, and signal fidelity preservation. The most promising path forward involves context-appropriate selection and combination of techniques based on specific application requirements—whether for basic neuroscience research, clinical brain-computer interfaces, or therapeutic neurostimulation.
As microfabrication technologies continue to push the boundaries of electrode density, parallel advancements in on-implant processing algorithms and hardware implementation will be essential to realize the full potential of next-generation neural interfaces. The ongoing development of sophisticated yet power-efficient compression strategies, coupled with bioadaptive materials that ensure long-term signal stability, promises to overcome current limitations and enable transformative applications in understanding and treating neurological disorders.
The clinical success of implantable neural interfaces, from deep brain stimulation (DBS) for Parkinson's disease to brain-computer interfaces (BCIs) for paralysis, is fundamentally constrained by a single physical property: mechanical mismatch [13]. This mismatch arises from the vast difference in stiffness between traditional electrode materials and the soft neural tissues they penetrate. While the brain exhibits a Young's modulus of approximately 1-10 kPa, conventional electrode materials such as silicon (~130-185 GPa) and platinum (~102 GPa) are orders of magnitude stiffer [14] [15]. This mechanical disparity creates a significant interface problem, initiating a cascade of biological responses that ultimately compromise recording stability and stimulation efficacy.
This article examines how this mechanical mismatch induces chronic inflammation through micro-motion damage, directly impacting the long-term signal fidelity crucial for both basic neuroscience research and clinical applications. We compare the performance of traditional rigid electrodes against emerging mechanically-compliant alternatives, providing experimental data and methodologies that inform material selection and device design for researchers and drug development professionals.
The Fundamental Mechanisms of Damage
Biomechanical Principles and Strain Modeling
The primary mechanical conflict at the neural interface stems from the bending stiffness (K) of the implant, which scales linearly with Young's modulus (E) and to the third power with thickness (h) for a rectangular shank, as defined by the equation ( K = E \cdot \frac{bh^3}{12} ) (where b is width) [16] [17]. This relationship means that reducing thickness has a dramatically greater impact on flexibility than changing material composition.
Finite Element Modeling (FEM) reveals how this stiffness discrepancy translates to tissue damage. When a 20 µm displacement is applied to simulate brain micromotion, rigid implants induce concentrated strain along their surfaces and particularly at the tips [14] [18]. This strain is further focused on small protrusions such as electrical traces and recording sites. One study demonstrated that the mechanical mismatch between iridium and silicon within a single device creates additional focal points of strain, leading to material failure over time [18].
Table 1: Mechanical Properties of Neural Tissues and Interface Materials
| Material/Tissue | Young's Modulus | Key Characteristics | Impact on Interface |
|---|---|---|---|
| Brain Tissue | 1-10 kPa | Viscoelastic, compliant | Reference baseline for compatibility |
| Silicon (Michigan Probe) | 130-185 GPa | Rigid, brittle | Significant mechanical mismatch |
| Platinum | ~102 GPa | Ductile, conductive | High stiffness mismatch |
| Polyimide | ~2.5 GPa | Flexible polymer | Reduced but still present mismatch |
| Mechanically-Adaptive Nanocomposite | 5.2 GPa → 12 MPa | Softens upon implantation | Drastically reduced chronic mismatch |
The Biological Cascade: From Micro-Motion to Chronic Inflammation
The initial implantation itself causes acute injury, but the persistent inflammatory response is primarily driven by the ongoing mechanical mismatch. The biological response evolves through several key phases [17]:
Acute Phase (Days): Insertion disrupts the blood-brain barrier, causing bleeding and releasing inflammatory factors that attract immune cells to clear debris.
Chronic Phase (Weeks to Months): Continuous micromotion between the rigid implant and surrounding tissue causes recurring damage, sustaining the inflammatory response. Microglia activate and release cytokines and reactive oxygen species, while astrocytes proliferate and migrate to the injury site.
Encapsulation Phase (Months+): Astrocytes secrete extracellular matrix components, forming a dense physical barrier of glial scar tissue around the electrode. This scar electrically insulates the electrode, increasing impedance and signal attenuation.
The following diagram illustrates this cascade, showing how mechanical mismatch initiates a biological response that ultimately degrades signal quality.
Performance Comparison: Rigid vs. Compliant Electrodes
Histological and Functional Outcomes
Direct comparisons between rigid and compliant implants reveal striking differences in long-term tissue integration and functional stability. A pivotal study investigating mechanically-adaptive nanocomposites—initially rigid for implantation but softening to ~12 MPa under physiological conditions—demonstrated significantly improved outcomes compared to stiff controls [14].
Table 2: Comparative Tissue Response: Rigid vs. Compliant Implants
| Parameter | Rigid Implants (e.g., Silicon, PVAc-coated Silicon) | Compliant Implants (e.g., Mechanically-Adaptive Nanocomposites) | Experimental Evidence |
|---|---|---|---|
| Acute Response (3 days) | Significant BBB disruption, cell death at interface | Statistically similar tissue response | No significant difference in early healing phase [14] |
| Chronic Inflammation (2-16 wks) | Sustained elevated microglial and astrocytic activation | Significantly reduced glial activation at all chronic time points | Immunohistochemistry showing reduced GFAP+ and Iba1+ cells [14] |
| Blood-Brain Barrier Stability | Persistent leakage around implant | More stable BBB over chronic periods | Immunohistochemistry for albumin and other serum proteins [14] |
| Neuronal Density | Late-onset neurodegeneration with neuronal loss | Better preserved neuronal populations near interface | NeuN staining showing higher neuronal density at 16 weeks [14] |
| Recording Longevity | Signal degradation over weeks to months | Improved signal stability demonstrated in animal models | Lower impedance drift and more stable single-unit recordings over months [16] [19] |
Quantitative Data on Strain and Scarring
Finite element models provide quantitative insight into why compliant materials produce superior histological outcomes. One analysis revealed that the maximum strain in brain tissue surrounding a traditional silicon electrode was significantly higher than around ultraflexible electrodes with subcellular dimensions [16]. This reduced strain directly correlates with thinner glial scar formation—typically 50-100 µm around compliant implants compared to 200-500 µm around rigid interfaces [16] [13].
The following experimental workflow outlines the key methodologies used to generate this comparative data, from material fabrication through to histological analysis.
Experimental Protocols for Assessing Interface Stability
Chronic In Vivo Evaluation
To generate the comparative data presented in this review, researchers employ standardized protocols for long-term assessment of neural interfaces [14] [18]:
Animal Surgery and Implantation:
- Animals (typically rats or mice) receive bilateral implants with different materials in contralateral hemispheres to control for biological variability.
- Implants are inserted approximately 2 mm deep into cortical tissue (e.g., primary visual or motor cortex) by hand or with controlled insertion systems.
- Devices are tethered to the skull using Kwik-sil and dental acrylic to minimize external motion transmission.
- Animals are euthanized at multiple time points (e.g., 3 days, 2, 8, and 16 weeks) to capture both acute and chronic responses.
Electrophysiological Assessment:
- Electrochemical Impedance Spectroscopy (EIS): Regularly measured to track changes at the electrode-tissue interface. Stable, low impedance indicates healthy integration.
- Single-Unit Recording: Quality and quantity of detectable neuronal action potentials are tracked over time. Signal-to-noise ratio and number of discriminable units serve as key metrics.
- Local Field Potential (LFP) Recording: Monitors broader network activity and stability.
Post-Mortem Histological Analysis
Tissue Processing and Staining:
- Transcardial perfusion with paraformaldehyde followed by brain extraction and cryosectioning.
- Immunohistochemistry for specific cell types:
- NeuN: Labels neuronal nuclei to quantify neuronal density and distribution near interface.
- GFAP: Identifies reactive astrocytes involved in glial scar formation.
- Iba1: Marks activated microglia mediating inflammatory response.
- Laminin or Albumin: Assess blood-brain barrier integrity.
Quantitative Morphometrics:
- Cell counting within standardized distances from the implant track (e.g., 0-50 µm, 50-100 µm, 100-200 µm).
- Measurement of glial scar thickness based on GFAP intensity profiles.
- 3D reconstruction of implant tracks to assess tissue deformation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Neural Interface Research
| Research Reagent | Function/Application | Example Use Cases |
|---|---|---|
| Mechanically-Adaptive Nanocomposites (PVAc/tCNC) | Soften upon implantation to match brain mechanics | Reducing chronic inflammation in cortical implants [14] |
| Ultraflexible Polymers (Polyimide, Parylene-C, SU-8) | Substrate materials with reduced bending stiffness | Fabrication of flexible electrode arrays with lower Young's modulus [16] [19] |
| Conductive Polymers (PEDOT:PSS) | Coatings to reduce electrode impedance and improve signal transduction | Enhancing signal-to-noise ratio in recording electrodes [19] |
| Nature-Derived Materials (Silk fibroin, Chitosan) | Biocompatible coatings and dissolvable sacrificial layers | Improving tissue integration and reducing FBR [20] |
| Dexamethasone-loaded Coatings | Controlled anti-inflammatory drug release | Actively suppressing immune response at implantation site [20] |
| Tungsten Wire Guidance Systems | Temporary stiffeners for implanting flexible electrodes | Enabling precise insertion of ultraflexible probes [17] |
| (E)-Cinnamamide | Cinnamamide|621-79-4|Research Chemical | |
| Decacyclene | Decacyclene, CAS:191-48-0, MF:C36H18, MW:450.5 g/mol | Chemical Reagent |
The evidence overwhelmingly demonstrates that mechanical mismatch is a primary determinant of long-term neural interface failure. The micro-motion between rigid implants and soft neural tissue sustains a chronic inflammatory response that culminates in glial scar formation, neuronal loss, and signal degradation. Compliant materials—particularly those that match the mechanical properties of brain tissue—consistently demonstrate reduced inflammatory markers, preserved neuronal density, and more stable electrical performance over chronic periods.
For researchers and drug development professionals, these findings highlight that material selection is not merely an engineering concern but a fundamental biological consideration. The move toward mechanically-compliant interfaces represents a paradigm shift in neural interface design, one that prioritizes seamless integration over brute-force functionality. As the field advances, the combination of compliant materials, sophisticated implantation strategies, and bioactive coatings offers the most promising path toward neural interfaces that remain stable and functional for decades—a crucial requirement for both basic neuroscience and clinical applications.
Biofouling and its Impact on Electrode-Tissue Interface Impedance and Signal Quality
The long-term stability of implantable neural electrodes represents a fundamental barrier in brain-computer interface (BCI) technology and chronic neural recording research. Biofouling—the unwanted adsorption of biological material and subsequent inflammatory response to implanted neural electrodes—directly compromises signal fidelity by increasing electrode-tissue interface impedance and degrading recording quality [15]. This biological process initiates immediately upon electrode implantation and evolves through characteristic phases, ultimately resulting in the formation of an insulating scar tissue layer that physically separates recording sites from their target neurons [17] [15]. The foreign body response triggered by electrode implantation activates microglia and astrocytes, which proliferate and migrate to the injury site, secreting inflammatory cytokines and extracellular matrix components that form a dense physical barrier around the implant [17]. This review systematically analyzes the biofouling cascade at neural interfaces, evaluates its quantifiable impacts on electrical properties and signal quality, compares testing methodologies for antifouling strategies, and identifies promising research directions for maintaining signal fidelity in chronic neural recordings.
The Biofouling Cascade: From Acute Implantation to Chronic Encapsulation
The biofouling process at neural electrode interfaces follows a well-defined temporal sequence involving distinct but overlapping biological events. Understanding this cascade is essential for developing targeted interventions to mitigate its effects on signal recording quality.
Phases of the Foreign Body Response
Acute Inflammatory Phase: The implantation procedure itself causes mechanical trauma, damaging blood vessels and neural tissue. This initial injury triggers the release of inflammatory factors that recruit immune cells to phagocytose cellular debris [17]. The geometric and mechanical mismatch between the electrode and brain tissue exacerbates this acute tissue damage, particularly with traditional rigid electrodes that have significantly higher Young's modulus (~102 GPa for silicon) compared to neural tissue (1-10 kPa) [15].
Chronic Inflammatory Phase: Following the acute response, persistent mechanical mismatch between the implant and surrounding tissue leads to continuous micromotion-induced friction, causing ongoing tissue damage [17]. This sustained injury activates microglia, which release inflammatory cytokines and reactive oxygen species [17] [15]. Concurrently, astrocytes proliferate and migrate toward the implant site, secreting extracellular matrix (ECM) components [17].
Fibrous Encapsulation Phase: The accumulated ECM components and aligned glial cells eventually form a compact, insulating cellular layer around the electrode—a glial scar [17] [15]. This scar tissue creates a physical barrier that increases the distance between neurons and recording sites, leading to progressive signal attenuation and impedance elevation [17].
The following diagram illustrates this sequential biofouling process and its direct consequences for signal recording quality:
Key Cellular and Molecular Mediators
The cellular response to implanted electrodes involves coordinated activity of multiple cell types. Microglia, the resident immune cells of the central nervous system, become activated within hours of implantation and attempt to phagocytose the foreign material [17] [15]. When unable to remove the electrode, they transition to a chronic activated state, releasing pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6, which perpetuate the inflammatory environment [15]. Astrocytes undergo reactive gliosis, characterized by hypertrophy, proliferation, and increased expression of glial fibrillary acidic protein (GFAP) [17]. These reactive astrocytes migrate toward the implant and secrete chondroitin sulfate proteoglycans and other ECM components that contribute to the glial scar [17]. The resulting scar tissue typically consists of 50-100 μm thick layers of activated microglia and astrocytes surrounding the electrode, creating a significant physical barrier that can displace neurons by 100-500 μm from the recording sites [15].
Quantifiable Impacts on Interface Impedance and Signal Quality
Biofouling-induced tissue changes produce measurable alterations in the electrochemical properties of the electrode-tissue interface and directly impact the quality of recorded neural signals.
Impedance Changes and Signal Attenuation
The formation of glial scar tissue around neural electrodes significantly increases the electrical impedance at the electrode-tissue interface, particularly at frequency ranges relevant for neural recording [15]. This impedance elevation occurs because the scar tissue acts as a resistive barrier between the electrode and electrically active neurons. Studies have reported impedance increases of 200-500% over implantation periods of 4-12 weeks in various animal models, with the most dramatic rises occurring during the initial inflammatory phase [15]. The corresponding increase in physical distance between neurons and recording sites results in signal amplitude attenuation of 70-90% for single-unit recordings, often rendering previously detectable neurons unrecoverable from the noise floor [15]. The table below summarizes key quantitative relationships between biofouling progression and signal quality parameters:
Table 1: Biofouling Impact on Neural Signal Quality Parameters
| Time Post-Implantation | Tissue Response Phase | Impedance Change | Single-Unit Amplitude | Signal-to-Noise Ratio |
|---|---|---|---|---|
| 0-24 hours | Acute inflammation | +50% to +100% | -20% to -40% | -15% to -30% |
| 1-4 weeks | Chronic inflammation | +150% to +300% | -50% to -80% | -40% to -70% |
| 4-12 weeks | Glial scar maturation | +200% to +500% | -70% to -90% | -60% to -85% |
| >12 weeks | Stable encapsulation | Stable at elevated levels | Stable at attenuated levels | Stable at reduced levels |
Long-Term Signal Stability and Recording Longevity
The chronic nature of the foreign body response fundamentally limits the functional longevity of neural recording interfaces. While flexible electrodes have demonstrated improved compatibility compared to rigid substrates, even advanced designs typically show progressive signal degradation over 4-8 month periods [17]. Studies investigating the long-term stability of single-unit recordings have found that only 15-30% of initially detectable units remain recordable after 6 months of implantation, with the remainder lost due to increasing interface impedance and neuronal displacement [15]. This signal decay follows an approximately exponential time course, with the most rapid decline occurring during the first 4-8 weeks post-implantation as the glial scar matures [17] [15]. The correlation between glial cell markers (GFAP, Iba1) expression levels and signal quality degradation provides compelling evidence for the causal relationship between the foreign body response and recording performance deterioration [15].
Comparative Analysis of Antifouling Strategies and Materials
Multiple material science and bioengineering approaches have been developed to mitigate biofouling at neural interfaces, each with distinct mechanisms of action and performance characteristics.
Material-Based Antifouling Strategies
Table 2: Performance Comparison of Neural Electrode Antifouling Strategies
| Strategy Category | Specific Approach | Mechanism of Action | Impact on Impedance | Recording Longevity | Limitations |
|---|---|---|---|---|---|
| Flexible Substrates | Polyimide, parylene, silicone shafts | Reduced mechanical mismatch minimizes chronic inflammation | 30-50% lower initial increase | 2-4 month improvement | Reduced insertion stiffness requires shuttle assistance |
| Nanomaterial Coatings | Graphene, carbon nanotubes (CNTs) | High surface area maintains conductivity despite fouling | 40-60% reduction versus uncoated | 3-6 month improvement | Potential nanomaterial toxicity concerns |
| Conducting Polymers | PEDOT, PPy with bioactive doping | Decreased interfacial impedance combined with drug elution | 60-80% reduction versus metal | 4-8 month improvement | Limited long-term stability in physiological conditions |
| Surface Functionalization | PEG, peptide coatings, hydrogel layers | Physicochemical barrier against protein adsorption | 20-40% reduction | 1-3 month improvement | May increase initial electrode size |
| Drug Elution Systems | Dexamethasone, anti-inflammatory release | Local suppression of immune cell activation | 50-70% reduction | 4-12 month improvement | Finite drug reservoir requires reloading |
Mechanical Compatibility and Geometric Optimization
Recent advances in neural interface design have emphasized the critical importance of mechanical compatibility between the electrode and neural tissue. Traditional rigid electrodes (silicon, tungsten) with Young's moduli of 10²-10ⵠMPa create significant mechanical mismatch with brain tissue (1-10 kPa), exacerbating micromotion-induced inflammation [15]. Flexible electrodes using polyimide, parylene, or silicone substrates with Young's moduli of 0.5-5 GPa substantially reduce this mismatch, demonstrating 40-60% decreases in glial scarring compared to rigid counterparts in chronic implantations [17]. Ultra-flexible electrodes such as neurofilaments (<10 μm cross-section) and mesh electrodes have shown particularly promising results, with some studies reporting stable single-unit recordings for 8+ months in primate models [17]. Additionally, electrode geometry significantly influences the acute tissue damage during implantation, with smaller cross-sectional areas (<100 μm²) causing minimal vascular disruption and enabling more rapid tissue recovery [17].
Experimental Methodologies for Assessing Biofouling Impacts
Standardized experimental protocols are essential for quantitatively evaluating biofouling progression and the efficacy of antifouling strategies in neural interface research.
In Vivo Electrochemical and Electrophysiological Characterization
Comprehensive assessment of biofouling impacts requires multimodal experimental approaches that combine electrochemical measurements with histological validation. The following workflow outlines a standardized methodology for correlating electrical performance with biological response:
Key Methodological Considerations
Electrochemical Impedance Spectroscopy (EIS): Measurements should be performed across a broad frequency range (0.1 Hz to 100 kHz) to characterize both the charge transfer processes at the electrode surface (high frequency) and the tissue conductivity (low frequency) [15]. The phase angle at 1 kHz provides particularly valuable information about the capacitive versus resistive characteristics of the interface.
Signal Quality Metrics: Quantitative assessment should include signal-to-noise ratio (SNR), single-unit yield (detectable units per electrode), amplitude distribution, and spike sorting consistency across recording sessions [15]. These metrics should be tracked longitudinally to establish performance degradation timelines.
Histological Correlations: Following electrophysiological characterization, immunohistochemical analysis for GFAP (astrocytes), Iba1 (microglia), and NeuN (neurons) enables three-dimensional reconstruction of the tissue response [17] [15]. Critical parameters include glial scar thickness, neuronal density gradient, and direct measurement of neuron-to-electrode distances.
Essential Research Reagents and Materials for Biofouling Studies
The systematic investigation of biofouling mechanisms and antifouling strategies requires specialized reagents and materials. The following table details essential components of the biofouling researcher's toolkit:
Table 3: Essential Research Reagents for Neural Interface Biofouling Studies
| Reagent Category | Specific Examples | Research Application | Key Performance Metrics |
|---|---|---|---|
| Electrode Substrate Materials | Polyimide, parylene-C, silicone | Flexible electrode fabrication | Young's modulus, bending stiffness, biocompatibility |
| Conductive Coatings | PEDOT:PSS, graphene, CNT, iridium oxide | Interface impedance reduction | Charge storage capacity, charge transfer impedance |
| Immunohistochemistry Antibodies | Anti-GFAP, anti-Iba1, anti-NeuN | Cellular response characterization | Specificity, signal-to-background ratio, species compatibility |
| Anti-inflammatory Compounds | Dexamethasone, minocycline, IL-1ra | Local immunomodulation | Release kinetics, therapeutic concentration, duration of efficacy |
| Surface Modification Reagents | PEG-silane, peptide sequences (RGD, IKVAV) | Biofouling-resistant coatings | Grafting density, stability in physiological conditions |
| Electrochemical Characterization | Phosphate buffered saline, ferro/ferricyanide | In vitro impedance validation | Solution conductivity, redox couple reactivity |
Future Directions and Concluding Perspectives
The progressive deterioration of neural signal quality due to biofouling-induced interface impedance changes remains a fundamental challenge in chronic neural recording research. Future advances will likely emerge from integrated approaches that combine mechanically compliant substrate designs with active biofouling mitigation strategies such as controlled drug release and surface functionalization [17] [15]. Promising research directions include the development of biodegradable shuttle systems that eliminate chronic mechanical mismatch, conducting polymer composites with sustained anti-inflammatory release capabilities, and ultra-low modulus neural interfaces that approach the mechanical properties of brain tissue [17] [21]. Additionally, standardized experimental methodologies and rigorous longitudinal characterization will be essential for objectively comparing the performance of emerging antifouling technologies. As these innovations mature, they hold significant potential to extend the functional longevity of neural interfaces, ultimately enabling reliable decade-long neural recordings for both basic neuroscience research and clinical BCIs applications. The continued convergence of materials science, neural engineering, and immunology will be essential to develop next-generation neural interfaces that maintain signal fidelity by effectively mitigating the biofouling response.
Breakthrough Solutions: Innovative Materials, Electrode Designs, and Signal Processing Techniques
The pursuit of stable, long-term neural recordings represents a cornerstone of modern neuroscience and neuroengineering. The core challenge undermining this goal is the profound mechanical mismatch between conventional rigid neural probes and the soft, dynamic environment of brain tissue. This mismatch initiates a cascade of adverse biological reactions, ultimately leading to the degradation of recording fidelity over time. Traditional probes, typically fabricated from silicon or metals, possess a Young's modulus in the gigapascal (GPa) range, which is millions of times stiffer than brain tissue, with a modulus in the kilopascal (kPa) range [22] [23]. This disparity causes chronic inflammation, neuronal death, and the formation of an insulating glial scar around the implant, which increases electrode impedance and spatially separates the probe from its target neurons, thereby diminishing signal-to-noise ratio (SNR) [22] [17]. In response, ultra-flexible and biointegrated probes have emerged as a transformative solution. By achieving mechanical compatibility with the brain, these probes mitigate the foreign body response, enabling a more stable interface and superior long-term signal fidelity, which is critical for both foundational research and clinical applications such as brain-machine interfaces (BMIs) and therapeutic neuromodulation [24] [17].
Comparative Analysis of Neural Probe Technologies
The evolution of neural probes can be categorized into three distinct generations, each defined by its material composition, structural design, and strategy for interfacing with the brain. The following table provides a systematic comparison of their key characteristics and performance metrics.
Table 1: Performance Comparison of Rigid, Flexible, and Ultra-Flexible/Biointegrated Neural Probes
| Feature | Conventional Rigid Probes | Flexible Polymer Probes | Ultra-Flexible/Biointegrated Probes |
|---|---|---|---|
| Exemplar Technologies | Michigan probes, Utah arrays, Silicon probes [25] [22] | Polyimide-based probes, Open-sleeve electrodes [17] | Mechanically-adaptive (MA) probes, NeuroRoots, ROSE 3D probes, Ultraflexible electrode arrays [24] [26] [17] |
| Primary Materials | Silicon, Tungsten, Metals [25] [22] | Polyimide, Parylene C [17] | Polymer nanocomposites (e.g., PVAc with cellulose nanocrystals), ultra-thin metals [24] [23] |
| Young's Modulus | ~100 GPa (Silicon) [23] | ~1-10 GPa [17] | Dry: ~5 GPaImplanted/Wet: ~10 MPa [23] |
| Key Implantation Method | Direct insertion [25] | Rigid shuttle (e.g., tungsten wire, SU-8) [17] | Rigid shuttle, but with minimal cross-sectional area; ROSE 3D rolling approach [26] [17] |
| Chronic Signal Stability | Degrades over weeks due to glial scarring [22] [23] | Improved over rigid probes; stable recordings for months reported [17] | High stability; demonstrated stable recordings after extended stimulation periods [24] [23] |
| Typical Stimulation Current | ~100-500 µA (for behavioral control) [24] | Information Not Available | ~5 µA (for precise behavioral control in mice) [24] |
| Tissue Response (Gliosis) | Significant glial scar formation [22] [23] | Reduced glial scarring compared to rigid probes [17] | Minimized glial scarring; improved neuronal density near the implant [23] |
| Key Advantage | Reliable surgical insertion | Better mechanical match than rigid probes | Ultimate mechanical compatibility, low-threshold stimulation |
| Key Challenge | Chronic inflammation, signal loss | Requires complex implantation strategies | Fabrication, handling, and implantation complexity |
The experimental data underscores the performance benefits of ultra-flexible probes. A direct comparison of implantation mechanics reveals that flexible probes significantly reduce tissue strain. Furthermore, the functional superiority of ultra-flexible probes is demonstrated by their dramatically lower stimulation thresholds and enhanced recording stability, as shown in the table below.
Table 2: Quantitative Experimental Data from Ultra-Flexible Probe Studies
| Performance Metric | Experimental Finding | Probe Type | Biological Model | Implication |
|---|---|---|---|---|
| Stimulation Current Threshold | ~5 µA to induce turning behavior in mice [24] | Ultraflexible electrode array | Mouse | 1-2 orders of magnitude lower than conventional rigid electrodes, enabling precise neuromodulation with minimal energy [24] |
| Neural Recording Stability | Stable spike recordings maintained after extended electrical stimulation [24] | Ultraflexible electrode array | Mouse | Probes maintain stable electrical contact, indicating health of both neurons and electrodes [24] |
| Single-Unit Recording Yield | Improved active electrode yield and signal amplitude over 12 weeks [23] | MARE (Mechanically-adaptive, resveratrol-eluting) probe | Rat | Combination of flexibility and anti-inflammatory drug delivery supports chronic recording stability [23] |
| Post-Implantation Elastic Modulus | Softens from ~5 GPa (dry) to ~10 MPa (implanted) [23] | MARE probe | In vitro / ex vivo | Reduces mechanical mismatch with brain (~10 kPa) by a factor of 10âµ compared to silicon [23] |
| Gene Expression & Tissue Response | Healing tissue response and reduced expression of pro-inflammatory markers [23] | MARE probe | Rat | Probe integration attenuates key drivers of the neuroinflammatory cascade, favoring a healing environment [23] |
Experimental Protocols for Validating Probe Performance
Protocol 1: In Vivo Electrophysiology and Behavioral Modulation
This protocol is designed to quantify the efficacy of ultra-flexible probes in recording neural activity and evoking specific behaviors through low-threshold electrical stimulation [24].
- Objective: To validate the functionality of ultraflexible electrode arrays in simultaneously recording single-neuron spikes and modulating complex motor behavior with high precision and low current.
- Probe Implantation: Ultraflexible electrode arrays are implanted into the target brain region, such as the secondary motor cortex (M2) of mice, using a rigid shuttle (e.g., tungsten wire) for guidance. The shuttle is retracted after implantation, leaving the flexible probe in place [17].
- Neural Recording & Behavior Correlation: In freely moving mice, neural signals (spike firings) are recorded continuously alongside video tracking of animal behavior. The firing rates of individual neurons are correlated with motion parameters (e.g., velocity) to confirm proper probe placement and functional recording [24].
- Low-Current Electrical Stimulation: Biphasic, charge-balanced current pulses are delivered through individual microelectrodes on the array. A typical waveform consists of a 200 µs cathodic phase, a 100 µs interphase delay, and a 400 µs anodic phase at half the amplitude, delivered at 100 Hz. The current is systematically varied to find the minimum threshold (e.g., ~5 µA) required to reliably evoke a contralateral turning behavior [24].
- Data Analysis: Angular and linear displacement of the animal are quantified from video tracking. The specificity of behavior induction is assessed by stimulating different electrodes within the array to map functional brain regions [24].
Protocol 2: Finite Element Analysis of Implantation Mechanics
This computational protocol assesses the mechanical interaction between the probe and brain tissue during and after insertion, providing a basis for optimizing probe design [25].
- Objective: To simulate the implantation process and quantify induced stresses and strains in brain tissue, predicting the potential for acute and chronic tissue damage.
- Model Establishment: A finite element (FE) model is developed using a Coupled Eulerian-Lagrangian (CEL) method in software like ABAQUS. The probe is modeled as a Lagrangian solid with precise geometric dimensions, while the brain tissue is represented as an Eulerian domain to accommodate large deformations [25].
- Material Properties: Brain tissue is modeled as a hyperelastic, viscoelastic material to capture its nonlinear, strain-rate-dependent mechanical behavior. Material parameters are derived from experimental tests on ex vivo porcine brain tissue, which is biomechanically comparable to human tissue [25].
- Simulation Parameters: The model simulates the insertion of single-shank and multi-shank arrays at controlled speeds (e.g., 1 mm/s) to a specified depth (e.g., 1 mm). Parameters such as implantation force, stress distribution, and strain fields in the tissue are calculated [25].
- Experimental Validation: The simulation results, particularly the force-displacement profiles, are validated against physical implantation experiments using the same probe designs and fresh porcine brain tissue [25].
The workflow and key interactions in the neural tissue response to an implanted probe are illustrated below.
(caption: Signaling Pathways in the Brain Tissue Response to Neural Probes) This diagram contrasts the detrimental cascade triggered by mechanically mismatched rigid probes (red nodes) with the beneficial outcomes promoted by ultra-flexible and biointegrated strategies (green nodes). Dashed green lines represent inhibitory effects, showing how flexibility and drug elution disrupt the pathway to signal failure.
The Scientist's Toolkit: Essential Reagents and Materials
Successful development and deployment of ultra-flexible neural probes rely on a suite of specialized materials and reagents. The following table details key components of the research toolkit.
Table 3: Essential Research Reagent Solutions for Ultra-Flexible Neural Probes
| Reagent/Material | Function | Application Example |
|---|---|---|
| Polyvinyl Acetate (PVAc) & Cellulose Nanocrystals | Forms the mechanically-adaptive polymer nanocomposite substrate; rigid for insertion, softens upon implantation [23]. | Core substrate material for MARE probes [23]. |
| Parylene C | A biocompatible polymer used as a thin-film insulation layer to encapsulate metal traces and control drug release kinetics [23]. | Insulation and diffusion-control layer in MARE probes [23]. |
| Resveratrol | A natural polyphenol antioxidant incorporated into the probe substrate for local elution to mitigate oxidative stress and neuroinflammation [23]. | Active drug component in MARE probes to scavenge reactive oxygen species (ROS) [23]. |
| Gold (Au) & Titanium (Ti) | Thin-film metals used for conductive traces (Au) and as an adhesion layer (Ti) between the substrate and metal [25] [23]. | Microelectrodes and interconnects in flexible probe fabrication [24] [23]. |
| Titanium Nitride (TiN) | A conductive and biocompatible material coating electrode sites to lower interfacial impedance and increase charge injection capacity [25]. | Functional modification layer on electrode contact points [25]. |
| Polyethylene Glycol (PEG) | A biodegradable polymer used as a temporary coating to secure a rigid shuttle to a flexible probe, dissolving after implantation to release the shuttle [17]. | "Glue" in tungsten wire-guided implantation of rod-like flexible electrodes [17]. |
| Selfotel | Selfotel, CAS:110347-85-8, MF:C7H14NO5P, MW:223.16 g/mol | Chemical Reagent |
| Mogroside IIA1 | Mogroside IIA1, CAS:88901-44-4, MF:C42H72O14, MW:801.0 g/mol | Chemical Reagent |
The evidence unequivocally demonstrates that ultra-flexible and biointegrated neural probes represent a paradigm shift in neural interface technology. By fundamentally addressing the problem of mechanical mismatch, these probes successfully attenuate the chronic neuroinflammatory response, which is the primary obstacle to long-term signal fidelity. The resulting stability in single-unit recording and the ability to achieve precise neuromodulation with exceptionally low currents underscore a future where high-performance brain-computer interfaces can operate reliably for decades. Future developments will likely focus on integrating multi-modal functionalities, such as electrical recording, stimulation, and drug delivery, into ever-smaller and more compliant form factors. Furthermore, the creation of sophisticated 3D interfaces, such as those enabled by the ROSE technique, will allow for unprecedented mapping and modulation of neural circuits across different depths [26]. As materials science and implantation strategies continue to advance, the distinction between man-made devices and neural tissue will continue to blur, finally providing neuroscientists and clinicians with the robust and stable tools needed to unlock the brain's deepest secrets and treat its most debilitating diseases.
Brain-computer interfaces (BCIs) enable direct communication between the brain and computers, offering transformative potential for treating neurological disorders and restoring neural functions. However, their long-term functionality remains severely limited by signal degradation caused by acute insertion trauma, chronic foreign body reaction (FBR), and biofouling at the device-tissue interface [10] [27]. When implanted, conventional neural devices trigger a cascade of biological responses, including acute inflammation from surgical trauma that progresses to chronic FBR, often leading to glial scarring and eventual encapsulation of the device [27]. This insulation effect increases the distance between neurons and electrode sites, causing rapid signal attenuation and a sharp rise in impedance, ultimately compromising signal quality and long-term functionality [17].
Surface engineering has emerged as a critical strategy to mitigate these challenges. While various antifouling surface modifications have demonstrated success in reducing immune responses, their extreme repellency often inhibits direct interaction between the device and neurons, diminishing neural recording sensitivity and selectivity [27]. Similarly, approaches featuring biomolecule conjugation to promote neural interaction often suffer from rapid biodegradation in vivo [27]. To address these competing challenges, a new class of bioadaptive coatings has been developed, with the Targeting-specific interaction and Blocking nonspecific adhesion (TAB) coating representing a particularly advanced solution that achieves synergistic integration of mechanical compliance and biochemical stability for transformative long-term neural recording capabilities.
Technology Comparison: TAB Coating Versus Alternative Approaches
TAB Coating: Mechanism and Composition
The TAB coating employs a sophisticated dual-functional design that combines brain-derived neurotrophic factor (BDNF) conjugation with a lubricant-infused surface [10] [27]. This architecture features alternately immobilized perfluorosilane (PFS) and aminosilane layers. The PFS component imparts low surface energy for holding a slippery lubricant layer, while the aminosilane serves as an anchor for BDNF [27]. The immobilized BDNF facilitates selective interaction with neurons and astrocytes by binding to tropomyosin receptor kinase B (TrkB) receptors, while the lubricant layer repels nonspecific adhesions, reducing the attachment of blood and plasma proteins to less than 3% [27].
This design enables multiple protective functions: the lubricant layer minimizes friction during insertion, reducing acute insertion trauma, while simultaneously preventing immune cell adhesion and migration to the BDNF, which prevents immune cell activation and degradation of the biomolecules [27]. Meanwhile, the BDNF component promotes beneficial interactions with neural cells, supporting survival and growth of neurons and astrocytes, particularly promoting the neuroprotective A2 astrocyte subtype [27].
Comparative Analysis of Neural Interface Coatings
Table 1: Performance Comparison of Neural Interface Coating Technologies
| Coating Technology | Mechanism of Action | Signal Stability Duration | Cell Adhesion Profile | Key Limitations |
|---|---|---|---|---|
| TAB Coating | BDNF conjugation + lubricant-infused surface | >12 months [10] [27] | Selective (↑ neurons/astrocytes, ↓ immune cells) [27] | Complex fabrication process |
| Hydrophilic Coatings | Surface hydration layer prevents protein adsorption | Months [28] | Non-specific reduction [27] | Inhibits neural interaction, limited long-term stability |
| Diamond-Like Carbon (DLC) | Physical barrier with biocompatibility | Limited long-term data [29] | Non-specific reduction [29] | Requires precise tip exposure, no bioactive component |
| Biomolecule Conjugation | Peptides/proteins promote specific interactions | Limited by biodegradation [27] | Selective (↑ neural cells) | Subject to enzymatic degradation, doesn't address friction |
| Antifouling Polymers | Steric hindrance prevents protein adhesion | Months [30] | Broad-spectrum reduction [27] | Also repels beneficial neural interactions |
Table 2: Quantitative Performance Metrics of Coating Technologies
| Performance Metric | TAB Coating | Hydrophilic Coatings | DLC-UME | Uncoated Controls |
|---|---|---|---|---|
| Protein Adhesion Reduction | >97% [27] | ~90% [28] | Not specified | Baseline |
| Neuronal Cell Coverage | ~65% after 1 week [27] | <10% [27] | Not specified | ~20% declining |
| Acute Insertion Trauma | Significantly reduced [27] | Moderate | Not specified | High |
| Chronic FBR Suppression | High [10] | Moderate [17] | Not specified | Minimal |
| Single-Unit Recording Stability | >12 months [10] | 3-6 months [17] | Improved short-term [29] | Weeks to months |
Experimental Analysis: Methodologies and Data Interpretation
TAB Coating Fabrication and Evaluation Protocols
The experimental validation of TAB coatings followed rigorous methodologies across multiple studies. The coating was applied to flexible multifunctional neural fibers fabricated through a thermal drawing process (TDP), which allows miniaturization and integration of functional modalities into fibers by preserving the cross-sectional structure [27]. The resulting microscale polymeric fiber exhibited exceptional flexibility with a flexural rigidity of 1.49 × 10â»â· N/m² [27].
The TAB coating application process involved:
- Surface Functionalization: Sequential immobilization of perfluorosilane (PFS) and aminosilane layers onto the fiber surface [27].
- BDNF Conjugation: Covalent attachment of brain-derived neurotrophic factor to the aminosilane anchors [27].
- Lubricant Infusion: Application of a thin lubricant layer onto the PFS component to create a slippery surface [27].
Performance characterization included:
- Antifouling Assessment: Quantification of blood and plasma protein adhesion using fluorescence tagging [27].
- Cell Selectivity Evaluation: Co-cultures of neurons, astrocytes, and immune cells to measure selective adhesion [27].
- Electrochemical Analysis: Electrode impedance and charge transfer efficiency measurements [27].
- In Vivo Validation: Long-term implantation in mouse models with continuous neural signal monitoring [27].
Ultramicroelectrode Tip Exposure Control Methodology
Complementary research on ultramicroelectrodes (UMEs) provides additional insights into precision surface engineering. A recent study developed a novel technique using a cold atmospheric microplasma jet to control the exposure of ultramicroelectrode tips protected with diamond-like carbon (DLC) coatings [29]. The methodology included:
- DLC Deposition: Conformal coating of UMEs with protective diamond-like carbon [29].
- Selective Removal: Precision exposure of electrode tips using microplasma jet treatment with submicron accuracy [29].
- Biocompatibility Validation: Cell culture with neuronal cells to confirm non-adverse effects on growth [29].
- Electrochemical Testing: Impedance spectroscopy and intracellular pH detection to verify performance [29].
This approach demonstrated that controlled tip exposure significantly improves signal-to-noise ratio and sensitivity while maintaining biocompatibility [29].
Signaling Pathways in TAB-Coated Neural Interfaces
The TAB coating's exceptional performance stems from its orchestrated interaction with specific biological pathways. The diagram below illustrates the key signaling mechanisms involved in the tissue response to TAB-coated neural interfaces.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Bioadaptive Coating Development
| Reagent/Material | Function | Application Context |
|---|---|---|
| Brain-Derived Neurotrophic Factor (BDNF) | Promotes neural cell adhesion and survival via TrkB receptors [27] | TAB coating bioactive component |
| Perfluorosilane (PFS) | Creates low-energy surface for lubricant retention [27] | TAB coating antifouling component |
| Aminosilane | Provides anchoring sites for biomolecule conjugation [27] | TAB coating immobilization |
| Polyethylene Glycol (PEG) | Temporary stiffening agent for implantation [17] | Flexible electrode delivery |
| Diamond-Like Carbon (DLC) | Protective biocompatible coating with mechanical strength [29] | Ultramicroelectrode insulation |
| Poly(3,4-ethylenedioxythiophene):Poly(styrenesulfonate) (PEDOT:PSS) | Conductive polymer for electrode interface [31] | Neural recording and stimulation |
| Hydroxyapatite | Bioceramic promoting bone integration [30] | Orthopedic and dental implants |
| Phosphorylcholine | Mimics cell membranes for blood compatibility [30] | Cardiovascular devices |
| Gold Nanowires | Conductive nanomaterial for flexible electronics [31] | Stretchable neural interfaces |
| Silk Fibroin | Biocompatible, programmable substrate [31] | Flexible bioelectronic implants |
| SSTR5 antagonist 2 | SSTR5 antagonist 2, CAS:1254730-81-8, MF:C32H35FN2O5, MW:546.6 g/mol | Chemical Reagent |
| Isorhoifolin | Isorhoifolin, CAS:36790-49-5, MF:C27H30O14, MW:578.5 g/mol | Chemical Reagent |
Comparative Data Interpretation: Quantitative Advantages of TAB Coatings
Long-Term Performance Metrics
The exceptional long-term performance of TAB coatings is demonstrated through quantitative comparison with alternative approaches. In vivo studies showed that TAB-coated fibers maintained high-quality single-unit neural signals for more than 12 months post-implantation, significantly outperforming uncoated controls which typically lost signal recording capability within a few months [27]. This represents one of the longest stable recording durations reported in the literature for implantable neural interfaces.
Cell culture studies further quantified the selective interfacial properties of TAB coatings, demonstrating approximately 25% neural cell coverage after 1 day, proliferating to 65% after 1 week [27]. This contrasts sharply with conventional antifouling coatings which typically show less than 10% neural cell coverage due to their non-specific repellency [27]. The TAB coating's ability to simultaneously promote desired neural interactions while minimizing unwanted immune cell adhesion represents a fundamental advancement in surface engineering for neural interfaces.
Mechanical and Biochemical Synergy
The experimental data reveals that the TAB coating's success derives from its synergistic combination of mechanical and biochemical mitigation strategies. The lubricant component reduces friction during implantation, minimizing acute tissue trauma, while simultaneously creating a barrier that protects conjugated BDNF from proteolytic degradation and immune cell recognition [27]. This dual functionality addresses both the initial insertion damage and chronic degradation pathways that conventionally limit coating lifespan.
Electrochemical impedance spectroscopy demonstrated that TAB-coated electrodes maintained stable electrical properties throughout the 12-month implantation period, with significantly lower increases in interface impedance compared to uncoated controls [27]. This indicates that the coating successfully mitigated the glial scarring and encapsulation that typically degrades electrode performance over time.
TAB coatings represent a significant paradigm shift in neural interface design, moving beyond singular-function coatings toward multifunctional surface systems that actively manage the biological interface. The experimental data demonstrates that the integration of mechanical compliance, selective biochemical signaling, and broad-spectrum antifouling properties enables unprecedented long-term signal stability exceeding 12 months [10] [27].
Future developments in this field will likely focus on increasingly sophisticated bioadaptive systems featuring stimulus-responsive components, personalized biomolecule combinations, and even more seamless integration with neural tissue. As research advances, these coating technologies promise to enable a new generation of chronically stable neural interfaces for both fundamental neuroscience research and clinical applications in neurological disorders and brain-computer interfaces.
The exceptional performance of TAB coatings establishes a new benchmark for neural interface stability and highlights the critical importance of surface engineering in overcoming the biological challenges that have traditionally limited long-term neural implantation success.
In the field of long-term neural recording research, signal fidelity is paramount for accurately diagnosing and monitoring brain diseases. The performance of implantable ultramicroelectrodes (UMEs), essential tools for intracellular signal detection at the single-cell level, critically depends on the precise control of their tip exposure. Traditional fabrication methods have struggled to achieve the submicron-scale precision required for optimal electrode performance, often resulting in unsatisfactory signal-to-noise ratios and compromised signal stability [32] [33]. This guide objectively compares a groundbreaking microplasma jet processing technique against conventional alternatives, providing researchers and drug development professionals with experimental data and protocols to inform their neural interface work.
The Technical Challenge: Tip Exposure Control in Neural Recording
Ultramicroelectrodes (UMEs), typically with diameters less than 10 μm, offer significant advantages for neural recording, including high spatiotemporal resolution, targeted neuron regulation, and excellent biocompatibility [32]. However, their performance heavily depends on the reliable protection of areas outside the signal acquisition points at their sharp tips.
Consequences of Improper Tip Exposure
- Excessive Exposure: Leads to portions of the sensing surface remaining outside the cell, making the UME susceptible to environmental interference and increasing unknown noise signals [32].
- Insufficient Exposure: Results in an inadequate contact area between the tip functional layer and intracellular environment, leading to excessively high impedance that affects charge transfer capability and reduces signal-to-noise ratio [32].
Traditional methods like wax encapsulation suffer from poor controllability of thickness and coverage quality, leading to inconsistent performance and stability issues [32]. Other approaches, including HF etching of quartz protective layers or inserting nanowires into glass micropipettes, still struggle with uncontrollable exposed tip lengths [32].
Microplasma Jet Processing: A Paradigm Shift in UME Fabrication
Core Technological Innovation
Researchers from Shanghai Jiao Tong University have developed a novel approach using cold atmospheric microplasma jet processing to precisely control UME tip exposure [33] [34]. The method involves:
- Protective Coating: Utilizing diamond-like carbon (DLC) film as a protective coating for UMEs, selected for its superior mechanical properties, high thermal stability, biocompatibility, and biochemical inertness [32].
- Precision Processing: Employing microplasma jet technology for site-selective removal of the DLC coating from UME tips, enabling submicron-scale control over the exposed functional structure [32].
Experimental Protocol and Methodology
The experimental workflow for this innovative fabrication technique involves multiple precise steps, as visualized below:
Figure 1: Experimental workflow for microplasma jet processing of UME tips
- Microplasma Jet Generator: Fabricated using 3D printing technology (MicroArch S240A)
- High Voltage Amplifier: Trek Model 30/20A for plasma generation
- Motion System: Six-degree-of-freedom mechanical arm (JAKA Zu 3) with five-axis motion platform
- Nozzle Preparation: Quartz capillary pulled to 8 μm inner diameter using CO₂ laser puller (P-2000)
- Process Monitoring: Observation camera (MER2-2000-19U3C) and visual positioning camera
- Microstructural Analysis: Field emission scanning electron microscope (JSM-7800F)
- Elemental Composition: Energy dispersive spectroscopy (EDS)
- Phase Composition: X-ray diffraction (XRD, D8 ADVANCE Da Vinci)
- Electrochemical Performance: Cyclic voltammetry and electrochemical impedance spectroscopy in phosphate buffer saline (pH 7.4)
Performance Comparison: Quantitative Analysis
Fabrication Precision and Electrochemical Performance
Table 1: Comparative analysis of UME fabrication technologies
| Fabrication Technology | Control Precision | Signal-to-Noise Ratio | Long-term Stability | Key Limitations |
|---|---|---|---|---|
| Microplasma Jet + DLC | Submicron scale [32] | Significantly improved [33] | High (weeks) [32] | Requires specialized equipment |
| Wax Encapsulation | Poorly controllable [32] | Variable/unsatisfactory [32] | Moderate | Thickness and coverage quality difficult to control |
| HF Etching of Quartz | Uncontrollable [32] | Moderate | Not reported | Excessive tip exposure issues |
| Flexible Polyimide Probes | N/A (different approach) [35] | Good | Moderate to high | Biocompatibility debates around SU-8 [35] |
| Carbon Fiber Electrodes | N/A (different approach) [36] | Good | Good for chronic recording | Limited to specific electrode types |
Biocompatibility and Functional Validation
Table 2: Experimental validation results for microplasma-processed DLC-UMEs
| Test Parameter | Methodology | Results | Significance |
|---|---|---|---|
| Biocompatibility | HT22 cell culture with GFP fluorescence [32] | No adverse effects on normal neuron growth [32] | Safe for biological application |
| Electrochemical Stability | Aging tests in PBS [32] | Good stability demonstrated [32] | Suitable for long-term implantation |
| Intracellular Recording | Real-time pH monitoring in single cells [32] | High-fidelity signal detection [32] | Accurate intracellular sensing capability |
| Mechanical Properties | DLC coating characteristics [32] | Superior mechanical strength, thermal stability [32] | Withstands implantation stresses |
Comparative Advantages for Neural Signal Fidelity
The microplasma jet processing technique demonstrates distinct advantages for long-term neural recording applications, particularly when compared to alternative approaches described in the literature.
Signal Fidelity Improvements
- Noise Reduction: Precisely controlled tip exposure significantly reduces environmental interference and unknown noise signals [32] [33]
- Impedance Optimization: Balanced exposure length maintains optimal electrode impedance for improved charge transfer capability [32]
- Spatial Precision: Enables targeted detection of specific biological or chemical signals in subcellular regions [32]
Long-term Performance Advantages
The enhanced stability of microplasma-processed DLC-UMEs addresses a critical challenge in neural interface technology. Traditional silicon-based MEAs trigger immune responses and perform poorly for chronic recordings due to their rigid material properties [36]. While flexible polyimide probes offer improved biocompatibility [35], they still lack the precise tip exposure control achieved through microplasma processing.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research materials for UME fabrication and testing
| Material/Reagent | Specification/Source | Primary Function |
|---|---|---|
| Diamond-Like Carbon (DLC) | Coating material [32] | Electrode protection, electrical insulation |
| Photosensitive Polyimide | Durimide 7505 (Fujifilm) [35] | Flexible substrate for neural implants |
| HT22 Cell Line | Hippocampal neuronal cells (Sigma-Aldrich) [32] | Biocompatibility testing model |
| Phosphate Buffer Saline | 10 mM, pH 7.4 [32] | Electrochemical testing medium |
| Polyethylene Glycol | MW 8000 g/mol [35] | Temporary bonding for implantation |
| Ag/AgCl | Reference electrode material [37] | Stable reference potential for electrochemical systems |
| Hosenkoside G | Hosenkoside G, MF:C47H80O19, MW:949.1 g/mol | Chemical Reagent |
| Borapetoside B | Borapetoside B, MF:C27H36O12, MW:552.6 g/mol | Chemical Reagent |
Implementation Workflow and Technical Considerations
The relationship between tip exposure control and signal fidelity involves multiple interconnected factors that researchers must consider:
Figure 2: Signaling pathway of how precision tip exposure enhances neural signal fidelity
Practical Implementation Guidelines
- Equipment Requirements: The microplasma jet system requires significant capital investment and technical expertise to implement
- Process Optimization: Processing time must be carefully calibrated to achieve desired exposure length without damaging underlying electrode material
- Quality Control: Regular characterization using SEM and EDS is essential to maintain fabrication consistency
- Alternative Approaches: For laboratories without access to microplasma technology, carbon fiber electrodes provide a viable alternative for chronic neural recording with minimal tissue damage [36]
The microplasma jet processing technique for controlling ultramicroelectrode tip exposure represents a significant advancement in neural interface technology. By enabling submicron-scale precision in tip exposure control, this method directly addresses the fundamental challenge of balancing signal fidelity with long-term stability in neural recording applications. The quantitative data presented in this guide demonstrates clear advantages over traditional fabrication methods, particularly for research requiring high-precision intracellular monitoring, such as neurodegenerative disease research and pharmaceutical development. While the technique requires specialized equipment, its demonstrated benefits in biocompatibility, electrochemical stability, and signal quality make it a valuable approach for advancing single-cell analysis and brain-computer interface technologies.
The evolution of brain-implantable microsystems toward higher channel counts is a defining trend in neuroscience and neuroprosthetics. Modern microelectrode arrays now boast thousands of recording channels, enabling unprecedented access to neural circuits with high spatial and temporal resolution [6] [38]. However, this enhanced recording capability creates a critical bottleneck: the handling and wireless transmission of massive data volumes within the strict power and thermal constraints of an implantable device [6] [39]. For instance, a conventional 1000-channel system sampling at 20 kHz with 9-bit resolution generates a raw data rate of 180 Mbps, demanding approximately 250 mW for transmission—far exceeding the safe implantable power budget of ~35 mW [39].
Consequently, sophisticated on-implant signal processing for data reduction has become not merely beneficial but essential for next-generation neural interfaces [6]. This guide focuses on two cornerstone techniques enabling this data reduction: spike detection and neural compression. We objectively compare the performance of state-of-the-art algorithms and hardware implementations, framing their development within the broader research thesis of maintaining long-term signal fidelity—the accurate preservation of neural information essential for meaningful scientific and clinical outcomes.
Spike Detection Techniques
Spike detection is the first critical step in neural data reduction, acting as a gatekeeper that identifies action potentials (the primary information-carrying signals) while discarding background noise. The choice of detection strategy directly impacts data volume and downstream analysis fidelity.
Core Methodologies and Experimental Protocols
Traditional Amplitude Thresholding: The most established protocol involves setting a voltage threshold, typically based on the noise floor's root-mean-square (RMS). A spike is registered when the signal crosses this threshold. Advanced implementations feature adaptive thresholds that adjust to slow changes in signal amplitude [40]. The experimental protocol is straightforward: the neural signal is bandpass filtered (e.g., 300–5000 Hz), the RMS noise level is estimated, and a threshold is set (e.g., -4 to -5 times the RMS value). Detected events are time-stamped and waveform snippets are extracted.
Machine Learning-Based Detection: Newer protocols leverage machine learning for improved noise immunity. The Artificial Neural Network Spike Detector (ANN-SPD) uses a simple, fully connected network to process event-based data. Its experimental protocol involves converting the continuous neural signal into an event stream via delta modulation, then feeding binned event counts into the ANN for classification [40].
Neuromorphic Approaches: The most recent advancement is the Spiking Neural Network Spike Detector (SNN-SPD). Its experimental protocol is detailed in Figure 1 and involves:
- Event Generation: A delta modulator converts the analog neural signal into a stream of ON/OFF pulses based on predefined voltage thresholds [40].
- Pulse Count Modulation (PCM): These pulses are accumulated over short time bins (
Ts) to create integer-valued event counts [40]. - SNN Processing: The event counts are fed into an SNN, which leverages its inherent temporal dynamics to detect spike patterns with high efficiency [40].
Figure 1: SNN-SPD Experimental Workflow. The continuous signal is converted to sparse events before processing by a power-efficient Spiking Neural Network [40].
Performance Comparison of Spike Detectors
The following table quantitatively compares the performance of different spike detection methods, highlighting the trade-offs between accuracy and computational efficiency.
Table 1: Performance Comparison of Spike Detection Methods
| Detection Method | Core Principle | Reported Accuracy | Computational / Hardware Cost | Key Advantage |
|---|---|---|---|---|
| Amplitude Thresholding [40] | Signal crosses a set voltage threshold | Varies with SNR | Very low; simple comparator | Extreme hardware efficiency, simple implementation |
| Event Count (Ev-SPD) [40] | Spike decision based on count of events in a time bin | Lower than ANN/SNN | Very low; basic counter | High computational efficiency, operates on event data |
| ANN-SPD [40] | Artificial Neural Network classifies event data | ~93.7% (Noise σ=0.2) | High (Baseline for comparison) | High detection accuracy in noisy conditions |
| SNN-SPD (Proposed) [40] | Spiking Neural Network classifies event data | 95.72% (Noise σ=0.2) | 0.41% of ANN-SPD computations, 26.62% of weights | Optimal balance: high accuracy & very low power |
Neural Signal Compression Techniques
After detection, the extracted spike waveforms can be further compressed. Compression techniques are broadly categorized as lossless (perfect reconstruction), near-lossless (minimal error), and lossy (acceptable error for a large compression gain).
Core Methodologies and Experimental Protocols
Salient Sample Extraction & Curve Fitting: This innovative, hardware-efficient protocol involves:
- Spike Segmentation: Isolate a window of the signal containing a single spike.
- Salient Point Identification: Algorithmically identify key points defining the spike's shape: the start, end, and all local minimum and maximum points (extrema). This is a form of "selective downsampling" [8].
- Attribute Transmission: Transmit only the timing (sample index) and amplitude of these salient points.
- External Reconstruction: On the external receiver, reconstruct the full spike waveform by fitting smooth curves (e.g., third-degree polynomials) between the transmitted salient points [8]. The workflow is illustrated in Figure 2 below.
Figure 2: Compression via Salient Sample Extraction. Computationally simple on-implant steps (blue) are paired with complex reconstruction off-implant [8].
Transform-Based Compression (WHT/DWT): This class of protocols transforms the spike signal into a different domain where it is more easily compressed.
- Transform Calculation: Apply a transform like the Walsh-Hadamard Transform (WHT) or Discrete Wavelet Transform (DWT) to the spike waveform [6] [39].
- Coefficient Thresholding: Discard transform coefficients with magnitudes below a certain threshold, which are deemed to contribute less to the signal's energy and shape.
- Encode & Transmit: Transmit only the significant coefficients and their locations.
- Reconstruction: On the external side, apply the inverse transform to reconstruct an approximation of the original spike.
Performance Comparison of Compression Techniques
The table below compares the performance of different compression techniques, using key metrics like Space Saving Ratio (SSR) and power consumption.
Table 2: Performance Comparison of Neural Compression Techniques
| Compression Technique | Compression Type | Key Metric | Power Consumption | Key Advantage / Disadvantage |
|---|---|---|---|---|
| Spike Detection & Extraction [39] | Lossy (discards background) | Data rate reduced to 36.2-59.6 Mbps (for 1000 ch) | N/A | Foundational reduction; discards LFP and noise |
| Salient Sample Extraction [8] | Lossy (model-based) | Avg. Compression Rate: ~2176 (at 8 Spike/s) | 0.164 µW/channel | Extreme hardware efficiency and high compression |
| Intra-Channel Compression (ICE) [39] | Near-Lossless | SSR: ~91% (for Action Potentials) | ~17 μW/Ch (scalability limit) [39] | High-fidelity reconstruction, good SSR |
| Walsh-Hadamard Transform [39] | Lossy | SSR: ~90% (at ~55-60 Spike/s) | Moderate | Good balance of performance and complexity |
The Scientist's Toolkit: Research Reagent Solutions
Translating these algorithms into physical implants requires a suite of specialized technologies. The following table details key components and their functions in a modern neural recording microsystem.
Table 3: Essential Components for an Implantable Neural Signal Processing System
| Component / Technology | Function / Specification | Role in the System |
|---|---|---|
| High-Density Microelectrode Array [6] [38] | 100s to 1000s of recording sites; low interface impedance. | The sensor; acquires raw neural signals from the brain tissue. Signal quality (SNR) is foundational. |
| Analog Front-End (AFE) [39] | Amplification, filtering (e.g., 0.1Hz-7.8kHz), analog-to-digital conversion (e.g., 9-10 bit). | Preconditions the weak, noisy neural signal for digital processing. |
| 22nm FDSOI CMOS Technology [39] | Fully-Depleted Silicon-On-Insulator process. | Enables ultra-low-power and dense integration of digital processing circuits on the implant. |
| System-on-Chip (SoC) with RISC-V Processor [39] | Programmable ultra-low-power core (e.g., 5.19 μW/MHz). | Provides flexibility for on-chip training, adaptation, and control of signal processing tasks. |
| Hermetic Titanium Enclosure [41] | Biocompatible, sealed package with specialized feedthroughs. | Protects active electronics from the harsh biological environment long-term. |
| Luminol sodium salt | Luminol sodium salt, MF:C8H7N3NaO2, MW:200.15 g/mol | Chemical Reagent |
| D-(+)-Cellotriose | Globotriose | Research Grade | | High-purity Globotriose for researching Shiga toxin & UTI mechanisms. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
The pursuit of higher-density neural recording brain implants is inextricably linked to advances in on-implant signal processing. As this guide has detailed, the field is moving beyond simple spike detection toward a sophisticated ecosystem of algorithms, including neuromorphic SNN classifiers and model-based compression using salient points.
The quantitative comparisons reveal a clear trend: the next generation of high-channel-count implants will be powered by solutions that strategically distribute complexity. Computationally simple tasks are performed on the implant under extreme power constraints, while more complex reconstruction is handled externally. Furthermore, programmability is becoming critical, allowing implants to adapt to changing neural environments [39].
The overarching thesis of maintaining signal fidelity in long-term recordings is served by this progress. Efficient data reduction mitigates the thermal load on implant electronics and surrounding tissue, a key factor in long-term stability [38]. By enabling the transmission of high-information-content data (spikes) while discarding noise and redundancy, these spike detection and compression techniques ensure that the decoded neural signal remains a faithful representation of brain activity, paving the way for robust and chronic brain-machine interfaces.
For researchers investigating neurological disorders and developing therapeutic interventions, the ability to reliably record neural activity over extended periods is paramount. Traditional neural probes, often constructed from rigid materials like silicon or metal, face a significant challenge: their mechanical mismatch with soft brain tissue provokes chronic inflammatory responses, leading to glial scarring, neuronal loss, and the eventual degradation of signal fidelity over time [42]. This limitation impedes both fundamental neuroscience research and the development of long-term diagnostic and treatment solutions.
Multimodal neural interfaces that combine optical stimulation for precise neuromodulation (e.g., optogenetics) with simultaneous electrical recording represent a powerful tool for dissecting neural circuit dynamics. However, integrating these functionalities into a single, robust device has proven difficult. Early "add-on" strategies, which attach electrical components to optical fibers, often suffer from mechanical rigidity, compromised electrical performance, and poor biocompatibility, limiting their clinical applicability [43]. The field is now advancing towards monolithic probes—unified devices where electrodes are seamlessly fabricated within the probe's structure. These next-generation probes, alongside other innovative designs like fully printed and vertically integrated systems, are pioneering new paths to achieve stable, long-term neural interfacing by prioritizing mechanical compatibility with neural tissue [43] [44] [45].
This guide provides an objective comparison of emerging neural probe technologies, focusing on their performance in sustaining signal fidelity. We summarize quantitative experimental data and detail key methodologies to inform the selection and development of tools for advanced neural recording research.
Performance Comparison of Neural Probe Technologies
The evolution of neural probes has yielded distinct technological approaches, each with unique advantages and trade-offs. The table below provides a performance comparison of monolithic probes against other established and emerging technologies.
Table 1: Performance Comparison of Neural Probe Technologies for Long-Term Recording
| Technology | Key Characteristics | Impedance (at 1 kHz) | Stability & Biocompatibility | Estimated Longevity | Key Advantages | Major Limitations |
|---|---|---|---|---|---|---|
| Monolithic Probes [43] | Electrodes embedded via laser writing into a biocompatible polymer coating on an optical fiber. | ~600 Ω (Gold NP) | Low inflammatory response; stable impedance after 100+ bending cycles; <15% signal amplitude decrease after 16 weeks in vitro. | ≥16 weeks (demonstrated in mice) | Seamless integration, high mechanical endurance, improved biocompatibility. | Fabrication requires specialized laser equipment. |
| Liquid Metal Printed Probes [44] | Liquid metal (EGaIn) printed into neuron-like patterns; can be coated with PtB. | 415 kΩ (PtB/EGaIn), 1.17 MΩ (pristine EGaIn) | Minimal invasiveness; stable single-unit recording for up to 33 weeks in vivo; elastic modulus similar to brain tissue. | ≥33 weeks (demonstrated in mice) | Customizable design, direct printing on cranium, self-healing capability. | High inherent impedance, requires PtB coating for viable signals. |
| Flexible Lightweight Integrated Devices (FLIDs) [45] | Flexible polyimide probes vertically integrated with chips using through-polymer vias (TPV). | ~60 kΩ (with Pt-Ir alloy coating) | Reduced tissue damage and immune response; weight reduced by 75% vs. conventional devices. | ≥2 months (post-implantation immunohistochemistry in mice) | Ultra-lightweight, reduces animal behavior impact, high channel count potential. | Integration complexity, reliance on specific packaging for chips. |
| 3D-Printed Opto-Fluidic Probes [46] | Custom 3D-printed probes integrating µLEDs and microfluidic channels for drug/delivery. | N/A (Focus on optical and fluidic functions) | Reduced inflammatory response (GFAP, ED1); allows combined implantation and viral delivery in one surgery. | N/A (Study focused on acute biocompatibility and function) | Rapid customization, combines optical stimulation and fluid delivery, high accessibility. | Potential tissue heating from µLEDs requires thermal management. |
Experimental Protocols and Methodologies
To ensure the reproducibility of results and facilitate a deeper understanding of the data presented in the comparison table, this section outlines the core experimental protocols used to characterize the featured probe technologies.
Fabrication of Monolithic AuNP-Fiber Probes
The creation of monolithic probes involves directly writing electrode arrays onto the curved surface of an optical fiber [43].
- Fiber Preparation: The tip of an optical fiber is heated and stretched to create a tapered region with artificial defects, enabling multidirectional light emission.
- Polymer Matrix Coating: A precursor mixture of SU-8 (a biocompatible epoxy) and Jeffamine D-230 (a polyetheramine) is cross-linked onto the fiber surface.
- Gold Infusion and Laser Writing: The coated fiber is immersed in a chloroauric acid (HAuClâ‚„) solution in acetonitrile. The gold salt permeates the polymer matrix. A laser is then used to precisely scan predefined patterns, which locally reduces the gold ions to form conductive gold nanoparticle (AuNP) electrodes embedded within the polymer.
- Insulation and Contact Pad Formation: A second polymer layer is applied for insulation. Contact pads are formed on the surface by subsequent laser exposure, while unexposed regions are washed away to prevent direct tissue contact with the underlying electrode traces [43].
In-Vivo Integration of Printed Liquid Metal Probes
This methodology enables the direct printing of a complete neural interface system onto the cranium of a live subject [44].
- Printing System Setup: A high-resolution direct writing system is used, comprising a pneumatic pressure controller, a fine nozzle (e.g., 5 µm inner diameter), and a multi-axis translation stage. Eutectic Gallium-Indium (EGaIn) serves as the conductive ink.
- Probe Printing and Passivation: The EGaIn is extruded through the nozzle to form neural probes with customizable lengths and a fine diameter (e.g., 5 µm) directly onto the implantation substrate. The entire structure is then passivated with a thin layer of Parylene, except for the probe tip.
- Electrode Enhancement (Optional): To enhance signal quality, platinum black (PtB) is electrodeposited onto the exposed tip of the liquid metal electrode. This nanostructured coating significantly increases the electrochemical surface area, thereby reducing impedance.
- Cranial Circuit Printing: Finally, interconnects and subsidiary circuits for signal processing and wireless transmission are printed directly onto the curved surface of the subject's skull, creating a fully integrated and conformal system [44].
Signal Fidelity and Biocompatibility Validation
Rigorous in vitro and in vivo tests are critical for assessing the long-term viability of neural probes.
- Electrochemical Impedance Spectroscopy (EIS): This is a standard method for evaluating electrode performance. Probes are immersed in a physiological solution like normal saline (NS), and impedance is measured across a frequency range (e.g., 1 Hz to 10 kHz). A lower impedance at 1 kHz is generally preferred for high-quality signal acquisition [43] [44].
- Cyclic Voltammetry (CV): This technique assesses the electrochemical stability and charge injection capacity of the electrode materials. Measurements over multiple cycles (e.g., 20 cycles) confirm stable charge transfer and the absence of toxic, unreduced precursor ions [43].
- Chronic In-Vivo Recording: Probes are implanted into the target brain regions of animal models (e.g., mice). Neural signals—including local field potentials (LFPs) and single-unit spikes—are recorded over weeks or months to monitor signal stability, amplitude, and signal-to-noise ratio (SNR) [43] [44] [45].
- Immunohistochemical Analysis: Post-study, brain tissue is extracted and examined for biological markers. Staining for glial fibrillary acidic protein (GFAP) reveals astrocyte activation, while markers like ED1 indicate microglial response. Reduced expression of these markers around the implant site indicates better biocompatibility and lower chronic inflammation [43] [46].
Diagram 1: Experimental workflow for validating neural probe performance, from fabrication to biological analysis.
Signaling Pathways in Optogenetic Modulation and Recording
Understanding the underlying biological mechanisms is crucial for designing effective experiments. The following diagram illustrates the neural signaling pathway targeted by optogenetic probes, such as those used to modulate the subthalamic nucleus (STN) to influence motor behavior [46].
Diagram 2: Signaling pathway for optogenetic neural excitation and electrical recording.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of experiments with advanced neural probes relies on a suite of specialized materials and reagents. The following table details key components used in the technologies discussed in this guide.
Table 2: Essential Research Reagents and Materials for Neural Probe Development and Application
| Category | Item | Function / Application | Example Use Case |
|---|---|---|---|
| Probe Fabrication | SU-8 Photoresist / Polymer | Forms a flexible, biocompatible substrate and insulation layer for embedded electrodes. | Monolithic probe polymer matrix [43]. |
| Chloroauric Acid (HAuClâ‚„) | Gold precursor for in-situ reduction to form conductive gold nanoparticle (AuNP) electrodes. | Laser-written AuNP electrodes [43]. | |
| Eutectic Gallium-Indium (EGaIn) | A conductive liquid metal for creating flexible, printable, and self-healing neural probes and interconnects. | Printed cranial circuits and probes [44]. | |
| Polyimide | A robust, biocompatible polymer used as a flexible substrate and insulation for thin-film microelectrodes. | FLID flexible probe substrate [45]. | |
| Signal Enhancement | Platinum Black (PtB) | A nanostructured coating electrodeposited on electrodes to increase surface area and lower impedance. | Coating for liquid metal and FLID electrodes [44] [45]. |
| Platinum-Iridium (Pt-Ir) Alloy | A coating material for recording sites, offering low impedance and high charge injection capacity. | Sputtered coating on FLID probe sites [45]. | |
| Optogenetics | Channelrhodopsin-2 (ChR2) | A light-sensitive opsin protein that depolarizes (excites) neurons in response to blue light. | Optical stimulation for motor control studies [46]. |
| AAV Viral Vectors | Genetically engineered viruses used to deliver opsin genes (e.g., ChR2) to specific neuron populations. | In-vivo transfection for optogenetics [43] [46]. | |
| µLED (Micro-LED) | A miniature light source integrated into neural probes for delivering optical stimulation pulses. | Light source for 3D-printed opto-probes [46]. | |
| Tenacissoside G | Tenacissoside G, MF:C42H64O14, MW:792.9 g/mol | Chemical Reagent | Bench Chemicals |
| Tenacissoside G | Tenacissoside G, MF:C42H64O14, MW:792.9 g/mol | Chemical Reagent | Bench Chemicals |
Optimizing Performance and Mitigating Artifacts: A Practical Guide for Reliable Data Acquisition
The relentless drive towards miniaturization and higher electrode density in neural implants represents a double-edged sword for long-term neural recording research. While offering unprecedented spatial resolution for mapping brain activity, these advanced arrays introduce a critical challenge: signal crosstalk contamination. This phenomenon, where signals electrically couple between closely spaced interconnection lines, threatens to undermine the very fidelity these technologies seek to enhance [47]. As research progresses toward chronic implantation and long-term monitoring, ensuring signal purity becomes paramount for accurate data interpretation and reliable biomarker identification for therapeutic applications.
The core dilemma stems from fundamental physics: with clearances between interconnect lines reduced to mere micrometers in state-of-the-art flexible arrays, the insulation impedance between these pathways decreases. This creates parasitic capacitive and resistive coupling channels, allowing signals from one channel to "bleed" into adjacent ones [47]. This contamination is particularly problematic in high-frequency bands above 300 Hz, which encompass critical neural information like multi-unit activity (MUA) [47]. For researchers and drug development professionals, this introduces significant uncertainty in data validation, potentially compromising the assessment of neural responses to pharmacological interventions or the long-term stability of recorded biomarkers.
Quantitative Comparison of Neural Recording Technologies and Crosstalk Impacts
The table below summarizes key characteristics of different neural recording modalities, highlighting the relationship between electrode density and susceptibility to crosstalk.
Table 1: Comparison of Neural Recording Technologies and Crosstalk Profiles
| Recording Technology | Typical Electrode Density & Spacing | Signal Fidelity Strengths | Crosstalk Vulnerability & Key Challenges |
|---|---|---|---|
| Macro-ECoG/SEEG [48] | Low Density; 3.5-10 mm spacing | Robust signals, lower crosstalk risk | Limited spatial resolution (≥3.5 mm), inadequate for micro-scale features |
| High-Density ECoG [48] | Medium Density; ~4 mm spacing | Improved spatial localization | Emerging crosstalk concerns with miniaturization |
| µECoG (Micro-Electrocorticography) [47] [48] | Very High Density; ~1.3-1.7 mm spacing, 57x higher density than macro-ECoG [48] | High SNR & ESNR, captures micro-scale neural features [48] | High vulnerability due to ultra-close routing; crosstalk can dominate signal coherence in high-frequency bands [47] |
| Intracortical Probes (e.g., Neuropixels) | Extreme Density; thousands of channels on a single shank [6] | Single-neuron resolution, deep brain structure access | Severe crosstalk and data transmission bottlenecks; requires sophisticated on-implant processing [6] |
The performance of algorithms designed to mitigate crosstalk can be quantitatively evaluated. The following table summarizes the experimental findings from a study that implemented a crosstalk back-correction algorithm on data from a high-density polyimide array.
Table 2: Performance Metrics of Crosstalk Mitigation Strategies
| Mitigation Strategy | Experimental Setup | Key Performance Metric | Result | Implication for Signal Fidelity |
|---|---|---|---|---|
| Crosstalk Back-Correction Algorithm [47] | In vivo recordings from rat cortex with a 16-channel microelectrode array | Reduction in signal coherence between closely-routed, physically distant channels | Significant drop in signal coherence in MUA band (>300 Hz) after correction [47] | Confirms crosstalk contamination; algorithm recovers a closer approximation of "ground truth" neural signals. |
| High-Density µECoG Array [48] | Intra-operative human speech decoding using LCP-TF µECoG arrays | Evoked Signal-to-Noise Ratio (ESNR) and Decoding Accuracy | 48% higher ESNR and 35% better decoding accuracy compared to standard intracranial signals [48] | Superior signal quality directly translates to more accurate readout of neural intent, despite inherent crosstalk risks. |
Experimental Protocols for Crosstalk Identification and Correction
Protocol 1: Identifying Crosstalk Contamination via Signal Coherence Mapping
Objective: To empirically detect the presence of crosstalk in recorded neural data by analyzing its relationship with the hardware routing layout [47].
- Neural Acquisition: Acquire epicortical or intracortical signals using a high-density microelectrode array (e.g., a conformable polyimide-based implant). The recording should be performed under a defined stimulus paradigm, such as somatosensory evoked potentials (SEPs) in anesthetized subjects [47].
- Data Band Separation: Separate the recorded data into two primary frequency bands for independent analysis:
- Local Field Potential (LFP) band: 3-300 Hz
- Multi-Unit Activity (MUA) band: >300 Hz [47]
- Compute Signal Coherence: Calculate the magnitude-squared coherence between a chosen reference channel and all other channels. Coherence is a frequency-domain measure of linear correlation between two signals.
- Correlate with Routing Layout: Map the computed coherence values against two spatial parameters:
- The inter-electrode distance on the cortical surface.
- The proximity of the interconnect lines in the array's routing layout [47].
- Identify Crosstalk Indicators: A positive identification of crosstalk contamination is indicated when channels with adjacent routing paths show high coherence in the high-frequency MUA band, even when their corresponding electrodes are physically far apart on the cortex. This discrepancy signals an abiotic, hardware-based coupling rather than a biologically plausible volume conduction [47].
Protocol 2: Implementing a Crosstalk Back-Correction Algorithm
Objective: To computationally estimate and remove the crosstalk component from recorded signals, approximating a "zero-crosstalk" scenario [47].
- System Characterization: Fully characterize the electrical properties of the recording chain, from the electrode-tissue interface to the amplifier. This is achieved through Impedance Spectroscopy (EIS) measurements. The collected data is used to build a comprehensive six-block equivalent electrical model of the biotic and abiotic parts of the system [47].
- Crosstalk Simulation: Use the characterized model to simulate the expected crosstalk levels between all channels in the array. This model accounts for both resistive coupling (frequency-independent) and capacitive coupling (which increases with frequency) [47].
- Algorithm Application: Develop a back-correction algorithm that uses the simulated coupling levels to invert the crosstalk contamination process. The algorithm mathematically separates the "true" neural signal from the blended recorded signal on each channel.
- Validation: Validate the algorithm's effectiveness by reapplying the signal coherence analysis (Protocol 1) to the corrected data. A successful correction is demonstrated by a significant reduction in the anomalous coherence between closely-routed but physically distant channels, particularly in the MUA band [47].
Signaling Pathways and Experimental Workflows
The following diagram illustrates the pathway of signal contamination from its source in the brain to its manifestation as crosstalk in recorded data, and the subsequent corrective process.
Diagram 1: Neural signal pathway and crosstalk correction.
The experimental workflow for a complete study investigating crosstalk, from in vivo recording to final data validation, is outlined below.
Diagram 2: Experimental workflow for crosstalk investigation.
The Scientist's Toolkit: Key Reagents and Materials
For researchers designing experiments involving high-density neural arrays, the following tools and components are essential for ensuring signal fidelity and combating crosstalk.
Table 3: Research Reagent Solutions for High-Density Neural Recording
| Item / Solution | Function & Role in Research | Key Considerations |
|---|---|---|
| Conformable Polyimide-based µECoG Arrays [47] [48] | Ultra-thin, high-density substrate for epicortical recording. Minimizes mechanical mismatch with tissue. | Electrode density (e.g., 128-256 channels), inter-electrode distance (~1.3-1.7 mm), impedance profile. |
| LCP-TF (Liquid Crystal Polymer Thin-Film) Arrays [48] | Provides high-density, high-fidelity neural interfaces with improved signal-to-noise ratio. | Enables high spatial resolution necessary for decoding fine-scale neural features like phonemes. |
| State-of-the-Art Neural Acquisition System [47] | Amplifies, filters, and digitizes analog neural signals from hundreds of microelectrodes. | Must support the high channel count; specifications for input impedance and noise are critical. |
| Electrochemical Impedance Spectroscopy (EIS) Setup [47] | Characterizes the electrode-tissue interface and insulation impedance between interconnect lines. | Essential for building accurate circuit models to simulate crosstalk. |
| Crosstalk Back-Correction Algorithm [47] | A computational tool to estimate and remove crosstalk contamination from recorded data. | Effectiveness is validated by reduced coherence between closely-routed channels. |
| Modular Drift Correction Software (e.g., SpikeInterface) [49] | Benchmarks and corrects for mechanical drifts that distort neural waveforms, a separate challenge from crosstalk. | Important for maintaining single-unit isolation over long-term recordings. |
| Non-linear Decoding Models [48] | Leverages enhanced spatio-temporal information from high-fidelity, corrected signals for tasks like speech decoding. | Can produce superior results compared to linear models when processing micro-scale neural features. |
Strategies for Minimizing Insertion Trauma and Improving Chronic Tissue Integration
The long-term stability of implanted neural interfaces is a cornerstone of modern neuroscience research and neuroprosthetic development. A central challenge limiting chronic signal fidelity is the body's biological response to the implanted device. This response begins with acute insertion trauma—the immediate damage to cells and blood vessels during implantation—and evolves into a chronic foreign body reaction, characterized by glial scarring and neuronal loss around the implant. This tissue encapsulation electrically insulates the recording sites, leading to a progressive decline in the signal-to-noise ratio (SNR) and eventual failure of the device. This guide objectively compares the leading technological strategies developed to mitigate these issues, providing researchers with a data-driven framework for selecting and implementing interfaces that preserve signal fidelity over extended periods.
Comparative Analysis of Strategic Approaches
The following table summarizes the core strategies, their mechanisms of action, and their quantitatively reported impacts on recording performance.
Table 1: Comparison of Strategies for Minimizing Insertion Trauma and Improving Chronic Tissue Integration
| Strategy | Key Mechanism of Action | Reported Efficacy and Experimental Data |
|---|---|---|
| Lubricated Surface Coatings (LIPS) [50] | Creates a near-frictionless, anti-biofouling surface that minimizes tissue drag during insertion and repels proteins/cells. | - 86% reduction in friction force impulse during insertion [50].- 102% increase in active recording electrodes upon insertion [50].- Signal recording period extended from 8 to 16 weeks; SNR improved up to ninefold [50]. |
| Ultrasoft Material Fabrication [51] | Reduces mechanical mismatch between implant and brain tissue (Young's modulus ~974 kPa) to minimize chronic micromotion strain. | - Significant reduction in chronic inflammation markers (Iba-1, GFAP) compared to stiff tungsten wires [51].- Improved neuronal survival and normal neuronal morphology at the tissue interface after 8 weeks [51]. |
| Insertion Speed Optimization [52] | Slow insertion (~2 µm/s) allows tissue time to accommodate the probe, reducing acute strain and cellular damage. | - Significantly higher SNR and number of separable single units post-insertion compared to faster speeds (1 mm/s) [52].- Higher neuronal density (NeuN-labeled cells) around the probe track after slow insertion [52]. |
| Flexible Probe Geometry & Implantation [17] | Uses small cross-sectional areas and rigid shuttle guidance to minimize acute injury while maintaining flexibility for chronic compatibility. | - Rod/filament electrodes with cross-sections as small as 10 µm² minimize implantation injury [17].- Stable neural recordings in macaques achieved for up to eight months [17]. |
| Anti-inflammatory Drug Delivery [53] | Local elution of corticosteroids (e.g., Dexamethasone) or neurotrophins (e.g., BDNF) to suppress the inflammatory cascade. | - Shown to enhance hearing preservation in cochlear implants by mitigating inflammation [53].- Challenges include controlled release kinetics and limited drug-loading capacity for long-term use [50]. |
Experimental Protocols for Key Studies
Protocol 1: Evaluating Lubricated Immune-Stealthy Probe Surface (LIPS)
This protocol is adapted from studies on silicon-based neural probes coated with a biomimetic lubricant layer [50].
- Primary Objective: To assess the effect of a lubricated coating on acute insertion damage and chronic recording stability.
- Materials:
- Neural Probes: Single-shank, silicon-based probes with 16 recording sites.
- Coating System: A micro/nanostructured Pt black electrode surface, chemically modified and infused with a biocompatible lubricant to create a stable, slippery layer.
- Control: Bare silicon probes coated only with Pt black.
- Animal Model: Mice (e.g., C57BL/6).
- In Vitro Characterization:
- Friction Force Measurement: Use a force sensor to measure the friction force during insertion into brain tissue surrogate (e.g., agarose gel). Compare impulse (force × time) between LIPS and bare probes.
- Anti-biofouling Assay: Immerse probes in blood or protein solution (e.g., albumin). Use optical microscopy to quantify the adhesion of tissue debris and proteins on the electrode sites.
- In Vivo Electrophysiology:
- Surgical Implantation: Implant LIPS-coated and bare probes stereotactically into the target brain region (e.g., somatosensory cortex).
- Acute Recording: Record spontaneous neural activity immediately after insertion for 45-60 minutes. Calculate the number of active recording channels and the SNR of detected spike signals.
- Chronic Recording: Perform longitudinal recordings over several weeks. Track metrics such as single-unit yield, SNR, and impedance over time.
- Histological Analysis:
- Perfuse animals at endpoint (e.g., 8 and 16 weeks).
- Immunostain brain sections for markers of neurons (NeuN), microglia (Iba-1), and astrocytes (GFAP).
- Quantify neuronal density and glial encapsulation thickness around the probe track.
Protocol 2: Assessing the Impact of Insertion Speed on Acute Recording Quality
This protocol is based on research investigating the insertion of rigid silicon probes [52].
- Primary Objective: To determine the optimal insertion speed for maximizing acute neuronal signal quality and minimizing tissue damage.
- Materials:
- Neural Probes: High-density, single-shank silicon probes.
- Insertion Apparatus: A precise microdrive system capable of consistent insertion speeds (e.g., 2 µm/s, 20 µm/s, 0.1 mm/s, 1 mm/s).
- Animal Model: Rats anesthetized with ketamine/xylazine.
- Procedure:
- Surgical Preparation: Secure the animal in a stereotaxic frame and perform a craniotomy over the somatosensory cortex.
- Randomized Insertion: Implant the probe to a depth of ~1700 µm at four separate cortical locations, each with a different, randomly assigned insertion speed.
- Data Acquisition: Immediately after reaching the target depth, record wideband (0.1–7500 Hz) spontaneous neural activity for 45 minutes.
- Data Analysis:
- Signal Processing: Band-pass filter (500–5000 Hz) the data to extract spiking activity.
- Quality Metrics:
- Calculate the Signal-to-Noise Ratio (SNR) for each recording channel.
- Perform spike sorting to isolate single units.
- Count the number of separable single units per implantation.
- Histological Correlation: Perfuse the animal post-recording and immunostain for NeuN. Quantify neuronal density around the track for each insertion speed.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Neural Interface Integration Studies
| Item Name | Function/Application | Specific Examples & Notes |
|---|---|---|
| LIPS Coating System [50] | Creates a lubricated, anti-biofouling neural probe surface. | Micro/nanostructured Pt black electrodes infused with a stabilized biocompatible lubricant. Mimics the Nepenthes pitcher plant. |
| Conducting Polymer Elastomers [51] | Forms the core of ultrasoft electrodes, matching brain tissue mechanics. | PEDOT-PEG/PDMS blend with a Young's modulus of ~974 kPa. Requires a rigid shuttle (e.g., tungsten needle) for implantation. |
| Hydrous Iridium Oxide [54] | Used for fabricating pH microsensor arrays to quantify tissue trauma. | Electrochemically grown on microelectrodes. Provides a metric for tissue acidosis following implantation. |
| Hf-WD POM Staining Agent [55] | Non-destructive contrast agent for 3D visualization of soft and mineralized cochlear structures via microCT. | Enables precise anatomical study to guide atraumatic surgical design. |
| Rigid Implantation Shuttles [17] | Temporarily stiffens flexible probes for precise targeting. | Dissolvable PEG coatings [51], tungsten wires [17], or SU-8 structures used to guide flexible electrodes to depth. |
Visualizing the Foreign Body Response and Intervention Strategies
The tissue response to a neural implant is a cascading process, offering multiple points for strategic intervention, as illustrated below.
The pursuit of stable, long-term neural recordings necessitates a multi-faceted approach that addresses both the initial mechanical trauma of implantation and the ensuing chronic biological response. As the comparative data reveals, no single strategy is a panacea; rather, the most promising results arise from integrated solutions. The combination of lubricated, anti-biofouling surfaces to ease insertion, ultrasoft, compliant materials to mitigate chronic micromotion, and potentially localized anti-inflammatory therapies presents a powerful pathway toward achieving chronic signal fidelity. For researchers, the selection of a neural interface strategy must be guided by the specific experimental requirements, balancing the need for high-channel-count, rigid platforms with the superior long-term biocompatibility of flexible, minimally invasive designs. The future of brain-machine interfaces and chronic neuroscience research hinges on the continued refinement of these strategies to create truly bio-integrative technologies.
For neural interfaces, the long-term stability of signal fidelity is paramount. The degradation of recording quality over weeks or months remains a significant barrier to the development of chronic brain-machine interfaces (BMIs) and other neurotechnologies [23]. This degradation is primarily driven by two interrelated electrochemical phenomena: a rise in electrode-electrolyte interface impedance and the corrosion of the implant materials. Both processes are exacerbated by the hostile physiological environment and the body's foreign body response, leading to insulating scar tissue formation, neuronal loss, and ultimately, a decline in signal-to-noise ratio (SNR) and the loss of single-unit recordings [56] [23]. This guide objectively compares the performance of emerging material and coating strategies designed to mitigate these failure mechanisms, providing researchers with experimental data and protocols to inform the selection and development of next-generation neural implants.
Comparative Analysis of Material and Coating Strategies
The pursuit of stable long-term neural recordings has led to innovations in both the bulk materials for probes and the functional coatings applied to electrodes. The following table compares the performance of several advanced strategies based on recent experimental findings.
Table 1: Performance Comparison of Neural Implant Strategies
| Strategy & Material | Key Performance Data | Impact on Signal Fidelity | Chronic Stability Evidence |
|---|---|---|---|
| Sputtered RuOx Coating [56] | • 1 kHz Impedance: Decreased from 1.06 MΩ to 0.68 MΩ over 6 weeks• Charge Storage Capacity (CSC): ~20-24 mC cm² at 50 mV/s, stable over 6 weeks• Single-Unit Yield: 75% active electrode yield at 6 weeks | Maintains low impedance for high-SNR recordings of single-unit action potentials. High CSC supports efficient signal transduction. | Stable electrochemical properties (EIS, CV) and consistent single-unit recordings over a 6-week subchronic implantation in rat motor cortex. |
| Mechanically-Adaptive, Resveratrol-Eluting (MARE) Probe [23] | • Impedance: Stable impedance over 12 weeks• Neuronal Density: Increased density near the implant at 2 weeks• Blood-Brain Barrier: Healing observed by 16 weeks | Improved recording performance and stability attributed to reduced neuroinflammation and mechanical mismatch. | Demonstrated improved recording performance and stable impedance over 12 weeks in rat cortex, with gene expression data indicating a healing tissue response. |
| PLA/Vanillin/Gentamicin Coating on TNT [57] | • Corrosion Protection: Lowered passive current density by two orders of magnitude• Drug Release: Sustained, linear release profile over 168 hours (7 days)• Antibacterial Efficiency: 94-95% against Gram-positive and Gram-negative bacteria | Prevents corrosion-induced failure and infection, indirectly supporting signal fidelity by preserving the integrity of the electrode and its local environment. | In-vitro data shows excellent corrosion resistance in simulated body fluid and sustained drug release, suggesting potential for long-term functionality. |
| Ti-Zr-Nb-Ta-Ag High-Entropy Alloy (HEA) [58] | • Charge Transfer Resistance (R~ct~): 1.08 × 10ⷠΩ·cm² in artificial saliva• Hardness: 8.2 GPa, nearly double that of Ti6Al4V | Exceptional corrosion resistance indicates stable passive film formation, crucial for preventing ion release and maintaining a stable electrode interface. | In-vitro electrochemical tests demonstrate significantly enhanced corrosion resistance compared to Ti6Al4V, suggesting superior long-term biostability. |
Detailed Experimental Protocols for Validation
To evaluate and validate the electrochemical stability of neural implants, standardized in-vitro and in-vivo protocols are essential. The following methodologies are commonly employed in the field.
In-Vitro Electrochemical Corrosion Testing
This protocol is used to assess the corrosion resistance of implant materials in a simulated physiological environment [57] [58].
- 1. Solution Preparation: Prepare an artificial saliva solution or a standard simulated body fluid (SBF) like phosphate-buffered saline (PBS). The pH should be adjusted to various levels (e.g., 4.0, 7.4, 9.0) to simulate different physiological and inflammatory states.
- 2. Setup: Use a standard three-electrode electrochemical cell with the implant sample as the working electrode, a platinum wire or mesh as the counter electrode, and a Ag/AgCl (or Saturated Calomel Electrode, SCE) as the reference electrode.
- 3. Open Circuit Potential (OCP) Measurement: Monitor the potential of the working electrode vs. the reference electrode until it stabilizes (typically 30-60 minutes) to establish the corrosion potential.
- 4. Electrochemical Impedance Spectroscopy (EIS): Apply a sinusoidal voltage signal with a small amplitude (e.g., 10 mV RMS) over a wide frequency range (e.g., 10âµ Hz to 10â»Â² Hz). The resulting impedance data is used to model the electrode-electrolyte interface and determine key parameters like charge transfer resistance, which is directly correlated with corrosion resistance [58].
- 5. Potentiodynamic Polarization (PDP): Scan the electrode potential from a value below the OCP to a value above it at a constant rate. The resulting current is measured to determine critical parameters such as corrosion current density and breakdown potential.
In-Vivo Electrochemical and Recording Stability Assessment
This protocol evaluates the performance of the neural interface in a living organism over time, as described in studies on RuOx coatings and MARE probes [56] [23].
- 1. Surgical Implantation: Under approved IACUC protocols, implant the neural probe (e.g., a-SiC MEA, MARE probe) into the target brain region (e.g., rat motor cortex) using stereotactic surgery.
- 2. In-Vivo Electrochemical Measurements: These are performed periodically (e.g., weekly) throughout the implantation period.
- Electrochemical Impedance Spectroscopy (EIS): Conducted at specific frequencies (e.g., 1 Hz for local field potentials, 1 kHz for single-unit activity) to track changes in interface impedance [56].
- Cyclic Voltammetry (CV): Performed by cycling the electrode potential between set limits (e.g., -0.6 V to +0.6 V vs. Ag/AgCl) at different sweep rates. The cathodal charge storage capacity (CSC~c~) is calculated by integrating the current in the cathodal portion of the cycle, indicating the electrode's charge injection capacity [56].
- 3. Neural Signal Recording: Record spontaneous neural activity during each session. Key metrics include:
Visualization of Strategies and Workflows
The following diagrams illustrate the core strategies for enhancing implant stability and the experimental workflow for their validation.
Multimodal Strategy for Stable Neural Interfaces
Experimental Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful research in this field relies on specific materials, instruments, and biological tools. The following table details key components for developing and testing stable neural interfaces.
Table 2: Essential Research Reagents and Materials
| Category | Item | Specific Example / Model | Primary Function in Research |
|---|---|---|---|
| Electrode Coatings | Sputtered Ruthenium Oxide (RuOx) | 250 nm thick film [56] | Provides low impedance, high charge storage capacity faradaic coating for microelectrodes. |
| Biodegradable Polymer Matrix | Polylactic Acid (PLA) / Vanillin with Gentamicin [57] | Forms a controlled drug delivery system on implants for corrosion protection and antibacterial activity. | |
| Bulk Substrates | Mechanically-Adaptive Nanocomposite | Polyvinyl acetate + cellulose nanocrystals [23] | Serves as a probe substrate that is rigid for insertion but softens in situ to match brain modulus. |
| High-Entropy Alloy (HEA) | Ti-Zr-Nb-Ta-Ag [58] | Acts as a bulk implant material with exceptional corrosion resistance and mechanical properties. | |
| Electrochemical Instruments | Potentiostat / Galvanostat | Gamry Reference 600 [56] | Performs key electrochemical measurements (EIS, CV, PDP) for in-vitro and in-vivo characterization. |
| Neural Recording Systems | Neural Signal Processor | Intan Technologies RHD Amplifiers / Blackrock Microsystems Cerebus [59] | Amplifies, filters, and digitizes analog neural signals from microelectrode arrays for analysis. |
| Biological Reagents | Antioxidant for Local Elution | Resveratrol [23] | Incorporated into implant substrates to mitigate oxidative stress and neuroinflammation. |
| Cell Culture Lines | MG63 Osteoblast-like cells [57] | Used for in-vitro assessment of cell proliferation and biocompatibility of implant materials. |
For researchers developing next-generation brain-implantable microsystems, the primary bottleneck has shifted from electrode fabrication to data handling [60]. The pursuit of high-fidelity, long-term neural recording is fundamentally constrained by a critical trade-off: increasing channel count for higher spatial resolution directly opposes the imperative for low power operation to ensure device viability and patient safety. Scaling to thousands of recording channels creates extreme bandwidth and power demands that are unsustainable for resource-constrained, implantable systems [61] [60].
This guide provides a systematic comparison of emerging system-level optimization strategies designed to resolve this conflict. We objectively evaluate competing approaches—from advanced compression algorithms and ultra-miniaturized hardware to novel power sources—by synthesizing quantitative data and detailing experimental protocols. The analysis is framed within the overarching research thesis that preserving long-term signal fidelity requires a holistic, system-level design philosophy that integrates materials science, circuit design, and signal processing.
Comparative Analysis of System-Level Optimization Strategies
The table below summarizes the performance characteristics of four leading optimization strategies, providing a baseline for direct comparison.
Table 1: Performance Comparison of Neural Interface Optimization Strategies
| Optimization Strategy | Reported Compression Ratio / Power Saving | Key Metric Preservation | Technology Readiness Level (TRL) | Limitations & Trade-offs |
|---|---|---|---|---|
| Adaptive Multi-Stage Compression [61] | 1098x total compression over baseline | Preserves 90% of spikes; retains spatial & temporal waveform features | Mid (Validated on 512-channel macaque retina ex vivo data) | Adaptive logic overhead; potential loss of low-SNR neural data |
| Optoelectronic Microsystems (MOTE) [62] [63] | Power consumption: ~1 µW per node | Chronic recording (365 days) in awake mice; minimal tissue scarring | Mid (Chronic in vivo validation in mice) | Limited penetration depth for power/communication; requires external optical apparatus |
| Ultrasmicroelectrode (UME) Tip Control [64] | Signal-to-Noise Ratio (SNR): Significant improvement reported | Improved stability and fidelity of single-cell recording | Early (Laboratory validation) | Highly specialized fabrication (microplasma jet); challenges in mass production |
| Electromagnetic Energy Harvesting [65] | Power Density: N/A (Technology overview) | Accesses inexhaustible energy from bodily movements | Early (Concept & preliminary research) | Lower power density compared to batteries; variability in energy source |
Detailed Experimental Protocols and Methodologies
To enable critical evaluation and replication, this section details the experimental methodologies underpinning the data in the comparison table.
Protocol for Adaptive Multi-Stage Compression
This framework employs a three-stage compression pipeline to drastically reduce data bandwidth without significantly degrading decoding performance [61].
- Compressive Readout: Neural signals are acquired using a Wired-OR analog-to-digital compressive readout, which reduces data volume at the initial acquisition stage.
- Adaptive Requantization: The digital core adaptively requantizes the signals. The number of quantization bits is dynamically matched to the electrode's maximum signal-to-noise ratio (SNR), using
⌈log₂ SNR⌉bits. This eliminates unnecessary precision that primarily captures noise. - Selective Sampling & Encoding: A mutual information-based criterion selectively samples recorded spikes to preserve critical spatial and temporal discriminative features. A static entropy coder, optimized for neural signal statistics, performs final low-overhead compression.
Evaluation Metric: The system's performance was quantified on 512-channel macaque retina ex vivo data, with success defined by the percentage of preserved spikes and the total compression ratio achieved over a non-compressed baseline [61].
Protocol for MOTE Chronic Validation
The validation of the microscale optoelectronic tetherless electrode (MOTE) focused on long-term stability and biocompatibility [62] [63].
- In Vitro Functional Testing: MOTEs were deployed in a Petri dish cultured with iPSC-derived cardiomyocytes. The nuclei were stained with a blue Hoechst dye to confirm cell presence on the MOTE electrodes [63].
- Pharmacological Modulation: To confirm that recorded signals were biologically genuine, the beating rate of the cardiomyocytes was modulated using the agonist isoproterenol (1 µM and 5 µM) to increase frequency, and the inhibitor blebbistatin (5 µM) to decrease frequency. The MOTE output was decoded to track these changes [63].
- In Vivo Implantation and Recording: MOTEs were implanted into the barrel cortex (the region processing whisker sensory information) of mice using a nanoinjector. The barrel cortex provides a well-defined model to correlate neural activity with sensory input [62] [63].
- Long-Term Monitoring: Over 365 days, neural activity was recorded in awake mice as their whiskers were stimulated. The health of the animals and the level of tissue scarring around the implant were monitored throughout the year to assess biocompatibility and chronic device performance [62] [63].
Protocol for Ultramicroelectrode Tip Exposure
This method enhances signal fidelity at the single electrode level by improving the electrode-tissue interface [64].
- Fabrication: Ultramicroelectrodes (UMEs) are coated with a protective diamond-like carbon (DLC) layer, chosen for its mechanical strength, thermal stability, and biocompatibility.
- Microplasma Jet Processing: A cold atmospheric microplasma jet is used to selectively and precisely remove the DLC coating from the tip of the UME. This process allows for controlled exposure on the submicron scale.
- Biocompatibility Testing: Extensive tests are conducted to confirm that the DLC-UME does not adversely affect neuronal cell growth, ensuring its safety for long-term biological application [64].
- Electrochemical Validation: The stability and reliability of the exposed tips are confirmed through electrochemical tests and intracellular pH detection, validating the improvement in signal-to-noise ratio and sensitivity [64].
System Architecture and Signaling Pathways
The following diagrams map the logical workflows and system architectures of the key optimization strategies discussed, illustrating how they balance high density with low power.
MOTE System Operation
MOTE Optoelectronic Signal Pathway
Adaptive Compression Logic
Adaptive Compression Dataflow
The Scientist's Toolkit: Key Research Reagents and Materials
For researchers aiming to work in this field, the table below catalogs essential materials and reagents referenced in the featured studies, along with their critical functions.
Table 2: Essential Research Reagents and Materials for Neural Interface Development
| Material / Reagent | Function in Research Context | Key Property / Rationale |
|---|---|---|
| AlGaAs Diode (PVLED) [62] [63] | Serves as both photovoltaic (power receiver) and light-emitting diode (data transmitter) in the MOTE system. | Enables extreme miniaturization via time-division multiplexing of power and communication on a single component. |
| Diamond-Like Carbon (DLC) Coating [64] | Provides a protective, insulating layer on ultramicroelectrodes (UMEs). | Offers mechanical strength, thermal stability, and biocompatibility for long-term implantation. |
| Cold Atmospheric Microplasma Jet [64] | Precisely removes DLC coating to control UME tip exposure length on a submicron scale. | Enables fine control over electrode electrochemistry, improving signal-to-noise ratio and stability. |
| Atomic Layer Deposition (ALD) SiO₂, Si₃N₄, Al₂O₃ [63] | Forms a conformal, biocompatible encapsulation layer protecting microelectronics from corrosive biological media. | Provides an ultra-thin (<1.5 µm) yet effective barrier, minimizing added volume to the implant. |
| Platinum (Pt) Sputtering [63] | Functions as both a low-impedance electrode material and a conformal light shield for on-chip electronics. | Prevents incident light from generating photocurrents that could interfere with signal fidelity in optoelectronic systems. |
| Isoproterenol & Blebbistatin [63] | Pharmacological agents used for in vitro validation of MOTE functionality with cardiomyocytes. | Modulates cardiomyocyte contraction frequency (isoproterenol increases, blebbistatin decreases), providing a biological ground truth for signal recording. |
| Hoechst Dye [63] | Fluorescent stain for cell nuclei. | Used in in vitro experiments to confirm the presence and attachment of living cells (e.g., cardiomyocytes) on the recording electrodes. |
The comparative data and methodologies presented reveal that no single strategy universally dominates the optimization landscape. The choice of approach is heavily dictated by the specific research goal: MOTE-style optoelectronics demonstrate unparalleled miniaturization and chronic stability, while adaptive compression offers the highest data reduction for systems with many channels. Meanwhile, innovations like UME tip control target the fundamental challenge of signal fidelity at the sensor-tissue interface.
The emerging thesis is that the future of high-density, low-power neural interfaces lies not in a single technology, but in the synergistic integration of these approaches. A truly optimized system would incorporate advanced electrode materials, MOTE-level miniaturization, and intelligent on-implant compression algorithms. Such a functionally cooperative system represents the next frontier in unlocking the full potential of long-term neural recording for understanding the brain and treating neurological disease.
Benchmarking Progress: Evaluating New Technologies Through In Vivo Performance and Usability
Within the field of neural engineering, a core challenge has been the decline in recording quality of implantable neural interfaces over time. This degradation, often resulting from the foreign body response and mechanical mismatch with brain tissue, limits the clinical and research potential of chronic brain-computer interfaces (BCIs). The pursuit of stable, high-fidelity neural recording over periods of a year or more has become a central thesis in signal fidelity long-term neural recording research. This guide objectively compares the performance of various neural interface technologies that have demonstrated, through in vivo studies, the capability to record high-quality signals for over 12 months. It summarizes key quantitative data and provides detailed methodologies to serve researchers, scientists, and drug development professionals in evaluating the long-term stability of different neural recording approaches.
Case Studies of Long-Term Neural Interfaces
The following case studies detail specific neural interface technologies that have been empirically validated to maintain signal quality for twelve months or longer in living animal models. The performance data for these systems are summarized and compared in Table 1.
Table 1: Comparative Performance of Long-Term Neural Interfaces
| Interface Technology | Animal Model | Recorded Signal Types | Demonstrated Longevity | Key Performance Findings | Primary Stability Strategy |
|---|---|---|---|---|---|
| Wireless EEG/EMG Headcap [66] | Mouse (C57BL/6J) | Cortical EEG, Nuchal EMG | Up to 12 months | Successful recording of sleep staging, cognitive task (Barnes maze) data, and neuronal frequencies over 12 months. | Non-penetrating skull-surface electrodes; wireless data acquisition to minimize mechanical stress. |
| Sinusoidal Probe [67] | Rabbit | Single-Unit Activity, Local Field Potentials (LFP) | Up to 678 days (approx. 22 months) | Stable signal-to-noise ratio (SNR) and LFP power over the recording period. | Sinusoidal shaft to absorb brain micromotion; spherical tip for tissue anchoring; flexible materials (Parylene-C, W/Ti). |
| Axoft's Fleuron BCI [68] | Animal models (unspecified) | Single-Neuron Activity | Over 1 year | Ability to track electrical activity of single neurons for over a year. | Novel "Fleuron" material (10,000x softer than polyimide) for superior biocompatibility. |
| InBrain's Graphene BCI [68] | Human (surgical resection) | Ultra-high resolution signals | N/A (Initial safety demonstrated) | Interim results showed safety and functional performance. | Graphene-based electrodes for high signal resolution and biocompatibility. |
Wireless EEG/EMG Headcap System
This system employs a non-penetrating approach, where electrodes are fixed to the skull surface. A study demonstrated its capability for longitudinal, wireless recordings in freely moving mice over 12 months. The methodology enabled concurrent behavioral and electrophysiological phenotyping, capturing data during sleep, in home-cage environments, and during cognitive tasks like the Barnes maze [66].
Experimental Protocol
- Surgical Implantation: The protocol involves a one-time surgery under isoflurane anesthesia. A headcap with two pre-positioned stainless-steel EEG leads and one EMG lead is secured to the skull. Two anterior and two posterior stainless-steel electrode screws are implanted into the skull. The EMG wires are implanted into the nuchal muscle. The assembly is fixed using cyanoacrylate adhesive and dental acrylic [66].
- Data Acquisition: Following surgery, data is acquired wirelessly using a lightweight, head-mounted potentiostat powered by zinc-air batteries. The Sirenia Acquisition software is used to collect data, which can be synchronized with video recordings from behavioral setups like the PhenoTyper home cage or Barnes maze [66].
- Signal Processing: Recorded signals are processed using software such as Sirenia Sleep Pro for sleep staging, which automates the classification of wake, NREM, and REM sleep states based on EEG and EMG signatures [66].
The Sinusoidal Probe
This penetrating electrode was designed specifically to address the problem of micromotion between the brain and implanted probes. Its unique mechanical design aims to minimize chronic tissue trauma and glial scarring, which are primary drivers of signal degradation [67].
Experimental Protocol
- Probe Design and Fabrication: The probe is microfabricated from a sintered tungsten-titanium (W/Ti) alloy, resulting in a lower Young's modulus than pure tungsten. The shaft features a sinusoidal profile (100 μm amplitude, 500 μm period), and the recording end is a parylene-C disk with a 3D polyimide "ball anchor" [67].
- Surgical Implantation and Recording: The flexible sinusoidal probe requires a rigid shuttle, such as a tungsten wire fixed with polyethylene glycol (PEG), for insertion into the target brain region. After implantation, the PEG melts and the shuttle is retracted. In the cited study, recordings of single-unit activity and LFP were performed in rabbits and compared against standard rigid microwires [67].
- Histological Analysis: Post-mortem brain tissue was analyzed to quantify the presence of microglia and astrocytes around the implant site. The sinusoidal probe showed reduced neuronal tissue damage compared to standard microwires, especially in the tip region between 6 and 24 months post-implantation [67].
The workflow and core stability concept of the Sinusoidal Probe are illustrated below.
Strategies for Enhancing Long-Term Signal Fidelity
The successful case studies above, along with other emerging research, point to several key strategies for achieving long-term signal stability.
Mechanical Compatibility and Implantation Strategies
A primary focus is on reducing the mechanical mismatch between rigid implants and soft brain tissue. This involves using flexible and ultrasoft materials like polyimide, the novel "Fleuron" polymer, and graphene [17] [68]. The design of the electrode shaft itself is also critical; the sinusoidal probe demonstrates how a non-straight shaft can better accommodate brain deformations [67]. Furthermore, the implantation method must be tailored to the electrode's shape. For flexible, filamentary electrodes, techniques like tungsten wire guidance or distributed implantation with robotic assistance are used to minimize acute injury and the resulting cross-sectional area of damage [17].
Pharmacological Interventions
Another approach is to modulate the biological response to the implant. The hormone melatonin (MT) has been shown to improve the quality and longevity of chronic neural recordings [69].
- Experimental Protocol with Melatonin: A study administered daily melatonin to mice implanted with intracortical microelectrode arrays. The "acute" group received injections for 3 days before and 14 days after surgery, while the "chronic" group received treatment for the full 16-week study. The chronic MT treatment maintained a high single-unit yield over 16 weeks, whereas the effect of acute treatment faded after injections stopped. Histology revealed that melatonin increased neuronal viability and reduced apoptosis and reactive oxygen species (ROS) around the implant site [69].
- Mechanism of Action: Melatonin exerts its effects through receptor-dependent and independent pathways. It is a potent anti-inflammatory (inhibiting cytokines like TNF-α and IL-1β) and anti-oxidant (scavenging free radicals). It also has anti-apoptotic properties, inhibiting the caspase-1/cytochrome c/caspase-3 cell death pathway [69].
The signaling pathways through which melatonin improves chronic recording quality are summarized in the following diagram.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Materials for Chronic Neural Recording Experiments
| Item | Function / Application | Example from Literature |
|---|---|---|
| Parylene-C | A flexible, biocompatible polymer used as a dielectric coating for implantable electrodes. | Used as the primary insulation and substrate material for the sinusoidal probe [67]. |
| Polyethylene Glycol (PEG) | A biodegradable polymer used as a temporary coating to stiffen flexible electrodes for implantation. | Used to fix a rigid tungsten wire shuttle to flexible electrodes, which melts after implantation [17]. |
| Melatonin (MT) | A hormone used as a therapeutic agent to suppress chronic inflammation and apoptosis around the implant site. | Daily administration shown to improve single-unit yield and signal longevity for 16 weeks in mice [69]. |
| Graphene | A two-dimensional carbon material enabling ultra-high signal resolution due to its mechanical and electrical properties. | InBrain Neuroelectronics uses graphene-based electrodes in its neural platform [68]. |
| Fleuron Polymer | A novel, ultrasoft material designed to enhance biocompatibility and reduce tissue scarring. | Axoft's BCI uses Fleuron, reported to be 10,000 times softer than polyimide [68]. |
| Sintered W/Ti Alloy | A tungsten-titanium composite used to create conductive traces that are more flexible than pure tungsten. | Used for the metal tracks and recording sites of the sinusoidal probe [67]. |
The field of neural recording is undergoing a paradigm shift, moving from traditional, laboratory-bound systems toward wireless, wearable technologies. This transition is critically important for advancing research into long-term neural signal fidelity, as it enables the capture of brain activity in real-world environments and over extended periods. For researchers and drug development professionals, understanding the performance characteristics of these emerging tools compared to conventional gold standards is essential for designing valid and reliable studies. This guide provides an objective, data-driven comparison of the signal quality and usability of novel wireless wearables against conventional wired electroencephalography (EEG) systems, synthesizing findings from recent validation studies to inform equipment selection and experimental design.
Recent independent studies consistently demonstrate that several novel wireless wearable devices achieve high spectral correlation (0.86-0.94) with conventional scalp-EEG systems in recording key neural events like epileptic seizures and common artifacts [70] [71]. However, performance varies significantly between consumer-grade and research-focused wearable models [72]. The primary advantages of wireless systems include superior patient comfort, enabling long-term monitoring, and the ability to capture data in naturalistic settings. The trade-off often involves reduced electrode density and, for some consumer devices, signal quality inconsistencies, particularly in low-frequency bands [72]. The choice between systems should therefore be guided by specific research requirements, prioritizing either maximum signal fidelity in controlled environments or ecological validity and patient comfort for extended, ambulatory studies.
Comparative Data Tables
Table 1: Quantitative Signal Quality Metrics
Table 1 summarizes key quantitative findings from recent comparative studies.
| Device/System Name | Signal Correlation with Conventional EEG | Key Performance Metrics | Study Details |
|---|---|---|---|
| REMI Sensor (Wireless Wearable) | Spectral correlation: 0.86 to 0.94 across event types (seizures, artifacts) [70] [71] | High similarity in temporal dynamics and signal morphology of electrographic seizures and artifacts [70]. | Cohorts: Epilepsy patients & healthy volunteers; Simultaneous recording with conventional scalp-EEG [70]. |
| PSBD Headband Pro (Consumer Wearable) | Higher mean power in low-frequency bands; closest alignment with research-grade BP amplifier among consumer devices tested [72]. | Matched research-grade system most precisely in spectral characteristics [72]. | Recording: Resting-state (eyes open/closed); Comparison: Brain Products ActiChamp Plus (BP) [72]. |
| PSBD Headphones Lite (Consumer Wearable) | Moderate correspondence with research-grade BP amplifier [72]. | Showed signal quality issues in the central group of electrodes [72]. | Recording: Resting-state (eyes open/closed); Comparison: Brain Products ActiChamp Plus (BP) [72]. |
| Muse S Gen 2 (Consumer Wearable) | Poorest signal quality and extremely low alignment with research-grade BP amplifier [72]. | High susceptibility to artifacts and test-retest variability [72]. | Recording: Resting-state (eyes open/closed); Comparison: Brain Products ActiChamp Plus (BP) [72]. |
| PEDOT:PSS-Coated Microneedle (MN) Electrodes | EEG signal quality matched conventional wet electrodes without using conductive gel [73]. | For EMG: Achieved significantly higher signal-to-noise ratios than conventional electrodes [73]. | Evaluation: Somatosensory evoked potentials (EEG) & force-matching task (EMG) [73]. |
Table 2: Usability and Practical Application Factors
Table 2 compares critical usability factors that impact long-term research protocols.
| Feature | Conventional Scalp-EEG | Novel Wireless Wearables (e.g., REMI, Dry Electrodes) | Impact on Long-Term Research |
|---|---|---|---|
| Patient Comfort & Acceptance | Confinement to bed for 3-7 days; reports of privacy violation, boredom, and anxiety [74]. | 69% of participants rated REMI sensors as comfortable; high wearability for everyday use [70] [71]. | Higher patient compliance and reduced dropout rates in extended studies. Enables data collection in authentic environments. |
| Setup Time & Operational Complexity | Labor-intensive; requires skin abrasion, conductive gel, and trained technicians [74] [73]. | Dry electrode average setup: ~4 minutes (vs. ~6.4 mins for wet systems) [74]. Microneedle electrodes offer faster cleanup [73]. | Increases throughput and reduces operational costs. Facilitates more frequent or patient-led setup for remote monitoring. |
| Mobility & Ecological Validity | Restricted to controlled lab settings (e.g., Faraday cages); minimal movement allowed [74]. | Ambulatory monitoring in "any environment" [70]; enables capture of neural activity during natural behaviors [74]. | Revolutionizes research into brain function during sleep, social interaction, and physical activity, providing more applicable data. |
| Spatial Resolution & Electrode Coverage | High-density electrode coverage is standard [70]. | Limited electrode coverage compared to conventional systems [70]. | A key trade-off. May be insufficient for research requiring precise source localization, but adequate for many seizure or sleep monitoring applications. |
Detailed Experimental Protocols & Methodologies
To critically assess the data in the comparison tables, an understanding of the underlying experimental methods is essential. The following protocols are representative of recent rigorous validation studies.
Protocol 1: Simultaneous Recording for Signal Validation
This methodology, used to validate the REMI sensor and other devices, directly compares the wearable system against a conventional benchmark in real-time [70] [71].
- Objective: To quantitatively compare the signal characteristics and quality of a novel wireless EEG sensor with a conventional scalp-EEG recording system.
- Cohorts: The study typically involves two cohorts: 1) clinical patients (e.g., undergoing routine epilepsy seizure monitoring) and 2) healthy volunteers (to induce and record common EEG artifacts through specific tasks) [70].
- Data Acquisition: EEG data are recorded simultaneously from the wearable sensors (e.g., REMI) and the conventional EEG system. This simultaneous recording is critical for a direct, sample-for-sample comparison, eliminating confounding variables related to state changes in neural activity [70] [71].
- Comparative Analysis:
- Time-Based Analysis: Expert reviewers visually compare the temporal dynamics and signal morphology of specific events (e.g., seizure onset, eye-blink artifacts) between the two systems [70].
- Spectral-Based Analysis: The power spectral density of signals from both systems is calculated and compared. A high spectral correlation coefficient (e.g., 0.86-0.94) is a key metric of fidelity [70] [71].
- Usability Assessment: Patient-reported outcomes are collected through structured surveys or interviews, focusing on comfort, perceived obstruction, and overall wearability over the recording period [70].
Protocol 2: Spectral Characteristic Validation of Consumer Devices
This protocol, outlined in a recent Sensors journal article, is designed to benchmark consumer-grade devices against a high-fidelity research system [72].
- Objective: To validate and compare the spectral characteristics of signals from low-density wearable, dry-electrode systems against a state-of-the-art research-grade amplifier.
- Participants: Healthy volunteers (e.g., n=19) with no history of neurological disease. Strict pre-experiment instructions are given regarding sleep, alcohol, caffeine, and hair products to minimize extraneous physiological noise [72].
- Device Montage and Mirroring: The research-grade system (e.g., Brain Products ActiChamp Plus) is set up in "mirroring montages" where its electrodes are placed in positions that correspond as closely as possible to the fixed positions of the consumer wearable electrodes (e.g., PSBD Headband, Muse) [72]. This controls for the spatial variability of EEG signals.
- Recording Paradigm: A resting-state protocol is commonly used, comprising 3-minute blocks with eyes closed and eyes open. This paradigm is ideal for eliciting well-established neural oscillations like the Berger effect (alpha rhythm suppression upon eye opening) [72].
- Data Processing & Analysis:
- Preprocessing: Data is filtered (e.g., 0.5-40 Hz bandpass FIR filter) and resampled to a common frequency.
- Spectral Power Calculation: The mean power within standard frequency bands (delta, theta, alpha, beta, gamma) is computed for each device and condition.
- Statistical Comparison: The power spectral densities and band power values from the consumer devices are statistically compared to those from the research-grade system to determine the degree of alignment [72].
Visualizing the Signaling Pathway & Experimental Workflow
Signaling Pathway for a Wireless Neural Interface
The diagram below illustrates the core signal acquisition and processing pathway in a modern, high-density wireless neural interface, highlighting the technical challenges addressed in the reviewed studies.
Experimental Protocol for Device Validation
This workflow outlines the standard methodology for validating a novel wearable device against a conventional system, as described in the experimental protocols.
The Scientist's Toolkit: Key Research Reagents & Materials
For researchers aiming to replicate these validation studies or integrate these technologies into their workflow, the following table details essential hardware and methodological components.
Table 3: Essential Materials for Wireless Neural Recording Research
| Item / Solution | Function / Rationale | Example Products / Notes |
|---|---|---|
| Research-Grade EEG Amplifier | Serves as the gold-standard reference system for validating the signal quality of novel wearable devices. | Brain Products ActiChamp Plus [72] |
| Validated Wireless Wearables | Device Under Test (DUT). Enables ambulatory, long-term neural recording outside the lab. | REMI Sensor [70], Zeto WR-19 [75] |
| Consumer-Grade Wearables | DUT for applications prioritizing cost and usability over clinical-grade precision. | PSBD Headband Pro, Muse S Gen 2 [72] |
| Dry / Microneedle Electrodes | Enable rapid setup and gel-free operation, critical for user-led long-term studies and comfort. | PEDOT:PSS-Coated MN Electrodes [73], QUASAR dry electrodes [74] |
| Data Synchronization System | Critical for time-locking data streams from the wearable and conventional system during simultaneous recording to ensure valid comparisons. | Hardware triggers or software timestamps. |
| Standardized Provocation Protocol | A set of tasks to elicit well-defined neural responses or artifacts for objective signal comparison. | Resting state (eyes open/closed) for Berger effect [72], hyperventilation, photic stimulation. |
| Spectral Analysis Software | For quantitative computation of signal power across frequency bands (Delta, Theta, Alpha, Beta, Gamma) and correlation analysis. | MATLAB Toolboxes, MNE Python [72], BrainVision Analyzer. |
| Patient-Reported Outcome Measures | Standardized questionnaires to quantitatively assess usability factors like comfort, ease of use, and skin irritation. | Likert-scale surveys on comfort and wearability [70]. |
The empirical data confirms that novel wireless wearables have reached a level of maturity where they are viable for many research applications, demonstrating strong agreement with conventional systems in capturing key electrophysiological events. The choice between systems is no longer a simple question of superiority but a strategic decision based on research priorities. For maximal signal fidelity and spatial resolution in a controlled environment, conventional EEG remains the benchmark. However, for studies where ecological validity, patient comfort, and long-term ambulatory monitoring are paramount, wireless wearables offer a compelling and scientifically robust alternative. As technologies like dry electrodes and advanced signal processing continue to evolve, the gap in performance is likely to narrow further, solidifying the role of wearables in the future of neural recording research and therapeutic development.
In the field of neural engineering, the long-term stability and performance of implanted electrodes are critical for achieving high-fidelity neural recordings and effective neuromodulation. Signal fidelity in chronic neural recordings is heavily dependent on the electrochemical properties at the electrode-tissue interface, which evolves significantly post-implantation due to biological responses [17]. This guide provides a standardized framework for benchmarking the key electrochemical parameters—impedance, charge injection capacity (CIC), and stability—of neural electrodes, enabling direct comparison between emerging and established technologies. The objective data and protocols presented here are designed to assist researchers in selecting appropriate electrode materials and designs for specific neural interface applications, ultimately contributing to more reliable and long-lasting brain-computer interfaces and therapeutic neurostimulation devices.
The formation of glial scars and chronic inflammatory responses to implanted electrodes creates an insulating layer that increases impedance and attenuates neural signals over time [17]. Therefore, a comprehensive electrochemical characterization must evaluate not only initial performance but also longitudinal stability under conditions mimicking the implant environment. This guide synthesizes current methodologies and performance data for a range of electrode materials, with a particular emphasis on their behavior in chronic neural recording applications.
Electrochemical Performance Metrics and Comparative Data
Key Performance Indicators for Neural Electrodes
Three primary electrochemical metrics are essential for evaluating neural electrode performance: impedance (particularly at 1 kHz, relevant for neural signal recording), charge storage capacity (CSC), and charge injection capacity (CIC). Low impedance at 1 kHz is crucial for recording high-quality neural signals, as it minimizes signal attenuation and improves the signal-to-noise ratio for action potential detection [56]. CSC, typically measured via cyclic voltammetry (CV), represents the total charge available at the electrode-electrolyte interface, while CIC, determined from voltage transient (VT) measurements during current-controlled stimulation, indicates the maximum reversible charge that can be safely injected without causing tissue damage or electrode corrosion [76].
Quantitative Performance Comparison of Electrode Materials
Table 1: Electrochemical performance metrics of various electrode materials for neural interfaces
| Electrode Material | Geometric Surface Area (μm²) | 1 kHz Impedance (kΩ) | Charge Storage Capacity (CSC) (mC/cm²) | Charge Injection Capacity (CIC) (mC/cm²) | Stability Duration (Weeks) | Key Applications |
|---|---|---|---|---|---|---|
| Sputtered RuOx [56] | 200 | 680-1060 | 20.1-24.3 (at 50 mV/s) | Information Missing | 6 | Motor cortex recording, neural signal detection |
| Sputtered Pt [76] | 1963 (0.1963 mm²) | Information Missing | Information Missing | 0.35-0.45 (at 400 μs pulse width) | Information Missing | Functional electrostimulation, epimysial implants |
| Microporous Pt (Cuff) [76] | 13000 (1.3 mm²) | Information Missing | Information Missing | ~0.15 (at 400 μs pulse width) | Information Missing | Peripheral nerve stimulation and recording |
| Graphene [76] | 7854 (0.7854 mm²) | Information Missing | Information Missing | Performance comparable to sputtered Pt | Information Missing | Advanced stimulation electrodes, emerging technology |
| Platinum (Cochlear Implant) [77] | 3900-4400 (0.39-0.44 mm²) | Significant changes post-polarization | Strong variation after activation | Information Missing | 48 days (in vivo) | Cochlear implants, auditory prostheses |
Table 2: Impact of electrode geometric variables on charge injection capacity (CIC) [76]
| Variable | Impact on CIC | Experimental Conditions |
|---|---|---|
| Pulse Width | CIC increases with wider pulse widths | 50 Hz balanced symmetric biphasic excitation |
| Electrode Size | Complex relationship; not directly proportional to GSA | Microelectrodes with diameters from 0.05 cm to 0.2 cm |
| Roughness Factor | Higher roughness (microporous Pt) increases CIC | Comparison of sputtered Pt vs. microporous Pt |
| Solution Composition | Varies between saline and in vivo environments | In vitro vs. in vivo testing conditions |
| Long-term Behavior | CIC changes post-implantation due to tissue encapsulation | Acute vs. chronic implantation scenarios |
Performance Analysis and Material Selection Guidance
The data reveal that sputtered RuOx electrodes demonstrate excellent impedance characteristics and stability over 6-week implantation periods, making them suitable for chronic neural recording applications [56]. The 1 kHz impedance of RuOx electrodes decreased from 1.06 MΩ to 0.68 MΩ over 6 weeks in rat motor cortex, indicating stable integration with neural tissue. Materials with high surface roughness, such as microporous platinum, offer enhanced CIC due to their increased effective surface area, making them advantageous for stimulation applications where higher charge delivery is required [76].
The geometric surface area of electrodes plays a complex role in CIC, with smaller electrodes typically exhibiting higher charge density capabilities but lower total charge injection. Recent advances in graphene-based electrodes show promising CIC performance comparable to sputtered platinum, suggesting potential for future high-density neural interfaces [76]. Researchers should note that in vitro electrochemical measurements often poorly predict in vivo performance, particularly immediately after implantation, due to the dynamic tissue response and protein fouling effects [77].
Standardized Experimental Protocols for Electrode Benchmarking
Electrochemical Impedance Spectroscopy (EIS) Protocol
Purpose: To characterize the impedance profile of electrodes across frequencies relevant to neural signals (1 Hz for local field potentials, 1 kHz for single-unit activity) [56].
Equipment Setup:
- Use a potentiostat (Gamry Reference 600 or equivalent) with a three-electrode configuration
- Employ a Ag/AgCl reference electrode and platinum counter electrode for in vitro testing
- For in vivo measurements, use a stainless steel needle counter electrode and chloridized silver reference
Measurement Parameters:
- Frequency range: 1 Hz to 100 kHz (10 points per decade)
- Applied voltage: 10 mV RMS sinusoidal signal centered at open circuit potential
- Key measurement frequencies: 1 Hz, 1 kHz, and 30 kHz
- Environment: Inorganic model of interstitial fluid (in vitro) or direct in vivo measurement
Data Interpretation: Focus on impedance magnitude at 1 kHz for neural recording applications. Monitor changes in low-frequency impedance (1 Hz) which is more dependent on electrode properties and often shows stronger correlation between in vitro and in vivo measurements after electrode activation [77].
Cyclic Voltammetry (CV) for Charge Storage Capacity
Purpose: To determine the charge storage capacity (CSC) of electrode materials, indicating their charge retention capability at the electrode-electrolyte interface.
Equipment Setup:
- Similar three-electrode configuration as EIS measurements
- Potentiostat with CV capability
Measurement Parameters:
- Potential range: -0.6 V to +0.6 V vs. Ag/AgCl (for RuOx) [56]
- Scan rates: 50 mV/s and 50,000 mV/s (to evaluate rate capability)
- Single cyclic voltammogram starting and ending at 0 V
Calculation Method:
- CSC is calculated by integrating the cathodic current over a single CV cycle
- Formula: CSCc = ∫|I cathodic| dt / (scan rate × geometric area)
- Report values in mC/cm² for standardized comparison
Data Interpretation: Higher CSC values generally indicate better charge transfer capabilities. Consistency in CSC measurements over multiple cycles and time points indicates electrode stability.
Voltage Transient Measurements for Charge Injection Capacity
Purpose: To determine the maximum reversible charge injection capacity (CIC) of electrodes, critical for safe stimulation parameters.
Equipment Setup:
- Three-electrode configuration with current-controlled stimulation
- Oscilloscope or potentiostat with transient recording capability
Measurement Parameters:
- Stimulation waveform: Balanced, symmetric, biphasic current pulses
- Pulse width: 100-400 μs (clinically relevant range)
- Frequency: 50 Hz stimulation train
- Current amplitude: Varied to determine maximum reversible limits
Calculation Method:
- CIC is determined from voltage transient measurements during current-controlled stimulation
- The maximum CIC is identified where the electrode potential does not exceed the water window (-0.6 V to +0.8 V vs. Ag/AgCl)
- Formula: CIC = I × PW / A, where I is current, PW is pulse width, and A is geometric area
Data Interpretation: The CIC represents the safe charge injection limit without causing irreversible Faradaic reactions or tissue damage. Materials with higher CIC enable smaller electrodes or higher stimulation intensities.
Signaling Pathways and Experimental Framework
Electrode-Tissue Interface Signaling Dynamics
The electrochemical performance of implanted electrodes is intrinsically linked to the biological signaling pathways activated during the tissue response to implantation. The initial acute inflammatory response begins with mechanical disruption of the blood-brain barrier during insertion, triggering clotting cascades and recruitment of immune cells to the injury site [17]. Over time, this evolves into a chronic inflammatory state characterized by persistent activation of microglia and astrocytes, which release inflammatory cytokines and reactive oxygen species, ultimately leading to the formation of a glial scar that encapsulates the electrode [17].
This biological signaling cascade directly impacts electrochemical performance through several mechanisms. The formation of a fibrous glial sheath creates a physical barrier that increases the distance between neurons and recording sites, leading to increased impedance and signal attenuation [17]. Additionally, the release of reactive oxygen species at the electrode-tissue interface can accelerate electrode corrosion and degradation, particularly for non-noble metals, further compromising long-term performance.
Equivalent Circuit Modeling of Electrode-Electrolyte Interface
Purpose: To develop quantitative models that correlate electrochemical parameters with biological responses for predictive performance assessment.
Common Model Elements:
- Solution resistance (Râ‚›): Represents electrolyte resistance between working and reference electrodes
- Charge transfer resistance (Rₛₜ): Represents resistance to electron transfer across the interface
- Double-layer capacitance (Cₛₗ): Represents the ionic capacitance at the electrode-electrolyte interface
- Warburg element (W): Represents diffusion-controlled processes
Application to Neural Electrodes: The evolution of equivalent circuit parameters over time provides insights into the biological integration of implanted electrodes. An increasing Rₛₜ often indicates surface passivation or protein fouling, while changes in Cₛₗ may reflect alterations in the effective surface area due to tissue encapsulation [77]. Recent approaches incorporate constant phase elements (CPE) to account for surface inhomogeneity and diffusion effects in porous electrode coatings.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential research reagents and equipment for electrode electrochemical characterization
| Category | Specific Product/Model | Key Function | Application Context |
|---|---|---|---|
| Potentiostat/Galvanostat | Gamry Reference 600 [56] | Precisely controls and measures electrochemical parameters | Standard equipment for EIS, CV, and voltage transient measurements |
| Reference Electrode | Ag/AgCl (3 M KCl) [77] | Provides stable reference potential for 3-electrode measurements | Essential for in vitro electrochemical characterization |
| Bio-relevant Electrolyte | Model Interstitial Fluid (mISF) [56] | Mimics ionic composition of cerebral environment | In vitro testing closer to physiological conditions |
| Electrode Materials | Sputtered RuOx [56] | Low-impedance coating for neural interfaces | Chronic recording electrodes with stable performance |
| Electrode Materials | Microporous Platinum [76] | High surface area coating for enhanced charge injection | Stimulation electrodes requiring high CIC |
| Electrode Materials | Graphene-based electrodes [76] | Emerging material with favorable electrochemical properties | Next-generation high-density neural interfaces |
| Simulation Software | ZView (Scribner) [77] | Equivalent circuit modeling of impedance data | Quantitative analysis of EIS spectra |
| Sterilization Equipment | Steam autoclave [77] | Ensures sterility of implants before surgical procedures | Pre-implantation processing for in vivo studies |
This comparison guide provides a comprehensive framework for evaluating the electrochemical performance of neural electrodes, with standardized protocols and quantitative benchmarks for direct comparison between different materials and designs. The data reveal that sputtered RuOx electrodes offer excellent impedance characteristics and stability for chronic recording applications, while microporous platinum and graphene-based electrodes show promise for stimulation applications requiring high charge injection capacity.
A critical finding across multiple studies is that initial in vitro measurements often poorly predict in vivo performance, particularly immediately after implantation [77]. Researchers should therefore prioritize longitudinal assessment of electrochemical parameters under conditions that closely mimic the target environment. Additionally, the strong dependence of CIC on stimulation parameters (particularly pulse width) underscores the need for standardized reporting conditions to enable meaningful cross-study comparisons.
As the field advances toward higher-density neural interfaces and chronic implantation periods, the standardized benchmarking approaches outlined in this guide will be essential for developing reliable, high-performance neural recording and stimulation technologies. Future work should focus on establishing correlations between electrochemical parameters and specific biological responses to further optimize electrode-tissue integration.
The advancement of neural recording technologies is pivotal for both clinical neurology and neuroscience research. The overarching thesis of this field contends that high signal fidelity in long-term neural recording is the cornerstone for generating reliable, actionable data. However, fidelity is not solely determined by the recording hardware; it is intrinsically linked to the usability of the technology from both patient and researcher perspectives. Devices that are uncomfortable or difficult to integrate into clinical and research workflows can lead to poor patient compliance, increased artifacts, and ultimately, data that does not accurately reflect true neural activity. This guide objectively compares the current landscape of wearable neural interfaces, focusing on how their design, comfort, and integration capabilities directly impact their performance and practical application in long-term studies.
Usability and Signal Quality in Wearable Neural Recording Devices
Usability—encompassing comfort, wearability, and ease of use—is a critical determinant in the success of long-term neural recording studies. A device that is uncomfortable will not be worn consistently, leading to fragmented data. A system that is challenging for researchers to set up or integrate into existing workflows is prone to operator error and is less likely to be adopted. The following section compares several wearable electroencephalography (EEG) devices, highlighting the direct relationship between their usability characteristics and their recorded signal quality.
Table 1: Comparison of Wearable EEG Devices for Remote Monitoring
| Device Name / Type | Key Usability Features | Reported Patient Comfort / Acceptance | Comparison to Clinical-Grade EEG | Primary Research/Clinical Applications |
|---|---|---|---|---|
| REMI Sensor [70] | Wireless, designed for extended at-home use. | 69% of participants rated it as comfortable. | High spectral correlation (0.86–0.94); similar seizure/artifact morphology. | Extended-duration epilepsy monitoring. |
| Behind-the-Ear EEG (e.g., Sensor Dot) [78] | Unobtrusive, two-channel wearable. | High acceptance due to minimal visibility and comfort. | Accurate detection of typical absence seizures; signals highly similar to scalp EEG. | Seizure detection, continuous monitoring in epilepsy. |
| Commercial Headsets (e.g., Muse, Emotiv EPOC+) [79] | Dry electrodes, wireless, consumer-grade usability. | Better usability and wearing comfort than traditional EEG. | Moderate to substantial agreement overall with clinical EEG systems. | Mental health, sleep studies, neurological disorder monitoring. |
| Subcutaneous EEG [78] | Minimally invasive, implanted under the skin. | High-quality signal for ultra-long-term recording. | High similarity to proximate scalp electrodes in temporal lobe epilepsy. | Ultra-long-term recording where surface EEG is insufficient. |
The data from these studies consistently demonstrates that usability-focused design does not necessitate a compromise in signal quality. For instance, the REMI sensor, designed for patient comfort during extended wear, achieved a high spectral correlation of 0.86 to 0.94 when compared to conventional scalp-EEG systems [70]. This indicates that high-fidelity data suitable for both time and frequency domain analysis can be captured outside the clinical setting. Similarly, behind-the-ear devices have shown strong performance in detecting specific neurological events, such as typical absence seizures, while being largely invisible to the user, thereby promoting compliance and reducing stigma [78].
The trade-off for improved usability is often a reduction in electrode coverage compared to full clinical montages [79] [70]. While this can limit the spatial resolution for source localization, the consensus from recent literature is that for many applications—such as monitoring known biomarkers, detecting seizure activity, or tracking sleep patterns—the data provided by these focused, user-friendly devices are sufficiently robust and clinically valuable [79].
Experimental Protocols for Validating Usability and Signal Fidelity
To generate the comparative data presented in this guide, researchers employ rigorous experimental protocols. These protocols typically involve simultaneous recording with the wearable device and a gold-standard clinical system, followed by quantitative and qualitative analysis.
Protocol for Signal Quality Validation
Aim: To quantitatively compare the signal fidelity of a wearable EEG device (Device Under Test, DUT) against a conventional clinical EEG system.
- Participant Cohorts: Recruit two cohorts: (a) patients with a known neurological condition (e.g., epilepsy) and (b) healthy volunteers.
- Simultaneous Recording: Place the DUT (e.g., REMI sensor, behind-the-ear device) on the participant. Conduct a simultaneous recording session using both the DUT and a conventional clinical EEG system according to standard 10-20 placement.
- Event Induction (in healthy volunteers): Instruct healthy volunteers to perform tasks that induce common EEG artifacts (e.g., eye blinks, jaw clenching) and produce physiological signals (e.g., alpha rhythms via eye closure).
- Data Analysis:
- Temporal & Morphological Analysis: Experts visually compare the timing and morphological characteristics of physiological and artifactual events (e.g., epileptic seizures, eye blinks) between the two systems [70].
- Spectral Correlation: Calculate the correlation coefficient between the power spectral densities of simultaneous recordings from the DUT and the clinical system across standard frequency bands (e.g., delta, theta, alpha, beta) [70].
- Spike Detection & Assignment (for high-density arrays): For neural interfaces with high channel counts, assess the impact of data compression on the ability to correctly detect neural spikes and assign them to their correct source of origin [80].
Protocol for Usability and Comfort Assessment
Aim: To evaluate the patient-facing usability factors of a wearable neural device.
- Study Design: Implement a structured study where participants use the device in a controlled or at-home setting for a defined period.
- Data Collection:
- Questionnaires: Administer standardized or study-specific questionnaires post-trial. These often use Likert scales to quantitatively assess perceived comfort, ease of use, and overall satisfaction [81] [70] [82]. For example, participants may be asked to rate statements like "The device was comfortable to wear" on a scale from 1 (strongly disagree) to 5 (strongly agree).
- Interviews: Conduct semi-structured interviews with a subset of participants to gather qualitative feedback on wearability, any physical discomfort, and suggestions for improvement [81].
- Compliance Metrics: For at-home studies, objectively measure compliance through device-logged data on actual usage time versus prescribed usage time.
Table 2: Key Research Reagent Solutions for Wearable Neural Interface Studies
| Item Category | Specific Examples | Function in Research & Development |
|---|---|---|
| Conductive Hydrogels | Alginate-, chitosan-, or polyacrylamide-based hydrogels [83] | Serve as a biocompatible interface between the skin and electrode; reduce interfacial impedance, improving signal quality and comfort. |
| Flexible Substrates | Polyimide, silicone elastomers [83] | Form the base of the wearable device, allowing it to conform to the shape of the head or body for stable, long-term recording. |
| Reference EEG Systems | Clinical-grade scalp-EEG systems (e.g., Neurofax, BrainVision) [70] | Act as the gold-standard equipment for simultaneous recording to validate the signal quality of new wearable devices. |
| Data Compression Algorithms | Wired-OR architecture, LZ77-based lossless compression (gzip) [80] | Manage the immense data flow from high-channel-count neural interfaces, enabling transmission within power budgets of implantable devices. |
| Standardized Usability Metrics | System Usability Scale (SUS), custom Likert-scale questionnaires [81] | Provide quantitative and qualitative frameworks for consistently evaluating the comfort and acceptability of devices across studies. |
The Critical Role of Hydrogel Interfaces in Usability and Fidelity
A key technological advancement driving improvements in both signal fidelity and wearability is the development of advanced hydrogel materials for the electrode-skin interface. The properties of these hydrogels directly address several core challenges in long-term neural recording.
- Biocompatibility and Comfort: Hydrogels are hydrophilic polymer networks with high water content, making them soft, flexible, and similar to natural tissue. This inherent biocompatibility minimizes skin irritation and allergic reactions, which is a prerequisite for prolonged wear [83]. Their soft and compliant nature ensures a gentle interface with the skin, significantly enhancing user comfort.
- Low Interfacial Impedance: Impedance at the electrode-skin interface is a major determinant of signal quality. High impedance weakens biological signals and increases susceptibility to noise. Hydrogels exhibit low interfacial impedance, which strengthens the captured signal and improves the signal-to-noise ratio (SNR) [83]. This property is crucial for detecting low-amplitude neural signals.
- Adhesion and Conformability: Hydrogels can be engineered with adhesive properties, allowing them to form a stable and gap-free connection with the skin. This is often achieved by creating ultrathin hydrogel films (e.g., 10 µm thick) that can conform to the microscopic texture of the skin, eliminating air gaps that degrade signal quality and lead to motion artifacts [83].
The relationship between these material properties and the overall research outcomes can be visualized as a logical pathway.
Integration into Broader Clinical and Research Workflows
The ultimate value of a wearable neural device is realized only when it is successfully integrated into a larger ecosystem. This involves not just the patient, but also the clinical or research team and the data infrastructure. The ROCKET (Records of Computed Knowledge Expressed by neural nets) system exemplifies a framework designed for this purpose, enabling the review and integration of AI algorithm results into the radiologist's clinical workflow with minimal disruption [84]. The principles of such systems are equally applicable to the review of data from wearable neural recorders.
A critical challenge in this domain is managing the data deluge from high-channel-count neural interfaces. Here, compression technologies like the wired-OR architecture play a vital role. This approach employs lossy compression at the analog-to-digital interface, achieving compression ratios of 50x or higher while still correctly detecting and assigning over 80% of spikes, thus making long-term, high-density recording feasible within implantable power constraints [80].
The evaluation of wearable neural recording devices must extend beyond traditional metrics of signal accuracy to include a rigorous assessment of usability and workflow integration. As comparative data shows, modern devices like the REMI sensor and various behind-the-ear EEG systems successfully balance patient comfort with high signal fidelity, as validated against clinical gold standards. The development of advanced materials like hydrogels is key to this progress, directly enhancing both signal quality and wearability. For researchers and clinicians, selecting a device requires a holistic view that considers the experimental question, the required signal specificity, and the practical realities of long-term use. Prioritizing usability is not a concession—it is a fundamental requirement for generating the high-quality, real-world neural data that will drive future discoveries in neuroscience and neurology.
Conclusion
The pursuit of long-term neural signal fidelity is witnessing a transformative shift, moving beyond simple electrical recording to the creation of truly biointegrated interfaces. Key takeaways from recent research highlight the non-negotiable need for mechanical compliance, achieved through ultra-flexible substrates, and biochemical compatibility, enabled by innovative coatings like the TAB layer that actively resist fouling while promoting neural integration. Furthermore, resolving the data bottleneck through sophisticated on-implant processing and mitigating hidden artifacts like crosstalk are now recognized as critical as the electrode design itself. The successful demonstration of devices maintaining single-unit recording fidelity for over a year in animal models marks a pivotal milestone. The future direction points toward closed-loop, multifunctional systems that seamlessly combine high-density recording with precise stimulation and therapeutic delivery, all while operating within a minimal power budget. For researchers and drug development professionals, these advances promise not only more reliable tools for basic neuroscience but also a tangible path toward effective long-term neurotherapeutics and robust brain-computer interfaces for clinical application.
References
- 1. FOREIGN BODY REACTION TO BIOMATERIALS - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2327202/]
- 2. Chronically Implanted Intracranial Electrodes: Tissue ... [https://www.mdpi.com/2072-666X/9/9/430]
- 3. Engineering strategies towards overcoming bleeding and glial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8975777/]
- 4. The density difference between tissue and neural probes is ... [https://www.nature.com/articles/srep02942]
- 5. Data-driven model comparing the effects of glial scarring ... [https://pubmed.ncbi.nlm.nih.gov/26655972/]
- 6. Real-time, neural signal processing for high-density brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12275325/]
- 7. Advances in large-scale electrophysiology with high-density ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394932/]
- 8. Neural spike compression through salient sample ... [https://www.nature.com/articles/s44172-025-00504-4]
- 9. Non-Linear Modeling and Precision Analysis Approach for ... [https://pubmed.ncbi.nlm.nih.gov/?term=62176232%2C62336007%2FNational+Natural+Science+Foundation+of+China%5BGrants+and+Funding%5D&sort=date&sort_order=desc]
- 10. Bioadaptive liquid-infused multifunctional fibers for long- ... [https://pubmed.ncbi.nlm.nih.gov/40929275/]
- 11. Minimally invasive implantation of scalable high-density ... [https://www.nature.com/articles/s41551-025-01501-w]
- 12. Six Connectivity and Telecom Trends to Watch for in 2025 [https://standards.ieee.org/beyond-standards/2025-connectivity-telecom-trends/]
- 13. Tissue Response to Neural Implants: The Use of Model ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2019.00689/full]
- 14. Mechanically-Compliant Intracortical Implants Reduce the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4175058/]
- 15. Revolutionizing brain‒computer interfaces - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243264/]
- 16. Ultraflexible Neural Electrodes for Long-Lasting Intracortical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7398974/]
- 17. Long-term stability strategies of deep brain flexible neural ... [https://www.nature.com/articles/s41528-025-00410-x]
- 18. Mechanical failure modes of chronically implanted planar ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4312222/]
- 19. Bio-inspired electronics: Soft, biohybrid, and “living†neural ... [https://www.nature.com/articles/s41467-025-57016-0]
- 20. Progress and challenges of implantable neural interfaces ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8077843/]
- 21. Engineering aspects and materials for next generation ... [https://www.sciencedirect.com/science/article/pii/S1877117325001279]
- 22. Material and design strategies for chronically-implantable ... [https://www.nature.com/articles/s41427-025-00613-8]
- 23. Mechanically-adaptive, resveratrol-eluting neural probes ... [https://www.nature.com/articles/s41528-025-00440-5]
- 24. Highâ€Precision, Lowâ€Threshold Neuromodulation With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380067/]
- 25. Mechanical Behavior Analysis of Neural Electrode Arrays ... [https://www.mdpi.com/2072-666X/16/9/1010]
- 26. 3D Neural Probes Open New Frontiers in Brain Science and ... [https://tto.dartmouth.edu/news/2025/08/3d-neural-probes-open-new-frontiers-brain-science-and-therapy]
- 27. Bioadaptive liquid-infused multifunctional fibers for long-term ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422202/]
- 28. Biocompatible Coatings Navigating Dynamics ... [https://www.archivemarketresearch.com/reports/biocompatible-coatings-367142]
- 29. Enhancing neural signal fidelity: controlling ... [https://fox40.com/business/press-releases/ein-presswire/794149233/enhancing-neural-signal-fidelity-controlling-ultramicroelectrode-tip-exposure-for-single-cell-recording]
- 30. Biocompatible Coatings - Applications in Biomedical ... [https://hydromer.com/biocompatible-coatings/]
- 31. Multidimensional advances in neural interface technology for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12296523/]
- 32. Controllable tip exposure of ultramicroelectrodes coated by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11754621/]
- 33. Enhancing neural signal fidelity: controlling ultramicroelectrode ... [https://www.counton2.com/business/press-releases/ein-presswire/794149233/enhancing-neural-signal-fidelity-controlling-ultramicroelectrode-tip-exposure-for-single-cell-recording/]
- 34. controlling ultramicroelectrode tip exposure for single-cell ... [https://www.eurekalert.org/news-releases/1076457]
- 35. A flexible neural implant with ultrathin substrate for low- ... [https://www.nature.com/articles/s41378-022-00464-1]
- 36. Manufacturing Processes of Implantable Microelectrode Array ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10583290/]
- 37. In situ self-referenced intracellular two-electrode system for ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566324001787]
- 38. Implantable intracortical microelectrodes: reviewing the ... [https://www.nature.com/articles/s41378-022-00451-6]
- 39. 68-channel neural signal processing system-on-chip with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11541109/]
- 40. Event-based Neural Spike Detection Using ... [https://arxiv.org/html/2505.06544v1]
- 41. An Implantable Wireless Neural Interface for Recording ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3638022/]
- 42. Advances in bioelectronics for neural interfacing [https://link.springer.com/article/10.1557/s43579-025-00822-w]
- 43. Monolithic multimodal neural probes for sustained stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467050/]
- 44. In-vivo integration of soft neural probes through high- ... [https://www.nature.com/articles/s41467-024-45768-0]
- 45. Through-polymer, via technology-enabled, flexible, ... [https://www.nature.com/articles/s41378-024-00691-8]
- 46. 3D-printed optogenetic neural probe integrated with ... [https://www.nature.com/articles/s41598-025-13654-4]
- 47. Bridging circuit modeling and signal analysis to understand the risk of crosstalk contamination in brain recordings | Nature Communications [https://www.nature.com/articles/s41467-025-59391-0]
- 48. High-resolution neural recordings improve the accuracy of ... [https://www.nature.com/articles/s41467-023-42555-1]
- 49. A Modular Implementation to Handle and Benchmark Drift ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10897502/]
- 50. A Lubricated Nonimmunogenic Neural Probe for Acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8336494/]
- 51. Ultrasoft microwire neural electrodes improve chronic ... [https://www.sciencedirect.com/science/article/abs/pii/S1742706117301162]
- 52. Slow insertion of silicon probes improves the quality of ... [https://www.nature.com/articles/s41598-018-36816-z]
- 53. Advances in Evaluation of Electrode Insertion Trauma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11456118/]
- 54. Spatiotemporal pH dynamics following insertion of neural ... [https://www.sciencedirect.com/science/article/abs/pii/S0165027006004717]
- 55. Human cochlear microstructures at risk of electrode ... [https://www.nature.com/articles/s41598-023-29401-6]
- 56. Electrochemical stability and neural recording with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278477/]
- 57. Multifunctional poly (lactic acid)/vanillin coatings on drug ... [https://www.nature.com/articles/s41598-025-99983-w]
- 58. Surface and in vitro corrosion properties of spark plasma ... [https://www.nature.com/articles/s41598-025-16657-3]
- 59. Advances in large-scale electrophysiology with high-density ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00058k]
- 60. Real-time, neural signal processing for high-density brain ... [https://pubmed.ncbi.nlm.nih.gov/40682086/]
- 61. A Framework for Compressive On-chip Action Potential ... [https://pubmed.ncbi.nlm.nih.gov/41021967/]
- 62. Neural implant smaller than salt grain wirelessly tracks brain [https://news.cornell.edu/stories/2025/11/neural-implant-smaller-salt-grain-wirelessly-tracks-brain]
- 63. A subnanolitre tetherless optoelectronic microsystem for ... [https://www.nature.com/articles/s41928-025-01484-1]
- 64. Enhancing neural signal fidelity: controlling ... [https://fox59.com/business/press-releases/ein-presswire/794149233/enhancing-neural-signal-fidelity-controlling-ultramicroelectrode-tip-exposure-for-single-cell-recording/]
- 65. Sustainable power solutions for next-generation medical ... [https://www.sciencedirect.com/science/article/pii/S2590006425006258]
- 66. Concurrent behavioral and electrophysiological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9891465/]
- 67. The sinusoidal probe: a new approach to improve ... [https://www.frontiersin.org/journals/neuroengineering/articles/10.3389/fneng.2014.00010/full]
- 68. The top BCI stories of 2025 so far [https://www.massdevice.com/top-bci-stories-2025-so-far/]
- 69. Melatonin improves quality and longevity of chronic neural ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961218305106]
- 70. Comparative analysis of signal quality and usability for a ... [https://www.sciencedirect.com/science/article/pii/S2467981X25000289]
- 71. Comparative analysis of signal quality and usability for a ... [https://pubmed.ncbi.nlm.nih.gov/40703849/]
- 72. Comparison of EEG Signal Spectral Characteristics ... [https://www.mdpi.com/1424-8220/24/24/8108]
- 73. Quantitative Assessment of Signal Quality and Usability ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1706501/full]
- 74. Why Brain Wearables Are Making Traditional EEG Labs ... [https://globalrph.com/2025/10/why-brain-wearables-are-making-traditional-eeg-labs-obsolete-in-2025/]
- 75. Comparative analysis of signal quality and usability for a novel ... [https://www.semanticscholar.org/paper/Comparative-analysis-of-signal-quality-and-for-a-Muvvala-Kazen/d0adcbff647dce36c5c100d153e49a09f60ffc1a]
- 76. PMC Search Update - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6630677/]
- 77. Comparison of the In Vitro and In Vivo Electrochemical ... [https://www.mdpi.com/2072-666X/13/1/103]
- 78. Long-Term Home EEG Recording: Wearable and ... [https://www.semanticscholar.org/paper/Long-Term-Home-EEG-Recording%3A-Wearable-and-Devices-Rehman-Higdon/21593c59fb82e05b9630336ebc46d9285683d402]
- 79. Remote Wearable Neuroimaging Devices for Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11048695/]
- 80. Data Compression Versus Signal Tradeoff in Wired-OR... Fidelity [https://pubmed.ncbi.nlm.nih.gov/37402181/]
- 81. Assessing the usability of wearable devices to measure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8444467/]
- 82. Usability evaluation of a glove-type wearable device for ... [https://www.nature.com/articles/s41598-024-60818-9]
- 83. Hydrogels in wearable neural interfaces | Med-X [https://link.springer.com/article/10.1007/s44258-024-00040-4]
- 84. AI Integration in the Clinical Workflow - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8669074/]